-png.png)
If you were to honestly ask yourself: What stops me from exercising? And your answer is that your COPD makes it too hard for you to breath, this article is for you!
If you have COPD, symptoms like difficulty breathing and muscle fatigue are most likely the main reasons you avoid from working out or beginning an exercise program in the first place. This is unfortunate because the best way to improve exercise tolerance and decrease breathlessness in COPD is to be active.
If you do not already know this, doing something active everyday is one of the best ways to treat COPD, and reduce your experience with symptoms while also slowing down the progression of your COPD, thereby adding years to your life.
If you're finding it difficult to exercise with COPD, try accomplishing some of these methods in this article to help improve your endurance and boost your energy levels, improving your well-being overall.
Talk to Your Doctor

Before getting into a new workout regime, speak with your doctor about exercise and your COPD.
It is important to review your health status and go over the specifics of your medications with your doctor. After this, your doctor may also suggest you take an exercise tolerance test (ETT). This test will measure your endurance and your overall ability to exercise.
Based on the results of your ETT your doctor should be able to help you organize an exercise program. This personalized exercise program will depend on your abilities, lung capacity, and COPD severity.
You exercise program should include a variety of stretching, strength training, and cardiovascular exercises, along with some light interval training.
A exercise program that will enhance your tolerance for physical activity

Remember the whole idea of beginning an exercise program is to build up the endurance you need to live a healthier and longer life with COPD. This means that you should start small, and do not try exercises that cause you to feel overwhelmed or exhausted.
In no time, you will begin to notice your capabilities are growing, but this will not happen overnight. Be patient and kind to yourself in the first few weeks, and your body will thank you for it!
Breathing exercises
You should practice certain breathing exercises, before performing any exercise program. Using breathing techniques while you exercise is a great way to help increase your lung capacity to be able to handle the added activity.
Breathing exercise can also be done while you are not doing any kind of exercise, because they help increase the capacity of your lungs which will also help reduce the symptoms associated with COPD.
Breathing exercise done regularly, can help make physical actives easier and more comfortable.
Breathing exercise include:
- pursed lip breathing
- coordinated breathing
- deep breathing
- huff cough
- diaphragmatic breathing
While you are exercising, always breathe slowly to save your breath. Inhale through your nose by keeping your mouth closed. This will warm up, filter, and moisturize the air you breathe in. Exhale your breath through pursed lips.
By breathing out slowly and gently through pursed lips you will develop more complete lung actions, strengthening your lungs and improving the quality of each breath you take.
Also remember, exercise will not harm your lungs, even when you experience shortness of breath during an activity, this means that your body needs more oxygen. If you slow down your breathing and concentrate on exhaling through pursed lips, you will restore oxygen to your system more rapidly, thereby makes the activity more comfortable.
Stretching and Flexibility

Stretching exercises are movements, postures, and poses that extend your muscles and ligaments. That being said, it is very important to “warm up” before you stretch. If your muscles are cold and tight, you may pull or tear muscles by stretching them out.
Think of your muscles as rubber bands, when the rubber is warm the band can continue to stretch further without tearing. If you freeze the rubber band and continue to stretch it out, it will tear or rip in half very easily.
If you consistently practice yoga and other stretching exercises where you are slowly lengthening your muscles, it will increase your range of motion and flexibility. It is a good rule of thumb to stretch before and after any cardiovascular exercises to prep your muscles for activity, thereby preventing the risk of injury, and after, to cool down and prevent muscle strain, and soreness.
Strength-Training Workouts

Strength training exercises are done by repeatedly contracting or tightening your muscles until they become tired. This can be done using weights or doing body weight exercises. With COPD, it is good to focus on doing upper-body strengthening exercises, as they are especially helpful in improving the strength of your respiratory muscles.
Also by focusing your exercise program on strength training exercises this will result in less shortness of breath, and a great substitute rather than trying to do more cardio workouts. You are likely less able to tolerate much cardio with your COPD.
Aerobic Workouts

Cardiovascular or aerobic exercises include walking, jogging, cycling, rowing, dancing, and water aerobics, all of which utilize large muscle groups to strengthen your heart and lungs. This work will improve your body’s ability to use oxygen.
These exercise will be difficult at first, especially with your COPD, however research shows that getting regular cardiovascular exercise can improve your breathing and decrease your heart rate and blood pressure.
Interval Training

During interval training, you repeat sequences of high-intensity exercise scattered with light exercise and some periods of rest.
For example, you may walk for 30 seconds, rest for 1 minute, then walk again for 1 minute, and rest for 2 minutes, and repeat the cycle for a total of 10 minutes. This training will allows you to catch your breath after more vigorous exercise.
Interval training in COPD patients is often used as part of a pulmonary rehabilitation program.
How often should you exercise if you have COPD?
The duration and the amount of exercise you need is completely dependent on your skill set. If you were always an athlete and have a higher tolerance for exercise already, you will need to exercise more frequently than someone who has never been interested in physical work outs before.
In order improve your tolerance for exercise you have to understand what you base level of physical activity is to begin with.
The frequency of your exercise program is how often you complete all of the exercises listed about. On average, to achieve maximum benefits, you should gradually work up to an exercise session lasting 20 to 30 minutes, at least 3 to 4 times a week. By exercising every other day you will be able to keep a regular exercise schedule, and by giving yourself a rest day in between, you will not get burnt out.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
How can oxygen therapy help to improve exercise tolerance?
If your health care professional has told you to use supplemental oxygen while doing activities, you should also use oxygen with exercise. Your usual oxygen flow rate (the number you set on your oxygen machine) may not be enough for you during exercise.
If you are preparing for an exercise program, speak to your doctor about the supplement oxygen requirements you have, and how to adjust you oxygen intake when you are exercising to match the recommended dose of oxygen you need for exercise.
If you do not already have a portable oxygen concentrator (POC), these little light-weight yet powerful machines are perfect for preforming any kind of physical activity.
For example the Caire Freestyle Comfort Portable Oxygen Concentrator only weighs 5 pounds and can operate at a pulse flow setting from 1 to 6. If your favorite form or physical activity is walking, having a POC that can join you will only incentivize you to walk further and more often!

The Caire Freestyle has a concave side to fit around your hip when you are carrying it across your shoulder. The carrying case is open at the top, making it easy to adjust the controls and pulse flow settings at anytime.
On the lowest flow setting with the 16-cell battery, you’ll experience an astounding 16 hours of battery life! That’s 3 more hours than top-of-its-class portable oxygen concentrators like the Inogen One G5. What this means is that you’ll be able to stay out walking or exercising and about for longer without having to come back home to recharge your unit.
Speaking of the Inogen One G5, this unit is also great for exercise and physical activity. The G5 is 4.7 pounds and can be set at a pulse flow of 1-6, making it one of the most powerful but also the lightest POC on the market.

So as your breathing rate and requirements change depending on if you are laying in bed or exercising, the Inogen One G5 has the ability to satisfy your oxygen demands.
The One G5 also has extended longer-lasting battery life compared to other Inogen models, allowing you to be mobile and stay mobile for longer periods of time.
There are so many other options when it comes to selecting the best portable oxygen concentrator for your exercise requirements, as well as your daily life. In order to ensure you purchase the right unit for your lifestyle, first speak with your doctor.
Your doctor will inform you how much oxygen you need per minute (LPM or Lp/min), and the correct dose (pulse or continuous flow) of oxygen your lungs require to function properly. Your doctor will also write a prescription for supplemental oxygen which is required if you are purchasing a POC or home oxygen concentrator from a licensed distributor.
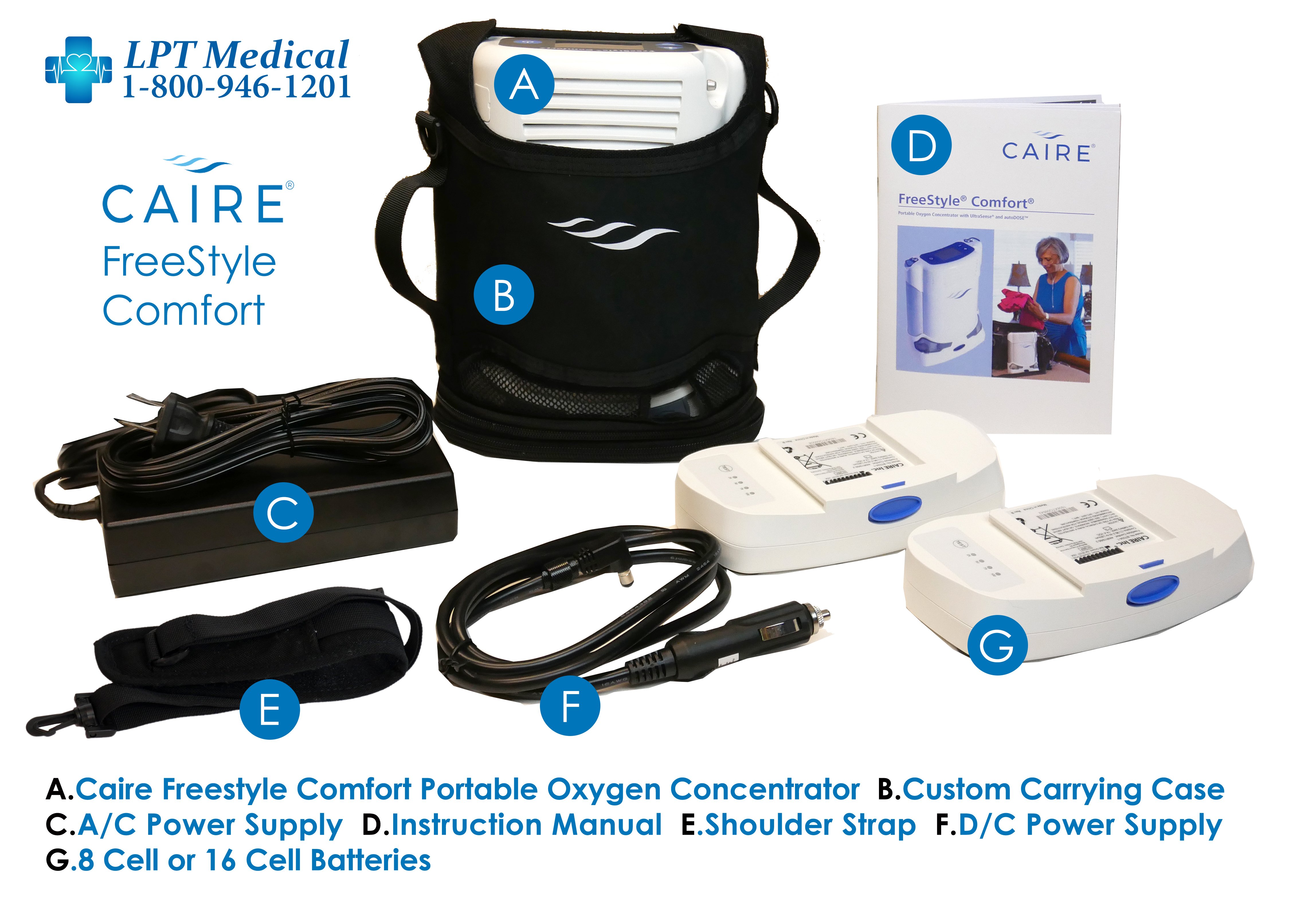
LPT Medical offers products from the most reputable manufacturers in the industry including but not limited to Inogen, Philips Respironics, Drive Medical, and more. These are the companies that are pushing the boundaries of what’s possible for patients suffering with a debilitating respiratory condition. And by offering these brands, we ensure that more people around the country have access to the most state-of-the-art oxygen therapy equipment in the world.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Stay motivated and continue to exercise
Exercise itself cannot cure or reverse COPD, but it can change the way you feel, breathe, and function.
Begin your exercise routine slowly by starting with easier exercises. Even if you think you want to push yourself and your limits, take it slow. Your muscles need to adjust to working like that!
The exercises you do should begin to get more challenging, and over time, you can walk faster for longer periods of time. Increase the amount of weight you use for strengthening exercises. And breathe better over-all. When you’ve reached the point that you’re feeling better and breathing better, keep this up every week at least three times a week.
If you are in the market for a POC, LPT medical is always here to help you find the best unit that will fit into your lifestyle and hopefully get you started or progressing further with your exercise program. To speak with a respiratory specialist call us at 1-800-946-1201.
.png)
Chronic obstructive pulmonary disease (COPD) is one of the most prevalent lung conditions, affecting more than 328 million people around the world and an estimated 16 million people in the United States alone.
Despite how common COPD is, it’s often overshadowed by other chronic illnesses like lung cancer, heart disease, and diabetes. A report published by the EMBO Journal found that, while COPD results in about 300,000 deaths per year — nearly double that of lung cancer — it received less than a third of the funding.
While the inequity in COPD research funding can only be addressed through political and social advocacy, healthy lifestyle choices remain the best way to prevent and treat COPD. And in order to make healthy lifestyle choices, you need to stay educated about how your lungs work. There are a lot of things to consider depending on what stage of your life you’re in and whether or not you’ve already been diagnosed with COPD.
In this post, we’re going to address some key facts about aging and how it affects the prognosis of people with COPD and those who are at risk of contracting COPD. In the meantime, if you are interested in getting tested for COPD, be sure to consult your doctor immediately to start discussing your symptoms.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
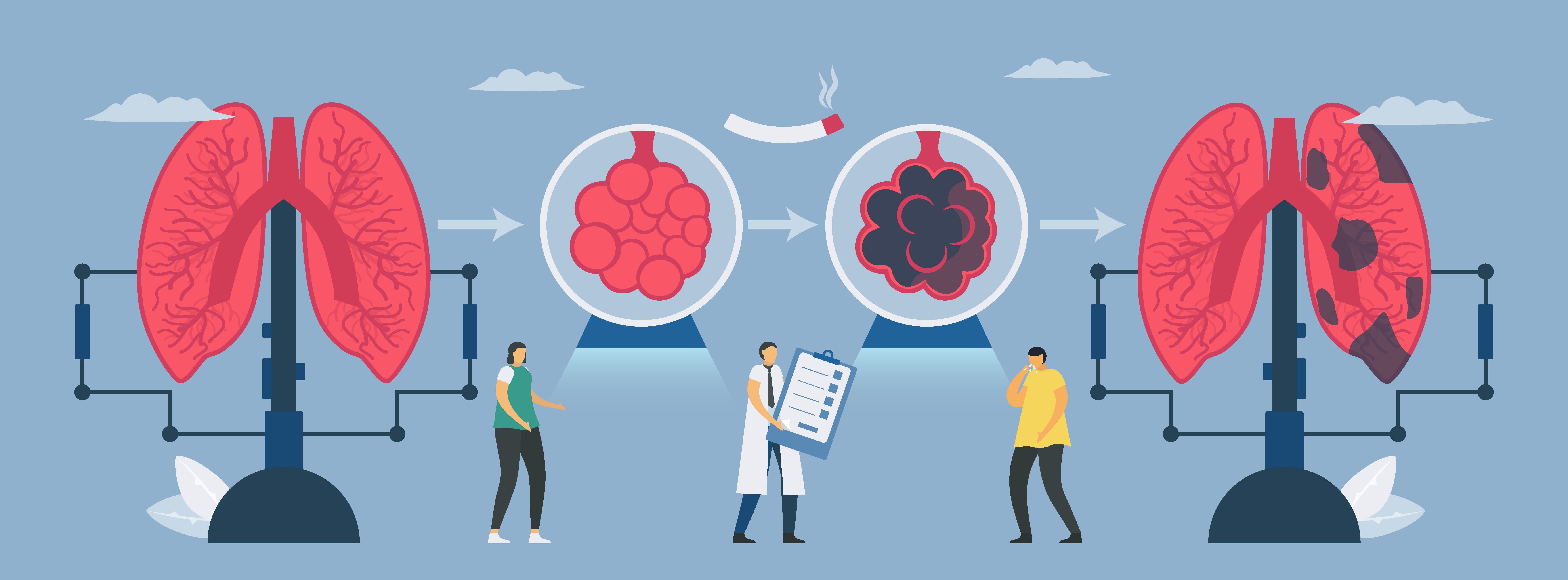
COPD Takes Several Years to Develop
One of the main differences that sets COPD apart from lung cancer and other chronic illnesses is the rate at which it develops. According to MedicineNet, small cell lung cancer is known to develop extremely quickly and can often result in death within 6 months if it is left untreated.
COPD is very different from this because you’ll see the disease develop over several years or even decades rather than over months. While smoking immediately results in symptoms like coughing, wheezing, and breathlessness, it takes several years before medical professionals can actually associate these symptoms with COPD.

Another factor contributing to the rate of onset of COPD is how many cigarettes you smoke and how frequently you smoke. While researchers aren’t entirely sure what amount of cigarettes will cause COPD, they do agree that even just one cigarette can cause permanent damage to the body.
Many people consider themselves to be “social smokers” because they only smoke when they’re with friends. These people may feel better about their habit because they feel more in control of how much they smoke, but the truth is, they may be at just as high of a risk of contracting COPD as a chronic smoker.

Another risk of being a “social smoker” is that you’re being exposed to a lot more cigarette smoke than you realize. A common myth about smoking is that inhaling second-hand smoke is more dangerous than actually smoking. This is not the case, but it is still equally damaging to inhale second-hand smoke, so you should avoid hanging out around people who smoke.
The key takeaway from this is that your body isn’t going to give you any major warning signs that you have COPD. Long-term symptoms of COPD are similar to the short-term side-effects of smoking which will mask any serious underlying issues you’re facing. The difference, of course, is that the symptoms you experience from COPD are permanent. The best way to avoid COPD is to quit smoking immediately and visit your doctor.
Underdiagnosis and Misdiagnosis are Common in COPD
Diagnostic error is a much more common issue than many people realize. According to Improveddiagnosis.org, an estimated 12 million Americans experience an inaccurate diagnosis in their life, and between 40,000 to 80,000 people die each year as a result of diagnostic errors in hospitals.

These are startling numbers, but you may be surprised to find that people showing signs of respiratory illness are some of the most commonly affected by diagnostic errors. Like we discussed in a previous post, COPD is not always an easy condition to diagnose. Inconsistencies in testing procedures like spirometry can throw off results and miscommunications between doctors and their patients can contribute to this.
One of the most common diagnostic errors is COPD patients being diagnosed with asthma. According to a study published in the National Jewish Health Journal, more than half of COPD patients may be misdiagnosed with asthma. This is not surprising, as both conditions exhibit similar symptoms such as coughing, wheezing, and shortness of breath.

The biggest danger of being misdiagnosed for respiratory symptoms is that you will receive the wrong treatment plan. Asthma is most often treated with fast-acting inhaled medication like bronchodilators which help to open up the airways and prevent asthma attacks. However, COPD treatment is more involved and includes things like supplemental oxygen therapy, long-acting inhaled medication, pulmonary rehabilitation, and an improved diet.
Someone who was misdiagnosed with asthma may live for years without being correctly diagnosed or they may never be correctly diagnosed with COPD. Another way COPD can be misdiagnosed is if a patient is diagnosed with asthma when they’re young. If respiratory symptoms increase with age, they may dismiss them as asthma symptoms, and never seek professional help.

The best way to avoid a missed or delayed diagnosis for COPD is to ensure that you’re always honest and upfront about your symptoms. It’s not normal to have a cough or chest pain that lasts more than a few days and asthma does not necessarily get worse with age. Visit your doctor often and don’t be afraid to ask a lot of questions.
Younger Generations Could be Less Predisposed to COPD
Not all news surrounding chronic obstructive pulmonary disease is negative. You’ll be happy to know that younger generations may be far less predisposed to contracting COPD than their parents and grandparents. This is primarily due to changing regulations surrounding smoking and pollution, and more stigma surrounding smoking at a young age.
![]()
On July 1, 2006, the Colorado Clean Indoor Air Act went into effect which banned smoking in public indoor places. This law was updated in 2019 to include the following:
- E-cigarettes and vaping are now included in the ban
- Originally, smoking was not permitted within 15 feet of a public building; this has been extended to 25 feet
- Exemptions for smoking areas in airports and hotels have been removed
While other states have their own rules and regulations concerning smoking and vaping, generally speaking, the country is moving in the right direction when it comes to lowering the risk of future generations contracting COPD, lung cancer, and other chronic lung conditions.
Another factor to consider is the increased social stigma attached to smoking. In the past, smoking was seen as stylish or cool, but over time, public perception of smoking has changed significantly. A study done by UC San Francisco and Stanford University School of Medicine examined the adolescent perception of smoking in 2001 versus 2015 and found that it’s largely looked down upon.
![]()
This study found that 94 percent of students in 2015 and only 65 percent in 2001 intended not to smoke and that only 17 percent of students believed smoking made them look more mature in 2015, as opposed to 27 percent in 2001.
Changes to environmental regulations could also play a major role in reducing COPD predisposition in future generations. Researchers have found that air pollution like dust, exhaust, fumes, and chemicals can all contribute to the onset of COPD, both in smokers and non-smokers. So, as we see a push towards cleaner or fewer emissions, we should see a corresponding drop in COPD cases all across the country.
Alpha-1 Deficiency Could Lead to Earlier Onset of COPD
Alpha-1 antitrypsin (AAT) deficiency is a genetically transmitted disorder that increases someone’s likelihood of contracting COPD. It occurs when there is a lack of the protein alpha-1 antitrypsin in the blood which the lungs use to reduce inflammation and infection in the lungs. Abnormal genes affect the way that alpha-1 protein is created and excreted from the liver.

Contrary to common belief, alpha-1 deficiency does not cause COPD in and of itself. However, it does make your lungs more susceptible to factors that can cause COPD. In other words, if you have alpha-1 deficiency and you smoke or you’re exposed to high levels of air pollution, you’re more likely to contract COPD, and you’ll likely contract it more quickly than someone without the disorder.
One of the biggest dangers of alpha-1 deficiency is that it’s fairly uncommon with only 100,000 cases in the United States. What this means is that doctors don’t typically test for it and it’s usually only discovered if you happen to have blood drawn for some other reason. AAT plays an important role in breaking down an enzyme called neutrophil elastase which is part of the natural immune response in the lungs. In a healthy person, these enzymes are controlled and cause no threat to the lungs, but in someone with AAT deficiency, it can cause permanent and irreversible damage.
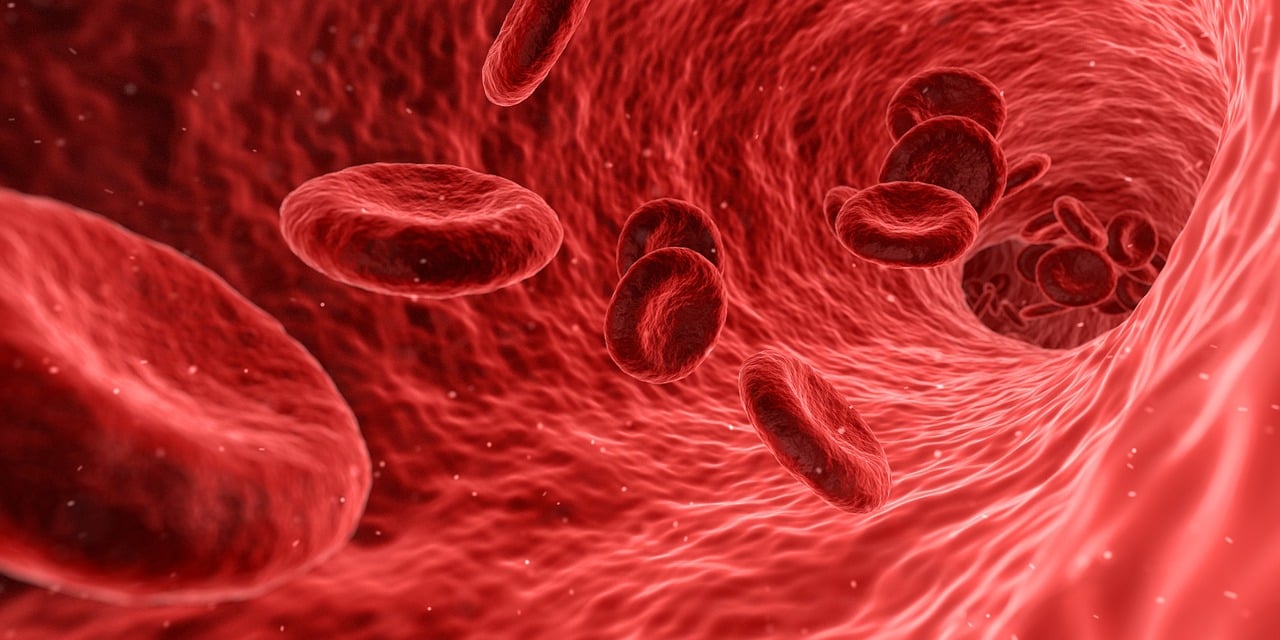
While rare, AAT deficiency simply reinforces the importance of getting tested as early as possible. There are many different treatment options for alpha-1 deficiency including augmentation therapy, which aims to infuse the missing protein directly into the patient’s blood. Other treatment options include vaccinations that prevent infections and an improved diet which promotes healthy lungs and liver.
COPD is Commonly Diagnosed in Late Adulthood
Even when COPD is diagnosed correctly, it’s usually only found in older adults. According to Healthline, of the 8.9 million Americans diagnosed with chronic bronchitis in 2016, 75 percent of them were over the age of 45. There are also stark gender differences with 5.9 million women receiving a diagnosis and only 3 million men receiving a diagnosis.

It’s estimated that about 40 percent of people with COPD have not yet been diagnosed. It’s safe to assume that many of these people are experiencing early stage 1 COPD and they are simply brushing off the symptoms as a sign of aging. However, it’s important to note that chronic coughing or wheezing are never symptoms of normal aging. COPD is often associated with recurring lung infections that can cause this.
No matter what age you’re diagnosed at, COPD treatment will look pretty similar. Since COPD is characterized by progressive lung inflammation and obstruction, your doctor’s primary goal will be to slow the rate of lung decline while simultaneously reduce your risk of exacerbation (a flare-up in your respiratory symptoms).
An improved diet is one of the primary treatments for COPD. Regardless of your age, your body needs a healthy balance of vitamins, minerals, and other nutrients in order to stay healthy. Your lungs depend on these in order to promote healthy blood flow, efficient breathing, and to help control inflammation which can cause chest pain and accelerate the progression of your disease.
Secondly, your doctor will likely set you up with a pulmonary rehabilitation routine. Think of this like a controlled exercise program that’s specifically designed to educate you about your lungs and how to train them for maximum efficiency. Of course, pulmonary rehabilitation will look different based on your age and what your physical abilities are. Ultimately, the goal isn’t to be an all-star athlete, it’s to keep your muscles in shape and improve your endurance so that you don’t feel out of breath so frequently.

Lastly, your doctor will look at medications such as supplemental oxygen, nebulizer therapy, and inhaled corticosteroids. Typically, patients with stage 1 or stage 2 COPD are instructed to use supplemental oxygen for several hours a day, whereas patients with more severe stage 3 or stage 4 COPD will likely need to use oxygen 24/7 in order to receive its full effects. Oxygen is effective at not only reducing COPD symptoms, but it can also reduce the likelihood that you will experience a COPD exacerbation. If you’re looking for an oxygen device for seniors, portable oxygen concentrators tend to be the best option because they offer the most freedom and independence.

A nebulizer is a small device that delivers medication as a mist that can be inhaled. Nebulizers are most often used by younger children or seniors who are not able to effectively time their breathing well enough to use an inhaler. They’re also much easier to use than oral medication which can be difficult to swallow. Some common drugs administered through nebulizer therapy include ipratropium bromide, cromolyn sodium, albuterol, levalbuterol, budesonide, and acetylcysteine.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Managing COPD is More Difficult in Seniors
Potentially the most urgent age-related issue associated with COPD is its effects on seniors. Old age is already associated with a number of issues such as joint pain, muscle pain, fatigue, and chronic health conditions which can only make coping with COPD more difficult. Generally speaking, the older your age, the shorter your life expectancy with COPD will be.
Joint and Muscle Pain
Chronic pain in the joints and muscles is more common than you may think. According to WebMD, about one in three adults have experienced joint pain in the past 30 days and this only gets worse with age. Joint and muscle pain can be brought on by an injury or one of many chronic underlying conditions such as osteoporosis, osteoarthritis, gout, or bursitis.

One of the ways these issues can affect COPD patients, in particular, is through reduced mobility. COPD is considered a debilitating disease meaning it makes you weak and feeble. Osteoporosis, a condition that results in weak, fragile bones, can contribute to COPD symptoms like rib or chest pain.
Respiratory Infections
Influenza and the common cold are two of the most common infections in the world. And as of late, we’ve been introduced to a new type of viral respiratory infection: COVID-19. While anyone can contract these illnesses, they’re more common in older adults and they can be far more deadly, especially when they’re combined with chronic diseases like COPD. According to the American Lung Association, you’re 7.7 times more likely to contract pneumococcal pneumonia (a type of bacterial pneumonia) if you have COPD and you’re over the age of 65.
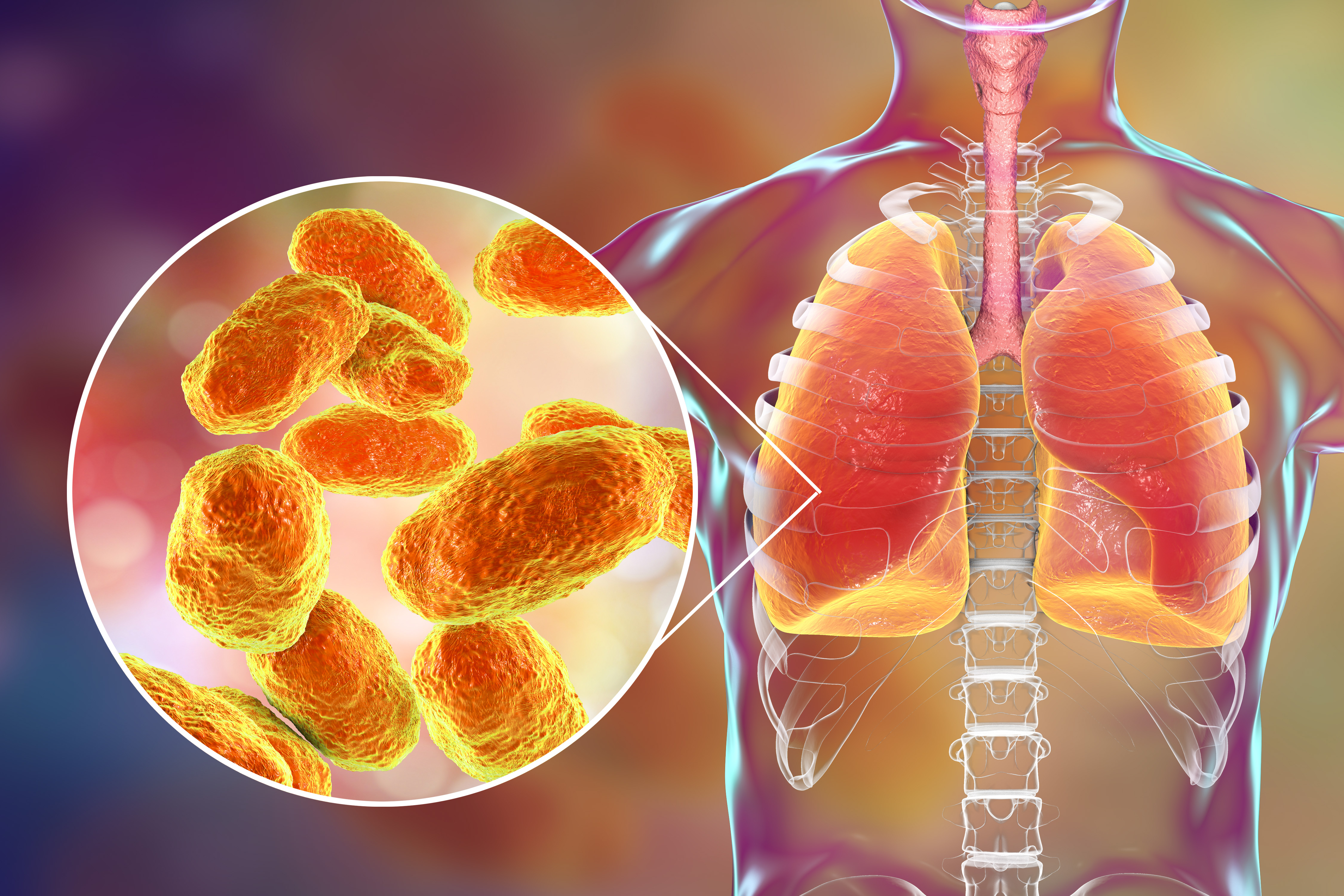
Since bacterial infections are responsible for around 40 to 50 percent of all COPD exacerbations, it is imperative that you do everything you can to avoid acute illness. Cleaning your home regularly with natural and safe cleaners is a great place to start, and you should visit a doctor immediately if you experience any unusual symptoms.
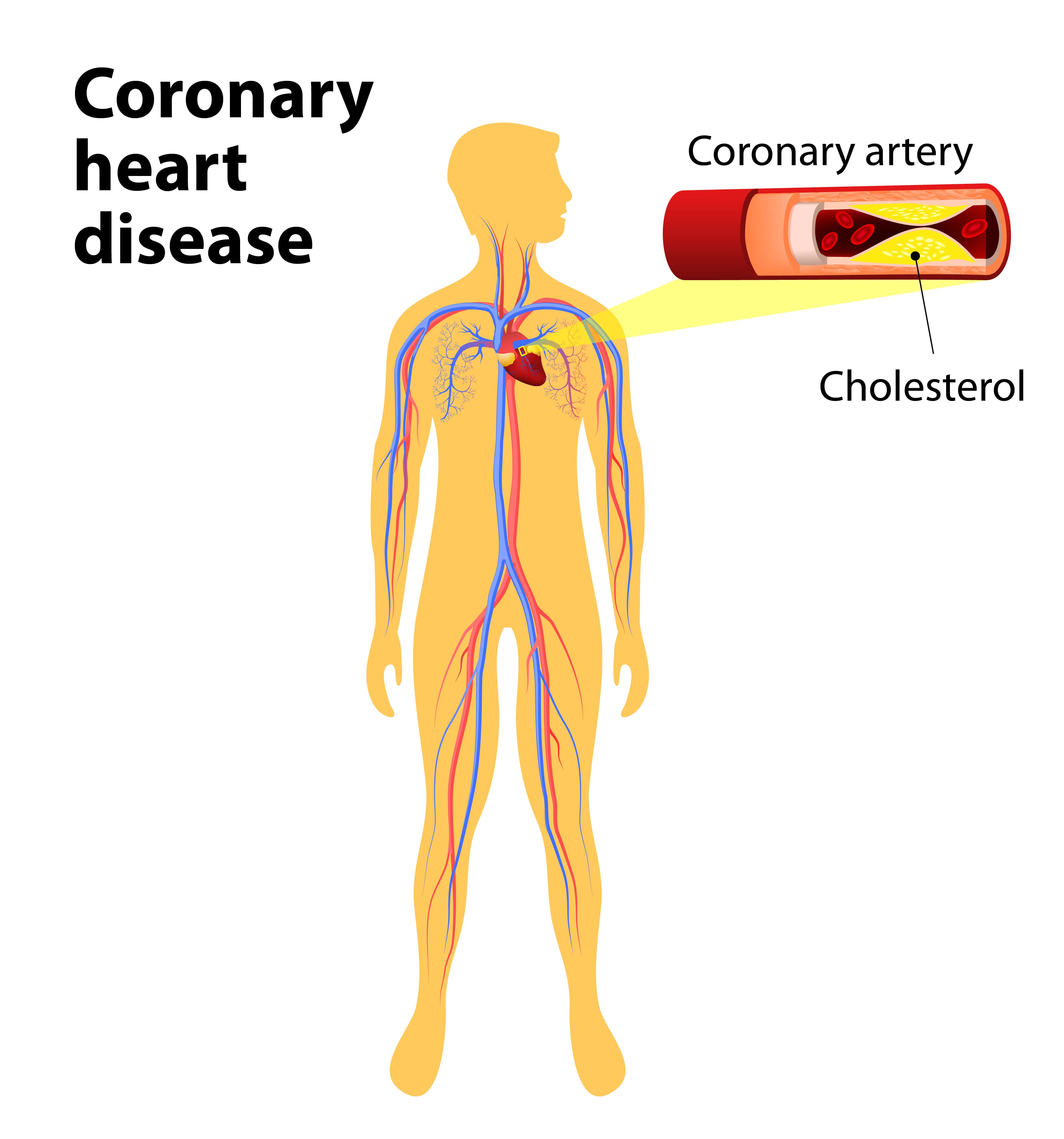
COPD Comorbidities
A comorbidity is a condition that exists alongside another one. Some of the most common comorbidities of COPD include obstructive sleep apnea (OSA), pulmonary hypertension, coronary artery disease, and heart failure. Sometimes, comorbidities can be treated with COPD medication or therapies, but other times, they require a separate treatment plan in order to address the underlying issues.
.jpg)
Obstructive sleep apnea is common. According to sleepapnea.org, between 11 and 19 percent of COPD patients have it and almost half of all COPD patients experience some type of sleep difficulty. If this is the case, your doctor may advise that you use supplemental oxygen therapy, CPAP therapy, or both that night in order to promote restful sleep.
Coronary heart disease is a condition that’s usually caused by the build-up of plaque in the arteries of the heart causing them to narrow and blocking blood flow. Just like COPD, one of the main causes of coronary heart disease is smoking, so it’s not surprising that having chronic bronchitis will raise your risk of contracting it by about 50 percent. Other risk factors of coronary heart disease include high cholesterol, systemic hypertension, and a high body mass index (BMI).
Conclusion
Chronic obstructive pulmonary disease is one of the leading causes of mortality in the world; It’s also one of the most preventable illnesses in the world. Whether you’re a young adult or a senior, it’s important to always make good health decisions and to be more aware of how your lifestyle affects your lungs.
Age has a significant impact on your ability to prevent and treat COPD. Younger generations may be less likely to contract COPD because of the stigma associated with smoking and pollution. On the other hand, seniors with COPD will have a harder time managing their disease than a young person due to comorbidities and other issues caused by aging.
Regardless of your age, your doctor should be the first person you go to if you’re experiencing chronic symptoms. Coughing, wheezing, and chest pain are not normal signs of aging, so if they persist for more than a couple of days, you should schedule an appointment as soon as possible.
.png)
Chronic obstructive pulmonary disease (COPD) is one of the most substantial health burdens in the world. According to the Centers for Disease Control and Prevention, “chronic lower respiratory disease” (primarily COPD) is fourth on the list of leading causes of death worldwide, behind heart disease, cancer, and unintentional accidents. And despite the fact that fewer people are smoking than ever before, experts are expecting the number of COPD cases to rise within the next 50 years.
While the vast majority of COPD cases are caused by cigarette smoking, many people are surprised to find that COPD is a diverse group of diseases that have a multitude of different causes. One of the other major causes of COPD is alpha-1 antitrypsin deficiency. This is a genetic condition that inhibits proteins that are responsible for protecting the lungs from inflammation and long-term damage. Other factors such as air pollution, irritants, and chemicals can contribute to the onset of COPD. However, these are more commonly associated with interstitial lung disease (ILD).
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
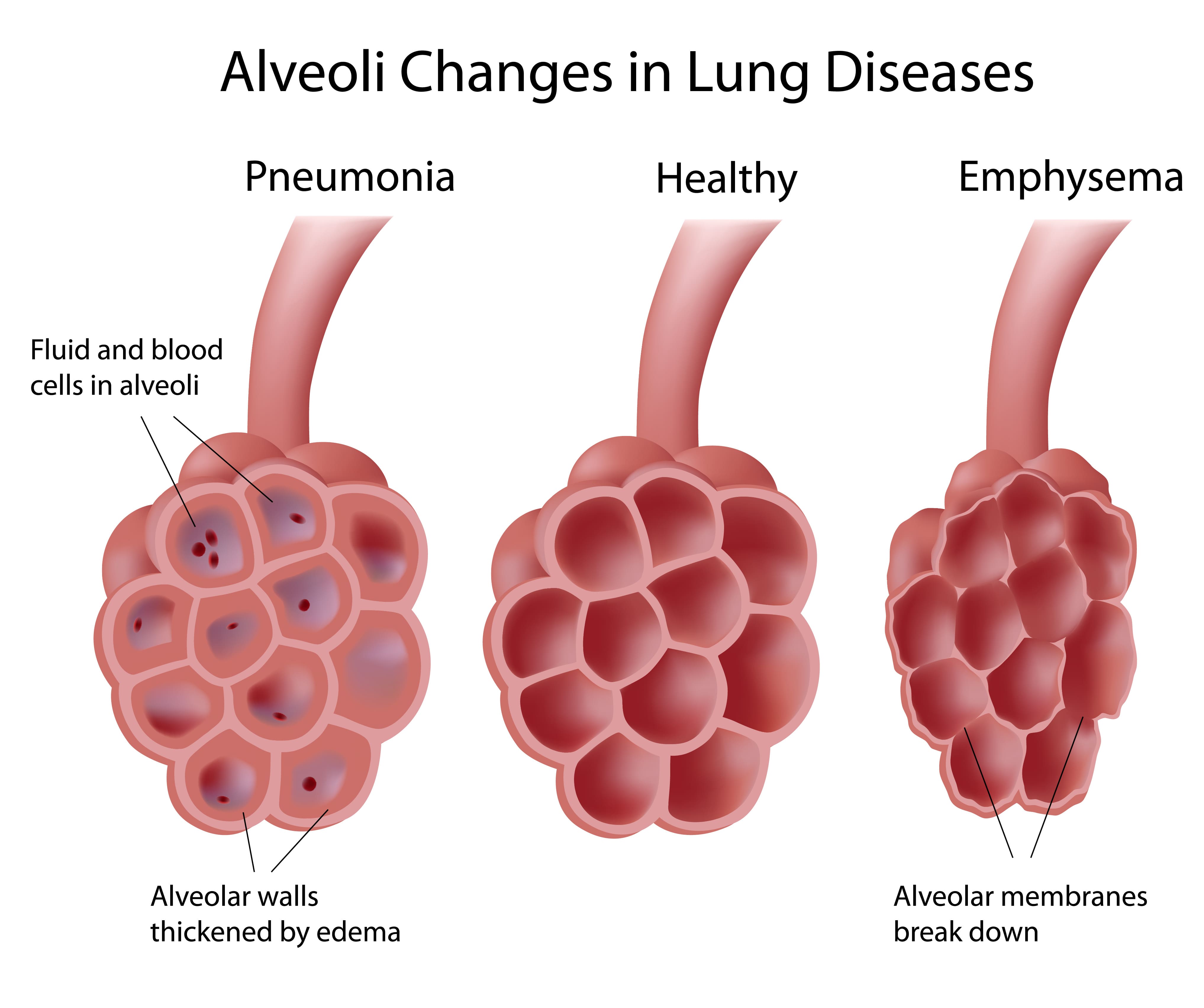
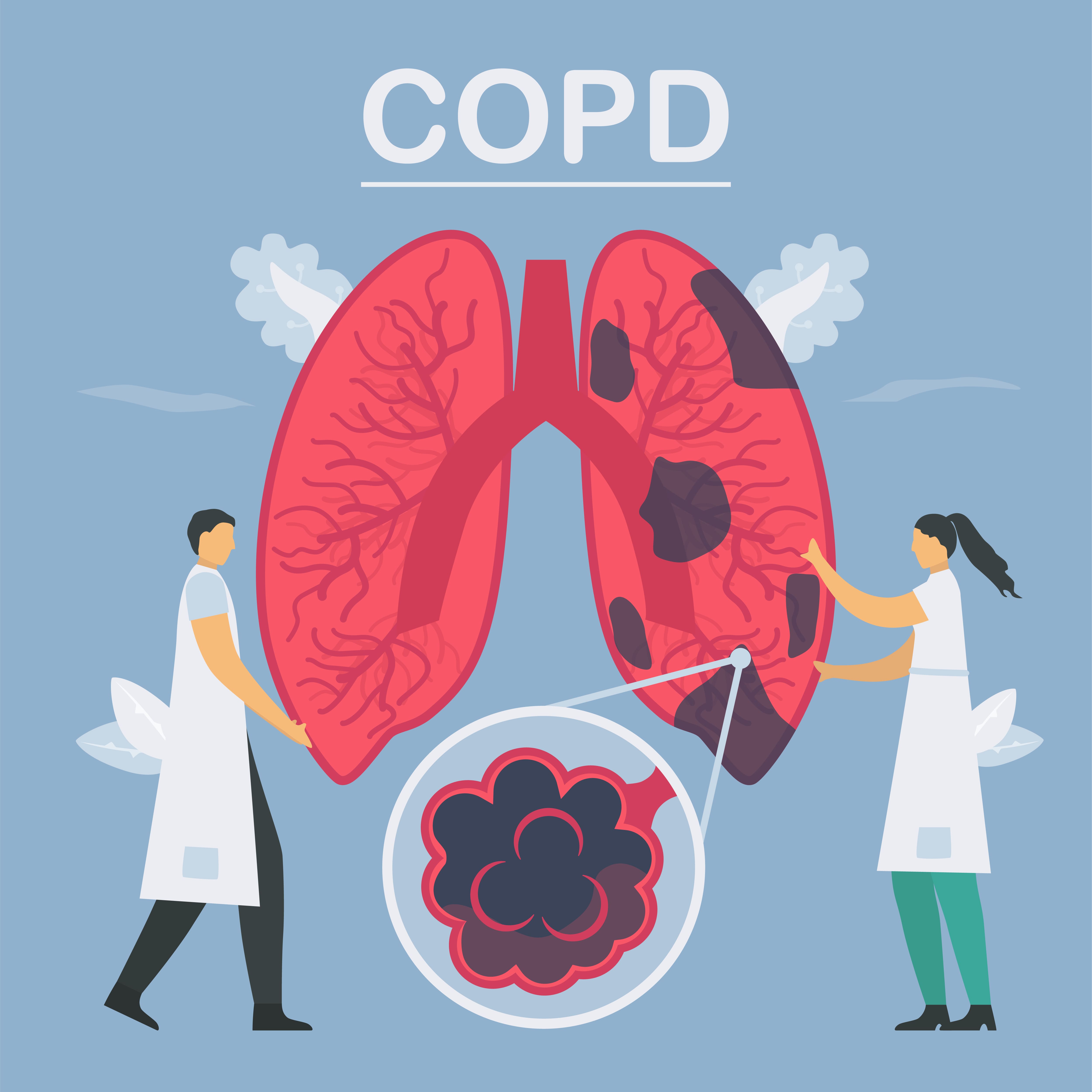
COPD is divided into two different types: chronic bronchitis and emphysema. Bronchitis affects the airways and emphysema affects the lungs. Many COPD patients have both of these diseases simultaneously but it is possible for someone to contract one without the other. And while many people think of emphysema as one disease, it’s actually divided into three different morphological categories. Depending on which one you have, you may require different treatments to manage your symptoms effectively.
In the following sections, we will provide you with an overview of emphysema as well as the three different subtypes. If you have any questions, don’t hesitate to reach out to us by leaving a comment or contacting us by phone or email.
What is Emphysema?
Emphysema is a condition that’s caused by the deterioration of lung function due to the loss of lung elasticity and the deterioration of the alveolar walls. The alveoli are tiny air sacs located at the end of the bronchioles, the small airways that lead into the lungs. There are around 300 to 500 million alveoli in the lungs, and they’re microscopic, so they’re extremely sensitive to foreign substances like cigarette smoke, chemicals, and air pollution.
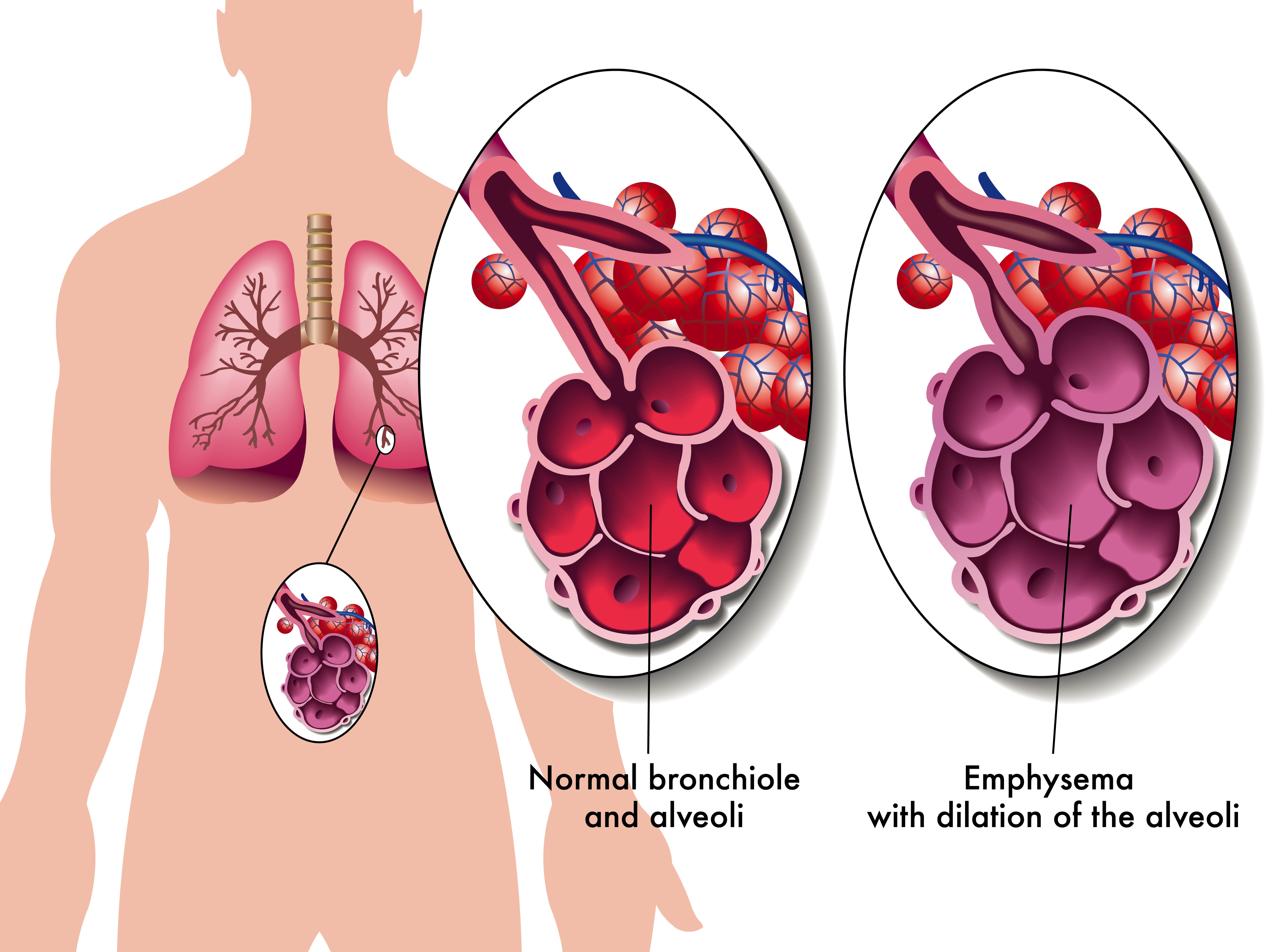
The alveoli play a vital role in the respiratory system because they transfer oxygen from the air that you breathe into the bloodstream. They also remove carbon dioxide from the bloodstream and send it back out of the lungs. This process is called diffusion and it is one of three processes that your lungs perform. Unfortunately, due to how complex the respiratory system is, if the process of diffusion is impaired, this can cause a lot of problems for the other two processes of the respiratory system: ventilation and perfusion.
Not only do alveoli transfer oxygen and carbon dioxide to and from the blood, but they’re also responsible for the spongy and elastic consistency of the lungs. As the walls of the alveoli break down, the elasticity of the lungs is lost and they become less efficient at absorbing air. Another issue this can cause is stagnant air that gets trapped in diseased areas of the lungs which can significantly increase the energy it takes to breathe and result in hyperinflation of the lungs. This also gives emphysema patients their “barrel-chested” appearance which is so often associated with the disease.
What Types of Emphysema Are There?
There are three types of emphysema that differ in terms of what causes them and the area of the lungs that are affected. Depending on which type of emphysema you’re diagnosed with, your doctor may have drastically different treatment options. No two cases of COPD are the same so your physician will work with you to determine what treatment will benefit you most.
Centriacinar Emphysema
Centriacinar emphysema (also called centrilobular emphysema) is a condition that affects the upper lobes of the lungs. Most often this type of emphysema starts in the middle of the lungs and progresses outwards. Centrilobular emphysema is almost always caused by smoking and second-hand smoke and it’s more common in people who’ve been diagnosed with coal workers’ pneumoconiosis (CWP) in the past.

Panacinar Emphysema
Panacinar emphysema (also called panlobular emphysema) is a condition that affects the entire acinus distal to the respiratory bronchioles. The acinus refers to the area at the end of the bronchioles and includes the alveolar ducts, alveolar sacs, and alveoli. It differs from centrilobular because it’s usually located in the lower parts of the lungs. Panacinar emphysema is most commonly caused by homozygous alpha-1 antitrypsin deficiency.
Alpha-1 antitrypsin deficiency (A1AD) is a hereditary disorder that causes low levels of the protein alpha-1 antitrypsin (A1AT) in the blood. This protein is made and released from the liver and it protects tissues in the lungs from being attacked by its own enzymes. A1AD patients may either experience abnormal proteins, poor production of these proteins, or both. All things considered, A1AD is a rare disease and it only amounts to a small percentage of the people diagnosed with COPD.
Paraseptal Emphysema
The third and final morphological subtype of pulmonary emphysema is called paraseptal emphysema. This type is usually localized around the septae or pleura in the lungs. This is a thin sheet of tissue that’s located around the outside of the lungs and inside the chest cavity. This type of emphysema is commonly associated with prior lung infections.
What are the Causes and Risk Factors of Emphysema?
Causes
Cigarette Smoking
Smoking is the most considerable cause of emphysema and all conditions under the umbrella term “COPD.” According to the Centers for Disease Control and Prevention (CDC), 80 percent of people with COPD have smoked in the past or are current smokers. Additionally, 38 percent of people who live with COPD continue to smoke. Despite these facts, only about 10 to 15 percent of smokers will develop some form of COPD. Smoking is more likely to cause cancer, heart disease, stroke, diabetes, and other chronic illnesses.

According to the Cleveland Clinic, the greatest predictor for someone developing emphysema from smoking is not whether or not they were a “light” or “heavy” smoker, it’s how long they smoked for — the longer someone smokes, the more likely they are to contract COPD. This is why doctors will always recommend immediate smoking cessation rather than simply “cutting back” on cigarettes.
Secondhand Smoke
Secondhand smoke refers to the inhalation of cigarette smoke involuntarily as a result of someone else smoking. While there is a commonly held belief that secondhand smoke is worse than actually smoking, this is not the case. The toxicology of tobacco smoke is the same regardless of whether it was inhaled intentionally or not. Either way, cigarette smoke in any form can cause COPD and emphysema.

It’s estimated that there are over 7,000 chemicals in cigarette smoke and smoke can linger in the air for several hours. In other words, living with a smoker or being in an area where someone has smoked recently will put you at a higher risk of chronic lung disease. Cigarette smoke dissipates more quickly outdoors so, generally speaking, it’s safer to be outside.
Air Pollution
Air pollution is a major contributor to the onset and progression of emphysema. According to the World Health Organization (WHO), there are five major types of air pollution: particulate matter, ground-level ozone, nitrogen dioxide, sulfur dioxide, and carbon monoxide. All of which can be inhaled into the lungs and cause permanent damage to the bronchioles and alveoli. Just like with cigarette smoking, the more you’re exposed to air pollution, the more likely it is to cause permanent damage to your lungs.
![]()
One great tool to help you learn about the air pollution in your area is AirNow.gov. All you have to do is enter your city or zip code and it will provide you a number between 0 and 500 with 0 being the least polluted and 500 being the most polluted. The EPA recommends that you should not go outside if the Air Quality Index (AQI) is above 150. However, if you already have a chronic lung disease like asthma or COPD, you should avoid going outside if the AQI is above 100.
What are the Four Stages of Emphysema?
Much like other chronic illnesses that take many years to progress, emphysema is broken down into different “stages” which medical professionals can use to identify the severity of your disease. Since early-stage emphysema has very mild symptoms, it’s often underdiagnosed or misdiagnosed as other chronic lung conditions such as asthma. Read below to learn about the four stages of emphysema.

Stage 1
Stage 1 emphysema is very mild. In fact, it’s often so mild that it is undetected and undiagnosed. People with stage 1 may experience a cough, minor chest pain, and some breathlessness. Stage 1 emphysema patients have a forced expiratory volume in one second (FEV1) of 80% or more.
Stage 2
Stage 2 is slightly more advanced than stage 1. This is when many people start to see their doctor because they begin to realize that their respiratory symptoms aren’t the result of aging or an acute condition. Stage 2 emphysema patients have an FEV1 between 50% and 80%.
Stage 3
By the time someone reaches stage 3 they have most likely received a diagnosis from their doctor. They’ve likely had several flare-ups in the past year and have been admitted to the hospital at least once. Stage 3 patients have an FEV1 between 30% and 50%.
Stage 4
Also known as “end-stage COPD,” this stage is characterized by severe breathlessness, coughing, wheezing, and fatigue which leads to exacerbations and hospitalization. Stage 4 patients have an FEV1 of less than 30%.
How is Emphysema Treated?
Supplemental Oxygen Therapy
Because emphysema can result in low blood oxygen levels (hypoxia) supplemental oxygen can be used to stabilize a patient’s oxygen levels and help alleviate emphysema symptoms like breathlessness, chest pain, and coughing. However, it’s important to note that oxygen therapy can be dangerous if it’s not used in the way that your doctor intends for you to use it. Oxygen is a controlled substance in the United States, so you’ll need a prescription in order to rent or buy an oxygen device.

There are many choices to consider when it comes to oxygen delivery devices so you’ll need to find one that best suits your needs and your lifestyle. Oxygen tanks are a very popular choice because they have a low upfront cost. However, they’re very heavy and need to be refilled constantly making them a poor choice for most oxygen users. Liquid oxygen tanks are an upgrade because they last longer and aren’t as heavy, but they cost more to maintain.

The best alternative to both of these is portable oxygen concentrators. An oxygen concentrator is an electronic device that takes in ambient air and removes nitrogen, argon, and other gases, then puts out medical-grade oxygen. The benefit of this is that you simply need to charge the batteries on your concentrator which is much more convenient than having to have an oxygen company fill your tanks.
Pulmonary Rehabilitation
Many years ago, exercise was not recommended for COPD patients because it was believed to exacerbate symptoms and increase the rate at which the disease progressed. However, in this day and age, pulmonary rehabilitation (exercise that’s focused on lung function) is championed as one of the best ways to treat chronic respiratory illness. This is due to a mounting body of evidence that shows even moderate exercise can improve COPD symptoms.

While you can exercise at home on your own time, it’s recommended that you start with a pulmonary rehabilitation program. Not only do these programs teach you how to exercise with emphysema, but they will also teach you important information about your disease and how it should best be managed. Read this post to learn more about how pulmonary rehabilitation works.
Dietary Changes
If you live by the motto “you are what you eat,” you probably understand the importance of a healthy, well-balanced diet. Nutrition affects everything from your heart health to your lung health and everything in between, so it’s wise to follow your doctor’s instructions on eating healthier meals. According to Lung.org, the metabolism of carbohydrates creates the most carbon dioxide, so they should opt for healthy fats instead which produce the lowest amount of carbon dioxide. HIgh-protein diets are also good for emphysema patients because they keep your lungs strong and efficient.
![]()
Medication
Emphysema treatment usually involves some combination of oral and inhaled medication. Oral steroids can provide you with short- or long-acting relief from your symptoms whereas inhaled medication like bronchodilators are designed to open up your airways quickly in the event of a COPD exacerbation. Your doctor will discuss with you exactly which medications you will need and when to use them.

Most oxygen patients are prescribed inhalers, nebulizers, or both. An inhaler is a portable device that administers medication in a mist form called “aerosol.” this enables the patient to administer the medication directly to their lungs thus allowing it to take effect more quickly. Nebulizers play a similar role in an emphysema treatment plan but they administer medication in a stream rather than a “puff” making them easier to use for most people.
Lifestyle Changes
There are many other lifestyle changes that you can make to treat emphysema and alleviate your symptoms. Focusing on getting more consistent and restful sleep is one way that you can feel more alert and prepared to take on the challenges of your disease. Ultimately, you should discuss your sleeping habits with your doctor to ensure that you’re doing everything you can to get a good night’s sleep.
![]()
Another lifestyle change you can make is changing your cleaning habits. Many common household cleaners are filled with dangerous chemicals like bleach and ammonia. When these substances are inhaled they can cause COPD exacerbation which leads to increased coughing, wheezing, and shortness of breath.
Conclusion
COPD is one of the most preventable chronic illnesses in the world and emphysema is one disease under this umbrella term. Emphysema patients experience impaired lung function due to a breaking down of the alveoli, or tiny sacs in the lungs that transfer oxygen and carbon dioxide to and from the blood. While there is no cure for emphysema, patients can experience significant relief and improved life expectancy with a carefully planned treatment routine.
Here at LPT Medical, we want COPD patients to experience relief from their respiratory symptoms while experiencing the freedom and independence they had before being diagnosed. If you haven’t done so already, ask your doctor if you might benefit from using a portable oxygen concentrator like the Inogen One G5 or the Caire FreeStyle Comfort. Both of these machines have a high oxygen output, they’re lightweight and easy to carry.

We all know that life can be exhausting, but when your exhaustion starts to become chronic, and it feeling tired or fatigued starts to affect other aspects of your life, it is time to take action. There are things you can do to fight off the exhaustion, so you can get back to a more energize state of being.
Exhaustion can impact many aspects of your life including your mood, mental health, physical strength and so much more. Feeling exhausted is not the end all be all, there are habits you can form and habits you can break that can help you get back to feeling more like yourself again.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The first part of fighting off the exhaustion is understanding why you feel this way. If you have chronic respiratory disease like COPD, fatigue is a very common symptom of your disease, but feeling exhausted can also be attributed to other aspects of you habits and daily routine.
Here are some reasons many people find themselves chronically exhausted due to their symptoms:
- Trouble breathing at night
- Excess mucus production while sleeping
- Hypoxemia (low oxygen levels)
However, your fatigue or exhaustion could be attributed to other things unrelated to your respiratory disease.
- Lack of exercise
- Poor diet
- Dehydration
COPD and exhaustion
-jpg.jpeg)
COPD inhibits your lungs from making the proper exchange of gases, therefore your body can’t get the oxygen it needs. With COPD, you develop low blood oxygen levels, a condition called hypoxemia. You can combat the symptoms associated with hypoxemia, like shortness of breath, by using supplemental oxygen. You can administer oxygen with a portable oxygen concentrator or liquid and gas oxygen tank.
Your doctor will write you a prescription that will tell you the exact amount of oxygen you need. It is important that you follow these instructions. If you do not get the oxygen your body needs you will feel tired because fatigue comes more quickly when your lungs can’t properly inhale and exhale air.
Once you start to feel fatigue from a lack of oxygen, you are less likely to engage in physical activity. By avoiding activity, your stamina starts to decline and you can grow tired more easily, this is the toxic cycle exhaustion can manifest in your life, and it is something that you can it avoid or break out of! To get back to a place where you feel more energized and capable, follow the simple steps laid out in this article.
To combat symptoms of fatigued associated with your COPD you will need to follow these 3 basic steps:
- Ask you doctor if you would benefit from using supplemental oxygen at night
- Clear your airways before bed effectively
- Stick to your COPD treatments: Medications, oxygen therapy, diet, and exercise
Supplemental Oxygen

Getting the oxygen you need at night can help you sleep more soundly, thereby helping you feel less fatigued during the day. COPD prohibits you from getting the oxygen your body needs, making it more difficult and laboring to breathe, so taking oxygen therapy during the day can help you feel less fatigued as well.
Depending on your condition, you will be prescribed pulse flow oxygen or continuous flow oxygen. Your doctor will tell you if you need to use your oxygen at night, during the day, or both. This will all be included in your prescription, and you should be diligent to follow the prescription as you would with any prescription medication.
Clearing your Airways
People with COPD and chronic bronchitis often have issues with producing a large amount of mucus. Once mucus starts to collect in your airways, breathing becomes more difficult, and can even result in an infection. There are a few techniques to remove mucus that are often done after using an inhaled bronchodilator medication. The medication helps loosen the mucus and open the airways to make these techniques even more effective. Common techniques used to help remove mucus can be ordered and demonstrated by your doctor.
Clearing your airways of mucus also can help you sleep more soundly allowing you to breathe more easily and reducing the amount of coughing you experience while you sleep.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
There are a number of mucus clearing techniques that you can try that will help you open up your airways.
Deep Coughing: First, take a deep breath. Hold your breath for 2-3 seconds. Forcefully expel your air using your stomach muscles. A deep cough is less tiring and more effective in clearing mucus out of the lungs than merely clearly your throat.
Huff Coughing: Huff coughing, or huffing, is an alternative to deep coughing.. Start by taking a breath that is deeper than a normal breath. Use your stomach muscles to make a series of three rapid exhalations with your airway open, making "ha, ha, ha" sound. Then, perform a series of controlled diaphragmatic breaths followed by a deep cough if you feel mucus moving.
Other Techniques: If you produce a large amount of mucus and huffing nor deep coughing help to clear your airways, your health care provider may recommend other techniques to help clear the mucus.
Your doctor may suggest using a mucus clearing device. There are several types of airway/mucus clearance devices that you can use to remove excess mucus and saliva from your airways. They will come in the form of a mouthpiece, a mask, a vest, etc. and to function they use air pressure, oscillation, or high-frequency sound waves to function.
Postural drainage is a technique that uses gravity to promote drainage of mucus from the lungs.
Any of these airway clearing techniques technique can be ordered and demonstrated by your doctor. Try doing this before bed to sleep without being interrupted by a mucus inducing cough or breathing complications.
Learn Breathing Exercises
One of the reasons COPD patients often feel exhausted, is because they are not getting enough oxygen, yet, you still might not qualify for supplemental oxygen. If this is the case for you, it could be very beneficial to work with a respiratory therapist. These healthcare providers are trained to teach you more efficient ways to breathe, which are often referred to as breathing exercises.
Breathing exercises like pursed lip breathing can improve fatigue by:
- Slowing down your respiratory rate
- Getting rid of the trapped carbon dioxide
- Relieving shortness of breath
A person can try pursed lip breathing during and after any activity that causes shortness of breath and before bed. To do pursed lip breathing work through these 4 steps:
- Breathe through the nose for around 2 seconds
- Purse or pucker the lips, as if blowing out a candle
- Slowly breathe out through the pursed lips for 4–6 seconds
- Repeat the exercise
Follow your COPD treatment plan and Take your Medication
There no cure for COPD yet, but taking the necessary treatment can help reduce your symptoms, including exhaustion. Managing shortness of breath and making it easier to breathe can help you feel less tired during the day and sleep more soundly at night.
Your doctor has probably prescribed medications to help you breathe easier. Common COPD medications include bronchodilator inhalers, which dilate or widen your airways, steroid inhalers, which reduce inflammation in your lungs, and again supplemental oxygen therapy, which relieves shortness of breath if you have low oxygen levels.
Following your own treatment plan along with a healthy diet and regular physical activity or exercise will help combat that feeling of fatigue and exhaustion.
A healthy COPD diet will have all of the nutritional foods that you need to feel more energize. It will exclude foods that make you feel overly full or bloated. Dieting does not mean eating less food, it means eating more food that is good for you, and cutting out foods that make you feel bad. It is still not as easy as it sounds, and dieting takes a lot of practice.
Exercising is the last thing people want to do when they feel weak or fatigued, however without physical actively your muscles and endurance will degrade, making any simple task more of a hassle. Start by doing a small amount of exercise every day, you will notice your stamina start to improve and you will feel a little bit stronger and less tired everyday.
Exercise during the day also promotes a healthier sleep at night, so if you have trouble falling asleep or staying asleep, being more physically active during the day will help.
Other Reasons you Feel Exhausted
Fatigue is one of the most common symptoms of COPD, especially as the disease progresses. Research suggests that about 50 to 70 percent of people with COPD also feel fatigued. Clearly, fatigue often goes hand in hand with COPD, but the reasons for this association are not clear nor does having COPD mean that you will always feel fatigue.

It is important not to chalk up your fatigue to the fact that you have COPD. You can take the necessary action and steps towards a lifestyle where you feel more energized and capable of doing more.
If you are having trouble sleeping for reasons unrelated to your COPD you can start by:
- Getting into a night time routine
- Avoiding caffeine before bed
- Limiting exposure to white light
- Drinking more water throughout the day
- Exercise more regularly
- Eating a balanced diet
- Treating other conditions
Taking action toward these seven steps will help you get on track so that you are sleeping more soundly more often. It is also important to start building up your stamina during the day so you don't feel drained doing everyday activities, you can do this by exercising, eating healthy, and drinking plenty of water.
Overview

As we mentioned above, fatigue is a very common symptom that has been linked to COPD. Excess carbon dioxide, shortness of breath, trouble sleeping, all contribute to feeling exhausted during the day.
By taking action to address other COPD symptoms you are also helping to combat your fatigue. Using your oxygen therapy as prescribed, keeping up with your COPD medication, and treating your COPD effectively will get you back to feeling energized.
While it can be hard to break the toxic cycle the fatigue creates, performing physical activities in some form daily will help you build up your stamina so that eventually everyday activities become doable again. Sleeping better at night will also give your body the refresh it needs to feel more energized during the day.
Sleeping more soundly isn't always easy. Sleeping better all comes down to building healthy habits surrounding your nighttime routine. If you still have trouble sleeping, you should talk to your doctor about your experiences sleeping, they may be able to suggest a remedy that will help you get the sleep you need.
Overall, it is our hope that anyone with COPD can get back to doing what they love. Even in the face of hardship, it is important to stay positive and continue to research ways in which you can improve your wellbeing. It is our goal to get this resource into the hands of people who need it. If you know someone that struggles with COPD and fatigue, please send them this article, and if this helped you in anyway, let us know by commenting below!
.png)
Whether you have a friend or a loved one with COPD or you have COPD yourself, you can likely attest to the fact that this disease can cause significant problems with mobility. The top causes of mobility issues in COPD patients include poor pulmonary function, leg swelling (peripheral edema), and loss of muscle mass (muscle atrophy). Combined with the effects of aging and other chronic conditions like osteoarthritis, COPD patients can experience a lot of difficulties getting around in their day-to-day life.
Aside from supplemental oxygen therapy, a healthy diet, and pulmonary rehabilitation, another thing that can help you get around are mobility aids. A mobility aid is a device that’s used to help older people and people with chronic conditions walk more easily. They’re often designed to improve balance, reduce physical load, and in COPD patients, they can even help to prevent exacerbations and flare-ups. There is a huge variety of mobility aids and you’re not just limited to choosing one or the other.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In the following sections, we’ll help you better understand the mobility options available to you as well as some other helpful information that will help you maintain your mobility as a COPD patient. As always, if you have any questions, please be sure to address them in the comment section or consult your doctor for more specific information pertaining to your disease and treatment plan.
Why Are Mobility Aids Important for COPD Patients?
According to an article published in the National Center for Biotechnology Information, balance deficit is a common issue among COPD patients. COPD is a progressive disease meaning it becomes worse over time. And as symptoms like breathlessness, chronic fatigue, and chest pain progress, so do issues related to balance and mobility. Believe it or not, studies have shown that COPD is one of the chronic illnesses with the highest rate of falls next to osteoarthritis.
Several months ago, we wrote an article discussing a common complication of COPD called peripheral edema. In short, this is a condition where your legs or feet begin to swell due to a buildup of fluid. One of the root causes of this condition is pulmonary hypertension or high blood pressure in the lungs. High blood pressure in the lungs puts more strain on the heart and prevents oxygen-rich blood from circulating to organs like the liver and kidneys. Since these organs are responsible for removing fluids from the body, swelling of the feet or legs are usually a sign of this happening.
While peripheral edema is a complex condition, it’s one of the issues contributing to the high risk of falls in COPD patients. As the disease progresses, COPD patients don’t just have to deal with increased respiratory symptoms, they have to deal with complications that can result from their disease. Someone with peripheral edema may not even realize they have it because it often comes on slowly and doesn’t cause any pain.
-jpg.jpeg)
Another issue contributing to the high rate of falls in COPD patients is muscle atrophy. In other words, as COPD progresses, patients tend to lose muscle mass from a variety of issues like a changed diet and reduced physical activity. Similar to peripheral edema, a patient may not realize that they are losing muscle mass until they experience a fall. This is why pulmonary rehabilitation is such an important part of any COPD treatment plan.
One final problem that can contribute to the fall rate in COPD is an exacerbation. An exacerbation is an event where respiratory symptoms suddenly worsen. According to COPD.com, the most common cause of exacerbation is a bacterial infection, but air pollution is another common cause. COPD exacerbations can lead to problems walking, balance issues, chest pain, headaches, and confusion, all of which can increase your risk of falls.

While mobility aids are not a replacement for your treatment plan, they play a crucial role in preventing falls, especially in people with late-stage COPD where the disease is the least predictable. Mobility aids don’t need to be prescribed by your doctor so it’s up to you and your loved ones to determine whether you need one or not. Continue reading to learn about some of the mobility options available to COPD patients.
Canes
Walking canes are the oldest type of mobility aid and they’re also one of the simplest. Most walking canes are made of wood or a light metal material meaning they’re easy to carry despite your level of physical impairment. Canes are also widely accessible, and you can buy them just about anywhere, or you could even make your own if you have time. Walking canes are great for taking weight off your joints and providing you with a little extra stability as you walk.

The key to improving your mobility with a cane is to get one that’s the appropriate size. While there is no hard and fast rule as to how you should choose a cane, it should be long enough that you aren’t bending over and straining your back in order to use it and it should be short enough that you can actually lean on it. For most people, this will be somewhere around their hip bone. Luckily, most modern canes are adjustable, so you’ll probably be safe buying one online rather than shopping around for one.

One thing to consider if you want to use a cane is how you will carry your supplemental oxygen device. If you have an oxygen tank and you wheel it behind you using a rolling cart, a walking cane might not be the best option for you because you won’t have any hands free to catch yourself if you fall. A cane is a better option if you carry your oxygen device on your back because it will help you keep a good posture as you walk.
Walkers
Walkers are another mobility option available to COPD patients. There are several different types including traditional walkers, two-wheel walkers, and four-wheel walkers. Traditional walkers tend to be a poor choice for most COPD patients because they need to be picked up as you walk which can be strenuous on your shoulders, arms, and back. Two-wheel walkers provide a little more mobility by allowing you to push the walker rather than lift it. However, for most people, four-wheel walkers, or “rollators” as they’re often called, will be the best option.

Modern rollators are more advanced than other types of walkers because they offer four swivel wheels that afford you more control. They also offer a braking system that’s controlled by two levers on the handlebars on either side of the device. They also provide a padded platform in the middle that you can either sit on or rest your oxygen device, purse, or handbag on as you walk. Some rollators even have a basket in front for added storage.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
It’s a good idea to speak with a mobility aid expert if you want to get a rollator. Since these devices are so popular, there are many different versions and brands available to choose from. What’s more, it’s easier to use one if you’ve been shown how to do so by someone who’s experienced with them. You’ll also need to have one fitted unless you can find one that’s adjustable.
Wheelchairs
When you think of a mobility aid, chances are, wheelchairs are the first thing that comes to mind. They’re commonly used by people who are permanently disabled, but how do they fare when it comes to someone with limited mobility? The answer ultimately depends on your individual circumstances. COPD patients with poor upper body strength may find it difficult to get around in a manual wheelchair, but if you have a caretaker or loved one who can push you around it shouldn’t be a problem.

Another option for you are motorized wheelchairs or “power wheelchairs” as they’re often called. The benefit of investing in a power wheelchair is that you will have the same mobility as a manual wheelchair, but you won’t have to push it with your arms. Power wheelchairs have a joystick that you use to move in any direction. They’re not overly complicated to operate but they can be difficult to transport and you’ll need to keep it charged if you want to stay out of the house for extended periods of time.
Scooters
Mobility scooters are similar to power wheelchairs but they differ in terms of their design. Unlike power wheelchairs which use a joystick, scooters are controlled with handlebars similar to a bike. Scooters can either have three or four wheels depending on what your preferences are. They also have baskets on the front that you can use to store things like your portable oxygen concentrator, a purse, or other personal belongings. Since there are so many options available when it comes to mobility scooters, it’s important to speak with an expert who can align you with the exact product you’re looking for.

Stairlifts
Stairlifts are a mobility aid that many people have never heard of, but they’re incredibly useful. Essentially, a stairlift is a chair that moves up and down a rail that’s installed on a flight of stairs in your home. The chair has a built-in motor that can be controlled with a joystick on the handlebars. This allows you to navigate the stairs in your home without the risk of experiencing a dangerous fall. The one downside to stairlifts is that they can be very expensive and many people can’t justify spending the money to have one installed in their home.

Surprisingly, stairlifts are extremely versatile and can be installed on most staircases regardless of their size or shape. What’s more, if you like to get outside, there are specially designed stairlifts that can be installed on outdoor staircases. They can be installed in several hours so you won’t have to wait days or weeks to start using them.
Will Medicare Pay for a Mobility Aid?
Whenever it comes to medical equipment, questions about health insurance and Medicare are sure to follow. And while it would be nice if Medicare paid for medical expenses like you’d expect them to, it’s never that simple. More often than not, they will cut corners providing you coverage for mobility aids and find any way they can to offer you the bare minimum rather than what you deserve.

In short, Medicare will provide some compensation for manual or power wheelchairs and scooters. Mobility devices like these are covered under Medicare Part B and it is classified as durable medical equipment (DME) the same as oxygen tanks and portable oxygen concentrators. But it’s important to note that not all devices are covered. Medicare has a list of devices that are covered, and some of them require prior authorization. So, it’s best to consult with both the mobility aid supplier and a Medicare representative before you make any decisions.
.jpg)
Another thing to note is that Medicare has a long list of prerequisites that you need to meet in order to qualify for compensation. First and foremost, the doctor that has prescribed you with COPD and the mobility aid supply company needs to be enrolled in Medicare. Additionally, you’ll need a written order from your doctor stating that you have a medical need for a mobility aid. For a full list of requirements, refer to the wheelchair and scooter benefit page of Medicare Part B.
Get a Handicap Parking Permit
Once you have your mobility aid of choice, you may want to consider getting a handicap parking permit. This permit will allow you to park in any handicap spot in the country making it much easier for you to get around. This is especially useful for people who are using electric scooters or power wheelchairs because you won’t have room to unload it in a standard parking spot.

In order to get a handicap parking permit, you’ll need to apply at your local Department of Motor Vehicles (DMV). Every state has different policies but you’ll likely have to provide a doctor’s note which outlines your lung condition and symptoms. You’re more likely to get approved if you can prove that you use an electric scooter or power wheelchair as opposed to a cane or walker so it’s best to put time into finding a mobility aid first.
.jpg)
Last but not least, if you’re given the option between a handicap sticker that goes on your car or a placard that you hang on the mirror, always go with the placard. This is because you can transfer these to any car that you’re in whether it belongs to a family member or friend. Be aware that it is illegal for them to use the placard without you actually being present and most states require you to be recertified for your handicap permit every couple of years.
Conclusion
Making the decision to use a mobility aid is an important step for many COPD patients. People with chronic respiratory conditions are at a higher risk of experiencing falls than the general public, but mobility aids will help to support your balance whether you’re inside or outside the home. Unfortunately, there is no one-size-fits-all solution. Everyone has their own needs and preferences so you should consider all options available to you.
Canes and walkers are a good place to start because they’re affordable and they’re easy to carry. However, you may want to consider a more long-term solution like a mobility scooter or power wheelchair. These devices are generally safe and easy to use, and they will make it easy to carry around your oxygen devices such as your oxygen tank, liquid oxygen tank, or portable oxygen concentrator.
Lastly, you should check with your health insurance to see if your mobility device is covered. This could save you hundreds if not thousands of dollars. You can also file for disability and receive a handicap parking permit which will afford you more convenience and freedom whenever you leave the house. In the meantime, if you’re looking for a lightweight and easy-to-use portable oxygen concentrators such as the Caire FreeStyle Comfort or the Inogen One G5, don’t hesitate to reach out to your respiratory specialists here at LPT Medical.
Chronic obstructive pulmonary disease (COPD) is an umbrella term used to define two different types of lung disease: chronic bronchitis and emphysema. The former is a condition that impairs the bronchioles, the airway tubes that lead into the lungs. The latter affects the tiny air sacs in the lungs called the alveoli. These are responsible for the transfer of oxygen and carbon dioxide to and from the bloodstream. Both chronic bronchitis and emphysema are called “obstructive” diseases because they make it more difficult for the patient to expel air from the lungs, thus leading to a buildup of CO2 in the blood.
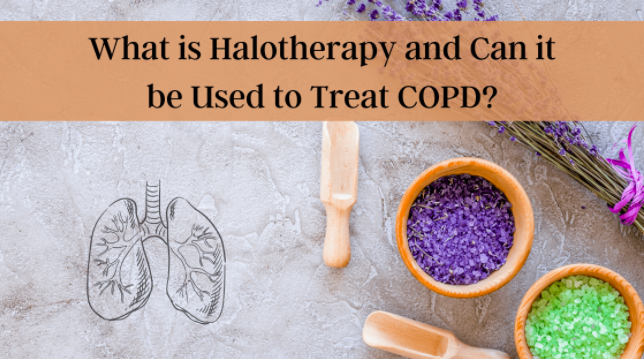
When a patient is diagnosed with COPD, they’re typically prescribed a standardized treatment plan including but not limited to supplemental oxygen therapy, a specialized diet, pulmonary rehabilitation, and breathing exercises. These are all clinically proven techniques that will help to prevent breathlessness, chest pain, and improve long-term prognosis. While most COPD patients adhere to these well-researched practices, some people look for additional “home remedies” to treat their disease. These are usually referred to as “alternative therapies.”
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Here at LPT Medical, we don’t advise using any type of alternative therapy unless it’s explicitly approved by your doctor or pulmonologist. Some alternative therapies and medications are touted as “cure-alls” or “cheap alternatives” to standardized medications, but more often than not, they don’t live up to their hype and they can even result in further damage to your lungs. In this post, we’re going to tell you all about the alternative therapy called halotherapy, or more commonly known as salt therapy. If you have any questions, please feel free to leave them in the comment section below and we’ll get back to you as soon as possible.
What is Halotherapy and How is it Used?
The term “halotherapy” comes from the Greek word “halos” meaning “salt.” In other words, it’s the use of salt as a therapy for a variety of different ailments. The idea of using salt as a type of therapy is believed to have originated in Europe several hundred years ago. Miners, who are known to contract deadly lung diseases (pneumoconiosis) like black lung and silicosis due to their exposure to mineral dust, did not experience the same effects when they worked in salt mines. Rather, salt mine workers appeared to thrive and experience great lung and skin health.

It wasn’t until 1826 that the first salt therapy facility was opened by a Polish physician named Feliks Boczkowski. At this treatment facility, he offered salt baths from naturally occurring underground brine. After World War II, Dr. K.H. Spannahel created a systemic approach to the climatological conditions of salt caves and attempted to confirm their medical effectiveness. Together, these two physicians helped to lay the foundation of modern speleotherapy (salt cave therapy).
Nowadays, there are many different types of salt therapy used to treat a variety of different conditions. Below are just a few:
Wet Salt Therapy
This therapy got its name because it involves the use of salt combined with water vapor. Wet salt therapy is one of the most common types of salt therapy and it’s also one of the easiest and most accessible for most people. It includes things like salt scrubs, salt baths, salt nebulizers, and saline solutions.

Dry Salt Therapy
This is a type of salt therapy that is completely void of moisture or humidity. This is considered the most “traditional” type of salt therapy and it includes salt caves, salt grottos, salt rooms, and salt chambers. Dry salt therapy is said to have many benefits for the body including improved breathing and softer skin.
Speleotherapy
“Speleo” is derived from the Greek word spḗlaion meaning caves. Speleotherapy is a type of salt therapy that involves going into naturally occurring caves below the earth’s surface. It’s believed that the natural climate and environment of these caves is great for treating respiratory diseases like asthma and chronic obstructive pulmonary disease.

Active Salt Rooms
This type of salt room uses a halogenerator. This is a device that crushes pure sodium chloride into a fine powder that can be dispersed as an aerosol into the room. This is done in a confined room where the amount of salt in the air can be closely monitored by a specialist. The climate and humidity of these rooms are also closely monitored.
%20(2).jpg)
Passive Salt Rooms
This is similar to active salt rooms but there is no halogenerator that puts out salt particles in the air. Rather, a passive salt room simply has blocks of various types of salt including Himalayan, Mediterranean, Caribbean, or Rock salt, and they’re designed to mimic the effects of being in an actual naturally occurring salt cave. Many people claim that having large quantities of salt like this in a confined space creates positive energy frequencies and a clean-air environment. This is also a major selling point for products like salt lamps which are very popular nowadays.
Can COPD Patients Benefit from Salt Therapy?
Now that you know a little bit about what salt therapy is, you’re probably wondering if there are any proven benefits for COPD patients. Unfortunately, there isn’t a simple “yes” or “no” answer to this. Despite being around for hundreds of years, there isn’t a significant amount of research done on the topic, and many health experts have conflicting opinions about how it should be used, or if it should even be used at all.
The reason salt therapy is associated with COPD in the first place is because of its antibacterial and anti-inflammatory properties. Hundreds of years ago, before the invention of refrigerators, salt was used to preserve meat. This worked because salt draws the moisture out and prevents harmful bacteria from forming. Proponents of salt therapy believe this can also benefit the respiratory system of COPD and asthma patients by killing harmful bacteria that could lead to infection.
Proponents of salt therapy also claim that salt can reduce inflammation in the lungs and airways, loosen excess mucus, and reduce immune system oversensitivity, all of which are symptoms of COPD. However, most of these claims have very little evidence backing them up and many studies have even shown that salt therapy can actually exacerbate the issues above rather than help to cure them.
According to the Asthma and Allergy Foundation of America (AAFA), inhaling concentrated salts (hypertonic saline) or any crystalloid solution containing more than 0.9% saline is proven to make asthma and COPD worse by irritating the airways, increasing mucus production, and causing a cough. As such, it’s important to understand the concentration of salt in the therapy you’re receiving.
Another important thing to note is that the popularity of salt therapy does not affirm its efficacy. Just turning on your TV or browsing the internet, you’re likely to see advertisements for salt therapy caves, salt lamps, and salt inhalers, and you likely hear claims that they can cure chronic illness, but this doesn’t make them true. Since salt therapy is not classified as an FDA approved medication, it’s also not regulated the way that your traditional COPD medication is.

That doesn’t make them completely immune to responsibility, however. With the advent of the novel coronavirus (COVID-19), salt therapy companies have been under close watch by the FDA when it comes to the claims they make about their products. Some salt therapy companies have made wild claims about their products curing or treating COVID-19 when there is little or no evidence to suggest this is the case. If you’d like to learn more about how these types of products are regulated, read through our post about dietary supplements.

Last but certainly not least, there’s a problem with a placebo effect concerning salt therapy. A lot of the research on salt therapy has been inconclusive because it’s based on anecdotal evidence. In other words, many patients are reporting that salt therapy is beneficial to their health, but there is little evidence to suggest there was a physical change to their disease. Rather they have an expectation that something will change, so that’s what they believe. This is a great selling point for many salt therapy companies because, generally speaking, people trust the opinion of others.
Should COPD Patients Use Salt Therapy?
The most important thing to remember when it comes to alternative therapies or home remedies is to always consult your doctor first. Your doctor may have additional insight into why you should or should not be using salt therapy and he/she will help you weigh the risks. You should also do research on the specific salt cave that you want to visit. While some of these places are sanitized regularly, others are teeming with bacteria which could increase your risk of respiratory infection.
It’s also important to weigh the risks of different types of salt therapy. For example, salt therapy caves or chambers are designed to have a very high saline concentration, so it’s more likely this type of therapy could exacerbate your symptoms. Conversely, simply having a salt lamp around your home is unlikely to result in a high concentration of salt in the air, so you can assume that they’re safe to use. Just don’t expect there to be any significant benefits for managing your disease.
What Should COPD Patients be Doing Instead of Salt Therapy?
While it may be tempting to join in on a fad like salt therapy, the best way to treat your COPD symptoms is with traditional methods that have been researched for hundreds of years and backed by thousands of different studies. Let’s take a look at each of these treatment options.
An Improved Diet
Your lungs play an extremely important role in a process called cellular respiration. This is a set of metabolic reactions in the cells of your body that convert chemical energy into adenosine triphosphate (ATP). In other words, the oxygen that your lungs take in is directly linked to the breakdown of nutrients in your body and it’s absolutely necessary for your body to produce energy that it can use. One of the most important things to note as a COPD patient is that certain foods create more waste products (carbon dioxide) than others do which can make breathing even more difficult.
![]()
Pulmonary Rehabilitation
Regular exercise is one of the most important things you can do for your health. Whether you’re young, old, sick, or healthy, exercising improves blood flow, heart strength, and reduces your risk of life-threatening conditions like heart disease and diabetes. Pulmonary rehabilitation is a type of exercise that’s specifically designed for people with COPD and other chronic respiratory diseases because it’s focused on strengthening the lungs, reducing breathlessness, managing weight, and preventing exacerbations. Learn more about how pulmonary rehab works in this post.

Supplemental Oxygen Therapy
Another standard treatment for chronic obstructive pulmonary disease is supplemental oxygen therapy. Since COPD patients have less efficient lungs than the general population, oxygen therapy is designed to supply them with a higher concentration of oxygen. In turn, this will alleviate difficulty breathing, ensure blood oxygen levels remain stable and help to prevent exacerbations and other complications. Many people are intimidated by oxygen therapy because they believe it will prevent them from getting around and living life on their own terms.

Fortunately, this is not necessarily the case. While older outdated oxygen devices like oxygen tanks and liquid oxygen tanks can be bulky and difficult to maneuver, they’ve since been replaced by lightweight portable oxygen concentrators. Unlike oxygen tanks, concentrators are battery-powered machines that never need to be refilled by an oxygen company. They’re also fully approved by the Federal Aviation Administration (FAA), so you’ll never have to worry about being restricted in where you can travel. For more information on portable oxygen concentrators, be sure to reach out to our respiratory specialists here at LPT Medical.
Smoking Cessation
Smoking cessation can be one of the greatest challenges for many COPD patients. Some people have smoked for decades, so being faced with a COPD diagnosis and the task of quitting immediately, it can be somewhat overwhelming. However, it’s also the single most important thing you can do to alleviate your symptoms and ensure the best long-term prognosis of your disease. Several months ago, we wrote a three-part guide on smoking cessation and recovery so be sure to check it out if you’re interested.

Inhaled Therapy
It’s important not to confuse “oxygen therapy” and “inhaled therapy.” Oxygen therapy is meant to increase blood oxygen levels whereas inhaled therapy is meant to administer COPD medication via a mist called “aerosol.” By inhaling medication rather than taking it orally, you’ll experience greater benefits and you’ll experience the effects almost immediately. Inhaled therapy is usually administered through either an inhaler or a nebulizer device.

Conclusion
While salt therapy (halotherapy) is a trendy topic these days, that doesn’t necessarily mean it’s an effective treatment option for COPD. Although salt therapy has been around for hundreds of years, it’s surprisingly understudied and there is very little empirical evidence to go off of. With that being said, salt therapy has been found to be rather safe as long as you’re not exposed to it in high quantities.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Regardless of what you’re trying to change with your COPD treatment plan, you should always consult your doctor first. He/she may want to take a look at your medical history before determining if it’s safe for you to use salt therapy, or may completely advise against it if there’s a chance it could make your symptoms even worse. You should also take time to plan your day ensuring that you’re focusing on things that you know will improve your symptoms.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!