Staying active is one of the most difficult, yet most important, things you can do to stay healthy with COPD. Regular exercise is not only beneficial for your disease, but it's absolutely necessary for your survival and maintaining a good quality of life.
The good news is that there are plenty of special techniques you can use, and activities you can do, to make exercising with COPD easier and more fun. With the right exercise routine and treatment plan, you can get all the physical activity you need to stay healthy without feeling breathless and fatigued.
Why Exercise is Important When You Have COPD

Regular exercise is necessary for a healthy lifestyle, whether you have a chronic disease or not. But when you have a serious respiratory disease like COPD, regular exercise is a necessity to prevent your disease from getting worse.
Physical activity is just as important for your heart, lungs, and muscles as it is for your psychological and emotional health. It gives you strength, energy, confidence, and is a great mood-lifter, too.
Although you might feel breathless easily when you first start out, regular exercise can actually strengthen your breathing muscles and make it easier to breathe in the long run. Also, getting out your energy through physical activity during the day will help you sleep easier and more comfortably at night.
Staying active will help you feel better, eat better, and increase your overall stamina and endurance. It also helps keep your heart healthy, boosts your immune system, and reduces your risk for heart disease and other complications. But it comes with more than just physical benefits; exercise can improve your mental health, too.
Living with COPD can be stressful and overwhelming, but physical activity can help relieve your worries and stress. Another benefit of staying active that's often underestimated is self-confidence. The satisfaction you gain from seeing yourself make progress and get stronger as you exercise is empowering and invaluable.
How Exercise Benefits Your COPD

It's important to understand that nothing, including exercise, can cure or reverse the severity of your disease. However, it can prevent your COPD symptoms from getting worse, and can slow down the progression of your disease.
Here is a list of some of the most important benefits you can gain from regular exercise when you have COPD:
- Symptom improvement, including reduced breathlessness and fatigue
- Stronger muscles and improved muscle tone
- Improved balance and flexibility
- Better circulation
- Lower blood pressure
- Better sleep and less restlessness
- A healthy weight (and the ability to lose weight, if needed)
- Reduced anxiety and depression
- Stronger bones
- Better self-esteem and self-image
- Increased strength, mobility, and ability to do daily activities
It's hard to overstate the benefits of regular activity when you have COPD. If you have trouble staying motivated, just remember that regular exercise can mean the difference between an early death or a long, fulfilling life with your COPD symptoms under control.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Preventing Progressive Physical Decline
Hopefully, a better understanding of the benefits of exercise is enough to motivate you to get started. However, it's just as important to know the consequences of not exercising and the effects it can have on your COPD.
Here are some of the consequences of not exercising when you have COPD:
- Muscle wasting, weakness, decreased physical strength
- Worsened breathlessness
- Weight gain
- Depression and anxiety
- Loss of independence and increased difficulty with everyday activities
Even if what you have to gain from regular physical activity isn't enough to motivate you, you should understand that you still have a lot to lose if you choose to stay sedentary.
Even if you feel weak and have difficulty breathing right now, it's no excuse to avoid exercise. If it's difficult now, it will only get worse and worse with time if you don't find a way to stay active.
The Basics of Exercising with COPD
Working With Your Doctor
When you have COPD, it's very important that you work with your doctor to put together an exercise routine that works for you. Every person and every case of COPD is unique, and different people might need to focus on different areas of strength.
You should plan to meet with your doctor to discuss physical activity as soon as possible after getting diagnosed with COPD. Make sure to talk to your doctor about all of your symptoms and physical struggles so he can tailor your exercise plan to your needs.
Exercising with COPD often requires special considerations and techniques so as not to make you feel breathless too easily. Make sure you talk to your doctor about how often and how long you should exercise, if there are any activities you should avoid, and if there are medications you can use to make exercising easier.
Exercising at Home
When you have a serious illness that makes it difficult to breathe, it can be hard to make it to the gym on a regular basis. This is especially true if you have decreased mobility or use supplemental oxygen.
That's why many people with COPD opt for exercise routines that they can do at home. It can make it easier to stay motivated, help you stick with a routine, and keeps you close to your medication, supplemental oxygen, and all the comforts of home.
While some people prefer the gym and think that it makes sticking with a routine easier, it's possible to get all the physical activity you need in and around your own home. All you need is an open space to move your body, a chair, and a small set of free weights to do all the exercises you need to stay healthy.
What Kinds of Physical Activities Are Recommended for COPD Patients?
When you have COPD, it's important to start any new exercise routine by taking it slow and setting small, realistic goals. Exercising is safe for your lungs as long as you stay within your doctor's recommendations and limitations, but you should still take care not to overexert yourself or push yourself too hard.
Every person's exercise plan with COPD looks different, and your routine might be more or less intense than other patients' based on your physical condition and the severity of your disease. The important part is to make progress without stretching yourself too far, and to set personal, reasonable goals that you can realistically meet.
That said, there are three things that every healthy exercise plan should include: cardiovascular activity, strength training, and stretching. We'll go through each one by one.
Cardiovascular Exercise

Cardiovascular exercise is a type of activity that includes walking, running, biking, swimming, and much more. It tends to work out large muscle groups and it's all about getting your heart pumping and keeping your body continuously moving.
Regular cardiovascular activity is vital for your heart and lungs and is an effective way to improve your overall tolerance for physical activity. Over time, cardiovascular exercise can lower your blood pressure and heart rate, strengthen up the muscles you use to breathe, and make it so your heart and lungs don't have to work as hard when you're active.
Cardiovascular exercise is also a great way to lose weight and improve your body's overall metabolism. Most doctors recommend getting 20-30 minutes of cardiovascular exercise at least three times a week, but you might need to work up to that amount slowly over time. Also, make sure you talk to your doctor before starting any new exercise routine.
Cardio exercises are usually divided into two groups: high impact (requiring a great deal of exertion) and low impact (requires less exertion). If your COPD is severe or you suffer from chronic pain, you may need to stick with low-impact exercises so you don't push yourself too hard.
Strength Training

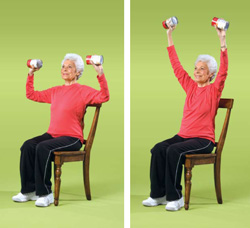
Strength training is a kind of anaerobic exercise that includes weight training, abs workouts, lifting, and more. It usually involves standing or sitting in one place and working out one muscle group at a time by flexing and lifting parts of your body.
There are many different benefits of strength training, including increasing your overall strength and endurance and boosting your metabolism. With this kind of exercise, you can gradually build up strength, balance, and endurance and focus your efforts on specific parts of your body that you want to improve.
Strength training exercises are often split up into two more categories: upper and lower body exercises.
Working out the muscles in your upper body is especially important if you have COPD, because it can strengthen the respiratory muscles you use to breathe. Upper-body strength training focuses on the arms, shoulders, neck, chest, abdomen, and back.
Lower-body strength training exercises are also important, because they can improve your mobility by making it easier to stand and walk for extended periods of time. Lower-body exercises include activities that work out your thighs, calves, ankles, and buttocks.
Stretching
Some people do a combination of strength training and cardiovascular training in the same workout, while some people alternate focusing on one or the other on different days of the week. Stretching, however, is something that you should do every day, and especially before every single workout.
Stretching can help you feel better by improving your range of motion, improving your flexibility, and reducing stiffness in your muscles and joints. It's a perfect way to start your day when you get up in the morning or to get your blood flowing when you've been sitting still for awhile.
Stretching is also an important safeguard against getting injured, which is why you should always stretch for 5-10 minutes before beginning any kind of physical activity. You should stretch each part of your body for at least 10 seconds to reduce your chance of muscle strain, soreness, and injury when you exercise.
Warming Up and Cooling Down
Every workout you do should include a brief 5-10 minute warm-up period before your main exercise and a 5-10 minute cool-down session afterward. This helps prevent injury and overexertion, and helps your body slowly adjust to increased activity.
This is especially important to do when you have COPD, so make sure you don't forget these steps.
How to Warm Up
A good warm-up exercise allows you to slowly and gradually increase your heart rate and breathing rate. This reduces strain and pressure on your heart and lets your body get accustomed to the physical activity.
As you do your warm up, start with easy, slow movements and increase your effort and level activity gradually as you go. You should always include at least a few minutes of stretching in your warm-up to loosen up your muscles and joints.
Here are some examples of common, effective warm-up exercises:
- Stretching your legs, arms, waist and neck
- Gently moving your joints, including your ankles, knees, shoulders, and elbows (move them left and right, up and down, and in a circular motion one at a time)
- Walking
- Very light, slow versions of your main workout activities
How to Cool Down
Cool-down sessions are very similar to warm-up sessions, except you want to slowly decrease your level of activity as you go, instead of increasing it. Start by gradually decreasing the intensity of your main workout toward the end, then cool down by walking, stretching, and doing light, low-impact movements.
A good cool-down session will reduce your heart rate and body temperature slowly back to normal and help you feel less sore and fatigued after your workout. Just make sure to decrease your exercise intensity little by little, and don't forget to spend a few minutes stretching your worn-out muscles before you call it a day.
Control Your Breathing
What makes exercising the hardest for people with COPD is the constant threat of breathlessness. If your disease is severe, even short periods of light activity can make it difficult to breathe.
That's why deep breathing techniques are an essential part of exercising when you have COPD. If you can prevent shortness of breath while you exercise, you'll have more energy and endurance to devote to getting in shape.
Make sure to practice breathing exercises and take breaks whenever you feel exhausted or short of breath. If you struggle with breathlessness often, talk to your doctor about pulmonary rehabilitation, supplemental oxygen, or other medications that might help you better control your breathing while you exercise.
It can be overwhelming and difficult to think of what to do when you can't catch your breath, which is why most doctors recommend that you take time to practice breathing exercises every day, even when you don't feel breathless. That way, when the time comes that you are struggling for air, you'll be able to easily remember the steps and bring your breathing back under control.
Pursed Lips Breathing

This breathing technique helps push trapped air out of your lungs and keeps your airways open longer so it's easier to breathe. You should use this breathing technique any time you exert yourself, do any kind of physical activity, or start to feel breathless.
Here's how to practice the pursed lips breathing technique:
- Relax your shoulders and straighten your back
- Take a deep breath in through your nose, making it last about 2-5 seconds.
- Then, purse your lips together, as if you were going to whistle or blow a kiss.
- Breathe out for about twice as long as you inhaled, but through your mouth instead of your nose (about 4-10 seconds).
- Repeat.
Diaphragmatic Breathing
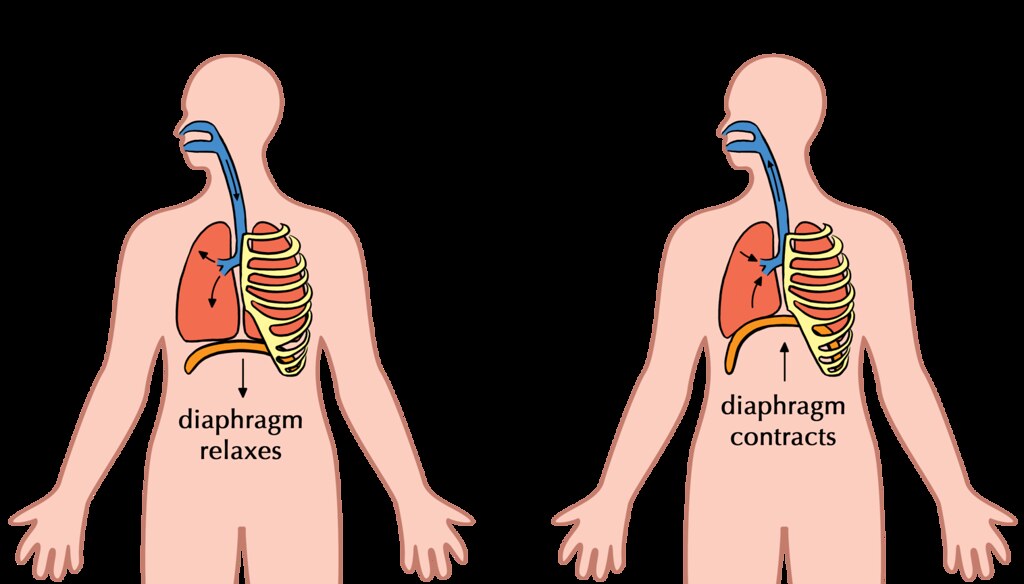
The purpose of diaphragmatic breathing is to help you use your diaphragm, instead of your chest muscles, to breathe. This technique helps you strengthen your diaphragm and use less effort and energy to breathe.
Here's how to practice the diaphragmatic breathing technique:
-
This technique is easiest to practice when you lie down flat on your back, but you can do it while standing or seated as well.
-
Lay one of your hands on your stomach, and the other on your chest.
-
Take a slow, deep breath in through your nose. Pay attention to your hands on your chest and abdomen; you want to feel your stomach rise as you inhale, and your chest to stay still.
-
Exhale slowly through your mouth, again paying attention to how your chest and abdomen move. You should feel your stomach deflate and your chest should stay as still as possible.
- The goal of this exercise is to focus on using your abdomen (diaphragm) to breathe. You should try to keep your chest as relaxed and still as possible, while moving only your stomach when you breathe.
Cardiovascular Exercises You Can Do at Home for COPD
Walking

Walking is a great light, low-impact exercise that's easy to do at home if you have COPD. It's a great way to improve your endurance, and studies show that walking at least four hours per week alone can significantly reduce your risk of heart disease.
The great thing about walking is that you can go at your own pace and it's easy to sit down and take a break whenever you feel tired or breathless. You can get your exercise by walking in your yard or around your neighborhood, or you could go out to a local park or trail for a more scenic stroll.
Here are some tips for walking for exercise when you have COPD:
-
Start small and slow. Don't push yourself too hard at first, but don't give up too easily, either.
-
Add a certain number of feet or steps on to the length of your walk every day (an extra 10 feet a day is a reasonable goal). If you ramp it up gradually, you will steadily get stronger with hardly any extra effort.
-
To control your breathing, exhale through pursed lips for about twice as long as you inhale. It can help to count the number of steps you take while you breathe in, and then take twice as many steps as you breathe out. This is a great way to get a steady rhythm going so you can keep control over your breathing.
- Make sure to turn around soon enough or walk a short enough loop that you can make it back to where you started before you get too fatigued. Don't be afraid to stop and rest any time you feel too tired or breathless, and don't start again until you are breathing normally.
Aerobics

You've probably heard of aerobics classes before; you can usually take them at your local gym or you can follow along with an aerobics training video at home. Even though they had their peak in the 80's, aerobics video routines are still an extremely effective, engaging way to get a good workout.
You can purchase aerobics workout DVDs or get a free aerobics workout by watching any of the many videos available on YouTube and elsewhere online. The best thing about it is that there are so many different kinds and lengths of aerobic workouts. You can tune in to a short ten-minute routine or a 30-minute one, or you can string several short aerobic workouts together with rests in between.
You can do dance aerobics, step aerobics, water aerobics, strength-training aerobics, and more. Aerobic workouts can be extremely satisfying and fun, and you're bound to be able to find a style that fits your interests.
Stair Climbing
Stair climbing is a moderate-intensity activity that you can do at home or any place with a set of stairs. Just make sure you have a handrail to stabilize yourself and stop to take breaks whenever you feel out of breath.
It's important to control your breathing, so practice slow, pursed-lips breathing as you do this exercise.
Tips for Stair Climbing with COPD
- Take a deep breath in before you start ascending the stairs.
- Take two steps up while you exhale slowly through pursed lips.
- Take another breath in and rest a moment before continuing
- Take another two steps up while you exhale again
- Descending the stairs isn't nearly as difficult, and you should be able to take more steps with each breath. Start on the inhale and count how many steps you can take down as you breathe in. Then, try to take twice as many steps down on your exhale as you breathe out slowly.
- Take your time! It's not a race or a contest, and it's okay to take it as slowly as you need to. You'll build up strength with time, but you have to start at your own pace.
Other Aerobic Exercises for COPD
We've listed some of the most common physical activities you can do to get a good aerobic workout with COPD. This is only a small list, however, and the possibilities for aerobic exercise are nearly endless!
Here are a few more ideas for aerobic activities you can do at home with COPD:
- Jogging or Running (high impact)
- Biking (low impact)
- Jump Roping (high impact)
- Playing with pets or children (low impact)
Strength Training Exercises You Can Do at Home

Strength training encompasses a large variety of stationary workouts that flex and strengthen your muscles. Many of these are exercises that don't require any extra equipment, and use simple movements and the weight of gravity to work out your body.
Some home strength training require, or are enhanced, by using free weights. You should start small, with 3 or 5 pound weights, and add more to your collection as you move up to more weight.
Yoga

Yoga is one of the best possible strength training exercises you can do with COPD. Why? Because it's slow-paced, great for your heart, and helps you practice steady, deep breathing while you exercise.
Yoga involves involves slow, steady movements and holding poses that help you build up muscle strength and improve your balance. Practicing controlled, deep breathing is also an integral part of yoga practice, which is particularly helpful if you struggle with breathlessness.
Yoga can help you build the strength you need to do even more kinds of exercise and can help you train yourself to control your breathing whenever you do physical activities. To practice yoga at home you can use yoga DVD's or you can access a huge number of yoga instructional videos online and on YouTube.
Chair Exercises

Many of the techniques we'll show you in the following sections “Upper Body Exercises” and “Lower Body Exercises” can be done as chair exercises. That means you can do them while sitting upright in a chair, and they're a great way to get some extra strength training in without having to leave your seat.
All chair exercises are exercises you can do at home, and they allow you to work out your muscles without having to expend energy to walk or stand. This can help reduce breathlessness and fatigue when you exercise, and is a great solution for people with COPD who have limited energy

In both developed and undeveloped countries around the world, it is estimated that 9-10% of people are affected by Chronic Obstructive Pulmonary Disease (COPD). Experts have made a prediction that by 2020, it will be the third leading cause of death in the world as the population ages and people continue to smoke. More than 12 million people have been diagnosed with COPD in the United States alone and it is the third leading cause of death claiming more than 120,000 American lives each year.
COPD is an umbrella term used to describe progressive lung diseases including chronic bronchitis, emphysema, refractory asthma and some forms of bronchiectasis. It is mainly characterized by shortness of breath. In its initial stages, COPD may show no symptoms or have very mild symptoms but as the disease progresses, the symptoms usually become more severe.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Physicians have traditionally measured the severity of COPD by the amount of air a person can forcibly exhale in one second (FEV1). The amount of air usually decreases as COPD becomes worse. Just the same, COPD affects other systems and body parts, which helps provide clues about the severity of the disease. A lot of physicians are now using the BODE index to categorize COPD and predict outcome. BODE is short for body-mass index, degree of airflow obstruction, dyspnea (breathlessness), and exercise capacity as measured in a 6-minute walk test.
You are probably familiar with COPD classic symptoms which include;
- Frequent respiratory infections.
- Lack of energy.
- Chronic cough with production of a lot of mucus.
- Experiencing shortness of breath, especially with physical activity.
- Chest tightness.
- Wheezing or hearing a whistling sound when you breathe.
- Blueness of the lips or fingernail beds.
You however may not be aware of the potential common complications associated with COPD and how you can limit them. Below is a list of 6 complications that you may face with COPD.
1. Cor Pulmonale

This refers to a failure of the right side of the heart. It is a condition in which the right side of the heart swells up (lower extremity edema) and cannot pump blood properly. COPD makes the heart work harder, especially on the right side which pumps blood into the lungs. Due to poor gas exchange in COPD, there are reduced amounts of oxygen in the blood causing blood vessels to constrict. Many of the capillaries around the alveoli are destroyed in the disease process making the heart work even harder for blood to be forced through fewer constricted blood vessels. Because of all this effort, the right ventricle swells up, the walls of the heart become thicker, and the chamber over time loses its ability to contract efficiently.
Symptoms of cor pulmonale include fainting spells and discomfort in the front of the chest. To control your symptoms your doctor may recommend a low-salt diet, medication or supplemental oxygen. If you are an active cigarette smoker, you should plan to quit. You should also engage in mild to moderate physical activity to build up heart and lung stamina. Remember to consult your doctor before you start any exercise regimen.
2. Pneumonia

Pneumonia is a lung infection that can be caused by a bacteria or a virus, and can lead to respiratory failure in patients with COPD. COPD weakens the respiratory system increasing vulnerability to pneumonia. Because people with COPD already have weakened airways and a worse immune system, the likelihood of them to die from pneumonia is higher than that of patients without COPD.
Symptoms of pneumonia usually include coughing, a fever, and having a difficult time breathing. Pneumonia is more common in COPD patients that take steroids for their symptoms. You should consider talking to your doctor about getting a pneumonia vaccine if you have not already gotten one.
One dose is usually enough for most people, a second dose may be suggested for some, including those that have been using steroids for a long time. Antibiotics can also be used to treat pneumonia caused by bacteria. Streptococcus pneumonia is the most common cause of bacterial pneumonia in patients with COPD. To reduce the risk of getting infected, you should;
- Drink plenty of fluids especially water, to maintain healthy bronchioles while thinning out mucus and secretions.
- Quit smoking.
- Wash hands consistently.
- Avoid contact with people you know are ill.
- Discourage sick family members and friends from coming to visit your home.
Overall good health is key to preventing infections.
3. Depression

Shortness of breath that limits your activities can have you feeling down in the dumps and lead to loss of interest or pleasure in activities. Having this feeling every once in a while is okay but when you feel this way frequently then you may be undergoing depression. One study estimated that 40 percent of people with COPD suffer from depression.
Depression can lead to the worsening of your physical symptoms because you may not fell like exercising and feeling low all the time might make it hard for you to follow your treatment plan.
You may even turn to alcohol, cigarette smoking or any other unhealthy habits to help you cope with depression which can lead to more harm to your body. Do not ignore how you are feeling and talk to your doctor about this so that they can get you the help that you need. Signs to look out for include;
- Feeling guilty or worthless.
- Being overly sensitive to criticism.
- Feeling hopeless or suicidal.
- Having trouble falling asleep or staying asleep.
- Having trouble making decisions and concentrating.
- Lethargy and lack of motivation.
Your doctor may recommend antidepressant medication or talk therapy. You may also decide to join a support group with other COPD patients or a pulmonary rehabilitation program to help you fight depression.
4. Osteoporosis

This is a complication that sometimes occurs with COPD causing the weakening of the bones. Bones are made with living tissue and as older bone tissue breaks down, new bone tissue is created. When the nutrients in the body are not enough to create new bone tissue, the bones may become weak and fragile, and when this occurs, the risk of getting fractures is greatly increased. Although no exact reason can be given by researchers on the coexistence of COPD and osteoporosis, some theories for what the cause may be include;
-
Cigarette smoking – some researchers believe that some chemicals in cigarette smoke cause changes in the body, and these changes include genetic changes that may cause bones to become weak and slow to heal.
-
Corticosteroids – these are commonly used by COPD patients to control COPD flare-ups and to reduce airway inflammation, and a common side effect of corticosteroids is osteoporosis.
- Low vitamin D levels – people with COPD may opt to stay indoors and lack of exposure to the sun, causing low levels of vitamin D. Low vitamin D levels have been linked to poor bone growth and skeletal mass, which may contribute to osteoporosis.
Your doctor can check your bone health with a bone density scan. You may need prescription medicine along with calcium and vitamin D supplements to keep your bones strong. You may also want to exercise as research has shown that progressively harder weight-bearing exercise, such as strength training can boost bone health. Consult your doctor before you start any exercise regimen.
5. Trouble sleeping

It is very common for people diagnosed with COPD to have trouble sleeping. In fact around 50 percent of COPD patients face this problem. This is a problem because getting enough sleep is vital for all body functions to work properly.
Sleeping problems linked with COPD include; low levels of oxygen during sleep, sleep apnea, depression, medication used to treat COPD symptoms and some of the COPD symptoms like coughing and wheezing.
You should let your doctor know if you are experiencing trouble sleeping so that he can figure out what is causing it and then treat it. A few things you can do to help with this problem include:
- Keep the room that you sleep in cozy, dark, cool and quiet.
- Practice airway clearance techniques throughout the day and right before you sleep to remove secretions in your airways.
- Ask your doctor if night-time use of supplemental oxygen is an option for you.
- Review the medicine that you are using with your doctor to see if it has any side effects. You may require an adjustment.
- Talk to your doctor about non-invasive positive-pressure ventilation (NIPPV) such as CPAP if you suffer from sleep apnea or other sleeping disorders.
- Try not to drink caffeinated beverages late in the day or avoid them altogether.
- Do not sleep lying flat. Elevate your upper body with pillows to help facilitate breathing.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
6. Pneumothorax

Pneumothorax, which is also referred to as a collapsed lung, occurs when a hole develops in the lung, allowing air to escape into the space around the lung causing the lung to partially or completely collapse.
People diagnosed with COPD are at higher risk of getting pneumothorax because the structure of their lungs is weak and vulnerable to the development of these types of holes. It can be caused by an injury to the lung, rib fracture, certain medical procedures and in some cases air pressure changes for example high altitude.
Signs to look out for include sudden sharp chest pains that worsen when you take a deep breath, rapid heartbeat, chest tightness, and cyanosis caused by lack of oxygen.
Pneumothorax can be treated by inserting a chest tube between the ribs into the space between the lung and the chest wall to help remove the air and re-inflate the lung. The chest tube stays in place for a number of days as the patient recovers in hospital. In some rare cases, surgery is required to prevent future occurrences.
If you have COPD, the first sign that something was not right was likely feeling shortness of breath, to the point that you wanted to see your doctor about it. It also could have been that incessant cough throughout the day and night.
It's easy to blame a cough on allergies or a common cold, but if it persists and becomes a regular thing, you should see your doctor to discuss the possibility of having COPD or another lung ailment. The sooner you find out if it is COPD causing your symptoms the sooner you will be able to treat the chronic illness, thereby slowing down the progression of your COPD.
The first thing that you need to understand is that coughing may seem like a symptom you want to relieve, but in the case of COPD, it actually serves a function.
Continue reading to understand how COPD and coughing are related, what you can do to ease a cough, and when to seek medical attention.
How are COPD and Coughing Related
If you have COPD you probably experience a persistent cough. This symptom is related to a condition of COPD called chronic bronchitis, which means that your airways are constantly irritated. This irritation is often caused by smoking or second-hand smoke, but it can also be caused by other irritants and biological factors, such as pollution or genetics.
The irritation in your airways causes two problems that prevent enough air from passing through to the lungs:
- The lining of your airways become swollen
- There is too much mucus produced by your lungs
People with chronic bronchitis can have a persistent cough because it is important to regularly clear their swollen airways of this excess mucus, which can sometimes be difficult and require extra attention and treatments, of which, we will discuss in more detail in the What you can do to ease a cough associated with COPD section of this article.
So, coughing caused by COPD is often productive and it is a natural function of your body that plays an important role in your breathing system. Coughing helps to move extra mucus out from your lungs. Coughing is also a reaction that can help remove certain irritants you may inhale into your lungs, like dust, pollution, and other common allergens.
When your cough produces mucus, which is also called sputum or phlegm, that means your body is working correctly to clear the excess mucus up through your swollen airways and into your throat and out of your mouth.
It is normal for the mucus to be clear or white, yellow, or green in color but if the mucus is very mucky, it may be a sign of a respiratory infection. We will go over this in more detail in the When you should see a doctor section
What you can do to ease a cough associated with COPD
To determine whether or not your cough needs to be treated with medication or other remedies, depends on the type of cough you are experiencing and whether or not your cough is actually helping to clear your lungs and airways.
You should consult with your doctor to determine the type of cough you are experiencing and how to deal with it going forward.
As we discussed in the section above, airway clearing coughs serves a meaningful purpose by clearing out mucus from your airways. In this case, it is best for you to continue coughing in order to avoid mucus building up in your lungs.
.png)
That being said, there are certain medications you can take as well as techniques you can learn how to perform in order to couch more effectively.
COPD and coughing medications
If your cough is due to very thick mucus, first you should try to drink more fluids. This can help make your mucus thinner and easier to clear. If this does not work well enough, then there are medicines called “expectorants” that can help make the mucus easier to cough up.
If your coughing becomes painful or difficult to control. In those cases, your doctor might recommend cough suppressants that keeps your body from coughing. These suppressants might also be used for coughs that do not produce mucus, like a dry smoker’s cough.
If you have COPD, coughing can also cause a “bronchospasm” or “spasm.” This happens when your muscles around your airways suddenly tense up causing your airways to become very narrow, This makes it even hard to breathe. To reduce coughing that causes spasms, healthcare providers might prescribe special types of inhaled medications called “bronchodilators” or inhaled steroids.
.png)
If you are not interested in getting on medication for you coughing, there are also three airways clearing techniques you can do to clear your lungs
Airway clearing techniques for COPD
One of the most effective ways to clear your airways is to use the effective, or controlled, cough technique. This cough comes from deep within your lungs and has just enough force to loosen and carry mucus through your airways without causing them to narrow or collapse. By utilizing the controlled coughing practice, you will save energy and therefore, oxygen.
- Controlled coughing: A type of cough that comes from deep in your lungs. It loosens mucus and moves it though your airways
- Postural drainage: You lie down in different positions to help drain mucus from your lungs
- Chest percussion: You lightly tap your chest and back. The tapping loosens the mucus in your lungs
To cough effectively:
- Sit on a chair or on the edge of your bed, with both feet on the floor. Lean slightly forward. Relax
- Fold your arms across your abdomen and breathe in slowly through your nose. (The power of the cough comes from moving air.)
- To exhale: lean forward, pressing your arms against your abdomen. Cough 2-3* times through a slightly open mouth. Coughs should be short and sharp. The first cough loosens the mucus and moves it through the airways. The second and third cough enables you to cough the mucus up and out.
- Breathe in again by "sniffing" slowly and gently through your nose. This gentle breath helps prevent mucus from moving back down your airways
- Rest
- Perform again if needed
Here is a link to postural drainage and chest percussion treatment and how to perform these mucus clearing techniques.

Natural home remedies for helping reduce COPD induced coughing
Eucalyptus oil
Eucalyptus oil contains a natural compound called eucalyptol. Eucalyptol may have the following benefits for people with COPD and may ease uncomfortable coughing symptoms:
- antioxidant and anti-inflammatory properties
- opens up the airways in the lungs
- reduces mucus production
- helps clear mucus from the lungs
- prevents flare-ups in moderate to severe COPD
One way you can use eucalyptus oil is by adding 12 drops of eucalyptus oil to 150 milliliters of boiling water and inhaling up to three times per day.
This will not work for everyone, and if you experience any side effect of the oil, stop using it immediately.
-1.png)
Quit Smoking to reduce dry coughing
Smoking is the leading cause of COPD in the United States and is responsible for around 90 percent of COPD-related deaths.
Tobacco smoke is known to irritate your airways and your lungs. Smoke causes inflammation and obstruction within your airways causing them to narrow, and making it very difficult for air to pass in and out.
If you smoke, the most important step to reduce COPD related symptoms and slowing down the progression of your COPD is to stop smoking. Quitting will put an end to “smoker’s cough,” the dry, hacking cough common among people who smoke.
A deep, productive cough that clears the airways of mucus may replace this dry cough also benefiting you and your breathing.
-png.png)
When you should seek medical attention
Call your doctor within 24 hours if you notice:
- You’re out of breath or coughing more than usual
- Being out of breath affects your daily routine
- You’re coughing up more gunk that normal
- The mucus you are coughing up is dark yellow, dark green, or rust-colored
- You have a fever over 101 F
- You feel dizzy or lightheaded
If you begin to experience any of these symptoms it could mean that you have a respiratory infection or your COPD is getting worse.
Call 911 or go to the emergency room if you’re still out of breath after using the medicines your doctor has prescribed for your COPD.

Other symptoms associated with COPD
One of the other many symptoms of COPD we mentioned very briefly in this article was shortness of breath. When you have COPD your lungs are no longer able to process oxygen like they once did. This is partly due to the irritation in your airways that also causes coughing.
Both chronic bronchitis and emphysema can cause shortness of breath. This symptom is also called “breathlessness” or “dyspnea".
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
If you airways are swollen and filled with mucus, not only does this initiated a coughing reaction, but it also inhibits oxygen from flowing through your lungs and into your blood stream and organs.
Not only is this feeling extremely uncomfortable, it is also life threatening, and if it goes untreated for a long period of time, you will inevitably be taking years off of your life.
Here are positive changes you can make to improve breathing with COPD:
Learn pursed-lip breathing This is a breathing exercise designed for people with COPD: Purse your lips and blow as much air out as you can before taking a deep breath in through your pursed lips again. Then slow down your breath so that you’re using as much of your lungs as you can. This technique slows your breathing rate and helps to keep your airways open which can also help to reduced coughing episodes.
Drink plenty of water because water helps thin out mucus so you can clear it better. Some people with COPD have conditions that could be made worse by extra fluid, however some people with COPD may be very dehydrated.Speak with your doctor to find out how much water you can safely drink.
Get informed and continue learning about COPD and how your lungs function. This can help you better understand and manage your condition. Pulmonary rehabilitation programs often offer this type of education.
Exercising regularly can make a big difference in your breathing capabilities and COPD symptoms. A lot of people with COPD get more and more out of breath as their disease progresses, but it’s not due of their lung function — it's because they’re not conditioning enough. Most doctors recommend walking for people with COPD since it’s moderate in intensity and easily accessible.
Know and avoid your triggers. If you have COPD and allergies, take steps to avoid anything you’re allergic to. This may mean putting dust covers on your pillows and mattress or keeping your pets out of the bedroom. High-efficiency particulate air filters can remove dust and other irritants from the air in your home. You may also consider a humidifier if dry air triggers your symptoms.
Get your rest Many people with COPD have an underlying sleep disorder, like sleep apnea, that makes it difficult to get good sleep. When you sleep better, you’ll feel better and breathe better, so if you are not able to fall asleep, or have trouble staying asleep, speak with your doctor to understand the root of this issue so you can solve it.

Stay on a healthy diet full of nutrient-dense foods is needed with COPD to maintain strength and fight off infections. Eating healthy can help you lose weight and breathe easier. If you’re underweight, ask your doctor about the best foods to eat and if nutritional supplements are right for you.
Take your medication COPD medications can help manage symptoms, including shortness of breath so be sure you’re taking the right medications and get evaluated to make sure your lung function is as good as it can be
If you have severely low oxygen levels this is called hypoxemia, your doctor will likely prescribe you medical-grade oxygen, for home oxygen therapy. Long-term oxygen therapy has many benefits if it is used correctly and It can even help you live longer.

Low oxygen symptoms of hypoxemia vary depending upon how severe your COPD is, and how severely it affects you. If you experience any of the symptoms listed below, contact your doctors as soon as possible. If you experience more than one of the following symptoms at one time, seek medical attention immediately:
- Confusion
- A sense of euphoria
- Restlessness
- Headache
- Shortness of breath
- Rapid breathing
- Dizziness, lightheadedness and/or fainting spells
- Lack of coordination
- Rapid heart rate
- Elevated blood pressure
- Visual disturbances
- A bluish tint to the lips, earlobes, and/or nail beds (cyanosis)
Hypoxemia is the main reason that people with COPD and other lung diseases are prescribed supplemental oxygen. There are a few forms of home oxygen therapy: You can opt for liquid oxygen tanks, gas cylinder tanks, or the most popular, convenient, and cheapest option a portable oxygen concentrator.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
If you are a good candidate for long-term oxygen therapy, this is a blessing in disguise. While it might seem as if you lung function is declining, once you are able to utilize oxygen, your quality of life will improve drastically. When you have adjusted to the oxygen therapy, you will begin to slow the progression of you COPD as well!
Once you find the right POC for you, your bones and muscles will feel stronger and energized, you will have improved exercise tolerance, your mood and stamina will boost, your quality of sleep may improve, and so much more.

If you feel like you have experienced any of the symptoms of hypoxemia, and are curious how to find the best portable oxygen concentrator to fit you oxygen requirements, fill out the blue box to the right, it is our official guide to portable oxygen concentrators.
Cough with a Purpose
Remember, COPD-related lung damage can’t be reversed, but it can be controlled if treated properly.
Now that you understand that your cough can in fact be beneficial for your health and in treating COPD, we hope that you can use the information in this article to cough effectively and efficiently. These coughing techniques, mixed with medication and other home remedies should reduce the dry uncomfortable smokers cough, and help you to cough with a purpose.
Even though this can be a pain, always feel free to excuse yourself during social gatherings, and other outings to clear mucus from your lungs and airways. This will allow you to go longer without coughing and spend more quality time with the ones you love while enjoying the things you like to do.
The more you practice these coughing techniques the more efficient you will become at clearing your airways, and therefore breathing!
If you have any questions please leave a comment on this blog below, and always feel free to share our blog with your friends and family. By explaining how beneficial your cough is for managing your COPD, they will better understand and be willing to help and encourage coughing rather than trying to help you avoid it.
When you inhale and exhale, the air in your lungs and airways may create turbulence called respiratory sounds — also known as “lung sounds” or “breath sounds.” You may know these sounds as “coughing” and “wheezing” but there’s actually a lot more to these sounds than you might initially realize. Breathing sounds are not only used to help diagnose lung conditions like COPD, asthma, and pneumonia but they can be used to assist medical professionals in directing and prescribing medication for these lung diseases.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In the following sections, we’re going to talk about four different types of respiratory sounds, what causes them, how they’re diagnosed, and how they’re treated. After reading, you’ll have a better understanding of the signs your lungs are giving you and what their implications are for your overall health and well-being. And as always, if you have an experience that you would like to share or you have any questions about what you read here, be sure to leave them in the comment section below.
What is the Significance of Respiratory Sounds?
When you visit the doctor with a list of symptoms, your doctor will use any and all tools in his/her toolbox in order to diagnose your condition. For example, your doctor may put you through a series of sleep studies if you report problems getting to sleep, staying asleep, or experiencing restful sleep. A sleep study can reveal exactly when the sleep disruptions are occurring and your doctor will be able to see what your brain activity is like when you sleep. By understanding the root cause of your sleeping problems, your doctor can provide you with treatment options that are tailored just for you.

One of the first methods your doctor will use when diagnosing a condition related to the heart or lungs is called auscultation. During auscultation, medical professionals use a device called a stethoscope in order to listen to the internal sounds of the body including the heart, lungs, and gastrointestinal system.
While auscultation is not the end all be all method for diagnosing lung conditions, it can help medical professionals rule out certain diseases without resorting to more invasive diagnostic methods. Some respiratory sounds like coughing and wheezing can be heard without a medical instrument but using a stethoscope, doctors can identify more subtle sounds that could not be heard otherwise.
Let’s take a look at the different types of lung sounds.
Normal Respiratory Sounds
Normal respiratory sounds are an indication that your respiratory system is healthy and functioning properly. But if you report having respiratory symptoms like chest pain, breathlessness, or chest tightness, your doctor will be able to perform a number of other tests to diagnose them.
CT scans, spirometry tests, pulse oximetry, and the six-minute walk test are just a few of the tests that can be used to diagnose lung disease.

Vesicular
The term “vesicular” is slightly misleading because “vesicle” refers to the alveoli (small air sacs in the lungs) which are responsible for the exchange of oxygen and carbon dioxide between the lungs and bloodstream.
However, the alveoli are not what makes the vesicular sounds. These sounds are soft, rustling, or blowing sounds heard throughout all of the lung fields. They’re heard throughout the duration of inspiration and continuously through one-third of expiration. Vesicular sounds are an indication that you’re able to fully inhale and exhale without obstruction.
Bronchovesicular
Bronchovesicular sounds are muffled but high pitch sounds where the expiratory and inspiratory phase is equal in duration. These sounds are heard over the first and second intercostal spaces (between the ribs) and the interscapular area (shoulder blade).
Bronchial
With bronchial sounds, the expiratory sounds are higher in pitch and intensity. The inspiratory sounds are lower-pitched, hollow, tubular sounds. Bronchial sounds are heard throughout the manubrium (the broad upper part of the sternum).
Tracheal
In tracheal sounds, the expiratory and inspiratory phases are equal in duration. The sound is loud, high-pitched, and heard directly over the trachea, the upper part of your respiratory system.
Abnormal Respiratory Sounds
Rales (Crackles)
Rales, or “crackles” as they’re more commonly called, are the result of fluid buildup in the airways (secretions). Rales are either exudate meaning they’re caused by a lung infection like pneumonia or they are transudate meaning they’re caused by congestive heart failure.
These noises can be heard when the patient inhales because the small airways pop open after collapsing during inhalation. There are three different types of crackles: fine, medium, and coarse.
- Fine crackles often occur during early inspiration and are fainter in volume.
- Medium crackles are more high pitched and they may indicate an interstitial process such as congestive heart failure or pulmonary fibrosis.
-
Coarse crackles last longer than fine or medium crackles and they tend to be louder and lower-pitched. They are most often a sign of excessive fluid on the lungs caused by pneumonia, chronic bronchitis, or pulmonary edema.
Wheezes
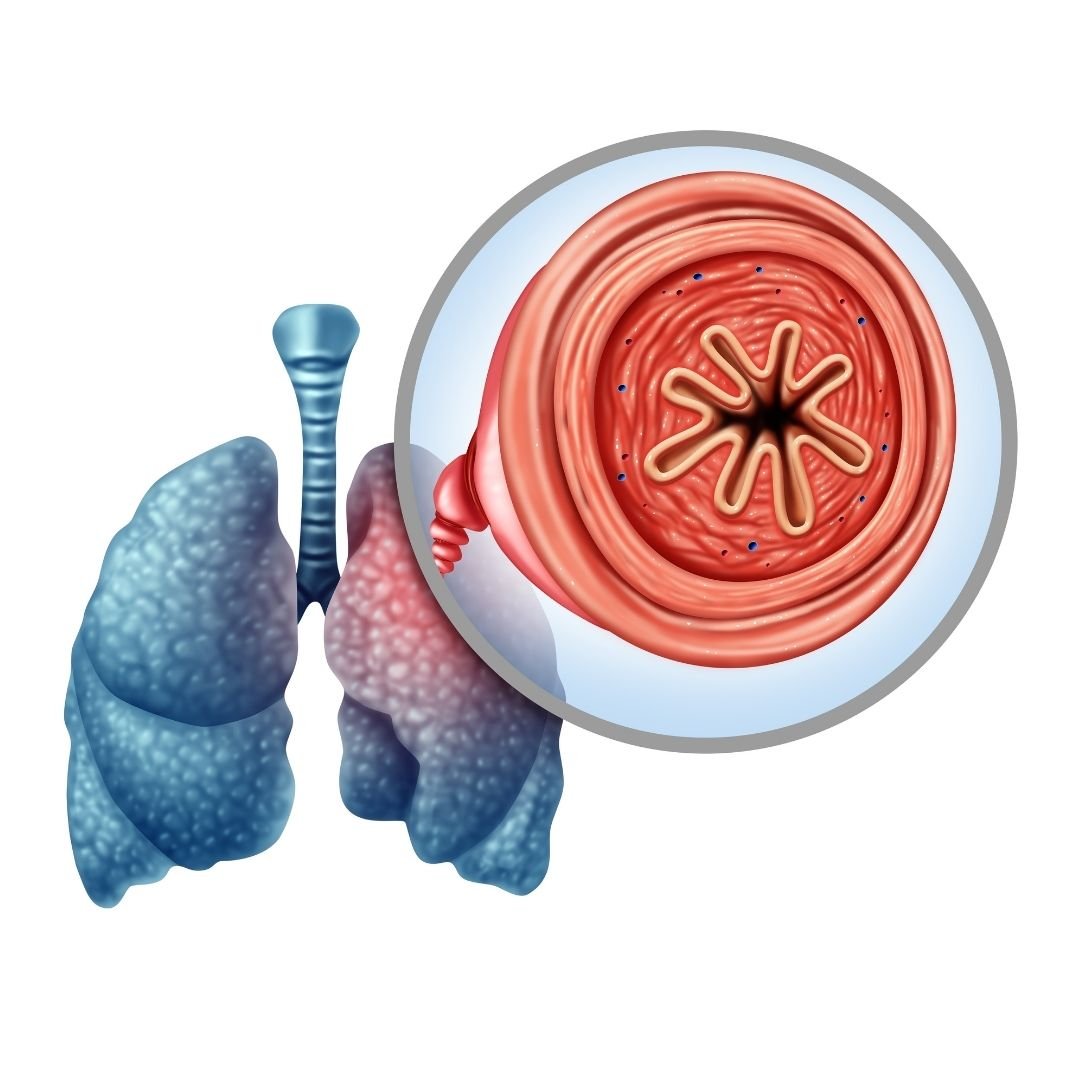
Wheezing is a sound that results from air being forced through a partially collapsed airway. When the same volume of air is being pushed through a smaller area, the velocity of the air increases which creates the sound.
Wheezing noises are often very high-pitched and continuous. Your doctor will be able to determine how many airways are obstructed based on whether the sound is monophonic (one sound) or polyphonic (multiple sounds). Expiratory phase wheezing may be connected to bronchiolar disease whereas inspiratory phase wheezing may be connected to tracheal stenosis.
Rhonchi
Rhonchi are similar to wheezing sounds but they are low-pitch and occur more frequently when the patient is exhaling. They can be an indication that the bronchial tubes or “bronchioles” are thickening due to the overproduction of mucus. Bronchioles are the tubes that lead from the trachea down to each lung. Rhonchi may be a sign of bronchitis or COPD.
Pleural Friction Rub
There’s a thin membrane that coats the outside of the lungs and the inside of the chest cavity called the pleura. The pleura secretes a lubricant that allows the chest wall to expand and contract freely. However, if the pleura becomes inflamed or damaged in some way, they will create a rough, scratchy sound that your doctor can pick up with a stethoscope.
This is called a pleural friction rub, or simply pleural rub. Pleurisy, pneumonia, and lung tumors are the most common causes of pleural rub.
Hamman’s Sign
Hamman’s sign (also called mediastinal crunch) is a crunching sound that occurs when there is air trapped in the mediastinum (the space between your lungs). The crunchy, scratchy noise that it causes is in sync with your heartbeat because the movement of your heart is what produces the noise.
In some cases, Hamman’s sign may mean you have a collapsed lung (pneumothorax) especially if it occurs in conjunction with shortness of breath and chest pain. However, it can also be caused by cystic fibrosis, pneumonia, or COPD.
.jpg)
How Are Respiratory Sounds Treated?
The way that respiratory sounds are treated depends entirely on what type of sound is being produced and what is causing them. This is why auscultation alone is usually not sufficient enough to diagnose a lung condition.
If you don’t have a history of respiratory issues, your doctor might perform further tests in order to determine if a chronic condition is the cause of the respiratory sounds. If you have a chronic disease like COPD, however, your doctor might ask you to increase your medication dosage.
-jpg.jpeg)
In COPD patients, the most common cause of breath sounds is mucus and phlegm that get lodged in the airways when you breathe. Clearing this mucus will not only help you breathe better but can also prevent conditions like bronchiectasis.
This is when you experience recurring lung infections due to bacteria that remain in the lungs for too long. Since lung infections are the most common cause of COPD exacerbation, it’s very important that you and your doctor deal with this problem as soon as it arises.
Medication
If your inability to clear the mucus is due to narrowed airways, your doctor may prescribe you something called a bronchodilator. These drugs open up the airways and prevent the “wheezing” noise whenever you try to cough.
Bronchodilators are almost always administered through either an inhaler or a nebulizer because this allows the medication to reach the affected area more quickly in the event of an emergency.

Controlled Coughing
Another method your doctor may recommend for dealing with blocked airways is breathing exercises or controlled coughing exercises. A normal cough is often erratic and solely focused on expelling as much air as possible.
On the other hand, controlled coughing is more focused on using air more effectively. There are several benefits of this. Firstly, it helps prevent breathlessness, fatigue, or something more serious like a hernia. Secondly, controlled coughing helps prevent the airways from closing which prevents mucus and phlegm from escaping. For more information on this, please read through our post titled “How to Cough Correctly with COPD.”

Smoking Cessation
Whether you’ve been smoking for a few days, a few months, or your whole life, there’s no better time to quit than now. Smoking is the number one cause of preventable illness in the world and there’s also a good chance that it’s causing the respiratory sounds that you’ve been experiencing too.
Smoking damages microscopic organelles in your airways called “cilia.” They are responsible for clearing mucus and phlegm out of the lungs and airways in order to prevent breathing obstruction and infection. In other words, the wheezing or crackling noise you hear when breathing could be caused directly by cigarette smoking.
![]()
When Should You Visit a Doctor?
You should visit a doctor any time that you experience unusual symptoms. While COPD is already associated with shortness of breath, if you notice your breathlessness becoming more severe or you notice wheezing or crackling noises in your chest, you should contact your doctor immediately. You can never be “too careful” when it comes to your respiratory health.
As aforementioned, if mucus or phlegm remains in the airways for too long without being cleared, this leaves you at risk of experiencing a lung infection, the number one cause of COPD exacerbation and hospitalization.

Conclusion
Respiratory sounds alone are usually not a cause for concern. Chances are, you’ve had the common cold before and know what it’s like to cough, wheeze, or experience difficulty breathing. However, if these symptoms become more persistent and last more than a few days, you should visit your doctor. By listening to your lungs, your doctor will have a better idea of what’s causing your symptoms and what further tests are needed in order to diagnose you with a respiratory condition.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
If you’ve been prescribed oxygen by your doctor either for temporary or long-term use, don’t hesitate to reach out to our respiratory specialists here at LPT Medical. We offer state-of-the-art portable oxygen concentrators which are much smaller, lighter, and more reliable than compressed or liquid oxygen tanks. We feature all of the top-rated brands including, but not limited to Caire Inc., Inogen, and Respironics. Simply tell us what your wants and needs are and we will provide you with a list of options that we believe will suit your circumstances.
Choosing a portable oxygen concentrator can be tricky because there are a lot of options out there. So best way to begin is by narrowing down your options based on a few components we will discuss in this article.
Based on whether you need pulse dose, continuous dose, or both and the flow rate you need, you will be able to narrow down your options.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
After you have a list of concentrators that will meet your oxygen requirements, you can continue narrowing down your option based on the unit’s weight, battery life, noise level, and sleep mode technology.
These priorities are based on your lifestyle and the qualities of life you value most.

You can start by asking yourself some questions:
Do I need a unit that is lightweight so that I can carry it easier while running errands?
Do I need a light weight unit so that I can start exercising more often?
Do I need a unit with long lasting battery life because I travel a lot?
Do I need a unit with long lasting battery life because I like to be outside without a power source for long periods of time?
Do I need a quiet unit because I am very sensitive to noise?
Do I need sleep mode technology because I already have trouble sleeping?
Once you have determined the list of units that meet your oxygen needs and have an idea of which lifestyle choices you prioritize, you should have a pretty great idea of which portable oxygen concentrator is best for you!
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
If you need help setting up these components, please call 1 - 800 - 946 - 1201, and a respiratory specialist will be happy to help guide you through this process.
Below is an infographic that goes through a few of the most popular oxygen concentrators on the market, and the “pros and cons” of each. You will notice there are very few cons, which is why they are so popular!

If any of these machines seem to be a great fit for you or if you do not see a machine that fits your needs, call us at 1 - 800 - 946 - 1201 or send us an email at info@lptmedical.com
You’ll be happy to know that every time you call LPT Medical, you’ll be connected with an experienced respiratory specialist who will be able to answer all your questions; whether it’s a question about an oxygen concentrator, financing information, Medicare, or pricing, we’ll get you squared away so you don’t have to worry.
The most popular portable oxygen concentrators of 2020 are linked here:
.png)

Spring is the season of new beginnings and fresh starts; it's the perfect time to get out your cleaning supplies and do some sprucing around the house. But spring cleaning isn't just a cliché, it makes sense to dedicate time once a year to catch up on chores and give some attention to neglected spaces in your home.
For people with COPD and other respiratory diseases, spring cleaning is an important opportunity to take care of lung irritants and hazards in the home. With spring allergens swelling and summer on the way, it's the perfect time to clear out clutter and make your home the cleanest, healthiest space it can be.
In this post, we're going to help you make the most out of spring cleaning by focusing on tasks that can help your COPD. We'll show you how to get rid of dust, mold, allergens, and how to improve your indoor air quality and ensure it continues to stay clean.
We'll give you tips for organizing your home to keep respiratory irritants at bay and ensuring outdoor allergens and pollutants don't build up in your home. We'll also show you how to protect your lungs from fumes, dust, and other particles while you clean, and how to make difficult cleaning projects easier to manage.
Keeping your home clean is not only good for a sound mind, but for healthy lungs as well. With the tips in this article, you can make sure you do spring cleaning right this year so you can enjoy the benefits of a healthy home the whole year round.
The Basics of Spring Cleaning
Regular cleaning year-round is important, but it's good idea to pause and pay attention to the details every so often. Even if you keep up with the necessities throughout the year, your house will inevitably collect hidden corners of dust and clutter and accumulate little maintenance and deep cleaning tasks that need attention.
If you let these things go for too long, they can become respiratory hazards and make your COPD symptoms worse. Dust, allergens, and toxic particles can sneakily build up in all sorts of places in your house, and spring cleaning is the perfect time to find and eradicate them all.

But before you get started, you should take some time to learn how to protect your lungs and go easy on your body while you clean. In the next sections, we'll discuss what kinds of supplies you'll need, what kinds of chemicals you should use, and how to protect your lungs from dust and fumes.
We'll also give you some general tips for cleaning as efficiently and effectively as possible, so you don't waste time and energy during your spring clean. COPD can make household tasks difficult, but planning ahead and learning new techniques can make cleaning easier and less tiring.
Protect Your Lungs When You Clean
The first thing you should consider is how you are going to protect your lungs from irritating particles and chemical fumes while you clean. After all, cleaning tends to kick up all sorts of respiratory irritants that can irritate your lungs and airways.
When you have COPD, cleaning without taking care to protect your lungs can do more harm than good, causing further lung damage and making your symptoms flare up. To clean safely, you need a two-pronged approach: using safe cleaning products and protecting your mouth and nose while you clean.
Avoiding Chemical Fumes

In general, you should avoid using commercial cleaning products, which are often made with harsh chemicals that can irritate your lungs airways. Instead, look for natural products made with mild ingredients or simply mix your own cleaning solutions at home.
Here are some chemicals that you should look out for and avoid using when you clean:
- Chlorine bleach
- Ammonia
- Detergents
- Aerosol sprays and fresheners
- Pesticides and fungicides
- Varnishes
- Floor wax and polish
- Oven cleaners
- Carpet cleaners
Commercial cleaning products aren't actually necessary for most cleaning tasks, and all you need is a few basic ingredients to make DIY cleaners for your home. Soap, vinegar, and baking soda are surprisingly effective for cleaning, and, when used in moderation, are much gentler on your lungs.
You should also stock some bleach and ammonia for more serious sanitizing, but be careful to never mix bleach and ammonia together. Be very careful to always examine the labels of any chemicals or cleaning products you have and only use them as directed.
Visit our previous post here for some recipes you can use to make your own safe cleaning solutions at home. You can also visit the EPA's website for “Safer Choice” products, which are specially labeled to indicate that they are safer for the environment and your health.
One of the most important things to remember is to never use chemicals in an enclosed space. At the very least, the fumes could irritate your eyes and airways, and at worst, they could even be deadly.
Any time you use a cleaning solution, think first about the space you will use them in and whether or not it needs extra ventilation to be safe. You may need to open some windows, turn on your bathroom vent, or set up a fan to increase air circulation in the room.
Particle Safety
Whenever you dust or do deep cleaning, you are likely to kick up all sorts of particles that have accumulated and laid dormant in dark corners. All of these particles, including dust, mold spores, pet dander, pollen, and smog and smoke particles, can inflame your lungs and cause your COPD symptoms to flare up if you're not careful.
That's why you need extra equipment to protect your mouth and nose from any particles or fumes you encounter when you clean. Even something as simple as covering your face with a scarf can keep you from breathing in large bits of dust, but you may need a special mask to protect your lungs from the smaller particles.

Particle respirators are much more effective than a basic surgical mask or face covering, and can screen out 95 percent of particles as tiny as 0.3 microns in width. This is the best choice if you suffer from allergies or are very sensitive to airborne particles.
To get a proper particle mask, look for an N95 respirator that is certified by the Food and Drug Administration (FDA) or the National Institute of Occupational Health and Safety (NIOSH). You can also see a list of official N95 mask manufacturers at the CDC's website here.
Some people have trouble breathing when using a respirator because of the resistance that the mask creates when you breathe. To reduce this resistance, look for an N95 respirator with an exhalation valve on the front of the mask.
If you have very severe COPD, even a little bit of dust or mold could cause your symptoms to flare up. In this case, you should talk to your doctor about what kinds of cleaning you can manage and enlist someone else to do the hazardous tasks.
Certain chemicals, like bleach, pinesol, and ammonia, can also cause inflammation and COPD flare-ups if you're not careful. Unfortunately, a particle mask alone is not enough to filter these fumes out of the air.
If you have to work with harsh chemicals, you can reduce the chance of exposing yourself to irritating fumes by being extra careful to ventilate the rooms you work in. If they still irritate your airways or you have to clean a more enclosed space, you will need to get a special gas mask or ask someone else to do the work for you.
General Cleaning Safety
Along with protecting your lungs, you should also take care to protect your hands, skin, and eyes from harsh chemicals when you clean. That's why you should always have some gloves and goggles on hand for particularly messy tasks or when you use any hazardous chemicals.

You should also pay special attention to any chemicals you use when you clean, reading the labels and making sure to dilute any concentrated chemicals appropriately. Never use any chemical for an unapproved purpose or mix chemicals together for any reason.
Make sure you wash any sponges or rags you use to clean so they don't accumulate bacteria or mold. Switch to fresh rags often to avoid spreading around bacteria or mold, especially after cleaning very dirty surfaces like toilets and sinks.
Enlist Help When Needed
If you are very sensitive to airborne irritants or have very severe COPD, then you don't want to take any chances when you clean. In some cases, this may mean hiring a cleaning professional or asking friends or family to help you clean your home.
For example, you should ask others to help with any tasks that cause your symptoms to flare up or require you to use toxic chemicals. That includes any cleaning projects that kick up a heavy amount of dust or mold, especially if you don't have adequate facial protection.

Make sure you take the time to inform any helpers or professional cleaners about your disease and your sensitivity to chemical fumes and fragrances. Tell them what kinds of products are okay to use and what chemicals are off-limits for your home.
If the work will stir up a lot of dust or requires harsh chemicals, you should be careful to stay out of the way so your lungs don't get inflamed. You might be able to simply go to a different room, or you may need to leave the house entirely until the task is done and your home has a chance to air out.
As your COPD progresses, you may find it too tiring to do major cleaning tasks or find that your lungs are just too sensitive to handle certain things. When this happens, there is no shame in asking for help and letting others take care of the work.
Chemicals and Equipment You Will Need

You don't want to begin your spring cleaning project only to find that you don't have the supplies you need. Before you get started, make sure you have all the basic supplies and cleaning solutions you will have to use.
Not only will this save you time as you clean, but it gives you a chance to replace all of your hazardous commercial cleaning products. Throw out any harsh or scented products and buy the ingredients you need to make your own, lung-healthy cleaning solutions instead.
Here is a general list of cleaning products and appliances you should have for your spring clean:
- Vacuum
- Broom
- Mop
- Sponges
- Dusting tool
- Cleaning rags and towels
- General purpose cleaning solution
- General purpose sanitizing solution
- Gloves
- Goggles
- Particle mask or respirator
- Soap
- Vinegar
- Ammonia
- Baking soda
Work from Top to Bottom

A good general rule of cleaning is to start at the top and work your way down. That way, you can knock dust and other particles down from high places without dirtying something below it that's already clean.
It's important to dust and wipe down all the surfaces in your home before starting on the floors. If you follow the guidelines and steps in this article, you should be able to tackle all the dust and grime in the right order.
Make Cleaning Tasks Easier
If you get breathless easily or have limited mobility, it can make major cleaning tasks difficult. That's why you need to have the right tools and techniques to reduce the strain.
Good Posture

Bending, stooping, and poor posture are all enemies of easy breathing. To reduce the pressure on your lungs and make it easier to catch your breath, make sure you practice proper posture when you clean.
As much as possible, try to keep your back straight, you shoulders back, and your chin parallel to the ground. This will keep your chest open to allow better breathing and prevent your muscles from getting sore.
Take Breaks
It may be unrealistic to try to do a thorough spring cleaning in a single afternoon or weekend. Instead, spread out your tasks over several days so you don't wear yourself out too much at once.
You should also take frequent breaks as you clean, especially when you start to feel tired or short of breath. If you break up tasks up into shorter, manageable chunks, you'll have plenty of time to rest in-between.

Pacing is also important, because trying to do too much at once can deplete all your energy very fast. If you take it slow and spread the work out, you'll be able to do more without feeling fatigued.
Use Proper Cleaning Tools and Aids

As you go about your house and clean, look for ways that you can decrease the amount of strain and energy you have to use. After all, you don't want to waste all your energy on house chores when there are so many other activities in life to enjoy.
For example, you could get a cleaning apron to wear around your waist that has slots for basic supplies like cleaning solutions and rags. Having an apron to store things in not only frees up your hands, but reduces the amount of times you have to walk back and forth across the room to get supplies.

Also, having a tall stool to perch on instead of standing can help you conserve energy and improve your balance. For example, you might pull up a stool to sit on as you wipe down your counters, unload the dishes, or sort and fold laundry.
Short stools are useful to use when you need to clean spaces that are low to the ground. You can use them to make tasks like spot cleaning floors or dusting low shelves much easier to do.
Whenever possible, you should also elect to buy long-handled cleaning tools like dusters, brooms, and mops. That way, you don't have to stoop or strain yourself as often while you clean.
Also take care when storing your cleaning products to ensure that they are within easy reach for next time. Items stored below shoulder height but above knee height are usually the easiest to reach.
Use Breathing Techniques

When you're doing chores around the home and start to feel breathless, pursed-lips breathing is one of your best resources. By helping you pace and control your breaths, pursed lips breathing can help you do more activities for longer without losing your breath.
It also helps to sync your breaths with your actions, timing them together to help you stay in control. To learn more about pursed-lips breathing, see our


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!















