LPT Medical is luckily enough to occupy a small office located halfway between West Palm Beach and Fort Lauderdale, in Boca Raton, Florida. This area provides a surprising amount of nature trails and walkways to explore, and not to mention stretches of glorious beaches. If you are a Boca Raton resident or a nearby city on Florida’s southeastern coast we wrote this blog for folks who are looking to get outdoors and go for walks more often.
LPT Medical is an oxygen supply company in Boca Raton, Florida. We are interested in providing oxygen patients with valuable information they can use to better manage their respiratory disease and take advantage of oxygen therapy benefits. This article is all about treating respiratory illness through exercise and specifically walking. Walking is the single most important and accessible form of exercise oxygen patients can add to their daily routine to improve their lung strength and health overall.
Daily walks are a great goal to set for yourself if you struggle with a respiratory disease, the challenging part is getting started and knowing where to go! The other challenging aspect of walking, is having the right oxygen equipment that can hep make exercise and walking more accessible.
Therefore, we would first like to discuss how oxygen patients can walk with more ease and comfort.

Exercising With Supplemental Oxygen Therapy
Exercise is a critical part of treating any respiratory disease, no matter how severe or minor. Oxygen patients are normally at the point in their disease where their blood oxygen levels are consistently low enough that supplemental oxygen is prescribed to them in order to boost their oxygen levels to a healthier rate.
This all might sound counterintuitive because exercise can make you short of breath, and this is something that we try to avoid as oxygen patients. However, exercise strengthens your muscles and lungs, thereby expanding your lung’s capacity to work better in conjunction with your supplemental oxygen.

Having the right oxygen equipment can make walking and exercise in general more attainable, and even enjoyable.
Many oxygen users explain how bulky and cumbersome liquid and gas oxygen tanks are. Lugging around an oxygen tank while you do simple tasks like getting the mail or cleaning up your home becomes nearly impossible, and nothing sounds worse than exercise.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
So while portable oxygen concentrators and liquid and gas tanks all have the same main function; to give your body the oxygen it needs to maintain a healthier blood oxygen level, oxygen methods will have very different effects on your daily life. For instance, having a portable oxygen concentrator will not only fuel your body with the oxygen it is lacking, but it will also give you the mobility and freedom to exercise, run errands, and so much more.

This is because pulse flow devices are normally very lightweight, for example, the Caire Freestyle Comfort portable oxygen concentrator only weighs 5 pounds. Portable oxygen concentrators also never run out of oxygen as a tank would, because they run off of battery power, and they simply need to be recharged. Devices like the Inogen One G3 can last for up to 8 hours before it needs to be plugged in. Having a device that will not run out of oxygen gives you the freedom to exercise and go for walks worry free.
Some concentrators like the Respironics SimplyGo can operate within pulse flow and continuous flow settings, no matter what your oxygen prescription is, there is likely a device that can take care of your needs while you rest and while you exercise.

As you can see, there are numerous reasons why your oxygen equipment can either help you or hold you back, especially when it comes down to something like exercise. If you are interested in learning more about the benefits of owning a portable oxygen concentrator please read our other blog by clicking here.
If you would like to speak with a respiratory specialist about portable oxygen concentrator costs, and more information, call 1(800)-946-1201 or email info@lptmedical.com
If you are an oxygen patient or simply enjoy going for walks in the Boca Raton area, continue reading to learn about some of the best places to walk around your neighborhood.
Gumbo Limbo Nature Center

One of the best places to walk in Boca Raton is in the large oceanfront Red Reef Park, home to the Gumbo Limbo Nature Center with trails, a butterfly garden, and a sea turtle sanctuary.
The Gumbo Limbo Nature Center is a beautiful half mile-round trip walk through the Coastal Hammock Forest. Walking a half mile may be too much for some oxygen patients, but remember, you can slowly work your way up to walking these longer distances.
The COVID-19 pandemic has limited capacity and closed down the north trails within the Gumbo Limbo Nature center, and parking lots remain closed in response to the Coronavirus pandemic until further notice. But there are still plenty of options to walk around and enjoy the beautiful terrain and explore very nice natural environments within the park. You can check out gumbolimbo.org and myboca.us for more information regarding closures and COVID-19 policies and protocols.
Downtown, Boca Raton

A simple walk downtown in Boca Raton can be lovely. You can opt to enjoy time inside while walking through the Boca Raton Museum of Art, a modern and contemporary American and European collection. Walking indoors is a great way to get in your exercise for the day if there is rain, wind, or other unfavorable weather.
You can also walk down streets in your local neighborhood, but if you easily tire of the same scenery, a trip downtown can be an easy way to change it up! Walking along a sidewalk in downtown is a great option for oxygen patients because it is flat, paved, and there are not many hills.
Arthur R. Marshall Loxahatchee National Wildlife Refuge

At the edge of Boynton Beach lies Arthur R. Marshall Loxahatchee National Wildlife Refuge a 145,000 acre buffer between suburbia and the Everglades. This is a beautiful area to get outside and enjoy the natural Southeastern Florida landscapes and wildlife.
Here, you can walk, attend events, fish, look at the wildlife, and even go boating. Pets are welcome, so if you have an animal that you like to take on walks, this is a special spot you can take a trip to enjoy the new scenery.
Daggerwing Nature Center

Behind Daggerwing Nature Center in the busy South County Regional Park, lies an accessible boardwalk trail which leads you into a small area of tropical habitat with ancient trees. This is a great way to experience a walk through a very old jungle.
If you are interested in ecology, the boardwalk brings you into a wetlands area where you will enter a dark hammock thick with a multitude of different tropical tree species. After passing a spur, the trail leads to an observation tower that overlooks the beautiful canopy. If you make it up the tower, you can stand high above the forest floor for a great up-close view of the canopy.
Sugar Sand Park

In Boca Raton, the urbanized trails at Sugar Sand Park are great for all ages and oxygen patients. From the nature center to the playground the area is surrounded by coastal shrubbery and pine flatwoods, but the paths are paved and great for wheeling you oxygen equipment around behind you.
If you want to get on one of the nature trails, there is the Sand Pine nature trail and The Slash Pine nature trail. Neither of these trails are paved, but the trails are flat and wide enough to bring oxygen equipment with you!
Doris Davis Foreman Wilderness

The Doris Davis Foreman Wilderness Preserve is a half mile loop through a lovely patch of tropical bustle in the center of suburban Parkland in Broward County.
This designated area of forest offers public access to all of the site's amenities, the area is designed to be accessible for all to marvel in its beauty! There is a 5 ft. wide by 900 ft. long pedestrian trail traveling through pine woods and a 1,550 ft. boardwalk that winds gently through cypress wetlands and past a breathtaking oak hammock. There are two seating and observation areas along the path with a pavilion area located along the trail for a nice spot to take a break.
Overview

If these nature trails do not get you excited to go out and walk, you might try walking on the beach. If you are able to carry your portable oxygen concentrator over your shoulder in its custom carrying case or via your portable oxygen concentrator backpack in order to avoid getting sand in the device, a nice walk along the boardwalk or even in the sand is a great way to get the exercise your body needs.
If you don't live anywhere near Boca Raton, you can try to Google search some areas within your city with nature paths or pedestrian walkways. If there are not a lot of trails where you live, If you like to golf, you can try to walk some of the green rather than using a golf cart the entire time.
Simply walking is so great for oxygen patients, because even with the supplemental oxygen therapy, your body still needs exercise in order to maintain and improve its strength. Oxygen therapy simply gives you the energy you need to exercise comfortably, and having the best oxygen equipment is giving you the tools to be able to exercise without getting weighed down.
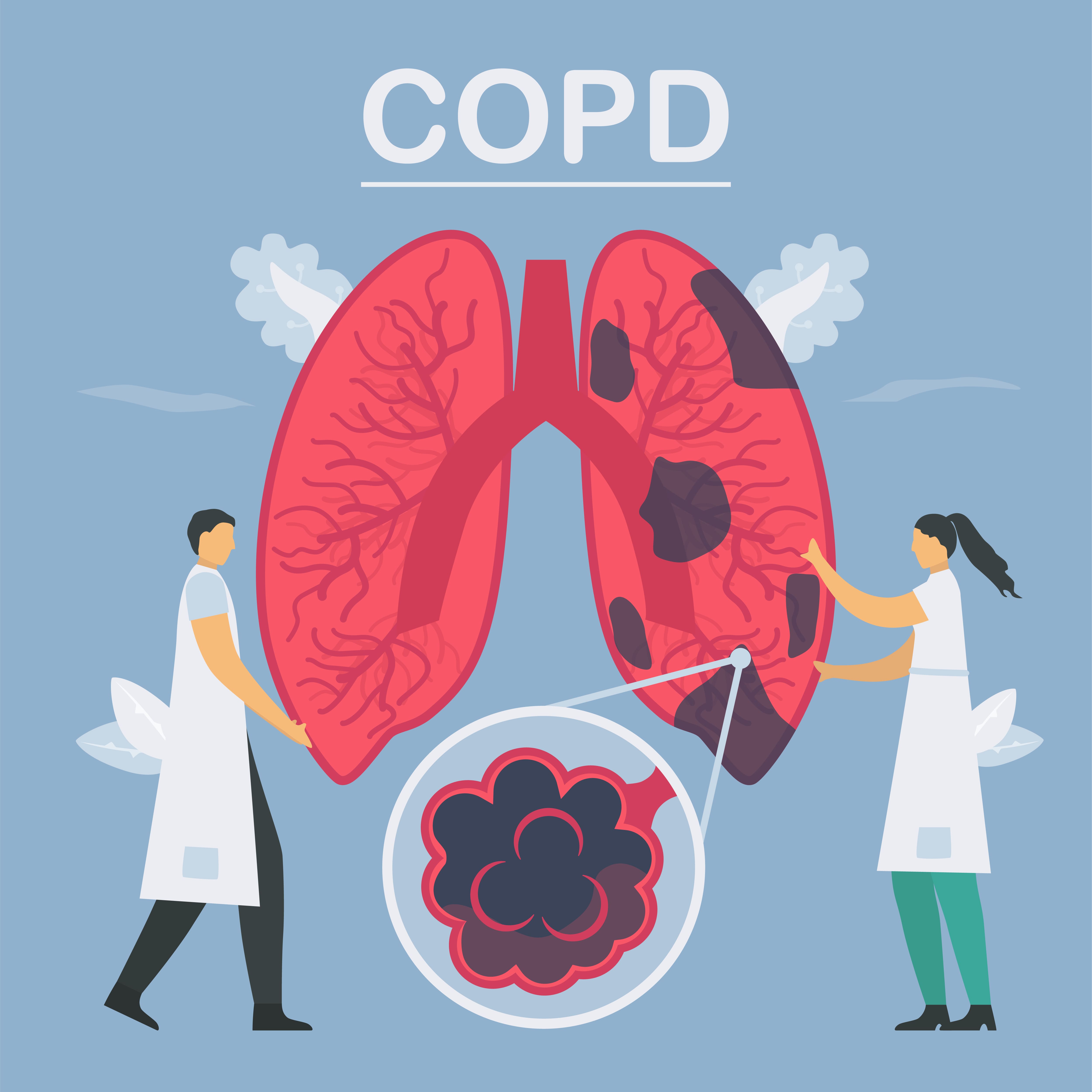
Chronic obstructive pulmonary disease (COPD) is one of the leading respiratory diseases in the world in terms of morbidity and mortality. Around 65 million people have it, and many experts are expecting that number to grow over the next 50 years. One thing that’s unique about COPD is the fact that it develops very slowly over the course of many years. Because of this, many COPD patients are susceptible to complications that are as bad, or even worse than their underlying condition.
One of the most notable examples of this which often occurs in the later stages of COPD is heart disease. Since the heart and lungs work together to distribute oxygen throughout the body, impaired lung function can result in added strain on the heart. Over time this can cause serious complications like right-sided heart failure, heart attacks, and coronary artery disease.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Fortunately, studies have shown that — by proactively managing your respiratory symptoms — you’ll significantly reduce your risk of experiencing complications from COPD. Treatments like oxygen therapy will reduce the workload on your heart and lungs and ensure that every organ in your body has the oxygen it needs to function properly. However, it’s still important to understand the complications of COPD so that you know what symptoms to look out for.
In the following sections, we’ll take a look at one of the lesser discussed COPD complications called pneumothorax, also known as a collapsed lung. If you have any questions about the content of this article, please address them in the comment section below. However, if you have questions about your COPD or treatment plan be sure to consult with your doctor. COPD is a complex disease, so something that works for one person may not work for another.
What is Pneumothorax?
“Pneumothorax” is the medical term used to describe a collapsed lung. This occurs when air enters the “pleural space” which is the area around your lungs. This disrupts the balance of pressure between the inside and outside of your lungs and can result in a collapse of the lung. Pneumothorax ranges in severity from mild to life-threatening. Mild pneumothorax often needs no medical attention and will heal over time.
What Types of Pneumothorax Are There?
There are two basic types of pneumothorax: traumatic and nontraumatic. Traumatic pneumothorax is caused by physical injuries such as a fall, car accident, or any other type of injury that damages the chest or lung wall. Nontraumatic pneumothorax is also called spontaneous pneumothorax because it occurs without injury. There are many different factors that can contribute to or cause the onset of non-traumatic pneumothorax and it tends to be more difficult to understand than its counterpart.

There seem to be two separate instances where non-traumatic pneumothorax occurs and as a result, researchers have created two different classifications: primary and secondary spontaneous pneumothorax. Primary spontaneous pneumothorax (PSP) is more common in younger adults with no lung disease and secondary spontaneous pneumothorax (SSP) is more common in older adults with lung conditions.
One final classification that should be mentioned is spontaneous hemopneumothorax (SHP). This is an extremely rare but serious condition where both air and blood fill the pleural cavity, usually in patients who have no known history of chronic lung disease.
.jpg)
What Are the Symptoms of Pneumothorax?
Symptoms of pneumothorax vary based on what is causing the condition. Since pneumothorax can develop very slowly this may cause someone to underestimate the risk. However, in certain situations, it can develop very quickly causing someone to immediately seek medical attention. In mild cases, you may not experience any symptoms at all or at least not enough to cause you any concern. Below are some possible symptoms of pneumothorax:

- Dyspnea - shortness of breath
- Tachycardia - a fast heart rate
- Chest pain
- Cyanosis - a bluish discoloration of the skin
- Tightness in the chest
Causes and Risk Factors of Pneumothorax
Causes:
Mechanical ventilation - Mechanical ventilation is a medical procedure that’s used to assist someone with breathing if they are undergoing surgery or they have a medical condition that is preventing their lungs from working. While ventilation is mostly a safe procedure, if it is administered incorrectly and there is an imbalance of pressure within the chest, it can cause the lungs to completely collapse.
.jpg)
Ruptured air blisters - Small blisters called blebs can form on the top of the lungs in people with damaged lung tissue. Over time, these blisters can burst, allowing air into the pleural space. This can put a lot of pressure on the lungs and cause them to collapse.
Chest injury - Chest injury is a very common cause of pneumothorax. Blunt or penetrating injuries can occur during car accidents, sports injuries, or falls. Chest injury can also occur during lung surgery or it can be caused by collateral damage from other types of surgery.
Risk Factors:
Age - Pneumothorax is more likely to occur in young people between the ages of 20 and 40 or older adults with chronic lung conditions.
Gender - Tall underweight men are more likely to contract pneumothorax.
Smoking - Risk of pneumothorax increases with time and the number of cigarettes smoked.

Lung disease - Having a chronic lung condition like COPD, asthma, or cystic fibrosis puts you at a higher risk of pneumothorax.
Genetics - Studies have shown that mutations in the FLCN gene can cause pneumothorax.
Medical history - People who have experienced pneumothorax in the past are more likely to experience it again.
Why is COPD a Risk Factor for Pneumothorax?
The term chronic obstructive pulmonary disease (COPD) is an umbrella term used to describe two different diseases: chronic bronchitis and emphysema. Chronic bronchitis is characterized by inflammation in the bronchioles (bronchial tubes) which are the airways that lead to the lungs. Emphysema causes the alveoli (tiny air sacs in the lungs) to fill with fluid and impair the transfer of oxygen and carbon dioxide to and from the bloodstream.
One of the main reasons that COPD contributes to pneumothorax is because of the inflammation and damage that occurs to the lungs. While on the surface it may seem like COPD is a simple condition, it’s actually very complex and it affects the respiratory system in more ways than one. One thing that emphysema causes in particular are a change in the structure of the lungs. As the alveoli in the lungs start to break down, they lose their elasticity making it much more likely for air pockets to form in the pleural space.
Bullous emphysema results when fluid-filled sacs begin to form in the lungs. Bullae usually form in the upper lobes of the lungs and lung function can be significantly impaired if they become inflamed or rupture. This also weakens the overall structure of the lungs putting you at a higher risk of experiencing pneumothorax and other related issues.
In some cases, emphysema patients are a candidate for lung volume reduction surgery. While it may sound counterintuitive to reduce the size of the lungs of someone who can’t breathe well, this surgery is designed to remove only the diseased tissue. In other words, the surgeon will remove tissue that has lost its elasticity or isn’t able to transfer oxygen to the blood. This prevents the lungs from trapping air and allows you to breathe much easier.
Unfortunately, lung surgery can also be the cause of pneumothorax, especially if it involves a highly invasive procedure like lung volume reduction surgery. Before you decide that surgery is the best procedure for treating your emphysema, be sure to speak with your doctor about the risk of pneumothorax and ask any questions if you have them.
What Do COPD Patients Need to Do to Prevent Pneumothorax?
Schedule Regular Checkups
Probably the best thing you can do to prevent pneumothorax as a COPD patient is to see your doctor regularly. As aforementioned, pneumothorax isn’t always a condition that progresses quickly. In some cases, it can progress slowly and heal on its own. But to give yourself the best chance possible to recover quickly and effectively, you need to be aware of what’s causing it. Visiting your doctor regularly will give you a chance to discuss your symptoms and learn about your condition.

Follow Your Treatment Regime
There’s no doubt about it, you have a lot to worry about as a COPD patient. COPD treatment regimes usually involve a lot of different lifestyle changes like oxygen therapy, pulmonary rehabilitation, a revised diet, and an improved sleep schedule. While it’s not easy following all of these things to a tee, it’s worth it if you want to minimize your risk for common COPD complications like pneumothorax.

Quit Smoking Immediately
Smoking is the primary cause of COPD and it’s also one of the biggest risk factors for pneumothorax. So, it goes without saying that immediate smoking cessation will be hugely beneficial if you’re concerned about this complication. Smoking has been proven to increase the likelihood that a bleb will rupture which leads to air building up in the pleural space which collapses the lung.

Have an Action Plan
Another thing you can do is to simply have a plan in place in the event that you experience serious symptoms. Considering the fact that COPD exacerbations are a common occurrence you should already have an emergency plan in place. One thing you should do right away is to install a medical alert system in your home. The medical alert system comes with a small pendant that you wear around your neck. If you experience a medical emergency, simply press the button and an ambulance will be sent to your home.

How is Pneumothorax Treated?
Observation
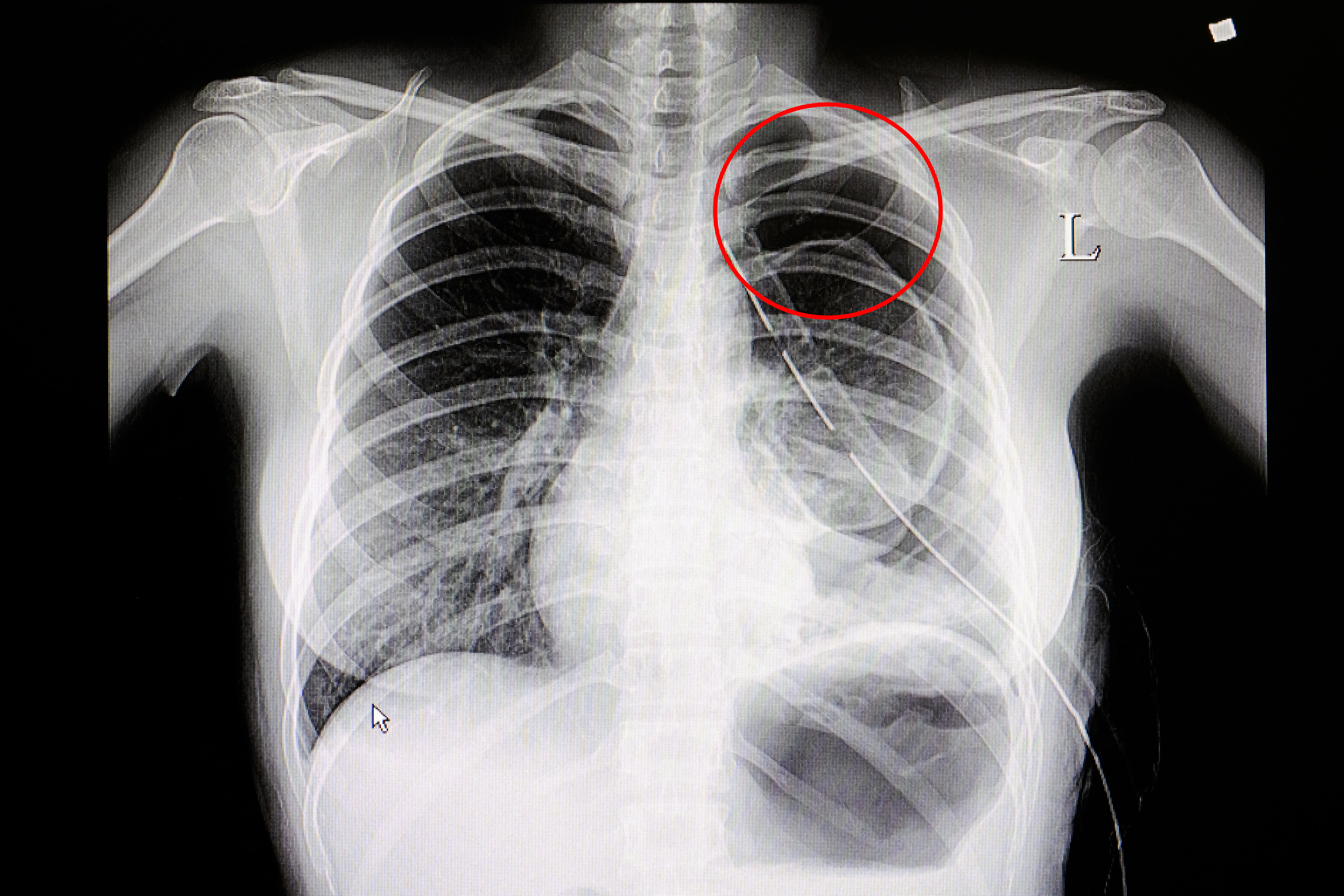
The first thing your doctor will likely do if he/she suspects you have pneumothorax is to test for and observe your lungs. Chest X-rays and computerized tomography (CT) are the two most common tests used to detect but ultrasound imaging can also be used to get a better look at the lungs. If these tests reveal that you have a pneumothorax, your doctor may continue to observe it over the course of several weeks or months if it’s not urgent.

Needle Aspiration
This is one common treatment option for pneumothorax where a special needle is inserted into the pleural area. This needle extracts air so that the lungs can begin to re-expand and you can breathe normally again. Typically the needle is left in for several hours to ensure that all of the excess air is removed. A similar procedure is done by inserting a tube into the pleural space instead of a needle.
Nonsurgical Repair
If the above methods don’t work, there are several non-surgical options that your doctor might try. Bronchoscopy is a procedure that’s commonly used to examine the lungs and diagnose lung conditions, but in pneumothorax patients, it can be used to place a one-way valve in the affected area of the lungs. This will allow air into the lungs but prevent it from going back into the pleural area, thus re-expanding the lungs.
Surgery
If all other treatment options are exhausted, a medical specialist may resort to surgery in order to repair your pneumothorax. The specific type of surgery used to treat pneumothorax is called video-assisted thoracic surgery (VATS) or thoracoscopy. There are two other surgeries that can be done at the same time to prevent the resurgence of pneumothorax. These procedures are pleurodesis and bleb resection.
.jpg)
Pleural abrasion is one of the most common types of pleurodesis and it involves applying a special chemical designed to seal up the area of the lung that is leaking. Another way this can be done is by extracting blood from another area of the body and using this as a type of sealant to repair the leak. This is referred to as an autologous blood patch.
Conclusion
Pneumothorax, or a collapsed lung, is a scary thought regardless of whether you are a COPD patient or someone who’s otherwise healthy. In some cases, pneumothorax can be harmless and will heal itself over time. But in other cases, it can be life-threatening and require immediate emergency medical attention. Unfortunately, pneumothorax shares many symptoms in common with COPD exacerbations so it’s best to see your doctor any time that you experience a flare-up in your symptoms.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Here at LPT Medical, we are serious about providing COPD patients with reliable portable oxygen devices. While oxygen therapy will not prevent pneumothorax, it will ensure that you are able to use supplemental oxygen therapy wherever you go and reduce your risk of experiencing severe side-effects of COPD. Portable oxygen concentrators like the Caire FreeStyle Comfort and Inogen One G5 are our most popular units, but we offer many other options as well including pulse dose portable oxygen concentrators, continuous flow portable oxygen concentrators, and stationary oxygen concentrators.

It is almost time to ring in the New Year, and that means new goals, healthier living, and hopefully the beginning to a successful year. Oxygen patients should be especially diligent to celebrate the new year with new ambition and resolutions towards a healthier future! If you are an oxygen patient either due to a chronic lung condition or other pulmonary disease, there are a few New Year’s Resolutions you might add to your list if you haven’t already.
Here at LPT Medical we aim to improve the quality of life for oxygen patients by ensuring that more people around the country have access to the most state-of-the-art oxygen therapy equipment in the world, and this year we expect to continue doing so!
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Therefore, we designed these11 New Years Resolutions for our readers around the world, who are mostly oxygen patients or folks with a chronic lung disease. While 11 resolutions is too many for one person, we hope that you can gather one or two of these ideas and implement them into your daily life to help improve the quality of your breathing and subsequently the quality of your life
Take Longer Trips Away From Home
2020 was a strange year, and for oxygen patients who already find themselves inside for most of the day, they had little opportunity to venture away from home. This year, make it a point to go outside more often, even if it's just to sit and enjoy the fresh air.

If you are more adventurous, you can make it a point to stay outdoors longer. If your oxygen equipment restricts you from adventuring outdoors for too long, it might be a good year to take advantage of your youthfulness and upgrade to an oxygen device like a portable oxygen concentrator that will allow you to be away from home for long periods of time.
Dial in your Oxygen Equipment
You are probably very familiar with your supplemental oxygen therapy equipment, but are you getting the most out of the life saving therapy as you could be?
There are limitations to what you can experience with an oxygen tank and portable oxygen canisters. For example, you cannot travel in an airplane with your oxygen, you have to bring extra heavy tanks with you when you do travel, or you have to limit your time away from home to get your oxygen delivery. On top of all of that, tanks are heavy and bulky and the canisters don’t last very long.
.jpg)
If you already have a portable oxygen concentrator (POC), do you have all of the accessories to take advantage of your battery powered device?
If you have a pulse flow POC, make sure your battery lasts long enough for you to get all of the things you want to do. If your battery tends to die earlier than you would like, you can buy an extra battery to replace the dead one, or purchase a large portable oxygen concentrator battery that can last twice as long as the smaller battery your device came with.

It is also important that you have both charging cables, the AC charging cord and the DC charging cord so you can charge your device in the comforts of your home, or on the go in your car, boat, or RV.
You can find all of you oxygen equipment accessories for a plethora of different brands and devices on our website. Or simply call one of LPT’s respiratory specialists located in Denver, Colorado at 1-800-946-1201 or reach our oxygen supply office in Boca Raton, Florida by emailing info@lptmedical.com.
Find Independence

A sense of independence is something a lot of respiratory patients struggle with. There is a lot of dependency on caregivers and loved ones especially when the disease starts to progresses into a severe state. The oxygen patient is often left doing minimal chores and housework simply due to their condition, and inability to lift heavier objects or clean with harsh cleaning products.
That being said, finding a sense of independence does not mean you have to put yourself in danger! As an oxygen patient you should not be exposing yourself to harsh chemicals of any kind, nor should you lift heavy objects that make you uncomfortable.
Instead, you can find independence in running more of your own errands or taking yourself to the doctors office for a casual checkup. You can start to cook more on your own by looking up easy recipes for oxygen patients! These are just a few ideas, but the possibilities are endless.
A small found sense of independence can do a lot for a person's wellbeing. It can bring you motivation to get healthier and you can start to do more and more activities on your own.
Enjoy Virtual Time With Family
Just because it is a New Year, doesn’t mean the pandemic is over! Even with the promising new vaccine, COVID-19 is still a valid concern especially for oxygen patients who cannot afford to catch the common cold let alone the Coronavirus causing COVID-19.
More time spent online connecting with family members is still a part of the future, so learning as much as you can about Facetime, Zoom, Google Hangouts can bring a lot of happiness and social connection into your life!
Plan a Trip For When You Can Travel Again

Nothing lasts forever, not even a global pandemic! So, there is no harm in wishful thinking.
When travel bans are lifted and it is safe to travel again, you will want to take advantage of your time, so having a flexible plan in place to experience a new place or visit family can help you stay positive for the days to come.
As an oxygen patient, you still have the opportunity to experience new things, with the help of a lightweight oxygen device, you won’t feel weighed down.
If you have a high oxygen prescription, and require a continuous flow of oxygen, portable, devices like the Respironics SimplyGo and the SeQual Eclipse 5 Portable Oxygen Concentrator are not bulky because they are designed for the oxygen patient that enjoys moving around, traveling and doing activities.

Walk More and Walk Further
Walking is one of the very best exercises you can do if you suffer from a chronic lung disease. Walking is safe and effective because it is a low impact activity so it is not hard on your joints.
Walking is great for oxygen patients for a number of reasons
- Improve your body's ability to use oxygen
- Builds up your endurance
- Strengthen your muscles and lungs
- Enhances your mood

Some oxygen patines feel hesitant to walk, either due to their lung condition or the oxygen equipment gets in the way.
If you are someone that wants to add walking into your weekly routine to enhance your physical and mental fitness, start by walking a small distance at a slow pace.
Over the year, you will start to notice that you can progress to further distances and even begin a brisk walking pace.
Eat Healthier Foods That Help Your Lung Condition

It may be surprising to some, but food has a large impact on your breathing. If you are eating food that helps with respiratory symptoms, you might notice some of your symptoms are less harsh. On the other hand, if you are eating food that promote bloating, your respiratory symptoms will get worse.
When you are bloated your diagram is putting added pressure on your lungs making it harder to breathe and your lungs have to work even harder than they already are.
We have a few blogs already about how you can eat healthier foods that will help easy respiratory symptoms:
Best Eating Habits for People with Respiratory Diseases
Elevate Your Nutrition with These 21 Healthy Meal Ideas and Diet Tips for People with COPD
Eat More Foods Rich in Antioxidants

One of the most important foods groups you can eat as an oxygen patient are foods rich in antioxidants. Antioxidants are known to help your lungs perform best, and foods rich with antioxidants are important for maintaining optimal health.
Here are some ideas of foods to eat that are high in antioxidants:
- Blueberries
- Cranberries
- Blackberries
- Prunes
- Strawberries
- Apples & pears (with peel)
- Grapes
- Peaches
- Bell peppers
- Asparagus
- Red cabbage
- Tomatoes
- Potatoes
- Broccoli
- Artichokes
- Kale
Talk to your Doctor More Often

As an oxygen patient, it is so important for your health to maintain a healthy weight, keep your blood pressure low, reduce stress and anxiety, and relieve depression. Talking with your doctor and attending your check-ups is the best way to keep these aspects of your life in check.
You should also regularly see your doctor to check on your oxygen prescription to make sure you are getting the most out of this therapy by taking in the appropriate amount of oxygen during activity and at rest.
Quit Smoking

This is a hard one, but it is the most important if you do smoke. First and foremost, smoking while using oxygen is extremely dangerous because oxygen is flammable, but it is also dangerous internally, for your already damaged lungs.
You would be surprised by how quickly your body starts to recover after you’ve quit smoking.
Certain qualities of life will start to get stronger, like your senses of smell and taste. You coughing will be noticeably less intense in the morning and throughout the day because the tar in your airways will get cleaned out.
Purchasing an electronic cigarette may help you to gradually decrease your nicotine intake, but eventually you'll want to quit inhaling products altogether to get the best results for your lungs. If you are on the path to quit E-cigarettes, you could also try using nicotine patches or gum.
Part of kicking the habit is keeping your hand busy with other things, and chewing gum to help with the mouth fixation.
Set Personal Goals
Setting your own goals can be a resolution in itself! You can start by using a health diary, you can track things like your diet, exercise, and moods in order to adjust the aspects of your life that you want to change or make better.
Tracking your health can include monitoring your pulse and heart rate, your oxygen levels, and much more, so learning how to track your health stats can be a goal of your to start of this new year!

Here is a very helpful in depth resource you can use to get started tracking your health.
Overview
There are plenty of attainable goals for oxygen patients that want to make the most out of their therapy and their life.
Simple changes in habits, like eating, exercise, and getting outdoors can lead to a healthier more independent life style.
And with the help of the right oxygen equipment, your oxygen therapy can help you reach heights you never thought possible.
We hope that you found one or two New Years resolutions in this article that you can implement into your life this year, and we will see you in 2021!


Managing chronic obstructive pulmonary disease (COPD) can feel like a balancing act a lot of the time. On one hand, you want to do everything you can to reduce the symptoms and prevent the progression of your disease. However, on the other hand, you don’t want to use any treatments that could cause serious side-effects. It’s not always easy to find a balance between these two things and create a routine that works for you.
This has never been more true than with home remedies. Simply put, a home remedy is an easy and accessible treatment option for an ailment that you can do at home. Home remedies are not prescribed by a doctor and they typically have more anecdotal evidence to prove their efficacy than hard scientific fact. What’s more, home remedies aren’t always focused on treating a specific disease like COPD. Instead, they could be focused on improving your health in general which, in turn, could help you treat your COPD.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Rather than taking a risk with home remedies you may find on social media or elsewhere on the internet, we’re going to outline some COPD home remedies that are proven to be safe and effective. Just remember that home remedies should never be put before the treatment plan prescribed by your doctor including but not limited to supplemental oxygen therapy, pulmonary rehabilitation, and an improved diet. As always, if you have any questions about what you read here, don’t hesitate to leave a comment and we’ll get back to you as soon as possible.
Dietary Supplements
Dietary supplements are commonly misunderstood in today’s world. Many people are under the impression that dietary supplements can replace a healthy diet and others are convinced that dietary supplements do nothing at all. However, the truth is somewhere between these two points of view. Supplements can potentially enhance your diet, but there are also a few things you need to be aware of in order to use them safely.

Dietary supplements are not considered “medication” by any means. In fact, the Food and Drug Administration (FDA) classifies them as a “food product.” The good news is that this means they are widely available and you won’t need a prescription in order to buy them. But the bad news is that supplements are not regulated the same way as medication. It also means you’ll have to do your due diligence and research supplements, as well as the company selling them before you make any commitments.
Vitamin D Supplements
It’s a well-known fact that many people develop vitamin D deficiency after contracting COPD. According to the National Emphysema Foundation, over half of all COPD patients develop vitamin D deficiency because they consume fewer foods that are high in vitamin D and they are less likely to spend time outside in the sunlight which is a major source of vitamin D for many healthy people.

The main problem associated with vitamin D deficiency is osteoporosis, a condition where the bones become weak and brittle. Vitamin D plays an important role in the absorption of calcium which gives the bones their structure and strength. Vitamin D also plays an important role in the growth and function of muscles which is also very important for COPD patients.
Ginseng
Ginseng has a long history of use in Chinese medicine. It’s an herb that’s believed to improve pulmonary function as well as respiratory endurance. It’s known for both its antioxidant and anti-inflammatory effects as well as being able to regulate blood sugar levels. While the benefits of ginseng look promising, it’s important to discuss with your doctor before using it because it’s known to interfere with certain COPD medications.

N-Acetylcysteine (NAC)
This is an antioxidant supplement that’s shown potential when it comes to thinning mucus, reducing phlegm, and clearing the airways. Like ginseng, NAC is a widely available supplement that can be bought without a prescription. However, it is also known to interfere with certain medications, so it’s important to consult with your doctor before using it to treat your COPD.
Smoking Cessation
The vast majority of people who have COPD have smoked in the past and about 38 percent of current COPD patients are also smokers. Many people believe that, since they’ve already contracted COPD, there is no reason to put in the effort to quit smoking. But this could not be farther from the truth. The main reason to quit smoking is to slow the progression of COPD, but there are a whole host of other reasons as well.

Smoking increases your risk of conditions like heart disease, heart attack, diabetes, and more. What’s more, current evidence suggests that smoking is associated with increased severity of disease and a higher likelihood of death in COVID-19 patients. Smokers are known for having impaired immune systems which could also put you at a higher risk of contracting respiratory infections.
While there are many prescription medications you can use to quit smoking such as Chantix or Zyban, there are also many natural methods for quitting smoking. One thing you should know about smoking and other types of addictions is that you need it in order to feel normal. If you’re deprived of it for too long, you will likely start to experience feelings of withdrawal. When this happens, you’ll experience intense cravings, along with headaches and a change of mood. This is when you’re most likely to fall back into your smoking habits.
In order to avoid these intense feelings, you may have to slowly wean yourself off cigarettes or use a common technique like nicotine replacement therapy. Unfortunately, many smokers feel like they’re up against impossible odds when it comes to smoking cessation. Maybe you’ve seen others around you fail at losing cigarettes or you just don’t feel like you have it in you. But the truth is, it takes many attempts to quit smoking. This study suggests that it could take anywhere between 8 and 14 attempts to drop a smoking habit for good.
Cleaning Your Home
For most people, cleaning the house is a chore. But for someone with COPD, it can be a lifesaver. There are two reasons you should clean your home on a daily basis: first and foremost, it helps to eliminate airborne allergens and bacteria from your home, and secondly, cleaning is a therapeutic activity that helps you feel accomplished and whole. When your living environment becomes messy or dirty, you’re far more likely to experience issues like anxiety and depression.

Before you start cleaning, you need to make sure you’re using safe cleaning products that don’t contain dangerous chemicals that could exacerbate your respiratory problems. Unfortunately, the cleaning product industry is rife with hazardous chemicals that, if inhaled, can lead to coughing, wheezing, chest pain, shortness of breath, and even permanent lung damage. In COPD patients, inhaled chemicals can even cause severe exacerbations.
Volatile organic compounds (VOCs) are some of the most common hazardous materials you should keep an eye out for. Some common personal and home care items that include VOCs are:
- Disinfectants and cleaners
- Pesticides
- Air fresheners
- Deodorant and cosmetics
- And fuel

Other hazardous things in cleaning products include bleach, ammonia, ethylene glycol, monobutyl acetate, sodium hypochlorite, and trisodium phosphate. If at all possible, you should entirely avoid using cleaning products with these chemicals in them. However, if you absolutely have to use them, you should ensure that the room is well-ventilated, you should always wear a mask, and avoid getting the cleaning product on your hands or near your eyes or mouth. Refer to the Cleveland Clinic for more information on cleaning safely if you have COPD.
Breathing Exercises
Breathing exercises may seem silly to someone who has never tried them. However, the more you look into them, the more you begin to realize the bad breathing habits people develop over the course of their life. As a society, we spend more time sitting and remaining sedentary than ever before. This has caused many people to develop a shallow, ineffective breathing method that can be dangerous for someone with COPD or other respiratory conditions.
Breathing exercises are very easy to practice in the comfort of your own home and they are the perfect thing to incorporate into your daily routine. Not only will breathing exercises help you correct bad breathing habits, but they will also teach you how to reduce and manage anxiety more effectively.
.jpg)
One of the worst habits for COPD patients to develop is chest breathing. This type of breathing is focused on using the chest muscles in order to expand the lungs which can be exhausting with inflamed and obstructed lungs. Chest breathing should be replaced with diaphragmatic deep breathing which is focused on using the diaphragm, the thin sheet of muscle above the stomach to expand the lungs.
Anxiety Management
Cleaning regularly and practicing breathing techniques are both great ways to reduce anxiety, but they aren’t the only ones. The tricky thing about anxiety, depression, and other mental health disorders is that they can be triggered by just about anything. Some people may experience anxiety about their health whereas other people may experience anxiety for reasons that are purely biological.
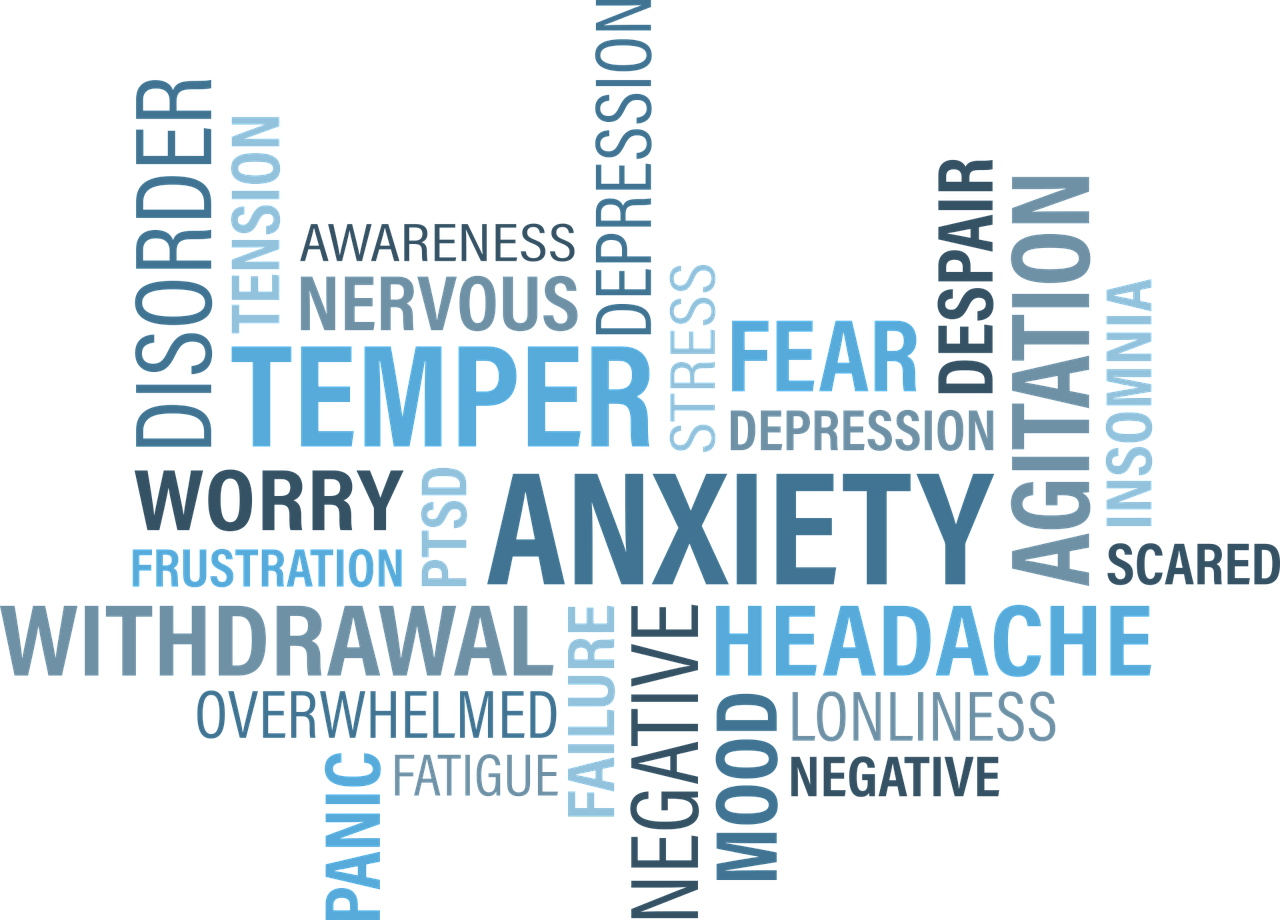
The first step to preventing anxiety is to simply follow your treatment plan as closely as possible. Your treatment plan is designed with your long-term well-being in mind and that includes your mental health. Things like exercise and a healthy diet will help with full-body wellness and they’re always the first things you should commit to if you want to feel happier and more motivated. If you’ve tried all of this and you’re still experiencing anxiety, cognitive behavioral therapy (CBT) is the best alternative.
Weight Management
COPD is commonly linked with weight loss. Due to the increased energy that it takes to breathe with COPD, a changing immune system, and other factors like a loss of appetite, many COPD patients find themselves losing an unhealthy amount of weight. Oftentimes, this weight can be muscle mass rather than fat which is the most dangerous part about it. Your body needs muscle strength in order to breathe and get around more efficiently, so it’s very important to keep a healthy weight with COPD.

Weight management is something that can be done at home. Your doctor has likely set you up with a new diet plan that includes high protein, fiber, and healthy fats. You should follow this plan as closely as possible. What’s more, you should eat regularly throughout the day instead of eating one or two big meals each day. This will prevent you from feeling exhausted or bloated after eating and keep your energy levels stable throughout the day.
![]()
The second thing you should be aware of is your exercise routine. Pulmonary rehabilitation isn’t just designed to keep your lungs strong, it’s also important for helping you manage your weight by keeping fat off and muscle on. Like your diet, the most critical thing with pulmonary rehab is consistency so try to incorporate fitness into your daily routine.
Healthy Sleep Habits
Your sleep/wake cycle doesn’t just affect your alertness throughout the day, it also affects your energy levels and your ability to take on the challenges that COPD presents. For example, someone with a healthy sleep schedule will have a better mental attitude and a better willingness to make lifestyle changes that will positively impact their respiratory health. A poor sleep schedule can also contribute to anxiety which can further exacerbate COPD.

The key to a healthy sleep schedule is consistency. Adults should be getting between 7 to 9 hours of sleep each night and your sleep schedule shouldn’t vary night-to-night. Try to get to bed and wake up at the same time each day. Doctors also recommend avoiding naps throughout the day, getting plenty of exercise, and avoiding using electronics before you go to bed.
If you’re concerned that you’re losing sleep at night due to low oxygen levels, you may want to speak with your doctor about using supplemental oxygen therapy while you sleep. You are likely already on some form of oxygen therapy, but using an oxygen concentrator while you sleep will ensure that your blood oxygen levels remain stable throughout the night. Portable oxygen concentrators like the Caire FreeStyle Comfort or the Inogen One G5 are great options because they’re small, quiet, and can be plugged into any wall outlet meaning they’ll never turn off on you in the middle of the night.

If you have obstructive sleep apnea (OSA) and need to use a CPAP or BiPAP machine while you sleep, you will need to use a continuous flow portable oxygen concentrator like the Respironics SimplyGo. This concentrator is designed to put out a constant stream of oxygen, so if your breathing is interrupted for any reason while you sleep, you can rest assured that you’ll still be receiving medical-grade oxygen.
Conclusion
When it comes to treating COPD, you need a comprehensive approach that takes into consideration all facets of your life from your sleep schedule to your mental well-being. Home remedies are a great way to make you more conscious about how your lifestyle is affecting your health and what steps you can take to reverse these issues.
At the same time, however, you need to be careful about what home remedies you use. Some people will make unfounded claims about dietary supplements or other remedies which can actually make your symptoms worse. This is why you should always consult your doctor before using a new product or making drastic changes to your lifestyle.
Above all, you should be focusing on the treatment plan that you’ve created with your doctor. Doing so will help you alleviate breathlessness, chest pain, and coughing associated with COPD and you can expect to see a better prognosis for your disease.
.png)
The novel coronavirus has completely reshaped the way that we view sanitation. Over the past year, organizations and individuals alike have taken steps to control the spread of disease, and the population as a whole has become more aware of the impact of infectious disease. Another thing that people have become more aware of is the impact of chronic respiratory diseases such as COPD, asthma, and pulmonary fibrosis. Studies have shown us that these people are “high risk” when it comes to infectious disease, so we need to take steps to protect their health.
Unfortunately, simply telling someone to “clean more often” or “clean more thoroughly” is bad advice. These statements fail to acknowledge that cleaning products themselves can actually put our health at risk. Many household cleaning products are filled with toxic chemicals that can irritate the eyes, skin, and throat. And in the worst cases, they can even contribute to COPD symptoms by exacerbating chest pain, difficulty breathing, and chronic coughing.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
In this post, we’re going to provide you with a comprehensive list of steps for cleaning your home as a COPD patient. We’ll give you advice on choosing cleaning products, how often you should clean, and other things you should take into consideration. If you have any questions, feel free to leave a comment. And if you find this information helpful, don’t hesitate to share it to help us get the word out about safe cleaning habits.
How to Choose Cleaning Products With COPD
The first step in cleaning your home is to choose the cleaning products that you will use. While this may sound like the easiest step, it’s actually the hardest. Cleaning products are rife with volatile organic compounds (VOCs). These are compounds that have a high vapor pressure and low water solubility. Many VOCs are artificial meaning they’re man-made, and they contain chemicals such as methyl tert-butyl ether (MTBE), trichloroethylene, oxygenates, and other industrial solvents.

According to the Environmental Protection Agency (EPA), concentrations of VOCs are up to ten times higher indoors than they are outdoors. This is largely due to the fact that VOCs are found in many household cleaning products and many homes are not ventilated well enough to rid them of harmful chemicals. But VOCs aren’t the only harmful ingredients found in home cleaning supplies. Many of them also contain carcinogens, chemicals that are known to cause cancer.
![]()
As a COPD patient, your goal should be to eliminate all hazardous cleaning products from your home. However, it’s especially important to avoid cleaning products that can exacerbate your respiratory symptoms. Products like air fresheners are particularly harmful to COPD patients because aerosol droplets can remain suspended in the air for long periods of time, meaning they can be inhaled. Generally speaking, “scented” cleaning products should be avoided at all costs. While we may enjoy a fresh smell and equate it with a clean home, most of these products contain harmful chemicals.
Before heading out to the store, create a list of ingredients that you should avoid. The ingredients below are commonly used in cleaning products and should be avoided:
- Perchloroethylene (PERC)
- Formaldehyde
- 2-Butoxyethanol
- Ammonia
- Sodium Hydroxide
- Chlorine
Some common cleaning products you should avoid include:
- Bleach
- Spray cleaners
- Fragrance sprays
- Carpet fresheners
- Fabric softeners
- Varnishes
-
Drain cleaners

Another thing to note is that you should be wary of anything labeled “green,” “organic,” or “eco-friendly.” Just because something is “organic” does not necessarily mean that it is healthy or safe. However, you may see products labeled as “safer choice.” These cleaning products are actually regulated by the Environmental Protection Agency (EPA) and they’re aimed at reducing, eliminating, or preventing pollution at its source. In many cases, these cleaning products can be a safer alternative for COPD patients but many of them still contain chemicals.
How to Make Safe Cleaning Products at Home
Believe it or not, homemade cleaning products can be extremely effective and they can also be much safer to use than store-bought items. When you make your own cleaners, you’ll know exactly what’s in them and you won’t have to worry about reading through and researching a long list of ingredients.

According to Healthline, some of the safest and most effective ingredients you can use to make homemade cleaning products include white vinegar, lemon juice, methylated spirits (denatured alcohol, and baking soda. Unlike the harsh chemicals found in store-bought products, COPD patients typically don’t have any reactions when exposed to these ingredients.

If you want to clean your floor or countertops, combine boiling water with either lemon juice, white vinegar, or methylated spirits. This will make a great degreaser and prove much more effective than a wet rag. If you want to clean a mirror, vinegar and water is a great combination. For removing stains, soda water is your best bet.
Keep Your Home Well Ventilated
Ventilation is imperative when it comes to keeping your home clean. Simply put, ventilation refers to the healthy exchange of air between the inside of your home and outdoors. This prevents harmful chemicals, moisture, and other allergens from concentrating in your home and posing a serious health risk. One of the best ways to ventilate your home is to simply crack a window when you’re cleaning.

If you’re worried about allergens making it into your home through the window, you can install a screen. While this won’t block out all allergens, it will prevent some of the larger particles from entering your home. Another thing you can do is change up the air filters on your HVAC system. The air filter or “particle filter” is designed to remove allergens from the air as it’s circulated throughout your home. However, over time, these filters can become very dirty. Not only will this start spiking your utility bills, but it won’t filter airborne pollutants correctly.
Choose the Right Tool for the Job
Aside from choosing the right cleaning products, you also need to choose the right tools for cleaning your home. COPD is a debilitating condition so you may need to find creative ways of doing things that won’t add any unnecessary strain on your lungs and the rest of your body. For example, if you need to clean in a hard-to-reach area, be sure to use a cleaning device with an extendable handle. This way, you won’t have to strain yourself or risk falling just to clean your home.

If you’ve been prescribed long-term supplemental oxygen therapy, another thing that can help is a portable oxygen concentrator. If you already use a stationary oxygen concentrator or oxygen tank for your oxygen needs, a portable oxygen concentrator will provide you with much more freedom to navigate your home with ease. Rather than having to be plugged into a wall outlet, POCs operate off of powerful lithium-ion batteries so you won’t be relegated to one room of the house.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Portable oxygen concentrators like the Caire FreeStyle Comfort and Inogen One G5 are very lightweight and compact, so you can carry them around all day without feeling exhausted or out of breath. The FreeStyle Comfort even has an ergonomic curve design that will prevent the unit from sliding around at your side while you’re cleaning the house. Once you’re ready for a break from cleaning, simply plug your device into the wall and by the time you’re ready to go again, you’ll have a full battery.

If you’re someone who needs more oxygen to keep you going, the Respironics SimplyGo may be the portable oxygen concentrator for you. This is a continuous flow unit meaning it puts out a constant stream of oxygen rather than “boluses” of oxygen like the FreeStyle Comfort and the Inogen G5. While the Respironics SimplyGo is a bit heavier than these two, it will provide you with more options including the ability to use your POC with your CPAP or BiPAP machine while you sleep.
Don’t Forget to Declutter Your Home
While you’re up and about cleaning your home, it’s also a good idea to spend some time decluttering your home. “Decluttering” simply means reorganizing or getting rid of some of your belongings in order to make your home more comfortable and easy to navigate. This is very important if you’re a COPD patient because having to navigate a messy home can be very challenging and dangerous.

We briefly discussed decluttering in our post about COPD and balance issues, but the basic idea is that you want to create a living space that’s accommodating of your lung condition. First and foremost, you should remove any belongings from the floor that could be a tripping hazard such as clothing, cables, and even furniture. Taking the time to move these things out of the way of where you walk in your home can go a long way toward making your home safer and more accommodating for you and your guests.

If you want to go the extra mile, you might want to consider installing a medical alert system in your home. This consists of a receiver that’s plugged into the wall and a small button that can be worn around your neck. If you take a fall or experience a COPD exacerbation in your home, simply press the button and medical personnel will immediately be sent to your home. These are a must-have for any COPD patient, especially if you don’t have friends or caretakers who visit your home regularly.
Get Outside When You Can
According to the EPA, indoor air pollution can be 2 to 5 times greater than outdoor air pollution. The reason for this is because indoor air pollutants are concentrated in a small area whereas outdoor air pollution can dissipate. While you can and should take the time to clean your home, you should be going outside as much as possible to get some fresh air.

AirNow.gov has a great air pollution map that will give you a good idea of how clean the air is in your area. Simply visit their site and type in your ZIP code. You’ll be given a number anywhere between 0 and 500 with 0 being the least polluted and 500 being the most polluted. It’s recommended that COPD patients avoid going outside if the air quality index (AQI) is over 100. However, people with severe COPD may only want to go outside when it’s below 50 AQI.
.jpg)
While the AQI is a good indication of the air quality in your area, it’s not 100% accurate. If you live in a very urban area with a lot of traffic, the air quality may be lower than what the website tells you. As such, it’s important to use your best judgment before going outside. Try going out when traffic has settled down and try to stay away from the roads as much as possible.
The temperature is another important factor to consider before going outside. Extreme conditions of any kind can lead to exacerbation of COPD. Low temperatures can be particularly difficult for COPD patients because inhaling cold air can thicken your mucus making it more difficult to breathe. Hot temperatures can cause you to feel exhausted more quickly and also exacerbate respiratory problems.
![]()
Schedule a Home Inspection
If you want to take the extra step towards making your home as accommodating as possible for your COPD, you should consider scheduling a home inspection. This is when a professional safety inspector walks through your home and performs a variety of tests designed to determine the safety of your home. While you may think of a home inspector as someone who examines the structural integrity of a home, they also play an important role in determining its cleanliness as well.
One important thing your home inspector will do is evaluate your HVAC system. This includes things like your heater, air conditioner, air ducts, and air filters. He/she will check to ensure that there are no leaks and that your system is circulating clean air throughout your home. The inspector will also look for water damage or plumbing leaks throughout the home that could lead to the growth of mold. Several types of mold, like black mold, can be very hazardous to your health. Black mold poisoning is associated with a chronic cough, fatigue, and irritation in the throat and eyes.

Home inspectors won’t fix these issues within your home. Rather, they provide you with a list of potential problems in your home and advise you on what to do or who to call to get the issues resolved. However, hiring a home inspector is still a very important step because you may be exposed to harmful airborne irritants unknowingly. Many people live with health issues for years only to find out they had a mold or HVAC problem that they were unaware of.
Recruit Help With Cleaning
There’s no doubt about it, cleaning can be exhausting. If you feel like you have a lot to clean and not a lot of time to do it, you may want to start outsourcing work to friends, family, or even a caretaker. While physical exercise is a must for any COPD patient, too much exercise or overexertion can lead to a flare-up in your symptoms, most notably chest pain, breathlessness, and fatigue.
.jpg)
There’s no shame in asking for help with cleaning your home, especially when your well-being is at stake. However, if you decide to recruit help from a friend or family member be sure to let them know about your safe cleaning routine. Let them know that you’re concerned about the chemicals in common store-bought cleaning products and show them how to make the homemade cleaning products we discussed earlier in this post.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Conclusion
Maintaining a healthy living environment is one of the most important things you can do as a COPD patient. Poor air quality in your home will not only irritate your skin and eyes, but it can damage your lungs and lead to flare-ups in your respiratory symptoms. COPD patients who do not breathe clean air are more likely to experience exacerbations that can lead to hospitalization.
Unfortunately, simply cleaning more often or more thoroughly is not the solution. You need to be careful about what cleaning products you’re using and how they affect the quality of air within your home. You should also take additional steps like ensuring your home is well-ventilated and that you’re keeping dust and mold in check.
If you found this post useful, don’t forget to bookmark it so you can refer back to it in the future. And if you have any questions or concerns, please don’t hesitate to leave them in the comment section below

Chronic obstructive pulmonary disease (COPD) is an umbrella term used to describe one of two different respiratory ailments: chronic bronchitis and emphysema. The former is characterized by swelling and inflammation of the bronchial tubes and the latter is characterized by damaged alveoli, the small air sacs in the lungs that are responsible for the transmission of oxygen and carbon dioxide to and from the blood.
When COPD is diagnosed, patients aren’t simply given a “one-size-fits-all” treatment plan. Instead, doctors will look at several different variables such as how developed the COPD is, where it’s located, and what caused it. By doing so, he/she will be able to create a treatment plan that is customized to your specific condition.
In this post, we’re going to be looking at the early stages of COPD. This is commonly referred to by medical professionals as “stage 1 COPD” because it’s when the signs of COPD first start to emerge. If you’re diagnosed during this stage, there are several things you should know, so stay tuned to find out, and be sure to get in touch with us if you have any questions.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
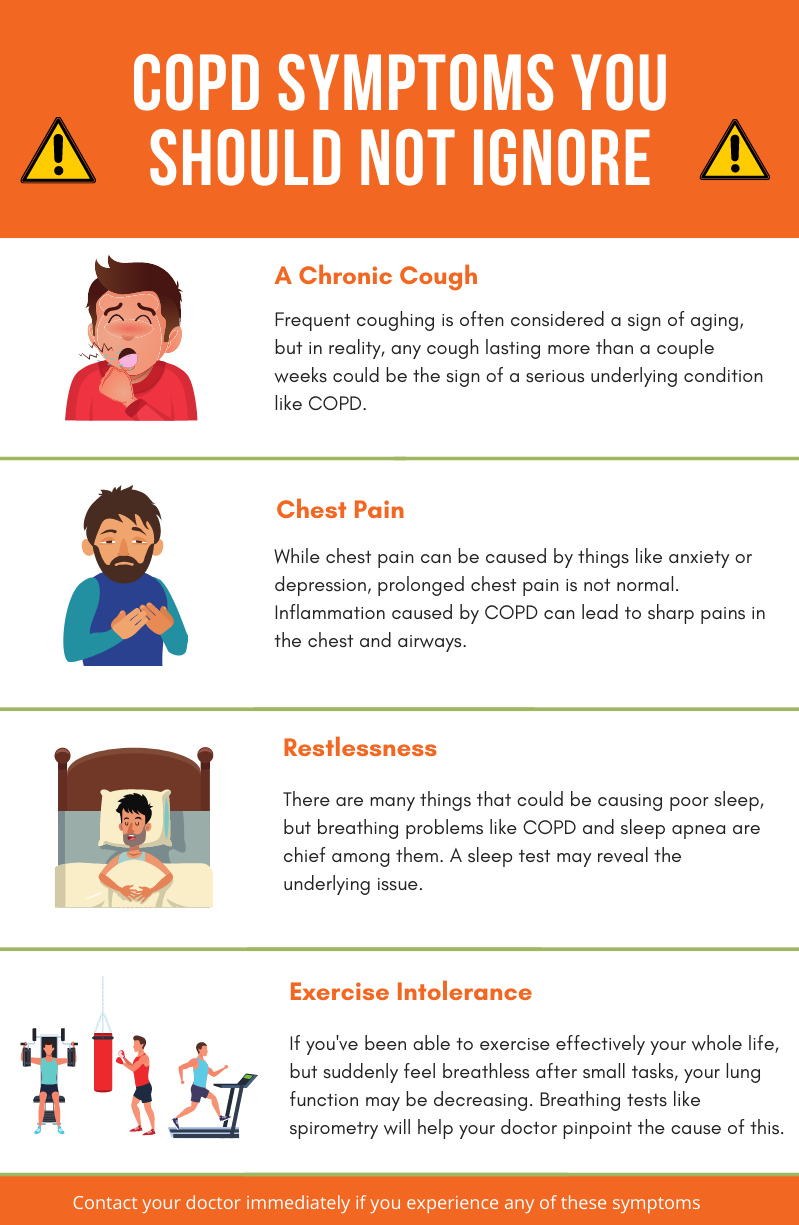
Symptoms of Early-Stage COPD
1.) You’re Not Alone
Did you know that about 16.4 million people in the United States have COPD and an estimated 328 million people have COPD worldwide? While it’s easy to feel alone when you’re diagnosed, in reality, it’s one of the most prevalent health conditions in the world ahead of lung cancer, diabetes mellitus, and even Alzheimer’s disease.

Unfortunately, most COPD patients don’t get this impression from watching the news, reading the paper, or simply going about their daily lives. Despite how common COPD is, it sorely under-discussed and underfunded. What’s more, there seems to be a general lack of understanding of what COPD even is.
According to the National Chronic Obstructive Pulmonary Experience (COPDE) Survey, 60 percent of respondents reported not having an action plan for dealing with exacerbations and 16 percent reported not even knowing what a COPD exacerbation was. Another study published in the European Respiratory Journal found that only about 50 percent of current or previous smokers surveyed knew what COPD was.
It’s difficult to say why COPD has less awareness in the general population and among smokers than other lung diseases, but there are definitely some likely causes. For starters, cancer often takes the spotlight these days. Cancer is one of the most talked-about chronic illnesses in this day and age. It’s the second-leading cause of death in the country, but only about one-fourth of the total cancer deaths are caused by lung cancer. This could lead to people unknowingly inflating the prevalence of lung cancer.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Another potential cause of the lack of awareness for COPD is the way it develops. While COPD tends to develop very slowly over the course of many years, lung cancer is often the opposite. Lung cancer is often considered to be one of the fastest-growing cancers and small cell lung cancer (SCLC) patients, in particular, often die after just 5 years. Another problem with lung cancer is its tendency to spread to other parts of the body.
Finally, you need to consider the fact that COPD is often affected by diagnostic error. In other words, someone may have COPD and not know it, or they might visit a doctor for their symptoms and get diagnosed with a condition other than COPD such as asthma or pulmonary fibrosis. Studies suggest that about one-fifth of smokers over the age of 40 show signs of COPD, but millions of them do not receive a diagnosis.

When you take all of these factors into consideration, along with the fact that lung cancer and COPD share the same awareness month (November), it’s not hard to see how COPD can often be overshadowed. It’s important to not diminish the awareness surrounding lung cancer because it is a very serious disease, however, it’s also important for COPD patients to know how common their illness is. What’s more, errors in spirometry testing can also lead to misdiagnosis of COPD.
2.) There is an Active COPD Support Community
Now that you’re aware of how common COPD is, you’re likely wondering what options you’ll have to get involved in the community. Luckily, there are a whole host of COPD communities out there composed of COPD patients, caretakers, researchers, medical specialists, medical device manufacturers, and more. And with how connected modern technology is, you’ll be surprised to find just how easy it is to get started.

We made a blog post in the past that covers this topic in detail, however, we’ll summarize its points here for your convenience. In simple terms, a COPD community is a place for people with COPD to come together to support each other and raise awareness for the problems they face. COPD communities can either be organized by an individual like a patient or a caretaker, or they can be created by an organization.
For example, the COPD Foundation created an online COPD forum called COPD360 Social. This forum is designed to connect and foster communication between COPD patients, healthcare professionals, caretakers, academic institutions, and researchers in order to aid in COPD prevention and management. Like other forums on the internet, COPD360 Social has a badge system that allows you to upvote a user’s responses. This way, the community decides which users are the most helpful and trusted. In order to make this platform accessible to people all across the world, it’s 100% free to use.

Another COPD organization that offers an online community is the American Lung Association. While the ALA puts a lot of their focus on lung cancer and creating cleaner air for future generations, they also host an online forum similar to the one offered by the COPD Foundation. The forum is accessed through Inspire.com. One of it’s best features is that it has a mobile application meaning you can access it via your phone or tablet from anywhere in the world.
One final COPD organization you should be aware of if you’ve just been diagnosed with early-stage COPD is COPD.net. This forum is hosted by Health Union, a social media platform designed to leverage technology to create more productive, impactful, and meaningful conversations between people with chronic illnesses. When you subscribe to COPD.net’s Help Center, you’ll receive weekly surveys and research opportunities, an e-newsletter, and you’ll be given access to the Q&A tool online.
Another great way to get involved is through social media sites. Facebook, for example, has a feature called “groups” that can be created or joined by any user. These groups are designed to bring people together to discuss specific topics and there are hundreds of them that discuss respiratory illness, smoking cessation, and other topics relevant to COPD patients. Getting started is easy. Simply go up to the search bar and type in the topic that interests you. Then click on “groups” and it will display a list of results. You can then join any group you want and begin conversing with other likeminded people.
Becoming involved in the community is extremely important for COPD patients, no matter what stage of their lives they’re in. A study published in PubMed, a public access journal, found that — regardless of the severity of COPD — most patients feel a strong desire to feel involved in social gatherings like holidays, one-on-one communication, or social media interactions. In other words, being engaged rather than simply participating gave them more of a sense of purpose in their daily lives.
3.) COPD Can’t Be Reversed, But it Can be Treated
One thing many people do when they’re first diagnosed with COPD is they immediately start searching for a cure. Unfortunately, COPD is not like an infection that can be cured with antibiotics and it’s not like a headache that will go away with time. COPD is permanent and it’s progressive meaning it can only get worse.

While this may seem like a pretty grim reality, it’s actually not! If you’re careful to implement effective lifestyle changes you’ll be able to drastically slow the progression of your disease, reduce respiratory symptoms, and experience peace of mind. But in order to make these changes, you need to know a little about COPD and what causes it.
COPD is the result of chronic inflammation in the lungs and airways. 85 to 90 percent of COPD cases are the result of cigarette smoking, but there is also a condition called Alpha-1 deficiency that leads to the onset of COPD in non-smokers. Alpha-1 is a protein that regulates immune reactions in the lungs, and when it’s not produced in high enough quantities, it can make your lungs vulnerable to permanent damage.

Over time, this inflammation becomes worse and further impairs your breathing so it’s imperative that you avoid anything that could irritate it such as cigarette smoke, car exhaust, or any other type of air pollution. It’s also important to avoid infection because this is the leading cause of COPD exacerbations (when symptoms rapidly get worse).
Supplemental oxygen therapy is one of the best ways to stabilize your condition, reduce respiratory symptoms, and improve your life expectancy. In the past, COPD patients would need to carry around bulky oxygen tanks, but portable oxygen concentrators have since replaced them as a lightweight and more convenient alternative.

Another key component of a COPD treatment plan is pulmonary rehabilitation. This is similar to how you would go through a physical therapy course if you sustained an injury to your legs or back but it focuses on the lungs. Not only will pulmonary rehab show you how to exercise effectively with COPD, but you will learn important lessons about how your lungs function and how to keep them healthy.
Last but certainly not least is the dietary component of your treatment plan. While it may not seem like your diet would have an immense impact on COPD progression, it actually does. Evidence suggests that antioxidants found in fruits and vegetables have anti-inflammatory properties that have positive effects on people with COPD and asthma. Similar studies also found that soluble fiber intake has the potential to protect against airways inflammation.
Conversely, foods that lead to weight gain, obesity, and fatigue can all add to your COPD symptoms. Studies have found that obesity can lead to alterations in immune function, insulin resistance, and dyslipidemia (an abnormal amount of lipids in the blood). However, being underweight with COPD has its problems as well, so a healthy weight should be your goal.
Supplemental oxygen, pulmonary rehab, and diet are a few, but not the only methods of treating COPD. Above all, you should be open and honest with your doctor about your symptoms so that he/she can create a treatment plan that’s based on your needs.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
4.) It’s the Best Time to Quit Smoking
If you haven’t done so already, now is the perfect time to quit smoking. As aforementioned, 85 to 90 percent of COPD cases are caused by smoking but it’s also important to remember that the majority of people who smoke are never diagnosed with COPD. Rather, they develop other chronic diseases such as lung cancer, diabetes, and heart disease. According to the Cleveland Clinic, smokers have a 70 percent higher risk of dying from coronary artery disease than nonsmokers.

Since smoking causes COPD, it can also make COPD symptoms worse by increasing the rate of inflammation in the lungs and airways. Smoking is known as an immunosuppressant drug meaning it reduces your body’s ability to prevent infection temporarily. Since infection is the leading cause of COPD exacerbation and we’re in the middle of a pandemic, smoking is the last thing you want to do!
5.) It’s the Best Time To Implement Long-Term Goals
Many people go their whole lives without implementing long-term goals. This can be very detrimental if you want to achieve your full potential, especially when it comes to your health. Whether you’ve been a long-term planner before or you’ve always stuck to short-term goals, there’s never been a better time to start.
As we’ve already established, smoking cessation should be your first goal, but ideally, this should be a short-term goal because immediate cessation is will help you better achieve your long-term goals. But aside from this, your first goal should be to create a COPD action plan and implement it successfully.
A COPD action plan is a personalized plan for managing your symptoms and exacerbations. For example, it could remind you how much you need to exercise each day or what foods you need to avoid in order to prevent respiratory flare-ups. We made a whole blog post about this subject so don’t hesitate to check it out.
6.) It’s Not the End
The last, but probably most important thing you should know about early-stage COPD is that it does not signify “the end” of your life. Not only that, but it is not even the beginning of the end. While being diagnosed with COPD is certainly not a positive experience, it is possible to achieve a positive outlook by changing your mindset and practicing healthy habits.

One positive thing to focus on is that COPD patients enjoy a far greater life expectancy than people with other chronic diseases. On average, a current smoker with stage 1 COPD has a life expectancy of 14 years. Compare this to the 50 percent of heart disease patients who live past 5 years or the 16 to 24-month median survival rate for small-cell lung cancer patients.
But it’s not just about survival rate, it’s also about quality of life. COPD patients who implement effective and proven treatment strategies like supplemental oxygen therapy, pulmonary rehabilitation, and an improved diet see improved quality of life.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Final Thoughts
COPD is a serious debilitating disease, but it is by no means the final straw. Even if you have been diagnosed with early-stage COPD, you have a lot of life to live and it can be enhanced by closely adhering to your doctor’s instructions.
In the meantime, getting involved in the COPD community, taking care of your mental health, and quitting smoking are all important steps to take after you receive a diagnosis. Doing so will ensure that you live a long, happy, and fulfilling life.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













