In this article we are talking about what it means to build new habits, break old ones, and create healthy routines. We will talk about how you can do this successfully, and why it is important for everyone that wants to live a healthy and long life, that cultivating healthy habits is the best way to do it!
The initial steps towards building a healthy routine and good habits can cause a lot of resistance, this is because humans are creatures of habit, therefore any kind of change even if it is good change, is often met with resistance. Resistance starts out as a small hesitation to grow or change, and then you become overwhelmed with it all to the point where you can’t commit to building a healthy routine anymore.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
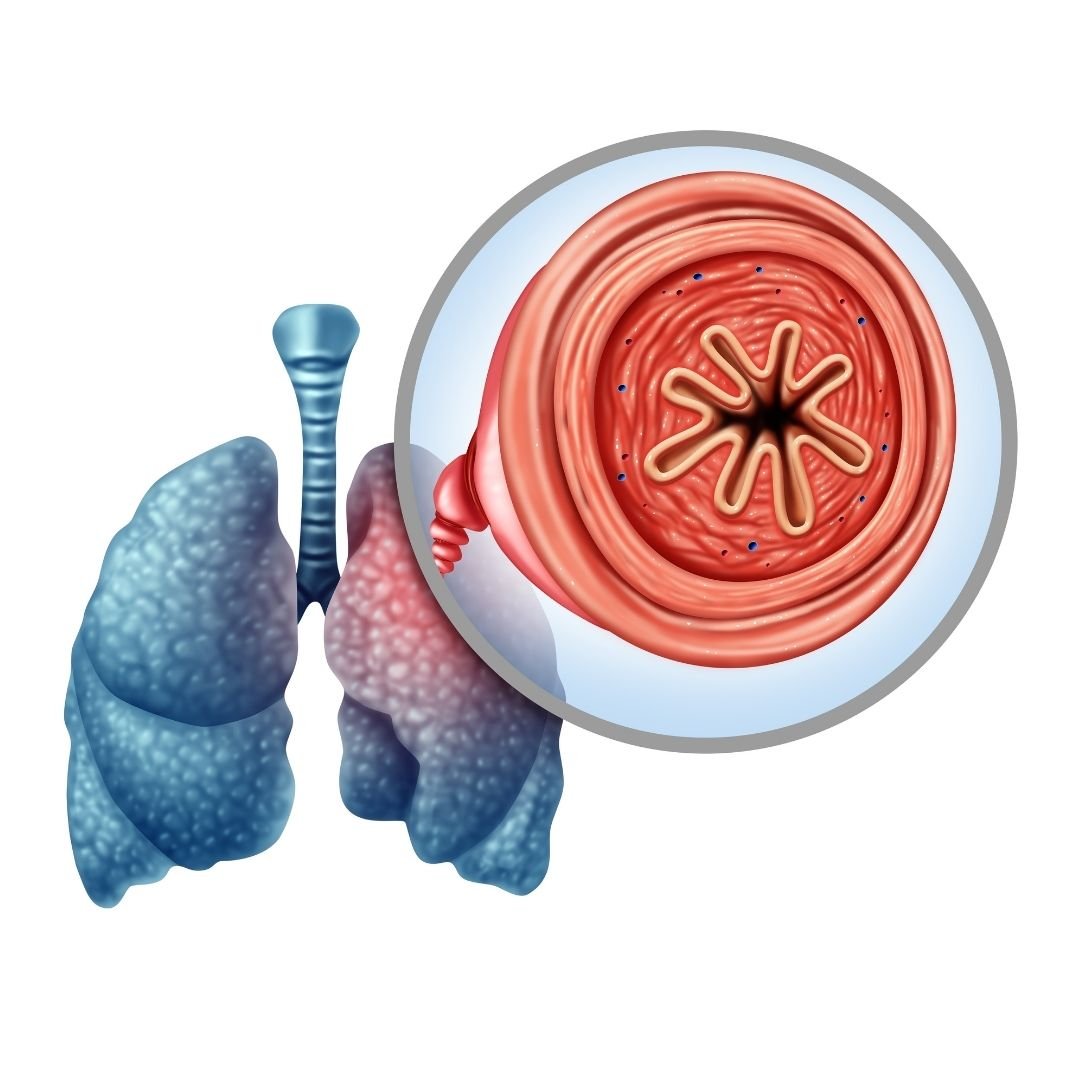
If you have Chronic obstructive pulmonary disease (COPD) building a health routine includes, taking you medication, accomplishing your oxygen therapy, exercising, eating well, among many other things.
COPD is a progressive and chronic lung disease, and it is treatable. COPD causes breathlessness, either due to inflammation in the airways, excess mucus production, or both. People with COPD are treating their condition to avoid exacerbations, improve quality of life, and of course to reduce the chance of death.
Ironically, COPD is often a result of a lifetime of unhealthy habits, like smoking cigarettes, In fact, the primary cause of COPD is exposure to tobacco smoke. So quitting life threatening habits is one of the steps we will discuss in this article.
In this article we will talk about the steps towards building healthy habits, and if you have COPD, how you can use these techniques to create a routine that helps you maintain your COPD treatment on a daily basis.
The first step to building healthy habits is to “Make it Easy”.
Make it Easy
Successfully implementing lasting changes into your life is hard, period. So, our first pieces of advice is to make it easy. Make the change so small and so easy that you have to do it!
The first step in creating healthy habits that stick, is to make the initial changes very simple. This way, there is no excuse not to do it!
There are two ways you can change, you can work towards quitting a nasty habit or getting in the routine of creating a healthy habit.
For instance, if you want to start exercising more, consider doing a minimal amount of exercise per day, this way you can’t excuse the action one day by saying you’re too tired. This goes back to minimizing the amount of resistance. The amount of exercise you set yourself up to accomplish everyday will be relative to your health, so whatever is doable for you whether that is walking to get the mail, or walking 1.5 miles, make it a point to do it everyday.

If you are working towards cutting something bad out of your life, such as eating fried foods, give yourself as easy alternative. Fried foods can cause bloating and discomfort by pushing on your diaphragm, making it difficult and uncomfortable to breathe. Excessively eating fried food can cause you to gain weight which increases pressure on your lungs. If you eat a lot of fried food, working to eat less fried foods can be a habit that you break.
Make this easy by giving yourself a tasty alternative, that fulfills the craving but isn't as bad for you. For instance, 100 grams of fried and battered chicken breast contains 13.2 g of fat, and over-roasted chicken breast only contains 0.39 g of fat.

Breaking habits along with building healthy ones takes time, start making simple changes to train yourself, and this will help you make bigger changes in the future once you are ready.
The next step to building healthy habits or breaking bad ones, is using incremental steps rather than all at once.
Take Multiple Steps to Reach Your Goals

This is a hugely important step to take when breaking down those sticky habits and in some cases curing addiction. Smoking is one of the leading causes of preventable death worldwide and is responsible for more than 480,000 deaths per year in the United States, which goes to show how quitting smoking is not easy.
if you normally smoke one pack a day, it would be unlikely that within one day you will quit smoking entirely. Nicotine is the most common addiction in the United States, a study by the CDC back in 2015 suggested that while about 70 percent of current adult smokers in the United States wanted to quit, about 55 percent had attempted to do so , but only 7 percent were successful in quitting.

Do not let the statistics deter you from trying! Simply start by quitting a little bit day by day and using supplementary hand and mouth fixation tools. Eventually, you can make a step towards going one full day without a cigarette, and subsequently a few days in a row.
There are thousands of quitting techniques circling the internet, and getting advice from you doctor can help you find a technique that works for you. If you fail the first time, try something else, and just take it one step at a time.
This brings us to the next step, and that is celebrating small victories.
Small Wins and The Snowball Effect

Celebrating the small victories in your journey to create new habits implements self trust into your life. Self trust is saying you are going to do one thing, and having the courage, strength, and honestly to stand by your words with your actions.
Self trust is an important aspect of building healthy habits, and breaking down bad ones. Using healthy routine building tools can help you build a solid foundation of self trust.
To celebrate your small wins you reward good behavior, this generates a snowball effect that can start rolling in a positive direction. The goal is to build a small habit initially, it can be easy at the beginning and by using incremental steps over the course of time, you will succeed. In doing so, you will gain the confidence in yourself and your ability to follow through.
Underwhelm yourself, do not overwhelm yourself. Feeling overwhelmed initiates a stress repose, making it even more challenging to do anything. You can build on the underwhelming feeling, and encourage yourself that more positive change can be done little by little.
Living with COPD is challenging enough, but standing by and not doing anything is worse than challenging yourself to break bad habits and build healthy ones.
As we mentioned above, changing your habits doesn't have to be hard, and in fact, it should be easy when you are first starting to make a change.This means creating an attainable plan of action that is easy to accomplish successfully. From there, you can start taking incremental steps towards a larger goal, this takes time and patience, but it is the best way to stay committed to a goal. Lastly, celebrate the small wins, and encourage yourself to continue doing better.
Health Habits for People With COPD
So now that you know where to start, comes the hard part. Deciding what it is you need in your life, or don’t need, that will improve your livelihood. We drafted a few of the habits that are great for people with any respiratory disease including COPD, you can also discuss with your doctor and decide together what it is you should work towards.

Eating more protein rich foods:
Protein is essential to daily living whether you have a respiratory disease or not. Protein gives you energy, something respiratory patients desperately need in order to get through the day. Protein helps build and repair muscle, tissues, and every cell in your body. It can also strengthen your immune system, making you less susceptible to sickness and infection.
Here are some tips for getting protein into you meals more often:
-
Try to eat 5-6 small meals daily. In each meal make sure that you have protein. You can try these small meal idea to get started:
- Peanut butter and crackers
- Handful of nuts or trail mix
- Apple with string cheese
- Greek yogurt with berries
- Sandwich with hummus and vegetables
- Baked potato with cottage cheese
- Hard boiled egg with whole grain toast
-
Bean burrito
-
Try making a smoothie with protein powder, fruit, and milk, and you can even add peanut or almond butter for an extra serving of protein
- Choose whey, pea, or bean protein for best quality.
- Look at the ingredient list to make sure protein is the main ingredient.
-
Avoid protein powders that have herbs or other foreign or unrecognizable ingredients.
- Try to plan your meals and snacks in advance. This will help if you tend to forget to eat or avoid eating because you do not have a strong appetite.
-
Before bed, have a protein-rich bedtime snack to make sure you meet your daily protein needs
- To increase the protein intake of foods you eat regularly, you can add dry milk powder into milk, oatmeal, overnight oats, or yogurt
Exercise 3-4 Times Per Week
This is a habit that is often met with a lot of resistance, and it is something you should work your way up to before going all in.

If you have COPD and do not exercise regularly, starting to exercise will be a challenge. This is when you have to force yourself to do easy exercise that you can accomplish, rather than setting the bar too high.
If you start exercising too much all at once, you will not feel good, and it can tire you out to the point where you end up quitting entirely.
Depending on your current physical activity, you and your doctor or respiratory therapist can set up an exercise program that will start off slow and steady and gradually gets more intense, until you are at a healthy place, which for people with COPD is often 20 - 30 minutes.
Here is a great resource for exercise options for respiratory patients: Improving Your Exercise Tolerance and Quality of Life with COPD.
Get a Portable Oxygen Device

It is normal for oxygen therapy to start interfering with the quality of your life, and while it is important to cover all of your oxygen therapy needs, you cannot let your oxygen therapy control the quality of your life.
If your oxygen tanks are heavy and bulky, it is harder to exercise.
If you have an oxygen tank you cannot travel with it on airplanes.
You might have difficulty carrying a large oxygen unit on errands and end up spending a lot of time at home.
There are a number of aspects that oxygen therapy has held oxygen patients back from doing, and this does not have to be your reality.
Switching to a lightweight, portable oxygen concentrator unit can make it easier to move around, exercise, travel, and so much more. Activities like going to restaurants, running errands, and even traveling can become a lot more convenient with the help of a lightweight battery powered portable oxygen concentrator.

Education is a very important aspect of buying a portable oxygen concentrator, understanding your condition as well as the device will set you up to succeed throughout your oxygen therapy treatment.
Portable oxygen concentrators costs range in prices, depending on if you need a pulse flow device like the Caire Freestyle Comfort, or a continuous flow device like the Respironics SImplyGo. Prices also depend on the batteries each device is equipped with, its weight, and the technological capabilities.
The best way to learn about your options is to speak over the phone with a respiratory specialist, they can converser with your doctor's office to find out exactly what your oxygen intake is, and from there find the perfect device for you.
Learn Breathing Techniques
Practice implementing breathing techniques into your daily life, it is a great way to control your COPD symptoms.
Pursed-lip breathing can open up your lungs, allowing you to take in more air. The purpose is to strengthen your lungs so you can enjoy more activities without breathlessness.
Follow these simple steps:
- Position your lips as if you’re about to whistle
- Breathe in slowly through your nose and count to two or three
- Breathe out through pursed lips and count to four or five
- Repeat this technique up to five times to control your breathing
- Do this multiple times per day if you have time
You can also discuss with your doctor about the possibility of attending a pulmonary rehabilitation course in your area. This type of rehab teaches you different ways to breathe, and better manage your other symptoms.
Learn Coughing Techniques
Coughing is a common symptom of COPD, however it actually has a useful purpose, if done so correctly.
Oftentimes, your cough can be caused by excess mucus that is trapped in your airways, coughing is the natural reaction your body initiates to clear the mucus. If you work on purposefully coughing correctly to clear your airways, you will experience less involuntary coughing throughout the day a night.
You can work on these techniques in the morning and night, as well as before and after you eat. Hopefully, the more you do it in the beginning, the more productive it becomes.
It is also important to take the necessary steps to prepare for clearing your airways, such as drinking plenty of water which will thin out the mucus, and do not eat food that promotes mucus production, such as having too much dairy in one meal.
Huffing, otherwise known as huff coughing, is a coughing technique that helps move mucus from your lungs and it is similar to exhaling onto a window to steam it up.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Huffing is not as forceful as a cough, but it can work better and be less tiring.
The Huff Coughing Technique:
- Tilt your chin tilted slightly up and mouth open
- Take a slow deep breath to partially fill your lungs
- Hold breath for two or three seconds
- Exhale forcefully, but slowly, in a continuous exhalation to move mucus from the smaller to the larger airways
- Repeat this maneuver two more times
- Follow with one strong cough to clear mucus from the larger airways
- Do a cycle of four to five huff coughs as part of your airway clearance
Accomplishing these huffing techniques enables air to get behind the mucus and separates it from the walls of your lungs so it can be coughed out.
There are a lot of other coughing techniques that can be found in this article: How to Cough Correctly with COPD
Overview
Building healthy habits start with a mind set. You can make positive changes in your life that will greatly impact your ability to do more things, and feel physically and mentally better.
Make the initial changes easy, this way your actions cannot be met with resistance, and accomplishing small goals will lead to your capacity to accomplish large goals.
Develop steps for yourself, when changing a habit or creating a new habit, take incremental steps to get to your desired results.
Lastly, cultivate a sense of achievement, even in your small endeavors. This creates self trust, that will reinforce your ability to change for the better.
.jpg)
If you have COPD, changing your habits may be an essential treatment that your doctor tells you is going to help you live longer, and healthier. Your chronic lung disease will not disappear, but you can take control of it.
We hope that you can use the tactics laid out in this article to make healthy lifestyle changes in all aspects of your life.
Chronic obstructive pulmonary disease (COPD) is one of the most common lung diseases in the world. It’s estimated that about 16.4 million people in the United States alone have COPD and millions more are either undiagnosed or at high risk of contracting it. Despite this fact, many people are woefully unaware of what causes this disease and how it should best be managed.
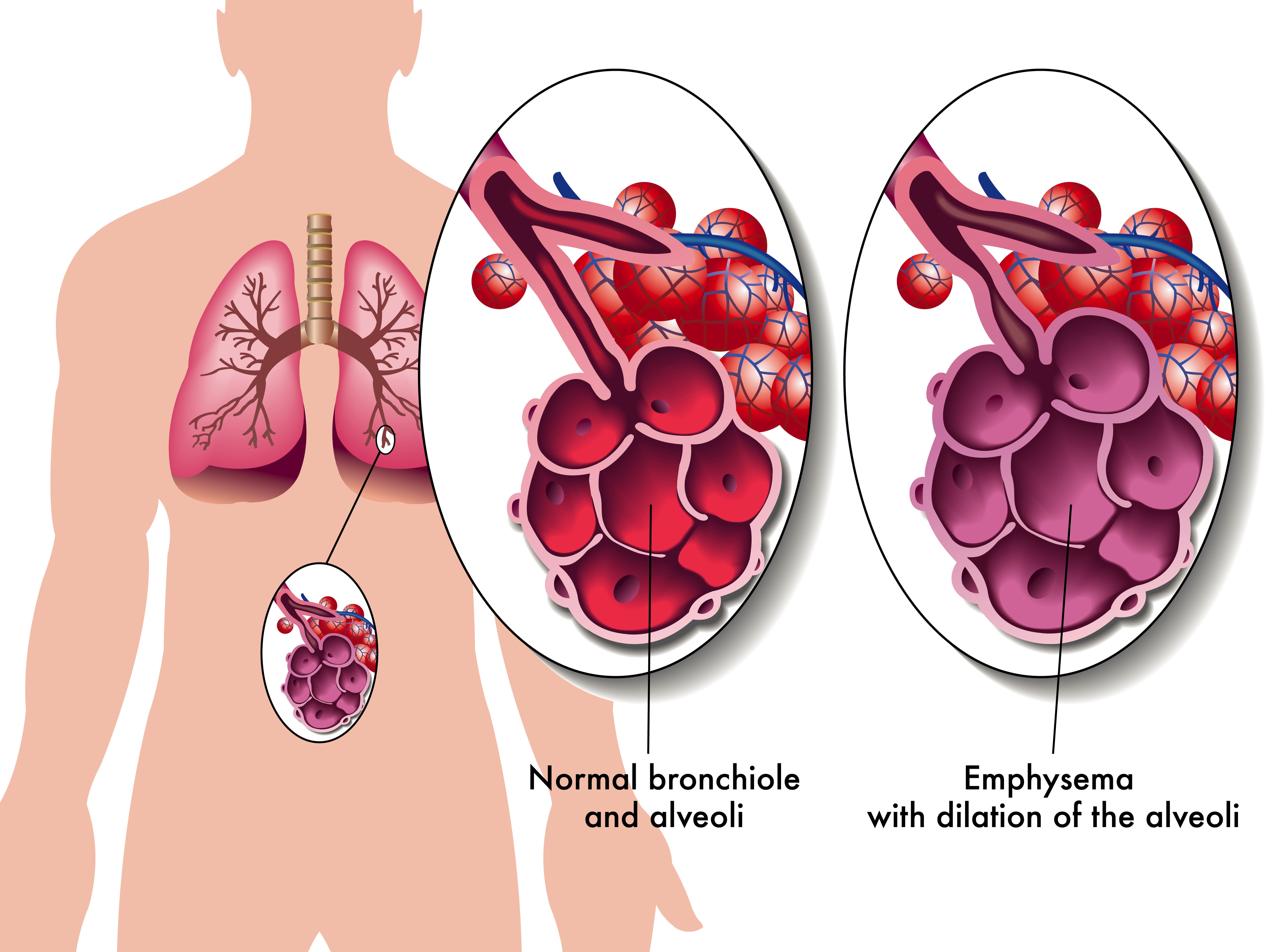
In short, COPD is an umbrella term that denotes two conditions: chronic bronchitis and emphysema. While the symptoms and pathogenesis of these two diseases are slightly different, they are both primarily caused by cigarette smoking. However, in rare instances, someone who has never smoked can contract COPD through something called alpha-1 antitrypsin deficiency (AAT deficiency).
One of the symptoms of COPD that’s particularly vicious is something called an exacerbation. This is similar to an asthma attack in that it causes respiratory symptoms such as breathlessness, chest pain, and sputum production to suddenly become worse, oftentimes requiring you to seek immediate medical attention. In this post, we will help you better understand COPD flare-ups and exacerbations, as well as how to avoid being hospitalized as a result.
If you have any questions or concerns, feel free to leave them in the comment section so we can address them.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What’s the Difference Between a Flare-Up and an Exacerbation?
Generally speaking, the terms “COPD flare-up” and “COPD exacerbation” are used interchangeably. They both refer to respiratory symptoms becoming worse due to environmental causes, infections, or any number of other things. However, when it comes to discussing these symptoms, it’s important to be precise not only about what’s causing them but how severe they are as well.

A mild COPD exacerbation is one that could lead to increased discomfort but is unlikely to cause any serious long-term consequences. These can typically be treated with short-acting bronchodilators (SABD) or “rescue inhalers” which work to quickly open up the airways allowing you to breathe better. Moderate COPD exacerbations should be supplemented with oral corticosteroids which suppress inflammation and antibiotics which can help fight inflammation.

The final type of exacerbation is a severe exacerbation, sometimes called an “acute” exacerbation. This type of exacerbation requires immediate medical attention and can even be life-threatening if it’s not treated appropriately. Ideally, the best way to prepare for this type of exacerbation is to have an action plan and ensure you always have someone on hand to either take you to the hospital or call an ambulance.
Why it’s so Important to Avoid Hospitalization With COPD
According to the American Journal of Respiratory and Critical Care Medicine, COPD is responsible for $72 billion a year in direct healthcare expenditures. The majority of these costs come from hospital visits which range from 4.5 to 8.8 days on average. Around two-thirds of all COPD hospitalizations are due to COPD exacerbations, and the majority of COPD exacerbations are caused by infections — specifically viral infections.

The primary reason it’s important to avoid hospitalization for COPD is because of the risks for your health. According to another study by the aforementioned medical journal, after testing over 2 million patients, the 1-year readmission rate was 64.2% and the 1-year mortality rate was 26.2% both of which were significantly higher than rates among the general COPD population. Readmission and mortality rates are also much higher among patients who were hospitalized with severe exacerbation of COPD.
The second most important reason to avoid hospitalization due to COPD is cost. Frequent or long-term admissions can pose a significant financial burden on people with COPD which can also lead to stress, anxiety, and even depression. In our last post, we highlighted some key ways that you can avoid unnecessary financial costs due to COPD so check it out if you’re interested in learning more.
Have a Plan to Deal With Exacerbations
First and foremost, if you want to avoid hospitalization due to COPD exacerbation, you need to have a plan of action before an emergency occurs. An action plan is a sort of written outline that you will follow in order to accomplish a certain goal. This way, if you notice your COPD symptoms starting to worsen, you can refer to your sheet instead of worrying about making difficult decisions at the moment.

In order to prepare your COPD action plan, you should first consult your doctor. He/she will likely already have a template that you can fill out to make this process a little easier. On this action plan, you will need to create an “action” for every symptom you experience. For example, if the symptom is a gradual decrease in your blood oxygen levels, you might make a note to increase your oxygen flow setting or contact your doctor. If you experience sudden shortness of breath, you might make a note to use your rescue inhaler.
Another important thing to know about your COPD action plan is that it should not be private information. You should make it a priority to go over your plan with friends and family, especially if they spend a lot of time with you. This way, if you are in a situation where you are unable to act out your action plan, they will be able to help. In this post, we discuss how you can prepare for medical emergencies and hospital visits with COPD, so check it out if you want to know more.
![]()
Change Up Your Diet
Diet can be a very difficult topic to discuss in this day and age. Most people have access to more types of food than ever before and there is a near endless list of diets that people swear by. As a result, it can feel like an insurmountable task trying to find something that keeps you happy and healthy. The good news, however, is that many years of research have been dedicated to COPD diets, so you shouldn’t have to do much scrambling to make sense of it all.
![]()
Generally speaking, COPD patients should maintain a diet that’s high in protein, fiber, and fat, but low in carbohydrates. The reason for this is that the metabolism of carbs produces the highest amount of carbon dioxide in the body while the metabolism of fat produces the least. Adequate protein ensures your respiratory muscles stay strong and efficient, and fiber helps to control blood glucose levels and reduce cholesterol in the blood.
Another reason to keep your diet healthy, natural foods rather than processed ones is because weight management is vital to COPD management. Most often, people tend to become underweight after contracting COPD due to a loss of appetite or other factors. Sometimes, people experience a loss of appetite because consuming food is more physically exerting than it was previously, and bloating can contribute to breathing difficulties. COPD patients who are underweight may find that they lack the energy or endurance to make it through the day.
On the other hand, being overweight with COPD can contribute to breathing problems as well. While it is less common for a COPD patient to become overweight than underweight, the problems associated with it can be just as severe. Simply put, having a higher body mass index (BMI) can be obstructive to your breathing by putting more strain on your lungs when you inhale. However, some studies have found mixed results when it comes to being overweight/obese with COPD.
Be Consistent With Your Exercise Routine
Consistency is unbelievably important when it comes to treating COPD and preventing exacerbations. For example, your diet is much more likely to benefit you if you keep up with your goals week in and week out. But if you do well one week then cheat the next, you’re going to put yourself at a much higher risk of COPD complications like exacerbations. This works pretty much the same way when it comes to your exercise routine.

Oftentimes, exercise specialists will talk about getting into a “routine.” In other words, you do the same exercise each day for an allotted period of time. By doing so, it will be much easier to track your progress and catch yourself when you fall back on your plan. This works well for most people who want to commit to an exercise routine, but it’s especially useful for COPD patients who benefit more from consistent moderate exercise rather than high-intensity exercise.
Avoid Getting Sick
Lung infection is both the number one cause of severe COPD exacerbation and the number one cause of hospitalization due to COPD. With that being said, staying healthy and avoiding infection (especially lung infections) is vital. One of the best things you can do right now to avoid getting sick is to quit smoking or avoid second-hand smoke if you live around smokers.
It’s been known for quite some time that smoking reduces the immune response in the body and also makes the smoker more likely to have exaggerated responses to viral infections. During influenza outbreaks and with the current situation we face involving COVID-19, smokers have a much lower survival rate when compared to the general population. Not to mention that smoking and second-hand smoke can trigger COPD exacerbations even if an infection isn’t present.

Another thing you can do to avoid getting sick is to be more conscious of your daily habits. For example, do you wash your hands frequently throughout the day? Do you take care to avoid places that are unclean or unsanitary? Do you stay away from people who exhibit symptoms of the cold or the flu? Do you clean surfaces in your home like door handles, coffee pot handles, or faucet handles? Are you following all the precautions recommended by the World Health Organization (WHO) in order to prevent contracting the novel coronavirus?
Last but certainly not least, you should be getting the doctor-recommended eight hours of sleep each night in order to avoid getting sick. According to WebMD, sleep deprivation suppresses the immune system and puts you at a higher risk of contracting colds, the flu, and other ailments. This is an especially difficult topic for many COPD patients because respiratory symptoms can make it difficult to maintain a healthy sleep schedule. In this post, we take a look at some actionable tips to improve your sleep if you have COPD.
Avoid Environmental Triggers
It can be a scary world out there for anyone who values their lung health. From wildfire smoke to car exhaust and pollen, it’s easy to feel like no place is safe. The Environmental Protection Agency (EPA) even reports that indoor air can be two to five times more polluted than outdoor air. Fortunately, it’s not all grim news for COPD patients who want to avoid exacerbation triggers. Just by following a few simple steps, you’ll be well on your way to avoiding the most common triggers.

Despite summer ending last week, we are still in the midst of wildfire season. As a result, COPD patients need to be aware of when they go outside, especially when it concerns exercising outdoors. Air quality index (AQI) is the measurement we use to determine how safe outdoor air is to breathe. Each day before you go outside, be sure to check AirNow.gov for the AQI in your area. If the AQI is above 100, this is a sign that the air quality is too poor for people with lung diseases like COPD, asthma, or pulmonary fibrosis.
Another thing you should be wary of is seasonal allergies. Contrary to popular belief, allergies are a reality during all times of the year as opposed to only being active during certain seasons. In September and October, allergens like ragweed are typically at their peak. According to WebMD, if you get allergies in the spring, you are about 75% likely to have reactions to ragweed. So, if you’re outside this trying to enjoy the fall colors and cool weather this year, just be aware that allergies are still a reality.

The final airborne COPD exacerbation triggers we’d like to talk about are the ones found in your home. Like we mentioned earlier, indoor air can potentially be more dangerous than outdoor air. This is because the air in your home is extremely concentrated, so if you track things in like dust, allergens, or smoke, it will likely start to build up in one area of your home unless you take the time to clean regularly. While it may not seem that important, taking the time to vacuum, dust, and wipe down surfaces every day can go a long way to preventing COPD exacerbations. What’s more, it will help you get your daily exercise.
Use a Reliable Portable Oxygen Machine
Last but certainly not least, having a reliable portable oxygen device that you can take anywhere will put you in the best position to avoid COPD exacerbations and hospitalization. For the vast majority of COPD patients, supplemental oxygen therapy is a medical necessity. Not only does it stabilize your lung condition, but it also ensures your blood oxygen levels are normal, which in turn saturates every organ in your body with the oxygen it needs to function properly.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
For the foreseeable future, portable oxygen concentrators are your best bet for reliable portable oxygen. Unlike oxygen tanks or liquid oxygen tanks, portable oxygen concentrators are electronic devices. So, instead of having to go out of your way constantly to have your tanks refilled by an oxygen specialist, you simply need to carry batteries with you. Fortunately, these batteries are lightweight and don’t take up very much space in your backpack or handbag.

Currently, the best portable oxygen concentrator on the market is the Caire FreeStyle Comfort. It weighs in at only 5 pounds and it offers 5 different flow settings that you can adjust on the fly as needed. One of the unique features of the FreeStyle Comfort is its ergonomic design which keeps the device comfortably at your side rather than jostling around as some other concentrators do.

Another portable oxygen concentrator we’d like to recommend is the Inogen One G5. While this POC came out last year, it’s still very relevant and a great choice for anyone who needs a reliable 24/7 medical oxygen supply. The Inogen One G5 has one more pulse flow setting than the FreeStyle Comfort and it weighs slightly less at just 4.7 pounds. Inogen is one of the top brands in the medical oxygen industry and they take pride in customer satisfaction.
In rare instances, your doctor may require you to use a continuous flow concentrator. If this is the case, we recommend the Respironics SimplyGo portable oxygen concentrator. This unit is twice as heavy as the Caire FreeStyle Comfort, but since it puts out a continuous flow of oxygen, it can be used with your CPAP or BiPAP machine if you have sleep apnea or another related sleeping disorder. If you’re looking for affordable portable oxygen concentrators, don’t hesitate to visit our online oxygen store.

Conclusion
Unfortunately, exacerbations and flare-ups are a reality for COPD patients. But that doesn’t mean that you can’t take steps to reduce your risk of experiencing hospitalization due to an exacerbation. Above all, following your treatment plan as closely as possible and preventing sickness like the cold or flu will be your best bet if you want to avoid hospital visits.
If you would like to learn more about managing chronic respiratory conditions such as COPD, stay tuned to our blog. We aim to equip our readers with the knowledge they need to combat breathlessness, chest pain, and fatigue in their daily lives, as well as learning how to cope with the mental aspects of chronic disease like anxiety and depression. Feel free to leave a comment below if you have any questions or concerns.
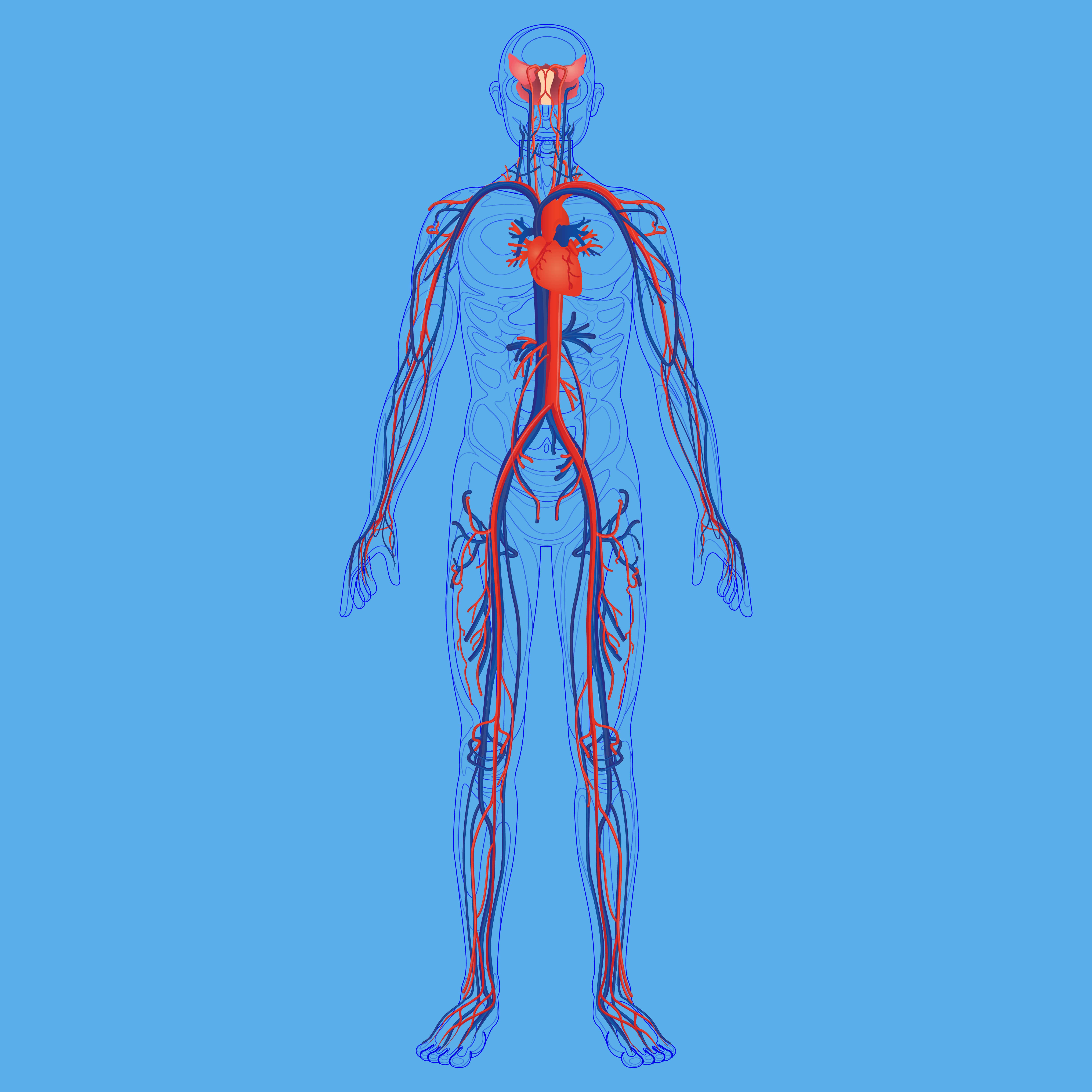
.png)
There are three main types of respiratory disease: airway diseases, lung tissue diseases, and circulatory diseases. The first type, airway diseases, affect the tubes called bronchioles, usually causing them to narrow, swell, or become filled with a slimy substance called mucus. Airway diseases include asthma, a specific type of chronic obstructive pulmonary disease (COPD) called chronic bronchitis, and bronchiectasis, a condition that results from recurrent lung infections.
The second type of respiratory disease, lung tissue disease, specifically affects the tissue within the lungs. Oftentimes, these diseases cause the lungs to become inflamed and lose their elasticity which is why they’re usually categorized as “restrictive” lung diseases because they prevent the lungs from expanding fully. Pulmonary fibrosis is one common type of lung tissue disease and it results from the formation of irreversible scar tissue in the lungs.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The final type of respiratory disease is lung circulation disease. This type is a little more complicated in that it affects the complex interactions between your lungs and the rest of your circulatory system. These diseases prevent the lungs from processing oxygen from the air you breathe and releasing carbon dioxide, resulting in an imbalance of gases in the body. As you can imagine, these diseases are closely linked with cardiovascular issues.
Believe it or not, COPD has elements of all three of these categories, so it’s more complicated than most people think. In the following sections, we’ll take a look at 7 interesting facts that you may not know about COPD. After reading this, we hope that you are more aware of the global burden of COPD and that you’ll feel inclined to share this information with friends and family members who may be at risk of contracting COPD.

It’s One of the Most Preventable Chronic Illnesses
When we say a disease is “preventable,” we mean that personal lifestyle choices most often cause the disease to take hold. For example, acute illnesses like the flu or the common cold can be prevented with vaccinations and proper hygiene. But when it comes to COPD, this is not quite so simple. According to lung.org, 85 to 90 percent of all COPD cases are caused by cigarette smoking, but there are also other risk factors at play such as environmental pollution and genetics which makes COPD a difficult disease to prevent.
![]()
When you compare COPD to some of the other leading preventable illnesses in the world, it’s not hard to see why COPD is so difficult to prevent. Heart disease, cancer, and diabetes are some of the most discussed diseases and more often than not, this results in a high level of funding while other prominent diseases like COPD are left behind. According to a survey published in ScienceDaily, 38 percent of people with COPD were unaware of the disease before being diagnosed. This often leads to people referring to COPD as a “silent disease,” because it can feel like patients don’t have much of a voice in the community at large.

Perhaps, one of the reasons that COPD has such a lack of awareness is because of how slowly the disease develops. Typically, COPD takes many decades to progress from its early stages to its later stages. This is in stark contrast to diseases like lung cancer which tend to come on more quickly. Unfortunately, this leads to people underestimating the risk of COPD and not taking it as seriously as it should be. Another thing that can overshadow COPD is the fact that lung cancer shares the same awareness month, November. Since lung cancer has more funding in the first place, many people overlook COPD funding and support.
COPD Cannot Be Reversed
COPD is what’s known as a “progressive disease.” What this means is that symptoms related to this respiratory condition get worse over time. While symptoms may subside after a flare-up or exacerbation, these events usually result in a permanent drop in lung function. This is in contrast to conditions like asthma which exhibits similar symptoms, but after experiencing an asthma attack, most people fully recover and don’t maintain any permanent damage to their lungs.
As a result, the most important thing you can do to prevent your disease from progressing, or at the very least, slow its progression is to avoid common COPD triggers. We discuss in detail in this post how you can avoid COPD exacerbations, but we’ll summarize the points here for your convenience. First and foremost, infections are the cause of around 51% of all COPD exacerbations, so preventing them should be your top priority.
When you were young and didn’t have any chronic conditions, you probably weren’t too concerned about the flu or the common cold. These are infections that our body has adapted immunity towards allowing us to fight them off quickly, with or without the use of medications. However, the older we get older, these seemingly harmless things become a lot more serious, especially for people with chronic respiratory illness. It’s estimated that bacterial infections are the cause of 40 to 50 percent of all COPD exacerbations and a significant portion of hospitalizations as well.

Another major cause of COPD flare-ups and exacerbation is air pollution. No matter where you are and what the time of year is, there is air pollution. And if you want to slow the progression of COPD, you should be careful to check the quality of air wherever you go. AirNow.gov is a great resource for anyone who wants an accurate and up-to-date description of the air quality in their area. It’s recommended that COPD patients avoid going outside if the AQI (air quality index) is over 100.
Smoking Cessation is Still Important
There’s a strong belief among many people who have been diagnosed with COPD that “the damage has been done” and that “smoking cessation won’t help.” However, this could not be farther from the truth. While there is no cure for COPD, smoking will most certainly make your symptoms worse. In fact, cigarettes are an immunosuppressant drug meaning they inhibit the body’s innate and adaptive immune system. This puts you at a higher risk of infection and hampers your body’s ability to heal.

According to reports from the Centers for Disease Control and Prevention (CDC), about 38 percent of Americans who have COPD are current smokers. This is pretty astonishing considering that smoking is entirely counterproductive to a COPD treatment plan. Unfortunately, everyone is different so there’s no set smoking cessation plan you should follow. Your best bet will be to speak with your doctor who can help you find something that will work for you.
![]()
Another thing that will help is being away from a household where people have smoked or currently smoke. Secondhand smoke can be equally as dangerous as smoking yourself and experts estimate that the harmful chemicals in cigarettes can linger in a room for as long as five hours. In other words, if you smell cigarettes, you’re probably inhaling harmful chemicals that could lead to a COPD exacerbation. If you live with someone who smokes, try asking them to do it outside.
Every Case of COPD is Different
While around 16 million Americans have COPD, every case is unique. COPD is an umbrella term that’s used to denote two different chronic illnesses: chronic bronchitis and emphysema. And while these conditions might exhibit similar symptoms such as a chronic cough, breathlessness, and fatigue, they’re very different in terms of their causes, risk factors, and prognosis. These conditions can also occur in different parts of the respiratory system and work in tandem with co-morbidities which further complicates treatment and outlook.

Emphysema is what many people think of as the “smoker’s disease.” It’s a condition that affects the alveoli, the tiny air sacs that scatter the lungs. These air sacs are responsible for the exchange of oxygen and carbon dioxide to and from the bloodstream, so they play a key role in our systemic health. In someone with emphysema, the alveoli begin to lose their shape and fill with fluid meaning the transfer of gases is less efficient.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
In many cases, doctors will prescribe supplemental oxygen therapy which can help reduce the burden on the lungs. But it’s important to understand exactly how much you should be receiving because too much oxygen can lead to oxygen toxicity. This can result in symptoms such as coughing, difficulty breathing, and in severe cases even death. Make sure you’re clear on when to use oxygen and how much to use and don’t assume that increasing your oxygen intake will help you feel better.
The treatment options for emphysema also vary based on where the emphysema is located. For example, if the emphysema is located in one specific area of the lung, you may be a candidate for lung volume reduction surgery. This is a procedure that involves removing the damaged tissue in the lungs which prevents air from getting trapped and causing difficulty breathing. While it may sound counterintuitive to remove part of your lungs in order to help you breathe better, sometimes the benefits outweigh the negatives.
In other cases, emphysema patients may be a candidate for something called endobronchial valves. This is a less intrusive alternative to lung volume reduction surgery and involves inserting one-way valves into certain airways. The end result is that air won’t get trapped in areas of the lungs with emphysema and you’ll be able to breathe easier.
Lastly, COPD can be complicated when co-morbidities such as sleep apnea are involved. Sleep apnea is a condition where the airways close up as you sleep resulting in disruptions in your sleep and more serious long-term effects such as an increased risk of high blood pressure (hypertension) and heart attack. When COPD and sleep apnea occur together it is referred to as overlap syndrome, and studies have found that this phenomenon is common, especially as COPD progresses.
There is a Genetic Component to COPD
There is a small group of COPD patients that are often excluded from larger discussions about COPD and its causes. These are people who contracted COPD without ever picking up a cigarette or spending time around smokers. While alpha-1 antitrypsin deficiency (A1AD) is rare, it is the number one cause of COPD in non-smokers and people who live otherwise healthy lives.

A1AD occurs when the liver does not produce the correct amount of the alpha-1 protein. This protein is responsible for protecting the lungs from damage due to inflammation and it also prevents damage due to scar tissue in the liver. In these people, even something as simple as exposure to poor air quality or higher than normal levels of air pollution can lead to permanent lung damage and even COPD.
While there is no cure for alpha-1 antitrypsin deficiency, there are treatment options available. It’s also very important to recognize it at an early age so awareness is key. One possible treatment option is called augmentation therapy (replacement therapy). This is where the patient receives replacement alpha-1 from a donor once a week through an IV treatment. While this is not a cure-all, it can play an important role in delaying damage to the lungs. This is another reason it’s important to start as soon as possible.
COPD is More Common in Women
For many decades, COPD was primarily a disease that affected men. This is largely due to the fact that women did not smoke very frequently before the 1950s. However, since then, the gap between men who smoke and women who smoke has narrowed significantly. With that being said, the number of smokers, in general, has decreased from 40 percent in the 1970s to around 14 percent in 2017.

Another reason COPD is more common among women is that women are proven to have a faster rate of decline in FEV1 (forced expiratory volume in one second) than men despite smoking less heavily. Studies have also shown that women have higher hospitalization rates and deaths due to respiratory failure or comorbidities.
COPD Patients Can Live a Long and Healthy Life
It’s so easy to fall into a line of thinking where being diagnosed with a chronic condition means it’s the end, but this couldn’t be farther from the truth. While receiving a COPD diagnosis should act as a wake-up call for heavy smokers, it is far from “the end.” Many COPD patients are able to live long, happy lives as long as they make a serious effort to change their lifestyle for the better.

According to Medicinenet.com, the five-year life expectancy for newly diagnosed COPD patients is 40% to 70%. This is despite the fact that as many as 38% of people diagnosed with COPD continue to smoke and many don’t follow through with the treatment plan that their doctor set forth for them. On the other hand, people who immediately quit smoking and implement healthy choices like supplemental oxygen therapy, a healthy diet, and a consistent exercise routine see much better results. Some people with COPD have lived well into their 70s and 80s.
Conclusion
COPD is a leading cause of death in the United States and it’s also one of the most preventable illnesses in the world. Despite this fact, many people are woefully unaware of what exactly it is and how it affects the body. In comparison to other chronic illnesses like lung cancer or heart disease, COPD receives a lack of funding. This has led to many people referring to it as an “invisible illness.” — many people are affected, yet many suffer in silence.
The good news is that everyone can play a role in the treatment and prevention of COPD. if you have COPD, you can take part in clinical trials which helps to pave the way for researchers and doctors. If you have a friend or loved one with COPD, you can take time out of your day to help them manage their disease. And if you don’t have any connection to COPD, you can still get involved by donating or volunteering with organizations like the American Lung Association or the COPD Foundation.
.png)
According to Philip Tierno, director of clinical microbiology at NYU, humans come into contact with around 60,000 germs every day. However, only about one to two percent of these are potentially harmful. Our body also has innate and adaptive immunity which helps to protect us from these dangerous bacteria. Innate immunity is the defense system that’s in place when we’re born, and adaptive immunity is our body’s defense which develops over time as we’re exposed to more and more bacteria.
With the advent of the novel coronavirus, people have been much more conscious about their exposure to bacteria and viruses. The World Health Organization (WHO) has put forth a list of best practices for avoiding exposure to COVID-19 such as social distancing practices, mask-wearing, and other hygiene measures. And at the end of last year, we saw the first COVID-19 vaccine being tested on high-risk patients.
Despite the urgency of the COVID-19 vaccine, many people still have doubts about getting vaccinated due to the perceived risks. Older adults with chronic illnesses such as chronic obstructive pulmonary disease (COPD) or other respiratory diseases are proven to be at the highest risk of both contracting and experiencing severe reactions to the virus, yet many of these people choose not to get the vaccine.
In this post, we’re going to go over everything you need to know about getting vaccinated as a COPD patient, why it’s important, and settle any doubts or fears that you may have about the process.
What is a Vaccine?
Aside from safe hygiene practices, vaccines are the best tool that we have to fight bacterial and viral infections. Vaccinations are made from the same germs that cause the disease, but they are either weakened or killed so they don’t actually make you sick. What this does is causes your immune system to produce antibodies that can be used to fight off the disease if you come into contact with it. In other words, you’re developing immunity to the disease without actually contracting it.

Vaccines are not a new concept by any means, but the practice of vaccinology has evolved over time. According to healthaffairs.org, the first successful vaccine is credited to Edward Jenner, an English physician. In 1796, he administered a vaccine to a small child which prevented smallpox. While this vaccine was effective in the general population, there were limitations when it came to administering the vaccine to large groups of high-risk people.
With modern technology, however, administering vaccines has become much easier and more effective. While the first COVID-19 vaccine was administered this past December, there are already over 39 million people worldwide who have been fully vaccinated and over 120 million who have received at least one dose. What’s more, the vaccine is being administered to high-risk patients and front-line healthcare workers before everyone else which will increase its effectiveness in the long term.
Why Do COPD Patients Need Vaccines?
Most COPD patients are considered “high risk” when it comes to transmittable diseases like COVID-19 and influenza. According to Healthline, COPD is most common in people over the age of 40, and studies have shown that the average age of death for COPD patients is around 77.4 years of age. According to the Centers for Disease Control and Prevention (CDC), seniors over the age of 65 are at the highest risk of COVID-19, making up about 80% of the total deaths. They also report similar trends with influenza and other infectious diseases.

Another factor that contributes to COPD patients being “high risk” is that many of them are smokers. According to Very Well Health, 38% of adults with COPD continue to smoke. Nicotine, one of the most harmful chemicals found in cigarette smoke, alters the immune response in your body putting you at a higher risk of contracting an infection. According to news-medical.net, carcinogens are the main immunosuppressive agents in cigarette smoke. One of the worst effects of nicotine is that it inhibits the release of reactive oxygen species (ROS) which weakens the ability of neutrophils to kill pathogens (a microorganism that causes disease).
Infection is the Most Common Cause of Exacerbation
A COPD exacerbation is a period of time where your respiratory symptoms suddenly worsen. For example, if you normally experience mild breathlessness and chest pain throughout your day, an exacerbation could cause you to experience more severe symptoms that prevent you from going about your day. Exacerbations can range in severity from mild to severe. They can also have varying time frames from several hours to several days depending on what caused it.
While many things can cause an exacerbation such as air pollution, over exercising, or allergies, lung infections are by far the most common cause. Although infections like pneumonia can be mostly harmless in younger people with healthy lungs, they can be much more serious in COPD patients. COPD, especially chronic bronchitis, is associated with swelling and increased mucus production in the airways. Infections like influenza can contribute to this issue making it even harder to catch a breath.
Infection Can Cause Hospitalization
Not only does infection result in COPD exacerbations, but it’s also the most common cause of hospitalization in COPD patients. Hospitalization is something that you want to avoid at all costs, not only because it’s an indication you’re suffering from something severe, but also because it’s a very heavy financial burden. In 2016, the average cost of a hospital stay was $11,700 meaning it’s the most costly healthcare spending in the country. For more information on avoiding hospitalization due to COPD, read through this post.

Another reason it’s important to avoid hospitals is because they’re not a safe place for you to be during a pandemic. While doctors want anyone and everyone who’s experiencing a medical emergency to feel safe going to a hospital, there’s no reason to risk it if you don’t have to. Not every hospital has the same policies or safety practices when it comes to COVID-19 prevention, so it’s important to research hospitals and do what you can to prevent being hospitalized.
It Protects Other People
Last but certainly not least, getting vaccinated plays an important role in protecting people around you. Infectious diseases are often passed from person-to-person via physical contact or simply breathing the same air. While getting vaccinated is not a surefire sign that you won’t carry a disease or pass it onto someone else, it can help. Even if you are vaccinated for COVID-19, however, you’ll still need to wear a mask and maintain safe social distancing.

Are There Risks to Getting a Vaccine?
Unfortunately, the risks of getting vaccinated are often blown out of proportion. People hear of friends or family members experiencing symptoms of the disease they’re being vaccinated for and this turns them off of receiving the vaccination themselves. But this is a perfectly natural reaction to the vaccination and it’s actually a good sign that the vaccine is working as it should. This is because your body is creating an immune response that leads to the creation of antibodies which inevitably prevents you from getting sick.
![]()
Which Vaccines Should COPD Patients Receive?
Influenza Vaccine
The influenza vaccine is possibly one of the most important vaccines you can receive because hundreds of thousands of people are hospitalized due to the flu every year. Flu symptoms include.
- Headache
- Runny nose
- Sore throat
- Fatigue
- Shortness of breath
- Cough
-
Fever

It’s recommended that you receive a flu vaccine every year because your body’s defenses will diminish over time. Another reason to keep up to date with your flu vaccines is that there are different strains of this virus. The vaccines may be updated from year-to-year in order to ensure that people have immunity to all of these changing strains.
Pneumococcal Vaccine
Pneumococcal disease is the name for infections caused by Streptococcus pneumoniae. You might have never heard of this type of vaccine and that’s because it’s not recommended for everyone. However, the reason it’s often recommended for COPD patients is to prevent pneumonia. This is a respiratory infection that attacks the alveoli, the tiny air sacs in the lungs that are responsible for the exchange of oxygen and carbon dioxide to and from the blood. COPD patients are more susceptible because they often struggle to clear mucus from the lungs which can carry bacteria.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Tdap Vaccine
Pertussis, or whooping cough as it’s more commonly known, can lead to pulmonary hypertension (high blood pressure in the lungs), brain damage, seizures, and even pneumonia. Even the mildest cases of whooping cough can exacerbate COPD symptoms, potentially leading to hospitalization. It’s recommended that adults receive one dose of the Tdap vaccine and they also have the option of getting a booster shot every 10 years which strengthens its effects.
Zoster Vaccine
Chickenpox is a highly contagious infection that’s characterized by rashes on the skin. If you’ve had this condition earlier in life you might experience a recurrence called shingles. This is because, after you recover from chickenpox, the virus moves to your nerve tissue where it can emerge later in your life. Fortunately, if you have never contracted chickenpox during your life, you are not at high risk for shingles.
Studies have shown that COPD patients who have had chickenpox are twice as likely to contract shingles as healthy individuals who have had chickenpox. This is most likely due to the widespread inflammation and immune system disruptions caused by the disease. Be sure to speak with your doctor about getting a zoster vaccine if you believe you’re at risk of contracting shingles.
COVID-19 Vaccine
The coronavirus is at the top of everyone’s minds at the moment, and rightfully so. Since early last year, people have been scrambling to find ways to live normal lives without putting themselves and others at risk of contracting this virus. Miraculously, healthcare professionals were able to test out the first-ever COVID-19 vaccine at the end of the year and now it’s being mass-administered all over the world.
As we’ve learned, the people who are at the highest risk of contracting and experiencing severe symptoms from COVID are older adults with chronic conditions, especially pulmonary disease, heart disease, and diabetes. If you fit any of these descriptions, it’s time to reach out to your doctor and ask about receiving a COVID vaccine.
Speak With Your Doctor First
Before going out to get a vaccine, it’s important to first speak with your doctor. Since vaccines are such an important part of COPD management, you’ll want to have a plan to follow before taking any action. Your doctor will recommend vaccinations based on your age, medical history, as well as the expected prognosis of COPD or any other chronic condition you have. In rare cases, your doctor may advise you to not receive a vaccine due to the perceived risks.

Other Safe Practices to Prevent Infection
Social Distancing
Social distancing, also known as physical distancing, is the practice of maintaining distance between yourself and others. While it’s debated exactly how much space you need in order to prevent the spread of illness, the World Health Organization (WHO) recommends six feet. However, it’s also important to consider the type of environment that you’re in. If you’re indoors where ventilation is poor, you may need to maintain more physical distance in order to be safe. Another thing you should do is be sure to cover your coughs and sneezes in your shoulder.

Wearing a Mask
Surgical masks and cloth face coverings are not designed to filter out viruses, but this doesn’t mean they aren’t helpful when it comes to preventing the spread of disease. Face coverings are effective at preventing large droplets of saliva or mucus from exiting or entering the mouth as well as helping to prevent germs from escaping when you cough or sneeze. It’s important to make sure you’re wearing your mask correctly by ensuring that it covers both your mouth and your nose. Also, make sure the ear straps are tight enough that you don’t have to constantly adjust the mask with your hands which can increase your risk of getting sick.
.jpg)
Practicing Good Hygiene
Hygiene is something that you can always work at to improve and it’s especially important during a pandemic. You should be washing your hands with soap and water periodically throughout the day especially before eating, drinking, and going to bed at night. Cleaning surfaces in your home such as door handles, tables, chairs, keyboards, and countertops will also help to prevent the spread of bacteria.

Follow Your COPD Treatment Plan
At the end of the day, following your COPD treatment plan is just as important as getting vaccinated. Smoking cessation, supplemental oxygen therapy, a consistent exercise routine, and a well-balanced diet will all promote a healthy immune system which is essential for warding off disease, including the novel coronavirus. It will also keep your symptoms in check so that if you do end up getting sick it will be less severe and easier to cope with.
.jpg)
While COPD is not a disease that can be stopped or reversed, a carefully planned treatment regime will significantly reduce adverse symptoms and slow the rate of respiratory decline. It can be overwhelming trying to completely overhaul your lifestyle so you should take things day-by-day and don’t be afraid to reach out to your doctor when you have any questions. Family and friends are also the best people to rely on when you’re facing challenges caused by your disease.
Conclusion
Like anything healthcare-related, vaccinology is a field that continues to grow and evolve. As new infectious diseases are discovered and others mutate, we need new technology and inventions in order to cope with them. Since the advent of the novel coronavirus in 2019, there’s been an increased emphasis on protecting high-risk individuals such as those with COPD and other chronic conditions as well as people over the age of 65 who have a less-active immune system.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
While there are occasionally risks associated with vaccines, for the most part, they play a crucial role in keeping people safe and healthy, especially those with chronic obstructive pulmonary disease. Fortunately, COVID-19 vaccines are being distributed all across the world for high-risk individuals, so it’s the perfect time to get one if you haven’t already.
Lastly, you should continue to follow your COPD treatment plan and speak with your doctor regarding your concerns. Supplemental oxygen therapy, pulmonary rehabilitation, and a balanced diet all play a crucial role in maintaining your health so it’s important to take a holistic approach to your health.
.png)
Chronic obstructive pulmonary disease (COPD) is a debilitating lung condition that affects around 16 million people in the United States. While there are many symptoms of COPD, shortness of breath, chest pain, and chronic fatigue are among the most crippling. In the early stages of COPD, these symptoms are mild and sometimes even go unnoticed by the patient. However, as time goes by, these symptoms become progressively worse and become even more of a burden for the victim.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Unfortunately, there is no magic wand that you can wave to reverse the effects of COPD. Treatment for this disease is aimed at slowing the rate that it progresses, reducing the risk of exacerbation, and managing chronic pain. And since every case of COPD is different, you’ll need to rely on information from your doctor and make lifestyle changes accordingly in order to achieve the best results.
But many COPD patients are left to wonder if there are other methods that can be used to ease the physical, emotional, and financial burdens of their disease. In our last post, for example, we took a look at some tips for living in the moment with COPD. Doing so will help you settle your regrets about the past and concerns about the future, instead, focusing them on things that you can change in the here and now.

Another thing you should be doing is applying for disability benefits which will help you out with some of the financial difficulties of managing a chronic disease. In this post, we’ll take a look at everything you need to know about Social Security Disability Insurance (SSDI) and how you can apply if you have COPD. If you have any questions, be sure to leave them in the comment section below so we can get back to you.
What is Social Security Disability Insurance (SSDI)?
SSDI is one service offered by the Social Security Administration (SSA). The SSA is a government-run agency that is responsible for assigning Social Security numbers and administering services related to their various insurance programs as well as the Supplemental Security Income (SSI) program for the aged, blind, and disabled. While most people in the country pay social security taxes, not everyone is eligible to receive benefits from it.

When you apply for social security disability, your condition will be compared to the disability “listing” found in the Social Security “Blue Book.” This book is accessible to anyone online and COPD is found under Section 3.02, under the title “Respiratory Disorders” and the subsection “Chronic Pulmonary Insufficiency.” However, when the claimant first requests disability benefits, it will be examined by local SSA field offices or state agencies who will verify non-medical requirements such as employment status, marital status, and age.
Unfortunately, there’s a lot of gray area when it comes to qualifying for SSDI. While the Blue Book clearly states what conditions you need to meet, there is some interpretation required, so it’s very important to fully understand how the process works before you file a claim. Another reason to be meticulous is that the turnaround time is generally quite long and might be even more backed up considering the COVID-19 pandemic. According to Nolo.com, 62% of people receive an answer within three months of filing an application.

What are the Requirements for COPD Patients to Qualify?
According to the SSA, a disability is defined as an inability to participate in something called “substantial gainful activity.” Essentially, what this means is that you are unable to work or make less money than the monthly income limits set by the SSA. This can either be due to a physical or mental disability that’s expected to last or has lasted 12 months or more.

The first thing you will need to gather to apply for benefits is a complete medical history of your COPD. In other words, you’ll need records of every medical event since you were diagnosed with COPD and even future medical procedures or tests if they apply. This should include things like the progression of your lung disease, symptoms, and any other physical examination that’s relevant. Below is a list of some of the test results you should include:
- Pulse oximetry
- Spirometry results
- Records of hospitalizations
- ABG tests
- Pulse Oximetry Levels
- Arterial Blood Gas
- Pulmonary (Lung) Function Tests
- Supplemental oxygen records (including your flow rate)
- CT scans or chest x-rays
Evidence of Comorbid Conditions
Like with many chronic conditions, COPD doesn’t just affect the lungs. The longer someone has COPD, the more likely they are to experience comorbid conditions such as sleep apnea, heart disease, high blood pressure, and even mental health conditions such as anxiety and depression. It’s important to include documented evidence of comorbid conditions because it will increase your chances of receiving benefits. The following are some examples of things you can include:
- Electrocardiogram (ECG) tests
- Heart stress test results
- Echocardiogram results
- History of heart attack, chest pain, or fainting
- Sleep tests
- Blood pressure tests
Evidence of COPD Treatment
Just like your medical history, it’s important to have full documentation of your COPD treatment history as well. Basically, this will show the SSA that you have been making every effort to improve the quality of your life despite the fact that COPD is an incurable disease. You will have the best chance of receiving disability benefits if you can prove that you still experience severe symptoms despite your treatment plan and you are unable to work as a result. Below are a few of the things you should include in this category:
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
- All medications that you are currently taking or have used in the past. Some common examples include inhaled steroids or bronchodilators, nebulizer treatments, antibiotics, or supplemental oxygen therapy. Be sure to include how your body reacted to these treatments.
- Pulmonary rehabilitation: including the duration and results
- Any medical procedures you’ve received such as endobronchial valve placement, lung volume reduction, or any other type of surgery.
- Include any complications related to these procedures
What Benefits Do COPD Patients Receive?
The amount of compensation that someone receives from SSDI will depend entirely on your lifetime earnings, so it’s very difficult to predict the exact amount that you will receive. According to DisabilitySecrets.com, most people receive between $800 and $1,800 each month with the 2021 average being $1,277. Another thing that will affect your earnings is whether or not you are receiving benefits from any other sources. The condition that you have and its severity will not affect how much compensation you receive.

The Social Security Administration uses a very complex formula to determine what your disability benefits will be, but it is possible to estimate your earnings by using an online social security disability payment calculator. In 2021, your disability benefits are based on the amount of income that you have paid Social Security taxes on. These are called “covered earnings.” Over the course of a year, the average covered earnings are called the average indexed monthly earnings (AIME).
.jpg)
The primary insurance amount (PIA) is calculated by applying a formula to your AIME which is the base figure that the SSA uses. If you want to learn more about how this is calculated, refer to this PDF document from the SSA. Alternatively, you can email or call your local SSA office where you will be connected with a representative who can help you predict the amount of your expected benefits.
Tips for Winning Your Disability Claim
Like we mentioned earlier, the amount that you will earn from Social Security benefits is pretty set in stone, so your focus should be on winning your case rather than earning as much as possible. Unfortunately, the burden of proving that your COPD is severe enough for benefits is largely in your hands. This is why you’ll need to be accurate and concise about the way you apply for benefits. The turnaround time for an SSDI application is several months at best, so you should be prepared to submit a thorough application the first time around rather than having to risk waiting for them to process your application a second time. Follow the tips below to get you started.
Speak With Your Pulmonologist
When it comes time to gather medical documents such as evidence of COPD treatment, procedures, or symptoms, it’s always best to get them from your pulmonologist rather than your primary care physician whenever possible. The reason for this is because the SSA may weigh this information more heavily since it’s coming from someone who specializes in COPD and other respiratory conditions.

Another reason to consult your pulmonologist ahead of time is that he/she may be able to provide you with more specific information about your disease including more thorough notes about the type of COPD you have and its expected prognosis. While pulmonologists are not specialists when it comes to disability benefits, they will help you to make the most convincing argument possible so that you can win your SSDI claim.
Hire an SSDI Attorney or Advocate
While your pulmonologist will provide you with information about your disease, SSDI attorneys and advocates are people who understand how the SSA works and how you can present the best case. While attorneys and advocates will provide you with mostly the same services, there are a number of differences between them that you should be aware of. First and foremost, an attorney is someone who is trained and has a degree in law whereas a non-attorney advocate does not have a law degree.
.jpg)
In order for someone to become an attorney, they need to have a bachelor’s degree, a Juris Doctorate (JD) degree and be admitted to a state bar. Attorneys are bound by professional conduct rules, they have many years of specialized training, and they have the ability to appeal your claim to the federal level if you want to dispute the SSA’s decision. If you decide to hire an attorney to help you with your SSDI claim, you should first ensure that they specialize in disability law.

A disability advocate (also called a legal representative, claimant representative, or disability representative) needs to pass an exam administered by the SSA, a background check, need professional liability insurance, and a bachelor’s degree. While disability advocates are highly educated on disability claims, they are not held to the same professional standards as attorneys are, and as a result, you will have less legal recourse if something doesn’t go as planned. In terms of payment, neither attorneys nor advocates are paid unless you win your case and they are entitled to the same fee which is paid directly by the SSA.
Take Your Time and be Thorough
Ultimately, the best way to win the SSDI benefits that you deserve is to be thorough with the application process. You want to provide an overview of your medical history and make it clear that you are taking the initiative to treat your COPD in the way that your pulmonologist advises. Before submitting your application, be sure to review it with a specialist who can point out any potential pitfalls. If your application is declined, the SSA will store your information in the event that you decide to dispute it.

Conclusion
Applying for benefits with COPD is not always an easy process. You need to be able to prove that your lung condition prevents you from participating in “substantial gainful activity” and you need to meet other requirements as well. Gathering the necessary medical information and knowing the right place to acquire it will give you the best chance of receiving benefits upon submitting your first application. You should also be consulting the Blue Book which outlines the exact requirements for qualifying for disability with COPD.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
COPD is one of the most common chronic conditions in the world and it represents a serious financial burden on individuals, especially in the latter stages of the disease. If you have any further questions about SSDI benefits, be sure to speak with your doctor or a disability attorney or advocate. Alternatively, you can leave your questions in the comment section below and we’ll get back to you as soon as possible.
.png)
Chronic obstructive pulmonary disease (COPD) is one of the diseases with the greatest financial burdens worldwide and within the United States. Studies have shown that the average annual COPD-related expenditure is around $4,147. And while 51% of these costs are covered by Medicare according to the Centers for Disease Control and Prevention (CDC), that still leaves roughly $2,000 a year that COPD patients need to spend out-of-pocket. Combine this with the cost of aging and limited retirement funds and it’s not hard to see why COPD is such a major financial burden for so many people.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Without a doubt, the later stages of COPD pose the greatest burden for most people. It’s during end-stage COPD that you’re most likely to experience hospitalization due to exacerbation and you’re also more likely to be hospitalized for an extended period of time. Since symptoms tend to develop more quickly during this time, you’re also more likely to schedule more doctor’s appointments, use your medication more frequently, and seek out other treatment options for your disease.
In this post, we’re going to discuss end-stage COPD (also called late-stage or stage 4 COPD). We’ll take a closer look at what exactly this term means, what to expect, and how to prepare for this stage of COPD in order to mitigate some of the physical and financial challenges it poses. If you have any questions, either leave them in the comment section below or reach out to your doctor to schedule an appointment.
What is End-Stage Chronic Obstructive Pulmonary Disease?
Since COPD is a long-term condition that progresses slowly, it’s generally divided into four different stages. These stages help healthcare specialists identify the symptoms of your disease, predict the prognosis of your disease, as well as your life expectancy. And because COPD manifests differently in every patient, that also means the stages are going to look different for everyone. While researchers have a good idea of the average life expectancy of someone with COPD, what ultimately matters is your own health. In this way, it’s often better to think of COPD as a sort of “catalyst” for other health issues.

The best way to know that you’re approaching late-stage COPD is based on your symptoms. Someone with end-stage COPD will likely experience similar symptoms that they’ve experienced for many years such as coughing, breathlessness, fatigue, or chronic pain. In end-stage, however, these symptoms become significantly more debilitating to the point where they may need to rely on caretakers, friends, or loved ones to take care of them. They’ll also experience more frequent trips to the hospital due to flare-ups and exacerbations.
-jpg.jpeg)
The term “end-stage” is controversial in many ways because it can imply that the patient doesn’t have much time left to live, but this isn’t always the case. Even when it’s evident that symptoms are increasing in frequency and severity, that doesn’t mean that won’t outlive them and go on to live many more years. However, using this term can be helpful when it comes to planning and the approach that you use to treat your disease. For example, some people prefer to switch to palliative care which is a type of specialized medical care that’s focused on optimizing a patient’s quality of life and ease discomfort.
How to Recognize End-Stage COPD
As aforementioned, late-stage COPD looks different for everyone. This is why it’s important to maintain open lines of communication with your doctor who can provide you with detailed information about your disease prognosis as well as advice on how to plan. Generally speaking, however, you’ll be able to notice an increase in the frequency and severity of symptoms you’re experiencing. Take a look at some of the symptoms below and see if you notice any similarities to what you’re experiencing.
- You experience heavy coughing or wheezing throughout the day
- You experience shortness of breath even while at rest
- You lack the energy or will to maintain your diet
- You’re becoming more reliant on friends and family for simple tasks
- You experience dizziness, confusion, or trouble sleeping
- You experience more frequent or severe exacerbations that lead to hospitalization
Another way to recognize end-stage COPD is by performing a spirometry test. A spirometer is a simple device used to derive two different results: Forced Expiratory Volume in one second (FEV1) and Forced Vital Capacity (FVC). Combined, these results will tell you how well your lungs are functioning, and if you have spirometry results already, you and your doctor will be able to compare them to determine how quickly your lungs are deteriorating. FEV1 refers to the total amount of air you can force from your lungs in one second and FVC refers to the total amount of air you can expel from the lungs in one breath.

From a diagnostic perspective, stage four COPD is recognized as an FEV1/FVC ratio of less than 70% or an FEV1 less than 30%. Even if your FEV1 is above 30%, however, your doctor may classify you as stage four severe COPD if you have chronic respiratory failure. Several other tests your doctor may use to diagnose stage four COPD include lung volume tests, gas diffusion tests which measure how well oxygen moves from the lungs to the bloodstream, and exercise tests.
How to Ease End-Stage COPD Symptoms
All-in-all, your treatment plan for end-stage COPD shouldn’t look all that different from your treatment plan for any other stage of COPD, but you may need to make adjustments based on your physical, mental, and emotional abilities. What’s more, there are several additional strategies you can add to your routine that can ease some of the pain and increase your comfort.
Supplemental Oxygen Therapy
Oxygen therapy is likely the most consistent treatment you’ve used since being diagnosed with COPD. Since COPD leads to progressive lung obstruction, one of the best ways to remedy this is by helping your lungs out and providing them with a higher concentration of oxygen. By doing so, your body will have the resources it needs in order to stay healthy. Unfortunately, many COPD patients use oxygen incorrectly or they use an oxygen device that doesn’t suit their needs and lifestyle.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
When it comes to oxygen delivery devices, there are several options available to you. Oxygen tanks have been around the longest, followed by liquid oxygen tanks, home oxygen concentrators, and portable oxygen concentrators. While each of these can provide you with the oxygen you need, portable oxygen concentrators tend to offer the most comfort and convenience in end-stage COPD. There are many reasons for this, but above all, they don’t need to be refilled.
.png)
Rather than containing compressed oxygen like oxygen tanks do, portable oxygen concentrators run off of powerful lithium-ion batteries which allows you more freedom to move around on your own time. Instead of having to call an oxygen company to deliver full tanks to you, simply plug your POC into any wall outlet and you’ll be able to recharge your batteries. You’ll even be able to use the device while it’s charging.

There are several different types of POCs you can choose from depending on your wants and needs. Pulse dose portable oxygen concentrators like the Caire FreeStyle Comfort or Inogen One G5 closely monitor your breathing and only deliver oxygen when you inhale. These devices are incredibly efficient, lightweight, and small. On the other hand, you could opt for a continuous flow portable oxygen concentrator like the Respironics SimplyGo which provides the user with a constant stream of oxygen. These machines tend to be slightly bigger and bulkier than their counterparts.
Nutritional Counseling
Like we mentioned before, malnutrition is a significant problem that many stage-four COPD patients face. Symptoms like breathlessness and chronic fatigue can lead to a situation where patients simply don’t have the energy to eat or they don’t get the same satisfaction from it that they used to. Conversely, it could lead to someone choosing foods that are convenient and provide a quick energy boost. Unfortunately, these foods tend to also be filled with sugar and other problematic ingredients that don’t provide your body with the nutrients it needs.
If either of these situations sounds like you, it might be a good idea to consider nutritional counseling. This is a type of therapy that’s focused solely on your eating habits and it attempts to break down any barriers you might be facing that are preventing you from sticking with the diet that your doctor has provided for you. Contrary to popular belief, nutritional counseling isn’t just for people facing weight issues, it’s also extremely beneficial for people with chronic illnesses like COPD who struggle to get the nutrients they need. It’s also useful for anyone who believes that they have “unhealthy” or “unproductive” eating habits.
Complementary Therapies
Complementary therapies are any therapy that can help you ease the burdens associated with late-stage COPD. As you can imagine, this varies greatly depending on the patient because everyone faces different issues with their disease. For some, this might mean attending cognitive behavioral therapy (CBT) sessions in order to prevent anxiety or depression, for others it could mean speaking with a spiritual or religious leader who can help you settle any concerns or fears about living out the later stages of your life.

Cognitive behavioral therapy is a type of psycho-social intervention that’s focused on correcting negative or inaccurate thought processes or actions. It’s a type of therapy that’s become very popular among older adults, especially those with chronic conditions, who want to seek more fulfillment in their daily lives. CBT takes place over the course of several weeks, months, or however long it takes for the patient to feel comfortable on their own.
Another type of therapy you might want to consider when it comes time to plan for end-stage COPD is massage therapy. Studies have shown that anxiety can cause a lot of tension to form in our bodies and this tension can lead to more anxiety. Massage therapy is a great way to break this tension causing us to feel better both physically and mentally. According to this medical report, there are two reasons massage therapy is beneficial for COPD patients. Firstly, it causes hyperemia which is the increase of blood flow to different tissues. Secondly, it activates the lymphatic system which is responsible for draining your body of toxins.
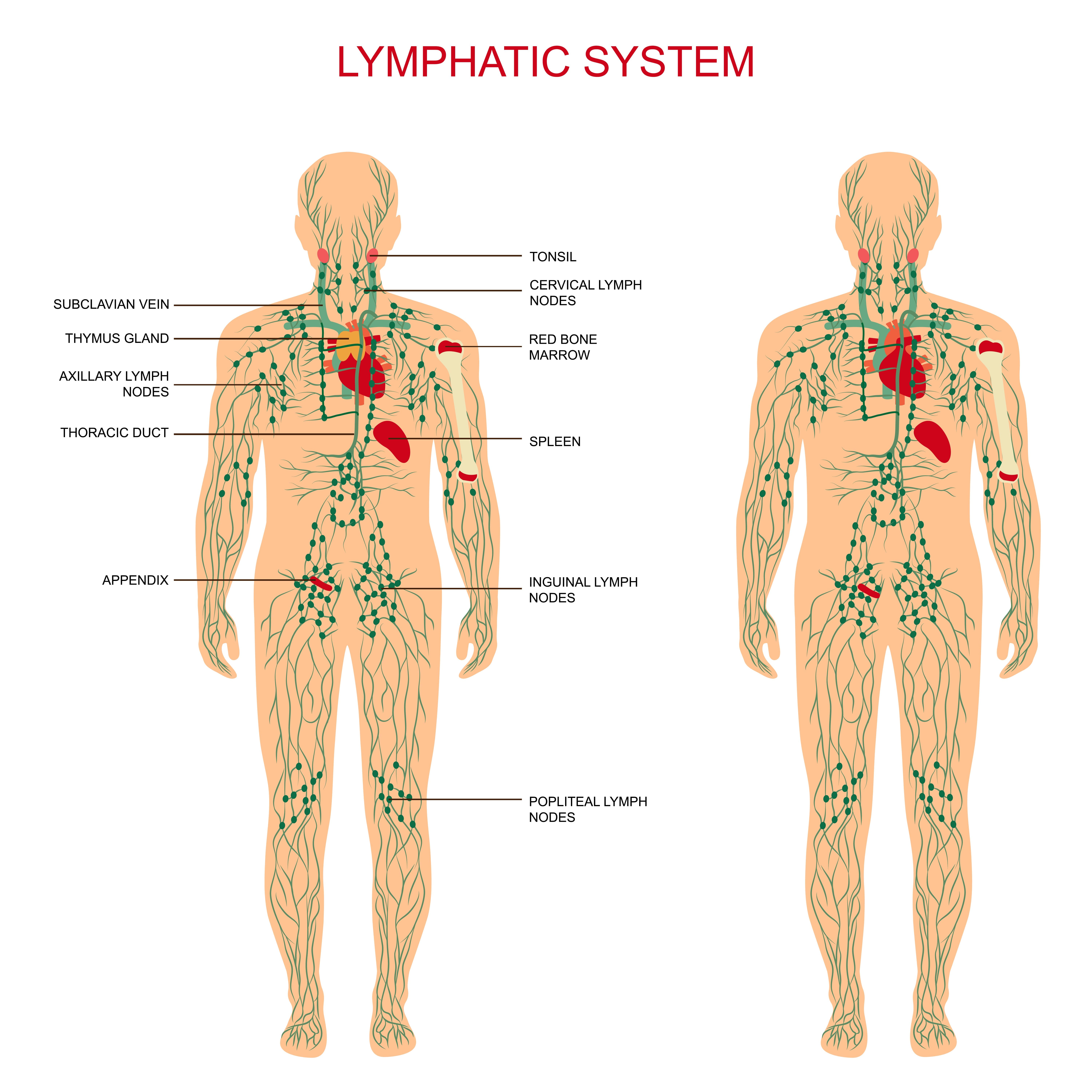
A Revised Pulmonary Rehabilitation Routine
Most people are well-aware that with aging comes problems with mobility, endurance, and strength. It’s a natural part of life that we lose a lot of our physical abilities as we get older, but that doesn’t mean you can’t continue to do pulmonary rehabilitation. It simply means that you will need to find new ways to do it. Some people find that the best option for them is to switch to exercises that involve sitting as well as ones that don’t require them to leave the house or meet up with other people.

The important thing to remember is that any form of exercise will benefit your lung health, not just exercises that work your lungs specifically. In many cases, this mindset can even be counterproductive in late-stage COPD because most people don’t have the lung capacity to perform any strenuous endurance exercise that gets your heart rate up. Rather, targeting specific muscle groups in your body will improve your strength and circulation, thus easing some of the burden on your lungs. Studies have shown that muscle requires less oxygen to use and it produces less carbon dioxide as waste, ultimately resulting in less air that your lungs need to take in.

The thing that we would like to stress, like we’ve done many times before, is the importance of consistency when it comes to your pulmonary rehabilitation. Just like maintaining a healthy diet, your exercise routine will be more effective if you are able to do it everyday without letting yourself fall back on your goals. Ideally, you should have someone like a friend or family member who can hold you accountable at least until you are able to do so for yourself.
Address Your Concerns With Your Doctor
Just like with any other stage of COPD, you’re going to want to work closely with your doctor in end-stage COPD. This is because you’ll want to make sure that your goals are in line with or at least not counterproductive towards your treatment goals. Like we mentioned earlier, end-stage COPD should be all about improving your comfort and reducing chronic pain. But this doesn’t mean that you should completely ignore the treatment plan that you’ve followed throughout your whole life with COPD.

Another reason to consult your doctor is because he/she will likely have some helpful resources for you in regards to finding other health specialists such as nutritionists or mental health experts. This will not only save you a lot of time but it will set you off on the right path. You should also make it a priority to visit your doctor more frequently so that you can make healthy choices that fall in line with your COPD treatment plan.
Conclusion
Chronic obstructive pulmonary disease (COPD) is an ailment that develops and progresses over the course of many years — sometimes even decades. This is why it’s important to always be adaptive when it comes to your treatment plan and lifestyle. While during stage one COPD, you were likely very active and took the time to travel as much as possible, stage four COPD treatment should focus more on improving your comfort and ensuring your psychological, physical, and even spiritual needs are met.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
While you should take the initiative to do these things for yourself, it’s also important to consult your doctor to make sure you don’t leave out any aspect of your treatment plan in the process. Even in end-stage COPD, you’ll need to keep up with your oxygen therapy, dietary plan, pulmonary rehabilitation, and avoid environmental triggers such as pollution or airborne allergens.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













