.png)
No matter what stage of life you are in, it’s always a good idea to find new ways to save money. If you’re someone with chronic obstructive pulmonary disease (COPD) or a similar lung disease, one of the best ways you can cut costs is by looking for ways to save money on medication, medical equipment, and other medical expenses. This study found that the average annual healthcare cost per COPD patient is around $4,147 and that increased disease severity is associated with higher healthcare costs.
Unfortunately, many people find that it’s not as easy as they thought it would be to save money on medical expenses. While there are many ways to save on medications, things like doctor’s visits, hospital visits, and pulmonary rehabilitation are pretty set in stone. And trying to avoid these things all together to save money could put your long-term health at risk. Be sure to visit a medical specialist whenever you need to, and find other ways to save such as on your medical oxygen equipment.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
If you’re just getting started with oxygen therapy, it might not be immediately evident how many options you have available to you and that just a few considerations could save you hundreds, if not thousands of dollars when it comes to purchasing and maintaining your oxygen device. In this post, we are going to highlight some tips for getting the best deal on an oxygen concentrator and avoiding some of the common pitfalls many people experience as a first-time oxygen buyer. If you have any questions, be sure to leave them in the comments or reach out to us by phone or email.
Find the Right Retailer to Buy From
By far the most important thing to remember if you’re looking for a good deal on an oxygen concentrator is to find a reputable retailer to buy from. The internet has made it easier than ever before to find the exact product you’re looking for and have it delivered on your porch within a matter of days. However, the internet has also opened the door for scammers and dishonest companies to get your money. This is why it’s so important to be prudent when it comes to the company that you work with.
![]()
Possibly the biggest scam you should be aware of when buying oxygen is companies that don’t ask to see your supplemental oxygen prescription. In the United States, oxygen is a “controlled substance” meaning it can’t simply be bought and sold freely without proof of medical necessity. If a company sells you oxygen without having you provide a prescription from your doctor, they are either doing so illegally, or they’re selling you low grade oxygen that will not meet your medical needs. Either way, these are deceptive business practices and they could be deceiving you in other ways as well.
Another thing to watch out for is something called “recreational oxygen.” This is not necessarily a scam or deceptive but it can lead to confusion when you’re trying to buy an oxygen concentrator to treat your COPD. Essentially, recreational oxygen is a type of low-grade oxygen used by hikers, climbers, or people traveling to higher altitudes than they’re used to. Allegedly, using these cylinders periodically can help you prevent breathlessness and altitude sickness, but there is little evidence to suggest this is the case. The important thing to remember is that “recreational” oxygen does not equate to “medical” oxygen.
.png)
Ultimately, the reason you should focus on finding a reputable oxygen retailer to work with is because purchasing the wrong device will set you back even further financially. Many people are ecstatic to find an oxygen device for a couple hundred dollars only to find out that it’s not going to meet their medical needs and that the company they bought it from doesn’t accept returns. Aside from breaking the bank, buying an oxygen device from a shady company can compromise your health and leave you without oxygen when you need it the most.
Decide Between New, Used, and Refurbished
Another way to get a great deal on an oxygen concentrator is to consider different buying options like new, used, and refurbished units. We wrote a post discussing all of the different buying options for portable oxygen concentrators in a different post, so be sure to check it out for more information. However, we’ll summarize the main points here for your convenience.
A “new” oxygen concentrator is one that has never been opened, turned on, or used in any way since it was manufactured. The obvious benefit to having a new concentrator is that the unit has no wear and tear and that you can expect it to last many years without needing repairs. What’s more, most new concentrators come with a manufacturer warranty which will cover you for several years if anything is wrong with the unit. Although rare, manufacturing defects are a possibility, so having the warranty will guarantee you repairs or a full replacement if your unit doesn’t work.

A “used” oxygen concentrator is one that has been owned by another oxygen patient in the past. The great news though is that “used” doesn’t mean that the unit is old and worn out. Some oxygen patients never use a unit or it is only lightly used before returning it. What this means is that you’ll be paying a discounted price on an item that is in “near mint” condition. When you purchase a concentrator from LPT Medical, you can rest assured that it’s been tested beforehand to ensure full functionality.
A “refurbished” portable oxygen concentrator differs slightly from a used unit in that repairs or replacements have been done to it. One of the common part replacements you’ll see in a refurbished oxygen concentrator are the sieve beds. These are specialized filters that remove unwanted gas from the air, allowing you to receive medical-grade oxygen. Over time, sieve beds can become worn out and need to be replaced.

One final option for you to get your hands on an oxygen concentrator is through renting one. This is not always the most practical option, but if you know you will only be needing one for a few days or weeks, it may be your most cost-effective option. Renting an oxygen concentrator is ideal for people who typically use an oxygen tank or stationary concentrator at home, but want to be able to go on a trip without having to hassle with lugging their tank around or finding a place to refill it.
Overall, there are benefits to each of the buying options, it’s just a matter of your individual situation. Be sure to ask our oxygen concentrator specialists here at LPT Medical if you have any questions or concerns.
Take Advantage of Package Deals
Package deals are one of the best ways to save money on an oxygen concentrator. A package deal is when you buy accessories alongside your oxygen concentrator unit and get a discount on your final price. This means you’ll be able to save a lot of money if you buy everything up front rather than buying each accessory separately. Package deals are not always going on, so be sure to talk with your oxygen concentrator specialist who can let you know what’s available.

One package deal many people enjoy is one that offers a carrying case, battery, and DC charging cable. This way, you will have the ultimate freedom to move around the minute you receive your oxygen concentrator instead of having to order additional accessories later on down the road. Most oxygen concentrators come with the standard size battery but if you think you will need a battery that lasts longer, you can always upgrade it and maybe even get some additional savings that way.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Another reason to take advantage of package deals is that it could help you save money on shipping. With very few exceptions, it’s almost always cheaper to ship everything in one box rather than individually. While it may not seem like that much extra to ship a couple of accessories, the costs can really start to add up.
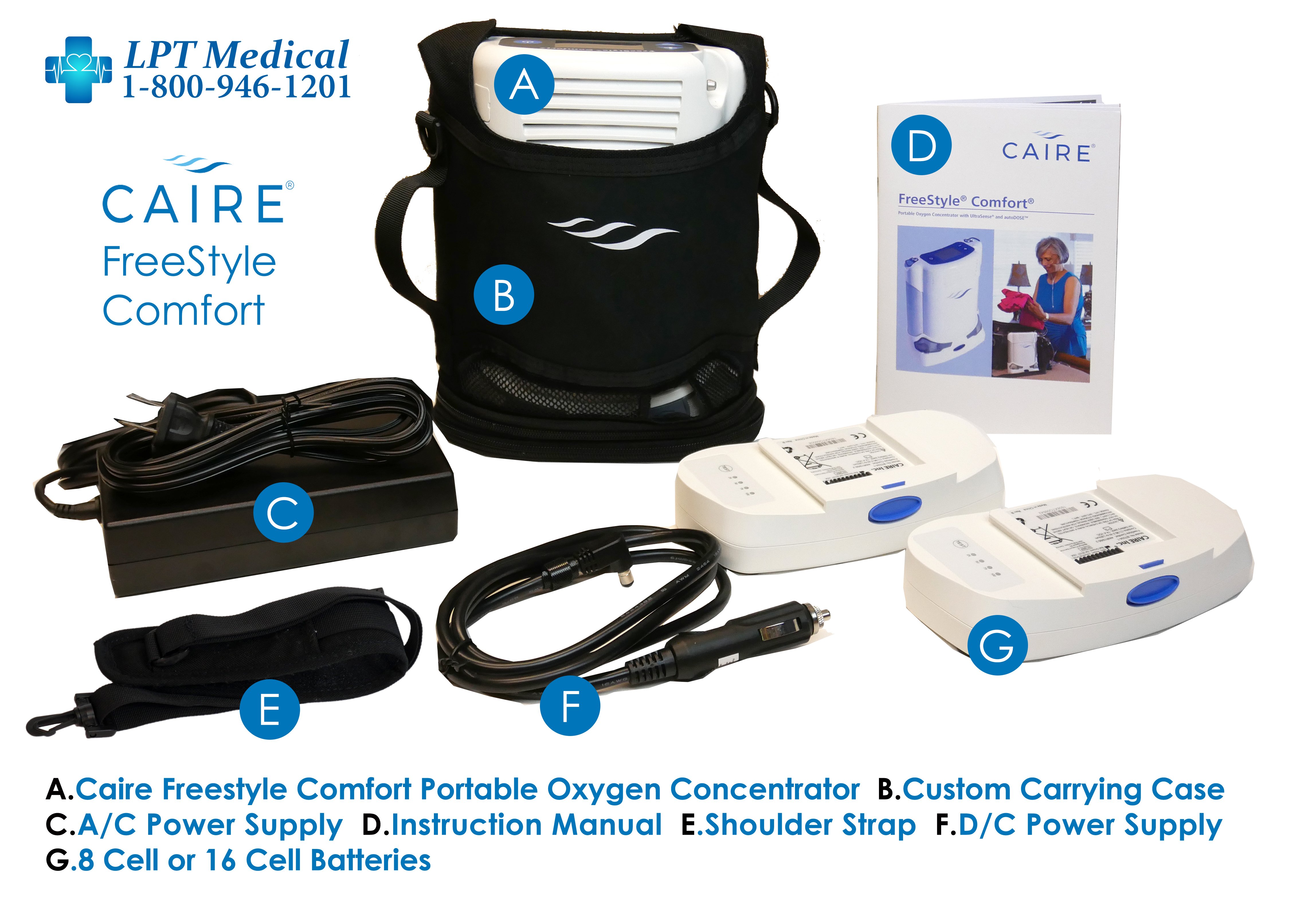
Two package deals we highly recommend are the Caire FreeStyle Comfort package and the Inogen One G5 package. These are some of the top-performing concentrators currently on the market, and when you consider everything that comes with them, you’ll see why they’re so popular. Just the base packages include an 8-cell battery, AC and DC charging cables so that you can charge your device anywhere, a carrying case, oxygen tubing, and a 3-year manufacturer warranty. Speak with one of our oxygen concentrator experts to see which one of these would be best for you.
Take Advantage of Sales
Sales are another thing you should keep an eye out for when you’re shopping for a portable oxygen concentrator. We offer a lot of oxygen concentrator sales here at LPT Medical because we want to get these devices to as many COPD patients as possible, even people who are on a tight budget. Currently, we are running a deal where you can get a free online pulmonary workshop course with the purchase of a new portable oxygen concentrator.
.jpg)
This program is called Thrive eLearning and it provides access to one-on-one counseling, support groups, and online courses that help you slow the progression of COPD. One of the important things you’ll learn during this course is breathing exercises which are a powerful tool for alleviating symptoms of breathlessness, fatigue, and chest pain which are commonly associated with COPD. You’ll also be able to connect one-on-one with doctors, caretakers, and other healthcare professionals, saving you time and money.

Sales are pretty common in the oxygen industry because the market is always changing. For example, we might offer a sale on one concentrator because a newer concentrator has hit the market. This is the perfect opportunity to get a great deal on a slightly older unit that still meets your needs perfectly. One of the best ways to keep up with these sales is to join our mailing list by filling out the form at the side of the page. You’ll be notified immediately whenever we have a new promotion going on!
Consider Your Financing Options
“Financing” an oxygen concentrator means splitting the payments up into more manageable monthly payments. While financing typically doesn’t save you money in the long run, it does lead to more financial security, because you won’t see the full cost of the concentrator come out of your bank account all at once. If at any time, you decide you want to pay off the rest of the concentrator all at once, you can do so without incurring any additional fees. Before committing to the financing terms, however, you should make sure that the company doesn’t charge a bunch of interest on top of the original price. Make sure you know what the exact amount of interest is and not just the monthly payments.

Conclusion
Oxygen concentrators are the ideal oxygen therapy device for most COPD patients. They’re very lightweight, compact, versatile, and most importantly, they provide you with medical-grade oxygen that you need to stay healthy. But if you want to get the best deal on an oxygen concentrator, you need to make several considerations first. Most importantly, you need to work with an oxygen concentrator retailer that you can rely on.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Here at LPT Medical, we take your oxygen needs seriously, and as such, we will take the time and diligence to understand both your medical and financial needs, then use our knowledge of the industry to align you with the perfect concentrator for you. It’s our goal to get an oxygen concentrator in the hands of any and all COPD patients who need them, so we will work with you to provide you with the best deal and we’ll even work with your healthcare provider to ensure you have all the necessary paperwork to buy an oxygen concentrator legally.
To get started, simply give us a call or shoot us an email.

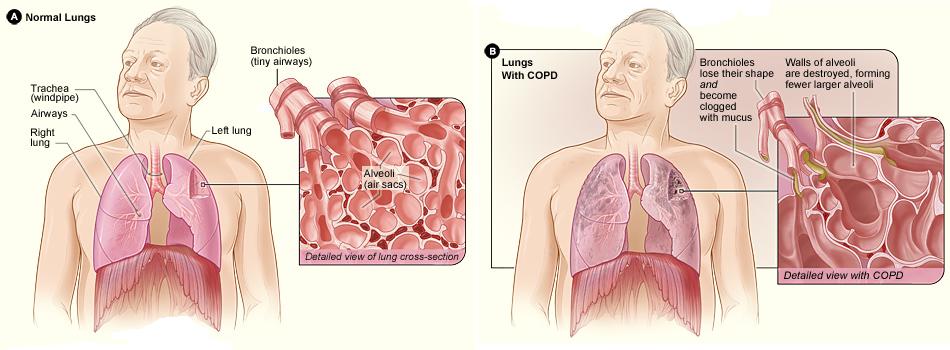
There are five big respiratory diseases that are the most common causes of severe illness and death worldwide- COPD, asthma, acute lower respiratory tract infections, tuberculosis and lung cancer. There are other forms of lung disease that also impact large populations around the world like occupational lung disease, pulmonary hypertension, sleep apnea, pulmonary embolism.
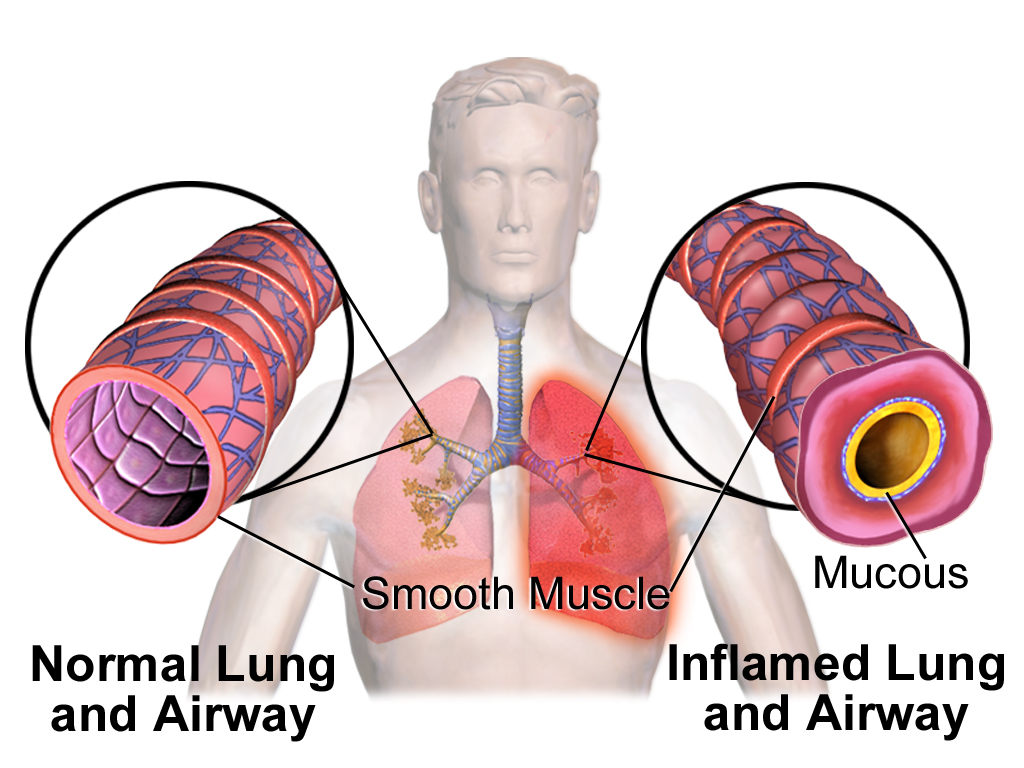
Chronic obstructive pulmonary disease, or COPD affects 16.4 million adults and accounts for two main groups of lung diseases, emphysema and chronic bronchitis, each contributes to the obstruction of air flow that interferes with a patient’s normal breathing.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
If you have been diagnosed with COPD, understand that your condition will worsen over time. However, you can take the necessary treatment that can improve your quality of life and slow down the progression of your disease and you can do so by overcoming hardships and challenges that your disease will inevitably present you. Its called a fight for a reason!
Early and accurate diagnosis of COPD is a huge factor in treating your disease, this may seem obvious, how can you treat a disease if you don’t know that you have it? But it is not that simple, inaccurate diagnosis of COPD happens all of the time, and it is important that you and your doctor are aware of the signs of COPD so you can catch it early on!
Testing for COPD
Doctors should use spirometry for the diagnosis of COPD according to a GOLD report that was released in 2020. This test is helpful in avoiding misdiagnosis and determining the severity or stage of your COPD.
When diagnosing COPD, a doctor is looking at things like:
- Symptoms
- Severity of airflow limitation
- History of exacerbations
- Presence of other health conditions
Looking Out for Early Signs of COPD

Looking out for COPD symptoms is not the easiest way to prevent COPD because oftentimes symptoms don't appear until lung damage has already occurred to the point of no return. The best way to look out for yourself and avoid getting COPD or at least be sure that you are slowing the progression of the disease if you already have it, is to reduce and eliminate your exposure to respiratory irritates, number one being cigarette smoke. Quit smoking!
If you have COPD you’ll start to notices signs and symptoms of COPD like:
- Shortness of breath, especially during physical activities
- Wheezing
- Chest tightness
- Chronic cough
- Excess production of mucus that may be clear, white, yellow or greenish
- Frequent respiratory infections
- Lack of energy
- Unintended weight loss (if your disease has progressed into more severe stages)
- Swelling in areas of your legs
All of these COPD symptoms can inflict pain and suffering on your day to day life, so treating your disease properly can help ease these discomforting symptoms.
Treating COPD Symptoms

COPD affects everyone differently, you might experience more shortness of breath throughout the day and someone else may have a chronic cough, COPD is not a straight laid out treatment plan, it requires you to be flexible and listen to your body.
You also have to listen to your doctor and take the medication and oxygen therapy as prescribed in order to reduce the chances of experiencing an exacerbation and hospitalization, and to slow down the progression of your disease.
Oxygen Therapy

Long term oxygen therapy is one of the most effective treatments for COPD if your blood oxygen levels are low enough, and is the only treatment that will actually add years to your life.
This is because once your COPD has infiltrated your lungs to the point where they can no longer function properly enough to provide your body with the oxygen it needs to survive, supplemental oxygen can oxygenate your blood for you.
If your blood oxygen levels are low enough, and your doctor prescribed you supplemental oxygen therapy, a portable oxygen concentrator is your ticket to a healthier lifestyle. With the help of your oxygen device you should be able to sleep better, exercise more, and breathe easier.

Overcoming Challenges Presented with Supplemental Oxygen Therapy
Overcoming challenges with your oxygen therapy will come with time, patience, and practice. As with anything, it will take time to get used to using your device.
Tubing
Using the tubing during the day and at night while you sleep is a learning process, but eventually it will be second nature.
If you feel like the tubing is rubbing uncomfortably on your ear or your face, try wrapping the tubing in fabric or foam. This is a great solution for irritated skin caused by the friction of a nasal cannula sitting against your face or on top of your ears. Because you have to wear this tubing all day and night, the constant contact can cause soreness and skin irritation over time, which can make oxygen therapy very uncomfortable.
Dryness and irritation
Sometimes, you will notice your supplemental oxygen can cause dryness and irritation, common areas that might be affected are your lips, the skin under the nose, and other areas of the face that are near or in contact with your nasal cannula, oxygen, mask, or tubing.
This can be the result of rubbing, chafing, or the constant flow of air drying out your skin. When you use oxygen continuously, it is common that your skin will dry out in the areas where air escapes the tubing.
A simple solution for dryness and irritation that can help your skin heal and reduce the chances of future inflammation is to start using water-based moisturizers on your face and lips. If that does not help, your skin irritation could be a sign that your oxygen mask or nasal cannula isn't fitting you properly. If it's too tight, too big, or sits too loosely on your face, it can cause unnecessary friction and chaffing.
If you are having chronic problems with soreness or irritation, talk to your doctor or your oxygen supply company about getting a new nasal cannula or oxygen mask. You might need to try a different size, a different design, or a different brand in order to find one that fits your face more comfortably.

For more tips and trick to make you oxygen therapy more comfortable, read this blog:
How to Make Supplemental Oxygen More Comfortable
Medication

Common COPD medication consists of long-acting and short-acting bronchodilators, inhaled steroids, combination inhalers, oral steroids, phosphodiesterase-4 inhibitors, theophylline, and antibiotics.
All of these mediations have some kind of set back or side effect that can disturb your day to day life. Managing your medication and taking it properly is one of the only ways you can combat these issues.

Overcoming Challenges Presented with Medication
First of all, if one of your medications is giving you horrible side effects, talk with your doctor about trying a different medication with the same purpose but perhaps a different medication will not have such great side effects.
There is a lot of research being done surrounding COPD, and new innovative medications become available from time to time, so be sure you stay up to date with COPD news and experiential treatments either by doing your own research online or speaking with your doctor.

There are many efforts to develop new drugs for COPD. A research team from NIH’s National Institute of Environmental Health Sciences (NIEHS) in Rome, Italy, investigated the use of hyaluronan. Hyaluronan is naturally produced by many of the tissues in your body, including your lungs. The idea of utilizing hyaluronan as a new drug for treating COPD wound be for healing and reducing inflammation. In animal studies, inhaled hyaluronan treatment was shown to reverse some types of COPD, so watch this space and others like it for new COPD clinical trials.
Exercise

If you have COPD, you already know that exercise is a huge aspect of your treatment plan, and finding a time to exercise everyday will help you manage your COPD and slow the progression of your disease. But you also must know how hard it is to find the motivation to exercise.
Overcoming Challenges Presented with Exercise
If your disease has progressed, and you are required to be on oxygen therapy, having the right oxygen equipment can help you find motivation to exercise more than any other one thing. A lightweight portable oxygen device will give you the ability to bring your oxygen with you for a long walk or bike ride so you can stay oxygenated during your exercise session.

If you need continuous flow oxygen, the Respironics SimplyGo is the lightest continuous flow device available today, and it is a great option for any oxygen patient that is looking for more range of motion and freedom to exercise.
Of course, even with the help of your oxygen device, exercise can still be challenging.
Here are a few tips for getting in shape with COPD:
- Start with small increments and time, and build from there.
- Write down an attainable goal everyday that involves moving your body or an exercise that you can do. Check off the goal once you’ve accomplished it.
- If you feel tired one day, try to go for a short walk instead of taking the day off
- Drink plenty of water and stay hydrated
- Eat a healthy and balanced diet that give you energy
- Join a pulmonary rehabilitation course to learn new exercise and be around people going through similar trials and tribulations as you

Mental Health and Depression
Dealing with a chronic illness will take its toll on your mental health because you are not always capable of doing the things you once loved. Not to mention that diseases like COPD can be intrusive and uncomfortable to live with.
Emotional health is just as important to take care of on top of your physical health that you treat with medication and oxygen therapy. One of the best ways to treat mental health issues is to seek out meaningful and helpful social interactions.
Try talking to support groups and opening up in your pulmonary rehabilitation courses, it is likely that someone in your COPD community is going through similar issues. If you have trouble opening up about your mental health in person, try joining facebook and online forums and talking to people online. Also don’t forget that confining in friends and loved ones may seem hard at first, but it can really help them understand your mood swings and symptoms that are not always as obvious.
Beyond social interaction, you can also talk to your healthcare team about your mental state. Asking for help is sometimes the only way to get your emotions under control, so ask your health care providers to work with you to understand the cause of your feelings, and to identify coping strategies that will work for you. They may recommend you speak with a mental health professional such as a counselor, psychologist or psychiatrist.
There are also medications available to help with anxiety and depression, but they have not always been found to be effective for people with COPD. Counseling, or talk therapy, can successfully help people living with COPD change patterns of negative thinking and behaviors, improve quality of life and reduce anxiety and depression.
Overview

Dealing with challenges is a guaranteed part of having a chronic illness like COPD, overcoming these challenges is left up to you.
There are active steps you can take to get through the obstacles, and if LPT Medical can help you get the oxygen device you need to combat supplemental oxygen related challenges, just call 1(800)-946-1201.
You can also find a plethora of respiratory disease resources on our website where you can get information about everything and anything you need to learn more about your condition and how to manage it!
.png)
When you think about your day as a whole, how much time do you spend thinking positive thoughts? What about negative thoughts? And have you ever wondered how these two different lines of thinking are affecting your well-being and your ability to cope with your lung disease? Chronic obstructive pulmonary disease (COPD) is an unbelievably complex disease. Like we’ve discussed in previous posts, it’s a “systemic disease’” meaning it can have manifestations in other areas of the body. So, we can’t even begin to imagine all of the ways it affects our physical and mental health.
But despite the complexity of COPD, seemingly small and insignificant things can have a considerable impact on the outcome of the disease. For example, getting on your feet and moving around for just a couple of minutes extra each day could reduce your risk for heart disease and stroke, while helping your body manage hypertension, muscle pain, and stiffness, all of which are common in COPD. What’s more, making small adjustments to your diet like reducing sugar intake and consuming more protein and healthy fats can also have a big impact on your disease outcome.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
While you may think of “positivity” as something that only impacts your happiness, we’re going to show you in the following sections how it’s inextricably linked to the outcome of your disease and how just a few adjustments to your thought process can make your life a lot easier. As always, if you have any questions for us, feel free to leave them in the comments below or reach out to us via phone or email.
Positivity Promotes Productivity
While you may think of COPD patients as mostly retired people, there is a surprising amount of them who still work part-time or full-time jobs. According to a study published in the European Respiratory Journal, it’s common for COPD patients to miss work due to exacerbations, recurring lung infections, or simply feeling burnt out from dealing with their disease. Another thing to consider is the types of jobs that people work. Someone who works an office job might be less inclined to miss work than someone who works outside in the sun or in a factory where air pollution can lead to respiratory exacerbations.
Equally important to productivity in the workplace is productivity at home. Many COPD patients have obligations at home such as cleaning, paying the bills, and taking care of their children or grandchildren. Completing these obligations can make you feel satisfied and whole so it’s best to stay positive and focus on what you’re trying to accomplish rather than focusing on how challenging it can be with a respiratory disease. But at the same time, everyone has their limits, so you should know what they are and be sure not to cross them.
Positivity Results in Better Decision Making
Good decision-making is paramount to COPD management. Ultimately, your decisions will mean the difference between managing your respiratory symptoms effectively or letting them run their course. For example, on any given day, you have the opportunity to use your medication as it’s prescribed or deal with the side effects of using it improperly. While it may be tempting to increase your dosage if you feel that it isn’t helping, a better decision would be to connect with your doctor first to see if it will have any unintended consequences.

One of the terms you might hear thrown around in the COPD community is something called “shared decision making.” In short, this refers to healthcare professionals working one-on-one with patients to make decisions about the patient’s health. In other words, the doctor isn’t simply telling the patient what to do. The patient is playing an active role in their own health decisions. This benefits the patient because they feel like their personal needs are being met and it benefits the doctor because he/she can learn more about what’s important to COPD patients.
Positivity Prevents Anxiety and Depression
Anxiety and depression are two of the most common mental health conditions. It’s estimated that around 18.1% of the population or 40 million people in the United States have anxiety. What’s more, these mental health conditions are significantly more common among COPD patients than in the general population. According to this study from the European Respiratory Journal, COPD patients are 85% more likely to experience an anxiety disorder when compared to healthy control subjects, and studies regarding depression have shown similar results.
There are several reasons for the high rates of mental illness among COPD patients. One possible reason is that COPD patients spend more time thinking or worrying about their health. From making it to the doctor’s office to taking medication, exercising, and maintaining a strict diet, your illness is something that’s always top of mind. As symptoms escalate, you’ll likely put even more of an emphasis on your health and well-being.

Another reason COPD patients have higher rates of mental illness is due to the physical effects of the disease. COPD is known to cause breathlessness, fatigue, and chronic pain, and rapid changes to your diet and sleep routine due to flare-ups and exacerbations can leave you feeling irritable and groggy. Studies have shown that COPD can even affect our hormones and brain chemistry which can manifest itself as behavioral changes. This is why treating your underlying disease is not only important for your physical health, but your mental health as well.
Positivity Improves Systemic Health
Believe it or not, having a positive attitude can also have beneficial effects on our systemic health. This study found that emotional well-being improves recovery time and survival after physical illness. Other studies have found that positive attitudes in older adults result in a stronger immune system. This is essential for people with COPD because a poor immune system can lead to infections, the primary cause of COPD exacerbation and hospitalization.
Several other health-related benefits of positive thinking include lower blood pressure, a lower risk of heart disease, easier weight management, and healthier blood sugar levels. Weight management, in particular, is an issue that many COPD patients face because they expend a lot more energy and burn more calories than they used to, meaning they tend to be underweight. However, the opposite can also be true. Some people tend to “stress eat” when they’re experiencing anxiety or unhappiness, which can lead to unhealthy weight gain.
Positivity Leads to More Social Support
Social support is extremely important for people with chronic conditions. Between daily conversations with friends and family and interactions with caretakers and healthcare providers, it’s your social support system that is keeping you motivated. If your disease progresses, you may find yourself relying even more on those around you. There’s nothing wrong with this, of course, but you should take care to foster positive relationships early on so that you have that extra support later in life.

If you think about it, you probably enjoy spending time around people who are positive and uplifting, so it’s only natural that others would feel the same. What this means is that, despite how difficult the challenges of COPD may become, it’s always beneficial to remain positive and to spread that positive energy to other people. One of the ways many patients like to spread positivity is through online social platforms like COPD360Social. This is a patient engagement platform that’s hosted by the COPD Foundation and allows COPD patients to discuss treatment options and coping mechanisms for their disease.
Positivity Helps You Stay in Control
“Control” is a very important topic to discuss when you have a chronic disease. Many people who have been diagnosed with a chronic illness suddenly feel like they have lost control of their lives and that their disease now defines who they are and what they are capable of. However, when you look at the big picture, you start to realize that this is not the case at all. Many of the world’s greatest achievers have had some form of chronic illness and the thing that sets them apart the most is that they were able to adapt and overcome the challenges that they were presented with. None of this would be possible without having control.
The first step to maintaining control of your life despite your COPD diagnosis is understanding that there is no “right way” to do something. For example, you might be someone who makes use of mobility aids like canes, walkers, manual scooters, or electric scooters. But you shouldn’t feel guilty or self-conscious about using these things even when people around you are not. Instead, you should feel overjoyed knowing that you’re doing what you can in order to stay active and maintain your independence.

Another important note about control is that you likely have a lot more of it than you believe. While the lung damage caused by COPD is not reversible, your lungs are not the only things that affect your breathing. Your breathing is also affected by your fitness level, your diet, heart health, blood circulation, and many other things. So, if you want to stay in control, focus on things that you can change like eating right, staying active, drinking plenty of water, keeping up with your oxygen therapy, and visiting the doctor regularly. Once you realize that you have control over all of these things, you’ll be a lot happier and more positive about your condition.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
The alternative to being “in control” is having a “lack of control.” If you take on the mentality that you’re not in control, you might begin to believe that your disease, healthcare providers, friends, or family members are responsible for your happiness and well-being. And well you should certainly rely on these people for help, it’s ultimately up to you to make a difference in your own life and do what’s necessary to improve your health.
How to Increase Positivity in Your Life
While negativity has a huge impact on the outcome of your respiratory disease, the good news is that there are many different ways to promote positive thinking in your life. The first and possibly most effective method is something called cognitive behavioral therapy (CBT). This is a form of psycho-social intervention that’s used for a number of different purposes including treating alcohol and drug abuse, eating disorders, marital problems, and mental illness. Recently, it’s come to light how effective CBT can be when it comes to providing coping skills to people with chronic conditions like COPD.

CBT is based on the premise that mental health conditions like anxiety and depression are caused by inaccurate thinking patterns and patterns of unproductive behavior. CBT aims to identify these things and take steps to reverse them and replace them with productive and positive thoughts and behaviors. During CBT, you will work one-on-one with a psychologist who will guide you through the process of correcting these things. The ultimate goal is to teach you the skills you need to be able to correct them on your own without the help of a professional.
Conclusion
COPD is one of the leading causes of morbidity and mortality worldwide. It’s estimated that around 65 million people in the world have been diagnosed with COPD and it affects some 16 million people in the United States alone. While these numbers may be shocking, it helps to know that many of these people have gone on to live long and happy lives by making healthy lifestyle choices like exercising, eating a well-balanced diet, and following their doctor’s instructions when it comes to oxygen therapy and medication.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Modern medical research has proven beyond a shadow of a doubt that mental well-being also plays a role in our overall health. People who embrace a positive line of thinking are better equipped to deal with anxiety and depression and in turn, they can mitigate many of the risks associated with COPD such as heart disease, high blood pressure, and stroke. Taking steps to reverse negative thinking can have many beneficial effects in both the short and long term. For many people, cognitive behavioral therapy is the preferred method for accomplishing this.
.png)
Here at LPT Medical, we want to make it as easy as possible for COPD patients to lead happy and productive lives. That’s why we offer lightweight and reliable portable oxygen concentrators like the Caire FreeStyle Comfort and the Inogen One G5. Unlike oxygen tanks, these devices will allow you to travel wherever and whenever you please. And since they’re so easy to use, you’ll be able to focus more of your attention on living your life rather than worrying about whether or not your oxygen needs are being met.
To learn more about portable oxygen concentrators, reach out to us either by phone or email.

Beside oxygen therapy, and utilizing a portable oxygen concentrator, people with COPD are left with few other options to explore that would potentially add years to their lives. Studies have shown that hypoxic patients’s respiratory health improves greatly from long-term oxygen therapy but a viable treatment beyond oxygen therapy, still must be explored.
There is a lot of research being done right now that is dedicated to new treatment methods for COPD. COPD is the fourth leading cause of death in adults in the United States, and over 16 million Americans are diagnosed with COPD currently. This disease is preventable, but once you have COPD, you have the disease for life. There are, however, actionable ways to control COPD and the symptoms involved, but it requires diligence and attention to your treatment plan that you have set up with your health care team.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Beyond the common treatments for COPD such as, long-term oxygen therapy, medication, exercise, diet, it is possible that you will still feel unwell and incapable of doing things you once loved to do.
This is very common among COPD patients, and it can lead to mental health disorders like depression and anxiety.
![]()
Avoiding further degradation of your respiratory health and overall well being is essential if you want to live a long and happy life with COPD.
In this blog, we summarize a lot of the research being done that can help you treat your COPD even further, either through surgery, new and innovative medications, and other treatments.
New Respiratory Drug Discoveries
Currently, Only about 50 percent of asthma patients, and an even lower percentage of people with COPD, suffer from lung inflammation and cannot open up their restricted airways even with the help of readily available medications. It is evident that there is still a lot of work to be done to develop medications that can help all people with obstructive respiratory diseases breathe better.
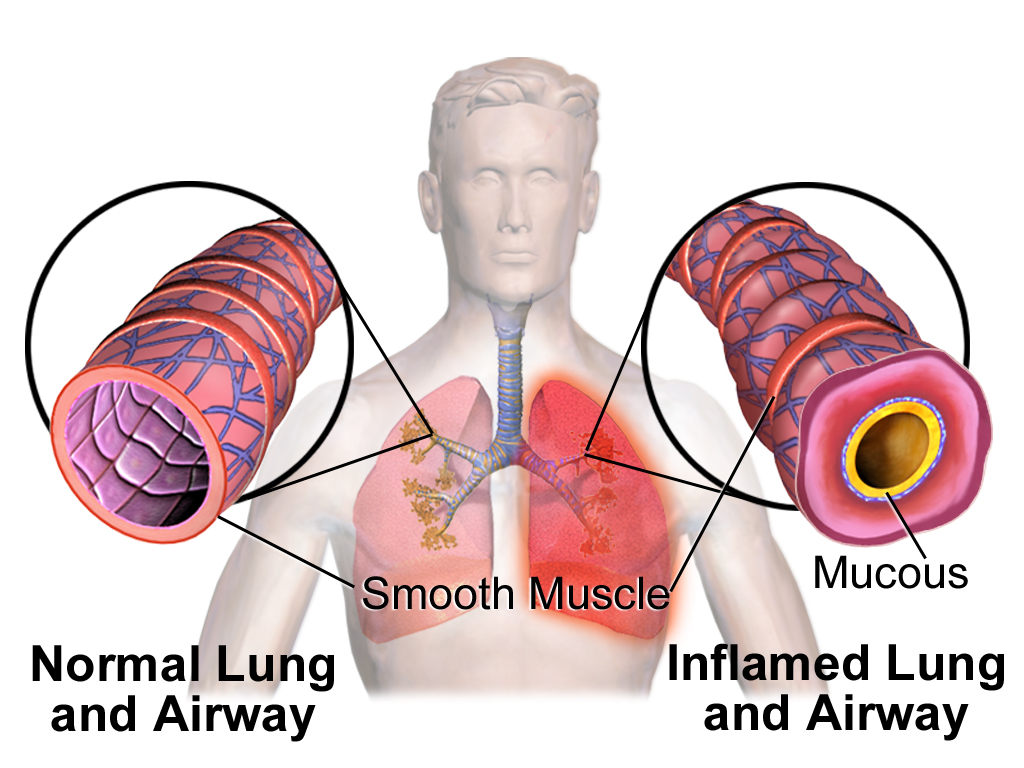
Medication - TASR5 Bitter Taste Receptor for COPD Patients 2021

If you have asthma or COPD, the tightening of smooth muscles surrounding your bronchial tubes narrows your airway and reduces air flow, this is often why you cannot breathe well. Dr Liggett's lab has discovered a TASR5 bitter taste receptor that can open your airway when activated. This is a promising new study that has paved the road for looking into new drugs to treat asthma and other obstructive lung diseases.
This new medication targets smooth muscle to open up constricted airways.
The medication is a promising bronchodilator agonist that shows a lot of potential in treating respiratory diseases. In the preclinical study, this new bronchodilator was 1,000 times more potent than some of the other agents that were tested.

The goals of this new mediation are to find a more potent agent that will activate this smooth muscle receptor and for it to accurately deliver the potencies by inhalation. T5-8 was the bronchodilator agent that showed the most promise.
Luckily, there were others options that worked well too, so there are multiple potential new drugs to carry out the next steps!
Zephyr Valve for COPD Patients in 2021

It is likely that your lung disease will begin to advance into a more severe state as you get older, even with proper treatment. Once your disease begins to get in the way of taking care of business the way you are used to, it is time that you do something.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
If you have chronic obstructive pulmonary disease (COPD), but noticed it getting worse over the past few years, it can easily begin to get in the way and you will be unable to do the things you love.
Things like attending family events, hobbies like golfing, or taking care of the house can soon become unattainable and sound impossible.

COPD affects 16 million people, and is the fourth leading cause of death in the United States.. The main symptoms, including chronic cough, fatigue, and shortness of breath, secondary symptoms include, mood swings, fatigue, and mental health issues all of which tend to worsen over time.
There is still no cure for COPD, but there are drugs and therapies readily available to treat these symptoms, however they are not always potent enough. Treatments include pulmonary rehabilitation, bronchodilators and corticosteroids, and lung volume reduction surgery help many people living with COPD.
A new option called the Zephyr Valve, which was FDA approved in 2018, is offering hope for people who suffer from COPD in an advanced state. The Zephyr Valve is designed for patients with advanced COPD, who’s breathlessness at rest or with activity is extremely high, and even with optimal medical treatment, they still suffer from significant hyperinflation and air trapping due to deterioration of lung tissue.
Another not so commonly noted problem with the way COPD affects patients is how the lungs become bigger, or hyperinflated. Shortness of breath and uncomfortable gastrointestinal symptoms are the result of overinflated lungs pressing down on the diaphragm.
The valves in the Zephyr Valvae are extremely small, they work by being implemented into the ‘bad’ diseased parts of the lung, in order to block the air from going into those sections. As a result, the non-diseased portion of the lung can expand and relieve the pressure on the diaphragm, allowing patients to breathe better.
If you treat your COPD properly- take your medications, adhere to your oxygen prescription, exercise and eat properly, and still your disease progresses past a certain degree, your pulmonologist may suggest you look into the Zephyr Valve placement.

If you qualify, there is no guarantee you’ll be completely better and feeling 100% all of the time, but there is overwhelming hope that you’ll have a better quality of life. You can get back to doing what you love or enjoying the simple things, will you still get tired? Yes, because you still have COPD. But the progress towards a happier more active life is a pursuit you can begin on!
Stem Cell Therapy for COPD in 2021
![]()
There is potential to help patients with COPD by using Mesenchymal Stem Cells. Stem cells work by promoting healing and regenerating, they do this by creating extra messenger cells called "cytokines".
Stem cells are amazingly unique, and they are capable of changing into any cell in the body. Once they are inserted, they can find damaged tissues around organs and rejerate new healthy cells within those organs. In your case, as a respiratory disease patient, it is your lungs that are deteriorating and damaged, and so stem cells can repair damaged lung tissue to combat emphysema or chronic bronchitis.
While stem cells rebuild healthy cells, they also have natural anti-inflammatory properties that can clear your airways as well.

Studies have shown the results of stem cell therapy and its effects on COPD. Over 82% of COPD patients that have tried stem cell treatment have significant improvements in their quality of life after their therapies.
The positive reported impacts stem cell therapy after transfusion are increased lung capacity and the ability to walk. These reports have highlighted stem cells' ability to be viable options for current patients with COPD.

And while stem cell treatment still will not cure COPD, it is able to repair damaged lung tissue and it being a relatively noninvasive procedure compared to other options, stem cell therapy is an attractive alternative for COPD patients. Studies have shown that certain cells- expanded cord tissue-derived mesenchymal cells- have very high anti-inflammatory properties and tissue regeneration capabilities, that are perfect for patients with COPD.
Cost of Stem cell therapy for COPD
The most affordable option for COPD patients is to find patient-funded clinical trials. COPD patients who get stem cell therapy can pay anywhere from $10000 - $35,000.
While you are researching stem cell clinics for COPD, be sure to find out how many cells are included in the treatment protocol, and what type of cells you would be receiving.
Currently, Medicare does not cover the cost of stem cell therapy for COPD.

Currently Available Treatments for COPD
New medications such as the TASR5 bitter taste receptor to treat COPD are not yet available for COPD patients, and the Zephyr Valve and Stem Cell Therapy may be out of your price range or you simply do not qualify for those treatments based on the current state of your disease.
Other more common treatments for chronic respiratory disease go a long way in cultivating a healthy lifestyle and improvements in your wellbeing.
Supplemental Oxygen Therapy

Oxygen therapy is among the most effective treatments there will ever be for COPD and patients with chronic hypoxia.
Supplemental oxygen therapy should be administered at least 15 hours a day, and for the best results, 24 hours per day, but this depends on your doctor’s recommendations and the prescription they will base upon your spirometry test results.
You will get your supplemental oxygen therapy administered with an oxygen device that you will bring with you everywhere you go. Having the best oxygen equipment will help you live a high quality life while getting the oxygen saturation your body needs to survive.

Portable oxygen devices are a great option for people who value the ability to exercise, run errands, and get out and about rather than spending a lot of time at home!
The best portable oxygen devices are called portable oxygen concentrators and they are the most efficient because they are battery powered oxygen devices so you can take them on airplanes, they are lightweight, and it extracts air from its surroundings so you never have to get them refilled with oxygen.
Pulmonary Rehabilitation

The goal of pulmonary rehabilitation is to rebuild strength so you can start to enjoy a more full and active life. These programs are set up to improve your lung function, reduce the symptoms you experience, and improve quality of life.
The courses are a mixture of educational classes and physical exercises that will increase your awareness about your lungs and your disease.
Your pulmonary rehab team is a team of doctors, nurses, physical therapists, respiratory therapists, exercise specialists and dietitians. With all of their help and expertise, you will develop a unique program that meets your specific needs.

Overview
As a company that works with respiratory patients on a daily basis LPT Medical has readily available reading material that will help answer all of your questions about your respiratory illness, how to treat it, and everything else you may want to know, just visit our respiratory resource center page.

This is not the end of COPD research in fact, it is the beginning. New and innovative mediations, procedures, and other respiratory devices will become available in 2021 and beyond that will help you breathe easier, and reduce the symptoms you experience from COPD.
Watch this space, and be sure to like LPT Medical on Facebook, subscribe to our newsletter, and comment on this blog because we are always posting news and information about respiratory illnesses, and learning about your disease is as important as treating it everyday.
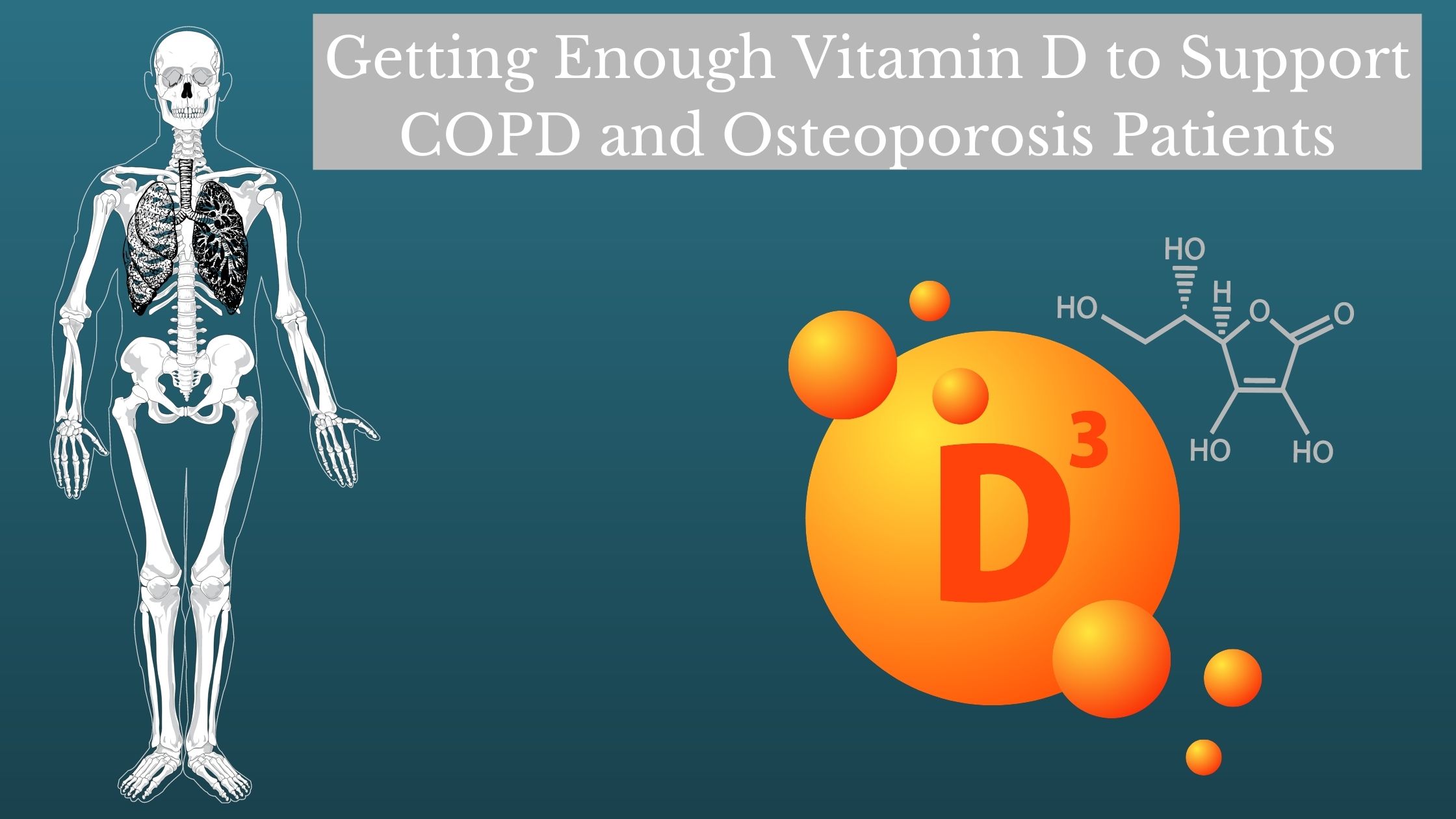
Vitamin D is an important part of everyone's diet, and if you aren’t getting enough vitamin D or if your body is not processing it correctly, you might notice the negative impacts this can have on your health. If you have chronic obstructive pulmonary disease, getting the right vitamins and minerals can be the difference between a good day and a horrible day, or a day spent at home or a day spent in the hospital.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What we put in our bodies matters, and how our bodies process those things we ingest also plays a critical role in the way our body as a system performs. If you do not get enough, too much, or your body cannot absorb things correctly, things get worse.
It might not be common knowledge that what we put into our stomachs actually affects our lungs, but it does.
People with chronic obstructive pulmonary disease also known as COPD, need plenty of vitamin D to encourage healthy bones and muscles and encourage a healthy immune system all of which contributes to a healthy lifestyle even with a chronic disease.
If you have COPD read this blog to learn about the benefits of eating food with plenty of vitamin D and when and why you should take vitamin D supplements, and when and why you should not.
Remember, not everyone is lacking in vitamin D, and so taking supplements could be redundant for you if your body doesn't need it, however, eating foods high in vitamin D is beneficial and will contribute to maintaining stable levels of vitamin D throughout your life.
Vitamin D Why Do We Need It?
Vitamin D helps regulate the amount of calcium and phosphate in the body. Therefore, these nutrients are helpful if we want to keep bones, teeth and muscles healthy, which for COPD patients is crucial.
Osteoporosis is a common and significant problem in patients with COPD that has advanced into severe stages. The cause of bone loss can be attributed to a number of COPD symptoms and side effects but includes smoking, vitamin D deficiency, low body mass index, amongst other conditions.
COPD is a respiratory disease that affects more than just your respiratory system, and the causes of COPD, such as smoking and exposure to pollution, can all contribute to other parts of your health.

When we talk about osteoporosis and bone loss and how it is related to COPD, we want to address the seriousness of the lack of recognition! Many patients with both or one of these conditions only know they have one or the other when they experience something related to the disease. In the case of osteoporosis, you might not know you have it until you get a fracture. If you have COPD you might not know it until your condition worsens and the lung damage causes you to experience exacerbations.
Preventing Bone Loss and Treating Osteoporosis
One of the most effective strategies to prevent bone loss and/or to treat osteoporosis include taking or eating foods high in calcium and vitamin D.

Hormone replacement when indicated by your doctor is also an option as well as, other vitamin D enhancing mechanisms.
COPD and osteoporosis are related due to the various risk factors that influence COPD, such as tobacco smoking, systemic inflammation, vitamin D deficiency, and the use of oral or inhaled corticosteroids (ICSs). All of these factors can work in developing COPD, but also contribute to bone loss and osteoporosis.

Osteoporosis is a disease characterized by low bone mass and the deterioration of bone tissue, which makes your bones fragile and more prone to fractures. Your bone density is directly related to the mineral your body is able to use to strengthen them.
It is not just patients with COPD, but patients with other chronic lung diseases like cystic fibrosis and idiopathic pulmonary fibrosis, also tend to have an increased prevalence of osteoporosis.

Now that there is an increased awareness by pulmonologists and the increased use of preventive strategies, the impact of osteoporosis on those patients with COPD should decrease. However, in order to actively avoid Osteoporosis if you already have COPD or not, you need to have enough vitamin D.
Getting Enough Vitamin D
Here are some basic ways you can effectively increase your vitamin D levels.
First of all, you need to know how much vitamin D you need in order to know what a healthy amount of vitamin D looks like.
How much vitamin D do you need?
It is up for debate within the scientific community how much vitamin D.
![]()
While the U.S. National Academy of Medicine considers 600–800 IU of daily vitamin D to be sufficient for the majority of the population, the U.S. Endocrine Society recommends 1,500–2,000 IU per day. Although it would be hard to take too much vitamin D, it is best to avoid long-term vitamin D doses in excess of 4,000 IU without supervision from a qualified healthcare professional.
Well what does all of this mean?
Try doing these 7 things to get enough vitamin D:
1. Spend time in sun
We often call vitamin D the “the sunshine vitamin” because sunlight is a great source of this nutrient! If you have COPD, getting out into the sunlight everyday should not be a daunting task, it can be as simple as sitting in a sunroom or on the front porch reading a book.

The sun helps enrich our vitamin D levels because human skin has a type of cholesterol that functions as a precursor to vitamin D so when this cholesterol is exposed to light and radiation from the sun, it becomes vitamin D that our body can use!
Surprisingly, vitamin D from the sun may last twice as long as vitamin D from food or supplements! That being said, just because you are getting plenty of sunlight there are variables in your body that would inhibit you body from making enough vitamin D from the sunlight.

Skin tone and age
Note that people with darker skin have more melanin and therefore need to spend more time in the sun to produce vitamin D than those with lighter skin and less melanin. Melanin is a compound that can prevent vitamin D production.
Age
Your age can also have an impact on the way your body produces vitamin D as well. As you get older, the way your body produces vitamin D becomes less efficient.
Geographical location and season
Obviously, the area you live in will determine that amount of sunlight and subsequently the amulet of vitamin D you’ll be able to produce year-round. If you live in an area with a lot of direct sunlight your physical proximity to the sun’s rays helps you produce vitamin D.
Inversely, if you live in darker or colder environments, your opportunities for adequate sun exposure and vitamin D production decreases.
Sunscreen and clothing
Certain types of clothing and sunscreen can hinder — if not completely block — vitamin D production. This does not mean you should go outside without sunscreen or UV protection! It is vital to protect yourself from skin cancer by avoiding overexposure to sunlight.
Note that it takes very little unprotected time, as few as 8–15 minutes of exposure is enough to make plenty of vitamin D for lighter-skinned individuals and slightly longer for those with darker skin, in the sun for your body to start producing vitamin D.
2. Eat fatty fish and seafood

Fatty fish and seafood are a few of the richest natural food sources where you can get plenty of vitamin D.
To put it into numerical values, a 3.5-ounce (100-gram) servings of canned salmon gives you 386 IU of vitamin D.
Other kinds of fish and seafood rich in vitamin D include:
- tuna
- mackerel
- oysters
- shrimp
- sardines
- anchovies
3. Eat mushrooms

Interestingly, mushrooms are the only food source that is vegetarian and also a source of vitamin D.
In a similar way as humans, mushrooms can make their own vitamin D when exposed to sunlight. The difference is that humans produce a form of vitamin D known as D3 and mushrooms produce D2.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Both D3 and D2 forms of this vitamin can increase your circulating vitamin D levels, though research suggests that D3 from sunlight is known to raise levels more effectively and efficiently than D2 from mushrooms.
The vitamin D content depends on the type of mushroom, but certain kinds can provide as much as 2,348 IU per 3.5-ounce serving, even more than canned salmon!
4. Add egg yolks to your diet

Egg yolks are another source of vitamin D that you can easily add to your routine.
Like many other natural food sources, egg yolks have variable vitamin D content.
Overview
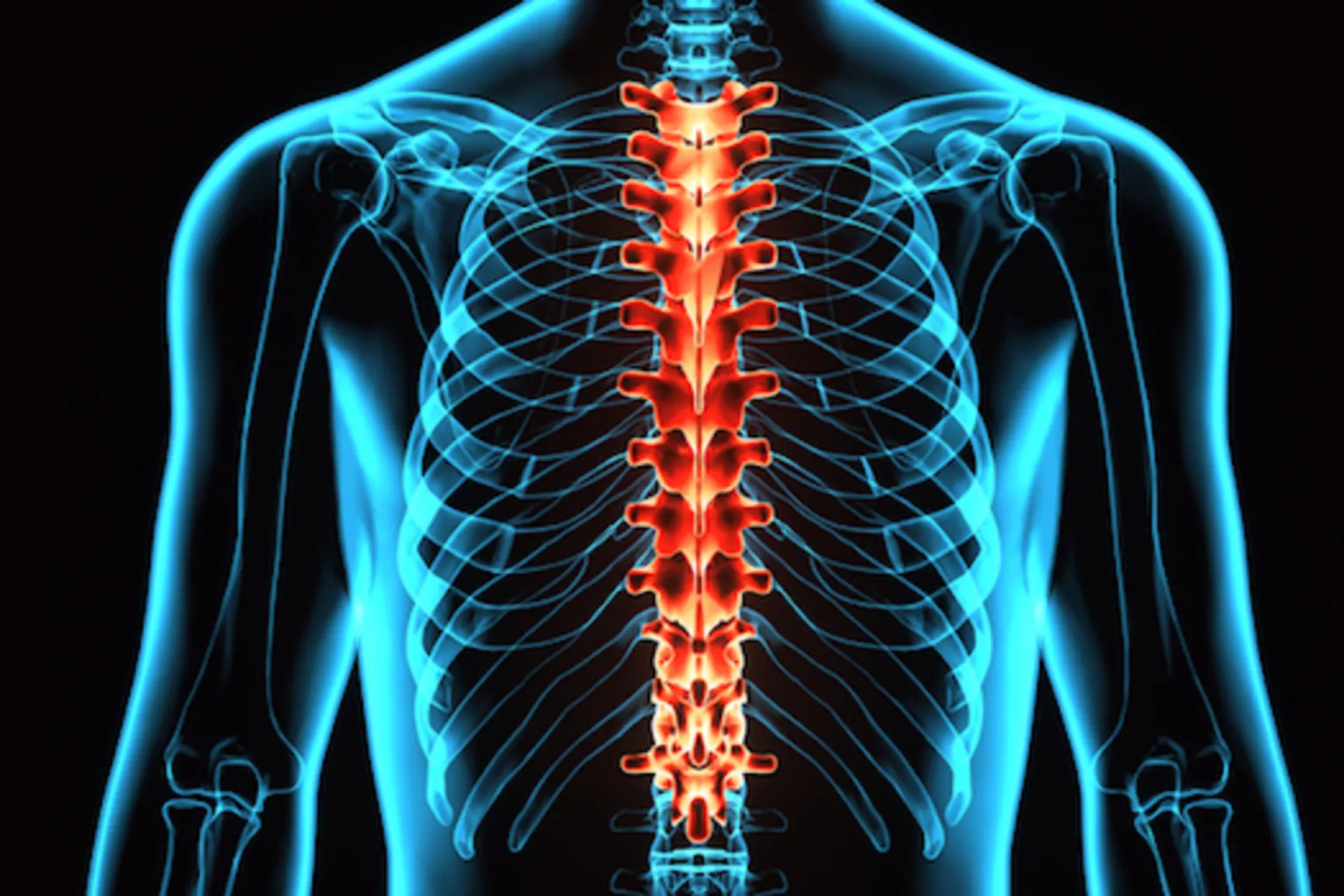
Health related issues go together like peanut butter and jelly, for example high cholesterol and heart attacks or osteoporosis and bone fractures. It's less intuitive that breathing problems and osteoporosis are also commonly related, but these conditions are seen together so often that it's obvious one influences the other.

What does breathing have to do with your bones? How can the shortness of breath you experience due to your COPD be related to your bone fractures?
When we look deeper at the relationship between osteoporosis and COPD we can see the logic. Not only is chronic obstructive pulmonary disease (COPD) linked to osteoporosis, furthermore, loss of lung capacity is associated with osteoporosis.
The blockage of lung blood vessels can be associated with a treatment for osteoporosis-related fractures. Understanding this relationship among others, can help you better manage both conditions.
Getting enough vitamin D is essential for both COPD and Osteoporosis, and in doing so you are advancing your health, and improving your quality of life!
If you live with COPD, asthma, or a similar chronic condition, it can sometimes feel like you’re walking on eggshells. These diseases cause the lungs, airways, and other areas of the body to become very sensitive to “triggers” like air pollution, infection, injury, and more. In certain situations, even your pulmonary rehabilitation routine can exacerbate these symptoms; this is why it’s always important to keep your doctor informed about what you’re experiencing.
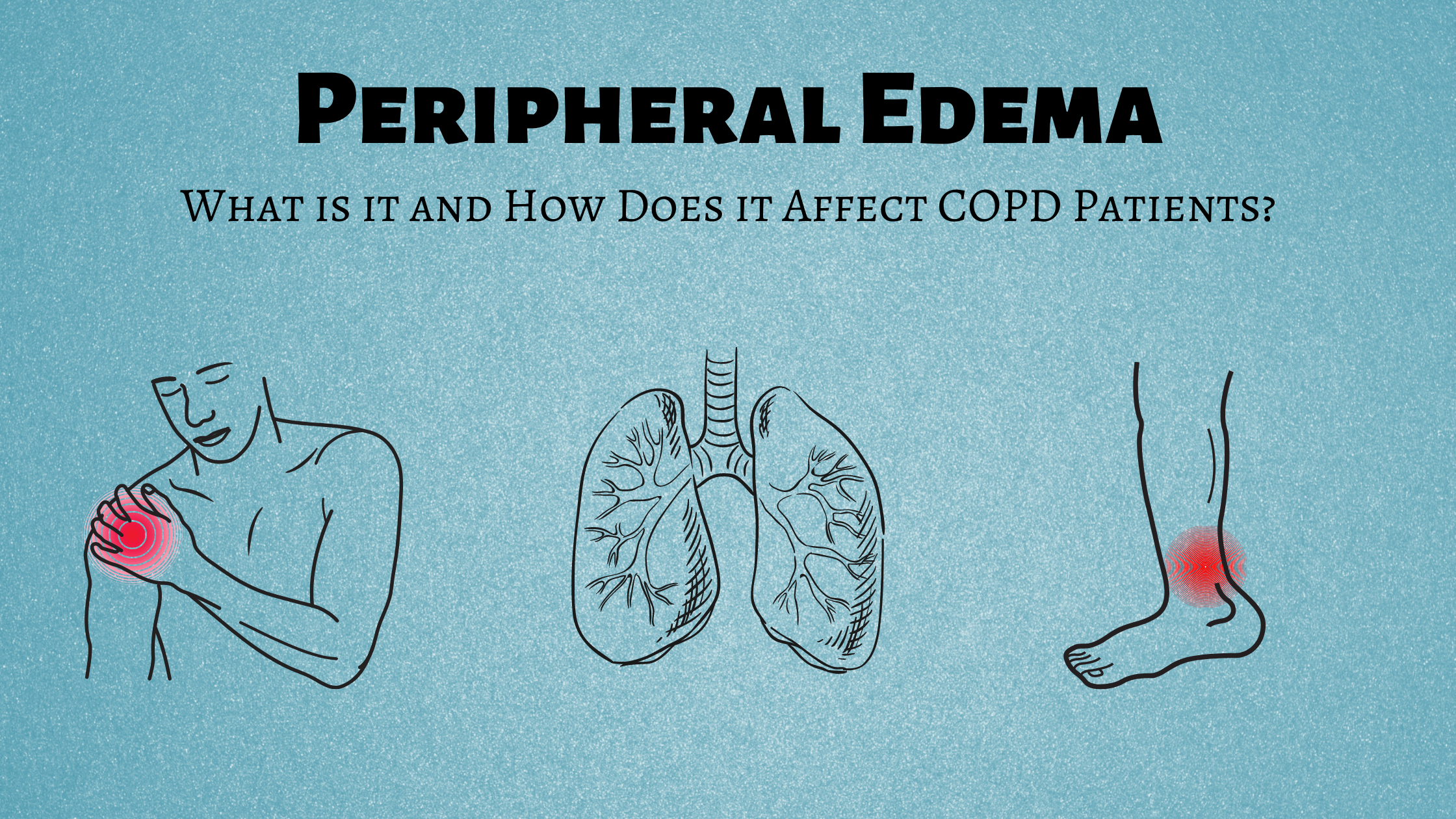
Oftentimes, COPD patients may encounter symptoms that are seemingly unrelated to their lungs. These are called “complications” because they are not common symptoms of lung disease but lung disease can often be a catalyst for things like heart disease, vascular disease, and even mental health disorders like depression or anxiety.
One frequent, but often overlooked complication of COPD is something called peripheral edema. The term “edema” refers to swelling in the body, usually due to the buildup of fluid and the term “peripheral” refers to areas away from the center of your body such as your legs, hands, or arms. In this post, we’ll help you better understand what peripheral edema is, what causes it, and what steps you can take to mitigate it.
If you have any questions, please feel free to leave them in the comment section below so we can get back to you.
What is Peripheral Edema?
“Peripheral edema” is the medical term for swelling in the limbs of the body. It can occur anywhere in the body, but it most commonly occurs in the lower legs or feet. Usually, edemas develop slowly over a couple of days or weeks, but in rare instances, it can happen over the course of a couple of hours. Many patients don’t realize there is swelling until they experience pain or they aren’t able to put on their shoes, shirt, or pants.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
There are six types of edema, but only three of them are known complications of COPD. These include peripheral edema, pulmonary edema, and pedal edema. Let’s take a look at each of the six types of edema to see how they compare.
Lymphedema
Lymphedema usually occurs in one of your legs or arms. Cancer patients who have damaged lymph nodes or people who have had them removed for cancer treatment often experience this symptom. Lymph nodes are an important part of the immune system because they block harmful substances, but if they are damaged they may cause your body to retain fluids, thus causing edema.
Cerebral Edema
Cerebral edema tends to be the most serious type of edema because it occurs in the brain. Some common causes of cerebral edema include head injuries, blood clots, tumors, and allergic reactions. Cerebral edema can often be life-threatening, so it’s best to seek immediate medical attention.
Macular Edema
The macula is at the light-sensitive area at the center of the retina in your eye. Macular edema occurs when blood vessels in this area begin to leak fluid and sometimes blood. If macular edema is left untreated, it can lead to permanent damage to the eyes or even blindness. If you’re experiencing pain in your eyes, a sharp headache, blurry, or impaired vision of any kind, you should immediately contact your doctor.
Pulmonary Edema
Pulmonary edema is the buildup of fluid in the lungs. This is most often caused by heart conditions like a heart attack, hypertension, or narrowed heart valves. Acute pulmonary edema which comes on quickly can be serious and even life-threatening, especially in patients who already have a chronic lung or heart disease.

Pedal Edema
This type of edema is found in the lower legs and feet. There are several known causes of this type of edema including venous edema which is the retention of low-protein fluid and increased capillary filtration. The second most common cause of pedal edema is lymphatic edema which we discussed earlier. These two different causes of pedal edema can either work independently or together to create swelling in the feet.
Peripheral Edema
The term “peripheral edema” is a little broader than the terms used above. While the others describe a specific type of swelling caused by a known condition, peripheral edema can occur in many parts of the body and it has many different causes.
What are the Symptoms of Peripheral Edema?
The primary symptom of peripheral edema is swelling in the extremities. This swelling is usually drastic enough that it will be noticeable by you or your loved ones, and as the swelling increases, you’ll likely have trouble putting on your shoes or clothing without having to force them on.
Another symptom of peripheral edema is reduced mobility. If you’re like most COPD patients, you’re probably trying to stay active in order to preserve your lung function and keep your muscles strong and efficient. If you’re developing peripheral edema, you may feel your legs becoming heavier or you may notice that you lose your sense of balance more easily than you did before.

In some, but not all cases, people with peripheral edema may experience pain and tightness in their legs or feet. As the amount of fluid increases in the affected area, you may notice the skin becoming shiny and red. You might also experience something called “pitting.” This is when you press on an area of your skin and the indentation remains there longer than it would on a healthier part of your body. Since the fluids that your legs or feet are retaining would normally be flushed out of the body, you might also see an increase in your body weight.
What Causes Peripheral Edema?
Peripheral edema has a variety of different causes. If your edema comes and goes within a day or two, this is likely a sign of a less serious underlying condition. But if the edema is chronic and it only seems to get worse as time goes on, this is likely a sign of a more serious underlying condition. Either way, it’s important that you speak with your doctor right away and be thorough about the symptoms you’re enduring. Since there are so many potential causes, peripheral edema is very difficult to diagnose accurately. As a result, the more information your doctor has, the better diagnosis he/she will be able to provide. Below are some of the top causes of peripheral edema.
Injuries
If you’ve ever had a fracture, strain, sprain, or bruise, you know that it’s usually accompanied by some swelling and pain. This is because your body releases white blood cells and other fluids to the area in order to repair the damage. Depending on the severity of the injury, it may take several days or weeks for the swelling to subside.
Prolonged Sedentary Behavior
Physical activity plays an important role in maintaining a healthy vascular system. Even moderate exercise that slightly raises your heart rate has significant benefits when it comes to promoting healthy circulation. However, as we age, it becomes increasingly difficult to exercise regularly. This sedentary lifestyle can affect blood flow throughout your body and lead to fluids building up in your extremities. Especially your legs.
High Sodium Intake
According to the U.S. Food and Drug Administration (FDA), the average American consumes about 3,400 mg of sodium per day but the recommended daily intake is 2,300 mg a day. Unfortunately, sodium plays a major role in the retention of fluids in your body and it can have adverse effects on your body’s ability to flush out toxins. Consuming high amounts of salt through processed foods can cause peripheral edema and if you’re already experiencing edema, it can make it worse.
Medications
Every drug, medication, or supplement has side-effects. Some drugs can cause or contribute to edema either by impairing lymph drainage or increasing the amount of fluid that is filtered from the blood capillaries into various tissues throughout the body. Here are a few of the medications that might cause complications:

- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Blood pressure medication
- Corticosteroids
- Hormones
- Diabetes medication
- Antidepressants
How Are Peripheral Edema and COPD Linked?
Peripheral edema is common in COPD patients. While COPD does not directly cause edema, it can result in a medical condition called pulmonary hypertension which causes peripheral edema. Oftentimes, when a COPD patient experiences swelling in the hands, legs, or feet, they don’t associate it with their lung condition. It’s often shrugged off as a sign of aging or they may take Benadryl or a similar drug thinking it’s an allergic reaction. Ideally, if you ever experience unusual symptoms it’s best to consult your doctor rather than trying home remedies because this may exacerbate the issue.
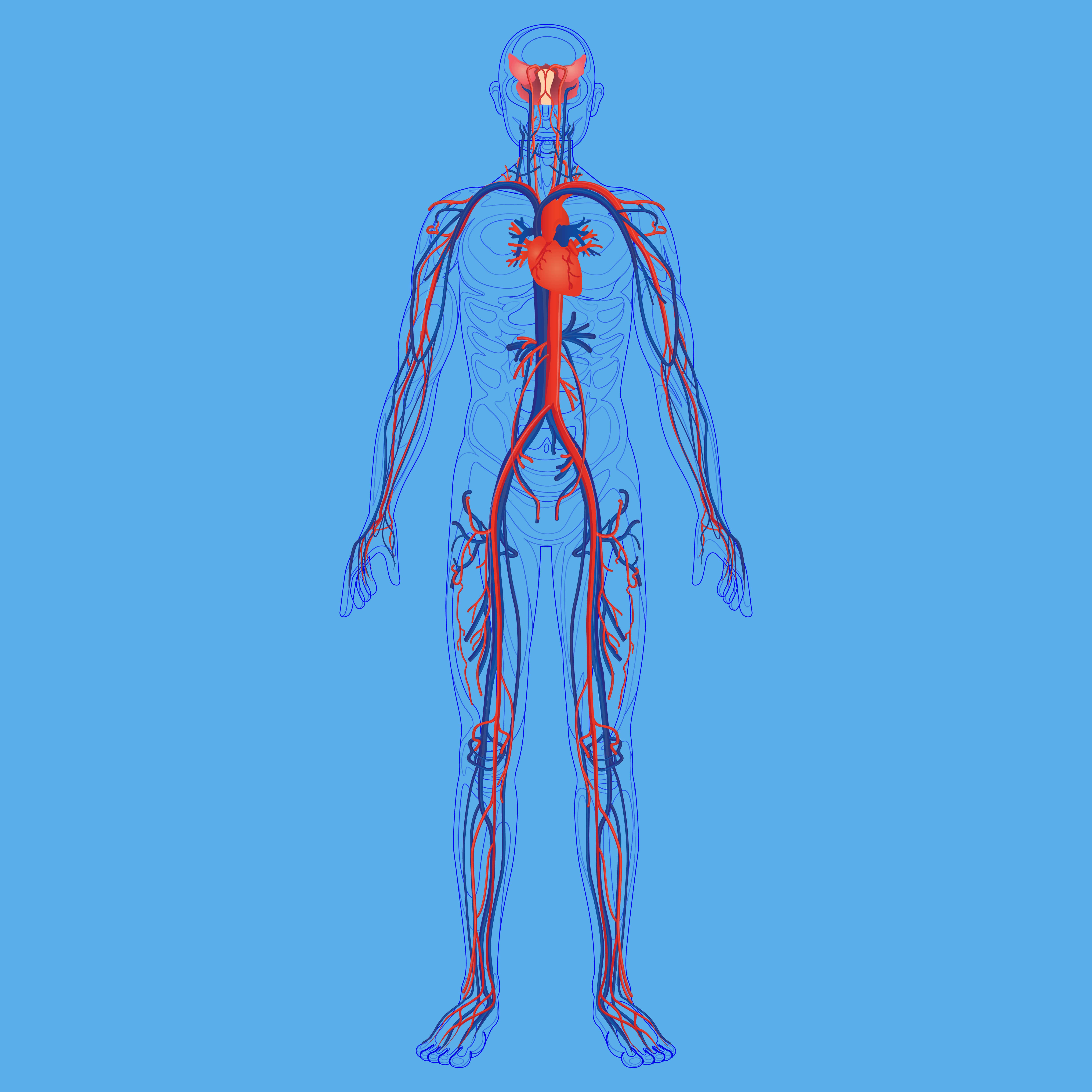
Pulmonary Hypertension
The function of the right side of the heart is to receive oxygen-poor blood and pump it into your lungs. As it passes through the lungs it is re-oxygenated by alveoli (tiny air sacs) then it moves through the left side of the heart to be pumped through the body. Pulmonary hypertension occurs when the blood pressure in your lungs is too high, thus resulting in strain on the right side of the heart. If this issue persists the heart can become overworked and enlarged, resulting in a condition called cor pulmonale.
Cor Pulmonale
Cor pulmonale is more commonly called right-sided heart failure and it’s usually an urgent medical condition. According to Medscape, COPD patients who develop cor pulmonale have a 30 percent chance of living for 5 years. Peripheral edema is sometimes, but not always, the result of cor pulmonale, so it’s imperative that you visit a doctor even if you don’t believe your swelling is due to any serious underlying condition.

COPD leads to pulmonary hypertension and eventually cor pulmonale through a process called hypoxic pulmonary vasoconstriction (HPV). This is a type of vascular remodeling that results in the constriction of vascular smooth muscle due to low partial pressure of oxygen (Po2). In other words, if your lung function is impaired due to emphysema or chronic bronchitis, the arteries in your lung will respond by reducing their size which will increase blood pressure.
Since pulmonary hypertension and cor pulmonale put so much strain on the heart, you may see the problems manifest in other areas of the body. Due to the force of gravity, blood and other fluids often start to pool up in extremities, primarily the feet and lower legs. If this is the cause of your peripheral edema, your doctor will need to treat your underlying lung problems and vascular problems in order to reduce the swelling. Supplemental oxygen therapy and blood thinners are often prescribed to treat pulmonary hypertension if you aren’t already on them.
How to Prevent Leg Swelling With COPD
If you want to prevent leg swelling with COPD, your best bet will be to follow your COPD treatment plan. Pulmonary rehabilitation is extremely important for preventing swelling because not only will it improve your endurance, but it will also strengthen your heart muscle, improve circulation, and reduce body fat which is a known contributor to peripheral edema. To combat leg swelling, your doctor may advise that you increase the amount of time spent doing pulmonary rehab, or he/she might advise that you split your exercise routines into shorter, more frequent intervals.

Hydration is another key treatment for leg swelling caused by COPD. Plasma, the primary component of your blood is made up of 90 percent water. And water is what keeps blood flowing freely throughout your body without clotting or pooling. So, it goes without saying that drinking more water will improve your circulation and keep you healthy. Most doctors will recommend around 8 to 12 glasses of water a day for the average COPD patient.
![]()
Last but certainly not least, you need to watch what you’re eating. Diet plays an extremely important role in your vascular health so eating the right food can relieve a significant amount of stress on your heart and thus prevent peripheral edema. Aside from staying hydrated, you’re going to want to consume less salt and sodium. What’s more, studies have shown that when coupled with a diet rich in calcium, magnesium, and potassium, low-salt and low-sodium diets are more effective.
Conclusion
If you’re currently experiencing swelling of the hands, legs, or feet with COPD, you’re not alone. This phenomenon can occur for a variety of reasons, most of which are not life-threatening. In fact, many seniors, even ones who are generally healthy, can experience it. But due to the fact that swelling can be a sign of pulmonary hypertension or right-sided heart failure you should plan on talking to your doctor as soon as possible, just to be safe.
In the meantime, you should plan on closely following your COPD treatment plan that you worked out with your doctor. While home remedies may help ease the discomfort and swelling a bit, the best way to treat peripheral edema is to treat the underlying disease that’s causing it. If you have any questions about what you read here, please feel to leave a comment or reach out to us.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!