They're in the air, in our homes, and in a wide variety of products we use every day—volatile organic compounds (VOCs) are everywhere. Unfortunately, exposure to too many VOCs can be bad for your health and particularly dangerous for your lungs.
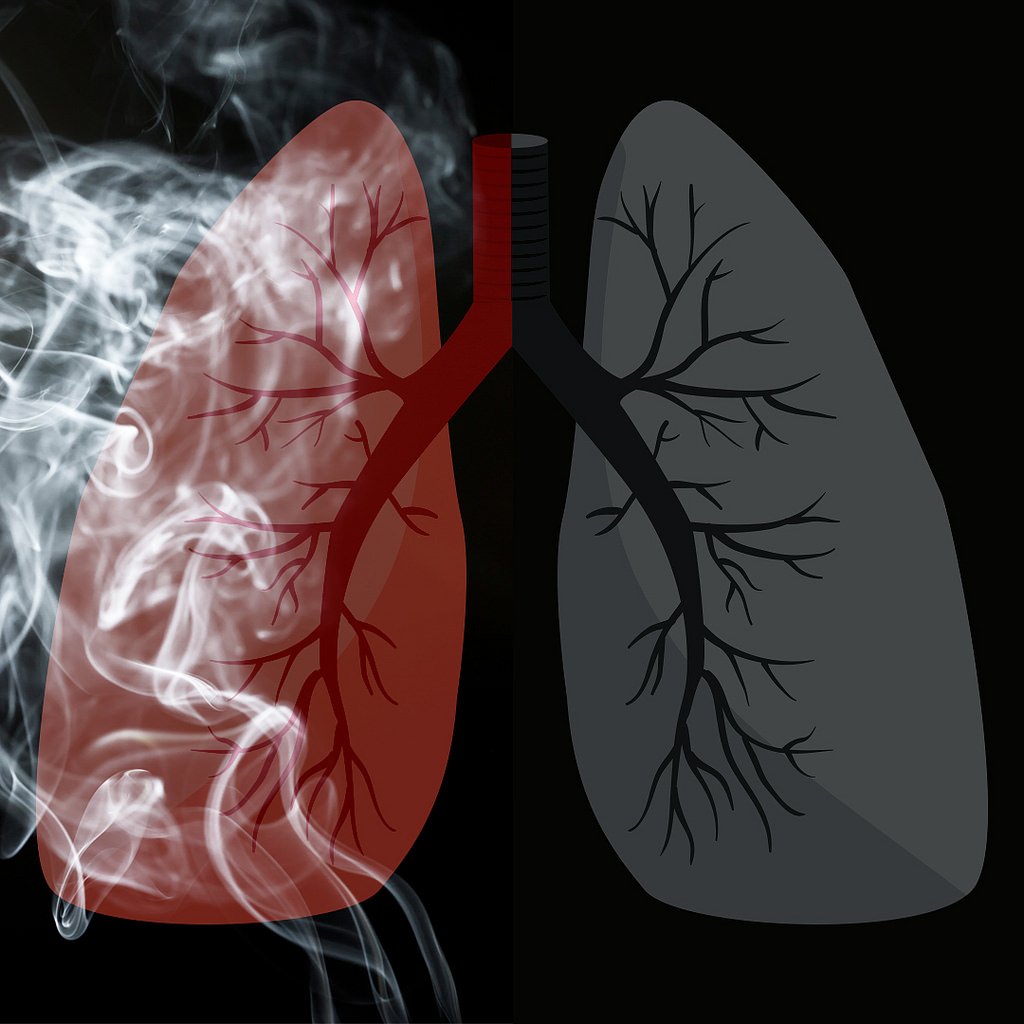
VOCs are a major source of air pollution, and they can cause a variety of respiratory problems including lung irritation, lung tissue damage, and serious lung diseases. Certain VOCs can also worsen existing breathing disorders like asthma and COPD.
Fortunately, you can limit your exposure to harmful VOCs if you learn how to recognize and avoid them. That's why, in this post, we're going to tell you everything you need to know about volatile organic compounds and your lungs, including how to protect yourself from hazardous VOCs.
We'll explain what VOCs are, where they come from, and what the research says about how they affect your health. We'll also show you which volatile organic compounds are most harmful to your lungs and how you can minimize your exposure to them at home.
Being able to identify and avoid breathing harmful VOCs is a valuable skill to have, especially if you suffer from a lung condition like COPD or asthma. Even if you are a healthy adult, learning about VOCs can help you make better choices that keep your lungs safe, healthy, and strong.
What are Volatile Organic Compounds?
Volatile organic compounds, or VOCs, are essentially just carbon-based chemicals that can quickly evaporate into a gas or vapor. Previously, VOCs were known throughout the US as reactive organic gases (ROG's), a term you might still come across today.
Whether or not you've ever heard about volatile organic compounds before, you almost certainly encounter many of them every day. Some of these VOCs are completely harmless, but some are dangerous chemicals that can have serious effects on your health.
When makes volatile organic compounds unique is that they evaporate very quickly, and the vapors they release mix into the air the air we breathe. This is how most people get exposed to VOCs both inside and outside their homes: simply by breathing and inhaling them into their lungs.
It's important to understand that “volatile organic compound” is a very general term that encompasses a huge variety of both natural and man-made chemicals. In fact, most of the things we consider to be fragrances or scents actually come from VOCs.
All VOCs are different, each with unique toxicities and varying levels of health risk. Some can only harm you in large amounts, some are toxic in lesser amounts, and some pose little, if any, danger to your health at all.
However, many VOCs are harmful, which is why many are classified as carcinogens, air pollutants, and even explosion risks. Some of the most common and dangerous VOCs are lung irritants which can irritate your airways, damage your lungs, and cause a variety of other serious respiratory conditions.

Volatile organic compounds can affect a variety of different systems and organs in the body, and what levels of exposure are considered “safe” vary significantly between VOCs. But as scientists continue to study their effects, some VOCs are turning out to be even more hazardous than originally thought.
For example, some VOCs become even more potent pollutants when they react with other gases in the air, like nitrogen oxide, to form ozone. Researchers are just now beginning to understand how serious this problem is, and have found that everyday products and chemicals containing VOCs are starting to rival vehicle emissions as a primary source of air pollution.
VOC-catalyzed ozone is particularly harmful because it collects at ground level where we breathe, and it's responsible for variety of short-term and long-term health effects. VOCs also contribute to the formation of fine particles in the air, which is another hazardous type of air pollution.
Here are some examples of common volatile organic compounds you might have heard of before:
- Isopropyl alcohol: used in cleaners and disinfectants
- Acetone: found in nail polish remover and paint removers
- Formaldehyde: found in building materials and molded plastics
Where Do VOCs Come From

Many of the most harmful VOCs come from fuel and manufacturing emissions, including gasoline, diesel fuel, and industrial processes. Others come from chemicals used in commercial products and materials like treated lumber, cleaning chemicals, and paint.
Many pesky airborne irritants, the kinds that make your eyes water or tickle your nose, are actually volatile organic compounds. So are many of the fragrances and chemicals found in basic products that you might use in your home every day.
In fact, common household products containing VOCs, such as cleaning solutions, furniture, and cosmetic fragrances, are a major cause of indoor air pollution. These VOC's, along with those caused by industrial emissions, make their way outdoors where they contribute heavily to smog and and other forms of outdoor air pollution.

Wood smoke and tobacco smoke also contain hazardous levels of volatile organic compounds, which are partially responsible for the deadly health effects of smoking. Unfortunately, tens of millions of Americans regularly inhale VOC's from cigarettes, second-hand smoke, wood-burning stoves, and hazardous workplaces.
Here are some examples of some common products and processes that expose you to harmful VOCs.
Sources of VOCs In and Around Your Home
- Cleaning solutions & disinfectant sprays
- Air fresheners and other artificial fragrances
- Cooking fumes
- Cigarette smoke
- Wood-burning fireplaces
- Scented hair, body, and cosmetic products
- Burning oil or fuel indoors
- Fireplaces and wood-burning stoves
- Pesticides and moth repellent
- Dry-cleaned clothing
- Furniture
- Many glues and adhesives
- Permanent markers, art paints, and other hobby or crafting supplies
- Varnishes and finishes
- Building materials: e.g. paint, paint remover, caulk and sealants, carpet, and flooring (The amount of VOCs emitted by these products declines over time.)
Sources of VOCs Outdoors
- Automobile emissions
- Diesel emissions
- Power plant emissions
- Fuel extraction and processing
- Manufacturing plant emissions
- Emissions from other chemical and industrial processes

How Dangerous are VOCs?
Fortunately, most of the harmful volatile organic compounds only pose a serious danger in large doses or long-term exposures. If you have healthy lungs and only get exposed to small amounts of VOCs, then you are unlikely to experience any major health effects.
However, people with existing lung diseases are often much more sensitive to the effects VOCs. For these people, even low VOC concentrations in the air can trigger respiratory symptoms like coughing and shortness of breath.
Still, even healthy people can experience short-term and long-term symptoms from low or moderate exposure to certain volatile organic compounds. Many people, for instance, get an itchy nose, watery eyes, or feel lightheaded when they use a noxious chemical like bleach.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Fumes from recently-painted walls can trigger symptoms for days, and new carpeting can emit high levels of VOC's (sometimes referred to as off-gassing) for weeks or months after installation. One study found that even just working in a newly-constructed building can expose you to enough VOC's to cause eye irritation and airway inflammation.
These symptoms are usually fairly mild and disappear on their own once you get away from the source of VOCs. You usually don't need medical treatment unless you've been exposed to unusually high concentrations or an especially toxic VOC.
Here are some of the most common short-term symptoms that VOCs can cause:
- Eye, nose, throat, and lung irritation
- Coughing and sneezing
- Shortness of breath
- Headaches
- Dizziness
- Minor skin irritation
- Worsened asthma and COPD symptoms
- Nausea or vomiting
Whether or not you realized it at the time, chances are almost certain that you've had minor reactions to VOCs before. For example, if you've ever used a cleaning product that made you sneeze, or felt your eyes stinging near a campfire or BBQ, then you've experienced the symptoms of mild VOC exposure.
This level of exposure is generally not dangerous on its own, especially if it only happens every once in awhile. However, if it happens regularly over the span of several years, it could cause long-term damage your lungs or lead to other health complications.
It's important to note that even a one-time exposure to extremely high levels of VOCs can result in much more serious and long-term symptoms. However, severe VOC exposures are relatively rare and happen most often to people in hazardous occupations that require them to work with or around dangerous VOCs.
Should I be Concerned About VOCs?
If you have a lung or breathing disorder like asthma or COPD, then you probably should be concerned about the amounts of VOCs you get exposed to day-to-day. People with lung conditions are much more vulnerable to the damaging effects of volatile organic compounds for a variety of reasons we'll cover in the next section below.
However, if you are a healthy adult, the answer is not so clear-cut. Researchers are still not sure what kind of impact low-level exposure to VOCs can have, in the long term, on your health.
Research suggests that all the VOCs you encounter as you go about daily life could have a cumulative effect, meaning that even mild exposure over a lifetime could lead to chronic disease. For example, several studies suggest that VOCs from regular activities like cooking and cleaning, if you do them frequently enough, could raise your risk for developing COPD later in life.
Because of this, experts generally recommend that you do your best to limit your exposure to VOCs outdoors and in your home. That could include using low-VOC products, keeping your house well-ventilated, and staying away from sources of second-hand smoke.
In general, exposure to VOC's is most likely to be dangerous if:
- You are exposed to moderate or high levels of harmful VOCs
- You are exposed to low levels of harmful VOCs for a long period of time
- You have asthma, COPD, or another respiratory disease
The most clear and severe cases of adverse effects tend to happen in people who are exposed to above average amounts of VOCs. Studies on a wide range of volatile organic compounds have found that overexposure can increase your risk for cancer, blood disorders, lung conditions, and other serious diseases.
Here are some of the long-term health problems that VOCs can cause:
- Lung damage
- Kidney damage
- Liver damage
- Central nervous system damage
- Blood disorders
- Anemia
- Increased risk for cancers like leukemia (from very heavy or long-term exposures)
Volatile organic compounds are an unavoidable part of daily life, but there are still many things you can do to protect yourself from their harmful effects. For instancde, many hazardous VOCs come from man-made sources that you can avoid and keep out of your home.
How VOCs Affect People with COPD and Other Lung Diseases
Volatile organic compounds that affect your respiratory system tend to have particularly bad effects on people with existing lung diseases, especially asthma and COPD. Because of this, many experts advise people with these health conditions to take special measures to avoid VOCs as much as possible.
Asthma and COPD make your lungs extra sensitive to the quality of the air you breathe. Even temporary exposure to small amounts of respiratory irritants, such as dust, fragrances, and VOCs, can trigger coughing fits, shortness of breath, and other respiratory symptoms.
If you have severe COPD, exposure to VOCs can make your breathing symptoms worse for hours or even days. They can also make you more likely to experience a COPD exacerbation.
If you have high levels of VOCs in your home or workplace, it can make it more difficult to manage your disease in general. You might experience more frequent flare-ups, worse shortness of breath, and an increased risk for lung infections.
Keeping your symptoms under control is a vital part of keeping your lungs healthy, and anything that triggers them on a regular basis can accelerate irreversible lung damage. Because of this, being exposed to harmful VOCs indoors every day can permanently worsen your COPD.
Over the long term, this could have a significant impact on your overall health and quality of life. It can make it more difficult to breathe, more difficult to sleep, and make activities like walking and doing chores around the house more tiring.
Which VOCs Are Bad for Your Lungs?
Now that we've gone over the basics of volatile organic compounds and their risks, let's take a closer look at some specific VOCs that you may be exposed to every day. In this section, we'll introduce you to several of the most common VOCs that are dangerous to breathe so you can better recognize and avoid them in everyday life.
Formaldehyde

You've probably heard of this volatile organic compound before; formaldehyde is an exceptionally common gas that is dangerous to breathe except in very low concentrations.
This VOC originates from a variety of natural and man-made sources. In fact, your body produces a tiny amount of formaldehyde as part of its normal metabolic functions.
However, many commercial products like wood, soaps, and adhesives contain hazardous amounts of formaldehyde. When you use these products in your home, they can emit enough formaldehyde vapor to make the air unhealthy to breathe.
Even very low levels of formaldehyde can cause mild symptoms like eye, nose, and throat irritation. Sensitivity to formaldehyde varies widely from person to person; some (e.g. people with asthma) experience strong allergic reactions when exposed to even a small amount, while others are only bothered by high concentrations of formaldehyde in the air.
The best way to avoid formaldehyde is to replace formaldehyde-containing products with non-toxic alternatives and avoid bringing formaldehyde-treated furniture and wood into your home. If you must, you should air out your house thoroughly and avoid spending time indoors until the bulk of the formaldehyde has had time to dissipate.
Here are some more details about where formaldehyde comes from, what the symptoms of formaldehyde exposure look like, and how it affects your lungs.

Where Formaldehyde Comes From
- Dish soap
- Cosmetics
- Fabric softeners
- Disinfectants
- Permanent-press fabrics
- Leather treatment products
- Treated woods (e.g. plywood)
- Cigarette smoke
- Burning wood and fuel
- Insulation materials
- Carpets
- Other building materials
- Paints and varnishes
- Glues and adhesives
- Paper
Symptoms of Formaldehyde Exposure
- Nose and throat irritation
- Eye irritation
- Skin irritation
- Runny nose
- Difficulty breathing
- Headache
- Nausea
- Lung function decline
- Nose and throat cancers (rarely from long-term or heavy exposures)
How Formaldehyde Affects Your Lungs
Formaldehyde is toxic to the tissue that lines your respiratory tract in relatively low concentrations. According to the Agency for Toxic Substances and Disease Registry, it is not healthy to breathe air with formaldehyde concentrations above .003 ppm (parts per million).
Some of the most common symptoms of exposure to formaldehyde-contaminated air are eye irritation, nose irritation, and airway inflammation. It can cause serious damage to the delicate tissues in your lungs in high enough concentrations, and long-term exposure can cause chronic respiratory symptoms.
Studies show that workers who are overexposed to formaldehyde on the job experience significant lung function decline. Although it is uncommon, occupational exposure can lead to occupational asthma and rare nose and throat cancers.
Formaldehyde is particularly dangerous for people with existing lung diseases, for whom low levels of formaldehyde can trigger breathing difficulties. One study, for instance, found that formaldehyde released by typical laminate flooring was enough to cause severe respiratory symptoms and possibly even cancers in people with asthma and COPD.
Occupations that Put You at Risk of Formaldehydes Exposure
- Manufacturing plastics, resins, and foam insulation
- Hospital or medical work
- Dentistry
- Laboratory workers
- Construction work
- Textile and furniture workers
- Agricultural work (especially livestock farming)
- Morticians who work with embalming fluids
- Beautician work that exposes you to formaldehyde-containing dyes, cosmetics, and other body products
Benzene
Benzene is an abundant volatile organic compound found in many substances you encounter every day. Most people get exposed to benzene by breathing in gasoline fumes (e.g. while filling up your car) or air contaminated by emissions from cars and other fuel-burning devices.
However, certain common household products like paints, carpet, and glues also contain harmful levels of benzene. These products can heavily pollute the air in your home, especially when used for large projects like installing new carpet or painting your walls.
As the case is with many other VOCs, researchers have difficulty estimating exactly how much benzene is safe to breathe. Recent studies suggest that even low-level benzene exposure (e.g. living next to a gas station) can, over time, raise your risk for leukemia and other serious diseases.
For frequent, long-term exposure, benzene levels as low as 1ppm can be dangerous and result in serious blood disorders

If you have chronic obstructive pulmonary disease (COPD), you know that your lung health is directly linked to your systemic health. Just having COPD puts you at a higher risk for respiratory infection, heart disease, high blood pressure, and even mental health conditions like depression and anxiety. But did you know that there’s even a link between your oral health and COPD?
Chances are, you’ve been told from a young age that brushing your teeth will help you prevent cavities and have a nice smile. But this leaves out a lot of details about how your oral hygiene plays a bigger role in your overall health and wellbeing. According to a study funded by the COPD Foundation, people with severe COPD have poor oral hygiene and they also have poor oral health-related quality of life.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In this post, we’ll discuss some of the reasons COPD patients tend to have poor oral health in comparison to the general population and we’ll also give you some tips for improving your oral health routine in order to live more comfortably with COPD. If you have any questions, please don’t hesitate to leave them in the comment section below so we can get back to you. Alternatively, you can reach out to your doctor for more information about this subject.
How Does COPD Affect Your Oral Health?
When someone is told that two seemingly unrelated organs in the body like the lungs and the teeth or gums are inextricably linked, they’re often surprised. However, the closer you look, the more you’ll realize that they’re related in a number of ways, whether it’s directly or indirectly. The body, as a whole, is a system, so it’s not surprising that something that affects one part will eventually have an effect on the whole.
The Effects of Smoking
The first reason that COPD patients are more likely to have dental health issues is that most COPD patients either currently smoke or were smokers in the past. According to the American Lung Association, around 85 to 90 percent of COPD cases are caused by cigarette smoking and around 38 percent of COPD patients report that they are still smokers. Over the decades, evidence has consistently shown that smoking is incredibly bad for your teeth and gums.

In your mouth, there is a constant battle going on between good bacteria which cleans your teeth and gums, and bad bacteria which leads to tooth decay and gum disease. Smoking negatively affects the quality of your saliva by destroying protective macromolecules, proteins, and enzymes. In other words, the immunological aspect of your saliva is severely hampered the more you smoke.
Smoking also affects your immune system as a whole meaning your body will be less equipped to deal with an infection in your gums or teeth. This study shows that cigarette smoking can have one of two effects on the body. It either exacerbates immune responses leading to chronic inflammation in the body or it attenuates the immune response. Either way, the immune system is less capable of doing its job and warding off infections before they become serious or even life-threatening.
Changes in Your Routine
There’s no doubt about it, being diagnosed with COPD can be life-changing. You might be pressured by your doctor or family to make sudden and drastic changes to your lifestyle, all of which can be daunting and feel like the weight of the world is on your shoulders. More often than not, this causes people to fall back on aspects of their daily routine that they’ve kept up on for many years like practicing good oral hygiene and even making it to the dentist regularly.

Considering the fact that COPD patients visit their doctor more frequently than the general population and many of them are working and maintaining their personal lives and relationships, it can be very difficult to find time to make it to the dentist. And the longer this goes on, the more likely it is that you could develop something like gum disease or periodontitis without even knowing.
COPD Medication
Believe it or not, the medication you take for COPD is another thing that could be causing a decline in your oral health. According to this patient education manual created by the American Thoracic Society, COPD medication can cause dry mouth, a condition where your salivary glands do not produce enough saliva. While this may seem rather harmless, it can actually be quite dangerous if it’s prolonged because saliva plays such a vital role in protecting your teeth and gums.

Inhaled bronchodilators (both short- and long-acting) can cause dry mouth. These medications are used to open up the airways to help you breathe easier and help them clear mucus. Also, inhaled anti-inflammatory medication (corticosteroids) like beclomethasone, budesonide, or fluticasone are known to cause dry mouth. Since these medications are a core part of your treatment plan, it’s best not to completely eliminate them, but to find a workaround for coping with dry mouth instead. This article will give you a good overview of how to deal with dry mouth.
Another potential issue caused by COPD medications is something called oral thrush. This is an infection that occurs in the mouth and throat due to a weakened immune system caused by inhaled medication. Typically, this condition is not serious, but it can cause discomfort while eating and you may need to take antifungal medication in order to get rid of it. Oral thrush is also known to cause or contribute to dry mouth.
How Does Your Oral Health Affect COPD?
Similar to how COPD affects your oral health, there’s also a mountain of evidence suggesting that your oral health can negatively affect your COPD. According to a study published in the Journal of Periodontology, periodontal disease may increase the risk of respiratory infection such as pneumonia in COPD patients. This is a condition that causes the alveoli (tiny air sacs in the lungs) to fill with fluid leading to a chronic cough and breathlessness.
It Can Alter Your Diet
Probably the most likely way that your oral health will affect your lung health is by altering your diet. If you’ve read our articles here at LPT Medical before, you likely know how important your diet is when it comes to reducing chronic pain while preventing breathlessness and fatigue. Most COPD patients should maintain a diet high in protein, healthy fats, and fiber, however, it depends on your individual circumstances.

As we get older, our dental health declines significantly. According to Boston Magazine, people between the ages of 35 and 44 years old have lost at least one tooth. And between the ages of 65 to 74, about 26 percent of people have lost all of their teeth. This is due to a number of causes such as tooth decay, gum disease, periodontal disease, and even traumatic injury. This can impact your diet because it may prevent you from eating certain foods.
-jpg.jpeg)
Unfortunately, foods that are easy to consume and provide us with a lot of energy also tend to be the worst for us. Things like fruit juice, soda, yogurt, and processed foods are convenient, but they’re also laden with sugar and additives that will exacerbate your respiratory symptoms and leave you feeling exhausted and unmotivated. Taking some extra time to cut or break your healthy foods up into smaller pieces may remedy this issue.
It Can Lead to Infections
Most dental infections occur in the tooth, gums, or supporting structures of the teeth. But did you know that dental infections can actually spread to other parts of the body if they aren’t treated? Most COPD patients have a weakened immune system meaning it will be more difficult for your body to fight it off. In certain cases, these infections can be severe and even life-threatening so it’s best to always seek help sooner rather than later. What’s more, dealing with dental issues can be extremely draining and it will take time and energy away from your COPD routine.

Preventing infections is absolutely imperative as a COPD patient. Lung infections are the most likely cause of flare-ups and exacerbations, and they’re also the most likely cause of someone being admitted to the hospital due to COPD. So, whenever you go to brush or floss your teeth, think of it as being beneficial for your full-body wellness rather than just your teeth and gums.
What Can be Done to Improve Your Oral Hygiene?
Brush More Frequently
Possibly the simplest way to improve your oral hygiene is to brush and floss more frequently. With the busy schedules that many people have nowadays, it can be hard to find the time to brush twice a day and floss, but it’s the best thing you can do for your oral health. People tend to skip flossing, but this is the only way to reach the bacteria between your teeth where it can cause the most harm. Be sure to brush your teeth at least twice a day and floss at least once a day.

Drink More Water
Proper hydration not only helps with organ function, but it can also help prevent cavities. When you think about all of the different foods you consume in a day, it’s not hard to see why this is so important. Water removes food from between your teeth, prevents dry mouth, and can dilute acids that stain and eat away at your teeth. Rather than drinking a bunch of water in the morning or right before bed, try drinking water throughout the day, especially during meals. This way, food particles don’t have the opportunity to latch onto your teeth and cause damage.
.jpg)
Schedule Regular Teeth Cleanings
While you can and should take your dental health into your own hands, it’s also important to see a dental specialist regularly. Even if you are careful with your brushing and flossing, any leftover plaque on your teeth when you go to bed at night will turn into something called tartar. This is basically a hardened version of plaque that can only be removed with special tools by your dentist. Another reason to schedule regular teeth cleanings is so that your dentist can make sure your teeth and gums are healthy and that you’re on the right track. Dental issues are almost always easier to fix when they’re detected early on.
Consider Dental Implants
It’s estimated that about 90 percent of people with no teeth use dentures. And while dentures can improve your smile, they don’t provide any benefits when it comes to eating. Dental implants, on the other hand, essentially provide you with a new pair of teeth that are just as effective as natural ones when it comes to chewing. In other words, you’ll be able to keep up with the dietary requirements that your doctor gave you to help you manage COPD. Dental implants can be used to replace just one missing tooth or a whole mouth of missing teeth.
.jpg)
The important thing to remember with dental implants is that your oral hygiene is still incredibly important. While implants can’t decay like your natural teeth can, you will still need to keep your gums healthy in order to prevent gum disease and periodontal disease. When you get dental implants, you will be provided with special cleaning tools and instructions on how to maintain your new teeth. Not everyone is a candidate for dental implants so you’ll need to schedule an appointment with a periodontist to see if they’re right for you.
Conclusion
There is a two-way road between your oral health and your lung health. Years of smoking and the development of COPD can contribute to problems like tooth decay and gum disease. On the other hand, maintaining a poor dental health regime can cause flare-ups in your respiratory symptoms. In other cases, poor dental health and poor respiratory health can contribute to comorbidities like heart disease, poor circulation, and more.
While you have a lot to worry about like making it to doctor’s appointments and pulmonary rehabilitation, it’s always important to make time for your oral health as well. The American Dental Association recommends brushing your teeth at least twice a day with fluoride toothpaste and you should go in for teeth cleanings every six months. And if you have any additional concerns about how COPD could affect your oral health, be sure to speak with your doctor immediately.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Lastly, if you’re a COPD patient looking for a better solution for your oxygen needs than a bulky oxygen tank, take some time to look through our portable oxygen concentrators here at LPT Medical. POCs are electronic oxygen delivery devices so you’ll never have to refill them. They’re also extremely travel-friendly and easy to use. We recommend the Inogen One G5 and Caire FreeStyle Comfort to most patients, but you can learn more about the specifications by reaching out to our respiratory specialists.
.png)
Oxygen therapy or supplemental oxygen is the use of oxygen for medical purposes. It’s used by around 1.5 million people in the United States and can alleviate symptoms associated with a variety of respiratory conditions such as chronic obstructive pulmonary disease (COPD), asthma, and cystic fibrosis. Although oxygen therapy is a common medical treatment, there seems to be a lot of confusion around what it is, how it works, and why it’s so important.
In order to help you better understand oxygen therapy, we’re going to take a look at some of the terms associated with it including medical oxygen terminology and medical equipment terminology. Medical terms include any terms associated with diagnosing oxygen issues in the body and oxygen equipment terms focus on the actual equipment and processes used to treat oxygen deficiencies. By doing so, you’ll have a better understanding of how oxygen therapy works and how it can benefit certain people.
In the following post, we’re going to take a look at the most common oxygen therapy terms and clarify any misconceptions that you may have about them. Whether you’ve recently had a blood gas test, been diagnosed with a respiratory disease, or you’re just curious, read on to learn more.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Medical Oxygen Terminology
Oxygen is one of the fundamental building blocks of life. All humans need oxygen to survive and all humans need the right amount of oxygen in order to be healthy. While the average person doesn’t spend their time thinking about their ability to breathe or process oxygen safely and effectively, for others, it’s a matter of life and death.
Underlying conditions like heart defects, lung diseases, or physical injury can cause oxygen deficiency and symptoms like lightheadedness, shortness of breath, and even organ failure. If you’re experiencing any of these symptoms, it’s best to visit a doctor as soon as possible and ask about getting a blood gas test. Let’s take a look at some of the medical terms associated with oxygen.
Oxygen Deficiency
Every time you breathe, oxygen enters your bloodstream and red blood cells transport it throughout the body. This oxygen is used to nourish all organs in the body and perform an important process called metabolism. In a healthy person, blood oxygen levels vary between 75 and 100 millimeters of mercury (mm Hg), but slight variations are usually not a concern.
When your blood oxygen level drops below 60 mm Hg you are considered oxygen deficient, and your doctor will most likely prescribe some type of oxygen therapy to return them to normal levels. You should see a doctor if you experience one or more of the following:
- Shortness of breath while exercising or during sleep
- Lightheadedness
- Weakness throughout the body
- Breathlessness while at rest
Oxygen Saturation
Oxygen saturation, also known as O sats, is a term that refers to the saturation of oxygenated hemoglobin in the blood. Hemoglobin is an iron-rich protein found in red blood cells and each one contains four globular protein subunits which can each carry one oxygen molecule. Because each organ in the body needs a very specific amount of oxygen, hemoglobin plays an important role in regulating oxygen levels and ensuring every cell in the body has the oxygen it needs.
One of the most important things to understand about oxygen saturation is the oxygen-hemoglobin dissociation curve, also known as the oxyhemoglobin dissociation curve. This curve compares the partial pressure of oxygen in the blood to the oxygen saturation level. Partial pressure (PaO2) refers to the actual oxygen content found in arterial blood. It’s a measurement of the pressure that’s exerted on a container wall within a mixture of other gases found in the arteries. Oxygen deficiency, like we discussed above, indicates a low partial pressure of oxygen and is measured in mmHg.
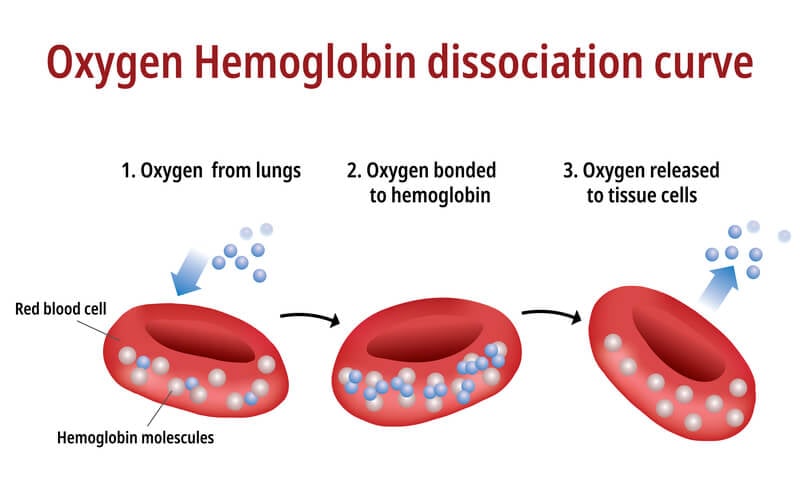
On the other hand, oxygen saturation levels are measured as a percentage. The percentage indicates the amount of hemoglobin (Hgb) binding sites that are carrying oxygen. Partial pressure of oxygen and oxygen saturation levels correlate directly meaning a higher partial pressure will result in a higher oxygen saturation level. If all hemoglobin binding sites are filled, this would result in a saturation of 100%.
When diagnosing the cause of symptoms like lightheadedness and shortness of breath, it’s important for your doctor to understand both the partial pressure of oxygen and your oxygen saturation levels. While partial pressure will give them a more accurate picture of your oxygen levels, oxygen saturation levels can be determined without drawing blood using a device like a pulse oximeter.
Hypoxemia and Hypoxia
Hypoxia and hypoxemia are two terms that are often confused, but it’s important to understand how they differ. Hypoxemia simply refers to low oxygen levels within the blood. Respiratory conditions like chronic obstructive pulmonary disease (COPD), pneumonia, or asthma are usually the cause of low oxygen levels, however, other risk factors include old age, smoking, and being at a high altitude. Typically, anything below 60 mmHg is a cause for concern, but your doctor may take action before that.
Hypoxia is similar to hypoxemia but instead refers to low oxygen levels in the tissues of your body. Hypoxia is sometimes, but not always, associated with hypoxemia. If hypoxemia is present, you will likely have lower oxygen levels in various tissues throughout the body. However, hypoxia can also be local meaning it’s only present in a certain tissue. This can result from low hemoglobin concentration (anemic hypoxia), low hemoglobin saturation (hypoxic hypoxia), or poor cardiac output (stagnant hypoxia).
While hypoxia is a partial obstruction of oxygen supply to a tissue, anoxia refers to a complete lack of oxygen in a tissue. This is usually caused by an injury that prevents blood flow like a hypoxic-anoxic brain injury. This type of hypoxia often results in permanent brain injury or death if they aren’t treated quickly and accordingly.
Oxygen toxicity (hyperoxia)
Around 21 percent of the air that we breathe is oxygen. The rest of the air is made up of about 78 percent nitrogen, as well as carbon dioxide, and a small amount of other gases. Because oxygen is such a crucial element for our bodies, you would think that breathing pure oxygen would be healthy, but this is not the case.
While hyperoxia is much more rare than hypoxemia, it’s still possible to have too much oxygen in the body. Oxygen toxicity is divided into two groups: acute toxicity and chronic toxicity. Acute toxicity can damage the central nervous system while chronic toxicity can lead to pulmonary edema, atelectasis, or lung passageway obstruction. Chronic oxygen toxicity has also been found to have an effect on the eyes, mainly in the form of retina damage.

Fortunately, it’s extremely uncommon to experience oxygen toxicity. Most cases of the condition involve divers because diving tanks deliver oxygen at a higher pressure than on land and often use special gas blends like enriched air nitrox. Although it is possible to experience chronic oxygen toxicity while on oxygen therapy, following your doctor’s instructions will ensure that you never get more oxygen than you need.
Cyanosis
Cyanosis is the discoloration of skin, usually on the hands or feet, due to low oxygen levels. The discoloration usually occurs at extremities because oxygen needs to travel the farthest to reach those points. It can result from things like low blood pressure when there is not enough pressure for blood to reach certain parts of the body or artery problems like clots, peripheral vascular disease, or venous insufficiency.
Medication and oxygen therapy are typically prescribed to treat cyanosis, but it will depend on what is causing the issue. For example, if it’s the result of blood clots, you may need blood thinners or other medications. However, if it’s due to a pulmonary issue, you may be prescribed medical oxygen.
Pulse Oximetry
Pulse oximetry is the simplest and least intrusive way to test your blood oxygen. A pulse oximeter device is usually attached to the finger and measures the level of oxyhemoglobin and deoxygenated hemoglobin in the arteries. Because deoxygenated blood is darker, it absorbs more light and because oxygenated blood is lighter, it reflects more light. Your pulse oximeter will compare these two values and give you a general idea of your oxygen saturation.

The benefit of pulse oximeters is that they’re portable and can be used wherever you need them. If you’re currently undergoing oxygen therapy, you should check your oxygen levels with a pulse oximeter regularly to ensure you’re maintaining healthy levels. However, pulse oximetry has limited uses. While your doctor will likely advise you to use one if you have low blood oxygen levels, he/she won’t use it to diagnose any medical condition.
Arterial Blood Gas Test
Arterial blood gas tests (ABG) are another common way of testing oxygen levels in the blood. While ABG tests are more intrusive than pulse oximetry, they provide your doctor with more accurate and detailed information about your health. Your doctor may recommend having an ABG test if you are experiencing nausea, difficulty breathing, shortness of breath, or they have reason to believe that you may have a lung or kidney disease.
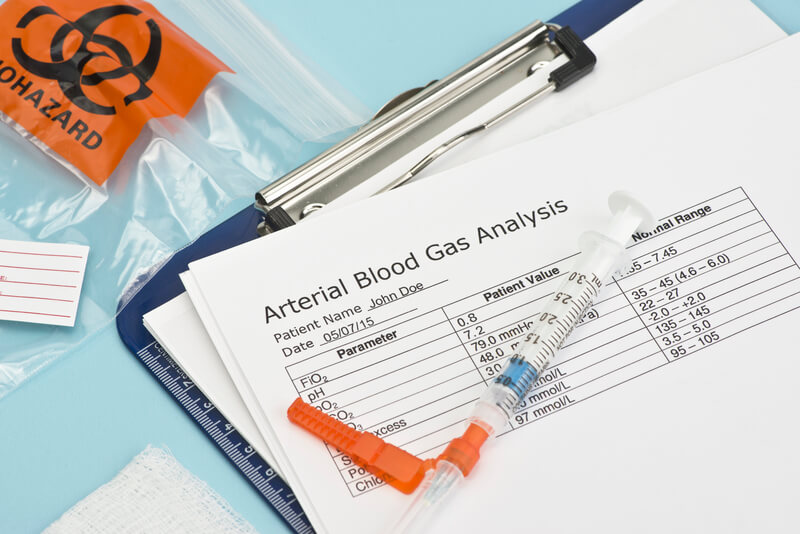
During a blood gas test, your doctor will collect a small sample of blood. This blood will usually be drawn from the arm, wrist, or groin using a small needle. Since blood needs to be tested within 10 minutes of being drawn, you’ll get your results shortly after. There are several pieces of information that can be drawn from your arterial blood gas test including:
Partial Pressure of Oxygen / Carbon Dioxide
This is a measurement of the pressure of oxygen or carbon dioxide that’s dissolved in the blood. This will tell your doctor how efficiently your body is able to bring oxygen into the bloodstream and remove carbon dioxide.
Oxygen Saturation
This result will reveal how much oxygen is being carried by the hemoglobin proteins in your bloodstream. Typically, blood saturation levels between 95 and 100 are healthy, and anything below 90 is a cause for concern.
Arterial Blood pH 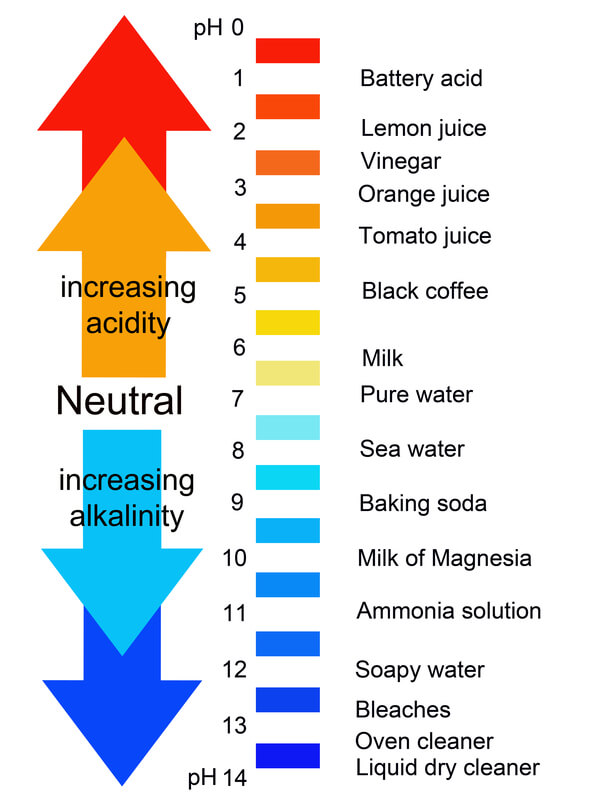
The arterial blood pH level will tell you the amount of hydrogen ions in your blood. Any pH lower than 7.0 is considered acidic while anything higher than 7.0 is considered acidic. A high pH score usually correlates with a higher bicarbonate level while a low pH level is associated with high carbon dioxide levels.
Bicarbonate
Bicarbonate is produced through your body’s metabolic process. It regulates pH levels in your body and then it is transported back to the lungs to be released as carbon dioxide. Low bicarbonate may cause a condition called metabolic acidosis resulting in high blood acidity and high bicarbonate may be a sign of metabolic alkalosis which causes pH to increase in tissue.
Oxygen Equipment Terminology
Oxygen equipment is any equipment used to administer medical oxygen. If your doctor prescribes you oxygen, you will have several options regarding the device and accessories that you use. However, it’s important that you follow your doctor’s directions carefully. Not all oxygen therapy devices are created equal, so you should take your time and ensure that all your needs are met before investing in anything.
Like any industry, the supplemental oxygen industry is constantly evolving and adapting to patients needs. There are hundreds of conditions and diseases that can result in low blood oxygen do everyone has unique circumstances. Let’s take a look at some of the most common oxygen equipment terminology you should be aware of.
Oxygen Tanks

Oxygen tanks are the most standard form of oxygen therapy. The oxygen that it dispenses is compressed and contained within the tank. When it runs out, you’ll need to either get it refilled by a professional or have it swapped out with another one that’s full. Most oxygen tanks are bulky and can’t be moved but you can buy portable ones that are a bit more manageable. However, the more lightweight and portable you oxygen tank is, the less oxygen you will get out of it.
One of the major downsides to using oxygen tanks for oxygen therapy is that they can be very dangerous. First and foremost, oxygen tanks present a major fire hazard. While the oxygen itself is not flammable, oxygen-rich environments can cause some materials to burn that wouldn’t normally burn and can make some things burn more than they normally would. Also, due to the size and material that oxygen tanks are made out of, they can cause injury fairly easily.
Liquid Oxygen Tanks
Liquid oxygen differs from regular oxygen tanks in that they are stored as a liquid rather than compressed air. According to the Lung Institute, liquid gas that’s converted to a gas expands 860 times meaning liquid oxygen tanks are much more compact than compressed oxygen tanks. This also means liquid oxygen is stored at a much lower pressure making it safer to use. The one downside is that it can be more pricey than traditional oxygen tanks due to the process of producing and storing it.
Oxygen Conserver Device (OCD)
An oxygen conserver, not to be confused with an oxygen concentrator is a device that attaches to an oxygen tank and manages its flow type. It’s called a conserver because it causes the oxygen to only be released when the patient inhales, thus conserving a significant amount of oxygen and allowing you to be out and about longer without having to refill your tank. A normal breathing pattern means inhaling one third of the time while exhaling the other two thirds, so oxygen conservers can be extremely effective.

Fixed-Pulse and Demand-Pulse
There are two different types of oxygen conservers: fixed-pulse and demand-pulse. A fixed-pulse conserver has a set volume of air that’s released when a patient inhales. This type of conserver is designed to release a fraction of inspired oxygen (FiO2) comparable to that of a continuous flow device.
Demand-pulse conservers are similar to fixed-pulse units in that they release oxygen when the patient inhales. However, these devices continue to release a set amount of oxygen after the initial volume is released. This could be a consistent flow or it could diminish until the valve completely closes.
Oxygen Concentrators
Oxygen concentrators are some of the most state-of-the-art oxygen therapy devices on the market. As opposed to oxygen tanks, oxygen concentrators don’t actually hold oxygen inside the unit; the oxygen is drawn from ambient air, purified and released in a concentrated form. The obvious benefit to this is that there is never a need to replace oxygen tanks or have them refilled.

There are two types of oxygen concentrators: home oxygen concentrators and portable oxygen concentrators. Home oxygen concentrators can be plugged into any wall outlet while portable concentrators use batteries. And because oxygen concentrators are powered by electricity, accessories similar to those on oxygen tanks are already built in to your device. For example, you can purchase either a continuous flow oxygen concentrator or a pulse-flow oxygen concentrator.
Pulse Flow vs Continuous Flow
Flow settings on oxygen concentrators work similar to conservers that you can buy for your oxygen tank. Continuous flow puts out a constant stream of oxygen and doesn’t account for the user’s breathing rate, whereas a pulse flow or pulse dose oxygen concentrator puts out a set amount of oxygen when the user inhales.
Liter Flow Settings
Another aspect of oxygen concentrators is the liter flow setting. Oxygen concentrators and portable oxygen concentrators can have up to six liter flow settings which determine how much oxygen is actually coming out of the device. While it may seem like the higher setting, the better, you need to follow your doctor’s prescription exactly. Luckily, with a home or portable oxygen concentrator, you can change the liter flow setting with the simple touch of a button. Portable oxygen concentrators range from 3 liters per minute (LPM) to 6 liters per minute. Home oxygen concentrators range from 5 LPM to 10 LPM.
Humidifier

A humidifier is a device that can be attached to many different types of oxygen concentrators, oxygen tanks, and even CPAP devices. If you experience irritation in the nasal passage while using medical oxygen, humidifiers will help prevent this and ensure that you’re breathing humidified air. You will, however, need to replace water in the humidifier when it runs out.
Cannula
A cannula is a plastic tube that delivers medical oxygen to a patient. One end attaches to your oxygen concentrator and the other has two prongs that are inserted into the nose. Because comfort is a major concern when it comes to oxygen therapy, there are a variety of cannulas on the market to help you find one that works best for you. Oxygen cannulas include but are not limited to: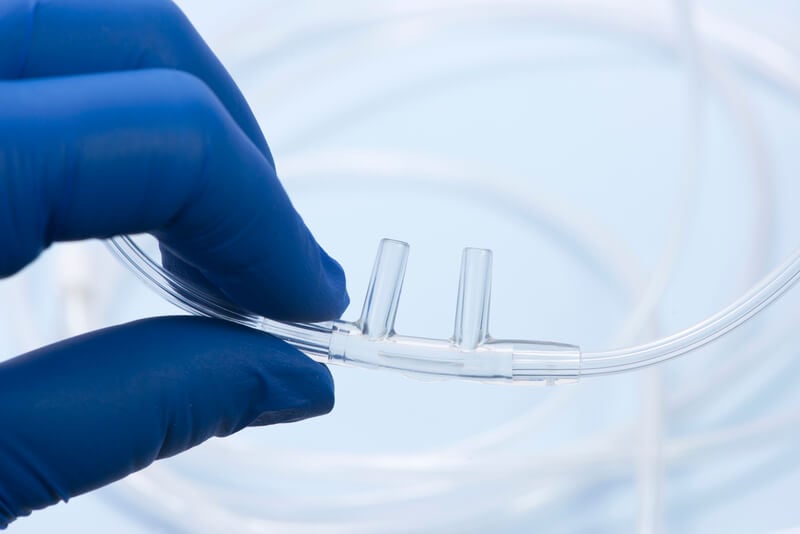
- Curved prong cannulas
- Flared prong cannulas
- Straight prong cannulas
Nebulizer
Although nebulizers aren’t technically “oxygen therapy,” they are part of what’s called “inhalation therapy.” Nebulizers work by using oxygen, compressed air, and a medical solution to create an aerosol, or a mixture of gas and liquid particles. While nebulizers can be used to treat conditions like asthma and COPD, they typically aren’t used to treat low blood oxygen levels like oxygen therapy does.
Recreational vs Medical Oxygen
One common point of confusion for someone that’s new to medical oxygen is understanding the difference between medical and recreational oxygen. Simply put, medical oxygen is used to treat low blood oxygen levels and diseases like COPD and asthma, whereas recreational oxygen is used to improve athletic performance. Many people use oxygen canisters if they're climbing or hiking at high altitude where the air is thin and there's very little oxygen.

Durable Medical Equipment (DME)
If you want to seek compensation from a private health insurance company or Medicare, you should understand the term “durable medical equipment.” Usually what this refers to is any equipment that can withstand repeated use, serves a medical purpose, and is not useful to someone without an illness. If there is any confusion about this, you should clarify with your insurance company.
Conclusion
Oxygen therapy is something that’s constantly evolving so it’s not uncommon for someone to be confused about how it works or why it’s important. Hopefully, this list helps to clarify any confusion about terms or concepts that you may have had and if not, be sure to check back regularly as we’ll upgrade it regularly with any new terms you should know.
If you just started oxygen therapy, your doctor will be your best resource for any concerns you have about oxygen devices, flow settings, and oxygen accessories. While oxygen therapy is becoming safer and easier to use by the year, you will still want to make sure you’re receiving the optimal treatment for your medical condition.
The stress and hassle of traveling can be a challenge for anyone, but it poses a special challenge for those struggling with chronic diseases like COPD.
If you or someone you love has COPD, then you know that it can make major changes in daily routine difficult to manage. COPD patients struggle every day to keep their symptoms under control and often have strict treatment regimens they have to follow carefully.
This difficulty gets amplified when you leave your house, and it can make any kind of traveling a daunting task. Especially if you use supplemental oxygen, it takes a significant amount of planning and preparation to safely spend an extended time away from home.
However, this doesn't mean that travel is impossible, even if it does make it more complicated. With the right planning and preparation, you can still go on trips and adventures without compromising your health.
The Challenges of Traveling with COPD

If you have COPD, there are many different things you need research and consider before planning an extended trip away. Overlooking even a small detail could be dangerous or throw a major wrench in your travel plans.
For instance, you need to thoroughly research your destination and where you're staying to ensure that you don't put your lungs in hazardous conditions. You also have to pack much more carefully so you don't forget any medication or medical equipment you need.
And if you have a prescription for supplemental oxygen, it gets even more complex. Knowing general oxygen safety isn't enough; you need to plan and prepare in order to avoid problems, accidents, and running out of oxygen.
If you suffer from COPD, failing to plan properly is not just irresponsible, but can actually be dangerous for your health. Poor preparation could result in missing your transportation or suffering from severe breathing problems far away from home.
In this article, we're going to show you how to make traveling with COPD and oxygen as safe and convenient as possible, whether you travel by plane, car, or any other mode of transportation. We'll tell you what to look out for, how to prepare, and how to handle your oxygen equipment safely on the journey.
Going far away from home can be scary when you have a chronic disease, especially if you have severe COPD. But if you follow the tips in this article, you'll be prepared for the challenge and able to embark on your journey worry-free.
The Challenges of Traveling with Oxygen

Millions of people in the US rely on supplemental oxygen, and it's a lifeline for many patients with COPD. If you or someone you love uses supplemental oxygen, then you need to learn all about how to safely use and transport oxygen when you travel.
Whether you use oxygen occasionally or continuously, lugging around heavy oxygen tanks and other equipment can be complicated and inconvenient. Being tethered to a medical device is not easy, and it's no wonder many patients feel limited or trapped by their oxygen therapy.
What makes traveling potentially dangerous for oxygen patients is that it takes you out of your familiar environment and far away from your doctor, home, and most possessions. If you forget any equipment, run out of oxygen, or something else goes wrong, it can be more difficult to get help in an unfamiliar place.
Another challenge of traveling with oxygen is that it disrupts your normal routine, which can make it difficult to keep up with your usual COPD treatment schedule. Traveling to new places can also expose you to new allergens and respiratory irritants, making flare-ups more likely and potentially increasing your oxygen needs.
There's also the problem of the mode of travel itself, which can limit your oxygen options and make therapy more complicated. For example, when you travel long distances by car, it can be difficult to access, adjust, and switch out your oxygen supply.
Traveling by plane is even more complicated because of airport security and restrictions on what you can bring aboard. Airlines usually only allow you to bring portable oxygen concentrators on the plane, as they consider liquid or compressed gas oxygen tanks a safety risk.
In general, traveling makes oxygen therapy more inconvenient at the same time that it becomes more difficult keep your symptoms at bay. It also means preparing for a variety of potential problems and situations that you can't control.
But even though living with COPD may make travel more complicated, you can still find ways to explore and have new adventures. In the next sections, we'll cover all of these complications and show you a variety of practical tips for traveling safely with oxygen and COPD.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
First Steps Before Your Trip
Talk To Your Doctor!
Consulting your doctor should be the very first step you take before planning an extended trip away from home. It's important to get your doctor's okay, as well as important medical records and prescription information, before you travel.
First, talk to your doctor about where you are visiting and what kinds of events and activities you are planning to participate in. That way, if there are any concerns or red flags, your doctor can warn you and give you advice to help you avoid problems.

Depending on the severity of your COPD and any recent medical problems, your doctor might impose limitations on your travel or what sorts of activities you can do. He may also be able to give you helpful advice for managing your symptoms and continuing treatment on your trip.
You should also ask your doctor for a detailed list of your medications in case you need to verify your medicine with travel personnel at any point along your trip. You should also make sure you have your doctor's up-to-date contact information in case you have an emergency or simply need to ask a question.
Research Your Destination

Before you get your heart set on a destination, make sure you take some time to research the place you want to visit. That way, you can find out about any conditions that could affect your COPD and make arrangements ahead of time to minimize your risk.
Local climate conditions including weather, air pollution, humidity, and altitude are all important things to look up before you travel to an unfamiliar location. You should also look up local hospitals and medical services near your travel destination so you can get help quickly if something goes wrong.
For example, you will need to take extra precautions if you are planning to travel to a high elevation, such as taking extra medication or adjusting your oxygen prescription. Since there is less oxygen at high altitudes, you will have more difficulty breathing, and portable oxygen concentrators may not function correctly.
In especially hot, humid, cold, or polluted environments, you should be ready for flare-ups and prepare to treat more aggressive COPD symptoms. You may need to pack extra medication or equipment (such as a particle mask) to help you cope with poor weather and air quality.

In some cases, the conditions might simply be too dangerous for your health, especially if your COPD is severe or you've experienced a recent hospitalization. If your ideal destination will make it too difficult to control your symptoms and get the medical care you need, you should look for a different place to visit.
Even though travel and vacations are important, they're not worth putting your lungs or your life at risk. Most of the time, you can find a great alternative destination that is more accommodating and easier on your body.
As we mentioned before, you should always consult your doctor before going on any kind of extended trip if you suffer from COPD. If you or your doctor have concerns about climate conditions or medical services during your travels, it's important to take them seriously, even if it means making compromises.
Here are some tips for finding a safe, comfortable travel destination:
- If you are traveling far, do some research on the local climate so you know what to expect.
- Look out for rural places that are far from a hospital or sophisticated medical services. It's important to be able to get quick and effective medical attention in the case of a serious exacerbation or emergency.
- If you are sensitive to weather conditions, try to avoid visiting places with extreme temperatures or humidity. If you can, visit more extreme climates during a season when the weather is more mild and tolerable.
- Exercise caution if you are traveling to a higher elevation than what you're used to, as the air will be thinner and more difficult to breathe. If you have severe breathing troubles, you may need to avoid visiting high altitudes altogether.
- Write down the addresses and phone numbers of local hospitals and clinics in all the areas you are traveling to. Your doctor may even be able to give you recommendations for trusted medical professionals in the region.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Choose Safe and Comfortable Lodging

Once you've chosen a suitable destination for your trip, you still need to find a comfortable place to stay. Unfortunately, not all hotels, resorts, and other types of lodging can accommodate people with special medical requirements.
If your COPD is severe or you use supplemental oxygen therapy, it's important to find lodging that accommodates your needs. You can often find information on medical conditions and disabilities on the company's website, but you should always call ahead to notify them and verify their amenities before your visit.
You should also make sure that the place you plan to stay at is clean, reputable, and has helpful, friendly staff. Here are some more tips for finding a safe and comfortable place to stay as you plan your next trip:
- If you are staying at an inn or resort, make sure they have smoke-free accommodations.
- Look up reviews from other guests who have stayed at the same place to make sure it is clean, safe, and friendly. Cross-reference reviews with the hotel's claims to ensure that what they promise doesn't differ significantly from the experiences of past guests.
- If your lungs are sensitive to fragrances and cleaning products, notify your hotel ahead of time. They may be able to use milder cleaning products or offer unscented toiletries in your room.
- Make sure that any events or venues you plan to visit are smoke-free environments.
- If you need any special help or disability accommodations, check with your hotel ahead of time to make sure they can provide adequate assistance.
- If you use oxygen, check with your hotel ahead of time to ensure there are no safety issues and that they are aware of your medical condition and needs.
- Make sure where you stay has a safe, secure place for you to store your oxygen or other medical equipment. You will need a well-ventilated place to secure any extra oxygen tanks you bring and a steady supply of electricity for your oxygen concentrator, if you have one.
- If you rely on an oxygen concentrator as your primary oxygen source, make sure you notify the hotel that you are bringing medical equipment that requires a constant electricity source. Make sure they have a backup generator or other safeguards in place in case of a power outage.
- If you have requested any special accommodations, make sure you check in with your hotel a few days before your visit to make sure everything is in order.
Stock Up on Oxygen and Other Medications

When you're far away from home, the last thing you want to do is run out of medication. It can be much more difficult to coordinate a prescription refill in an unfamiliar town, and disruptions in your daily medication schedule can be dangerous.
Not having your oxygen, inhaler, or rescue medication when you need it can cause dangerous breathing issues and even require you to go to the hospital. At the very least, going without your medication can cause your symptoms to flare up, which is never pleasant and could lead to a more serious exacerbation.
That's why you should talk to your doctor about stocking up on extra medications to bring with you if you are planning an extended trip. You may need more than your typical amount to last the duration, and you should ask for extra in the case of emergencies or in case you are away longer than expected.
If you use supplemental oxygen, it's particularly important to talk to your doctor and your oxygen supplier before the trip. They can help you make sure that you have enough extra oxygen to last in case of an emergency or one of your other oxygen sources malfunctions.
Depending on where you are traveling to and what company supplies your oxygen, you may even be able to get oxygen delivered to your travel destination while you're there. Each company is different, so you will need to work with your provider ahead of time to find a solution that works for your trip.
Once you've ensured that you will be in no danger of running out of oxygen, you should stock up on other oxygen delivery equipment you may need. You might want to bring extra sets of nasal cannulae, humidifier bottles, and any padding you use to make oxygen therapy more comfortable.
Gather Medical Paperwork

It's important to bring all of your medication with you on your trip, which means you should have a copy of your doctor's records for all of your prescriptions. You should also bring a copy of your COPD treatment and action plans to reference if you need to.
You should keep this paperwork with you at all times when you travel for both medical and security reasons. If you are traveling by plane, train, boat, or using any other transportation service, you may need to present your medical and prescription records to bring medication or oxygen on board.
It's also a good idea to have all of this information on hand in the case of an emergency or hospitalization. Doctors and emergency personnel will be better able to help you if they have immediate, detailed information on your medical condition.
Oxygen Travel Checklist

Careful planning ahead of trips is essential if you use oxygen therapy, especially if you need to use it continuously. It's important to take this preparation step seriously, or you could end up with a serious medical emergency.
To help you the next time you travel, here is a checklist of vital steps you should take before taking any kind of trip with oxygen:
- Notify the place you will be staying at that you are bringing oxygen. Ask if there are any special requirements or safety concerns.
- Get a note from your doctor with your brief medical history and a detailed list of all the medications you use, including your oxygen prescription. Keep it with you at all times when you travel.
- Make sure you have enough oxygen to last your whole trip. Contact your oxygen supply company if you need to stock extra.
- Make sure that your mode of transportation allows you to bring oxygen on board. Be aware that some transportation companies only allow portable oxygen concentrators or have restrictions on the number, type, size, or weight of oxygen canisters you can bring.
- If you are bringing a portable oxygen concentrator, make sure that you have enough batteries to make it last your whole trip. Depending on your mode of transportation, you may be able to plug your concentrator in to your car or recharge your batteries via an A/C outlet along the way.
- Make sure you have a safe, secure place to store extra oxygen tanks during your journey. If needed, your oxygen supply company might be able to deliver oxygen canisters to your destination for you.
- Flying with oxygen can be complicated, and what you need to do depends on which airline you are flying with. Refer to the section on traveling by plane (below) for more information.
Traveling by Car with COPD

Compared to other forms of transportation, traveling by car gives you more control over your trip and your immediate environment. This can make managing your COPD while you travel much easier, since you have more control over your schedule, your space, and any equipment and medications you bring.
Car travel also makes it much easier to bring oxygen and manage your oxygen therapy. As long as you can fit your equipment and canisters safely in your car, you don't have to worry about any restrictions or limitations on the kind of oxygen you can bring along.
Taking a road trip in your car is one of the most convenient ways to travel when you have COPD, but it still comes with some challenges. Before you plan your next road trip, you should learn how to protect your lungs on the road and transport your oxygen safely.
Avoid Respiratory Irritants

Pollution and respiratory irritants are the most hazardous aspects of car travel for people with COPD. When you spend extended amounts of time on the road, you need to be especially careful to protect yourself from car fumes and other respiratory irritants.
First, never smoke in the car or allow anyone else with you to smoke in the car or around you during the trip. This is particularly vital if you are transporting oxygen in your car, as sparking a cigarette becomes a major fire hazard.
If possible, make sure you are riding in a non-smoker's vehicle; even if no one is actively smoking, simply being inside a smoker's car can irritate your lungs and cause your symptoms to flare up. If there is no non-smoker's vehicle available, consider getting the car thoroughly cleaned by a professional or renting a different car for your trip.
Second, keep the windows rolled up as much as possible to keep air pollution, allergens, and exhaust fumes from wafting into your car. You can also set your car's ventilation system to continuously re-cycle the air in the car's cabin, which prevents it from pulling in polluted air from the road.
Over-Prep Your Vehicle and Route

When you have a chronic disease, mishaps like getting lost or stranded can be especially dangerous. If your car breaks down, you could end up stuck in hazardous conditions or even run out of oxygen.
That's why you should always get your car inspected and serviced before a long trip to check for any problems or malfunctions. Make sure they check all the basics, like ensuring your car has fresh oil and that your air filter, engine fluids, and brake pads don't need to be replaced.
You should also keep an emergency preparedness kit in your car along with a first aid kit, a spare tire and jack, and a small gas canister in case you run out of fuel. Your emergency kit should include, at a minimum: a tire guage, an emergency flare, reflective markers, jumper cables, extra water supply, blankets, and a flashlight.
To reduce the chances of any mishaps, you should plan your travel route thoroughly and carefully, making note of any road closures or other potential problems along your path. Make sure you have a map, smartphone, or a GPS device available in case you need to make last minute changes to your route along the way.
As you plan your route, try to avoid busy highways, high-traffic roads, and areas with high levels of allergens you are sensitive to. This will reduce the amount of respiratory irritants your lungs are exposed to and make your symptoms less likely to flare up.
Take Breaks
Even though you spend most of the time sitting down, extended road trips can be physically exhausting. Being stuck in such a small, cramped place can get extremely uncomfortable after awhile.
Building stops and breaks in to your trip, however, can significantly reduce the stress and physical strain of long trips in the car. Make sure you give yourself plenty of opportunities to pause, stretch your legs, and take bathroom trips along the way.
If you need to, break your trip up into smaller chunks find places along your route you can stay at overnight. This can help the trip feel more bearable and can also make it easier to keep up with your normal COPD treatment routine.
Sitting for very long periods of time is not healthy for your body, so you should take every opportunity to stretch and move around when you travel. Stand up, take a short walk, and get your blood flowing at regular intervals during your trip.
Taking Oxygen on Your Road Trip

Transporting oxygen in your own car is much simpler than taking it on any other mode of transportation. The only major things you have to worry about is bringing enough oxygen and making sure you have a safe place to store it in your car.
Oxygen canisters, whether liquid or gas, should always be stored upright in a well-ventilated place. That means you should never transport oxygen canisters in your trunk, which is too small and enclosed a space to store them safely.
Instead, it's best to store extra oxygen canisters on the floor of your car in the space behind the driver's or passenger's seat. If you are using oxygen while traveling, you can store your current oxygen supply in the seat next to you. If you are a passenger, you can also store your canister or portable oxygen concentrator on the floor in front of you, if there's space.
If you are traveling in a warm climate, make sure you never leave your oxygen cylinders for too long in the hot car. If you will be leaving the car in the heat for an extended period of time, you will need to remove the cylinders from your vehicle and find a secure, climate-controlled place to store your oxygen while you're gone.
Lastly, it's important to make sure that you bring enough oxygen with you to last you your whole trip. If you don't have enough space to store it all in your car, talk to your oxygen supply company to see if they can deliver more to you at your destination.
Flying by Plane with COPD

Planes are one of the more difficult modes of transportation to use if you have COPD. It's significantly more difficult if you are traveling with oxygen, because of airport restrictions and security. In fact, if you don't have a portable oxygen concentrator, you cannot bring oxygen on a plane at all.
There are several important things to remember b
Living with a respiratory disease can make normal activities and hobbies difficult. Traveling, however, can be particularly challenging to do when you suffer from a chronic respiratory condition.
Traveling brings up concerns about medication, supplemental oxygen, access to proper medical care, and more. But if you're traveling to a higher elevation than you are accustomed to, then you have to consider the effects of high altitude as well.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The thin air at high elevations can cause a variety of respiratory symptoms in healthy people and is particularly troublesome for people who suffer from COPD or another respiratory illness. Short periods of exposure to the thin air found at high altitudes can cause shortness of breath and a condition known as altitude sickness. Long-term exposure can lead to even more serious and potentially life-threatening complications.
If you live at high altitude or plan to travel to high elevations, it's important to understand how the thin air can affect your condition over time. If you're not accustomed to high altitudes, you need to know what to expect so you can take the proper precautions before traveling to areas where it may be a concern.
In this post we're going to help you do just that by telling you everything you need to know about respiratory diseases and high altitudes. We'll explain how high altitudes affect your respiratory illness, how to prevent negative symptoms, and what kinds of tools and medications can reduce your chances of adverse effects.
How High Altitudes Affect Your Body

High-altitude regions like the mountains host some of the most beautiful landscapes and alluring vacation spots. But the effects of high altitude in these areas can be troublesome, especially if you are living with a chronic respiratory disease.
The air at higher elevations is much thinner than the air at sea level and contains significantly less oxygen. Because of this, your lungs have to work extra hard to absorb enough oxygen to meet your body's needs.
Your lungs compensate for the lack of oxygen at high altitudes by increasing your breathing rate, and your cardiovascular system compensates by increasing your blood pressure and heart rate. This can cause you to feel extra breathless and fatigued.
These changes are often harmless, but for some people high altitudes cause a lot of discomfort. Some people are more sensitive to changes in elevation than others and are more prone to experience a variety of symptoms associated with altitude sickness.
Altitude Sickness

Altitude sickness occurs when your body can't get enough oxygen because of the thin, oxygen-poor air at high elevations. When this happens, your blood oxygen saturation drops and your body kicks into high gear to respond.
Some of the symptoms of altitude sickness are caused by your body's attempt to make up for the lack of oxygen, while other symptoms are a result of hypoxia. Anyone can succumb to altitude sickness, but those with respiratory diseases are especially at risk.
Here are some of the common symptoms of altitude sickness to watch out for:
- Headache
- Light headedness
- Nausea and vomiting
- Shortness of breath
- Decreased appetite
- Difficulty sleeping
- Rapid heart rate
- Rapid breathing
- Reduced endurance and fatigue
There is another type of altitude sickness called high-altitude pulmonary edema, which occurs when fluid builds up in your lungs as a result of traveling to high elevations. This is a very rare condition, but it can be life-threatening if not treated quickly.
Symptoms of pulmonary edema include worsened shortness of breath, a wet cough, frothy sputum, and heart palpitations. If you experience these symptoms after traveling to a high altitude, seek emergency medical attention immediately.
How High Altitudes Affect People with Respiratory Diseases

Scientists who research the effects of elevation on COPD have found that high altitudes tend to make COPD symptoms worse.
High altitudes require you to breathe faster, breathe deeper, and use more energy to breathe. If the air is very oxygen poor, it can be impossible to get enough oxygen and cause your blood oxygen levels to drop, leading to hypoxia.
Thus it should come as no surprise that people with respiratory diseases have to be extra cautious in the thin air at high elevations. After all, traveling to high altitudes causes breathlessness and other respiratory symptoms often in healthy adults, so it stands to reason that people with reduced lung function would struggle even more.
The extra strain that the thin air puts on your lungs makes it harder to breathe and can make symptoms that you already have worse. High altitudes also affect your endurance; you might notice that you feel fatigued and short of breath easily when doing any kind of physical activity at high elevations.
High altitudes are not all bad for your lungs, however. In fact, if you suffer from asthma or allergies, spending time at a high altitude might actually improve some of your symptoms.
That's because there's less less pollen and other allergens in the air at high altitudes. So, while spending time in high altitudes might make your COPD symptoms worse, it might also soothe other symptoms of asthma and allergies if you suffer from them as well.
Factors to Consider Before Traveling to High Altitudes

High altitudes affect every individual differently, but there certain factors that put you more or less at risk of suffering ill effects. If you're planning to travel to a higher elevation, make sure you take the following factors into consideration before you go:
The Severity of Your Disease
If your respiratory disease is mild, you might only notice minimal negative effects at high elevations. But if your disease is severe, you should be prepared for the possibility that you will experience greatly worsened symptoms or exacerbations because of the thin air.
That's why it's important to consult with your doctor before you travel, especially if you are heading to a climate or an elevation that's significantly different from what you are used to. Your doctor will be able to warn you about any potential problems and help you get any medications or treatments you might need before you go.
The Difference in Elevation
How much the altitude affects you depends on what elevation your body is already accustomed to. If you already live at a higher altitude, then traveling to the mountains will be easier than it would be for someone who lives at sea level.
The relative difference in altitude between where you live and where you are traveling matters, and you can calculate it by subtracting your home city's elevation from the elevation of your travel destination. To do this yourself, you can visit elevationmap.net to find the elevation of cities all across the world using their handy search tool.
Living at High Altitudes

If you live at a high elevation, then you have probably already adjusted to the acute effects of the high altitude. Our bodies adapt to handle the thin air fairly quickly, and it usually only takes a couple weeks at most to shake off the negative symptoms.
There are two main changes that happen in your body over time that helps it acclimate to oxygen-poor high altitudes. First, your lungs adapt by enlarging to increase their oxygen absorption abilities, making it easier to breathe. Second, your circulatory system adapts by making extra blood vessels and red blood cells in order to more efficiently transport oxygen to all the different parts of your body.
However, even after your body adapts, the thin air can still negatively affect your respiratory disease in the long term. It makes it more difficult to manage respiratory symptoms like breathlessness and wheezing and can lead to more serious complications over time.
The oxygen-poor air at high elevations force your lungs to work much harder to get enough oxygen than they would have to at sea level. The higher the altitude, the more the effect worsens, which is why most doctors recommend that people with chronic respiratory diseases live at lower altitudes if possible.
If you do choose to live at a high altitude, it's important to get your blood oxygen levels tested regularly and have an effective treatment plan to prevent your blood oxygen saturation from falling too low. If you aren't extra careful to make sure you are getting enough oxygen every day, you could suffer from hypoxia which leads to pulmonary hypertension, heart failure, and death.
Make sure to talk to your doctor if your respiratory symptoms are severe or you are concerned about the long-term effects that living at a high altitude could have on your lungs. Your doctor can help you better understand the risks and help you determine whether or not moving to a lower altitude would be good for your health.
Tips for Managing High Altitudes
It's important to be knowledgeable and prepared before traveling to high altitudes, especially if you have reduced lung function because of a respiratory illness. That means knowing the risks of high elevations and understanding how to minimize those risks as well.
In this next section we'll discuss what you can do to minimize your chances of complications and discomfort when spending time at high altitudes. We'll tell you what you should bring, what you should watch out for, and how you can help your body and lungs adjust to the thinner air.
Take it Slow
Whenever you travel to a high altitude that you're not used to, it's important to give your body time to adjust. Even healthy adults have to take it easy while their bodies acclimate to the thinner air, so you should be doubly cautious if you suffer from a chronic respiratory illness.
First, don't plan anything more than light activity for the first few days you spend at a high elevation. You can expect to have much less physical endurance than you typically have, so don't plan long hikes, aerobic exercise, or any kind of strenuous activity until after you've had time to adjust.
It takes most people at least several days to adjust completely to the high altitude, but it can take up to a week or two for some. The higher the elevation that you're traveling to is compared to the altitude you're accustomed to, the longer it will probably take you to adjust. Make sure you plan accordingly.
Drink Plenty of Water

High altitudes cause you to lose water and get dehydrated more easily. Dehydration is a main contributor to symptoms of altitude sickness, and drinking plenty of water is one of the best ways to prevent it.
That means you'll have to remember to drink extra water when you travel to higher elevations if you don't want to feel breathless and fatigued. If you go on any hikes or excursions, make sure to bring an extra water bottle or two along with you.
Avoid or Limit Alcohol
For many people it's only natural to celebrate with alcohol while traveling or enjoying a well-earned vacation. However, if you're traveling to a high elevation, you should be very cautious about how much you drink.
Alcohol's effects tend to be stronger at high altitudes and can make altitude sickness even worse. You might also find that it takes less alcohol to feel tipsy or that you experience worse dehydration or hangovers when you drink.
It's best to avoid drinking any alcohol until after your body has adjusted to the high elevation. If you do choose to drink, take it slow, and remember that it will take less alcohol than usual for you to feel its effects.
Regardless of elevation, alcohol can still cause your throat to relax at night when you sleep, making it more difficult to breathe. To keep this from happening, take care not to drink alcohol late in the evening or in the three to four hours before you go to sleep.
Tools For Managing High Altitudes
If you suffer from a chronic respiratory disease, you should expect to have extra breathing difficulties when you travel to higher altitudes. It's important to go prepared with all the tools and medications you might need to manage your symptoms in the oxygen-poor air.
Supplemental Oxygen

Low oxygen levels at high elevations make it difficult for people with reduced lung function to breathe in enough oxygen to meet their bodies' needs. You might find that you need to use extra supplemental oxygen when you travel to higher altitudes, even if you haven't needed it before.
If you currently require supplemental oxygen therapy, you'll need to be extra cautious when you travel to a higher altitude. Make sure you have a large enough supply of portable oxygen to last you the whole trip, accounting for the fact that you might need more than you usually do.
It's a good idea to have your doctor do an oxygen evaluation before you travel or move to a higher elevation, even if you don't use supplemental oxygen right now. You doctor can test your lung function to determine whether or not you are likely to need supplemental oxygen or adjust your current oxygen prescription if needed.
Pulse Oximeter

When you travel to higher altitudes, the lack of oxygen in the air can make you more prone to hypoxia, or low blood oxygen saturation. And if you're not used to managing your disease in the thin air, you might not be able to notice or prevent it from happening as easily as you could at home.
That's why you should consider bringing a personal pulse oximeter with you on your trip if you travel to a high elevation. Personal pulse oximeters are small, portable devices that you can use to read your blood oxygen levels in moments, simply by clipping the device to the end of your finger.
You might need to keep track of your pulse oximeter readings for awhile before you understand exactly how they change in relation to different activities and symptoms. You can also talk to your doctor to learn more about how to properly use your pulse oximeter, how to interpret its readings, and to calibrate your pulse oximeter if needed.
Pulse oximeters are very cheap and very useful for a variety of situations. When you travel to high altitudes, you can check it often to make sure you are getting enough oxygen and better understand how the altitude affects your COPD. A pulse oximeter is also a useful tool to use if you use supplemental oxygen therapy, because it lets you know when your blood oxygen drops too low.
All of Your Medication

It is especially important to keep all of your medications and treatment tools with you when you're at a high altitude. That way you'll be prepared if you start to feel chest tightness, shortness of breath, or any other respiratory symptoms.
Make sure to talk to your doctor about any extra medications you might need to help you feel comfortable at a higher elevation, especially if you know that you're sensitive to high altitudes. Even if you usually only need your inhaler occasionally or during heavy activity, you might find that you need to use your medications more often at high elevations, or during periods of lighter activity as well.
Conclusion
It's important to know what you're getting into before you travel to a high altitude if you have COPD. If you aren't prepared, you might find yourself too breathless to participate in any fun activities you have planned.
If you follow the tips on this list, you should be able to minimize the negative effects of high altitude and avoid getting stuck in bed with altitude sickness. If you bring all the tools and medications you need, you'll be prepared to manage any worsened COPD symptoms that you experience.
If you grew up hearing the phrase “an apple a day keeps the doctor away,” then you’ve probably spent your life trying to eat healthy foods. However, “eating healthy” isn’t necessarily just about eating healthy food; it’s about getting the right balance of nutrients that your body needs.
If you eat an apple every morning, that’s great! Apples are perfect for a quick energy boost, they help with weight loss, and they’re a heart healthy snack. But they also lack many of the vitamins and minerals that lead to optimal health.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Another thing many people don’t consider is that nutritional needs are different for everyone. Whereas everyone needs the same nutrients to stay healthy, diets need to be adjusted and adapted to each individual’s needs at any given time.
Although eating right may sound like a simple concept, it can be complicated by things like changing tastes as we age and medical conditions that affect the way food is processed in the body. Chronic obstructive pulmonary disease (COPD) is just one condition that often has this effect on the body.
How COPD Affects Your Appetite and Sense of Taste
You may be wondering, “how can a disease that affects the lungs affect your appetite?” This is a valid question and one that can’t be answered easily. However, a good place to start is by remembering that everything you put in your body affects every aspect of your health in some way or another — whether directly or indirectly.

And when it comes to COPD specifically, your respiratory health is linked to your diet in one key way: metabolism. Metabolism is the process through which your body breaks down the food you eat and converts it into usable energy. Whether you’re at the gym exercising or you’re in bed sleeping, your body is always using energy, and thus your body always needs a source to draw energy from.
In the metabolic process, there are three main components that your body uses: the food and drink that you consume and the oxygen that you breathe. After consuming a food or drink, it goes to your stomach where it is broken down with digestive juices. The contents move to the small intestines which absorb the nutrients and transport them to your bloodstream.
Meanwhile, the air that you breathe passes over the alveoli in your lungs. A red blood cell protein called hemoglobin moves this oxygen into the bloodstream. Once these nutrients and oxygen are in the blood, it begins a process called cellular respiration where the oxygen breaks down glucose and stores energy in the cells. Nitrogenous wastes like CO2 are also released through this process.
Because oxygen is such a crucial component in converting the food you eat into usable energy, a chronic lung condition like COPD can have an immense impact on your appetite, sense of taste, and general eating habits. Although the most common effect of COPD is weight loss, it can also lead to weight gain in some cases.
Weight Loss in COPD Patients
In a country where 70 percent of people are classified as either overweight or obese, it may come as a surprise that some people suffer with the opposite problem — weight loss. However, according to the Lung Institute, an estimated 40 to 70 percent of COPD patients report losing weight unintentionally.
For a COPD patient, just the act of breathing takes significantly more effort than those without the condition. The Cleveland Clinic reports that breathing can burn up to 10 times as many calories for someone with COPD which can become more severe as the disease progresses. And without an increase in caloric intake, this will inevitably lead to weight loss.

Unintentional and rapid weight loss can be a serious problem and lead to symptoms like muscle loss, loss of energy, and an increased risk of injury and illness. You should visit a doctor regularly to ensure that you are maintaining a healthy weight and aren’t losing weight too quickly as a result of your respiratory condition.
Pulmonary Cachexia
Although weight loss is generally perceived as a good thing for most people, not all weight loss is healthy, even in someone who may be considered overweight. Pulmonary cachexia is one side-effect of COPD that can lead to the unhealthy loss of both muscle and fat tissue. In severe cases, cachexia may result in the loss of a significant amount of muscle function.
Although the exact cause of cachexia is not known, studies have shown that intracellular mechanisms like myonuclear and protein turnover may be the primary cause. In other words, even people who eat enough and get all the proper nutrients through their diet may still experience a loss in body mass index (BMI).

According to Physiology.org, cachexia is a common side-effect of COPD with about 20 to 40 percent of COPD patients affected. Although this condition occurs gradually in most people it’s likely accelerated during acute exacerbations, so it’s important to keep up with the treatment plan your doctor has set for you.
Inflammation
Inflammation in the lungs is the primary cause of COPD and potentially one of the leading causes of weight loss in COPD as well. Both emphysema and bronchitis — the two main types of COPD — result in inflammation in the lungs. Bronchitis is an inflammation of the bronchial tubes which bring air to the alveoli. Emphysema on the other hand, is the result of inflammation on the alveoli, usually due to exposure to irritants like cigarette smoke.
Studies have shown that 85 percent of people experience at least one digestive problem with COPD like bloating which can make it difficult to eat. Although there are a number of things that could potentially be causing this, many COPD patients suffer from hyperinflated lungs due to inflammation and too much air getting trapped in the lungs when breathing. This can put stress on the rib cage, diaphragm, and stomach, especially while eating.
Hormonal Changes
The adrenal glands sit on top of the kidneys and are responsible for a number of important roles in the body. First, and most importantly, they produce hormones that are essential for the normal function of your body. This includes things like regulating your body’s reaction to stress, regulation of blood pressure, and metabolism. There are a number of disorders that can result if the production of hormones is out of balance.
According to COPD News Today, inhaled corticosteroids used to treat COPD and asthma may be at fault for an increased risk of adrenal gland suppression. It’s often difficult to diagnose corticosteroid-induced adrenal suppression because the symptoms can vary widely from something as simple as tiredness to something as serious as a life-threatening illness.
Fortunately, only a small number of people have experienced this issue with inhaled corticosteroids and COPD patients should not quit taking them before speaking with their doctor first.
Anxiety
Anxiety can lead to complications when it comes to weight regulation. One of the primary characteristics of stress and anxiety is an increased release of adrenaline and cortisol in the body. This initiates the “fight or flight” response in your body that can increase your metabolism and cause you to lose weight more quickly. What’s more, anxiety can lead to decreased serotonin and dopamine (the feel good hormone) in the brain. This means you’ll likely feel less enjoyment from eating and you may avoid it as a result.

It’s not uncommon for those coping with COPD to experience anxiety. As symptoms of breathlessness, coughing, and fatigue increase, it’s easy to feel trapped and uncomfortable in your own body. They also may feel stress about being reliant on a loved one for daily tasks or stressed about going somewhere that may cause an exacerbation. For more information on managing anxiety with COPD, read our blog titled COPD and Anxiety: How to Find Peace of Mind.
Weight Gain in COPD Patients
Although it’s significantly less common for someone with a chronic respiratory disease to experience weight gain, it is certainly possible and learning how to keep unnecessary weight off is just as important when it comes to preventing serious COPD exacerbations.
One of the serious threats of being overweight with COPD is the increased risk of obstructive sleep apnea (OSA). According to WebMD, more than half of people with OSA are either overweight or obese. Since sleep apnea causes disruptions in breathing at night, it can be a potentially life-threatening condition for someone who is also suffering with COPD.
Inactivity
Possibly the most common cause of weight gain with COPD is inactivity. As COPD progresses, lung function is reduced significantly. Using a spirometry test, pulmonologists are able to determine both your forced expiratory volume (FEV1) and your forced vital capacity (FVC). Below are the levels of lung function you can expect with each stage of COPD.
- Mild COPD (grade 1) - 80 percent or higher FEV1
- Moderate COPD (grade 2) - 50 to 79 percent FEV1
- Severe COPD (grade 3) - 30 to 49 percent FEV1
- Very severe COPD (grade 4) - Under 30 percent FEV1
It goes without saying that as someone progresses through these stages of COPD, their ability to perform physical tasks will diminish. Many people find that they aren’t able to exercise or perform chores around the house like they used to. Fortunately, pulmonary rehabilitation is an effective method for reducing symptoms of COPD and helping people to regulate their weight more easily while coping with the condition.
Lifestyle Changes
Being diagnosed with COPD means making a lot of lifestyle changes that you may not be prepared to make. Although most people eventually adapt and adjust to a new way of life, some people may find it difficult to cope at first.

It’s easy to fall into bad habits like eating unhealthy food or skipping out on breathing exercises or pulmonary rehabilitation classes. However, these are likely all things that your doctor has recommended as part of your treatment plan and you should take care to follow them as best as possible. You might also be on a strict diet regimen that focuses on providing you with nutrients that you need to improve lung function and reduce COPD symptoms. Although it may seem different at first, stick with it until it becomes routine.
Steroids
Steroids are one of the many medications used to treat acute COPD exacerbations and can be either taken orally or inhaled. These steroids help to fight inflammation in the lungs, reduce swelling, and suppress the immune system so that your body doesn’t attack healthy cells.

Unfortunately, these benefits don’t come without side-effects. Many people who take steroids for COPD experience an increased appetite, fluid retention, and a change in where the body stores fat. This added weight usually appears in the neck, abdomen, and face. And generally, the longer you’re on the steroid and the higher the dose, the more likely you are to experience these symptoms.
Fluid Retention
One thing many people don’t consider when it comes to weight gain is that much of it could be caused by increased fluid retention in their body. Fluid retention is when your body stores water instead of using it. This can be caused by a number of things like pain relievers, antidepressants, and other medications, but one of the most common causes of fluid retention is a high sodium diet and lack of exercise.
Loss of Taste Plays a Role in Weight Management
Aside from the risk factors above, loss of taste or taste dysfunctions can make it difficult to regulate weight and follow a strict dietary routine required for COPD treatment. There are a number of potential causes for this, however, most people tend to experience it more with age, after taking medication, and after smoking. And let’s face it, if you’re not enjoying the food that you’re eating, it’s going to be a lot less likely that you are able to continue eating it.
Medication
Prednisolone is a steroid that can be used to regulate inflammation, metabolism, mineral balance, and the immune system. It’s commonly prescribed by doctors to treat COPD symptoms such as chest tightness, chest pain, and breathlessness. However, some patients report experiencing a metallic taste in their mouth after taking it.

Other drugs like inhaled corticosteroids used to treat asthma and COPD can leave a strange taste in your mouth after using them. Although the taste tends to go away after an hour or two, it can certainly have an impact on your diet, especially if you take medication right before eating.
Age
Taste loss is natural as you age. Over time, taste buds will shrink and be less sensitive to food, especially salty, sweet, or bitter flavors. Since COPD is much more common in old age, it’s imperative that you avoid adding salt or sugar to the food that you eat. Sodium causes your body to retain water, leading to weight gain and increasing your chance of experiencing breathlessness and sleep apnea. Sugar, on the other hand, will also lead to weight gain and leave you feeling fatigued.

Before adding anything to your diet, you should speak with your doctor who may be able to recommend seasonings that won’t add any additional side effects. Also, be sure to look up recipes for low-sodium meals.
Dry Mouth
Dry mouth is just what it sounds like — dry mouth due to a lack of saliva production. COPD patients often experience dry mouth when undergoing oxygen therapy because the air that’s processed through their machine is not humidified. Having dry mouth frequently can lead to taste loss and difficulty eating.
Fortunately, there are solutions to this problem. Whether you’re using a CPAP machine for sleeping, a home oxygen concentrator, or a portable oxygen concentrator, you can purchase a humidifier that either attaches to the device or you can use a regular home humidifier.
What You Can Do To Manage Your Weight
Weight management doesn’t just help you feel better, it’s crucial for preventing serious COPD exacerbations. If you’re overweight, you’ll be more likely to develop sleep apnea which can result in more exacerbations. On the other hand, if you’re underweight, you may start losing muscle mass rather than fat which makes it more difficult to breathe.
Routine Doctor Visits
The best way to manage your weight with COPD is to ensure that you always visit your doctor routinely. Unfortunately, visiting your doctor once a year is not enough for him/her to be able to notice what is actually causing the weight loss or weight gain, so you’ll need to see them regularly to make sure you’re on the right track.
As we mentioned earlier, maintaining your weight isn’t just about eating right. Your doctor will need to adjust your diet regularly to ensure you’re getting the right nutrients.
Stay Active
It’s normal for someone with COPD to experience declining physical abilities, but in the grand scheme of things, any form of exercise you can manage will help, no matter how insignificant it may seem.

Pulmonary rehabilitation is a type of exercise routine that’s designed specifically for those coping with a chronic respiratory condition. It teaches COPD patients the best way to exercise, what exercises benefit the lungs the most, as well as breathing exercises that will help you feel less fatigued. Not only will pulmonary rehabilitation help you keep off unnecessary weight but it can help you retain your muscle mass.
Reduce Salt Intake
The average American diet is very high in salt which is known to increase blood pressure and cause weight gain, especially through water retention. Although it’s healthy to have some sodium in your diet, it’s best to get it naturally through your food rather than through added salt. Since your sense of taste tends to decline with age, you should try to avoid adding additional salt to every meal and use other seasonings to add flavor instead.
Oxygen Therapy
One of the most effective and common treatment options for COPD is oxygen therapy. And the good news is that keeping up with your oxygen therapy treatment will also help you manage your weight. Like we mentioned before, taking a breath can burn as much as 10 times as many calories for someone with a chronic respiratory disease. However, when you use an oxygen therapy device you won’t be exerting any extra energy to breathe.
If you are on the go frequently and want an oxygen therapy device to match that lifestyle, portable oxygen concentrators will help you achieve that. Since oxygen concentrators draw ambient air, you won’t need to carry a heavy and bulky oxygen tank around with you.
Ask For Help
After being diagnosed with a condition like COPD, there’s always the question of how much independence you should maintain. Independence can be great for self-esteem and to help you lead a more fulfilling life. However, simultaneously, you should never be afraid to ask for help when you need it.

Chances are, you know what it takes to maintain a healthy weight, but if you don’t have the energy to cook like you used to or maintain a healthy lifestyle, you may find it more difficult to manage your weight. A little help from a friend or a loved one can go a long way towards improving your health and you’ll become closer in your relationship as a result.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Conclusion
Maintaining a healthy weight while coping with COPD isn’t all about your diet. There are a number of complications that COPD patients need to deal with in order to avoid unintentional weight loss or weight gain. While a healthy diet should be the foundation of your COPD treatment plan, you should take into consideration all of the above in order to achieve optimal results.
While it’s great to make changes to your routine in order to improve your health, it’s best to consult a doctor or pulmonary specialist first. What may be beneficial for one person could be detrimental for another and having a clear treatment plan to follow is key to your success.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













