When you inhale and exhale, the air in your lungs and airways may create turbulence called respiratory sounds — also known as “lung sounds” or “breath sounds.” You may know these sounds as “coughing” and “wheezing” but there’s actually a lot more to these sounds than you might initially realize. Breathing sounds are not only used to help diagnose lung conditions like COPD, asthma, and pneumonia but they can be used to assist medical professionals in directing and prescribing medication for these lung diseases.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In the following sections, we’re going to talk about four different types of respiratory sounds, what causes them, how they’re diagnosed, and how they’re treated. After reading, you’ll have a better understanding of the signs your lungs are giving you and what their implications are for your overall health and well-being. And as always, if you have an experience that you would like to share or you have any questions about what you read here, be sure to leave them in the comment section below.
What is the Significance of Respiratory Sounds?
When you visit the doctor with a list of symptoms, your doctor will use any and all tools in his/her toolbox in order to diagnose your condition. For example, your doctor may put you through a series of sleep studies if you report problems getting to sleep, staying asleep, or experiencing restful sleep. A sleep study can reveal exactly when the sleep disruptions are occurring and your doctor will be able to see what your brain activity is like when you sleep. By understanding the root cause of your sleeping problems, your doctor can provide you with treatment options that are tailored just for you.

One of the first methods your doctor will use when diagnosing a condition related to the heart or lungs is called auscultation. During auscultation, medical professionals use a device called a stethoscope in order to listen to the internal sounds of the body including the heart, lungs, and gastrointestinal system.
While auscultation is not the end all be all method for diagnosing lung conditions, it can help medical professionals rule out certain diseases without resorting to more invasive diagnostic methods. Some respiratory sounds like coughing and wheezing can be heard without a medical instrument but using a stethoscope, doctors can identify more subtle sounds that could not be heard otherwise.
Let’s take a look at the different types of lung sounds.
Normal Respiratory Sounds
Normal respiratory sounds are an indication that your respiratory system is healthy and functioning properly. But if you report having respiratory symptoms like chest pain, breathlessness, or chest tightness, your doctor will be able to perform a number of other tests to diagnose them.
CT scans, spirometry tests, pulse oximetry, and the six-minute walk test are just a few of the tests that can be used to diagnose lung disease.

Vesicular
The term “vesicular” is slightly misleading because “vesicle” refers to the alveoli (small air sacs in the lungs) which are responsible for the exchange of oxygen and carbon dioxide between the lungs and bloodstream.
However, the alveoli are not what makes the vesicular sounds. These sounds are soft, rustling, or blowing sounds heard throughout all of the lung fields. They’re heard throughout the duration of inspiration and continuously through one-third of expiration. Vesicular sounds are an indication that you’re able to fully inhale and exhale without obstruction.
Bronchovesicular
Bronchovesicular sounds are muffled but high pitch sounds where the expiratory and inspiratory phase is equal in duration. These sounds are heard over the first and second intercostal spaces (between the ribs) and the interscapular area (shoulder blade).
Bronchial
With bronchial sounds, the expiratory sounds are higher in pitch and intensity. The inspiratory sounds are lower-pitched, hollow, tubular sounds. Bronchial sounds are heard throughout the manubrium (the broad upper part of the sternum).
Tracheal
In tracheal sounds, the expiratory and inspiratory phases are equal in duration. The sound is loud, high-pitched, and heard directly over the trachea, the upper part of your respiratory system.
Abnormal Respiratory Sounds
Rales (Crackles)
Rales, or “crackles” as they’re more commonly called, are the result of fluid buildup in the airways (secretions). Rales are either exudate meaning they’re caused by a lung infection like pneumonia or they are transudate meaning they’re caused by congestive heart failure.
These noises can be heard when the patient inhales because the small airways pop open after collapsing during inhalation. There are three different types of crackles: fine, medium, and coarse.
- Fine crackles often occur during early inspiration and are fainter in volume.
- Medium crackles are more high pitched and they may indicate an interstitial process such as congestive heart failure or pulmonary fibrosis.
-
Coarse crackles last longer than fine or medium crackles and they tend to be louder and lower-pitched. They are most often a sign of excessive fluid on the lungs caused by pneumonia, chronic bronchitis, or pulmonary edema.
Wheezes
Wheezing is a sound that results from air being forced through a partially collapsed airway. When the same volume of air is being pushed through a smaller area, the velocity of the air increases which creates the sound.
Wheezing noises are often very high-pitched and continuous. Your doctor will be able to determine how many airways are obstructed based on whether the sound is monophonic (one sound) or polyphonic (multiple sounds). Expiratory phase wheezing may be connected to bronchiolar disease whereas inspiratory phase wheezing may be connected to tracheal stenosis.
Rhonchi
Rhonchi are similar to wheezing sounds but they are low-pitch and occur more frequently when the patient is exhaling. They can be an indication that the bronchial tubes or “bronchioles” are thickening due to the overproduction of mucus. Bronchioles are the tubes that lead from the trachea down to each lung. Rhonchi may be a sign of bronchitis or COPD.
Pleural Friction Rub
There’s a thin membrane that coats the outside of the lungs and the inside of the chest cavity called the pleura. The pleura secretes a lubricant that allows the chest wall to expand and contract freely. However, if the pleura becomes inflamed or damaged in some way, they will create a rough, scratchy sound that your doctor can pick up with a stethoscope.
This is called a pleural friction rub, or simply pleural rub. Pleurisy, pneumonia, and lung tumors are the most common causes of pleural rub.
Hamman’s Sign
Hamman’s sign (also called mediastinal crunch) is a crunching sound that occurs when there is air trapped in the mediastinum (the space between your lungs). The crunchy, scratchy noise that it causes is in sync with your heartbeat because the movement of your heart is what produces the noise.
In some cases, Hamman’s sign may mean you have a collapsed lung (pneumothorax) especially if it occurs in conjunction with shortness of breath and chest pain. However, it can also be caused by cystic fibrosis, pneumonia, or COPD.
.jpg)
How Are Respiratory Sounds Treated?
The way that respiratory sounds are treated depends entirely on what type of sound is being produced and what is causing them. This is why auscultation alone is usually not sufficient enough to diagnose a lung condition.
If you don’t have a history of respiratory issues, your doctor might perform further tests in order to determine if a chronic condition is the cause of the respiratory sounds. If you have a chronic disease like COPD, however, your doctor might ask you to increase your medication dosage.
-jpg.jpeg)
In COPD patients, the most common cause of breath sounds is mucus and phlegm that get lodged in the airways when you breathe. Clearing this mucus will not only help you breathe better but can also prevent conditions like bronchiectasis.
This is when you experience recurring lung infections due to bacteria that remain in the lungs for too long. Since lung infections are the most common cause of COPD exacerbation, it’s very important that you and your doctor deal with this problem as soon as it arises.
Medication
If your inability to clear the mucus is due to narrowed airways, your doctor may prescribe you something called a bronchodilator. These drugs open up the airways and prevent the “wheezing” noise whenever you try to cough.
Bronchodilators are almost always administered through either an inhaler or a nebulizer because this allows the medication to reach the affected area more quickly in the event of an emergency.

Controlled Coughing
Another method your doctor may recommend for dealing with blocked airways is breathing exercises or controlled coughing exercises. A normal cough is often erratic and solely focused on expelling as much air as possible.
On the other hand, controlled coughing is more focused on using air more effectively. There are several benefits of this. Firstly, it helps prevent breathlessness, fatigue, or something more serious like a hernia. Secondly, controlled coughing helps prevent the airways from closing which prevents mucus and phlegm from escaping. For more information on this, please read through our post titled “How to Cough Correctly with COPD.”

Smoking Cessation
Whether you’ve been smoking for a few days, a few months, or your whole life, there’s no better time to quit than now. Smoking is the number one cause of preventable illness in the world and there’s also a good chance that it’s causing the respiratory sounds that you’ve been experiencing too.
Smoking damages microscopic organelles in your airways called “cilia.” They are responsible for clearing mucus and phlegm out of the lungs and airways in order to prevent breathing obstruction and infection. In other words, the wheezing or crackling noise you hear when breathing could be caused directly by cigarette smoking.
![]()
When Should You Visit a Doctor?
You should visit a doctor any time that you experience unusual symptoms. While COPD is already associated with shortness of breath, if you notice your breathlessness becoming more severe or you notice wheezing or crackling noises in your chest, you should contact your doctor immediately. You can never be “too careful” when it comes to your respiratory health.
As aforementioned, if mucus or phlegm remains in the airways for too long without being cleared, this leaves you at risk of experiencing a lung infection, the number one cause of COPD exacerbation and hospitalization.

Conclusion
Respiratory sounds alone are usually not a cause for concern. Chances are, you’ve had the common cold before and know what it’s like to cough, wheeze, or experience difficulty breathing. However, if these symptoms become more persistent and last more than a few days, you should visit your doctor. By listening to your lungs, your doctor will have a better idea of what’s causing your symptoms and what further tests are needed in order to diagnose you with a respiratory condition.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
If you’ve been prescribed oxygen by your doctor either for temporary or long-term use, don’t hesitate to reach out to our respiratory specialists here at LPT Medical. We offer state-of-the-art portable oxygen concentrators which are much smaller, lighter, and more reliable than compressed or liquid oxygen tanks. We feature all of the top-rated brands including, but not limited to Caire Inc., Inogen, and Respironics. Simply tell us what your wants and needs are and we will provide you with a list of options that we believe will suit your circumstances.
Asthma and COPD are often confused, but they are two very different diseases. Even though they both cause similar respiratory symptoms, they affect the lungs in distinct and different ways.
COPD is an age-related disease that usually affects smokers and people with long-term exposure to toxins that damage their lungs. Asthma, on the other hand, is often inherited and affects children, teens, and adults of all ages.
Understanding the differences between these two respiratory conditions is important for adults who experience chronic respiratory symptoms, especially if they have already been diagnosed with asthma. While asthma and COPD are separate conditions, in some cases, asthma can cause or contribute to COPD.
COPD is one of the most under-diagnosed and commonly mis-diagnosed diseases, so it's important for doctors and patients alike to be knowledgeable about what sets it apart. That's why, in this article, we're going to show you how to recognize and distinguish the differences between asthma and COPD.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Asthma Versus COPD

It is difficult to tell asthma and COPD apart by symptoms alone. Serious symptoms like coughing and difficulty breathing can be caused by asthma, COPD, or a combination of both at the same time.
Here are some of the symptoms that asthma and COPD share:
- Coughing
- Wheezing
- Shortness of breath
- Rapid breathing
- Bronchial spasms
- Chest tightness and discomfort
Despite their similarities, from a medical standpoint, it's vital to be able to tell the two diseases apart. Both asthma and COPD require different medical approaches and respond to different treatments and medications.
Moreover, in some cases, people with asthma are actually more prone to developing COPD later in life. Studies show that about forty percent of people with COPD also have asthma, so it's vital for patients to understand the relationship between the two conditions.
In this next section we're going to help you do just that by explaining the causes and symptoms of asthma and COPD. Next, we'll break down the many differences between asthma and COPD and explain the characteristics that distinguish them from one another.
By the end of this article, you'll have a much better understanding of how the diseases are similar and different and be better able to tell the two conditions apart.
Understanding COPD

COPD can be a difficult disease to understand, partially because it is an umbrella term that encompasses two separate but related conditions: emphysema and chronic bronchitis. Both are chronic, incurable lung conditions, usually caused by smoking.
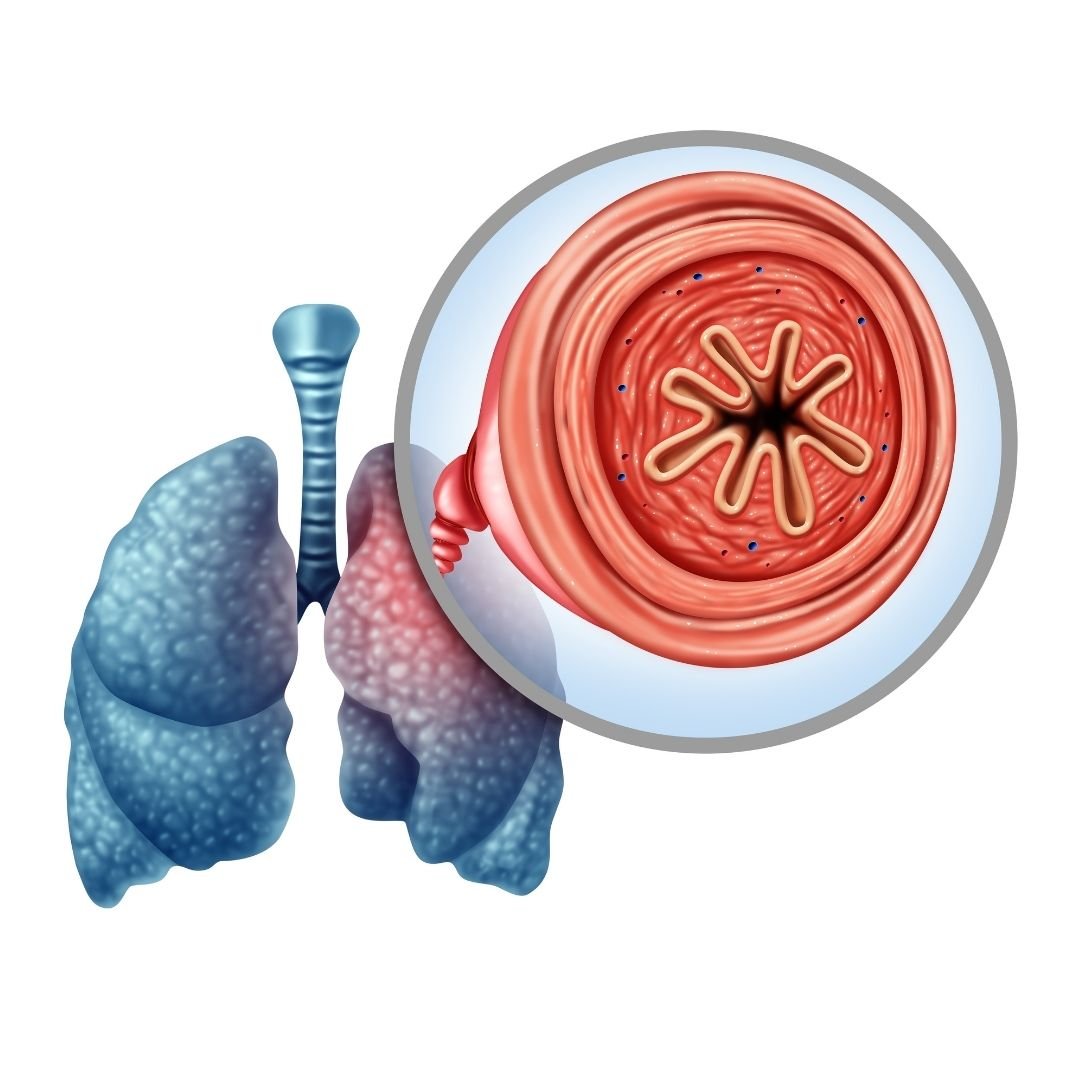
Emphysema occurs when the air sacs (alveoli) in the lungs get damaged, causing lung function decline and over-inflation in the lungs. People with emphysema have difficulty absorbing enough oxygen and pushing all of the air out of their lungs.
Chronic bronchitis occurs when the airways become inflamed, thickened, and narrowed due to inflammation and excess mucus. Most people with COPD have some combination of both emphysema and chronic bronchitis.
Both chronic bronchitis and emphysema cause similar symptoms that get worse and worse over time. While proper treatment and a healthy lifestyle can slow down disease progression, they can't stop COPD from inevitably getting worse.
Over time, COPD leads to more serious complications like pulmonary hypertension, heart failure, respiratory failure, and death. But with a healthy lifestyle and high-quality medical treatment, many people with COPD are able to live and stay active for many years.
Common Symptoms of COPD:
- Coughing
- Wheezing
- Chest Tightness
- Shortness of breath
- Thick or excess mucus
- A chronic cough that produces phlegm (especially in the morning)
- Frequent respiratory illnesses and infections
- Fatigue
- Unintended weight loss
- Swelling in hand, ankles, feet, and legs (edema)
Understanding Asthma
Unlike COPD, which usually shows up later in life, asthma can be inherited and often shows up in early childhood. Most people discover they have asthma after they experience an exacerbation, often in reaction to an allergen or respiratory infection.
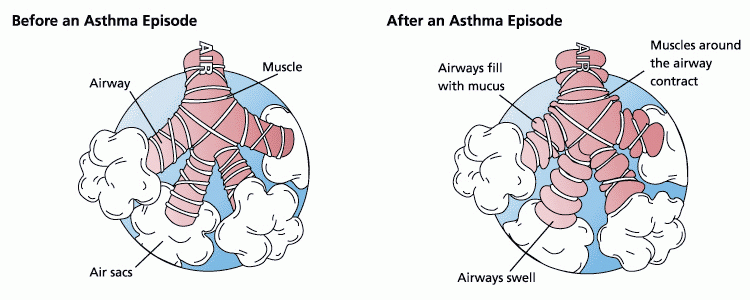
People with asthma don't have symptoms all the time. Asthma symptoms usually only show up in response to an environmental trigger, which is often pollen, smoke, or cold air. Because of this, asthma is often considered to be an allergic disorder.
When someone with asthma is affected by a trigger, it causes the muscles in their lungs and airways to violently constrict in an attempt to keep irritating molecules out. This causes a fit of coughing and wheezing that often requires medication to stop.
Asthma attacks can be life-threatening if not treated quickly. Most of the time, treatment involves inhaling bronchodilators and corticosteroids to control inflammation.
Common Symptoms of Asthma:
- Coughing
- Wheezing
- Shortness of breath
- Chest pain and tightness
- “Asthma attacks” consisting of coughing and wheezing that are worsened by illnesses and allergies
How to Tell Asthma and COPD Apart
Differences in Age of Onset

Many people first start to show symptoms of asthma in early childhood and get diagnosed with the disease at an early age. Some people grow out of their asthma symptoms, but many people continue to have the condition throughout their adult life.
COPD, on the other hand, is an acquired disease that doesn't show up until later in life. It's a result of cumulative damage to the lungs and airways over many years, and is usually diagnosed after the age of forty.
Symptoms are usually mild in the early stages of COPD, but get more and more severe with time. In the later stages of the disease, people with COPD usually exhibit severe respiratory decline and need supplemental oxygen to breathe.
While asthma symptoms might be exacerbated by allergies and other triggers for short periods of time, the symptoms don't usually get worse with time. In-between exacerbations the symptoms usually disappear, and the disease doesn't usually progress into anything more serious.
Differences in Causes
COPD is usually caused by exposure to smoke, pollution, and other substances that damage your lungs. In fact, about 90% of COPD cases are caused by smoking tobacco.
Common Causes of COPD:
-
Smoking cigarettes and other forms of tobacco
-
Long-term exposure to other sources of smoke, including wood-burning stoves, cooking fumes, and secondhand smoke.
-
Long-term exposure to respiratory irritants like bacteria, mold, and chemical fumes (e.g. in the workplace).
-
Exposure to respiratory toxins like asbestos and radon
- Alpha-1 Antitrypsin Disorder, a genetic disease that causes thickened mucus in the lungs, airways, and other parts of the body.
The causes of asthma, on the other hand, are not as well understood. Like COPD, asthma can result from lung damage due to exposure to respiratory toxins. However, this is actually the least common cause.
Asthma is much more likely to show up early in life, before the lungs have a chance to accumulate any serious damage. Instead, asthma is more likely to be the result of genetics, early childhood respiratory infections, or allergies.
Common Causes of Asthma:
-
Genetic-linked Asthma: Asthma linked to a family history of asthma and other allergic disorders like hay fever and eczema
-
Illness-induced Asthma: Asthma caused by recurrent respiratory infections or serious lung infections early in life
-
Allergy-induced Asthma: Asthma caused by airborne irritants and allergens like pollen, mold spores, dust mites, and pet dander
- Occupational Asthma: Asthma caused by long-term occupational exposure to smoke, dust, or chemical fumes and gases
Differences in Symptoms

As you can see, asthma and COPD symptoms can seem very similar on the surface. However, if you pay closer attention to these symptoms and when they occur, you can better tell the difference between the two diseases.
For example, the most common symptoms of both asthma and COPD are coughing, wheezing, and difficulty breathing. These symptoms tend to show up early on in both diseases, but the frequency of these symptoms differs between the two.
People with asthma tend to only show symptoms when they're triggered by an exacerbation. Once the exacerbation has been treated with medication, the symptoms usually disappear.
People with COPD tend to experience chronic symptoms that don't ever completely go away. While certain triggers and exacerbations can make their symptoms much worse, COPD patients generally face milder symptoms of coughing and breathlessness every day.
Another difference is in the nature of the cough. Asthma tends to cause a dry cough that comes with bouts of breathlessness and wheezing, while COPD tends to cause a wet, phlegm cough that appears every day, independent of breathing difficulties.
Differences in Triggers

Besides examining potential causes and specific symptoms, another way to tell asthma and COPD apart is by their triggers. Some of the triggers for worsened asthma and COPD symptoms are the same, but some are unique.
As we've mentioned, asthma symptoms tend to be severe and show up in response to weather, allergens, and heavy physical activity. COPD symptoms, on the other hand, are chronic and milder, although exposure to extreme weather, exercise, allergens, and other respiratory irritants can worsen symptoms to a degree.
However, these irritants usually only trigger slightly worsened coughing and breathlessness in people with COPD, not an actual exacerbation. True exacerbations are much more serious and are usually only caused by respiratory illnesses and infections.
Severe asthma exacerbations, on the other hand, can be easily triggered by minor environmental irritants like cold air and pollen.
Common Triggers for Asthma Exacerbations:
- Allergens
- Exercise
- Cold air
Common Triggers for COPD Exacerbations:
- Respiratory infections
- Respiratory illnesses like the cold, flu, or pneumonia
- Exposure to pollutants and lung irritants
By paying attention to what activities and environments cause your symptoms to act up, you can often determine whether asthma or COPD is the more likely culprit. Keep a look out for distinguishing triggers and make sure to report any new symptoms or sensitivities to your doctor as they come up.
Asthma Can Increase Your Risk for COPD
Despite being distinct and separate diseases, in some cases asthma and COPD are intimately related. Studies show that up to forty percent of people with COPD also have asthma, which indicates that people with asthma are at a much higher risk for the disease.
Doctors and researchers aren't quite sure what might cause people with asthma to develop COPD (known as asthma-COPD overlap syndrome), but it might have to do with the chronic respiratory inflammation that asthma causes. Severe, untreated asthma, researchers postulate, might cause changes in the lungs and airways that reduce lung function over time.
If their lung function has already been affected, people with severe, untreated asthma may be even more prone to developing COPD. This is especially true if they smoke or are exposed to other respiratory irritants over a long period of time.
To the best of medical knowledge, the best way to prevent asthma-related COPD is early asthma treatment and symptom management. Asthma patients who are diagnosed early and get medicine to treat their symptoms usually don't experience complications later in life.
Diagnosing COPD

COPD symptoms tend to show up later in life, usually after the age of forty. Symptoms often start with coughing and breathlessness during exercise, which prompts many patients to visit their doctor to determine the cause.
The doctor will then do a general physical exam and test the patient's lungs. To do this, doctors use a special lung test called a spirometry test.
To do this simple test, the patient takes a deep breath and then blows as hard as they can into a spirometer. Based on the spirometer's score, the doctor can tell how much the patient's lung function has declined, if at all.
Based on the spirometry results, the physical exam, and the patient's age and smoking history, the doctor will determine whether COPD is an accurate diagnosis. If the patient is over forty, has decreased lung function, and is a current or former smoker, COPD is very likely.
Unlike asthma, COPD does not respond completely to treatment with medications like steroids and bronchodilators. An asthma patient's lung function tends to return to normal after treatment, whereas COPD patients experience a permanent loss in lung function that cannot be restored with medications.
While COPD symptoms can be treated with medicine, they never quite go away completely. The damage that the lungs have already sustained can never be undone.
Diagnosing Asthma
Asthma symptoms often show up by the age of five, starting with bouts of wheezing and dry coughing. These ailments usually prompt a visit to the doctor, who does a general physical exam and listens to the patient's lungs for wheezing and abnormalities.
The doctor will note any allergies the patient has along with any additional respiratory symptoms. Doctors also use spirometry tests to check overall lung function in suspected asthma patients.
If asthma is suspected, the doctor will then prescribe an inhaled bronchodilator medication (inhaler) for the patient to use if the symptoms show up again. If the patient responds well to the medication and the symptoms disappear quickly after using their inhaler, the doctor will usually diagnose the patient with asthma.
Medical Treatments for Asthma and COPD

Treatment approaches to asthma and COPD are both similar and different. Asthma treatment focuses on using medication to treat asthma symptoms exacerbations when they come. COPD treatment, on the other hand, tend to focus on exercise, diet, and lifestyle changes that can strengthen the lungs and prevent further respiratory decline.
Bronchodilators are a type of inhaled medication used to reduce coughing and wheezing by opening up the airways and making it easier to breathe. Both people with asthma and people with COPD use bronchodilator medications to treat immediate respiratory symptoms, and it's a primary method of treatment for COPD.
People with asthma usually also take inhaled corticosteroid medications on a regular basis to help manage inflammation and prevent exacerbations. While COPD patients sometimes take corticosteroids as well, it's not as common for long-term treatment.
As the disease progresses, people with COPD often end up needing to use supplemental oxygen therapy in order for their lungs to absorb enough oxygen to meet their body's needs. This is rarely needed for people with asthma except in the midst of a severe exacerbation. This is because asthmatic lungs are generally healthy and able to absorb enough oxygen on their own in normal circumstances.
In the latest stages of the disease, some COPD patients are eligible for lung reduction surgery or lung transplant surgery. These are last-resort measures that are usually only used if a patient is unable to survive on their own without them.
Lifestyle Treatments for Asthma and COPD
Treating asthma usually doesn't require any major lifestyle changes besides not smoking and avoiding respiratory irritants. Asthma patients focus mainly on controlling inflammation and preventing exposure to triggers that result in exacerbations.
COPD, on the other hand, requires a myriad of lifestyle changes and a tailored treatment plan. The most important thing to do is to quit smoking, but after that a healthy diet, exercise, and medications take priority. Although continued respiratory decline is inevitable for most people with COPD, these lifestyle changes can slow down the disease's progression and improve their ability to breathe.
Obviously, people with asthma can benefit from a healthy diet and lifestyle, too. Both people with asthma and COPD should never smoke, stay physically active, and eat a balanced diet full of fruits, veggies, and lean protein.
Staying hydrated is also very important for managing a respiratory illness like asthma or COPD. Water thins out the mucus in your airways, making it easier to breathe, and keeps the rest of your body's functions running efficiently.
Exercise is also very important, but especially for people with COPD. People with asthma should get plenty of physical activity too, but for people with COPD it is vital to prevent further physical and respiratory decline.
Disease Outlook for Asthma and COPD

People with asthma generally only have to worry about avoiding their triggers and treating inflammation with medication. While poor lifestyle choices like smoking and exposure to respiratory irritants can sometimes make asthma worse, most people with asthma live healthy lives and experience no decrease in lifespan.
COPD, on the other hand, tends to slowly worsen over time no matter how well it's treated. Quitting smoking and building healthier habits can improve your lifespan and quality of life, but it cannot prevent the disease from continuing to progress.
However, many people with COPD are able to live good, fulfilling lives in spite of their disease. This depends partially on an early diagnosis, but primarily on how well you comply with your COPD treatment plan.
How much physical activity you get, how well you manage your symptoms, and how well you practice other healthy lifestyle and diet habits can have a major effect on your body's strength and ability to cope with the disease.
Conclusion
If you are an adult with worrisome respiratory symptoms, it can be difficult to get an accurate diagnosis. One reason for this is the fact that both asthma and COPD share identical symptoms and sometimes share a common cause.
Both asthma and COPD are relatively common diseases, which makes it all the more important for more people to be able to recognize and seek treatment for both. The relationship between the two conditions can be complicated, and it's important for patients and their loved ones to be aware.
Now that you've learned more about the two diseases, you will be better equipped to help yourself, your friends, and your loved ones get proper diagnosis and treatment for their respiratory symptoms. While you should always defer to a doctor for a final diagnosis, this knowledge is vital to help the estimated thirteen million people with COPD who are still un-diagnosed get the medical attention they need.
While neither disease can be cured, the symptoms of asthma and COPD can be reduced and controlled with the right kind of care. The earlier someone with asthma or COPD gets an accurate diagnosis and begins treating their disease, the easier it is to stay healthy and maintain a good quality of life.
.png)
Last year, we were very happy to announce that we would be selling the Caire FreeStyle Comfort, the latest pulse flow portable oxygen concentrator by Caire, Inc. This concentrator was miles ahead of anything that Caire had manufactured in the past, and it even held its own against the most popular oxygen concentrator on the market: the Inogen One G5.
One of the reasons we continue to support the FreeStyle Comfort is that it’s backed by a company that prioritizes quality above all else. Whether you have COPD, cystic fibrosis, or any other chronic lung condition, you need an oxygen device that you can rely on wherever you go and for many oxygen patients, the FreeStyle Comfort has been the best oxygen concentrator for that.
If you keep up with our blogs, however, you know that we like to approach every subject from as many angles as possible in order to give you a better understanding of your needs and the industry as a whole. In this post, we’re going to be comparing and contrasting the Caire FreeStyle Comfort portable oxygen concentrator and standard compressed oxygen tanks. As always, if you have any questions, be sure to leave them in the comment section below, or feel free to give us a call and address them with one of our respiratory specialists.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Oxygen Output
Supplemental oxygen isn’t a one-size-fits-all solution. Every oxygen patient has varying degrees of lung function and as a result, everyone requires a different amount of oxygen in order to stay healthy. For example, someone with stage 1 COPD may only experience a small amount of airway obstruction, so they might only need to use oxygen for an hour or two a day. However, someone with severe stage 3 or 4 COPD may need to use oxygen 24 hours a day.
.jpg)
Another important factor to consider is the “grade” or “purity” of the oxygen you’re inhaling. Earth’s atmosphere is made up of only about 21 percent oxygen. The rest of the atmosphere is composed of various other gases including nitrogen, argon, and carbon dioxide. Medical-grade oxygen, on the other hand, always has over a 90 percent purity rating. This should not be confused with “recreational” oxygen which is sold in canisters and doesn’t require a prescription to purchase.
Both portable oxygen concentrators, like the Caire FreeStyle Comfort and oxygen tanks put out medical-grade oxygen. In fact, oxygen tanks are refilled with something called a HomeFill Station which operates like an oxygen concentrator. The main difference between the two is that an oxygen tank will allow you to put out oxygen at a higher flow rate. This is ideal for people with severe lung impairment, but it’s not necessary for the vast majority of respiratory patients.
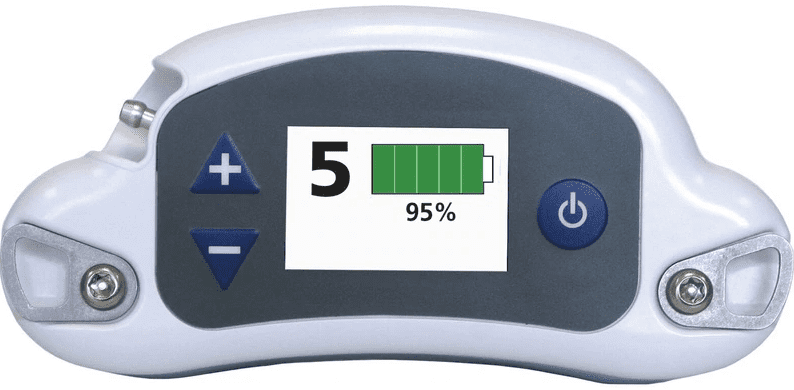
Another thing to note is that the Caire FreeStyle Comfort is a pulse dose machine. What this means is that oxygen is only administered when the user inhales rather than continuously flowing out of the device like with an oxygen tank. Because of this, many people underestimate the value of pulse dose oxygen concentrators. The FreeStyle Comfort puts out 1,050 milliliters per minute of oxygen which is roughly the equivalent of 3 liters per minute on a continuous flow device such as an oxygen tank.
Ultimately, it will be up to your doctor or pulmonologist whether you should use the Caire FreeStyle Comfort or an oxygen tank. While oxygen tanks tend to be the default for many people, they are not necessarily the best option, especially for people who want to maintain their freedom, independence, and mobility while on oxygen.
Portability
If you think about it, “portability” has been a defining feature of this millennium so far. Ever since the early 2000s, we’ve seen technology become smaller, lighter, and more powerful than ever before; this is really no different when it comes to O2 devices. Just several decades ago, oxygen concentrators were mostly only used in the home. While there were portable versions, they were cumbersome and difficult to maneuver.
Fast forward to today and you’ll find that oxygen patients have a wide variety of lightweight portable oxygen devices to choose from. The AirSep Focus is the lightest portable oxygen concentrator ever produced, weighing in at just 1.75 pounds! However, it’s only able to go up to a pulse flow setting of 2 (330 ml/min), so it may not be enough oxygen for many patients.

The Caire FreeStyle Comfort, however, is the perfect balance of both portability and power. It weighs in at only 5 pounds and it’s able to output over three times as much oxygen as the AirSep Focus. Its dimensions are only 10” H x 7.3” L x 3.1” W, so it’s also very small, compact, and easy to carry. Whether you’re just going for a walk in the park or you’re going on a long vacation, you’ll find that the FreeStyle Comfort is as easy to transport as a small purse or handbag.

Unlike portable oxygen concentrators, oxygen tanks haven’t gotten any smaller in the past couple of decades. Oxygen can only be compressed a certain amount before it becomes too dangerous to use, so the size of your tank directly correlates with the amount of oxygen you will have access to. While there are “portable oxygen cylinders” they will only offer you several hours of freedom before they need to be refilled.
Safety
Safety should always be the first priority when choosing an oxygen device. Unfortunately, oxygen manufacturers have not always been able to provide this to their patients. Oxygen is considered by the U.S. Food and Drug Administration (FDA) to be a controlled substance. First and foremost, oxygen is an oxidizer meaning it makes everything it’s exposed to more flammable.
Secondly, it is possible to overdose on oxygen and experience something called oxygen toxicity. This condition is characterized by lightheadedness, fatigue, muscle twitching, and nausea. Prolonged exposure to high levels of oxygen can even be deadly. This is why it’s so important that oxygen is used exactly as instructed by your doctor.
While oxygen tanks are mostly safe to use, they still pose more of a safety risk than pulse dose oxygen concentrators like the Caire FreeStyle Comfort. For one, oxygen tanks are stored at very high pressures of around 2,000 to 3,000 psi (pressure per square inch). This makes them a huge explosive hazard whereas oxygen concentrators do not pressurize oxygen at all.

Another reason oxygen tanks are more dangerous is that they are continuous flow. When you release the pressure valve on an oxygen tank, oxygen will constantly flow out of the nasal cannula until you turn it off. This is dangerous because if it were exposed to fire it would oxidize it making it burn more. This can be somewhat remedied by using a pulse dose conserver which can be attached to the top of the tank, but there’s still a chance it could be leaking oxygen.
Finally, the weight and size of oxygen tanks are a potential hazard. Oxygen tanks are made of metal and they’re usually very heavy and bulky. If one happens to fall on you while you’re removing it from storage it could cause serious injury. Its bulkiness can also make it a tripping hazard and make it difficult and stressful to transport.

The Caire FreeStyle Comfort doesn’t have most of these issues because it’s so light and portable. You can easily carry it on one shoulder without it causing back pain and you’ll never have to wheel it around using a rolling cart. Since it’s so small, it’s very easy to store and keep somewhere that you’ll remember where it is.
Cost-Effectiveness
When money is tight, every financial decision you make counts. On the surface, it may seem like oxygen concentrators are the cheapest form of supplemental oxygen. But when you take into consideration long-term costs, they’re actually one of the more expensive options out there. Conversely, portable oxygen concentrators, in general, are designed to save you a significant amount of money over time.
The Caire FreeStyle Comfort has a Manufacturer’s Suggested Retail Price (MSRP) of $2,495, but it comes with a battery, AC and DC charger, carrying case and strap, and a 3-year warranty. What this means is that if anything that comes with your POC breaks or isn’t functioning properly within 3 years, you can have it replaced free of charge. This warranty can be extended to give you even more coverage and security.

Even if you don’t choose to extend the warranty, Caire builds their portable oxygen concentrators to last. On average, a new portable oxygen concentrator will last 5 to 7 years depending on how well the user takes care of it, and we’ve even seen them last much longer than that in certain cases. If you’re interested in learning how to clean and maintain oxygen equipment, we wrote a great post on this subject a couple of years back. You can find it here.
Another thing to note is that the Caire FreeStyle Comfort requires very little long-term maintenance. Whereas oxygen tanks need to be filled up every time they run out, oxygen concentrators simply need to be plugged into a wall outlet to recharge. You’ll never need to go out of your way to find an oxygen supplier to refill it and you won’t have to invest in a HomeFill Station which can break the bank.

Even if you purchase your Caire FreeStyle Comfort at the suggested retail price of $2,495 that works out to about $41 per month over 5 years or $30 a month over 7 years. However, if you take advantage of a sale, it will be even less than that! There are also a whole host of financing options you can use to make payments easier and you can even trade-in your oxygen concentrator whenever you’d like if you’re thinking of upgrading. On the other hand, you likely won’t get anything for trading in an oxygen tank and you may even have trouble finding someone to take it.
Ease-of-Use
In this day and age, it’s more important than ever to simplify your life. No matter whether you’re old or young, poor or wealthy, most people just have too many things on their plate to worry about. For some people, simplifying could mean downsizing by getting rid of things that you don’t need or it could just mean replacing those things with ones that are easier to manage.

When most people try a portable oxygen concentrator like the Caire FreeStyle Comfort for the first time, they find that it’s much easier to manage for several different reasons. First and foremost, they work great as an all-in-one oxygen machine. Rather than using a portable oxygen cylinder while you’re out of the house and then having to switch over to your home oxygen tank when you get home, the FreeStyle Comfort can be used as both a portable and home unit.
Another factor contributing to its ease-of-use is the interface. Just like the concentrator itself, the interface is electronic and there are no knobs that you have to turn or worry about. Simply turn the device on and select the flow setting that you would like to use. If there are any problems, the device uses an alarm to notify you.
Durability
Respiratory patients depend on their oxygen. But what happens if you accidentally drop your oxygen device or bump into something? While the Caire FreeStyle Comfort may not look durable at first glance, you might be surprised to find that it’s very compact and solid. All of the delicate electronic components that keep the device running are protected by a hard outer shell that will protect from scratches and dents. The carrying case that comes with the device will also give some added protection. And since it’s light enough to carry on your shoulder, you’ll be able to navigate more easily without the chance of dropping it or bumping into anything.

While oxygen tanks are mostly made of metal, the nobs and nozzles on top of the tank are plastic. If any of these things are damaged, it could lead to a leak in the tank. Oxygen tanks are more prone to damage when you use a rolling cart because you aren’t always able to see what obstacles are in your way without looking behind you. Oxygen tanks also have an awkward shape that can make them difficult to handle.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Final Thoughts
It’s not always easy to make decisions about your health as a COPD patient. There are many different oxygen devices for seniors and you may have no idea where to begin when it comes time to choose one. While oxygen tanks have been used for many years, they’re certainly starting to show their age when it comes to portability, cost, and general ease-of-use.
Portable oxygen concentrators, however, are more technologically advanced and offer you more freedom for you to live life on your own terms. The Caire FreeStyle Comfort is one of the newest POCs the industry has to offer and it doesn’t disappoint. Weighing in at only 5 pounds with a maximum oxygen output of 1,050 ml/min of oxygen, it will meet your needs wherever you are in the world.
%20(1).png)
A new study of more than 2000 individuals who are diagnosed with chronic obstructive pulmonary disease (COPD) found that patients struggle with a range of other physical and emotional symptoms, which go beyond the respiratory impairments that are well known to providers.
The study which was conducted by the Health Union national survey, ‘COPD in America 2017’, was released through COPD.net which is the Health Union’s online community. It found that, health care providers were often not very helpful in addressing issues related to the emotional impact that COPD patients were struggling with.

COPD is an umbrella term used to describe progressive lung diseases including chronic bronchitis and emphysema, where changes in the airways block the normal air flow in and out of the lungs causing shortness of breath. It is estimated that over 65 million people worldwide have moderate to severe COPD this is including 15 million adults in the United States.
Breathlessness is the most common and toughest symptom to manage according to 84 percent of the respondents, yet they also mentioned a number of other frustrations and problems that they face. 81 percent of the respondents reported experiencing fatigue and getting tired easily; 66 percent reported weakness and being tired while exercising and 52 percent reported pain, chest tightness and pressure.
Leon Lebowitz, respiratory therapist and COPD.net contributor explained that while a number of people may think that COPD is just a disease of the lung, the reduced oxygen as a result of lung damage can affect every part of the body. For instance, fatigue is exacerbated by the lack of oxygen making daily functioning more difficult.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
“It is a difficult balancing act. Breathing is the primary issue – it is what brings people to the Emergency Department,” Lebowitz said. “People often come in and say ‘if I can breathe, I can deal with everything else.’ For a person to adjust, they have to learn to pace themselves. So if they have a bad day, they take it easy, and when it is a good day, they enjoy life.”
Another mysterious yet frequently reported symptom is rib cramping. Thirty-nine percent of respondents reported that they had experienced this symptom the preceding month. 42 percent stated that they had spoken to their health-care providers about it, but 69 percent of this portion reported that they walked away from the visit without a solution or treatment for the problem.
“I wish my physician understood the cramping in my ribs. I feel that they don’t have an explanation as to why I get these cramps and they are very painful,” reported one of the respondents.
Keeping that frustration in mind, the survey also not surprisingly unveiled the emotional impact of COPD which often takes a back seat to the physical challenges, even though it can be more overwhelming than it is perceived.

For instance, 51 percent of the respondents reported problems with panic disorders or anxiety to their doctors, and only 40 percent of this portion mentioned that their doctor was effective in helping them manage it. Additionally, 24 percent have a mood disorder such as bi-polar disorder or depression.
“Depression is a real symptom of COPD,” said Michelle Vincent, COPD.net patient contributor. “Finding support groups was a huge boost. I like being able to talk to and get to know people who are going through the same things that I am. It makes me feel like I’m not alone. I like being able to give back to the community too.”
A majority of the respondents stated that they did not feel confident that they could keep the emotional distress caused by COPD from interfering with their lives. Regardless of the challenge they faced, only 19 percent reported that they are currently involved in a COPD support group. A patient contributor from COPD.net said, “I wish my doctor would better understand the anxiety and stress I am feeling about it. He never helps me address this.”
The survey revealed that chronic coughing, having trouble sleeping and unintended weight gain were among the issues raised under the most challenging and frustrating symptoms the respondents faced. The respondents also reported that it was not easy to avoid COPD triggers since they are everywhere in the environment.

A flare can be triggered by almost anything especially strong scents and weather changes among many others. Examples of such triggers include mildew, smoke, mold, dust, chemical fumes, grass, cleaning products, perfumes and respiratory infections.
Thirty-five percent of the respondents found it to be somewhat easy to avoid the triggers, 27 percent reported that it was not easy at all, 25 percent reported that it was slightly easy, 12 percent reported that it was moderately easy and 1 percent found it to be very easy.
When a flare hits, it is very common for a patients to experience incontinence. It isn’t just the lungs that get affected during a flare, the breathlessness and the intense coughing causes incontinence in 59 percent of the respondents. In the survey, 19 percent reported experiencing incontinence often, 23 percent experienced it sometimes and 17 percent experienced it rarely. 41 percent did not experience it at all.

Many of those that experience incontinence find it to be very embarrassing and due to the shame that many sufferers feel, it is under-discussed, leading many to think that they are the only ones with the problem. Incontinence refers to the inability to hold your urine or bowel movements long enough to get to a toilet.
The fear of embarrassment prevents very many patients with COPD from enjoying various aspects of life and leads to them distancing themselves from other people. Incontinence should however not be seen as unacceptable or embarrassing behavior because it is an involuntary operation of the body.
When the respondents were asked to describe COPD in one word some of the descriptions included; irritating, avoidable, nasty, lonely, draining, thief, misery and nightmare. They expressed a lot of anxiety and fear over the future with COPD. It is however important to note that COPD is not a death sentence and that there are very many people that are willing to lend a helping hand at any given time.
“The results of this survey clearly illustrate why COPD.net has been so successful in providing support to people living with COPD,” said Tim Armand, president and co-founder of Health Union. “ The world of the COPD patients can seem a lonely, confusing and isolating place, but here they can find a community that understands, is willing to listen, and provides information they can use in their daily lives.”
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Studies find that use of disinfectants once every week can increase the risk of developing chronic obstructive pulmonary disease (COPD) by as much as 32%. This according to a joint 30-year study by the French National Institute of Health and Medical Research (INSERM) and Havard University which found that the use of products such as glutaraldehyde, hydrogen peroxide, bleach, alcohol and quaternary ammonium compounds (quats) (commonly found in furniture and floor disinfectants) increased the risk of developing COPD by 22 – 32 % in an occupational setting.

Researchers looking at the incidence of COPD in more than 55,000 nurses in the US, found that the regular use of disinfectants has been linked to a higher risk of developing the disease.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
COPD which affects an estimated 30 million people in the United States is a group of lung conditions such as chronic bronchitis and emphysema which make it hard to breathe air into and out of the lungs. This is due to the narrowing of the airways as a result of blockage and inflammation in the lungs.
Symptoms caused by the blockage of the airways include; breathlessness, wheezing, chest pain and a chronic cough. It commonly affects heavy smokers over the age of 35 and can also be developed through exposure to second hand smoke and other lung irritants such as chemical fumes, dust and air pollution. It is strongly recommended that you wear a face mask should you be in contact with any of these at your place of work or your environment in general.
Nearly 120,000 people lose their lives to COPD every year in the United States making it the third leading cause of death in the country. An estimated 12 million people living in the United States are believed to be undiagnosed and unaware that they have the disease.

Dr. Orianne Dumas (PHD) from INSERM, Villejuif, France, told the European Respiratory Society (ERS) International Congress that certain tasks such as frequent exposure to disinfectants, cleaning surfaces and specific chemicals in disinfectants increased the risk of developing COPD by 22%. This is according to data from the Unites States Nurses Health Study II (NHS II) which was surveyed for 8 years.
“The potential adverse effects of exposure to disinfectants on COPD have received much less attention, although two recent studies in European populations showed that working as a cleaner was associated with a higher risk of COPD. To the best of our knowledge, we are the first to report a link between disinfectants and COPD among other healthcare workers and to investigate specific chemicals that may underlie this association,” Dumas said.
“Our findings provide further evidence of the effects of exposure to disinfectants on respiratory problems and highlight the urgency of integrating occupational health considerations into guidelines for cleaning and disinfection in the healthcare settings such as hospitals.”
More than 100,000 nurses in the United States enrolled in the NHS II which began in 1989. Dumas and her colleagues analyzed data from those who were still working as nurses in the year 2009 and had no previous history of COPD. The number of nurses that fell under this category was 55,185 nurses. They were followed by Dumas’ group for a period of approximately eight years up until May, 2017. Within this period, 663 nurses had developed COPD.

Their exposure was evaluated through the Job-Task-Exposure matrix which assigned exposure to disinfectants by task or job and a questionnaire. Results were adjusted based on factors that might affect the results such as ethnicity, age, Body Mass Index (BMI) and smoking. The nurses were surveyed after every two years said Dumas.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Mina Gaga, MD of the Athens Chest Hospital and ERS president-elect, said, “This study shows that you have to be careful when you are around substances known to be a lung irritant, and we also know that lung irritation may lead to development of COPD down the road.”
“We do tell people who work with these chemicals to use them properly and particularly not to mix them, but you can’t completely eliminate their use because there is a need to keep things clean with these agents,” she told MedPage Today.
She made a suggestion that people, “Use caution and use common sense: Open a window when using them. This is true for anyone, not just nurses in hospitals.”

Dumas said at the press conference that 37% of the nurses reported weekly involvement in the use of disinfectants to clean surfaces and 19% in the use of disinfectants to clean medical instruments. She reported a suggested association for weekly use of disinfectants to clean medical instruments.
In a separate study conducted in 2017, Dumas and her colleagues described disinfectants used by nurses, and investigate quantitative and qualitative differences according to workplace characteristics and region. Dumas’ group found that working in a hospital was tied to higher disinfectant use but lower spray use. Also, nurses working in a smaller hospital setting (50 to 200 beds) were more likely to use disinfectants and sprays. Finally, spray use was higher in the Northeast than in the West.
Dumas said, “These are preliminary findings and more research needs to be carried out. In particular, we need to investigate the lifetime impact on COPD of lifetime occupational exposure to chemicals and clarify the role of each specific disinfectant. We hope to receive funding from the United States Centers for Disease Control and Prevention to continue this important work.”
She added that, “Some of these disinfectants such as bleach and quats are used frequently in ordinary households and the potential impact of domestic use of disinfectants on COPD development is unknown. Earlier studies have found a link between asthma and exposure to cleaning products and disinfectants at home, such as bleach and sprays, so it is important to investigate further.”
Dr. Dumas put a lot of emphasis on the fact that since this was an observational study, the findings are not able to show that disinfectants cause COPD but that there is an association between some of the disinfectants which are used and the development of the disease.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
If you have COPD, you're probably no stranger to feeling drained, tired, and lethargic. Fatigue is a common problem for COPD patients, and a serious one at that. Fatigue is a common culprit behind exercise avoidance and sedentary living, which causes many patients to experience a quicker physical decline.
Fatigue is often used as a synonym for feeling tired or exhausted, but it's actually different in several ways. First, fatigue isn't necessarily related to activity or quality of sleep; you can feel fatigued even if you haven't done anything tiring and even if you get plenty of rest at night.
Fatigue is a kind of whole-body exhaustion that takes “feeling tired” to a new level. It hurts your ability to concentrate, drains your energy, and often worsens anxiety. Fatigue makes you feel too tired to do things that you usually enjoy, and can make simple things like dressing, reading, or leaving the house feel like monumentally difficult tasks. Often, fatigue is a sign that your body is having trouble keeping up with its energy needs.
Fatigue can make everything feel like a chore, like you have to drag yourself to every activity and social engagement. Some patients feel so fatigued every day that they stop exercising, isolate themselves in their homes, and give up on healthy lifestyle habits and treatment goals that are necessary for their well-being.
That's what makes fatigue such a major concern for COPD patients and the doctors that treat them. When left untreated and unmanaged, fatigue discourages many people with COPD from doing the very activities that would help preserve their health and quality of life.
In this article we're going to help you beat COPD-related fatigue by giving you thirteen useful tips for reducing fatigue and maximizing the amount of energy you have to invest in your life every day. But first, let's look at what causes fatigue and how it affects the lives of people with COPD.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Causes of COPD-Related Fatigue

COPD is a chronic, continually-progressing disease, and simply managing the symptoms alone can get exhausting. But there are several specific ways in which the disease causes patients to suffer from fatigue.
COPD-related problems like decreased lung function, lack of exercise, and lack of oxygen all result in fatigue. Unhealthy habits can also make it worse; a poor diet, sedentary lifestyle, and lack of sleep all contribute to COPD-related fatigue.
Let's take a closer look at some of the main causes of fatigue for COPD patients.
Lack of Exercise
COPD symptoms can make exercise very difficult, which can start you on a negative cycle of exercise avoidance, fatigue, and physical decline. The less you exercise, the more breathless and fatigued you will feel, which then makes it more and more difficult to stay active.
This is partially due to loss in physical strength, but fatigue is also directly related to the lung function decline that happens when you don't get enough exercise. The more your lung function is reduced, the more easily you become winded, and the more likely you are to have low-blood oxygen levels and fatigue as a result.
Hypoxemia

Having blood oxygen levels that are too low is known as hypoxemia, and it's a condition that causes your body to feel very fatigued. This discourages many people with COPD from being as active as they should be, even though exercise is essential for keeping your lungs and body strong.
Hypoxemia is often treated with supplemental oxygen, which delivers extra oxygen to your lungs so that your blood oxygen saturation doesn't drop too low. If you experience frequent fatigue, your doctor can evaluate your blood oxygen to see if supplemental oxygen is right for you.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Lack of Sufficient Nutrients

COPD causes uncomfortable symptoms that make it difficult for many patients to eat properly. Patients with inflated lungs due to emphysema, in particular, have difficulty breathing when they eat.
Because of this, many patients avoid meals and don't get enough calories and nutrients. This is especially common in the later stages of COPD.
People with COPD also tend to need more calories because of their declining lung function. Damaged lungs aren't able to absorb as much oxygen with every breath, and have to work harder to keep your blood oxygen levels up. This results in your lungs and the muscles that support them working overtime when you breathe.
Studies show that the breathing muscles of people with COPD use up to ten times the amount of energy compared to people with healthy lungs. This means that most COPD patients burn extra calories just walking, living, and breathing.
Because of this, many people with COPD have to eat a higher calorie diet to supply their lungs and breathing muscles with the nutrients they need. This helps them meet their daily nutrient requirements, have more energy, and experience less COPD-related fatigue.
How to Beat COPD Fatigue and Have More Energy Every Day
Depending on the severity of your COPD and how active you are, you might find even simple, everyday tasks difficult to do. If you're not careful, fatigue can quickly lead to a sedentary lifestyle and an even quicker decline in your physical ability.
Maintaining your physical mobility is key for maintaining a good quality of life, which is why treating COPD-related fatigue is so important. If you can reduce your fatigue, you will have more energy and strength to live a healthy, active life.
There are a variety of treatments for COPD-related fatigue and daily habits you can practice to boost the amount of energy you have every day. Continue reading for a variety of different ideas, including dietary tips, lifestyle habits, and exercises that can help you overcome COPD-related fatigue.
Pulmonary Rehabilitation

|
| Photo by Sgt. Andy Bellami |
As we've mentioned before, lack of exercise is a major contributing factor to COPD-related fatigue. When you avoid physical activity, it causes your muscles to atrophy, and even weakens the muscles you use to breathe. It also causes your lung function to decline, increasing COPD symptoms and making it harder for your lungs to supply enough oxygen to your body.
Luckily, there is a special type of class designed to help COPD patients who struggle with this exact problem. It's called pulmonary rehabilitation, and it uses a variety of hands-on methods to help you increase your strength, endurance, and quality of life.
Pulmonary rehabilitation classes are usually six to eight weeks long and often held as group lessons. Classes are generally run by a team of social workers, dietitians, and medical professionals that are knowledgeable about chronic respiratory diseases. Classes include exercise instruction, lessons on breathing exercises and medications, and opportunities to learn a variety of useful skills that will help you stay active and maintain your independence with COPD.
Here is a list of some of the benefits you can receive from taking a pulmonary rehabilitation class:
- Improved blood circulation
- Reduced breathlessness
- Deeper breathing
- Improved physical fitness and exercise endurance
- Improved mood and motivation
- The skills for proper COPD dieting
- Reduced chance of COPD exacerbations and hospitalizations
- Increased mobility and ability to do daily activities
- Knowledge about COPD medications and treatments
- Improved quality of life
Regular Exercise

People with COPD often feel like they don't have enough strength or energy to devote to exercise. However, if you start getting regular physical activity, you're more likely to have more energy, not less.
Regular physical activity is a cornerstone of COPD treatment because it keeps your body, lungs, and breathing muscles strong. It also helps battle anxiety, fatigue, and certain kinds of chronic pains.
When fatigue makes you feel the most like staying in bed, that's when you need to get up and be active the most. Staying sedentary will only make you feel worse; you have to get your body moving in order to overcome fatigue and find the energy you need to start your day.
If you're not used to exercising, you can start with light stretching, walking, and body weight exercises like leg lifts. Try taking up an active hobby, like biking, gardening, or swimming for extra physical activity.
Don't get sucked into a negative spiral of exercise avoidance, which inevitably leads to worsened symptoms, worsened fatigue, and accelerated physical decline. You should try to stay as active as you can for as long as you can, and always follow the exercise plan recommended by your doctor.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Don't Skip Breakfast

Breakfast is an essential part of a healthy morning routine and will give your body a nutritional boost of energy. If you have COPD, it's especially important to start off your day with a nutritious, balanced meal of fruit, protein, and whole grains.
Eating food in the morning gives your metabolism a jump-start and can help you feel awake, energized, and alert during the day. Don't skip breakfast or wait too long to eat, otherwise you're likely to feel tired sluggish, and fatigued.
Minimize Stress

Living with constant stress not only eats away at your mental resources, but it drains your physical resources as well. Stress is a huge contributor to fatigue, and it's a common problem for people with COPD.
If you experience an excessive amount of stress, changing your habits and environment can make it easier to cope. You can relieve stress through physical activity, meditation, spending more time with loved ones, eating a healthy diet, journaling, and more.
Try to identify stress-inducing people, situations, and environments in your life that you have control over. Then, work on finding solutions that allow you to avoid, minimize, or cope calmly with the things that cause stress in your life.
If you are dealing with chronic stress-induced fatigue, don't hesitate to talk to your doctor about mental health services and resources that are available in your city. Consider joining a support group, seeing a therapist, or asking a psychologist about medications that might help with your anxiety.
Eat Nutritious, High-Calorie Foods

Increasing the amount of calorie-dense foods you eat is a great way to make sure you meet your daily calorie requirements. High-calorie foods are particularly helpful if you're struggling to get enough calories because of breathlessness, appetite loss, or trouble keeping up with a high-calorie diet.
If this sounds like you, then you may need to add more healthy, calorie-dense fats and proteins to your diet. Foods like yogurt, cheese, and ice cream, for example, are great options that you could eat as part of a meal or as a stand-alone snack.
It can also help to prioritize the highest-calorie foods first. For example, if you often find yourself unable to finish your food at mealtimes, eat the most nutritious, calorie-dense items on your plate first. It can also help to avoid drinking liquids before or during meals, that way you're less likely to feel bloated and breathless, and you'll have as much room in your stomach as possible for food.
Here are some nutritious, high-calorie foods that can help you meet your daily calorie needs:
- Milk
- Yogurt
- Cheese
- Ice cream
- Nuts (e.g. almonds and walnuts)
- Nut butters (e.g. peanut butter or almond butter)
- Eggs
- Olive oil and other vegetable oils (e.g. sunflower oil)
- Smoothies
- Protein shakes
As a final tip, eating small meals instead of large ones can make it easier to get enough calories without ever feeling too full. Try eating five or six smaller meals spread out throughout your day instead of the traditional, larger meals at breakfast, lunch, and dinner.
Care For Your Mental Health

Anxiety and depression are common mental health issues that come along with COPD. Coping with the diagnosis alone can be difficult, and the stress of managing the disease and losing physical independence can be difficult to weather on your own.
Fatigue is a common symptom associated with both depression and anxiety, and is sometimes a major factor in COPD-related fatigue. That's why neglecting your mental health is not an option; caring for yourself and your emotions is necessary for both your physical and mental wellbeing.
If you suffer from chronic anxiety, depression, or are having trouble coping with COPD on your own, don't hesitate to seek help. You can talk to your doctor, therapist, or any other licensed mental health professional to get advice, support, and prescription medication if you need it.
You can also find support in group therapy, both in person and online. Your doctor or another mental health professional could help you find mental health support groups and other services in your area, or you can join one of several COPD and lung disease support groups online.
Eat a Lung-Healthy Diet

Did you know that eating a diet high in carbs can actually strain your lungs? That's right, foods high in carbohydrates make your lungs have to work harder to breathe compared to foods high in healthy fats and proteins.
Because of this, you should try to limit the amount of carbohydrates in your diet and replace them with more lean proteins and healthy fats. This will help your lungs work more efficiently, which lowers your risk of experiencing low blood oxygen levels and hypoxemia-related fatigue.
In this way, eating fewer carbs can actually give you more energy and reduce fatigue caused by low oxygen levels in your blood. However, you still need a limited amount of carbs in your diet, and cutting them out completely would cause malnutrition and even worse fatigue.
When you do eat carbohydrate-rich foods, make sure they contain complex carbohydrates instead of simple carbs. Choose things like whole-grain breads and whole-wheat pastas, which contain complex carbs, instead of white breads and pastas, which are stuffed with simple carbs.
Simple carbohydrates cause your blood sugar to spike and fall rapidly, which gives you a limited burst of energy that quickly gives way to fatigue. Avoiding all simple carbs, including sugars, helps keep your blood sugar stable and prevents sudden blood sugar spikes that ultimately lead to fatigue.
Avoid Caffeine

Caffeine might give you energy and help stave off fatigue in the short run, but too much can make you feel worse. Many people get addicted to the caffeine “high,” but end up crashing and feeling even more tired, anxious, and fatigued later on.
Caffeine can also hurt your ability to sleep, which will sap your energy reserves even more if you suffer from chronic fatigue. It's best to avoid caffeine when possible, or to wean yourself off of it for good. At the very least, be careful to cut off your caffeine intake at least six to eight hours before bedtime.
Make Sure You Get Enough Vitamin D

Many people who suffer from fatigue are actually deficient in vitamin D, and correcting the deficiency can significantly improve fatigue. In fact, it's common for doctors to prescribe vitamin D supplements for people with fatigue-related disorders.
It just so happens that vitamin D deficiency is particularly common in COPD patients—up to 66 percent of patients are deficient—and it is a common factor contributing to COPD-related fatigue. Studies show that vitamin D deficiency also affects patients' bone strength and ability to breathe, and that supplemental vitamin D can help improve exercise endurance and strengthen the muscles used for breathing.
If you have COPD and suffer from chronic fatigue, you should talk to your doctor to get tested for vitamin D deficiency. Your doctor can determine if a deficiency is causing your symptoms and prescribe you a vitamin D supplement if needed to correct it.
But you don't always need a supplement; minor vitamin D deficiencies can often be corrected by increasing the amount of vitamin D in your diet and by spending more time in the sun. Just letting the sun touch your skin for ten to twenty minutes a day is enough to give you a significant boost of vitamin D.
Most people should get anywhere from 400-800 IU, or 10-20 micrograms, of vitamin D per day. People who don't spend much time in the sun will need to get most of their Vitamin D from their diet.
There are several kinds of foods that naturally contain vitamin D, and even more that are fortified with extra vitamin D. Here are some good dietary sources of vitamin D you should know:
- Egg yolks
- Cheese
- Salmon
- Mackerel
- Tuna
- Sardines
- Beef liver
- Cod liver oil
- Cereals fortified with vitamin D
- Milk or yogurt fortified with vitamin D
- Orange juice fortified with vitamin D
Supplemental Oxygen

If you have advanced COPD and are experiencing chronic fatigue, it might be because your blood oxygen is low. In the later stages of COPD, many patients have to use supplemental oxygen to prevent hypoxemia and hypoxemia-related fatigue.
Supplemental oxygen is not right for everyone and has to be prescribed by your doctor. Some people need supplemental oxygen all the time, while others only need it during exercise, exacerbations, or while they sleep.
If you are having trouble breathing and getting enough oxygen at night, you might need nighttime oxygen to help you sleep better and keep your blood oxygen levels up while you sleep. You might also want to get tested for sleep apnea, a breathing-related sleep disorder that causes your body to be starved of oxygen at night, leading to daytime sleepiness and fatigue.
Your doctor will be able to test your lung function, your oxygen saturation, and review other information to determine whether you need supplemental oxygen and whether or not your insurance will cover the cost. In some cases you can use other treatments, like medications, exercise, or breathing techniques, to improve your breathing efficiency, instead.
Take Hydration Seriously

Dehydration doesn't feel good; it can cause headaches, dizziness, and fatigue. And what's worse, if you have COPD, not getting enough water can make symptoms like coughing and breathlessness worse, too.
Water has a multitude of benefits; it helps thin out your mucus, supports healthy metabolism, and lubricates your lungs and airways to prevent irritation. Staying hydrated also keeps your energy levels up, improves your mood, and can even prevent illnesses and infections.
Many sources recommend drinking up to 6-8 cups of water a day, but it varies greatly from person to person and depends on your age, sex, weight, and more. The CDC recommends drinking water whenever you feel thirsty.
If you have trouble drinking enough water, you can try keeping an extra large water bottle with you throughout the day. Use it to motivate yourself, make hydrating as convenient as possible, and to help you keep track of how much you drink.
Often, people who are dehydrated feel sluggish without even knowing why. When you feel particularly lazy or fatigued, try drinking a large glass of cold water. Wait a few minutes and, chances are, you'll feel much better and have more energy afterward.
Conserve Your Energy for What Matters

While you should always try to be as active as possible in your daily life, in the later stages of COPD it is usually necessary to start cutting out some activities and active responsibilities. That might mean delegating certain tasks to friends and family members, hiring help, or using tools and techniques to reduce the amount of effort that daily tasks require.
As you lose mobility and have less strength and energy during the day, time and energy-saving tips can be life-savers. If you can find ways to simplify tasks and responsibilities like cooking, cleaning, and running errands, you'll have more energy for the activities you enjoy.
You can increase your energy to a certain extent through effective COPD treatment and using the methods on this list, but your mental and physical energy stores will still be limited. That's why you need to know when to rest and take it easy so you don't overexert yourself or have to give up on important activities.
It's important to save enough energy during the week to stretch, exercise, and socialize. If you conserve your energy wisely, you will be more likely to be able to find the strength to participate in other healthy activities like sports, hobbies, and social outings. These kinds of activities are necessary for maintaining a healthy body, healthy mind, and enjoying your life to the fullest.
Learn to Recognize Fatigue

When you wake up and feel sluggish, or when you feel breathless and tired, you might not realize that the reason is fatigue. If you don't understand fatigue and how it differs from other types of malaise, it's easy to mislabel it as as anxiety, illness, hunger, physical exhaustion, or lack of sleep.
The problem with this is that, if you attribute fatigue to something else, you could steer yourself toward solutions that won't be effective. For example, mistaking fatigue as physical exhaustion could lead you to avoid exercise, when in reality exercise could actually reduce your fatigue.
Fatigue is more than simply feeling a little tired or run down, but the symptoms are often generic and vague. This makes fatigue sometimes difficult to spot.
Here are some of the most common symptoms of fatigue:
- Chronic feelings of sleepiness and tiredness
- Loss of appetite
- Irritability and mood swings
- Sore, aching, or weakened muscles
- Dizziness
- Headache
- Blurred vision
- Difficulty concentrating
- Slowed movement and reflexes
- Lack of motivation
When you feel tired and lethargic, take time to think about your sleep quality, recent heavy exercise, or anything else that could be causing you to feel run down. If you can rule out other causes, there's a good chance the culprit is fatigue.
When you know that you're suffering from fatigue, you can start to address it by putting some of the techniques we've discussed in this article to use. You should also talk to your doctor if you experience chronic fatigue. Your doctor can evaluate your blood oxygen, medications, and suggest other treatments that can start you on the path to regaining your energy and joy in life.
Conclusion
Recognizing and treating fatigue is a key part of managing COPD. Luckily, there are many effective ways for people with the disease to manage their fatigue and find the energy they need to participate in life to the fullest.
Even though fatigue is still somewhat poorly understood, there are plenty of non-drug treatments that can help many people with COPD beat, or at least manage, their chronic fatigue. More solutions will likely emerge as doctors and researchers continue to develop a better understanding of the causes and effects of COPD-related fatigue.
By watching your diet, exercise, hydration, and taking care of your mental health, you'll be much better able to keep your body strong and combat th


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













