If you’ve just been diagnosed with chronic obstructive pulmonary disease (COPD), you’re probably just beginning to learn about some of the common symptoms associated with this disease. Most people — whether they’re early stage, late stage, or anywhere in between — will experience breathing difficulties, chest pain, and a chronic cough. And as it progresses, COPD patients are more likely to experience complications like hypertension, recurring respiratory infections, and heart problems.
Unfortunately, it’s not always easy to identify the root cause of COPD symptoms. For example, you might wake up one day feeling more chest pain or stiffness than usual. This could be caused by many things such as changes in environmental factors, your diet, exercise routine, or medication. If you experience an unusual or recurring symptom, be sure to take note of it and address it with your doctor during your next appointment.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
One fairly common symptom of COPD you should know about is bronchospasms. This occurs when your airways narrow, leading to difficulty breathing, chest pain, and coughing. If you’d like to learn more about bronchospasms, read on to discover what causes them, how they can affect your respiratory health, and much more. If you have any questions or concerns, don’t hesitate to leave them in the comment section below or reach out to us.
What are Bronchospasms?
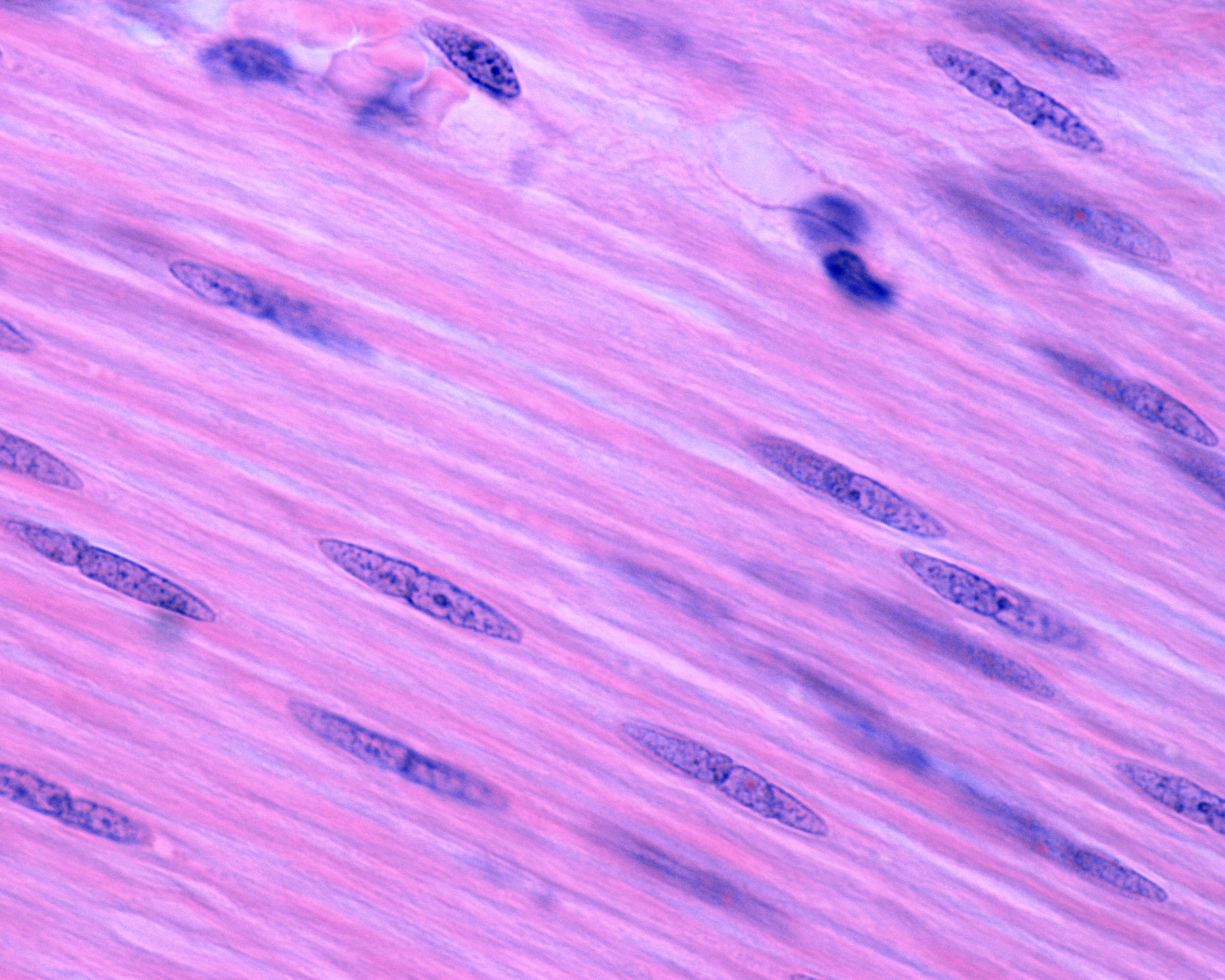
Bronchospasms (also called bronchial spasms) result when your airways constrict making it difficult to breathe. As the name suggests, bronchospasms affect the bronchial tubes or the “bronchioles” in the lungs. These tubes are responsible for the transfer of air to and from the lungs. However, when they begin to constrict they don’t allow air to be transferred properly, often causing wheezing and chest pain. The bronchioles contain what’s called “involuntary” smooth muscle fibers. This means that you can’t consciously control these muscle functions similar to how you can’t control when your heart pumps blood.
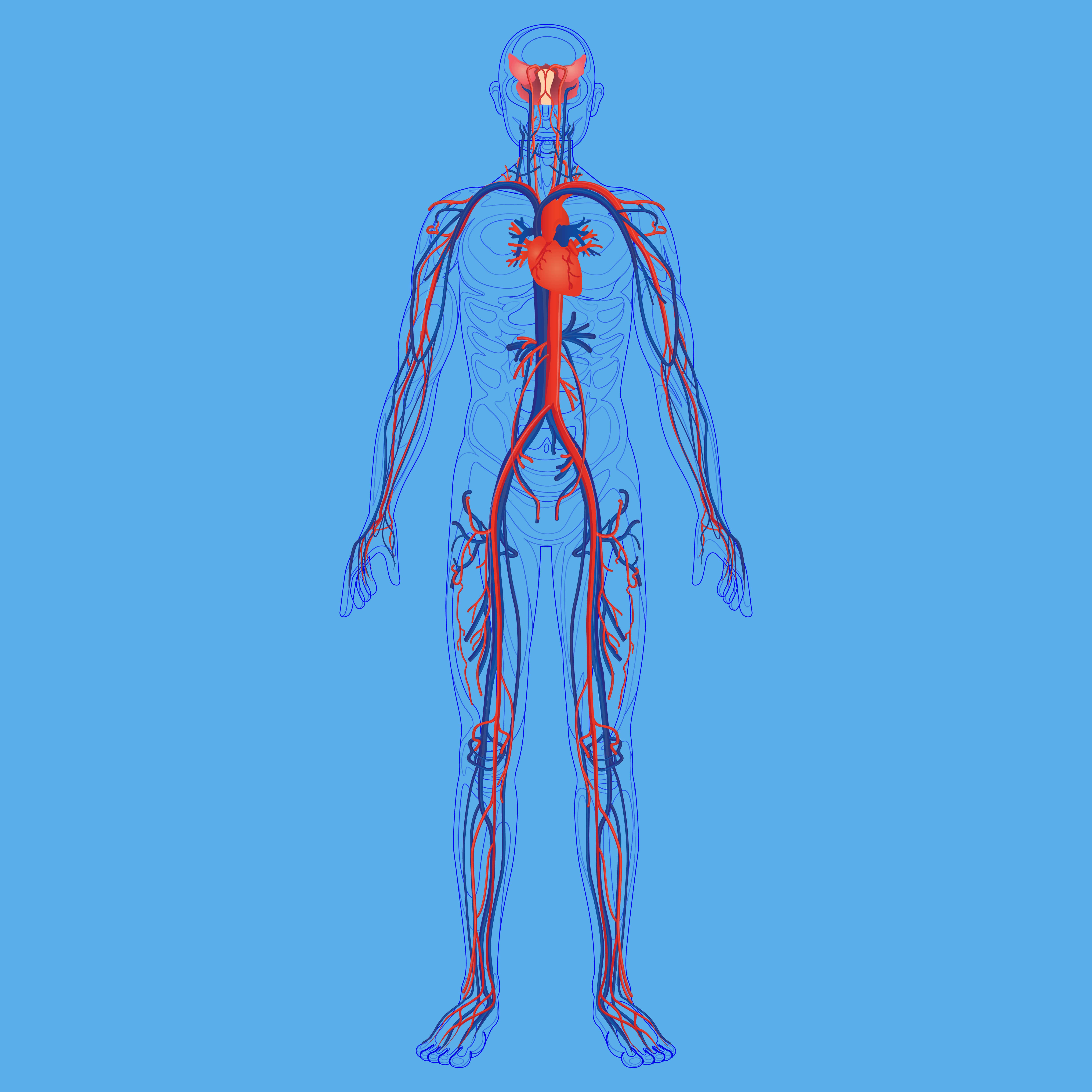
Your ability to take oxygen-rich air into your lungs and expel carbon dioxide-rich air is imperative for your overall health and well-being. Oxygen that enters the lungs is transferred to the blood through the alveoli, tiny air sacs that scatter the lungs. From there, your blood vessels carry oxygen to every organ in your body. Oxygen is an essential resource for every organ and tissue because it breaks down food so that your body can use it as energy. When tissues or organs don’t have the oxygen they need to function properly, it is called hypoxia.
Not only do bronchospasms block air from coming into the lungs, but they can also block air from going out. This is equally problematic because your lungs need to be able to replace carbon dioxide-rich air with oxygen-rich air, otherwise carbon dioxide will begin to build up in the blood. Too much carbon dioxide in the blood is called hypercapnia and it can result in many of the same symptoms as a lack of oxygen like shortness of breath, fatigue, and dizziness.

Bronchospasms primarily occur in patients with chronic bronchitis or asthma. Chronic bronchitis is one of two chronic respiratory diseases under the umbrella term “COPD.” The other being emphysema which affects the alveoli in the lungs. While chronic bronchitis and asthma share many symptoms such as wheezing, shortness of breath, and chest tightness, they have different causes. Chronic bronchitis is primarily caused by cigarette smoking and asthma is mostly hereditary. Bronchospasms can also be induced by anaphylaxis (a severe allergic reaction) or exercise.
What Causes Bronchospasms?
There are many different causes of bronchospasms so it will be challenging to narrow down what’s causing your symptoms without speaking with your doctor. There may be one specific thing that’s causing your bronchospasms or there could be multiple things involved. Let’s take a look at some of the potential causes of these symptoms.
Air Pollution
Pollutants are one of the most common and avoidable causes of bronchospasms. According to the Centers for Disease Control and Prevention (CDC), there are six criteria of air pollutants including particle pollution, sulfur oxides, ground-level ozone, nitrogen oxides, lead, and carbon monoxide. All of these types of pollution can lead to respiratory exacerbations including bronchospasms, chest pain, coughing, and wheezing.
![]()
The best way to avoid hazardous air pollution is by checking the air quality in your area before you go outdoors. AirNow.gov is an excellent resource for asthma and COPD patients who want to be more conscious about the quality of air they’re breathing. Simply type in your area code or city and you will be provided with a forecast of the air quality in your area. It will specify the types of pollutants that are currently present so you can plan your day accordingly.
.jpg)
Air quality index (AQI) is the unit of measurement for air quality. It runs from 0 to 500 with 0 being the best air quality and 500 being the worst. Generally speaking, COPD and asthma patients should not go outside if the AQI is above 100.
Airborne Allergens
An allergen is a type of antigen that causes a severe immune response to something that would normally be harmless. Allergens can be airborne such as pollen or mold, or they can be food-based such as nuts, shellfish, or soy. If you have COPD or asthma, avoiding these triggers is imperative if you want to avoid bronchospasms and other potentially life-threatening symptoms.

There are many sites that can keep you up to date on the active allergens in your area, but Pollen.com is probably one of the most accurate and easy to use. Just like AirNow.gov, you simply have to type in your area code and you’ll have access to current information about the allergens that you should be concerned about. This is a great resource if you want to figure out what allergens affect you the most and how to avoid them.
Infections
COPD and asthma patients can have what’s called a disruption to the epithelial lining which makes them more likely to contract infections like the flu or COVID-19. Essentially, many of the immune cells in the throat and lungs become compromised due to chronic inflammation. Over time, the body loses its ability to fight off bacteria or viruses that enter the body.
Bronchiectasis is another condition that can lead to infections in COPD patients. While bronchiectasis is not caused by COPD, it is more common among COPD patients, especially in later stages of the disease. Bronchiectasis causes mucus and bacteria to build up in the lungs and prevents it from clearing properly meaning you’ll experience frequent and recurring lung infections.

Lastly, cigarette smoking will put you at a greater risk of contracting a lung infection. While many COPD patients are able to quick smoking after receiving a diagnosis, as many as 38 percent of COPD patients continue smoking. Smoking suppresses the immune system making you more likely to get sick and even causing infections to be more severe and longer-lasting. Immediate smoking cessation will help you prevent lung infection and stay healthy.
Medication
The use of certain medications can result in drug-induced bronchospasms. A few of them in particular, such as non-steroidal anti-inflammatory drugs (NSAIDs) are very well-known and widely used. For example, ibuprofen and aspirin are both NSAIDs.These drugs are used as painkillers to treat things like headaches, toothaches, and soreness. However, for some people with asthma, they can cause bronchospasms.

According to Healthline, NSAIDs inhibit a protein called cyclooxygenase and many asthma patients are sensitive to these effects. One possible reason for this is due to the overproduction of leukotrienes. These are chemicals that are released into the bronchial tubes and cause the bronchial muscles to constrict and spasm. To be safe, it’s best to consult with your doctor before using any type of medication, even if it is an over-the-counter medication.
How are Bronchospasms Diagnosed?
Your doctor may use a number of different methods to diagnose you with bronchospasms depending on your medical history and whether or not you’ve already been diagnosed with asthma or COPD. He/she will likely start by using a stethoscope to listen for any irregularities in your breathing. And if any are detected, you may be administered one of the following tests to determine if you have bronchospasms.
Spirometry
During a spirometry test, you will be blowing into a device called a spirometer. There are two different readings that your doctor will derive from this: forced vital capacity (FVC) which is the total amount of air you can exhale and forced expiratory volume in one second (FEV1) which is the total volume of air you can push out of your lungs in one second.

Pulse Oximetry
If you have COPD and you’re on oxygen, you likely already know what a pulse oximeter is. It’s a small device that attaches to your finger and reads your blood oxygen level. Your doctor may use one of these devices to see if your bronchospasms are reducing the amount of oxygen that is making it into your blood.

Arterial Blood Gas Analysis
Arterial blood gas tests are similar to pulse oximetry but they are more invasive by requiring you to draw blood. They also provide your doctor with a lot more information about your blood composition which can assist in diagnosing bronchospasms and other respiratory problems.
Eucapnic Voluntary Hyperventilation (EVH) Test
This is a type of test that attempts to simulate the effects of prolonged exercise. In other words, it allows your doctor to understand how your lungs and airways react when you are at a point of physical exertion. This test can take between 60 and 90 minutes to complete but it can be convenient in diagnosing bronchial spasms.
How Are Bronchospasms Treated?
Bronchospasms can be treated with a combination of home remedies and treatment methods prescribed by your doctor. Below are just a few of the ways your doctor may treat these respiratory symptoms.
Short-Acting Bronchodilators
Short-acting bronchodilators are used in asthma and COPD patients to provide quick relief from respiratory symptoms. They work by opening up the airways when you’re faced with severe breathing problems, chest pain, or coughing. Short-acting bronchodilators are taken with either an inhaler or a nebulizer so that the medication reaches the lungs faster.

Long-Acting Bronchodilators
If your bronchospasms are less severe, your doctor may prescribe you long-acting bronchodilators. These medications will take much longer to start working but they will also provide a much longer period of relief. Long-acting bronchodilators are typically administered orally.

Corticosteroids
If your bronchospasms were induced by an allergic reaction, your doctor may advise corticosteroids. These types of steroids will reduce inflammation in the airways and suppress the immune system which could be causing them to constrict. He/she may use any combination of the above treatment options to help you cure your bronchospasms.
What Can Be Done to Prevent Bronchospasms?
Since bronchospasms put you at a higher risk of experiencing severe complications from COPD, it’s important to do what you can to prevent them. For most people, preventing bronchospasms simply means following the treatment plan that your doctor has already created for you. If you believe that you aren’t doing enough to prevent them, consult with your doctor for more information.
Oxygen Therapy
Supplemental oxygen therapy is one of the foundational treatments for COPD and it can also help you prevent bronchospasms. The goal of oxygen therapy is to maintain a healthy blood oxygen level in your body when your lungs aren’t able to do so on their own. For some patients, this could mean using oxygen intermittently, but for others, it could mean using oxygen 24/7. Your doctor will help you decide what’s best for you.
.png)
We recommend using a portable oxygen concentrator such as the Caire FreeStyle Comfort or the Inogen One G5 because these units are lightweight and allow you to take your oxygen supply anywhere in the world with ease. They’re also extremely reliable, so you don’t have to worry about losing access to your oxygen when you need it the most.
Exercising Safely
Exercise is a fundamental aspect of any COPD treatment routine. Pulmonary rehabilitation (PR) is used to increase the strength and efficiency of the lungs while helping COPD patients maintain their weight and promote healthy circulation. However, if you exercise too much or you don’t exercise in a way that’s advised by your doctor, you might experience exercise-induced bronchospasms (EIB).

To avoid exercise-induced bronchospasms, be sure to avoid exercising in the cold. Cold, dry air can cause your mucus to become thick and difficult to clear. Air that’s filled with pollen or other allergens can also irritate your airways causing bronchospasms. Lastly, you should be careful not to overexercise. High-intensity exercise is not typically recommended for treating COPD and it can put you at a higher risk for experiencing exacerbations or other serious complications. Stick to a moderate, but consistent exercise routine.
Diet
Your dietary habits can make the difference between a healthy and unhealthy respiratory system. As aforementioned, consuming food that you’re allergic to can exacerbate your respiratory symptoms and cause bronchospasms. COPD patients tend to retain sodium, so you should avoid food with added salt and drink plenty of water. Being well-hydrated means your mucus will be less viscous and easier to clear from your airways. Foods to avoid include coffee, sugary drinks, fried foods, and milk.

Another thing to be wary of is dietary supplements. While dietary supplements are often hyped-up through advertising and word of mouth, they have negative side-effects just like over-the-counter and prescription drugs. The problem is that dietary supplements are registered as “food products” through the Food and Drug Administration (FDA) so companies can often get away with overexaggerating the benefits of their supplements without discussing the potential side-effects.
Conclusion
Bronchospasms are a common symptom of COPD and asthma, but under certain circumstances, they can also occur in healthy people. Severe allergic reactions, air pollution, and medications can all cause bronchospasms and they can range in severity from moderate to life-threatening. While there are several home remedies that can help alleviate the symptoms of bronchospasms, your best bet will be to speak with your doctor as soon as possible.
In the meantime, your best course of action is to follow your COPD treatment plan. Using supplemental oxygen as prescribed, following a strict diet, and maintaining a healthy and consistent exercise routine will all promote healthy lungs and airways, thus helping you to prevent bronchospasms and other respiratory complications. You should also take the time to check the air quality in your area before going outside so that you can avoid air pollution.
Here at LPT Medical, our goal is to provide as many COPD patients as possible with durable and reliable portable oxygen concentrators. With a portable oxygen concentrator at your side, you’ll have the freedom to go about your daily life without having to worry about not having medical oxygen that meets your respiratory needs. If you need help choosing an oxygen concentrator, please feel free to give us a call at 1-888-416-3855.

