When you inhale and exhale, the air in your lungs and airways may create turbulence called respiratory sounds — also known as “lung sounds” or “breath sounds.” You may know these sounds as “coughing” and “wheezing” but there’s actually a lot more to these sounds than you might initially realize. Breathing sounds are not only used to help diagnose lung conditions like COPD, asthma, and pneumonia but they can be used to assist medical professionals in directing and prescribing medication for these lung diseases.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In the following sections, we’re going to talk about four different types of respiratory sounds, what causes them, how they’re diagnosed, and how they’re treated. After reading, you’ll have a better understanding of the signs your lungs are giving you and what their implications are for your overall health and well-being. And as always, if you have an experience that you would like to share or you have any questions about what you read here, be sure to leave them in the comment section below.
What is the Significance of Respiratory Sounds?
When you visit the doctor with a list of symptoms, your doctor will use any and all tools in his/her toolbox in order to diagnose your condition. For example, your doctor may put you through a series of sleep studies if you report problems getting to sleep, staying asleep, or experiencing restful sleep. A sleep study can reveal exactly when the sleep disruptions are occurring and your doctor will be able to see what your brain activity is like when you sleep. By understanding the root cause of your sleeping problems, your doctor can provide you with treatment options that are tailored just for you.

One of the first methods your doctor will use when diagnosing a condition related to the heart or lungs is called auscultation. During auscultation, medical professionals use a device called a stethoscope in order to listen to the internal sounds of the body including the heart, lungs, and gastrointestinal system.
While auscultation is not the end all be all method for diagnosing lung conditions, it can help medical professionals rule out certain diseases without resorting to more invasive diagnostic methods. Some respiratory sounds like coughing and wheezing can be heard without a medical instrument but using a stethoscope, doctors can identify more subtle sounds that could not be heard otherwise.
Let’s take a look at the different types of lung sounds.
Normal Respiratory Sounds
Normal respiratory sounds are an indication that your respiratory system is healthy and functioning properly. But if you report having respiratory symptoms like chest pain, breathlessness, or chest tightness, your doctor will be able to perform a number of other tests to diagnose them.
CT scans, spirometry tests, pulse oximetry, and the six-minute walk test are just a few of the tests that can be used to diagnose lung disease.

Vesicular
The term “vesicular” is slightly misleading because “vesicle” refers to the alveoli (small air sacs in the lungs) which are responsible for the exchange of oxygen and carbon dioxide between the lungs and bloodstream.
However, the alveoli are not what makes the vesicular sounds. These sounds are soft, rustling, or blowing sounds heard throughout all of the lung fields. They’re heard throughout the duration of inspiration and continuously through one-third of expiration. Vesicular sounds are an indication that you’re able to fully inhale and exhale without obstruction.
Bronchovesicular
Bronchovesicular sounds are muffled but high pitch sounds where the expiratory and inspiratory phase is equal in duration. These sounds are heard over the first and second intercostal spaces (between the ribs) and the interscapular area (shoulder blade).
Bronchial
With bronchial sounds, the expiratory sounds are higher in pitch and intensity. The inspiratory sounds are lower-pitched, hollow, tubular sounds. Bronchial sounds are heard throughout the manubrium (the broad upper part of the sternum).
Tracheal
In tracheal sounds, the expiratory and inspiratory phases are equal in duration. The sound is loud, high-pitched, and heard directly over the trachea, the upper part of your respiratory system.
Abnormal Respiratory Sounds
Rales (Crackles)
Rales, or “crackles” as they’re more commonly called, are the result of fluid buildup in the airways (secretions). Rales are either exudate meaning they’re caused by a lung infection like pneumonia or they are transudate meaning they’re caused by congestive heart failure.
These noises can be heard when the patient inhales because the small airways pop open after collapsing during inhalation. There are three different types of crackles: fine, medium, and coarse.
- Fine crackles often occur during early inspiration and are fainter in volume.
- Medium crackles are more high pitched and they may indicate an interstitial process such as congestive heart failure or pulmonary fibrosis.
-
Coarse crackles last longer than fine or medium crackles and they tend to be louder and lower-pitched. They are most often a sign of excessive fluid on the lungs caused by pneumonia, chronic bronchitis, or pulmonary edema.
Wheezes
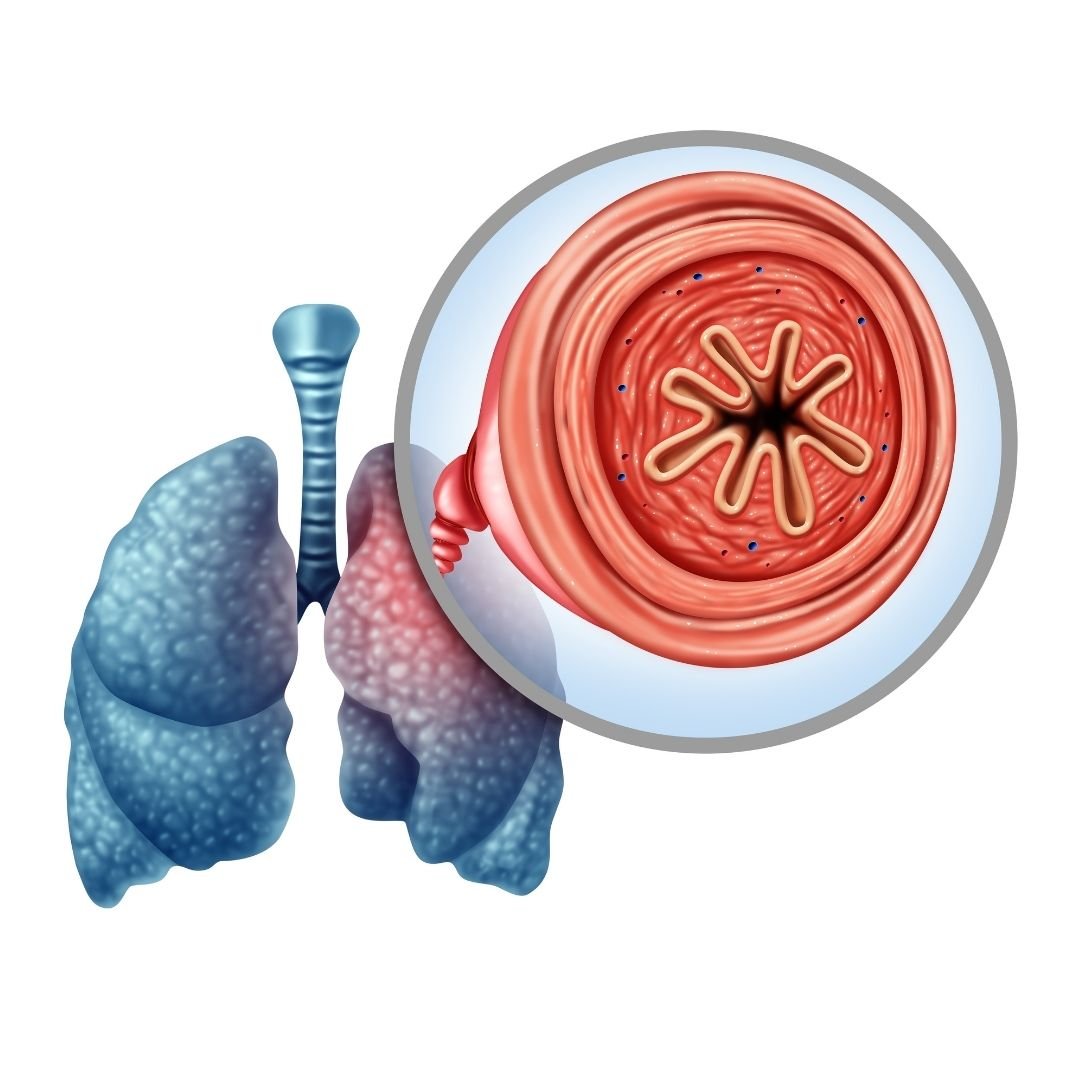
Wheezing is a sound that results from air being forced through a partially collapsed airway. When the same volume of air is being pushed through a smaller area, the velocity of the air increases which creates the sound.
Wheezing noises are often very high-pitched and continuous. Your doctor will be able to determine how many airways are obstructed based on whether the sound is monophonic (one sound) or polyphonic (multiple sounds). Expiratory phase wheezing may be connected to bronchiolar disease whereas inspiratory phase wheezing may be connected to tracheal stenosis.
Rhonchi
Rhonchi are similar to wheezing sounds but they are low-pitch and occur more frequently when the patient is exhaling. They can be an indication that the bronchial tubes or “bronchioles” are thickening due to the overproduction of mucus. Bronchioles are the tubes that lead from the trachea down to each lung. Rhonchi may be a sign of bronchitis or COPD.
Pleural Friction Rub
There’s a thin membrane that coats the outside of the lungs and the inside of the chest cavity called the pleura. The pleura secretes a lubricant that allows the chest wall to expand and contract freely. However, if the pleura becomes inflamed or damaged in some way, they will create a rough, scratchy sound that your doctor can pick up with a stethoscope.
This is called a pleural friction rub, or simply pleural rub. Pleurisy, pneumonia, and lung tumors are the most common causes of pleural rub.
Hamman’s Sign
Hamman’s sign (also called mediastinal crunch) is a crunching sound that occurs when there is air trapped in the mediastinum (the space between your lungs). The crunchy, scratchy noise that it causes is in sync with your heartbeat because the movement of your heart is what produces the noise.
In some cases, Hamman’s sign may mean you have a collapsed lung (pneumothorax) especially if it occurs in conjunction with shortness of breath and chest pain. However, it can also be caused by cystic fibrosis, pneumonia, or COPD.
.jpg)
How Are Respiratory Sounds Treated?
The way that respiratory sounds are treated depends entirely on what type of sound is being produced and what is causing them. This is why auscultation alone is usually not sufficient enough to diagnose a lung condition.
If you don’t have a history of respiratory issues, your doctor might perform further tests in order to determine if a chronic condition is the cause of the respiratory sounds. If you have a chronic disease like COPD, however, your doctor might ask you to increase your medication dosage.
-jpg.jpeg)
In COPD patients, the most common cause of breath sounds is mucus and phlegm that get lodged in the airways when you breathe. Clearing this mucus will not only help you breathe better but can also prevent conditions like bronchiectasis.
This is when you experience recurring lung infections due to bacteria that remain in the lungs for too long. Since lung infections are the most common cause of COPD exacerbation, it’s very important that you and your doctor deal with this problem as soon as it arises.
Medication
If your inability to clear the mucus is due to narrowed airways, your doctor may prescribe you something called a bronchodilator. These drugs open up the airways and prevent the “wheezing” noise whenever you try to cough.
Bronchodilators are almost always administered through either an inhaler or a nebulizer because this allows the medication to reach the affected area more quickly in the event of an emergency.

Controlled Coughing
Another method your doctor may recommend for dealing with blocked airways is breathing exercises or controlled coughing exercises. A normal cough is often erratic and solely focused on expelling as much air as possible.
On the other hand, controlled coughing is more focused on using air more effectively. There are several benefits of this. Firstly, it helps prevent breathlessness, fatigue, or something more serious like a hernia. Secondly, controlled coughing helps prevent the airways from closing which prevents mucus and phlegm from escaping. For more information on this, please read through our post titled “How to Cough Correctly with COPD.”

Smoking Cessation
Whether you’ve been smoking for a few days, a few months, or your whole life, there’s no better time to quit than now. Smoking is the number one cause of preventable illness in the world and there’s also a good chance that it’s causing the respiratory sounds that you’ve been experiencing too.
Smoking damages microscopic organelles in your airways called “cilia.” They are responsible for clearing mucus and phlegm out of the lungs and airways in order to prevent breathing obstruction and infection. In other words, the wheezing or crackling noise you hear when breathing could be caused directly by cigarette smoking.
![]()
When Should You Visit a Doctor?
You should visit a doctor any time that you experience unusual symptoms. While COPD is already associated with shortness of breath, if you notice your breathlessness becoming more severe or you notice wheezing or crackling noises in your chest, you should contact your doctor immediately. You can never be “too careful” when it comes to your respiratory health.
As aforementioned, if mucus or phlegm remains in the airways for too long without being cleared, this leaves you at risk of experiencing a lung infection, the number one cause of COPD exacerbation and hospitalization.

Conclusion
Respiratory sounds alone are usually not a cause for concern. Chances are, you’ve had the common cold before and know what it’s like to cough, wheeze, or experience difficulty breathing. However, if these symptoms become more persistent and last more than a few days, you should visit your doctor. By listening to your lungs, your doctor will have a better idea of what’s causing your symptoms and what further tests are needed in order to diagnose you with a respiratory condition.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
If you’ve been prescribed oxygen by your doctor either for temporary or long-term use, don’t hesitate to reach out to our respiratory specialists here at LPT Medical. We offer state-of-the-art portable oxygen concentrators which are much smaller, lighter, and more reliable than compressed or liquid oxygen tanks. We feature all of the top-rated brands including, but not limited to Caire Inc., Inogen, and Respironics. Simply tell us what your wants and needs are and we will provide you with a list of options that we believe will suit your circumstances.

