
The holidays can be a stressful time for everyone and people with COPD should take extra precautions to avoid over-exerting themselves mentally and physically, over-eating, and stressing. If you are one of the 16 million Americans with COPD, avoiding these COPD triggers over holidays will make everything more enjoyable and you will run a lower risk of getting sick or experiencing a COPD exacerbation.
However, this holiday season, 2020 and going into 2021, the global COIVD-19 pandemic is making this holiday season even more difficult, especially for our family and friends that have COPD.
With COVID-19 cases increasing as we are getting more into the holiday season, public health experts are encouraging people to be even more stringent about social distancing, and limiting travel.
These unprecedented circumstances have changed almost everything, including the ways we interact with people. Connecting virtually with loved ones and family members is one of the only ways to safely spend this lovely time of year together, even in the weeds of a pandemic.
If you have never tried FaceTime, Zoom, Skype, Google Hangouts or any other form of face to face virtual communication, there is no better time to do so! Also, stay on the look out for a new LPT Medical blog about connecting with family and friends digitally!
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The Importance of Holidays and Social Connection
Holidays give us a sense of belonging, and they bring our most loved people together into one place. This tradition should continue into this year in some way shape or form. So, start spreading the idea that creating new traditions amongst your family members can be very joyful and fun.
That being said, holidays can be exciting and fun, but for people who suffer from Chronic Obstructive Pulmonary Disease (COPD) holidays can also initiate stress and other COPD triggers.
In this article we are going to discuss how you can avoid COPD exacerbations throughout the holidays, and minimize your chances of getting sick.

COPD and the Holidays
If you have COPD, be prepared this holiday season. It is unfortunate, but living carefree and enjoying the holidays can be difficult for those that suffer from ongoing medical conditions, such as COPD. The extra effort it takes to just to breathe can cause any holiday to be just that much more stressful, not to mention the added stress of a global pandemic. However, there is relief, and we have compiled some helpful COPD tips for the holiday!
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Helpful COPD Tips for the Holidays
The holiday season is famously the time of year we get to relax and spend quality time with loved ones, but it does pose real risk for additional anxiety and increased stress, which can be triggering for patients with COPD. So here some helpful tips for you!
Traveling

Of course it is recommended not to travel for the holidays this year, but if you are traveling, be prepared, be prepared more than you have ever been before.
You don't only need to remember all of your medications and be sure you have your portable oxygen concentrator (POC) or oxygen tank, you also have to make sure that you have an extra POC battery, and your POC AC and DC charger cables. Should your POC start to run low, you want to avoid having to stop into a location to charge your oxygen device in order to avoid contact with strangers and surfaces. If you do not have an extra battery or other oxygen accessories, all of those items can be found on our website.
Watch What you Eat
If you have COPD it is important to avoid overeating. This is much easier said than done especially during the holidays, but portion control can be the difference between enjoying your holiday versus spending it in the hospital
Medically, a full stomach can press on the diaphragm. This will increase the regular symptoms of COPD that include breathlessness, and can often induce a COPD exacerbation.

Eating healthy foods that help with COPD symptoms is a must during the holidays, especially if cold weather is a factor in your area. Minimizing the chances of triggering a COPD exacerbation is key to enjoying the holidays, and if you can’t control the cold weather, you can control what you eat, so eat healthy.
Everything may look delicious, but go with the fresh veggies, greek yogurt dip, whole grain items, potatoes and smoked turkey (in small portions) because these are all great options to choose from. You can even suggest these dishes in advance, some people love to have ideas before they decide on what food they will bring to the potluck.
Save money
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Limit shopping to what’s absolutely necessary. This year is more financially taxing for most people than any year in the past, so there is no absolutely no shame in expressing your gratitude in other ways rather than in material gifts.
As a person with COPD, it is never advisable to be out shopping among large groups of people, especially during the COVID-19 pandemic and flu season. Luckily, you can do much of your shopping from the comfort and safety of your home!

Even small local businesses have developed their online platform as a result of COVID-19 restrictions in many areas. So you will still have the option of buying thoughtful gifts that only your favorite local stores supply rather than buying from bulk operations like Amazon.
Our small family owned business, LPT Medical, invites you to shop with us online or over the phone at 1-800-946-1201 for any of your oxygen therapy necessities or accessories. From portable oxygen concentrators like the Caire FreeStyle Comfort, The Inogen One G5, or the Respironics SimplyGo, to any and all of the accessories you need to make the most of them we have some great holiday deals that our respiratory specialists would be happy to discuss with you. If you would like to know how much portable oxygen concentrator costs please call us at 1-800-946-1201, for all of your oxygen inquires and questions.

Watch What you Carry

If you do decide to venture out to go shopping, don’t be afraid to use a cart! And make sure you clean the handles of the cart with an antibacterial cleaner before you use it. If you don't already have a portable oxygen concentrator backpack, you might find it useful for carrying your oxygen device along with your other essentials everywhere you go this holiday season, to ensure you do not forget anything.
The Inogen One G4 backpack has also been reviewed as one of the easiest ways to transport your oxygen with you wherever you go, and it is also user friendly, so if you need to adjust your oxygen flow or mess with the settings, the POC is conveniently located so you can get to it without rummaging through your bag! There are also custom backpacks for the One G3 and One G5.

Stay Warm
If you haven't already read our LPT Medical blogs about avoiding COPD exacerbations, cold weather and COPD are not the perfect combination, so dressing warm for both the expected outdoor temperatures and the indoor ones is essential for maintaining your health over the holidays.
Here is a tip if you use supplemental oxygen keep your oxygen tubing under a layer of clothing so that the air you breathe will be warmer. Also, consider wearing a scarf or a CT face mask to make breathing colder air easier while you are outside!
A CT mask is the perfect holiday gift for a loved one with COPD it converts the cold dry air into moist warm air, and help respiratory patients breathe in cold air, just take note these masks do not protect against COVID-19

Be Prepared
Have all of the tools you need for everyday activities, including medications, daily inhalers and fast-acting inhalers for emergencies. If you use supplemental oxygen, make sure that you have an adequate oxygen supply by either ensuring that you have enough oxygen left in your tanks or an extra portable oxygen concentrator battery to keep your POC charged all day and night.
Trust Yourself

This holiday season is not the same as many others, where gatherings and events could go on for a long period of time, and someone with COPD might have to step out for the night due to feeling overwhelmed and tired. This is normally when we would recommend trusting this instinct and leaving when you know you have had enough rather than over-extending yourself, and weakening your immune system to the point where you are more susceptible to illness.
But this season, you might be feeling lonely, anxious, or even frightened, and it is important to recognize these emotions as valid, and understand that millions and millions of people are feeling similarly. Click here for a guide about encouraging mental health for people with COPD.
This is why it is so important for mental health to stay connected with your family and loved ones during this holiday season even if you cannot be together in person.
Overview
These suggestions for staying safe and sane during the holidays may seem like common sense, but oftentimes a reminder to trust your instincts, eat healthy, stay warm are positive health checkups we do not do enough!
Also, we wrote this article mainly as a reminder, that even if you do struggle with breathing problems, due to a chronic illness or other ailment, that does not mean that you should not experience the joy that comes with sharing the holidays with those we love.

If you are struggling with staying connected, subscribe to our daily newsletter to be updated every time we post a new blog, Or you can join our facebook group, by searching LPT Medical COPD & Respiratory support group on the Facebook App. Our emails and our Facebook group connect you with the best resources and information for anyone that suffers from a respiratory disease, or chronic illness like COPD. Our readers utilize this information to make valuable life changing decisions.
We like to write about changing your habits, your medical oxygen supply needs, tips and tricks to get through just about any obstacle life throws at you. So if you need the gift of connection, please comment below this article with any inquiries, questions, or happy holiday wishes. From LPT Medical’s family to you and yours, we are wishing you a safe and joyful holiday season.

You might be surprised to learn that the food you eat influences more than your digestive system, and your diet actually has a big impact on other systems in your body. The food you eat can fuel your muscles, strengthen your bones, clear your mind, and even help you breathe better, if you are eating the right foods.
You need a variety of foods with different nutrients to get all of the needs your body requires, and no single food will supply you with everything— which is why a healthy diet is one with plenty of variety.
If you have a respiratory disease, breathing complications are obviously one of the main symptoms that that you have to struggle with daily. Options to combat breathlessness are medications like bronchodilators in the form of inhalers, and utilizing oxygen therapy in the form of a portable oxygen concentrator. However, simple daily tasks should also be noted as some of the most important ways to treat and manage your respiratory disease, and this includes changing your diet.

If you have a respiratory disease, you can eat a specific diet that will actually help you to breathe easier, and will contribute to relieving your respiratory systems and help to ease the experience with pains or implications your disease may be posing on you.
You and your healthcare team should devise a meal plan, just for you, based on your symptoms and personal nutrient deficiencies. You can also start to meet with a registered dietitian nutritionist (RDN) that will help you figure out the best foods for you. You can find a RDN who specializes in diets for respiratory illnesses by asking your doctor to recommend you to one or visiting the Academy of Nutrition and Dietetics online and doing your own research.

So while your diet plan will be specific to you and your needs, changing your diet and eating healthy can be very challenging especially if you don’t normally pay much attention to your diet. Therefore, you can take some advice in this article that will help you develop healthier eating habits.
Maintaining a healthy weight

You should start to weigh yourself regularly, and monitor whether you are gaining or losing weight after setting up your diet plan. If you continue to lose or gain weight while following your recommended diet, talk to your doctor and RDN and make sure this is normal, and if you should be maintaining a steady weight, become informed on how to make changes in your diet. There are several health complications that can result from being underweight or overweight.
Maintaining a healthy weight is so important because if you are well-nourished you will be able to handle infections should you be exposed to a virus or bacteria. When people with a respiratory disease get an infection, it can become serious quickly and result in hospitalization either due to exacerbated symptoms or other complications. Should you catch a common cold or flu and illness does occur, having a well-nourished diet can help you fight off the infection, respond better to treatment, and have less severe symptoms.
Food and your respiratory system

Your metabolism will change the food in your body into energy that your muscles use. Your lungs are a muscle too that need fuel to operate correctly, and if you have a respiratory disease, like COPD for instance, your lungs are already compromised in doing their job. Therefore, the proper mix of nutrients in your diet can help you breathe easier.
Carbohydrates

If you have a respiratory disease, eating a diet with fewer carbohydrates and more fat will help you breathe easier.
Specifically choosing complex carbohydrates, such as whole-grain bread and pasta, fresh fruits and vegetables and limiting simple carbohydrates, like table sugar, candy, cake and regular soft drinks.
Fiber

Eating 20 to 30 grams of fiber each day, from items such as bread, pasta, nuts, seeds, fruits and vegetables.
Protein

Eat a good source of protein at least twice a day to help maintain strong respiratory muscles. Good choices include eggs, cheese, meat, fish, poultry, nuts and dried beans or peas.
Mono-saturated fats
Choose mono- and poly-unsaturated fats, which do not contain cholesterol. These are fats that come from plant sources, such as canola, safflower and corn oils.
Foods to avoid
1. Trans fats and saturated fat. For example, butter, lard, fat and skin from meat, hydrogenated vegetable oils, shortening, fried foods, cookies, crackers and pastries.
2. Acidic foods and drinks. Eating acidic food and drinks like coffee creates heartburn and people with lung disease may find that acid reflux increases their lung disease symptoms. limit acidic foods and drinks like citrus, fruit juice, tomato sauce, coffee and spicy foods in order to reduce acid reflux symptoms, and therefore, lung disease symptoms.

3. Carbonated beverages. Unsurprisingly, carbonated beverages are filled with sugar, empty calories and lots of carbonation. Therefore, they contribute to weight gain and increased bloating. The increased gas and bloating are two factors you want to avoid if you have a lung disease. Bloating and weight gain can put more pressure on your already weakened lungs. Avoid carbonated beverages such as sodas, beer, sparkling wine or sparkling cider also contribute to dehydration. So, when you’re thirsty, hydrate with water.

4. Cold cuts. A study from European Respiratory Journal suggests that added nitrates from food like cold cuts increase the risk for COPD related hospital readmissions. Limit your cured meats such as bacon, cold cuts, ham and hotdogs because all of which contain additives called nitrates.
5. Cruciferous vegetables. Vegetables, such as cabbage, broccoli, radishes and cauliflower, are filled with nutrients and fiber, but if they give you extra gas, try limiting them, and substituting other veggies into your diet when you can. Gas and bloating are uncomfortable for people with respiratory disease because these symptoms can make breathing difficult.
6. Dairy products. While milk is filled with calcium, for people with lung disease, dairy products can worsen symptoms because it contains casomorphin which has been known to increase mucus in your intestines. People with lung disease often experience an increased production of mucus in their airways already, and clearing the mucus is an important aspect of managing the disease.
7. Excessive Salt A salt-heavy diet can be a problem for people with lung disease. Salt retains water, and having too much water in your system can cause breathing problems. Try using herbs and spices to enhance the flavor of your food rather than salt.
8. Fried Foods. Fried foods can cause bloating and discomfort which pushes on your diaphragm, making it difficult and uncomfortable to breathe. Eating a lot of fried food will lead to weight gain, which will add increased pressure on your lungs.
Some of these foods listed in this section are guilty pleasures, and every once a while it can be ok, even if you have a lung disease. However, if any of these foods are a part of your daily diet, it might be time to make a serious change and cut these foods out of your diet.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
This is not easy, foods that are high in sugar and fat can be addicting, and no one ever said sticking to a well balanced diet was easy.
Here are some tips for changing your diet
While we have explained some basic nutrition guidelines for people with respiratory disease, we also know how challenging it can be to avoid certain foods as well as consistently adding certain foods into your daily meals.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
We created a list of tips and some useful suggestions that will make changing your diet, and maintaining a health weight more attainable.
- Rest just before eating if eating makes you short of breath or tired
- Instead of eating three large meals a day, it may be helpful to aim to eat four to six smaller meals. This should reduce stomach fullness and associated pressure on the lungs.
- Eat your main meal earlier: You may find that you have more energy throughout the day if you eat your main meal earlier in the day.
- Avoid foods that cause gas or bloating, this makes breathing more difficult, these include onions, cauliflower, broccoli, melons, peas, corn, cucumbers, cabbage, brussels sprouts, turnips, raw apples, and beans (except green beans). Fried and greasy foods can also cause gas or bloating.
- Eat more small meals a day around 4-6 compared to 3 big meals. This allows your diaphragm to move frequently and freely and helps your lungs fill with air and empty out more easily without a completing full stomach
- If drinking liquids with meals makes you feel too full to eat, limit liquids with meals and instead drink liquids after meals
- Ask you doctor or nutritionist about adding a nutritional supplement at night time to avoid feeling full during the day
- Ask your doctor or nutritionist about drinking a high-protein, high-energy drink that can help boost nutrition if you are unable to tolerate high volumes of food
- Choose foods that are easy to prepare, try using a crock pot that cooks your food for you over a period of time
- Eat in a relaxed enviorment
- Eat socially with friends and family
- Take your breathing medications and/or clear your airways about 1 hour before eating
- Sit up straight while you are eating to relieve pressure on your lungs
- If you use supplemental oxygen, use it while you are eating. Eating and digestion require energy, which causes your body to use more oxygen
- Eat and chew slowly so you are less likely to become short of breath. Try putting your spoon or fork down between bites to slow your eating speed and don’t get out of breath
Setting goals and tracking your diet
Setting goals is a great way to get started on a new eating plan. One way you can do this is by tracking your progress, and developing goals based on what you have accomplished already. You can also develop goals based on what your and your nutritionist and/or doctor decide would be the best for you.
.jpg)
You can set a variety of goals pertaining to your diet and weight and it's a great way to stay in check with what matters to you and getting healthier so you are better capable of managing your COPD.
Some goals you might try to set are:
- Gaining or losing 5 pounds depending on your current weight
- Adding more protein into your meals, and limiting your simple carbohydrates intake to once per week
- Cooking more healthy foods rather than ordering take out
- Buy a cookbook filled with healthy meals and trying a new recipe once per week
Once you have developed a few goals, the next step is to make an action plan, you can do this by asking yourself, “What steps do I need to accomplish to reach my goal?’” Then you can determine which step you will take first, and when.
Here is an example of how to set and make a plan for accomplishing goals:

Tracking your health is a great way to monitor what you're eating and how the foods you eat influences your mood, symptoms, and energy. You can make a list of the meals you ate and next to each meal take a few notes about how you felt afterwards.
You can keep track of what food makes you feel bloated so you know to avoid that in the future, and keep track of the foods you enjoy that give you energy throughout the day.
We call this a respiratory health diary, and this tactic is very helpful for people with respiratory diseases, but anybody can benefit from tracking their health.
![]()
A health diary can help you with just about any aspect of how to manage your disease, including monitoring symptoms, keeping your prescriptions in line, and making healthy changes like reaching a healthy weight.
If you have a respiratory illness, your ability to set goals and reach them can have a huge impact on your quality of life and the course of your disease. Having a dedicated health tracking system to help you manage your well-being with aspects like diet, exercise, and disease management has a huge impact on your health and well-being and your quality of life over-all.
Overview
Having a respiratory illness is not easy, nor is changing your diet. But the truth is, even if you have the best portable oxygen concentrator in the world, the Caire Freestyle Comfort is not going to do all of the work you need to do in order to get your respiratory disease under control.
While having the right oxygen equipment is important and taking your medication is imperative, eating right is also essential in creating a high quality of life.
Eating right contributes to your mood and mental state, it gives you energy to exercise, and helps you to feel less bloated thereby making it easier for you to breathe. That being said, actually sticking to a diet that is right for you is easier said than done, but we hope one of the strategy and tactics we listed in this article can contribute to helping you get on a diet plan and stick to it!
If you have COPD or another disease that is causing low blood oxygen levels supplemental oxygen therapy can be a life saver, quite literally. If done correctly you can add years to your life simply by adhering to your oxygen prescription. Beyond taking your oxygen as prescribed, you can start to eat healthier, stop smoking, and start exercising all of which are habits that will contribute to a healthy and long life with a respiratory illness.
In this article we are focusing on supplemental oxygen as a treatment for COPD.
Research shows that oxygen is the only drug that can prolong life in patients with chronic obstructive pulmonary disease (COPD). In fact, oxygen not only prolongs life, it improves the quality of life and has numerous health benefits for people with chronic low oxygen levels due to a variety of diseases.

Despite all of the research suggesting oxygen can make your life living with COPD more comfortable and enjoyable, some people still struggle with oxygen therapy and claim it is uncomfortable, it is limiting, and weighs them down. We wrote this article for those people who feel they are not living out the benefits oxygen therapy has to offer.
Many people live happy joyful lives traveling, exploring new relationships, trying new and exciting things, all while managing and treating their COPD. People who can live with such an invasive and chronic illness still have their hardships, but they are also committed to their treatment plan for COPD daily which makes living with this disease more manageable.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In this article we are going to explain the do’s and don’ts of oxygen therapy so that you can start managing your COPD to the best of your ability, and finally start reaping the benefits oxygen therapy has to offer.
What is oxygen therapy?
The overarching goal for your oxygen therapy is to ensure that you maintain adequate blood oxygen levels under all conditions, all day and all night. The duration of oxygen you need and the flow setting you should use for your oxygen delivery is determined by your doctor.
They will test you while you are resting and during activities. If your blood oxygen levels are calculated to be lower than the normal range at rest, continuous oxygen delivery, meaning for 24-hours a day, is the single most important treatment, above eating healthy and exercising, that can prolong your life.
By getting you blood oxygen levels back to a normal level while you sleep, exercise, and do daily activities, your body will not have to suffer through the negative consequences of intermittent or chronic low blood oxygen levels that COPD poses.

There are three main forms of home oxygen therapy. You can take it in gas form via an oxygen cylinder (the old-fashioned bullet-shaped metal tanks), in liquid form via a barrel-shaped metal tank that converts the liquid to gas upon release, or via a portable oxygen concentrator which extracts oxygen from your environmental air and compresses it into medical-grade oxygen.

Your doctor will work with you to decide what your oxygen needs are and your oxygen supply company will work with you and your doctor to find the best device to fit your needs. They will write you a prescription for the exact flow rate (liters per minute), frequency, and delivery system that is the best fit for you.
Do's and Don'ts
Don’t take more or less of your oxygen unless directed otherwise by your doctor

Oxygen is not just a gas making up a part of the air we breathe, it is a medicine. Supplemental oxygen is prescribed by your doctor, and just like other medications, it should only be taken under your doctor’s direction.
Oxygen saturation is usually considered to be normal if it is above 90% for a healthy individual living at sea level, however your doctor should be able to determine what the normal level of oxygen saturation is dependent upon your condition and individual characteristics. Typically, if your oxygen saturation is below 88% without oxygen, you will likely be prescribed supplemental long term oxygen therapy (LTOT).
When you are prescribed oxygen, your doctor will measure your blood oxygen levels while you are at rest, while you exercise, and while you sleep or rest. Some people will require supplemental oxygen continuously; others only require it intermittently or only during the night.

The specific frequency and duration you need supplemental oxygen during the day and night is dependent upon your pulmonary function tests (PFTs) that are performed by your doctor. In individuals with COPD, hypoxia in the lungs means oxygen levels become extremely low, and if you do not take your oxygen when you are supposed to, or you leave it at a low setting that does not match your prescription, your lungs and furthermore your organs will not get enough oxygen. This will cause damage and injury throughout your body.
It is also possible for oxygen users to use too much oxygen, causing a condition called oxygen toxicity. This is seen in deep sea divers, premature babies, and patients with COPD who inaccurately utilize their oxygen supply when there is high exposure to high concentrations of oxygen. You should carefully monitor yourself for signs and symptoms of oxygen toxicity throughout your treatment, especially when you first start oxygen therapy.
Signs of too much oxygen and symptoms of oxygen toxicity include:
- Headache
- Hiccups
- Shivering
- tingling in the limbs
- Vision
- hearing changes
- Fatigue
- Hyperventilation
If you continue to abuse your oxygen supply, and the high exposure to oxygen continues, vertigo and nausea will occur, followed by behavioral changes (irritability, anxiety, confusion), clumsiness and eventually convulsions.
Even though it is possible to get too much oxygen from your oxygen concentrator it is unlikely when you use your oxygen concentrator as it has been directed and prescribed to you.
This is hugely why all oxygen supply companies will require a prescription from your doctor, and why your doctor should choose your oxygen prescription based on valid results from your pulmonary tests. Your doctor will prescribe the lowest possible concentration to you that will still provide therapeutic benefits, in order to avoid symptoms of too much oxygen but also make sure your blood oxygen levels get back to normal.
Do be sure to have an oxygen device that can cover your needs should they increase over-time

If you have COPD, and you see your doctor regularly, one of the tests they will look for is determining the severity of your COPD and how it has progressed since they last saw you.
Because CODP is a chronic illness, there is no cure, and it also progresses over time, meaning you may not need supplemental oxygen now, but one day you might. And if you have an oxygen prescription now, that might change in the future should the prescription no longer fulfill your body’s oxygen requirements and it will need to be increased.
This is why it is important when you are in the market for an oxygen device, specifically while you shop for a portable oxygen concentrator that the machine is capable of increasing its oxygen output beyond your oxygen requirements at the time. If you have a reliable sales person and you are purchasing the device from an licensed distributor of medical equipment, this will be one of the main priorities both you and the company's representative should be looking into: the device's flow rates and its capabilities to fulfill you oxygen requirements and beyond.
You may also need to increase your oxygen prescription in the case of an emergency or if you are experiencing a mild to severe COPD exacerbation where your symptoms are escalated. Your doctor will inform you of when and why you should increase your oxygen output in these scenarios and you should feel confident in doing so. If you do not, you should speak with your doctor or other healthcare specialists that you work with closely to ensure you know this protocol.
As we mentioned above, taking too much oxygen or not getting enough, are both harmful practices that will impose harmful side effects on your body.
Do not smoke

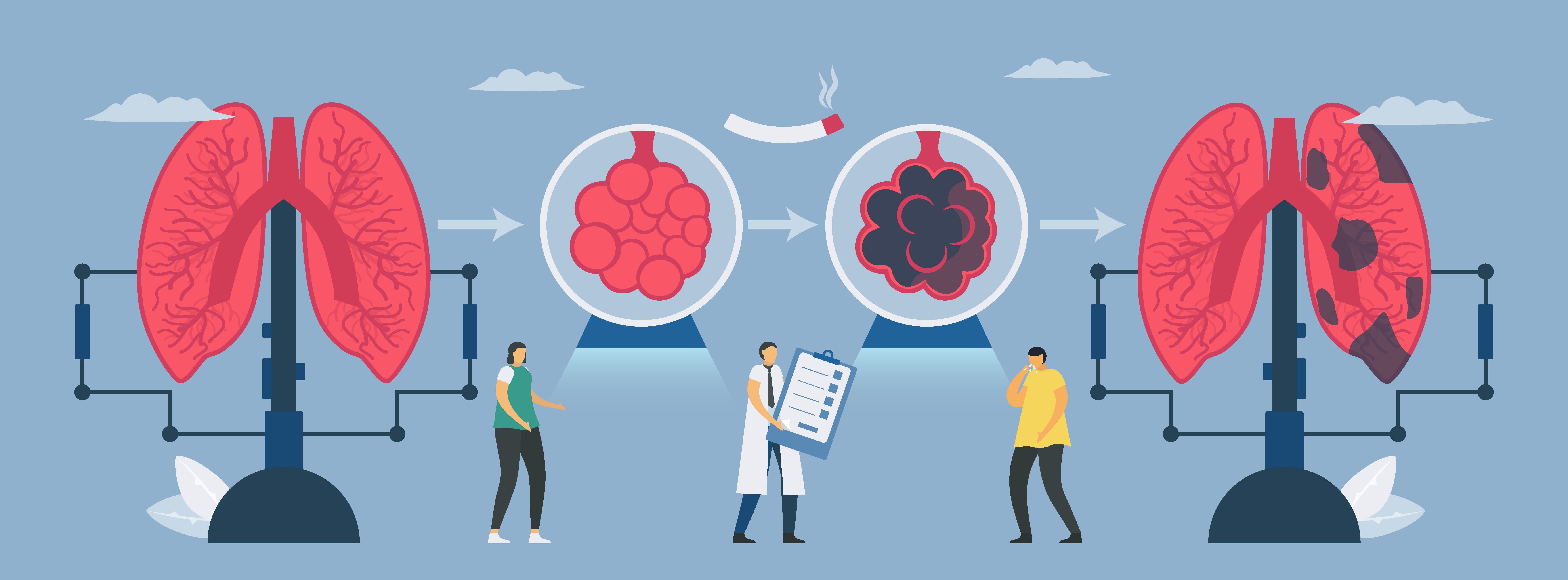
Everyone is going to tell you to quit smoking if you have COPD. While it is too late to reverse your disease, it is not too late to stop it from progressing into a more severe state, and the single most important thing to do is to quit smoking or quit being around smoke.
It is also important to quit smoking if you use supplemental oxygen for a few reasons. The first being that it is unsafe for you and the people in your home and vicinity. Especially if you use oxygen cylinders or liquid tanks, because these methods of oxygen delivery create an oxygen-rich environment. Oxygen is a flammable gas, and a cigarette or a lighter near a flammable gas is just bad news all together.
You should make sure to notify your fire department that you are an oxygen user, and let them know the method of oxygen delivery you use. Confirm that you have a fire extinguisher inside your home, and functioning smoke alarms, all of which are precautionary measures should a fire ever occur.
This is also a great place to note that you should stay at least 10 feet away from open flames, such as a fireplace, gas heater or stove, candles, etc.
Do ask a lot of questions
COPD is confusing! And there is no one right answer for everyone! So ask questions until you are comfortable and confident in all of your endeavors including home oxygen therapy.
Ask your doctor questions about your treatments, medications, and prescriptions. Ask them where you can get involved with a pulmonary rehabilitation course. Ask them to go over your action plan for a COPD exacerbation, and then ask them again. If you have a disease like COPD, you must be in the know at all times, and feel fully confident of what is going on inside your body so you know what to look out for when something changes.
Here is a great resource about communicating with your doctor, and asking the questions you might not even know to ask: COPD Education is Key: 15 Questions you Need to ask your Doctor

When you are shopping for a portable oxygen concentrator, or another form of oxygen therapy, ask your respiratory specialist about the reasons they recommend one portable oxygen concentrator over another.
Why the Caire FreeStyle Comfort fits your friend’s oxygen requirements but you require something more powerful like the Respironics SimplyGo. Ask them questions about traveling with a portable oxygen concentrator compared to oxygen tanks. Ask them how you can charge your portable device’s batteries while you’re at home or in the car.

If you get your oxygen delivered be sure to closely monitor your gauges on your oxygen equipment so you are never running low. Promptly notify your oxygen supplier with plenty of time for them to deliver refills, and upon delivery be sure to ask questions of your oxygen delivery person.
If you're new to oxygen therapy, or are thinking about changing your oxygen method to a more portable system, call us at 1-(800)-946-1201, and we will help you decide on the best portable oxygen concentrator that fits your needs, and also makes your life easier. If you have questions about how much portable oxygen concentrators costs, you will not find the true answer online.
A basic google search will take you to pages that lists these devices anywhere from $2,000 - $3,000, for example the Inogen One G5 is listed on google for almost $3,000. This is because the manufacturers require its distributors to only advertise their devices at set prices, and so the best way to get accurate prices is to call and speak with a respiratory specialist over the phone.
Don’t be careless with storing and transporting your oxygen
If you use an oxygen cylinder or liquid oxygen tanks, you have to store the devices properly. They cannot fall over, and should remain upright and tied into place while being transported.
If you have an oxygen concentrator, you should be careful with the device naturally, but if you are prone to being clumsy or dropping your things, having a durable portable oxygen device should be on your list of priorities.
If you are worried about breaking your portable oxygen device, you might want to consider a device like the SeQual Eclipse 5 which is one of the most, if not the most, popular continuous flow portable oxygen concentrators on the market. That is largely due to its long-standing track record for being durable and reliable as it was intentionally created for the US Military. The hard-bodied shell of the Eclipse 5 is extremely protective. It will keep your concentrator protected from everyday wear and tear, accidental bumps and bruises, and if you have pets or grandkids in the house it will be able to withstand their crazy antics.

The Invacare Platinum Mobile is another durable pulse flow portable oxygen concentrator built for mobility and designed to withstand the trials of everyday life. This concentrator has a rugged design with reinforced bumpers and cushions to protect the unit from daily wear and tear. It contains a foam encapsulated compressor and latch-free doors to absorb shock because sometimes occasional bumps can simply be unavoidable, it is even water resistant!
Don’t run low on oxygen

As we have mentioned in this article, it is critical for you to take your oxygen as prescribed, so running lower on your oxygen supply or running low on the batteries, is not a good practice.
If you use an oxygen canister, or oxygen tanks, always put an order in for your delivery service to have them refilled before you run out.
If you have a portable oxygen concentrator, be sure to keep your device charged, and try to avoid letting the battery die in order to preserve the overall battery life. You can also notify your local utility company and let them know that you have an oxygen concentrator in use, so that you will be given priority during power outages. You may also want to consider buying a backup generator in the event of power outages, so you are still bale to charge your breathing device's batteries.
Do’s and don’ts for using liquid oxygen
Here are some additional factors you should know while using liquid oxygen:
DON'T tip the device or lean it, make sure it is stable and upright at all times, or the liquid can leak out
DO keep the tank at least 5 feet away from space heaters, electric or gas heaters, steam pipes, furnaces, and radiators
Do’s and don’ts for using oxygen concentrators
Here are a few more tips for using an oxygen concentrator:
DON’T ever use an extension cord to plug in your concentrator and do not plug anything else into the same outlet while you are charging your device
DO keep the unit about 6 inches away from the wall curtains or anything else that might obstruct the filter and prevent air circulation around it; this will also help avoid heat build up
DON'T cover the unit with anything like blankets or towels; this will also help avoid heat build up
If you would like more tips and tricks for making supplemental oxygen therapy more enjoyable overall click here to read How to Make Supplemental Oxygen More Comfortable
Overview
Oxygen therapy can be of great benefit to you and you loved ones. It can give you the energy and strength you need to start doing the things you love to do again. With certain oxygen device like portable oxygen concentrators , you can travel by plane, and easily carry with you to run errands or exercise.
All oxygen therapy methods share a similar goal, and that is to get your blood oxygen levels back to a normal rate. If you need your therapy to do even more for you in order to be satisfied, you should talk to you doctor about the possibilities of switching to a portable oxygen concentrator, so you can start getting more than just the essentials from your tanks or canisters.
Until then, we hope that you have found some useful information that you can bring home with you to make the most out of your oxygen therapy and start living the life you want to, whether thats being more active, having more energy, or coping with your COPD more effectively.
%20(1).png)
If you have chronic obstructive pulmonary disease (COPD), cystic fibrosis, or any other debilitating lung condition, you likely depend on a strict treatment regime that encompasses all facets of your life. Typical treatment plans usually involve an improved diet high in protein and fiber, an exercise routine that improves lung strength and endurance, and most importantly oxygen therapy which helps stabilize your lung condition and ensure blood oxygen levels are normal.
One concern many people have with these lifestyle changes is that they make you increasingly dependent on medical devices like your oxygen concentrator, nebulizer, or inhaler. If these devices stop working suddenly, you may be stuck in a situation where you’re unable to get the medication you need. This issue only gets worse as your disease progresses because your doctor may require you to use oxygen for longer periods of time each day.

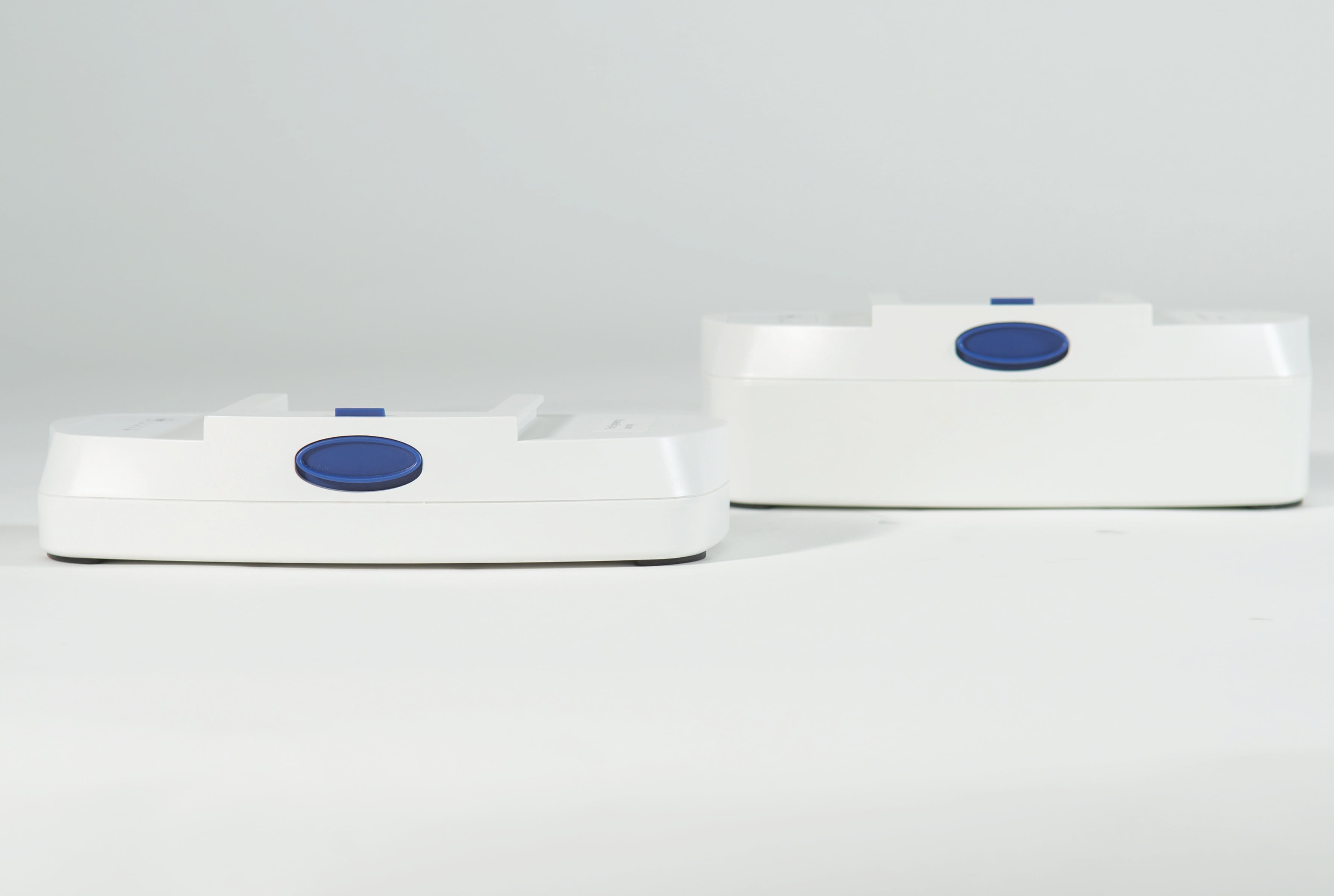
Fortunately, we live in a time of innovation and the medical devices we have access to today are far more reliable than in the past. Portable oxygen concentrators, for example, are battery-operated oxygen machines that are praised for their reliability and long lifespan. Rather than going out of your house each day worrying that you may lose access to your oxygen supply, portable oxygen concentrators allow you to focus on things that are important to you in your day-to-day life.
If security is important to you, stick around because we’re going to take a look at the most reliable portable oxygen concentrators in 2021. Whether you’re a first-time buyer or you’ve owned a POC in the past, you’re sure to find something on this list that suits your lifestyle. If you have any questions, be sure to leave them in the comment section below or reach out to us to speak with a respiratory specialist.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Why Choose a Portable Oxygen Concentrator?
You may be thinking to yourself, “what’s so special about portable oxygen concentrators?” After all, there are plenty of other options available like oxygen tanks, liquid oxygen tanks, and stationary oxygen concentrators. And while these oxygen devices have served their purpose for many decades, they simply can’t compete with the state-of-the-art design of modern portable oxygen machines.

The truth is that oxygen tanks and stationary concentrators have overstayed their welcome in many ways. Oxygen manufacturers have shifted their focus to battery-powered portable oxygen delivery systems because they provide their customers with more freedom and convenience in their daily lives. Rather than being confined to your home with a heavy and bulky oxygen tank, POCs allow you the freedom to live life on your own terms.
At this point in time, portable oxygen concentrators are the only oxygen delivery devices that are approved by the Federal Aviation Administration (FAA) for in-flight use due to safety concerns. What this means is that if you choose to use an oxygen tank or liquid oxygen tank, you’re largely forfeiting your ability to travel long-distance. On top of this, other modes of transportation like driving, walking, or taking the bus will be much more difficult and stressful.
.jpg)
The Caire FreeStyle Comfort
If reliability is important to you, there is no better portable oxygen concentrator out there than the Caire FreeStyle Comfort. In fact, this is one of the only concentrators currently in use by military personnel meaning it’s a trusted product even under the most strenuous of circumstances. The Caire FreeStyle Comfort also sees use in a variety of other industries including space exploration laboratories, hospitals, and in-home use.

While Caire Inc. may not be a household name in the oxygen industry, you may recognize their products under the name AirSep, Helios, and SeQual. The Companion 5, for example, is one of their top stationary oxygen concentrator designs offering economic in-home oxygen delivery and easy-to-use controls. They’ve also produced continuous flow portable oxygen concentrators like the SeQual Eclipse 5 which offers up to 3 liters per minute (LPM) of oxygen and 9 pulse flow settings.
One of the most unique things about the Caire FreeStyle Comfort is its mobile application, CAIREView Telehealth Technology. This app can be downloaded on any phone, tablet, or computer and connect to your Caire FreeStyle Comfort via Bluetooth. It has two primary benefits. First and foremost, it enables you to track all your oxygen usage through a simple-to-use dashboard. It will provide you with information such as hours of use, flow settings used, and alerts.

Secondly, this application allows for periodic monitoring to ensure that patients comply with their oxygen treatment plan. Clinicians will be able to view up-to-date data about your oxygen usage and assist remotely by monitoring your device settings. This feature significantly increases the reliability of your device, because in the rare chance that it stops working or you stop receiving the oxygen you need, your doctor will know about it immediately and he/she will notify you.
Caire FreeStyle Comfort Specs
|
Weight
|
5 pounds
|
|
Flow Rate
|
Pulse 1-5
|
|
Warranty
|
3-year
|
|
Height
|
10 inches
|
|
Width
|
7.3 inches
|
|
Depth
|
3.1 inches
|
|
FAA Approved?
|
Yes
|
|
Battery Duration
|
Up to 16 hours
|
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
The Inogen One G5
Inogen is one of the top pulse dose portable oxygen concentrator manufacturers in the industry. While Inogen has only been around since 2001, they made a name for themselves very quickly. While they started off with stationary oxygen concentrators, they made their way into portable oxygen concentrators with the Inogen One G1. There are currently five generations of Inogen POCs, and their latest, the Inogen One G5, is one of the most advanced on the market.

On most fronts, the G5 is pretty neck-in-neck with the Caire FreeStyle Comfort. They both offer 6 pulse flow settings, they’re both around 5 pounds, and they’re about the same size. However, the Inogen One G5 has a great reputation for having an extremely low failure rate and a long lifespan between 5 and 7 years.
Similar to the Caire FreeStyle Comfort, the G5 is accompanied by a mobile application called Inogen Connect. This app was introduced with the Inogen One G4 and allows you to manage your flow rate and device settings remotely. This is great if you carry your POC on your back and don’t want to take it out all the time to adjust your oxygen settings.
Inogen One G5 Specs
| Weight |
4.7 Pounds |
| Dimensions |
8.15" H x 7.19" L x 3.26" W |
| Flow Settings |
Pulse Settings 1-6 |
| Sound Level |
37 dBA @ Setting 2 |
| Expected Battery Life |
Up to 13 Hours |
.png)
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The Inogen One G3
Although the Inogen One G3 released all the way back in 2012, that hasn’t set it back when it comes to being a dependable portable oxygen concentrator. While the G3 certainly has a little less oxygen output than the Inogen One G5 or the Caire FreeStyle Comfort, it makes up for it with an array of useful accessories that help you customize your oxygen therapy.

One of the most unique accessories for the Inogen One G3 is the GO2 Carryall. This product is designed to look like any ordinary purse or handbag but it holds your G3 snuggly and securely inside. It also comes with both a hand strap and a shoulder strap so you can choose exactly how you want to carry your portable oxygen concentrator.
One thing you’ll notice right away about the GO2 Carryalls is that they’re way more fashionable than any other POC carrying case you’ve seen in the past. They come in either black or brown to match your wardrobe and they’re made of genuine leather so that no one would ever suspect there’s a portable oxygen machine inside. There’s also plenty of room for personal belongings like your car keys, a wallet, or your G3 user manual.

While fashion is important for many people, the most important thing about the GO2 Carryalls is that they protect your Inogen One G3. When your G3 is inside one of these bags, you can rest assured that it will be protected from things like scratches, dents, and even minor water damage. Although the GO2 Carryalls are water-resistant, they are not fully waterproof, so you’ll want to find some cover if you’re getting rained on.
All-in-all, the GO2 Carryalls make the G3 one of the most reliable oxygen concentrators on the market. These bags have a mesh material on the side where the intake vents are located so that your device never overheats or stops working. It also enables you to carry your Inogen One G3 conveniently at your side so that you can keep track of it. However, if the GO2 Carryalls don’t appeal to you, you’ll be happy to know that there are three other carrying options: the G3 custom carrying case, the G3 backpack, and the G3 rolling backpack.
Inogen One G3 Specs
|
Weight |
8-Cell: 4.8 Pounds; 16-Cell: 5.8 Pounds |
|
Dimensions |
7.25” Wide x 3” Deep x 8.75” High |
|
Flow Rate |
Pulse Flow Settings 1-5 |
|
Battery Life |
8-Cell: Up to 4 Hours; 16-Cell: Up to 8.5 Hours |
|
Power |
100-240 VAC, 50/60 Hz; 11-16 VDC |
|
FAA Approved |
Yes |
|
Warranty |
3 Years |
The Respironics SimplyGo
All of the aforementioned machines have been pulse dose portable oxygen concentrators. What this means is that they closely monitor your breathing rate and deliver oxygen only at the peak of your inhalation. The Respironics SimplyGo differs from these in the fact that it also has a continuous flow setting. In other words, it can deliver oxygen indiscriminate from your breathing rate. The Respironics SimplyGo can deliver up to 2 LPM of continuous flow oxygen.

One of the most important things to note about the Respironics SimplyGo is that it is the lightest continuous flow portable oxygen concentrator on the market. Whereas most continuous flow units need to be wheeled around on a carrying cart, the SimplyGo is light enough to carry on your shoulder or your back. This may not seem like a big deal, but for someone who’s been prescribed continuous oxygen, it can be a life-changer.
If you’ve been an oxygen patient for some time, you know that having to wheel around your oxygen concentrator can be a huge pain. Not only do you have to make sure that it’s not bumping into anyone but there’s always a chance of your oxygen tubing getting caught on something and damaging your unit. Walking in a busy area is difficult and it can distract you from what you’re trying to do.
Using the convenient carrying case, you can ensure that you always have a reliable source of oxygen wherever you go. The Respironics SImplyGo was designed for people with the highest oxygen demands so it can run 24/7 without running into any problems. Since it’s a continuous flow POC, it’s perfectly compatible with CPAP, BiPAP, or APAP machines. In other words, it’s one of the most reliable portable oxygen concentrators for people who have both COPD and sleep apnea.
Respironics SimplyGo Specs
|
Weight |
10 Pounds |
|
Dimensions |
10” H x 11.5” W x 6” D |
|
Flow Rate |
Continuous Flow 0.5-2.0 LPM Pulse Flow Settings 1-5 |
|
Battery Life |
Continuous Flow Up To 0.9 Hours Pulse Flow Up To 3.0 Hours |
|
Power |
100-240 VAC, 50/60 Hz; 19 VDC |
|
FAA Approved |
Yes |
|
Warranty |
3 Years |
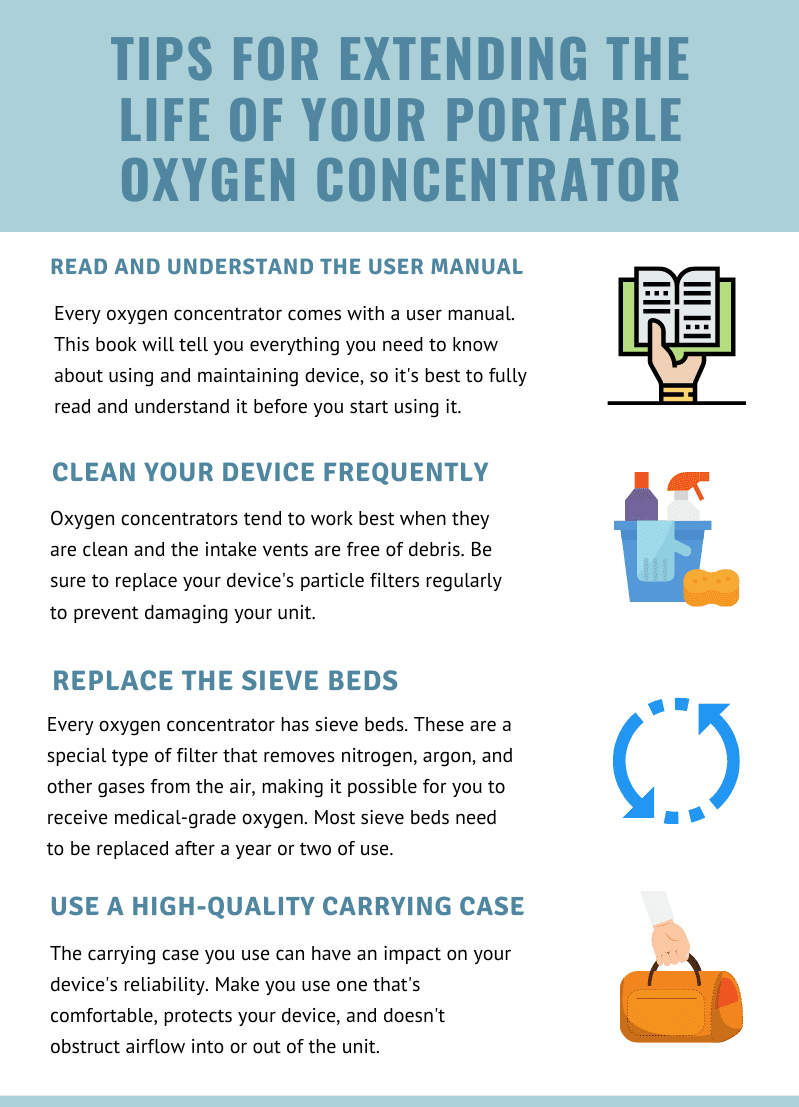
Tips for Extending the Life of Your Portable Oxygen Concentrator
Conclusion
Dependability is one of the most important attributes of portable oxygen concentrators. If you’re looking for a POC, it means you want to be able to get out of the house and enjoy your freedom, so your device needs to be able to match your lifestyle. While there are plenty of great oxygen concentrators out there, the ones above will offer you the reliability you need to live life on your own terms.
If you’re still struggling to find the right portable oxygen concentrator for you, don’t hesitate to reach out to our respiratory specialists here at LPT Medical. We’ll walk you through all your options ensuring that both your oxygen needs are met and you have a unit that will give you the freedom you need to go about your daily life.
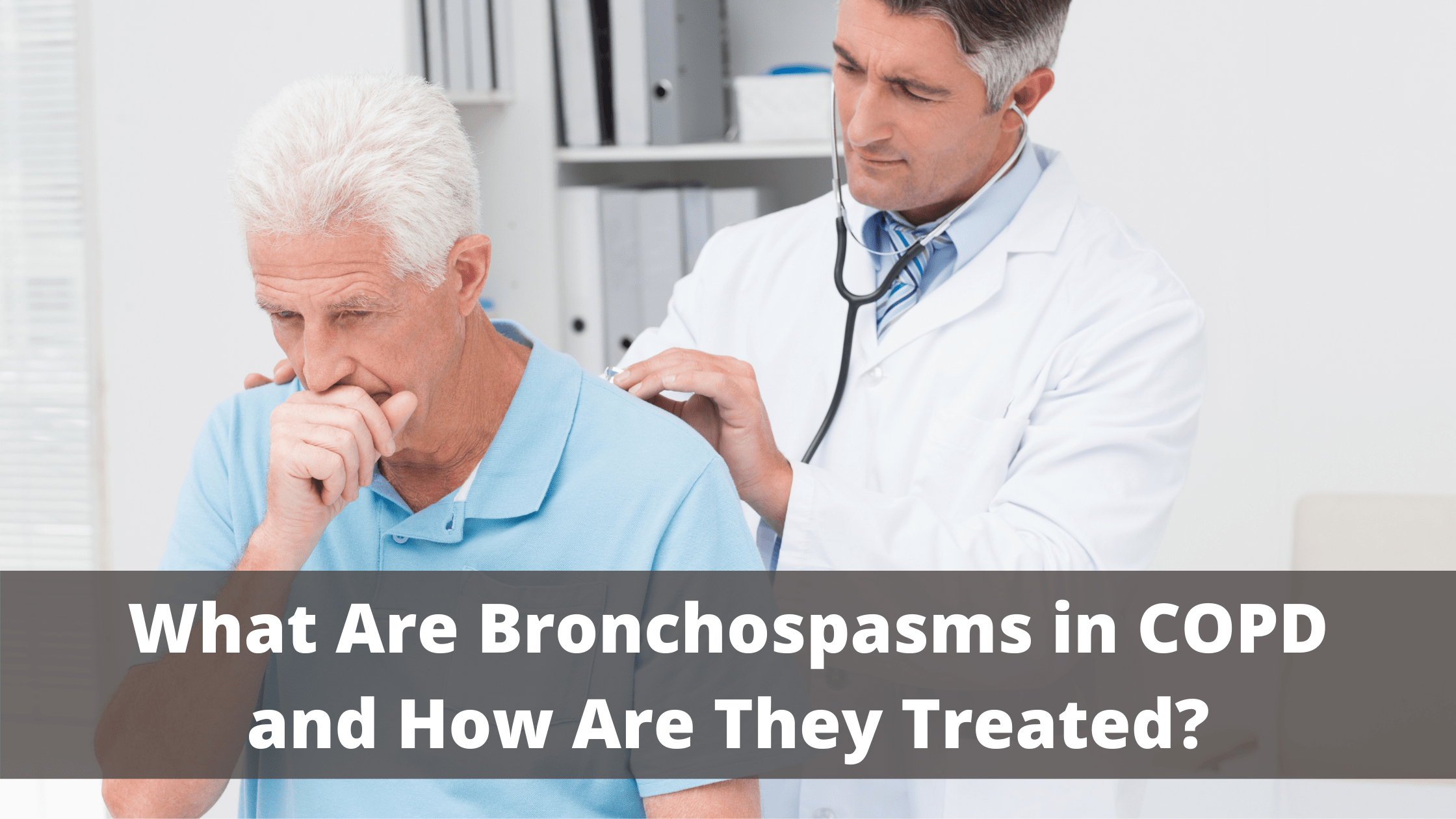
If you’ve just been diagnosed with chronic obstructive pulmonary disease (COPD), you’re probably just beginning to learn about some of the common symptoms associated with this disease. Most people — whether they’re early stage, late stage, or anywhere in between — will experience breathing difficulties, chest pain, and a chronic cough. And as it progresses, COPD patients are more likely to experience complications like hypertension, recurring respiratory infections, and heart problems.
Unfortunately, it’s not always easy to identify the root cause of COPD symptoms. For example, you might wake up one day feeling more chest pain or stiffness than usual. This could be caused by many things such as changes in environmental factors, your diet, exercise routine, or medication. If you experience an unusual or recurring symptom, be sure to take note of it and address it with your doctor during your next appointment.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
One fairly common symptom of COPD you should know about is bronchospasms. This occurs when your airways narrow, leading to difficulty breathing, chest pain, and coughing. If you’d like to learn more about bronchospasms, read on to discover what causes them, how they can affect your respiratory health, and much more. If you have any questions or concerns, don’t hesitate to leave them in the comment section below or reach out to us.
What are Bronchospasms?
Bronchospasms (also called bronchial spasms) result when your airways constrict making it difficult to breathe. As the name suggests, bronchospasms affect the bronchial tubes or the “bronchioles” in the lungs. These tubes are responsible for the transfer of air to and from the lungs. However, when they begin to constrict they don’t allow air to be transferred properly, often causing wheezing and chest pain. The bronchioles contain what’s called “involuntary” smooth muscle fibers. This means that you can’t consciously control these muscle functions similar to how you can’t control when your heart pumps blood.
Your ability to take oxygen-rich air into your lungs and expel carbon dioxide-rich air is imperative for your overall health and well-being. Oxygen that enters the lungs is transferred to the blood through the alveoli, tiny air sacs that scatter the lungs. From there, your blood vessels carry oxygen to every organ in your body. Oxygen is an essential resource for every organ and tissue because it breaks down food so that your body can use it as energy. When tissues or organs don’t have the oxygen they need to function properly, it is called hypoxia.
Not only do bronchospasms block air from coming into the lungs, but they can also block air from going out. This is equally problematic because your lungs need to be able to replace carbon dioxide-rich air with oxygen-rich air, otherwise carbon dioxide will begin to build up in the blood. Too much carbon dioxide in the blood is called hypercapnia and it can result in many of the same symptoms as a lack of oxygen like shortness of breath, fatigue, and dizziness.

Bronchospasms primarily occur in patients with chronic bronchitis or asthma. Chronic bronchitis is one of two chronic respiratory diseases under the umbrella term “COPD.” The other being emphysema which affects the alveoli in the lungs. While chronic bronchitis and asthma share many symptoms such as wheezing, shortness of breath, and chest tightness, they have different causes. Chronic bronchitis is primarily caused by cigarette smoking and asthma is mostly hereditary. Bronchospasms can also be induced by anaphylaxis (a severe allergic reaction) or exercise.
What Causes Bronchospasms?
There are many different causes of bronchospasms so it will be challenging to narrow down what’s causing your symptoms without speaking with your doctor. There may be one specific thing that’s causing your bronchospasms or there could be multiple things involved. Let’s take a look at some of the potential causes of these symptoms.
Air Pollution
Pollutants are one of the most common and avoidable causes of bronchospasms. According to the Centers for Disease Control and Prevention (CDC), there are six criteria of air pollutants including particle pollution, sulfur oxides, ground-level ozone, nitrogen oxides, lead, and carbon monoxide. All of these types of pollution can lead to respiratory exacerbations including bronchospasms, chest pain, coughing, and wheezing.
![]()
The best way to avoid hazardous air pollution is by checking the air quality in your area before you go outdoors. AirNow.gov is an excellent resource for asthma and COPD patients who want to be more conscious about the quality of air they’re breathing. Simply type in your area code or city and you will be provided with a forecast of the air quality in your area. It will specify the types of pollutants that are currently present so you can plan your day accordingly.
.jpg)
Air quality index (AQI) is the unit of measurement for air quality. It runs from 0 to 500 with 0 being the best air quality and 500 being the worst. Generally speaking, COPD and asthma patients should not go outside if the AQI is above 100.
Airborne Allergens
An allergen is a type of antigen that causes a severe immune response to something that would normally be harmless. Allergens can be airborne such as pollen or mold, or they can be food-based such as nuts, shellfish, or soy. If you have COPD or asthma, avoiding these triggers is imperative if you want to avoid bronchospasms and other potentially life-threatening symptoms.

There are many sites that can keep you up to date on the active allergens in your area, but Pollen.com is probably one of the most accurate and easy to use. Just like AirNow.gov, you simply have to type in your area code and you’ll have access to current information about the allergens that you should be concerned about. This is a great resource if you want to figure out what allergens affect you the most and how to avoid them.
Infections
COPD and asthma patients can have what’s called a disruption to the epithelial lining which makes them more likely to contract infections like the flu or COVID-19. Essentially, many of the immune cells in the throat and lungs become compromised due to chronic inflammation. Over time, the body loses its ability to fight off bacteria or viruses that enter the body.
Bronchiectasis is another condition that can lead to infections in COPD patients. While bronchiectasis is not caused by COPD, it is more common among COPD patients, especially in later stages of the disease. Bronchiectasis causes mucus and bacteria to build up in the lungs and prevents it from clearing properly meaning you’ll experience frequent and recurring lung infections.

Lastly, cigarette smoking will put you at a greater risk of contracting a lung infection. While many COPD patients are able to quick smoking after receiving a diagnosis, as many as 38 percent of COPD patients continue smoking. Smoking suppresses the immune system making you more likely to get sick and even causing infections to be more severe and longer-lasting. Immediate smoking cessation will help you prevent lung infection and stay healthy.
Medication
The use of certain medications can result in drug-induced bronchospasms. A few of them in particular, such as non-steroidal anti-inflammatory drugs (NSAIDs) are very well-known and widely used. For example, ibuprofen and aspirin are both NSAIDs.These drugs are used as painkillers to treat things like headaches, toothaches, and soreness. However, for some people with asthma, they can cause bronchospasms.

According to Healthline, NSAIDs inhibit a protein called cyclooxygenase and many asthma patients are sensitive to these effects. One possible reason for this is due to the overproduction of leukotrienes. These are chemicals that are released into the bronchial tubes and cause the bronchial muscles to constrict and spasm. To be safe, it’s best to consult with your doctor before using any type of medication, even if it is an over-the-counter medication.
How are Bronchospasms Diagnosed?
Your doctor may use a number of different methods to diagnose you with bronchospasms depending on your medical history and whether or not you’ve already been diagnosed with asthma or COPD. He/she will likely start by using a stethoscope to listen for any irregularities in your breathing. And if any are detected, you may be administered one of the following tests to determine if you have bronchospasms.
Spirometry
During a spirometry test, you will be blowing into a device called a spirometer. There are two different readings that your doctor will derive from this: forced vital capacity (FVC) which is the total amount of air you can exhale and forced expiratory volume in one second (FEV1) which is the total volume of air you can push out of your lungs in one second.

Pulse Oximetry
If you have COPD and you’re on oxygen, you likely already know what a pulse oximeter is. It’s a small device that attaches to your finger and reads your blood oxygen level. Your doctor may use one of these devices to see if your bronchospasms are reducing the amount of oxygen that is making it into your blood.

Arterial Blood Gas Analysis
Arterial blood gas tests are similar to pulse oximetry but they are more invasive by requiring you to draw blood. They also provide your doctor with a lot more information about your blood composition which can assist in diagnosing bronchospasms and other respiratory problems.
Eucapnic Voluntary Hyperventilation (EVH) Test
This is a type of test that attempts to simulate the effects of prolonged exercise. In other words, it allows your doctor to understand how your lungs and airways react when you are at a point of physical exertion. This test can take between 60 and 90 minutes to complete but it can be convenient in diagnosing bronchial spasms.
How Are Bronchospasms Treated?
Bronchospasms can be treated with a combination of home remedies and treatment methods prescribed by your doctor. Below are just a few of the ways your doctor may treat these respiratory symptoms.
Short-Acting Bronchodilators
Short-acting bronchodilators are used in asthma and COPD patients to provide quick relief from respiratory symptoms. They work by opening up the airways when you’re faced with severe breathing problems, chest pain, or coughing. Short-acting bronchodilators are taken with either an inhaler or a nebulizer so that the medication reaches the lungs faster.

Long-Acting Bronchodilators
If your bronchospasms are less severe, your doctor may prescribe you long-acting bronchodilators. These medications will take much longer to start working but they will also provide a much longer period of relief. Long-acting bronchodilators are typically administered orally.

Corticosteroids
If your bronchospasms were induced by an allergic reaction, your doctor may advise corticosteroids. These types of steroids will reduce inflammation in the airways and suppress the immune system which could be causing them to constrict. He/she may use any combination of the above treatment options to help you cure your bronchospasms.
What Can Be Done to Prevent Bronchospasms?
Since bronchospasms put you at a higher risk of experiencing severe complications from COPD, it’s important to do what you can to prevent them. For most people, preventing bronchospasms simply means following the treatment plan that your doctor has already created for you. If you believe that you aren’t doing enough to prevent them, consult with your doctor for more information.
Oxygen Therapy
Supplemental oxygen therapy is one of the foundational treatments for COPD and it can also help you prevent bronchospasms. The goal of oxygen therapy is to maintain a healthy blood oxygen level in your body when your lungs aren’t able to do so on their own. For some patients, this could mean using oxygen intermittently, but for others, it could mean using oxygen 24/7. Your doctor will help you decide what’s best for you.
.png)
We recommend using a portable oxygen concentrator such as the Caire FreeStyle Comfort or the Inogen One G5 because these units are lightweight and allow you to take your oxygen supply anywhere in the world with ease. They’re also extremely reliable, so you don’t have to worry about losing access to your oxygen when you need it the most.
Exercising Safely
Exercise is a fundamental aspect of any COPD treatment routine. Pulmonary rehabilitation (PR) is used to increase the strength and efficiency of the lungs while helping COPD patients maintain their weight and promote healthy circulation. However, if you exercise too much or you don’t exercise in a way that’s advised by your doctor, you might experience exercise-induced bronchospasms (EIB).

To avoid exercise-induced bronchospasms, be sure to avoid exercising in the cold. Cold, dry air can cause your mucus to become thick and difficult to clear. Air that’s filled with pollen or other allergens can also irritate your airways causing bronchospasms. Lastly, you should be careful not to overexercise. High-intensity exercise is not typically recommended for treating COPD and it can put you at a higher risk for experiencing exacerbations or other serious complications. Stick to a moderate, but consistent exercise routine.
Diet
Your dietary habits can make the difference between a healthy and unhealthy respiratory system. As aforementioned, consuming food that you’re allergic to can exacerbate your respiratory symptoms and cause bronchospasms. COPD patients tend to retain sodium, so you should avoid food with added salt and drink plenty of water. Being well-hydrated means your mucus will be less viscous and easier to clear from your airways. Foods to avoid include coffee, sugary drinks, fried foods, and milk.

Another thing to be wary of is dietary supplements. While dietary supplements are often hyped-up through advertising and word of mouth, they have negative side-effects just like over-the-counter and prescription drugs. The problem is that dietary supplements are registered as “food products” through the Food and Drug Administration (FDA) so companies can often get away with overexaggerating the benefits of their supplements without discussing the potential side-effects.
Conclusion
Bronchospasms are a common symptom of COPD and asthma, but under certain circumstances, they can also occur in healthy people. Severe allergic reactions, air pollution, and medications can all cause bronchospasms and they can range in severity from moderate to life-threatening. While there are several home remedies that can help alleviate the symptoms of bronchospasms, your best bet will be to speak with your doctor as soon as possible.
In the meantime, your best course of action is to follow your COPD treatment plan. Using supplemental oxygen as prescribed, following a strict diet, and maintaining a healthy and consistent exercise routine will all promote healthy lungs and airways, thus helping you to prevent bronchospasms and other respiratory complications. You should also take the time to check the air quality in your area before going outside so that you can avoid air pollution.
Here at LPT Medical, our goal is to provide as many COPD patients as possible with durable and reliable portable oxygen concentrators. With a portable oxygen concentrator at your side, you’ll have the freedom to go about your daily life without having to worry about not having medical oxygen that meets your respiratory needs. If you need help choosing an oxygen concentrator, please feel free to give us a call at 1-888-416-3855.
.png)
Most people don’t put a lot of thought into the way that they get around. As humans, we learn to walk from a very young age and we use our basic motor skills all the time. So, for most people, it’s difficult to imagine being in a situation where these basic functions are impaired. However, for someone with COPD, problems with mobility, balance, and coordination can be a daily struggle. Healthy, functioning lungs are essential for physical exertion, no matter how little it may be.
A study on pubmed.gov followed COPD patients over the course of six months and found that about one-third of them experienced a fall at some point. The same study also states that COPD is one of the chronic conditions with the highest fall rates, right behind osteoarthritis, a very common degenerative joint disease that’s caused by the wearing down of cartilage on the bones.
Unfortunately, the high risk of falls in COPD patients is very much an under-discussed topic. That’s why, in this article, we’ll take a look at the main causes of falls and how you can avoid them. If you have any questions, please feel free to leave them in the comment section below and we’ll get back to you as soon as possible.
What Causes Balance Issues in COPD Patients?
COPD balance and coordination issues aren’t limited to one cause. There are many different factors that need to be considered in order to pinpoint and mitigate your risk of experiencing a fall. Comorbidities, age, COPD stage, and environmental factors can all play a role, so it’s important to be open-minded about possible prevention methods.
Low Blood Oxygen Levels
Oxygen is a vital resource for your body. It’s used to break down stored energy that you get from food and convert it into usable energy for every cell in your body. Since COPD patients have impaired lung function due to excessive inflammation, medical oxygen can be used to lessen the load on the lungs and ensure that your blood oxygen levels stay within a normal range. Contrary to what many people believe, there are no “side-effects” of medical oxygen. As long as you’re using it as prescribed, medical oxygen will only benefit you.

When it comes time to buy an oxygen device, you’ll have several options. Oxygen tanks, liquid oxygen tanks, and oxygen concentrators are all popular options. However, portable oxygen concentrators will be the best option for most oxygen patients because they’re lightweight, small, and easy to carry as you go about your day. The Inogen One G5 and Caire FreeStyle Comfort, for example, are two of the most popular options because they have a high oxygen output, and they both weigh under 5 pounds.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Another great option if you have higher oxygen demands is the Respironics SimplyGo. This is the lightest continuous flow portable oxygen concentrator and it offers up to 2 liters per minute (LPM) of oxygen. The Respironics SimplyGo can either be carried on your shoulder with the adjustable strap, or it can be wheeled behind you using the rolling cart. Be sure to speak with one of our respiratory specialists here at LPT Medical to learn which portable oxygen concentrator is right for you.
Peripheral Edema
"Edema” is a term that refers to swelling, usually due to the buildup of fluid. Peripheral edema occurs when fluid begins to accumulate in an extremity away from the heart such as the hands, feet, or legs. While this condition can happen to anyone, it’s more common among COPD patients and it can be a warning sign of several serious medical conditions including pulmonary hypertension (high blood pressure in the lungs) and cor pulmonale (right-sided heart failure).

Another problem that can be caused by edema is problems with balance and coordination. This condition often develops slowly and without the patient knowing, so you might start losing control of your balance without knowing it as well. Oftentimes, people first notice that there’s a problem when their shoes or clothing don’t fit anymore. In order to avoid this situation, check your legs and feet daily for swelling, redness, or pitting. This is when you press your skin and it leaves an indentation.
Malnutrition
COPD patients are more likely to experience malnutrition than the general public. There are many possible reasons for this, but a loss of appetite, changing food preferences, and problems with digestion are among the most common causes. COPD patients often find themselves in a difficult situation where they’re hungry but aren’t in the mood to eat because it can leave them feeling bloated and exhausted.

One significant concern is something called muscle atrophy (muscle wasting). Many people are under the impression that they’re losing fat, but it’s actually muscle weight that they’re losing. Inevitably, this can lead to problems with balance, coordination, and exercise tolerance. This is why it’s so important for COPD patients to consume enough protein. Today’s Dietician recommends you get at least 20 percent of your calories from protein.
Medication Side-Effects
Every medication has side-effects, including those used to treat COPD. One of the most common inhaled COPD medications, bronchodilators, are used to open up the airways helping you to breathe easier. However, bronchodilators have a number of adverse side-effects including but not limited to trembling, muscle cramps, and nausea, all of which can contribute to balance problems and even result in serious falls.

Just like with oxygen, it’s important to use medication only as it’s prescribed by your doctor. What’s more, you should be cautious about the way you use it. For example, if you’re using a bronchodilator, try sitting down beforehand. This way, if you start feeling dizzy or lightheaded, you won’t run the risk of falling down. Bronchodilators are fast-acting, so if you feel okay after a couple of minutes, you can stand up and go about your business.

Corticosteroids are another popular medication used to treat COPD. These are a type of steroid that is used for the long-term treatment of COPD and asthma, and they help to reduce inflammation and tightening in the airways and lungs. However, corticosteroids used in large doses can contribute to bone deterioration and the development of osteoporosis. This condition not only increases your risk of falls, but it also increases your risk of experiencing bone fractures after falling.
Sedentary Lifestyle
Living a “sedentary lifestyle” means not getting up and moving around very often. Many people become more sedentary the older they get and developing a chronic condition like COPD can cause someone to become sedentary as well. The problem with this is that it can lead to a lot of health issues, one of which is an increased likelihood of experiencing a fall. This study found that physical activity is associated with better balance and slowing the rate of physical deterioration in older adults.
Environmental Factors
All of the issues above are caused by the symptoms of COPD and COPD treatment. But you also need to consider how your environment is contributing to your risk of falls. Living in a home that is cluttered or not designed to accommodate someone with a chronic respiratory disease can put you at a higher risk of falling.

Since it’s winter, there are also environmental factors related to the weather. According to the World Health Organization (WHO), 56 percent of all falls occur outside the home such as in the yard, on the sidewalk, or in a public area. So before you go anywhere, you should consider what obstacles will be presented and how you can navigate them safely without experiencing a fall.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
What Can Be Done to Prevent Falls With COPD?
Although falls are very common in COPD patients, the good news is that they’re highly preventable. Just a few small adjustments to your lifestyle could make a huge difference but you need to know what’s causing them in the first place.
Carry a Pulse Oximeter
A pulse oximeter is a small electronic device that slips over your finger and tells you your blood oxygen levels. It is a non-invasive device, meaning you won’t need to draw blood in order to use it. It works by passing light through your finger and calculating your blood oxygen levels based on the amount of light that’s absorbed by oxygenated or deoxygenated blood. Pulse oximeters are lightweight and portable medical devices.

The reason it’s so important to have a pulse oximeter is to be able to check your blood oxygen levels and heart rate, especially when you’re away from home. Just a quick pulse oximeter reading and you’ll know exactly what adjustments you need to make to your oxygen therapy device. Pulse oximeters are usually recommended over arterial blood gas analysis (ABG) because they’re less intrusive and you receive your results almost instantaneously. The quality of the device matters too, so be sure to spend some time looking for a pulse oximeter with good reviews.
ABG analysis and pulse oximetry also differ in terms of the information they provide. While a pulse oximeter just reads the percentage of hemoglobin in the blood that is saturated with oxygen (SpO2), ABG tests will provide you with a whole host of information including blood alkalinity, the partial pressure of CO2 and oxygen (PaCO2 and PaO2), and much more. This information is useful for other reasons, but it’s not necessary if you’re just trying to maintain your blood oxygen levels.
Carry a Medical Alert System
A medical alert system or personal emergency response system (PERS) is a small device that’s worn around your neck or on your wrist. If you ever experience an emergency like a fall or a COPD exacerbation, simply press the button on the device and a notification will be sent to a 24/7 call center. Once the notification is received they will call 911 and emergency medical personnel will be sent to your home immediately.

Adjust Your Eating Habits
As aforementioned, many COPD patients are underweight. As respiratory symptoms get worse, many people find it difficult to eat a full meal without feeling bloated and tired. One of the best ways to deal with this is to spread your meals throughout the day rather than having one or two bigger meals. This will give your body lots of time to digest rather than having to do it all at once.
![]()
Another reason to spread your meals out is that it helps you avoid the temptation to eat unhealthy foods. When you’re feeling hungry and lacking energy, you’re more likely to give in to foods that will provide you with a quick energy boost. These foods are usually high in sugar and other unhealthy ingredients which can exacerbate COPD symptoms and leave you feeling drained.
Get Active
Many people are under the impression that the sole purpose of pulmonary rehabilitation is to improve lung function. And while that may be the most important reason, it’s not the only reason. Even a moderate form of exercise can provide some major benefits as long as it’s done consistently. According to the Mayo Clinic, regular exercise helps prevent a whole host of health problems, including but not limited to high blood pressure, type 2 diabetes, depression, and heart disease.

Another reason for COPD patients to exercise is that it increases their muscle tone, thus increasing their oxygen efficiency. As a COPD patient, you want every muscle in your body to be strong not only to improve balance and posture but to reduce the amount of oxygen required for getting around. Exercise also improves blood circulation which is very important for maintaining your mobility.
Create a Safe Living Space
No matter whether you live alone or with friends or family, making adjustments to your living space can go a long way towards preventing falls. Keeping your home organized and free of debris will give you fewer obstacles to trip over or navigate around as you go about your daily life. Many falls occur in the bathroom, so that might be the best place to start with. Another way to create a safe living space is to install mobility aids such as hand railings, stairlifts, or ramps.

Address Your Concerns With Your Doctor
Anxiety is associated with an increased risk of falls, so if you have concerns about balance or coordination issues caused by COPD or your COPD treatment plan, you should address them with your doctor immediately. Chances are, the feelings you’re experiencing are perfectly normal and your doctor might be able to make changes to your medication, exercise, or diet plan in order to improve your balance. As the saying goes, there’s no such thing as a “stupid question” especially when your health is concerned.

Conclusion
Although COPD is a leading morbidity in the United States, many people are not fully aware of what it’s like to live with this disease. Balance and coordination issues are pervasive among COPD patients and they become more prevalent with age and as the disease progresses. The tips outlined above will help you mitigate the risks of falls.
Here at LPT medical, we want you to be educated about your disease so that you can make the best decisions for your long-term health. We carry a wide range of portable oxygen concentrators from popular brands like Caire Inc., Inogen, and Respironics. And we take pride in providing oxygen patients all over the country with reliable lightweight devices that help them get around more easily while limiting the risk of a fall.
If you’re interested in our portable oxygen concentrators for sale, please reach out to us either by phone or by email.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!
















