Living with a serious disease like COPD can be scary, stressful, and sometimes even overwhelming. Just the feeling of shortness of breath, the main symptom of COPD, can be a very frightening sensation.
Feeling anxious, overwhelmed, and even depressed is a natural and, to an extent, even a healthy reaction to getting diagnosed with a chronic disease. However, you shouldn't let these negative feelings control your life.
If you don't take steps to manage your anxiety and fears they can end up taking a huge toll on your emotional and physical health. It's okay to feel anxious and depressed sometimes, but it's also important to learn to manage and minimize your stress.
In this article we'll help you better understand the effects of chronic anxiety and how to manage it while living with COPD. We'll show you a variety of effective relaxation techniques, breathing exercises, and lifestyle changes you can use to help you navigate the difficult emotional aspects of COPD.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Understanding The Emotional Impact of COPD

Everyone experiences feelings of depression and anxiety from time to time. It happens as a natural reaction to unfortunate events and the troubles of everyday life.
However, nothing can truly prepare you for the emotional effects of getting diagnosed with a disease like COPD. Negative emotions like fear, anxiety, worry, and guilt can easily get out of hand if you don't learn how to manage them in healthy ways.
Here are some common emotional reactions people experience after getting diagnosed with COPD:
- Anxiety and panic
- Depression
- Anger
- Fear and worry
- Grief
- Helplessness
- Frustration
- Guilt and remorse
- Feeling loss of control
As you can see, living with a chronic disease can be an immense emotional challenge. The good news is that it often gets better after you have time to adjust and get used to your treatment plan.
It is normal to feel a great deal of fear, stress, and guilt at first, but you can take back control over your physical and mental health by giving yourself time to adjust and make the life changes necessary to stay healthy. You will also find your disease much easier to manage if you seek support from friends and family and practice healthy coping mechanisms and relaxation techniques.
If you are able to manage the emotional aspects of your disease, it will become much easier to manage your symptoms, live a healthy lifestyle, and follow your treatment plan. That's why it's so important for people with COPD to learn how to manage negative emotions and practice habits that foster a positive mindset.
In the following sections we'll show you a variety of tips and techniques to help you feel better and manage the difficult emotional aspects of COPD. But first, we'll discuss how to recognize the signs of anxiety and depression and how to break out of negative thought cycles related to COPD.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Recognizing the Signs of Anxiety

Anxiety is often associated with the “fight or flight” response, an instinctual reaction that all humans experience when confronted with danger. In many cases anxiety actually serves a practical purpose; it helps prepare us to recognize and respond to real threats.
However, anxiety becomes a problem when it happens too often and won't go away. This happens when we feel anxiety in response to things that are not real, immediate threats, like worrying over an argument or feeling anxious about the future.
Since there's no solution or easy “off” switch when you worry about these types of things, sometimes the anxiety just doesn't go away. It's easy to get caught in negative thought loops where you worry about the same things over and over again when there's no actual purpose or use for dwelling on those worries all.
It's common to feel anxiety in response to thoughts, fears, and situations that are out of your control, especially when you suffer from a chronic health condition like COPD. It's important to be able to recognize these feelings of anxiety because when you know they're there, you can actually do something about it.
Here are some of the immediate physical effects of anxiety you should learn to recognize:
- Rapid breathing
- Rapid heart rate
- Nausea
- Shortness of breath
- Sweating
- Paleness or flushing
- Stiff, tensed muscles
- Twitching or trembling
- A tight feeling in your throat
- Dry throat
Anxiety can also have less obvious physical effects in the short term that can affect your COPD:
- Re-distribution of fluids throughout your body (and your lungs, which can affect breathing)
- Increased blood sugar (because it triggers extra glucose production in the liver)
- Increased blood flow throughout your body
As you can see, all of these different anxiety symptoms can affect your breathing and your COPD. Anxiety affects your heart rate, breathing rate, water distribution, and breathing muscles, all of which affect your respiratory system and together can make your COPD symptoms even worse.
If left untreated, chronic anxiety can even cause more serious health complications that are particularly dangerous for people who have COPD. Long-term anxiety can suppress your immune system, affect your short-term memory, cause problems with digestion, and even increase your risk for premature heart disease.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Breaking Out of The Negative Feedback Cycle of Anxiety
|
|
| Image courtesy of Fayez on Flickr. |
Because the physical effects of anxiety often mimic or exacerbate symptoms of COPD, bouts of acute anxiety can quickly spiral out of control. You might start out feeling a little bit stressed out, but when the anxiety symptoms kick in it can be difficult to stay calm and control your breathing.
The cycle happens like this:
- You start to feel stress or anxiety
- The anxiety makes your throat tighten and increases your breathing rate, making you feel short of breath.
- Feeling short of breath inspires even more fear and anxiety, causing your heart to race even faster.
- Your increased heart rate and muscle tension makes it even more difficult to breathe, which inspires more anxiety... and the cycle continues on.
When you get stuck in this feedback loop, it can be difficult to calm down enough to pull yourself out of it. It becomes easy to confuse symptoms of anxiety with symptoms of COPD, and you can't manage your anxiety if you don't realize that it is what's causing your physical symptoms.
In these situations, breathing exercises and relaxation techniques are the most effective ways to bring your anxiety and physical symptoms back under control. However, the best solution is to learn how to recognize the early signs of anxiety so you can get a handle on it before the negative cycle starts.
The Negative Feedback Cycle of Depression

Feeling depressed can also start a negative feedback loop that can be detrimental to your health. This happens when depression snuffs out your energy and motivation, leading to habits and behaviors that continue to make your depression, and your COPD, worse.
Here are some of the common symptoms of depression:
- Decreased energy and fatigue
- Feelings of sadness, anxiety, and emptiness
- Feelings of helplessness, worthlessness, or guilt
- Pessimism, cynicism, and hopelessness
- Restlessness and irritability
- Loss of interest in hobbies, exercise, and other activities
- Changes in eating habits (increased or decreased appetite)
- Increase in aches and pains, headaches, and other physical ailments
- Reduced ability to focus and concentrate
The negative feedback loop of depression begins with feelings of hopelessness and helplessness that cause you to give up on healthy habits and treatment goals. When you're depressed, you're likely to give up and avoid activities when you feel breathlessness or other symptoms of COPD, which only leads to even worse symptoms and fuels further depression.
It's important to familiarize yourself with the symptoms of depression so you can address it and manage it if it occurs. It's also important to recognize the unhealthy habits that start the negative feedback loop of depression so you can take care of it before it spirals too far and takes a permanent toll on your health.

Here's what the negative feedback loop of depression looks like:
- You feel depressed and hopeless because of your disease, so you choose to stay inside and do nothing instead of pursuing hobbies and other activities. You might have difficulty getting out of bed and motivating yourself to continue healthy habits like exercising and cooking healthy meals.
- As a result of being less active, your symptoms get worse and your disease may progress even further. You feel more breathless and fatigued and have even less energy to exercise and do other activities.
- This leads to even more anxiety and depression, which makes you feel even less motivated and less capable of managing your health. As your physical condition declines, it becomes more and more difficult to stay active and causes even more emotional distress.
- This leads to even more depression, more time spent sedentary, and more physical symptoms. If the cycle isn't interrupted, it can make your COPD symptoms irreversibly worse and cause permanent physical decline.
Anxiety and Depression Can Have Long-Term Effects on Your Health
A certain amount of anxiety is healthy, and can even motivate us to take positive actions and make healthy choices. But when anxiety or depression is prolonged, it can have serious negative effects on your body.

Here are some of the long-term effects that chronic anxiety and depression can have on your body:
- Insomnia
- Suppressed immune system
- Reduced ability to focus and problem solve
- Impaired short-term memory
- Reduced sex drive
- Changes in your metabolism
- Indigestion
- Increased susceptibility to stomach ulcers
- Cardiovascular problems
- Nervous system malfunction
This is why it's very important to get support and learn new habits if you suffer from anxiety or depression on a daily basis. If you let it eat away at you for too long, it can have devastating effects on and start an unhealthy, downward spiral of physical and emotional distress.
How to Deal with the Emotional Aspects of COPD
There are many proven and effective methods for dealing with challenging, stressful times such as living with COPD. Relaxation techniques like meditation, breathing exercises, and a variety of other activities can make all the difference when you're dealing with overwhelming emotions.
In this next section, we're going to introduce you to a variety of these techniques that you can use today to help reduce your anxiety, feel better, and gain back control over your life. If you take the time to learn and practice some of these techniques when you feel down or overwhelmed, you can teach yourself to redirect your negative energy to relaxing and calming activities, instead.
Therapeutic Activities for Emotional and Mental Health
Physical Exercise

Staying active and doing physical activities is one of the best ways to keep your mind and body healthy. It's a great way to get rid of extra tension and negative energy, and it can strengthen your breathing muscles and help your COPD symptoms, too.
Regular exercise gives you more energy and strength during the day at the same time that it makes it easier to relax and sleep at night. You'll feel stronger, more confident, and more in control of your health if you get plenty of physical activity.
Here are just a few of the many emotional benefits of exercise:
- Decreased stress and anxiety
- Improved memory and cognition
- Increased energy levels
- Increased ability to focus and problem-solve
- Increased feelings of happiness and well-being
- Better self image and increased self-confidence
- Feelings of satisfaction and accomplishment
- Protection against cognitive decline
- Increased ability to relax and sleep well at night
Along with its quantifiable physical and mental benefits, regular physical activity will help you feel more confident, secure, and give you a wonderful sense of accomplishment.
If you're not used to exercising regularly, work with your doctor to put together an exercise plan that will ease you into the habit. Start small and set realistic goals, and don't push yourself to the point of feeling too breathless or fatigued. At the same time, don't be afraid to challenge yourself and be as active as you can.
If you like structured activities, you can try joining a gym, group sport, or an exercise club. Many gyms offer a variety of classes such as aerobics, yoga, and tai chi that are great for building physical strength as well as practicing relaxation and breathing techniques.
Yoga & Tai Chi

Yoga and Tai Chi are both great physical activities for people with COPD. They are designed to improve your physical strength and endurance while practicing breathing and relaxation techniques at the same time.
Yoga is a slow-paced exercise that involves holding different stretches and poses which can be adjusted for different strength and skill levels and for people with limited mobility. It's incorporation of deep breathing exercises and meditative practices makes it perfect for patients with COPD, and can help you learn how to control your breath when you exercise.
Tai Chi is a more active exercise technique that uses graceful, flowing actions and encourages constant movement. Like yoga, what makes Tai Chi such a great exercise for COPD is that it also teaches deep breathing techniques as an integral part of the practice.
Both of these exercises are great for building physical endurance and deep breathing skills that can help you manage both the physical symptoms and emotional strain associated with COPD. If you'd like to give these exercises a try, you can look for a gym near you that offers group classes.
If you don't want to go to the gym, you can also follow Tai Chi or Yoga instructional videos by yourself in your own home. You can find guided Yoga and Tai Chi video classes in stores, at your library, and even watch them for free on sites like YouTube and elsewhere online.
Mindfulness Meditation

Mindfulness meditation is one of the most highly-researched and effective methods for reducing anxiety and depression. In fact, it's considered to be so effective for mental well-being that it should be the one thing you try even if you don't use any of the other techniques on this list.
Mindfulness meditation isn't anything like the kind of meditation you've probably seen in movies and pop culture. It's actually a very simple and relaxing activity that anyone can do; all it takes is a bit of time and patience to see results.
Practicing mindfulness meditation is all about clearing your mind of worries, letting go of distracting thoughts, and living in the present moment. It helps you learn how to separate yourself from your stress and your anxious thoughts, enjoy life without worry, and achieve a quiet inner peace.
To practice basic mindfulness meditation, you start by finding a quiet, comfortable place to sit and close your eyes. Then, you practice just living and being in the present moment. Let go of any specific thoughts and worries, and instead just focus on your breathing and listen to your thoughts as they go by without judgment.
It can be helpful to listen to a guided meditation audio clip or follow along with a written meditation guide. Mindful.org is a great resource for a variety of textual guides and information on mindfulness meditation, or you use one of UCLA Health's guided audio meditation sessions by visiting their website here.
Keep a Journal

Journaling is a proven and effective way to cope with difficult emotions and challenging times in life. In fact, research shows that journaling is a powerful tool for emotional and physical health, and something everyone should do for their mental well-being.
Journaling allows you to write and sort through your thoughts in an entirely private, safe, and non-judgmental environment. No one else will ever have to know the thoughts you put down; you are writing for just you and you alone.
Your journal can be whatever you want to make of it, but its' most helpful when you use it to better understand yourself, others, and sort through difficult feelings. It can be helpful to keep track of your moods and emotions on a daily basis so you can notice trends and patterns and see how you change and grow.
Here are some tips for a successful journaling experience:
-
Let Go of Your Internal Filter: Don't think about good grammar, good taste, or what anyone else would think about what you write. Try to write quickly and let the words flow, don't analyze them or judge them. The point is to write down raw, pure, honest thoughts, which is impossible to do if you're constantly editing yourself as you write.
-
Journal Every Day: It's easiest to journal regularly if you make it a daily habit. Keep a dedicated journal in an easy-to-access space, and try to set aside at least fifteen minutes of time every evening to write.
- Write About What Matters to You: No one else will see your journal, so you can structure it however you like and write about whatever you want to. Let go of your inner critic and write about whatever comes to mind, or whatever has been on your mind lately.
Practice Breathing Exercises

It can be scary, or even panic-inducing, when you find it difficult to breathe. In fact, it's very common for people who have COPD to experience anxiety during bouts of breathlessness or wheezing.
One of the best defenses against this kind of worry and panic is breathing techniques. Breathing exercises like pursed lips breathing and diaphragmatic breathing are extremely effective and simple ways to calm down and reduce anxiety when you experienced worsened symptoms of COPD.
Most doctors recommend practicing breathing exercises every day, even when you don't feel anxious or breathless. This helps you learn the techniques thoroughly so you can easily remember how to do them in the moment when anxiety and panic strikes.
Diaphragmatic Breathing Technique
Diaphragmatic breathing helps you learn to use your diaphragm instead of your chest muscles to breathe. This allows you to breathe with less effort and can reduce symptoms like chest tightness, breathlessness, and fatigue that often get worse when you feel anxious.
How to Practice Diaphragmatic Breathing
- First, lie on your back in a comfortable position.
- Put one hand on your chest, and the other on your belly.
- Take a deep breath in while trying to breathe from your belly, not your chest. You should feel the hand on your stomach rise while the hand on your chest stays still.
- When you exhale, once again try to push from your stomach instead of your chest. You should feel the hand on your stomach fall as you breathe out while the hand on your chest stays still.
- Repeat until you are successfully breathing from your belly and not your chest. Over time, this will become second nature and you will have better control over your breathing.
Pursed Lips Breathing Technique
Many people with COPD have airways that collapse and lungs that trap air, making it difficult to breathe. Pursed lips breathing helps you open up your airways and push all the air out of your lungs with each breath, which makes it easier and more comfortable to breathe.
How to Practice Pursed Lips Breathing
- Stand or sit in a relaxed position with your back straight.
- Relax your chest muscles and take a deep breath in through your nose lasting about two seconds.
- When you breathe out, purse your lips together (as if you were blowing a kiss) and exhale slowly through your mouth. You should take about twice as long to exhale as you did when you inhaled, about four seconds.
- Repeat several times, or until you feel your breathlessness subside.
Bringing your breathing back under control is the first and most important step to bringing your anxiety and panic back under control, too. Unfortunately, it can be difficult to remember how when you feel anxious or panicked, which is why it's important to practice often.
If you or someone you love suffers from a chronic respiratory disease, you might be curious about supplemental oxygen therapy. Whether you are already using supplemental oxygen or you think that you might need it, it's helpful to learn more about the therapy and the benefits it could have for you.
Oxygen is an effective medication for a variety of chronic respiratory conditions, including COPD and cystic fibrosis. It improves your ability to breathe and can also prevent a variety of serious health conditions, including respiratory failure, heart attacks, dementia, and even death.
Unfortunately, many patients struggle to comply with oxygen therapy and don't use their supplemental oxygen as often as they should. This is partially due to the fact that oxygen therapy can be very uncomfortable to use, especially if you have to use it continuously every day.
But if you are ever prescribed supplemental oxygen, it's vital to be diligent about the therapy and always use it as prescribed, even if it's difficult to get used to at first. You may feel less discouraged, however, if you take the time to fully understand how important the medication is to your health.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
That's why, in this guide, we're going to tell you all about the benefits of supplemental oxygen therapy and what it can do for people with chronic respiratory diseases. We'll show you how it can improve your physical endurance, your ability to breathe, your ability to sleep, and many other factors that affect your quality of life.
Most importantly, we'll show you why it's important to keep up with your oxygen therapy and not give up when you feel discouraged. When you can appreciate supplemental oxygen as the life-improving and life-saving medication it is, it's easier to understand why it's worth the trouble to do.
Supplemental Oxygen 101: What It Is, How it Works, and Why It's Important
Supplemental oxygen therapy helps you breathe better, but it does much more than that. Even though it is just a gas, medical oxygen is actually a potent medication that affects both your cardiovascular system and your lungs.
Before we dive right in to the many benefits of supplemental oxygen therapy, let's take a quick look at how exactly oxygen therapy works. We'll explain how it affects your body in general as well as how it helps people with specific respiratory conditions.
To skip this and jump ahead to the benefits, you can go ahead and click here.
How Does Supplemental Oxygen Therapy Work?

The primary purpose of supplemental oxygen therapy is to improve your ability to breathe. It's an effective way to get more oxygen flowing through your body when your lungs have trouble absorbing enough on their own.
In the most basic sense, oxygen therapy works by taking oxygen from a concentrated source (like an oxygen tank) and delivering it to you via a long, plastic tube. You breathe it in to your lungs through an oxygen mask or a nasal cannula, which is a smaller oxygen delivery device with two short tubes that rest just inside your nostrils.
This works because the air that comes from your oxygen source contains a much higher percentage of oxygen than the air you breathe normally. This means there's more total oxygen available for your lungs to absorb when you inhale.
Your lungs then transfer this oxygen to your blood, where it gets pumped around your body so your different cells and organs can use it. By using supplemental oxygen, you helps ensure that there's enough oxygen available to meet your body's needs.
Oxygen therapy allows you to breathe air that is up to 99 percent pure oxygen. That's a lot of oxygen compared to the proportion in the air you normally breathe, which is about 21 percent.

Oxygen-rich air is easier to breathe and easier for the air sacs in your lungs to absorb. This allows your lungs to work more efficiently and prevents your blood oxygen levels from falling too low.
Healthy lungs generally don't have any problem getting enough oxygen from regular, ambient air, but people who use supplemental oxygen usually don't have healthy lungs. Oxygen therapy is usually only necessary when there's not enough healthy tissue in your lungs to absorb the amount of oxygen your body needs.
This usually happens when a large number of air sacs are unable to function, whether it's caused by permanent lung damage or the effects of a temporary illness. When this happens, providing extra oxygen-rich air allows the functioning lung tissue that's left to absorb more oxygen than it would from the ambient air.
This allows you to breathe more efficiently and get more oxygen molecules into your bloodstream. That is the ultimate goal of supplemental oxygen therapy: to keep your blood oxygen saturation at a healthy level when your lungs can't do it alone.
Who Needs Supplemental Oxygen Therapy?
Because it's basic purpose is general—to help struggling lungs absorb more oxygen—supplemental oxygen can treat a variety of health conditions that affect the lungs. That includes serious respiratory infections that impair the lungs' ability to function, as well as chronic breathing disorders like asthma and COPD.
Doctors prescribe supplemental oxygen therapy for the following health disorders:
- Chronic Obstructive Pulmonary Disease (COPD)
- Pulmonary Fibrosis
- Cystic Fibrosis
- Pneumonia
- Severe Asthma
- Sleep Apnea
Supplemental Oxygen for COPD
Of all the respiratory conditions that require supplemental oxygen, COPD is the most common by far. In fact, nearly 82% of medicare patients on long-term oxygen therapy have COPD.
However, not all people with COPD need supplemental oxygen, and many don't begin oxygen therapy until they reach the later stages of the disease. Doctors usually prescribe oxygen when a COPD patient experiences chronically low blood oxygen levels, known as chronic hypoxemia.
This usually happens when your blood oxygen saturation regularly falls below about 88 to 90 percent (healthy levels are 95% or higher). At this point, oxygen therapy is necessary to bring your blood oxygen saturation back up to healthier levels.

This is important, because chronic hypoxemia is a dangerous health condition that can cause serious damage to your heart and lungs over time. Oxygen can also treat general COPD symptoms by helping you breathe better and keep respiratory symptoms like shortness of breath under control.
Some COPD patients need to use supplemental oxygen 24/7, while others only have to use it during specific activities that cause their blood oxygen levels to drop. For example, some people with COPD only use oxygen when they sleep or do physical activities that strain their lungs.
Sometimes COPD patients need to use oxygen temporarily during emergencies or to help them recover from lung infections or major symptom flare-ups (known as exacerbations). However, once they have to depend on supplemental oxygen for regular disease maintenance, most patients need to continue using it for the rest of their lives.

If you have COPD, you are likely to need oxygen therapy eventually, even if you don't use it right now. Researchers estimate that at least twenty percent of people with COPD use long-term oxygen therapy, and most patients end up using supplemental oxygen at some point during the course of treatment.
People who have cystic fibrosis and pulmonary fibrosis suffer from similar lung problems as people with COPD. They often use supplemental oxygen for the same reasons, including to treat hypoxemia and relieve shortness of breath.
Supplemental Oxygen for Asthma and Lung Infections
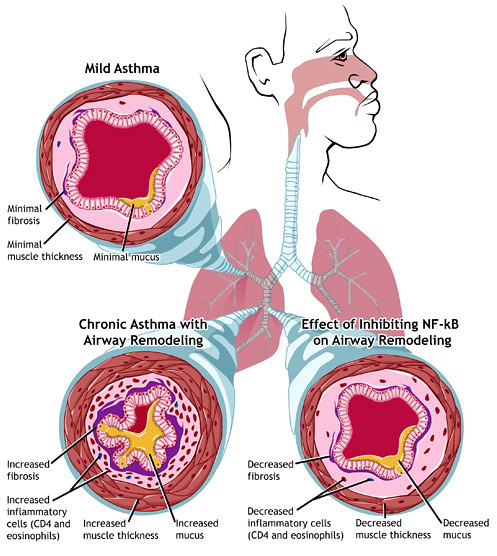
People with asthma usually don't have to use supplemental oxygen regularly like people with COPD. However, some asthma patients may need oxygen therapy to help them breathe during or after a very severe asthma attack.
Asthma attacks are generally the result of severe inflammation in the lungs which can prevent them from absorbing oxygen efficiently. During life-threatening emergencies, supplemental oxygen can help the lungs absorb enough oxygen to prevent serious complications or death.
The same is true for people suffering from severe lung infections like pneumonia. The illness can become so severe that the lungs no longer function sufficiently on their own without the help of supplemental oxygen therapy.
Supplemental Oxygen for Obstructive Sleep Apnea
Obstructive sleep apnea is a common sleeping disorder among healthy adults and among people with asthma and COPD. It occurs when you stop breathing for short periods of time repeatedly during sleep.
This is usually caused by the muscles in your throat relaxing so much that they collapse, blocking air from flowing through your airways. This inhibits your breathing, or makes it stop altogether, for up to minutes at a time, which can deprive your body of oxygen during the night.
This problem can usually be corrected by wearing a special mouthpiece or by using a CPAP or BiPAP machine to keep your airways open while you sleep. However, some people with sleep apnea also use supplemental oxygen to help them breathe easier through the night.
Many experts believe that supplemental oxygen alone is an unnecessary and less effective treatment for sleep apnea, and should only be used in combination with a CPAP/BiPAP machine. Some people with co-occurring sleep apnea and COPD use this combined method to help them maintain healthy blood oxygen saturation levels at night.
The Benefits of Using Supplemental Oxygen
 |
| Photo from rick on Flickr. |
Improves Your Respiratory Symptoms
We've briefly explained already how supplemental oxygen helps you breathe better and helps your lungs absorb more oxygen. We've also mentioned how this can prevent hypoxemia, a condition that occurs when there's not enough enough oxygen in your blood to meet your body's oxygen needs.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What we haven't discussed yet is what effect this can have on the respiratory symptoms you experience every day. Fortunately, studies show that supplemental oxygen can actually help you feel better in general and improve your quality of life.
For example, many studies have shown that that oxygen therapy can improve shortness of breath in people with COPD, especially when used during physical activity. In fact, according to the American Thoracic Society and other researchers, oxygen therapy may be even more effective than bronchodilator medications at reducing shortness of breath caused by COPD.

Other studies have shown that supplemental oxygen can effectively reduce psychological ailments like anxiety and depression, as well as improve health-related quality of life in people with COPD. It can also reduce your chances of experiencing a COPD exacerbation, and help you recover if you do.
By helping you breathe more efficiently and reducing strain on your lungs, supplemental oxygen can help you feel much more comfortable in general. It may also help you feel more safe and secure as you go about your day; you'll know that you always have an oxygen source nearby in case your symptoms flare up and you find yourself struggling to breathe.
You might also find that you have more energy to be active and do everyday tasks when you use supplemental oxygen. Having low blood oxygen makes you feel drowsy and foggy, but these symptoms should at least partially recede when you use oxygen therapy to restore healthier blood oxygen levels.
Reduces Your Risk for Heart Disease and Other Health Complications

Every tissue and organ in your body needs oxygen, which is why hypoxemia is so dangerous to your health. When your blood oxygen levels are low for long periods of time, it can cause a variety of serious health complications.
Left untreated, hypoxemia is extremely hard on both your lungs and your cardiovascular system. This can lead to high blood pressure, pulmonary hypertension, heart failure, and heart attacks. Less commonly, hypoxemia can also cause a rare blood disorder known as secondary polycythemia, which happens when your body creates an excess of red blood cells in an attempt to compensate for low amounts of oxygen in the blood.
However, supplemental oxygen therapy reduces your risk for these health conditions by increasing your blood oxygen saturation. While this may not completely reverse your hypoxemia, it can reduce it by helping your lungs more adequately meet your body's oxygen needs.
Makes Exercise Less Difficult

Without supplemental oxygen, many people with COPD and other chronic respiratory conditions cannot exercise very well on their own. That's because physical strain increases the amount of oxygen your body needs, forcing your lungs to work harder and making it more difficult to breathe.
However, supplemental oxygen works as an aid to help you breathe better when you walk, exercise, or do any kind of physical activity. This can help you get around easier, be more active, and exercise better than you could before.
Here are some of the main ways that supplemental oxygen affects your ability to exercise:
- Improves your exercise tolerance, which is your ability to complete physical activities
- Improves your exercise endurance, which is your ability to walk or do other physical activities for extended periods of time
- Reduces respiratory symptoms and discomfort during exercise
- Allows you to exert yourself harder and do more intense exercises
Oxygen therapy does these things primarily by relieving shortness of breath and keeping your blood oxygen levels up while you exercise. This makes it possible to to exercise longer and do more intense physical activities without having to stop due to breathlessness or fatigue.
When combined with an exercise training program, research shows that supplemental oxygen amplifies the physical benefits, especially the ability to exercise for longer periods of time. Studies show that supplemental oxygen also boosts endurance by improving muscle metabolism and efficiency, which allows your muscles to work harder without getting fatigued.
While many of these studies focus on people with COPD, research shows that these benefits hold true for people with a variety of respiratory diseases, including pulmonary fibrosis and cystic fibrosis.
Overall, supplemental oxygen makes it easier to exercise in general and improves your ability to do more strenuous physical activities that you might otherwise feel too breathless to complete. In this way, supplemental oxygen also makes it easier to build the strength and endurance you need to live a healthy lifestyle in spite of your respiratory symptoms.
This is one of the greatest benefits of supplemental oxygen, because it can help you maintain the physical mobility you need to participate in all kinds of activities and events. It's much easier to do just about everything when you can walk and move around without suffering from debilitating breathing problems.
When you don't get enough physical activity, you can lose your ability to get around and do normal daily activities, which can significantly affect your ability to manage your respiratory disease. But by allowing you to be more active, supplemental oxygen can help prevent this and variety of other complications that can result from inactivity, including heart disease and diabetes.

Getting more exercise sets off a wonderful snowball effect that can improve your health and your quality of life in a variety of ways. It can improve your physical endurance, your breathing efficiency, and make it easier to take care of yourself and maintain your physical independence.
In fact, research shows that exercise training can reduce respiratory symptoms like shortness of breath even more significantly than medication and oxygen therapy alone. By pairing oxygen therapy and exercise training together, you have a powerful tool that can help you stay active, get more fit, and reap the greatest possible benefits from your effort.
If you take the opportunity, the breathing boost you get from supplemental oxygen can help you develop the strength and endurance you need to do more of the things in life that you enjoy. It can also improve your daily life in general by allowing you to go out and about and take care of your health, work, and other life responsibilities more easily.
Improves Alertness and Cognitive Function

Supplemental oxygen therapy can not only improve your physical abilities, but it can also help you think, reason, and remember things better, too. That's because low blood oxygen levels can have subtle effects on the brain that supplement oxygen can correct.
When your blood oxygen saturation is low, it can make you feel foggy-headed, fatigued, and less alert. This can make daily life more difficult to manage and make it harder to keep up with healthy habits like exercise.
Chronic low blood oxygen levels can also lead to a condition known as mild cognitive impairment, which is extremely common in people with respiratory diseases, especially advanced COPD. Mild cognitive impairment affects your memory, your judgment, and increases your risk for psychological symptoms like anxiety and depression.
Mild cognitive impairment is easy to miss, since the symptoms are often very mild. If you aware of it, you're likely to notice that you are more forgetful, make more impulsive decisions, or have trouble focusing your mind on complex tasks.
Fortunately, studies show that using supplemental oxygen can prevent cognitive decline, or at least prevent it from getting worse after it begins. Some studies even suggest that oxygen therapy can reverse the symptoms of mild cognitive impairment by improving blood flow through the brain.
Supplemental oxygen can also prevent mild cognitive decline from progressing to full-blown dementia, as many cases of cognitive impairment tend to do. This is an important benefit, since research shows that people with chronic respiratory diseases lik

Cold weather is right around the corner, depending on where you live, this can be a dreadful time of year for many people. Especially for people with conditions like chronic obstructive pulmonary disease (COPD).
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Low Temperatures and nasty weather can cause COPD symptoms to get worse, which is why you have to be super careful and prepared for winter. The cold and dry air can ignite a flare-up and even require you to go to the hospital. According to a study, temperature extremes, below freezing, are particularly dangerous.
An influx of cold air into the lungs can trigger a number of negative responses in your lungs, and the cold air will narrow your airways.
When this happen you may experience the following symptoms:
- Dyspnea
- Wheezing
- Coughing
- Shallow breathing
- Increased mucus production
- Difficulty clearing airways
All of these symptoms are uncomfortable and can cause a COPD exacerbation and may require you to take a trip to the hospital if your symptoms don't improve.

More snow and frozen sidewalks are just two of the many challenges we face during these winter months. On top of all of this, travel to and from the doctors office is sometimes impossible. Taking care of yourself and taking the necessary precautions during this time is crucial for your health and wellbeing.
If you are an oxygen patient, meaning you have a pulmonary condition that restricts your ability to breathe the proper amount of oxygen into your body, this blog will be a great resource for you to help combat the cold weather and its effects on your body.
We will give you all of the tips and tricks for not only surviving the winter months, but how to create an environment in your home and mind that is nurturing and comforting!
1. Getting Enough Exercise

Exercise is a crucial part of COPD treatment and helps all people with or without respiratory illnesses.
Keeping your lungs strong also helps keep your muscles and bones healthy, so you can live a longer, happier life. In the winter exercise is especially challenging.
![]()
Driving in the snow can be so dangerous, even just walking to your car you risk the chance of slipping on ice. Driving to your pulmonary rehab course or to the gym might not be an option for you in the winter months.
Here are some great alternatives, but check with your doctor before starting an exercise program:
2. Walk

Just about everyone with COPD can walk, even if you don’t exercise much, walking is a great way to start. The best part is that you can do it anywhere, and it is still beneficial. If you have a treadmill, or space in your living room, simply just walking around your home can contribute greatly to your health.
If it seems daunting, start with super small objectives and then add 30 seconds or 10 yards each day. This slow and short pace will still be so good for you.
While walking outside, try breathing through your nose instead of your mouth may also be helpful as this will warm the air before it reaches the lungs.
3. Bike
A stationary bike is a great option for people with COPD, especially when it is too cold or snowy outside to ride a bike outdoors. Being in the privacy of your home can also help a lot of people get over the fear of exercising in front of others, which is very common.

A stationary bike is a safe way for people with COPD to reap the benefits of biking, without venturing too far away from their home. And if you need oxygen therapy, you are able to exercise with your portable oxygen concentrator tanks right next to you without carrying the extra weight with you on the bike.

4. Weighting lifting
Lifting light weights can help you maintain strength so you are able to do everyday things, like reach a high shelf or carry a gallon of milk.

You can order cheap hand weights from amazon, stretchy bands, or just use water bottles or soup cans to try arm curls by following these simple steps:
- Hold the weights at your sides palms forward
- Breathe in
- Lift toward your chest
- Keep elbows down
- Exhale slowly
- Slowly lower your arms back down as you breathe in.
- Build up to two sets of 10-15 repetitions.
any exercise makes you short of breath, stop and sit down for a few minutes.
5. Avoid Oxygen Delivery Delays

Getting your oxygen delivered as an oxygen patient is something that you always have to worry about. In the winter, be weary of delivery delays and other weather impacts in delivery services!
Keep an oxygen canister for emergencies on reserve for if your oxygen refill is delayed.
If you have a portable oxygen concentrator, you will not have to worry about getting your oxygen delivered. Instead you might have to worry about power outages.

Keep an extra oxygen concentrator battery or a charged battery on deck for bad storms where the power potentially goes out. An external battery charger would also be a helpful tool for these situations!
6. Meal Prep and Grocery Shopping
Eating and diet are very important aspects of your COPD treatment. Eating foods that don’t bloat or put more pressure on your lungs is crucial to combat exacerbations and other health related issues.
In the winter, you can meal prep for the week to avoid multiple grocery store trips, and also to maintain a healthy diet. Here are some helpful tips for winter dishes that will help you maintain a healthy weight throughout the winter:
Eat protein-rich foods
Eat high-protein, high quality foods, such as
- grass-fed meat
- pastured poultry & eggs
- fish — particularly oily fish such as salmon, mackerel, and sardines.

Complex carbohydrates
complex carbohydrates are your friend because these foods are also high in fiber. FIber helps improve the function of the digestive system and blood sugar management.
Make a chili or soup with some of the following ingredients:
- peas
- bran
- potatoes with skin
- lentils
- quinoa
- beans
- barley
- fresh produce
You can also do fresh fruits for breakfast but some are more suitable than others, here is a list of some good ones:
- Avocados
- Tomatoes
- Bananas
- Oranges
Vegetables are always a good option, they contain vitamins, minerals, and fiber. These nutrients will help to keep your body healthy, again some vegetables are better than others for people with lung conditions:
- Dark leafy greens
- Asparagus
- Beets
- Potatoes
A healthy diet won’t cure COPD, but eating right will help your body fight off infections, including chest infections that may lead to hospitalization. Avoiding the hospital in the winter and at all times of the year is always the goal. Eating healthfully will help you reach this goal and it will give you energy to exercise and improve your mood too.
7. Get a Face Mask For Keeping Cold Air Out of Your Lungs
![]()
Breathing in the cold air can irritate your lungs, restrict your airways, causing increased symptoms and in some cases exacerbations.
By covering your nose and mouth with a scarf and breathing in through your nose and out through your mouth you will warm the air before it reaches your airways.
A CT Mask is specifically designed for people living with COPD or asthma to help with breathing in cold air while outdoors.
8. Staying Warm Inside Safely

Keeping your home at a comfortable temperature is important, but if you have COPD or asthma, don’t use fireplaces. The wood can cause smoke build-up which can also aggravate your respiratory symptoms.
While you are indoors, the air humidity should be around 40%. If you live in a particularly dry area, you can reach this humidity with a humidifier.
9. Avoid Infections
.jpg)
To reduce your chances of visiting the hospital this winter, avoid infections. You can do this by washing your hands often and thoroughly. And to make sure you stay up-to-date on recommended vaccinations, especially for the flu and pneumonia.
The Cleveland Clinic also recommends that you:
- stay hydrated
- practice good hygiene
- keep your home sanitized
- avoid crowded places and people who are sick to reduce your risk of getting an infection
- If you do get a cold or the flu, it’s important to treat it as soon as possible.

There are also outbreaks of flu in periods of cold weather, so protect yourself against infections and take advantage of the free flu vaccine you are entitled to!
Overview
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
By following these steps, you will have a better chance of staying healthy over the cold winter months.
These tips and tricks can take some getting used to but once you are able to nail down a winter routine and execute your COPD treatment effectively in the winter and only takes a little bit of patience after that for spring to roll around again!
If you are shopping for a portable oxygen concentrator, us here at LPT Medical are here to help! We have an inventory of pulse flow and continuous flow devices, all of which are top on the line and reliable devices that will get you through any season!
We also have oxygen accessories that we sell separately so if you need an extra battery, external battery chargers, tubing we got you covered!

Just call us anytime at 1(800)-946-1201

Many people with respiratory diseases COPD and Cystic Fibrosis have to deal with extra phlegm and congestion in their lungs and airways. It's an unfortunate symptom that can be difficult to manage, especially during periods of illness and exacerbations.
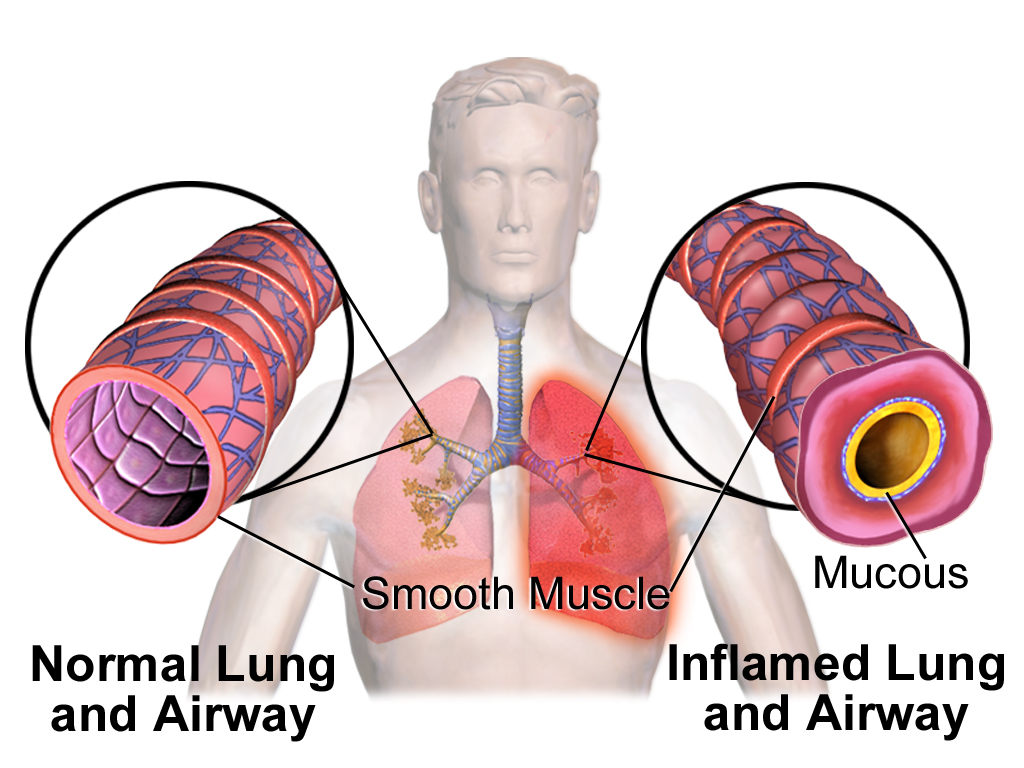
The reason for the excess mucus is inflammation in the respiratory tract caused by the disease. This kicks your mucus membranes into overdrive in an attempt to lubricate and soothe the lungs and airways, but it often leads to way too much extra mucus that is difficult to clear out.
Another cause of congestion in people with COPD is damaged lung tissue, which is not nearly as good at moving mucus up and out of your chest as healthy lungs are. When you pair that with decreased lung function and restricted airways, it can be nearly impossible to force out phlegm without some extra help.
For someone with COPD, excess mucus is particularly difficult to deal with because of common symptoms like chest tightness and airway restriction. When there's extra mucus and phlegm hanging around in the respiratory tract, it is especially difficult and uncomfortable for someone with COPD to breathe and cough controllably.
Fortunately, there are many different techniques and medications that can clear up congestion for people with a respiratory disease. That's why in this article we are going to teach you 16 effective methods respiratory patients can use to loosen and expel excess mucus.
It's important to note that if you suffer from any respiratory disease, not just COPD, and have trouble dealing with mucus, these tips will work for you.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Physical Techniques to Help Clear Mucus for COPD
1. Controlled Deep Coughing

Coughing is the body's natural, instinctual way to get rid of chest congestion, and it's often surprisingly effective. When your COPD causes your airways to get clogged up with mucus, coughing is one of the first things you should try.
However, uncontrolled, frantic coughing is usually not the best way to clear mucus from your airways. That's why doctors have developed coughing techniques to help you control your coughing and make it even more effective, especially for COPD patients who have difficulty producing strong, productive coughs.
A “controlled deep cough” is a simple, heavy cough that you force from deep in your lungs. Start by sitting in a comfortable place, leaning forward slightly, taking a long, deep breath in.
Next, hold your breath for just a few seconds and then use your abdominal muscles to forcefully push the air out through your mouth. You can even cross your arms over your stomach and use gentle pressure on your abdomen to help expel the breath.
While practicing this technique, you might get the urge to clear your throat or begin coughing reflexively, but do your best to ignore the impulse. Instead, take a few normal breaths, and then try another deep, controlled cough.
This method is more comfortable, and more effective, than a hacking, uncontrolled cough.
2. Controlled Huff Coughing
Another form of controlled coughing, huff coughing, is a gentle and effective way to clear phlegm out of your airways. It's also known as the forced expiration technique and it works because it keeps the throat open and effectively moves mucus out of the lungs.
There are 5 simple steps to performing a huff cough:
-
Start by sitting upright in a comfortable seat and lift your chin slightly.
-
Empty your lungs by exhaling slowly and completely for several seconds.
-
Next, take a slow, deep breath in, using your diaphragm (belly breaths).
-
Hold your breath for 2-3 seconds, then force the air out through your mouth in three rapid huffs, taking care to keep your throat open
- Repeat the technique, but take a slightly smaller breath this time. You can repeat the huff coughing technique as needed, alternating between small and large breaths.
Successful huff coughing usually requires about 3-5 repetitions with at least 5-10 normal breaths in between. A respiratory therapist or doctor can help you perfect the proper huffing technique, and remember to stop huffing if you begin to feel pain or exhaustion.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
3. Chest Percussions

Chest percussion is a type of chest physical therapy that essentially involves tapping or clapping on your chest with your hand. This physically loosens and breaks down mucus that is stuck in your airways, making it easier to cough up out of your lungs.
The proper technique is to sit while leaning back and use a cupped hand to deliver very firm, but gentle claps to the upper-left and upper-right part of your chest (in the space between your collarbone and nipple). You will want to start by tapping the left side of your chest for 2-3 minutes, and then repeat the percussions on the right side for another 2-3 minutes.
You should feel the mucus loosening in your chest as you perform the percussions and feel the urge to cough immediately after. Allow yourself to cough up as much mucus as you can in-between percussions until you've cleared all the excess phlegm from your chest.
Percussions should always be firm, but not painful, and done in a steady rhythm. Always make sure to position your hands in the correct place before performing any kind of percussion.
Do NOT perform percussions on any of these areas:
- Avoid the stomach
- Avoid the breastbone
- Avoid the spine
- Avoid the lower ribs and lower back (to prevent injuring organs)
4. Back Percussions

Back percussions usually require you to have a caregiver or respiratory therapist there to help out. They are very similar to chest percussions, but you lean forward and have someone else tap key spots on your back instead of your chest.
Start in a leaning-forward position, by holding a pillow to your chest and bending forward at the waist. Then have your therapist or caregiver tap gently but firmly on your back with a cupped hand, in the space right above your shoulder blade.
Tap for 2-3 minutes in that spot, then repeat again above your right shoulder blade. The mucus in your chest should loosen, allowing you to cough and expel it from your lungs.
5. Vibration

Vibration is another form of chest physiotherapy that is often done in combination with chest and back percussions. You can perform vibration therapy on the same areas that you do percussions on: both sides of the upper chest and back.
To do manual vibrations, simply place both hands, flat and palm-side down, on the target area. Then, using gentle pressure with the heels of both hands, tense your hands and wrists and shake them in a vibration-like motion. The patient should exhale slowly as you perform the vibration.
COPD patients will most likely need a caregiver or respiratory therapist to help perform vibrations, but there is special equipment available that allows patients do it on their own. There's an inflatable vest called a high-frequency chest wall oscillator that uses air pressure to deliver high frequency vibrations to the chest and back.
You usually use a high-frequency chest wall oscillator for about five minutes at a time with breaks to allow you to cough and clear out the loosened mucus between sessions. Chest wall oscillator devices are surprisingly non-bulky and streamlined, and there are several different versions on the market, including the Vest Airway Clearance System and the SmartVest.
6. Positioning to Promote Drainage

Another form of chest physiotherapy, postural drainage, is about placing your body in different poses or positions to help mucus drain downward out of your lungs. The unique positions encourage different lobes, or sections, of your lung to drain out until you can cough up or spit out the phlegm.
Positional drainage is often much more effective when you use it in combination with chest percussions and vibrations. It works best if a caregiver or respiratory therapist helps by performing the vibrations while the patient relaxes in a postural drainage position and exhales slowly.
Here are a couple of common postural drainage positions (although there are still many others!):
-
Draining mucus from the back of the lungs: In this position, you lie on your stomach and place pillows under your hips (usually three pillows are recommended) to raise your lower back and a small pillow under your head for comfort. Place your arms above your head and breathe deep from your belly.
- Draining mucus from the sides of your lungs: To drain the sides of your lungs, lie on one side and place a few pillows under your hip and a small pillow under your head. Stay in this position for 5 or 10 minutes, breathing deep from your belly for the duration.
The gravity along with the percussions and vibrations should effectively move the mucus out of your lungs, into your larger airways, and to your mouth where you can expel the excess sputum.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
A Last Word on Chest Physiotherapy
Most chest physical therapy sessions last somewhere between 20-40 minutes, and include alternating a variety of techniques including positional drainage, vibration, percussion, deep coughing, and huff coughing. You can do multiple sessions per day if needed, in fact doctors usually encourage COPD patients with excess mucus to do chest physiotherapy once in the morning and once before bed.
As you should before starting any kind of new therapy, make sure you talk to your doctor before starting or changing your chest physiotherapy regimen. Your doctor will be able to give you the best advice for how, when, and how often you should do it.
7. Active Cycle of Breathing Technique (ACBT)

The Active Cycle of Breathing Technique, or ACBT, is a three-step method for clearing mucus from your airways that is often recommended to patients with COPD. Like some of the other techniques we've discussed so far, ACBT includes coughing techniques, but combines them with chest and breathing exercises for maximum effect.
Follow these three steps to perform the Active Cycle of Breathing Technique:
Step 1: Relaxed, Controlled Breathing
Breathing slowly and steadily can help relax your airways and make it easier to expel mucus. Even though it can be difficult when you are congested, you want to try not to wheeze or breathe heavily before attempting to cough up mucus with this method.
Start by sitting up in a comfortable position and relaxing your chest, shoulders, and abdominal muscles. Breathe gentle, regular breaths by inhaling through your nose and exhaling from your mouth.
You want to breathe very gently with your lower chest so your upper chest can relax. You should feel your stomach rise and fall as you breathe, and it can help to lay one of your hands on your stomach to feel your abdomen expand as you take each breath.
Practice this controlled, gentle breathing for at least six breaths before moving on the next step.
Step 2: Chest Expansion Exercises
Now that you've relaxed your chest and practiced even breathing, it's time to loosen up and expand your chest. Doing this is as simple as taking in a large, deep breath.
Once you've filled your lungs up with air, hold it in for a moment or two, and then exhale gently. Don't force the air out.
Step 3: Controlled Huff Coughing
Now that you've used breathing and chest exercises to relax and expand the muscles in your chest and around your lungs, it's time to clear out the phlegm with huff coughing. This time, you do want to use forced expiration to get the mucus out of your airways.
Continue controlled huff coughing until you've forced all of the excess mucus out of your lungs and chest. Refer to the section near the beginning on huff coughing for a more detailed guide on how to use the huff cough technique.
8. Autogenic Drainage
Autogenic drainage is often used as alternative to the active cycle of breathing technique. It has three main phases in which you loosen mucus up from the walls of your respiratory tract, move it up through your airways, and expel it by coughing.
Phase 1: Dislodging Mucus
In this step, you take a small breath through your nose into your lower chest and hold it for three seconds. Then, exhale gently with the same force as if you were sighing, prolonging the breath. Repeat several times.
Phase 2: Moving Mucus out of Small Airways
This time, you want to take a larger, slower breath into your upper chest. Hold it for three seconds, and exhale quickly, drawing it out to be longer than when you breathed in.
Phase 3: Expelling Phlegm Out of Chest and Airways
In this phase, you should feel the phlegm moving in your chest, giving you the urge to cough. First, take a large, deep breath in and hold it for three seconds. Then breathe out normally.
Continue taking long, deep inhales, holding your breath for a few moments, and then exhaling normally until you feel mucus in your upper chest and throat. Use huffing exhales to force the up the phlegm and cough it out.
Medications and Medical Equipment to Help Clear Mucus for COPD
9. Expectorants

Expectorants are common over-the-counter medications that help thin and loosen up mucus in your chest and make it easier to cough up. However, studies show that expectorants might not be as effective or useful for people who have COPD.
Expectorants seem to work best in patients who have chronic bronchitis, but even then the benefits aren't particularly impressive. Make sure you talk to your doctor before taking expectorants to treat your COPD symptoms, and be aware that it might not work.
Some of the more common over the counter expectorants include Mucinex and Robitussin DM.
10. Mucolytics

Mucolytics are a type of oral medication used to treat COPD patients with thick mucus and difficulty expelling it from the respiratory tract’s Much like expectorants, mucolytics cause mucus to become thinner and easier to clear out of airways.
Unlike expectorants, which are usually taken as needed, mucolytics are usually taken daily to prevent symptoms. Mucolytics seem to be more effective than expectorants for patients with COPD, and can even prevent and treat exacerbations.
Some examples of mucolytic drugs often prescribed to patients with COPD:
- Carbocisteine
- Erdosteine
- Mecysteine
11. Saline Nebulizer
Nebulizers are often used to dispense medication to patients with asthma and COPD, but the evidence is piling up that COPD patients can also benefit from using a nebulizer with a plain saline (salt water) solution.
One study found that a nebulized saline treatment was able to help 65% of COPD patient participants to more easily expel mucus from their airways. It even managed to reduced breathlessness in some COPD patients, too.
Using a saline nebulizer is considered very safe, but you should still talk to your doctor first before trying any kind of new medical treatment. You also need to make sure you use a medically approved, hypertonic saline solution.
12. Positive Expiratory Pressure Devices

Positive Expiratory Pressure (PEP) is a type of therapy that helps you push your breath through your smaller air passages and loosen up mucus there. A PEP device is essentially just a mouthpiece or face mask that provides resistance when you exhale into it.
The extra air pressure that this creates helps force thick, stubborn mucus out your airways and up to your mouth, where you can cough or spit up the sputum.
You can use a Positive Expiratory Pressure device in three simple steps:
- Seal your lips around the mouthpiece of your PEP device and take a deep breath.
- Now, forcefully exhale through the device for several seconds, drawing it out as long as possible.
- The pressure should give you urge to cough as it dislodges mucus in your airways. When you get the urge, take in another breath and practice deep or huff coughing to expel the mucus.
13. Lung Flute

The Lung Flute is similar to a PEP device, but it uses a reed attached to the mouthpiece to create a vibrating sensation. The vibrations the lung flute produces travel from your lips, down your airways, and to your lungs to help loosen up trapped mucus.
The Lung Flute creates pressure and loosens and breaks down mucus even in the deepest parts of your lungs, unlike other mucus clearing devices. COPD patients usually use their Lung Flute at least twice daily, but your doctor will help you develop a regimen that is right for you.
The Lung Flute is simple to use. Just follow these steps:
-
Sit in a comfortable position and put the lung flute to your lips, angling the flute slightly downward.
-
Take a deep breath in, seal your lips around the mouthpiece, and exhale very gently through your mouth. You will hear the reed attached to the mouthpiece fluttering as you blow out. (It might take some practice to move the reed correctly)
-
Remove the flute from your lips and take another deep breath, and repeat another exhale through the mouthpiece, making sure it flutters the reed.
- Put down the mouthpiece and take several normal breaths. Repeat steps as necessary, blowing through the reed in repetitions of two blows at a time. You should feel the mucus collecting in your upper airways a few minutes after your lung flute therapy session, at which point you should practice controlled coughing techniques to expel the phlegm.
Diet & Lifestyle Techniques to Help Clear Mucus for COPD
14. Drink Plenty of Water

If you don't drink enough fluids throughout the day your mucus gets thicker and more difficult to drain or expel. Thick, sticky mucus is difficult to cough up and tends to get stuck in your airways, making it more difficult to breathe.
That's why it's especially important for people with COPD to drink enough water. Keeping your body hydrated helps keep your mucus thin and fluid, which makes it much easier to clear out of your airways.
But staving off congestion is only one of many reasons to drink plenty of water. You're more likely to stay active and stress-free if you're hydrated, whereas dehydration can affect your mood and leave you feeling sluggish and fatigued.
15. Avoid Too Much Milk and Dairy

It is an often-repeated tale that drinking milk and eating dairy causes your body to produce extra mucus, but it turns out that's not exactly true. Studies do show, however, that milk and dairy cause the mucus in your airways to get thicker, which is probably how the myth originated.
If you avoid having too many dairy products in your diet, it can help keep your mucus thin and more manageable. As we've discussed, thinner mucus is better because it's easier to drain and cough up from your chest.
If you eat a lot of dairy products and also have trouble with thick mucus that's difficult to expel, you might want to reduce t
In order to maintain a healthy and well-balanced diet, it’s essential to consume a wide variety of nutrients. Most of these nutrients can be found in the food that we eat, but occasionally it’s advised that you take dietary supplements in order to boost your intake of certain vitamins and minerals.
While everyone needs the same nutrients, it’s usually a matter of what quantity you should consume them in. For example, babies need to consume a lot of vitamin D which helps regulate calcium and phosphate in the body. In turn, this aids in the development of strong bones, teeth, and muscles.
Similarly, a healthy adult may need to consume different quantities of nutrients than an adult with a chronic disease. COPD patients, in particular, are reported to have deficiencies in vitamin D and other nutrients with antioxidant capacity such as vitamins A, C, and E.
But getting the right nutrients isn’t as simple as it sounds. You’ll need to consult with your doctor and maybe even a dietitian who can examine your condition and compile a dietary plan that will work best for you.
In this post, we’ll take a look at some of the supplements that are most commonly used in COPD patients and we’ll provide you with all the information you need to know to start discussing supplements with your doctor. If you have any questions, don’t hesitate to leave them in the comment section so we can reach out to you.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
The Good and the Bad of Dietary Supplements
According to a 2017 survey by the Council for Responsible Nutrition (CRN), 76 percent of U.S. adults use dietary supplements. And while supplements are widely available and easily accessible, they aren’t always used in a responsible way.
Unfortunately, just like drugs, dietary supplements have well-known and well-documented side-effects. Supplements contain active ingredients and if they aren’t used in moderation, they can have strong adverse effects on the body.

One of the greatest dangers of supplements is that they aren’t regulated the same way many drugs are. According to the American Cancer Society, both supplements and drugs are regulated by the United States Food and Drug Administration (FDA). However, drugs are often considered unsafe until proven safe, whereas supplements are considered safe until proven unsafe.
The reason this happens is that supplements are categorized as a “food product” making them immune to many of the tests that are required to bring drugs to store shelves. Drug manufacturers are required to put their products through a series of clinical trials that test their safety and efficacy. On the other hand, supplement manufacturers only need to prove that their products do not result in “a significant or unreasonable risk of illness or injury.”
Because supplements are “self-prescribed,” it’s a lot more difficult for health professionals to track their use. Rather than being able to prescribe each vitamin and mineral that their patient takes, doctors and nutritionists need to rely on their patients to do their own research and address any concerns they have before purchasing any type of dietary supplement.
Lastly, supplement manufacturers do not need to seek approval from the FDA in order to market their products. Supplement advertisements often tout anecdotal evidence rather than empirical evidence as proof that their supplements work. In other words, their evidence is based on an individual’s experience instead of proven facts and statistics.
Dietary Supplements and COPD
With all of this being said, the best advice for COPD patients interested in dietary supplements is to be cautious about what you read. While supplements don’t typically have side-effects as severe as drugs, they still contain powerful active ingredients that can make COPD more difficult to manage if you don’t know what you’re doing.

Another thing to note is that supplements are not a “cure-all” and they’re not intended to treat a specific disease or illness. They’re most commonly used to treat nutrient deficiencies in your body, and you won’t know what these deficiencies are unless you discuss your symptoms with your doctor.
COPD is a progressive and irreversible lung disease characterized by chronic inflammation and obstructed airflow. COPD varies widely in terms of severity and many patients will experience comorbidities such as sleep apnea, osteoporosis, cardiac disease, as well as mental health disorders like anxiety or depression.

As a result, it’s impossible for a pulmonologist to provide a “one-size-fits-all” treatment plan for a COPD patient. Each patient is considered a unique case, so even if something works for one COPD patient, it doesn’t necessarily mean it will work for all of them. Without further ado, let’s take a look at some of the most commonly recommended supplements for COPD.
Vitamins
Every day, your body works around the clock to produce skin, bone, and muscle. It sends nerve signals throughout the body and creates rich red blood cells that nurture every organ in the body. But without essential nutrients like vitamins, your body would not be able to do any of this.

Your body requires about 30 different types of vitamins, minerals, and dietary components. But the problem is, many of these components are not produced by the body naturally, so you need to get them from either the food you eat or dietary supplements.
Vitamin D
Vitamin D plays a number of important roles in the body. First and foremost, it promotes healthy calcium absorption. Calcium is a mineral that’s responsible for muscle function, hormonal secretion, nerve transmission, and vascular vasodilation and contraction. Vitamin D also plays an important role in the reduction of inflammation, immune function, and the modulation of cell growth.
.jpg)
Vitamin D deficiency is one of the most common side-effects associated with COPD. It’s estimated that about 25 percent of people with COPD have low levels of vitamin D. This occurs for two main reasons: COPD patients often don’t eat the recommended amount of meals each day because eating can be physically exhausting and lead to difficulty breathing.
Secondly, many COPD patients, especially those with stage 3 or stage 4 COPD, don’t get outside very much. Since a large portion of our vitamin D intake is absorbed from sunlight, respiratory patients are often deprived of this.
While COPD patients can take regular vitamin D supplements or vitamin D with calcium, vitamin D3 is a better alternative for many people. The reason for this is because vitamin D3 contains both sunlight and dietary-activated vitamins — both of which COPD patients lack.

Generally, vitamin D is believed to reduce the rate of lung decline for people with severe lung disease. Because vitamin D helps regulate inflammation, COPD patients may experience fewer exacerbations that are less severe. Regular vitamin D levels will also help prevent osteoporosis and other bone conditions that can make living with COPD even more difficult.
Too much vitamin D may result in vitamin D toxicity. This can cause too much calcium to build up in the blood (hypercalcemia), which can cause fatigue, weakness, and nausea. If hypercalcemia progresses, it can lead to the formation of calcium stones and pain in the bones and kidney.
Minerals
Like vitamins, minerals are one of the essential nutrients for your body. Minerals are naturally occurring inorganic materials that play a number of important roles like maintaining healthy brain function, muscle function, and heart function. There are two types of minerals: trace minerals and macrominerals.

Macrominerals include magnesium, phosphorus, sodium, potassium, chloride, sulfur, and calcium. Generally speaking, macrominerals are needed in much higher doses than trace minerals and they play a larger role in your body functions. Trace minerals, on the other hand, include fluoride, selenium, cobalt, zinc, iodine, copper, and iron.
Magnesium Sulfate
Magnesium sulfate (MS) is widely used as a treatment for asthma due to its bronchodilatory effects. What this means is that it can help widen the airways in the event of a severe asthma exacerbation. Unfortunately, MS has not been tested as widely when it comes to treating COPD, so its efficacy is still up for debate.

Several placebo-controlled trials have been conducted to test the benefits of magnesium sulfate in treating COPD. However, they have yielded mixed results and didn’t present enough evidence to indicate that COPD patients should adjust their treatment plan to accommodate for oral or nebulized magnesium sulfate supplements.
Zinc
Zinc is an essential trace element that plays an important role in immunity. While zinc can be found naturally in foods like whole grains, red meat, and poultry, it can also be taken in the form of dietary supplements. Zinc is an antioxidant, meaning it protects your cells against dangerous free radicals that are produced when your body breaks down food or you’re exposed to tobacco smoke.

An imbalance between antioxidant capacity and oxidative stress is believed to play a major role in the development of COPD, so zinc may have beneficial effects when it comes to regulating this. Since zinc plays such an important role in regulating the immune system, COPD patients with zinc deficiency will be at a higher risk of experiencing lung infections that can lead to exacerbations.
Omega-3 Fatty Acids
Omega-3 fatty acids are not one nutrient, but rather, a whole family of essential fatty acids. Since your body cannot produce these fatty acids on its own, you need to get them through your diet. Some examples of food that contain omega-3 include fish (salmon), flax seeds, chia seeds, and walnuts.
Omega-3 supplements are very popular nowadays and for good reason. It’s been proven to lower blood pressure, slow plaque development in the arteries, improve heart health, and even help you manage anxiety or depression. Omega-3 supplements, in particular, are great for people who don’t consume a lot of fish or other foods that contain omega-3.
One of the ways omega-3 helps COPD patients is by fighting inflammation. According to Richard Phipps, Ph.D. professor of Environmental Medicine and director of URSMD Lung Biology and Disease Program, “We never really knew why diets high in omega fatty acids seemed good, but now we know it’s because they provide the precursors for molecules that help shut down excessive inflammation.”
While many people take omega-3 supplements like fish oil without consulting their doctor, it’s recommended that COPD patients ask their pulmonologist first. There are three different types of omega-3s including alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA), all of which have different uses. What’s more, it’s important to consume the correct ratio of omega-3 to omega-6 fatty acids.
If you have a shellfish allergy, be aware that omega-3 supplements may contain trace amounts of shellfish. Be sure to address this with your doctor if you’re concerned about it.
NAC (N-Acetylcysteine)
N-acetylcysteine is an antioxidant that potentially has beneficial effects for people with COPD. While NAC has been shown to reduce cough and phlegm and thin mucus in some patients, it has shown little to no effect in others. More studies are needed to fully understand the pros and cons of using NAC to treat COPD.

From what we know so far, however, NAC seems very safe to use. What’s more, it can be taken either orally, or through a nebulizer which gives COPD patients plenty of options. NAC is typically prescribed in tandem with other treatment options rather than being used as a primary treatment for COPD.
Ginseng
Aside from vitamin D, ginseng is one of the most common supplements used for COPD. Ginseng is a root that’s found in many places around the world, but the most popular are American ginseng and Asian ginseng, the latter of which has been used in medicine for centuries.

While ginseng has many benefits for people with different conditions, for COPD patients, it has powerful antioxidants and anti-inflammatory properties. Another benefit of ginseng is that it’s an all-natural herbal supplement. So, unlike manmade vitamin and mineral supplements, it’s much easier for patients to verify that they are receiving a pure product without any additives.
Questions to Ask Your Doctor
Everyone needs to maintain a healthy balance of vitamins and minerals to be healthy. However, like drugs, taking too many dietary supplements can have adverse side-effects. Many people take a daily “multivitamin” which contains a variety of vitamins and minerals. And while these have some proven health benefits for some people, they don’t target specific nutrients that will benefit COPD patients.

If you want to do what’s best for your health, especially if you have COPD or another chronic illness, it’s best to consult your doctor. He/she will help you understand how dietary supplements fit into your overall COPD treatment regimen and give you an idea of what side-effects to expect. Ask your doctor the following questions to get you started:
- Are there any tests I can take to see if I have vitamin deficiencies?
- How will supplements affect my COPD diet?
- What are the benefits and risks of the supplements I’m taking?
- How can I ensure the supplements I’m using are safe?
- Are there any effective alternatives to the supplements I’m taking?
-
How will supplements affect my comorbidities such as sleep apnea, heart problems, or anxiety?
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Conclusion
Nutrition plays a fundamental role in our overall health. By getting our recommended daily value of vitamins and minerals, we provide our bodies with the raw materials they need to perform functions such as regulating blood production and blood flow, building strong healthy bones, and regulating metabolism. Dietary supplements are a great way to fine-tune our diet, but they can be equally destructive if they aren’t used correctly.
Similar to drugs, every dietary supplement has side-effects. If you’re someone with COPD or any other chronic illness, this could make your symptoms worse and even increase your chance of experiencing exacerbations. This is why it’s important to first discuss with your doctor so that he/she can recommend supplements that will work in tandem with your COPD treatment regimen, rather than working against it.
As soon as the cold weather creeps in, it's inevitable that wood-burning stoves start firing up all across the country. For many people, burning wood is a long and cherished tradition, both for warmth and for recreation.
Unfortunately, most people don't realize how devastating wood smoke can be to their health. Research shows that it may even be twelve times more dangerous than cigarette smoke when breathed in similar quantities.
The truth is, burning wood in your home can increase your risk for a variety of serious health problems, including heart disease and COPD. It can also cause serious respiratory symptoms in healthy adults and especially in people with COPD.

Fortunately, wood smoke is not an issue for most people who only encounter it occasionally at bonfires and barbecues. However, there is still a large number of people—especially those who use wood furnaces to heat their homes—who get exposed to wood smoke much more frequently.
Unfortunately, those most at risk from wood smoke are those who already suffer from lung diseases like COPD. Even small amounts of wood smoke can cause serious breathing problems for people who suffer from asthma, COPD, and other respiratory problems.
That's why an important part of staying healthy with COPD is knowing how to recognize and avoid respiratory hazards, including wood smoke. That means avoiding all sources of pollution and especially keeping the air inside your home healthy and clean.
That's why, in this guide, we're going to tell you everything you need to know about wood smoke and COPD. We'll explain how wood smoke affects your lungs, how it can worsen COPD, and how to avoid exposing yourself to harmful quantities of wood smoke.
We'll also discuss how using a wood-burning stove for heat is a major source of indoor air pollution and extremely hazardous for people with COPD. To help you keep your lungs healthy, we'll show you a variety of things you can do to make your wood-burning appliances safer or replace them with less hazardous alternatives.
Why Wood Smoke is So Bad For You

Wood smoke and COPD have one main thing in common: they both cause irreparable damage to your lungs over time. Wood smoke is also a serious respiratory irritant that can exacerbate the symptoms of COPD and other respiratory diseases.
Wood smoke is dangerous for two main reasons: First, it releases dangerous amounts of tiny particles that get trapped in your lungs when you breathe them in. Second, it emits a variety of toxic gases that can damage your lungs and impair your ability to breathe.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
These toxic substances can trigger serious immediate symptoms as well as long-term heart and respiratory problems. That's why many health and advocacy organizations strongly warn against the practice of using wood to heat your home.
According to the Utah Physicians for a Healthy Environment, “wood smoke is uniquely toxic among all sources of urban air pollution.” This is in part because particle pollution from wood smoke is “extraordinarily small” and has the ability to causes prolonged damage to your body's cells.
Toxic Fumes from Wood Smoke

When wood burns (or combusts), it releases a wide variety of gases that are harmful to your lungs. These gases hurt your respiratory system mainly through inflammation, damage to delicate lung tissues, and by limiting your lungs' ability to absorb oxygen when you breathe.
Here's a quick snapshot of just a few of the many toxic fumes found in wood smoke:
- Nitrogen Oxides: can cause lung and airway irritation, shortness of breath, and an increased risk of lung infections, particularly for people with asthma or COPD
- Volatile Organic Compounds: can irritate the respiratory tract and some can even cause cancer
- Formaldehyde: can cause eye irritation, headaches, and can trigger respiratory symptoms like coughing and wheezing
- Hydrocarbons: cause lung inflammation, respiratory symptoms, and can cause lung diseases like asthma and COPD
- Benzene: can cause anemia, excessive bleeding, and suppress your immune system
- Sulfur Dioxide: causes eye irritation, respiratory inflammation, and bronchospasms, especially in people with COPD and other respiratory problems
- Dioxins: can cause cancer
- Carbon Monoxide: reduces your lungs' ability to absorb oxygen, straining your lungs and cardiovascular system; it can both cause and worsen respiratory symptoms and, in high enough levels, cause suffocation
- Acrolein: can irritate your eyes and respiratory tract
Ultra-fine Particles from Burning Wood
Wood smoke contains tons of microscopic particles, often called ultrafine particles, which experts consider to be the greatest health hazard caused by smoke. When you breathe in air contaminated by these tiny particles, they get trapped and stay deep inside your lungs.
The most dangerous ultrafine particles are known as PM2.5, which stands for particles that are smaller than 2.5 microns across. For reference, that's about half the size of a red blood cell or 30 times smaller than the width of a human hair.
Wood smoke produces a large number of PM2.5 particles, which are incredibly toxic to your lungs and cardiovascular system. These ultrafine particles can also irritate your eyes, your nose, and even your digestive system.
These tiny airborne particulates have been proven time and time again to be directly linked to a variety of serious respiratory and cardiovascular conditions. These include respiratory decline, asthma, heart disease, COPD, and chronic respiratory symptoms.
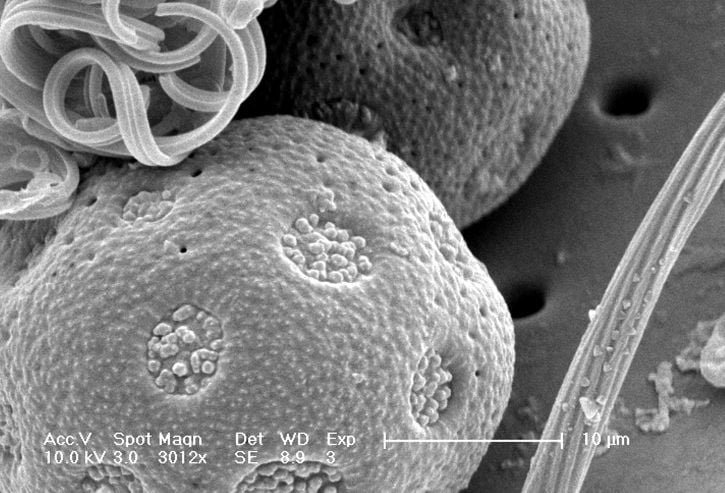
Fine particulates can even trigger heart attacks in people with existing cardiovascular disease, a health problem that is very common among COPD patients. Particle pollution is also linked to premature death in people suffering from heart disease and COPD.
You are more likely to develop health problems when the concentration of particulates in the air is high and you are exposed to them regularly over a long period of time. One common way that people get exposed to harmful levels of particle pollution long-term is by using wood-burning appliances to heat their homes.
Wood Smoke and COPD
Smoke from wood-burning stoves and fireplaces is both a cause of COPD and a major hazard for people who have COPD already. That's why it's so important for all people, and especially COPD patients, to be aware of the dangers of wood smoke.
Most importantly, you should never rely on a wood-burning stove to heat your home during the winter if you suffer from COPD. The indoor pollution it creates, even if it's only minor, is simply too much to risk for someone with a serious respiratory condition.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
COPD makes your lungs much more sensitive to the damaging effects of harmful particles and gases. That means it takes less smoke to inflame your lungs and trigger respiratory symptoms.
Even a tiny amount of smoke could make you feel breathless or bring on a serious coughing fit. Even if you don't experience any immediate effects, being around wood smoke can still harm your lungs.
Like any source of pollution, breathing in the toxic byproducts of burning wood too often could cause your COPD to progress even faster. It can speed up lung function decline and cause permanent worsening of existing COPD symptoms.
That's why using a wood-burning stove to heat your home throughout the winter is such a major risk. Even if you take the proper precautions, you could still get exposed to enough wood smoke pollution over time to experience negative health effects.
Having COPD means your lungs are already damaged and you only have a limited amount of lung function remaining. The risk of losing even more lung function is just not worth using a wood-burning stove for heat.
How Much Wood Smoke is Too Much?

Burning wood in the fireplace every once in awhile isn't likely to cause major problems for most people. However, burning wood in your home frequently over many years can seriously damage your lungs.
Most of the risk from wood-burning stoves and fireplaces comes from how it can damage your lungs and cardiovascular system over the long term. That's why heating your home with a wood-burning stove is so much more dangerous than using your fireplace once in awhile; wood-burning furnaces have to run 24/7 all winter long to keep your house warm.
That adds up to months and months of exposure to wood fumes and particulates for many hours every day. What's more, the pollution can remain in your home for days or weeks after you stop burning wood, affecting you long after the winter is over.
Ultrafine particles don't disappear on their own, and they are small enough to pass straight through the vast majority of air filters. As a result, they continue to circulate through the air in your home until they settle into a fine dust on your walls, furniture, and floors.
This toxic particulate matter is especially pesky to get rid of because it constantly cycles between settling and getting kicked back up into the air. It may take multiple deep cleans and airing out your house to to get rid of all the particle pollution left over from weeks or months of burning wood.
However, the dangers of wood smoke are still very much present even if you don't burn wood every day. Even short-term exposure can irritate your lungs, which can cause serious problems for people with COPD.
If you have COPD, asthma, or any other respiratory problems, then breathing in any amount of wood smoke can be harmful. It can cause serious immediate symptoms as well as long-term damage that can make your existing chronic symptoms even worse.
What About “Safe” Wood-burning Systems?

You might think that having a modern, efficient, professionally-installed wood stove is enough to keep you safe. Unfortunately, no matter what precautions you take, burning wood can still endanger your health.
While modern, EPA-approved wood-burning stoves are much safer than older appliances, no wood-burning appliance is completely safe. There is always a risk that smoke or particulate matter could make it into your home.
Even well-ventilated wood-burning furnaces can still leak a steady stream of pollutants that build up in the air indoors over time. You release even more harmful gases and particles into your home every time you open the furnace door.
It's nearly impossible to burn wood in a wood stove or fireplace without introducing wood smoke pollution into your home. A good rule of thumb is that if you can smell the fire at all, then you are inevitably also breathing in the toxic gases and ultra-fine particulates from the smoke.
No matter how you cut it, burning wood for heat is much riskier than using a modern gas or electric furnace. If you have COPD, asthma, or another respiratory condition, it's always best to assume that no wood-burning appliance is safe, especially for extended periods of use.
Other Wood-Burning Hazards
There are other costs to burning wood besides the negative effects on your health. Wood-burning stoves and fireplaces are actually a major cause of environmental pollution and cause more than fifteen thousand house fires every year.
Pollution Caused by Wood Burning

In addition to polluting the air indoors, home wood-burning also causes a surprising amount of outdoor air pollution. In fact, the World Health Organization estimates that outdoor pollution caused by residential wood burning caused approximately 9,200 deaths in the US in 2010.
In te San Francisco Bay area, nearly thirty percent of the particle pollution present during the winter comes from wood-burning in home fireplaces and stoves. Other studies show that burning wood creates even more pollution than burning oil, coal, or gas.
This is one of the major reasons why countries around the world discourage wood burning and urge people who do burn wood to use more modern, efficient stoves. Doing so could significantly reduce outdoor air pollution during the winter months and reduce the risk your wood stove poses to your fellow neighbors and citizens.
Fires Caused by Wood Burning

Every year in the US, about thirty people die and eighty people are injured in house fires caused by wood-burning stoves and fireplaces alone. Contrary to what most people believe, the vast majority of these deaths and injuries are the result of smoke inhalation rather than burns.
Uncontrolled fires release massive amounts of noxious fumes and fine particles that build up quickly inside a house. Just a couple minutes of breathing this smoke can cause smoke inhalation, respiratory failure, and permanent lung damage.
Smoke inhalation is life-threatening for healthy adults, but it's even more deadly for people with COPD and other lung diseases. Since their lungs already function poorly, COPD patients are much more vulnerable to suffocation and suffering from disabling breathing problems from the smoke.
That's why, if you burn wood in your home, it's important to consider the immediate risk of uncontrolled fires as well as the long-term costs to your health. Even if you escape from a house fire without getting hurt, the smoke you inhaled in the meantime could still cause serious, long-term damage to your lungs.
Alternatives to Burning Wood for Heat

If you use a wood-burning stove or furnace to keep your home warm, it may be time to consider upgrading to a better heating system. There are several other home heating options that are both cheaper and more efficient than burning wood for heat.
Despite what many people believe, heating your home with wood is not exactly budget-friendly. In fact, wood-burning stoves and furnaces are generally more expensive to run than other home heating options.
Even if you are hesitant to take on the initial cost and hassle of replacing your home heating system, remember that doing so may actually save you money in the long run. Even if you have to take a temporary hit to your budget, you can't place a value on the benefit of protecting yours and your family's health.
Here are some of the benefits of switching to a non-wood-burning heating system:
- Fewer emissions and outdoor pollution
- Significantly less indoor pollution
- Extremely simple to use and maintain
- More energy-efficient
- More effective at heating
- Often cheaper to run and maintain
- Eliminates the need to buy or store fuel
Here are some home heating options that don't burn wood:
- Central gas heating furnace
- Central electric heating furnace
- Boiler (radiant heating system)
- Solar Heater
- Heat Pump
How to Make Your Wood-Burning System Safer
Ideally, you should not use a wood-burning stove at all, especially if you have COPD. Just about any other heating option is better and safer for your lungs and overall health.
However, if you still choose to use a wood stove or furnace, there are many things you can do to reduce your risk. If you follow he best wood-burning practices, you can minimize the amount of harmful pollution your wood-burning stove emits into your home.
Get a Modern, EPA-Approved Appliance

There are many reasons to upgrade your old wood-burning stove to an EPA-certified model. Modern wood-burning stoves are much more efficient, environmentally-friendly, and significantly safer than older wood-burning appliances.
Unfortunately, the EPA estimates that 65% of wood stoves in the US are old and inefficient models. If your home uses one of these older stoves, then upgrading to a newer model could significantly reduce the risk it poses to yours and your family's health.
Here are some more benefits of using an EPA-certified wood-burning stove:
- They reduce pollution by 50-60 percent
- They use less fuel (about one-third less wood)
- They burn fuel more efficiently
- They circulate heat more efficiently (less heat loss)
Because of new EPA regulations introduced in 2015, nearly all wood-burning heating appliances now sold in the US must meet the EPA's requirements. These requirements are designed to reduce both indoor and outdoor pollution by ensuring that wood stoves emit no more than 4.5 grams of particulate matter per hour.
That means just about any wood stove that you buy from a US retailer should be EPA-certified and create relatively low amounts of pollution. However, even the safest wood-burning stove is still less safe and more polluting than non-wood-burning heating appliances.
If you use an older wood stove and you or anyone else in your household suffers from COPD, then upgrading your furnace should be a top priority. Home wood-burning is simply too hazardous for vulnerable lungs, especially if you don't use an appliance that meets modern safety standards.
Depending on where you live, you may even be eligible to participate in a wood stove change-out program. These programs may be able to help you cover some of the cost of installing a more efficient wood stove (or another type of heating system) if you otherwise couldn't afford to replace your old, inefficient stove.
To learn what options are out there, take a look at the EPA's complete list of certified wood stoves here. You can also contact your local air quality agency to see if there are any wood stove exchange programs in your area that can help you manage the cost.
Opt for a Pellet Stove

If you must use a fuel-burning appliance to heat your home, you should know that there are other options besides a typical wood-burning stove or furnace. One of these options is a pellet stove, which is generally cleaner and safer to use than a traditional wood-burning stove.
Pellet stoves are a special type of fuel-burning appliance that burn small manufactured pellets instead of firewood. These pellets are usually made up of compressed sawdust or wood chips, but some stoves can also burn pellets made of compacted paper, grass, corn, and other organic materials.
Of all of the different wood-burning appliances out there, pellet stoves are often considered the most clean and efficient option. They produce less smoke and are much easier to use and manage than traditional wood-burning stoves.
One thing that makes pellet stoves cleaner than wood-burning stoves is the type of fuel they use; pellets are reliably drier and more uniform in shape and size than firewood. Pellets are manufactured to contain just the right amount of moisture, and they tend to burn more evenly and completely in the stove.
It also takes much less effort to keep a fire going in a pellet stove. Most have auto-start ignitions and automated pellet feeding systems that make re-fueling the stove incredibly easy. In fact, most pellet stoves can keep themselves going for about 24 hours on a single hopper load.
Pellet stoves also get hotter because they use fans to circulate the air in the stove and ensure minimum heat loss. Unlike wood stoves, pellet stoves require electricity to power the hopper, ignition, and fans.
Pellet stoves generally cost about the same price as a typical wood-burning stove, but the fuel can b


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!














