.png)
There are three main types of respiratory disease: airway diseases, lung tissue diseases, and circulatory diseases. The first type, airway diseases, affect the tubes called bronchioles, usually causing them to narrow, swell, or become filled with a slimy substance called mucus. Airway diseases include asthma, a specific type of chronic obstructive pulmonary disease (COPD) called chronic bronchitis, and bronchiectasis, a condition that results from recurrent lung infections.
The second type of respiratory disease, lung tissue disease, specifically affects the tissue within the lungs. Oftentimes, these diseases cause the lungs to become inflamed and lose their elasticity which is why they’re usually categorized as “restrictive” lung diseases because they prevent the lungs from expanding fully. Pulmonary fibrosis is one common type of lung tissue disease and it results from the formation of irreversible scar tissue in the lungs.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The final type of respiratory disease is lung circulation disease. This type is a little more complicated in that it affects the complex interactions between your lungs and the rest of your circulatory system. These diseases prevent the lungs from processing oxygen from the air you breathe and releasing carbon dioxide, resulting in an imbalance of gases in the body. As you can imagine, these diseases are closely linked with cardiovascular issues.
Believe it or not, COPD has elements of all three of these categories, so it’s more complicated than most people think. In the following sections, we’ll take a look at 7 interesting facts that you may not know about COPD. After reading this, we hope that you are more aware of the global burden of COPD and that you’ll feel inclined to share this information with friends and family members who may be at risk of contracting COPD.

It’s One of the Most Preventable Chronic Illnesses
When we say a disease is “preventable,” we mean that personal lifestyle choices most often cause the disease to take hold. For example, acute illnesses like the flu or the common cold can be prevented with vaccinations and proper hygiene. But when it comes to COPD, this is not quite so simple. According to lung.org, 85 to 90 percent of all COPD cases are caused by cigarette smoking, but there are also other risk factors at play such as environmental pollution and genetics which makes COPD a difficult disease to prevent.
![]()
When you compare COPD to some of the other leading preventable illnesses in the world, it’s not hard to see why COPD is so difficult to prevent. Heart disease, cancer, and diabetes are some of the most discussed diseases and more often than not, this results in a high level of funding while other prominent diseases like COPD are left behind. According to a survey published in ScienceDaily, 38 percent of people with COPD were unaware of the disease before being diagnosed. This often leads to people referring to COPD as a “silent disease,” because it can feel like patients don’t have much of a voice in the community at large.

Perhaps, one of the reasons that COPD has such a lack of awareness is because of how slowly the disease develops. Typically, COPD takes many decades to progress from its early stages to its later stages. This is in stark contrast to diseases like lung cancer which tend to come on more quickly. Unfortunately, this leads to people underestimating the risk of COPD and not taking it as seriously as it should be. Another thing that can overshadow COPD is the fact that lung cancer shares the same awareness month, November. Since lung cancer has more funding in the first place, many people overlook COPD funding and support.
COPD Cannot Be Reversed
COPD is what’s known as a “progressive disease.” What this means is that symptoms related to this respiratory condition get worse over time. While symptoms may subside after a flare-up or exacerbation, these events usually result in a permanent drop in lung function. This is in contrast to conditions like asthma which exhibits similar symptoms, but after experiencing an asthma attack, most people fully recover and don’t maintain any permanent damage to their lungs.
As a result, the most important thing you can do to prevent your disease from progressing, or at the very least, slow its progression is to avoid common COPD triggers. We discuss in detail in this post how you can avoid COPD exacerbations, but we’ll summarize the points here for your convenience. First and foremost, infections are the cause of around 51% of all COPD exacerbations, so preventing them should be your top priority.
When you were young and didn’t have any chronic conditions, you probably weren’t too concerned about the flu or the common cold. These are infections that our body has adapted immunity towards allowing us to fight them off quickly, with or without the use of medications. However, the older we get older, these seemingly harmless things become a lot more serious, especially for people with chronic respiratory illness. It’s estimated that bacterial infections are the cause of 40 to 50 percent of all COPD exacerbations and a significant portion of hospitalizations as well.

Another major cause of COPD flare-ups and exacerbation is air pollution. No matter where you are and what the time of year is, there is air pollution. And if you want to slow the progression of COPD, you should be careful to check the quality of air wherever you go. AirNow.gov is a great resource for anyone who wants an accurate and up-to-date description of the air quality in their area. It’s recommended that COPD patients avoid going outside if the AQI (air quality index) is over 100.
Smoking Cessation is Still Important
There’s a strong belief among many people who have been diagnosed with COPD that “the damage has been done” and that “smoking cessation won’t help.” However, this could not be farther from the truth. While there is no cure for COPD, smoking will most certainly make your symptoms worse. In fact, cigarettes are an immunosuppressant drug meaning they inhibit the body’s innate and adaptive immune system. This puts you at a higher risk of infection and hampers your body’s ability to heal.

According to reports from the Centers for Disease Control and Prevention (CDC), about 38 percent of Americans who have COPD are current smokers. This is pretty astonishing considering that smoking is entirely counterproductive to a COPD treatment plan. Unfortunately, everyone is different so there’s no set smoking cessation plan you should follow. Your best bet will be to speak with your doctor who can help you find something that will work for you.
![]()
Another thing that will help is being away from a household where people have smoked or currently smoke. Secondhand smoke can be equally as dangerous as smoking yourself and experts estimate that the harmful chemicals in cigarettes can linger in a room for as long as five hours. In other words, if you smell cigarettes, you’re probably inhaling harmful chemicals that could lead to a COPD exacerbation. If you live with someone who smokes, try asking them to do it outside.
Every Case of COPD is Different
While around 16 million Americans have COPD, every case is unique. COPD is an umbrella term that’s used to denote two different chronic illnesses: chronic bronchitis and emphysema. And while these conditions might exhibit similar symptoms such as a chronic cough, breathlessness, and fatigue, they’re very different in terms of their causes, risk factors, and prognosis. These conditions can also occur in different parts of the respiratory system and work in tandem with co-morbidities which further complicates treatment and outlook.

Emphysema is what many people think of as the “smoker’s disease.” It’s a condition that affects the alveoli, the tiny air sacs that scatter the lungs. These air sacs are responsible for the exchange of oxygen and carbon dioxide to and from the bloodstream, so they play a key role in our systemic health. In someone with emphysema, the alveoli begin to lose their shape and fill with fluid meaning the transfer of gases is less efficient.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
In many cases, doctors will prescribe supplemental oxygen therapy which can help reduce the burden on the lungs. But it’s important to understand exactly how much you should be receiving because too much oxygen can lead to oxygen toxicity. This can result in symptoms such as coughing, difficulty breathing, and in severe cases even death. Make sure you’re clear on when to use oxygen and how much to use and don’t assume that increasing your oxygen intake will help you feel better.
The treatment options for emphysema also vary based on where the emphysema is located. For example, if the emphysema is located in one specific area of the lung, you may be a candidate for lung volume reduction surgery. This is a procedure that involves removing the damaged tissue in the lungs which prevents air from getting trapped and causing difficulty breathing. While it may sound counterintuitive to remove part of your lungs in order to help you breathe better, sometimes the benefits outweigh the negatives.
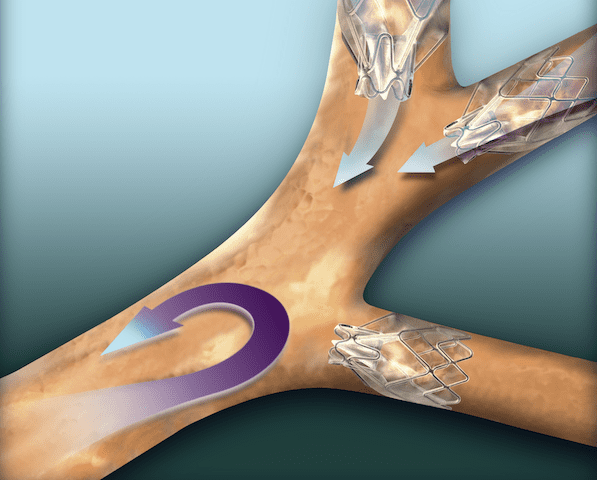
In other cases, emphysema patients may be a candidate for something called endobronchial valves. This is a less intrusive alternative to lung volume reduction surgery and involves inserting one-way valves into certain airways. The end result is that air won’t get trapped in areas of the lungs with emphysema and you’ll be able to breathe easier.
Lastly, COPD can be complicated when co-morbidities such as sleep apnea are involved. Sleep apnea is a condition where the airways close up as you sleep resulting in disruptions in your sleep and more serious long-term effects such as an increased risk of high blood pressure (hypertension) and heart attack. When COPD and sleep apnea occur together it is referred to as overlap syndrome, and studies have found that this phenomenon is common, especially as COPD progresses.
There is a Genetic Component to COPD
There is a small group of COPD patients that are often excluded from larger discussions about COPD and its causes. These are people who contracted COPD without ever picking up a cigarette or spending time around smokers. While alpha-1 antitrypsin deficiency (A1AD) is rare, it is the number one cause of COPD in non-smokers and people who live otherwise healthy lives.

A1AD occurs when the liver does not produce the correct amount of the alpha-1 protein. This protein is responsible for protecting the lungs from damage due to inflammation and it also prevents damage due to scar tissue in the liver. In these people, even something as simple as exposure to poor air quality or higher than normal levels of air pollution can lead to permanent lung damage and even COPD.
While there is no cure for alpha-1 antitrypsin deficiency, there are treatment options available. It’s also very important to recognize it at an early age so awareness is key. One possible treatment option is called augmentation therapy (replacement therapy). This is where the patient receives replacement alpha-1 from a donor once a week through an IV treatment. While this is not a cure-all, it can play an important role in delaying damage to the lungs. This is another reason it’s important to start as soon as possible.
COPD is More Common in Women
For many decades, COPD was primarily a disease that affected men. This is largely due to the fact that women did not smoke very frequently before the 1950s. However, since then, the gap between men who smoke and women who smoke has narrowed significantly. With that being said, the number of smokers, in general, has decreased from 40 percent in the 1970s to around 14 percent in 2017.

Another reason COPD is more common among women is that women are proven to have a faster rate of decline in FEV1 (forced expiratory volume in one second) than men despite smoking less heavily. Studies have also shown that women have higher hospitalization rates and deaths due to respiratory failure or comorbidities.
COPD Patients Can Live a Long and Healthy Life
It’s so easy to fall into a line of thinking where being diagnosed with a chronic condition means it’s the end, but this couldn’t be farther from the truth. While receiving a COPD diagnosis should act as a wake-up call for heavy smokers, it is far from “the end.” Many COPD patients are able to live long, happy lives as long as they make a serious effort to change their lifestyle for the better.

According to Medicinenet.com, the five-year life expectancy for newly diagnosed COPD patients is 40% to 70%. This is despite the fact that as many as 38% of people diagnosed with COPD continue to smoke and many don’t follow through with the treatment plan that their doctor set forth for them. On the other hand, people who immediately quit smoking and implement healthy choices like supplemental oxygen therapy, a healthy diet, and a consistent exercise routine see much better results. Some people with COPD have lived well into their 70s and 80s.
Conclusion
COPD is a leading cause of death in the United States and it’s also one of the most preventable illnesses in the world. Despite this fact, many people are woefully unaware of what exactly it is and how it affects the body. In comparison to other chronic illnesses like lung cancer or heart disease, COPD receives a lack of funding. This has led to many people referring to it as an “invisible illness.” — many people are affected, yet many suffer in silence.
The good news is that everyone can play a role in the treatment and prevention of COPD. if you have COPD, you can take part in clinical trials which helps to pave the way for researchers and doctors. If you have a friend or loved one with COPD, you can take time out of your day to help them manage their disease. And if you don’t have any connection to COPD, you can still get involved by donating or volunteering with organizations like the American Lung Association or the COPD Foundation.

