Portable oxygen concentrators are state-of-the-art medical oxygen units designed for mobility, reliability, and ease of use. Anyone who has been prescribed supplemental oxygen by their doctor is a good candidate for these units because they enable you to maintain your freedom and independence while ensuring your oxygen needs are always met. In the video above, we unbox one of the most popular portable oxygen concentrators on the market — the Inogen One G5.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Inogen is one of the top manufacturers in the industry, consistently putting out reliable and affordable devices like the Inogen One G3 and the Inogen One G4. Their latest portable oxygen concentrator, the Inogen One G5, introduces some new features and improves upon several aspects of its predecessors such as battery life, oxygen output, and weight. Continue reading below to learn more about what the Inogen One G5 has to offer.
Outstanding Oxygen Output
Millions of people around the world rely on medical oxygen to keep themselves safe and healthy. The problem is that traditional oxygen therapy devices like oxygen tanks are extremely bulky and difficult to maneuver, meaning you need to sacrifice a significant amount of your freedom just to use one. However, the experts over at Inogen were able to craft an oxygen device that’s compact, lightweight, and offers up to 6 oxygen pulse flow settings that you can easily adjust on the fly depending on your needs.

The Inogen One G5 offers more flow settings than any other pulse dose concentrator on the market. What this means for you is that you’ll have more versatility than ever before. For example, if you’re exercising and your blood oxygen levels drop, you’ll be able to increase your oxygen flow to accommodate this change. What’s more, the Inogen One G5 has something called Intelligent Delivery Technology® built into it which closely tracks changes in your breathing and adjusts the oxygen delivery accordingly. You can even use your G5 unit while you’re sleeping!
Ease of Use
These days, technology is progressing at the speed of light and it can feel like a full-time job trying to keep up with everything. So, it’s understandable if you are discouraged by the idea of learning yet another electronic device. However, you might be astonished to find out just how easy the Inogen One G5 is to use. Watch the video above to see how quick and painless it is to unbox the Inogen One G5 and start using it.

On the user interface, you’ll notice that there are only five buttons: one for turning the device on or off; two for adjusting the flow setting up or down; one for notifications; and one for volume. That’s it! There’s no need to spend hours reading through the user manual just to get started. If you want, you can even give one of our respiratory specialists here at LPT Medical a call and we’ll walk you through the basics of your device and answer any questions you may have.
Long-Lasting Battery
Unlike oxygen tanks which need to be refilled daily or weekly, you’ll simply need to charge the battery to keep your Inogen One G5 running. Since the G5 is an electronic device, you can recharge it using any wall or car outlet. There are two different battery options including the 8-cell battery and the 16-cell battery. The 8-cell comes standard with every G5 unit, but you can always upgrade to the 16-cell if you think you’ll need more battery life.

The G5 utilizes powerful lithium-ion batteries like the ones found in modern cell phones and laptops. The smaller 8-cell battery will provide you with up to 5 hours of operating time on a pulse dose setting of 2 while the 16-cell will provide 10 hours of use. If you want to carry more than one battery at a time, you can use an accessory called the external battery charger to charge two batteries at once. This is ideal for people who are on the go or travel frequently.
Approved by the FAA
The Federal Aviation Administration (FAA) oversees safety regulations for commercial flights within the United States. Normally, the FAA does not allow oxygen devices on aircraft because they can be a hazard to passengers. However, the Inogen One G5 is so safe that it has FAA approval for in-flight use. This means that you can finally start traveling across the country or world again to visit friends and family or take a well-deserved vacation. But before you do so, you need to have at least one and a half times the duration of your flight in battery life, and you need to contact your airline at least 48 hours in advance. This will afford you enough time to complete any paperwork that they may require.

Advantages of the Inogen One G5
- It’s compact and weighs under 5 pounds
- It’s reliable and can be used 24/7
- It offers 6 pulse flow settings
- It closely monitors your breathing for optimal oxygen delivery
- It’s approved by the FAA
-
It’s easy to use, clean, and maintain
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}Inogen One G5 Specs
Weight
4.7 Pounds
Dimensions
8.15" H x 7.19" L x 3.26" W
Flow Settings
Pulse Settings 1-6
Sound Level
37 dBA @ Setting 2
Expected Battery Life
Up to 10 hours
Living with a chronic disease like COPD requires making a variety of changes and lifestyle adjustments. You have to pay extra attention to your overall health in order to keep your lungs and body in the best shape possible.
Of all the healthy habits you can pursue, eating a nutritious, wholesome diet is one of the most important and beneficial. It can also be one of the most challenging to commit to, because it requires you to give up some of the junk food and unhealthy snacks you enjoy.
Eating unhealthy foods isn't just bad for your metabolism or waistline, but can also increase your risk for a variety of conditions including diabetes and heart disease. If you have COPD, eating certain foods can even put strain on your lungs and make it more difficult to breathe.
That's why, in this article, we're going to help you get a jump start on a healthier diet by telling you about eleven foods you should avoid when you have COPD. We'll show you what foods to cut down on, what foods to cut out completely, and what foods you can eat as a healthy alternative to junk in your diet.
So, if you want to improve your diet and learn how to avoid foods that can exacerbate your COPD, this article is for you. You'll learn how your diet can affect your COPD symptoms, how to avoid hidden sources of sugar and salt, and how to start putting together a healthy COPD diet plan that works for you.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
The Foods You Eat Can Affect Your COPD
 |
| Image courtesy of FFCU. |
Many people with COPD and other lung diseases don't realize how much their eating habits can affect their disease and its symptoms. But the truth is that there are certain nutrients, and certain types of foods, that can have a noticeable affect on your lung function, energy levels, and how you feel.
When you have COPD, your lungs have to work extra hard to get enough oxygen to all the parts of your body that need it. Certain foods can actually make your lungs have to work even harder, which can make symptoms like breathlessness and fatigue significantly worse.
COPD symptoms are also affected by a variety of foods that can cause indigestion, bloating, or excess mucus production. Certain foods commonly cause gas, bloating, or heartburn, all of which can cause chest discomfort and make it more difficult to breathe. Increased mucus production can obstruct and narrow airways, which worsens COPD symptoms.
If you have COPD, it's important to understand the dietary factors that can exacerbate existing symptoms and affect your lungs' ability to work efficiently. If you know what foods to avoid, you can reduce your exposure to things that can hurt your lungs and start improving your diet for better overall health.
What You Need to Know About Carbohydrates and COPD
Carbohydrates are one of the most important nutrients to pay attention to if you have a lung disease like COPD. The relationship between carbohydrates and lung function is complicated, but it's vital for every COPD patient to be aware of.
First, you have to understand that there is a direct relationship between the foods we eat and gas exchange in the lungs. Gas exchange is, of course, the lung's main purpose: we exhale carbon dioxide gas and inhale oxygen gas.

Carbon dioxide gas is a waste product that comes from our bodies' metabolic processes, like breaking down food. One of the major purposes of our lungs is to get rid of this carbon dioxide waste by expelling it through our breath when we exhale.
The way our bodies work, carbon dioxide waste is a necessary result of turning food into energy that our muscles and organs can use. Everything we eat gets broken down into both nutrients and waste products, and the carbon dioxide waste always has to get processed by the lungs.
However, researchers have found that some foods create less carbon dioxide waste than others when your body breaks them down. This means that these foods create less work for the lungs, because they produce a smaller load of carbon dioxide for them to process.
 |
| . Image courtesy of herlitz pbs. |
Research also shows that eating foods with a heavier carbon dioxide load can actually make your COPD worse. This happens because the lungs have to work harder and use more energy to get rid of all that extra carbon dioxide.
If you have strong, healthy lungs, having excess carbon dioxide waste to get rid of is not usually a problem. However, if you suffer from COPD or another respiratory condition, it can have detrimental effects.
If you have COPD, excess carbon dioxide waste results in reduced lung function, which can cause a variety of COPD symptoms to get worse. It can make you feel extra breathlessness, chest discomfort, fatigue, and even increase your risk for exacerbations.
So, which foods create the most carbon dioxide, and which foods produce the least? According to researchers, the answer lies in the three main food groups: carbohydrates, fats, and proteins.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Carbohydrates Create the Most Carbon Dioxide Waste

Researcher has found that, of all the major food groups, carbohydrates produce the most carbon dioxide waste by far. Because of this, many doctors recommend that people with COPD avoid diets high in carbs and eat more fat and protein instead.
This aspect of a healthy COPD diet is not negligible, and may be more important than many people understand. A number of researchers have studied the direct effects of carbohydrates on people with COPD, and they've found that their effects on lung function are both significant and measurable.
According to one study, COPD patients who had a single high-carb drink had increased symptoms and reduced lung function afterward. Compared to patients that drank a high-fat drink containing the same number of calories, COPD patients who had the high-carb drink required more oxygen, couldn't walk as far, and had extra difficulty breathing during activity.
This suggests that the carbohydrate and fat content of the food you eat can have a huge effect on your lungs, COPD symptoms, and your ability to exercise. If you want to stay healthy and feel your best, you should always be mindful of the nutrient content of the meals you eat and limit the amount of high-carb foods you eat.
Damaged lungs often have enough difficulty meeting the body's basic respiration needs under even the most ideal circumstances. By avoiding carbohydrates and substituting healthy fats and protein instead, you can significantly reduce the amount of strain you put on your lungs and make it easier to breathe with COPD.
Fats and Proteins Have the Lowest Carbon Dioxide Load
Because of the detrimental effects of carbohydrates on lung function, research supports a COPD diet that's high in fat and protein and low in carbs. These foods create significantly less carbon dioxide waste, and are thus easier on the lungs.
Most doctors recommend that people with COPD eat foods with a lot of healthy fats, such as fish, nuts, and moderate amounts of dairy. This ensures that you get enough calories and nutrients to meet your energy needs while creating the least amount of carbon dioxide for your lungs to process.
You should talk to your doctor to work out a well-balanced high-fat, high-protein diet that you can follow. If you are able to stick to it and minimize the amount of carbohydrates you eat, you will likely find that you can breathe easier, exercise longer, and better manage your COPD.
Foods to Avoid if You Have COPD
Once you've talked to your doctor about what a healthy diet looks like for you, it's all up to you to find and prepare healthy foods that will meet your requirements and help keep your body strong. That's when knowing what foods are healthy and unhealthy and what foods to avoid comes in handy.
We've put together the following list to help you identify unhealthy foods in your diet, replace them with more nutritious alternatives, and make healthier choices at mealtime every day. So to kick start your journey to healthier living, here's eleven foods that you should avoid if you have COPD.
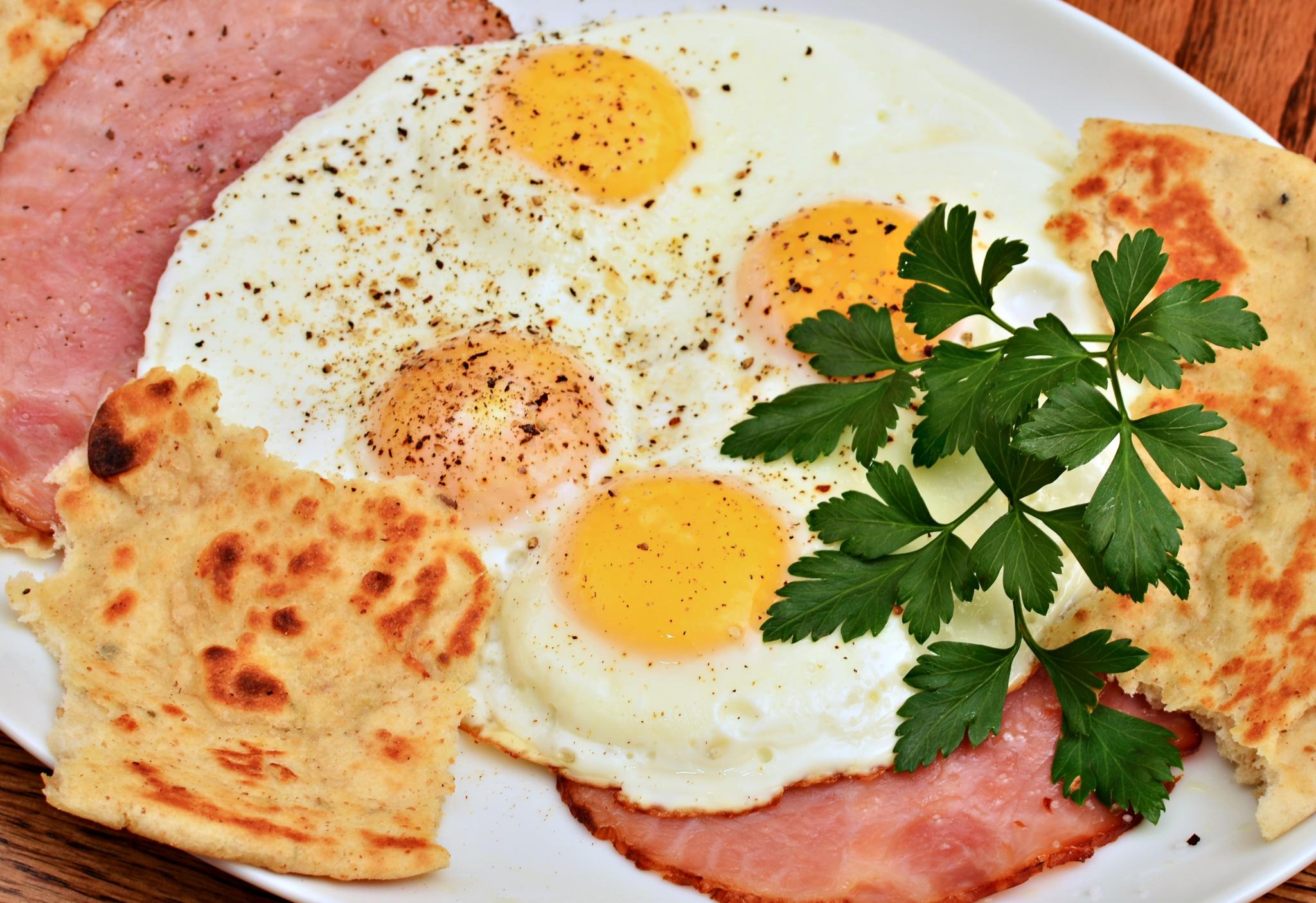
Avoid Processed Meats

Cured and processed meats, such as bacon and ham, are bad for you for a number of reasons. They contain loads of salt, plenty of saturated fat, and can even increase your risk for heart disease, diabetes, and certain types of cancer.
However, processed meats might be particularly dangerous for people who have COPD, according to recent research. Multiple studies have found a link between COPD patients who eat more cured meats and worsened lung function and increased exacerbations and hospitalizations.
Here is a list of cured and processed meats you should avoid:
- Bacon
- Ham
- Corned Beef
- Sausage
- Spam
- Deli Meats
Alternatives to Processed Meats

As an alternative to cured meats, try preparing fresh meats like shredded chicken or baked turkey to use in sandwiches and other dishes. For a quick and easy meat option, use packages of cooked shrimp or canned tuna, instead.
If you're used to packing a quick deli sandwich for lunch every day, you can reduce your processed meat intake by substituting some creative sandwich or salad options on some days, instead. You can experiment with different types of veggie sandwiches and wraps, tuna salad, egg sandwiches, and fruit sandwiches until you find an alternative you like.
Avoid Foods High in Salt

Image By David Dewitt: https://thecozycoffee.com/salt-in-coffee/
Getting too much salt in your diet is bad for your heart and also bad for your COPD. It can also make your body retain extra water, which can make it much more difficult and uncomfortable to breathe.
Even a single high-salt meal can cause bloating and make your COPD symptoms worse. Beware of broths (such as chicken and beef broths), frozen foods, and processed meats, which tend to contain an excessive amount of sodium.
Unfortunately, salt is hidden in a wide variety of everyday foods you wouldn't expect, which is why you should always check nutrition labels. Here are some common sources of excess sodium to avoid:
- Canned foods (including canned beans, vegetables, pastas, and soups)
- Frozen foods (including frozen TV dinners, frozen burritos, and frozen pizzas)
- Salted nuts
- Crackers and potato chips
- Many broths and soups
- Soy sauce and prepackaged marinades
- Instant puddings and baking mixes
- Condiments like mustard and ketchup (in large quantities)
- Pickled vegetables (like olives and pickles)
- Processed cheeses, cheese sauces, and spreads
- Many breads, biscuits, and bread mixes (like pancake mixes, waffle mixes, and Bisquick)
- Canned tomato sauces, salsas, and pasta sauces
- Prepackaged box mixes (e.g. pasta mixes, au gratin potatoes, flavored rice dishes, stuffing mixes, etc.)
Alternatives to High-Salt Foods
Luckily, you can usually find low-sodium versions of many of your favorite foods if you look. You can get low-sodium broths, no-salt-added canned goods, and a variety of salt substitutes at most grocery stores.
Cooking your own meals from scratch at home, however, is the best way to avoid getting too much salt in your diet. When you make your own broths, soups, beans, and raw veggies, you have full control over the ingredients at every step. This makes it much easier to limit the amounts of salt, fat, and other unhealthy ingredients in your meals.
If you often add extra table salt to your food when you eat, try substituting other ingredients and spices, instead. Even though salt is a simple, cheap, and easy flavoring for food, you can make your food much healthier and even more delicious by using salt-free alternatives.
There are hundreds of different spices you can experiment and get creative with, and most are very inexpensive to buy. Try different combinations of flavorings like garlic, onion, paprika, ginger, and other spices, and you'll find that your food doesn't even need the extra salt at all!
Avoid Caffeinated Drinks

Caffeinated, carbonated beverages cause bloating and gas, and are usually overloaded with sugar. They tend to be high in calories, high in salt, and have next to zero nutritional value.
Additionally, caffeine on its own can be problematic for people who suffer from COPD. It increases your heart rate, blood pressure, and breathing rate, all of which puts extra strain on your lungs.
Because of this, caffeine can make it more difficult to breathe and control COPD symptoms like wheezing and fatigue. Doctors recommend that people with the disease limit their caffeine intake as much as possible, especially if it causes their symptoms to get worse.
Alternatives to Caffeinated Drinks

If you're a soda, coffee, or caffeine addict, it can be difficult to quit cold turkey. Caffeine can have very unpleasant withdrawal symptoms, too, including irritability, anxiety, headaches, and fatigue.
It's often easier to cut down or eliminate caffeinated drinks when you do it gradually and replace them with healthier, non-caffeinated alternatives. Try cutting down on your caffeine intake by drinking one less cup per day or per week, that way you have time to adjust and build a healthier habit in the meantime.
Here are some healthy alternatives to caffeinated drinks:
- Fruit- and herb-infused water
- Decaffeinated coffee
- Decaffeinated tea
- Green juices
- Lemon water
- Low-sugar fruit juices (in moderation, ideally with pulp, or diluted with soda water)
Avoid Fried Foods

Despite being a universal favorite, fried foods are some of the most unhealthy foods you can eat. They are chock full empty calories and loaded with large amounts of added oil and fat.
Eating fried foods is bad for COPD because it can give you gas, make you bloated, and make it even more difficult and uncomfortable to breathe. They are also extremely calorie-dense and can make it more difficult to stay at a healthy weight.
You should try to cut fried foods out of your diet as much as possible to stay healthy and reduce your likelihood of experiencing worsened COPD symptoms. Instead, choose healthier baked and grilled options that are lower in fat and easier on your digestive tract.
Substitutes for Fried Foods
The best way to cut fried foods out of your diet is to avoid eating out at fast food restaurants and prepare most of your meals at home. If you do eat out, look for healthier baked or grilled menu items or opt for a light soup or salad instead.
It can be difficult to avoid fried foods like french fries and fried chicken if you're not prepared and don't have other substitutes ready. But you get a little creative, you can always find a healthier and equally delicious way to prepare the same foods that you love to eat fried.
Here are some healthier alternatives to substitute for fried foods in your diet:
Substitute fried meats and veggies for oven-baked, grilled, or steamed versions. This lowers the amount of calories and fat makes them less likely to cause stomach discomfort.
If you're addicted to fries and just can't give them up, try making your own homemade baked french fries from fresh potatoes in your oven at home. You can make them with much less salt and fat than the deep-fried versions at fast food restaurants have, or even use sweet potatoes for extra nutrients.
Avoid Sugary Foods

Sugary foods are difficult to stay away from, but it's worth putting in the effort to cut them out of your diet. Sugars are just empty calories with no real nutritional value, and eating a lot of sugary foods puts you at a greater risk for obesity, diabetes, and heart disease.
It's important to be aware that most processed and prepackaged foods contain a lot of added sugar, even if they aren't foods that you'd think of as being “sweet.” This includes most of the breads, boxed dinners, canned foods, fruit preserves and sauces you can find at the grocery store.
You should also look out for foods labeled as “low-fat” or “gluten-free,” because they are often no more nutritious than the regular version. Stripping the fat or gluten out of a food makes it bland and tasteless, and manufacturers often make up for this by loading their low-fat and gluten-free products with lots of added sugar.
To avoid all of these disguised sources of sugar, always check the nutritional label on the foods you buy. Avoid buying frozen, canned, and processed foods as much as possible and prepare your meals at home, instead.
Sugars are also a major source of refined carbohydrates, which put extra strain on your lungs an make COPD symptoms worse. It's important for people with the disease to limit carbohydrates in their diet, especially refined carbohydrates like sugar, white breads, and pastas.
Here are some common sources of sugar you should avoid:
- Refined carbohydrates (e.g. white breads, pastas, and crackers)
- Store-bought jellies, yogurt, sauces, and dressings
- Store-bought canned pasta sauces
- Breakfast cereals, flavored oatmeal, granola
- Canned soups and beans
- Sodas, fruit juices, sports drinks, coffee drinks, and flavored milk
- Canned fruits and dried fruits
- Many brands of nut butters
- Protein bars and cereal bars
Alternatives to Sugary Foods

Be wary of low-sugar foods that use low-calorie sugar substitutes like xylitol, mannitol, and sorbitol. These sugar alcohols are difficult to digest and cause many people to experience gas, bloating, and diarrhea when eaten in moderate amounts.
The best way to cut sugar out of your diet is to eliminate processed foods and prepare meals from whole ingredients at home. When you do your own cooking, you get to control all the ingredients that go into your food at every step, which makes it easy to cut down the amounts of salt, sugar, and other unhealthy additives.
Here are some common flavoring alternatives that are more nutritious than refined sugar:
- Honey
- Molasses
- Unsweetened applesauce
- Cinnamon
- Lemon or lime
- Fruits (e.g. use cranberries, lemons, blueberries, pureed bananas, etc. as substitutes for sugar in drinks, smoothies, muffins, and other dishes)
- Use milk or cream instead of sugar in your coffee or tea
- Dilute fruit juices with club soda to reduce calories and sugar
Avoid Alcohol (Especially Before Bed)

Alcohol is toxic on a basic level and is not very healthy for anyone to consume. However, if you have COPD, you should be especially careful about when and how much you drink alcoholic beverages.
You should try to limit your alcohol intake as much as possible, but especially at night. If you drink alcohol too close to bedtime, it can disrupt your sleep and even make it more difficult to breathe.
Because alcohol is a sedative, it can make the muscles in your throat to relax too much while you sleep. This narrows your airways and can cause them to collapse together, obstructing your ability to breathe.
Alternatives to Alcohol
If you're used to having a beer or a glass of wine before bed, try having it earlier in the day or replace it with a non-alcoholic alternative. A cup of water, decaffeinated tea, or a glass of warm milk are all soothing options that can help you relax without disrupting your breathing when you sleep.
Another option is to replace alcoholic drinks with non-alcoholic beer or virgin cocktails that mimic the taste. Here are some creative substitutes you can use use instead of liquor to make tasty mocktails at home:
- Vanilla extract instead of bourbon or scotch
- Almond extract instead of amaretto
- Apple juice, apple cider, or white grape juice instead of brandy
- Espresso, coffee syrup, or instant coffee instead of coffee liqueur
- Orange juice, apple juice, or pineapple juice instead of sherry
- Agave juice instead of tequila
- Apricot juice, peach juice, or pear juice instead of cognac
- Orange juice concentrate instead of curacao or triple sec
- Ginger ale or sparkling white grape juice instead of champagne
Foods You Might Need to Limit if You Have COPD
Regular physical activity is a vital part of keeping yourself healthy if you have COPD. Unfortunately, the very nature of the disease makes exercise more difficult, with fatigue and breathing difficulties being some of the major symptoms.
Because of this, doctors have long recommended pulmonary rehabilitation to COPD patients who have trouble staying active or getting enough exercise. Pulmonary rehabilitation classes are designed to help people with breathing disorders learn how to work out and stay healthy while keeping their symptoms under control.
Unfortunately, there are often not enough spaces in pulmonary rehabilitation programs to accommodate every patient who needs to attend. In fact, many patients in rural areas don't even have the option of attending pulmonary rehabilitation without driving many hours from where they live.
Another problem with pulmonary rehabilitation classes is the cost. One study found that the average patient has to pay more than $2,000 just to participate in a single group pulmonary rehabilitation class.
Because of this, many people with COPD and other respiratory diseases who could benefit from pulmonary rehabilitation classes have to do without, either because all the classes in their area are full, there are no nearby programs at all, or because they simply cannot afford the cost. However, researchers have begun identifying alternatives to pulmonary rehabilitation so that more patients with respiratory diseases like COPD can get the treatment they need.
For instance, certain exercise techniques, like Tai Chi and yoga, can be very effective for helping patients with COPD build their exercise tolerance and improve their symptoms. Patients often need help from trained instructors to learn how to exercise well, and attending these types of exercise classes can provide the structure and learning environment that people with COPD need.
While attending an actual pulmonary rehabilitation is still the ideal choice when possible, studies show that techniques like Tai Chi can be just as beneficial for improving your physical health. In this post, we'll introduce you to these techniques and show you how you can use them to improve your fitness, build up your exercise tolerance, and reduce your COPD symptoms.
Tai Chi for COPD

Tai Chi is a lesser-known type of exercise in western countries like the United States, but it has long been recommended to people with COPD for both its mental and physical benefits. It is an exercise style made up of many different “forms,” or poses and movement techniques, that focus on balance, muscle control, and breathing.
The origins of Tai Chi lie in ancient China, where it was originally used as a form of self defense. It is still used today, often as type of gentle, low-impact exercise meant to improve physical fitness and psychological health.
There are many different Tai Chi styles, each of which focuses on a different aspect of the technique. Some forms of Tai Chi emphasize physical strength, some emphasize martial arts, and others put more focus on the meditation and breathing aspects of Tai Chi.
Although Tai Chi is traditionally grounded in the Chinese philosophies of Qi and yin and yang, you don't have to understand or subscribe to these belief systems in order to practice the technique. The exercise techniques alone have been shown to confer a variety of health benefits, especially for people with age-related diseases.
What Makes Tai Chi Special

Tai Chi is considered a wonderful exercise technique for seniors and people with chronic diseases. This is because it uses slow, low-impact movements that are perfect for people with limited strength and physical mobility.
Sometimes described as “meditation in motion,” Tai Chi is known for its integrated mind-body techniques. The different Tai Chi forms are practiced using relaxed, fluid movements that don't stress your muscles and train you to focus on the sensations you feel in your body.
Tai Chi is made up of a variety of different forms, which are individual sets of movements and poses that make up the physical aspect of Tai Chi. Some forms are short and simple, requiring just a few discrete movements at a time, while some are longer and more complex.
Just about anyone can practice Tai Chi, and the techniques can be modified for people with disabilities or people with limited strength and endurance. However, its focus on mindfulness and breathing makes it particularly helpful for people with respiratory diseases like COPD.

Tai Chi not only helps you stretch and tone your muscles, but it teaches you how to manage your thoughts and breathing as you exercise. This makes it a perfect exercise for COPD patients who have trouble exercising without experiencing breathlessness and fatigue learn how to better control their breathing and exercise more effectively.
You can also use the breathing and relaxation techniques you learn from Tai Chi in a variety of circumstances outside of Tai Chi practice. It can help you calm yourself when you feel anxious, steady your breathing when you feel short of breath, and translate the breathing techniques you've learned to other physical activities to reduce your symptoms and increase your endurance.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Studies on Tai Chi and COPD

Health researchers have long been interested in Tai Chi as a form of exercise to improve strength and overall health. More recently, a number of studies have looked at the potential of Tai Chi as a treatment for COPD and come up with encouraging results.
One of the most recent studies, which was published in the journal Chest, found that patients who practiced Tai Chi for twelve weeks showed improvements in muscle strength, respiratory symptoms, and their ability to exercise without feeling breathless. What's more, the patients who did Tai Chi saw just as much improvement, if not more improvement, than patients who attended a standard pulmonary rehabilitation program for the same length of time.
The participants in this particular study used a type of Tai Chi known as the 24-form Yang style, which they practiced for five hours total every week. However, other forms of Tai Chi are also effective, as an academic review of the research on Tai Chi for COPD shows.
A Cochrane review looked at a number of studies on Tai Chi and COPD and found that Tai Chi was just as effective at reducing shortness of breath as standard COPD treatments. And although the evidence for this was not conclusive, the studies also appeared to reveal a slight advantage of Tai Chi over typical treatments, with participants who practiced Tai Chi having slightly better lung function and being able to walk further without feeling too short of breath.

The Cochrane review also found that there were no negative side effects or adverse events from practicing Tai Chi in any of the studies they reviewed. They concluded that “Tai Chi is safe to practice in people with COPD,” although it's still always best to check with your doctor before you starting any new exercise routine.
The American Lung Association also recommends Tai Chi as a form of light exercise and a way to reduce the psychological and emotional stress that many people with COPD suffer. They encourage patients who experience chronic anxiety, fatigue, or frequent COPD symptom flare-ups to try Tai Chi as a way to improve their physical and mental well-being.
Here is a quick run-down of all the major benefits you can get from practicing Tai Chi:
Benefits of Tai Chi
- Teaches you how to regulate your breathing while exercising and doing physical activities
- Puts minimal strain on muscles and joints
- Helps you minimize shortness of breath when you walk and work out
- Can improve your lung function
- Reduces stress and anxiety
- Improves mood and energy
- Improves exercise endurance
- Increases muscle strength and tone
- Increases balance and flexibility
Practicing Tai Chi

If you're interested in trying Tai Chi yourself, the best way to do it is to join a group Tai Chi class. While it is certainly possible to learn and practice it on your own, the help and skill you can gain from having an actual Tai Chi instructor is indispensable.
One of the major benefits of learning Tai Chi in a class is that it gives you the opportunity to get in-person feedback and encouragement. Your instructor can answer your questions, help you learn difficult movements, and correct your form so you learn the proper techniques.
Then, once you've built up your skills to a comfortable level, you will be able to practice Tai Chi effectively on your own. There are even many Tai Chi exercise DVD's and online instructional videos that you can use to and follow along with at home.
As you look around for classes and instructional videos, it helps to know which of the Tai Chi styles you'd like to learn. There are five styles total, but two of them—the Chen style and the Yang style—are the major parent styles from which all the other styles of Tai Chi are derived.
Here's a quick breakdown of the differences between these two main styles to help you as you seek out resources for learning Tai Chi.
The Two Major Tai Chi Styles:
- Chen Style: This is the oldest style of Tai Chi, which is often considered the most difficult. It combines quick, powerful movements along with slow ones and tends to require more strength and skill than other styles.
- Yang Style: This is the most popular form of Tai Chi today and it is practiced as a form of low-impact exercise all across the world. This style uses only slow, flowing movements and is known for its relaxing effects. The 24-form Yang style is a version of this style that uses simpler movements and is more accessible to people with chronic diseases and disabilities.
If you are not familiar with Tai Chi or have limited strength and mobility, you may want to start with the simpler, 24-form yang style. This is the style used in one of the more recent studies on Tai Chi and COPD and is also one of the most common forms practiced in the West.
According to research on Tai Chi and COPD, you should start to see results after about four months of taking classes and practicing at home. Then, if you find that it works well for you, you can continue to use Tai Chi as part of your regular exercise regimen to improve your COPD.
Examples of Tai Chi Forms for COPD

If you think you might be interested in trying Tai Chi, it can help to get a better idea of what it looks like in practice. Here are a few examples of some common Tai Chi movements along with videos to show you how they are done.
Holding Up the Sky
This is one of the most popular Tai Chi forms that is practiced all across the world, and it is a great exercise for beginners. It helps you consciously control your breathing rhythm and put it in sync with your body's movements.
Closing Posture
This form is a great cool-down exercise that can help you relax and steady your breathing. It can also be a great meditative exercise for reducing stress and anxiety.
Windmill Exercise
This Tai Chi form is a slow, relaxing exercise that stretches and tones the muscles in your arms, shoulders, and chest. It can also help you work on your breathing rhythm and open up your chest cavity to give your lungs more room to expand.
Yoga for COPD

Yoga is another form of exercise that studies show can help COPD patients improve their symptoms and their ability to exercise. Similar to Tai Chi, yoga is a thousand-year-old discipline that uses breathing and meditation practices along with low-impact physical activity as an essential part of its practice.
Yoga originally came from India and is made up of two main “pillars”: asana and pranayama. Asanas are the body postures or poses that make up the physical exercise portion of yoga, while pranayama is the deliberate practice of controlling and regulating your breathing.
When most people think of yoga, they think of the asana portion and familiar poses such as “downward facing dog” or the “tree” pose. These poses and the slow, fluid movements you use to transition between them are powerful, yet low-impact exercises that can help you build balance, strength, and muscle control.
However, true yoga practice encompasses much more than the body postures and the flowing movements you use to transition between them. Traditionally, yoga is meant to be a whole-body wellness discipline that promotes mental, emotional, and physical wellbeing.
What Makes Yoga Special?

Yoga is a fantastic exercise for COPD patients because it low-impact, slow-paced, and teaches you how to better control your breathing. Other things that make yoga unique are its mental and meditative practices, which are interwoven with the postures (asanas) and breathing techniques (pranayamas).
The wonderful thing about yoga is that it is accessible to just about anyone, even the elderly and people with chronic illnesses and pain. The different poses, or asanas, are generally simple to perform, and the more advanced positions can be modified for lower strength and skill levels.
The slow, steady movements make most yoga routines easy for people with breathing difficulties to follow without feeling short of breath. However, despite the fact that it is a slow, low-impact exercise, yoga still confers many physical benefits, including better muscle tone, respiration, and cardiovascular health.
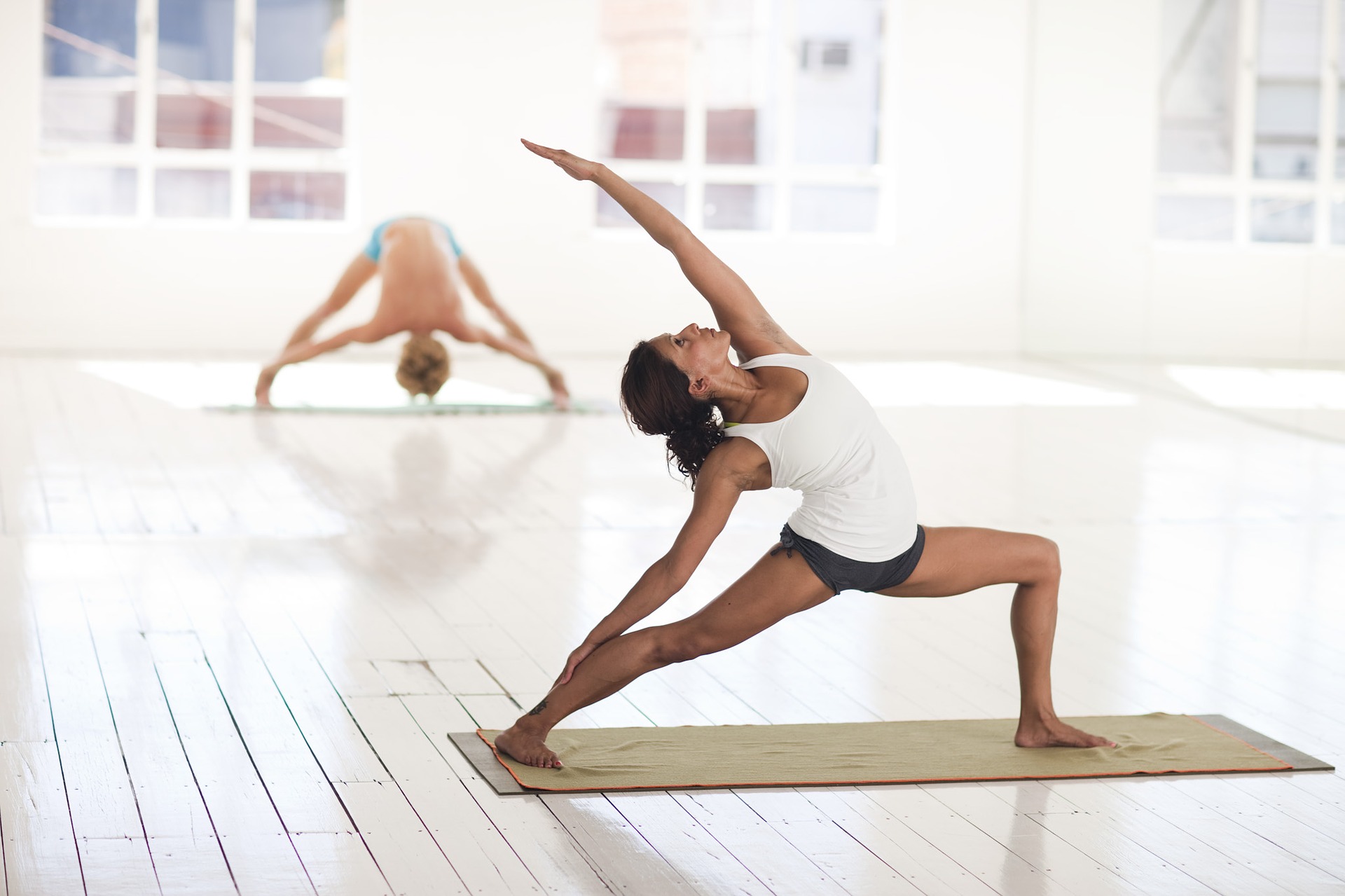
image credit: Ryderwear
The different yoga asanas work out a variety of different muscle groups in your arms, legs, shoulders, back, and core, helping you strengthen your body and improve your balance and flexibility. Some studies even show it can help with chronic pain and cardiovascular disease, afflictions that commonly affect people with COPD.
Pranayamas, on the other hand, are meant to help you observe, control, and extend your breaths in time with your movements, and is one of the major features of the exercise that makes it so useful for people with COPD. Being able to regulate and control the rhythm of your breathing is an important skill that can help patients with breathing disorders strengthen their breathing muscles and reduce shortness of breath.
The mental and emotional aspects of yoga are also represented by pranayama, which trains you to calm your mind and body through deep breathing and meditation. Yogic breathing teaches you to focus your mind on your breaths and bodily sensations and get rid of unnecessary thoughts.
Because of this, yogic breathing is a tool that you can use and practice anywhere to reduce anxiety, clear your mind, and steady your breathing. Whenever your mind feels cluttered with negative thoughts and emotions, or you feel anxious or stressed out, you can use the skills you've built through yogic breathing to relax your body and calm your mind.
Studies on Yoga and COPD

Research on yoga as a potential treatment for a variety of diseases has increased in recent years as the practice has become more popular in western societies. As part of this new wave of interest, several studies have been done to evaluate yoga as a potential treatment for COPD, with very positive results.
The meditative and breathing aspects of yoga, in particular, have been shown to help patients with COPD breathe easier and more efficiently while they exercise. One study, published in the Journal of Cardiopulmonary Rehabilitation and Prevention, found that patients were able breathe more slowly and deeply during yoga lessons.
The most promising result, however, was that patients actually showed improvements in their blood oxygen saturation levels during the yoga sessions. This indicates that yogic breathing could not only help patients control and regulate their breaths, but can also improve their overall breathing and respiration efficiency.
Another study found that practicing pranayama (yogic breathing) alone yielded positive results in patients with COPD. Compared to a control group, who only received pranayama education, those who actually practiced pranayama with trained coordinators showed minor improvements in their walking endurance and lung function measures.

Additionally, yoga as an exercise seems to be particularly suited for people with respiratory diseases like COPD who tend to find other exercises tiring and difficult to do without experiencing shortness of breath. Because of this, some researchers even think that yoga could be an effective alternative to pulmonary rehabilitation. Most agree, at the very least, that the practice represents a “tremendous opportunity” for patients with COPD.
One academic review that looked at a variety of different studies on yoga and COPD concluded that, although the evidence was limited, it all points to the encouraging conclusion that yoga training can improve both lung function and exercise capacity in people with COPD. In the future, researchers hope to develop custom yoga programs that are designed specifically to help people with breathing disorders improve their respiration and overall physical health.
Although most of these are still early studies, they show the real-world potential of yoga and yogic breathing as a tool to treat respiratory disorders like COPD. More research is needed to better understand the effects of yoga and whether or not it is an effective replacement for pulmonary rehabilitation, but for now it seems to be a safe and promising option for patients.
Here is a quick run-down of some of the major benefits you can gain from practicing yoga:
Benefits of Yoga
- Improved lung function
- Improved muscle tone
- Improved balance
- Improved core strength
- Improved range of motion
- Reduced anxiety
- Lower blood pressure
- Increased ability to relax and reduce stress
- Improved quality of life
Practicing Yoga
If you have difficulty exercising and experience frequent shortness of breath, practicing yoga can be an effective way to improve your symptoms and exercise endurance. Especially if you are unable to participate a pulmonary rehabilitation program, finding a reputable yoga class could help you achieve many of the same benefits.
By far the best way to practice yoga is by joining a class led by an experienced practitioner. Even better would be to join a yoga program designed specifically for people with breathing disorders or COPD if there are any options in your local area.
Either way, it's best to start with a group class before attempting to do yoga on your own at home. There's no substitute for in-person instruction; it helps you ensure that you're using the correct posture and positions and allows you to master techniques at a level you couldn't reach without feedback from a skilled practitioner.
Pranayama, in particular, is often considered an advanced technique that most people cannot master without proper instruction. However, once you've become confident in your skill, you should be able to reap many of the same benefits of yoga by practicing it at home.
Some people find that taking regular yoga classes is more fun and effective than doing it alone, and continue to take classes even after they've learned the basics. In most places, you can find many different types of yoga classes with different styles and skill levels, so that anyone can find a yoga class they can learn from, whether they're a beginner or advanced.
If you finish taking a yoga class and decide to give it a go on your own, there are thousands of resources you can use to help you practice yoga at home. You can find plenty of instructional DVD's, YouTube videos, and books that can help you hone your technique an
Staying active is one of the most difficult, yet most important, things you can do to stay healthy with COPD. Regular exercise is not only beneficial for your disease, but it's absolutely necessary for your survival and maintaining a good quality of life.
The good news is that there are plenty of special techniques you can use, and activities you can do, to make exercising with COPD easier and more fun. With the right exercise routine and treatment plan, you can get all the physical activity you need to stay healthy without feeling breathless and fatigued.
Why Exercise is Important When You Have COPD

Regular exercise is necessary for a healthy lifestyle, whether you have a chronic disease or not. But when you have a serious respiratory disease like COPD, regular exercise is a necessity to prevent your disease from getting worse.
Physical activity is just as important for your heart, lungs, and muscles as it is for your psychological and emotional health. It gives you strength, energy, confidence, and is a great mood-lifter, too.
Although you might feel breathless easily when you first start out, regular exercise can actually strengthen your breathing muscles and make it easier to breathe in the long run. Also, getting out your energy through physical activity during the day will help you sleep easier and more comfortably at night.
Staying active will help you feel better, eat better, and increase your overall stamina and endurance. It also helps keep your heart healthy, boosts your immune system, and reduces your risk for heart disease and other complications. But it comes with more than just physical benefits; exercise can improve your mental health, too.
Living with COPD can be stressful and overwhelming, but physical activity can help relieve your worries and stress. Another benefit of staying active that's often underestimated is self-confidence. The satisfaction you gain from seeing yourself make progress and get stronger as you exercise is empowering and invaluable.
How Exercise Benefits Your COPD

It's important to understand that nothing, including exercise, can cure or reverse the severity of your disease. However, it can prevent your COPD symptoms from getting worse, and can slow down the progression of your disease.
Here is a list of some of the most important benefits you can gain from regular exercise when you have COPD:
- Symptom improvement, including reduced breathlessness and fatigue
- Stronger muscles and improved muscle tone
- Improved balance and flexibility
- Better circulation
- Lower blood pressure
- Better sleep and less restlessness
- A healthy weight (and the ability to lose weight, if needed)
- Reduced anxiety and depression
- Stronger bones
- Better self-esteem and self-image
- Increased strength, mobility, and ability to do daily activities
It's hard to overstate the benefits of regular activity when you have COPD. If you have trouble staying motivated, just remember that regular exercise can mean the difference between an early death or a long, fulfilling life with your COPD symptoms under control.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Preventing Progressive Physical Decline
Hopefully, a better understanding of the benefits of exercise is enough to motivate you to get started. However, it's just as important to know the consequences of not exercising and the effects it can have on your COPD.
Here are some of the consequences of not exercising when you have COPD:
- Muscle wasting, weakness, decreased physical strength
- Worsened breathlessness
- Weight gain
- Depression and anxiety
- Loss of independence and increased difficulty with everyday activities
Even if what you have to gain from regular physical activity isn't enough to motivate you, you should understand that you still have a lot to lose if you choose to stay sedentary.
Even if you feel weak and have difficulty breathing right now, it's no excuse to avoid exercise. If it's difficult now, it will only get worse and worse with time if you don't find a way to stay active.
The Basics of Exercising with COPD
Working With Your Doctor
When you have COPD, it's very important that you work with your doctor to put together an exercise routine that works for you. Every person and every case of COPD is unique, and different people might need to focus on different areas of strength.
You should plan to meet with your doctor to discuss physical activity as soon as possible after getting diagnosed with COPD. Make sure to talk to your doctor about all of your symptoms and physical struggles so he can tailor your exercise plan to your needs.
Exercising with COPD often requires special considerations and techniques so as not to make you feel breathless too easily. Make sure you talk to your doctor about how often and how long you should exercise, if there are any activities you should avoid, and if there are medications you can use to make exercising easier.
Exercising at Home
When you have a serious illness that makes it difficult to breathe, it can be hard to make it to the gym on a regular basis. This is especially true if you have decreased mobility or use supplemental oxygen.
That's why many people with COPD opt for exercise routines that they can do at home. It can make it easier to stay motivated, help you stick with a routine, and keeps you close to your medication, supplemental oxygen, and all the comforts of home.
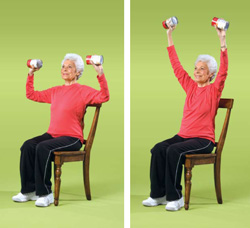
While some people prefer the gym and think that it makes sticking with a routine easier, it's possible to get all the physical activity you need in and around your own home. All you need is an open space to move your body, a chair, and a small set of free weights to do all the exercises you need to stay healthy.
What Kinds of Physical Activities Are Recommended for COPD Patients?
When you have COPD, it's important to start any new exercise routine by taking it slow and setting small, realistic goals. Exercising is safe for your lungs as long as you stay within your doctor's recommendations and limitations, but you should still take care not to overexert yourself or push yourself too hard.
Every person's exercise plan with COPD looks different, and your routine might be more or less intense than other patients' based on your physical condition and the severity of your disease. The important part is to make progress without stretching yourself too far, and to set personal, reasonable goals that you can realistically meet.
That said, there are three things that every healthy exercise plan should include: cardiovascular activity, strength training, and stretching. We'll go through each one by one.
Cardiovascular Exercise

Cardiovascular exercise is a type of activity that includes walking, running, biking, swimming, and much more. It tends to work out large muscle groups and it's all about getting your heart pumping and keeping your body continuously moving.
Regular cardiovascular activity is vital for your heart and lungs and is an effective way to improve your overall tolerance for physical activity. Over time, cardiovascular exercise can lower your blood pressure and heart rate, strengthen up the muscles you use to breathe, and make it so your heart and lungs don't have to work as hard when you're active.
Cardiovascular exercise is also a great way to lose weight and improve your body's overall metabolism. Most doctors recommend getting 20-30 minutes of cardiovascular exercise at least three times a week, but you might need to work up to that amount slowly over time. Also, make sure you talk to your doctor before starting any new exercise routine.
Cardio exercises are usually divided into two groups: high impact (requiring a great deal of exertion) and low impact (requires less exertion). If your COPD is severe or you suffer from chronic pain, you may need to stick with low-impact exercises so you don't push yourself too hard.
Strength Training

Strength training is a kind of anaerobic exercise that includes weight training, abs workouts, lifting, and more. It usually involves standing or sitting in one place and working out one muscle group at a time by flexing and lifting parts of your body.
There are many different benefits of strength training, including increasing your overall strength and endurance and boosting your metabolism. With this kind of exercise, you can gradually build up strength, balance, and endurance and focus your efforts on specific parts of your body that you want to improve.
Strength training exercises are often split up into two more categories: upper and lower body exercises.
Working out the muscles in your upper body is especially important if you have COPD, because it can strengthen the respiratory muscles you use to breathe. Upper-body strength training focuses on the arms, shoulders, neck, chest, abdomen, and back.
Lower-body strength training exercises are also important, because they can improve your mobility by making it easier to stand and walk for extended periods of time. Lower-body exercises include activities that work out your thighs, calves, ankles, and buttocks.
Stretching
Some people do a combination of strength training and cardiovascular training in the same workout, while some people alternate focusing on one or the other on different days of the week. Stretching, however, is something that you should do every day, and especially before every single workout.
Stretching can help you feel better by improving your range of motion, improving your flexibility, and reducing stiffness in your muscles and joints. It's a perfect way to start your day when you get up in the morning or to get your blood flowing when you've been sitting still for awhile.
Stretching is also an important safeguard against getting injured, which is why you should always stretch for 5-10 minutes before beginning any kind of physical activity. You should stretch each part of your body for at least 10 seconds to reduce your chance of muscle strain, soreness, and injury when you exercise.
Warming Up and Cooling Down
Every workout you do should include a brief 5-10 minute warm-up period before your main exercise and a 5-10 minute cool-down session afterward. This helps prevent injury and overexertion, and helps your body slowly adjust to increased activity.
This is especially important to do when you have COPD, so make sure you don't forget these steps.
How to Warm Up
A good warm-up exercise allows you to slowly and gradually increase your heart rate and breathing rate. This reduces strain and pressure on your heart and lets your body get accustomed to the physical activity.
As you do your warm up, start with easy, slow movements and increase your effort and level activity gradually as you go. You should always include at least a few minutes of stretching in your warm-up to loosen up your muscles and joints.
Here are some examples of common, effective warm-up exercises:
- Stretching your legs, arms, waist and neck
- Gently moving your joints, including your ankles, knees, shoulders, and elbows (move them left and right, up and down, and in a circular motion one at a time)
- Walking
- Very light, slow versions of your main workout activities
How to Cool Down
Cool-down sessions are very similar to warm-up sessions, except you want to slowly decrease your level of activity as you go, instead of increasing it. Start by gradually decreasing the intensity of your main workout toward the end, then cool down by walking, stretching, and doing light, low-impact movements.
A good cool-down session will reduce your heart rate and body temperature slowly back to normal and help you feel less sore and fatigued after your workout. Just make sure to decrease your exercise intensity little by little, and don't forget to spend a few minutes stretching your worn-out muscles before you call it a day.
Control Your Breathing
What makes exercising the hardest for people with COPD is the constant threat of breathlessness. If your disease is severe, even short periods of light activity can make it difficult to breathe.
That's why deep breathing techniques are an essential part of exercising when you have COPD. If you can prevent shortness of breath while you exercise, you'll have more energy and endurance to devote to getting in shape.
Make sure to practice breathing exercises and take breaks whenever you feel exhausted or short of breath. If you struggle with breathlessness often, talk to your doctor about pulmonary rehabilitation, supplemental oxygen, or other medications that might help you better control your breathing while you exercise.
It can be overwhelming and difficult to think of what to do when you can't catch your breath, which is why most doctors recommend that you take time to practice breathing exercises every day, even when you don't feel breathless. That way, when the time comes that you are struggling for air, you'll be able to easily remember the steps and bring your breathing back under control.
Pursed Lips Breathing

This breathing technique helps push trapped air out of your lungs and keeps your airways open longer so it's easier to breathe. You should use this breathing technique any time you exert yourself, do any kind of physical activity, or start to feel breathless.
Here's how to practice the pursed lips breathing technique:
- Relax your shoulders and straighten your back
- Take a deep breath in through your nose, making it last about 2-5 seconds.
- Then, purse your lips together, as if you were going to whistle or blow a kiss.
- Breathe out for about twice as long as you inhaled, but through your mouth instead of your nose (about 4-10 seconds).
- Repeat.
Diaphragmatic Breathing
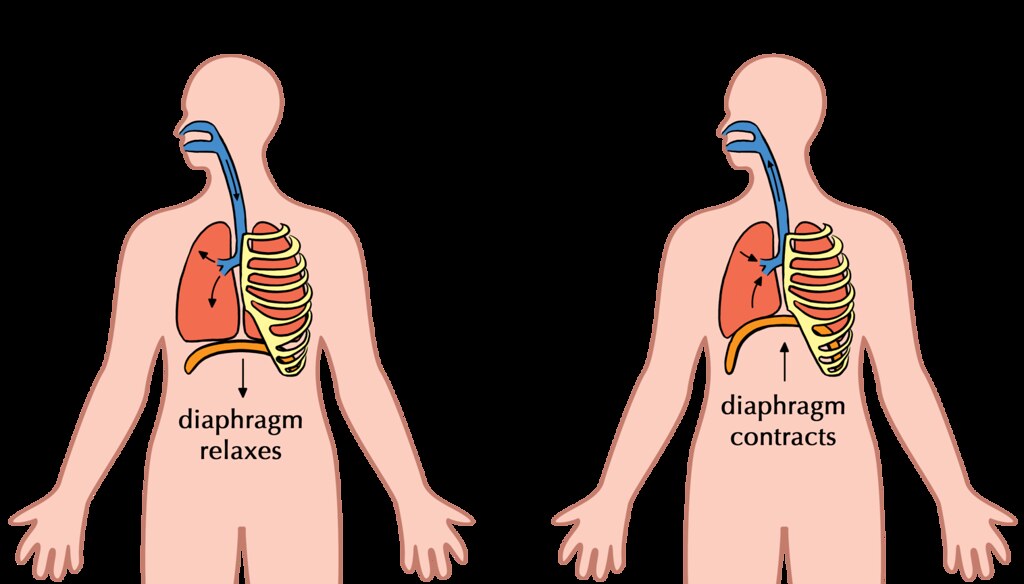
The purpose of diaphragmatic breathing is to help you use your diaphragm, instead of your chest muscles, to breathe. This technique helps you strengthen your diaphragm and use less effort and energy to breathe.
Here's how to practice the diaphragmatic breathing technique:
-
This technique is easiest to practice when you lie down flat on your back, but you can do it while standing or seated as well.
-
Lay one of your hands on your stomach, and the other on your chest.
-
Take a slow, deep breath in through your nose. Pay attention to your hands on your chest and abdomen; you want to feel your stomach rise as you inhale, and your chest to stay still.
-
Exhale slowly through your mouth, again paying attention to how your chest and abdomen move. You should feel your stomach deflate and your chest should stay as still as possible.
- The goal of this exercise is to focus on using your abdomen (diaphragm) to breathe. You should try to keep your chest as relaxed and still as possible, while moving only your stomach when you breathe.
Cardiovascular Exercises You Can Do at Home for COPD
Walking

Walking is a great light, low-impact exercise that's easy to do at home if you have COPD. It's a great way to improve your endurance, and studies show that walking at least four hours per week alone can significantly reduce your risk of heart disease.
The great thing about walking is that you can go at your own pace and it's easy to sit down and take a break whenever you feel tired or breathless. You can get your exercise by walking in your yard or around your neighborhood, or you could go out to a local park or trail for a more scenic stroll.
Here are some tips for walking for exercise when you have COPD:
-
Start small and slow. Don't push yourself too hard at first, but don't give up too easily, either.
-
Add a certain number of feet or steps on to the length of your walk every day (an extra 10 feet a day is a reasonable goal). If you ramp it up gradually, you will steadily get stronger with hardly any extra effort.
-
To control your breathing, exhale through pursed lips for about twice as long as you inhale. It can help to count the number of steps you take while you breathe in, and then take twice as many steps as you breathe out. This is a great way to get a steady rhythm going so you can keep control over your breathing.
- Make sure to turn around soon enough or walk a short enough loop that you can make it back to where you started before you get too fatigued. Don't be afraid to stop and rest any time you feel too tired or breathless, and don't start again until you are breathing normally.
Aerobics

You've probably heard of aerobics classes before; you can usually take them at your local gym or you can follow along with an aerobics training video at home. Even though they had their peak in the 80's, aerobics video routines are still an extremely effective, engaging way to get a good workout.
You can purchase aerobics workout DVDs or get a free aerobics workout by watching any of the many videos available on YouTube and elsewhere online. The best thing about it is that there are so many different kinds and lengths of aerobic workouts. You can tune in to a short ten-minute routine or a 30-minute one, or you can string several short aerobic workouts together with rests in between.
You can do dance aerobics, step aerobics, water aerobics, strength-training aerobics, and more. Aerobic workouts can be extremely satisfying and fun, and you're bound to be able to find a style that fits your interests.
Stair Climbing
Stair climbing is a moderate-intensity activity that you can do at home or any place with a set of stairs. Just make sure you have a handrail to stabilize yourself and stop to take breaks whenever you feel out of breath.
It's important to control your breathing, so practice slow, pursed-lips breathing as you do this exercise.
Tips for Stair Climbing with COPD
- Take a deep breath in before you start ascending the stairs.
- Take two steps up while you exhale slowly through pursed lips.
- Take another breath in and rest a moment before continuing
- Take another two steps up while you exhale again
- Descending the stairs isn't nearly as difficult, and you should be able to take more steps with each breath. Start on the inhale and count how many steps you can take down as you breathe in. Then, try to take twice as many steps down on your exhale as you breathe out slowly.
- Take your time! It's not a race or a contest, and it's okay to take it as slowly as you need to. You'll build up strength with time, but you have to start at your own pace.
Other Aerobic Exercises for COPD
We've listed some of the most common physical activities you can do to get a good aerobic workout with COPD. This is only a small list, however, and the possibilities for aerobic exercise are nearly endless!
Here are a few more ideas for aerobic activities you can do at home with COPD:
- Jogging or Running (high impact)
- Biking (low impact)
- Jump Roping (high impact)
- Playing with pets or children (low impact)
Strength Training Exercises You Can Do at Home

Strength training encompasses a large variety of stationary workouts that flex and strengthen your muscles. Many of these are exercises that don't require any extra equipment, and use simple movements and the weight of gravity to work out your body.
Some home strength training require, or are enhanced, by using free weights. You should start small, with 3 or 5 pound weights, and add more to your collection as you move up to more weight.
Yoga

Yoga is one of the best possible strength training exercises you can do with COPD. Why? Because it's slow-paced, great for your heart, and helps you practice steady, deep breathing while you exercise.
Yoga involves involves slow, steady movements and holding poses that help you build up muscle strength and improve your balance. Practicing controlled, deep breathing is also an integral part of yoga practice, which is particularly helpful if you struggle with breathlessness.
Yoga can help you build the strength you need to do even more kinds of exercise and can help you train yourself to control your breathing whenever you do physical activities. To practice yoga at home you can use yoga DVD's or you can access a huge number of yoga instructional videos online and on YouTube.
Chair Exercises

Many of the techniques we'll show you in the following sections “Upper Body Exercises” and “Lower Body Exercises” can be done as chair exercises. That means you can do them while sitting upright in a chair, and they're a great way to get some extra strength training in without having to leave your seat.
All chair exercises are exercises you can do at home, and they allow you to work out your muscles without having to expend energy to walk or stand. This can help reduce breathlessness and fatigue when you exercise, and is a great solution for people with COPD who have limited energy

In both developed and undeveloped countries around the world, it is estimated that 9-10% of people are affected by Chronic Obstructive Pulmonary Disease (COPD). Experts have made a prediction that by 2020, it will be the third leading cause of death in the world as the population ages and people continue to smoke. More than 12 million people have been diagnosed with COPD in the United States alone and it is the third leading cause of death claiming more than 120,000 American lives each year.
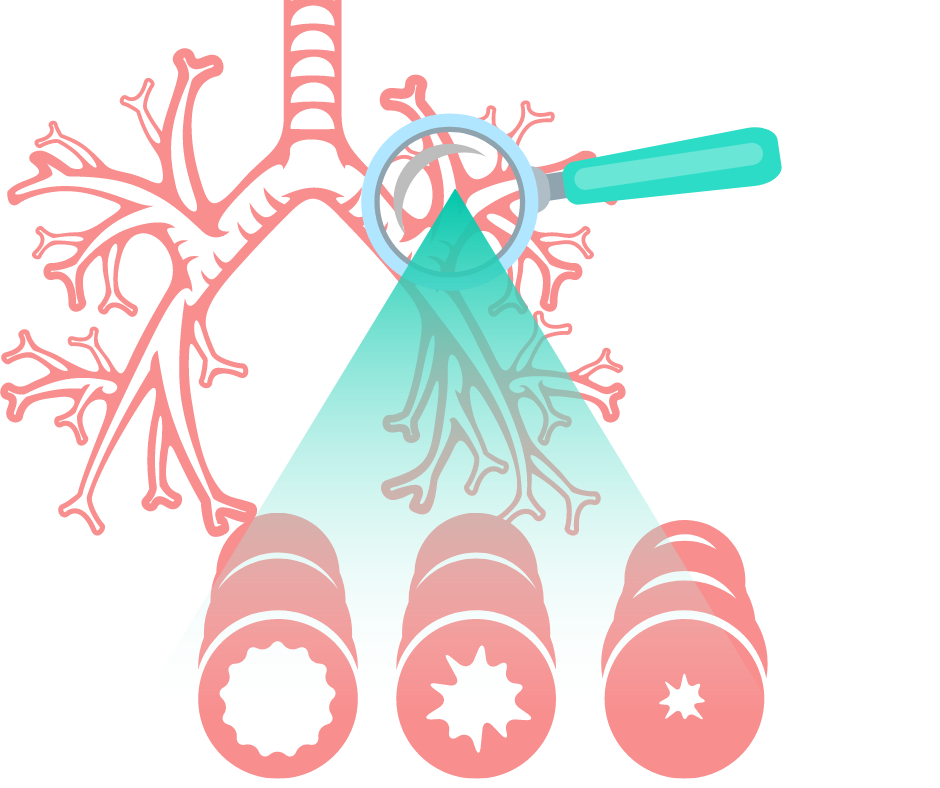
COPD is an umbrella term used to describe progressive lung diseases including chronic bronchitis, emphysema, refractory asthma and some forms of bronchiectasis. It is mainly characterized by shortness of breath. In its initial stages, COPD may show no symptoms or have very mild symptoms but as the disease progresses, the symptoms usually become more severe.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Physicians have traditionally measured the severity of COPD by the amount of air a person can forcibly exhale in one second (FEV1). The amount of air usually decreases as COPD becomes worse. Just the same, COPD affects other systems and body parts, which helps provide clues about the severity of the disease. A lot of physicians are now using the BODE index to categorize COPD and predict outcome. BODE is short for body-mass index, degree of airflow obstruction, dyspnea (breathlessness), and exercise capacity as measured in a 6-minute walk test.
You are probably familiar with COPD classic symptoms which include;
- Frequent respiratory infections.
- Lack of energy.
- Chronic cough with production of a lot of mucus.
- Experiencing shortness of breath, especially with physical activity.
- Chest tightness.
- Wheezing or hearing a whistling sound when you breathe.
- Blueness of the lips or fingernail beds.
You however may not be aware of the potential common complications associated with COPD and how you can limit them. Below is a list of 6 complications that you may face with COPD.
1. Cor Pulmonale

This refers to a failure of the right side of the heart. It is a condition in which the right side of the heart swells up (lower extremity edema) and cannot pump blood properly. COPD makes the heart work harder, especially on the right side which pumps blood into the lungs. Due to poor gas exchange in COPD, there are reduced amounts of oxygen in the blood causing blood vessels to constrict. Many of the capillaries around the alveoli are destroyed in the disease process making the heart work even harder for blood to be forced through fewer constricted blood vessels. Because of all this effort, the right ventricle swells up, the walls of the heart become thicker, and the chamber over time loses its ability to contract efficiently.
Symptoms of cor pulmonale include fainting spells and discomfort in the front of the chest. To control your symptoms your doctor may recommend a low-salt diet, medication or supplemental oxygen. If you are an active cigarette smoker, you should plan to quit. You should also engage in mild to moderate physical activity to build up heart and lung stamina. Remember to consult your doctor before you start any exercise regimen.
2. Pneumonia

Pneumonia is a lung infection that can be caused by a bacteria or a virus, and can lead to respiratory failure in patients with COPD. COPD weakens the respiratory system increasing vulnerability to pneumonia. Because people with COPD already have weakened airways and a worse immune system, the likelihood of them to die from pneumonia is higher than that of patients without COPD.
Symptoms of pneumonia usually include coughing, a fever, and having a difficult time breathing. Pneumonia is more common in COPD patients that take steroids for their symptoms. You should consider talking to your doctor about getting a pneumonia vaccine if you have not already gotten one.
One dose is usually enough for most people, a second dose may be suggested for some, including those that have been using steroids for a long time. Antibiotics can also be used to treat pneumonia caused by bacteria. Streptococcus pneumonia is the most common cause of bacterial pneumonia in patients with COPD. To reduce the risk of getting infected, you should;
- Drink plenty of fluids especially water, to maintain healthy bronchioles while thinning out mucus and secretions.
- Quit smoking.
- Wash hands consistently.
- Avoid contact with people you know are ill.
- Discourage sick family members and friends from coming to visit your home.
Overall good health is key to preventing infections.
3. Depression

Shortness of breath that limits your activities can have you feeling down in the dumps and lead to loss of interest or pleasure in activities. Having this feeling every once in a while is okay but when you feel this way frequently then you may be undergoing depression. One study estimated that 40 percent of people with COPD suffer from depression.
Depression can lead to the worsening of your physical symptoms because you may not fell like exercising and feeling low all the time might make it hard for you to follow your treatment plan.
You may even turn to alcohol, cigarette smoking or any other unhealthy habits to help you cope with depression which can lead to more harm to your body. Do not ignore how you are feeling and talk to your doctor about this so that they can get you the help that you need. Signs to look out for include;
- Feeling guilty or worthless.
- Being overly sensitive to criticism.
- Feeling hopeless or suicidal.
- Having trouble falling asleep or staying asleep.
- Having trouble making decisions and concentrating.
- Lethargy and lack of motivation.
Your doctor may recommend antidepressant medication or talk therapy. You may also decide to join a support group with other COPD patients or a pulmonary rehabilitation program to help you fight depression.
4. Osteoporosis

This is a complication that sometimes occurs with COPD causing the weakening of the bones. Bones are made with living tissue and as older bone tissue breaks down, new bone tissue is created. When the nutrients in the body are not enough to create new bone tissue, the bones may become weak and fragile, and when this occurs, the risk of getting fractures is greatly increased. Although no exact reason can be given by researchers on the coexistence of COPD and osteoporosis, some theories for what the cause may be include;
-
Cigarette smoking – some researchers believe that some chemicals in cigarette smoke cause changes in the body, and these changes include genetic changes that may cause bones to become weak and slow to heal.
-
Corticosteroids – these are commonly used by COPD patients to control COPD flare-ups and to reduce airway inflammation, and a common side effect of corticosteroids is osteoporosis.
- Low vitamin D levels – people with COPD may opt to stay indoors and lack of exposure to the sun, causing low levels of vitamin D. Low vitamin D levels have been linked to poor bone growth and skeletal mass, which may contribute to osteoporosis.
Your doctor can check your bone health with a bone density scan. You may need prescription medicine along with calcium and vitamin D supplements to keep your bones strong. You may also want to exercise as research has shown that progressively harder weight-bearing exercise, such as strength training can boost bone health. Consult your doctor before you start any exercise regimen.
5. Trouble sleeping

It is very common for people diagnosed with COPD to have trouble sleeping. In fact around 50 percent of COPD patients face this problem. This is a problem because getting enough sleep is vital for all body functions to work properly.
Sleeping problems linked with COPD include; low levels of oxygen during sleep, sleep apnea, depression, medication used to treat COPD symptoms and some of the COPD symptoms like coughing and wheezing.
You should let your doctor know if you are experiencing trouble sleeping so that he can figure out what is causing it and then treat it. A few things you can do to help with this problem include:
- Keep the room that you sleep in cozy, dark, cool and quiet.
- Practice airway clearance techniques throughout the day and right before you sleep to remove secretions in your airways.
- Ask your doctor if night-time use of supplemental oxygen is an option for you.
- Review the medicine that you are using with your doctor to see if it has any side effects. You may require an adjustment.
- Talk to your doctor about non-invasive positive-pressure ventilation (NIPPV) such as CPAP if you suffer from sleep apnea or other sleeping disorders.
- Try not to drink caffeinated beverages late in the day or avoid them altogether.
- Do not sleep lying flat. Elevate your upper body with pillows to help facilitate breathing.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
6. Pneumothorax

Pneumothorax, which is also referred to as a collapsed lung, occurs when a hole develops in the lung, allowing air to escape into the space around the lung causing the lung to partially or completely collapse.
People diagnosed with COPD are at higher risk of getting pneumothorax because the structure of their lungs is weak and vulnerable to the development of these types of holes. It can be caused by an injury to the lung, rib fracture, certain medical procedures and in some cases air pressure changes for example high altitude.
Signs to look out for include sudden sharp chest pains that worsen when you take a deep breath, rapid heartbeat, chest tightness, and cyanosis caused by lack of oxygen.
Pneumothorax can be treated by inserting a chest tube between the ribs into the space between the lung and the chest wall to help remove the air and re-inflate the lung. The chest tube stays in place for a number of days as the patient recovers in hospital. In some rare cases, surgery is required to prevent future occurrences.
If you have COPD, the first sign that something was not right was likely feeling shortness of breath, to the point that you wanted to see your doctor about it. It also could have been that incessant cough throughout the day and night.
It's easy to blame a cough on allergies or a common cold, but if it persists and becomes a regular thing, you should see your doctor to discuss the possibility of having COPD or another lung ailment. The sooner you find out if it is COPD causing your symptoms the sooner you will be able to treat the chronic illness, thereby slowing down the progression of your COPD.
The first thing that you need to understand is that coughing may seem like a symptom you want to relieve, but in the case of COPD, it actually serves a function.
Continue reading to understand how COPD and coughing are related, what you can do to ease a cough, and when to seek medical attention.
How are COPD and Coughing Related
If you have COPD you probably experience a persistent cough. This symptom is related to a condition of COPD called chronic bronchitis, which means that your airways are constantly irritated. This irritation is often caused by smoking or second-hand smoke, but it can also be caused by other irritants and biological factors, such as pollution or genetics.
The irritation in your airways causes two problems that prevent enough air from passing through to the lungs:
- The lining of your airways become swollen
- There is too much mucus produced by your lungs
People with chronic bronchitis can have a persistent cough because it is important to regularly clear their swollen airways of this excess mucus, which can sometimes be difficult and require extra attention and treatments, of which, we will discuss in more detail in the What you can do to ease a cough associated with COPD section of this article.
So, coughing caused by COPD is often productive and it is a natural function of your body that plays an important role in your breathing system. Coughing helps to move extra mucus out from your lungs. Coughing is also a reaction that can help remove certain irritants you may inhale into your lungs, like dust, pollution, and other common allergens.
When your cough produces mucus, which is also called sputum or phlegm, that means your body is working correctly to clear the excess mucus up through your swollen airways and into your throat and out of your mouth.
It is normal for the mucus to be clear or white, yellow, or green in color but if the mucus is very mucky, it may be a sign of a respiratory infection. We will go over this in more detail in the When you should see a doctor section
What you can do to ease a cough associated with COPD
To determine whether or not your cough needs to be treated with medication or other remedies, depends on the type of cough you are experiencing and whether or not your cough is actually helping to clear your lungs and airways.
You should consult with your doctor to determine the type of cough you are experiencing and how to deal with it going forward.
As we discussed in the section above, airway clearing coughs serves a meaningful purpose by clearing out mucus from your airways. In this case, it is best for you to continue coughing in order to avoid mucus building up in your lungs.
.png)
That being said, there are certain medications you can take as well as techniques you can learn how to perform in order to couch more effectively.
COPD and coughing medications
If your cough is due to very thick mucus, first you should try to drink more fluids. This can help make your mucus thinner and easier to clear. If this does not work well enough, then there are medicines called “expectorants” that can help make the mucus easier to cough up.
If your coughing becomes painful or difficult to control. In those cases, your doctor might recommend cough suppressants that keeps your body from coughing. These suppressants might also be used for coughs that do not produce mucus, like a dry smoker’s cough.
If you have COPD, coughing can also cause a “bronchospasm” or “spasm.” This happens when your muscles around your airways suddenly tense up causing your airways to become very narrow, This makes it even hard to breathe. To reduce coughing that causes spasms, healthcare providers might prescribe special types of inhaled medications called “bronchodilators” or inhaled steroids.
.png)
If you are not interested in getting on medication for you coughing, there are also three airways clearing techniques you can do to clear your lungs
Airway clearing techniques for COPD
One of the most effective ways to clear your airways is to use the effective, or controlled, cough technique. This cough comes from deep within your lungs and has just enough force to loosen and carry mucus through your airways without causing them to narrow or collapse. By utilizing the controlled coughing practice, you will save energy and therefore, oxygen.
- Controlled coughing: A type of cough that comes from deep in your lungs. It loosens mucus and moves it though your airways
- Postural drainage: You lie down in different positions to help drain mucus from your lungs
- Chest percussion: You lightly tap your chest and back. The tapping loosens the mucus in your lungs
To cough effectively:
- Sit on a chair or on the edge of your bed, with both feet on the floor. Lean slightly forward. Relax
- Fold your arms across your abdomen and breathe in slowly through your nose. (The power of the cough comes from moving air.)
- To exhale: lean forward, pressing your arms against your abdomen. Cough 2-3* times through a slightly open mouth. Coughs should be short and sharp. The first cough loosens the mucus and moves it through the airways. The second and third cough enables you to cough the mucus up and out.
- Breathe in again by "sniffing" slowly and gently through your nose. This gentle breath helps prevent mucus from moving back down your airways
- Rest
- Perform again if needed
Here is a link to postural drainage and chest percussion treatment and how to perform these mucus clearing techniques.

Natural home remedies for helping reduce COPD induced coughing
Eucalyptus oil
Eucalyptus oil contains a natural compound called eucalyptol. Eucalyptol may have the following benefits for people with COPD and may ease uncomfortable coughing symptoms:
- antioxidant and anti-inflammatory properties
- opens up the airways in the lungs
- reduces mucus production
- helps clear mucus from the lungs
- prevents flare-ups in moderate to severe COPD
One way you can use eucalyptus oil is by adding 12 drops of eucalyptus oil to 150 milliliters of boiling water and inhaling up to three times per day.
This will not work for everyone, and if you experience any side effect of the oil, stop using it immediately.
-1.png)
Quit Smoking to reduce dry coughing
Smoking is the leading cause of COPD in the United States and is responsible for around 90 percent of COPD-related deaths.
Tobacco smoke is known to irritate your airways and your lungs. Smoke causes inflammation and obstruction within your airways causing them to narrow, and making it very difficult for air to pass in and out.
If you smoke, the most important step to reduce COPD related symptoms and slowing down the progression of your COPD is to stop smoking. Quitting will put an end to “smoker’s cough,” the dry, hacking cough common among people who smoke.
A deep, productive cough that clears the airways of mucus may replace this dry cough also benefiting you and your breathing.
-png.png)
When you should seek medical attention
Call your doctor within 24 hours if you notice:
- You’re out of breath or coughing more than usual
- Being out of breath affects your daily routine
- You’re coughing up more gunk that normal
- The mucus you are coughing up is dark yellow, dark green, or rust-colored
- You have a fever over 101 F
- You feel dizzy or lightheaded
If you begin to experience any of these symptoms it could mean that you have a respiratory infection or your COPD is getting worse.
Call 911 or go to the emergency room if you’re still out of breath after using the medicines your doctor has prescribed for your COPD.

Other symptoms associated with COPD
One of the other many symptoms of COPD we mentioned very briefly in this article was shortness of breath. When you have COPD your lungs are no longer able to process oxygen like they once did. This is partly due to the irritation in your airways that also causes coughing.
Both chronic bronchitis and emphysema can cause shortness of breath. This symptom is also called “breathlessness” or “dyspnea".
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
If you airways are swollen and filled with mucus, not only does this initiated a coughing reaction, but it also inhibits oxygen from flowing through your lungs and into your blood stream and organs.
Not only is this feeling extremely uncomfortable, it is also life threatening, and if it goes untreated for a long period of time, you will inevitably be taking years off of your life.
Here are positive changes you can make to improve breathing with COPD:
Learn pursed-lip breathing This is a breathing exercise designed for people with COPD: Purse your lips and blow as much air out as you can before taking a deep breath in through your pursed lips again. Then slow down your breath so that you’re using as much of your lungs as you can. This technique slows your breathing rate and helps to keep your airways open which can also help to reduced coughing episodes.
Drink plenty of water because water helps thin out mucus so you can clear it better. Some people with COPD have conditions that could be made worse by extra fluid, however some people with COPD may be very dehydrated.Speak with your doctor to find out how much water you can safely drink.
Get informed and continue learning about COPD and how your lungs function. This can help you better understand and manage your condition. Pulmonary rehabilitation programs often offer this type of education.
Exercising regularly can make a big difference in your breathing capabilities and COPD symptoms. A lot of people with COPD get more and more out of breath as their disease progresses, but it’s not due of their lung function — it's because they’re not conditioning enough. Most doctors recommend walking for people with COPD since it’s moderate in intensity and easily accessible.
Know and avoid your triggers. If you have COPD and allergies, take steps to avoid anything you’re allergic to. This may mean putting dust covers on your pillows and mattress or keeping your pets out of the bedroom. High-efficiency particulate air filters can remove dust and other irritants from the air in your home. You may also consider a humidifier if dry air triggers your symptoms.
Get your rest Many people with COPD have an underlying sleep disorder, like sleep apnea, that makes it difficult to get good sleep. When you sleep better, you’ll feel better and breathe better, so if you are not able to fall asleep, or have trouble staying asleep, speak with your doctor to understand the root of this issue so you can solve it.

Stay on a healthy diet full of nutrient-dense foods is needed with COPD to maintain strength and fight off infections. Eating healthy can help you lose weight and breathe easier. If you’re underweight, ask your doctor about the best foods to eat and if nutritional supplements are right for you.
Take your medication COPD medications can help manage symptoms, including shortness of breath so be sure you’re taking the right medications and get evaluated to make sure your lung function is as good as it can be
If you have severely low oxygen levels this is called hypoxemia, your doctor will likely prescribe you medical-grade oxygen, for home oxygen therapy. Long-term oxygen therapy has many benefits if it is used correctly and It can even help you live longer.

Low oxygen symptoms of hypoxemia vary depending upon how severe your COPD is, and how severely it affects you. If you experience any of the symptoms listed below, contact your doctors as soon as possible. If you experience more than one of the following symptoms at one time, seek medical attention immediately:
- Confusion
- A sense of euphoria
- Restlessness
- Headache
- Shortness of breath
- Rapid breathing
- Dizziness, lightheadedness and/or fainting spells
- Lack of coordination
- Rapid heart rate
- Elevated blood pressure
- Visual disturbances
- A bluish tint to the lips, earlobes, and/or nail beds (cyanosis)
Hypoxemia is the main reason that people with COPD and other lung diseases are prescribed supplemental oxygen. There are a few forms of home oxygen therapy: You can opt for liquid oxygen tanks, gas cylinder tanks, or the most popular, convenient, and cheapest option a portable oxygen concentrator.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
If you are a good candidate for long-term oxygen therapy, this is a blessing in disguise. While it might seem as if you lung function is declining, once you are able to utilize oxygen, your quality of life will improve drastically. When you have adjusted to the oxygen therapy, you will begin to slow the progression of you COPD as well!
Once you find the right POC for you, your bones and muscles will feel stronger and energized, you will have improved exercise tolerance, your mood and stamina will boost, your quality of sleep may improve, and so much more.

If you feel like you have experienced any of the symptoms of hypoxemia, and are curious how to find the best portable oxygen concentrator to fit you oxygen requirements, fill out the blue box to the right, it is our official guide to portable oxygen concentrators.
Cough with a Purpose
Remember, COPD-related lung damage can’t be reversed, but it can be controlled if treated properly.
Now that you understand that your cough can in fact be beneficial for your health and in treating COPD, we hope that you can use the information in this article to cough effectively and efficiently. These coughing techniques, mixed with medication and other home remedies should reduce the dry uncomfortable smokers cough, and help you to cough with a purpose.
Even though this can be a pain, always feel free to excuse yourself during social gatherings, and other outings to clear mucus from your lungs and airways. This will allow you to go longer without coughing and spend more quality time with the ones you love while enjoying the things you like to do.
The more you practice these coughing techniques the more efficient you will become at clearing your airways, and therefore breathing!
If you have any questions please leave a comment on this blog below, and always feel free to share our blog with your friends and family. By explaining how beneficial your cough is for managing your COPD, they will better understand and be willing to help and encourage coughing rather than trying to help you avoid it.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!














