_%20(1).png)
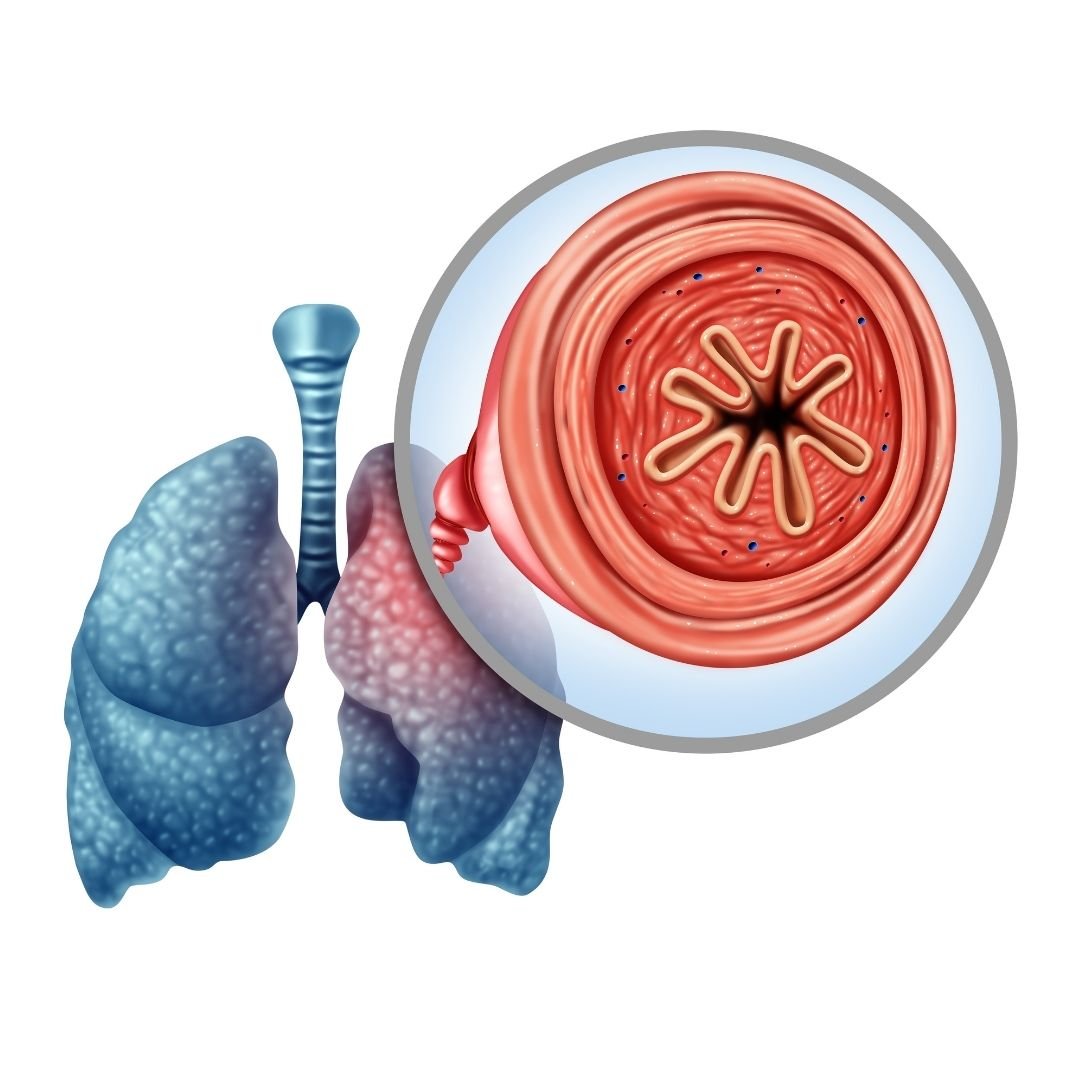
One of the most common questions we hear COPD patients ask is, “how can I clear my airways when they get congested?” As a COPD patient, you’re likely to experience coughing fits that are brought on by the buildup of mucus and sputum in the airways and lungs. And sometimes, no matter how hard you try, you feel like you can’t clear them in order to catch a breath of fresh air. This is far more common than you might expect and it can be a frustrating and sometimes even scary experience.
Another thing that many people don’t realize is that airway clearance can be a lot more complicated than learning how to cough correctly. There are many different techniques that can be applied, and it’s also helpful to know why your airways are becoming congested in the first place. In this post, we’ll help you understand some of these concepts and provide you with a step-by-step guide on how to clear your airways safely.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
As always, it’s imperative that you speak to your doctor if you experience ongoing issues with coughing, wheezing, or shortness of breath. These symptoms tend to get worse over time unless the root cause is dealt with. What’s more, coughing fits can lead to flare-ups and exacerbations which can put you in the hospital.
Why does COPD Make it Difficult to Clear Your Airways?
There are two different types of chronic lung disease: obstructive and restrictive. A restrictive lung disease like pulmonary fibrosis or interstitial lung disease is one that affects the lungs’ ability to expand. An obstructive lung disease like COPD or bronchiectasis, however, prevents you from fully expelling air from the lungs. This is especially problematic when the patient tries to cough because they may not have the force necessary to clear mucus and other substances from the airways.

Another reason that COPD makes it more difficult to clear your airways is that this disease is associated with changes in the way that mucus and sputum are produced in the body. In a healthy individual, mucus plays a vital role in the body’s immune function. The body carefully regulates the mucus lining the airways and lungs so that there is enough to trap bacteria but not so much that you choke or can’t breathe naturally. However, in COPD patients, there is usually an overproduction of mucus due to oversized mucus glands and an overabundance of goblet cells.
If you’re a current smoker, this could be another reason that you’re experiencing issues with airway obstruction. According to the Centers for Disease Control and Prevention (CDC), as many as 38 percent of COPD patients are current smokers. This study published in the Karger medical journal found that moderate and heavy smokers have a higher impairment in mucociliary clearance than their non-smoking counterparts. One of the key ways that smoking affects airway clearance is by damaging and killing cilia. These are tiny hair-like organelles that help to push mucus and other debris out of the airways.
Since there are so many different causes of airway obstruction in COPD, it’s important to have a comprehensive treatment plan to deal with these symptoms. Airway clearance therapy can and should be used, but it won’t be as effective if you aren’t following all other aspects of your treatment plan that your doctor has designed for you. Ideally, if you’re following your treatment plan carefully, you won’t experience mucus buildup as frequently and you’ll only need to use airway clearance techniques in rare circumstances.
What is Airway Clearance Therapy (ACT)
Airway clearance therapy, or sometimes called airway clearance techniques, is a group of scientifically backed methods used for clearing mucus from the airways. These techniques were developed as a more controlled version of our body’s natural airway clearance techniques like coughing and wheezing. A chronic and persistent cough or episodes of wheezing can be extremely unhealthy, especially if they lead to you losing sleep or feeling lightheaded or fatigued. Airway clearance techniques aim to not only make COPD patients more aware of how they’re coughing, but also provide them with some entirely new methods that may be more effective.
-jpg.jpeg)
Generally speaking, airway clearance techniques are divided into seven different categories. Everyone has a slightly different way of practicing these techniques, so don’t be alarmed if your pulmonologist tells you something that differs from what you have read here. Our goal is simply to provide you with an overview so that you can better understand how airway clearance therapy works.
1.) Controlled Coughing
Like we mentioned before, uncontrolled coughing is problematic in COPD patients. Without understanding how your lungs, airways, and mucus work, simply expelling air in an attempt to dislodge any obstruction can be more effort than it’s worth. One of the biggest problems associated with normal coughing or wheezing is that it often causes the airways to collapse, meaning that no matter how hard you cough, the mucus will be stuck. If you hear a wheezing or whistling noise when you cough, this is a sure sign that your airways collapse when you cough. Controlled coughing is focused on keeping the airways open so that you’re not wasting valuable energy and oxygen.

The first rule of controlled coughing is to avoid inhaling sharply through your mouth. This can send mucus back down the airways and be very counterproductive. Instead, inhale slowly but deeply through your nose. This way you have enough oxygen to cough correctly. It’s best to practice controlled coughing while sitting down and you should try to relax as much as possible. Especially try to eliminate the tension in your shoulders and chest because this can contribute to the airways becoming narrow.
Once you’re seated, lean forward slightly and place your hands on your abdomen. You’re going to cough three times and you should really focus on the quality of each one to ensure that the mucus is moving out of your airways rather than back down into your lungs. Be sure to take a deep breath through your nose between each cough to ensure that you move enough air. If you need to take a moment to relax between each cough, this can be helpful.
Another technique that’s similar to controlled coughing is huff coughing. For the most part, you will follow the same steps as you would for controlled coughing. However, instead of coughing, you’re going to be forcing air through your airways similar to how you would fog up a mirror or how you would clean a phone screen or your glasses. In other words, you’re expelling air out your mouth without creating any vibrations in your chest or throat.
2.) Autogenic Drainage (AD)
The aim of autogenic drainage is to move mucus from the smaller airways into the larger airways (peripheral airways into central airways). By doing this, it is much easier to dislodge the mucus because it’s all in one area. The rationale for autogenic drainage is based on a principle of solid mechanics called shear force. This is when unaligned forces are applied to an object causing it to bend in two different directions. In the case of autogenic drainage, the mucus and other secretions in the airways are the object that’s being manipulated. This is done through a series of carefully monitored breathing techniques.
3.) Postural Drainage and Percussion (PDP)
Postural drainage and percussion, also known as chest physical therapy (CPT), is a technique that involves using your hands to assist with airway drainage. While you can do PDP on your own, it’s often recommended that you have someone assist you with it, whether it’s a friend, loved one, or your physical therapist. Like autogenic drainage, PDP is a technique that will take some time to perfect so it helps to be patient as you learn the ins and outs of this method.
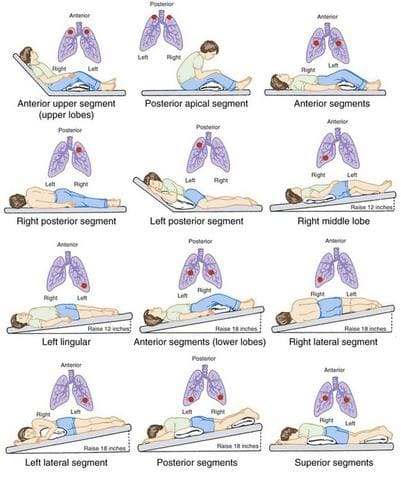
The reason this method is called “postural” drainage is that you are going to use different positions that leverage gravity in order to drain the mucus from your airways. The general rule of thumb is that your hips should be higher than your chest. Whether this means laying on your back, side, or stomach, you can do whatever is most comfortable for you. Many people prefer to use pillows or blankets to elevate their hips.
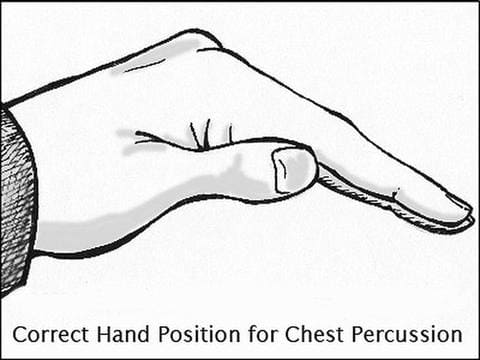
Once you’ve found a comfortable position you can begin the percussion. Most specialists recommend cupping your hand and placing it palm down on your chest. This will allow you to break up the mucus in your chest without hurting yourself. The percussion can also be done on your back but it’s best to have a partner to help you out with this.
4.) Positive Expiratory Pressure (PEP) Therapy
Essentially, the term positive expiratory pressure means experiencing greater resistance when you’re exhaling than when you’re inhaling. This is done with a PEP device which you hold to your mouth and breath into. The device allows you to inhale normally, but when you go to exhale, you experience resistance about four times greater than what you would normally experience. What this does is keeps your airways open as you exhale and allow the force of your air to get behind the mucus and push it out of the airways.

5.) Oscillating Positive Expiratory Pressure
Oscillating positive expiratory pressure therapy is very similar to the method above. However, an oscillating PEP device uses high-frequency oscillations that break up mucus as you exhale. Oscillating PEP devices look similar to traditional PEP devices but they have a ball inside that rattles around as you exhale. This is what creates the vibrations in your upper chest. After blowing into the device several times, you can take a break to clear out any mucus that the device brought up. Then simply repeat the process.
6.) High-Frequency Oscillating Vest
A high-frequency oscillating vest is another tool that can be used for airway clearance. This is an inflatable device that looks a lot like a life vest. The oscillating vest is connected to an air compressor via two hoses. Once it’s turned on, the vest inflates and deflates in rapid succession. The basic principle is that it uses positive and negative pressure changes in the chest to augment peripheral and tracheal mucus movement towards the airway opening. After a set period of time, the device is stopped and the patient can cough to bring up the mucus.

While high-frequency oscillating vests are very effective, they aren’t without disadvantages. These vests can be very expensive to purchase and maintain. What’s more, they’re not very portable in comparison to the PEP devices which we discussed earlier. If you’re someone who travels a lot you might find that high-frequency oscillating vests are more trouble than they’re worth.
7.) Active Cycle of Breathing Technique (ACBT)
The active cycle of breathing technique is an airway clearance method that combines positioning, breathing, and coughing. Since this is the most complex airway clearance technique it’s also the most flexible when it comes to being adapted to fit a variety of patient’s needs. The goals of ACBT include improving the effectiveness of your coughs, improving lung ventilation, and clearing secretions from the lungs. Below are the three different phases of ACBT:

Phase 1 - Breathing Control and Relaxation
The first step in ACBT is to bring your breathing under control and completely relax your body. The majority of the tension in your body will be located in your shoulders, chest, and back, and many people are unaware of how much this can affect the way you breathe. Start by closing your eyes and placing your hands on your stomach. Sit with your back straight and begin to practice pursed lips breathing. This is where you inhale slowly through your nose and exhale fully through pursed lips.
Phase 2 - Thoracic Expansion Exercises
As the title suggests, the aim of phase 2 in the active cycle of breathing technique is to expand the chest. During this step, you will take 3 to 5 deep breaths in through your nose and out through your mouth while keeping your shoulders and chest relaxed. At the peak of each inspiration, you will hold your breath for 2 to 3 seconds. After the allotted time, simply release the air rather than trying to force it out.
Phase 3 - Forced Expiratory Technique (FET)
The forced expiratory technique is another way of saying “huff” cough. Like we described under the “controlled coughing” section, a huff cough is a way of clearing mucus without allowing the airways to collapse. You’re simply pushing air out the lungs but putting more air behind it than you would with a normal breath. You should repeat this after each thoracic expansion that you do.
Other Ways to Prevent Airway Obstruction With COPD
Drink Plenty of Water
Your ability to prevent airway obstruction depends heavily on your level of hydration. Mucus is made up of about 97 percent water. However, slight variations in this can cause it to become extremely thick and difficult to clear from the airways. Since every organ in your body uses water, it’s imperative that you aren’t starving yourself of this vital resource. According to COPD.net, the average COPD patient should drink between 8 and 12 glasses of water every day.

As you work to increase your water intake, it’s also important to reduce your intake of other types of fluid. Milk, and dairy products in general, are known for thickening your mucus so you’re going to want to avoid these as much as possible. Much like salt, sugar has the ability to dehydrate you, so you should avoid sugary sodas, fruit juices, or sweetened tea. If you absolutely have to drink something other than water, try unsweetened hot green tea which will not only thin your mucus but has a number of other health benefits as well.
Maintain a Balanced Diet
Healthy eating is all about getting the right balance of nutrients that your body needs to stay healthy. For COPD patients and people with other respiratory illnesses, this could mean consuming less sodium and salt which contributes to problems like airway obstruction. You should also avoid highly processed foods which can contribute to bloating and thus making it more difficult to breathe. Most COPD patients tend to do better with a diet that is high in protein and healthy fat which is easy to digest and will support healthy lung function.
![]()
Use COPD Medications Effectively
Depending on how severe your COPD is, your doctor has likely prescribed you some medication for coping with your symptoms. One of the most common medications for COPD is called bronchodilators. These medications open up the airways so that you can breathe easier and they can make it easier for you to perform the airway clearance techniques listed above. Ask your doctor about changing up your treatment schedule to assist with airway clearance.

Another medication that can help with airway clearance is a class of drugs called expectorants. These are medications are designed to thin the mucus in your airways making it easier to clear. Expectorants aren’t designed specifically for COPD patients because they’re also used to treat congestion associated with the common cold and the flu. While expectorants are available for over-the-counter purchase, you should be sure to ask your doctor before using them because they may have adverse interactions with the COPD medications you already take.
Pulmonary Rehabilitation
Pulmonary rehabilitation (PR) is an exercise and education program focused on improving lung strength and function. COPD patients should begin pulmonary rehabilitation right after they’re diagnosed so that they learn the best way to take care of their lungs and slow the progression of COPD. Another benefit of PR that many people don’t realize is that it can help with airway clearance. According to a study published in the European Respiratory Journal, exercise improves mucosal clearance in the small airways by releasing moderators that increase fluid secretion and stimulate cilia beat frequency. What’s more, PR increases lung strength and endurance which can help you perform the airway clearance techniques listed above.

Get More Restful Sleep
Getting restful sleep is a problem that many people face for their whole lives. According to the Sleep Association, around 50 to 70 million people suffer from a sleep disorder in the United States. So, as you can imagine, there is a lot of overlap between people suffering from COPD and people suffering from sleep disorders. If you’ve never been diagnosed with a sleep disorder or provided with treatment for your sleep disorder, now is the best time to seek help. Addressing your sleep problems will have undeniable benefits when it comes to helping you manage your COPD. If you’d like to learn more about getting restful sleep with COPD, please read through this article.

Conclusion
Airway clearance therapy is an incredibly important skill for all COPD patients to learn. However, it’s not an all-in-one solution. Drinking enough water, getting enough sleep, eating right, and exercising are all great ways to prevent airway obstruction and prevent the need for alternative therapies. If you’re experiencing frequent coughing or wheezing, we recommend contacting your pulmonologist immediately so that you can address your concerns.
Here at LPT Medical, we specialize in life-saving oxygen equipment which can help you maintain your oxygen levels if you are experiencing a coughing fit or COPD exacerbation. We will help you get the best deal on the market for portable oxygen concentrators like the Caire FreeStyle Comfort or the Inogen One G5. These devices are much lighter and reliable than traditional oxygen delivery devices allowing you to go more places without worrying about whether or not you’re getting enough oxygen. Since the oxygen is administered through a nasal cannula you can still do all of the airway clearance techniques above while you’re receiving oxygen.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
It’s very important to us that you receive the oxygen concentrator that’s right for you. When you reach out to us, you will be connected with a respiratory specialist who will ask you questions about your oxygen use and lifestyle. If cost is a concern for you, we also have a variety of different buying options including new, used, and refurbished concentrators. We also have financing options available if you’d like to pay in easy monthly installments. Reach out to us either by phone or email for more information.
It is normal for COPD symptoms to change throughout the day in response to your environment, your activities, and even your circadian rhythm. However, many people with COPD, and especially those with severe COPD, notice their symptoms tend to get worse in the morning.
COPD symptoms can be frustrating any time of the day, but they can be particularly burdensome to deal with first thing when you get up. They are more than just a nuisance; morning COPD symptoms can disrupt your morning routine and have a major effect on your quality of life.
Unfortunately, many patients struggle to manage their morning symptoms effectively. That's why, in this post, we're going to tell you everything you need to know about morning COPD symptoms and what you can do to keep them under control.
The following sections will explain why COPD symptoms tend to worsen in the morning, what kinds of symptoms are common, and how they can affect your daily activities and your overall quality of life. Then, we'll discuss a variety of different techniques, including medications, non-pharmacological therapies, and simple habit changes that can help you better manage and minimize your morning symptoms.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
The Burden of Morning COPD Symptoms

According to one research survey, a large proportion of people with COPD—about 37 percent—experience worse symptoms in the morning while they're getting ready to start their day. The number was even higher for people with severe COPD, with 46% reporting more severe symptoms during the morning time.
The most common morning symptoms tend to be shortness of breath, persistent coughing, and coughing up phlegm. They tend to begin immediately after waking up, but many patients also report that their symptoms frequently wake them up from sleep.
For many patients, the worst part of morning COPD symptoms is that they make normal activities like showering, dressing, and getting around the house much more difficult to do. They can also make it more difficult to work, to exercise, and to take care of your overall mental and physical health.
Morning symptoms like breathlessness and coughing can also be exhausting to manage, making your chest muscles sore and draining your energy before your day even gets started. They might make you feel sluggish, fatigued, and too sick to go into work or keep up with your usual routine.
These difficulties can be discouraging, and the added stress of anticipating the daily struggle with morning symptoms can be difficult to cope with psychologically. This can trigger significant anxiety and even depressive symptoms that make it difficult to get up, stay active, and face each new day.
Fortunately, morning symptoms are manageable and treatable if you know the proper steps to take. By working with your doctor and examining your daily habits, you can adjust your lifestyle and treatment plan in ways that help keep your morning symptoms in check.
What Causes Morning COPD symptoms

Unfortunately, the research on morning COPD symptoms is limited, and experts aren't exactly sure why COPD tends to get worse in the morning hours specifically. However, there are several studies that highlight this issue and offer some helpful insight into potential causes and solutions.
For example, experts have pinpointed a variety of factors that could trigger more severe COPD symptoms in the morning and early in the day. These include things like smoking, the effects of poor diet and sleep, and the physical exertion required by many morning activities.
Here's a list of some culprits that are likely responsible for triggering morning COPD symptoms:
- Smoking
- Not adhering to your treatment plan
- Nighttime breathing patterns and sleep posture
- Timing of medications like bronchodilators and supplemental oxygen
- Activities like showering and getting ready for the day
For example, it's common to do activities in the morning that require you to walk and be on your feet, such as showering, getting dressed, cleaning house, and working in the garden. In fact, lots of people tend to be more active in the morning than they are during most other parts of the day.
This extra exertion can trigger breathlessness, coughing, and fatigue in people with chronic lung diseases, especially those who suffer from severe COPD. Certain morning activities may also expose you to respiratory irritants, like pollen (from going outdoors), excess humidity (from the shower), and volatile organic compounds (from body, beauty, and cleaning products).
What You Can Do to Manage and Minimize Your Morning COPD Symptoms
Use Proper Coughing & Mucus Clearance Techniques

A very common symptom of COPD is excess mucus in the airways, which often causes a chronic cough. This kind of cough is triggered by the need to bring mucus up and out of your lungs, which helps clear out your airways so you can breathe.
The phlegm that you cough up is known as sputum, which consists of mucus from your lungs and airways mixed with saliva from your mouth. A large percentage of people with COPD experience a chronic cough with sputum that tends to be the worst in the morning.
Luckily, there are several different exercises, known as mucus clearance techniques (or airway clearance techniques), that you can use to reduce the amount of mucus that builds up in your airways. These include techniques you can do on your own like controlled coughing, methods that require another person to help (e.g. chest percussion), and techniques that require special tools (e.g. lung flute)
Here's a list of some of the most common and effective mucus clearance techniques for COPD:
- Huff coughing
- Deep coughing
- Postural drainage
- Chest percussion
- Using a lung flute (a special medical instrument that produces vibrations to loosen mucus)
- Using a high frequency chest wall oscillation (a special vest that vibrates your chest)
The purpose of all of these techniques is to loosen up the mucus sticking to walls of your lungs and airways so you can get it out by coughing. This helps clear some of the obstruction from your airways, making it easier to breathe and reducing your need to cough as you go about your day.

You might find that mucus clearance techniques help your morning cough most when you use them right before bed or shortly after getting up in the morning. Either way you decide to do it, mucus clearance techniques are an important part of COPD treatment that can reduce your risk for lung infections and exacerbations in addition to treating your chronic cough.
To learn more about the different types of mucus clearance techniques and how to do them, check out this comprehensive guide. It includes step-by-step guides for a several different techniques, as well as a variety of other tips and tricks for reducing mucus in your airways.
Practice Breathing Techniques in the Morning

If you tend to suffer from shortness of breath early in the day, then practicing breathing exercises in the morning might be able to help. There are several different kinds of breathing techniques you can use, all of them simple and easy to do.
Pursed-lips breathing, for instance, is a technique that allows you to breathe better and more easily push all the air out your lungs when you exhale. This is especially helpful for getting rid of trapped air in the lungs, which worsens shortness of breath and is especially common in people with emphysema.
Another breathing technique is diaphragmatic breathing, a technique that encourages you to use your diaphragm, instead of your chest muscles, to breathe. This reduces strain on your chest and breathing muscles, making it easier and more comfortable to breathe.
Studies show that breathing techniques can reduce shortness of breath both during exercise and at rest. They can also help you learn how to control your breathing better in situations that tend to make you feel short of breath.
The great thing about breathing techniques is that they are so simple to remember and you can do them anytime and anywhere you need. You can even start practicing breathing exercises before getting out of bed!
By paying more attention to your breathing and putting exercises you've learned to use, you can prevent or reduce the amount of breathlessness you experience as you go about morning activities that tend to trigger shortness of breath. Pursed-lips breathing, for instance, can help you keep your breathing steady and under control when you shower, get dressed, and do other tasks around the house.
If you want to learn how to perform these and other breathing techniques, check out our guide to COPD breathing exercises here. This article includes several step-by-step guides to help you practice breathing exercises at home as well as a variety of practical tips for how to use these techniques more effectively.
Talk to Your Doctor about Adjusting Your Medication

If you notice that your COPD symptoms tend to get worse in the morning, it's important to tell your doctor. The more your doctor knows about your symptoms and when they they flare up, the better he can tailor your treatment to manage your symptoms throughout the day.
For example, your doctor might suggest that you use a quick-acting bronchodilator medication first thing in the morning after you get up. He might also have you try a new medication (e.g. a twice-daily maintenance inhaler instead of a once-a-day medication) or instruct you to take your medications at a different time of day so that they are more effective in the morning.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Your doctor can also prescribe new medications or adjust your medication dosage so your symptoms are better controlled. He can also tell you whether or not you could benefit from over-the-counter medications to target specific morning symptoms; over-the-counter expectorants, for instance, loosens up mucus to facilitate airway clearance and potentially reduce a morning cough.
Of course, you should never change your medication dosage or schedule without your doctor's explicit permission. You should always follow your treatment plan exactly as written, and all adjustments must be approved and supervised by your doctor.
However, before you even consider talking to your doctor about changing your treatment plan, you first need to make sure that you're currently taking your medications as prescribed. If you aren't following your COPD treatment plan and using your medications exactly as instructed, then that's the first thing you need to change.
Unfortunately, studies show that a large number of people with COPD don't take their medications consistently or correctly, and this is a major cause of morning COPD symptoms. Other studies show that more than two-thirds of people with COPD do not use their inhalers correctly.

This is extremely important, because taking your medication exactly as directed and carefully following the instructions for your inhaler is necessary to keep your COPD symptoms under control. Poor inhaler technique alone can have a huge impact on your health by preventing you from getting a full dose of medication.
Because of this, you should regularly review your COPD action plan and your medication instructions until you're positive you fully understand your own treatment. Also, you should never hesitate to ask your doctor to explain anything related to your health and your treatment, including how to use your inhaler and how to follow your COPD action plan.
Get Better Sleep

How well you sleep during the night can have a major impact on how well you feel in the morning when you get up. It can also have a major impact on your COPD symptoms and your overall health.
Unfortunately, about forty percent of people with COPD struggle to get good-quality sleep during the night. This can be caused by a variety of factors, including worsened nighttime symptoms, sleep disorders, and normal biological changes that happen in your body while you sleep.
For instance, your respiration rate declines when you fall asleep, causing you to breathe more slowly and shallowly than you do when you're awake. This can worsen COPD symptoms like shortness of breath at night, making it more difficult to fall and stay asleep.
Some COPD patients also experience nighttime oxygen desaturation, or hypoxemia, which happens when your lungs are unable to absorb an adequate amount of oxygen to meet your body's needs. This can cause you to wake frequently during the night and lead to a variety of other symptoms, including morning fatigue and cognitive impairment.
Research shows that poor nighttime sleep quality is linked to a variety of morning symptoms that many people with COPD experience on a regular basis. This includes symptoms like breathlessness, more frequent exacerbations, and more difficulty getting out of bed in the morning.
Poor sleep alone can also cause mild cognitive impairment, which is a common in people with COPD. This causes problems like memory loss and concentration difficulties that can affect your morning routine; for instance, it could make it more difficult to remember things like taking your medications or other important tasks you need to finish to get ready for the day.
So, now that you understand how sleep quality can impact your morning symptoms, what can you do in order to actually get better sleep? Unfortunately, the answer isn't always simple, and you may need to work with your doctor or a sleep specialist in order to find solutions that work for you.
For example, if you experience nighttime oxygen desaturation, your doctor might prescribe supplemental oxygen for you to use specifically at night while you sleep. This will help keep your blood oxygen levels up at night, which can reduce fatigue, cognitive impairment, and other symptoms of oxygen deprivation that you experience in the morning.
Sleep posture is also important, as some sleeping positions make it easier or more difficult to breathe. Most experts suggest that people with COPD sleep on their side for better breathing, since sleeping on your back or stomach can put extra weight and pressure on your chest.
There are also a variety of practical changes you can make to your bedroom and bedtime routine that make it easier to sleep comfortably and get quality rest at night. A good place to start is establishing a consistent nighttime routine, which is a simple yet proven method for improving your sleep.
You should also try to create a bedroom environment that is quiet, relaxing, and free from stressors and distractions. It helps to treat your bed like a sacred place meant only for sleep and sex, and avoid using electronics or doing anything else besides resting when you are in your bed.
If you wake frequently during the night or feel tired in the morning despite getting adequate sleep, you might also need to get tested for a sleep disorder like obstructive sleep apnea. Sleep apnea is a very common disorder that affects a large number of people with COPD, and getting diagnosed and treated for it can drastically improve your sleep.
Treat Yourself to Proper Nutrition

If you find it difficult to muster up the energy in the morning that you need to face the day, then improving your diet might help. Unfortunately, many people with COPD struggle with activities like shopping, cooking, and even eating because they make it more difficult to breathe.
However, these activities are all necessary parts of eating a healthy diet, which is particularly vital for people with COPD. Eating whole, nutritious foods ensures that your body has the energy it needs to stay active, and that your lungs have the fuel they need to function efficiently.
While it may not have a direct effect on morning COPD symptoms like breathlessness and coughing, a healthy diet can boost your energy levels and make it easier to manage your morning routine. When your body is properly nourished, you may find it easier to get out of bed in the morning and stay active throughout the day.
A nutritious diet can also help combat fatigue, a common COPD symptom that can reduce your ability to work, exercise, and function well in the morning. It can also help prevent lung infections and a variety of other COPD- and age-related health conditions like heart disease and osteoporosis.
If you have trouble eating enough nutritious foods or need help understanding what a healthy diet looks like, you can always ask your doctor or a dietitian for help. They can help point you in the right direction and even help you put together a personalized nutrition plan.
We've also created a number of healthy diet and nutrition guides specifically for people with COPD. You can use these resources to learn more about what a COPD-healthy diet looks like, how to recognize healthy versus unhealthy foods, and even how different foods can affect your COPD symptoms.
These guides also include a plethora of practical tips that can help you smoothly integrate healthier diet and eating habits into your daily life. They will show you how to make shopping for, cooking with, and eating nutritious foods more manageable, even if you suffer from severe COPD.
Check out the following guides for more information:
- Healthy foods you should eat if you have COPD
- Unhealthy foods you should avoid if you have COPD
- Tips for simplifying and streamlining your shopping, cooking, and meal planning
- How a carb-heavy diet can make it harder to breathe
Streamline Your Morning Routine

Nearly three-quarters of people with severe COPD experience morning symptoms that are bad enough to interfere with their morning routines. If you are one of those people, try not to get discouraged; there are a variety of things you can do to streamline your morning routine and make it easier to manage.
You can start by looking for ways to reduce the amount of physical activity you have to do in the morning. If you can minimize the amount of walking, reaching, and bending you have to do, you can reduce the amount of breathlessness you experience as you go about your morning routine.
For example, you can intentionally organize your home in such a way that the items you use every morning are in the most logical, convenient, and easy-to-reach places. This includes things like clothing, towels, toiletries, and cooking supplies that you need to access every day.
Showers are another major source of breathlessness and fatigue in the mornings; this is due to both the physical exertion required to shower and the humidity it releases into the air. However, you can reduce your symptoms both during and after showering by using shower aids (like shower chairs and handles) and by taking care to vent humidity from the bathroom via a window or vent.
You might also be able to reduce the strain that morning activities put on your lungs by reducing your total morning workload. For example, you could move some of the tasks you normally do in the morning to a different time of day when your symptoms are likely to be less severe, or you could ask friends or family members to help you with the most exhausting tasks.
Which methods work for you will depend on your home's layout, your individual lifestyle, and the severity of your disease. Whatever you choose, it's important when you have COPD to make adjustments to your daily habits and routines as needed so that you can live and work as comfortably as possible.
Eliminate Respiratory Irritants from Your Morning Routine


In this blog, we are going to go over everything you need to know about traveling by airplane with oxygen equipment. Now that travel restrictions and COVID-19 precautious are not as strict as they were before, we want give oxygen patients the tools to travel safely with oxygen and with COVID-19 still being a huge safety concern in our everyday lives.
If you are a respiratory patient, this doesn't mean you do not have the ability to explore or visit destinations around the world, and if you need your oxygen therapy all day everyday, this does not mean you have to be stuck at home or in your hometown for the rest of your life. That being said, traveling during a global pandemic is not something that should be taken lightly!
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In today’s world, there is modern technology that allows oxygen patients to fly with their oxygen equipment with zero safety hazard, before portable oxygen concentrators were developed, this was not possible. Of course, in today's day and age, there are also safety hazards when it comes to the spread of Coronavirus and everyone should be aware of these risks while traveling and do their best to mitigate the risk of transmitting COVID-19.
Oxygen Equipment and Airline Regulations

First of all, the Air Carrier Access Act does not require airlines to provide medical oxygen to any eligible respiratory patients during flights, so do not expect to be given oxygen on your flight. Very rarely will airlines provide supplemental medical oxygen on flights for their passengers, and if they do this oxygen service typically costs a fee.
Also liquid oxygen and oxygen gas tanks are considered hazardous material, and these devices are not allowed on aircrafts.
Just because liquid and gas oxygen tanks are not safe to fly with doesn't mean oxygen patients are out of luck. U.S. airlines allow passengers to bring their own portable oxygen concentrators (POCs) onto airplanes.

In the next section we will go over the requirements for POCs and elaborate on what air carriers will require from passengers who need supplemental medical oxygen during their flights.
Approved Portable Oxygen Concentrators for Air Travel
The Federal Aviation Administration (FAA) requires POC manufacturers, such as Inogen, ResMed, Philips Respironics, to label their new models of POCs, and these labels explain the devices compliance with FAA requirements. If you have a newer POC that is FAA approved, its label will read: “The manufacturer of this portable oxygen concentrator has determined this device conforms to all applicable FAA requirements for portable oxygen concentrator carriage and use on board aircraft.”

Oftentimes airline personnel can check for this label to see whether or not the POC is approved to be used on the aircraft. With older models that do not have labels, airline personnel can look these devices up to check out its FAA approval status.
There are some POCs that are older and do not have a label, and it can still be used on the plane if it is FAA approved. In these cases, airlines can use the list published in Special Federal Aviation Regulation (SFAR) to determine whether or not the POC may be used during a flight.
Here are the POC models that do not have an FAA label but they are FAA approved for in flight-use:

- AirSep Focus
- AirSep FreeStyle
- AirSep FreeStyle 5
- AirSep LifeStyle
- Delphi RS-00400
- DeVilbiss Healthcare iGo
- Inogen One
- Inogen One G2
- Inogen One G3
- Inova Labs LifeChoice
- Inova Labs LifeChoice Activox
- International Biophysics LifeChoiceInvacare Solo2
- Invacare XPO2
- Oxlife Independence Oxygen Concentrator
- Oxus RS-00400
- Precision Medical EasyPulse
- Respironics EverGo
- Respironics SimplyGo
- SeQual Eclipse
- SeQual eQuinox Oxygen System (model 4000)
- SeQual Oxywell Oxygen System (model 4000)
- SeQual SAROS
- VBox Trooper Oxygen Concentrator
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
There are newer devices like the Inogen One G4 and Inogen One G5 for example, that will have the label stating they are FAA approve for inflight use.
On Board with your Inogen Portable Oxygen Concentrator

There are some things you need to know and tasks you must accomplish before you travel with a POC. First of all, be aware that the FAA and the airline you are flying on may have different requirements and you must follow both the FAA and the airline’s regulations.
- The FAA regulations do not require that you tell your air carrier about your POC in advance, however almost every airline will have you notify them that you will be flying with oxygen at least 48 hours before your flight.
- If you are flying on Southwest and JetBlue, these airlines also also ask you to check in for your flight at least one hour before takeoff if you are traveling with oxygen.
- There are some instances when your airline will require a physician's statement
- There are some airlines that will require you to demonstrate how you respond to your POC's alarms before you board the aircraft.
Despite what airline you are flying, check the procedures before your trip. You can find updated rules for oxygen equipment on their website.
Charging your Portable Oxygen Concentrator

Even though some aircrafts have electrical outlets, sometimes they will not let you plug your POC into the airplane's electrical system to charge it during the flight. Therefore, you will need to bring an extra battery to power your POC if your flight is longer than your battery will last.
You should try to practice arriving at your gate early, and charging your device while you are waiting in the terminal for your flight to take off, that way you are beginning the flight with full battery power.
You should also bring an extra battery for traveling because you also have to have enough battery power for the taxi time before taking off, takeoff, in-air time, and landing, and baggage claim. Once you are in your rental car or picked up from the airport, you can plug in your device into the cigarette lighter with the DC charging cable.
Depending on your airline, they will require some kind of reassurance that you have enough battery power, for example, some airlines will check to make sure you have enough battery to power your POC for flight time plus three hours.
You can buy extra batteries for your portable oxygen concentrator on LPTMedical.com or call 1(800)-946-1201.
Because both your POC and extra batteries will be considered medical devices they will not count as your carry-on baggage, but they will be screened by TSA personnel.
Renting Portable Oxygen Concentrators
LPT Medical allows you to rent FAA-approved portable oxygen concentrators.
Flying Internationally with Oxygen

If you are flying internationally with your oxygen device, reach out to your airline and let them know that you will need to bring your portable oxygen concentrators with you on board. They will inform you of any other regulations in place based on the country you are flying to.
Traveling During the COVID-19 Pandemic
As of April 2021, the CDC recommends to delay traveling at this time even if you are vaccinated, and suggests that travel increases your chance of spreading and getting COVID-19.
If you are traveling there are recommendations you should follow in order to keep yourself and others around you safe.
If you must travel, take these steps to protect yourself and others:
- If you are eligible, get fully vaccinated for COVID-19
- Before you travel, get tested with a viral test 1-3 days before your trip
- Wear a mask over your nose and mouth when in public
- Avoid crowds and stay at least 6 feet from anyone who did not travel with you
- Get tested 3-5 days after your trip and stay home and self-quarantine for a full 7 days after travel, even if your test is negative. If you don’t get tested, stay home and self-quarantine for 10 days after travel
- Follow all state and local recommendations or requirements after travel

Be aware that any air passengers coming into the United States, including U.S. citizens, are required to have a negative COVID-19 test result or documentation of recovery from COVID-19 before they board a flight to the United States. Other countries have other restrictions.
For respiratory patients, COVID-19 is a very real threat to their longterm health wellbeing and even their lives. Mitigating the spread of COVID-19 and reducing the chances of transmission can help save lives, and therefore avoiding travel or traveling very safely it crucial.
Overview

With the current state of the global pandemic, travel should not be high on anyone’s list of priorities. And while travel plans may be delayed until further notice, as an oxygen patient you should feel confident and comfortable traveling with your trusted portable oxygen concentrator and extra batteries.
When it does come time to book your flight, notify your air carrier as soon as possible to they can note that you intend to bring a POC with you.
Fulfill any requirement that airlines ask of you in advance, this way if you need a physician’s statement, you can ask them to write that for you prior to your departure. There are airlines with relatively restrictive rules regarding oxygen on board, so be sure to ask a lot of questions when you are speaking with the airline representative so you get all of the information you need to travel with less hassle.

Lastly, be sure to double check the length of your flight with the airline and then factor in any delays that would impact the battery life of your POC
Pretty much, all you have to do is plan in advance, so that traveling with your POC is a smooth process and less stressful.
Nowadays, we rely on our devices for just about everything. Cellphones, for example, are used for everything from making calls and sending text messages to tracking our fitness progress or staying connected with online communities. If you’ve been diagnosed with COPD or another chronic respiratory ailment, this reliance on technology doesn’t go away. In some cases, you might even be more dependent on technology than previously. This isn’t necessarily a bad thing though as long as you’re using devices that are reliable and match your lifestyle.
In this post, we’re going to take a look at seven of the most important devices you can own with chronic obstructive pulmonary disease (COPD). Whether you’ve just been diagnosed or you’ve been living with COPD for some time, these devices are considered to be essential by many or at the very least, incredibly convenient to have. If you have any questions, be sure to leave them in the comment section below, and don’t forget to bookmark our blog page so that you never miss our latest articles.
Portable Oxygen Concentrator
At one point or another, most COPD patients will need to use supplemental oxygen. When the lungs are impaired due to chronic inflammation, supplemental oxygen ensures that the oxygen levels in your blood are normal; and in turn, every organ in your body receives the oxygen it needs to function properly. Supplemental oxygen not only improves your longevity as a COPD patient, but it can also help you feel better in the moment. Oxygen therapy will reduce breathlessness, fatigue, and lightheadedness associated with low oxygen levels.

However, many people falter when it comes to actually choosing the oxygen device that they will use. Patients and healthcare providers often default to oxygen tanks or liquid oxygen tanks because they are cheap and thus have a low barrier of entry. However, when it comes to the patient’s long-term health and well-being, they often find that these oxygen devices are lacking in many ways. First and foremost, they have to be refilled once the oxygen in them is depleted. This can be costly and takes your time and attention away from more important things like spending time with friends and family.

Another problem with oxygen tanks is that they are heavy and bulky. Chances are, you’ve seen people walking around while lugging around a big green tank behind them. The reason these tanks are so big is that they contain compressed oxygen gas which takes up a lot of space. This problem is somewhat mitigated by using a tank that stores oxygen in its liquid form but this still has a lot of problems associated with it. In most cases, the best alternative is to use something called a portable oxygen concentrator.
Unlike oxygen tanks which limit your freedom and mobility, portable oxygen concentrators are designed for people who are on the go frequently and need something reliable. Rather than storing oxygen within the unit, POCs draw in ambient air and remove unnecessary gases, then put out medical-grade oxygen. POCs are electronic devices that run off of powerful lithium-ion batteries. In other words, you simply need access to either a wall or car outlet to charge the batteries, then you will be set for the rest of the day!
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Nebulizer
Another important device to own as a COPD patient is a nebulizer. What a nebulizer does is crush up your COPD medication into a fine mist called aerosol so that it can be inhaled more easily by the patient. This helps the medication reach your lungs faster and thus is faster-acting than medication that is taken orally. You should be sure to speak with your doctor to see if nebulizers are right for you.

Many people think of nebulizers as devices that they can only use at home, however, there’s been a sudden emergence of portable nebulizers that you can take with you if you go on a trip. Nebulizers differ from inhalers in that they put out a constant stream of aerosol whereas inhalers put out “puffs.” This is beneficial for people with severe COPD who may not be able to inhale deeply or sharply enough to bring the medication into their lungs. With a nebulizer, however, you can simply breathe naturally and be sure that the medication is reaching your lungs.

Much like portable oxygen concentrators, nebulizers are usually electronic devices that either run off of a battery or they need to be plugged into an electrical outlet. It should be noted that not all medications can be administered through a nebulizer. Most likely, your doctor will only have you use medication known as bronchodilators which open up your airways in the event of a COPD exacerbation. Bronchodilators include Pulmicort, Xopenex, albuterol, and more.
Pulse Oximeter
A pulse oximeter is a device that measures the level of oxygen saturation in your blood. Pulse oximeters are very small and lightweight and they’re the least invasive way to check whether you’re getting enough oxygen or not. One of the only other alternatives is arterial blood gas (ABG) analysis which requires your doctor to draw blood in order to determine your oxygen saturation level. While these readings are oftentimes more accurate than pulse oximetry they require you to be at the doctor’s office in order to get your results. Pulse oximeters can be used anywhere and anytime.
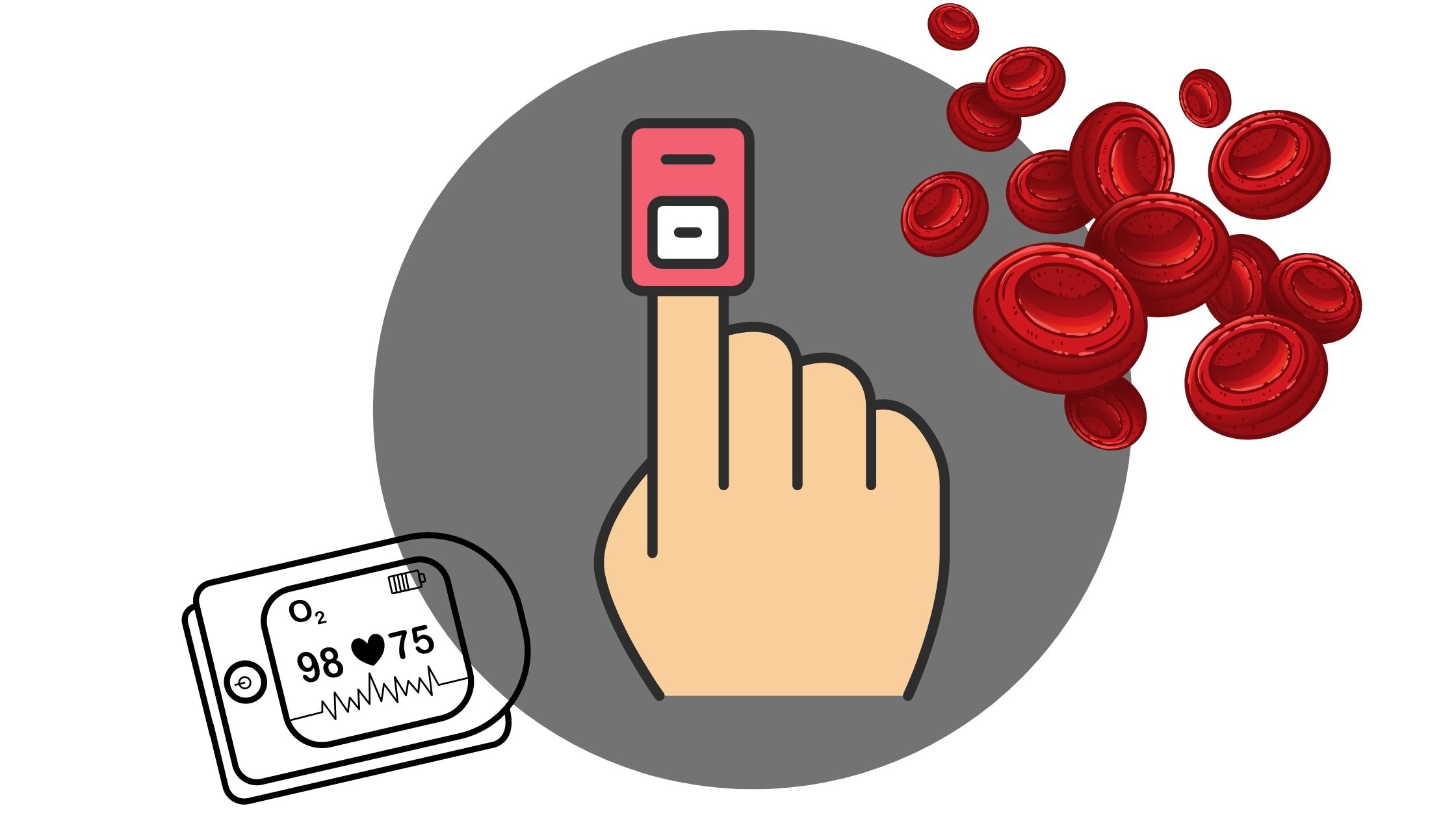
Pulse oximeters work by passing light through the finger and measuring the amount of light that comes out the other side. This determines the amount of oxygenated and deoxygenated blood cells and thus your blood oxygen saturation. Many people are surprised to find that these devices cost under $20. However, if you want a more advanced one that connects to your cellphone or smart device, it could run you over $100. Either way, this is something that all COPD patients should have so that they can ensure that they’re receiving enough oxygen. It can also help you determine whether your oxygen device is working properly.
High-Frequency Chest Wall Oscillation Vest
Mucus plays a very important role in the body. It coats the lining of your lungs and airways and if you inhale irritants or bacteria, the mucus traps it so that it can be cleared before it leads to an infection. Unfortunately, many COPD patients aren’t able to create an expiratory force great enough to clear mucus, and as a result, it becomes lodged in the airways. Years of smoking can also damage the cilia in the airways which are small cells that help pass the mucus out of the lungs. Most COPD patients are taught about airway clearance techniques but these can become very exhausting to do on a daily basis.

Alternatively, COPD patients can invest in something called a high-frequency chest wall oscillation vest. This looks just like a life jacket but it attaches to a machine that vibrates the vest at a high frequency. This causes the mucus in your chest to loosen, and after a few minutes, you can remove the vest and try a huff cough to expel the mucus. The main downside to these vests is that they can run you a pretty penny so it’s best to speak with your doctor before investing in one. What’s more, they aren’t very portable so you should plan to buy one for in-home use only.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Positive Expiratory Pressure Device
A positive expiratory pressure (PEP) device has a similar function to that of a high-frequency chest wall oscillation vest which we discussed above. However, the PEP device is much smaller and lighter so you can carry it in your purse, handbag, or pocket when you leave the house. With the PEP device, you will blow into a mouthpiece that creates air resistance. This air resistance will keep your airways open as you exhale meaning the mucus can move more freely without obstruction.

If you’ve ever tried the technique called pursed-lip breathing, you know what to expect with a PEP device. During pursed-lip breathing, you inhale deeply through your nose and then out through pursed lips. This helps to reduce chest tightness and get more air into your lungs. The PEP device makes this a little easier because you don’t have to control the amount of resistance so you can focus more on your breathing. PEP devices are also fairly cheap at around $30 to $50 apiece.
Mobility Devices
Words cannot express how important it is to maintain your mobility as you get older. Unfortunately, someone with COPD will likely begin to lose their mobility sooner than most due to reduced lung capacity, however, the good news is that there are plenty of mobility aids to keep you on your feet and moving. Probably one of the more popular mobility devices for people with respiratory ailments is a rollator. This is like a walker but it has wheels on the bottom and brakes so that you have better control. In the middle, there is a small platform where you can put your oxygen device your sit on if you get fatigued.

Another mobility aid that many COPD patients use is an electric scooter. These are best for people with very advanced lung disease who may not be able to walk more than a short distance on their own. Electric scooters offer a lot of storage room for your portable oxygen concentrator as well as personal belongings. However, the downside is that they need to be recharged after a certain amount of use and they are difficult to transport from place to place. Unless you have a caretaker who can help you out with these things, an electric scooter may not be the best option for you.

Last but certainly not least, there are in-home mobility devices like stairlifts. A stairlift is essentially an elevator designed for people who have trouble walking up and down the stairs. While these devices are very safe to use and can save you a lot of hassle, they are also pretty expensive because a professional will need to come to your home to install them. What’s more, they can wear out over time so you may need to call someone to have it repaired or replaced at some point.
Smartphone or Tablet
Most people have some type of smart device but for the few who do not, it’s worth upgrading, especially if you have COPD or another respiratory condition. Many portable oxygen concentrators like the Inogen One G5 and Caire FreeStyle Comfort make use of smartphone applications to enhance the user’s experience. These apps allow you to do things like track your oxygen usage, check the device user manual and even remotely check your oxygen flow and battery life.

There are many other applications that can make your life easier with COPD. For example, AirNow.gov has a mobile application that allows you to quickly and easily check the air quality in your area which is useful for planning trips. There are apps that can help you plan your diet and exercise routine with COPD as well. Be sure to check out this post where we take a look at some of the best mobile applications for COPD patients.
Conclusion
Being diagnosed with COPD can be life-changing. You’ll need to take steps to slow the progression of your disease like improving your diet, exercise routine, and taking regular trips to the doctor’s office. While this may seem overwhelming at first, it’s helpful to know that there are many resources at your disposal. Not least of which are devices like portable oxygen concentrators, nebulizers, and pulse oximeters. If you have any questions about what you read here, please don’t hesitate to leave a comment. If you’re on the market for a portable oxygen concentrator be sure to reach out to our respiratory specialists by phone or email.
.png)
With the advent of the novel coronavirus earlier this year, most people in the country have undergone drastic lifestyle changes in order to prevent putting themselves and others at risk. And while many businesses are beginning to open back up and we’re seeing things go back to normal, policies like “social distancing” and “safer at home” are likely to continue for quite some time.
Although these policies are intended to keep people safe, sometimes they can have the opposite effect. Spending too much time at home and away from people has well-documented adverse side-effects and some people are combating this by spending more time than normal outside exercising — this wouldn’t be a problem if it weren’t for the heatwave that’s currently spreading across much of the country.
Under normal circumstances, people could go to public areas like theaters or restaurants to seek relief from the heat, but instead, they’re being forced to choose between being cooped up in a non-air conditioned home or being outside under the hot sun. This issue is amplified for people with COPD and other chronic respiratory illnesses because the heat can lead to many different complications.
In order to help you prepare for the hot summer ahead, we’re going to give you 7 helpful tips for preventing heat-related COPD complications. If you still have concerns about coping with the change of weather, be sure to contact your doctor immediately to see if he/she has any additional recommendations for you. Remember that any changes to your treatment plan should first be approved by your doctor.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
How Heat Affects COPD
Your body works around the clock to maintain a normal temperature. The ideal temperature for most people is between 97°F (36.1°C) and 99°F (37.2°C), but it may vary slightly depending on the person’s age and gender. If someone’s body temperature goes above this threshold, it’s usually a sign of an infection, illness, or heatstroke.

When someone is exposed to high temperatures for prolonged periods of time, it can result in something called a heat injury. This may result in symptoms such as confusion, disorientation, and cramps. If the heat is sustained for long enough, it could result in serious health complications like heat exhaustion, heatstroke, or heat edema (swelling of the hands and feet due to water retention).
One heat-related illness that’s of particular concern to people with COPD is heat tetany. This refers to a short period of stress characterized by hyperventilation (breathing very heavily and quickly), respiratory problems, and muscle spasms as a result of heat exposure. This can even cause something called bronchospasm which is a sudden constriction of the muscles in the walls of the bronchioles in the lungs.

Another way the heat can affect your COPD is through high humidity which often accompanies it. If you’ve traveled to or live in the south, you’re probably well-acquainted with the feeling of being in a hot and humid climate, but the truth is, humidity can be found anywhere depending on the time of year. Humidity has some beneficial effects on the body, but due to its density, it can increase airway resistance and even make it harder for your body to stay cool making it a nightmare for anyone with COPD.
How to Prevent Heat-Related COPD Complications
Stay Hydrated
Proper hydration is one of the most important things you can do for your health and it’s especially important for COPD patients who live in a hot environment. COPD is characterized by excess mucus production which often becomes thick, sticky, and difficult to clear. If you’re dehydrated, it can make it even harder to remove this problematic mucus from the lungs and airways.

Another reason to stay hydrated is because water is the most important substance involved in maintaining our body temperature. When we start to overheat, our bodies secrete sweat which evaporates and lowers our body temperature. While more than half of the human body is water, we lose up to 3 quarts of water each day from breathing, urinating, and sweating, so it’s imperative that we drink enough to maintain every important function in the body.
Schedule Your Walks
Walking is one of the best exercises you can do for COPD. It helps to increase your pulmonary function, build muscles in your legs and arms and gives you the opportunity to practice your breathing techniques. However, walking outside during the hottest time of day can put you at a higher risk of experiencing a heat stroke or other heat-related injuries.

Fortunately, with some careful planning, you can be sure to avoid this. In the summer, the hottest time of day tends to be from noon to around 3 or 4:30, so it’s best to schedule your walks around this. Try to schedule your walks for early in the morning when the sun is up but hasn’t been out long enough for it to get too hot.
Another thing you should do is keep an eye on your local forecast. Although you can go for a walk when the skies are clear, it’s even better to go when there’s some cloud coverage. Clouds block a lot of the UV rays from the sun, especially the most harmful UV-B rays which put you at a lower risk of overheating or getting sunburned. However, you should still be sure to wear sunscreen every time you go out.

One final reason to schedule your walks is to avoid the busiest times of the day. As aforementioned, there are a lot of people outside trying to enjoy the nice weather. Some people are out mowing the lawn or doing other yard work which can cause a lot of allergens to mix into the air. You can also keep an eye on the pollen count forecast to avoid allergy triggers in your area. Ultimately, avoiding these airborne irritants will help you manage your COPD symptoms more easily.
Don’t Over Exercise
While exercise is a very important part of treating COPD, it’s also imperative that you learn to recognize the signs of overexercising. This is especially true when it’s so hot outside because it may happen a lot faster than you’re expecting it to. As a result, it’s a good idea to keep a close eye on exactly how much time you spend exercising.

According to the Cleveland Clinic, COPD patients should gradually work up to exercising around 30 minutes a day, at least three days a week. Exercise will help improve your circulation, strengthen your heart, lower blood pressure, improve COPD symptoms and much more.
If you enjoy exercising outside, be sure to check the weather at the beginning of the week and plan out what days and time you will exercise. It’s recommended that you follow each workout day with a day of rest, but if you need to workout two days in a row to avoid the heat, this can be considered too.
Another thing you should do is play it by ear. Heat exhaustion is characterized by fatigue, restlessness, dizziness, and muscle cramps. So, if you experience any of these symptoms throughout the week, it’s a good idea to change up your workout schedule in order to recover. If these symptoms continue, be sure to consult your doctor.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Change Your Wardrobe
Believe it or not, the clothes you wear can have a huge impact on your ability to stay cool on a hot day. First and foremost, you should wear loose-fitting clothing. Cotton t-shirts and shorts tend to be your best bet because they are lightweight, breathable, and won’t make you feel like you’re suffocating.

When it comes to footwear, sandals or a more breathable pair of tennis shoes are great options. Sandals are great if you don’t want to wear socks and retain extra heat. But if you want a little more arch support, you can wear a light pair of tennis shoes with thin socks.
To top off your wardrobe, try wearing a baseball cap or gardening hat which will help to keep the sun off your head, face, and neck. These areas tend to be the most vulnerable to heat injury and you’re more prone to feel delirious, noxious, or even lose consciousness if your head is exposed to too much sun and heat.

Keep an Ice Pack Handy
One simple way to keep cool during the summer is to keep an ice pack handy to lay on your skin if you feel like you’re overheating. It’s best to have multiple ice packs so that you can have a backup. Then when one melts, you can simply go to the freezer and swap it out with another one. If you don’t have an ice pack, you can fill a bag with ice and this will work just as well.

One thing to note before trying this is that ice can cause frostbite or ice injury if it’s applied directly to the skin for prolonged periods of time. This can lead to numbness, itchiness, or pain and can even lead to damaged blood vessels and reduced blood flow. To prevent this, try wrapping the ice pack or bag of ice in a cloth towel. Ultimately, the goal is to lower your body temperature slightly, you don’t want the ice to be so cold that it stings or causes numbness on your skin.

If you don’t have access to ice or ice packs, cold water can be an effective alternative. Simply rub some water on your legs, arms, chest, or face, and rather than wiping it off with a rag, let it evaporate off. If you do this too much, however, it could dry out your skin, so be sure to do it in moderation and keep some lotion handy to help your skin retain moisture.
Avoid Hot Foods and Beverages
While it may be tempting to indulge in burgers, hot dogs, or barbeque during this time of year, it’s generally best to avoid them if you want to keep your body temperature down. Hot foods and beverages are comforting all times of the year, but they don’t help when it comes to managing your body temperature and they can make COPD symptoms worse.
Another reason to avoid hot foods is because they can increase the temperature of your home. Running the stove or the oven for a long period of time not only raises the temperature in your kitchen, but it can raise the temperature of your whole home. If you’re looking for great food to eat in the summer, it’s better to reach for something like fruits or vegetables which tend to have high water content meaning they’re refreshing and they’ll keep you hydrated.

Hot drinks like coffee or tea are another thing to avoid this time of year. While this little boost of caffeine may help you wake up in the morning, there are better ways to do this that won’t have potential side-effects on COPD.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Quit Smoking Immediately
According to the Centers for Disease Control and Prevention (CDC), about 38 percent of COPD patients report being current smokers. This is astonishing considering that about 80 percent of deaths due to COPD could have been avoided without smoking. One thing that many people don’t realize is that smoking when it’s hot out may amplify the negative effects.

While hot weather and humidity can already put a lot of strain on your body, making it harder and harder to breathe, smoking increases your body temperature and irritates the airways which are already irritated. Smoking also alters mucus production in the body which could make it more difficult to clear respiratory irritants like pollen. It also gives you withdrawals which decrease your mood and make you less likely to follow through with your COPD treatment routine.
One of the main reasons people get back into smoking is out of boredom or they’re looking for quick relief from stress or anxiety. While smoking may seem like an easy solution, over time, it will only cause more harm than good. It’s understandable why someone would have a craving for cigarettes when they’re stuck at home, but the truth is, there are plenty of things to keep your mind busy without taking up smoking again. Check out this post where you’ll learn about 7 COPD-friendly activities to keep you busy during the quarantine.
![]()
Conclusion
Temperature and climate might not always be something you think about when it comes to managing a respiratory illness. However, according to the Environmental Protection Agency (EPA), there are 1,300 deaths per year due to heat-related illnesses and there are far more than that who are admitted to the hospital from things like heat stroke, heat edema, or heat exhaustion.
Unfortunately, due to the nature of chronic respiratory illness, COPD patients are much more likely to experience heat-related injuries. Follow some of the tips above to help you prepare for the heatwaves we’re experiencing across the country, and if you have any further concerns or you’re thinking about changing your treatment plan, be sure to reach out to your doctor or pulmonologist for guidance.
In the meantime, take some time to look at our portable oxygen concentrators. If you’re a COPD patient who loves to exercise, these devices will allow you to do so while maintaining your oxygen saturation and preventing COPD symptoms such as breathlessness, chest pain, and fatigue. Fill out the form at the side of the page and one of our respiratory specialists will reach out to you shortly.
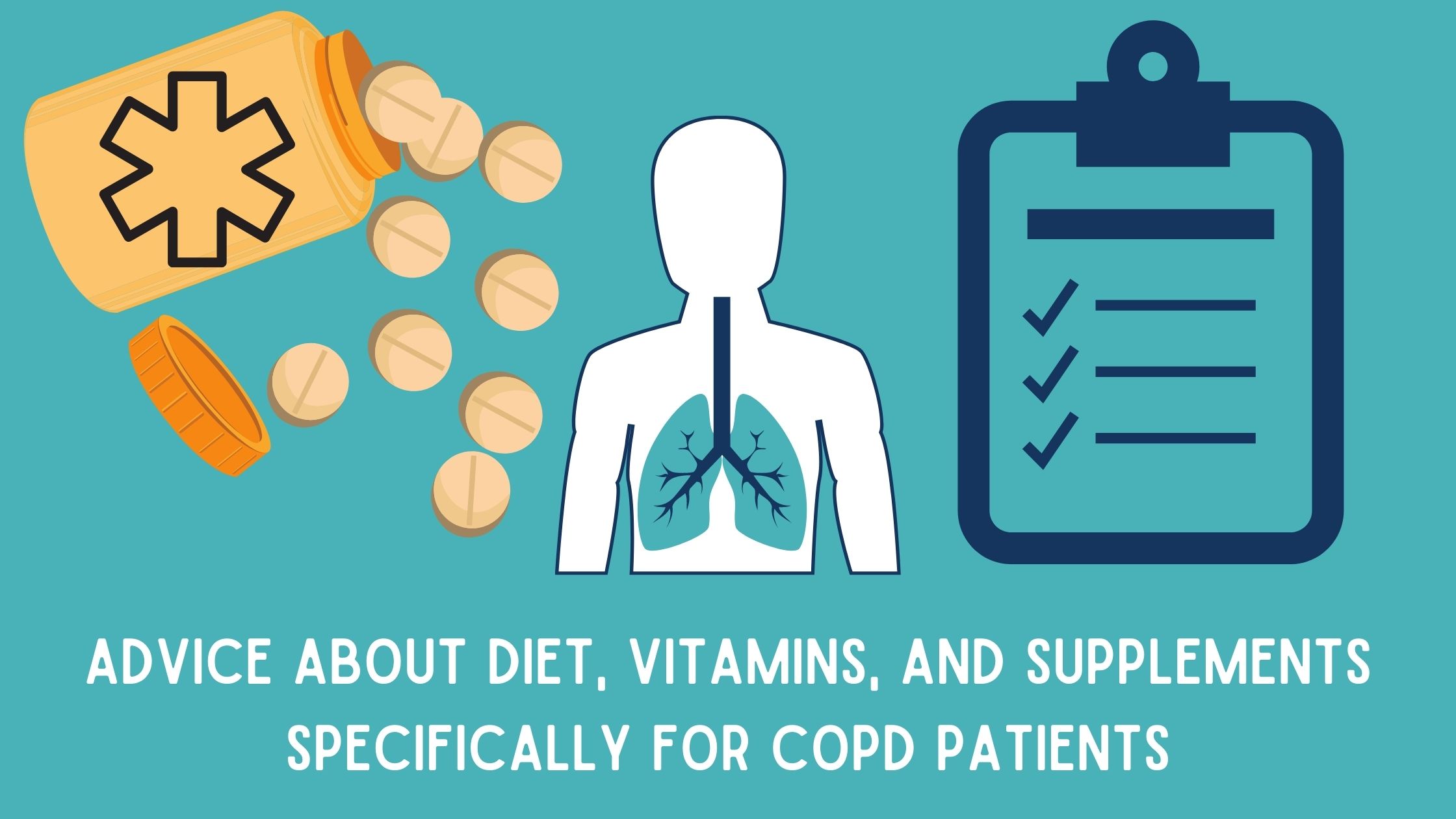
Chronic obstructive pulmonary disease (COPD) is a term that categorizes a few chronic lung conditions: chronic bronchitis, refractory asthma, and emphysema all of these conditions restrict airflow in some way.
There are about 15.7 million people in the United States who have reported that they have been diagnosed with COPD. This is a progressive disease that gets worse overtime especially if the patient does not treat it properly.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Treating COPD is a lifelong journey comprised of doctors visits, respiratory tests, exercise, oxygen therapy, changing eating and drinking habits, and taking vitamins and supplements.
In this article we are going to focus on how COPD patients can develop a healthy eating habits and take vitamins and supplements in order to help ease the symptoms of COPD.
COPD Information
If you have COPD, it is likely that you find it increasingly difficult to breathe, and this can impact so many aspects of your life. The other symptoms you may experience are coughing, wheezing, excess mucus production, feeling of tightness in your chest, and fatigue.
COPD does not only affect your ability to breathe, but can cause a lot of other problems due to the lack of oxygen in your blood. Many COPD patients need supplemental oxygen therapy, and these patients have to use a device called a portable oxygen concentrator or an oxygen tank in order to get the right amount of oxygen. Oxygen will be prescribed to you if you need it.

In conjunction with your oxygen therapy, you can do a number of things to treat your respiratory condition, one of those treatments is eating healthy and getting the right amount of nutrition. If your diet doesn't give you the vitamins and nutrients you need, it could be helpful to take supplements and vitamins that would support any deficiencies you may have.
Nutrition and Eating Healthy for COPD

Nutrition is a crucial part of treating COPD, and oftentimes one of the hardest things to keep up with, vitamins and supplements can help you get the nutrients your diet is lacking or important vitamins that your body is craving.
Vitamins and minerals give you energy and stamina, and you get vitamins form food and water, if you are not eating the right foods, you may have vitamin deficiencies. If you have COPD, it is likely that you require 430–720 more calories per day than healthy people.
Calories are the fuel that gives your body energy to function. You can get healthy calories from grains, vegetables, fruits, proteins, and fats you eat. COPD patients often require these extra calories because of the added effort they need to breathe. Therefore, malnutrition is also something many people with COPD struggle with. Malnutrition can affect you for a long time, and can negatively impact your disease progression.
It is recommended that eating a high fat, low carbohydrate diet can help people with breathing problems.
Best Eating Habits for People with COPD

Building healthy eating habits is an essential part of treating your COPD. Many people with COPD do not have an appetite or have a hard time finding the energy to cook and eat, and therefore suffer from malnutrition. Follow these following tips to make eating easier.
- Try making food easier to chew, you can do this in a number of ways. When you are cooking vegetables, cook them fully until they are soft. You can mince or grind the meat down and make bowl styled dishes. You can also focus on eating foods that are already easy to chew like pasta, mashed potatoes, thick soups, creamed soups, and casseroles fruit smoothies.
- If you feel short of breath while you are eating you should try to rest 30 minutes before meals. Start practicing pursed-lips breathing and other breathing exercises daily that will improve your breathing endurance.
- While you eat, make sure your body is in a position to expand your lungs, try sitting upright and lean forward with your elbows on the table and keep your feet on the floor.
- Ask your healthcare provider, if you are using a pulse flow oxygen device or a continuous oxygen device, if you should increase your flow rate during meals but do not adjust your oxygen flow without talking with your doctor first.
- Eating and cooking can be exhausting for lung patients, to avoid fatigue, try the “Meals on Wheels” in your community or a similar service that will provide you with nutritious, low-cost meals. By using a service like this, you won’t have to prepare meals.
- Eating too much too often will make you feel tired, instead try eating six small meals each day instead of three big ones. This will also keep your metabolism from slowing you down. The key to maintaining energy throughout the day is to conserve oxygen, and digestion takes up your energy and therefore takes up your valuable oxygen. If you eat smaller meals, you use less oxygen.
- If you enjoy cooking, try to find easy-to-make recipes, and if you don’t enjoy cooking as much, ask family or friends to help with making meals. Even though sugar can sometimes give you a small burst of energy, sweets, cookies, cakes, and other deserts, also known as simple carbohydrates will hold carbon dioxide inside of you causing tiredness.

- Bloating is extremely uncomfortable for lung patients because your stomach is pushing on your diaphragm making it even more difficult to breathe. To avoid this bloating feeling, do not rush your meals, and no not eat when you are short of breath, by doing so, you can simultaneously swallow air making your bloating worse.
- Spread out the amount of fluids you drink, and try drinking one hour before and one hour after a meal in order to decrease the amount of stuff in the stomach at one time.
- Onions, cabbage, sauerkraut, broccoli, Brussels sprouts, and beer all cause bloating, so try to avoid these foods when you can. Fried, fatty food and other high-fat foods are hard to digest and can only be processed in your body very slowly slowly, causing a feeling of bloating.
- Lactose may cause bloating, if you feel bloated after eating or drinking milk, yogurt, cottage cheese, or other dairy products, try avoiding dairy.
- By adding lots of fiber and fluid to your diet you can avoid constipation and bloating.
Supplements and Vitamins

Beyond developing a healthy respiratory diet that works to mitigate your COPD symptoms and helps give you energy, there are also many different supplements and vitamins that you can try to support your medical treatment and help manage your symptoms.
Various vitamins (vitamin C, D, E, A, beta and alpha carotene) can help improve COPD symptoms, exacerbations and pulmonary function and high vitamin intake would probably reduce the annual decline of FEV1.
Vitamins you Need if you Have COPD

COPD flares or exacerbations are episodes of escalated symptoms. When you experience a flare up, you may need to use your rescue inhaler or medication, increase the oxygen output on your portable oxygen concentrator if your doctor recommends it, and in some cases seek emergency medical attention.
In order to avoid COPD exacerbations all together you can do a number of things:
- Take your oxygen as prescribed everyday
- Practice breathing exercises to increase your endurance
- Avoid allergens
- Avoid chemicals and harsh cleaning product
- Avoid bad air quality, and get a home air purifier
- Exercise regularly
- Eat a respiratory friendly diet as mentioned in the beginning on this blog
- Take supplements and vitamins that are good for your health
LPT medical has a COPD resource center on our website where you can go to find information regarding all of these actions you can take to avoid COPD exacerbations and how to take the best care of your condition.

Continue reading this blog for information about how certain supplements can help improve your condition.
Vitamin D
Research shows that many people with COPD also have very low vitamin D, therefore taking vitamin D supplements can help your lungs function better.
The main reason people with COPD can have Vitamin D deficiencies is due to the lack of sun contact, resulting in lack of vitamin D production in skin.
Taking vitamin D-3 supplements for COPD can help protect you from experiencing moderate or severe flare-ups.
Vitamin C
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Research shows that having low levels of vitamin C can lead to symptoms like shortness of breath, mucus, and wheezing, all of which are already symptoms of COPD, and avoiding excess
Vitamin E

Vitamin E is important for your vision, reproduction, your blood, brain and skin.
Studies have shown that long-term use of Vitamin E can help prevent COPD because it has antioxidant properties, which may protect your cells against the effects molecules that are produced when your body is exposed to tobacco smoke and radiation.
If you experience consistent flare-ups of COPD, it is likely that you have lower levels of vitamin E than normal. Taking a vitamin E supplement can help your body get back to normal vitamin E levels.
Vitamin A

Vitamin A is crucial to the functioning of your immune system and plays a vital role in your cells to growth. Taking Vitamin A supplements may help you lungs function at a high capacity if you have a vitamin A deficiency.
Magnesium
Some COPD medications can interfere with your body’s ability to absorb magnesium, this can be harmful for COPD patients because magnesium supports lung function. Taking a magnesium supplement could cause side effects. If you do take magnesium supplements be sure to monitor yourself carefully.
Calcium

There are some COPD medications that may cause you to lose calcium and calcium can help your lungs function. You should try to intake more calcium-rich foods in your diet and if you are still unable to reach your calcium requirements, it may be necessary to take a calcium supplement.
Omega-3 fatty acids

Omega-3 fatty acids can reduce the inflammation in your lungs from COPD. You can eat more fish, seeds, and nuts, to get Omega-3 fatty acids, but you can also take fish oil supplements to make sure that you are getting enough.
Overview
COPD is a chronic illness, and there is no cure, however you can treat your disease. If you maintain a strict COPD treatment regimen you can regulate you symptoms. By taking your medication, adhering to your oxygen prescription, eating healthy and getting the nutrients you body needs you can slow down the progression of your COPD.
If you have issues eating, and find it hard to maintain a healthy diet, we hope that you found some of the ideas listed in this article that will help you get the nutrients you need in order to help relieve your COPD symptoms.
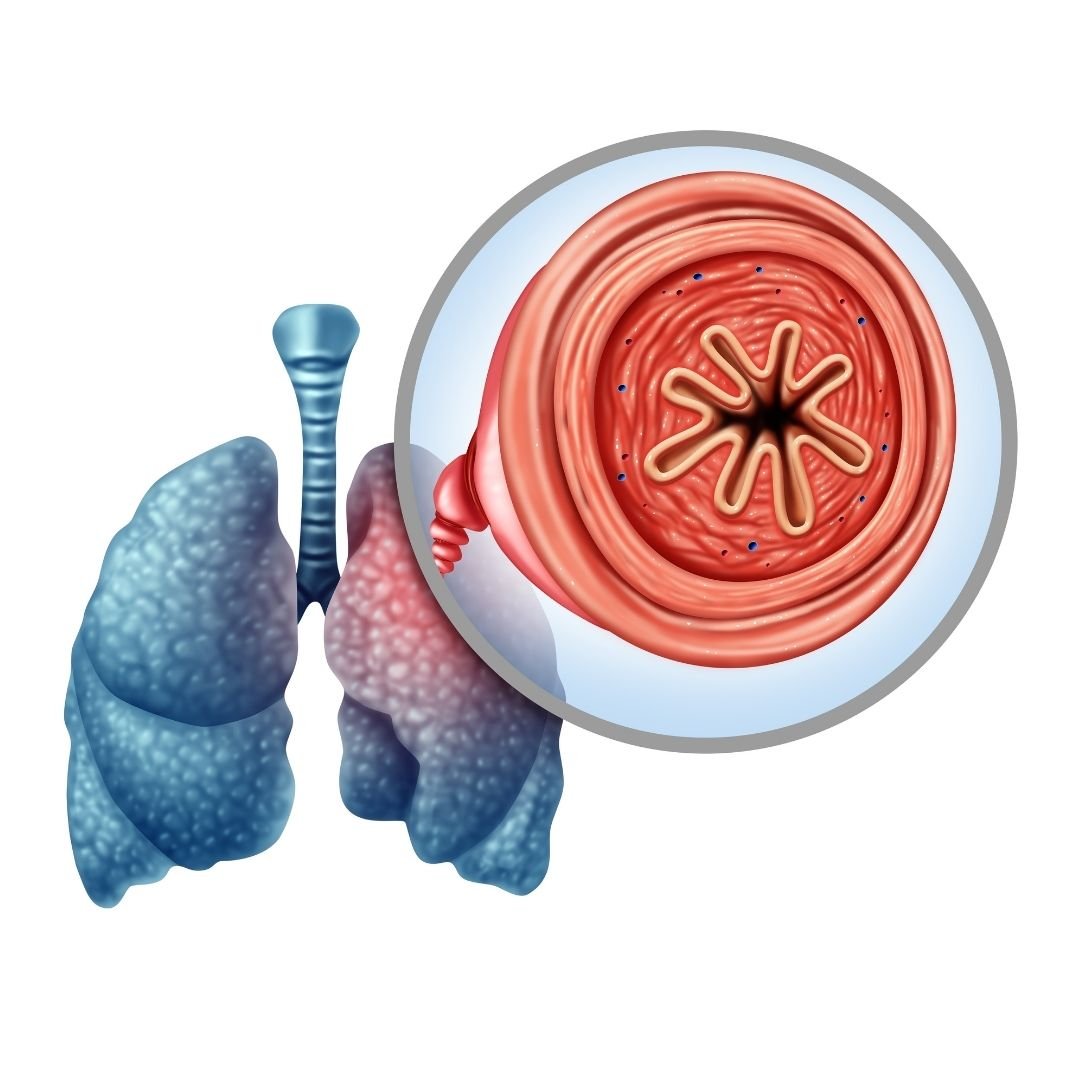
If you have COPD it is likely that your body is lacking in vitamins you needs, and if you are experiencing certain signs of vitamin deficiencies, you should speak with your doctor about taking specific supplements.
Getting the right amount of nutrients and taking supplements can help you better manage you COPD symptoms and helps you body function optimally.
If you learned anything in this blog, or feel as though someone in you life could benefit from any of this information, please leave a comment or share this blog with your friends and family!


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













