.png)
Chronic obstructive pulmonary disease (COPD) is one of the most substantial health burdens in the world. According to the Centers for Disease Control and Prevention, “chronic lower respiratory disease” (primarily COPD) is fourth on the list of leading causes of death worldwide, behind heart disease, cancer, and unintentional accidents. And despite the fact that fewer people are smoking than ever before, experts are expecting the number of COPD cases to rise within the next 50 years.
While the vast majority of COPD cases are caused by cigarette smoking, many people are surprised to find that COPD is a diverse group of diseases that have a multitude of different causes. One of the other major causes of COPD is alpha-1 antitrypsin deficiency. This is a genetic condition that inhibits proteins that are responsible for protecting the lungs from inflammation and long-term damage. Other factors such as air pollution, irritants, and chemicals can contribute to the onset of COPD. However, these are more commonly associated with interstitial lung disease (ILD).
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
COPD is divided into two different types: chronic bronchitis and emphysema. Bronchitis affects the airways and emphysema affects the lungs. Many COPD patients have both of these diseases simultaneously but it is possible for someone to contract one without the other. And while many people think of emphysema as one disease, it’s actually divided into three different morphological categories. Depending on which one you have, you may require different treatments to manage your symptoms effectively.
In the following sections, we will provide you with an overview of emphysema as well as the three different subtypes. If you have any questions, don’t hesitate to reach out to us by leaving a comment or contacting us by phone or email.
What is Emphysema?
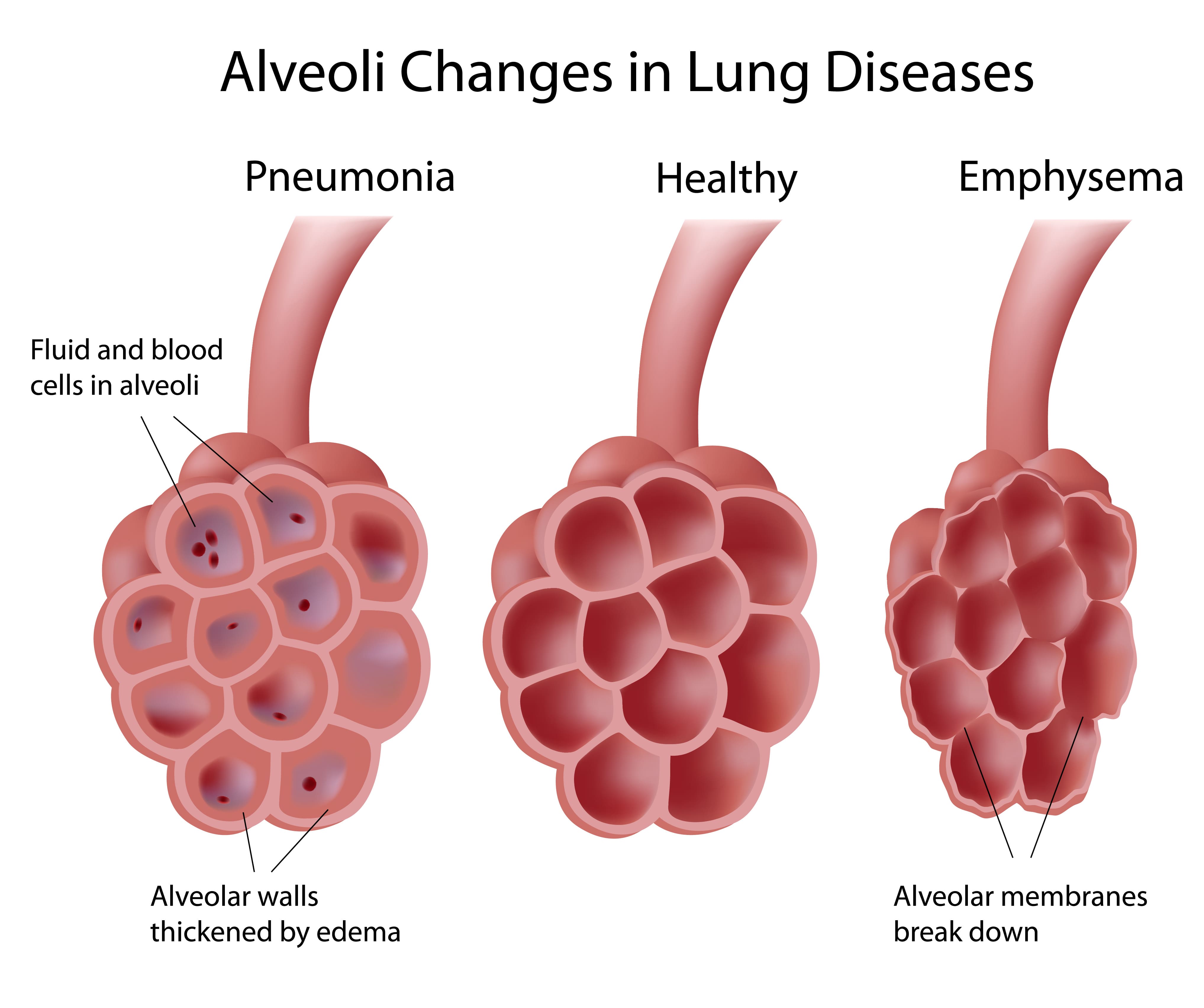
Emphysema is a condition that’s caused by the deterioration of lung function due to the loss of lung elasticity and the deterioration of the alveolar walls. The alveoli are tiny air sacs located at the end of the bronchioles, the small airways that lead into the lungs. There are around 300 to 500 million alveoli in the lungs, and they’re microscopic, so they’re extremely sensitive to foreign substances like cigarette smoke, chemicals, and air pollution.
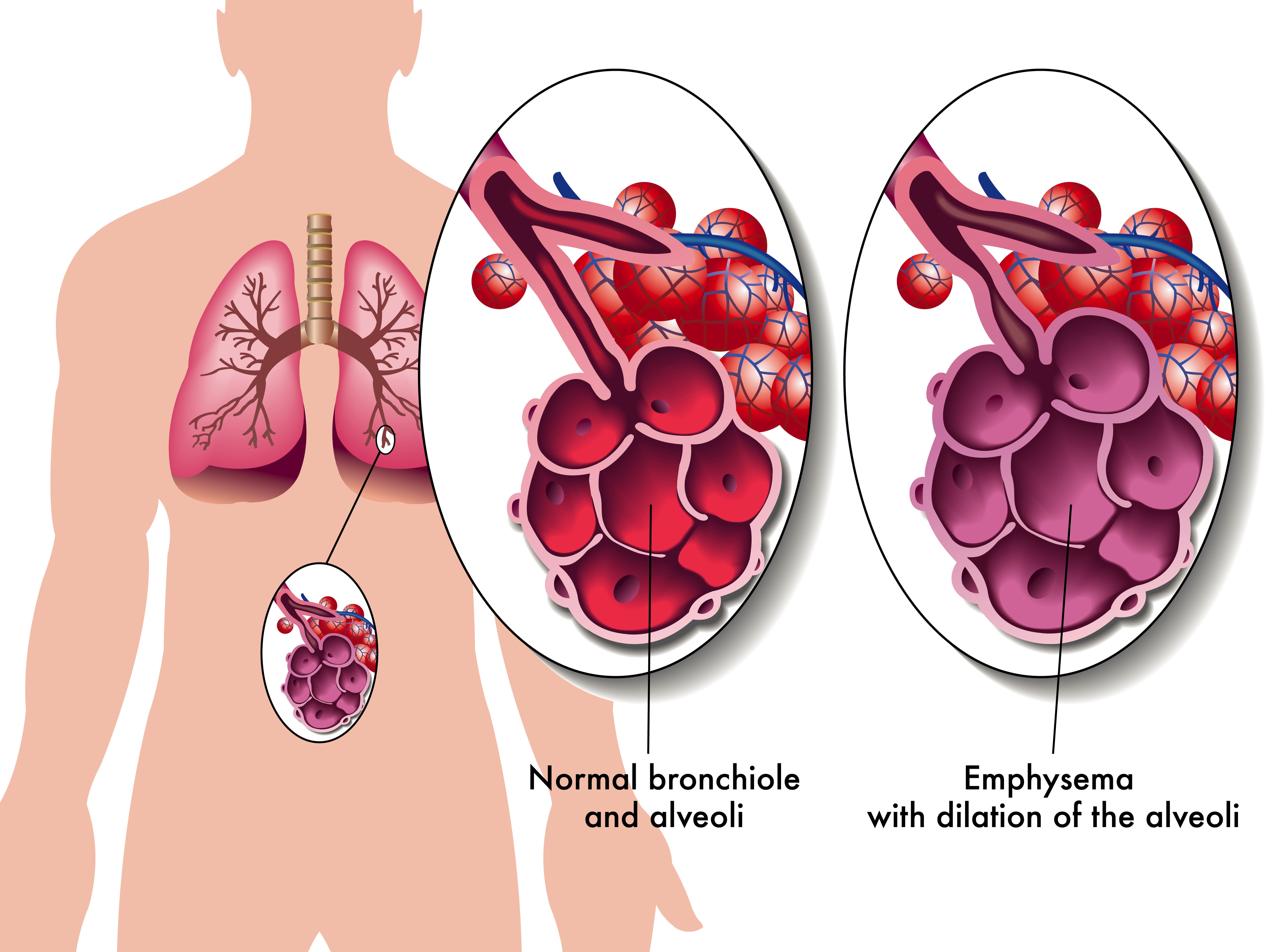
The alveoli play a vital role in the respiratory system because they transfer oxygen from the air that you breathe into the bloodstream. They also remove carbon dioxide from the bloodstream and send it back out of the lungs. This process is called diffusion and it is one of three processes that your lungs perform. Unfortunately, due to how complex the respiratory system is, if the process of diffusion is impaired, this can cause a lot of problems for the other two processes of the respiratory system: ventilation and perfusion.
Not only do alveoli transfer oxygen and carbon dioxide to and from the blood, but they’re also responsible for the spongy and elastic consistency of the lungs. As the walls of the alveoli break down, the elasticity of the lungs is lost and they become less efficient at absorbing air. Another issue this can cause is stagnant air that gets trapped in diseased areas of the lungs which can significantly increase the energy it takes to breathe and result in hyperinflation of the lungs. This also gives emphysema patients their “barrel-chested” appearance which is so often associated with the disease.
What Types of Emphysema Are There?
There are three types of emphysema that differ in terms of what causes them and the area of the lungs that are affected. Depending on which type of emphysema you’re diagnosed with, your doctor may have drastically different treatment options. No two cases of COPD are the same so your physician will work with you to determine what treatment will benefit you most.
Centriacinar Emphysema
Centriacinar emphysema (also called centrilobular emphysema) is a condition that affects the upper lobes of the lungs. Most often this type of emphysema starts in the middle of the lungs and progresses outwards. Centrilobular emphysema is almost always caused by smoking and second-hand smoke and it’s more common in people who’ve been diagnosed with coal workers’ pneumoconiosis (CWP) in the past.

Panacinar Emphysema
Panacinar emphysema (also called panlobular emphysema) is a condition that affects the entire acinus distal to the respiratory bronchioles. The acinus refers to the area at the end of the bronchioles and includes the alveolar ducts, alveolar sacs, and alveoli. It differs from centrilobular because it’s usually located in the lower parts of the lungs. Panacinar emphysema is most commonly caused by homozygous alpha-1 antitrypsin deficiency.
Alpha-1 antitrypsin deficiency (A1AD) is a hereditary disorder that causes low levels of the protein alpha-1 antitrypsin (A1AT) in the blood. This protein is made and released from the liver and it protects tissues in the lungs from being attacked by its own enzymes. A1AD patients may either experience abnormal proteins, poor production of these proteins, or both. All things considered, A1AD is a rare disease and it only amounts to a small percentage of the people diagnosed with COPD.
Paraseptal Emphysema
The third and final morphological subtype of pulmonary emphysema is called paraseptal emphysema. This type is usually localized around the septae or pleura in the lungs. This is a thin sheet of tissue that’s located around the outside of the lungs and inside the chest cavity. This type of emphysema is commonly associated with prior lung infections.
What are the Causes and Risk Factors of Emphysema?
Causes
Cigarette Smoking
Smoking is the most considerable cause of emphysema and all conditions under the umbrella term “COPD.” According to the Centers for Disease Control and Prevention (CDC), 80 percent of people with COPD have smoked in the past or are current smokers. Additionally, 38 percent of people who live with COPD continue to smoke. Despite these facts, only about 10 to 15 percent of smokers will develop some form of COPD. Smoking is more likely to cause cancer, heart disease, stroke, diabetes, and other chronic illnesses.

According to the Cleveland Clinic, the greatest predictor for someone developing emphysema from smoking is not whether or not they were a “light” or “heavy” smoker, it’s how long they smoked for — the longer someone smokes, the more likely they are to contract COPD. This is why doctors will always recommend immediate smoking cessation rather than simply “cutting back” on cigarettes.
Secondhand Smoke
Secondhand smoke refers to the inhalation of cigarette smoke involuntarily as a result of someone else smoking. While there is a commonly held belief that secondhand smoke is worse than actually smoking, this is not the case. The toxicology of tobacco smoke is the same regardless of whether it was inhaled intentionally or not. Either way, cigarette smoke in any form can cause COPD and emphysema.

It’s estimated that there are over 7,000 chemicals in cigarette smoke and smoke can linger in the air for several hours. In other words, living with a smoker or being in an area where someone has smoked recently will put you at a higher risk of chronic lung disease. Cigarette smoke dissipates more quickly outdoors so, generally speaking, it’s safer to be outside.
Air Pollution
Air pollution is a major contributor to the onset and progression of emphysema. According to the World Health Organization (WHO), there are five major types of air pollution: particulate matter, ground-level ozone, nitrogen dioxide, sulfur dioxide, and carbon monoxide. All of which can be inhaled into the lungs and cause permanent damage to the bronchioles and alveoli. Just like with cigarette smoking, the more you’re exposed to air pollution, the more likely it is to cause permanent damage to your lungs.
![]()
One great tool to help you learn about the air pollution in your area is AirNow.gov. All you have to do is enter your city or zip code and it will provide you a number between 0 and 500 with 0 being the least polluted and 500 being the most polluted. The EPA recommends that you should not go outside if the Air Quality Index (AQI) is above 150. However, if you already have a chronic lung disease like asthma or COPD, you should avoid going outside if the AQI is above 100.
What are the Four Stages of Emphysema?
Much like other chronic illnesses that take many years to progress, emphysema is broken down into different “stages” which medical professionals can use to identify the severity of your disease. Since early-stage emphysema has very mild symptoms, it’s often underdiagnosed or misdiagnosed as other chronic lung conditions such as asthma. Read below to learn about the four stages of emphysema.

Stage 1
Stage 1 emphysema is very mild. In fact, it’s often so mild that it is undetected and undiagnosed. People with stage 1 may experience a cough, minor chest pain, and some breathlessness. Stage 1 emphysema patients have a forced expiratory volume in one second (FEV1) of 80% or more.
Stage 2
Stage 2 is slightly more advanced than stage 1. This is when many people start to see their doctor because they begin to realize that their respiratory symptoms aren’t the result of aging or an acute condition. Stage 2 emphysema patients have an FEV1 between 50% and 80%.
Stage 3
By the time someone reaches stage 3 they have most likely received a diagnosis from their doctor. They’ve likely had several flare-ups in the past year and have been admitted to the hospital at least once. Stage 3 patients have an FEV1 between 30% and 50%.
Stage 4
Also known as “end-stage COPD,” this stage is characterized by severe breathlessness, coughing, wheezing, and fatigue which leads to exacerbations and hospitalization. Stage 4 patients have an FEV1 of less than 30%.
How is Emphysema Treated?
Supplemental Oxygen Therapy
Because emphysema can result in low blood oxygen levels (hypoxia) supplemental oxygen can be used to stabilize a patient’s oxygen levels and help alleviate emphysema symptoms like breathlessness, chest pain, and coughing. However, it’s important to note that oxygen therapy can be dangerous if it’s not used in the way that your doctor intends for you to use it. Oxygen is a controlled substance in the United States, so you’ll need a prescription in order to rent or buy an oxygen device.

There are many choices to consider when it comes to oxygen delivery devices so you’ll need to find one that best suits your needs and your lifestyle. Oxygen tanks are a very popular choice because they have a low upfront cost. However, they’re very heavy and need to be refilled constantly making them a poor choice for most oxygen users. Liquid oxygen tanks are an upgrade because they last longer and aren’t as heavy, but they cost more to maintain.

The best alternative to both of these is portable oxygen concentrators. An oxygen concentrator is an electronic device that takes in ambient air and removes nitrogen, argon, and other gases, then puts out medical-grade oxygen. The benefit of this is that you simply need to charge the batteries on your concentrator which is much more convenient than having to have an oxygen company fill your tanks.
Pulmonary Rehabilitation
Many years ago, exercise was not recommended for COPD patients because it was believed to exacerbate symptoms and increase the rate at which the disease progressed. However, in this day and age, pulmonary rehabilitation (exercise that’s focused on lung function) is championed as one of the best ways to treat chronic respiratory illness. This is due to a mounting body of evidence that shows even moderate exercise can improve COPD symptoms.

While you can exercise at home on your own time, it’s recommended that you start with a pulmonary rehabilitation program. Not only do these programs teach you how to exercise with emphysema, but they will also teach you important information about your disease and how it should best be managed. Read this post to learn more about how pulmonary rehabilitation works.
Dietary Changes
If you live by the motto “you are what you eat,” you probably understand the importance of a healthy, well-balanced diet. Nutrition affects everything from your heart health to your lung health and everything in between, so it’s wise to follow your doctor’s instructions on eating healthier meals. According to Lung.org, the metabolism of carbohydrates creates the most carbon dioxide, so they should opt for healthy fats instead which produce the lowest amount of carbon dioxide. HIgh-protein diets are also good for emphysema patients because they keep your lungs strong and efficient.
![]()
Medication
Emphysema treatment usually involves some combination of oral and inhaled medication. Oral steroids can provide you with short- or long-acting relief from your symptoms whereas inhaled medication like bronchodilators are designed to open up your airways quickly in the event of a COPD exacerbation. Your doctor will discuss with you exactly which medications you will need and when to use them.

Most oxygen patients are prescribed inhalers, nebulizers, or both. An inhaler is a portable device that administers medication in a mist form called “aerosol.” this enables the patient to administer the medication directly to their lungs thus allowing it to take effect more quickly. Nebulizers play a similar role in an emphysema treatment plan but they administer medication in a stream rather than a “puff” making them easier to use for most people.
Lifestyle Changes
There are many other lifestyle changes that you can make to treat emphysema and alleviate your symptoms. Focusing on getting more consistent and restful sleep is one way that you can feel more alert and prepared to take on the challenges of your disease. Ultimately, you should discuss your sleeping habits with your doctor to ensure that you’re doing everything you can to get a good night’s sleep.
![]()
Another lifestyle change you can make is changing your cleaning habits. Many common household cleaners are filled with dangerous chemicals like bleach and ammonia. When these substances are inhaled they can cause COPD exacerbation which leads to increased coughing, wheezing, and shortness of breath.
Conclusion
COPD is one of the most preventable chronic illnesses in the world and emphysema is one disease under this umbrella term. Emphysema patients experience impaired lung function due to a breaking down of the alveoli, or tiny sacs in the lungs that transfer oxygen and carbon dioxide to and from the blood. While there is no cure for emphysema, patients can experience significant relief and improved life expectancy with a carefully planned treatment routine.
Here at LPT Medical, we want COPD patients to experience relief from their respiratory symptoms while experiencing the freedom and independence they had before being diagnosed. If you haven’t done so already, ask your doctor if you might benefit from using a portable oxygen concentrator like the Inogen One G5 or the Caire FreeStyle Comfort. Both of these machines have a high oxygen output, they’re lightweight and easy to carry.

