
While COPD is usually characterized as a breathing disorder, it is a complex disease that can cause a variety of different ailments besides respiratory decline. One of of these is back pain, a serious ailment that afflicts nearly fifty percent of patients with COPD
Back pain caused by COPD can be mild or severe, and in extreme cases even debilitating. It can be acute and short-term, or it can be chronic, lasting for days or months at a time.
Besides being plain painful, back pain can interfere with your daily life and make it difficult to continue your normal routine. If severe, it can even interfere with your COPD treatment and leave you unable to exercise and do other things that are important for your health.
Luckily, back pain is very treatable, and there are many simple things you can do in your daily life to minimize your back pain. In this guide, we're going to introduce you to a variety of natural techniques and practical methods you can use to get relief.
Whether it's acute or chronic, most types of back pain can be reduced with healthy habits and lifestyle changes like exercise, posture, and diet. That's why it's so important to examine your everyday habits and lifestyle to identify things that might be contributing to your pain.
If you don't start treating your back pain now, it may only get worse over time. That's why it's important to take action now, before the pain takes an even greater toll on your life and your ability to manage your COPD.
Instead of waiting it out or assuming your back pain will go away on its own, learn what kinds of actions you can take in your daily life keep your back healthy and strong. In this article, we are going to help you do just that, by helping you understand why COPD causes back pain and how you can use a variety of simple methods to treat your back pain at its source.
Understanding Back Pain and COPD

Back pain is a very general symptom that can have a variety of different causes. But if you have COPD, your back pain could be directly or indirectly caused by your disease.
COPD-related back pain tends to be chronic and also tends to affect the lower back. In fact, research shows that more than forty percent of people with COPD experience chronic lower back pain.
COPD patients can suffer from any type of back pain or a combination of multiple kinds at once. Here is a quick overview of the main types of back pain and how to recognize them.
Acute Back Pain

Acute back pain is usually defined as short-term back pain lasting for less than six weeks. It is usually caused by injury or trauma and resolves relatively quickly.
Many people feel acute back pain as a sharp pain or dull ache. The pain can be minor or it can be severe enough to affect your daily life, making it difficult to move, work, and sleep.
Chronic Back Pain
Chronic back pain is back pain that lasts longer than six weeks and doesn't get better on its own. It can be caused by inflammation, strain, or injury and doesn't usually get better on its own.
Chronic back pain is often in the lower back and feels like a deep aching or burning. It tends to travel from your back to your hips and legs and get worse when you stay still for long periods of time.
Mechanical Back Pain
Mechanical back pain is any kind of back pain caused by a mechanical injury to your muscles or spine. That includes pain from strain, accidental injuries, poor posture, and other physical causes.
Inflammatory Back Pain

Inflammatory back pain is, in a way, more chemical than it is physical. It is caused inflammation inside your body that damages the tissue of your muscles, bones, and/or joints in your back.
Back pain caused by inflammation is often chronic and gets worse when you sit for too long or don't get enough physical activity. Chronic back pain is usually more difficult to relieve and manage than acute or mechanical back pain, and the most common treatments are exercise and anti-inflammatory drugs.
How COPD Causes Back Pain
Osteoporosis
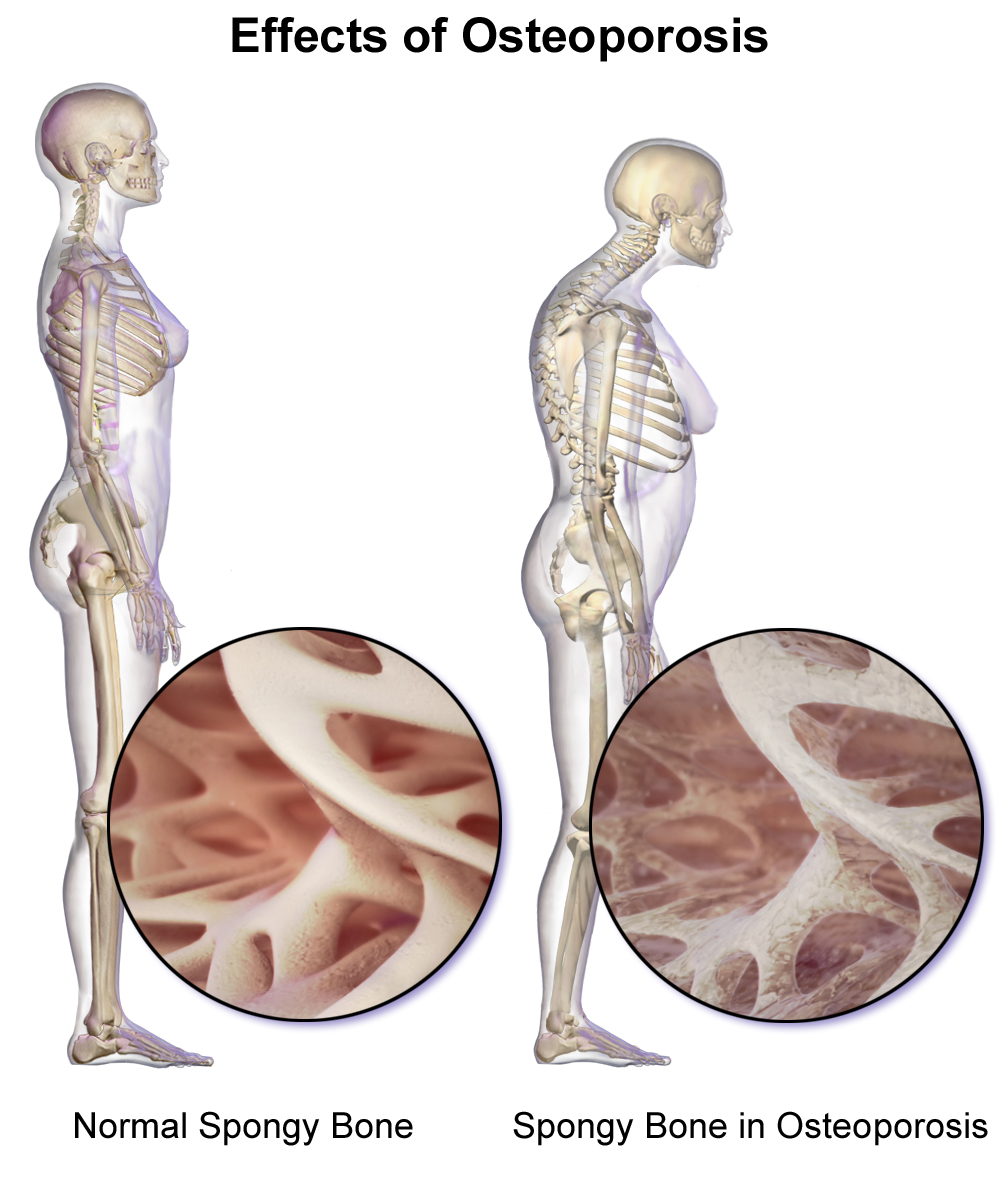
Osteoporosis is a common cause of back pain in people with COPD. You can get osteoporis if you don't eat enough calcium, which impairs your body's ability to build and repair your bones.
As a result, your bones become very thin, weak, and brittle. They can become so weak, in fact, that a minor bump, fall, or even normal activities and movements can cause your bones to break.
Most people don't notice any symptoms in the early stages, but osteoporosis can cause severe pain as it progresses and causes invisible injuries. This pain usually stems from tiny cracks, breaks, and compression fractures that patients often don't even realize they have.
The most common causes of osteoporosis-related back pain are spinal compression fractures, which usually cause a more severe kind of back pain. This type of injury tends to hurt most when you stand, walk, twist, and bend, and tends to lessen when you lie down.
Osteoporosis is particularly common in COPD patients, who often struggle to get enough nutrients from their diet—including calcium—because of how the disease affects their bodies. COPD patients also tend to avoid exercise, which weakens your bones and can lead to bone-related back pain.
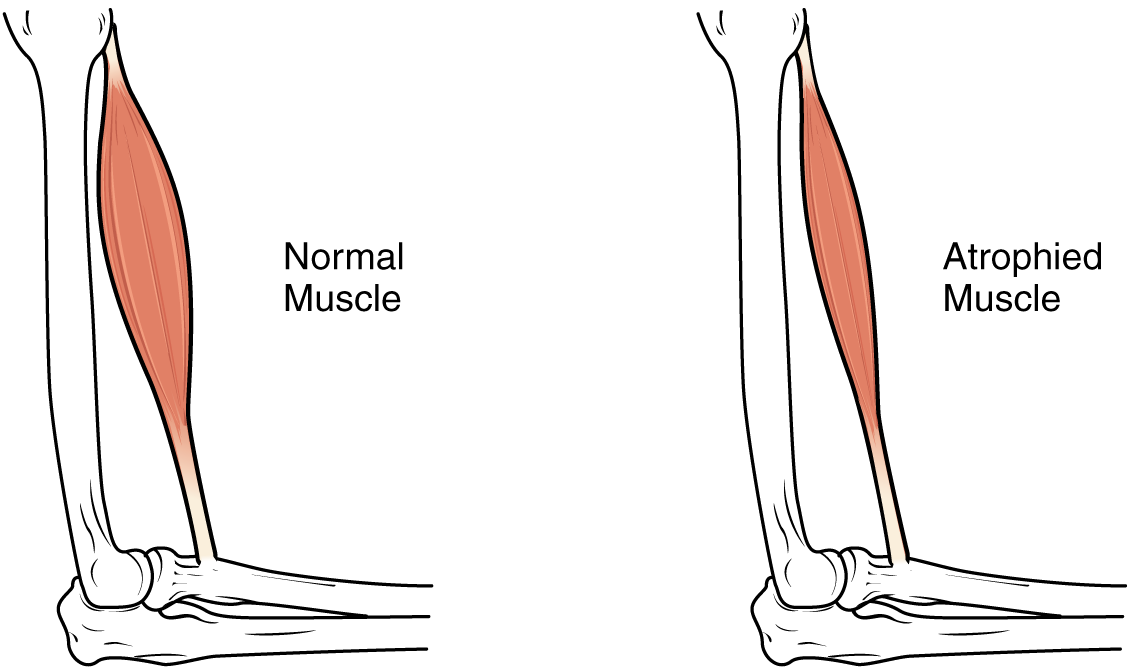
Lack of Physical Activity (Muscle Atrophy and Disuse Syndrome)
Not getting enough exercise is another major factor that makes people with COPD more prone to back pain. This is a risk for patients with advanced COPD, in particular, who often find it difficult to stay active because of their severe physical and respiratory symptoms.
Not getting enough physical activity causes your muscles to break down (atrophy) and can even weaken your bones and joints. It also hurts the flexibility of your back, which can cause stiffness and pain when you move.
Unfortunately, many people avoid exercise when they have back pain, which can end up making it even worse. This can start a vicious cycle where lack of physical activity causes back pain, and untreated back pain can causes patients to avoid physical acitivity even more.
Patients that live too sedentary a lifestyle can also develop disuse syndrome, a disorder that stems from not using your body enough. It can lead to back pain, other chronic pains, cardiovascular disease, and mental disorders like anxiety and depression.
Chronic Inflammation

One of the most direct ways that COPD can cause back pain is through chronic inflammation. This happens when your immune system's inflammatory response stays active all the time, which is a very common symptom of COPD.
Chronic inflammation wears down your body and can cause a variety of serious health conditions, including heart disease and depression. Another side effect of chronic inflammation is chronic pain, including chronic back pain, which you may feel in your muscles, bones, and joints.
Inflammatory back pain is different from mechanical back pain, and can be a sign of arthritis. While mechanical back pain usually comes from physical injury to the muscles and bones in your back, inflammatory back pain is the result of inflammation in the joints of your spine.
Back pain caused by inflammation lasts for at least three weeks and is usually felt most in the lower back. In severe cases, it can lead to a type of arthritis called ankylosing spondylitis, which can affect a variety of joints in your body, and can even cause sections of your spine to fuse together in its later stages.
Inflammatory back pain gets worse when you don't move around for long periods of time and improves with movement and exercise. It doesn't get better with rest and tends to be more severe in the morning after you've been lying in bed all night.
How to Treat Back Pain from COPD
If you have COPD and suffer from back pain, you don't have to suffer in silence. There are many different options for treating back pain, including home treatment, medication, and implementing new habits in your daily life that support a healthy back.
Practice Good Posture

Bad posture can both cause back pain and make existing back pain worse. It can cause muscle strain and stiffness, compress your bones and joints, and lead to variety of back aches and pains.
On the other hand, good posture supports your spine and the muscles in your back so they don't get tired or strained. By adjusting your posture, you can relieve existing back pains and prevent more pain in the future.
People with COPD are particularly prone to bad posture because of their respiratory symptoms and tendency to avoid exercise. Because of this, it is particularly important for you to watch your posture if you suffer from COPD.
Sleeping posture, in particular, is a problem for many people with COPD. One reason for this is that lying down on your back puts extra weight on your chest, which makes it more difficult to breathe.
One solution to this is to sleep on your side, which many patients find makes it easier to breathe and sleep at night. However, to keep your spine aligned and prevent back pain, you should also put a small pillow between your knees.
Another common posture issue among people with COPD is bending over at the waist whenever they feel short of breath, because they feel it makes it easier to breathe. However, you can breathe just as well and prevent unnecessary back pain by practicing breathing exercises in an upright posture.
If you suffer from back pain and COPD, don't underestimate the power of good posture to improve how you feel. Changing your posture habits can not only relieve your back pain, but it can improve a variety of other symptoms of COPD.
To learn more about how your posture can affect your COPD, visit our guide on how to improve your COPD with good posture.

Here are some more tips for practicing proper posture to reduce back pain with COPD:
Good Standing Posture:
- Stand completely upright with your shoulders parallel to your hips and feet.
- Bend your knees slightly and place your feet slightly apart at about shoulder's width.
- Keep your shoulders pulled back, yet relaxed. Do not let them slump forward.
- Keep your chin parallel to the ground.
- Put your weight on the balls of your feet and shift from one foot to another if needed.
Good Sleeping Posture
- Sleep with a good-quality, firm mattress and pillow.
- Sleep on your back or on your side, but avoid sleeping on your stomach.
- If you sleep on your back, put a small pillow under your knees to help keep your spine straight.
- If you sleep on your side, put a small pillow between your knees to keep your hips and spine aligned.
- Consider getting a special pillow or mattress designed to aid with good sleep posture or back pain.
Don't Stay Sedentary

Many cases of back pain are caused by lack of physical activity, which is something that people with COPD often struggle with. Exercising with COPD symptoms can be very challenging, and too many patients simply give up and settle into an unhealthy, sedentary lifestyle.
However, being inactive leads to even more problems, including back pain, disuse syndrome, and worsened COPD symptoms. The more sedentary you are, the worse your symptoms will get, and the more your aches and pains will multiply.
This happens because, when you don't get enough exercise, your muscles atrophy and get weaker and stiffer; this can lead to both long-term and short-term back pains. Additionally, as your back muscles lose strength and tone, they also become more prone to cramping and injury.
The solution to this is getting more physical activity and doing exercises that limber up and strengthen the muscles in your back. Regular exercise will not only protect your back from injury, but it can even relieve your back pain significantly.
Regular activity is especially helpful for your back if you live a sedentary lifestyle or suffer from inflammatory back pain. In those cases, getting more movement and exercise is perhaps the single most effective thing you can do to reduce your pain.
In order to keep your back in good shape, make sure to get at least 20 minutes of moderate physical activity at least three times per week. It also helps to get up at regular intervals throughout the day to stretch your back, shoulders, and spine.
Exercise Your Back

Many different kinds of physical activities can relieve pain and pressure in your back. Anything that gets your body moving can help, including stretching exercises, strength training, and cardiovascular activities like walking or biking.
Stretching and strength training exercises are particularly helpful for loosening up your back muscles and strengthening the muscles that help support your back. Muscle groups to target include your abdominal muscles, hamstring muscles, and the muscles in your upper and lower back.
For the best results, you should do strength training exercises at least four times a week in sets of 3-5 repetitions. It may take some time to see results, but you should notice an increase in strength and a decrease in pain within about six weeks of starting exercise.
It is normal to feel some pain and discomfort when you first start working out and strengthening your back. However, you should be careful to start small, take it slow, and stop if it makes your pain worse.
It helps to start out with low-impact exercises like walking, stretching, and water aerobics that won't over-stress injured muscles and joints. Abdominal muscle exercises are another great place to start because they are simple to do and they help support your back.

Personal hygiene is one of those things that everyone knows is important, but few actually take seriously enough. For most people, hygiene is simply a routine part of life, not something they go out of their way to think about pay attention to.
But if you suffer from COPD, it's important to make good personal hygiene a top priority in your daily routine. Proper hygiene is your very first line of defense against illnesses and dangerous COPD exacerbations that can make your disease even worse.

LPT Medical's newest and most impressive portable oxygen concentrator, the ARYA P5 portable oxygen concentrator
However, practicing good personal hygiene takes more effort than most people think. Doing it right takes extra time out of the busy day, and it's very tempting to cut corners to save time.
That's why everyone should take the time to review the important components of good personal hygiene now and then. If you have COPD, then you have even more at stake, and you should take extra care to learn all the proper techniques.
In this post, we're going to show you what good personal hygiene looks like and how it can help you protect your lungs and manage your COPD. This guide will discuss a variety of important hygiene issues, both general and COPD-specific, and help you learn the skills you need implement good hygiene practices in your everyday life.
Why Hygiene is So Important for People with COPD
Most people understand the basics of good hygiene, but not everyone is great at practicing it consistently. Even so, imperfect hygiene is not usually a problem for most healthy adults.
However, good personal hygiene is much more important for people who suffer from COPD. The disease suppresses patients' immune systems, which makes them particularly vulnerable to disease-causing germs like viruses and bacteria.
Even worse, it can be very dangerous to get even a little bit sick if you have COPD. Respiratory illnesses, in particular, can wreak havoc on your lungs and immune system, making it much more difficult to breathe and control other COPD symptoms.
That's why practicing good hygiene is so vital; it protects you from the germs, bacteria, funguses, and respiratory irritants that cause you to get ill. You can't always control whether or not you get sick, but practicing good personal hygiene is one of the few effective things you can do to reduce your risk.
Even minor viruses like the common cold can worsen breathing problems significantly and permanently damage your lungs. Because of blockages and narrowing in your airways, COPD also makes it harder to flush viruses and bacteria out of your respiratory tract.
This significantly raises your risk for secondary lung infections like pneumonia if you get sick. COPD also makes it more difficult to recover from illnesses and infections.
In this way, COPD not only causes you to get sick more often, but also causes you to stay sick for a longer period of time. Unfortunately, one of the consequences of staying sick longer is an increased probability of minor illnesses causing serious infections and permanent damage to your lungs.
In the most serious cases, getting sick when you have COPD can lead to respiratory failure, hospitalization, and even death. That is why it is so important to practice impeccable hygiene if you suffer from COPD.
The Benefits of Good Hygiene

The main benefit of good hygiene is a significantly reduced chance of getting sick. That's because, when you practice good hygiene, you prevent a myriad of disease-causing pathogens like viruses, bacteria, and parasites from making it into your body.
Good personal hygiene is also good for those around you because it prevents you from spreading germs and sicknesses to other people. By practicing good hygiene, you can help protect other people with immune-suppressing diseases like COPD and prevent them from getting illnesses that could potentially threaten their lives.
Along with these physical benefits of good hygiene, there are social and psychological benefits as well. When you keep yourself clean, healthy, and groomed, you are likely to feel more confident and capable in other ways, as well.
Here are some of the main benefits of healthy hygiene habits:
- Improved overall health
- Reduced risk of disease and infections
- Reduced exposure to allergens and other respiratory irritants
- Reduced risk of COPD exacerbations
- Reduced risk of hospitalization
- Reduced risk of spreading germs and illnesses to others
- A cleaner, healthier living environment
- Improved confidence, self-image, and self-esteem
- Other people see you as more healthy, desirable, and attractive when you have good hygiene
What Does Good Personal Hygiene Look Like?

You probably already know the basics of good hygiene like bathing and washing your hands. But there's also a good chance you don't know, or have forgotten, the details of what good hygiene entails.
Still, knowing the basics works well enough for most people most of the time. At worst, most healthy adults will only get a mild illness every so often if they expose themselves to germs.
However, living with COPD means you can't cut any corners without putting your health in serious risk. That means you need to go out of your way to practice impeccable hygiene, even if you've gotten away with an average amount of effort so far in your life.
But to do that, you need to understand what good hygiene is and exactly what you have to do to practice it. Fortunately, practicing good hygiene is relatively easy to do and even simpler to learn.
The basics of good personal hygiene include:
- Knowing when to wash your hands
- Knowing how to wash your hands properly
- Knowing how to prevent yourself from spreading germs to others when you are sick
- Knowing how to avoid transferring germs to your body in public places
- Knowing how to practice good dental hygiene
- Knowing how to clean your body and your clothes to prevent germ buildup
How to Practice Good Hygiene to Improve Your COPD
In this guide, we're going to give you a refresher course on how to practice good personal hygiene. We'll also address a variety of personal hygiene issues and challenges that affect people with COPD specifically.
In these next sections, we will go through each important hygiene issue step by step so you can learn the proper techniques. We'll also give you tips for how to practice good hygiene every day and fit important hygiene practices into your daily routine.
Learning the tips and techniques we explain in this guide will help you ensure that you are doing everything you can to protect yourself from sickness and disease. That way, you can live your life more safely, more confidently, and with a reduced risk of serious COPD complications.
Wash Your Hands Often

Even though washing your hands might seem like obvious advice, it is so essential to personal hygiene that it's still important to review. It is the first step to practicing good hygiene and one of the most effective ways you can protect yourself from disease.
Unfortunately, most people are not as diligent about hand-washing as they should be, even knowing how important it is. Many people remember to wash their hands before eating or going to the bathroom, but get lazy or forget to do it in other situations.
Another problem is that most people don't take enough time to wash their hands thoroughly enough, which makes their hand-washing less effective. As a result, their hands may still harbor harmful bacteria even after washing up.
How to Wash Your Hands the Right Way

If all you do is rub your hands together with soap while giving them a quick rinse under the faucet, then you're not washing them well enough. In fact, if it takes you less than a full twenty to thirty seconds (count it!), then you probably need to correct your technique.
Here is a quick overview of proper hand-washing technique, as recommended by the CDC:
- Use clean, running water to rinse and wet your hands before applying soap.
- Rub the soap between your hands until it forms a lather.
- Scrub your hands for at least twenty seconds, getting your nails, wrists, and between your fingers.
- Rinse off all the soap under clean, running water.
- Dry your hands off on a clean towel.
To wash your hands properly, you need to make sure you scrub every part of your hands thoroughly with soap, including your fingers, fingernails, palms, wrists, between your fingers, and the backs of your hands. Any kind of regular, non-antibacterial soap will do the trick, including bar soap, liquid soap, and foaming soaps.
You may need to wash the skin above your wrists and further up your forearms after cleaning, washing dishes, or doing anything else that is likely to fling bacteria around. If your hands are especially dirty, you should also use a nail brush to scrub around and underneath your fingernails to remove excess dirt and grime.

Here are some more tips for more effective and hygienic hand washing:
- Avoid antibacterial soaps and hand sanitizers: Using antibacterial soaps and hand sanitizer is almost never necessary because regular soaps and sanitizers are effective. Additionally, anti-bacterial soaps are bad for the environment, and may even be bad for your health.
- Keep your hand towels clean and dry: If your hand towel stays moist for too long, it creates a perfect environment for mold and bacteria to grow. Let your hand towels dry thoroughly between uses and wash them regularly, especially if you notice a bad or musty smell.
- Don't re-contaminate your hands: After you get your hands all clean, you don't want to have to start over again. That's why you should be careful not re-contaminate them right away by touching a dirty faucet or door handle on your way out of the bathroom. When using a public bathroom, cover your hand with a tissue if necessary to avoid touching dirty public surfaces.
To see proper hand-washing technique in action, check out this video from the CDC.
When to Wash Your Hands

You probably already know that you should wash your hands before and after eating and after you use the bathroom. However, there are many other situations that call for thorough hand-washing, and some are less obvious than others.
In general, you should wash your hands after completing any activity that puts you in contact with germs. That includes anything that involves handling dirty items, touching public surfaces, or coming into contact with someone who is sick or injured.
Here is a more complete list of situations in which you should wash your hands:
- Before and after handling food
- Before and after eating
- Before and after treating a wound
- Before and after touching your face, especially your eyes, nose, and mouth
- Before and after caring for a sick person
- After sneezing, coughing, or blowing your nose
- After using the bathroom
- After changing a diaper or handling pet waste
- After touching a pet or other animal
- After touching another person
- After handling garbage or waste
- After touching a public item or surface (like a public pen or ATM)
- After smoking
Use Hand Sanitizer

Sometimes, you won't have access to a sink when you need to wash your hands. In case this happens, it's a good idea to keep hand sanitizer with you whenever you leave the house.
For the best protection, you should always use alcohol-based hand sanitizers instead of antibacterial ones. To be effective, your hand sanitizer should contain no less than 60 percent alcohol.
These hand sanitizers can kill the majority of bacteria and fungi on your hands as well as many viruses. The higher percentage of alcohol the sanitizer contains, the more effective it will be against all kinds of microbes.
However, hand sanitizer only works effectively if you use it right. If your hands are greasy or grimy when you apply hand sanitizer or you wipe the solution off too soon, then you won't get its full protection.
But even though it can be good in a pinch, hand sanitizer is not a good substitute for hand-washing in all cases. Using hand sanitizer is not nearly as effective as washing your hands, and you should only use it as a backup for times when hand-washing is not an option.
Here are some tips for using hand sanitizer correctly to protect yourself from illnesses and infections:
- Use hand sanitizer by pouring a dime-sized dollop into the palm of your hand and rubbing the solution thoroughly into your palms, fingers, and the backs of your hands.
- Make sure you don't have dirt, oils, or grime on your hands before applying hand sanitizer, otherwise it may not be effective.
- Once the solution has been absorbed into your skin, let your hands air dry. (Don't wipe your hands off; it should only take a few seconds for the solution to dry on its own.)
- Do not rely on hand sanitizer to clean harmful chemicals like pesticides off your hands.
Bathe Often for Healthy Skin and Lungs

No matter how careful you are to avoid germs, your body inevitably picks plenty of them up from your environment throughout the day. When you go outside, cook, clean, and sweat, you are exposed to all sorts of bacteria, fungi, and other harmful particles that stick to your hair, clothes, and skin.
<

COPD is a relatively common and well-researched condition, which means there are lots of different medications and treatments to help people who suffer from the disease. These include a variety of "natural" treatments for COPD patients that can alleviate both physical and psychological symptoms.
Natural COPD treatments are non-pharmacological treatments that you can take control of yourself. They are opportunities to make changes to your personal habits, health routines, and nutrition to more effectively treat your COPD symptoms at home.
In this post, we're going to introduce you to a number of natural treatments that you can use to improve your COPD. We'll show you how supplements, lifestyle changes, and other natural solutions can help you better manage your symptoms and improve your quality of life.
By helping you take a more well-rounded approach to your health, natural treatments can boost your physical health, mental health, and help you avoid serious health complications from COPD. Using natural treatments can also help you feel more in control of your health and your overall well-being.
The treatments we discuss in this guide are generally safe, accessible, and effective, as long as they are used in combination with standard treatments for COPD. Continue reading to learn more about a variety of natural COPD treatments and what they can do for you.
What is a “Natural” Treatment?

It's important to understand that “natural” is a word that means many different things to different people. It doesn't have any definite scientific or legal definition, which is why it's important to specify what we mean when we refer to a treatment as “natural”.
In this guide, we use “natural” to refer to treatments that don't rely on medical equipment or standard pharmaceutical medications. Instead, the natural treatments we will discuss are the kinds that don't require a prescription or significant supervision from a doctor.
These natural treatments, which include things like nutritional supplements, mind-body exercises, and healthy lifestyle changes, are still recommended by doctors and supported by many in the medical community. This is key, because you should never try to treat your disease with unknown or unsupported treatments.
It's also vital to understand that these natural treatments are not alternatives to taking your prescription medication and should never be used as a replacement for proper medical care. Unfortunately, there is no real replacement or “alternative” to medical COPD treatments, and you should never use any natural treatments that interfere with your primary COPD treatment plan in any way.
The “standard” treatment for COPD, which includes medication, lifestyle changes, and other medical treatments, has been carefully crafted and tested by medical experts. It is still the best known way to manage COPD, and the only known way to slow down the progression of the disease.
However, there are still a variety of natural techniques that you can use to improve your COPD symptoms and your quality of life. Doctors often recommend these natural options, in addition to standard treatments, as a means for their patients to better manage and cope with their disease.
Many people with COPD also appreciate natural treatments because they give them a stronger sense of ownership and involvement in their health. They allow you to take certain aspects of your treatment into your own hands, giving you a better sense of control over your disease.
Natural treatments also help you stay focused on important non-physical aspects of your life, such as your mental and emotional health. In this way, it can expand the scope of your treatment and ensure that you cover all your bases when it comes to your physical and mental well-being.
Natural Treatments for COPD

Now that you understand what a natural treatment is, let's take a closer look at what these treatments actually are. In the next sections, we'll introduce you to a wide selection of the most effective natural treatments you can use to improve your COPD.
Nutritional Supplements

A large number of people with COPD struggle to maintain proper nutrition. Often, this is a result of poor appetite, poor diet, or severe COPD symptoms that make it difficult to eat.
This is exacerbated by the fact that many COPD patients need extra calories to fuel their breathing muscles, which have to work overtime to help them breathe. This need for a high-calorie diet makes it much easier for people with COPD to become malnourished.
Another nutritional problem results from the fact that COPD tends to affect people later in life, when living a healthy lifestyle is often a struggle. At the same time that their bodies are especially vulnerable to nutritional deficiencies, many older adults struggle to get enough nutrients from their diet.
That's why many people with COPD take nutritional supplements to keep their brain, lungs, and the rest of their body strong. These supplements not only prevent nutritional deficiencies and help you manage your COPD symptoms, but some may also help stave off serious diseases and other health complications.
The nutritional supplements we discuss in this section could be beneficial to many COPD patients, but will not be useful to everyone. And remember, you always need to talk to your doctor before making any changes to your diet or nutrition.
When possible, it is best to get your nutrients from a well-balanced diet instead of a supplement. However, taking nutritional supplements is a helpful and often necessary way to ensure you get all the nutrients you need every day.
What's more, studies show that some supplements can even help patients who don't have nutritional deficiencies improve their COPD. What works for you will depend on your individual physiology, your symptoms, and what your doctor recommends.
Calcium
Because many patients suffer from bone density loss, calcium is important for people with COPD. Calcium is the primary nutrient responsible for keeping your bones healthy and strong, and getting too little causes bone loss and osteoporosis.
Getting enough calcium is particularly important for people with COPD, who are more prone to osteoporosis. This is because certain COPD medications, older age, and systemic inflammation caused by COPD all impair your body's ability to repair your bones.
Once you start to lose bone density, you become more prone to accidents, skeletal disfigurement, and loss of physical mobility. Even just one bad fall or injury could result in a break that significantly affects your ability to manage your COPD.
That's why experts recommend that COPD patients take extra steps to prevent calcium deficiency, which often includes taking calcium supplements. You should also make an effort to get plenty of calcium from food sources like dairy, vegetables, and fortified grains.
Getting lots of calcium through diet and supplements is a great natural treatment that helps COPD patients keep their bones and bodies strong. It may even prolong your life by protecting you against debilitating injuries and major losses in physical mobility.
Vitamin D

Vitamin D is another vital nutrient that your body needs to prevent serious problems and health conditions related to COPD. In fact, your body can't even absorb calcium without vitamin D, which makes is just as important as calcium for keeping your bones in good shape.
But vitamin D is needed for much more than just your bones; it plays a role in your immune system, your cardiovascular health, and may even play a direct role in treating COPD. Unfortunately, a large number of COPD patients have vitamin D deficiencies, particularly those whose disease is more severe.
Because of this, many experts recommend that COPD patients take extra vitamin D to supplement their diets. Studies show that getting enough vitamin D can prevent exacerbations, preserve your cardiovascular health, and even slow the progression of your disease.
Some research even suggests that taking Vitamin D supplements can improve your ability to breathe. By strengthening your breathing muscles and making it easier to exercise, vitamin D may be an effective way to improve your physical fitness and mobility.
Vitamin A
Vitamin A is an important nutrient for keeping your lungs healthy and strong. It works in your lungs to build and repair lung tissue, which is what makes it particularly important for people with COPD.
If you don't get enough vitamin A from your diet, it can make your lungs more vulnerable to infections. By reducing your lungs' ability to repair themselves, it may even make them more prone to damage from inflammation caused by respiratory illnesses and irritants like smoke.
That's why experts recommend that COPD patients take vitamin A supplements if they are likely to have a deficiency. Studies show that it may even reduce your risk for respiratory infections and further damage to your lungs.
However, taking a vitamin A supplement is not recommended if you get enough of the vitamin in your diet. In fact, too much vitamin A can cause serious health problems like liver damage, which is why you should always consult your doctor before starting a new supplement.
The Antioxidant N-Acetylcysteine
Researchers have found that COPD patients experience more “oxidative stress” than people who don't have the disease. Although experts still don't completely understand how oxidative stress works, it seems to play a role in worsening lung damage and respiratory function in people with COPD.
This has led many COPD researchers to investigate antioxidants, which they believe may be able to reduce oxidative stress in the lungs. In that way, they believe that certain antioxidants may slow down the respiratory decline experienced by COPD patients.
One antioxidant, known a N-Acetlycysteine, shows the most potential as a treatment for COPD. Researchers believe that it may have a protective effect on the lungs by protecting them from damage caused by oxidative stress.
Some studies also show that N-Acetylcysteine can also reduce chronic inflammation, which is another major cause of COPD-related lung function decline. By reducing both inflammation and oxidative stress, some researchers believe that this antioxidant may be a natural way to slow down the progression of COPD.
Other studies show it may have potential for reducing airway blockage by reducing the amount of excess mucus that builds up in the lungs and airways. As a result of all these benefits, experts believe that N-Acetylcysteine may be able to reduce COPD exacerbations and respiratory decline.
While researchers are still investigating the proper usage and dosage, N-Acetylcysteine shows great promise for clinical use. With permission and supervision from your doctor, you may be able to use this antioxidant as a natural treatment for your COPD.
Vitamin C & Vitamin E
Vitamin C and E are both antioxidants as well as essential nutrients your body needs for metabolism. Researchers believe they may also play a role in the health of your bones, immune system, cardiovascular system, and more.
Some studies suggest that vitamins C and E may be important for lung health, too. Several studies have found, for example, that COPD patients with more vitamin E and C in their bodies have better lung function than those with lower vitamin levels.
Research also shows that being deficient in vitamins C and E can worsen symptoms like breathlessness, wheezing, and excess phlegm. COPD patients also tend to have significantly lowered amounts of these vitamins in their bodies when they experience a COPD exacerbation.
Vitamins E and C may also help improve patients' ability to stay active and do physical activities. One study found, for instance, that patients taking Vitamin E and C supplements had significantly increased exercise endurance compared to those who didn't.
All of this evidence suggests that getting plenty of vitamin C and E in your diet may be an effective, natural way to reduce your COPD symptoms and your risk for exacerbations. If you have trouble getting enough from your diet, you may need to take vitamin C and E supplements to help you manage your COPD.
Omega-3 Fatty Acids

Omega-3 fatty acids are a type of healthy fat found mainly in fish like salmon, mackerel, and sardines. Omega 3's are known for reducing inflammation, which makes them a promising natural supplement for COPD, which is known as an inflammatory disease.
Since chronic inflammation makes many COPD symptoms worse, Omega-3's may be able to improve breathlessness, fatigue, and other symptoms by reducing inflammation. However, researchers are still not sure whether or not the benefits of omega-3's for COPD are substantial enough for practical use.
However, there has been some encouraging research that suggests omega-3 fatty acids could be an effective tool for treating lung infections. One study in mice showed that omega-3 supplements successfully reduced inflammation in the lungs and improved their ability to fight off bacterial infections.
Another study on human COPD subjects found that those who took omega-3 supplements had increased exercise endurance and fewer signs of inflammation. On the other hand, some studies have failed to find a clear link between omega-3 fatty acids and inflammation in people with COPD.
However, there is a stronger link between omega-3 fatty acids and heart disease, which means that omega-3 supplements may still have significant benefits for people with COPD. Heart disease is a common complication of COPD and affects a large percentage of patients, so supplementing your diet with omega-3's may still protect you from serious cardiovascular complications related to COPD.
Herbal Supplements
While herbal supplements cannot treat COPD directly, some believe that certain herbal supplements can alleviate COPD symptoms. For example, some believe that herbal remedies like turmeric and ginseng can help with ailments like congestion and inflammation.
It's important to remember, however, that most herbal supplements have been researched but not found to have any significant therapeutic effects. While some may show some promise, there is not yet enough evidence to say that they are effective treatments for any COPD symptoms.
However, research on these herbal supplements is ongoing, and scientists may be able to confirm some of their suspected benefits in the future. As it is, however, you should stick to tried and true treatments that are well-researched and well-supported by evidence.
It's also important to tell your doctor about any herbal supplements you take, because they could interfere with other medications and treatments your doctor prescribes. However, it is best to avoid using herbal supplements entirely unless you use them under the strict supervision of a licensed doctor.<

Giving your lungs a break is an important daily task you, as a responsible COPD patient, should work towards.
Every time you are able to make your lungs work less, you are bettering your condition and your livelihood. This can be as simple as getting an air purifier in every room of your home and should be as constant as adhering to your oxygen prescription daily.
In this blog we talk about the easiest way to give give you lungs a break. The best thing you can do is acquire a portable oxygen concentrator that will help you move through the day and your life with ease. In order for that to be a possibility, you need a supplement oxygen device unit this is lightweight, reliable, and affordable!

As you probably know Chronic Obstructive Respiratory Disease is a progressive illness that is not curable. Therefore, your treatment and how you manage this disease is essential to ensure your COPD does not progress quickly into a more severe stage of COPD.
Resting you lungs is, in itself, a treatment for managing COPD. By reading this blog, you can expect to learn the best oxygen units that will help you to manage your disease effectively and subsequently improving your quality of life with COPD.
Taking your Oxygen Therapy Seriously

If you are prescribed oxygen therapy, adhering to your prescription as you doctor orders is essential for taking care of your lungs, and overall health and well-being.
Long-term oxygen therapy is the only known treatment for COPD that is proven to extend the life expectancy of COPD patients. Therefore, using your oxygen equipment correctly can help you live a better quality life longer.
In this section we will discuss three portable oxygen concentrators all of which are reliable but each device is designed to cater to a different oxygen patient.
The ARYA P5 portable Oxygen Concentrator

The ARYA P5 portable oxygen concentrator is already making a name for itself in the oxygen industry as one of the smallest and quietest portable oxygen concentrators on the market. It is one of the newest portable oxygen concentrators available and it's not only small, it's also reliable, gets great battery life, and offers 10 different oxygen settings for more accurate dosing.
Along with being one of the smallest and quietest portable oxygen concentrators on the market, the ARYA P5 portable oxygen concentrator has some amazing features that set it apart from the rest of the units on the market.
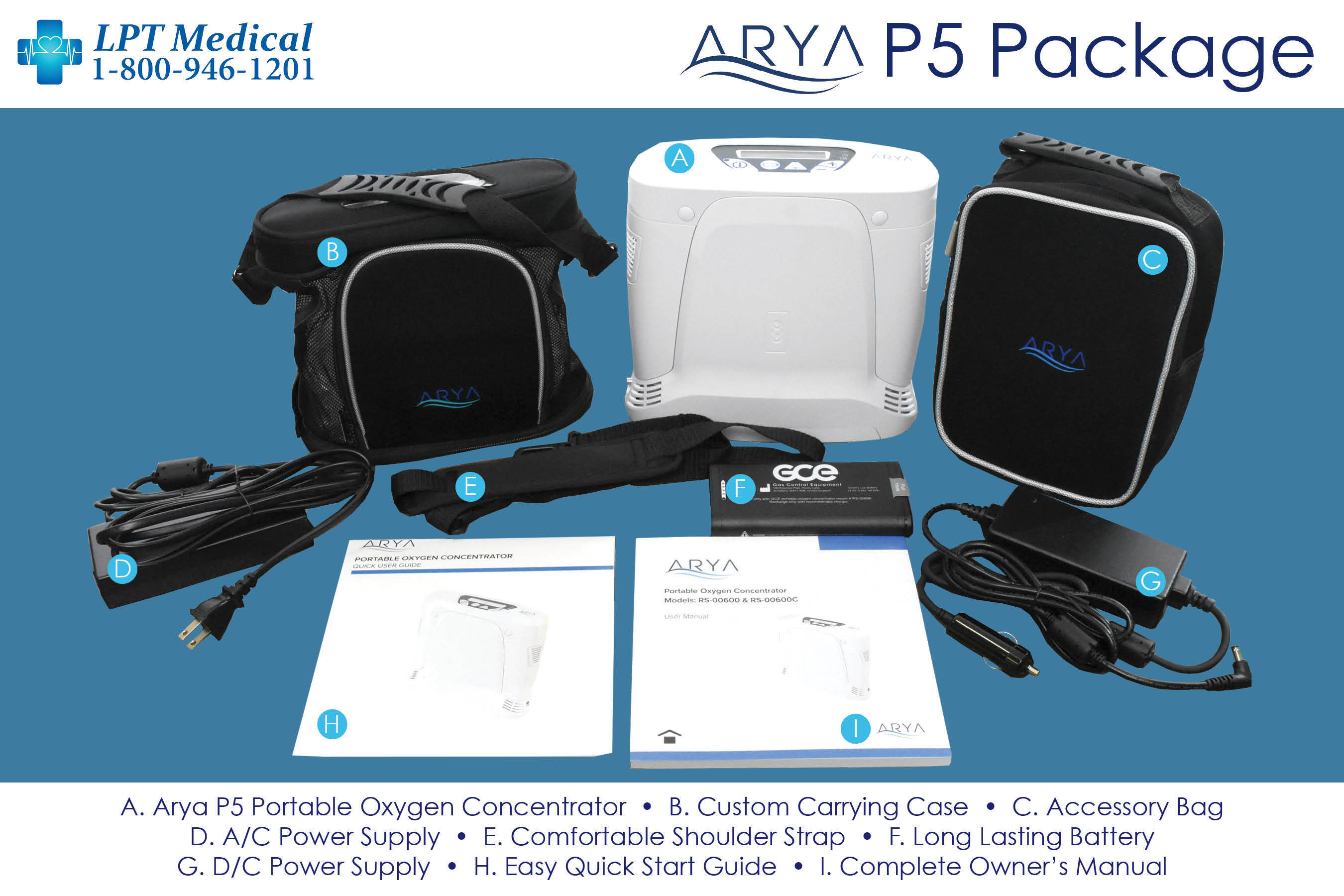
The ARYA P5 is going to make getting back to living an active life as easy as possible. It’s lightweight with long-lasting battery life helping you regain your freedom and independence. It gets up to 8 hours of battery life and offers 10 different oxygen settings! There’s no other lightweight portable oxygen concentrator on the market that will give you more accurate oxygen dosing while running for up to 8 hours
There are several reasons why oxygen patients should be excited about the new ARYA P5 portable oxygen concentrator. The first, and most importantly, is that the oxygen delivery service is unmatched.

When looking for a portable oxygen concentrator, the second most important priority should be the weight and size of the oxygen device.
As mentioned above, the ARYA P5 is one of the smallest and lightweight portable oxygen concentrators money can buy! It weighs just 5.5 pounds with the battery installed, and it stands 9.8” W x 3.8” D x 9.25” H.
At 5.5 pounds, the ARYA P5 is going to be a great companion for anyone that is interested in a healthy and active lifestyle. Exercise becomes easier, being more mobile and independent is also an option now. Traveling no longer seems like a chore, but it is something to be excited about!
Not to mention, with the ARYA P5 you will have the oxygen you need without sacrificing other parts of life. Go exercise, grab lunch with your friends, or spend a day golfing without feeling weighed down by your oxygen.
The ARYA P5 is a device that will help first time oxygen users and long time oxygen users by giving everyone who needs supplemental oxygen therapy the freedom and independence they need.
The ARYA P5 offers a high oxygen output to accommodate as many oxygen users as possible. The ARYA P5 has 10 adjustable oxygen settings. It offers pulse flow settings 1-5 and increases by increments of 0.5. This precision oxygen delivery is important for people so they are getting the exact amount of oxygen their bodies require, not too much and not too little!

It offers pulse flow settings 1-5 that can be adjusted in 0.5 increments. So whether you’re exercising, feeling sick, or are experiencing an exacerbation you will be able to increase the machine’s oxygen output to get the oxygen you need. Just remember to check with your doctor before you increase the flow rate on your machine.
The ARYA P5 also comes equipped with RATE RESPONSIVE THERAPY™ (RRT) that delivers oxygen on demand! Everytime the device senses an inhalation, the breadth th triggers the device to respond accordingly. Whether a patient is climbing the stairs or taking a walk, ARYA P5 will automatically respond to the breath rate by adjusting the amount of oxygen needed to ensure the patient remains saturated.
The ARYA Portable Oxygen Concentrator

The ARYA Portable Oxygen Concentrator is a pulse flow portable oxygen concentrator (POC) that can cover oxygen patients that need pulse flow oxygen delivery less than 5 liters per minute.
One of the best things about the ARYA portable oxygen concentrator aside from it being lightweight (5 pounds) and having a long lasting battery (up to 16 hours) is the comprehensive warranty. It's not often you see a manufacturer give you an extended warranty on the portable oxygen concentrator as well as the sieve beds!
With the ARYA portable oxygen concentrator you will have added peace of mind knowing you get lifetime warranty on the unit and an industry leading 5 year warranty on the sieve beds!
Most manufacturers offer a 3 year warranty on their unit and a 1 year warranty on the sieve beds. But ARYA truly stands behind their product like no one in the industry.
The Respironics SimplyGo

The Respironics SimplyGo is both a pulse flow and continuous flow POC. It has the capabilities to support oxygen patients that need pulse flow operation up to 6 liters per minute or 2 liters of continuous flow.
Weighing in at a mere 10 pounds and standing 10" H x 6" D x 11.5" W, the SimplyGo is one of the smallest and lightest continuous flow portables available! You will be able to bring it with you wherever you go and you will have no problem finding a place to store it.
Your SimplyGo will easily fit underneath the seat in front of you on the airplane, you can store it on the floor of your car or in the passenger seat as you drive, and when you don’t need to use it you will be able to put it in your closet without having to clear space for it.

Although 10 pounds is extremely light for a continuous flow portable oxygen concentrator, it’s still pretty heavy to carry. But you won’t need to worry about that! Your SimplyGo package will include a custom carrying case and a wheeled travel cart so you have the option to carry it over your shoulder or you can pull it behind you on the travel cart.
The SeQual Eclipse 5

The SeQual Eclipse 5 POC is a popular continuous flow device that is also reliable and durable. It is rated to last for years and the POC of choice of the U.S. military!
The pulse flow settings range from 1-9 and the continuous flow settings range from 0.5-3.0 LPM, so it is able to cover most oxygen patient’s needs, and some!
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
As mentioned above, the SeQual Eclipse 5 is one of the most, if not the most, popular continuous flow portable oxygen concentrators on the market. That is largely due to its long-standing track record for being durable and reliable. If it’s good enough for the US Military, that should tell you something.
The hard-bodied shell of the Eclipse 5 is extremely protective. It will keep your concentrator protected from everyday wear and tear, accidental bumps and bruises, and if you have pets or grandkids in the house it will be able to withstand their crazy antics.
One of the best things about the Eclipse 5 is that it requires very little maintenance from you to keep it running. All you need to do is wash your filter once every week or two depending on how often you use your Eclipse and you are good to go!
Many people don't realize that COPD is not just a respiratory disease, but a disease that affects many different parts of the body besides lungs. Because of this, there are many health problems and conditions that accompany COPD, including high blood pressure and heart disease.
High blood pressure is a serious problem that affects more than one in three Americans, and the prevalence is even higher in people with COPD. This elevated risk stems from a variety of factors, including lung damage, inflammation, and a history of smoking.
Ideally, every person with COPD would be well-informed about how their disease affects their heart and blood pressure. Unfortunately, many patients don't realize how serious the cardiovascular problems caused by COPD really are.
If you ignore high blood pressure, it can lead to a vicious cycle in which COPD worsens your high blood pressure and your high blood pressure worsens your COPD. In order to protect your heart and lungs, you need to understand how COPD and high blood pressure are connected.
That's why, in this post, we're going to help you understand the relationship between COPD and blood pressure. We'll show you how high blood pressure happens, why it matters, and what you can do to prevent high blood pressure with COPD.
The more you understand about your disease and the effects it has on your body, the better you will be able to protect yourself from the many damaging effects of COPD. If you understand the link between COPD and high blood pressure, you can take more steps to keep your heart healthy and reduce your chances of developing more serious heart problems related to COPD.
Understanding How Blood Pressure Works

According to the American Heart Association, blood pressure is a measure of “the force of your blood pushing against the walls of your blood vessels.” How high your blood pressure is depends on how wide your blood vessels are and how fast your heart pumps blood through them.
If your blood vessels get more narrow, then your blood pressure goes up. Your blood pressure also rises any time your heart pumps harder, pushing more blood through your vessels at a time.
Your blood pressure at any given moment depends on a variety of factors, including your mood and activity level. For example, your blood vessels constrict when you exercise or get excited, which causes your blood pressure to rise.
This kind of blood pressure change is triggered by chemical signals in your body and it is known as vasoconstriction. It happens when your body purposefully constricts your blood vessels, often as a way to help you get more oxygen when you exercise or experience stress.

Vasoconstriction is only temporary, however, and your blood pressure returns back to a normal, baseline level after the chemical signal subsides. It is normal for your blood pressure to fluctuate throughout the day in this manner, but it is dangerous for your blood pressure to stay elevated for too long.
Chronic high blood pressure, also known as hypertension, happens when your blood pressure stays high long-term. This can happen via vasoconstriction, in the case of chronic stress or stimulant use, but it is often the result of a different type of blood vessel constriction that happens when your arteries get damaged, inflamed, or clogged up.
The main reason chronic high blood pressure is bad for you is that it puts extra pressure on your heart and blood vessels. Chronic hypertension forces your heart to work overtime, all the time, in order to keep your blood circulating efficiently.
One of the most common causes (and complications) of chronic high blood pressure is atherosclerosis, a condition that develops when plaque builds up on the insides of your arteries. This plaque clogs up your blood vessels, restricting the amount of space that your blood can flow through.
When this happens, your heart has to pump harder all the time in order to force blood through the narrowed spaces in your arteries. As your heart struggles to overcome the pressure in your blood vessels, it experiences continuous back-pressure. This eventually damages your heart's ability to pump and can lead to more serious health conditions.
The Hose Analogy For Understanding Blood Pressure

To help you understand how this works, think about how water pressure works in a hose. The pressure of the water that comes out of the hose is affected by both the speed of the water and the size of the hose's opening, just like your blood pressure is affected by how fast your heart pumps and how wide your arteries are.
For example, when you turn up the spigot on the hose to increase the flow of water, this causes the pressure of the water coming out of the hose to go up. This is similar to how your blood pressure goes up when your heart pumps faster.
Now think about what happens if the inside of the hose got clogged up with grime, or if you put your finger on the end of the hose to block part of the opening. This would also increase the water pressure, because the same amount of water is being forced through a narrower opening. This is just like how your blood pressure increases when when your arteries get narrowed, whether it happens through constriction or atherosclerosis.
How COPD Affects Your Blood Pressure

Because the heart and lungs are designed to work together, the effects of COPD on the lungs naturally affects your heart and the rest of you cardiovascular system. In fact, some COPD experts are beginning to think that COPD's affects on the heart are just as serious as the damage it does to the lungs.
In fact, there isn't just one, but many different mechanisms through which COPD raises your blood pressure. Let's look at each of these mechanisms to better understand how COPD affects your heart.
Low Blood Oxygen
One of the main ways that COPD affects your heart is by restricting your oxygen. Because the lungs are damaged, they often can't absorb enough oxygen to keep your blood oxygen levels high.
Having too little oxygen in your blood is known as hypoxemia, and it makes it difficult for your heart to ensure that enough oxygen makes it to all the different parts of your body that need it. When this happens, your body has to compensate in a variety of ways to keep as much oxygen circulating as possible.
One of the ways your body compensates for low blood oxygen levels is by pumping faster to push more blood through your body at a time. This increases your blood pressure, but has the advantage of circulating oxygen more quickly through your system.
This faster blood flow allows your body to better keep up with its oxygen needs, reducing the effects of hypoxemia. However, this causes your blood pressure to increase any time your oxygen needs increase, even during light activity.
It also makes your blood pressure rise any time your lung function decreases, such as during a COPD flare-up or exacerbation. As your COPD progresses and you experience hypoxemia more often, it can cause chronic hypertension and damage your heart and lungs.
Thicker Blood
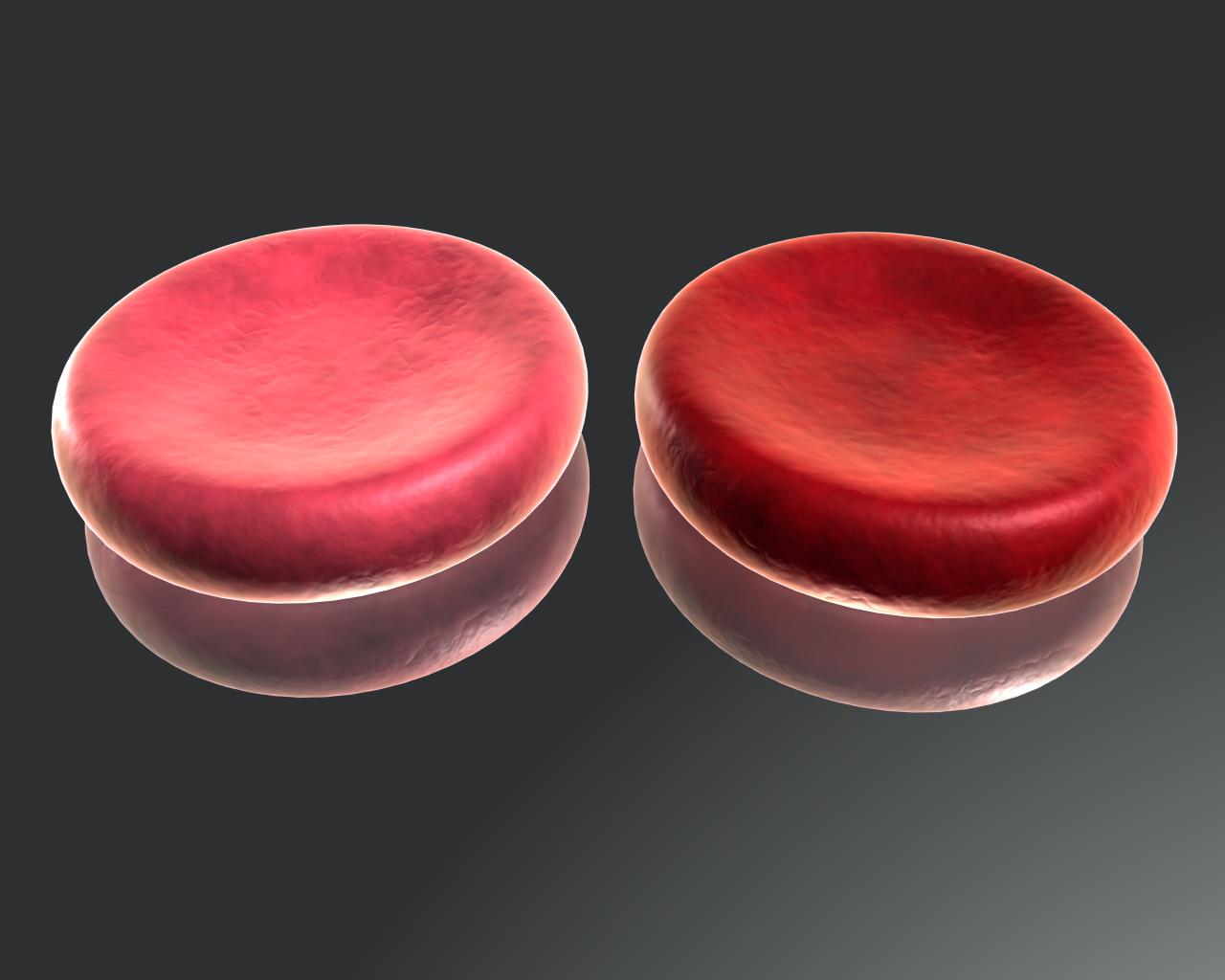
Increasing your red blood cell count is another way that your body compensates for low blood oxygen levels caused by COPD. It does this in the hope that having more red blood cells will allow your blood to absorb more oxygen from your lungs.
However, more red blood cells makes your blood more thick and viscous, which makes it harder for your heart to push it through your vessels. This increases your blood pressure and forces your heart to pump more forcefully, which significantly increases the amount of back-pressure on your heart.
Inflammation

COPD is known as an inflammatory disease because COPD patients consistently show elevated levels of inflammation throughout their bodies. This inflammation is well-known for damaging the lungs, but it can damage your heart and blood vessels, too.
Studies investigating the causes of high blood pressure consistently find that inflammation and hypertension are closely linked. Experts believe that inflammation in your blood vessels causes them to constrict and inhibits their ability to dilate.
Over time, the inflammation can even damage the insides of your arteries, making it easier for plaque to form and leading to atherosclerosis. Researchers have long connected COPD-related inflammation to patients' increased risk of high blood pressure, heart disease, and cardiac-related deaths.
Smoking

As we mentioned earlier, smoking is a major cause of high blood pressure and atherosclerosis. The fact that many COPD patients have a shared history of smoking is a major contributor to high blood pressure in people with COPD.
While researchers aren't exactly sure how it happens, the evidence is clear that smoking increases your blood pressure and damages your arteries. There is also a strong link between smoking and more serious cardiovascular problems like heart attacks and stroke.
The Symptoms of High Blood Pressure

High blood pressure does not usually cause any major symptoms, at least until it becomes very severe. Symptoms usually begin to show up once high blood pressure has progressed to a more serious condition like coronary artery disease (a more severe form of atherosclerosis).
Those who do experience symptoms of high blood pressure usually only notice mild symptoms like headaches and minor shortness of breath. If you suffer from COPD, these symptoms are easily obscured by the more severe symptoms of the disease.
Once high blood pressure has progressed to more serious cardiovascular disease, additional symptoms may appear. Unfortunately, the symptoms often don't become significant enough to notice until after your heart and blood vessels have sustained serious damage.
However, it is helpful to know what symptoms of high blood pressure and cardiovascular disease that you can look out for. The main early signs are headaches, shortness of breath, and feeling lightheaded or dizzy.
Here are some more signs and symptoms of high blood pressure and cardiovascular disease:
- Shortness of breath (especially while at rest)
- Headaches
- Dizziness and lightheadedness
- Fainting
- Chest pain, tightness, or discomfort
- Fatigue
- Nausea
- Irregular heartbeat
- Weakness, numbness, pain, or swelling in your extremities (hands and feet)
If you experience any of these symptoms, you should see your doctor right away. The sooner you get diagnosed for your heart problem, the sooner you can get proper treatment and take steps to prevent it from progressing into a more serious disease.
The Dangers of High Blood Pressure
What makes hypertension dangerous is the fact that it subjects the walls of your heart and blood vessels to extra pressure that can cause permanent damage. Over time, hypertension can weaken both your arteries and your heart, leading to serious heart problems and other complications.
This is particularly dangerous for COPD patients, who are especially prone to cardiovascular problems and heart disease. Additionally, COPD symptoms like inflammation and low blood oxygen levels can worsen high blood pressure and accelerate the rate at which it get worse.
Here are some of the major problems and complications that high blood pressure can cause:
- Heart disease (also known as coronary artery disease)
- Heart attack
- Heart failure
- Stroke
- Metabolic syndrome
- Problems with memory and cognition
- Kidney damage
- Vision loss
- Dementia
Some of these problems are more likely to affect people with COPD than others. Here is a closer look at some of the most common complications and health conditions that hypertension causes in people with COPD.
Atherosclerosis, Coronary Artery Disease, and Left-Sided Heart Failure

No mater the cause of your high blood pressure, hypertension increases your risk for atherosclerosis. The pressure of your blood against the inside of your blood vessels causes tiny tears and inflammation, which provide perfect spots for plaque to stick to your artery walls.
Since most COPD patients already have a history of smoking, their blood vessels are already more prone to atherosclerosis. This makes high blood pressure even more likely to cause more severe cardiovascular problems for people with COPD.
Over time, atherosclerosis causes your arteries to narrow and harden, causing a more severe form of atheroscelrosis known as heart disease (or coronary artery disease). As the blockages become even more severe, it causes the left side of your heart to enlarge.
Heart enlargement is one of the most dangerous effects of high blood pressure, and it causes your heart muscle to weaken over time. It happens when the pressure of the blood in your arteries gets so high that it creates a significant amount of back-pressure in your heart whenever it tries to pump.
This pressure causes blood to back up in your pumping chamber, which causes it to both pump faster and expand. While this allows the chamber to better handle the increased amount of blood, it also weakens the muscles in the walls of your heart, which eventually leads to heart failure.
Heart failure happens when your heart becomes so weak that it can no longer pump blood through your body effectively, causing your blood oxygen levels to fall dangerously low.
Heart disease, which is the root of heart failure, is also the cause of most heart attacks. And because fatal heart attacks are a major cause of death for people with COPD, it's important for patients to take their blood pressure, atherosclerosis, and other cardiovascular problems seriously.
Worsened Respiratory Symptoms

If you’re a respiratory patient with a condition such as COPD, pulmonary fibrosis, or cystic fibrosis, you’ve likely accepted change as a normal part of your life. Being able to implement treatments into your life such as pulmonary rehabilitation, supplemental oxygen therapy, and an improved diet routine is never easy, but it is essential if you want to feel better and improve your long-term prognosis.
But it’s important to remember that COPD treatment rarely remains stagnant. There will likely be a time — whether it’s several weeks, months, or years down the line — when you’ll need to make adjustments to your routine. This could be due to your doctor discovering more information about your condition or it could be caused by a serious event such as a COPD exacerbation.
Either way, you’re going to need to be adaptable in the way that you approach your condition.
For example, if your doctor prescribes you 4 hours of supplemental oxygen a day, you might be tempted to get a cheap oxygen device that will simply “get the job done.” However, since COPD is a progressive disease, it’s safe to assume that you will eventually be prescribed more oxygen use by your doctor.
When this happens, you’ll be stuck in a difficult situation where you need to sell your old oxygen device and get a new one that better suits your long-term needs.
This is why we recommend small lightweight portable oxygen concentrators to the vast majority of people who need oxygen. Even if you don’t think you’ll be getting out of the house every day, portable oxygen allows you to have much more freedom within your own home.
LPT Medical's respiratory specialists will be able to get you the best deal possible on them. So give us a call or fill out the form at the side of the page to get your free oxygen concentrator guide.
In the meantime, we’re going to be taking a look at the smallest portable oxygen concentrators of 2022. Feel free to leave a comment if you have any questions.
Why is it Important to Have a Small Portable Oxygen Concentrator?
The term “portable oxygen” implies that the machine is lightweight, durable, easy to use, and most importantly — small. Just like how you judge the portability of your phone by how well it fits in your pocket, concentrators can be judged by how easily they can be carried on your shoulder. The smaller the concentrator, the easier it will be to carry it under your shoulder without interrupting your walking.

Another major benefit of small portable oxygen concentrators is that they’re much easier to store. If you ever need to put your concentrator in storage, you can rest assured you’ll find a place for it.
Also, since you don’t have to transport small portable oxygen concentrators on the ground, you won’t have to worry about not being able to put it on a table where it could spread germs. This is especially important during this time when people are trying to avoid coronavirus.
There are three different types of oxygen concentrators: home oxygen concentrators, continuous flow oxygen concentrators, and pulse dose oxygen concentrators.
The latter two are the only ones that can be labeled “portable” because they can actually deliver oxygen while you’re moving. Home oxygen concentrators, however, need to be connected to a wall outlet in order to put out oxygen.
.png?width=628&name=The%20Best%20Portable%20Oxygen%20Concentrators%20of%202017%20(6).png)
The AirSep Focus
The AirSep Focus not only holds the title for the lightest portable oxygen concentrator but it holds the title for the smallest portable oxygen concentrator as well. Weighing in at only 1.75 pounds and with dimensions of 6.4” H x 2.5” D x 4.8” W, the AirSep Focus is truly a mini portable oxygen concentrator. In fact, this device is so small that you can even wear it on your belt!
The AirSep Focus has 2 pulse flow settings with a total oxygen output of 330 milliliters per minute (ml/min). This is not always enough for oxygen patients, so that will completely rule out this option even if you do like the idea of having an ultra-lightweight portable oxygen concentrator.

The AirSep Focus has less then average battery life compared to some other devices we talk about iin this blog. Battery life is what enables you to get out for longer without having to run home and charge your device, and the AirSep Focus only offers 1.5 hours per charge with the standard battery and 3.5 hours per charge with the 8-cell battery.
However, the purchase of an AirSep Focus comes with two micro-batteries, so you’ll get 3 hours of battery life right out of the box.
Since AirSep wanted to make the Focus as simple and small as possible, you won’t be able to adjust the flow rate or audible output settings. In fact, unlike most other portable oxygen concentrators, the Focus doesn’t even have an interface with controls on it. Simply turn the device on and you’ll start receiving oxygen. This makes for a very “bare-bones” experience that’s perfect for someone who isn’t looking for something too fancy.
AirSep Focus Specs
| Volume |
76.8 in² |
| Dimensions |
4.8” Wide x 2.5” Deep x 6.4” High |
| Weight | 1.75 Pounds |
| Flow Rate |
Pulse Flow Setting 2 |
| Battery Life |
Up to 3 Hours |

The Inogen One G4
In a way, Inogen is like the Apple of oxygen concentrator manufacturers. While they haven’t produced medical equipment for as long as other companies like Caire Inc. or ResMed, their consistent drive to improve the freedom and independence of oxygen patients everywhere has put them at the forefront of the oxygen industry since the early 2000s.

The Inogen One G4 was released all the way back in May of 2016, but it’s still one of the most popular portable oxygen concentrators on the market. It weighs in at only 2.8 pounds and it has dimensions of 7.2” H x 5.91” L x 2.68” W, so it’s the smallest and lightest portable oxygen concentrator behind the AirSep Focus.
While the Inogen One G4 is not small enough to clip to your belt like the AirSep Focus, it is small enough to fit in a purse or handbag. However, we don’t recommend doing this because it could damage the machine and prevent it from processing oxygen correctly. Fortunately, the G4 comes with a convenient carrying case and adjustable strap so that you can sling it over your shoulder.

The only real limitation the G4 is that it doesn’t go beyond 630 ml/min of oxygen output or a pulse flow setting of 3. This is almost twice as much as the AirSep Focus, however, it still may not be enough for many oxygen patients. Before investing in the G4, make sure that your doctor approves of it first so that you don’t end up with an oxygen machine that doesn’t meet your needs.
Inogen One G4 Specs
| Volume |
114 in² |
| Dimensions |
7.2” H x 5.91” L x 2.68” W |
| Weight | 2.8 Pounds |
| Flow Rate |
Pulse Flow Settings 1-3 |
| Battery Life |
Up to 4.5 hours |
The Inogen One G5
As we said, Inogen does not take their work lightly, and this is no different when it comes to their latest portable oxygen device — the Inogen One G5. Releasing in the summer of 2019, the G5 immediately seized the title of “the most powerful pulse dose portable oxygen concentrator” with 1,050 ml/min of oxygen output. As of right now, the only other oxygen machine to match that is the Caire FreeStyle Comfort which was released earlier this year.

All things considered, the Inogen One G5 is one of the best portable oxygen concentrators for people with high oxygen demands. It offers an outstanding battery life allowing you to get out of the house and stay out for longer, it’s under 5 pounds, and it’s compact and durable. Since it’s so new, you can expect it to be fully supported by Inogen and oxygen retailers for many years to come.

There are a number of accessories sold separately from the G5 that can help you make the most of it. For example, the 16-cell battery will effectively double your battery life, allowing you to stay out and about for up to 13 hours on a flow setting of 1! The G5 external battery charger is also a great option for people who are on the go and want to be able to charge batteries more quickly. Normally, batteries need to be connected to the unit in order to charge, but this device will enable you to charge one separately.
Inogen One G5 Specs
| Volume |
191 in² |
| Dimensions |
8.15" H x 7.19" L x 3.26" W |
| Weight | 4.7 Pounds |
| Flow Rate |
Pulse Flow Settings 1-6 |
| Battery Life |
Up to 13 hours |
.png?width=218&name=G5-Oxygen-Concentrator_418x418-removebg-preview%20(1).png)
The Respironics SimplyGo
It’s not very often that we would mention a continuous flow portable oxygen concentrator on a list of “the smallest portable oxygen concentrators,” however, the Respironics SimplyGo is the one exception. Continuous flow machines tend to be much heavier and larger than pulse dose units because they have to put out a much larger volume of oxygen than their counterparts.

Unfortunately, not all patients are able to use a pulse dose machine, either because it doesn’t provide them with enough oxygen, or their doctor specifically advises them to use continuous flow. The Respironics SimplyGo is 10” H x 6” D x 11.5” W and weighs in at only 10 pounds making it both the lightest and smallest continuous flow portable oxygen concentrator on the market. While the SimplyGo can be carried using a shoulder strap, if you have chronic back pain or some other disability, it’s recommended that you use the rolling cart. Fortunately, this accessory comes with the device, so you won’t need to make any additional purchases in order to experience the freedom that you deserve!

If that was not enough, you’ll be happy to know that the Respironics SimplyGo also comes with a pulse flow option. There are 5 different settings with a maximum oxygen output of 2,000 ml/min and the standard continuous flow option will afford you between 0.5 and 2.0 liters per minute (LPM) of oxygen. Keep in mind that your battery will last longer on one charge when you’re using the pulse dose setting as opposed to the continuous flow setting.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!















