.png)
If you have COPD or any respiratory or circulatory disease that inhibits your lungs or heart from producing enough oxygen for your body you have probably been prescribed supplemental medical oxygen. Oxygen treatment increases the amount of oxygen that flows into your lungs and bloodstream. If your COPD is severe, and your blood oxygen levels are low, getting more oxygen can help you breathe better and live longer.
You have a lot of options when it comes to choosing a method for oxygen treatment, and ultimately your decision should be made adhering to your doctor's prescription recommendations and then addressing your personal goals and financial responsibilities. This article will help you in determining how to weigh your options.
Your doctor may prescribe a range of oxygen flow rates for a range of different conditions, such as:
- COPD
- Pulmonary fibrosis
- Severe asthma attack
- Pneumonia
- Pneumothorax (collapsed lung)
- Sleep apnea
Flow rates are based on your personal diagnosis and how low your blood oxygen levels are for different activities, such as during rest, sleep, or exercise.

It is very important that you follow you doctor's instruction exactly how they are prescribed, because using too much or too little oxygen can have consequences.
There are a few different delivery methods involved when it comes to taking supplemental oxygen therapy.
Delivery methods include:
- Oxygen concentrators:
- Oxygen-gas cylinders
- Liquid-oxygen devices
So what are the benefits and proof that treating COPD and other diseases using supplemental oxygen improves your quality of life?
Benefits of treating COPD with supplemental oxygen
Supplemental oxygen therapy has been proven to give you more energy, and reduce the risks of heart failure and lung disease. You can also take extra oxygen while you exercise to perform better and have less shortness of breath. Supplemental oxygen has also been proven to enhance your mental awareness and overall mood.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
After you get used to living with supplemental oxygen, the long-term treatment may improve your quality of life.
The two most popular supplemental oxygen treatment methods are oxygen tanks and portable oxygen concentrators (POC) and while both methods can deliver oxygen to your body, a POC is much more convenient and offers you more freedom and independence.

How oxygen concentrators work:
As mentioned above, oxygen tanks require constant refilling, and those costs will add up. Oxygen concentrators take air from the surrounding area and turn it into concentrated oxygen, this will never need to be refilled, instead it runs off battery power, so it's always prudent to have a spare battery as well as an AC/DC adapter.
Comparing oxygen tanks to oxygen concentrators


The most obvious reason as to why you would choose a POC over an oxygen tank is because you do not need to get it refilled. Refilling your oxygen tank is very time consuming and not to mention very expensive, especially in the long-run.
Everyone’s first hesitation of buying an oxygen concentrator is the up-front cost, however if you compare the amount you spend on refills every year with an oxygen tank, the amount of money and time you save purchasing an oxygen concentrator in the long run will outweigh the costs associated with an oxygen tank.
The other aspect to be weary of when comparing oxygen concentrators to oxygen tanks, is understanding what your oxygen needs are.
Ask yourself these questions after consulting with your doctor:
- What type of flow: Pulse flow or continuous flow, is right for your body?
- What are all of your expenses associated with an oxygen tank per year?
- How much independence are you searching for?
- Are you interested in increasing your physical activity?
- Do you want to travel soon?
What type of flow: Pulse flow or continuous flow, is right for you?
If you answered pulse flow, a POC might be the best choice for you because pulse flow units don’t need to put out as much oxygen, and so these units tend to be much much smaller and lighter and they also have longer battery life so you are able to be mobile longer.
An average pulse flow portable oxygen concentrator will weigh around 5 to 6 pounds whereas the average continuous flow portable oxygen concentrator will weigh 10 pounds or more.
If you need continuous flow oxygen therapy you have the option to stick with an oxygen tank, because they will always offer a continuous flow of oxygen. But you could also decide on a continuous flow oxygen concentrator, like the DeVilbiss 5 Liter Home Oxygen Concentrator depending on what your priorities are. The next few questions will help you determine these.
You should know that many continuous flow POCs like the Oxlife Independence and the Respironics SimplyGo allow you to switch between continuous flow and pulse flow.

What are all of your expenses associated with an oxygen tank per year?
If you find that you are spending more on refilling your oxygen tank than it would cost to pay off a POC or home oxygen contractor, it may be time to switch to a more affordable option. A wise financial investment will provide you with long-term benefits to your health and peace of mind, and in this case, provides you with financial benefits as well.
Some people are satisfied with the refill process of their oxygen tank, and are not interested in managing the battery life of a concentrator, if this is the case for you, an oxygen tank still might be the best option and change may cause more confusion than necessary.
How much independence are you searching for?
If you are an independent person, an oxygen tank may be restricting you from doing everyday chores on your own either because the tank is too heavy or the cart doesn’t allow you to move around freely to do yard work, go grocery shopping, etc.
If you are eager to gain independence, the Caire FreeStyle Comfort is one of the most efficient portable oxygen concentrators currently on the market. The main selling point for this portable oxygen concentrator is its battery life and subsequently more freedom for you.
On a setting of 1, the FreeStyle Comfort can run up to 16 hours on one charge, which is currently the longest battery life offered by any portable oxygen concentrator.
Additionally, the FreeStyle Comfort goes up to a flow setting of 5, weighs in at only 5 pounds, so while you are carrying your oxygen unit you would be able to do your own daily tasks with no shortness of breath, and you would not feel fatigued from carrying it.
If you are looking to move around and do more things for yourself, a POC is a great option over an oxygen tank.
.jpg)
Are you interested in increasing your physical activity?
Physical activity has many benefits for lung capacity and is a common COPD treatment. If you're interested in becoming more physically active, switching from an oxygen tank to a POC may be the right choice for you.
Oxygen tanks are cumbersome and hard to maneuver, making any physical activity seem even more challenging that it already is for many people with COPD. Out of all of the pulse flow portable oxygen concentrators on the market, the Inogen One G5 is one of the lightest, smallest, and easiest to carry.

The G5 weighs about 4.7 pounds with the single-cell battery, the G5 is no heavier than a handbag or purse with a couple of your personal belongings in it. Also, unlike oxygen tanks, the Inogen G5 has a very natural box-like shape that won’t get in your way as you walk and go about your day. You’ll be able to carry it on your back, at your side, or even simply carry it in your hands.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
You would be able to take the G5 breathing device hiking, biking, and to pulmonary rehabilitation classes with ease and not have to worry about the added weight when exercising.
When it comes to exercise with the G5 you will not have to worry about your oxygen demands not being satisfied because the Inogen One G5 portable oxygen concentrator offers pulse flow settings of 1-6. So as your breathing rate and requirements change depending on if you are laying in bed or exercising, the Inogen One G5 has the ability to adjust to your oxygen intake needs.

Do you want to travel soon?
One of the most important aspects of a POC is that they can travel freely on most major airlines as instructed by the Federal Aviation Administration (FAA). POCs are safe on airplanes because they do not contain pressurized oxygen like oxygen tanks do.
They simply take ambient air, remove nitrogen, argon, and other impurities, then put out medical-grade oxygen via the nasal cannula. POCs will not create an oxygen-rich environment, because it will only work when it detects your breath, so if you happen to drop the cannula, it won’t continue to put out oxygen.
With a POC you are also able to take a cruise or take a long road trip. Taking a cruise is one of the best ways to explore an area of the world that you’ve never been to before and it’s also a great way to catch up with friends and family while not exerting too much energy. While oxygen tanks are often permitted on cruise ships, this doesn’t necessarily mean you’ll have a way to refill it.
If you want to take a long road trip, your POC will easily fit into the car and the space in front of your knees. Not to mention, you will also have access to a power source because the AC/DC charger has an adapter to fit into your car’s power source, so there is no stressing about recharging the battery or bringing along a few extra batteries for an emergency.
Your options explained
So far we have explained the benefits of treating COPD with supplemental oxygen therapy, and went over some questions you should consider asking yourself before switching from an oxygen tank to an oxygen concentrator.
Just to review, portable oxygen concentrators offer four other major benefits over traditional tanks:
- They do not need to be refilled instead they just need to be recharged or have an extra battery on deck.
- They’re lighter and easier to carry. Oxygen tanks can be big and heavy, but POCs are meant to be portable and only weigh a few pounds.
- They’re safer. Oxygen tanks can leak oxygen and create an oxygen-rich environment, which is a fire hazard, and will not allow you to travel by plane.
-
They’re ultimately cheaper. An oxygen concentrator may cost more upfront, you will not constantly have to pay for oxygen refills, saving time and money in the long run.
Now, some of the benefits listed above may not apply to you because you may need a continuous flow of oxygen, in which case, oxygen tanks will deliver you oxygen on a continuous flow basis. This is necessary for individuals with very low levels of oxygen capacity in their lungs and severe COPD.
However, a tank is still not your only option.
Continuous flow portable oxygen concentrator: Respironics SimplyGo
The best option you have for a continuous flow oxygen concentrator is a Respironics SimplyGo Portable Oxygen Concentrator. The Respironics SimplyGo has been one of the top continuous flow portable oxygen concentrators on the market. It is small, weighing 10 pounds, but is also backed by one of the biggest names in the respiratory field, SimplyGo is as reliable as they come.
There are other very reliable home oxygen concentrators available as well. So you just have to determine whether a concentrator or oxygen tank is the right choice for you.
Oxygen tanks provide continuous flow oxygen, which means that if it is turned on, oxygen is flowing constantly, even while you are not inhaling or when you remove your nasal cannula or mask. An oxygen tank holds a limited amount of compressed or liquid oxygen, you can use this until it runs out, so you must get the tank refilled, or replace it.
An oxygen concentrator, compresses and purifies your surrounding air to provide an unlimited amount of medical-grade oxygen, as long as the oxygen concentrator has battery power.
Depending on the model, an oxygen concentrator can provide either continuous flow oxygen or pulse dose oxygen. A Respironics SimplyGo POC offers both settings. If you are using this concentrator in a pulse flow setting, you will have up to 6 hours of battery life and up to 1.8 hours of battery life on a continuous flow setting. Its compressor is rated to last 20,000 hours.

That being said, this portable oxygen concentrator is designed to run 24/7 365 and is warranted for up to 3 years, which offers you major advantages over an oxygen tank.
The SimplyGo will easily fit underneath the seat in front of you on the airplane, you can store it on the floor of your car or in the passenger seat as you drive, and when you don’t need to use it you will be able to put it in your closet without having to clear space for it.
One additional feature the SimplyGo has to offer is its sleep mode technology. Whether you’re on the airplane or relaxing in your chair at home, and you feel yourself dozing off, you can turn sleep mode technology on to ensure your oxygen gets delivered while you are sleeping.
When you turn sleep mode technology on your SimplyGo increases its sensitivity to detect your breath and it softens the pulse flow delivery so it doesn’t wake you up.If your SimplyGo doesn’t detect a breath or if you breathe through your mouth it will automatically switch back over to continuous flow to ensure you get your required oxygen.

An oxygen tank and continuous flow concentrator can be used in the same way—to provide supplemental oxygen to someone in need of continuous flow oxygen therapy— but the biggest difference between a continuous flow concentrator and an oxygen tank depends on what you prefer to be reliant on.
You can either rely on charging your concentrator’s batteries and being aware of nearby power source to plug in your machine to charge. Or you can consistently rely on refilling your oxygen tank with medical-grade oxygen and replacing your tanks with new oxygen when you run out.
With a continuous oxygen concentrator you are significantly lowering the risk of creating an oxygen-rich environment, which is a safety concern with many oxygen tanks.
It all come down to your needs and preferences

The first step in choosing your best supplemental oxygen therapy options is to discuss with you doctor what your flow rates needs are. Remember your flow rates may vary through the day and night and this should be taken into account as well.
Then, you will to financially address your investments, would you prefer paying the costs up front, or accumulating costs over a long period of time. Then do the math a determine which option is cheaper in the long-run.
While addressing you financials, you need to take into consideration all of your personal goals and address what option is better for maintaining your livelihood. Do you want to exercise more? are you interested in traveling?
We will be here when you are ready to discuss your options with a professional.
If you thought this article was helpful, please leave a comment and share with others so they may find their own insights into such a large decision.
"Is being barrel chested bad?" — In the later stages of COPD, some people with the disease begin to notice a barrel-shaped chest that, understandably, leads to concern. Although this is not always a serious issue, it can be a sign of emphysema, a type of COPD.
While having a barrel chest alone isn't dangerous for your health, a barrel chest can be a sign of another serious problem. If you have COPD or know someone who does, then you should know what barrel chest is and how to recognize it.
In this post, we're going to tell you all about barrel chest, what causes it, and what it means for people with COPD.
What is Barrel Chest?
The main characteristic of a barrel chest is an especially wide, rounded chest cavity. For some people, a barrel chest is part of their natural body shape, while others develop a barrel chest over time as a result of an underlying medical condition.
Disease-related barrel chest usually develops as a result of strain, pressure, or damage to the rib cage that causes it to expand. This can be caused by underlying problems with the lungs, joints, or skeletal structure supporting the rib cage.
Barrel Chest Caused by COPD

Emphysema, a type of COPD, is one of the most common causes of barrel chest. This happens because enlarged lungs and chronic airway obstruction caused by COPD makes it difficult to push all the air out of the lungs when you exhale.
Usually your rib cage is very flexible so that it can expand when you inhale and contract when you exhale. When you have emphysema, however, some air stays trapped in your lungs even after you exhale, which exerts pressure on your rib cage as it tries to contract.
This is known as lung hyperinflation, and it prevents your rib cage from contracting all the way back down after you exhale. Instead, the rib cage is forced to stay open in a slightly expanded state. This results in the barrel-chested appearance and is usually associated with the later stages of COPD.
The trapped air that causes barrel chest can make it difficult to inhale, as stale, trapped air is already present in the lungs. This makes it more difficult to breathe and makes other COPD symptoms, like coughing and wheezing, even worse.
Trapped air can also cause changes to the shape of the diaphragm, causing it to become weaker and making belly breathing (diaphragmatic breathing) more difficult. As a result, many COPD patients rely heavily on their chest muscles, instead of their diaphragm, to breathe. This can cause problems like chest tightness and pain, and wear out the muscles you use to breathe more quickly, making COPD symptoms even worse.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Barrel Chest Caused by Severe Asthma

Severe asthma can cause a barrel chest in a similar way to COPD. However, unlike COPD-related barrel chest, which generally doesn't develop until late adulthood, asthma-related barrel chest can appear in childhood.
This is because asthma can make it difficult to exhale fully and push all the air out of your lungs. This causes air to get trapped in the lungs just as it does in patients with emphysema, preventing the rib cage from contracting and causing a barrel-chested appearance.
Barrel Chest Caused by Arthritis

Arthritis is a disease that affects the joints, and it causes barrel chest in a different way than COPD or asthma. It wears down the joints in the rib cage that anchor your rib bones to your spine, making the rib cage less flexible.
Because of this, the rib cage can no longer expand and contract as easily as it is supposed to. Over time, this stiffness can prevent the rib cage from contracting altogether, forcing it to stay stuck in the expanded position. This causes the chest to have a wider, barrel shape.
Barrel Chest Caused by Calcium Deficiency
If you don't get enough calcium and vitamin D in your diet, it impairs your body's ability to repair and strengthen your bones. In severe cases of calcium deficiency, known as osteoporosis, the bones become so weak and brittle that minor bumps and falls can cause them to bruise and break.
Calcium deficiency affects the bones in your rib cage as well, causing them to become weak and misshapen. Over time, this can deform your rib cage and breast bone, changing the outward appearance and leading to a barrel-shaped chest.
Barrel Chest Caused by Genetics and Environment

As we mentioned above, sometimes barrel chest isn't caused by any disease or medical condition, but is just a natural physique. Some people, men especially, are simply born with the genetics and physical characteristics that lead to a barrel chest.
A barrel-shaped chest physique is also common in certain populations of people that live at high altitudes, including native peoples in the Andes Mountains and the Himalayas. Researchers suspect that the barrel-shaped rib cage could be an adaptation to cope with the thinner air at high elevations.
Bodybuilders also can develop a barrel-shaped chest by bulking up the muscles in their chest. While this can sometimes look similar to a barrel-shaped chest caused by other medical conditions, it is not a medical concern.

For people who develop a barrel chest due to genetics or exercise, having a barrel chest doesn't require any treatment and is nothing to be concerned about. There are also some very rare genetic disorders that cause some babies to have a barrel chest from birth, as a result of a congenital abnormality in their skeletal structure.
Multiple Causes
Sometimes there is more than one cause behind COPD-related barrel chest. For example, severe asthma is a common risk factor for COPD, and patients who have both may have a greater risk of developing barrel chest as a result of both conditions combined.
COPD patients are also particularly prone to arthritis, which can contribute to a barrel chest in addition to lung problems caused by COPD. It is particularly important for COPD patients to get adequate calcium and vitamin D in their diets to prevent bone density loss and osteoporosis.
How to Treat Barrel Chest Caused by COPD
There is no treatment for barrel chest specifically, because on its own having a barrel chest is not bad for your health. What really matters is the underlying cause, and any treatment for barrel chest will focus on treating the underlying medical conditions that caused it.
In the case of emphysema, a barrel chest is a strong sign that your lungs are trapping a lot of air. The most effective treatment, then, is to treat the underlying COPD symptoms, especially trapped air in the lungs.
Follow your COPD Treatment Plan
Every part of a COPD treatment plan is designed to keep the lungs and the body as strong and efficient as possible. If you follow your treatment plan carefully, including eating a healthy diet and exercising, you can improve your COPD symptoms and prevent other symptoms like barrel chest.
However, there are specific breathing exercises for emphysema that can be very effective at helping you push all of the air out of your lungs when you exhale. These breathing exercises combined with other COPD treatments can reduce your risk of barrel chest and may even prevent a barrel chest from getting worse.
Practice Breathing Exercises

Pursed-lips breathing is an exercise that is very effective at helping patients with COPD control their breathing during exercise and any kind of physical activity. It can effectively ward off breathlessness and even prevent air from staying trapped in your lungs.
The purpose of pursed-lips breathing is to force air out through a small opening in your lips. This creates pressure in your lungs and airways when you exhale, which helps push any trapped air out of your lungs.
Most medical professionals recommend that people with COPD practice pursed-lips breathing every day and use it as often as possible, especially whenever they experience breathlessness or other respiratory symptoms. Pursed-lips breathing might also be able to prevent or delay the onset of emphysema-related barrel chest.
Here is how you practice pursed-lips breathing:
- First, find a comfortable place to sit or lie down and relax the muscles in your chest, shoulders, and neck.
- Inhale, breathing in for about two seconds.
- Next, purse your lips as if you were about to whistle or blow out a candle.
- Then, exhale through pursed lips for about four seconds (twice as long as your inhale).
- Repeat
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Get Plenty of Calcium and Vitamin D

People with COPD often have difficulty getting adequate amounts of nutrients, and especially calcium and vitamin D, from their diets. This is partially because of COPD symptoms that make it difficult to eat and prepare healthy meals, and partially because many patients have increased calorie requirements because of the strain the disease puts on their lungs.
Therefore, eating plenty of foods rich in calcium and vitamin D is a vital part of any COPD-friendly diet. Calcium is necessary for healthy bones and preventing arthritis, while vitamin D is necessary for your body to be able to absorb and process the calcium you eat.
By ensuring that your bones have plenty of nutrients to stay strong, you can prevent osteoporosis and osteoporosis-related barrel chest. That's why it's important to follow your COPD treatment plan and the dietary guidelines provided by your doctor.
Here are foods you can eat to increase the amount of calcium in your diet:
- Milk and dairy products
- Soy beans and tofu
- Green, leafy vegetables (e.g. cabbage, broccoli, and okra)
- Nuts
- Calcium-fortified products like breads and cereals
Here are some foods you can eat to increase the amount of Vitamin D in your diet:
- Fatty fish (e.g. salmon, tuna, and trout)
- Fortified milk and orange juices
- Egg yolks
- Cod liver oil
- Vitamin D supplements
- Spend more time in outside; about ten minutes in the sun allows your body to absorb a significant amount of vitamin D through your skin

Conclusion
Whether or not your have COPD, it's important to be able to recognize what a barrel-shaped chest is and what it could mean. While having a barrel chest is not necessarily a health concern in itself, anyone who notices a barrel chest that develops over time should get evaluated by a doctor for potential underlying causes.
Even COPD patients who develop a barrel chest should get evaluated by their doctor. It could be a warning sign that your COPD is getting worse and your treatment plan needs to be adjusted.
Even if emphysema is the primary cause of barrel chest, other medical conditions, like osteoporosis, could also be contributing to the change in the rib cage's shape. That's why it's important not to ignore a barrel chest if you develop one, even if you think that it is most likely related to your COPD.
Now that you have a better understanding of what a barrel-shaped chest is and the medical conditions that cause it, you will be better able to recognize it in yourself and others and be better able to tell when it should be taken seriously. If you or someone you know has COPD, watching out for a barrel chest can help you better manage and monitor the disease.
In this fast-paced, busy world that we live in, it can be difficult to find the time or the means to practice mindfulness. From going to work to cooking dinner, dealing with family matters, and spending time with friends, we often don’t take the time to decompress and ensure that our thoughts and feelings are in line with what we’re trying to accomplish.
What’s more, if you have a chronic illness like COPD, the problem of having an overburdened mind is often compounded by physical symptoms like breathlessness, chest pain, and fatigue. Many COPD patients describe feeling “claustrophobic” or “confined” within their own body, leaving them little recourse but to focus on the negatives of their disease rather than the positives.
Ultimately, this mindset is not sustainable, so you’ll need to find some way to set your mind at ease. For many people, meditation is the best way to do this. Meditation is the use of various different techniques designed to train your mind to focus on a particular activity or thought. What results is that you’ll have more control over your mindset pertaining to your disease and its progression.
In this post, we’ll discuss a variety of different types of meditation and we’ll give you some tips for implementing them into your life as a COPD patient. If you’re looking for further reading, check out our post about 6 Effective Breathing Techniques and Exercises for COPD and Techniques for Coping with COPD and Anxiety.
What is Meditation?
Many people live their whole lives without trying or even considering the use of meditation. It’s often written off as a religious or spiritual practice that’s not useful for most people. And while this is partially true — meditation is used in many religious traditions such as Buddhism — it’s actually more commonly used in a non-religious context.
According to Positive Psychology, meditation is a practice that’s been around for thousands of years, but it was first depicted by wall art paintings in India around 5000 to 3500 BCE. Meditation moved to the west as early as the 1700s, but it wasn’t until the 1900s that it began to be separated from its religious roots.

Today, the beneficial effects of meditation are well-studied and well-documented. The practice has been examined extensively by prestigious institutions and has yielded mostly positive results, especially when it comes to treating depression and anxiety. What’s more, other studies have shown a positive correlation between meditation and easing the pain caused by a chronic illness such as COPD.
How Does Meditation Affect the Brain?
In this day and age, we have an incredible amount of technology that can be used to examine what goes on in the brain. Technology such as polysomnography has enabled researchers to study what goes on in the brain during sleep and has made it easier for doctors to diagnose conditions like obstructive sleep apnea (OSA) and insomnia.
Similar technology has been used to study the brain during physical activity and even meditation. Magnetic resonance imaging (MRI) is one such device that’s used to produce pictures of the anatomy and the physiological processes of the body. It allows researchers to precisely monitor changes in brain wave activity during different activities.
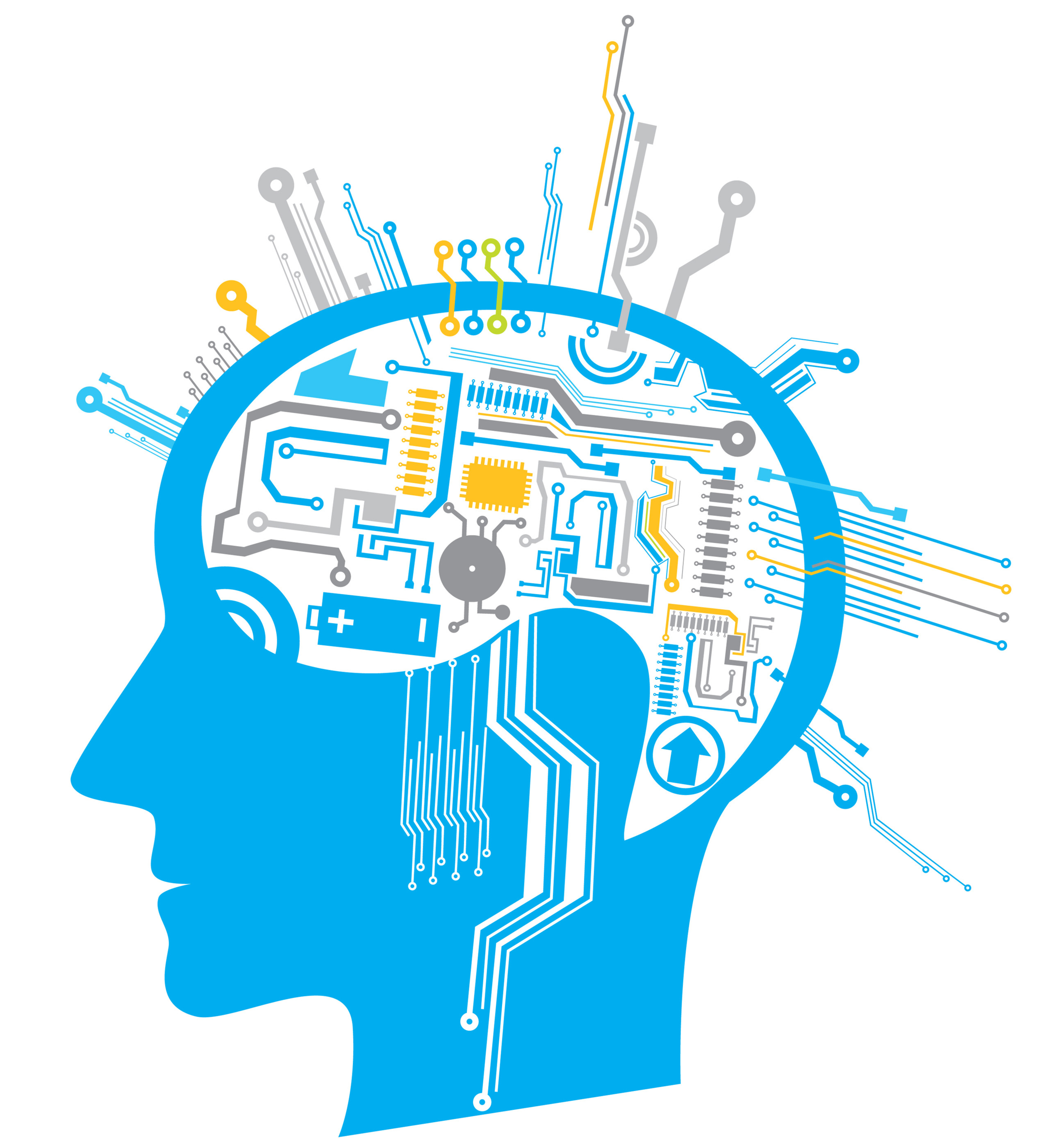
Brain waves are the electrical impulses which oscillate at different frequencies and at different wavelengths. Brain waves are altered depending on the state of consciousness that we’re currently experiencing. For example, if someone is wide awake, they will have different brain wave activity than someone who is in light sleep or deep sleep.
Researchers have found that people who are anxious or tense they often have more high-frequency beta waves present. This includes people with mental disabilities such as ADD, ADHD, or learning disabilities, but it can also include people with chronic conditions like COPD who might experience a higher degree of anxiety than the general public.

In many cases, trying to force these feelings out can exacerbate them, leading to a negative feedback loop. However, if you learn to influence brain waves through meditation and neurofeedback training, you can reduce feelings of anxiety. As we come to better understand brain waves and how to influence them, we will likely see more doctors prescribing it as an alternative to anxiety medication which always has some negative side-effects.
Can Meditation Alter the Course of COPD?
Now that you know meditation can be used to treat anxiety and depression caused by COPD, you’re likely wondering whether meditation can help alter the long-term prognosis of your disease. In other words, are there any physical manifestations of the benefits that we see from people who meditate regularly?
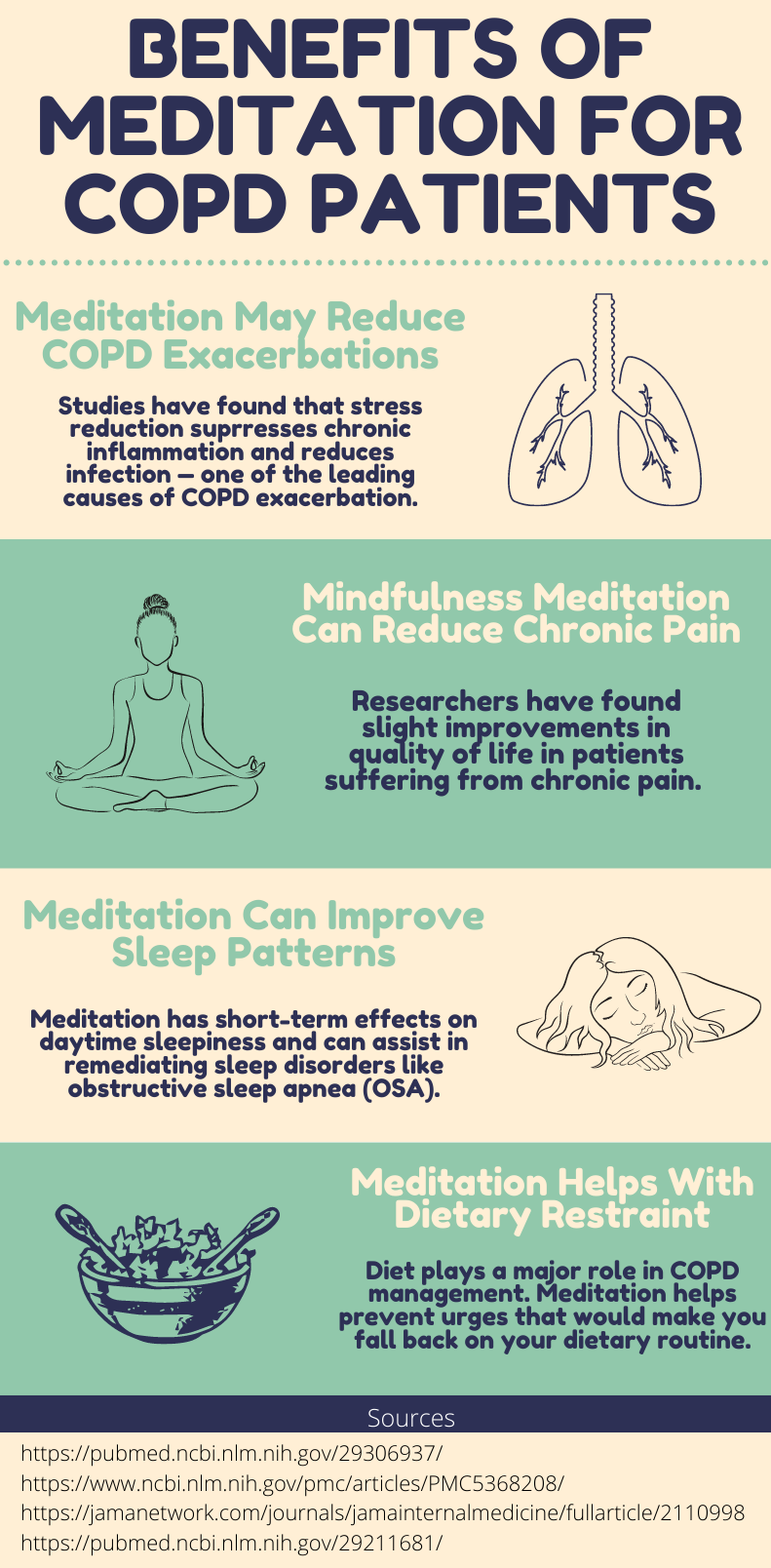
Unfortunately, it’s a little more complicated than a simple “yes” or “no” answer. Generally, meditation is accepted as an effective method for treating not only comorbid anxiety from COPD but physical respiratory symptoms as well. This study found that after 12 weeks of yoga training, many COPD patients saw improved lung function, inflammation, and quality of life.
.jpg)
Other studies, however, have cast more doubt on the effectiveness of meditation for COPD patients. This study found that meditation presenting emotionally-triggering skills such as mindful awareness to emotions or dyspnea can actually contribute to anxiety. However, both of these studies were limited by a small sample size.
Possibly one of the most popular forms of meditation for COPD patients is something called “movement meditation.” This practice focuses on being mindful of your body’s movements rather than focusing on the goal of the movement. According to a study found in COPD News Today, COPD patients practicing Tai Chi (a type of movement meditation) five hours per week saw more benefits after 12 weeks than those practicing standard pulmonary rehabilitation.

While there is limited evidence suggesting that meditation directly improves outcomes for COPD patients, there are plenty of ways that it improves outcomes indirectly. Anxiety is a well-known contributor to the frequency and severity of COPD exacerbations and anxiety can cause sleep disruptions which can lead to fatigue and other factors that make COPD more difficult to cope with. Therefore, treating anxiety with meditation has undeniable benefits when it comes to COPD outcomes.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What Types of Meditation Are There?
Focused Meditation
Focused meditation is a practice where you concentrate intently on one object, sound, tactile sensation, smell, or taste. This is often used as a sort of stepping stone to classical meditation which requires you to block all thoughts.
.jpg)
Focused meditation is a great place to start because it doesn’t require you to have an instructor and it’s very accessible for most people. By having a focal point of thought, you’ll be able to more easily control your internal dialog and catch yourself whenever your mind starts drifting. Another great thing about focused mediation is that you can start with shorter sessions. Just five minutes a day of focused meditation will get you started on the right foot.
Movement Meditation
Like the name suggests, movement meditation is a type of meditation you do while you’re physically moving. It’s the perfect exercise for anyone who wants to experience a greater connection between their mind and body, as well as people who have difficulty concentration their thoughts while they are sitting still.

Movement meditation is one of the most popular types of meditation for people with COPD and other respiratory conditions because it helps them eliminate anxiety while mastering their breathing and motor functions. Movement meditation is also a great exercise to complement pulmonary rehabilitation routines because it can build endurance and muscle.
Tai Chi is one of the most practiced forms of movement meditation in the world and it’s especially popular among older adults and seniors who suffer from chronic illness. It originated in ancient China where it was originally intended as a form of fighting. However, over time, Tai Chi was adopted and developed by many different cultures, making it what it is today.
We’ve already written in great detail about Tai Chi and its many benefits for COPD patients, however, we’ll summarize it here for your convenience. Essentially, Tai Chi is a form of low-impact exercise that combines a variety of different poses with fluid and controlled movements. In other words, you won’t be moving your legs and arms around erratically without purpose; you’ll instead be focusing on making every movement meaningful.

Creating this mind-body connection is very important for people with COPD because as your disease progresses, it becomes increasingly difficult to control things like your breathing which are unconscious motor movements in people with healthy lungs. As such, it’s recommended that COPD patients learn Tai Chi as soon as they’re diagnosed because it will take some time to learn how this form of movement mediation works, and its benefits will increase exponentially as time goes on.
Tai Chi also has several undeniable benefits when it comes to mindfulness. One of the reasons anxiety and depression are so common among COPD patients is that they feel a loss of control. Chest pain, fatigue, breathlessness, and exacerbations caused by COPD cannot always be predicted, so Tai Chi affords these people the ability to be in full control of something. Many people swear by this, saying that it has renewed a sense of control and purpose in their life.
There are three different ways to practice Tai Chi: as an individual, in a group setting, or with an instructor. Currently, due to COVID-19, it’s recommended that you practice Tai Chi on your own, however, if you can find a group that takes social distancing measures seriously, this could be an option too. If you’re doing it on your own, this guide will be helpful in getting you started on the right foot.

Yoga can also be considered a type of movement meditation, however, whereas Tai Chi is more focused on the act of moving, yoga is more focused on the various positions. Another difference between the two is that Tai Chi is usually performed in a standing position while yoga is done on the ground. Since yoga requires a lot of strength and agility, it’s not always recommended for people who are physically impaired.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Mantra Meditation
A “mantra” is a word, syllable, or phrase that’s repeated during meditation. This is very similar to focused meditation in that you’re concentrating on one specific thing, however, mantra mediation differs because there is usually a purpose or a meaning behind the sound that’s being produced. Mantras can also be repeated by the mediator whereas the sounds produced in focused meditation are usually external.
.jpg)
The idea behind mantra meditation is that every sound is a tool for transforming consciousness. So, instead of simply training your mind to concentrate, you’re also altering your state of mind rather than just your thoughts. The type of sound that you produce, its frequency, and volume will all be determined by what state of mind you’re trying to produce. One of the most popular types of mantra meditation is called transcendental meditation.
Mindfulness Meditation
Mindfulness meditation is directed at helping you be more present in the current moment. In other words, whereas focused meditation and mantra meditation are aimed at focusing on one specific sensation, mindfulness mediation is designed to help you better understand the urges and feelings you are currently experiencing.
Another core component of mindfulness meditation is understanding your breathing. Unlike with breathing techniques, there is no special way that you have to breathe. As the name “mindfulness” suggests, you should be focusing on how your breathing is in the current moment, not how you want it to be.
Benefits of Meditation for COPD Patients
Conclusion
Mindfulness is something that many people struggle with. It’s easy to forget that an overworked mind that’s crowded with thoughts can not make decisions effectively. And living with this burden for months or years on end can be exhausting to say the very least.
There are many different types of meditation, but they’re all aimed at helping you control your thoughts and motor functions, and giving you the skills you need to live in the moment rather than being distracted by thoughts of the past or future.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
As a COPD patient, there is no understating the importance of effective meditation. If you become overwhelmed by negative thoughts about your disease, you may want to take a step back and start incorporating meditation techniques into your daily routine.
While meditation is by no means a replacement for your COPD treatment plan, certain types of meditation like Tai Chi and yoga can be used in tandem with your pulmonary rehabilitation plan and breathing techniques. But as always, be sure to check in with your pulmonologist to learn the best way to do this.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!










