Respiratory Resource Center - LPT Medical
How to Treat Bloating Caused by COPD
Everyone experiences bloating every now and then, often the...
Read MoreThe Majority of COPD Patients Use Their Inhaler Incorrectly. Are You One of Them?
If you are like most people with COPD, then...
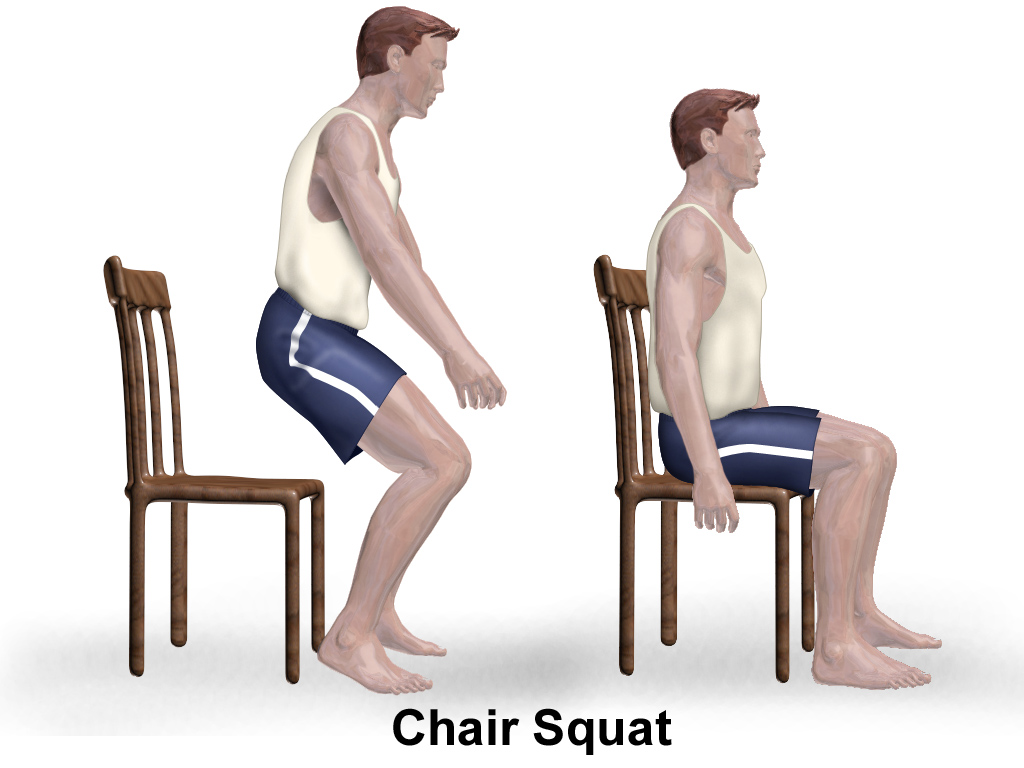
Read MoreTips and Tricks for Exercising on Oxygen Therapy
Exercise is absolutely vital for healthy living, especially if...
Read More