
If you have chronic obstructive pulmonary disease (COPD), you know that your lung health is directly linked to your systemic health. Just having COPD puts you at a higher risk for respiratory infection, heart disease, high blood pressure, and even mental health conditions like depression and anxiety. But did you know that there’s even a link between your oral health and COPD?
Chances are, you’ve been told from a young age that brushing your teeth will help you prevent cavities and have a nice smile. But this leaves out a lot of details about how your oral hygiene plays a bigger role in your overall health and wellbeing. According to a study funded by the COPD Foundation, people with severe COPD have poor oral hygiene and they also have poor oral health-related quality of life.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In this post, we’ll discuss some of the reasons COPD patients tend to have poor oral health in comparison to the general population and we’ll also give you some tips for improving your oral health routine in order to live more comfortably with COPD. If you have any questions, please don’t hesitate to leave them in the comment section below so we can get back to you. Alternatively, you can reach out to your doctor for more information about this subject.
How Does COPD Affect Your Oral Health?
When someone is told that two seemingly unrelated organs in the body like the lungs and the teeth or gums are inextricably linked, they’re often surprised. However, the closer you look, the more you’ll realize that they’re related in a number of ways, whether it’s directly or indirectly. The body, as a whole, is a system, so it’s not surprising that something that affects one part will eventually have an effect on the whole.
The Effects of Smoking
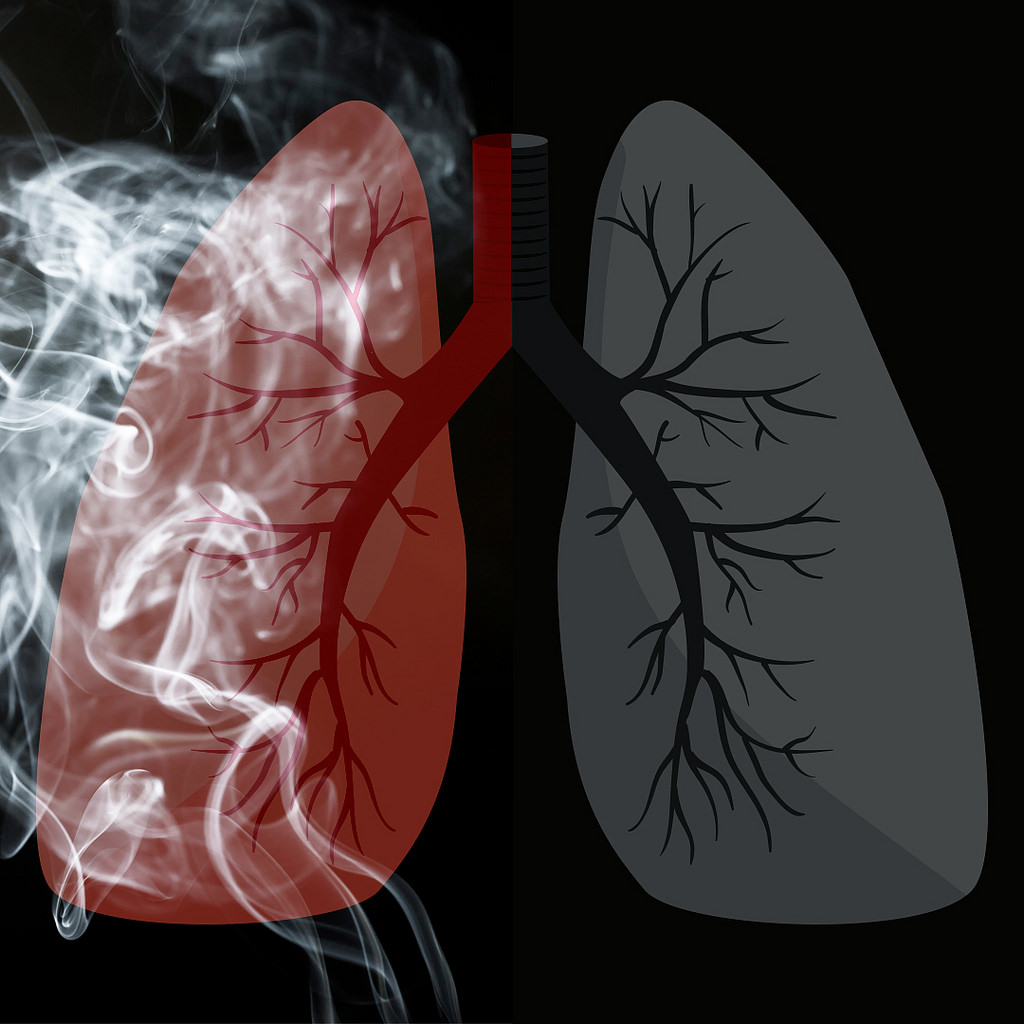
The first reason that COPD patients are more likely to have dental health issues is that most COPD patients either currently smoke or were smokers in the past. According to the American Lung Association, around 85 to 90 percent of COPD cases are caused by cigarette smoking and around 38 percent of COPD patients report that they are still smokers. Over the decades, evidence has consistently shown that smoking is incredibly bad for your teeth and gums.

In your mouth, there is a constant battle going on between good bacteria which cleans your teeth and gums, and bad bacteria which leads to tooth decay and gum disease. Smoking negatively affects the quality of your saliva by destroying protective macromolecules, proteins, and enzymes. In other words, the immunological aspect of your saliva is severely hampered the more you smoke.
Smoking also affects your immune system as a whole meaning your body will be less equipped to deal with an infection in your gums or teeth. This study shows that cigarette smoking can have one of two effects on the body. It either exacerbates immune responses leading to chronic inflammation in the body or it attenuates the immune response. Either way, the immune system is less capable of doing its job and warding off infections before they become serious or even life-threatening.
Changes in Your Routine
There’s no doubt about it, being diagnosed with COPD can be life-changing. You might be pressured by your doctor or family to make sudden and drastic changes to your lifestyle, all of which can be daunting and feel like the weight of the world is on your shoulders. More often than not, this causes people to fall back on aspects of their daily routine that they’ve kept up on for many years like practicing good oral hygiene and even making it to the dentist regularly.

Considering the fact that COPD patients visit their doctor more frequently than the general population and many of them are working and maintaining their personal lives and relationships, it can be very difficult to find time to make it to the dentist. And the longer this goes on, the more likely it is that you could develop something like gum disease or periodontitis without even knowing.
COPD Medication
Believe it or not, the medication you take for COPD is another thing that could be causing a decline in your oral health. According to this patient education manual created by the American Thoracic Society, COPD medication can cause dry mouth, a condition where your salivary glands do not produce enough saliva. While this may seem rather harmless, it can actually be quite dangerous if it’s prolonged because saliva plays such a vital role in protecting your teeth and gums.

Inhaled bronchodilators (both short- and long-acting) can cause dry mouth. These medications are used to open up the airways to help you breathe easier and help them clear mucus. Also, inhaled anti-inflammatory medication (corticosteroids) like beclomethasone, budesonide, or fluticasone are known to cause dry mouth. Since these medications are a core part of your treatment plan, it’s best not to completely eliminate them, but to find a workaround for coping with dry mouth instead. This article will give you a good overview of how to deal with dry mouth.
Another potential issue caused by COPD medications is something called oral thrush. This is an infection that occurs in the mouth and throat due to a weakened immune system caused by inhaled medication. Typically, this condition is not serious, but it can cause discomfort while eating and you may need to take antifungal medication in order to get rid of it. Oral thrush is also known to cause or contribute to dry mouth.
How Does Your Oral Health Affect COPD?
Similar to how COPD affects your oral health, there’s also a mountain of evidence suggesting that your oral health can negatively affect your COPD. According to a study published in the Journal of Periodontology, periodontal disease may increase the risk of respiratory infection such as pneumonia in COPD patients. This is a condition that causes the alveoli (tiny air sacs in the lungs) to fill with fluid leading to a chronic cough and breathlessness.
It Can Alter Your Diet
Probably the most likely way that your oral health will affect your lung health is by altering your diet. If you’ve read our articles here at LPT Medical before, you likely know how important your diet is when it comes to reducing chronic pain while preventing breathlessness and fatigue. Most COPD patients should maintain a diet high in protein, healthy fats, and fiber, however, it depends on your individual circumstances.

As we get older, our dental health declines significantly. According to Boston Magazine, people between the ages of 35 and 44 years old have lost at least one tooth. And between the ages of 65 to 74, about 26 percent of people have lost all of their teeth. This is due to a number of causes such as tooth decay, gum disease, periodontal disease, and even traumatic injury. This can impact your diet because it may prevent you from eating certain foods.
-jpg.jpeg)
Unfortunately, foods that are easy to consume and provide us with a lot of energy also tend to be the worst for us. Things like fruit juice, soda, yogurt, and processed foods are convenient, but they’re also laden with sugar and additives that will exacerbate your respiratory symptoms and leave you feeling exhausted and unmotivated. Taking some extra time to cut or break your healthy foods up into smaller pieces may remedy this issue.
It Can Lead to Infections
Most dental infections occur in the tooth, gums, or supporting structures of the teeth. But did you know that dental infections can actually spread to other parts of the body if they aren’t treated? Most COPD patients have a weakened immune system meaning it will be more difficult for your body to fight it off. In certain cases, these infections can be severe and even life-threatening so it’s best to always seek help sooner rather than later. What’s more, dealing with dental issues can be extremely draining and it will take time and energy away from your COPD routine.

Preventing infections is absolutely imperative as a COPD patient. Lung infections are the most likely cause of flare-ups and exacerbations, and they’re also the most likely cause of someone being admitted to the hospital due to COPD. So, whenever you go to brush or floss your teeth, think of it as being beneficial for your full-body wellness rather than just your teeth and gums.
What Can be Done to Improve Your Oral Hygiene?
Brush More Frequently
Possibly the simplest way to improve your oral hygiene is to brush and floss more frequently. With the busy schedules that many people have nowadays, it can be hard to find the time to brush twice a day and floss, but it’s the best thing you can do for your oral health. People tend to skip flossing, but this is the only way to reach the bacteria between your teeth where it can cause the most harm. Be sure to brush your teeth at least twice a day and floss at least once a day.

Drink More Water
Proper hydration not only helps with organ function, but it can also help prevent cavities. When you think about all of the different foods you consume in a day, it’s not hard to see why this is so important. Water removes food from between your teeth, prevents dry mouth, and can dilute acids that stain and eat away at your teeth. Rather than drinking a bunch of water in the morning or right before bed, try drinking water throughout the day, especially during meals. This way, food particles don’t have the opportunity to latch onto your teeth and cause damage.
.jpg)
Schedule Regular Teeth Cleanings
While you can and should take your dental health into your own hands, it’s also important to see a dental specialist regularly. Even if you are careful with your brushing and flossing, any leftover plaque on your teeth when you go to bed at night will turn into something called tartar. This is basically a hardened version of plaque that can only be removed with special tools by your dentist. Another reason to schedule regular teeth cleanings is so that your dentist can make sure your teeth and gums are healthy and that you’re on the right track. Dental issues are almost always easier to fix when they’re detected early on.
Consider Dental Implants
It’s estimated that about 90 percent of people with no teeth use dentures. And while dentures can improve your smile, they don’t provide any benefits when it comes to eating. Dental implants, on the other hand, essentially provide you with a new pair of teeth that are just as effective as natural ones when it comes to chewing. In other words, you’ll be able to keep up with the dietary requirements that your doctor gave you to help you manage COPD. Dental implants can be used to replace just one missing tooth or a whole mouth of missing teeth.
.jpg)
The important thing to remember with dental implants is that your oral hygiene is still incredibly important. While implants can’t decay like your natural teeth can, you will still need to keep your gums healthy in order to prevent gum disease and periodontal disease. When you get dental implants, you will be provided with special cleaning tools and instructions on how to maintain your new teeth. Not everyone is a candidate for dental implants so you’ll need to schedule an appointment with a periodontist to see if they’re right for you.
Conclusion
There is a two-way road between your oral health and your lung health. Years of smoking and the development of COPD can contribute to problems like tooth decay and gum disease. On the other hand, maintaining a poor dental health regime can cause flare-ups in your respiratory symptoms. In other cases, poor dental health and poor respiratory health can contribute to comorbidities like heart disease, poor circulation, and more.
While you have a lot to worry about like making it to doctor’s appointments and pulmonary rehabilitation, it’s always important to make time for your oral health as well. The American Dental Association recommends brushing your teeth at least twice a day with fluoride toothpaste and you should go in for teeth cleanings every six months. And if you have any additional concerns about how COPD could affect your oral health, be sure to speak with your doctor immediately.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Lastly, if you’re a COPD patient looking for a better solution for your oxygen needs than a bulky oxygen tank, take some time to look through our portable oxygen concentrators here at LPT Medical. POCs are electronic oxygen delivery devices so you’ll never have to refill them. They’re also extremely travel-friendly and easy to use. We recommend the Inogen One G5 and Caire FreeStyle Comfort to most patients, but you can learn more about the specifications by reaching out to our respiratory specialists.
.png)
If you tuned into our blog earlier this month, you know that we discussed COPD as a “systemic disease.” In other words, it’s a disease that affects every part of the body, not just the lungs. This is an important distinction to make because it enables both patients and medical professionals to detect systemic manifestations earlier on and treat them more effectively. One of the systemic manifestations that we mentioned in this post is osteoporosis, a disease that affects the density of the bones.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Osteoporosis is a common comorbidity of COPD, meaning the two conditions often exist side-by-side. Because of the nature of the two diseases, there are many complications that arise as a result of having them both. For example, both COPD and osteoporosis increase the patient’s risk of experiencing a fall as well as getting seriously injured from a fall. In this post, we’re going to take a closer look at the connection between COPD and osteoporosis, how they’re related, and how to cope with each. If you have any questions or concerns, be sure to leave them in the comment section below so that we can get back to you.
What is Osteoporosis?
Your bones are in a constant state of repair. Cells called osteoblasts synthesize bone material and assist in the mineralization of bone tissue. Simultaneously, cells called osteoclasts degrade old bone tissue and send calcium back into the blood. After a year, your body has regenerated about 10 percent of its bone tissue. The reason your body does this is that bone tissue does not last forever. It needs to be replaced regularly in order for your bones to be strong enough to support the weight of your body.
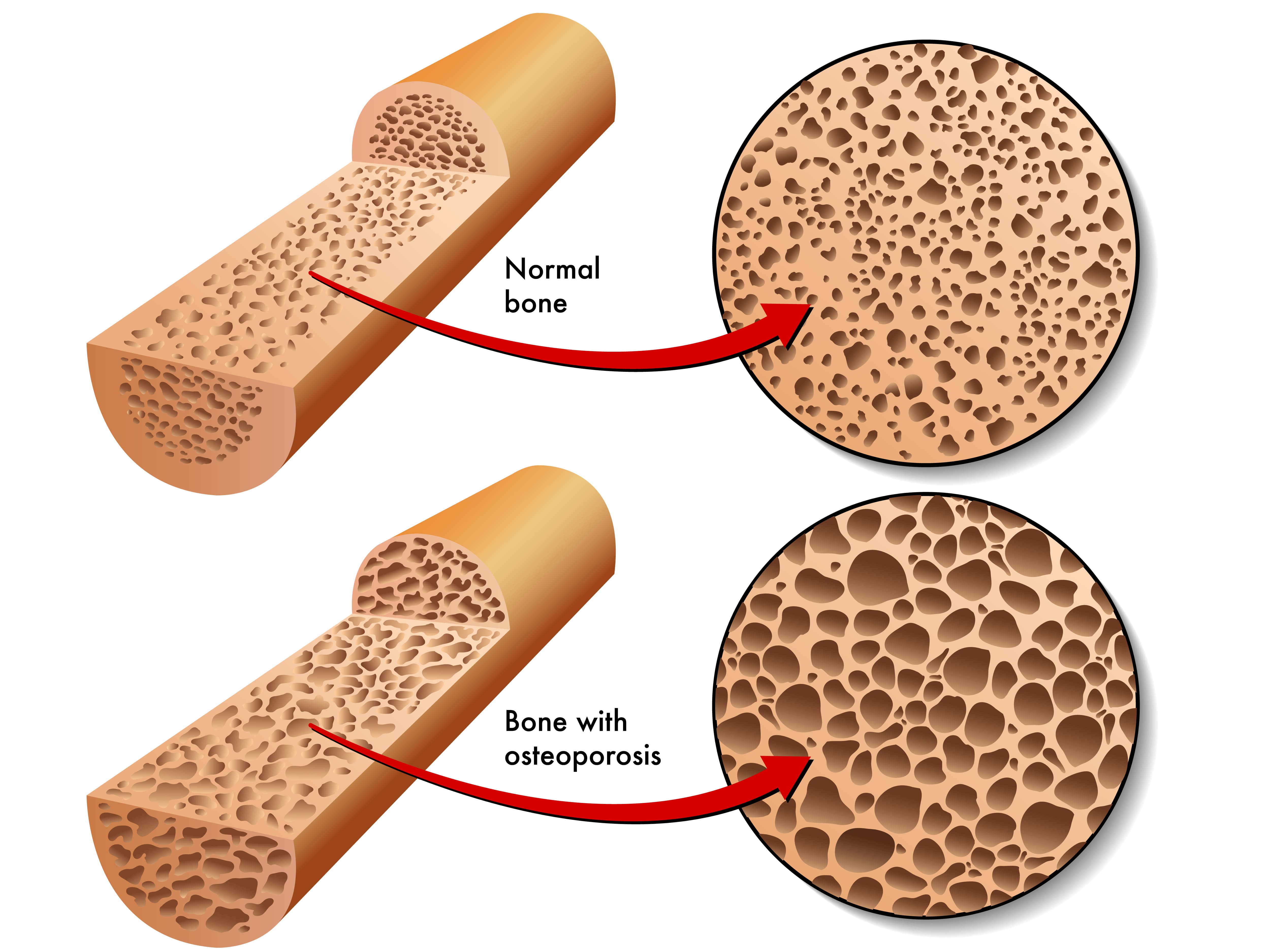
It’s natural for bone remodeling to occur more slowly the older we get. However, if the rate at which bone is produced is much slower than it’s being removed, or it’s being removed much quicker than it’s being replaced, this is known as osteoporosis, a disease that affects around 10 million Americans. Osteoporosis is more common in women over the age of 50, but anyone can get it at any age.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Osteoporosis usually develops very slowly and people are at a higher risk if they have a lower “peak bone mass.” Most people reach this point when they’re in their mid-twenties to thirties, so osteoporosis can sometimes (but not always) be predicted. Oftentimes, there are no warning signs of osteoporosis until the patient experiences a fracture. However, some people will experience joint pain, back pain, or a stooped posture. One instance where you may receive an early diagnosis of osteoporosis is if your doctor believes you are at high risk for this condition.

Bone fractures in the hip or spine are some of the most serious complications of osteoporosis because they impair the patient’s mobility. Falls are the most common cause of these types of injury but in severe cases, bones can fracture from simply bumping into something, bending over, or coughing. While there is no cure for osteoporosis there are many treatment options available that can help boost the rate of bone growth in your body, thus helping to prevent fractures and chronic pain.
How is Osteoporosis Diagnosed?
The main test used to diagnose osteoporosis is called a bone mineral density (BMD) test. It uses a type of low-energy X-ray called Dexa-Scan (dual-energy X-ray absorptiometry or DXA) to calculate the density of bone in the spine and hip. Your bone mineral density (BMD) is compared to the mean BMD for your age to determine if you have either osteoporosis or osteopenia. This is a condition that simply means you have low bone mineral density, it doesn’t necessarily mean that you will develop osteoporosis in the future or that you’re at risk of experiencing a fracture. If your BMD is less than one standard deviation below the mean, your bones are normal. Between -1 and -2.5 standard deviations is considered osteopenia and more than -2.5 is osteoporosis.
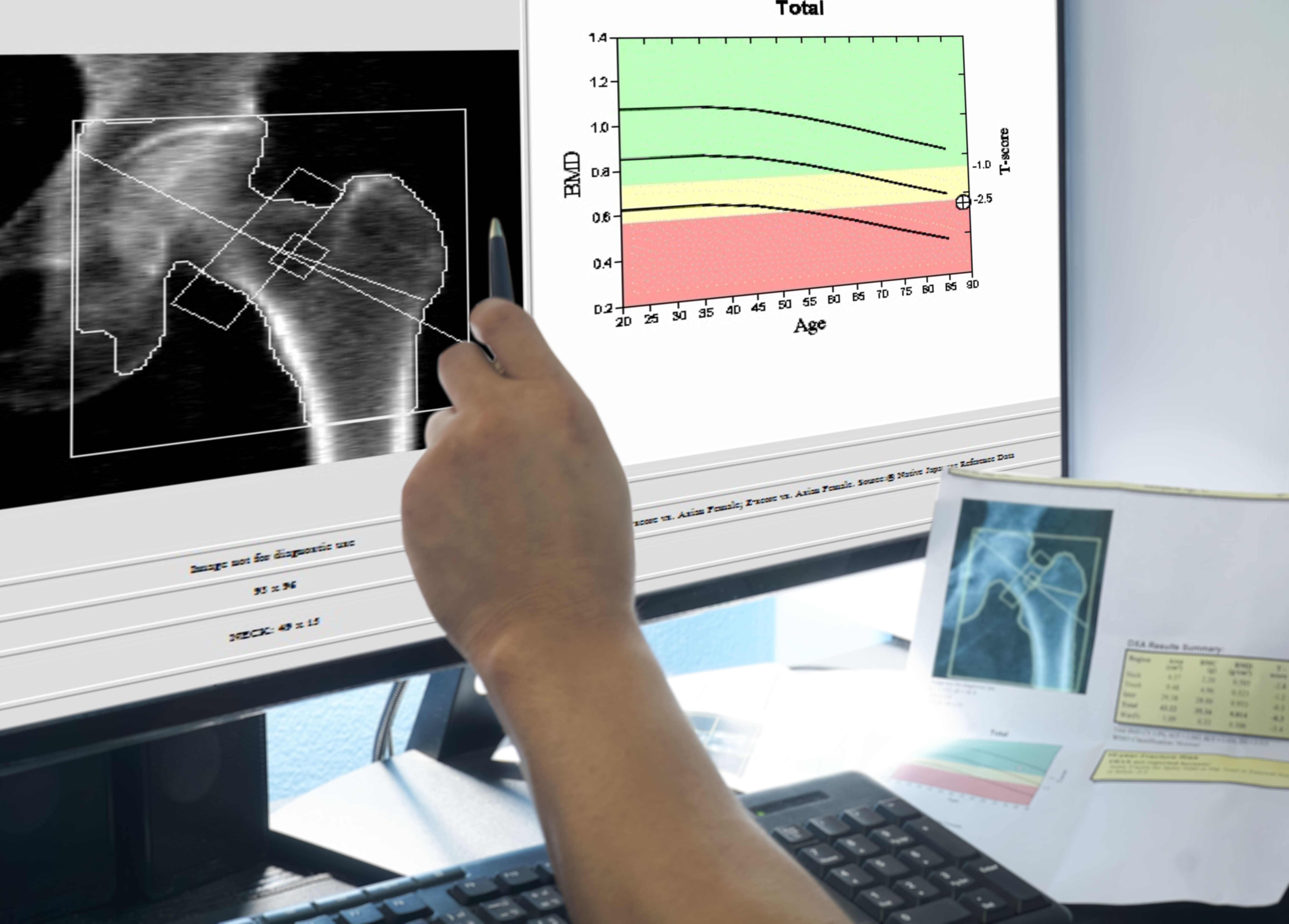
There are many other tests that can be performed to assist health professionals to determine if you have osteoporosis. Computerized tomography (CT) scans, X-rays, ultrasounds, and body composition analysis which shows the percentage of body weight due to bone, fat, muscle, and water. There are also many blood tests that can assist in diagnosing osteoporosis including blood calcium tests, vitamin D tests, thyroid tests, and testosterone tests. Be sure to ask your doctor if you’re not sure which test you need to take.
What’s the Link Between COPD and Osteoporosis?
At first glance, you might notice a lot of similarities between COPD and osteoporosis. Both conditions are more common in older adults, more common in women, and they can’t be cured. However, they’re both highly treatable. In other words, you’re at a higher risk of contracting COPD and osteoporosis based on your age and gender alone. But when you take a closer look, you’ll notice that there are many common side-effects of COPD that put you at a higher risk of osteoporosis in old age.

According to a study published by the National Health and Nutrition Examination Survey (NHANES) which included 14,828 subjects over the age of 45, there was an 8.5% prevalence of osteoporosis in non-COPD patients, but there was a prevalence of 16.9% in COPD patients. Let’s take a look at some of the side effects of COPD that may lead to osteoporosis.
A History of Smoking
Smoking is the most common preventable cause of morbidity and mortality worldwide. Smoking has countless systemic effects ranging from lung cancer to heart disease. Studies have also shown for decades that tobacco use has extremely adverse effects on bone health, not least of which is decreased bone density. According to UCI Health, there are several reasons why smoking is so bad for bone health. Firstly, it reduces the flow of blood to your bones by causing your blood vessels to constrict. This means your bones are being deprived of vital resources including osteoblasts, the bone-producing cells. Smoking has also been shown to hamper the resorption of calcium meaning it can’t be replaced in the bones.

There isn’t much to say about smoking and COPD that hasn’t already been said. According to the American Lung Association, about 85 to 90 percent of COPD cases are caused by cigarette smoking. What’s more, about 38 percent of people with COPD continue to smoke after receiving a diagnosis. It goes without saying that, if you’re a current smoker, the sooner you quit, the better. The respiratory effects of smoking are bad enough on their own, but when they’re combined with chronic pain and an increased risk of fractures, these issues are exacerbated.
Diet
Your body needs a large variety of vitamins and minerals in order to maintain every bodily function from digestion to blood flow. But when you develop a chronic condition, you often need to adjust your diet to accommodate for certain deficiencies that you may develop. In COPD and many other respiratory diseases, vitamin D deficiency is very common. Vitamin D is essential for everyone because it plays a vital role in helping your body absorb calcium which is the main support structure for your bones. Without it, your bones will become weak and brittle.

One of the main reasons respiratory patients are vitamin D deficient is that they oftentimes aren’t exposed to as much sunlight as their healthy counterparts. Sunlight is the most important natural source of vitamin D, but many COPD patients are immobilized by symptoms like fatigue, breathlessness, and chronic pain. One way to combat this is to simply sit by a window where you’re receiving direct sunlight. If you live in an area that doesn’t receive sunlight for prolonged parts of the year, you can supplement your diet with vitamin D-rich foods like oily fish, red meat, or egg yolks.
Body Mass Index (BMI)
Body mass index is derived from your body weight and height. Anything between a BMI of 18.5 and 24.9 is normal, but if you dip below this or go above it, it may be cause for concern. While the United States suffers from an obesity epidemic, COPD patients often suffer from the opposite problem — being underweight. According to the Lung Institute, COPD patients burn an average of 10 times as many calories while breathing as their healthy counterparts do. This is why many doctors recommend that COPD patients increase their caloric intake after being diagnosed. According to Healthline, about 25 to 40 percent of people with COPD have low body weight.

Having a BMI under 21 is also a risk factor for low bone mineral density (BMD) and osteoporosis. Studies have shown that BMI inversely correlates with BMD, so the lower your body weight is in comparison to your height, the more at risk you are for developing weak bones. As a COPD patient, the best thing you can do to prevent this is to ensure that you are eating enough and that you are following your doctor’s advice on what to eat. If you experience exhaustion from consuming large meals, try eating smaller meals all throughout the day in order to meet the calorie requirement that your doctor has set. This also helps your body out with digestion and prevents feelings of fatigue and bloating after eating.
Physical Activity
Exercise is one of the key components of an effective COPD treatment regime. Exercise keeps the lungs strong and healthy, reducing symptoms of breathlessness and chest pain. Strong muscles also use oxygen more effectively meaning you’ll be able to stay out of the house and stay active longer without taking a break. And while exercise can’t reverse COPD, it can improve your life expectancy and quality of life. Be sure to discuss with your doctor which exercise program will be best for you. Most health specialists recommend pulmonary rehabilitation which involves lung education, strength training, and endurance training.

According to Orthoinfor.aaos.org, exercise affects bones similar to how it affects muscle — it makes it stronger. Bone is living tissue and when stress is applied to it, it reacts by building more tissue. So, it goes without saying that, by exercising regularly, you can keep your bones in good condition and prevent osteoporosis. Unfortunately, due to the respiratory symptoms of COPD, many people are left feeling unmotivated or unable to exercise, and in turn, their bone health begins to suffer. You should aim to exercise at least 3 to 4 times per week and since hip and spinal fractures are most common in osteoporosis, be sure to get on your feet and work your whole body, not just your arms. Exercise also strengthens your stabilizer muscles, helping to improve balance and prevent falls.
COPD Medication
One final way that COPD affects your bones is through your medication. Your medication is a vital part of your treatment plan, but you have to be careful with it because, like any medication, it has both short- and long-term side effects. Most of the side effects should be listed on the container of the medication, but for more specific information, be sure to consult your doctor. The main COPD medication of concern when it comes to bone health is corticosteroids. These drugs are used by COPD patients to reduce inflammation which can prevent flare-ups and exacerbations. Corticosteroids are usually inhaled via an inhaler or nebulizer in order to reach the lungs more quickly.

The way that corticosteroids affect the bones is by altering the way the body uses vitamin D and calcium. Oftentimes, corticosteroids increase the rate at which bone breaks down and reduces its ability to absorb calcium. If corticosteroids are used heavily, this could lead to rapid bone deterioration, so it’s important to use them only as they’re prescribed. If you’re still concerned about bone loss even while taking the normal dosage, be sure to ask your doctor if there are any alternative medications that you can take without this side effect.
Conclusion
COPD is one of the most common chronic illnesses in the world. However, many people are unaware of the many systemic manifestations of this disease. About 36 to 60 percent of COPD patients have osteoporosis which is higher than the general population. The good news is that just a few lifestyle changes can significantly reduce your risk of experiencing low bone mineral density and osteoporosis. Immediate smoking cessation, a revised diet, regular physical activity, and careful use of your COPD medication are just a few of the most important.
If you’re a COPD patient who’s struggling to get on your feet and maintain an exercise routine, consider upgrading your obsolete oxygen device to a portable oxygen concentrator. POCs are much smaller and lighter than a standard oxygen tank meaning you won’t feel out of breath after a short walk. Portable oxygen concentrators like the Inogen One G5 and Caire FreeStyle Comfort have taken the oxygen industry by storm with a simple, easy-to-use interface, sleek design, and high oxygen output. If you’d like to learn more about these devices and all that they have to offer, don’t hesitate to reach out to our oxygen concentrator specialists here at LPT Medical.
_%20(1).png)
One of the most common questions we hear COPD patients ask is, “how can I clear my airways when they get congested?” As a COPD patient, you’re likely to experience coughing fits that are brought on by the buildup of mucus and sputum in the airways and lungs. And sometimes, no matter how hard you try, you feel like you can’t clear them in order to catch a breath of fresh air. This is far more common than you might expect and it can be a frustrating and sometimes even scary experience.
Another thing that many people don’t realize is that airway clearance can be a lot more complicated than learning how to cough correctly. There are many different techniques that can be applied, and it’s also helpful to know why your airways are becoming congested in the first place. In this post, we’ll help you understand some of these concepts and provide you with a step-by-step guide on how to clear your airways safely.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
As always, it’s imperative that you speak to your doctor if you experience ongoing issues with coughing, wheezing, or shortness of breath. These symptoms tend to get worse over time unless the root cause is dealt with. What’s more, coughing fits can lead to flare-ups and exacerbations which can put you in the hospital.
Why does COPD Make it Difficult to Clear Your Airways?
There are two different types of chronic lung disease: obstructive and restrictive. A restrictive lung disease like pulmonary fibrosis or interstitial lung disease is one that affects the lungs’ ability to expand. An obstructive lung disease like COPD or bronchiectasis, however, prevents you from fully expelling air from the lungs. This is especially problematic when the patient tries to cough because they may not have the force necessary to clear mucus and other substances from the airways.

Another reason that COPD makes it more difficult to clear your airways is that this disease is associated with changes in the way that mucus and sputum are produced in the body. In a healthy individual, mucus plays a vital role in the body’s immune function. The body carefully regulates the mucus lining the airways and lungs so that there is enough to trap bacteria but not so much that you choke or can’t breathe naturally. However, in COPD patients, there is usually an overproduction of mucus due to oversized mucus glands and an overabundance of goblet cells.
If you’re a current smoker, this could be another reason that you’re experiencing issues with airway obstruction. According to the Centers for Disease Control and Prevention (CDC), as many as 38 percent of COPD patients are current smokers. This study published in the Karger medical journal found that moderate and heavy smokers have a higher impairment in mucociliary clearance than their non-smoking counterparts. One of the key ways that smoking affects airway clearance is by damaging and killing cilia. These are tiny hair-like organelles that help to push mucus and other debris out of the airways.
Since there are so many different causes of airway obstruction in COPD, it’s important to have a comprehensive treatment plan to deal with these symptoms. Airway clearance therapy can and should be used, but it won’t be as effective if you aren’t following all other aspects of your treatment plan that your doctor has designed for you. Ideally, if you’re following your treatment plan carefully, you won’t experience mucus buildup as frequently and you’ll only need to use airway clearance techniques in rare circumstances.
What is Airway Clearance Therapy (ACT)
Airway clearance therapy, or sometimes called airway clearance techniques, is a group of scientifically backed methods used for clearing mucus from the airways. These techniques were developed as a more controlled version of our body’s natural airway clearance techniques like coughing and wheezing. A chronic and persistent cough or episodes of wheezing can be extremely unhealthy, especially if they lead to you losing sleep or feeling lightheaded or fatigued. Airway clearance techniques aim to not only make COPD patients more aware of how they’re coughing, but also provide them with some entirely new methods that may be more effective.
-jpg.jpeg)
Generally speaking, airway clearance techniques are divided into seven different categories. Everyone has a slightly different way of practicing these techniques, so don’t be alarmed if your pulmonologist tells you something that differs from what you have read here. Our goal is simply to provide you with an overview so that you can better understand how airway clearance therapy works.
1.) Controlled Coughing
Like we mentioned before, uncontrolled coughing is problematic in COPD patients. Without understanding how your lungs, airways, and mucus work, simply expelling air in an attempt to dislodge any obstruction can be more effort than it’s worth. One of the biggest problems associated with normal coughing or wheezing is that it often causes the airways to collapse, meaning that no matter how hard you cough, the mucus will be stuck. If you hear a wheezing or whistling noise when you cough, this is a sure sign that your airways collapse when you cough. Controlled coughing is focused on keeping the airways open so that you’re not wasting valuable energy and oxygen.

The first rule of controlled coughing is to avoid inhaling sharply through your mouth. This can send mucus back down the airways and be very counterproductive. Instead, inhale slowly but deeply through your nose. This way you have enough oxygen to cough correctly. It’s best to practice controlled coughing while sitting down and you should try to relax as much as possible. Especially try to eliminate the tension in your shoulders and chest because this can contribute to the airways becoming narrow.
Once you’re seated, lean forward slightly and place your hands on your abdomen. You’re going to cough three times and you should really focus on the quality of each one to ensure that the mucus is moving out of your airways rather than back down into your lungs. Be sure to take a deep breath through your nose between each cough to ensure that you move enough air. If you need to take a moment to relax between each cough, this can be helpful.
Another technique that’s similar to controlled coughing is huff coughing. For the most part, you will follow the same steps as you would for controlled coughing. However, instead of coughing, you’re going to be forcing air through your airways similar to how you would fog up a mirror or how you would clean a phone screen or your glasses. In other words, you’re expelling air out your mouth without creating any vibrations in your chest or throat.
2.) Autogenic Drainage (AD)
The aim of autogenic drainage is to move mucus from the smaller airways into the larger airways (peripheral airways into central airways). By doing this, it is much easier to dislodge the mucus because it’s all in one area. The rationale for autogenic drainage is based on a principle of solid mechanics called shear force. This is when unaligned forces are applied to an object causing it to bend in two different directions. In the case of autogenic drainage, the mucus and other secretions in the airways are the object that’s being manipulated. This is done through a series of carefully monitored breathing techniques.
3.) Postural Drainage and Percussion (PDP)
Postural drainage and percussion, also known as chest physical therapy (CPT), is a technique that involves using your hands to assist with airway drainage. While you can do PDP on your own, it’s often recommended that you have someone assist you with it, whether it’s a friend, loved one, or your physical therapist. Like autogenic drainage, PDP is a technique that will take some time to perfect so it helps to be patient as you learn the ins and outs of this method.
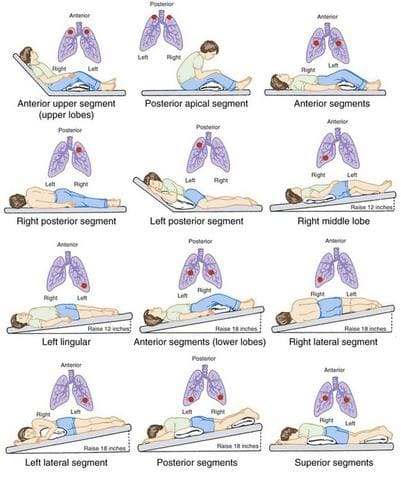
The reason this method is called “postural” drainage is that you are going to use different positions that leverage gravity in order to drain the mucus from your airways. The general rule of thumb is that your hips should be higher than your chest. Whether this means laying on your back, side, or stomach, you can do whatever is most comfortable for you. Many people prefer to use pillows or blankets to elevate their hips.
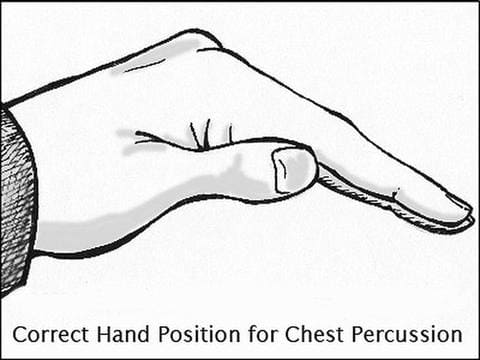
Once you’ve found a comfortable position you can begin the percussion. Most specialists recommend cupping your hand and placing it palm down on your chest. This will allow you to break up the mucus in your chest without hurting yourself. The percussion can also be done on your back but it’s best to have a partner to help you out with this.
4.) Positive Expiratory Pressure (PEP) Therapy
Essentially, the term positive expiratory pressure means experiencing greater resistance when you’re exhaling than when you’re inhaling. This is done with a PEP device which you hold to your mouth and breath into. The device allows you to inhale normally, but when you go to exhale, you experience resistance about four times greater than what you would normally experience. What this does is keeps your airways open as you exhale and allow the force of your air to get behind the mucus and push it out of the airways.

5.) Oscillating Positive Expiratory Pressure
Oscillating positive expiratory pressure therapy is very similar to the method above. However, an oscillating PEP device uses high-frequency oscillations that break up mucus as you exhale. Oscillating PEP devices look similar to traditional PEP devices but they have a ball inside that rattles around as you exhale. This is what creates the vibrations in your upper chest. After blowing into the device several times, you can take a break to clear out any mucus that the device brought up. Then simply repeat the process.
6.) High-Frequency Oscillating Vest
A high-frequency oscillating vest is another tool that can be used for airway clearance. This is an inflatable device that looks a lot like a life vest. The oscillating vest is connected to an air compressor via two hoses. Once it’s turned on, the vest inflates and deflates in rapid succession. The basic principle is that it uses positive and negative pressure changes in the chest to augment peripheral and tracheal mucus movement towards the airway opening. After a set period of time, the device is stopped and the patient can cough to bring up the mucus.

While high-frequency oscillating vests are very effective, they aren’t without disadvantages. These vests can be very expensive to purchase and maintain. What’s more, they’re not very portable in comparison to the PEP devices which we discussed earlier. If you’re someone who travels a lot you might find that high-frequency oscillating vests are more trouble than they’re worth.
7.) Active Cycle of Breathing Technique (ACBT)
The active cycle of breathing technique is an airway clearance method that combines positioning, breathing, and coughing. Since this is the most complex airway clearance technique it’s also the most flexible when it comes to being adapted to fit a variety of patient’s needs. The goals of ACBT include improving the effectiveness of your coughs, improving lung ventilation, and clearing secretions from the lungs. Below are the three different phases of ACBT:

Phase 1 - Breathing Control and Relaxation
The first step in ACBT is to bring your breathing under control and completely relax your body. The majority of the tension in your body will be located in your shoulders, chest, and back, and many people are unaware of how much this can affect the way you breathe. Start by closing your eyes and placing your hands on your stomach. Sit with your back straight and begin to practice pursed lips breathing. This is where you inhale slowly through your nose and exhale fully through pursed lips.
Phase 2 - Thoracic Expansion Exercises
As the title suggests, the aim of phase 2 in the active cycle of breathing technique is to expand the chest. During this step, you will take 3 to 5 deep breaths in through your nose and out through your mouth while keeping your shoulders and chest relaxed. At the peak of each inspiration, you will hold your breath for 2 to 3 seconds. After the allotted time, simply release the air rather than trying to force it out.
Phase 3 - Forced Expiratory Technique (FET)
The forced expiratory technique is another way of saying “huff” cough. Like we described under the “controlled coughing” section, a huff cough is a way of clearing mucus without allowing the airways to collapse. You’re simply pushing air out the lungs but putting more air behind it than you would with a normal breath. You should repeat this after each thoracic expansion that you do.
Other Ways to Prevent Airway Obstruction With COPD
Drink Plenty of Water
Your ability to prevent airway obstruction depends heavily on your level of hydration. Mucus is made up of about 97 percent water. However, slight variations in this can cause it to become extremely thick and difficult to clear from the airways. Since every organ in your body uses water, it’s imperative that you aren’t starving yourself of this vital resource. According to COPD.net, the average COPD patient should drink between 8 and 12 glasses of water every day.

As you work to increase your water intake, it’s also important to reduce your intake of other types of fluid. Milk, and dairy products in general, are known for thickening your mucus so you’re going to want to avoid these as much as possible. Much like salt, sugar has the ability to dehydrate you, so you should avoid sugary sodas, fruit juices, or sweetened tea. If you absolutely have to drink something other than water, try unsweetened hot green tea which will not only thin your mucus but has a number of other health benefits as well.
Maintain a Balanced Diet
Healthy eating is all about getting the right balance of nutrients that your body needs to stay healthy. For COPD patients and people with other respiratory illnesses, this could mean consuming less sodium and salt which contributes to problems like airway obstruction. You should also avoid highly processed foods which can contribute to bloating and thus making it more difficult to breathe. Most COPD patients tend to do better with a diet that is high in protein and healthy fat which is easy to digest and will support healthy lung function.
![]()
Use COPD Medications Effectively
Depending on how severe your COPD is, your doctor has likely prescribed you some medication for coping with your symptoms. One of the most common medications for COPD is called bronchodilators. These medications open up the airways so that you can breathe easier and they can make it easier for you to perform the airway clearance techniques listed above. Ask your doctor about changing up your treatment schedule to assist with airway clearance.

Another medication that can help with airway clearance is a class of drugs called expectorants. These are medications are designed to thin the mucus in your airways making it easier to clear. Expectorants aren’t designed specifically for COPD patients because they’re also used to treat congestion associated with the common cold and the flu. While expectorants are available for over-the-counter purchase, you should be sure to ask your doctor before using them because they may have adverse interactions with the COPD medications you already take.
Pulmonary Rehabilitation
Pulmonary rehabilitation (PR) is an exercise and education program focused on improving lung strength and function. COPD patients should begin pulmonary rehabilitation right after they’re diagnosed so that they learn the best way to take care of their lungs and slow the progression of COPD. Another benefit of PR that many people don’t realize is that it can help with airway clearance. According to a study published in the European Respiratory Journal, exercise improves mucosal clearance in the small airways by releasing moderators that increase fluid secretion and stimulate cilia beat frequency. What’s more, PR increases lung strength and endurance which can help you perform the airway clearance techniques listed above.

Get More Restful Sleep
Getting restful sleep is a problem that many people face for their whole lives. According to the Sleep Association, around 50 to 70 million people suffer from a sleep disorder in the United States. So, as you can imagine, there is a lot of overlap between people suffering from COPD and people suffering from sleep disorders. If you’ve never been diagnosed with a sleep disorder or provided with treatment for your sleep disorder, now is the best time to seek help. Addressing your sleep problems will have undeniable benefits when it comes to helping you manage your COPD. If you’d like to learn more about getting restful sleep with COPD, please read through this article.

Conclusion
Airway clearance therapy is an incredibly important skill for all COPD patients to learn. However, it’s not an all-in-one solution. Drinking enough water, getting enough sleep, eating right, and exercising are all great ways to prevent airway obstruction and prevent the need for alternative therapies. If you’re experiencing frequent coughing or wheezing, we recommend contacting your pulmonologist immediately so that you can address your concerns.
Here at LPT Medical, we specialize in life-saving oxygen equipment which can help you maintain your oxygen levels if you are experiencing a coughing fit or COPD exacerbation. We will help you get the best deal on the market for portable oxygen concentrators like the Caire FreeStyle Comfort or the Inogen One G5. These devices are much lighter and reliable than traditional oxygen delivery devices allowing you to go more places without worrying about whether or not you’re getting enough oxygen. Since the oxygen is administered through a nasal cannula you can still do all of the airway clearance techniques above while you’re receiving oxygen.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
It’s very important to us that you receive the oxygen concentrator that’s right for you. When you reach out to us, you will be connected with a respiratory specialist who will ask you questions about your oxygen use and lifestyle. If cost is a concern for you, we also have a variety of different buying options including new, used, and refurbished concentrators. We also have financing options available if you’d like to pay in easy monthly installments. Reach out to us either by phone or email for more information.
Nowadays, we rely on our devices for just about everything. Cellphones, for example, are used for everything from making calls and sending text messages to tracking our fitness progress or staying connected with online communities. If you’ve been diagnosed with COPD or another chronic respiratory ailment, this reliance on technology doesn’t go away. In some cases, you might even be more dependent on technology than previously. This isn’t necessarily a bad thing though as long as you’re using devices that are reliable and match your lifestyle.
In this post, we’re going to take a look at seven of the most important devices you can own with chronic obstructive pulmonary disease (COPD). Whether you’ve just been diagnosed or you’ve been living with COPD for some time, these devices are considered to be essential by many or at the very least, incredibly convenient to have. If you have any questions, be sure to leave them in the comment section below, and don’t forget to bookmark our blog page so that you never miss our latest articles.
Portable Oxygen Concentrator
At one point or another, most COPD patients will need to use supplemental oxygen. When the lungs are impaired due to chronic inflammation, supplemental oxygen ensures that the oxygen levels in your blood are normal; and in turn, every organ in your body receives the oxygen it needs to function properly. Supplemental oxygen not only improves your longevity as a COPD patient, but it can also help you feel better in the moment. Oxygen therapy will reduce breathlessness, fatigue, and lightheadedness associated with low oxygen levels.

However, many people falter when it comes to actually choosing the oxygen device that they will use. Patients and healthcare providers often default to oxygen tanks or liquid oxygen tanks because they are cheap and thus have a low barrier of entry. However, when it comes to the patient’s long-term health and well-being, they often find that these oxygen devices are lacking in many ways. First and foremost, they have to be refilled once the oxygen in them is depleted. This can be costly and takes your time and attention away from more important things like spending time with friends and family.

Another problem with oxygen tanks is that they are heavy and bulky. Chances are, you’ve seen people walking around while lugging around a big green tank behind them. The reason these tanks are so big is that they contain compressed oxygen gas which takes up a lot of space. This problem is somewhat mitigated by using a tank that stores oxygen in its liquid form but this still has a lot of problems associated with it. In most cases, the best alternative is to use something called a portable oxygen concentrator.
Unlike oxygen tanks which limit your freedom and mobility, portable oxygen concentrators are designed for people who are on the go frequently and need something reliable. Rather than storing oxygen within the unit, POCs draw in ambient air and remove unnecessary gases, then put out medical-grade oxygen. POCs are electronic devices that run off of powerful lithium-ion batteries. In other words, you simply need access to either a wall or car outlet to charge the batteries, then you will be set for the rest of the day!
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Nebulizer
Another important device to own as a COPD patient is a nebulizer. What a nebulizer does is crush up your COPD medication into a fine mist called aerosol so that it can be inhaled more easily by the patient. This helps the medication reach your lungs faster and thus is faster-acting than medication that is taken orally. You should be sure to speak with your doctor to see if nebulizers are right for you.

Many people think of nebulizers as devices that they can only use at home, however, there’s been a sudden emergence of portable nebulizers that you can take with you if you go on a trip. Nebulizers differ from inhalers in that they put out a constant stream of aerosol whereas inhalers put out “puffs.” This is beneficial for people with severe COPD who may not be able to inhale deeply or sharply enough to bring the medication into their lungs. With a nebulizer, however, you can simply breathe naturally and be sure that the medication is reaching your lungs.

Much like portable oxygen concentrators, nebulizers are usually electronic devices that either run off of a battery or they need to be plugged into an electrical outlet. It should be noted that not all medications can be administered through a nebulizer. Most likely, your doctor will only have you use medication known as bronchodilators which open up your airways in the event of a COPD exacerbation. Bronchodilators include Pulmicort, Xopenex, albuterol, and more.
Pulse Oximeter
A pulse oximeter is a device that measures the level of oxygen saturation in your blood. Pulse oximeters are very small and lightweight and they’re the least invasive way to check whether you’re getting enough oxygen or not. One of the only other alternatives is arterial blood gas (ABG) analysis which requires your doctor to draw blood in order to determine your oxygen saturation level. While these readings are oftentimes more accurate than pulse oximetry they require you to be at the doctor’s office in order to get your results. Pulse oximeters can be used anywhere and anytime.
Pulse oximeters work by passing light through the finger and measuring the amount of light that comes out the other side. This determines the amount of oxygenated and deoxygenated blood cells and thus your blood oxygen saturation. Many people are surprised to find that these devices cost under $20. However, if you want a more advanced one that connects to your cellphone or smart device, it could run you over $100. Either way, this is something that all COPD patients should have so that they can ensure that they’re receiving enough oxygen. It can also help you determine whether your oxygen device is working properly.
High-Frequency Chest Wall Oscillation Vest
Mucus plays a very important role in the body. It coats the lining of your lungs and airways and if you inhale irritants or bacteria, the mucus traps it so that it can be cleared before it leads to an infection. Unfortunately, many COPD patients aren’t able to create an expiratory force great enough to clear mucus, and as a result, it becomes lodged in the airways. Years of smoking can also damage the cilia in the airways which are small cells that help pass the mucus out of the lungs. Most COPD patients are taught about airway clearance techniques but these can become very exhausting to do on a daily basis.

Alternatively, COPD patients can invest in something called a high-frequency chest wall oscillation vest. This looks just like a life jacket but it attaches to a machine that vibrates the vest at a high frequency. This causes the mucus in your chest to loosen, and after a few minutes, you can remove the vest and try a huff cough to expel the mucus. The main downside to these vests is that they can run you a pretty penny so it’s best to speak with your doctor before investing in one. What’s more, they aren’t very portable so you should plan to buy one for in-home use only.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Positive Expiratory Pressure Device
A positive expiratory pressure (PEP) device has a similar function to that of a high-frequency chest wall oscillation vest which we discussed above. However, the PEP device is much smaller and lighter so you can carry it in your purse, handbag, or pocket when you leave the house. With the PEP device, you will blow into a mouthpiece that creates air resistance. This air resistance will keep your airways open as you exhale meaning the mucus can move more freely without obstruction.

If you’ve ever tried the technique called pursed-lip breathing, you know what to expect with a PEP device. During pursed-lip breathing, you inhale deeply through your nose and then out through pursed lips. This helps to reduce chest tightness and get more air into your lungs. The PEP device makes this a little easier because you don’t have to control the amount of resistance so you can focus more on your breathing. PEP devices are also fairly cheap at around $30 to $50 apiece.
Mobility Devices
Words cannot express how important it is to maintain your mobility as you get older. Unfortunately, someone with COPD will likely begin to lose their mobility sooner than most due to reduced lung capacity, however, the good news is that there are plenty of mobility aids to keep you on your feet and moving. Probably one of the more popular mobility devices for people with respiratory ailments is a rollator. This is like a walker but it has wheels on the bottom and brakes so that you have better control. In the middle, there is a small platform where you can put your oxygen device your sit on if you get fatigued.

Another mobility aid that many COPD patients use is an electric scooter. These are best for people with very advanced lung disease who may not be able to walk more than a short distance on their own. Electric scooters offer a lot of storage room for your portable oxygen concentrator as well as personal belongings. However, the downside is that they need to be recharged after a certain amount of use and they are difficult to transport from place to place. Unless you have a caretaker who can help you out with these things, an electric scooter may not be the best option for you.

Last but certainly not least, there are in-home mobility devices like stairlifts. A stairlift is essentially an elevator designed for people who have trouble walking up and down the stairs. While these devices are very safe to use and can save you a lot of hassle, they are also pretty expensive because a professional will need to come to your home to install them. What’s more, they can wear out over time so you may need to call someone to have it repaired or replaced at some point.
Smartphone or Tablet
Most people have some type of smart device but for the few who do not, it’s worth upgrading, especially if you have COPD or another respiratory condition. Many portable oxygen concentrators like the Inogen One G5 and Caire FreeStyle Comfort make use of smartphone applications to enhance the user’s experience. These apps allow you to do things like track your oxygen usage, check the device user manual and even remotely check your oxygen flow and battery life.

There are many other applications that can make your life easier with COPD. For example, AirNow.gov has a mobile application that allows you to quickly and easily check the air quality in your area which is useful for planning trips. There are apps that can help you plan your diet and exercise routine with COPD as well. Be sure to check out this post where we take a look at some of the best mobile applications for COPD patients.
Conclusion
Being diagnosed with COPD can be life-changing. You’ll need to take steps to slow the progression of your disease like improving your diet, exercise routine, and taking regular trips to the doctor’s office. While this may seem overwhelming at first, it’s helpful to know that there are many resources at your disposal. Not least of which are devices like portable oxygen concentrators, nebulizers, and pulse oximeters. If you have any questions about what you read here, please don’t hesitate to leave a comment. If you’re on the market for a portable oxygen concentrator be sure to reach out to our respiratory specialists by phone or email.
Chronic obstructive pulmonary disease (COPD) is a term that categorizes a few chronic lung conditions: chronic bronchitis, refractory asthma, and emphysema all of these conditions restrict airflow in some way.
There are about 15.7 million people in the United States who have reported that they have been diagnosed with COPD. This is a progressive disease that gets worse overtime especially if the patient does not treat it properly.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Treating COPD is a lifelong journey comprised of doctors visits, respiratory tests, exercise, oxygen therapy, changing eating and drinking habits, and taking vitamins and supplements.
In this article we are going to focus on how COPD patients can develop a healthy eating habits and take vitamins and supplements in order to help ease the symptoms of COPD.
COPD Information
If you have COPD, it is likely that you find it increasingly difficult to breathe, and this can impact so many aspects of your life. The other symptoms you may experience are coughing, wheezing, excess mucus production, feeling of tightness in your chest, and fatigue.
COPD does not only affect your ability to breathe, but can cause a lot of other problems due to the lack of oxygen in your blood. Many COPD patients need supplemental oxygen therapy, and these patients have to use a device called a portable oxygen concentrator or an oxygen tank in order to get the right amount of oxygen. Oxygen will be prescribed to you if you need it.

In conjunction with your oxygen therapy, you can do a number of things to treat your respiratory condition, one of those treatments is eating healthy and getting the right amount of nutrition. If your diet doesn't give you the vitamins and nutrients you need, it could be helpful to take supplements and vitamins that would support any deficiencies you may have.
Nutrition and Eating Healthy for COPD

Nutrition is a crucial part of treating COPD, and oftentimes one of the hardest things to keep up with, vitamins and supplements can help you get the nutrients your diet is lacking or important vitamins that your body is craving.
Vitamins and minerals give you energy and stamina, and you get vitamins form food and water, if you are not eating the right foods, you may have vitamin deficiencies. If you have COPD, it is likely that you require 430–720 more calories per day than healthy people.
Calories are the fuel that gives your body energy to function. You can get healthy calories from grains, vegetables, fruits, proteins, and fats you eat. COPD patients often require these extra calories because of the added effort they need to breathe. Therefore, malnutrition is also something many people with COPD struggle with. Malnutrition can affect you for a long time, and can negatively impact your disease progression.
It is recommended that eating a high fat, low carbohydrate diet can help people with breathing problems.
Best Eating Habits for People with COPD

Building healthy eating habits is an essential part of treating your COPD. Many people with COPD do not have an appetite or have a hard time finding the energy to cook and eat, and therefore suffer from malnutrition. Follow these following tips to make eating easier.
- Try making food easier to chew, you can do this in a number of ways. When you are cooking vegetables, cook them fully until they are soft. You can mince or grind the meat down and make bowl styled dishes. You can also focus on eating foods that are already easy to chew like pasta, mashed potatoes, thick soups, creamed soups, and casseroles fruit smoothies.
- If you feel short of breath while you are eating you should try to rest 30 minutes before meals. Start practicing pursed-lips breathing and other breathing exercises daily that will improve your breathing endurance.
- While you eat, make sure your body is in a position to expand your lungs, try sitting upright and lean forward with your elbows on the table and keep your feet on the floor.
- Ask your healthcare provider, if you are using a pulse flow oxygen device or a continuous oxygen device, if you should increase your flow rate during meals but do not adjust your oxygen flow without talking with your doctor first.
- Eating and cooking can be exhausting for lung patients, to avoid fatigue, try the “Meals on Wheels” in your community or a similar service that will provide you with nutritious, low-cost meals. By using a service like this, you won’t have to prepare meals.
- Eating too much too often will make you feel tired, instead try eating six small meals each day instead of three big ones. This will also keep your metabolism from slowing you down. The key to maintaining energy throughout the day is to conserve oxygen, and digestion takes up your energy and therefore takes up your valuable oxygen. If you eat smaller meals, you use less oxygen.
- If you enjoy cooking, try to find easy-to-make recipes, and if you don’t enjoy cooking as much, ask family or friends to help with making meals. Even though sugar can sometimes give you a small burst of energy, sweets, cookies, cakes, and other deserts, also known as simple carbohydrates will hold carbon dioxide inside of you causing tiredness.

- Bloating is extremely uncomfortable for lung patients because your stomach is pushing on your diaphragm making it even more difficult to breathe. To avoid this bloating feeling, do not rush your meals, and no not eat when you are short of breath, by doing so, you can simultaneously swallow air making your bloating worse.
- Spread out the amount of fluids you drink, and try drinking one hour before and one hour after a meal in order to decrease the amount of stuff in the stomach at one time.
- Onions, cabbage, sauerkraut, broccoli, Brussels sprouts, and beer all cause bloating, so try to avoid these foods when you can. Fried, fatty food and other high-fat foods are hard to digest and can only be processed in your body very slowly slowly, causing a feeling of bloating.
- Lactose may cause bloating, if you feel bloated after eating or drinking milk, yogurt, cottage cheese, or other dairy products, try avoiding dairy.
- By adding lots of fiber and fluid to your diet you can avoid constipation and bloating.
Supplements and Vitamins

Beyond developing a healthy respiratory diet that works to mitigate your COPD symptoms and helps give you energy, there are also many different supplements and vitamins that you can try to support your medical treatment and help manage your symptoms.
Various vitamins (vitamin C, D, E, A, beta and alpha carotene) can help improve COPD symptoms, exacerbations and pulmonary function and high vitamin intake would probably reduce the annual decline of FEV1.
Vitamins you Need if you Have COPD

COPD flares or exacerbations are episodes of escalated symptoms. When you experience a flare up, you may need to use your rescue inhaler or medication, increase the oxygen output on your portable oxygen concentrator if your doctor recommends it, and in some cases seek emergency medical attention.
In order to avoid COPD exacerbations all together you can do a number of things:
- Take your oxygen as prescribed everyday
- Practice breathing exercises to increase your endurance
- Avoid allergens
- Avoid chemicals and harsh cleaning product
- Avoid bad air quality, and get a home air purifier
- Exercise regularly
- Eat a respiratory friendly diet as mentioned in the beginning on this blog
- Take supplements and vitamins that are good for your health
LPT medical has a COPD resource center on our website where you can go to find information regarding all of these actions you can take to avoid COPD exacerbations and how to take the best care of your condition.

Continue reading this blog for information about how certain supplements can help improve your condition.
Vitamin D
Research shows that many people with COPD also have very low vitamin D, therefore taking vitamin D supplements can help your lungs function better.
The main reason people with COPD can have Vitamin D deficiencies is due to the lack of sun contact, resulting in lack of vitamin D production in skin.
Taking vitamin D-3 supplements for COPD can help protect you from experiencing moderate or severe flare-ups.
Vitamin C
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Research shows that having low levels of vitamin C can lead to symptoms like shortness of breath, mucus, and wheezing, all of which are already symptoms of COPD, and avoiding excess
Vitamin E

Vitamin E is important for your vision, reproduction, your blood, brain and skin.
Studies have shown that long-term use of Vitamin E can help prevent COPD because it has antioxidant properties, which may protect your cells against the effects molecules that are produced when your body is exposed to tobacco smoke and radiation.
If you experience consistent flare-ups of COPD, it is likely that you have lower levels of vitamin E than normal. Taking a vitamin E supplement can help your body get back to normal vitamin E levels.
Vitamin A

Vitamin A is crucial to the functioning of your immune system and plays a vital role in your cells to growth. Taking Vitamin A supplements may help you lungs function at a high capacity if you have a vitamin A deficiency.
Magnesium
Some COPD medications can interfere with your body’s ability to absorb magnesium, this can be harmful for COPD patients because magnesium supports lung function. Taking a magnesium supplement could cause side effects. If you do take magnesium supplements be sure to monitor yourself carefully.
Calcium

There are some COPD medications that may cause you to lose calcium and calcium can help your lungs function. You should try to intake more calcium-rich foods in your diet and if you are still unable to reach your calcium requirements, it may be necessary to take a calcium supplement.
Omega-3 fatty acids

Omega-3 fatty acids can reduce the inflammation in your lungs from COPD. You can eat more fish, seeds, and nuts, to get Omega-3 fatty acids, but you can also take fish oil supplements to make sure that you are getting enough.
Overview
COPD is a chronic illness, and there is no cure, however you can treat your disease. If you maintain a strict COPD treatment regimen you can regulate you symptoms. By taking your medication, adhering to your oxygen prescription, eating healthy and getting the nutrients you body needs you can slow down the progression of your COPD.
If you have issues eating, and find it hard to maintain a healthy diet, we hope that you found some of the ideas listed in this article that will help you get the nutrients you need in order to help relieve your COPD symptoms.
If you have COPD it is likely that your body is lacking in vitamins you needs, and if you are experiencing certain signs of vitamin deficiencies, you should speak with your doctor about taking specific supplements.
Getting the right amount of nutrients and taking supplements can help you better manage you COPD symptoms and helps you body function optimally.
If you learned anything in this blog, or feel as though someone in you life could benefit from any of this information, please leave a comment or share this blog with your friends and family!
Supplemental oxygen therapy, or simply oxygen therapy, is a treatment that has been around since the late 1800s. It was primarily used to treat the symptoms of pneumonia, but doctors were uncertain how much to administer, how long to keep patients on oxygen, and if there were any serious side-effects. It wasn’t until the late 1900s that there was a significant amount of research on the use of medical oxygen and doctors became more aware of how to use it.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
But the usage of medical oxygen is not the only thing that developed over this time. There were also a number of scientific advancements that revolutionized the way oxygen was administered. For example, the invention of the lithium-ion battery in 1991 made it possible for oxygen manufacturers to produce extremely small, lightweight, and powerful oxygen devices called portable oxygen concentrators. These devices replaced the heavy and bulky oxygen tanks that came before them.
In this post, we’re going to help you understand supplemental oxygen better by outlining some of the conditions that may require its use. Remember that oxygen is a controlled substance in the United States, so if you believe you may need it for medical purposes, you’ll need to get a prescription from your doctor first. If you have one of the following conditions, reach out to your doctor to find out what your oxygen requirements are. Then you can look into the various oxygen devices on the market.
Chronic Obstructive Pulmonary Disease (COPD)
COPD is probably the first condition you think of when you hear the words “supplemental oxygen.” Not only because most COPD patients are on oxygen, but because COPD is one of the most common chronic respiratory conditions in the world. According to the Centers for Disease Control and Prevention (CDC), there are around 16 million people with COPD in the United States alone. Worldwide, there are more than 65 million people with COPD.

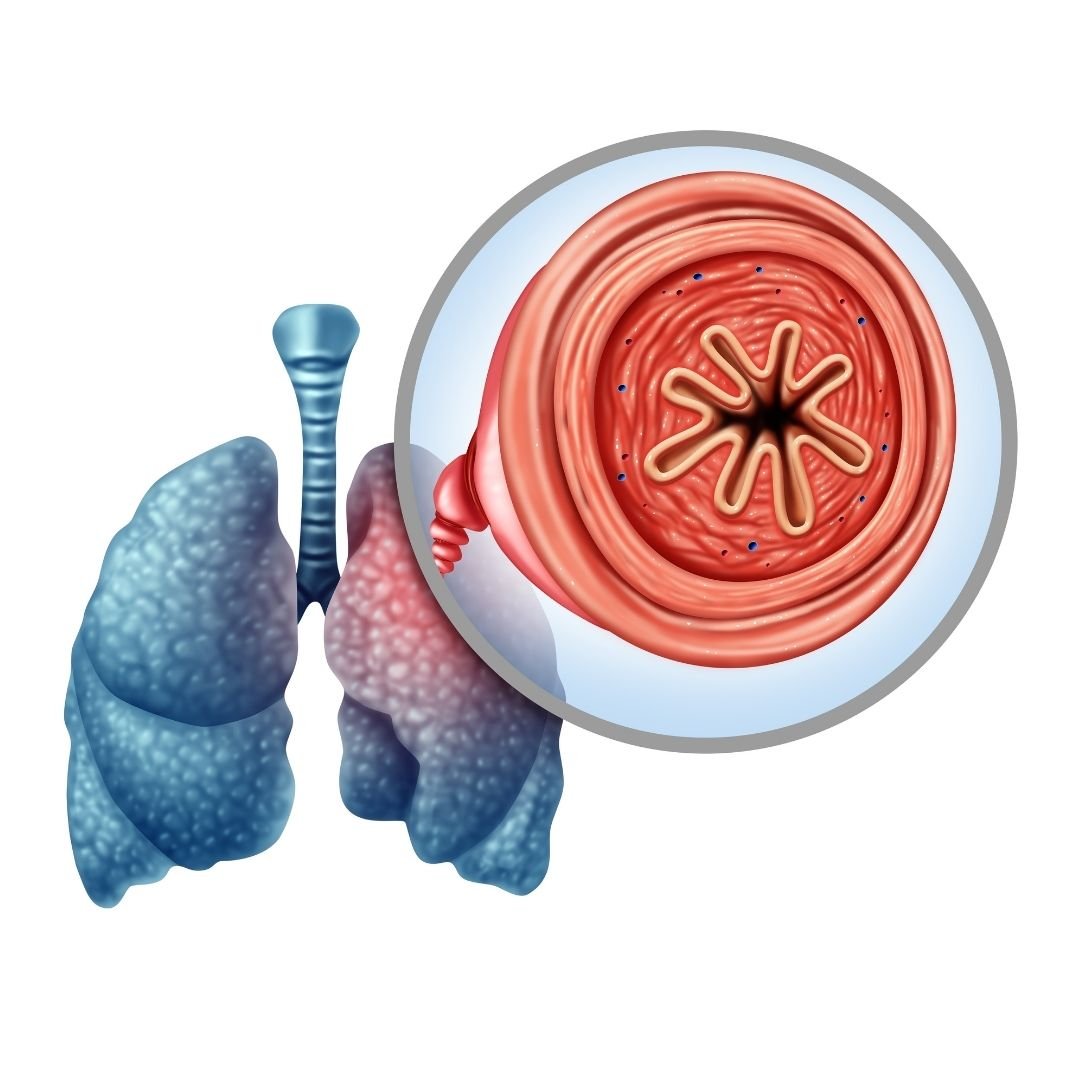
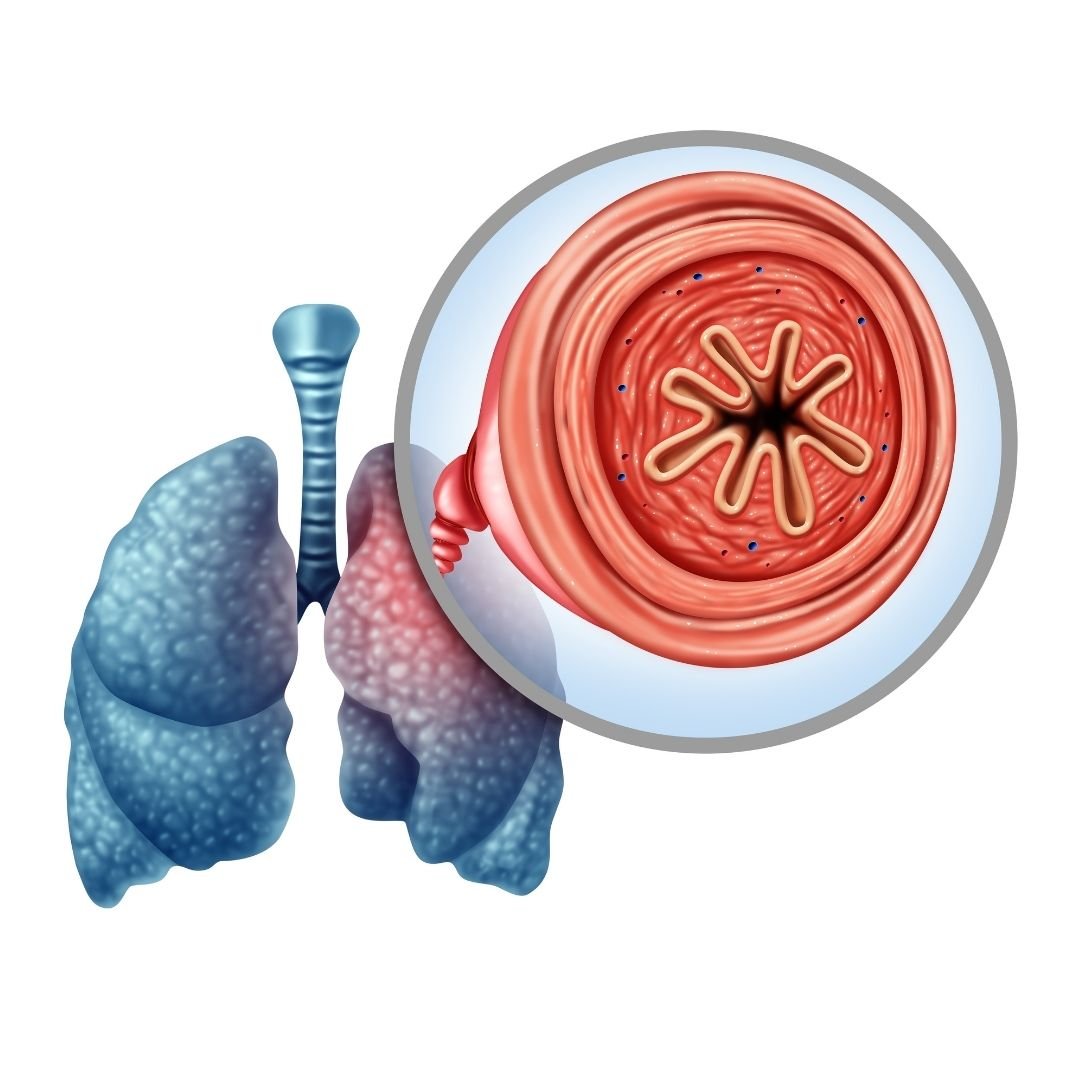
COPD is actually an umbrella term that denotes two separate but similar diseases: chronic bronchitis and emphysema. The former is a disease that affects the airways leading to the lungs called bronchioles. These airways become inflamed and hardened making it difficult to breathe and to clear mucus out of the lungs and throat. Trapped mucus can lead to frequent and recurring lung infections. Chronic bronchitis differs from acute bronchitis in that the damage is permanent and irreversible.
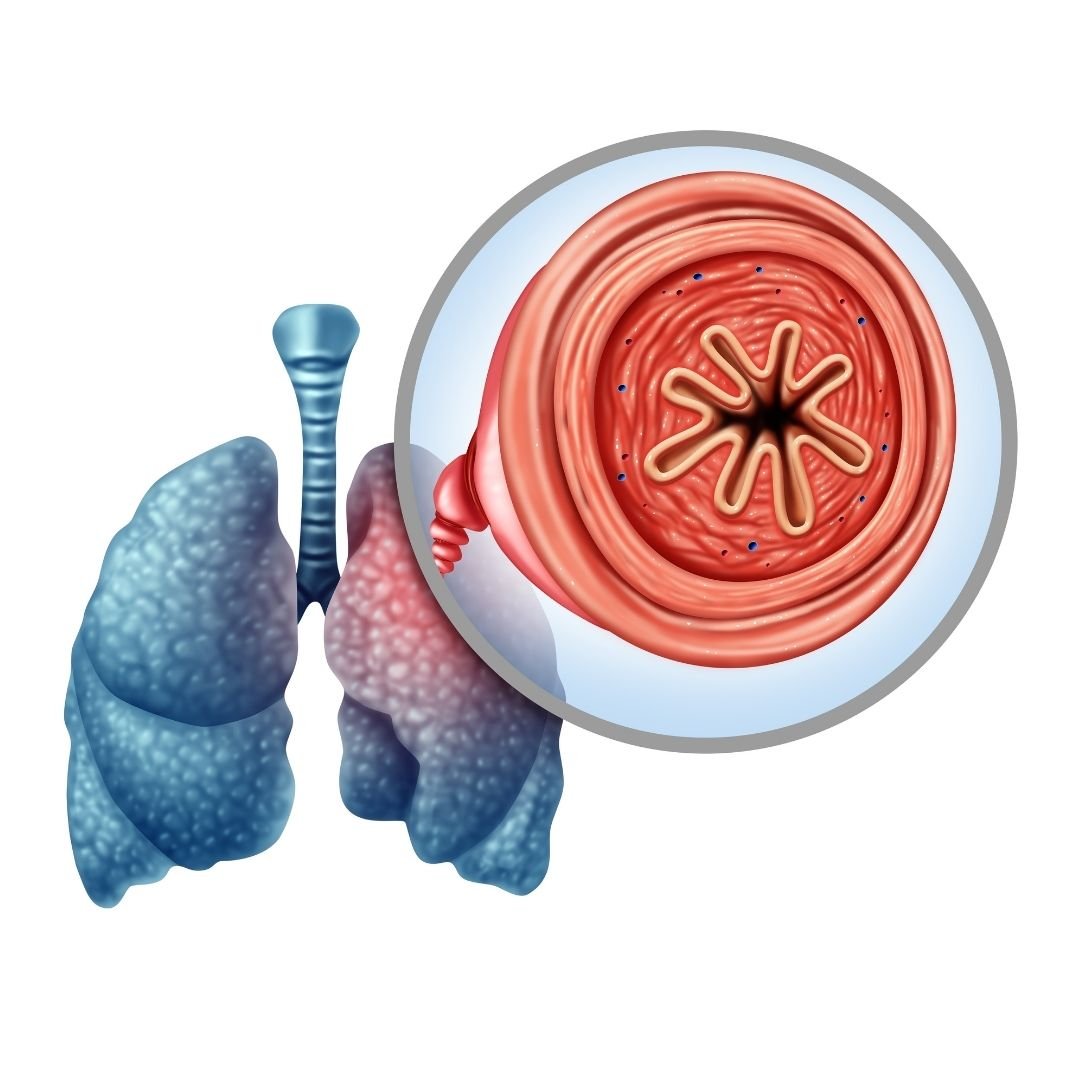
Emphysema, the other condition under the COPD umbrella, is characterized by damage to the alveoli. These are the tiny air sacs in the lungs where the exchange of oxygen and carbon dioxide takes place. When lung damage occurs, usually due to cigarette smoking or the inhalation of air pollution, the alveoli begin to swell and fill with fluid. This makes the lungs much less efficient at transferring oxygen to the blood and the lungs also become less elastic meaning it’s physically harder to breathe.
When is Supplemental Oxygen Needed?
COPD is a disease that develops slowly over the course of many years. In fact, the disease is divided into four different stages, each marked by progressively worsening symptoms. Stage one COPD is very mild and may even go unnoticed by the patient. Many people ignore the signs of stage one COPD because they simply view it as a sign of aging. According to COPD.net, it’s estimated that about 12 million people have COPD that has not been diagnosed. Most of whom are in stage one COPD.

What this means in terms of supplemental oxygen is that most people will not need it during the early stages of the disease. However, as your symptoms progress, you’ll need to communicate closely with your doctor so that he or she knows when it’s best for you to begin oxygen therapy. Before giving you a prescription for oxygen, your doctor will likely perform a test called an arterial blood gas analysis (ABG test). This test will tell you and your doctor the amount of oxygen and carbon dioxide in your blood so that you can determine if supplemental oxygen will benefit you or not.

Since arterial blood gas analysis requires you to draw blood, there is another less invasive option called pulse oximetry. A pulse oximeter is a small device that slips over your finger. It passes rays of light through your finger in order to approximate your blood oxygen saturation levels. While these tend to be less accurate than ABG tests, they can be extremely convenient, especially for checking your oxygen levels at home without the help of a doctor.
Cystic Fibrosis (CF)
Cystic fibrosis is a disease that’s characterized primarily by damage to the lungs and digestive system. It’s a hereditary condition meaning that it’s passed on from parents to their offspring. Around 75 percent of people diagnosed with CF are diagnosed under the age of two. This is in stark contrast to COPD where most cases are diagnosed in patients over the age of 40. According to Medical News Today, all newborns in the United States are screened for cystic fibrosis.
Cystic fibrosis patients have a mutation in the gene that creates the cystic fibrosis transmembrane conductance regulator (CFTR). This is a protein that helps regulate fluids and salt throughout the body. This is why CF patients often struggle with overproduction of mucus and sweat inside and outside their body which can lead to blockages and frequent infections, especially in the lungs and the digestive tract. Like COPD, CF is a progressive disease meaning there is no cure and will likely get worse without effective treatment.
When is Supplemental Oxygen Needed?
Supplemental oxygen therapy is a very common treatment option for cystic fibrosis patients. Unfortunately, since cystic fibrosis is so rare, there are far fewer studies to go off of when determining if supplemental oxygen is right for each patient. However, clinical trials have shown that oxygen therapy can stabilize CF and allow patients to sleep better, exercise effectively, and maintain an otherwise normal life. But since CF causes thick mucus, treating this disease is usually focused on reversing these effects. So, mucus thinners are usually the most important treatment option for CF patients.
.png)
Supplemental oxygen can be prescribed for either short- or long-term use in cystic fibrosis. If the patient is experiencing chronic low blood oxygen levels, you might be required to use oxygen for several hours a day or more. On the other hand, if your low blood oxygen levels are intermittent and caused by things like flare-ups you might be prescribed the use of oxygen only when your respiratory symptoms are elevated.
Pulmonary Fibrosis (PF)
Pulmonary fibrosis is a condition that is commonly confused with chronic obstructive pulmonary disease, but they are not the same thing. While they certainly exhibit some of the same symptoms, they differ greatly in terms of what causes them, the type of damage that’s done to the lungs, and the long-term outlook for patients. Like the name suggests, COPD is an “obstructive” disease. This means that it impairs your ability to expel air from the lungs. Pulmonary fibrosis, on the other hand, is a restrictive lung disease meaning it prevents the lungs from fully expanding.
Another difference between the two is that COPD results in inflammation in the lungs due to exposure to cigarette smoke whereas pulmonary fibrosis is characterized by fibrosis or “scar tissue” in the lungs from years of exposure to pollution. In COPD, the airways become narrowed preventing you from expelling air and leading to a buildup of carbon dioxide in the blood. In pulmonary fibrosis, the lungs themselves may be stiff or too weak to inhale and exhale fully. On the surface, these things are indistinguishable, but there are some significant differences in the way they are treated.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Whereas COPD is mainly caused by cigarette smoking or alpha-1 antitrypsin deficiency, there are many potential causes of pulmonary fibrosis. Idiopathic pulmonary fibrosis (IPF) is the most common type. The term “idiopathic” simply means that the disease developed with no known cause. IPF is most common among people between the ages of 50 and 70. Pulmonary can be caused by other diseases, most commonly autoimmune diseases like rheumatoid arthritis, Sjogren’s syndrome, or scleroderma. Gastroesophageal reflux disease (GERD) and viral infections can also lead to an increased risk of contracting pulmonary fibrosis.
There is also a genetic component to cystic fibrosis. Studies have shown that genes play a role in determining whether someone contracts pulmonary fibrosis. But more research is needed to say exactly how it contributes. Pulmonary fibrosis that is believed to have genetic cause is referred to as “familial PF.”
![]()
Lastly, pulmonary fibrosis can be caused by exposure to hazardous materials. Occupational hazards like silica and asbestos are most likely to cause PF. It can also be caused by radiation treatments and certain types of medications. Cigarette smoking is not a cause of pulmonary fibrosis but it can be a risk factor meaning it makes someone more likely to contract pulmonary fibrosis.
When is Supplemental Oxygen Needed?
As you can imagine, prescribing supplemental oxygen for pulmonary fibrosis can be a little more challenging than with other conditions. There are many different causes of fibrosis in the lungs so it’s more difficult to determine if additional oxygen is needed. Regardless, supplemental oxygen is still widely in use by people with pulmonary fibrosis and many people say that it helps them live an active lifestyle and feel better in their day-to-day lives.

According to UCSF Health, pulmonary fibrosis patients need oxygen when their saturation falls below 89 percent or arterial oxygen pressure falls below 60 mmHg. This is regardless of whether the patient is at rest, active, or asleep. Oxygen is a vital resource for your body and it’s used by every organ in the body so maintaining the proper oxygen levels in the blood at all times can go a long way towards preventing pulmonary fibrosis symptoms.
Severe Asthma
Asthma is the world’s most common respiratory condition. According to the Asthma and Allergy Foundation of America, 7.7 percent of American adults and 8.4 percent of American children have it. The number of people who have it has also been increasing since the 1980s likely due to an increase in environmental pollutions like airborne pollens, car pollution, and even changes in the climate.
Asthma is a condition where a patient’s airways become narrowed, inflamed, and filled with mucus which makes it difficult to breathe as well as causing chest pain and fatigue. While COPD and asthma attacks are very similar events, the main difference between the two is that asthma is not a progressive disease so the airways typically go back to normal after an attack rather than becoming increasingly more inflamed like they would in a COPD patient. Asthma is also not caused by smoking, however, it is a risk factor.
-jpg.jpeg)
The good news when it comes to asthma is that only about 5 to 10 percent of cases are severe and life-threatening. The majority of asthma patients find themselves limited in their exercise ability and they might experience more frequent and severe allergic reactions, especially to seasonal allergies. But most people with asthma are able to live normal lives without a major reduction in their life expectancy.
When is Supplemental Oxygen Needed
Unlike with the other conditions listed above, supplemental oxygen is really only prescribed in rare cases of asthma. In chronic bronchitis, the airways are always inflamed and damaged and in emphysema, the lungs are always inflamed, so this explains why many COPD patients need to be on oxygen 24 hours a day. However, in asthma, the airways are mostly healthy when the patient is not experiencing an asthma attack.

Generally, rescue inhalers and nebulizers are used to treat asthma attacks. These medications are designed to open up the airways and reduce inflammation so that the patient can breathe normally. However, there is a type of asthma attack often referred to as “acute severe asthma” or a “severe asthma exacerbation” where supplemental oxygen is almost certainly needed. These types of asthma attacks do not react the same way to traditional asthma medications like bronchodilators so patients need to receive supplemental oxygen in order to maintain healthy blood oxygen saturation.
Congestive Heart Failure
Congestive heart failure, also known as heart failure, is a disease where your heart doesn’t pump blood in the way that it should. This is usually brought on by a number of conditions such as narrowed heart arteries (coronary artery disease) or high blood pressure. What results in your heart muscle being too weak or stiff to pump blood as effectively as it did when you were healthy. According to the Cleveland Clinic, heart failure is the leading cause of hospitalization in people 65 years and older.

Just like your lungs, your heart plays an important role in your systemic health. When your body isn’t able to pump blood effectively, other areas of your body may suffer just as greatly. Edema is one sign that you’re experiencing heart failure. This is when your extremities such as your hands, feet, or legs begin to fill with fluid, usually turning a purple color. And while edema on its own is not usually a serious problem, it’s a sign that you could be suffering from heart failure or some other heart-related problem.
Another area of the body that’s affected by your heart health is your lungs. This is because your heart and lungs work together to circulate oxygen-rich blood throughout your body. When your heart is unable to circulate blood properly it can lead to symptoms like shortness of breath, problems exercising, and chronic fatigue. This is often caused by either congestion in the lungs or a lack of oxygen in the tissues throughout your body which can make you feel tired and weak. You might also experience dizziness, confusion, or problems concentrating.
When is Supplemental Oxygen Needed?
Since congestive heart failure is a disease that affects the heart, it’s hard to compare to the other diseases on this list which are all lung diseases. However, despite this fact, congestive heart failure still sometimes requires the use of supplemental oxygen. More often than not, your doctor will prescribe you with supplemental oxygen when your heart failure causes low levels of oxygen in your blood. According to Web MD, you’re less likely to be prescribed oxygen if you just have mild symptoms because too much oxygen can be very dangerous in heart failure patients.

All things considered, supplemental oxygen is not a cure-all when it comes to heart disease. In reality, it won’t do a lot to help you manage heart disease symptoms. What it aims to do is prevent collateral issues caused by heart disease. In other words, it prevents further damage from being done to your body.
Conclusion
Supplemental oxygen therapy is a treatment with a long history. It’s been used for hundreds of years to help pneumonia patients manage their symptoms and over the years, researchers have discovered many other conditions that can benefit from supplemental oxygen. If you have one of the conditions listed above, it may be worth asking your doctor if you could benefit from using supplemental oxygen.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
If your doctor prescribes you supplemental oxygen, you’re going to need an oxygen device that’s right for you and your needs. Here at LPT Medical, we have a wide selection of stationary oxygen concentrators, portable continuous flow oxygen concentrators, and portable pulse dose oxygen concentrators. These devices are significantly less bulky and heavy than traditional oxygen delivery methods such as oxygen tanks and liquid oxygen tanks, but they provide you the same medical-grade oxygen. Feel free to reach out to us either by email or by phone to speak with an oxygen concentrator specialist.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!












