Having a dry mouth is a symptom that many COPD patients experience, although it is often overlooked. Compared to more visible or more serious ailments, like coughing and shortness of breath, many patients consider their dry mouth symptoms to be low priority or never bring them up with their doctor at all.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
However, a dry mouth is an extremely uncomfortable symptom, and it is likely to only get worse if you leave it untreated. If ignored for too long, it can even lead to more serious problems like gingivitis, oral thrush, and tooth decay.
That's why in this post we're going to show you what to do if you experience a dry mouth because of your COPD. We'll introduce you to a variety of products and techniques that can treat dry mouth symptoms and show you how to prevent them from returning in the future.
If you or someone you know is suffering from a dry mouth, then this guide will give you the tools you need to track down both the cause and the solution. A dry mouth can happen for a variety of different reasons, and by better understanding the causes and potential treatment options you'll be much more likely to find a solution that works effectively for you.
Dry Mouth Symptoms
The clinical term for a dry mouth is xerostomia, and it happens when your mouth can't produce enough saliva to keep itself moist. It can happen for a variety of reasons, including stress, breathing through your mouth, and taking certain medications.
COPD patients are particularly likely to get a dry mouth as a result of COPD medications and symptoms. It's nothing to worry about if it only happens every once in a while, but you'll need to find a solution if it happens more often than that.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Having a dry mouth can make a variety of things difficult, including eating, chewing, and swallowing. A dry mouth can also make it difficult to talk or make your voice sound scratchy and hoarse.
A dry mouth is often accompanied by a dry throat, nose, or sinuses. This can cause the lining of your nose and upper airways to become irritated and sore, and even lead to nosebleeds and infections.
Here are some of the common symptoms of dry mouth (xerostomia):
- Dry or sticky feeling in your mouth
- Thick, stringy saliva
- Dry tongue
- Dry or sore throat
- Hoarse voice
- Trouble chewing, swallowing or speaking
- Changes in your ability to taste food
- Problems with dentures
Risks and Complications of Not Treating Dry Mouth

Having a dry mouth is more than just unpleasant; it can actually be bad for your health. If it happens frequently, it can cause a variety of other symptoms in your mouth, nose, and throat.
That's why it's important not to ignore dry mouth symptoms if they don't go away quickly on their own. Left untreated, a dry mouth can accelerate tooth decay and lead to other infections and problems.
Tooth Decay
To stay healthy, your mouth should produce enough saliva to stay moist all of the time. However, when you are sick, take certain medications, or suffer from a respiratory disorder like COPD, it can dry out your mouth so much that your saliva glands can't keep up.
This is bad for your oral health, because saliva plays an important role in keeping your teeth and gums clean. It washes bacteria and food particles off of your teeth and has anti-bacterial and anti-fungal properties.
Keeping your mouth moist prevents bacteria from taking hold and prevents tartar build-up on your teeth. If not managed effectively, having a frequent dry mouth leads to tooth decay and cavities.
Mouth Infections and Gum Disease

If left untreated for too long or not properly managed, a dry mouth can lead to bacterial and fungal infections in your gums and other surfaces in your mouth. This can cause your gums to become inflamed, leading to gingivitis and full-blown gum disease.
Symptoms of gingivitis include swollen, sensitive or bleeding gums, bad breath, and pain when you chew. If you experience any of these symptoms along with a dry mouth, you should go see your dentist right away.
A dry mouth can also allow fungus to flourish in your mouth, causing a yeast infection known as candidiasis or oral thrush. Thrush appears as white patches on your tongue, throat, and roof of your mouth.
A dry mouth can also cause sores by leaving you vulnerable to bacterial infections on the surface of your mouth. It can also cause your lips and the skin around your mouth to crack, which is painful and puts you even more at risk for infection.
What is Causing Your Dry Mouth?
Many COPD patients suffer from a dry mouth for a variety of different reasons. Many COPD symptoms can dry out your mouth and throat, as can many different medications used to treat COPD.
If you know what is causing your dry mouth, then it will be easier to find an effective solution that can treat it. To help you understand the cause of your dry mouth, let's take a look at some of the different ways that living with COPD can dry out your mouth and throat.
COPD Medications

Many of the medications used to treat COPD can cause your mouth to get dry. It is a common side effect of inhalers, steroids, and several other drugs used to manage COPD symptoms.
Short-acting bronchodilators are one of the worst culprits and one of the biggest medicinal causes of dry mouth in people with COPD. Most people with COPD have to take bronchodilator medications via an inhaler at least once a day to keep their airways open and their symptoms under control, which can leave them with uncomfortable dry mouth symptoms every day.
Many COPD patients also use steroid inhalers to treat inflammation and prevent exacerbations. Steroid medications are known to dry out your mouth, especially when you take them with an inhaler.
Along with a dry mouth, steroid inhalers, bronchodilator inhalers, and especially combination inhalers (steroid plus bronchodilator) can cause throat irritation, hoarseness, and complications like yeast infections and cavities. If you have COPD, it's important to know how to manage these and other dry mouth symptoms to avoid permanent damage to your oral health.
Another medication many COPD patients take frequently is antibiotics, which are used to treat COPD exacerbations and treat infections in the lungs and upper airways. Many antibiotics can also cause dry mouth symptoms, including Azithromycin, a common antibiotic used to treat COPD.
Luckily, most courses of antibiotics are short, so even if you experience a dry mouth, you shouldn't have to manage it for more than a week or two. However, you should talk to your doctor anytime you experience side effects from your medications, including dry mouth. Your doctor may even be able to give you a slightly different medication to see if your symptoms improve.
Other Medications

Many other medications can also cause a dry mouth, including antidepressants, antacids, quit-smoking medications, and anti-inflammatory drugs. While these drugs are not necessarily COPD medications, they are frequently used by people with COPD to treat other conditions and complications related to or worsened by their disease.
Oxygen
Supplemental oxygen is also a medication, but it deserves a category of its own for its role in causing dry mouth. The majority of oxygen patients suffer from mouth and throat dryness occasionally, and, for some patients, it's a constant struggle to keep their mouth from getting dry.
Often, mouth dryness comes from having a continuous flow of oxygen forced through your mouth and throat, which can dry up the saliva in your mouth after a while. Pulse-flow oxygen is less harsh and less likely to dry you out, but many patients are unable to use pulse-flow technology to meet their oxygen needs.
You are more likely to experience a dry mouth while using oxygen at night, especially if you sleep in a dry room or breathe through your mouth when you sleep. Your mouth and throat are especially likely to get dry if air has an opportunity to leak out of your mouth or nose. This can happen if your oxygen mask doesn't form a tight enough seal or if your mask uses a pillow cushion under the nose.
Using a CPAP or BiPAP machine to treat sleep apnea can have the same drying effect as using supplemental oxygen. Since many people with COPD also have sleep apnea, this is a common cause of dry mouth in COPD patients.
COPD Symptoms That Cause Dry Mouth
COPD wreaks havoc on your respiratory system, causing a variety of uncomfortable symptoms, including a dry mouth. Whenever you have a bout of coughing, wheezing, or shortness of breath it can leave your mouth and throat feeling scratchy and dry.
Your mouth and throat are integral parts of your respiratory system and get directly affected by the conditions in your airways. And as an entry point through which air enters your body, it is one of the parts most affected when you breathe in dry, irritating air.
Whenever you experience a flare-up or exacerbation, it can make a dry mouth even worse, and put you at a higher risk of illness and infection. That's why you should avoid allergens, germs, and respiratory irritants like perfumes and air pollution that could make your symptoms worse.
Here are some of the symptoms and conditions that can cause a dry mouth with COPD:
- Coughing
- Wheezing
- Mouth breathing
- Flare-ups and exacerbations
- Exposure to dry air
- Exposure to smoke, pollution, and irritating particles
- Exposure to allergens, mold, and dust mites
Solutions to Treat a Dry Mouth
Make Adjustments to Your Oxygen Delivery System
The best way to treat a dry mouth is to treat the underlying problem. For many people with COPD (but not all), the main underlying cause of mouth dryness is supplemental oxygen therapy.
Luckily, there are a variety of things you can do to minimize dryness from oxygen therapy and make it more comfortable for your mouth, nose, and throat. These include things like using the right kind of oxygen mask or nasal cannula and getting a humidifier for your oxygen device.
Get a Humidifier Bottle for Your Oxygen Delivery System or CPAP/BiPAP Machine

If you use supplemental oxygen, then you know that the flow of air from your oxygen delivery device can severely dry out your mouth and throat. Higher oxygen flow rates tend to cause worse dryness and may even irritate your lungs and airways.
That's why many oxygen patients get a humidifier bottle to attach to their oxygen delivery system. All you have to do is fill it with distilled water and connect it to the tubing to bubble the air from your oxygen source through. This moisturizes the air to make it less dry by the time it reaches your mouth or nose.
If you experience a dry mouth, nose, or throat more than occasionally while using oxygen, talk to your doctor about getting a humidifier to attach to your oxygen delivery device. However, whether or not you can use a humidifier may depend on your personal oxygen requirements, and it won't work with pulse flow oxygen.
You can also get a humidifier for your CPAP or BiPAP machine if you use one to treat sleep apnea. Talk to your doctor about getting a humidifier for your machine if you often find yourself waking up with a dry mouth or throat during the night.
Using a humidifier bottle can make a huge difference in your comfort and dry mouth when you use oxygen. To learn more about how to make supplemental oxygen more comfortable, visit our previous post here.
Don't Let Your Oxygen Mask Leak

If you have a humidifier for your oxygen but still experience a dry mouth or throat, then it could be because your oxygen mask is leaking. If there is a gap between the edges of the mask and your skin, it allows the humid air from your oxygen supply to escape while letting dry, outside air in.
This can cause severe dryness and is most likely to happen if you use a nasal pillow mask or a mask that doesn't fit correctly. In that case, you may need to replace your mask with one that fits your face better and doesn't allow air to leak out.
Get a More Comfortable Oxygen Mask or Nasal Cannula
Sometimes you can reduce mouth, throat, and nasal dryness from oxygen therapy just by using the right kind of nasal cannula or mask. For example, you can get high-flow nasal cannulae that help by simply reducing the speed at which the air rushes into your nose.
Nasal cannulae and masks come in a wide variety of designs and materials you can choose from. You might have to try out a few different types before you find the one that's most comfortable and convenient for you.
Using the right mask can make all the difference in how comfortable oxygen therapy is and how dry your mouth, nose, and throat feel. To learn more about all the different options for oxygen masks and nasal cannulae, visit our previous post here.
Rinse Out Your Mouth

When your mouth is dry, simply rinsing it out with water once every hour or two can help you keep it moist. You can rinse your mouth out with plain tap water or use a solution of water with added salt or baking soda, if you like.
You can also use oral rinses like Biotene mouth wash whenever your mouth feels dry. These rinses add extra moisture and protect your teeth from harmful bacteria and fungi.
Some oral rinses can even soothe your mouth if it's irritated or strengthen your teeth to fortify them against bacteria and decay. However, it's important to find a mouthwash or oral rinse that is alcohol-free, because alcohol can irritate your mouth and dry it out even more.
Here is a list of some alcohol-free mouth rinses you can use to treat a dry mouth:
- Biotene Mouthwash (made by GSK)
- Oasis Moisturizing Mouthwash (made by GlaxoSmithKline)
- Eco-DenT Ultimate Natural Daily Rinse (made by Eco-DenT)
- Crest Pro-Health Rinse (made by Procter and Gamble)
Use Saliva Substitutes and Oral Gels
There are a variety of saliva substitutes and oral gels on the market that you can use to moisturize your mouth when it gets dry. While they only provide temporary relief from dryness, they tend to be more effective than simply rinsing your mouth with water or mouthwash.
Saliva substitutes mimic the salinity and acidity of natural saliva and come in sprays and liquid solutions. You can buy them over the counter at most drug stores, although you may need to ask a pharmacist for help hunting them down.
You can use your saliva substitute as often as you like throughout the day as long as you have permission from your doctor. However, you are not supposed to eat or drink for fifteen minutes after use.
Oral gels use a special gel solution to lubricate the inside of your mouth and are also available over the counter. Oral gels are great for sealing in moisture and can last for up to four hours after application.
Here is a list of oral gels and saliva substitutes you can use to treat dry mouth:
- Biotene Oral Balance Moisturizing Gel and Dry Mouth Liquid (made by GSK)
- Mouth Kote (Parnell Pharmaceuticals)
- Oasis Moisturizing Mouth Spray (made by GlaxoSmithKline)
- Saliva Substitute (made by Roxane Laboratories)
- Sprey Rain Oral Mist Spray (made by Xlear)
Get Prescription Medication

There are a couple of prescription-only medications that can stimulate extra saliva production and relieve dry mouth symptoms. However, these medications, called secretogogues, are usually only available for patients with chronic, severe dry mouth caused by head and neck radiation therapy.
However, if you experience a frequent dry mouth from oxygen therapy or other medications, you should still talk to your doctor to see if you have any prescription medication options. If your dry mouth is severe and poses a threat to your oral health, your doctor may consider prescribing you a saliva secretogogue medication.
If your dry mouth is causing a bacterial or fungal infection, your doctor or dentist may also prescribe you an antibacterial or antifungal medication. These types of infections are more common when you don't have enough saliva to neutralize bacteria and fungi in your mouth.
Rinse Your Mouth After Using Your Inhaler

Whenever you use an inhaler, you should always rinse out your mouth immediately afterward. Most inhalers include this as part of their instructions, but many patients ignore this step or get lazy over time.
Some studies show that only about half of the medication you inhale ends up actually making it to your lungs and airways; the rest ends up coating your mouth. That's why rinsing your mouth out after using your inhaler is so important, especially if you use it every day.
Swishing water around your mouth removes the residue of the medication, which is what causes dry mouth when you use your inhaler. Washing it off helps your mouth stay moist and prevents cavities, oral thrush, and bacterial infections like gingivitis.
However, you have to remember to rinse your mouth out immediately after you use your inhaler in order for it to be effective. Studies show that putting it off for even one minute gives the medication enough time to absorb into your mouth, causing dryness and other complications.
Use Moisturizers and Creams

While these aren't for your mouth exactly, moisturizers and creams are a godsend for chapped lips and skin. After all, if your mouth is dry and dehydrated, there's a pretty good chance that your skin and lips are on the dry side, too.
Oxygen therapy, in particular, can cause your lips and the skin around your mouth to get dry, irritated, and cracked. Luckily, all it takes is regular moisturizer application to keep your skin smooth and moist.
Since oxygen is highly flammable, oxygen patients should always avoid using chapsticks and moisturizers that contain petroleum, which is also a very flammable substance. Instead, you should only use water-based lubricants and lip balms when you use supplemental oxygen.
If you don't use oxygen, then you are free to use whatever kind of skin or lip moisturizer you prefer. However, moisturizing creams tend to be thicker and work better than lotions, and simple petroleum jellies like Vaseline work exceptionally well for chapped lips and skin.
You can also use water and petroleum-based lubricants to lubricate the outside of your nose and just inside your nostrils if they get dry. If you experience nasal dryness, a saline nasal spray or nasal gel can give you temporary relief.
If you use supplemental oxygen, Surgilube is a great water-based lubricant used by many oxygen patients and hospitals. It's an inexpensive, all-purpose lubricant that can come in handy for a variety of moisturizing needs.
Make Hydration a Priority

Dehydration is a common problem in people with COPD, and it can cause your mouth to dry out, too. Even if your dry mouth is caused by a medication or any other reason, getting dehydrated can make it much worse.
If you struggle with a dry mouth often, then you should be making drinking enough water a top priority in your daily routine. Not only will it help with your dry mouth, but it can reduce a variety of symptoms caused by COPD.
However, it can be difficult to remember to drink enough water throughout the day, even if you know that it's a healthy thing to do. Fortunately, there are plenty of tried-and-true ways to help yourself build healthy hydration habits.
Use Water Bottles

For people who have COPD, living in a clean environment should be a top priority. Because the disease makes the lungs hyper-sensitive to irritants, even small amounts of dust and allergens can set off coughing fits and make daily COPD symptoms worse.
Unfortunately, there are many places in your home that can trap particles that irritate your lungs, and it can be difficult to track them all down. Harmful particles can accumulate in your carpet, furniture, and all the nooks and crannies of your home, where they lie in wait until they get stirred up into the air you breathe.
One of these hidden sources of respiratory irritants could be your bedding, which is an oft-overlooked hot spot for dust and allergens. Many people don't realize how quickly their pillows, mattresses, and bed sheets can accumulate hazardous particles that can trigger COPD symptoms.
In this article, we're going to show you how to get rid of dust, mold, dust mites, and other particles in your bedding and keep them away for good. That way, you can rest assured every night knowing your lungs are protected while you sleep.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
A Very Real Hazard
_Lorryia_formosa_2_edit.jpg)
It's easy to underestimate the dangers that respiratory irritants in your sheets, pillows, and mattress can pose for your lungs if you have COPD. However, based on how much time you spend in and around your bed, it should not be difficult to imagine how being exposed to them night after night could affect your lungs on a daily basis.
Because you spend so much time in your bedroom, keeping it clean and lung-friendly should be one of your top priorities. Most people spend a minimum of seven to eight hours in their bed every night, and it can have a significant affect on your ability to breathe if you are surrounded by hazardous particles and allergens while you sleep.
If you don't take special precautions, dust, mold, pollen, and other irritants that live in your bed enter your lungs at night when you breathe. This can inflame your lungs, causing you to wake up with worse symptoms that can last throughout the day.
That's why it's so important to give your bedding some extra attention if you have COPD. Just being more careful and deliberate in the types of fabrics you use and how you care for them can go a long way toward improving your COPD symptoms.
The Hazards Hiding in Your Sheets

According to a microbiologist from the New York School of Medicine, beds are uniquely prone to collecting all kinds of nasty and potentially hazardous substances. “You have spores of fungi, bacteria, animal dander, pollen, soil, lint...” he says, along with skin cells, oils, cosmetics, and bodily secretions, among others.
While some of these are simply gross, others can actually be dangerous for your lungs, especially if you have COPD. Dust mites, mold, pollen, and pollutant particles, in particular, can inflame your lungs, cause uncomfortable symptoms, and exacerbate your COPD.
Dust Mites

Wherever there's fabric, there's a good chance there is an invisible army of dust mites living in the fibers. Dust mites live off of dead skin, dust and fibers, and thrive in places like your carpet, furniture, and—you guessed it—your bedding.
Dust mites particularly like anything that's made with plush or layered fabrics like pillows, comforters, mattresses, and thick blankets. These items tend to trap lots of dust and dead skin for the little bugs to to munch on.
While they don't affect everyone, dust mites cause many people to experience symptoms like coughing, sneezing, and nasal congestion when they're around. If you have COPD and are sensitive to dust mites, exposure to the mites in your mattress and bedding can inflame your lungs and airways and make your COPD symptoms worse.
Mold

Mold is another respiratory irritant that could be lurking in your pillows, mattress, or bed sheets. Exposure to mold can irritate your lungs and cause a variety of uncomfortable symptoms, including coughing, wheezing, nasal stuffiness, eye irritation, and even skin irritation in some cases.
Some people are more sensitive to mold than others, but patients with COPD should be careful to steer clear of damp, moldy environments. That includes looking out for mold growth in your home, including in your fabrics and bedding.
Bed sheets, blankets, and other fabrics can get moldy after you wash them if you leave them sitting in the washer too long or don't dry them out quickly enough. You can usually tell if they've grown any mold because they'll have a musty, mildew odor, even after they've dried.
Your mattress and pillows can collect mold, too, if they get get wet for any reason. That's why it's important to avoid spilling water in your bed and to dry up any damp spots immediately.
If you live in a humid climate, things will get damp easier and dry out more slowly, which means you'll need to be even more on the lookout for mold and mildew. It's also important to know that mold is almost guaranteed to grow in any place that stays damp for more than 24 hours, no matter where you live.
Keeping your bed free from mold is important for protecting your lungs and keeping respiratory symptoms at bay. If you have musty sheets or hidden mold in your mattress, it can cause your COPD symptoms to flare up and hurt your ability to breathe every day.
Pollen, Pollution, and Other Particles
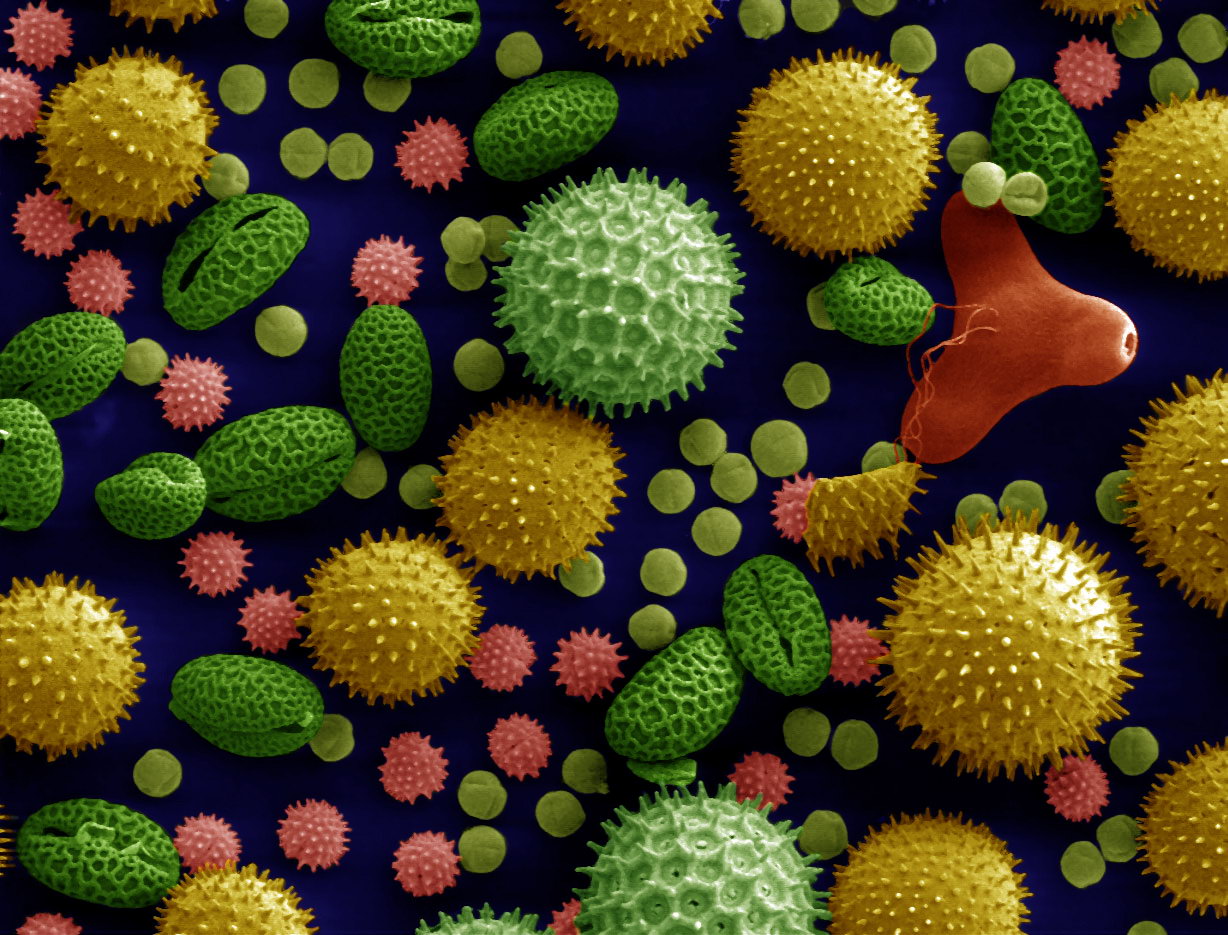
When you go outside or spend time in a place with poor indoor air quality, any dust, pollen, or particle pollution you encounter sticks to your hair, clothes, and skin. If you aren't careful when you go home or get into bed, you can scatter these harmful particles around your home, into the air, and in your sheets.
Pollen and pollution levels tend to fluctuate between seasons and even from day to day, so your risk may change depending on where you live and the time of year. The particles can get in by hitching a ride on your person or by blowing in through open windows throughout the day.
If you have COPD, these allergens and pollutants can be especially dangerous, making it difficult to breathe and triggering COPD symptom flare-ups. Because the disease makes your lungs more sensitive to even small amounts of these irritants, it's important to take steps to minimize them in your bed and in your home.
How to Know if Your Bedding is the Problem

Many people experience worsened COPD symptoms at night and in the morning because they have trouble breathing while they sleep. In many cases, changing your sleeping position, using nighttime oxygen, or getting diagnosed and treated for sleep apnea can solve this problem.
However, sometimes worsened nighttime and morning COPD symptoms is a sign that there's something in your house or bedroom that's irritating your lungs while you sleep. This can cause you to experience worsened breathlessness during the night, which can make it difficult to fall asleep and deprive you of oxygen when you do.
As a result, you may wake up congested, fatigued, and feeling like your lungs and airways are inflamed. You might notice that your COPD symptoms are worse in the mornings and get better as the day goes on.
If this happens to you, make sure you talk to your doctor to make sure that you don't need nighttime oxygen or have an underlying sleep disorder or other problem. If the problem persists, it could be a sign that your bedding is exacerbating your COPD symptoms at night.
If so, then following the tips in this article to clean and care for your bedding could make a huge difference in how you feel every day. By removing a major source of respiratory irritants, it could make a significant difference in your ability to breathe and keep your COPD symptoms under control.
If you've taken care of your bedding, talked with your doctor, and you still notice your symptoms getting worse after spending time in your bedroom or at home, the air inside your house might be polluted. It could be a sign that you need to do a deep, whole-house cleaning and maintenance check to eradicate any other hidden sources of lung irritants in your home.
Here are some of the major symptoms of exposure to indoor respiratory irritants. If you experience these symptoms when you're at home, especially if they get worse after sleeping in your bed, it could be a a strong sign that your bedding is making your COPD worse:
Symptoms of exposure to indoor irritants (e.g. mold, dust mites, and other particles in your bedding):
- Nasal congestion
- Coughing
- Wheezing
- Shortness of breath
- Sneezing
- Itchy or runny nose
- Itchy and watery eyes
- Irritated, itchy skin or rashes
How to Keep Your Bedding COPD-Safe
Clean Your Sheets Often

The best way to get rid of the bulk of allergens and respiratory irritants is to wash your sheets, blankets, and covers often. It generally takes a week or more for them to accumulate in significant amounts, so a thorough wash once a week should be sufficient.
However, if you're like most people, you probably only change your sheets every couple weeks at most, or maybe even less often. Even though most people know they should wash their sheets more, it's an easy task to forget and neglect.
If you tend to put off washing your sheets or struggle to keep up with laundry, try to carve out a specific time in your schedule every week to throw all your bedding in the wash. Just be sure to use very hot water so it sanitizes the fabric and kills any mites or mold spores.
However, comforters and duvets can be washed less often since they don't usually come into direct contact with your skin. It's usually fine to wash these heavier top blankets about once every month or so.
Get an Extra Bedding Set

It's difficult to wash your sheets, pillow cases, and blankets often if you only have one set. To reduce the hassle, invest in a second bedding set so you can simply switch them out when one needs to be cleaned.
This makes it easier to change your sheets frequently and can really come in handy when there's an unexpected mess or spill in your bed. Just make sure to store your extra set of sheets and blankets away in a cool, dry place, preferably in a sealed container or linen bag.
Avoid Materials that May Trigger Allergies
Certain types of blankets and pillows are more likely to cause respiratory symptoms than others. For example, pillows and duvets stuffed with down feathers can trigger respiratory symptoms and breathing problems in people who are sensitive to the material.
If you experience worsened breathlessness or other COPD symptoms at night, you might want to check whether or not you are allergic to any of the materials or stuffing in your bed. If any of your pillows or blankets contain down or other allergy-triggering materials, try removing and replacing them with cotton-stuffed versions to see if your symptoms improve.
However, if you've removed any potential allergy-causing materials and still feel worse at night, then it's a good sign that something else is irritating your lungs. It could also be a sign that you are particularly sensitive to dust mites and need to dust mite-proof your bed.
Purchase Mattresses and Pillows that are Resistant to Dust Mites and Other Allergens

The types of fabrics and materials used in your bedding can make a big difference in how susceptible they are to dust mites and mold. Some materials tend to attract these respiratory irritants more readily, while others are more resistant.
If you have COPD, you might consider replacing your mattress and pillows with hypo-allergenic, dust mite-resistant versions. These products are made with materials designed to keep dust mites and other hazardous, lung-irritating particles from ever getting into their fibers in the first place.
Especially if you suffer from allergies, asthma, or are sensitive to dust mites and particles, getting hypo-allergenic products could help eliminate many of the irritants that trigger COPD symptoms at night. You may find that you sleep better, breathe better, and feel better during the day when you're not breathing in inflammatory particles all throughout the night.
Many hypoallergenic pillows and mattresses are made of allergy-resistant materials like latex, bamboo, and silk. You can often find them at department stores, mattress retailers, and in many shops online.
Choose Hypo-Allergenic Sheets and Blankets
Unfortunately, putting hypo-allergenic covers on your mattress and pillows won't do anything to protect you from irritants in your blankets and sheets. Aside from regular washing, the only way to have irritant-free sheets is to get them in an allergy-proof material.
For example, silk is naturally resistant to a variety of allergens and respiratory irritants, including dust mites, mold, and mildew. Wool is another great bedding material that repels dust mites and other allergens, and it's perfect for keeping your bed warm during the cold, winter months.
If you tend to sweat or overheat at night, you should also look for fabrics that are breathable and good at wicking moisture away so your bedding doesn't get musty. Wool is fantastic at wicking away moisture and can help keep your mattress dry at night.

Here is a list of some the best hypo-allergenic and COPD-friendly bedding materials:
- Bamboo: anti-microbial and resistant to mold and mildew
- Latex: anti-microbial and anti-bacterial
- Silk: resistant to dust mites, mold, and mildew
- Wool: resistant to dust mites and great at wicking away moisture
- Down and Hypodown: naturally dust mite-repellant and lightweight (Do not use down if you have a down allergy; use synthetic down alternatives or hypodown instead.)
Protect Your Mattress and Pillows

The next best thing to buying a new, allergen-resistant mattress and pillow is getting dust mite-resistant covers for your bed. Sometimes called allergy covers or hypo-allergenic covers, they provide an extra barrier to prevent dust mites from infesting the inside of your bed.
Dust mite-resistant covers work because they use a finely-weaved fabric that's so tight that dust mites can't crawl through. This can be especially useful for preventing dust mites from proliferating in your mattress and pillows when the weather turns humid and damp.
For the best results, you should keep the cover tightly zipped on your mattress and pillows all of the time from the minute you bring them into your home. It's important to use the covers consistently, because thy will do nothing against any dust mites that take up residence in the fibers when the cover is not in place.
While some research casts doubt on the effectiveness of hypo-allergenic mattress and pillow covers, other studies show that they can reduce symptoms and complications in people with allergies and asthma. This indicates they are also effective for people with other breathing disorders, including patients with COPD.
In fact, the Lung Institute Recommends that COPD patients use zippered, dust-mite proof cases on their pillows and mattress to reduce their symptoms at home. Especially if you know that you are sensitive to dust mites, dust mite covers can be a simple and effective way to eliminate another COPD trigger from your bedroom.
Be Careful What You Track In to Bed

While cleaning your covers and replacing your pillows regularly is important, there is plenty you can do to minimize the number of hazardous particles that make it into your sheets in the first place. You can do this by being especially careful about what you track into your bedroom and what you wear when you go to bed.
The clothes you wear accumulate all sorts of particles throughout the day no matter where you go. Even if you avoid pollution and do your best to stay away from respiratory irritants, the fibers in your clothes are bound to trap a certain amount of dust, pollen, mold spores, and particle pollution.
That's why you should always remove your clothes before getting in your bed unless they're fresh, clean bedclothes that you just slipped on. Never get into bed wearing anything you've gone out in or even worn about the house.
Instead, always remove your clothes and/or change into fresh clothing before you crawl under your shets. That's the only way you can make sure that none of the hazardous particles in your clothes get transferred onto your sheets.

Here are some more tips for keeping respiratory irritants out of your bed:
- Try showering at night before bed, instead of in the morning, to remove any dust, pollen, or other particles from your skin and hair.
- If you like to wear any clothes to bed, make sure they are clean and wait to put them on until right before you get in.
- Don't allow your pets to sleep with you or get in your bed, especially under the sheets.
- Don't put clutter, dirty clothes, jackets, shoes, or other items on your bed.
Keep Your Bed and Bedding Dry

If you're sensitive to mold or dust mites, then it's important to keep your sheets, blankets, pillows, and mattress as dry as possible at all times. Damp and humid environments encourage dust mites to multiply and mold spores to grow in your sheets.
Because moldy fabrics don't usually look moldy, it can be easy to miss or underestimate. And since dust mites are invisible, you won't know if they've infested your sheets until they start triggering your COPD.
The first sign of mold growth is usually a damp, musty smell that may be very faint at first. It's a good idea to smell your blankets and sheets—or any clothing and fabrics, for that matter—for any hint of a moldy or mildewy smell before you put them on your bed.
Clean up any spills in your bed quickly and get damp spots to dry as fast as possible before mold has a chance to sprout up. Whenever you wash your blankets or sheets, make sure to put them in the dryer or hang them up to air dry immediately.
You should also avoid anything that makes your bedroom too humid, which could encourage mold and dust mites to multiply. If your shower is attached to your bedroom, make sure to close the door and run the ventilation fan or open a window to vent the humid air outside.
It should go without saying that you should dry your skin and hair off as much as possible before getting into bed, and that you should never set a damp towel on your sheets after you shower. If your hair is still damp at bedtime, wrap it up in a towel or put a thick towel over your pillow to protect it from getting wet.
If you do notice a moldy or musty smell in your bed or sheets, wash all of your bedding thoroughly with hot water and detergent to remove the mold. You can also add a cup or two of vinegar to the load during the rinse cycle to get rid of the musty smell.
For very moldy clothes or blankets, soak them in vinegar before putting them in the wash to kill most of the mold first. You can also wash your clothes with bleach or borax, although these methods can ruin or discolor fabrics if you are not careful.
Mold in your mattress can be more difficult to spot, but it can sometimes be identified by smell or by looking for spotting on the surface. If you find a small amount of mold or mildew on the surface of your mattress, you can usually take care of it by scrubbing it off with a mix of warm water and a cleaning solution like rubbing alcohol, vinegar, or bleach; just be sure to dry it off immediately after.
Laying your mattress out in a sunny spot can also help once you've removed all visible signs of mold. The sun's rays and heat will kill any leftover mold on or just under the mattress's surface.
Control the Humidity in Your Room
Many people with COPD struggle to breathe in humid weather, in part because humid air is hard on your lungs. However, many of the respiratory symptoms that COPD patients experience in high humidity could be the result of other respiratory irritants, like dust mites and mold.
That's because warm, humid weather creates ideal conditions for mold and dust mites to thrive and multiply in your home. Humidity also makes everything take longer to dry, further increasing the chances for mold growth on damp towels, sheets, and clothes.
If you live in a humid climate, or get a bout of humid weather, you should be extra diligent about inspecting your house for mold and keeping things like your clothes and sheets dry. You
Many people with COPD also struggle with anxiety. It's an understandable reaction to the daily worries and hardships of living with a chronic disease. However, for patients who don't find ways to treat their anxiety and manage it in healthy ways, that anxiety can grow to the point that it causes serious problems and affects many aspects of their lives.
One result of this chronic anxiety is panic disorder, or frequent panic attacks. A panic attack is, according to the Mayo Clinic, “a sudden episode of intense fear that triggers severe physical reactions when there is no real danger or apparent cause.”
Although they can be frightening and overwhelming, panic attacks are just that—panic. They aren't actually dangerous or life-threatening, even though they can trick your brain into thinking they are.
However, even though they are harmless in the short term, panic attacks are incredibly unpleasant to experience and can take a serious toll on your mental health. That's why treating anxiety and looking after your mental and emotional health is so important if you have COPD.
COPD patients are more prone to panic attacks for a variety of reasons, and the symptoms of COPD can make them even more difficult to manage and prevent. In this article, we're going to help you understand how panic attacks affect people with COPD and what you can do to recognize, manage, and prevent panic attacks in your own life.
What is a Panic Attack?

Panic attacks are explosive episodes of anxiety that often have no obvious cause. While they usually only last a short period of time—usually about ten minutes—those minutes can be absolutely agonizing.
In fact, the fear and physical symptoms of a panic attack are often so intense that panic attack sufferers believe they are experiencing a life-threatening problem like a heart attack. However, even though the symptoms can be terrifying, panic attacks are almost always harmless.
Panic attacks and panic disorder tend to run in families, and are often triggered by intense anxiety. They are more likely to happen after experiencing stressful or traumatic life events and changes, such as diagnosis of a chronic disease, divorce, or the death of a loved one.
Panic attacks often come suddenly and unexpectedly, and nobody knows exactly why they happen. We do know, however, that panic attacks are inextricably linked with anxiety, and, in at least some cases, are the result of chronic anxiety building up to a breaking point.
The most obvious symptoms of panic attacks include a rapid heartbeat, chest pain, shortness of breath, and intense fear. A panic attack is triggered in part by your body's fight or flight response and is meant to help you respond to real danger. However, when you suffer from anxiety, panic attacks can happen when there is no real threat of danger.
In people who have COPD, panic attacks can happen as a result of health anxiety caused by living with the chronic disease. Episodes of wheezing and shortness of breath caused by COPD can be terrifying, and it's easy to mistake panic attack symptoms for the symptoms of a COPD.
In fact, COPD patients are up to ten times more likely to suffer from panic attacks than people without the disease. And while panic attacks are generally harmless in the immediate term, they can interfere with the treatment and management of COPD symptoms and make your COPD worse if not properly treated.
Here are some of the most common symptoms of a panic attack:
- Rapid, pounding heartbeat
- Shortness of breath
- Dizziness or light-headedness
- Headache
- Nausea
- Sweating
- Chills
- Hot flashes
- Abdominal pain or cramping
- Trembling or shaking
- Tightness in the chest and throat
- Chest pain
- Feelings of dissociation or detachment
- Feelings of fear or terror
- Sense of impending doom
- Fear of death or of going crazy
- Numbness or tingling sensations
The Panic Feedback Loop

A panic attack can start unexpectedly at any time, and it is particularly frightening if you don't recognize it for what it is. Some people in the midst of a panic attack feel as though they are having a heart attack or like they are suffocating and can't breathe.
You might be driving down the road, making a sandwich, or lying in bed when a panic attack hits. They usually come with very little warning, and they can happen frequently or only on rare occassions.
As you can imagine, having COPD can make a panic attack even more frightening, since COPD is life-threatening disease that already makes it difficult to breathe. A panic attack can worsen COPD symptoms like wheezing and shortness of breath, causing even more panic as you struggle to breathe.
Because of this, many COPD patients who experience panic attacks assume that they are experiencing a medical emergency related to their COPD. It can be difficult to tell the difference between COPD symptoms and panic symptoms, which makes panic attacks harder to recognize.
This can cause a panic feedback loop, a downward spiral of anxiety, panic, and breathlessness that can make panic attacks more intense and more frequent. It's a difficult spiral to get out of, and the longer you are stuck in it, the harder it becomes to break free.
Here's what the panic feedback loop looks like:
- You start to feel anxious, fearful, and short of breath.
- When you notice those feelings, it causes you to become even more anxious.
- The increased anxiety triggers and even stronger fight-or-flight response, making the physical and emotional panic attack symptoms even worse.
- The worsened symptoms make you feel even more panicked and anxious, and the cycle continues.
When you're stuck in the panic feedback loop, the only way out is to seize back control over your body and mind. You can do this by using breathing techniques, mental techniques, and therapy to train yourself to respond to react to panic in more healthy, calming ways.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
How to Prevent Panic Attacks

At this point, you probably have a much better understanding of the mechanisms behind panic attacks and why they are so problematic for people with COPD. Now, you can build on that understanding by learning new skills and techniques to help you prevent panic attacks and manage them if they come.
Even though COPD symptoms like shortness of breath make panic attacks more likely and more difficult to control, you can still manage them effectively with the right knowledge and skills. If you can learn to recognize a panic attack when one hits, keep yourself calm and collected, and know what treatment options to seek, then you will find it much easier to manage your anxiety and your COPD.
Mind Over Matter
Panic attacks are self-feeding monsters, as we discussed with the panic feed-back loop. If you let fear and panic take over, it will only escalate your symptoms and make the panic attack even worse.
That's why slowing down and taking the time to get your thoughts back under control is one of the most important things you can do to stop a panic attack. It's difficult when you can hardly breathe and your mind is racing, but it's possible if you practice the following strategies:
Separate Yourself from Your Panic

When your heart is pounding and you feel paralyzed by fear, it is difficult to think clearly and rationally. To overcome the chaotic panic, you have to step back from it and find a way to ground yourself in reality.
It can help to remember that the emotions you feel during a panic attack are essentially irrational; they are unnecessary, out-of-proportion feelings triggered by an exhausted brain. When you're in the midst of a panic attack, remind yourself that you're not actually in danger, but simply experiencing a symptom of chronic anxiety.
It may feel like you're dying, or that your world is falling apart, but remember that the feeling is only temporary. Remind yourself that the panic will disappear soon, and even sooner if you can manage to calm yourself down.
Re-frame Your Panic

Instead of fighting against the panic, which can make you feel even more anxious and afraid, try to relax and let it wash over you instead. Remember that you have nothing to fear, that you are simply experiencing the symptoms of a panic attack, and accept the anxiety as an unavoidable symptom.
Although it might seem counter intuitive, struggling against the panic and telling yourself you need to calm down can actually make your panic attack worse. Instead, tell yourself that it's okay to feel anxious, and you will be able to help yourself feel less distressed.
Instead of thinking about the anxiety as a bad thing, re-frame it as something more positive and less scary. For example, you can use the panic attack as an opportunity to learn more about yourself and practice all the healthy coping mechanisms you've learned.
Positive Visualization

Positive visualization is a powerful tool that you can use to calm and redirect your mind away from anxiety and fear. It's basically a way to trick your brain into feeling more calm and letting go of distressing thoughts.
To practice positive visualization, all you have to do is picture yourself in a calm, pleasant, serene environment far away from unpleasant feelings and sensations. You might visualize yourself in a cozy, safe spot in front of a flickering fireplace, or relaxing in a warm, lush field far away from civilization and all of the stressors of modern life.
To be effective, your visualization needs to go beyond a simple image and should engage all of your five senses. Think about what it would actually feel like to be in your calming scene, including what you would hear, touch, smell, and taste if you were actually there.
Visualization can be as simple as taking a few minutes to sit quietly and reflect or as involved as a longer meditation session. For more information on positive visualization and instructions on how to start, you can use this comprehensive guide from the Calm Clinic.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Try the 5-4-3-2-1 Grounding Technique
Panic attacks can be overwhelming, filling your mind with so much fear that it's impossible to think clearly. It can make you feel like you are suffocating, going crazy, or like your life is in immediate danger.
In order to calm down, you need to pull your head out of the panic and convince yourself that you are safe. One way to do this is with the 5-4-3-2-1 grounding technique, a simple exercise you can use to reel in your fear and bring your mind back to the present.
Here's how you do it:
-
First you need to pause, take a deep breath, and look around you at your present environment.
-
Then, name five objects you can see in the space around you. It could be anything; a chair, a light switch, or a stain on the wall.
-
Next, name four things that you can feel or touch around you. For example, you might be able to feel your hair tickling your face, your clothes brushing your skin, or feel the smooth texture of your cell phone with your fingers.
-
Name three things that you can hear in your environment (not in your head). You might be able to hear a ticking clock, the whir of air through a vent, or the soft sound of your own breathing.
-
Name two things that you can smell. It could be a stale smell of dust in the air, the smell of your perfume or cologne, or the smell of an object in the room.
- Finally, name one thing you can taste, whether it's the neutral taste of your tongue, a strong fragrance in the air, or the remnants of the last thing you ate or drank.
The point of this exercise is to force your brain to focus on what's real instead of the fear inside your head. It can be even more effective if you name the things out loud so you can hear them audibly as recite them in your head.
By forcing yourself to acknowledge the present and the physical environment around you, it's easier to stay calm and grounded. It helps you to convince yourself that you are safe and in no immediate danger in the midst of irrational panic.
Distract Yourself from Your Panic

Finally, once you've reeled in your panic a bit and put things in perspective, you should try to take your mind off of the anxiety. Sometimes, simply distracting your brain from the physical and emotional sensations caused by the panic attack is enough to make the panic subside.
For example, try some simple mental exercises like counting up by multiples of three or reciting the alphabet backward. You can also try reciting a favorite poem, song, or bible passage to help keep your mind busy.
If you have the opportunity, you can also distract your brain with outside stimulation, such as listening to music or watching a video online. Anything that re-focuses your mind on something besides your anxiety can help you regain your sense of calm and control.
Tune in To Your Body

The earlier you can recognize a panic attack, the easier it is stop it. Sometimes you can even feel the signs before the panic hits, but recognizing those signs requires you to pay special attention to your body.
First, study the symptoms of panic attacks until you are confident that you can recognize them. Then, the next time you experience one, pay special attention to how your body feels and how the symptoms manifest for you personally.
Staying tuned in to your body and mind can help you recognize the first signs when something goes wrong. This is not only a way to recognize panic attacks, but also a good general habit to have to look after your mental health.
As soon as you recognize the warning signs or the symptoms of a panic attack, you can then begin to mentally fortify yourself against the panic. You can tell yourself that it is only a panic attack, and use mind-over-matter techniques to keep yourself calm.
Control Your Breathing
The most noticeable and frightening symptoms of panic attacks are the ones that make it difficult to breathe. Shortness of breath, hyperventilating, and light-headedness caused by a panic attack can cause you to panic even more, which only worsens the symptoms further and makes it more difficult to calm down.
This is especially true for people with COPD, who struggle with breathing difficulties on a daily basis. Patients who are already anxious about their life-threatening respiratory disease can easily fall into the panic feedback loop and get caught in the cycle of ever-escalating panic.
That's why one of the most effective things you can do when you're experiencing a panic attack is to get back control over your breathing. It's not always easy to do, but it's almost guaranteed to help you stay calm and make the panic pass sooner.
Rapid, frantic breathing sends panic signals to your brain, while breathing slow and steady signals your brain to calm down. One of the best ways to slow and control your breathing is with a technique called pursed-lips breathing, a common strategy recommended for managing breathlessness for people with COPD.
 |
| Image courtesy of hans van den berg on Flickr. |
ThePursed-Lips Breathing Technique:
-
Sit or stand up straight in a comfortable position. Relax your neck, shoulders, and chest.
-
Take a deep breath in through your nose lasting about two seconds.
-
Purse your lips, as if you were about to blow a kiss, and then breathe out slowly through your mouth for about two seconds (twice as long as the inhale).
- Repeat
Another helpful breathing technique is diaphragmic or abdominal breathing. It helps you learn to breathe with your diaphragm, rather than your chest muscles, which allows you to breathe more deeply and evenly. This not only helps with anxiety, but can also improve COPD symptoms by allowing you to breathe with less energy and strain.

The Diaphragmatic Breathing Technique:
-
Lie down flat on your back or sit in a comfortable, upright position. Keep your neck, shoulders, and chest relaxed.
-
Place one hand on your chest and one hand on your stomach so you can feel when they rise and fall. The goal of diaphragmatic breathing is to feel your stomach, but not your chest, expand and fall as you breathe in and out.
-
Next, take a deep breath in through your nose, using your diaphragm instead of your chest muscles. You should feel the hand on your stomach rise while the hand on your chest stays still.
- Finally, breathe out slowly through your mouth. You should feel the hand on your stomach fall while the hand on your chest doesn't move at all.
- Repeat for several minutes.
Even though it is hard to think straight when you're in the midst of a panic attack, try to remember these simple, easy breathing exercises to help you stay calm. It can help to purposefully practice pursed-lips and diaphragmatic breathing when you're not anxious, that way it will be easier to remember how to do it when you feel panicked.
Do a Relaxing Activity

When you're experiencing a panic attack, it can be difficult to think about anything besides the frightening symptoms and the terror that's taken over your body. But sometimes, giving yourself a positive physical sensation or activity to focus on can take your mind away from your anxiety.
Simple, relaxing activities like reading, doodling, watching a favorite TV show, or coloring in a coloring book help give your hands and your mind something else to do besides focusing on the panic attack. You can also try activities that are tactile or give you a pleasant physical sensation, such as taking a warm shower, wrapping yourself in a soft blanket, or curling up with a hot cup of tea or hot chocolate.
Think Twice About Using Your Bronchodilator Medication
![]()
When you are having trouble breathing during a panic attack, it can be tempting to reach for your inhaler like you do when your COPD symptoms flare up. However, since the breathlessness is caused by panic, not COPD, your bronchodilator is unlikely to be much help.
In fact, bronchodilators act like stimulants and can make the panicked feeling more intense. They can end up increasing your heart rate, cause trembling and shaking, and make you feel even more anxious than you did before.
That's why it's important to learn other calming techniques to help you cope with the symptoms of panic attacks. Try using breathing techniques, meditation, or other relaxation techniques to bring your breathing back under control.
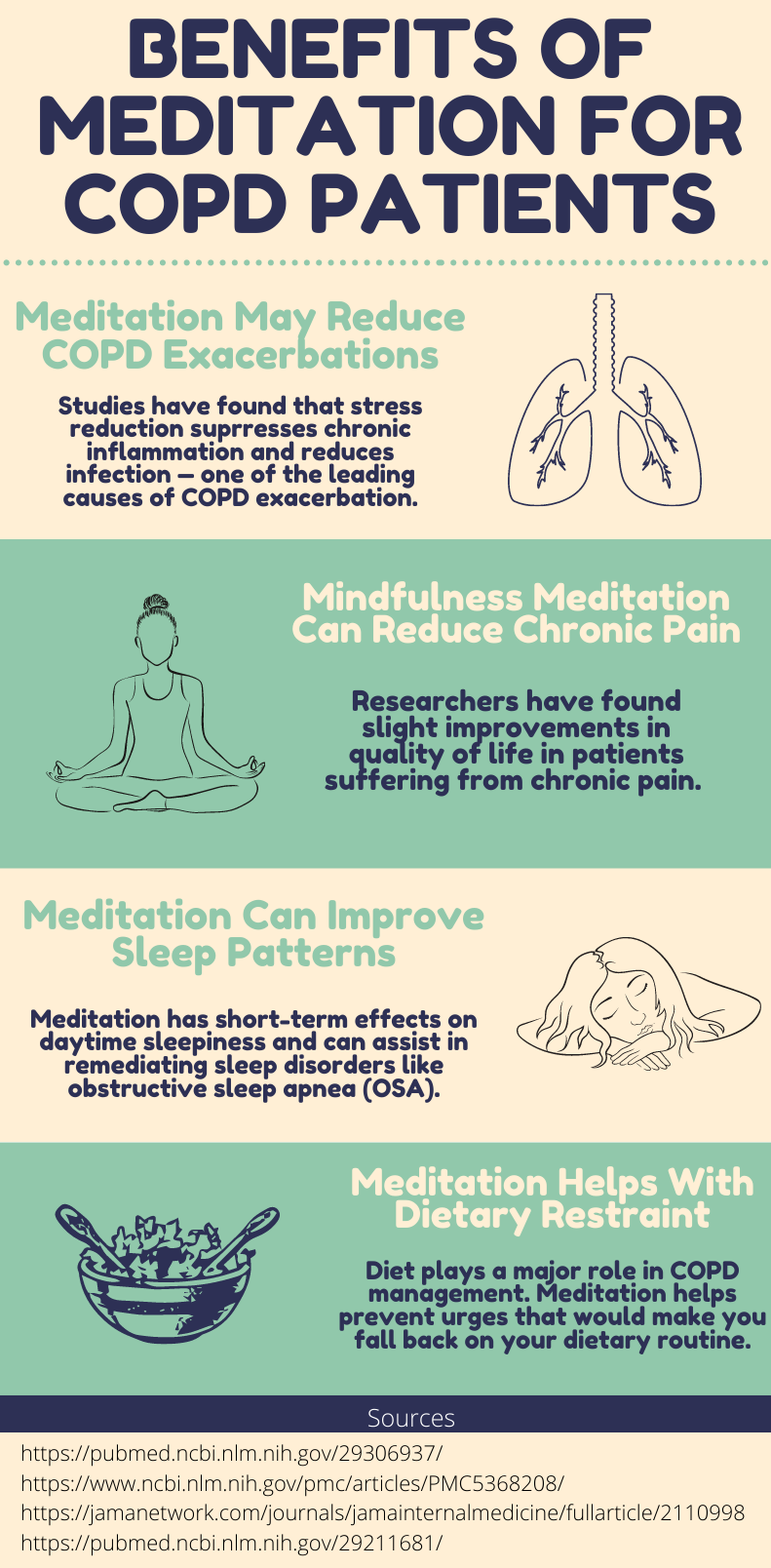
Mindfulness Meditation

Mindfulness meditation is a kind of mental exercise that helps you let go of worry and focus on the present. It's a technique that's highly regarded in the mental health field and is a common treatment recommended to people struggling with anxiety.
To practice mindfulness, you simply sit quietly for a set period of time and try to keep your mind calm and focused on the present moment. Try not to think any conscious thoughts, and let any worries or negative thoughts wash over you like water.
Mindfulness coaches often suggest focusing on your breathing and your body sensations as a way to keep your brain focused on the here and now, instead of what's going on in your head. It's a great way to learn how to stay calm when panic attacks strike and to cope with general breathing problems caused by COPD.
It's often easiest to begin practicing mindfulness meditation by following along with a written or audio-based guide. The University of California, Los Angeles has several free guided meditation audio classes you can use, or you can use the written guide at mindful.org that contains loads of useful tips and advice for getting started.
Seek Emotional Support

When you're in the midst of a panic attack, it can be extremely difficult to think straight, let alone calm yourself down. That's why it can help to call a close friend or family member for support.
It can help to tell your confidant ahead of time about your panic attacks and what they can do to help. Sometimes, just having someone there to ground you in reality and assure you that everything will be okay is enough to make a difference.
In fact, it helps to have someone you can go to for support anytime you feel anxious or depressed, even if it's not a full-blown panic attack. Having someone you can trust and talk to about your feelings is a wonderful form of therapy, and it can help you to begin healing your anxiety, which is the root cause behind most panic attacks.
Another great way to get emotional support is to join a support group for people with anxiety or people with COPD. Group therapy sessions are an opportunity to share your worries, struggles, and successes while learning from others who are facing similar har
Happy Winter Solstice! But for many it is not a “happy” time of year. The winter blues, winter funk, or seasonal affective disorder— Doesn’t matter what you call it, it can be debilitating.
So, while the days in the northern hemisphere are starting to get longer again, there is still a long winter ahead for those of us that live in cold states!
![]()
Colder and dark days mean many Americans are beginning to feel the effects of seasonal affective disorder (SAD), and on top of winter, is the ever present pandemic!
SAD can make it more difficult to manage COVID-19 anxiety, and if you also suffer from respiratory diseases including but not limited to COPD (chronic obstructive pulmonary disease), pulmonary fibrosis, pneumonia, severe asthma attack, cystic fibrosis this seasonal depression, the cold weather, the pandemic— it is all piling up.

We created this guide that will give you several coping mechanisms designed to ease symptoms of seasonal affective disorder, COVID-19 anxiety, and respiratory disease.
What is SAD? Do I Have It?
![]()
SAD is a type of depression that is brought on by cold temperatures during the fall and winter months. People tend to go outside less frequently which leads to vitamin D deficiency resulting in mood changes and other symptoms of depression.
Here are some of the basic feelings of depression however this can look different from person to person. During these episodes, symptoms occur most of the day, nearly every day and may include:
- Feelings of sadness, tearfulness, emptiness or hopelessness
- Angry outbursts, irritability or frustration, even over small matters
- Loss of interest or pleasure in most or all normal activities
- Sleep disturbances
- Tiredness and lack of energy
- Reduced appetite and weight loss
- Increased cravings for food and weight gain
- Anxiety, agitation or restlessness
- Slowed thinking, speaking or body movements
- Feelings of worthlessness or guilt, fixating on past failures or self-blame
- Trouble thinking, concentrating, making decisions and remembering things
- Frequent or recurrent thoughts of death, suicidal thoughts, suicide attempts or suicide
- Unexplained physical problems, such as back pain or headaches
Mental disorders like anxiety and depression often coincide, these mental disorders are the most common mental illness in the U.S., affecting 40 million adults in the United States.
SAD is categorized differently than depression and anxiety, while the symptoms are very similar, the reason in which you experience these feelings are rooted in the change of seasons. It is important to distinguish the difference between the two.
When distinguishing between a diagnosis of depression and depression with a seasonal pattern, it all comes down to timing!

A person suffering from major depressive disorder with a seasonal pattern would experience the common symptoms listed above common in winter months as opposed to the rest of the year.
Being diagnosed with depression with seasonal pattern or SAD, you would have to experience:
- At least two years of symptoms that become worse during a specific time of the year
- The seasonal depressive episodes must significantly outweigh the nonseasonal episodes
If you are diagnosed with SAD it is likely you will be treated similarly with the same approach to someone who experiences depression. Therapy and the use of anti-depressant medications are commonly prescribed for someone with depression, whether seasonal or not.

It is recommended that people with SAD shouldn’t not go untreated nor wait out the depressive episode until the end of the season.
It's a harmful mentality that someone can endure a depressive episode for a period of several weeks during the winter months. Basic human functions will steadily decline and there is no good reason not to seek professional help to learn helpful skills for a more enjoyable life all year around.
SAD and COVID-19

SAD and COVID-19 are a recipe for depressive episodes and increased anxiety.
As we roll into another pandemic winter, the ever present seasonal affective disorder is being compounded by COVID-19 anxiety for many Americans.
Most Americans are still processing traumatic experiences from the events of the past year and a half, whether you have suffered the loss of a loved one or had a hard time coping with isolation and quarantine, the world in a pandemic can be a cruel and unruly place.
In comparison the United States is in a much better position than last winter with the COVID-19 vaccine availability and current rollout of booster shots, however, the uncertainty of how the pandemic will continue to effect us can make the mental distress persist.

In a vicious cycle, SAD can make it even more difficult to cope with COVID-19 anxiety, and treating SAD can seem impossible under COVID-19 pressures.
Here are some ways to manage both issues simultaneously.
Managing SAD and COVID-19 Anxiety
If you’re feeling the double trouble of seasonal affective disorder and pandemic anxiety, experts recommend the following coping mechanisms that can help ease symptoms of both.
Maintain a routine
It sounds simple but having a semblance of a daily routine is very important, especially when things seem overwhelming. Having a few daily tasks to come back to when you feel overwhelmed gives you a sense of accomplishment.
Write down some small achievable goals to work towards each day. It is common to immediately feel like you're drowning in responsibilities, so begin your day by crossing goals off of your list. This can make a big difference in your attitude moving forward.
One goal you can make is to “make your bed” every morning. Once you’ve done that, acknowledge your accomplishment and continue moving through your day!
Another goal can be to take 10 minutes out of every morning for deep breathing and stretching. Simply checking tasks off of a list can go a long way in reassuring yourself that you are capable.
Try light therapy

Phototherapy, or light therapy, is a recommended treatment for seasonal affective disorder. It involves sitting or working near a light therapy box, which mimics natural outdoor light.
Sunlight is the best source of vitamin D, finding other ways to source this crucial vitamin is essential for your mood and mental health. You can do it with light therapy, foods you eat that are high in vitamin D, and supplements if your doctor approves.
Get moving
![]()
Physical activity can improve mental health and overall well-being. Remember that exercise doesn’t have to mean going to the gym or taking a fitness class, just a little physical activity like taking a walk, doing some exercise at home, using a quick YouTube workout video — is all beneficial!
Find your community
Unfortunately the pandemic is making it challenging to connect with people in person safely but you can still surround yourself virtually by people who support you, inspire you, or are just fun to talk online and over the phone.
Look for Facebook Groups or online forums. People are often posting their vulnerabilities to share and connect with others who have similar experiences to you!
Bottling up your emotions is very unhealthy. Use your social circle for support. Sharing how you are feeling with your loved ones can help you, as well as help them, understand what you are going through!
Practice meditation

A proven way to help ease symptoms of depression and anxiety is meditation. The power or mindfulness should not be underestimated, especially when talking about SAD and COVID-19 anxiety. Medications encourage people to slow down their thoughts and breathe deeply.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Medication sounds easy, but to remain still, breathe, and trying to stay present is harder than it sounds, but as with anything, it just takes a little practice. Start with small goals and understand that medication is not an attempt to turn off your thoughts, but a way to slow down your thoughts and to be aware of your surrounding thoughts so you are more in control of them.
There are a lot of new apps you can download on your smartphone or tablet that will help you get into the practice of mediation!
Create a bucket list
Think about something you enjoy doing, it could be anything, write it down in a journal and make this your new bucket list! Having plans for enjoyable activities can help ease day-to-day stresses.
This could include doing a wine tasting from home, getting around to reading a new book, creating a weekly movie and dinner night, or starting a new hobby that sounds fun.
![]()
Beyond these everyday activities and practices to help you ease SAD and COVID-19 anxiety, there are more drastic measures you can take.
Managing episodes of anxiety and depression is possible with support, however some people do require professional help, and that is ok!
Seek professional help

It is very common that people with SAD and anxiety seek a mental health professional and have very positive experiences in doing so! Even if you did not need a to see a therapist before, the pandemic could have shifted a lot for you mentally, and it is never too late to adjust to these changes with the help of a mental health professional.
63 percent of people previously diagnosed with depression and anxiety reported their associated symptoms were “worse” or “much worse” during the COVID-19 pandemic than they were before.
Affording Treatment or Medication

Roughly 20% of people that responded to a GoodRx survey noted that they couldn't afford their medication during the pandemic. Also, 37 percent of respondents reported at least one issue related to administration of their medication, including missing, skipping, or rationing prescriptions; changing pharmacies; or having issues with a pharmacy refilling their prescription.
If you’re unable to afford your anxiety or depression medications, consider the following.
Shop around and look for coupons

Take the time to research different pharmacies around you, prices vary depending on where you pick up your prescriptions.
Contact the pharmaceutical company that makes your medication to ask for coupons or price reduction promo codes. Pharmaceutical companies also offer patient assistance programs to help people that are struggling to afford their medications.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Request a 90-day supply
Ask your doctor to write a prescription for a 3-month supply rather than a monthly supply. Paying more upfront for your medication may reduce the total cost of the prescription.
Anxiety and Depression Due to Respiratory Illness
![]()
On top of all of the covid-19 anxiety and SAD, if you also suffer from a common respiratory disease, you are not alone!
Nearly 37 million Americans live with a chronic lung disease like asthma and COPD, which includes emphysema and chronic bronchitis.
If you require supplemental oxygen therapy, LPT Medical can help you ease the burden of dealing with heavy and cumbersome oxygen tanks. We have a wonderful selection of the newest and most reliable portable oxygen concentrators on the market!

Having a lightweight portable oxygen device can change your way of life by creating opportunities for you to be more independent! Oxygen therapy can be a stressful and invasive form of therapy, so having a device that is compact in size, runs on battery power, makes oxygen therapy more doable!
Adhering to the prescription your doctor gives to you is important to ensure you treat the hypoxia caused by respiratory illness. When your oxygen levels are too low, your mood and mental health can suffer.

Here at LPT Medical, we are continually working to reduce the burden of living with lung disease by offering oxygen therapy products and oxygen therapy accessories that you can rely on for years.
Overview
These next few months will be cold and dark, that doesn’t mean you have to live in a constant state of depression. Seek help and treatment for SAD. Small everyday tasks can bring joy back into your life.

If you are also struggling with COVID-19 anxiety and the pressure of dealing with and managing a respiratory disease, don’t give up. There are social circles available to you online that can help you cope with the very natural feeling you are having.
There is light at the end of the tunnel, seasons will come and go, it is our hope that you consider some of the information within this blog to help you cope with the challenges of winter, COVID, and chronic respiratory disease.
If you have COPD, then you know that your lungs are particularly sensitive to the environment and the quality of the air you breathe. Even minor irritants like dust, smog, or cold air can worsen your symptoms and make it even more difficult to breathe.
The cold weather and harsh, dry air is irritating to anyone's respiratory system, but it can cause debilitating symptoms for people with weakened and sensitive lungs. That's why the winter months tend to be particularly challenging for people with COPD.
Cold weather and COPD has been a topic of interest to researchers for some time, and many studies have proven that winter weather can significantly worsen COPD symptoms. In fact, studies show a very strong link between extended periods of cold weather and increased hospitalizations for people with COPD.
Because of this, doctors and health organizations like the Lung Institute urge people with COPD and other respiratory conditions to be especially cautious in cold weather. It's important to protect yourself and prepare yourself for the winter to prevent dangerous and even deadly COPD exacerbations.
If you're heading into the winter months and want to know how the weather will affect your COPD, then this article is for you. In the following sections, we'll help you understand why cold weather tends to make COPD worse and give you a variety of tips to help you better manage your disease this winter.
How Cold Weather Affects Your Respiratory System

Although most people have experienced coughing or inflamed airways in cold weather, it's easy to underestimate how severely the cold air can affect your respiratory tract. According to the Lung Institute, cold air can have an “extreme” effect on your lungs and “cause dramatic changes to the respiratory system.”
One of the most immediately noticeable changes is narrowed airways that restrict airflow and make it difficult to breathe. This can be dangerous for people with severe COPD and trigger bouts of serious breathlessness, coughing, and wheezing.
Another way cold weather affects your body is by triggering a sudden increase in breathing rate followed by a sudden drop in breathing rate when you get cold. This effect is a major cause of cold-related deaths in the elderly and can happen even when the weather is only mildly cold, in temperatures as high as forty degrees Fahrenheit.
Another effect of cold weather is an increase in blood pressure, which is hard on your heart and lungs. This happens when extremely cold air causes your blood vessels to narrow, which forces your heart to work harder to circulate blood and oxygen throughout your body.

In most healthy people, these changes only cause minor symptoms and discomfort. But for people with COPD and other serious conditions, these respiratory changes that happen in response to cold air can cause serious problems and even be life-threatening.
However, it's not just the temperature that causes increased respiratory strain in the winter. Cold air also happens to be drier than warm air because it can't hold as much moisture. This can cause humidity to drop far below the ideal level.
Dry air is generally more difficult to breathe, especially for people with COPD and other respiratory conditions that make their airways sensitive to irritation. Cold air dries out and irritates your airways, causing airway constriction and inflammation that makes it difficult to breathe.
Cold, dry air also tends to increase mucus production, which can worsen coughing and breathlessness in people with COPD. The density of the air also plays a role; cold air is denser than warm air, which means cold air creates more resistance in your airways and makes it harder to breathe.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Other Winter Hazards

Another major problem many COPD patients have during the winter is getting enough physical activity. Having to stay indoors can disrupt your usual exercise routine and make it easy to get out of the habit of being active.
The wintertime is also the peak season for colds, the flu, and other contagious illnesses. Cold weather is also a friendly environment for bacteria that cause respiratory infections and exacerbations.
Since most COPD exacerbations are caused by contagious illnesses and infections, it's particularly important for people with the disease to avoid getting sick. Combined with all the other complications that cold air can cause, contracting any kind of respiratory illness puts you at an extremely elevated risk for serious and even life-threatening exacerbations.
But even though the wintertime can be dangerous for people with COPD, there are plenty of things you can do to protect yourself and your lungs from the hazards of the cold air. There's no reason to worry if you prepare and take the right precautions.
In the next sections we'll show you all the steps you can take this winter season to stay healthy and keep your COPD symptoms under control. Continue reading for a plethora of practical tips and advice for staying warm, breathing easier, and avoiding worsened symptoms and exacerbations this year.
How to Protect Yourself from Cold Weather
Breathing Techniques for Cold Weather

If you have COPD, you've probably noticed that it's harder to control your breathing when the weather is cold. All it takes is a sudden breath of cold air to shock your respiratory system and cause you to lose your breath.
This makes it more difficult for people with COPD to breathe normally and catch their breath in the cold winter air. However, if you practice proper breathing techniques you can reduce the shock of the cold air on your lungs and get your breathlessness under control.
The pursed lips breathing technique is recommended for any situation when you find it difficult to breathe, but it can be particularly helpful in the cold. The technique is simple: make sure you breathe in through your nose for a couple of seconds count, and then exhale slowly for twice as many seconds while pursing your lips together (as if you were blowing a kiss).
Breathing in through your nose protects your lungs because it gives the cold air time to warm up slightly and absorb moisture it as it travels through your nasal passages. If you breathe in through your mouth, the cold, dry air goes straight to your lungs and causes much more irritation.
It's a good idea to practice the pursed lips breathing technique at home when you have full control of your breathing and your symptoms aren't acting up. That way it will feel more natural when you use it in a breathing crisis, and it will be easier to get your breathing back under control.
There are a variety of other breathing techniques you can use to control your breathing whenever cold air or anything else triggers a bout of breathlessness or coughing. Visit The Lung Institute here to learn more about effective breathing exercises and techniques.
Cover Up Your Nose and Mouth

If you have to be out in the cold, there are a couple of things you can do to make the air you breathe less harsh. In addition to wearing warm clothes and a coat, you can also wrap a scarf around your nose and mouth.
This warms up the air before it reaches your nostrils and is a great way to protect your lungs and make the harsh air easier to breathe. Wearing a scarf over your face also traps the moisture from your breath, which helps humidify the air slightly before you breathe it in.
Another option is to get a cold-weather mask, like a CT Mask, designed for people with respiratory illnesses like COPD. Like a scarf, CT masks trap the warmth and moisture from your breath when you exhale in order to warm and humidify the next breath of air you breathe in.
CT masks are reusable, washable, and made from soft, flexible materials for comfort. Although more pricey than a scarf, CT masks are often more comfortable, more effective, and more convenient for keeping your lungs warm when you go outside.
Cover Your Oxygen Tank and Tubing
If you use supplemental oxygen, you have to consider how to keep your oxygen warm when you go out and about in the winter. If the air in your oxygen tank or the tubing gets too cold it can be uncomfortable and difficult to breathe.
If you take your oxygen supply with you out in the cold weather, make sure to insulate the tank and tubing from the cold air. You can do this by keeping your portable oxygen tank in an insulated bag or case that protects it from the cold air and elements.
Another option—better for shorter jaunts—is to hold the tank under your coat so your body heat keeps it warm. Whatever you do, you should always try to keep your tubing secured under your coat or jacket so it doesn't cool down the oxygen coming from your tank.
Avoid Sick People and Crowded Places

When you have COPD, you are particularly susceptible to respiratory illnesses and even minor infections can be devastating to your health. That means you have to be especially careful to avoid germs and stay away from people who are sick.
It's best to avoid extremely crowded places and events during the winter when colds, the flu, and other respiratory illnesses are at their peak. When you do go to public places, make sure to wash your hands often and use hand sanitizer when needed.
Avoid touching your nose, mouth, or any part of your face when you're out in public unless you wash your hands first. That way you don't infect yourself with germs picked up from all the surfaces you've touched.
Keep Your Medications Handy

When the weather is cold and the air is dry, you're likely to experience more severe symptoms than usual. That means you will probably need to use your inhaler and other medications more often during the winter months.
You should always bring your inhaler, supplemental oxygen (if you use it), and any prescribed quick-relief medications with you, especially if you will be spending any amount of time outdoors. That way you'll have everything you need to get your symptoms back under control if the cold air starts to bother you.
You might even find that your usual prescription medications and therapies aren't enough to control your symptoms during long periods of cold weather. If this is the case, you should talk to your doctor right away so he can adjust your prescriptions or treatment plan to better manage your symptoms.
Watch Air Quality Forecasts

Extreme temperatures, both hot and cold, tend to worsen air quality. Because of this, air pollution is a major culprit behind increased COPD symptoms in the winter.
This is partly because people tend to generate more pollution in the winter by using fireplaces, wood-burning stoves, and leaving their cars running idle. But another cause of poor winter air quality is the cold air itself, which tends to trap smog and other particulates close to the ground instead of letting them disperse into the atmosphere.
If you have COPD, you should always avoid spending time outdoors when the air quality is poor, no matter the time of year. You can check your local air quality forecast daily at airnow.gov and plan your outings and activities for days when the air quality is good.
If you don't already know how, it's important to learn how to interpret air quality warnings and how they apply to COPD. For example, “moderate” quality air is considered acceptable for healthy individuals to breathe but can be harmful to people with COPD, especially in the latter stages of the disease.
Don't Neglect Indoor Air Quality

While it's a good idea to stay indoors on days when the outdoor air quality is poor, it won't do you much good if your indoor air is polluted, too. Many people don't realize that indoor allergens and pollutants can actually get worse in the winter and exacerbate your COPD symptoms.
For example, many appliances utilize combustion and can emit harmful fumes into your home. Many of these, including fireplaces, stoves, water heaters, and dryers, tend to be used more often in the winter months, too. It's important to make sure all of your appliances are well-ventilated and working properly to minimize the amount of pollution they leak into your home.
The winter months also coincide with holidays like Halloween and Christmas, which usually means digging for seasonal clothes and decorations. This often involves moving old boxes in your attic or basement and digging in the back of your closets. Unfortunately, moving around items in storage tends to unleash dust and other allergens from their resting place, which can hurt your indoor air quality and make COPD symptoms worse.
Since there are fewer opportunities to open the windows and air out your house in the winter, it's important to be especially vigilant about cleaning up dust, removing mold, and changing the air filters in your house's ventilation system. These are simple steps, but they can make a huge difference in the air quality in your home and how you feel.
Extra Tips for Staying Warm in the Cold

If you have COPD, keeping out of the cold should be a top priority in the winter. However, you can't always stay indoors, so you should be prepared to bundle up and protect yourself from the cold weather when it can't be avoided.
Dressing for the cold weather might seem like a no-brainer, but it's something you should really think about if you have COPD. The disease makes your body particularly susceptible to dangerous cold-weather reactions like increased blood pressure and irregular breathing. This is why it's so very important to keep your body warm
If you do have to go out on cold days, you should always take extra time to make sure you have everything you need to stay warm. You should check the temperature forecast daily and make sure to take wind chill, precipitation, and other weather conditions into consideration.
You should also never forget to bring your inhaler or rescue medications with you in case your symptoms get much worse in the cold. Here are some more general tips and techniques you can use stay warm and protect your lungs this winter:
-
Dress in layers so you can always adjust to different temperatures. You can simply add an extra jacket or sweater if you get cold, and if you get too hot later, all you have to do is remove a layer.
-
Wear long-sleeved undershirts, long underwear, or leggings for an extra under-layer in extremely cold weather.
-
Don't forget about other pieces of important winter outerwear like scarves, hats, and gloves. It's also a good idea to keep an extra set of gloves in your car or handbag in case you forget when you leave the house.
-
Always check your local weather forecast and plan around harsh weather and temperatures. Make sure to take humidity, air pollution, and wind chill into consideration too.
-
Always cover and insulate your oxygen tank and tubing in cold weather.
- Consider wearing a CT mask or other cold weather mask to warm up the air as you breathe.
Stay Hydrated

Cold, dry air tends to irritate your airways and thicken the mucus in your lungs. Both of these things lead to increased coughing and breathlessness, especially for people with COPD.
One of the ways to combat this is to drink extra water during the winter. Dehydration thickens mucus and makes COPD symptoms worse, while proper hydration keeps your airways moist and your mucus thin. This it much less likely that phlegm will obstruct your breathing or trigger a coughing fit, and makes it much easier to get mucus out with controlled coughing techniques.
You should always drink at least 6-8 glasses of water per day to stay hydrated, possibly more if you exercise. If you tend to forget, it helps to keep a couple of re-usable water bottles filled in places around your house. Keep a filled bottle in key, noticeable places like your fridge, living room, and nightstand for convenience.
Staying Active During the Winter
One indirect yet dangerous effect of cold weather on COPD is that it makes it more difficult to get enough physical activity. It's not just because the cold air makes breathing during exercise more difficult, but also because it often means staying indoors and giving up outdoor activities that help you stay active.
However, if you have COPD then you know that exercising is one of the healthiest, most important things you can do to treat your disease. It can improve your lung function, strengthen your breathing muscles, reduce COPD symptoms like coughing and breathlessness, and even slow down the progression of your disease.
Because of this, most doctors recommend getting as much exercise as you can, and that includes during the winter months. Even though the cold weather makes physical activity more difficult, it's still just as important for your health to find ways to stay active.
In this next section, we're going to help you out by showing you a variety of convenient ways you can stay active this winter. We'll and show you a variety of indoor activities and exercises you can do to avoid the cold weather and give you tips for handling the cold air when you can't avoid it.
Join a Gym

The gym is an obvious option for getting physical activity during the winter. Even if you don't go to a gym any other time of the year, it might be your best option when the weather is too cold to exercise outside.
Nearly all gyms have treadmills, exercise bicycles, stair steppers, and other machines for light to moderate aerobic activities. Some even have indoor tracks for a more natural walking or jogging experience.
Gyms also give you access to a variety of weights and strength training machines that you can use to build muscle more easily. Weight machines are often easier for less experienced people and those with limited mobility to use.
Gyms also have employees on hand that can teach you how to use the equipment and help you with any questions you have. Some gyms even host group exercise classes you can join, although you often have to pay an extra fee.
Find Alternative Places to Walk

Many people with COPD use walking as a primary source of exercise. It's a popular way for people with respiratory illnesses to stay active and is often recommended by doctors for being low-impact, effective, and less likely than many other exercises to make you feel out of breath.
Unfortunately, the cold winter weather makes it unpleasant, and even dangerous, to exercise outside if you have COPD. If you usually like to stroll around your neighborhood or an outdoor park, you'll have to find another way to get that exercise indoors, instead.
One of the most obvious and popular options for indoor walking is to join a gym. However, treadmills, indoor tracks, and monthly membership fees aren't for everyone. As an alternative, you can look for large, public buildings that have plenty of room to walk around.
Walking laps around an indoor shopping mall, for example, is a great option for exercising when it's too cold to walk outside. There are plenty of long, flat hallways to stroll down and plenty of interesting things and people to look at to stave off boredome.
You can also bring along a friend or two to make your indoor walks more fun. Some malls even have community walking groups or stay open after-hours to promote public walking indoors.
Other places that often have enough floor-space for walking include large community centers, department stores, and warehouse stores like Ikea. These places are generally open to the public most of the day and have plenty of space for walking laps.
When all else fails, you can get in your daily steps in by walking around your own home, instead. If you have enough space, you can do laps through the halls and climb up and down stairs for exercise. You can also walk or jog in place while listening to music or watching your favorite TV show.
Invest in a Pedometer

If you're used to walking outdoors during the warmer months, you probably measured your progress based on the distance of your walking route. But when you're forced to change your routine in the winter and move your walking indoors, it can be much more difficult to estimate how much exercise you got.
That's why you should consider getting a pedometer to help you keep track of how much walking you do this winter. That way, if you walk laps around your home, local mall, or another indoor place you can always know exactly how far and how many steps you walk. It's a great way to track your steps if you walk in place, too.
But pedometers aren't just for tracking your steps; they're a fantastic tool for motivation, too. Using a pedometer to track your progress helps you set goals, celebrate improvements, and challenge yourself to get in as many steps as you can every day.
Try At-Home Strength Training Exercises

Strength training is very important for people with COPD because it helps you build muscle and exercise endurance. In fact, many COPD patients who have trouble exercising say that muscle weakness and soreness holds them back even more than breathing difficulties do.
If the winter weather is disrupting your exercise routine or making it difficult to go to the gym, there are plenty of options for exercising at home. You don't even need weights or special equipment in order to tone and build strength, although a small set of light free-weights can make it easier build muscle and open up even more options and exercise techniques.
Many exercises you can do in your home are simple and take minimal equipment. All you have to do is clear out a space large enough to move around in and you can begin practicing a variety of strength training exercises right away.
To learn more, visit our previous article on how to effectively exercise at home here. It will teach you about a variety of different strength training exercises and other physical activities you can do without ever having to set foot outside.
Get Into Stretching

As a respiratory disease, COPD comes with many symptoms, but the most serious and uncomfortable of these symptoms is difficulty breathing. These breathing problems have a variety of interconnected causes, including airway obstruction, reduced lung function, and a reduced capacity for exercise that are all caused by COPD.
In fact, almost every COPD treatment is, ultimately, aimed at managing your breathing. Bronchodilator medications, supplemental oxygen, and even diet and exercise regimens are all meant to help relieve airway obstruction and help you breathe as efficiently as possible.
But there's another type of COPD treatment that is invaluable for managing COPD symptoms and keeping your breathing under control: practicing breathing exercises. You've probably heard about breathing exercises from your doctor, but you might not yet understand how handy and effective they can be.
Breathing exercises are perhaps the most convenient and useful techniques that any COPD patient could add to their toolbox. They're absolutely safe, surprisingly effective, simple enough for anyone to learn quickly, and one hundred percent cost-free.
In this article, we're going to teach you about all of the breathing techniques that doctors and researchers recommend for people with COPD. We'll not only introduce you to the most effective breathing exercises and teach you how to practice them but also help you understand how they work and what the best times are to use them.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Breathing Exercises for COPD

One thing that makes breathing exercises such a valuable treatment option is the fact that you can use them anytime and anywhere as long as you remember the steps. So, if you'd like to add some new techniques to your COPD treatment tool set, continue reading to learn how to use several different breathing exercises to help you breathe easier and better manage your COPD symptoms.
The Stop, Reset, and Continue Technique

When you have trouble breathing it can be a very scary experience. However, if you let yourself become too anxious or distracted by worry, it will make it even harder for you to catch your breath.
Once breathlessness starts, it can easily cascade out of control, becoming worse and worse if you don't manage it quickly. That's when you need to stake a step back, pause, and regroup so that you can begin using proven strategies to get your breathing back under control.
Simply worrying about feeling breathless can even trigger a bout of breathlessness or hyperventilation on its own, especially if you suffer from chronic anxiety or panic disorder. Whatever the cause of your breathlessness, it's important to keep a level head whenever the symptom strikes.
That's why the "stop, reset, continue" technique is such a valuable tool for any person who has COPD. It helps you stay calm, re-focus, and then begin steadying your breathing until it returns to normal.
Here is how you practice the stop, reset, and continue technique:
-
Stop whatever activity you are doing and sit or lie down whenever you start to feel short of breath.
-
Reset your breathing by relaxing the muscles in your shoulders and chest and practicing a breathing exercise (such as pursed lips breathing, which we'll discuss in the next section below) until you are able to catch your breath.
- Continue whatever activity you were doing before, at a slower pace if necessary, while continuing to consciously control your breathing.

You can use this technique if you get breathless from physical activities like walking, exercising, or doing chores around the house. It can also work when you feel short of breath for other reasons, such as when you experience an exacerbation or when your symptoms flare up because of exposure to allergens, pollution, temperature extremes, and other respiratory irritants.
The "stop, reset, continue" method works because it keeps you in clear-headed command of your thoughts and your breathing. It helps cut through anxiety, reminds you not to panic, and allows you to concentrate on practicing breathing exercises and other treatments that can help you recover.
This may seem like a simple technique, but it can be surprisingly effective in the moment. The next time you have trouble catching your breath, just repeat the simple steps "stop, reset, and continue" to remind yourself that you have the ability to bring your breathing back under control.
As you do your breathing exercises, you might need to remind yourself to stop, reset, and continue multiple times as you lose control or focus. Reset as many times as you need until your get your symptoms under control.
When you feel short of breath, you should also use your quick-relief medications--such as your bronchodilator, supplemental oxygen, or inhaled corticosteroids--as directed by your doctor. Using these in combination with breathing exercises can be more effective than just practicing breathing exercises alone.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Pursed Lips Breathing
Pursed lips breathing is the number one, staple breathing technique that everyone with COPD should know how to use. It's probably the most simple, effective, and versatile method for preventing and treating breathlessness caused by COPD.
If you don't have this method memorized yet, then now is the time to learn it by heart. Once you have the basic steps down, you can use pursed lips breathing to aid you in a multitude of situations and circumstances.
That's because pursed lips breathing isn't just something you use when you feel breathless to get your breathing back under control. It's also a technique for preventing breathlessness when you exert yourself and helping you breathe easier in any situation.
Research shows that using pursed lips breathing helps open up your airways, reduces airflow resistance, and uses less effort and energy to breathe. It also makes your breaths easier to control when you exercise or when you experience a flare-up that makes your symptoms worse, which can prevent breathlessness from ever occurring in the first place.
One study showed that COPD patients who practiced pursed-lips breathing while exercising had increased exercise endurance and were able to take in more oxygen as they worked out. Pursed-lips breathing also helped steady patients' breathing rates, reduced rapid breathing, and even increased the levels of oxygen in their blood.
Pursed lips breathing can be particularly helpful for people with emphysema, who often have trapped air in their lungs that makes it difficult to breathe. Pursed lips breathing helps push the trapped air out, allowing you to take deeper breaths and absorb more oxygen every time you inhale.
How to Practice Pursed Lips Breathing
Pursed lips breathing is simple to learn and easy to do, but that doesn't mean you don't need to practice. You should take the time to practice pursed lips breathing every day until it becomes second nature. To do that, you need to concentrate on the steps and the process, not just go through the motions.
Here is how you perform the pursed lips breathing technique:
-
Lie down or sit upright in a chair and relax the muscles in your shoulders and chest.
-
Take a slow, deep breath in through your nose (not your mouth) for two seconds. You can repeat the words in your head, "Inhale, one, two" to help you keep rhythm if you like.
-
Next, purse your lips as if you were about to whistle or blow out a candle.
-
Then, breathe out slowly and steadily for a count of four (twice as long as your inhale) through your pursed lips. You can repeat the words "Exhale, one, two, three, four," in your head to help you keep pace.
- Repeat.
The are a couple of key things to remember while practicing pursed-lips breathing: First, inhale only through your nose and exhale only through your mouth. Second, make sure to exhale for about twice amount of time that you spent inhaling.
You can use the pursed lips breathing technique any time you like, and it can even help you breathe easier when you're not experiencing any acute COPD symptoms. However, pursed lips breathing is especially effective to use when you exercise or exert yourself in any way.
For example, you can use pursed lips breathing when you climb stairs, do housework, or get up from a chair to keep your breathing even and steady. This can prevent fits of coughing and breathlessness, help you increase your endurance and tolerance for physical activities, and live a more comfortable, active life.
If you would like to see a visual demonstration of how to practice pursed lips breathing, check out this video from National Jewish Health.
Coordinated Breathing
Coordinated breathing is a technique for keeping your breathing controlled and steady when you exercise or do any other kind of physical activity. It makes it easier to breathe, reduces shortness of breath, and helps you stay focused on your breathing as you exercise.
"Coordination" is the key part of coordinated breathing, because it helps you time--or coordinate-- your breaths to keep pace with the rhythm of your movements. This helps you breathe steadily and deeply while you perform physical activities and prevents you from holding your breath, which is a common, but counterproductive reaction that many people have when they exert themselves or feel breathless.
How to Practice Coordinated Breathing
 |
| Photo by Ilke Cole |
The purpose of coordinated breathing is to help you remember to breathe steadily while you exercise instead of breathing erratically or holding your breath. You should practice coordinated breathing any time you work out or do a tiring physical activity.
Coordinated breathing is, more or less, a modified version of pursed lips breathing that helps you match the breathing technique with your movements as you exercise. If you haven't yet memorized and mastered pursed lips breathing, you will probably need to practice it while resting first to let it sink in before you can rely on it to help you in the middle of physical activity.
Here's how you perform the coordinated breathing technique:
-
Before you start a movement that's part of your exercise or activity, take a deep breath in through your nose for a couple of seconds.
- Begin doing your activity and, as you reach the most difficult or exerting part, purse your lips and exhale slowly for twice the number of seconds that you breathed in.

It can help to count your breaths in your head or out loud while you exercise to help you focus on coordinated breathing and keep the correct rhythm. Counting out loud also keeps you from holding your breath and helps you remember to stop or slow down if you get too breathless to speak.
Here are a couple examples of what coordinated breathing looks like in practice when you use it during everyday exercises and activities:
Coordinated Breathing While Climbing Stairs:
-
Start by taking a deep breath in for about two seconds.
-
Then, while breathing out slowly through pursed lips for about four seconds, climb 1-4 steps up.
- Pause, then repeat.
Coordinated Breathing While Vacuuming:
-
Before you start, take a deep breath in for about two seconds.
-
Next, push the vacuum forward while you breathe out slowly through pursed lips for about four seconds.
-
Inhale again for two seconds as you pull the vacuum back toward you.
-
Then, exhale again for about four seconds as you push the vacuum forward once more.
- Repeat.
Another great way to practice coordinated breathing is through certain types of yoga, like Vinyasa, which focus on combining breathing with fluid movements. Tai chi is another type of healthy exercise you can do that utilizes coordinated breathing as part of its routines.
 |
| Photo by Airman 1st Class J. Zuriel |
Check out this video for a helpful demonstration of how to use coordinated breathing during Vinyasa yoga. Even if you don't practice yoga, this video provides a practical example of how to coordinate your breathing with body movements that you can apply to any kind of activity you do.
Deep Breathing
Deep breathing is an effective method for getting trapped air out of your lungs and getting bigger, fuller breaths. Deep breathing can also help you stay calm and reset your breathing pattern when you feel short of breath.
This breathing technique works by filling your lungs up to maximum capacity and then slowly deflating them until every last bit of air is pushed out. This helps gets rid of any stale air that has been trapped in your lungs, which then allows you take in more fresh, oxygen-rich air with every breath.
Deep breathing can also help you relax your body and mind when you feel anxious or stressed. And, since anxiety is a common precursor to worsened shortness of breath, it might even help you preempt bouts of breathlessness triggered by anxiety.
How to Practice Deep Breathing
Deep breathing is a great exercise to practice along with other breathing techniques like pursed-lips breathing and diaphragmatic breathing (discussed in the next section below). When you feel short of breath, it might help to try deep breathing first, that way you can push any trapped air out of your lungs before moving on to other techniques.
Here is how you perform the deep breathing technique:
-
Find a comfortable place to stand or sit and relax your shoulders and chest muscles.
-
Push your elbows back slightly to open up your chest cavity and give your lungs more room to expand.
- Take a deep breath in through your nose until your lungs are fully inflated.
-
Hold your breath for about five seconds. You can count the seconds off in your head to help you stay focused.
- Exhale slowly through your mouth until you have pushed all of the air out of your lungs.
Diaphragmatic Breathing

Diaphragmatic breathing, also known as belly breathing (and sometimes "deep breathing"), is a versatile breathing exercise that can help you breathe more fully, steadily and slowly. It not only prevents breathlessness caused by COPD, but it can help you relax your chest, make it easier to breathe, and allow you to more quickly catch your breath when your symptoms act up.
Diaphragmatic breathing is a classic techniques that has long been recommended to patients with COPD. It is a breathing exercise meant to train your body to breathe from your belly (using your diaphragm) instead of using your chest muscles to breathe.
This is beneficial to people with COPD because their lungs and chest muscles already have to work overtime to make up for the fact that they can't absorb oxygen efficiently. This can cause chest soreness and discomfort, making it more difficult and uncomfortable to breathe.
The idea behind diaphragmatic breathing, however, is that it takes the work of breathing off of your chest muscles and puts it on your diaphragm, which is better designed to handle the work. This can help you breathe easier, get more oxygen to your lungs, and prevent the muscles in your chest, shoulders, and back from getting sore and worn out from breathing.
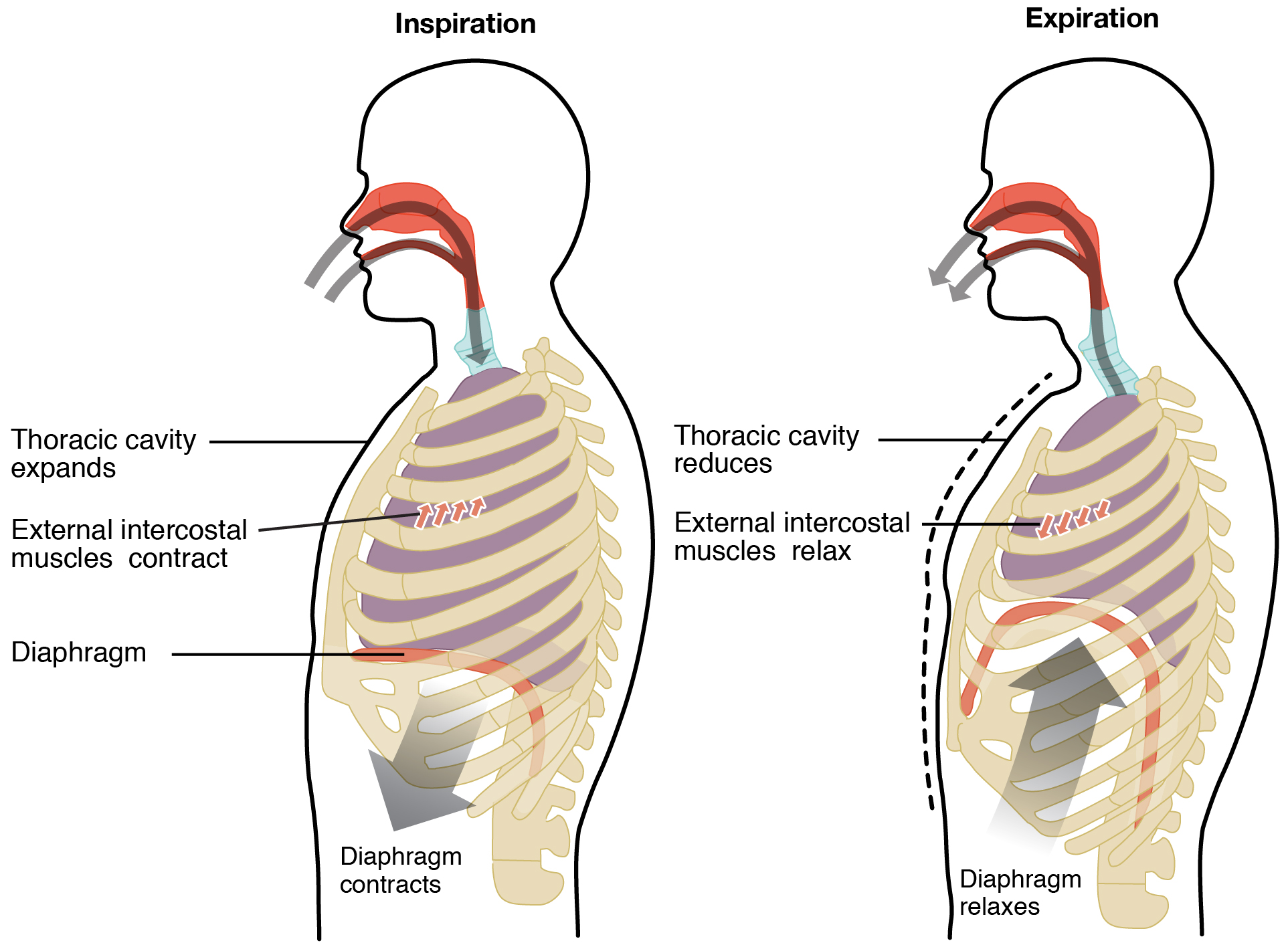 |
More recently, however, experts have begun questioning the long-term effectiveness of diaphragmatic breathing for people with COPD. While it can help you breathe from your diaphragm in the short term, more recent research suggests that it may not have the expected long term effects.
For example, some studies show that even when you practice diaphragmatic breathing regularly, it usually doesn't stick. It may not be possible to "retrain" your muscles because, as soon as you're not consciously thinking about breathing with your diaphragm, you'll likely go right back to using your chest muscles to breathe.
However, even if you can't retrain your body to use diaphragmatic breathing all the time, it can still have immediate, short-term benefits. Consciously practicing diaphragmatic breathing when you do activities or experience worsened COPD symptoms can provide some relief and reduce the amount of effort it takes to breathe.
For example, if you have severe COPD or experience a flare-up or exacerbation, you might experience worsened chest pain or sore chest muscles from coughing and wheezing. At times like these, you may be able to take some of the strain off of your chest and temporarily relieve some discomfort by practicing diaphragmatic breathing.
How to Practice Diaphragmatic Breathing

To practice diaphragmatic breathing, it's best to lie on your back in a quiet, comfortable place. However, you can also practice this technique while sitting or standing if needed.
Here is how you practice diaphragmatic breathing:
-
Sit down in a chair or lie down in a comfortable position. Make sure to relax the muscles in your shoulders, neck, and chest.
-
Then, place one of your hands on your chest and one on your belly so you can feel them expand as you breathe.
-
Take a deep breath in, concentrating on using your belly (diaphragm) to breathe. You should feel your stomach inflate and the hand resting on your belly should rise as you inhale. Focus on keeping your chest still.
-
Next, exhale slowly though pursed lips, focusing on using your belly to push the air out while keeping your chest still. You should feel your belly deflate and the hand on your stomach should fall as you breathe out.
- Repeat.
The key part of diaphragmatic breathing is keeping your chest muscles relaxed while you breathe with your stomach (or diaphragm). Placing your hands on your stomach and chest helps you focus on this goal and easily identify which muscles you are using to breathe.
For more information and a demonstration of how to practice this technique, check out this video on diaphragmatic breathing from the American Lung Association. This video will help you better understand the benefits of diaphragmatic breathing and how to use the exercise to improve your breathing in everyday life.
The Power of a Relaxed Posture

You might have noticed that the first step to practicing any of these breathing techniques is to relax your body. That is because it's common to tense up the muscles in your shoulders, neck, and back when you are struggling to breathe.
This tense posture happens naturally, but it can make it even more difficult to breathe when you feel short of breath. Instead, you should always do your best to keep your body relaxed, even when you're feel like you can't breathe.
Keeping the muscles in your neck, chest, and shoulders relaxed can help relieve airway obstruction and make it easier to catch your breath. It not only relaxes the muscles in your chest cavity, giving your lungs more room to expand, but also relaxes the muscles in your throat and airways so air can more easily flow through.
Relaxing your body can also help you feel more calm, as tense muscles send signals to your brain that make you more aroused and anxious. The more calm you are, the easier it is to slow your breathing rate and stay focused on productive breathing exercises that can make the breathlessness pass.
Pulmonary Rehabilitation
Pulmonary rehabilitation is like a special health class designed to help people with COPD and other respiratory diseases improve their breathing and better manage respiratory symptoms like shortness of breath. Taking a pulmonary rehabilitation class is a fantastic way to learn more about breathing techniques and how to use them during exercise and in your everyday life.
In pulmonary rehab, you will get plenty of opportunities to learn and practice practical breathing strategies and exercises along with other patients who have COPD. You'll also learn how to use your medications to control your symptoms, how to make lung-healthy lifestyle choices, and how to exercise while coordinating your breathing and keeping your symptoms under control.
Pulmonary rehabilitation is often recommended to COPD patients who have trouble exercising, doing daily activities, or managing their symptoms on their own. If you would like to join a pulmonary rehabilitation class you will need to talk to your doctor to get a referral first.
Practice Makes Perfect!
If you have COPD, there's no excuse for not learning and utilizing these extremely simple, yet surprisingly powerful, techniques for controlling your breathing. They're not only easy to learn, but easy to practice compared to other COPD treatments because they take such a little amount of effort and time out of your day.
After studying this article, you should know how to practice the most effective COPD breathing exercises and understand when each is most helpful to use. If you put in the time to study and practice these techniques, you'll be better able to catch your breath and keep your breathing steady in the midst of difficult COPD symptoms.
As we've mentioned before, practicing breathing techniques regularly, especially when you're not having trouble breathing, is key for reaping maximum benefits from the exercise. After


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













