One of the things that makes COPD so dangerous is the fact that it makes your body more vulnerable to disease. It not only makes you more likely to get sick, but it makes it harder to recover from illnesses, too.
For people with COPD, any sickness—even a common cold—can be serious or, in some cases, even life-threatening. Even worse are respiratory infections like pneumonia, which can cause permanent damage to lungs affected by COPD.
Because of this, it is imperative for every person with COPD to take good care of their immune system. Because your immune system is so closely linked with all of your body's other systems, that means making healthy choices when it comes to your diet, sleeping habits, personal hygiene, and even your mental health.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In this guide, we're going to tell you everything you need to know about how to keep your immune system in the best shape possible while managing your COPD. Using the practical tips in this article, you can make sure you are giving your body everything it needs to protect itself from illnesses and infections.
Because you never know when sickness will strike, it's important to make your immune system's health a priority now, and not put it off for the future. By building healthy immune habits early and continuing to be diligent, you may be able to prevent a number of illnesses that could worsen your COPD.
In this Guide:
- What Works and What Doesn't
- How Your Immune System Works
- How COPD Affects Your Immune System
- Practical Tips You Can Use to Boost Your Immune System the Right Way
- Vitamins and Nutrients You Need for a Healthy Immune System
- The Anti-Inflammation Diet
- Things that Don't Help Your Immune System
What Works and What Doesn't
The world around us is full of products that make lofty claims about boosting your immune system and staving off disease. You've probably seen them advertised on TV, in magazines, health food stores, and even your local supermarket.
Unfortunately, these products are usually nothing more than glorified snacks that won't boost your immune system in any way. So far, scientists haven't been able to confirm that any health food or supplement on its own will reliably improve your resistance to illness.
However, researchers have identified a variety of healthy habits and nutrients that support your immune system and keep it running smoothly. On their own, they are unlikely to make much of a difference, but putting them all together will help you build a healthier lifestyle that boosts your body's ability to fight off infection and disease.
It's important to know that keeping your immune system healthy isn't about taking a certain supplement or miracle vitamin; it's about giving your immune system everything it needs to stay strong. It's also about avoiding activities and habits that weaken your immune system's ability to respond to threats.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
In these next sections, we're going to tell you all about all the nutrients, healthy habits, and other treatments like vaccines that you need to keep your immune system primed and ready to fight disease. While none of these things are miracle cures, they are the most effective, proven ways to keep your immune system strong and working as effectively and efficiently as possible.
How Your Immune System Works

The immune system is a very complex system that protects your body in a variety of different ways. It not only fights off pathogens, like viruses and bacteria, that make you sick, but it also helps your body destroy harmful toxins and misbehaving cells like cancer cells.
Your immune system is made up of many different tissues, cells, and molecules that are spread all throughout your body. But in general, your immune system can be categorized into two main parts: the innate immune response and the adaptive immune response.
The Innate Immune Response

The first step of your body's immune response is often referred to as the “innate” immune response. This is a broad, generalized immune reaction that gets triggered whenever you are sick, injured, or your body detects pathogens or irritation.
The innate immune response is quick, and its goal is to destroy any bacteria, viruses, parasites, or other harmful pathogens that enter your body. It does so by mobilizing pathogen-destroying cells (called leukocytes) and triggering inflammation.
Inflammation causes changes in your body that allow your immune system to heal the injury more quickly. It also triggers reactions like fever, runny nose, coughing, and sneezing that help your body flush pathogens out of your body more quickly.
In some cases, your innate immune response can become over-sensitive and react to things that are not harmful, causing it to trigger the inflammatory response when it is not needed. This can lead to chronic inflammation, which is linked to a variety of chronic diseases, including heart disease and COPD.
One of the most important parts of the innate immune system is a category of cells called leukocytes, also known as white blood cells. Leukocytes are one of the most important parts of the immune system and they come in a variety of different types.

The primary responsibility of leukocytes is to track down and destroy all kinds of viruses, bacteria, and other pathogens, and each type of leukocyte has its own pathogen-hunting specialty. For example, phagocytes, which make up one category of leukocytes, kill pathogens by surrounding them and dissolving them with a cocktail of toxic chemicals.
Leukocytes lie in wait in many different places throughout your body, ready to spring into action as soon as they detect a pathogen to destroy. They can also travel around in your bloodstream, which allows them to quickly get to any place in the body where they are needed.
The Adaptive Immune Response

One of the most incredible talents of the immune system is its ability to learn and adapt to its environment. This is the job of the second main part of your immune system, the “adaptive” immune response.
Unlike the innate immune system, which fights pathogens in general, the adaptive immune system is responsible for tracking down and killing specific pathogens. It does this by creating antibodies whenever it encounters a new type of pathogen that it hasn't seen before.
Antibodies are molecules that can only stick to one specific type of pathogen, such as a specific type of virus or a particular bacteria species. When an antibody encounters the matching pathogen, it binds, or sticks, itself to the pathogen's surface.
This tag alerts leukocytes to the pathogen's presence and marks it for destruction. As a result, your immune system will recognize the pathogen much more quickly than it would if there were no antibodies around to help.
In this way, antibodies act as a sort of “memory” that allows your immune system to quickly identify viruses and bacteria that it has encountered before. This helps your immune system respond more rapidly and effectively to threats, reducing your chance of getting sick.
How COPD Affects Your Immune System
COPD has long been known to weaken the immune system and make patients more prone to disease. While researchers still do not fully understand why this happens, the link between COPD and poor immune system function is clear.
One reason for this is chronic inflammation, which afflicts the vast majority of patients with COPD. Studies show that chronic inflammation has a detrimental effect on the immune system, reducing its ability to fight disease.
Usually, inflammation triggers your immune system to act and neutralize whatever caused the inflammation. But in the case of chronic inflammation, your immune system overreacts when there is no real physical threat to neutralize.
As a result, the inflammation continues indefinitely and your immune system stays perpetually preoccupied with the imaginary threat. This unchecked inflammation puts a great deal of stress on your body (including your lungs) and makes your immune system less effective at countering real threats.
As the Cleveland Clinic puts it, “sustained, high levels of inflammation point to an overworked, over-tired immune system that can't properly protect you.” Unfortunately, chronic inflammation is a reality for the majority of people with COPD.
This has led some researchers to believe that COPD may be, at least in part, an autoimmune disease. An autoimmune disease is a disease that causes your body's immune system to mistakenly attack your body's own healthy cells.
The immune systems of people with COPD tend to overreact to minor irritants that you breathe in, causing inflammation in the lungs. Instead of attacking just the irritant, the immune system may end up attacking healthy lung tissue, resulting in permanent damage to the lungs that researchers believe may both cause and worsen COPD.
Chronic inflammation in the lungs can also make the lung tissue more susceptible to bacteria that cause respiratory illnesses and infections. Another problem is constant airway blockage from excess mucus and airway constriction, which makes it easier for infections to take hold in your lungs and airways.
It is also very common for COPD patients to suffer from anxiety, stress, and depression, which are known to weaken your immune system. COPD also impairs many patients ability to sleep, and lack of sleep is also linked to poor immune system function.
Other immune system problems faced by patients are indirectly caused by the symptoms of COPD itself. For instance, patients who get short of breath easily often struggle to keep up with healthy habits that are necessary for a healthy immune system, including exercising and eating a healthy diet.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
However, probably the most important reason that COPD patients have to take extra good care of their immune systems is to avoid COPD exacerbations. Exacerbations can be triggered by even mild illnesses and infections, and a healthy immune system is your first line of defense against getting sick.
Exacerbations make your COPD symptoms much worse and they can last for weeks or longer, which makes it very difficult to stay active and live a healthy lifestyle. Serious exacerbations can be even more devastating, causing permanent lung damage, sending you to the hospital, or even leading to respiratory failure and death.
Practical Tips You Can Use to Boost Your Immune System the Right Way
Because the immune system is so complex and varied, there is no one, definitive way to “boost” it. However, that doesn't mean that that your lifestyle and behaviors don't affect how your immune system works.
Lots of factors, including your nutrition, exercise habits, mental health, and more can have a significant effect on how efficiently your immune system functions. Luckily, that means that there are many things you can do in your daily life to keep your immune system healthy.
Stop Smoking

Smoking tobacco is bad for your immune system and makes your more prone to getting sick. Because most people who have COPD are smokers or former smokers, this is a common problem among COPD patients.
Smoking negatively affects the leukocytes in your body and suppresses your immune response. It also causes inflammation in your lungs that can make your COPD symptoms much worse.
Smoking also causes damage to other cells all throughout your body, which triggers a chronic state of inflammation. This inflammation increases your risk for infections, heart disease, and other serious health conditions.
However, if you quit smoking, your immune system can and will recover. If you have COPD and you still smoke, then it is absolutely imperative that you quit.
Quitting smoking is one of the best things you can do to improve your health and your overall quality of life with COPD. If you need help, visit the CDC's website to learn about a variety of quit smoking resources that can help you succeed.
It's never too late to stop smoking. Doing so will not only help your immune system, but it can also improve your COPD symptoms and prevent other serious diseases.
Don't Drink Too Much

While there's nothing wrong with a drink now and then, too much alcohol can hurt your immune system. It does this by suppressing the activity of leukocytes and reducing your immune system's ability to recognize and respond to threats.
Any kind of excessive drinking, including binge drinking and chronic alcohol use, can weaken your immune system. In fact, studies show that alcohol effects your immune system within twenty minutes of taking a drink, and that just one instance of binge drinking can significantly increase your risk for infection for days after you've sobered up.
This leaves your body more vulnerable to illnesses, infection, and other diseases like cancer. In combination with the already present immune-suppressing effects of COPD, excessive drinking can be particularly dangerous for COPD patients.
That's why, if you have COPD, you should be especially careful to avoid alcohol or at least drink in moderation. US guidelines for alcohol use recommend that you drink no more than seven standard drinks per week.
If you struggle with alcohol abuse or need help quitting or reducing your drinking, visit the Alcohol Rehab Guide to learn about a variety of resources that can help.
Stay Active

If you have COPD, then you know that staying active is important for keeping your heart and lungs healthy. However, physical activity is just as important for your immune system, as well.
Researchers aren't sure exactly why, but getting regular exercise improves your immune system's ability to fight off disease. One study showed that just twenty minutes of physical activity every day can reduce inflammation and help your immune system function more effectively.
Even though COPD can make exercise difficult, it's important to find some physical activities that you find engaging and fun. Even if you have to start small, you can improve your physical strength and endurance with time.
If you need help working out a feasible exercise plan, don't be afraid to ask your doctor for advice. If your COPD symptoms are preventing you from exercising, your doctor may be able to recommend another treatment, like pulmonary rehabilitation or supplemental oxygen, that can help you stay active.
Getting regular exercise can be as simple taking daily walks, bicycling, or doing aerobic exercises at home. For more tips on how to stay active with COPD, visit our guide to exercising at home with COPD here.
Vaccination
Vaccination is the only targeted treatment scientists have found that can reliably and significantly boost the immune system on its own. That's why doctors often urge COPD patients to get vaccinated as a first line of defense against illnesses like the flu and pneumonia.
Vaccines work by exposing your body to a tiny amount of a disease-causing pathogen that has been weakened or killed. The vaccine doesn't contain enough of the pathogen to get you sick, but it contains just enough for your immune system to recognize it and respond.
Your immune system reacts to the vaccine by making specific antibodies that target the pathogen in the vaccine. Then, if you are ever exposed to the pathogen in the future, your immune system will be primed and ready to destroy it before it has a chance to get you sick.
Here are the vaccines typically recommended for people with COPD:
- The Influenza Vaccine: Get vaccinated every year to protect yourself before flu season.
- Td Vaccine: Get vaccinated once every ten years to protect yourself from tetanus.
- Pneumococcal Vaccine: Get vaccinated once before the age of 65, and then twice again after the age of 65 to protect yourself from bacterial pneumonia
If you are not sure if you are up to date on these or any other vaccines, talk to your doctor. He can review your records and tell you what vaccines could be beneficial for you.
Reduce Stress
Chronic stress and other mental disorders like depression are well-known triggers for inflammation and immune system distress. Because of this, keeping stress at a minimum and treating anxiety and depression are important for keeping your immune system in good shape.
For instance, a variety of studies have found that people who experience chronic stress are more likely to contract a common cold. Chronic stress can also reduce your body's ability to heal itself, fight cancer, and gain immunity from vaccines.
Depression has also been linked to chronic inflammation and reduced immune system function. While researchers are still trying to understand exactly why this happens, they do have some idea of how it works.
Stress increases the amount of a “stress chemical” known as cortisol, which triggers inflammation. It also reduces the number of leukocytes in your body, making it harder for your immune system to fight off disease.
Unfortunately, chronic stress, anxiety, and depression are very common among people with COPD. Fortunately, there are many different things you can do to reduce your stress, treat depression, and improve your mental and emotional health.
Check out these guides for managing stress, anxiety, and depression:
- How to Treat Depression When You Have COPD
- How to Treat Anxiety and Panic Attacks When You Have COPD
Get Good Sleep
Sleep is an incredibly undervalued activity in the modern world. Despite the fact that it's necessary for survival, many people don't sleep enough and don't understand the importance of high quality sleep.
Many studies have shown that you are more likely to get sick when you don't get proper sleep. Being sleep deprived can also hamper your ability to recover from illnesses and infections, causing you to stay sick for longer.
Poor sleep has particularly serious consequences for people with COPD and can significantly increase their chances of experiencing a COPD exacerbation. Some studies have also found that sleep deprivation significantly impairs COPD patients' ability to breathe.
That's why it's so important to make sleep an important priority in your life. Most adults need at least 7-8 hours every single night, and any less can significantly affect your quality of life.
Unfortunately, COPD patients in particular often struggle to sleep because of their disease. This is partially because many COPD symptoms, including breathlessness, airway blockage, and chest discomfort, get worse for many patients in bed at night.
Fortunately, there are many things you can do to improve your sleep quality and your ability to fall sleep at night. It's all about establishing a consistent, relaxing nighttime routine and making sure you have a comfortable sleeping environment.
Here are some tips for improving your sleep when you have COPD:

If you have COPD it is important to take care of your body and your lungs, people do this by quitting smoking, exercising whenever possible, taking medication, and adhering to a strict treatment plan. Beyond these measures, it is important to also pay mind to your mental health, in doing so people with COPD become more motivated and cultivate a positive mind set.
When people's COPD symptoms begin to worsen is when their mental health also deteriorates and subsequently influences people to pay less attention to their COPD treatment thereby negatively effecting their health and well being. This is whats known as a negative feedback loop, which is a reaction that causes a decrease in function. So, creating a healthy environment to live in, by keeping your home clean and irritate free, is so crucial for these patients in order to find "homeostasis" which is essentially a state of normalcy.
In this article we are going to discuss how you can create a healthy living space mentally while living with COPD, but we are also going to give you ways to make your physical living space inside your home more COPD friendly.
Creating a healthy living space inside your mind

We wrote an entire article about the mental health of COPD patients and how this disease can influence depressive and anxious feelings, you can read that article by clicking here.
Now we are going to go over a few ways you can cultivate a more positive mindset while living with COPD, with a following section about living in a healthy environment physically with COPD.
Social connections
Connection is an important part of dealing with COPD and the mental stress and confusion that often comes with the territory. While it is not something your doctor would prescribe, connecting with others is something you doctor should or likely has already recommended. It is also important to maintain a healthy relationship with the people who were in your life before you were diagnosed. It can be challenging to rely on the people in your everyday life more than you had before, so finding a sense of independence is critical here.

In this section we are going to talk about connecting with new people, fostering relationships with your caregivers, and finding your own independence in order to maintain these healthy relationships with others.
One of the easiest and most beneficial ways to connect with other people who have COPD is to enroll in pulmonary rehabilitation. Your doctor should be able to refer you to a program in your area. For example, if you live in Florida in the Boca Raton area you are assured quality care at their South Miami Hospital Pulmonary Rehabilitation program. They have licensed, certified respiratory and physical therapists trained and certified by the National Board of Respiratory Care.
In a pulmonary rehab course, you will work closely with a team of professionals including:
and sometimes other clinical experts as needed

With the help of all of these experts, you will learn about multiple facets of your life. You will learn about your medical condition, how to exercise properly and within your capabilities, respiratory advice and management, managing eating habits and mental stress, all while connecting with others who are suffering from COPD as well.
While all of these aspects of pulmonary rehab are important, but the social component is so valuable for your mental state of mind. Seeing and hearing other people’s hardships throughout their diagnosis can help you feel less “alone”. Feeling alone is one of the main reasons people with COPD struggle to stay positive, thereby neglecting their treatment regimen and their mental health.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
So cultivating relationships with people in your pulmonary rehab program who have similar medical conditions, is a great way to connect and feel less alone.
The other way you can create new relationships within a community that you can relate to on a medical level is joining facebook support groups. This is as simple as searching LPT Medical COPD & Respiratory Support Group on facebook and requesting to be added to the group. Once the admin has accepted you, say hello by posting a comment about something you want to talk about.

Even though you are sharing with others online, these people are real, and connecting via the internet is one of the safest ways to relate to people right now amidst a global pandemic.
When it comes to fostering old relationships with your loved ones through the duration of your disease, we could write an entire blog post, so we did, you can read it by clicking here
The main points of this article are as follows:
- Learn how to communicate effectively
- Learn as much about your disease together as possible, education is key in the management and treatment process, the more you know the more comfortable you will both feel
- Destress in any way you can that works for you, such as , exercise, alone time, breathing exercises, medication, or gardening.
- Find independence where you can get it
Point number 4. brings us into the final part of this section: Finding independence. Your independence is so important for your mental health, the current relationships you have, and future ones as well.
Independence
Before you were diagnosed with COPD, you could shower, walk to get the mail, do yard work, without thinking twice about it. Now, you might have to ask for help more often than you are used to because you are unable to do these chores on your own anymore. Many people find asking for help to be frustrating, and if this is not something you are used to, you must find ways to cope, but also find ways in which you can regain your independence.

If you are an oxygen user, your oxygen device may get in the way of you doing things that you could once do on your own. If your oxygen device is too heavy, not portable, or you do not enjoy using your oxygen device, it may be time for an upgrade.
There are modern forms of oxygen therapy that allow you to get back to doing more things you want to do. By buying a portable oxygen concentrator you will be able to travel alone, carrying your device on your own, and feel more confident managing your oxygen therapy on your own.
Depending on the model of portable oxygen concentrator they range from 4 - 18 pounds based on the flow settings and battery life. Having a device that runs on battery life is essential for independence because you will not have to rely on an oxygen refill company to deliver your oxygen tanks every week. Instead you will be responsible for charging your unit or keeping an extra battery on you.
Depending on your oxygen prescription, the right portable oxygen concentrator should have flow setting well above what your are prescribed. For example, it your Doctor writes you a prescription for 630 ml/min of oxygen, the Inogen One G3 could be the perfect oxygen device for you, because it has the capability to run at 1050 ml/min of oxygen so if you ever need to increase your oxygen output in your oxygen device, you will not have to return the device for a new one, you can simply adjust the setting.

As an established oxygen supply company in Denver, CO we have access to the top tier oxygen equipment on the market, but we also have over 10 years experience working with oxygen patients in all levels of their diagnosis. Of the many things we have learned in our experience, one of the most important is to focus one everyone's individual oxygen requirements but also their lifestyle.
Portability and accessibility are two of the main reason oxygen patients decide to switch from traditional oxygen tanks to portable oxygen concentrators, but there are other factors to think about when deciding on your oxygen equipment.
Click here to read about oxygen therapy equipment and how they all compare.
The next part of encouraging a positive mindset is learning how to enjoy the little things.
The little things
We have all heard the saying “enjoy the little things” and while it sounds like a clique, there are a lot of benefits to finding simple pleasures, especially if you have COPD. As a COPD patient, you are still capable of enjoying life, and similarly to the way you once did before you ever started experiencing symptoms.

But if there are aspects of your life, you won’t get back due to your disease, this is the perfect opportunity to try new things. And if you change your perspective this way, there is nothing that can stop you.
Examples of the little things would include family time, reading, movie marathons, gardening, walking, cooking, or any hobby of your choosing. You can start by setting goals; if you don't have a hobby, make a list of new activities or hobbies you want to try. Then make a list of the tools or motivation you would need to start doing said hobby.
Simply looking forward to something is a form of enjoying the little things. Spending more time in your day being active and having something to do will also give your mind something else to focus on besides your COPD symptoms.
Making you physical living space COPD friendly

When you have a disease like COPD, it's vital to breathe air that is clean and healthy as often as possible. Respiratory diseases cause your lungs and airways to be extra sensitive to irritation and inflammation, and even the smallest amounts of airborne contaminates can worsen COPD symptoms and even cause exacerbations.
Air filters

Many people underestimate the importance of using a high quality air filter and neglect their house's ventilation system. Choosing a quality air filter is just another choice the is over-saturated with brands and models so you may not know what to look for or how to choose a kind that's effective and meets your individual needs.
Additionally, there are many different portable and small-space air purifiers you can find, as well as dedicated whole-house air purification systems that hook up to your HVAC system. However, it can be difficult to understand all of these different options, how they work, and how to know if you need one for your home. SO, we wrote an entire blog post about this!
You can read it by clicking here!
Temperature
The next thing you should try to do in your home, is adjust your heating in order to keep your home at a temperature between 19 and 21°C. Cold temperatures may influence your COPD symptoms making you feel worse.
Home renovations
It is also crucial that you avoid using strong chemical products such as polish and paints when or if you ever do home renovations or basic house work. These products can irritate your airways causing you to experience worse symptoms.
Cleanliness

The cleanliness of your home is one of the major factors in determining the indoor air quality. Therefore, cleaning with the intention to maintain good air quality is crucial to avoid COPD flare-ups.
Dust and dust mites, pets, smoking indoors, cleaning solutions, room fresheners and candles, are a few of the irritates that can spark a COPD exacerbation progressing your COPD faster into a more severe state. This is because when you breathe in irritates, they can cause problems like increased mucus production, making it difficult for you to clear your airways, or your airways begin to spasm, making it very hard for you to catch your breath even doing the most simple tasks.
Neglecting to clean your home of dust, allergens, pet dander, smoke and other respiratory irritates can cause major damage to your lungs, but it can also make your life a lot more chaotic than it needs to be. If your home environment is toxic to your lungs you will find yourself visiting the emergency room all the time, and once you’ve recovered from the exacerbation in the hospital and go home, the cycle will continue.
Cleaning products

So you should keep your house clean, but you also need to be aware of the cleaning product you are using because they can be harmful to inhale, and for someone with COPD, this can cause exasperated symptoms. Having a low or no scent home is a good rule to follow. Fresh lemons (or lemon concentrate), baking soda, water, simple dish washing detergent, vinegar, and rubbing alcohol can be used in various combinations to clean most things.
If you ever need to use bleach, try to leave the house or go into a different room while someone else in your household cleans with bleach.
Smoking
It is exceptionally important to keep your home a smoke free environment, meaning no cigarettes or e-cigarettes, and it is best to avoid vape products as well.
Smoke particles are often microscopic, that are byproducts of burning substances or other chemical processes, which can be inhaled into the lungs and cause irritation.
You should not only quit smoking yourself, you should not allow others to smoke inside you home. There are no good ways of getting rid of smoke entirely, and it’s harmful to have in your home for multiple reasons. It not only creates a lot of these microscopic particles that can live in your walls, carpets, and decor, it makes up gases and toxins that are truly lethal.

Natural gas
You might not realize it at first, but if you have a gas stove, or gas fireplace, you have to be cautious about the exposure to nitrogen dioxide emissions. These emissions can come from natural gas. In order to avoid these irritates, adequate ventilation in your kitchen is the best way to remedy this.
Pets
If you have any pets that shed, pet dander isn’t necessarily an issue for all people living with COPD. If you have even mild allergies this may cause exacerbated COPD symptoms. Regularly vacuuming and wiping surfaces, cleaning furniture, and linens in your home can help reduce pet dander.
Dust and carpets
It is so important to dust often in your home. Dust can be especially irritating to people with COPD who have allergies. In addition to keeping home surfaces free from dust, experts also recommend minimizing carpeting in your home.

If it is possible you should remove carpet from your home because dust mites will get into your carpet and live there, making it difficult to remove. Hardwood floor is much easier to manage, and does not hold pet dander or dust like carpet does, making your living environment more manageable with less irritates in the air. If it’s not possible to get rid of your carpet, use a vacuum cleaner with a built in air filter to bring up the dust mites and other irritants found in carpet.
Bedding
Dust mites are also found in bed linens. So you should try to keep them clean as much as possible. This is as simple as washing your sheets using hot water and replacing pillows more frequently.

Humidity
Depending on your body and your COPD, the humidity level in your home could be another irritant in and of itself. Keeping the humidity at a manageable so it is easier to breathe is great, but also keeping the humidity below 50 percent in your home is a good way of helping to control mold and dust mites. Dust mites grow fast when there is a humid environment. Be sure to always use the exhaust ventilation in your bathroom during and after you shower, provided that the vent sends damp air outside of the home and doesn’t simply recirculate it. If you don’t have ventilation in your bathroom, you may want to consider installing it.
Oxygen
It is so important that you follow your oxygen prescription to a T, so having oxygen equipment that you can carry with your throughout your house with ease is very helpful. Even "heavier" devices compares to the lightweight Caire Freestyle Comfort should still be maneuverable. The Respironics SImplyGo weighs 10 pounds, and stands 10" H x 6" D x 11.5" W meaning your SimplyGo will easily fit underneath the seat in front of you on the airplane, you can store it on the floor of your car or in the passenger seat as you drive,, and while this device may be heavier than other pulse flow devices, the SimplyGo is one of the smallest and lightest continuous flow portables available! You will be able to bring it with you wherever you go and you will have no problem finding a place to store it.

The SimplyGo includes a custom carrying case and a wheeled travel cart so you have the option to carry it over your shoulder or you can pull it behind you on the travel cart and it will make it around the house with you and .
If you need oxygen 24/7 is it helpful to own your own portable oxygen concentrator that is designed to run day and night. The Respironics SimplyGo is CPAP/BiPAP compatible and it even offers sleep mode technology! When you are relaxing in your chair at home, and you feel yourself dozing off, you can turn sleep mode technology on to ensure your oxygen gets delivered while you are sleeping. The sleep mode technology on your SimplyGo increases its sensitivity to detect your breath and it softens the pulse flow delivery so it doesn’t wake you up.
Overview
Living with COPD is all about balance, and creating good habits while overcoming bad ones. The goal is to create positive feedback loops that promote function in your mind and in your body.
Believe it or not, the way your body feels influences the way your mind reacts, feels, and makes decisions, and vise versa. The decisions you make and your emotions will directly effect how you body feels physically.
If you can keep your home clean and free from irritates your COPD are less likely to get worse overtime and your body will feel better allowing your emotions to be more positive and capable of making good decisions. Creating a healthy living space in your home is just one example of the many actions you can take in order to live a longer and healthier life with COPD.
We covered a lot of information in this article, and if you made it this far, leave a comment, let us know how you find inner peace both in your mind and your home!
%20(1).png)
A portable oxygen concentrator is a medical oxygen device used to treat respiratory illnesses such as chronic obstructive pulmonary disease (COPD) and cystic fibrosis (CF). Unlike other oxygen machines like oxygen tanks or stationary oxygen concentrators, portable oxygen concentrators are designed to be lightweight, efficient, and provide the patient with as much freedom as possible while still ensuring their oxygen needs are met. If you’ve never purchased an oxygen machine before or you’re looking for an upgrade to your current device, you’re probably trying to find a good starting point.
Oxygen concentrators are fairly complex and as such, there are a lot of factors to take into consideration including oxygen output, battery life, weight, size, and design. While all of this information is out there on the web, you may find it challenging to consolidate your findings and make an educated decision about your oxygen needs. In the past, we’ve provided oxygen patients with a number of helpful resources such as this guide which covers the highest performing concentrators of 2021 or this post where we discuss the lightest portable oxygen concentrators of the year.
To provide you with even more resources for choosing a portable oxygen concentrator in 2021, we’ve created a comprehensive guide that covers the process of choosing a POC from start to finish. After reading this guide, you’ll know exactly what to look for in your new oxygen machine and after it arrives at your door, you’ll feel much more confident about the decision you’ve made. Keep reading to get started, and if you have any questions for us, be sure to fill out the contact form at the side of the page. A respiratory specialist will reach out to you shortly to answer any questions you may have.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Why Use a Portable Oxygen Concentrator?
The first question you’re likely wondering about portable oxygen concentrators is, “why should I use one?” This is a valid question because there are many oxygen machines on the market such as oxygen tanks, portable oxygen cylinders, home oxygen concentrators, and more. Each of these has its pros and cons, but in general, portable oxygen concentrators will provide you with the greatest value and serve you best in the long term.

Several decades ago, you weren’t likely to find many options when it came to medical oxygen. Before the 1970s, oxygen patients had to rely on bulky, heavy, and dangerous oxygen tanks, some of which could weigh in excess of 100 lbs. At the turn of the century, home oxygen concentrators and portable oxygen concentrators became the dominant source of oxygen for many patients. Liquid oxygen cylinders also became popular because they could hold more oxygen than a compressed oxygen tank and they could be carried in most places.

Fast forward 20 years and you’ll find that POCs are the preferred choice for most oxygen patients. As they’ve become more powerful, lighter, and their battery life has increased, there are fewer and fewer reasons to purchase or rent an oxygen tank. Stationary oxygen concentrators still work great, but they usually cost as much as portable units meaning they’re almost entirely obsolete unless you can find a great deal on a used or refurbished one.
Pulse Flow vs. Continuous Flow
Now that you’ve established you need a portable oxygen concentrator in favor of other medical oxygen machines, it’s time to decide between pulse flow and continuous flow. A continuous flow oxygen concentrator is one that puts out a steady stream of oxygen like a water fountain. All oxygen tanks are continuous flow unless they have something called an oxygen conserver which attaches to the top of the unit. A pulse flow oxygen concentrator, on the other hand, has additional technology in it that detects your breathing and only puts out oxygen when you inhale.

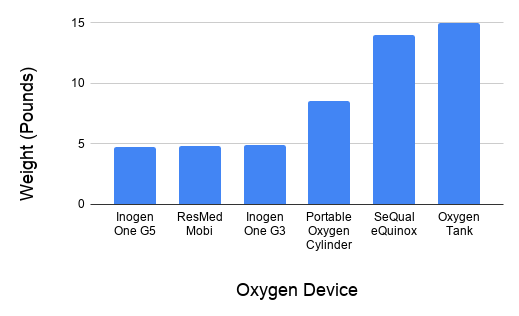
Since pulse flow units don’t need to put out as much oxygen, manufacturers are able to make them much smaller and lighter. An average pulse flow portable oxygen concentrator will weigh around 5 to 6 pounds whereas the average continuous flow portable oxygen concentrator will weigh 10 pounds or more. Each type of concentrator has comparable oxygen output, but your doctor may advise that you use one in favor of another. It should also be noted that many continuous flow POCs like the Oxlife Independence allow you to switch between continuous flow and pulse flow.
.png)
Ultimately, pulse flow will be the way to go for most oxygen patients. These POCs are light enough to carry on your shoulder, easy to use, and some can even provide up to 16 hours of battery life on one charge!
What Are the Best Portable Oxygen Concentrator Brands?
Brand is an incredibly important thing to consider when you first purchase a portable oxygen concentrator. For better or worse, we live in a time where eCommerce is king. What this means for the consumer is that it’s harder to simply walk into a store and test a product before you buy it. As a result, you need to have faith in the brands that you work with.

When it comes to portable oxygen concentrators, companies like Inogen, Respironics, AirSep, Caire Inc., ResMed, GCE, and SeQual Technologies are some of the most reputable oxygen manufacturers in the industry. If you encounter an oxygen retailer who offers products from a brand other than the ones listed above, you should thoroughly research them before buying a portable oxygen concentrator from them.
It’s illegal to sell a medical oxygen device without first verifying oxygen use, so oxygen concentrators listed on sites like eBay or Amazon either aren’t approved for medical use or the vendor is breaking the law. Always purchase portable oxygen concentrators from verified POC distributors like LPT Medical. When you contact us, you will always be asked for proof of oxygen use, so it helps to have your doctor’s phone number handy so we can take care of this as quickly as possible.

Another important distinction to make is the difference between recreational and medical oxygen. Recreational oxygen is used for things like scuba diving, hiking, or other outdoor activities. Some people would claim that recreational oxygen use improves respiratory performance but others believe it’s a fad. Medical oxygen, on the other hand, usually has between 90% and 96% purity rating, much more than in recreational oxygen.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Portable Oxygen Concentrator Specifications
No portable oxygen concentrator was created equal when it comes to specifications. Aside from choosing the right brand, you need to examine each spec to ensure that the POC you’re getting fits your needs and your lifestyle. Most oxygen retailers list product specs on their product page, but if you can’t find what you’re looking for, try Googling the name of the oxygen concentrator followed by the word “manual.” In the results, you should see a PDF for the unit you’re interested in. Read through this to find information about its oxygen output, battery life, weight, and more. Alternatively, you can contact one of our respiratory specialists here at LPT Medical and we’ll answer any questions about your POC of choice.
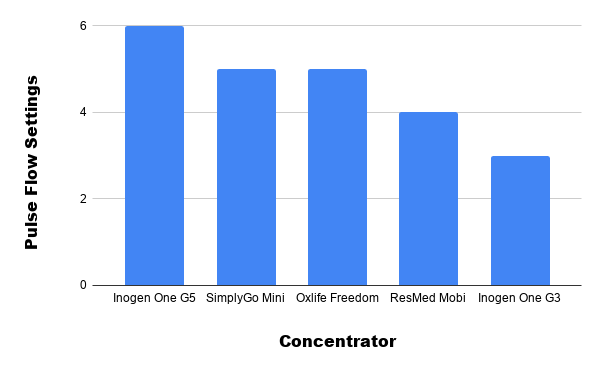
Oxygen Output
Hands down the most important aspect of your portable oxygen concentrator is its total (maximum) oxygen output. Unlike oxygen tanks that offer virtually any oxygen setting you want, pulse flow portable oxygen concentrators are limited by the size and efficiency of their compressor. There are pulse flow units on the market that range anywhere from 300 ml/min to 1,260 ml/min and they range anywhere from 2 to 6 different pulse flow settings. Most oxygen patients require at least 400 ml/min which is usually a setting of 2 or 3 on most POCs.

Before purchasing any portable oxygen concentrator it’s important to clearly understand your oxygen needs. Next time you go to the doctor or pulmonologist, ask him/her the following questions:
- How long do I need to use oxygen each day?
- Should I use my oxygen concentrator while sleeping?
- Should I use pulse flow or continuous flow oxygen?
- What are my oxygen needs? (milliliters per minute and liters per minute)
As you ask your doctor these questions, be sure to write them down along with your doctor’s personal phone number or the number of the doctor’s office. When you go to purchase a portable oxygen concentrator, you can simply provide your respiratory specialist with the number so they can verify your oxygen use.

Another thing to note about maximum oxygen output is that you want to have room to move up. COPD is a progressive disease meaning it gets worse as time goes on. So, for example, if your doctor says you need 400 ml/min of oxygen, it would be wise to invest in a concentrator that’s capable of putting out 600 or 700 ml/min of oxygen — the same applies to continuous flow concentrators.
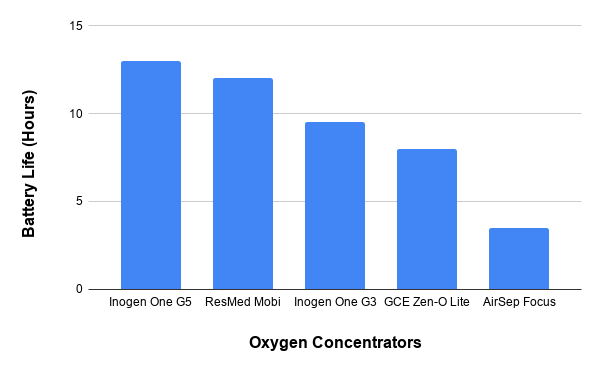
Battery Life
For the majority of oxygen patients, battery life is the second most important aspect of a portable oxygen concentrator. After all, a POC that can only run for an hour without needing to be charged doesn’t really offer much portability at all, and at the end of the day, you may feel that you have less freedom than you did with your oxygen tank.

Most portable oxygen concentrators use what’s called lithium-ion batteries. These types of batteries have been used primarily in electronic devices like cell phones, laptops, and tablets since the 1990s. The reason they’re so popular is because they’re eco-friendly, lightweight, and most importantly, powerful. Since portable oxygen concentrators have both electrical and mechanical components, it’s important that the batteries are as efficient as possible in order to keep people out and about longer.

Portable oxygen concentrators vary widely in terms of battery life. POCs like the Caire Freestyle Comfort and Inogen One G5 offer upwards of 13 hours of battery life on one charge, however, ultra-lightweight POCs like the AirSep Focus only hold a couple of hours of battery life on one charge. Continuous flow portable oxygen concentrators also tend to provide less battery life because they put out more oxygen than pulse flow units do.

If you don’t mind sacrificing some weight for extra battery life, you may want to invest in portable oxygen concentrator accessories like the G5 backpack. Rather than having to carry your extra batteries in your hand or a separate bag, this will enable you to carry everything in one place. Once you’re ready to swap out your batteries, you’ll have everything in the same place, ready to go.
Weight
As we get older, our ability to carry heavy things diminishes. What’s more, many people, young and old suffer from back pain, so carrying around a 10-pound oxygen tank is simply not an option for many people. With that being said, you may be surprised to know that there are portable oxygen concentrators as light as 1.75 pounds! What this means is that even people with scoliosis or other conditions that affect the back and shoulders can still experience the freedom of having oxygen on the go.

Another reason to invest in a light portable oxygen concentrator is that you’ll be able to carry more personal belongings. Whether you simply want to get out and go for a walk or you’re planning a trip or vacation, it’s always nice to be able to carry personal items like your cell phone, wallet, keys, or a camera. Unfortunately, anything over 6 pounds or so will likely cause you some struggle. What’s more, continuous flow POCs are typically over 10 pounds and need to be rolled behind you using a cart, so these will be off-limits to you if you do a lot of traveling.
Size
In this day and age, most people expect their electronic devices to be small and easy to carry. As computers get smaller, we’re able to have more power in the palm of our hands than ever before — this is no different when it comes to portable oxygen concentrators.
Before the 1970s compressed oxygen tanks were the only means of oxygen delivery. These tanks were not only bulky and oversized, but they had an awkward shape to them that made them difficult or impossible to transport. As the need for portable oxygen arose, people began to realize that a different type of oxygen delivery would be needed. Oxygen concentrators became popular around this time because they have an infinite source of oxygen as long as there’s a battery for it to run on. As batteries improved, oxygen concentrators improved with them.

The two smallest portable oxygen concentrators currently on the market are the Inogen One G4 and the AirSep Focus, both of which are small enough to fit in a purse! While we don’t recommend purchasing a POC solely based on its size, the benefits of small portable oxygen concentrators are undeniable. You’ll be able to hold the device at your side more easily, store it in tight areas, and take it into crowded areas such as public transportation without bumping into people.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Sound Level
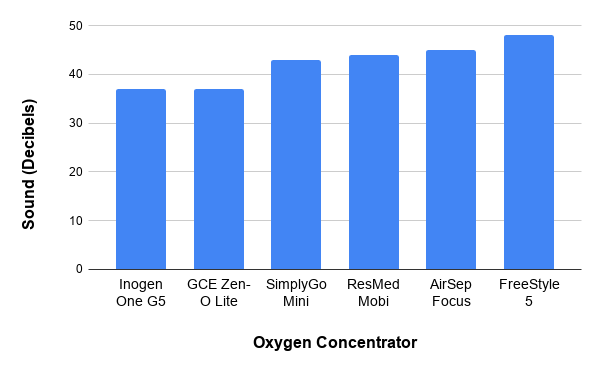
Typically, one of the first questions people have when transitioning from oxygen tanks is “do portable oxygen concentrators make noise?” The answer to that question is “yes.” However, chances are, they make a lot less noise than you think they do. In general, oxygen concentrators range in noise emission from around 37 decibels (dBA) to around 50 dBA, but most pulse flow portable oxygen concentrators are around 40 dBA or below. To put this into perspective, this is about the noise level of a quiet conversation or whisper even.
In the grand scheme of things, using a portable oxygen concentrator will afford you the same freedom as an oxygen tank. You’ll still be able to go to church, a quiet library, or see a movie without disturbing anyone. However, it’s important to note that many POCs have something called audible alerts. These are beeps and other sound effects that notify you when your oxygen machine is low on battery or it’s in need of some other type of maintenance. It’s a good idea to turn these notifications off before you go anywhere in order to avoid any disturbances. If you don’t know how to do this, be sure to consult your user manual or speak with a respiratory specialist.
Warranty
A warranty is a written agreement that the oxygen manufacturer will repair or replace an oxygen unit within a given amount of time. Many electronic devices have warranties available for them and they’re a great way to protect your purchase in the event that you drop it or something malfunctions unexpectedly. Due to the reliability of modern portable oxygen concentrators, most reputable brands like Inogen, AirSep, Caire, and GCE will offer a free 3-year warranty that comes with the purchase of the device. Most of them will allow you to extend to a 4- or 5-year warranty for a set charge.

It’s not common for manufacturers to give out free warranties on their devices, especially one as long as 3 years. If they ever have to replace the machine entirely, they may be doing it at a loss, so the fact that they give such a great warranty is a sign that the oxygen device is extremely reliable and the manufacturers themselves have a lot of confidence in it. However, no matter if your POC malfunctions on its own or you dropped it, you’ll rest easy knowing you have that safety blanket.
FAA Approval
The Federal Aviation Administration (FAA) oversees all safety regulations pertaining to in-flight oxygen use. In the past, there was no such thing as an “FAA Approved oxygen device” because oxygen tanks were too bulky and dangerous to use on a plane. However, since the early 2000s, the majority of portable oxygen concentrators have been approved for in-flight use. What’s more, the United States Department of Transportation (DOT) ruled that on flights of more than 19 seats, air carriers must allow those with disabilities to use FAA approved portable oxygen concentrators.
.jpg)
When it comes to flying comfortably and with ease, pulse flow portable oxygen concentrators are the way to go. As opposed to continuous flow units that can weigh upwards of 20 pounds, pulse flow devices can easily be moved around or stored under the seat for takeoff and landing. If you need to get up during the flight to go to the bathroom, you’ll be able to walk down the aisle without bumping into anyone. Although most continuous flow POCs are FAA approved, you’ll have a much harder time trying to travel with one especially when it comes to flying.
Additional Features
At this point, you’re probably wondering “what else could portable oxygen concentrators possibly offer?” Fortunately, several oxygen manufacturers have gone above and beyond when it comes to providing you with the best device for managing your condition. The Inogen One G5 is one example with its new Inogen Connect application. When you download it onto your smartphone or tablet, you can connect it to your Inogen One G5 via Bluetooth and see up-to-date information about its battery life, column status, and much more.

Another example is the CAIREView™ Telehealth Technology which comes equipped with each Freestyle Comfort POC device. Telehealth technology is defined as a device that enables patients to receive health-related services through a digital medium. CAIREView keeps track of important information on your machine like oxygen usage, flow setting, as well as device integrity and relays this information to the oxygen manufacturer so they can ensure you’re using the machine properly. What’s more, they can even troubleshoot minor issues remotely so you don’t have to send it in to have it repaired.
Conclusion
Choosing a portable oxygen concentrator isn’t always easy especially if you’ve never bought one before. Above all else, you need to make sure that your POC meets your oxygen needs, is light enough to carry, and provides you with a long battery life. Pulse flow POCs tend to meet these standards more easily because they are more technologically advanced than their continuous flow counterparts.
Secondly, you should take other factors into consideration such as sound level, warranty, FAA approval, and additional features. This will allow you to pinpoint a POC that matches your lifestyle that you will enjoy for years to come. If you have any questions about anything you read here, you can feel free to reach out to one of our respiratory specialists who will ensure you get the POC you want and need. Fill out the contact form at the side of the page to get started.
.png)
In the 21st century, we are highly dependent on energy sources like natural gas and electricity. We use fuel to power our cars, cook and heat our homes, and we use electricity to charge our phones, computers, and more. But what happens when we lose access to these resources due to a natural disaster or some other problem? In some situations, this can be a minor nuisance; but in others, it could be life-threatening.
Fortunately, hospitals and other medical facilities have back-up generators that allow them to use life-saving medical equipment even in the event of a power outage. But what about individuals living at home who are reliant on electronic devices? What safety measures are in place to ensure these people are able to use the medical devices they need to stay healthy?
The truth is that there aren’t many safety nets in place to help people experiencing power outages, so this is why it’s always important to be prepared, especially if you depend on electricity to power your medical equipment. In this post, we are going to highlight all the steps you should take to be prepared for a power outage if you have COPD or any other chronic respiratory disease.
What Causes Power Outages?
Before we can discuss the different ways to plan for power outages, it’s important to understand what actually causes them. According to the U.S. Energy Information Administration, the average household experienced one outage in 2016, accounting for 112 minutes of lost power. Although this is the average, this does not mean that power outages cannot last longer. Depending on what causes the power outage, they could last anywhere between several days and several weeks. So you should always plan for the worst-case scenario.

According to Constellation, the most common cause of power outages are severe weather and natural disasters. High winds, snowstorms, and thunderstorms can all knock power lines over causing entire neighborhoods to lose power. Extreme temperatures can also lead to power outages if it results in people overusing their air conditioners or heaters. There are so many different variables that come into play, so it’s best to always be prepared for an outage, regardless of the time of year and what the weather is like.
Install an Emergency Power System
The first thing you should do to prepare for power outages is to have an emergency power system in your home. There are many different options for powering your home in the event of an emergency, so you will have to do a lot of research to determine which one will best meet your needs. However, a good place to start is by contacting your utility company. Some utility companies provide backup generators for people with medical conditions free-of-charge. Others may add an additional fee to your monthly utility bills. Below are some of the most widely used emergency power supplies:
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Home Backup Generators
A home backup generator, also known as a standby generator, is a permanent power generator that is installed outside of your home. These generators resemble air conditioning units and they run off of your existing natural gas or LP fuel supply. While home backup generators are the most costly option for backup power, they are also the most convenient and reliable. These units are designed to turn on automatically when a power outage is detected, so you won’t have to go outside to turn it on. Since these generators are permanent, they will give your home’s value a nice boost if you ever decide to sell it. As you can imagine, home backup generators are extremely advanced, so you will need to hire a professional to install one for you.

Portable Generators
A portable generator, also known as a recreational generator, is a type of generator that’s commonly used for camping and other outdoor activities. However, they can also be a good way to power your home during a power outage. Unfortunately, these devices don’t start automatically when your power goes out, so you’ll have to go through the hassle of setting it up when your power goes out. What’s more, these units use fossil fuels which can exacerbate your respiratory symptoms, so be sure to never use one inside of your home. The benefit of portable generators is that they are much more affordable than home generators.

Solar Generators
Just like the name suggests, solar generators are powered by the sun. The only scenario where you should purchase a solar generator is if you live in an area that is very sunny to ensure that your generator is fully charged when you need it most. Since these generators don’t burn any fuel, they won’t exacerbate your lung symptoms and they aren’t noisy. Solar generators are fairly expensive but they are worth the price for many people.
Install a Medical Alert System
An emergency alert system is a device designed to alert medical professionals if you experience a medical emergency like a COPD exacerbation or a fall. Each medical alert system comes with a pendant that you wear around your neck and a receiver that plugs into the wall. In the event of an emergency, press the button on the pendant and an ambulance will be dispatched to your home.

What many people don’t know is that many medical alert systems have backup batteries that will kick in if there is a power outage. Generally speaking, most backup batteries will last a day or two, but you should speak with the company that manufactures it to learn the full details. Medical alert systems are an invaluable tool to have when the power goes out so be sure to get one installed as soon as possible.
![]()
Another way to prevent falls when the power goes out is to have a flashlight on hand. Chances are, even if you have a generator in your home, you’re going to want to conserve energy by keeping as many lights off as possible. A flashlight will help you navigate your home safely while doing so.
Keep Backup Batteries or Oxygen Tanks
COPD patients have a variety of options at their disposal when it comes to medical oxygen. Some of the most popular options include oxygen tanks, liquid oxygen tanks, and oxygen concentrators. The one you choose as your “backup” oxygen supply in the event of a power outage will depend on what your needs are.

The most notable benefit of having backup oxygen tanks is that they don’t require electricity in order to operate. Oxygen tanks have compressed oxygen inside them, so all you need to do is connect your nasal cannula and you’ll have access to medical-grade oxygen. However, the downsides of oxygen tanks are that they are very heavy and bulky so you won’t be able to get around your home while you’re using one.
Liquid oxygen tanks work a little differently than normal oxygen tanks. Rather than storing the oxygen as a gas, these tanks store oxygen as a liquid. Since gas is expanded, storing it as a liquid allows you to carry more of it with the same size and weight tank. This will allow you more freedom in the event of a power outage. However, there is one glaring flaw with liquid oxygen tanks which makes them impossible to recommend for this situation. Oxygen needs to be stored at very low temperatures in order to stay as a liquid, so over time liquid oxygen will begin to evaporate, According to the Lung Institute, liquid oxygen will evaporate in a week or two depending on the type of tank you have.
.png)
Last but certainly not least there are oxygen concentrators. Unlike the previous two oxygen devices, concentrators are electronic devices. They work by drawing in ambient air and putting out medical-grade oxygen. It may seem silly to use an electronic oxygen device during a power outage, but you may be surprised to find that they are actually the best backup oxygen device for this situation. Portable oxygen concentrators run off detachable batteries that can be stored for emergencies.

These batteries are also very small and only weigh about a pound so you can store as many as you’d like. One important thing to note is that batteries should be used from time to time in order to help them keep their charge. Be sure to swap out the batteries occasionally so that each one is being used. Let’s take a look at some of the best portable oxygen concentrators to have during a power outage.
Best Oxygen Concentrators for a Power Outage
The Caire FreeStyle Comfort
The FreeStyle Comfort is currently one of the most popular portable oxygen generators on the market. It’s a pulse dose portable oxygen concentrator meaning it has built-in technology that tracks your breathing and only delivers oxygen when you inhale through the nasal cannula. What this means is that it’s able to conserve electricity while still giving you the oxygen you need to stay healthy. With the larger 16-cell battery, the FreeStyle Comfort can run for up to 16 hours on one charge.

The FreeStyle Comfort is one of only a few portable oxygen concentrators that weigh at or under 5 pounds. Additionally, it’s one of the most compact concentrators so you can carry it around on your shoulder with ease. In the event of a power outage, the FreeStyle Comfort will provide you with plenty of battery life, ease-of-use, and mobility. It has a maximum oxygen output of 1,050 milliliters per minute (ml/min).
The Inogen One G5
The Inogen G5 is another pulse dose portable oxygen concentrator under 5 pounds. With the 8-cell battery, the G5 weighs only 4.7 and has a battery duration of 6 ½ hours. The battery life can be doubled with the 16-cell battery affording you up to 13 hours of battery life on one charge. Just like with the FreeStyle Comfort, the batteries are very small and lightweight so you can store as many as you think you’ll need to make it through a power outage.
.png)
One of the great things about the Inogen G5 is the number of accessories there are for it. The G5 external battery charger is very useful if you’re planning for a power outage because it allows you to charge one battery separate from the G5 unit itself. In other words, it allows you to charge your batteries more quickly so that you can always be prepared. Another great accessory to have during a power outage is the DC charging cable. This is a type of cable that allows you to charge your G5 in the car via a cigarette outlet. Keep a DC charging cable in your car so that you’re always prepared if you need to leave the house in a hurry. The best part about this is that you can use your device while it’s charging meaning there will never be an interruption in your oxygen treatment.
The Respironics SimplyGo
The last portable oxygen concentrator we’d like to recommend for power outages is the Respironics SimplyGo. Certain patients are prescribed continuous flow oxygen which is where oxygen is administered irrespective of the user’s breathing rate. When this is the case, the SimplyGo is the lightest and most reliable unit available to you. The SimplyGo has a maximum flow rate of 2 liters per minute (LPM) at it weighs only 10 pounds which is significantly lighter than most continuous flow POCs on the market. Unfortunately, the SimplyGo offers significantly less battery life than the aforementioned POCs, so you may need to keep even more batteries charged.

Create a List of Contacts
Having a convenient list of contacts you can call during a power outage is very important. You don’t want to be searching the internet using what little electricity you have to find out the number of your utility company or your neighbor’s phone number. Take some time right now to write down your contacts so that you don’t have to do it when an emergency occurs.

Firstly, you should write down the numbers of a couple of friends or family members who could come pick you up if your power is out. Secondly, you should have your doctor or pulmonologist’s number as well as the closest medical oxygen company. If you happen to run out of oxygen for one reason or another you can reach out to them and have them deliver some oxygen tanks. Lastly, don’t forget to write down the number of your utility company. Be sure to call them immediately when the power goes out so that you can plan accordingly.
Keep Non-Perishable Food in Your Home
One of the most notorious issues with power outages is that all of the food in your fridge will begin to spoil. This can be absolutely devastating if you like to keep your fridge well-stocked with lots of food and beverages. It’s a good idea to get in the habit of buying healthy non-perishable food at the grocery store that can hold you over if you experience a power outage. Apples are a great source of energy and they will stay fresh for up to a week while sitting on the counter. However, be sure to ask your doctor about non-perishable foods that are healthy for COPD patients.
.jpg)
Speak With Your Doctor
Last but certainly not least, you can and should speak with your doctor about managing your COPD during a power outage. Your doctor might have some helpful information or resources for you to refer to. Most likely, he/she will tell you the minimum flow rate you’re allowed to use on your oxygen tank or concentrator in order to maintain your blood oxygen levels. Also, be sure to ask your doctor if it’s okay to cease your pulmonary rehabilitation routine while the power is out so that you can conserve your oxygen supply.

Conclusion
While it’s rare to experience a power outage that lasts more than a couple of hours, it’s crucial that you are prepared for the worst-case scenario. Studies have shown that power outages are associated with a greater risk of exacerbation and hospitalization in COPD patients. Ensuring that you always have access to a dependable medical oxygen supply will help you to stabilize your respiratory condition.
What’s more, you should work together with your doctor to create a power outage action plan. You may be able to reduce your oxygen flow rate in order to conserve your oxygen concentrator battery life during a prolonged power outage. And ideally, you’ll have some sort of backup generator that you can use to hold you over until the electricity returns to your home.
Here at LPT Medical, we can help you prepare for power outages by providing you with a durable and reliable portable oxygen concentrator like the Caire FreeStyle Comfort or the Inogen One G5. While we can’t guarantee that your battery will last the duration of the outage, we can help you find the best concentrator for your needs. Please don’t hesitate to reach out to us either by email or by phone.
Oxygen concentrators are one of the most reliable and effective treatments for COPD, pneumonia, cystic fibrosis and a host of other medical conditions. But like any other machine on the market, oxygen concentrators and portable oxygen concentrators can malfunction. The great news is that there is a host of helpful information out there to get your device working for you again.
If you try fixing your own device to no avail, you can always ask a loved one for a helping hand. There are also online forums where you can speak with other people undergoing oxygen therapy or you can always consult the user manual for detailed information on your product.
However, it can still be confusing trying to keep up with all the changes going on in the oxygen therapy field so we’re going to do our best to provide you with a comprehensive guide on fixing some of the most common malfunctions with modern oxygen concentrators.
If you purchase a new device or a new concentrator releases, be sure to check back here as we’ll update it with the most current and relevant information you need to know.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Common Oxygen Concentrator Errors
Probably the most important thing to note when troubleshooting an oxygen concentrator is that it’s not the same as an oxygen tank. Whereas oxygen tanks are purely mechanical, an oxygen concentrator has electrical components that need to work in order for oxygen to come out of the device.
What this means is that if your device suddenly stops working, it could be due to a temporary glitch in the system that can be fixed easily and without a significant amount of technical knowledge of the device. Let’s take a look at some of the most common errors and how to fix them easily.
No Breath Error
If you’re using a full battery but end up getting a “no breath” error on your oxygen concentrator control panel, there are several things that may be causing this. The “no breath” error typically occurs when your device hasn’t detected a breath for a certain period of time, so if you’ve been using it, you should check to make sure there are no kinks in the cannula tubing and that the cannula is connected to the concentrator.

This error may also result if your cannula isn’t positioned properly in your nose. Although you can position the nasal cannula prongs up or down in the nose, they should be facing down in order to have the best results and to ensure that oxygen is sent directly into the nasal canal.
Oxygen Error
Since oxygen concentrators don’t have an oxygen tank on them, they draw ambient air and turn it into pure oxygen. This happens in a five step process:
- Taking in ambient air
- Compressing the oxygen
- Removing oxygen from the air
- Adjusting the flow rate
- Delivering purified air
If your device runs into an issue with any step in this process, you may be given an oxygen error indicating that oxygen output is low or isn’t working as it should. Although this could be a complex issue with the device, you should try turning it off and on again to see if the error message goes away.

 Battery Won’t Charge
Battery Won’t Charge
If your battery won’t hold a charge or your oxygen concentrator won’t turn on, you should make sure the power cable is plugged in correctly. If it is, you should use another electrical device to try the outlet and make sure it’s working. And if it does, there may be a problem with your charging cable or the battery in your device. You can also try taking the battery pack off of your concentrator and putting it back on and checking to ensure it isn’t loose.

Oxygen Purity Error
Another important function of your oxygen concentrator is to purify the air that you breathe through your cannula. Breathing clean air is crucial to preventing COPD exacerbations but if your device becomes clogged with airborne particles or the sieve bed quits working, you may get a purity error. Sieve beds generally last a year or so but, amount of use, proper storage and humidity present can reduce its life expectancy.
System Too Hot or Cold
Like all electronic devices, oxygen concentrators need to be kept at a reasonable temperature in order to prevent overheating or becoming too cold for use. If not, you may get an error on your control panel or an audible notification or the device may simply shut off. Make sure that all air intakes and outputs are free of obstruction and try switching out your battery if one gets too hot.

Troubleshooting Checklist
Before you contact your equipment provider, there are a few things you can try, no matter what error or symptom you’re experiencing. Follow this checklist to see if it fixes your device.
Perform a hard reset
Turn the oxygen concentrator off and unplug it from the wall. Remove the battery pack and leave it for 30 minutes. After the allotted time, plug it back into the wall, turn it on, and put the battery pack in after 10 minutes.
- Check all vents and your cannula to ensure they aren’t obstructed
- Ensure your battery isn’t loose or try replacing it with a backup
- Check for physical damage on the system or the battery
- Research any error message in your device manual
- Take note of the error code and frequency of the issue you’re experiencing
If you should need to contact the equipment provider for assistance, the error code or symbol will help them identify what is causing the issue.
General Operating Guidelines
In order to prevent errors in the future, you should follow your oxygen concentrator’s best practices. Although every oxygen concentrator or portable oxygen concentrator is different, there are some general rules of thumb that you should follow. Be sure to consult your user manual for more specific information about maintaining your device and contact your equipment provider if you have any further questions.
Storing Your Concentrator
Oxygen concentrators should be stored in an environment that is not too cold, too hot, or too humid. Concentrators that are stored in these environments for a prolonged period of time may experience damage to their internal components and may not work.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Don’t Smoke Around It
It’s generally safe to assume that any airborne pollutants will be bad for your oxygen concentrator and this is especially true when it comes to smoking. If smoke enters the vents on the device it could damage internal components and cause your sieve beds to wear down more quickly. If you’re setting the device on the floor, make sure it’s in a clean area without a lot of dust or dirt.

Troubleshoot Before Leaving Your Home
If you have a portable oxygen concentrator, it’s generally best to troubleshoot any issues before leaving the home. Although your device may still be working after an error message appears, it may stop working when you’re out and about and need it most.
Replace Your Filter
Some concentrators have a gross particle filter that catches a lot of airborne particles like dust and dirt. It’s important that you replace this filter after a year or so in order to prevent breathing in impure air and keep your device running smoothly. You should also clean it every month with a gentle household detergent and water.

Replace Your Nasal Cannula
After a month or two of use, your cannula may become worn, kinked, and otherwise inefficient. Not only can a worn cannula lead to errors on your oxygen concentrator but you may not be receiving as much oxygen that you should if there is a leak or the tube is bent. You should inspect and clean your nasal cannula tubing regularly to prevent this.

Fully Charge and Deplete Your Batteries
Your oxygen concentrator batteries will last longer if you charge them up fully and then deplete them fully at least once a month. Just like with your phone or laptop, you should try to avoid charging your oxygen concentrator batteries multiple times a day. And if you have an extra battery pack, be sure to swap it out with your main one every once in a while so it gets some use.
Ask For Help
Above all, you should never wait to get your questions answered about your oxygen concentrator. Although they’re usually very reliable, getting your device fixed sooner rather than later will ensure it lasts as long as possible. Keep your equipment suppliers phone number on hand to ensure you always have someone to go to if your device isn’t working.
Conclusion
Home and portable oxygen concentrators have come a long way in a short time. While this means you have access to a high-tech oxygen therapy device wherever you need it, you may find it difficult to get the information you need to maintain your device and fix errors.
If the issue you’re experiencing wasn’t discussed here be sure to consult your device manual or contact your equipment provider. If you have a caregiver, he/she will help you maintain and clean your oxygen concentrator and troubleshoot any errors. Online COPD forums are also a great place to speak with other people who may be experiencing the same issues with their device.
If you have COPD, the first sign that something was not right was likely feeling shortness of breath, to the point that you wanted to see your doctor about it. It also could have been that incessant cough throughout the day and night.
It's easy to blame a cough on allergies or a common cold, but if it persists and becomes a regular thing, you should see your doctor to discuss the possibility of having COPD or another lung ailment. The sooner you find out if it is COPD causing your symptoms the sooner you will be able to treat the chronic illness, thereby slowing down the progression of your COPD.
The first thing that you need to understand is that coughing may seem like a symptom you want to relieve, but in the case of COPD, it actually serves a function.
Continue reading to understand how COPD and coughing are related, what you can do to ease a cough, and when to seek medical attention.
How are COPD and coughing related
If you have COPD you probably experience a persistent cough. This symptom is related to a condition of COPD called chronic bronchitis, which means that your airways are constantly irritated. This irritation is often caused by smoking or second-hand smoke, but it can also be caused by other irritants and biological factors, such as pollution or genetics.
The irritation in your airways causes two problems that prevent enough air from passing through to the lungs:
- The lining of your airways become swollen
- There is too much mucus produced by your lungs
People with chronic bronchitis can have a persistent cough because it is important to regularly clear their swollen airways of this excess mucus, which can sometimes be difficult and require extra attention and treatments, of which, we will discuss in more detail in the What you can do to ease a cough associated with COPD section of this article.
So, coughing caused by COPD is often productive and it is a natural function of your body that plays an important role in your breathing system. Coughing helps to move extra mucus out from your lungs. Coughing is also a reaction that can help remove certain irritants you may inhale into your lungs, like dust, pollution, and other common allergens.
When your cough produces mucus, which is also called sputum or phlegm, that means your body is working correctly to clear the excess mucus up through your swollen airways and into your throat and out of your mouth.
It is normal for the mucus to be clear or white, yellow, or green in color but if the mucus is very mucky, it may be a sign of a respiratory infection. We will go over this in more detail in the When you should see a doctor section
What you can do to ease a cough associated with COPD
To determine whether or not your cough needs to be treated with medication or other remedies, depends on the type of cough you are experiencing and whether or not your cough is actually helping to clear your lungs and airways.
You should consult with your doctor to determine the type of cough you are experiencing and how to deal with it going forward.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
As we discussed in the section above, airway clearing coughs serves a meaningful purpose by clearing out mucus from your airways. In this case, it is best for you to continue coughing in order to avoid mucus building up in your lungs.
.png)
That being said, there are certain medications you can take as well as techniques you can learn how to perform in order to couch more effectively.
COPD and coughing medications
If your cough is due to very thick mucus, first you should try to drink more fluids. This can help make your mucus thinner and easier to clear. If this does not work well enough, then there are medicines called “expectorants” that can help make the mucus easier to cough up.
If your coughing becomes painful or difficult to control. In those cases, your doctor might recommend cough suppressants that keeps your body from coughing. These suppressants might also be used for coughs that do not produce mucus, like a dry smoker’s cough.
If you have COPD, coughing can also cause a “bronchospasm” or “spasm.” This happens when your muscles around your airways suddenly tense up causing your airways to become very narrow, This makes it even hard to breathe. To reduce coughing that causes spasms, healthcare providers might prescribe special types of inhaled medications called “bronchodilators” or inhaled steroids.
.png)
If you are not interested in getting on medication for you coughing, there are also three airways clearing techniques you can do to clear your lungs
Airway clearing techniques for COPD
One of the most effective ways to clear your airways is to use the effective, or controlled, cough technique. This cough comes from deep within your lungs and has just enough force to loosen and carry mucus through your airways without causing them to narrow or collapse. By utilizing the controlled coughing practice, you will save energy and therefore, oxygen.
- Controlled coughing: A type of cough that comes from deep in your lungs. It loosens mucus and moves it though your airways
- Postural drainage: You lie down in different positions to help drain mucus from your lungs
- Chest percussion: You lightly tap your chest and back. The tapping loosens the mucus in your lungs
To cough effectively:
- Sit on a chair or on the edge of your bed, with both feet on the floor. Lean slightly forward. Relax
- Fold your arms across your abdomen and breathe in slowly through your nose. (The power of the cough comes from moving air.)
- To exhale: lean forward, pressing your arms against your abdomen. Cough 2-3* times through a slightly open mouth. Coughs should be short and sharp. The first cough loosens the mucus and moves it through the airways. The second and third cough enables you to cough the mucus up and out.
- Breathe in again by "sniffing" slowly and gently through your nose. This gentle breath helps prevent mucus from moving back down your airways
- Rest
- Perform again if needed
Here is a link to postural drainage and chest percussion treatment and how to perform these mucus clearing techniques.

Natural home remedies for helping reduce COPD induced coughing
Eucalyptus oil
Eucalyptus oil contains a natural compound called eucalyptol. Eucalyptol may have the following benefits for people with COPD and may ease uncomfortable coughing symptoms:
- antioxidant and anti-inflammatory properties
- opens up the airways in the lungs
- reduces mucus production
- helps clear mucus from the lungs
- prevents flare-ups in moderate to severe COPD
One way you can use eucalyptus oil is by adding 12 drops of eucalyptus oil to 150 milliliters of boiling water and inhaling up to three times per day.
This will not work for everyone, and if you experience any side effect of the oil, stop using it immediately.
-1.png)
Quit Smoking to reduce dry coughing
Smoking is the leading cause of COPD in the United States and is responsible for around 90 percent of COPD-related deaths.
Tobacco smoke is known to irritate your airways and your lungs. Smoke causes inflammation and obstruction within your airways causing them to narrow, and making it very difficult for air to pass in and out.
If you smoke, the most important step to reduce COPD related symptoms and slowing down the progression of your COPD is to stop smoking. Quitting will put an end to “smoker’s cough,” the dry, hacking cough common among people who smoke.
A deep, productive cough that clears the airways of mucus may replace this dry cough also benefiting you and your breathing.
-png.png)
When you should seek medical attention
Call your doctor within 24 hours if you notice:
- You’re out of breath or coughing more than usual
- Being out of breath affects your daily routine
- You’re coughing up more gunk that normal
- The mucus you are coughing up is dark yellow, dark green, or rust-colored
- You have a fever over 101 F
- You feel dizzy or lightheaded
If you begin to experience any of these symptoms it could mean that you have a respiratory infection or your COPD is getting worse.
Call 911 or go to the emergency room if you’re still out of breath after using the medicines your doctor has prescribed for your COPD.

Other symptoms associated with COPD
One of the other many symptoms of COPD we mentioned very briefly in this article was shortness of breath. When you have COPD your lungs are no longer able to process oxygen like they once did. This is partly due to the irritation in your airways that also causes coughing.
Both chronic bronchitis and emphysema can cause shortness of breath. This symptom is also called “breathlessness” or “dyspnea".
If you airways are swollen and filled with mucus, not only does this initiated a coughing reaction, but it also inhibits oxygen from flowing through your lungs and into your blood stream and organs.
Not only is this feeling extremely uncomfortable, it is also life threatening, and if it goes untreated for a long period of time, you will inevitably be taking years off of your life.
Here are positive changes you can make to improve breathing with COPD:
Learn pursed-lip breathing This is a breathing exercise designed for people with COPD: Purse your lips and blow as much air out as you can before taking a deep breath in through your pursed lips again. Then slow down your breath so that you’re using as much of your lungs as you can. This technique slows your breathing rate and helps to keep your airways open which can also help to reduced coughing episodes.
Drink plenty of water because water helps thin out mucus so you can clear it better. Some people with COPD have conditions that could be made worse by extra fluid, however some people with COPD may be very dehydrated.Speak with your doctor to find out how much water you can safely drink.
Get informed and continue learning about COPD and how your lungs function. This can help you better understand and manage your condition. Pulmonary rehabilitation programs often offer this type of education.
Exercising regularly can make a big difference in your breathing capabilities and COPD symptoms. A lot of people with COPD get more and more out of breath as their disease progresses, but it’s not due of their lung function — it's because they’re not conditioning enough. Most doctors recommend walking for people with COPD since it’s moderate in intensity and easily accessible.
Know and avoid your triggers. If you have COPD and allergies, take steps to avoid anything you’re allergic to. This may mean putting dust covers on your pillows and mattress or keeping your pets out of the bedroom. High-efficiency particulate air filters can remove dust and other irritants from the air in your home. You may also consider a humidifier if dry air triggers your symptoms.
Get your rest Many people with COPD have an underlying sleep disorder, like sleep apnea, that makes it difficult to get good sleep. When you sleep better, you’ll feel better and breathe better, so if you are not able to fall asleep, or have trouble staying asleep, speak with your doctor to understand the root of this issue so you can solve it.

Stay on a healthy diet full of nutrient-dense foods is needed with COPD to maintain strength and fight off infections. Eating healthy can help you lose weight and breathe easier. If you’re underweight, ask your doctor about the best foods to eat and if nutritional supplements are right for you.
Take your medication COPD medications can help manage symptoms, including shortness of breath so be sure you’re taking the right medications and get evaluated to make sure your lung function is as good as it can be
If you have severely low oxygen levels this is called hypoxemia, your doctor will likely prescribe you medical-grade oxygen, for home oxygen therapy. Long-term oxygen therapy has many benefits if it is used correctly and It can even help you live longer.

- Confusion
- A sense of euphoria
- Restlessness
- Headache
- Shortness of breath
- Rapid breathing
- Dizziness, lightheadedness and/or fainting spells
- Lack of coordination
- Rapid heart rate
- Elevated blood pressure
- Visual disturbances
- A bluish tint to the lips, earlobes, and/or nail beds (cyanosis)
Hypoxemia is the main reason that people with COPD and other lung diseases are prescribed supplemental oxygen. There are a few forms of home oxygen therapy: You can opt for liquid oxygen tanks, gas cylinder tanks, or the most popular, convenient, and cheapest option a portable oxygen concentrator.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
If you are a good candidate for long-term oxygen therapy, this is a blessing in disguise. While it might seem as if you lung function is declining, once you are able to utilize oxygen, your quality of life will improve drastically. When you have adjusted to the oxygen therapy, you will begin to slow the progression of you COPD as well!
Once you find the right POC for you, your bones and muscles will feel stronger and energized, you will have improved exercise tolerance, your mood and stamina will boost, your quality of sleep may improve, and so much more.

If you feel like you have experienced any of the symptoms of hypoxemia, and are curious how to find the best portable oxygen concentrator to fit you oxygen requirements, fill out the blue box to the right, it is our official guide to portable oxygen concentrators.
Cough with a Purpose
Remember, COPD-related lung damage can’t be reversed, but it can be controlled if treated properly.
We hope you and your caregivers understand more about COPD and coughing, and how avoiding coughing is not always the best option.
Now that you understand that your cough can in fact be beneficial for your health while treating COPD, we hope that you can use the information in this article to cough effectively and efficiently. These coughing techniques, mixed with medication and other home remedies should reduce the dry uncomfortable smokers cough, and influence you to cough with a purpose.
Even though this can be a pain, always feel free to excuse yourself during social gatherings, and other outings to clear mucus from your lungs and airways. This will allow you to go longer without coughing and spend more quality time with the ones you love while enjoying the things you like to do.
The more you practice these coughing techniques the more efficient you will become at clearing your airways, and therefore breathing!
If you have any questions please leave a comment on this blog below, and always feel free to share our blog with your friends and family. By explaining how beneficial your cough is for managing your COPD, they will better understand and be willing to help and encourage coughing rather than trying to help you avoid it.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













