Getting diagnosed with COPD and watching your body change can be a disheartening thing to go through. This, along with the symptoms of COPD, make depression a reality for a large number of COPD patients.
It's not too difficult to see why; COPD can lead to weight loss, fatigue, sleep disorders, poor nutrition, and a variety of other uncomfortable symptoms. These ailments can be distressing on their own, leading to health anxiety, a negative outlook, and a feeling of loss of control over one's life.
According to some studies, up to forty percent of COPD patients suffer from depression. What's worse, many cases go untreated, which makes patients more likely to suffer a quicker physical decline and death.
But, while COPD can be difficult to cope with, there are plenty of options for support and treatment that can help you take back control over your life. Even though depression can make obstacles seem too difficult to face, the truth is that you can find the power within yourself to overcome them.
It is important to remember that it's more than possible to live a happy and fulfilling life despite the hardships that come along with COPD. If you can shake yourself free of anxiety and depression, you'll find that you have the ability cope in healthy ways and confidently meet any challenges that come your way.
It's hard to see the light when you are in the midst of depression and everything seems hopeless and bleak. That's why it's so important to recognize the signs of depression and seek treatment, and in this article we're going to show you how.
In the next sections, we'll show you how to identify depression and explain how it affects people with COPD. Then, we'll show you how to utilize available mental health resources and how to use a variety of practical techniques to help yourself out of depression.
What is Depression?
The term “depression” is often used loosely in casual conversation, but in reality, it is a serious medical illness. It is much more than just feeling a little down for a few days; it's a deep state of sadness and helplessness that affects many aspects of sufferers' lives.
Depression is often marked by hopelessness, lack of motivation, and lack of interest in activities that you used to enjoy. Depression often interferes with your ability to function and participate in activities at work, home, and with friends.
People who are depressed are also more at risk for a variety of other health problems, including obesity, substance abuse, and premature death. In general, people who are depressed have difficulty maintaining healthy habits and lead a significantly reduced quality of life.
Depression should always be taken very seriously and should never be ignored. If you or someone you know is showing the warning signs of depression, you should encourage them to seek help as soon as possible.
Symptoms of Depression

The main characteristics that separate clinical depression from normal sadness or negative moods is its severity and its duration. Everyone has a bad day or bad week every once and awhile, but people who suffer from depression often experience weeks or months of despair along with a variety of noticeable physical symptoms.
Here are some of the most common symptoms of depression:
- Sadness
- Emptiness
- Hopelessness
- Anxiety
- Helplessness
- Feelings of worthlessness
- Feelings of guilt
- Difficulty concentrating
- Difficulty sleeping
- Irritability
- Loss of appetite or increase in appetite
- Fatigue
- Lack of interest in hobbies and activities you used to enjoy
- Thoughts of death or suicide
How Depression Affects People with COPD

If left untreated, depression in people with COPD can significantly increase their risk for physical decline. It can increase patients' risk of exacerbations, loss of physical mobility, malnutrition, and even death.
There are many reasons for these risks, most of which have to do with changes in behavior and motivation that happen to COPD patients who are depressed. For example, depression can affect both your appetite and your sleep quality, leading to malnutrition and sleep deprivation. This, in turn, weakens your body, makes COPD symptoms worse, and depresses your immune system, making you more prone to exacerbations and hospitalizations.
Studies also show that people with COPD who are depressed are more likely to be hospitalized, less likely to adhere to COPD treatments, and have a much higher risk of death. They are also more likely to smoke and suffer from an overall decreased quality of life.
One of the most damaging effects of depression is how it can take away your motivation to do things that make you healthy and happy. Many people who are depressed stop exercising, eating, and socializing, which are important to living a healthy life with COPD.
There is hardly anything more essential for keeping yourself healthy with COPD than following your treatment plan, eating a healthy diet, and, especially, getting plenty of exercise. However, depression can take away your motivation to do all of these things, causing you to skip meals, workouts, and medication doses. This is a large part of the reason why many depressed COPD patients suffer a more rapid physical decline.
Another reason is the fact that being depressed can make it much more tempting to reach for unhealthy coping mechanisms like cigarettes and other drugs. Since smoking is one of the most damaging things you can do to your body when you have COPD, depression can be even more damaging to patients who are former smokers or who are currently trying to quit.
For all of these reasons, it's vitally important for COPD patients who suffer from depression to seek support and treatment as early as possible. It's certainly not something you should ever take lightly or ignore, as it could have huge and irreversible effects on your health.
Everyday Techniques for Reducing Depression for People with COPD

Everyday activities like diet and exercise can have a huge impact on how you feel. Building healthy habits in these areas is an important first step to breaking free from depression and getting yourself back on track to living a healthy, fulfilling life.
Exercise More

When you are feeling depressed, exercising and being active might sound like the last thing in the world that you want to do. However, getting out of bed every day and doing some physical activity can actually improve your depression, not to mention that it's absolutely necessary to prevent early death from COPD.
It can be difficult and disheartening to exercise when you're experiencing COPD symptoms like breathlessness and wheezing, which on its own can contribute to depression and exercise avoidance. However, skipping exercise will only make that same problem worse, making your body weaker and your lungs decline quicker.
On the other hand, forcing yourself to get out, move your body, and increase your fitness can do wonders for both your body and mind. It not only stimulates your brain and promotes a more positive mood, but it can also increase your physical strength and mobility, allowing you to breathe better, do more, and have more energy.
Here are some of the benefits of exercise for people with COPD:
- More efficient use of oxygen
- Stronger breathing muscles and using less energy to breathe
- Reduced shortness of breath
- Reduced anxiety and depression
- Improved self-esteem and self-image
- Increased physical endurance
- Increased energy levels and reduced fatigue
- Improved sleep quality and reduced insomnia
- Increased cardiovascular health and fitness
- Improved muscle strength

It's not hard to see how getting regular exercise can help with depression caused by COPD. As you see your physical strength and condition improve, you are bound to feel more confident and more optimistic about your future.
Committing to exercising even when you feel down will also allow you to stave off some of the most devastating effects of depression for people with COPD—loss of physical strength and quicker lung function decline. It can also put you in a much better place both physically and mentally to cope with and manage your disease.
That's why it's so important to exercise according to your COPD treatment plan, even when it's hard and you don't feel like it. As soon as you start to neglect your exercise plan, you can quickly fall into a negative downward spiral, where it becomes more and more difficult to exercise.
If you find exercise difficult or don't know where to start, talk to your doctor about joining a pulmonary rehabilitation program. There are also many resources online, such as the Cleveland Clinic, that offer advice and ideas for specific exercises for people with COPD.

Here are some general tips and resources to help you exercise with COPD:
-
Start small and work your way up. Start by walking short distances or doing low-impact strength exercises, and increase the distance you walk and the number of repetitions you do by just a little bit every week. The improvements you make will motivate you to keep going and help you work up to more activity over time.
-
If you have limited strength or physical mobility, try starting out with some chair exercises. These allow you to work out different parts of your body while sitting in a chair, which helps with balance and reduces the amount of strength you have to expend while still toning your muscles. Check out this comprehensive guide for a huge list of chair exercises with accompanying illustrations and instructions for how to perform them.
-
Stretching exercises are easy to do and can improve your strength, mobility, and range of motion. You should always stretch before you workout, but you can also try stretching in the mornings and evenings to get some extra activity and keep yourself limber throughout the day. Check out this guide from Lung Foundation Australia that includes instructions for how to do a variety of different stretches.
-
Use breathing exercises, such as pursed-lips breathing and diaphragmic breathing to help with breathlessness and wheezing when you work out. You should also keep your bronchodilator, supplemental oxygen, and any emergency medications with you in case you need them. Check out this guide from the Cleveland Clinic on how to manage your breathing while you exercise.
- Try joining a fitness class or trying an exercise like yoga or Tai Chi. Having instruction (at a gym or from an exercise tape) can help you get started more easily and keep you motivated to continue. Yoga and Tai Chi are especially good exercises for people with COPD because they incorporate breathing control and meditation in their routines.
Eat Well

When you are depressed, you might not feel like eating as much as you should. It can also make you feel sluggish and unmotivated, making you more likely to reach for convenient, unhealthy options, like fast food, instead of making nutritious meals at home.
But when you have COPD, proper nutrition is vital for keeping your body and lungs healthy. Lungs affected by COPD use up more energy when you breathe, meaning that many patients actually need extra calories to keep their lungs working efficiently.
Eating well is also important for improving depression, as the foods you eat can have a huge impact on both your body and your mind. If you eat unhealthy foods or let yourself become malnourished, you will feel even more tired, fatigued, and depressed.
A variety of nutritional deficiencies and imbalances can contribute to depression, including deficiencies in fats, amino acids, Vitamin D, and blood sugar imbalances. However, proper nutrition can help restore balance to your body and mind, giving your brain the vitamins and nutrients it needs to keep you happy and healthy.

Unfortunately, the symptoms of COPD often make it difficult to maintain a healthy weight and get enough nutrition. However, having a healthy BMI is important for managing the disease; obese COPD patients face a wide variety of health risks, while underweight patients are also more likely to experience more rapid physical decline and other health complications.
Some COPD patients find it difficult to get enough to eat because of COPD symptoms like breathlessness, which often are worse on a full stomach. If you are also depressed, you may experience a reduced appetite, reduced motivation, and reduced enjoyment from the taste of food, which makes it even more difficult to get enough calories and nutrients every day.
If you have COPD, you should think of every meal as an opportunity to strengthen your body and support the health and function of your lungs. Even though it can be difficult and time consuming, it's important to eat whole, home-cooked foods as much as possible so you have maximum control over what nutrients you put in your body.

Even though it might be difficult and require some adjustments to your schedule, you can find ways to eat healthy with minimal effort and discomfort. Here are a variety of tips and techniques for eating well to improve your depression and your COPD:
-
Increasing your intake of certain foods has been shown to help fight depression. These include foods containing Vitamin D, omega-3 fatty acids, vitamin D, vitamin C, magnesium, selenium, and B vitamins.
-
Avoid sugary drinks, caffeine, and fried foods, which can contribute to depression. Instead, increase your intake of water, healthy fats, complex carbohydrates, and whole fruits and vegetables. Here is a guide from Healthline to help you choose healthy, nutrient-rich foods for your kitchen.
-
To avoid feeling uncomfortable and breathless when you eat, have several smaller meals throughout the day instead of large ones. This will help you eat enough calories without ever feeling too full.
- Prepare meals and freeze them ahead of time to eat on days when you feel especially depressed or fatigued. That way, even when you don't have the energy or motivation to cook, you can eat a nutritious, home-cooked meal with hardly any effort at all.
Get Out, Socialize, and Have Fun

Being depressed tends to cause people to isolate themselves and give up on the hobbies and activities that used to make them happy. This is partially due to a lack of energy and motivation, and partially due to a feeling of helplessness and a perceived inability to enjoy things that used to be fun.
However, even when things seem bleak, it's important not to neglect the people, hobbies, and productive activities that used to make you happy. Even if it doesn't feel satisfying right away, being social and active can improve your depression and will likely feel more satisfying with time.
Depression has an uncanny ability to make you avoid the very things that you need the most in order to break free from depression. Just remember that, even though things may seem hopeless right now, you will be much worse off if you give up and drop out of life's activities.
When you feel like staying indoors and avoiding the world, try calling up a friend or family member instead. Often, simply talking to someone else can help to pull you out of the fog and give you a more positive perspective on life.
It's okay to take days off and focus on self-care, but it's important not to let yourself stay in bed all the time and avoid the people who care about you. If you make an effort to get out of the house and spend time with family and friends, you will find it much easier to cope with depression and COPD.

And remember, it's okay to talk to your friends and family about your depression and let them know that you need support. Most people who care about you will understand and be willing to support you when you really need them.
Having a support group of family and friends and activities will give you something to get out of bed for and live for everyday. So don't let yourself become isolated from the people and things that matter in life; once you break out of your bubble, you might just start to notice all the many things that make life worth living.
.png)
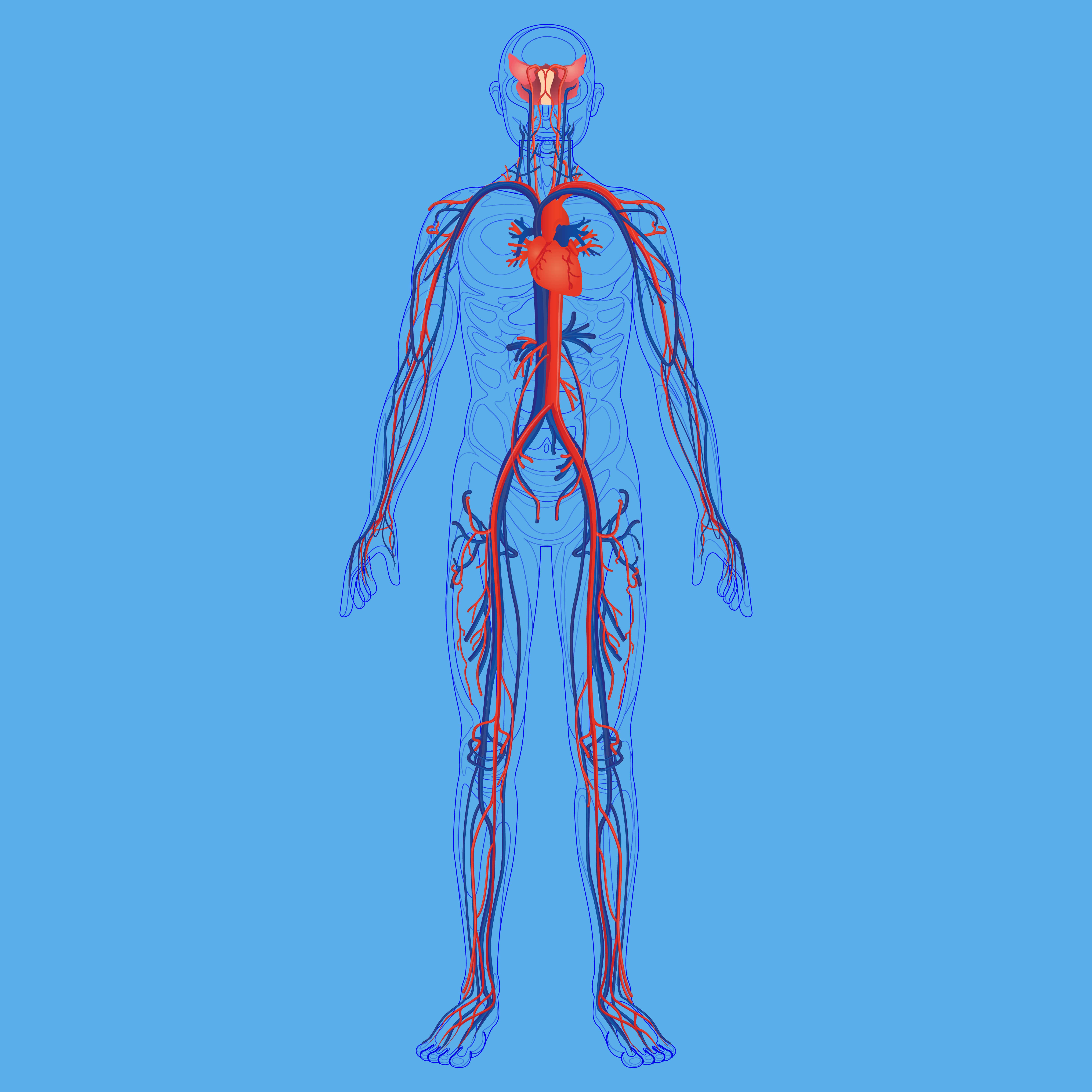
The medical term “localized disease” refers to a condition that is confined to one organ or system of the body. For example, an ear infection is a localized disease because it typically only affects the “middle ear” just behind the eardrum. While ear infections can spread to other parts of the body, this is very uncommon. A “systemic disease”, on the other hand, is one that has systemic manifestations. For example, diabetes is a disease that affects the level of glucose in your blood. Since every organ in the body is reliant on this blood, diabetes can have many systemic effects ranging from cardiovascular disease to nerve damage.
Traditionally, chronic obstructive pulmonary disease (COPD) has been considered a localized disease. Cigarette smoking either results in chronic inflammation in the bronchioles (chronic bronchitis), the lungs (emphysema), or both. But an increasing amount of evidence suggests that COPD should be re-labeled as a systemic condition rather than a localized one. Or at the very least, patients and medical specialists should treat COPD as if it were a systemic issue.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In this post, we’re going to help you understand the big picture of COPD. Instead of looking at respiratory symptoms associated with COPD like chronic cough, breathlessness, and chest pain, we’re going to focus on the systemic issues that can manifest as a result of this disease and why other respiratory diseases like asthma don’t put you at the same risk. If you have any questions, please address them in the comment section and we’ll get back to you soon.
Why COPD is a Systemic Disease
In the world of medical treatment, not everything is set in stone. Sometimes, medical specialists disagree on how to diagnose conditions and how to treat them both in the short- and long term. While it’s generally accepted that supplemental oxygen therapy, a revised dietary regime, and a pulmonary rehabilitation plan are the best ways to treat COPD, other aspects of the disease are not as clear-cut and straightforward. For example, some medical specialists may focus on treating the respiratory symptoms associated with COPD while others will focus on a more holistic approach that encompasses your systemic well-being.
While there’s nothing wrong with focusing on the respiratory symptoms associated with COPD, there’s an increasing amount of evidence to suggest that it can have equally adverse effects elsewhere in the body. The benefit of viewing COPD as a systemic disease is that it may help pulmonologists detect these symptoms early on and better understand how they are linked to COPD. Early disease detection is almost always associated with better outcomes for their patients. In the following sections, we’ll take a look at just a few of the systemic manifestations of COPD.
Systemic Inflammation
Inflammation is a natural part of your body’s immune response. It’s the way your body reacts to infection or physical injury. Essentially, the body sends white blood cells to the affected area which protect it from foreign invaders. When inflammation occurs it can cause the affected area to become red, itchy, and swollen. Acute inflammation plays an important role in healing the affected area, but if the inflammation persists longer than usual it can become chronic and can begin to cause serious damage to your tissues and organs.
Airborne irritants are one common cause of inflammation in the body. When pathogens are inhaled into the lungs, they become inflamed leading to coughing, chest stiffness, and chest pain. In the case of cigarette smokers who often inhale smoke once or more each day, this inflammation can become chronic and irreversible — this is known as chronic obstructive pulmonary disease. In the past, researchers believed this inflammation was localized, however, now there’s reason to believe that it can spread to other areas of the body.

The systemic inflammatory response associated with COPD is not fully understood, but there are a number of theories about how it starts. The first theory is that inflammatory mediators are transferred to the bloodstream from the lungs and are sent to other areas of the body. The idea behind this is that smoking increases the permeability of the pulmonary vessels, thus allowing inflammatory cells that would normally not cross over into the blood. This study found that people with poor pulmonary function experience higher levels of permeability than people with healthy pulmonary function.
Cachexia and Muscle Wasting
According to Medical News Today, about 25 to 40% of people with COPD experience weight loss. While many people are delighted to find out that they’re losing weight, the type of weight loss caused by COPD and other respiratory conditions isn’t usually healthy. The most common cause of this weight loss is a lack of appetite. COPD patients experience higher levels of fatigue and breathlessness than people with healthy lungs both of which can make eating a normal-sized meal exhausting and overwhelming. Oftentimes, respiratory patients reach for foods that provide them with a quick energy boost but likely don’t provide the body with the nutrients it needs.

Another reason for weight loss in COPD is that many people believe that they should be eating less food if they are less active than they used to be before contracting COPD. However, due to impaired lung function, COPD patients are actually expending a lot more energy than they realize because they have to work harder to get oxygen into their lungs and release carbon dioxide. Typically, doctors and dieticians will advise COPD patients to increase their calorie intake by about 430 to 720 each day depending on their weight and size.
One of the biggest problems with weight loss in COPD patients is muscle wasting, also known as muscle atrophy. This is when your muscles begin to deteriorate either due to a poor diet, lack of exercise, or both. This is a particularly dangerous side-effect of COPD because some people are under the impression that they’re losing fat when they’re actually losing muscle. This puts the patient at risk for falls, exacerbations, and other serious accidents.
Cachexia is a more generalized term to describe a state of “ill health” that results from having a chronic condition. If muscle wasting and weight loss occur quickly in a patient, it may cause them to feel sick to their stomach, dizzy, or confused. Your body might also have a difficult time adapting to your new lifestyle whether that involves a new diet, exercise routine, sleep schedule, etc.
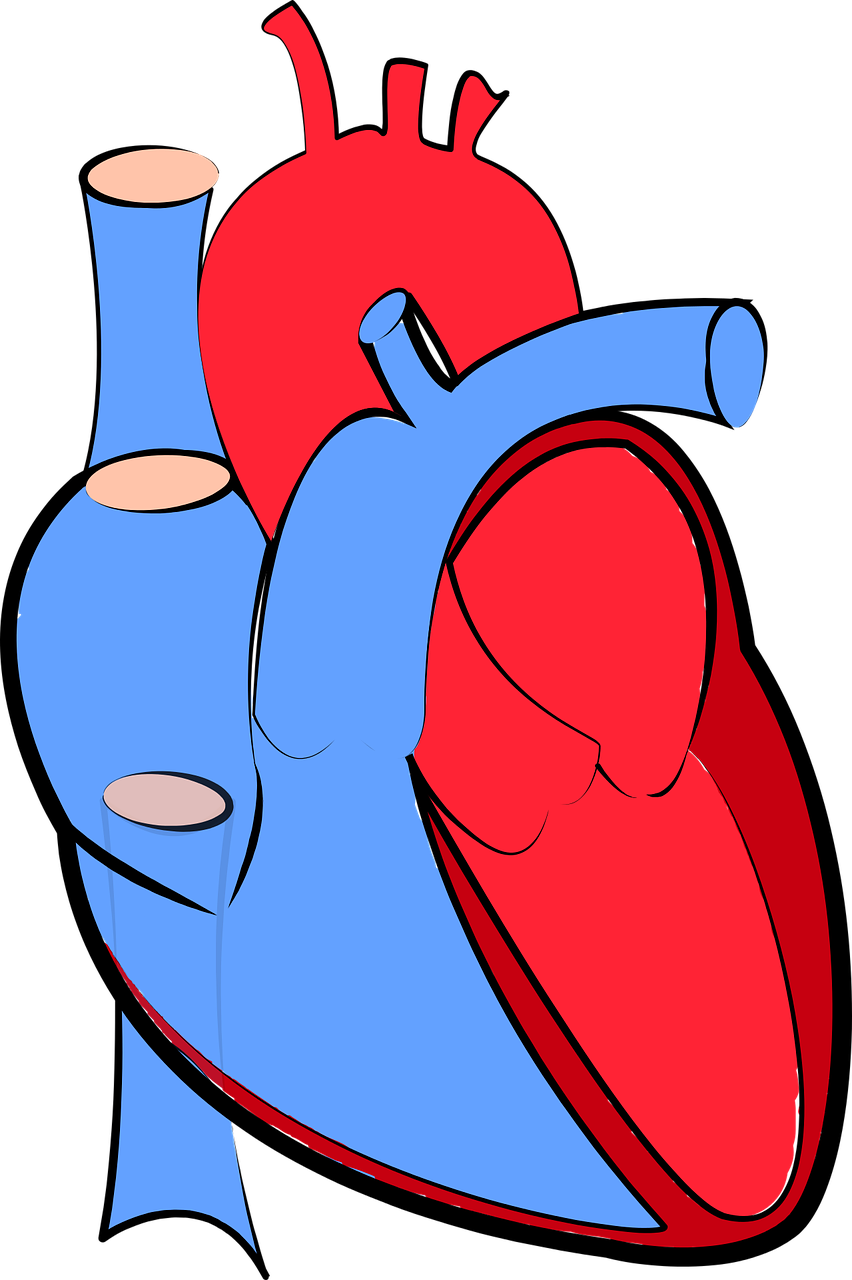
Cardiovascular Disease
Cardiovascular disease is the most common cause of death in the United States and globally. This is an umbrella term that describes disorders of the blood vessels and heart. Some common disorders include rheumatic heart disease, cerebrovascular disease, and coronary heart disease. COPD and cardiovascular diseases are often associated because they share similar risk factors and they act synergistically as negative prognostic factors. Pulmonary hypertension and ischemic coronary disease are two common progressions of COPD.
The lungs, heart, and circulatory system all work together to bring oxygen into the body and send it to each organ, so it makes sense that if the lungs aren’t functioning as they should, it’s going to cause problems with your cardiovascular system. One of the ways this can manifest is through hypertension, also known as high blood pressure. Hypertension is common in COPD patients and can worsen during exercise, sleep, or respiratory exacerbation. Combatting this underlying issue may put you at a much lower risk of cardiovascular disease.
Osteoporosis
Your bones play a vital role in the overall construction of your body. In order to keep bone tissue strong, it’s constantly removed and replaced. In an osteoporosis patient, the new tissue doesn’t generate as fast as it’s removed making the bones brittle and weak. This is referred to as low bone mineral density (BMD). Osteoporosis can lead to a number of symptoms such as joint pain and broken bones, but many patients will experience no symptoms at all. Osteoporosis is common in old age, but it’s even more common in people with COPD and other respiratory diseases.
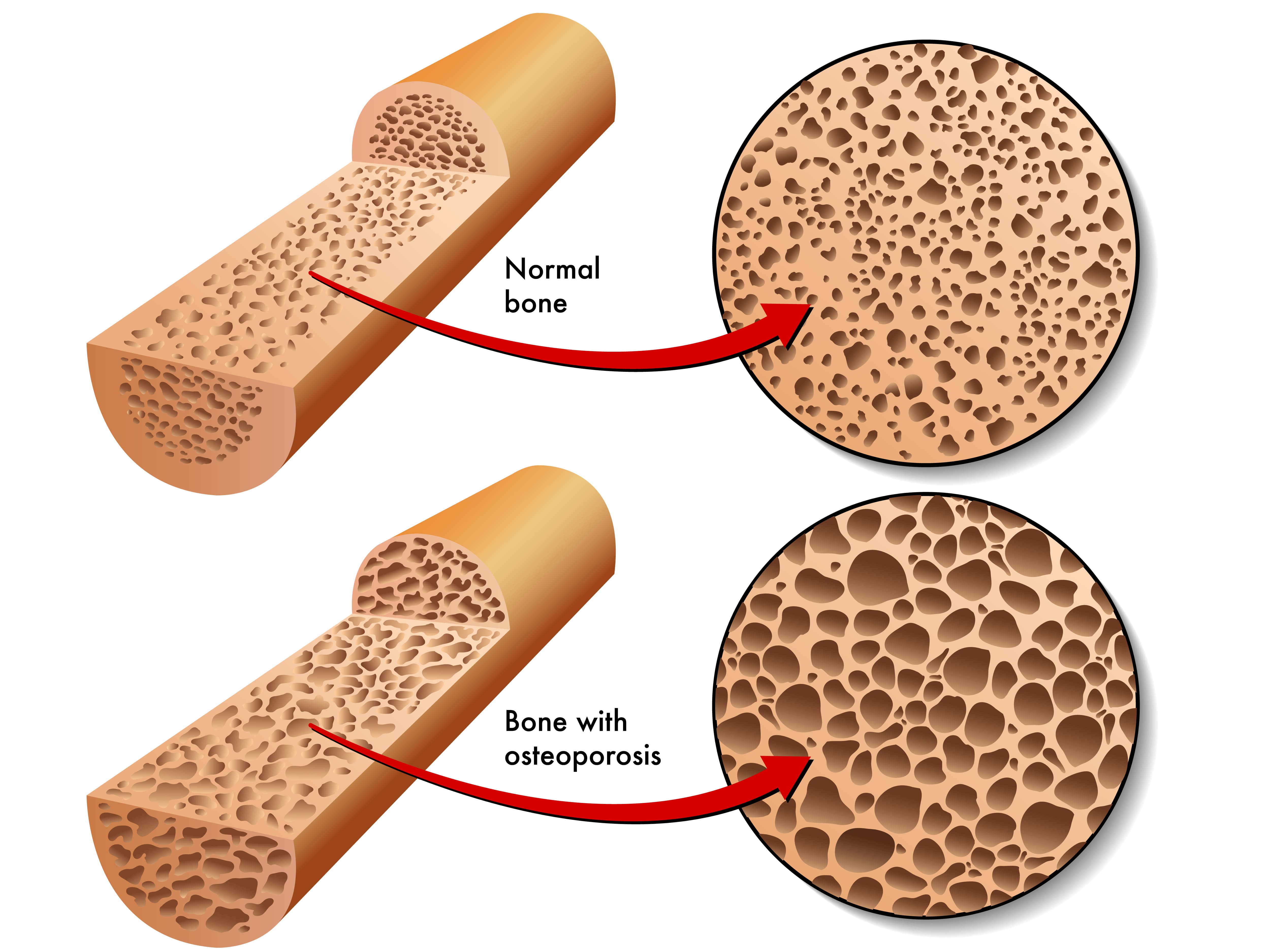
One cause of osteoporosis in COPD patients is the use of corticosteroids. This is a type of drug that’s used to reduce inflammation in the body, which in turn alleviates some of the symptoms associated with COPD. Corticosteroids have been found to affect the way body uses calcium and vitamin D to build bones. To counter this, your doctor may prescribe you a very low dose of corticosteroids. Ideally, it would be enough to treat your symptoms, but not enough to result in serious side effects like osteoporosis.
Anemia
Anemia is a condition in which your body doesn’t have enough healthy red blood cells. The primary function of red blood cells is to transport hemoglobin throughout the body. Hemoglobin is a chemical that carries oxygen molecules. Similar to not receiving enough oxygen in your lungs, anemia leads to feelings of dizziness, fatigue, and confusion. The reason anemia occurs more frequently in COPD patients is likely due to the abnormal immune response. Like we discussed earlier, COPD can lead to the release of inflammatory mediators in the blood. A specific type of inflammation-causing protein called cytokines reduces the lifespan of red blood cells and makes it more difficult for the bone marrow to produce more, thus resulting in fewer red blood cells.
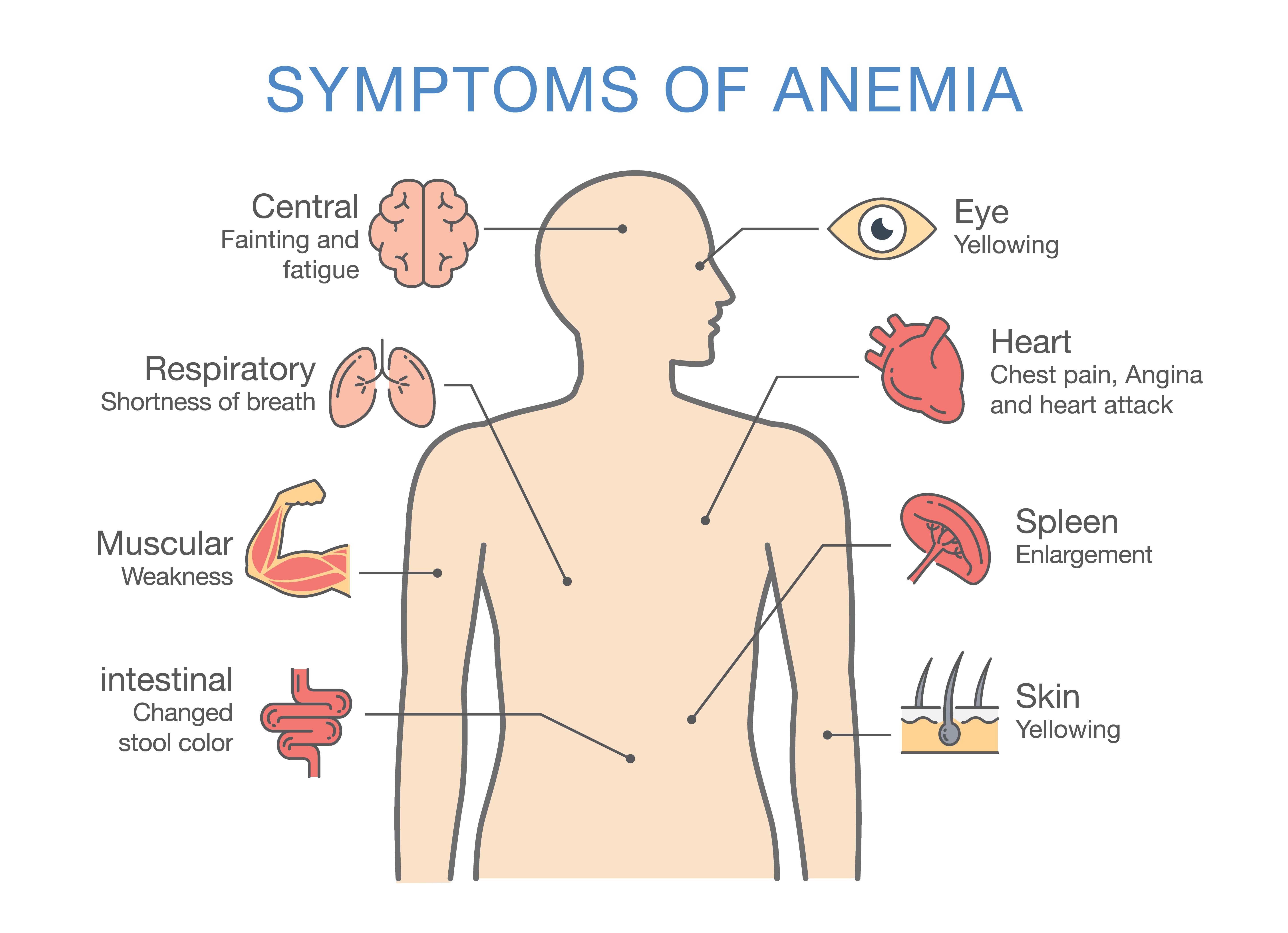
Another way that COPD can cause anemia is through iron deficiency. Iron is an essential mineral that your body needs to create hemoglobin, the chemical that carries oxygen and myoglobin, the protein that provides oxygen to the muscles. COPD patients may become iron deficient if their diets change enough that they exclude foods that are high in iron. This includes things like red meat, seafood, dark green vegetables, and beans. While anyone can develop anemia for a variety of reasons, it is more common in COPD patients. COPD patients with anemia are found to have worse outcomes due to respiratory exacerbations than those who are not anemic.
Anxiety and Depression
According to a study published in Health Psychology Research, not only do people with chronic illness have higher rates of anxiety, but anxiety rates are highest among people with obstructive lung disease as well as cardiovascular diseases. While there are many reasons why this could be the case, it’s likely mainly due to the way COPD affects your breathing. Studies have shown a strong correlation between anxiety and shortness of breath. There’s a negative feedback cycle where breathlessness can increase anxiety and anxiety, which in turn, creates tightness in the chest, causing more breathlessness. COPD patients can break this cycle by practicing breathing exercises. For more information on breathing exercises to reduce anxiety, read through this article.

Depression is another issue associated with COPD. About 40% of COPD patients have depression compared to about 6% of the general population. Depression can result from prolonged anxiety or it can be a completely separate issue. One of the most effective treatment options for depression is cognitive behavioral therapy (CBT). This is a type of psychological intervention that aims to pinpoint and reverse negative or inaccurate thoughts that can lead to anxiety and depression. CBT is being increasingly used by people with chronic conditions as a way to cope with the challenges of their disease. For more information on cognitive behavioral therapy, please read this article.
Conclusion
While on the surface it may seem like COPD is a disease that only affects your breathing, it’s actually far more complex than that. Your respiratory system plays a vital role in your holistic well-being and when you experience chronic inflammation in the lungs and low blood oxygen levels, this can affect your health in more ways than you think. Muscle wasting, cardiovascular disease, osteoporosis, anemia, and anxiety are just a few of the systemic manifestations of COPD.
If you’re concerned about how your COPD is affecting your heart, bones, or mental health, it’s important to address them with your pulmonologist. He/she may be able to perform tests or provide you with additional treatments that can put your mind at ease and ensure that you prevent any systemic conditions from occurring as a result of your COPD. What’s more, you should take care to follow your current treatment plan because this will help you manage your symptoms effectively.
In the meantime, if you’re on the market for a reliable, affordable, and easy-to-manage portable oxygen device, look no further than LPT Medical. We have a wide variety of oxygen concentrators to choose from including pulse dose portable oxygen concentrators, continuous flow portable oxygen concentrators, and stationary oxygen concentrators. We offer some of the latest models including the Inogen One G5, Caire FreeStyle Comfort, and Respironics SImplyGo. If you have any questions for our respiratory specialists, please don’t hesitate to give us a call or reach us by email.

Getting enough sleep can help your well being in a number of ways, your mental health, your physical capabilities, and so much more. But if you have sleep apnea, falling asleep, let alone sleeping through the night is an impossible task.
There are many reasons why people have sleep apnea, and understanding why you have sleep apnea is a critical step in treating it. Once you understand the root of the issue and what is causing it, you will be able to actively target the issue and hopefully get back to bed!
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In this blog we will discuss why sleep is so important, especially as you get older. We will also talk about sleep apnea diagnosis and the telltale signs that you should talk to your doctor about your sleep. Once you are diagnosed with sleep apnea, you may need to start using a portable oxygen concentrator while you sleep, so we will discuss your oxygen therapy options as well.
7 Reasons Sleep is so Important
![]()
1. Sleep Boosts your Immune System
It is important for your body to get the sleep it needs so that your immune cells are rested and strong to fight off allergies, germs, viruses and whatever aliment comes their way. Avoiding sickness like colds or the flu reduces your chance of ever experiencing a COPD exacerbation. The American Academy of Sleep Medicine suggests that sufficient sleep can also enhance vaccines effectiveness, which is obviously a plus, especially now that the COVID-19 vaccine has been rolled out in the United States, and it is crucial for COPD patients health.
2. More Sleep Will Help Shed the Extra Weight
Getting a full eight hours of sleep doesn’t mean you will wake up and lose the weight you need to, but sleeping can help your body from packing on extra pounds. Without sleep, your body produces something called ghrelin, a hormone that will boost your appetite, not great if you want to lose weight. Without sleep your body also will not produce leptin, a hormone that helps you realize that you are full, also not great for loosing weight. Not to mention, stress increases the likelihood that you will stress eat, and you might not have the energy to fight craving if you are stressed and under slept.
3. Sleep Can Strengthen Your Heart
Your heart loves sleep. Lack of sleep can cause your body to release something called cortisol which can lead to high blood pressure and heart attacks. Cortisol is a stress hormone that triggers your heart to work harder. Your heart also needs rest to function properly.
4. Better Sleep Means a Happier You
Good sleeping can lead to good moods. Simply waking up feeling rested helps your energy levels soar. This gives you energy to deal with whatever life throws at you, or it at least helps you deal with the obstacles and challenges in everyday life. Having the ability and energy to manage and deal with your emotions will help focus on the happier emotions.
5. Sleeping Can Increase Productivity
Getting enough sleep cultivates a healthy attention span and promotes concentration. Sleep also helps several other aspects of thinking including memory, problem-solving, creativity, emotional processing, and judgment, all of which promote success at work!
7. Sleep Can Increase Exercise Performance
Exercise is essential if you have COPD. Exercise promotes your lung and muscle capacity so you are able to do more everyday activities and tasks, and it also helps to slow down the progression of your COPD. Sleep is a form of exercise recovery, and recovery helps your hand-eye coordination, reaction time and muscle recovery. Plus, depriving yourself of sleep can have a negative impact on your energy level, and decrease your strength and power, both of which you will need to have a healthy COPD exercise regime.

When Should You Talk to Your Doctor About your Sleep
You should talk to your doctor about your sleep if you are not sleeping through the night on a consistent basis. If your lack of sleep is affecting your life while you are awake, you should contact your doctor to set up an evaluation. Your doctor will look at your signs, symptoms, and a sleep history. If you have a partner who shares a bed with you, their insight into your sleeping patterns could be helpful to know!

From there, you could be referred to a sleep disorder center. A sleep specialist can determine your need for further evaluation.
Diagnosing Sleep Apnea

To diagnose sleep apnea test will be conducted:
Nocturnal polysomnography is a test where you will be hooked up to equipment that monitors your heart, lung and brain activity, breathing patterns, arm and leg movements, and blood oxygen levels while you sleep.
Home sleep tests provide you with tools to diagnose sleep apnea at home. These tests usually measure your heart rate, blood oxygen level, airflow and breathing patterns.
Based on the results of these tests and how abnormal they are, your doctor might be able to prescribe a therapy without further testing. However, these tests do not always doesn't detect all cases of sleep apnea, and if your results are normal, your doctor might still recommend polysomnography to understand your sleeping condition further.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
If you have obstructive sleep apnea, you may have to go see an ear, nose and throat doctor to rule out blockage in your nose or throat.
However it is more likely that you have central sleep apnea because this is much more common, and if you have COPD it is likely that your sleep apnea can be tied to your respiratory condition.
Tips and Tricks for Sleeping Better if you have Central Sleep Apnea

People with chronic obstructive pulmonary disease (COPD) face distinct challenges getting enough sleep. COPD symptoms including coughing, pain and shortness of breath, all make it difficult to sleep. But as we mention in the section above, sleep is essential for COPD patients because sleep is important for resting your pulmonary muscles — and for simply functioning at a reasonable capacity.
COPD is not the only reason you are not sleeping well, there could be a number of reasons beyond these symptoms that induce sleeping problems. Understanding what these reasons are could help you find your way to a better night’s sleep.
Cut out mid day coffee or tea

Even though you may be tired from not resting enough the night before, that afternoon cup of coffee could be keeping you up. Having a cup of coffee or tea may help the afternoon crash problem you experience, but the extra caffeine late in the day could be impacting your ability to fall asleep that night, and that is a very counterproductive cycle.
Cultivate healthy sleeping habits
Make adjustments to your schedule and the ambiance of your bedroom to help improve your sleep. Start by limiting you napping because too much sleep during the day can disrupt regular sleeping patterns at night. Your naps should be no longer than20 minutes, this should help support your much needed night time rest.
![]()
Stick to a routine, this means going to bed and getting up at the same time every day. This will help reinforce natural sleep/wake cycles.
Elevating yourself by sleeping in a slightly upright position helps reduce stress on your lungs. It also can reduce acid reflux symptoms if you have trouble sleeping due to that.
Adjust your lifestyle
Adjusting your lifestyle means creating healthy habits.
First and foremost, if you smoke, get help to quit. Do not let anyone in your home smoke in order to keep your house free of secondhand smoke, dust, and pollutants. Your breathing is directly impacted by what you breathe in and when you inhale smoke, your air passages get smaller, which makes it harder to breathe.
Start an exercise program, you can join a pulmonary rehabilitation course to learn how to exercise effectively and safely. If you have COPD you can often experience drops in oxygen levels at night and in some cases you may need oxygen therapy while you sleep, but to avoid having to get on oxygen therapy, physical activity will help you build up your oxygen supply. Aim for 30 minutes of exercise a day, three times a week.
A sleep diary is very helpful for COPD patients who have trouble sleeping because it reminds you what works and what doesn’t. Write down what you ate that day, medicines you took, and activities for the day and then write down when you went to bed and woke up. Take a look at it after a few days and you will be able to see what helps you sleep better.
Getting ready for bed prepares you for sleep, even if you are not tired yet, start doing your bedtime routine at the same time every night, this will remind your body that it is time to start relaxing. Try these tips for relaxation:
- Take a warm bath to help your body reach a nice temperature for rest
- Journal or write a to-do list for the next day to clear your mind
- Relax your muscles with light stretching
- Listen to soothing music or a hypnosis recording
- Shut off your electronic devices an hour before bed
- Create a comfortable and cool space with a temperature between 60-71 F.
- Get rid of clutter as it can cause stress
- Aromatherapy with lavender can make it easier to fall asleep
Your sleep position is very important in terms of your lung capacity. Having a good sleeping posture helps open your airways making it easier to breathe. Sleep with your head slightly higher than the rest of your body rather than laying your head completely flat. If you sleep on your side, place a pillow between your knees and keep your back straight. When you sleep on your back, bend your knees slightly with a pillow placed under them.
Sleeping with an Oxygen Concentrator

Sleeping with a portable oxygen concentrator is something you will have to get used to doing. Your breathing pattern changes while you sleep, and you may breathe deeper when you sleep, or it is possible you have a shallower breathing pattern. That is why, if you use oxygen therapy while sleeping, your nighttime oxygen solution may differ from what you use for supplemental oxygen during the day.
Pulse dose portable concentrators can be an effective nighttime solution for some patients, and you can check with your doctor if your pulse flow device is sufficient in ensuring you have adequate blood oxygen levels while sleeping. But your doctor might determine your specific needs require a continuous flow portable oxygen concentrator. Your doctor will be able to perform a series of tests and studies in order to determine exactly what flow-setting you’ll need while you sleep, allowing you to choose your nighttime oxygen machine accordingly.

Once you know what nighttime oxygen machine you need, you can call 1(800)-946-1201 to speak with a respiratory specialist at LPT Medical. We will help you get the device that will cover your oxygen needs at the best possible price.

There are several portable oxygen options to choose from. If you have trouble sleeping, you can look into specific portable oxygen units that have certain features that make them better suited for overnight use. As long as they meet your prescribed oxygen needs, the concentrators discussed here are ideal for your nighttime oxygen solutions.
Best Pulse Flow and Continuous Flow Oxygen Concentrators for Sleeping in 2021

The Respironics SimplyGo is the most flexible option for you in order to satisfy both daytime and nighttime oxygen demands. This device was engineered with your travel needs in mind, so it comes equipped with three modes of oxygen delivery – Continuous Flow Mode, Pulse Mode, and Sleep Mode!
The SimplyGo can run off power from a wall outlet, a cigarette lighter or a charged battery, so you can transport your device with you anywhere. This is the most popular oxygen solution for those that who use sleep therapy equipment, such as a CPAP machine, in conjunction with oxygen.
The SimplyGo is ideal for your 24/7 usage and with its advanced ‘Sleep Mode’ technology you will be delivered a pulse dose of oxygen for a longer duration for a comfortable sleep. If you begin to breathe shallowly or through your mouth, the SimplyGo will automatically switch to the continuous flow mode, and deliver oxygen at 2 LPM to ensure you are adequately oxygenated.
This is something oxygen tanks and canisters will never have the capacity to do. This feature gives you peace of mind that you are being oxygenated throughout the night and getting better sleep for an overall better life.
Here are the SimplyGo specs:
- Pulse Settings: 1 to 6
- Continuous Liter Flow: 0.5 to 2 LPM
- Battery life: Up to 3 hours (on the setting of 2)
- Weight: 10 lbs (with battery included)
- Dimensions: 11.5 W x 10 H x 6 D (inches)
The Inogen One G5 may be a good option for your nighttime use if you are prescribed nighttime supplemental oxygen and approved pulse dose delivery. This is a smaller and lighter machine conducive to an active person’s lifestyle, or simply designed with ease and comfort in mind. The Inogen One G5 weighs 4.8 lbs and will give you 13 hours of pulse dose oxygen when paired with a 16-cell One G5 battery.

Beyond the benefits of its small and compact design, long lasting battery life, and powerful pulse flow settings, is the benefit of owning an oxygen device that provides extremely quiet operation, rated at 38 decibels. That means it won’t disturb you or anyone around you, while you’re asleep.
Here are Inogen One G5 Specs:
- Pulse Settings: 1 to 6
- Battery life: Up to 6 hr 30 min (with single battery)
- Weight: 4.8 lbs (with single battery)
- Dimensions: 3.26 x 8.15 x 7.19 (W x H x D in inches, with single battery)
Overview
The bottom line: you need to sleep well. Sleep is your beginning and the end of each day, so it is a massive part of your life and it should be treated as such, and pay mind to it. If you have trouble sleeping, speak to your doctor about steps you should take to sleep better. People who get less sleep tend to be heavier and are more likely to be diabetic. On top of that they are less energetic, experience bad moods, and lower productivity.
There are so many ways that you can get into a healthier rhythm of sleep, but if you have central sleep apnea, you will need to take added measures to start sleeping again beyond changing your daily habits and creating a sleep routine.
It may be necessary for you to go on oxygen at night. If so, you can get set up with a portable oxygen concentrator that is approved for nighttime use by calling 1(800)-946-1201.

Some would say it is as certain as death and taxes... allergies. They cannot be avoided, and it's something many people dread every year. If you suffer from any respiratory illness like COPD, asthma, or cystic fibrosis, allergy season is a bearer of bad news.
If you have respiratory issues, allergy season is not something you can take lightly. Breathing in allergens can influence COPD exacerbations or if you have another form of chronic pulmonary respiratory disease allergies cause increased discomfort and worse symptoms.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
COPD is one of the most common pulmonary diseases and it affects 16 million Americans. Allergies impact more than 50 million Americans every year, and many of those people also have COPD or other respiratory conditions that makes allergy season even more unbearable.
Allergy season starts in the spring and continues until the fall. Different allergens and the substances that trigger allergies, appear at different times of the year. Allergies also affect people differently, and in some cases one trigger, will not affect another.
During the spring months in March and April, tree pollen is the most common allergen, then by weeds and grasses.

From May-July all the trees, grass and weeds are creating allergens at the same time, making it a bad time for allergy sufferers. May is the beginning of peak allergy season which continues throughout July.
July to September is when ragweed starts to flower. This flowering plant is a lead cause of seasonal allergies, with 75% of all sufferers allergic to it.
October marks the end of allergy season, as the temperatures drop, and plants start to die, the air starts to rid itself of allergens, bringing an end to outdoor allergy season. While your normal respiratory symptoms will persist to some degree, at least they are not exaggerated by outdoor aliments.
![]()
Surviving allergy season
The best thing for respiratory patients to do is to minimize your exposure to allergens as best as possible. This means do not go outside when the pollen count is high or when the allergen you are allergic to is in bloom. You can utilize this Interactive Allergy Map to see what allergy conditions are in your area and get forecasts for tree, grass and ragweed pollen.
You can also try:
- To keep your pets in the house on high-pollen days so they do not drag pollen into your house.
- If you have an air filter already, be sure the screen is clean and change it often
- When you have allergy symptoms, such as itchy eyes or a runny nose, talk to your doctor about allergy medication. Taking an over-the-counter antihistamine may work for you.
- Medications such as diphenhydramine (Benadryl) and cetirizine (Zyrtec) can stop your immune response to allergy triggers and potentially lessening breathing difficulties
- You may need nasal steroids, decongestants, and inhalers to decrease your inflamed airway
- Buy a cabin air filter for your car that’s specifically designed to keep allergens out

Keep you home free of allergens by
- Install a good filtration system in your air conditioner
- Keeping your windows closed during allergy season or when the allergen forecast suggest the air is saturated with allergens
- Vacuum and dust regularly to get rid of any pollen or mold spores that may have gotten in from outside
- Get an air filter for inside your home
Talk to your doctor about your allergy symptoms and how seasonal allergies affect your COPD They may suggest a variety of options, which could include:
- trying a prescription allergy medication
- using your inhaler more often during peak allergy season
- getting an allergy test to see which allergens are causing your reactions
- trying allergy shots (immunotherapy) to reduce allergy symptoms
- Change your clothes when you go inside on high pollen days
- Keep windows and doors closed to reduce pollen entering the house
Continuing to Treat your Respiratory Illness

The most important thing you can do during allergy season is to continue to treat your condition to the best of your ability.
Treating your condition starts with you and ends with you, it is your responsibility to go to the doctors and get tested should your condition change. You should have the best oxygen equipment available to treat your condition in order to reap the many benefits of oxygen therapy. You can buy a portable oxygen concentrator with a built in filtration system that will help you breathe pure medical grade oxygen for the duration of allergy season.

You can purchase a new or used portable oxygen concentrators at LPT Medical, an oxygen equipment company based in Denver, Colorado.
Treating your COPD means continuing to exercise. You can find manageable home workouts that you are able to do indoors when high allergen counts are high.
Tacking your symptoms throughout allergy season is also important, so keep a detailed diary that explains when you took your COPD medications and your allergy medication, and note how it affects you. This will also help you keep track of whether or not your medication is giving you side effects.
Talking to your doctor is always a great place to start when it comes to your health, they will likely understand your condition the best, and be able to prescribe you allergy medication if you need it or recommend over the counter drugs that will help you manage allergies in conjunction with your disease.
Start by explaining your allergy symptoms and how seasonal allergies affect your COPD symptoms. They may suggest a variety of options, which could include:
- trying a prescription allergy medication
- using your inhaler more often during peak allergy season
- getting an allergy test to see which allergens are causing your reactions
- trying allergy shots (immunotherapy) to reduce allergy symptoms
Allergy Medication: Functions, Side Effects, and COPD
There are a lot of allergy medications, and it is important you discuss with your doctor before taking any medications because there could be side effects that negatively impact your COPD or other respiratory issues you may have.
Allergy medications can be taken as pills, liquids, inhalers, nasal sprays, eyedrops, skin creams and shots. There are over-the-counter medications and others that are prescription only, be sure you discuss with your doctor before using over-the-counter medications as well.

Here an overview of the types of allergy medications and why they're used and how they will affect you if you have COPD or another chronic respiratory illness.
Antihistamines
The purpose of antihistamines is to block histamine. Histamine is a symptom-causing chemical released by your immune system during an allergic reaction, and the goal of medication would be to suppress this reaction and make you more comfortable around allergens.
Antihistamines come in pill and liquid form and in over-the-counter and by prescription.
The function of antihistamine medications is to ease your runny nose, itchy or watery eyes, hives, swelling, and other signs or symptoms of allergies.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The side effects can make you feel drowsy and tired, and it should be taken with caution when you need to drive or do other activities that require alertness.
Antihistamines that tend to cause drowsiness include:
- Diphenhydramine
- Chlorpheniramine
These antihistamines are much less likely to cause drowsiness:
- Cetirizine (Zyrtec, Zyrtec Allergy)
- Desloratadine (Clarinex)
- Fexofenadine (Allegra, Allegra Allergy)
- Levocetirizine (Xyzal, Xyzal Allergy)
- Loratadine (Alavert, Claritin)
Antihistamine also comes in nasal spray forms to help relieve sneezing, itchy or runny nose, sinus congestion, and postnasal drip and does not normally cause drowsiness.

Side effects of antihistamine nasal sprays might include:
- a bitter taste
- In some cases drowsiness
Prescription antihistamine nasal sprays include:
- Azelastine (Astelin, Astepro)
- Olopatadine (Patanase)
- Eyedrops
Antihistamine eye drops are available over-the-counter or by prescription, and are used to treat itchy, red, swollen eyes. The drops can be made of antihistamines and other medicines.
Side effects of eye drops might include:
- headache and dry eyes.
If your antihistamine drops cause stinging or burning, you can put them in the refrigerator before you use them. The types of eye drops include:
- Ketotifen (Alaway, Zaditor)
- Olopatadine (Pataday, Patanol, Pazeo)
- Pheniramine and naphazoline (Visine, Opcon-A, others)
Antihistamines and COPD

Pretty much all nonprescription products have drawbacks, especially for those with respiratory problems such as COPD, asthma, wheezing, emphysema, or chronic bronchitis. It is prudent of the pharmacist to be aware that as a patient you have been diagnosed with a respiratory problem, and they can advise against the use of products including antihistamines, unless your physician has suggested that you do use them.
If you have COPD pharmacists can recognize your COPD through your profiles, and past prescriptions which may include inhaled bronchodilators, inhaled steroids, or other medications to treat your COPD.
All first-generation antihistamines are labeled asking patients to seek the advice their doctors before using this medication if they have COPD.
Antihistamines are not considered a treatment option for COPD but they are often used for seasonal allergies.
The benefits of taking on antihistamine could be outweighed by the negative impacts it has for patients with COPD, because drying effects of first-generation antihistamines, could dry out your mucus and inhibit the your ability to remove it.
Click here to read about coughing and clearing techniques for COPD patients
Decongestants

Decongestants are used for immediate yet temporary relief of nasal and sinus congestion that could be caused by allergies. There are side effects that can cause trouble sleeping, headache, increased blood pressure and irritability.
Decongestants come in pills and liquid form.Many decongestants, such as Sudafed, are available over-the-counter but should still be taken with caution.
Several oral allergy medications have both a decongestant and an antihistamine. Examples include:
- Cetirizine and pseudoephedrine (Zyrtec-D 12 Hour)
- Desloratadine and pseudoephedrine (Clarinex-D)
- Fexofenadine and pseudoephedrine (Allegra-D)
- Loratadine and pseudoephedrine (Claritin-D)
- Nasal sprays and drops
Nasal decongestant sprays and drops relieve nasal and sinus congestion but you can only use these for a short period of time. If you use these drugs for more than three consecutive days it could result in a cycle where your congestion gets worse. Examples of nasal decongestants include:
- Oxymetazoline (Afrin)
- Tetrahydrozoline (Tyzine)
Respiratory Disease and Decongestants
Decongestants are not recommended for people with high blood pressure, cardiovascular disease, glaucoma or hyperthyroidism. Experts will also advise against COPD patients taking antihistamines and decongestants because these medications can thicken your mucus, making it even more difficult to cough up.
Decongestants also can raise blood pressure, and some of the drugs that you may use to treat your COPD also raise your heart rate and the combination of this can be harmful.
Bottomline is these allergy medications should be used with caution. And it is a good idea to talk with your doctor about the best treatments for your allergies.
Overview
It stands to reason that if you’re experiencing a lot of coughing and sneezing due to seasonal allergies, it could be more difficult to cope with your day-to-day symptoms attributed to your COPD.
That being said, it is crucial you continue to treat your COPD, on top of taking care of seasonal allergies.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
If you suffer from seasonal allergies and have COPD, it’s important to follow your doctor’s orders regarding how best handle your seasonal allergies.
There is no cure for seasonal allergies, they can be managed. Reducing your exposure to allergens is by far the healthiest and most effective way to deal with allergy symptoms.
Beyond that, you can keep your home dust and allergen free by using an air filtration system, keeping your doors and windows closed, and minimizing the time your pets stay outside.
Your doctor may also be able to recommend an allergy medication that would help you manage your seasonal allergies if it is safe for you.
.png)
Mental illness is a growing problem in the United States. According to Mental Health America (MHA), 1.5 million more Americans experienced mental health issues in 2017 than the previous year. What’s more, surveys from the Centers for Disease Control and Prevention (CDC) indicate a sharp increase in self-reported behavioral health symptoms since the beginning of the COVID-19 pandemic. While there are many possible factors that are contributing to these issues, one of the lesser discussed factors is social isolation.
Social isolation is defined as either a partial or total disconnect from social networks. According to a report from the National Academies of Sciences, Engineering, and Medicine (NASEM), one-third of adults aged 45 and older feel lonely, and nearly one-fourth of adults aged 65 and older are considered to be socially isolated. Additionally, people with chronic illnesses — especially debilitating illnesses like COPD — can lead to a higher risk of social isolation and loneliness.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
COPD is often labeled as an “invisible illness” because it’s not always possible for an outside observer to fully understand what COPD patients are experiencing. While some COPD patients may be able to get around just fine and keep up with their friends, that doesn’t mean they aren’t experiencing adverse physical or psychological symptoms. In this post, we’re going to bring some awareness to social isolation and loneliness in COPD, why it happens, and how it can be prevented.
What are the Effects of Social Isolation?
According to a national survey conducted by Cigna, nearly half of the 20,000 participants reported feeling lonely. These numbers are concerning because there are a number of mental and physical health risks associated with loneliness. A study from Brigham Young University found that social isolation has as many health risks as having an alcohol use disorder or smoking 15 cigarettes a day and that it’s as harmful to mental health as obesity.

While the outlook for people experiencing social isolation and loneliness may seem grim, there is actually a growing amount of awareness surrounding the issue. People are beginning to associate the growing loneliness in society with the excessive use of technology and social media which is taking people away from face-to-face interactions. On the other hand, many people believe that social media is giving people experiencing loneliness an outlet to discuss these issues.
Why Do COPD Patients Experience Social Isolation?
Social isolation isn’t always as clear-cut as many people believe. While you may have an idea of a socially isolated person as someone who lives alone and doesn’t go out to visit people, this is only half of the story. There are many COPD patients who have close family members and belong to close-knit communities, but still, feel socially isolated. In order to understand this, let’s take a look at some of the reasons why COPD patients experience social isolation.

Chronic Pain and Fatigue
Chronic obstructive pulmonary disease affects an estimated 16 million people in the United States alone. However, no two cases of this disease are the same. While some COPD patients may be able to get out and do anything they want, others are held back by symptoms like chronic pain, fatigue, and persistent breathlessness. When this is the case, people often struggle to find the motivation to work through these challenges in order to get out and spend time with friends and family members.
![]()
COPD is a disease that develops slowly over the course of many years. So, it’s unlikely that will find yourself suddenly deciding to stay in rather than going out to meet people. Although, in many ways, this can be even worse than the alternative because you might not realize that you’re changing your lifestyle. Some studies estimate that about 70% of COPD cases are undiagnosed meaning millions of people could be experiencing social isolation due to a condition that they’re not even aware of. Oftentimes, the symptoms are shrugged off as a normal sign of aging.
Risk of Exacerbation or Infection
If we’ve learned anything from the past year it’s that viruses can spread quickly and they don’t affect all demographics in the same way. The novel coronavirus (COVID-19) hit the COPD community in a way that nobody could’ve predicted, and even now, over a year later, people are still feeling the effects of it. The Centers for Disease Control and Prevention (CDC) lists COPD as “high risk” for experiencing severe symptoms from COVID-19 and this rings true for many other viruses as well like the flu and viral pneumonia.
Another reason the COPD community has been hit so hard by the virus is due to the average age of people with this disease. It’s estimated that most people are at least 40 years old by the time they start experiencing COPD symptoms. But since COPD develops slowly, many people don’t start experiencing severe symptoms until they’re in their 60s. The CDC also states that people over the age of 65 are at high risk for severe COVID-19 symptoms, so this is a major factor at play too.

On top of the ongoing pandemic, COPD patients also have to worry about air quality. Highly polluted areas or places with a lot of allergens like pollen can result in respiratory exacerbation and even hospitalization. Because of this, it’s recommended that COPD patients plan their day so that they aren’t outside when air pollution is at its worst. Airnow.gov is a great tool if you want to quickly learn about the air quality in your area. Simply input your city or zip code and you will be provided with a number between 0 and 500 with 0 being no pollution and 500 being severely polluted. It’s recommended that COPD patients do not go outside if the air quality index (AQI) is above 100.
A Changing Lifestyle
Being diagnosed with COPD can be a life-changing moment. One day you’re following your normal routine, and the next your doctor is asking you to make a number of lifestyle changes to improve your health. A typical COPD treatment regime involves an improved diet, a pulmonary rehabilitation plan, and supplemental oxygen therapy which helps to keep oxygen levels stable. This can be somewhat overwhelming at first and will take some time to get accustomed to but it’s well worth the effort in the end.

One major lifestyle change that many people are unprepared for is moving into an assisted living facility or receiving in-home care. As COPD patients age, it becomes increasingly more difficult for them to maintain their independence, and oftentimes, friends and family members don’t have the means to be a full-time caretaker. While assisted living can be a convenient option for most people, it leaves open the possibility of social isolation and loneliness.
Social Stigmatization
The term “stigma” is the disapproval of someone based on their perceived characteristics. And although it’s a harsh reality to face, some people view people with chronic conditions as “less capable” even when these claims are completely baseless. The stigma surrounding COPD usually has to do with physical symptoms like coughing or wheezing or medical equipment like oxygen tanks or inhalers. But the bottom line is that it can make people with COPD feel like they don’t belong or aren’t able to keep up with the people around them.

What Can be Done to Prevent Social Isolation in COPD Patients?
Be Open About Your Experiences
The first step to solving problems like isolation and loneliness is to be more open about your experiences with your friends and family members. It’s not always easy putting into words exactly how COPD makes you feel and how it affects your mental health because you may not even be fully aware of how it has. However, by at least trying, you’ll make the people around you more aware of what you’re going through. What’s more, there’s a chance that your friends and family are thinking about the same thing but aren’t quite sure how to ask you about it.
Speak With Your Doctor
Another person you should be open with about your experiences is your doctor or pulmonologist. The reason it’s so important to tell your doctor is that he/she may be able to make adjustments to your treatment plan in order to help you get back on your feet and spend more time with loved ones. At the end of the day, there is no such thing as a “silly question” when it comes to your health. Chances are, many other COPD patients are dealing with a similar situation to yours, so opening up about your social isolation and loneliness will have a positive effect on the COPD community as a whole.

Your doctor might also be able to connect you with a mental health professional who can work with you step-by-step on how to prevent loneliness. Cognitive behavioral therapy (CBT) is a popular form of psycho-social intervention that aims to pinpoint and correct negative or inaccurate thinking patterns that can lead to loneliness. Of course, if the only thing holding you back is your physical symptoms, CBT won’t do much for you. However, if you feel like it’s mainly your mindset holding you back, CBT can work wonders. Many people around the world with chronic illnesses make use of CBT, so you’re not alone.
Embrace Online Communities
Like we mentioned earlier, there are many downsides to online communities. However, it’s impossible to deny the benefits as well. Older generations of Americans are becoming increasingly proficient with computers and social media which can be a great benefit for someone with COPD. Online communities such as COPD360Social hosted by the COPD Foundation or COPD.net’s help center are great for anyone who wants to share advice with other like-minded COPD patients. You might also consider Facebook groups which are free to join and participate in.
.jpg)
Make Use of Technology
In this day and age, we’re completely surrounded by technology wherever we go. While this can definitely be overwhelming at times, it can also be extremely beneficial if we take the time to learn how to use it. As a COPD patient, there are many technologies out there that can make your life much easier, it’s usually just a matter of finding what’s right for your lifestyle and budget. Mobility aids are a great example of a technology that can help you get back out and become a member of the community again. Walking canes, manual wheelchairs, electric scooters, and stairlifts all help you get around with more ease and also help prevent you from overexerting yourself and experiencing an exacerbation. Read this post to learn more about mobility aids for COPD.
.jpg)
Another technology you should consider investing in if you’re a COPD patient is a portable oxygen concentrator. These concentrators work similarly to your supplemental oxygen tank, however, they’re much lighter, smaller, and easier to use. Portable oxygen concentrators are electronic devices so you’ll never need to call an oxygen company to come refill them. You simply need a full battery and you’ll have access to oxygen wherever you go. Another benefit of POCs is that they don’t have the same social stigma attached to them as do oxygen tanks so you’ll feel more confident and secure with your new POC.
Conclusion
COPD is a chronic respiratory disease characterized by breathlessness, chronic pain, and fatigue. It’s the leading cause of morbidity and mortality in the world. Despite this, many people with COPD are suffering from “invisible” symptoms like anxiety, depression, and loneliness. In this article, we took a close look at how social isolation can affect both COPD patient’s mental and physical well-being, as well as offering some insight into how to remedy this. Fortunately, there are many steps that someone can take to prevent loneliness with COPD.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
If you’re looking for more great information that will help you manage the symptoms of your COPD, stay tuned to our blog here at LPT Medical. We try to cover a lot of topics that are under-discussed in the COPD community like the mental health aspects of the disease. If you have any questions or thoughts, feel free to leave them in the comment section below. And in the meantime, if you’re looking for an oxygen device that meets all your needs, take a look at our portable oxygen concentrators. We offer some of the top-rated concentrators on the market including but not limited to the Caire FreeStyle Comfort, Inogen One G5, and Respironics SimplyGo.
If you’d like to speak with an oxygen concentrator specialist please call us or send us an email.
.png)
Supplemental oxygen therapy is a foundational part of most COPD treatment plans. The ultimate goal of oxygen therapy is to provide the lungs with a higher concentration of oxygen which helps ensure that your blood oxygen levels remain normal. While most COPD patients need to use supplemental oxygen at some point in their lives, the experience tends to vary from person to person.
If you’ve been on oxygen for some time, you know that there are good days and there are bad days. One day, everything may be working exactly as it should and you forget that you’re even on oxygen. However, the next day, you might experience discomfort with your nasal cannula, dryness in your nose, equipment failure, or any other number of issues. It’s during times like these that we begin to wonder if supplemental oxygen is too intrusive to be worth our time and effort.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
And while it’s true that oxygen therapy can be intrusive sometimes, the alternative can be far worse. Having low blood oxygen levels (hypoxemia) for prolonged periods of time can have devastating effects on the body including breathlessness, dizziness, confusion, and eventual organ damage or failure. Your body absolutely needs oxygen, so if you’re thinking about reducing your oxygen flow, be sure to consult your physician beforehand.
To help you cope with the unpredictability of oxygen therapy, we’re going to offer seven tips to get you back on the right track and experience peace of mind again.
Start With Choosing the Right Oxygen Device for Your Needs
If you get the sense that oxygen therapy is always an uphill battle, there’s a good chance that you have the wrong oxygen device for your needs. Unfortunately, the greatest strength of the oxygen industry is also its greatest weakness — there are too many options. Traditional oxygen tanks, liquid oxygen tanks, stationary oxygen concentrators, and portable oxygen concentrators are just a few of the options out there. And even once you decide which one is best for you, you’ll have many different brands and devices to choose from, all of which vary greatly in terms of what they offer the patient.

Take traditional oxygen tanks, for example. These devices have been around for many decades and they’ve provided millions of COPD patients with reliable oxygen. However, since the early 2000s, they’ve become nearly obsolete due to technological advancements in the oxygen industry. While oxygen tanks are still popular, most people prefer having a portable oxygen concentrator instead. Rather than being heavy, bulky, and intrusive like oxygen tanks, portable oxygen concentrators are ultra-lightweight, comfortable, and convenient. And most importantly, they provide patients with reliable medical-grade oxygen.

One of the most popular types of POC is a pulse dose POC. These concentrators closely track your breathing rate and administer oxygen only when you’re inhaling. In other words, your concentrator battery will last much longer than it would with a standard continuous flow concentrator because it isn’t having to constantly work to put out oxygen. The Inogen One G5 and the Caire FreeStyle Comfort are two of the most popular pulse dose units because they both weigh under 5 pounds, they have low failure rates, and they’re backed by some of the most reputable brands in the industry.
Choosing the Right Nasal Cannula
Aside from having the right concentrator, having the right nasal cannula is one of the best things you can do to make supplemental oxygen less intrusive. The nasal cannula is the part of the oxygen tubing that allows the oxygen to flow freely into your nose so that you can inhale it. However, as you can imagine, it can be quite annoying having the cannula in your nose all the time. Many people report experiencing irritation or dryness in their nostrils. Also, many people report experiencing irritation on their ears where the oxygen tubing rests.

The simplest solution to this problem is to use an ultra-soft nasal cannula that isn’t as abrasive as the standard cannulas. Many oxygen concentrators also have the option to add a humidifier to the device which prevents the nostrils from drying out after extended periods of use. There are also many different types of nasal sprays and lubricants on the market that you can apply before and after using your oxygen concentrator. However, be sure not to use petroleum-based skin products because these are highly flammable and will be made even more flammable as medical-grade oxygen is applied.
Find the Right Oxygen Accessories for Your Lifestyle
Everyone has a different lifestyle. Some people prefer to stay at home while others prefer to be out of the house as much as possible. So, it goes without saying that not everyone has the same oxygen needs. The amazing thing about portable oxygen concentrators is that they can be customized to different lifestyles with the use of different accessories. For example, if you own the Caire FreeStyle Comfort, you’ll be able to choose between the standard carrying case and the backpack. The former is better for people who want to minimize the amount of weight they’re carrying while the latter is great for anyone who wants to carry a lot of extra personal belongings.

Another decision you’ll have to make is what size of batteries you will need. Most portable oxygen concentrators out there come with several different sizes of battery and you can make a decision based on how long you typically stay out of the house. For example, the Inogen One G5 offers two different battery options — 8-cell and 16-cell. If you just take a quick trip out of the house to go to the grocery store, you might only need the 8-cell battery. However, if you travel around a lot, you might want the 16-cell battery which offers about twice the battery life.

If you’re someone who likes to take road trips, a DC charging cable is a must-have accessory. DC charging cables allow you to charge your POC via a car outlet which is incredibly handy if you’re going to be in the car for hours on end. The best part is that many POCs can be used while they’re charging, so whenever you leave the car to sightsee, you’ll have a fully charged battery to work with.
Take Some Time to Read the User Manual
Think of your portable oxygen concentrator user manual as your all-in-one guide for using your new device. It will teach you everything you need to know from turning the device on to adjusting the flow rate and understanding the different visual and audible alarms. While it may be tedious to sit there and read through the whole manual in one sitting, you should at least sift through it in order to learn the basics of how to operate it. This way, if you’re out of the house, you won’t be left to wonder what a specific button or function does.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Another important thing you’ll learn from the user manual is how to troubleshoot your portable oxygen concentrator. Troubleshooting refers to the steps that you take if something should go wrong in order to remedy the issue. You’ll be surprised to find that the majority of issues that portable oxygen concentrators have can easily be solved with a quick fix. Since POCs are electronic devices like computers, simply turning the device off and then on again can solve a lot of issues, so it’s often the first thing you should try when something goes wrong.
Keep Up With Device Maintenance
Like with any oxygen therapy device, it’s important to take care of your portable oxygen concentrator. The good news is that maintaining a POC is much easier than many people realize and it won’t cost you an arm and a leg to do it either. One thing you should do regularly is clean your device. As you can imagine, when you’re carrying your POC with you everywhere, it can start to gather dirt and germs which could make you sick or even damage the device. Simply wipe your device down with a disinfectant wipe once or twice a week and make sure you don’t get any of the electrical components wet. You should also be sure to take off the particle filter occasionally, wash it off, and replace it because this protects the internal components of the POC and also purifies the air you breathe.

Two other components you should replace regularly are your nasal cannula and your sieve beds. The nasal cannula needs to be replaced regularly because it can get worn out over time and starts to get really dirty. The sieve bed is a special filter inside your POC that removes specific gases from the air like nitrogen which enables you to receive medical-grade oxygen. If the sieve beds are in poor condition, you may not be receiving the oxygen you need to stay healthy. Every device is different, but generally speaking, you should replace the sieve beds every year or two. Ideally, your nasal cannula should be replaced every two weeks.
Plan Your Trips Carefully
You would not be making full use of your portable oxygen concentrator if you didn’t get out of the house and enjoy the freedoms that you used to before starting oxygen therapy. There are near endless possibilities when you own a POC, but it’s still important to be prepared every time you leave the house. For example, if you leave the house without fully charged batteries, you might find yourself in a difficult situation where you either have to find a place to recharge them or return home earlier than expected. The best way to prevent this is to always know how long you will be out of the house. Make sure you have enough battery life to get you through the day plus a few extra hours to account for any change of plans.

One thing that’s really handy to have on long trips away from home is an external battery charger. Most portable oxygen concentrator batteries need to be attached to the unit in order to be charged. This means that you can only charge one battery at a time. However, with an external battery charger, you’ll be able to charge two batteries at once. This is very useful if you’re going to be on the go a lot and don’t want to sit around waiting for your batteries to charge.
Speak With Your Doctor
Last but certainly not least, you should speak with your doctor if you’re having trouble incorporating oxygen therapy into your life. Your doctor should be the first person you contact if you’re thinking about making changes to your oxygen treatment plan because he/she will be able to tell you whether or not it is safe to do so. Many people believe that if there are no immediate symptoms caused by reducing their oxygen flow, then it’s safe to do so. Unfortunately, this is not the case. Although you may feel fine at first, prolonged hypoxemia can cause a lot of harm to your body including dizziness, confusion, and even organ damage. By talking to your doctor you may be able to work out a treatment plan that takes into consideration both your comfort and your long-term health goals.

Conclusion
Having a reliable supply of medical-grade oxygen is essential for any COPD treatment plan. Unfortunately, many people end up purchasing the wrong oxygen device for their needs and find that it’s too intrusive for it to be worth their time and effort. This is why it’s recommended that COPD patients use small, lightweight, and convenient portable oxygen concentrators like the Caire FreeStyle Comfort or the Inogen One G5. After using a POC for the first time, many patients realize that oxygen therapy doesn’t have to be intrusive or cause stress in their lives.
Here at LPT Medical, we take your oxygen needs very seriously. We don’t want you to be stuck with an oxygen device that you’re unhappy with or that isn’t meeting your needs. This is why we have a team of oxygen concentrator specialists who will take the time to understand what you’re looking for, then align you with the oxygen device that will best suit your individual needs. We also have a number of financing and buying options available. Contact us either by phone or email to learn more.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!














