Getting enough sleep is a daily challenge for many people with COPD. Between coughing, breathing troubles, and shortness of breath, it's no wonder that the disease makes it difficult to relax and sleep soundly at night.
Up to fifty percent of people with COPD report sleeping problems, which makes it a major concern for COPD treatment. Good quality, adequate sleep is necessary for a healthy body and immune system, and constant sleep disturbances can make COPD patients much more prone to illnesses, exacerbations, and other dangerous complications.
What's more, COPD patients are disproportionately affected by sleep disorders. For example, people with COPD are more likely to have sleep apnea, a dangerous condition that occurs when your airways collapse and restrict your airflow when you sleep.
In this article, we're going to show you a variety of different ways to improve your quality of sleep at night. But first, you need to understand why getting enough sleep is so important for your mental and physical state.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Why it's Important to Get Enough Sleep
Sleep deprivation can have devastating effects on your ability to concentrate, remember things, and deal with the pressures of everyday life. It also weakens your physical state, making you more prone to getting sick and having an acute COPD exacerbation.
If you have trouble getting enough sleep or wake up often during the night, it actually suppresses your immune system and makes you more likely to get sick. Some studies have shown that COPD patients who get poor sleep are up to fifty percent more likely to experience an acute exacerbation.
Lack of sleep also contributes to a variety of other health issues and chronic diseases including diabetes, high blood pressure, obesity, mood disorders, and inflammation. It also affects your mental state, making it more difficult to focus, problem-solve, and remember things. It can even lead to anxiety and depression over time.
To avoid these problems and keep your body healthy, getting enough sleep is a must. If you are having difficulty sleeping on a regular basis, you should start trying new ways to get better sleep right away.
Even though COPD can make sleeping challenging, there are plenty of ways to reduce and manage nighttime symptoms and make yourself more comfortable at night. Instead of giving up on good sleep, take some time to learn about the variety of medications, medical tools, and lifestyle changes that are proven to help you sleep better.
In this article, we'll show you many different techniques you can use to make it easier to fall and stay asleep every night. If you want to learn how to get better sleep, reduce your COPD symptoms, and experience the benefits of being well-rested, continue reading this article for a variety of practical tips you can use to get better quality sleep with COPD.
Why COPD Makes it So Difficult to Sleep

There are many reasons that a large percentage of COPD sufferers find it difficult to relax and get good quality sleep at night. COPD symptoms on their own often interfere with rest, but other, indirect effects of COPD can also make it difficult to sleep.
Many people with COPD experience disease-related anxiety or depression, or are at a higher risk for other conditions that affect sleep, including GERD and sleep apnea. In addition, medications used to treat COPD symptoms can cause poor sleep as well.
Here are a few major factors that contribute to sleep problems in people with COPD:
-
Disruptive COPD symptoms: It's not hard to imagine how feeling short of breath or having a coughing fit can make it difficult to relax and fall asleep at night. Shallow breathing at night can also cause blood oxygen levels to drop, which can cause you to wake up abruptly and frequently as a result.
-
Anxiety and mental health problems: COPD is a difficult chronic disease to live with, and it can take a huge toll on your emotional and mental health. It's common for people with COPD to experience anxiety disorders, depression, and general emotional distress, all of which can make it difficult to sleep.
-
Medications used to treat COPD: Some COPD medications, especially bronchodilator medications, can make it more difficult to sleep. Some medications have indirect side effects that can affect your ability to sleep as well, such as medications that cause nightmares or cause frequent urination during the night.
-
Obstructive Sleep Apnea: Obstructive sleep apnea is a breathing-related sleep disorder that affects a large percentage of COPD patients. It causes frequent lapses in breathing during sleep and causes people with the condition to startle awake frequently at night. Sleep apnea can still affect your sleep even if you don't know you have it and if, like most sufferers, you don't remember waking up during the night.
-
GERD (Gastroesophageal Reflux Disease): This is a condition that occurs when stomach acid leaks into your throat, and it affects a large number of people with COPD. GERD symptoms tend to be most noticeable at night while lying down, and it can affect your quality of sleep.
- Difficulty sleeping in a comfortable position: COPD-related breathing problems can make it difficult to breathe while lying down. As a result, many people with COPD end up sleeping in uncomfortable, unhealthy positions, such as sitting up in a chair.

While COPD can make getting adequate, good-quality sleep a challenge, it's a challenge that can be conquered with simple solutions and adjustments to your daytime and nighttime routines. In this article, we're going to show you how to conquer each of these COPD-related sleeping problems so you can get the rest and energy you need to enjoy your life to the fullest.
There are a variety of practical ways to conquer the most common emotional, physical, and environmental causes of poor sleep in people with COPD. With this guide, you can begin addressing your sleep barriers today and start building a sleep-healthy lifestyle that will give you the consistent, restful sleep you've always wanted.
How to Get Better Sleep if You Have COPD
Change Your Bedtime Routine
Many sleep problems in the modern world result from poor habits. Even if COPD is the main cause of your sleeping difficulties, looking at your overall bedtime routine is still wise.
For example, habits like exercising in the evening or spending time on your phone or computer late at night make it much more difficult for your body to feel tired at bedtime. Also, running errands, doing chores, and working late in the evening doesn't put you in a good mindset for sleep.

Many of these habits are simple to change and can be surprisingly effective at improving your quality of rest. One of the most important things you can do is establish a relaxing, consistent bedtime routine that allows you to gradually wind down in the evenings.
For example, try planning relaxing activities like reading, yoga, or listening to music close to the time that you go to sleep. Work these kinds of activities into a routine you can follow every night, that way, when you follow your bedtime routine, your brain and your body will know it's time to rest and start preparing to go to sleep.

Here are some general tips for nighttime habits that can improve your ability to sleep:
-
Dim the lights at least an hour or so before you go to bed. That will help your brain and body start to feel drowsy so it's easier to fall asleep when it's time.
-
Don't do stressful or mentally taxing activities before bed. Try to find relaxing, idle activities that allow your mind to wind down and let go of worries.
-
Go to bed at the same time every night and set your alarm for the same time every morning, even on weekends. This will help your body adjust to your sleep pattern and fall asleep naturally at the right time every night.
-
Practice relaxation exercises like mindfulness meditation, breathing exercises, or yoga in the evenings to help your body and mind relax.
-
Try taking a warm shower or bath near bedtime; warming up your body will help you feel more sleepy.
-
Try drinking warm milk or decaffeinated tea to relax and wind down before bed. Just don't drink anything with caffeine and avoid drinking too close to bedtime if it will make you have to get up to go to the bathroom during the night.
-
Never use your computer, phone, or laptop in your bed or too close to bedtime. The light from the screen tricks your brain into thinking it's still daytime and makes it more difficult to go to sleep.
-
Use your bed for two things only: sleeping and sex. That way your body will know it's time to sleep and feel drowsy when you get in bed. Don't read books, browse the internet, or watch TV in your bed. It's a hard habit to break, but it can save you from many restless nights.
-
Clear your airways before bed to reduce symptoms like coughing and shortness of breath. Use proven mucus clearance techniques like chest percussion and huff coughing.
- Don't sleep with pets in your bed, no matter how much you like to have them by your side. Studies show that pets can severely disturb your sleep, even if you're not aware of it. Get your pet a nice warm bed of their own to keep next to yours. Don't worry, both you and your pet will adjust quickly and you'll have more energy to give them in the mornings.
Stay Away from Alcohol and Caffeine at Night

While caffeine is an obvious cause for poor sleep, many people don't realize that alcohol can hurt your quality of sleep as well. Caffeine affects your brain and makes it difficult to fall asleep, while alcohol affects your brain and muscles, making it more difficult both to breathe and to stay asleep through the night.
One way that alcohol affects your sleep is by causing the muscles lining your throat and airways to relax too much when you sleep. This causes your airways to collapse or sag and obstruct airflow, which affects your ability to breathe and absorb oxygen at night.
This is a greater risk for people with COPD, who already tend to suffer from sleep disorders and nighttime breathing problems. Alcohol also affects your brain and your sleep cycles, and drinking alcohol too close to bedtime leads to worsened sleep quality.
Caffeine is a stimulant that can also affect your ability to fall asleep at night, especially if consume it too close to bedtime. For the best possible sleep, you should avoid caffeine for at least eight hours before you go to bed or cut it out of your diet altogether.
Avoid Foods that Trigger GERD
Gastroesophageal reflux disease (GERD) is a common digestive issue in people with COPD. In fact, by some estimates, up to fifty percent of COPD patients also suffer from GERD.
Some of the common symptoms of GERD are indigestion and difficulty breathing at night, which is particularly uncomfortable for people with respiratory diseases. These symptoms are most noticeable during the night because, when you're lying down, it's easier for stomach acid to leak into your esophagus. This causes heartburn and throat irritation that make it difficult to sleep and can leave you with a sore throat in the morning.
The best way to prevent nighttime GERD symptoms is to eat a GERD-friendly diet. If you suffer from GERD, be careful not to eat foods, like acidic foods, that might trigger your GERD symptoms, especially at night before bed.
Another thing that can help is to eat something bland and absorptive before going to sleep. Try eating a few light crackers, like plain saltine crackers, before bed to keep your hunger and stomach acid at bay.
If you still struggle with GERD symptoms after adjusting your diet, talk to your doctor about medications and antacids you can take to keep your symptoms under control. In severe cases, you might need stronger medications or surgery to treat your GERD.
Don't Eat too Close to Bedtime

Many people with COPD find that a full stomach makes them feel extra breathless. This happens when your stomach expands and presses on your lungs and diaphragm, making it more difficult to breathe.
This can make you very uncomfortable, especially if you're trying to rest. Feeling bloated and breathless makes it hard to relax and will likely hurt your quality of sleep at night.
The best way to prevent this is to eat several smaller meals throughout the day, instead of three large ones. Also, be careful not to eat too much too close to bedtime, otherwise, you'll be at risk for breathlessness and indigestion as you try to sleep.
You don't want to go to bed hungry, though, so have a light, healthy snack ready in case your appetite kicks in before you go to sleep. Saltine crackers, a bit of cheese, or another small, quick, low-sugar snack will do.
Make Your Bedroom More Pleasant

Many people underestimate the impact that their environment has on their ability to sleep. If the bed and the room you sleep in doesn't feel comfortable, it makes it much more difficult to relax and rest at night.
Take a moment to look around your bedroom, and ask yourself, “Is this a place I look forward to sleeping in?” Is the room cozy and comfy, quiet, and free from clutter?
It's important to sleep in an environment that is quiet, dark, and comfortable, otherwise, it will be difficult to sleep undisturbed. Your sleep environment should be free from messes, bright screens and electronics, and anything else that could be distracting or stressful while you're trying to sleep.
Here are some tips for making your bedroom environment more cozy and comfortable:
-
Save up for a better mattress or more comfortable bedding. Lying on a luxurious mattress or wrapping yourself in soft, silky sheets can help you relax at night and even look forward to going to bed.
-
Clean up messes and clutter and organize your space. Make sure every item in your bedroom has a proper place so it's easy to keep clean.
-
White noise can be very effective at blocking sounds that come from outside your room. Get a white noise machine to place near a noisy window or door to drown out disruptive sounds while you sleep.
-
If bright light comes in through your window in the morning, consider getting a blackout curtain to keep your room dark. You could also hang a thick blanket in front of the window or get a comfortable eye mask to block the sun from your eyes.
-
Keep anything that reminds you of work or responsibilities out of your bedroom. Keep your bills, work documents, and other task-related items somewhere else, so they don't trigger anxiety before bed.
- It's easier to sleep if you keep your room cool at night. You can do this by setting your AC to a comfortable temperature, opening a window, or aiming a fan at your bed.

It's easy to ignore messes and environmental annoyances in the bedroom, but it's not a part of your house you should neglect. It's worth taking some time to personalize, organize, and turn your bedroom into a place where you can actually be comfortable and enjoy sleeping.
Take Care of Your Mental Health

If you're having trouble relaxing and sleeping at night, it might be because of mental distress. It's normal and common for people with COPD to experience negative emotions or psychological disorders like anxiety and depression, all of which can severely interfere with your ability to sleep.
Living with a chronic disease is hard; it can be exhausting, frightening, and take a huge toll on your life. It's natural to experience anxiety, depression, and emotional distress as your symptoms worsen and you lose your physical independence.
That's why it's so important to look after your mental health and see a mental health professional if you can't cope on your own. Instead of withdrawing or letting anxiety eat away at your life, turn to your family, friends, and pets for joy and comfort. Do your best to continue doing the hobbies and activities you enjoy and don't let your disease define your life or who you are.
Part of looking after your mental health includes setting aside time for quiet and relaxation every day. Proven techniques like mindfulness meditation or creative hobbies are a great way to unwind and refuel your mental resources.

A healthy diet, healthy sleep schedule, and regular exercise can also do wonders for your mental health. Getting regular aerobic exercise, in particular, is a very effective treatment for anxiety that will also help you feel tired enough to go to sleep at night.
If you suffer from severe anxiety or depression that disrupts your daily life, talk to your doctor about treatments or medications that can help. Your doctor might refer you to a psychologist or psychiatrist or prescribe anti-depressant medications to help you improve your mental health and quality of life.
Consider Therapy

People with COPD often feel isolated, disconnected, and find it difficult to ask for support. But everyone needs mental and emotional help now and then, especially when going through a difficult time like managing a chronic disease.
Many people find that counseling and talk therapy help them confront their anxiety, depression, and other negative emotions related to their disease. Individual therapy provides a safe, intimate setting to unpack personal thoughts, worries, and fears and work through mental barriers that make it difficult to fully enjoy life.
You can also find COPD therapy groups where you can connect with other people who understand what you're going through. There are a variety of both online and local therapy groups designed specifically for people with COPD and other chronic diseases.
Talking with other COPD patients and sharing your challenges and successes is a great way to regain confidence and a feeling of control over your disease. You can also get useful advice, emotional support, and new friends through group therapy that you would never have gotten if you tried to cope on your own.
Keep a Journal

If you suffer from anxiety or depression, then you know how they can take a toll on your ability to sleep. Many people with COPD experience hopelessness, despair, fear, and worry, which often intensify and are difficult to ignore at night.
That's why it's important to quiet your mind and let go of your worries and fears before bed. One method for doing this is journaling, an activity researchers have proven time and time again is a powerful and effective tool for mental health.
There are no hard rules for journaling; a huge part of its benefits come from the freedom that journaling gives you to write and express yourself freely, without strict guidelines or judgment. All you have to do is spend at least a few solid minutes writing something—anything—about yourself, your life, or your thoughts.
Journaling before you go to bed is a great way to unload all the distressing thoughts and worries that have accumulated in your head during the day. Recording your hopes, your fears, or even your to-do list in your journal can help you let go of heavy thoughts and feel calm enough to sleep.
Here are some general tips to help you get the most out of journaling:
-
Try to write in your journal regularly, ideally every day. That way it becomes a habit and something you can look forward to that will help you relax before bed.
-
Don't edit, scrutinize, or judge yourself as you write. Let the words flow freely and uncensored; it's about the action of writing, not how eloquent or pretty it looks on paper.
-
It's okay not to write in full sentences. It's okay to write stories, lists, and streams of consciousness. You don't have to be grammatically correct, and you don't even have to make sense. A journal is about expressing yourself in whatever way you please.
- Your journal is, primarily, for you and you alone. However, if you desire, you can share pages or passages with others. Sometimes it's easier to express yourself and communicate on paper, and sharing your thoughts and feelings with others can be therapeutic.
Progressive Muscle Relaxation
Another technique that can help to quiet nighttime anxiety and restlessness is progressive muscle relaxation. It is a method for reducing muscle tension and relaxing your body before you sleep, and it's often recommended for people who suffer from insomnia.
Anxiety and mental distress affect more than just your emotional state; they have noticeable physiological effects, too. Anxiety, in particular, tends to manifest in your body as muscle tension and jitters that can make relaxation all but impossible.
Progressive muscle relaxation addresses anxiety from the outside in; that is, by relaxing your muscles and reducing the physical effects of anxiety, it helps to reduce the feeling of anxiety that you experience on the inside, as well. It also helps prevent muscle spasms and tightness, so you can relax and feel more comfortable in bed.
Y
When you think about your daily routine, what comes to mind? Maybe you think of making your bed, taking a shower, or making a cup of coffee. These are all things that most people do sequentially and sometimes even subconsciously. But have you ever wondered why it’s so easy to do these things regularly, but something like implementing a new diet or exercise routine can feel near impossible to achieve?
As COPD patients, we’re faced with a difficult decision: either ignore our treatment plan and maintain the unpredictability of life or live life by the books, following every rule that our doctor tells us. However, with some hard work and determination, it’s possible to accomplish both of these tasks without having to stress about whether you’re making the right decisions.
If you’re a COPD patient who has trouble making and sticking to a routine, read on because we’re going to take a deep dive into some of the biggest roadblocks preventing COPD patients from living a healthy and happy life. As always, if you’re planning on making any major changes to your treatment plan, be sure to speak with your doctor first.
Why Are Routines So Important?
A routine is something that you do habitually. In other words, it’s something you do without giving much of a second thought to. These can either be good things like going to bed at the same time each night; or bad things like smoking cigarettes after lunch. But the one thing they have in common is that they both feel natural in your day-to-day life. Without having these routines, we might feel a lack of structure or direction in our lives.

Another problem with having no routine is that it can be mentally and physically exhausting to accomplish goals. For example, if you’re constantly having to fight yourself to eat the right foods or take your medication on time, you might get behind on them and get discouraged. Each time this happens, you’re getting farther and farther away from accomplishing your goal.
But one of the most common misconceptions about good habits is that just because something works for one person does not necessarily mean it will work for another. This is why it’s important to start with a broad overview, then narrow down something that will work for you.
Make Sure You Understand Your Long-Term Goals
Generally speaking, bad habits are the result of a narrow-minded approach to your health. For example, if you take a smoke break in the middle of the day you’re only taking into consideration how you’re feeling at that moment. You might feel stressed or antsy early in the day, but after smoking, you feel satisfied and complete. However, in reality, smoking actually increases stress, because, after an initial release of dopamine in the brain, you’ll begin to experience withdrawals which make you feel even worse than before.

Whether you’re struggling with bad habits involving smoking, your diet, exercise, or anything else, the best place to start is by shifting your focus to long-term thinking. Rather than creating habits that satisfy your immediate desires, you should be creating habits that reinforce what you’re trying to accomplish in life. This is an important step because the more clearly you define what you’re trying to do, the more obvious it will be if you start falling back on your goals.
Eliminate Any Distractions
Distractions are so commonplace in the modern world. If you own a phone, tablet, computer, or any other electronic device, you’re probably well aware of how easy it is to spend hours on these devices without even acknowledging what’s going on in the real world. According to Kommando Tech, people check their phones an average of 58 times a day. Even if you’re looking at your device for a fraction of a second to check or reply to a message, you’re still taking your mind off of whatever you were doing. Over time, this could become a significant roadblock preventing you from implementing healthy habits.

Electronics are not the only distractions in our lives, however. If you take some time to think about the distractions in your life, you’ll likely come up with a good list of things. For many people, a dirty or cluttered home can be a distraction. According to Men’s Health, a messy home can contribute to anxiety, affect your quality of sleep, and contribute to avoidance strategies that make us less productive. These are just a few of the distractions that could be present in your life. Be sure to take some time to sort these out before you move on.
Make Reminders Around Your Home
Chances are, you have that one friend who likes to create reminders for everything, even for things that don’t seem important. From an outside perspective, this can be a little overbearing; but if you’re the one setting the reminders, it might make more sense to you. Reminders are a great way to force yourself to stick to a routine, at least until you’re able to do it without them. Some people prefer to make physical reminders on a notepad or sticky note, but others prefer to use digital reminders on their phone or computer. Better yet, you could try a combination of the two.
Physical reminders are great if you want to keep yourself on track throughout the day. For example, you could place sticky notes on the door reminding you to take your medication before leaving the house or you could put sticky notes on your fridge to remind you what foods to avoid. Setting reminders on your phone can also be useful if you want to remind yourself of doctor’s appointments or when to exercise. The type of reminders you need will depend entirely on what habits you struggle with keeping, but generally speaking, they’re a great way to keep you on track.
Find Ways to Make Your Routine Easier
Most people prefer to find the path of least resistance when it comes to accomplishing their goals. There’s no point in adding any unnecessary struggle, especially if your health is at risk. So, it goes without saying that any little thing you can do to make your health routine easier to follow will be very beneficial in the long run. One of the best things you can do to simplify your COPD treatment plan is to invest in a portable oxygen concentrator.

A portable oxygen concentrator is an electric oxygen generator used to replace old, outdated types of oxygen equipment like oxygen tanks and liquid oxygen tanks. They work by drawing in ambient air that you would normally breathe and then removing gases like nitrogen, argon, and more. The device then puts out medical-grade oxygen through the nasal cannula. You’ll receive the exact same amount of oxygen with a portable oxygen concentrator, but the device is much easier to manage.
First and foremost, portable oxygen generators are much lighter than oxygen tanks. A pulse dose concentrator like the Inogen One G5 is under 5 pounds making it very easy to carry on your shoulder or back. Oxygen tanks, however, tend to be much heavier at around 10 to 15 pounds. As a result, you’ll need to wheel your oxygen tank around using a carrying cart. This is especially inconvenient if you need to go up a flight of stairs or some other obstacle.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Another problem with oxygen thanks is that they are very bulky and oblong. So when it comes to storing one, you’ll have a difficult time. Since they’re highly pressurized and contain medical oxygen, they can be very dangerous. Oxygen tanks can be stored at 2,000 pounds per square inch (PSI) or more which makes them a hazard to keep around the house. Portable oxygen generators don’t have any compressed oxygen inside the unit so they don’t have this problem.
Finally, portable oxygen concentrators are simply put, much easier, and convenient to use. Oxygen tanks need to be refilled by a professional when they run out of oxygen, but POCs just need to be recharged. Since the batteries are so light, you can carry plenty of backup batteries with you wherever you go and you’ll never run out of oxygen. You can even use your POC while it’s plugged into the wall charging.
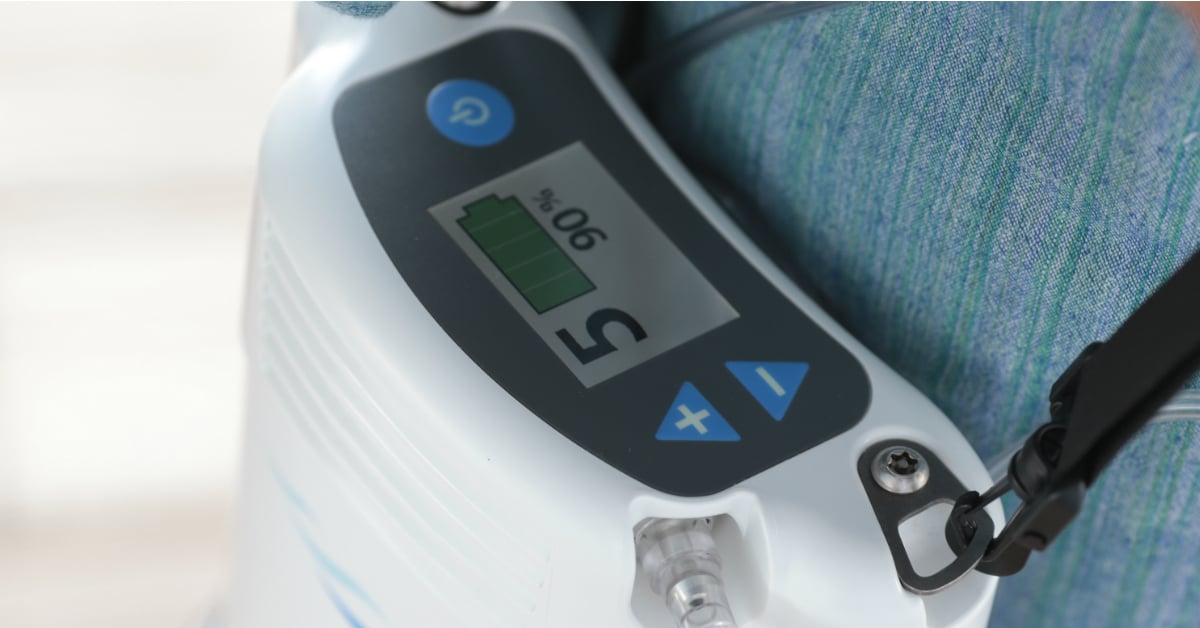
The reason POCs make your COPD routine easier is that they are mostly out of sight and out of mind. Rather than having to worry about whether or not you’re getting enough oxygen wherever you go, POCs provide you with a consistent and reliable source of oxygen that won’t fail when you need it the most. COPD patients who use concentrators find that they spend less time thinking about their disease and more time living their lives.
Don’t Get Thrown Off by a Change of Plans
It’s happened to all of us… we’re doing a great job of maintaining good habits and working towards our goals. Then, all of a sudden, something happens that causes us to get off course. Life isn’t always going to be predictable, so we need to be prepared when our plans change and we aren’t able to follow through with our normal routine.

It’s important that you have the freedom to attend family events and visit friends whenever you want. But at the same time, you need to have a plan to stay on track towards meeting your goals even with all of life’s surprises. One way to do this is to simply notify your friends and family about your routine so that they can help you stay on track.
Get Plenty of Sleep
One of the most important factors that will help you maintain a routine is alertness. Studies have found that COPD patients are significantly more likely than the general public to experience sleep disruptions that can lead to daytime sleepiness and even contribute to COPD flare-ups like breathlessness, chest pain, and fatigue. It’s important to fix these underlying issues if you want to have the energy to follow through with your routine. Try some of the following tips to improve sleep with COPD:
![]()
- Changing your sleeping position can take some stress off your lungs and promote more restful sleep. The Lung Institute recommends sleeping on your side with your head slightly propped up to improve breathing.
- Avoid taking naps during the day. A consistent nighttime sleeping pattern will keep you more alert and prevent daytime drowsiness.
- Avoid using electronics right before bed. Staring at a screen as you’re winding down for the night can mess with your body’s circadian rhythm.
- Exercise more consistently. Moderate exercise increases the amount of slow-wave sleep you get. In other words, you get more “deep sleep” where your body and mind are able to rejuvenate.
- Get tested for a sleep disorder. COPD-OSA overlap syndrome is a common cause of sleep disruptions. Treating obstructive sleep apnea will be the best way to experience better sleep at night.
- Speak to your doctor about your medication. Certain COPD medications may contribute or outright cause sleep problems.
Speak With Your Doctor
Ultimately, your doctor will be your greatest resource if you’re having trouble following your treatment plan. He/she may have some helpful tips to keep you on track, or your doctor may be able to alter your treatment regime completely in order to make it easier to follow. Another thing that your doctor can do is refer you to a mental health specialist who can help you cope with the mental and emotional aspects of dealing with chronic obstructive pulmonary disease. Cognitive behavioral therapy is one of the most trusted forms of therapy.

Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) is a type of therapy that aims to change the way that you think and act. It’s designed to target negative or inaccurate thinking patterns that can lead to you developing bad habits. CBT is a type of psychotherapy (talk therapy) that usually involves a one-on-one conversation with a mental health counselor. Most commonly, CBT is used to treat mental health conditions like depression, anxiety, or eating disorders, but it can be used by anyone to help people cope with difficult situations like living with COPD. Below are the steps involved in a CBT session:
Identifying the problem: Before you can solve the problem you need to know what’s causing it. Your first session of CBT will likely be focused on targeting troubling situations or conditions in your life. This could be things like COPD symptoms, or a troubling experience involving a flare-up or exacerbation.
Becoming aware of your thoughts and feelings about these events: Next, it’s important for you and your therapist to understand exactly how you’re reacting to these problems. You may be asked to keep a daily journal where you write down your change of emotions throughout the day.
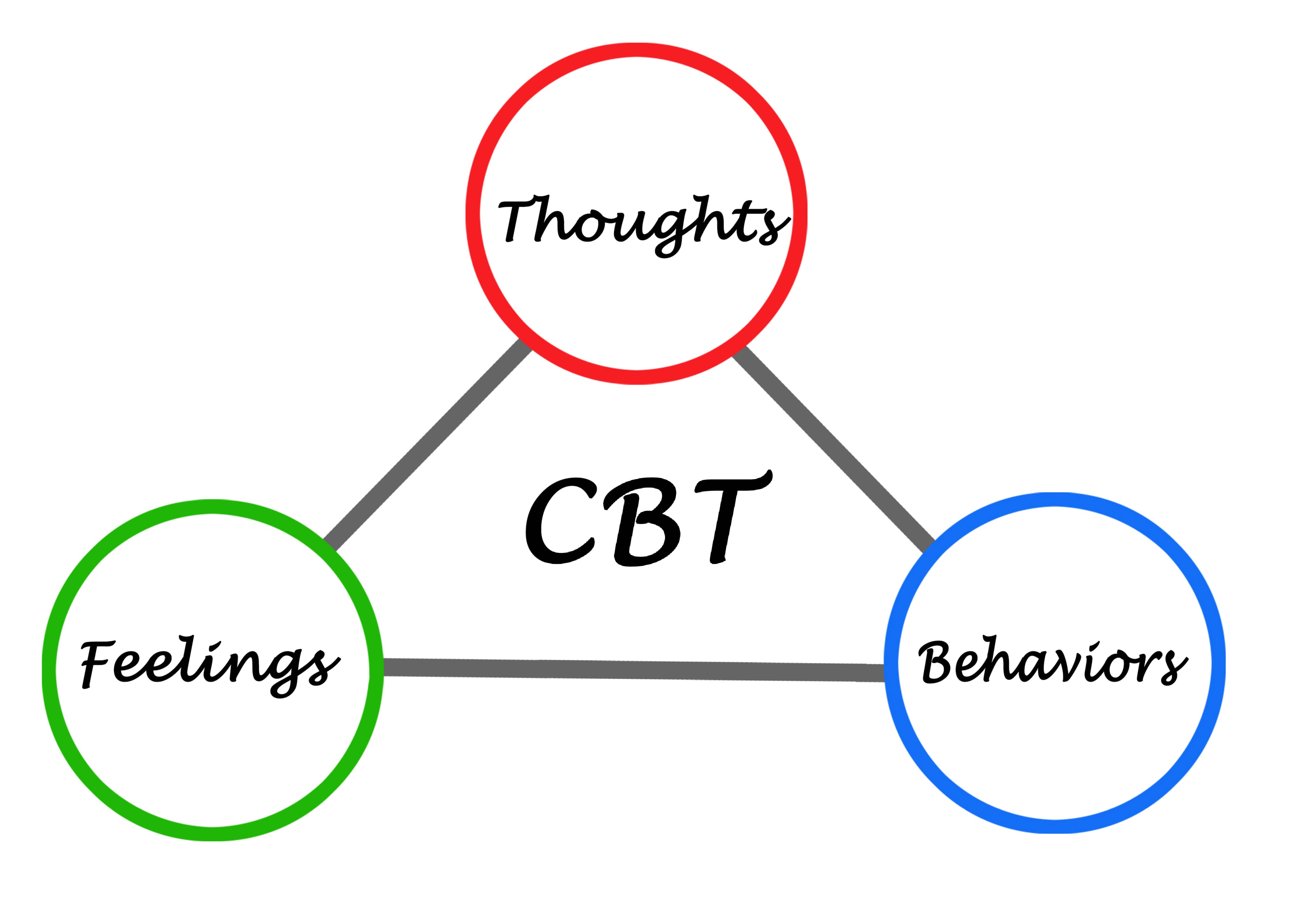
Understanding negative or inaccurate thinking: Destructive thoughts are usually the result of an inaccurate interpretation of an event. This step will help you identify these thoughts so that they can be reversed.
Reinforcing positive thinking patterns: Finally, you and your therapist will working on reinforcing constructive thoughts throughout your daily life. This could take several weeks or several months depending on how receptive you are to the changes.
Conclusion
At the end of the day, it’s much easier to give in to bad habits than to reinforce good habits, especially if you suffer from a chronic illness like COPD. Being diagnosed with COPD means having to take on new responsibilities and pay closer attention to how your daily routine affects your long-term health. This can feel overwhelming at times, but if you break it down and understand how habits develop in the first place, it will be much more manageable.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
In this post, we showed you just a few of the things you can do to maintain healthy habits with COPD. However, as we mentioned, everyone is different and what might work for one person may not work for another. If you’re still struggling with managing COPD symptoms, be sure to stick to our blog. We try to provide respiratory patients with a unique perspective on their disease as well as providing tips that you won’t find anywhere else.
If you’re looking for a portable oxygen concentrator for sale in Denver, don’t hesitate to reach out to our respiratory specialists here at LPT Medical. Since most COPD patients need 24/7 supplemental oxygen, it’s our goal to ensure they are able to do this comfortably and without affecting their daily routine. Call us at 1-800-946-1201 today to speak with a respiratory specialist.

It’s pretty amazing to think about how quickly health care advances these days. Just in the past couple of decades, medical specialists have made significant strides with everything from mapping the human genome to improving telemedicine and even introducing robotic surgery. According to Singularity Hub, we’re likely to see medicine advance more in the next 10 years than it did in the past 100 years.
If you have a respiratory condition such as asthma, COPD, or cystic fibrosis, you might also be surprised to find that your treatment plan would have looked very different 100 years ago than it does today. Using modern testing procedures and techniques, doctors are able to provide a more accurate diagnosis than ever before and help patients plan their life accordingly.
With all that being said, the way we treat COPD will likely look very different in another 10 years than it does today. As we speak, researchers are working on a number of different medicines, tests, and surgeries that may prove to be breakthroughs in the way that we treat and diagnose one of the world’s most prevalent illnesses.
In this post, we’re going to take a look at several different emerging medical breakthroughs that COPD patients should keep an eye on in the coming years. While these procedures show promise, it’s important to remember that they’re still in a developmental stage. Currently, your best bet for reducing COPD symptoms and slowing the progression of your disease is to follow your doctor’s instructions.
Stem Cell Therapy
Stem cell therapy is possibly one of the most talked-about medical breakthroughs, not just for COPD, but also for a variety of other conditions such as macular degeneration, spinal cord injury, stroke, burns, heart disease, and more. Also known as “regenerative medicine,” the goal of stem cell therapy is to generate healthy cells in the body to replace diseased ones.
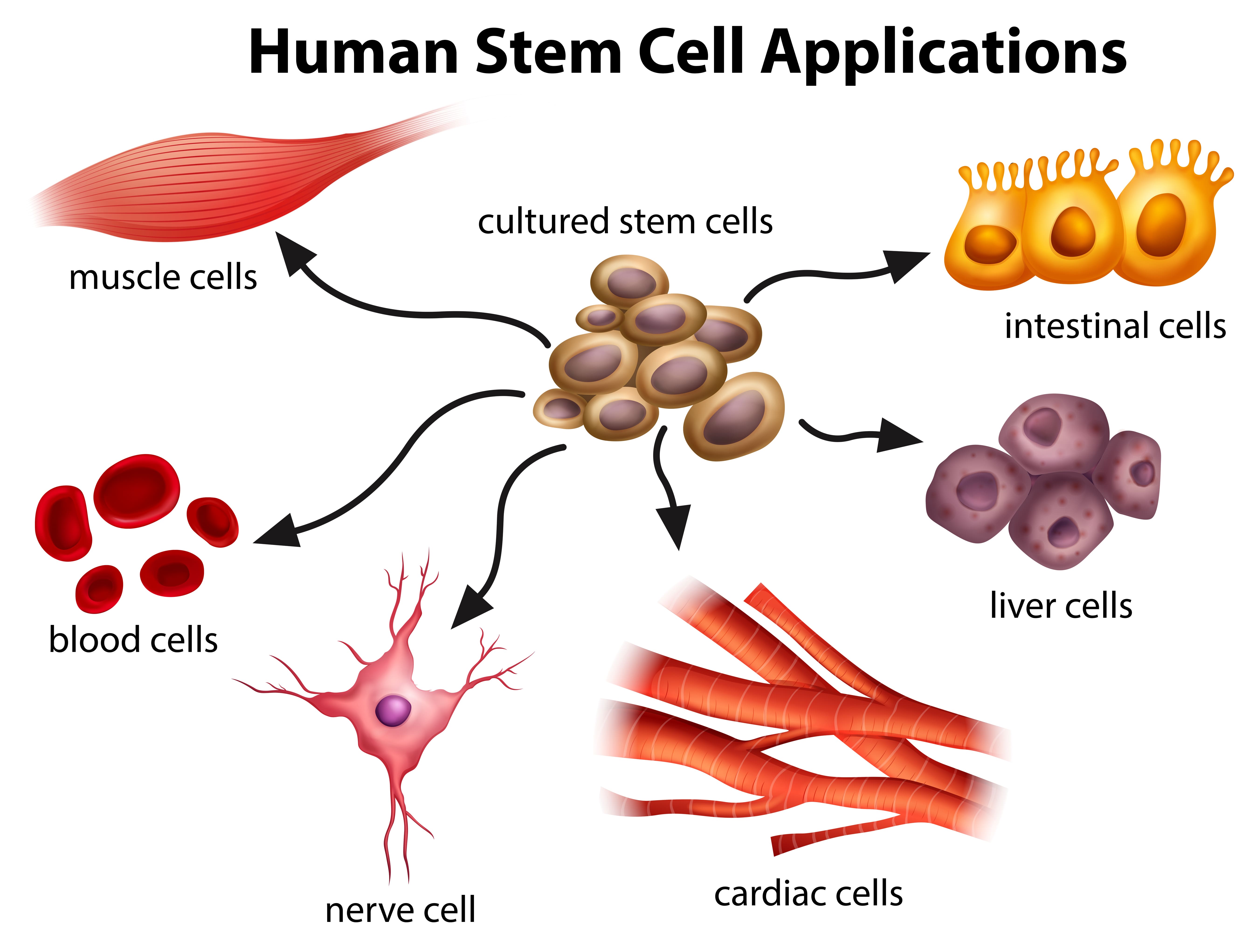
In essence, a stem cell is a sort of canvas on which all other types of cells are made. When they’re exposed to the right conditions — either in the body or in a lab — stem cells divide into “daughter cells” which are more specialized and suited to accomplish a certain task or goal. For example, white blood cells can be produced to help fight and dispose of foreign invaders in the body.
The reason there is so much talk around COPD and stem cell therapy is that COPD is a “progressive disease.” What this means is that once inflammation starts to develop in the airways of the lungs, the damage cannot be reversed. In order to slow the disease progression, you’ll need to follow a strict treatment plan created by your pulmonologist.
According to DVCStem, stem cells can repair damaged lung tissue to combat either emphysema or chronic bronchitis, the two diseases that makeup COPD. A study conducted by the Lung Institute showed a number of positive results, stating that patients “averaged an increase of 35.5% to their Quality of Life (QLS) score within three months of treatment.” It also found that 84% of patients saw an increase in their quality of life after 3 months.
However, since stem cell therapy is such a new procedure, more tests are needed to verify its efficacy using larger sample sizes and other factors such as exercise tests, hospital visits, the use of oxygen therapy, and more. Periodic patient follow-up will also help researchers better understand the long-term benefits of stem cell therapy on COPD. So far, these studies have shown no negative side-effects to using stem cell therapy.
Endobronchial Valves
Endoscopy is the process of inserting a tube with a camera into the body in order to view certain organs in more detail. In certain situations, health professionals may need to look inside a patient’s airways either to examine signs of damaged tissue or to take samples. This is known as a bronchoscopy.
One of the more recent advancements in endoscopy is something called an endobronchial valve (EBV). This is a small implantable medical device that can help people with lung disease (primarily emphysema) breathe easier. While endobronchial valves were approved by the U.S. Food and Drug Administration in 2018, they’re still considered a developing technology, and studies are being done to improve their efficacy.
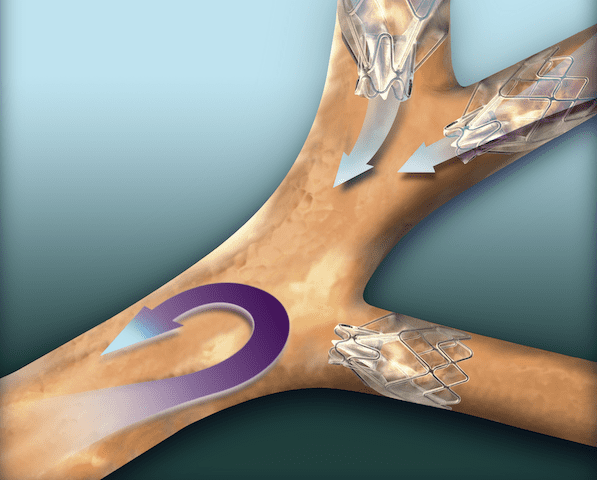
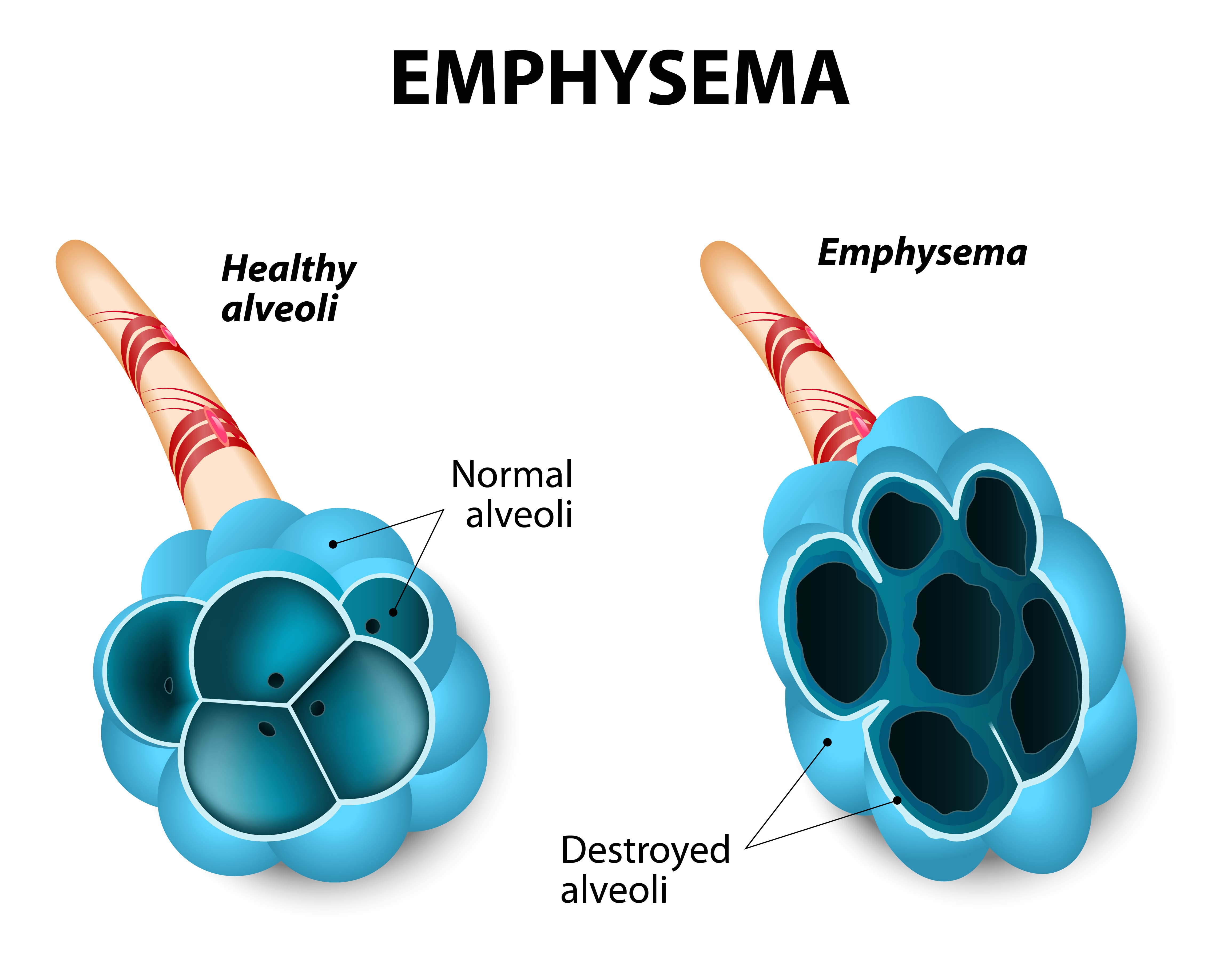
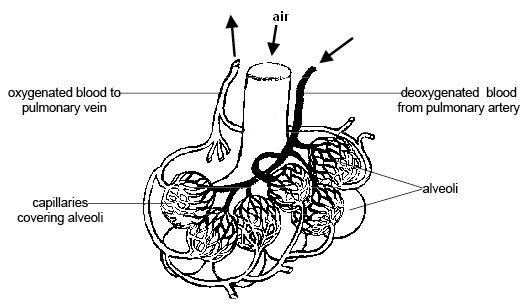
According to the Cleveland Clinic, about 3 million people have emphysema in the United States. It’s one of the diseases under the umbrella term “COPD” and it’s characterized by swollen and damaged alveoli, the tiny air sacs in the lung that are responsible for the transfer of oxygen and carbon dioxide to and from the blood.
One of the primary symptoms of emphysema is breathlessness. As the air sacs in the lungs become inflamed, they lose a lot of their elasticity and they begin to trap air inside the lungs. This stagnant air, also known as “dead-space ventilation,” prevents new, oxygen-rich air from entering the lungs making it very difficult to get the oxygen your body needs.
While it may sound counterintuitive, endobronchial valves actually block off a portion of the lungs that are most damaged by emphysema. By doing so, medical professionals can actually improve the mechanical efficiency of the lungs meaning it will take less energy and effort to breathe. Endobronchial valves are one-way, meaning inspired air is redirected to healthy parts of the lungs but carbon dioxide-rich air is still able to escape from the damaged part.
One of the greatest benefits of endobronchial valves is that they are an effective alternative to other more invasive procedures such as lung volume reduction surgery and lung transplant surgery. Lung volume reduction is a procedure that surgically removes the damaged tissue in the lungs while lung transplants are a full replacement of both lungs. Either way, these procedures are extremely invasive and they can be very costly as well.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
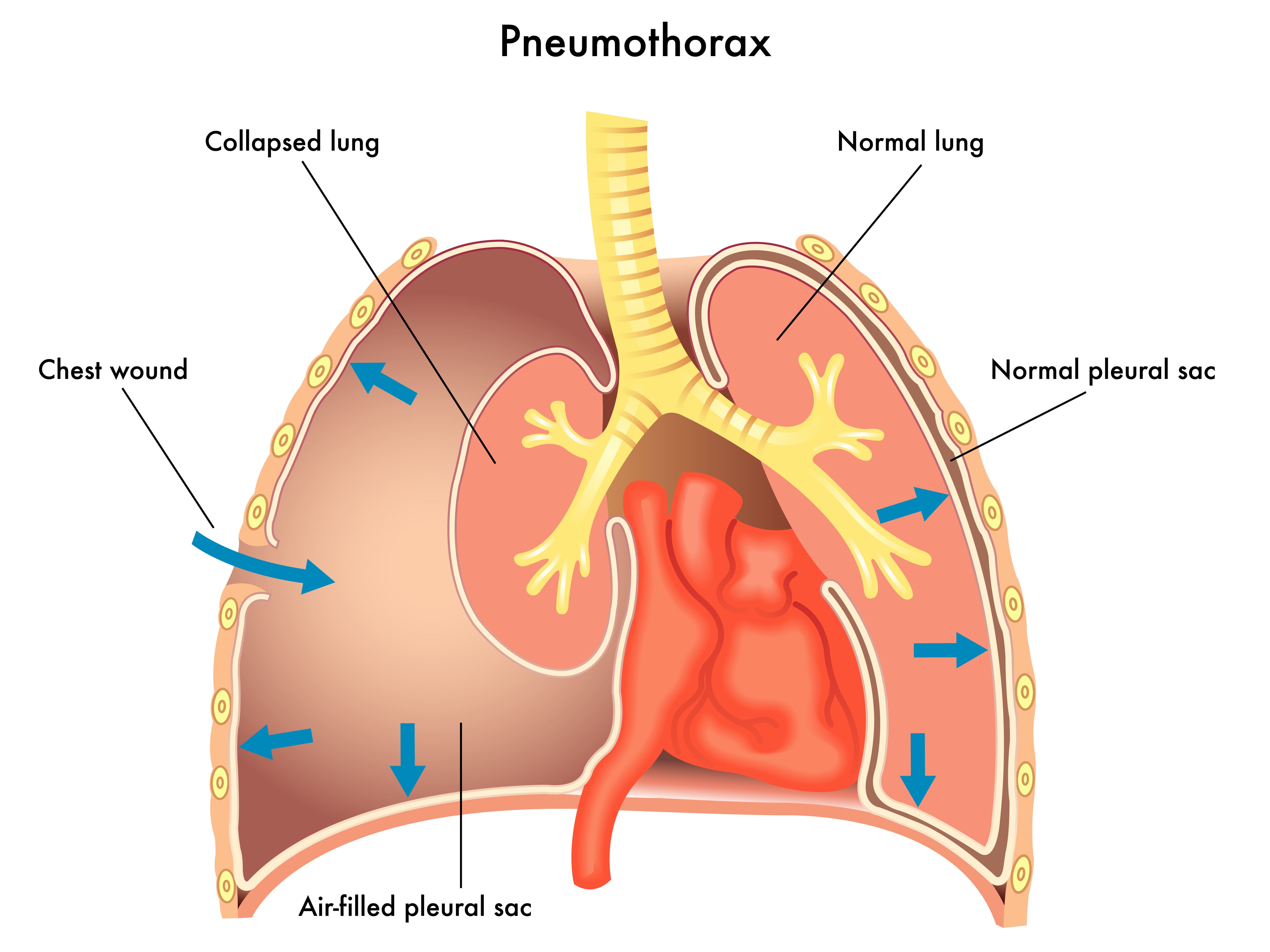
With that being said, endobronchial valves are not without their problems as well. While they have been proven to increase Forced Expiratory Volume (FEV1) for many patients, there isn’t enough information to verify its efficacy for all patients. The number one complication associated with these valves is pneumothorax, a condition where the lungs partially or fully collapse. The good news is that endobronchial valves can be quickly and easily removed if this risk is identified.
There are several other implantable medical devices that can be used for lung volume reduction in emphysema patients. Endobronchial coils, for example, are implanted through a similar process as endobronchial valves, and they’re intended to prevent hyperinflation of the lungs. Intrabronchial valves are another device with a similar function to endobronchial valves but they’re typically used to manage post-operative air leaks and allow mucus to clear correctly.
Targeted Lung Denervation (TLD)
Targeted lung denervation is another type of bronchoscopic therapy that can be used to treat COPD. During this procedure, a specialized catheter is inserted into the main bronchial pathway. At the end of this catheter is an electrode that emits RF frequency. Ultimately, the goal is to interrupt nerve transmissions which has a permanent bronchodilatory effect. It also reduces mucus production and decreases airway inflammation through the reduction of acetylcholine. This neurotransmitter is known to affect mucus secretion, inflammation, and muscle tone.
According to studies published in Healio, a medical journal, targeted lung denervation is associated with a lower risk of COPD exacerbation and lower hospital admittance after a 1-year period. Another study found that targeted lung denervation therapy was just as effective as long-acted inhaled anticholinergic therapy (drugs that block these neurotransmitters) and there were no noted adverse side-effects either. We’ll likely need to see more thorough studies of this procedure before it becomes a major treatment option for COPD patients.
Bronchoscopy Thermal Vapor Ablation (BTVA)
Yet another lung volume reduction technique, bronchoscopy thermal vapor ablation helps to limit hyperinflation in emphysema patients. Studies have shown that this method can be particularly useful in treating patients with upper lobe-predominant emphysema by improving lung function, exercise capacity, and quality of life.
Prior to the procedure, medical specialists will use a specialized program that’s designed to target the most emphysemic areas of the lungs. Once these areas are located, a catheter is applied that delivers heated water vapor. This results in a thermal reaction and immune response which leads to permanent fibrosis and atelectasis. This has a similar effect to other lung volume reduction techniques by reducing tissue and air volume and improving lung mechanics.
Typically, BTVA is done under deep sedation or general anesthesia and patients are monitored for a minimum of 24 hours after the procedure. Periodic checkups are advised for at least three to six months after the procedure to ensure no complications occur. While future studies are needed, BTVA has been proven to have a favorable benefit-risk in patients with heterogeneous emphysema.
Bronchial Rheoplasty
Not all bronchoscopy therapies are aimed at lung volume reduction. Bronchial rhinoplasty, for example, is used for patients with chronic bronchitis who are experiencing increased mucus production. Mucus can be a serious problem for COPD patients because the cilia which typically clear mucus from the airways is usually impaired or damaged due to chronic inflammation. Additionally, many patients, especially those with stage 3 or stage 4 COPD, are unable to perform mucus clearing techniques such as huff cough.
.jpg)
Bronchial rhinoplasty is a procedure that involves targeting cells that are producing excess mucus and applying electrical currents. This results in mucus-producing cells dying off and being replaced with healthier ones. In the fall of 2019, the RheOx Bronchial Rheoplasty system was granted Breakthrough Device Designation by the FDA, representing a significant step forward for bronchial rhinoplasty.
Robotic Lung Volume Reduction Surgery
In early 2019, the first-ever robotic lung volume reduction surgery was performed in Northwestern Memorial Hospital using the da Vinci Xi Surgical System. This system was developed by Intuitive, a company that’s been at the forefront of surgical robotics for over 20 years.

The reason this is such a significant breakthrough is that it is far less invasive than traditional lung volume reduction surgery. According to OR Today, RLVRS requires only three 8-millimeter incisions on the chest in order to remove damaged tissue in the lungs. This is much smaller than the incision required in the traditional surgery meaning it can effectively reduce scarring and pain for the patient.
Another benefit of robotic surgery is that it significantly reduces the risk of collateral damage. According to the Journal of Robotic Surgery, robotic surgery provides surgeons with a number of benefits over traditional surgery like improved depth perception and steadier incisions. Robotic surgery enables surgeons to work around tissues or organs rather than having to cut through them.
Interleukin-5 (IL-5) Antagonists
Oftentimes, standard COPD treatment options don’t work on certain patients. In this case, doctors need to perform more tests in order to better understand their condition. For example, your doctor can use blood tests to determine if you have eosinophilia or not. This results when there are a high number of white blood cells called eosinophils in your blood. According to this report, one-third of all COPD patients show signs of eosinophilia.
The problem with a high eosinophil count is that it is likely a significant contributor to airway inflammation. They have been associated with an increased risk of exacerbations as well as reduced lung function in both COPD and asthma patients. Interleukin-5 (IL-5) antagonists are a developing class of drugs that are specifically designed to target the IL-5 receptor in the body, thus reducing the release of eosinophils.
Like with most of the therapies on this list, we will need to see more evidence before IL-5 antagonists become a major part of COPD treatment plans. IL-5s have been used to treat asthma for several years, but we don’t have a significant enough body of evidence to prove its efficacy and safety when treating COPD.
Conclusion
As you can see, there are a number of exciting medical breakthroughs for emphysema and chronic bronchitis patients to follow. In the past, respiratory patients have typically been prescribed a standardized treatment plan. However, with more advanced testing methods, doctors are able to divide their patients into smaller groups with more specialized treatment regimens.
Whether you’ve just been diagnosed with COPD or you’re well-acquainted with your COPD treatment plan, it’s worth addressing these new therapies with your doctor. There may be additional opportunities for further testing, allowing you to better understand your disease and benefit from treatments that are not yet widely available. Clinicaltrials.gov is another great resource if you’d like to learn about getting involved with new therapies and medications.
Because COPD is a breathing disorder, most of the symptoms of the disease are caused by not being able to get enough oxygen when you breathe. However, there is another, equally serious breathing problem that COPD patients face, which is not exhaling enough carbon dioxide (CO2) when they breathe—known as CO2 retention.
When this happens, it allows excess carbon dioxide to build up in your blood, which can cause serious symptoms and make it more difficult to breathe. Although it is most likely to happen to patients suffering from severe COPD, anyone with the disease, especially those using supplemental oxygen, are at risk for CO2 retention.
In this post, we're going to explain how carbon dioxide retention happens and how it affects your health and your COPD. We'll also give you tips on how to avoid CO2 retention and how to recognize the signs in case it ever happens to you.
How Does CO2 Retention Happen?
COPD causes your airways to get narrowed and obstructed, which makes it more difficult for air to flow through. This, along with the damage to the air sacs in your lungs, causes the majority of COPD symptoms like coughing, wheezing, and shortness of breath.
Sometimes, the same airway obstruction that makes it difficult to inhale enough oxygen in also makes it difficult to exhale effectively. And because you release carbon dioxide—a waste product—when you exhale, breathing out is just as important as breathing in.
How Your Lungs Process Oxygen and Carbon Dioxide
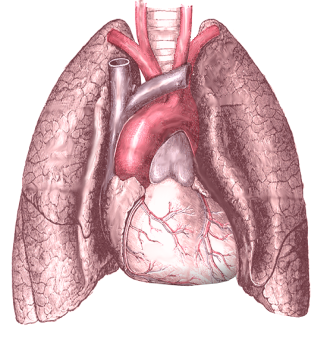
Breathing is about maintaining a balance between oxygen and carbon dioxide; you take in oxygen when you inhale, and breathe out carbon dioxide when you exhale. These gases are both carried by your red blood cells, which cart them to and from your lungs.
The first, oxygen, is an important fuel that all the cells in your body need a constant supply of in order to survive. The other, carbon dioxide, is a waste product that your body gets rid of in order to make room for more oxygen.
When you breathe in, empty-handed red blood cells pick up oxygen molecules from your lungs before beginning their journey to carry that oxygen all around your whole body. This exchange between your blood and the oxygen in your lungs happens in the alveoli, or the tiny air sacs in the lungs.
As the oxygen gets used up by the different organs and cells in your body, it gets turned into the waste product carbon dioxide. Then, the cells hand off this CO2 to empty-handed red blood cells in your bloodstream, which then carry the CO2 back to the air sacs in your lungs.
Then, before you exhale, all of those CO2-carrying red blood cells release their carbon dioxide into your lungs. When you breathe out, you exhale all of that CO2, and the red blood cells, empty-handed once more, are ready to pick up more oxygen the next time you inhale.
Why COPD Causes CO2 Retention

COPD can disrupt the process described above by preventing you from getting rid of enough carbon dioxide when you breathe. It does this in two ways: by destroying the tiny air sacs in your lungs, and by preventing you from pushing all of the air out of your lungs when you exhale.
COPD can make it difficult to breathe out because of airway narrowing, blockage, and other changes in the lungs. This leaves excess CO2 trapped in your lungs after you exhale, which takes up space that is needed to hold oxygen-rich air when you breathe in.
COPD also damages and destroys your air sacs, or alveoli, which is where oxygen and carbon dioxide is passed between your blood and the air in your lungs. When you have COPD, there are fewer healthy alveoli and fewer places for this exchange to happen, which makes it difficult to get enough oxygen into your blood and also difficult to get enough CO2 out of your blood and into your lungs.
Over time, as your COPD progresses and your lung function declines, you may retain more and more carbon dioxide as you breathe. As that excess CO2 builds up in your blood, it causes an imbalance between your blood oxygen and carbon dioxide levels, which can cause serious symptoms and oxygen deprivation.
Co2 retention also happens through a phenomenon known as ventilation-perfusion mismatch. This happens when your body gets confused about which parts of your lungs to prioritize, which reduces the efficiency of gas exchange in your lungs.
Usually, your lungs constrict your blood vessels in such a way that they decrease the amount of blood that flows to poorly functioning air sacs that have been damaged by COPD. At the same time, they increase blood flow to the most healthy alveoli so they can absorb as much oxygen (and release as much carbon dioxide) as possible.
However, this ventilation-perfusion ratio can get thrown off, usually because of high-flow oxygen therapy, COPD exacerbations, or other COPD symptoms. That causes this blood flow strategy in the lungs to break down; less blood flows to the parts of the lungs that function efficiently, and more blood flows through damaged alveoli that are less capable (or completely incapable) of exchanging oxygen and carbon dioxide efficiently.
The result is low blood oxygen levels (hypoxemia) and high blood carbon dioxide levels (hypercapnea) that make it more and more difficult to breathe. When mild, this can often be corrected with supplemental oxygen therapy and other COPD medications, however, it can be caused by improperly-dosed oxygen therapy, as well.
Why CO2 Retention is Dangerous

When too much CO2 is trapped or “retained” in your lungs after you exhale, it makes it much harder to breathe. This is partially because oxygen-rich air that enters your lungs when you inhale mixes with the leftover CO2, diluting the oxygen concentration of the air in your lungs and making it more difficult for the air sacs to absorb enough oxygen.
Another problem is that the excess CO2 gets picked up by empty-handed red blood cells and re-absorbed back into your blood. Since red blood cells can only hold one gas at a time, it leaves fewer red blood cells free to pick up oxygen when you breathe in.
The problem can get worse as more and more CO2 builds up in your bloodstream, making it harder and harder to absorb oxygen from your lungs. If your blood CO2 gets too high, it's known as hypercapnea, and it can lead to serious breathing problems and dangerously low levels of oxygen in your blood.
Because of this, the main symptoms of hypercapnea overlap with the symptoms caused by hypoxemia, which happens when your blood oxygen saturation gets too low. If left untreated for too long, hypercapnea-related hypoxemia can cause serious health complications, including respiratory failure and death.
However, CO2 retention poses a more immediate risk of making your COPD more difficult to manage and making symptoms like coughing, wheezing, and shortness of breath worse. You are more likely to experience hypercapnea during symptom flare-ups, respiratory illnesses, and COPD exacerbations, but CO2 retention can also happen slowly and gradually over time.
In fact, the early symptoms of CO2 retention may be so mild or non-existent that you don't notice them until it gets much worse. That's why it's important to understand what CO2 retention is, how it happens, and how to recognize it; the sooner you realize it's happening, the sooner you can seek treatment and get your COPD back under control.
Left unchecked for too long, CO2 retention deprives your body of oxygen, which can cause serious health problems like heart disease, pulmonary hypertension, and cognitive dysfunction. If it gets too bad, severe hypercapnea can cause respiratory failure, organ damage, and death.
Respiratory failure happens when you have so much CO2 in your blood that it raises your blood's acidity beyond healthy levels. This is a condition known as acute respiratory acidosis, and it is is a life-threatening medical emergency.
A less severe form of respiratory acidosis, known as chronic respiratory acidosis, can happen gradually over time. It does not pose as immediate a risk as acute respiratory acidosis, and, because it happens little by little, the body adapts to the blood's acidity. This makes the symptoms are subtle, if noticeable at all.
If you have COPD and are worried about CO2 retention, hypercapnea, or chronic respiratory acidosis, then ask your doctor to take another look at your blood oxygen, CO2 levels, and your lung function tests (he should already do this at your regular appointments). Always tell your doctor about any new symptoms you have, even if they are mild, and don't be afraid to discuss any concerns you have about your health.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The Symptoms of CO2 Retention and Hypercapnea

The first symptoms of CO2 retention or hypercapnea are usually headaches, breathlessness, drowsiness, and lack of energy. These symptoms happen because you can't absorb enough oxygen and your blood oxygen saturation gets low.
As it gets worse, hypercapnea can cause difficulty thinking and concentrating, confusion, and muscle twitches. In serious cases, it can cause severe oxygen deprivation which leads to swelling in the hands and feet (edema), a bluish tint to the skin (especially fingers and lips), seizures, coma, respiratory failure, and death.
Here is a list of some of the general symptoms of CO2 retention:
- Mild headaches
- Feelings of drowsiness, fogginess, or sleepiness
- Lack of energy or fatigue
- Inability to focus or think straight
- Feeling dizzy or disoriented
- Shortness of breath
Here is a list of the more severe symptoms of hypercapnea:
- Unexplained confusion
- Abnormal muscle twitching
- Abnormal depression or paranoia
- Irregular heartbeat
- Bluish tint to the skin and lips
- Swollen hands and feet (edema)
- Hyperventilation
- Seizures
- Loss of consciousness
These symptoms can occur quickly or happen gradually over time. If you experience mild symptoms for more than a couple of days, then you should schedule an appointment to see your doctor. If your symptoms are severe, then you should seek medical attention at an emergency room immediately.
Causes of CO2 Retention for People with COPD
As we discussed, CO2 retention is often caused by airway obstruction, damaged lung tissue, and ventilation-perfusion mismatch in the lungs. However, there are a variety of other things that can make CO2 retention worse.
Oxygen Therapy

A common cause of CO2 retention is supplemental oxygen therapy. If your oxygen dosage is wrong or you get too much oxygen for any other reason, it can cause too much CO2 to build up in your blood.
This happens because, when you get excess oxygen with every breath, it can cause red blood cells to drop carbon dioxide to pick up oxygen instead. As a result, the dropped CO2 dissolves into your blood instead of getting released into your lungs for expulsion.
This dramatically throws off the balance of oxygen and carbon dioxide exchange in your lungs, causing more and more CO2 to build up in your bloodstream. In this way, portable or home oxygen therapy can make CO2 retention much worse and cause hypercapnea when prescribed or used incorrectly.
Another way that oxygen therapy can worsen CO2 retention is by causing ventilation-perfusion mismatch. Although researchers aren't sure exactly why, this happens when you get more oxygen at a time than what you actually need.
The best way to avoid oxygen therapy-induced CO2 retention is to follow your oxygen prescription exactly. To reduce the chances of hypercapnea, your doctor should prescribe you enough oxygen to keep your blood oxygen saturation at about 90 percent, but not much higher.
If you are worried about CO2 retention, you can always have your doctor check to make sure your flow rate is adjusted correctly and that you are using your equipment properly. Then, it's up to you to follow your doctor's instructions and only use your oxygen as often as your doctor recommends.
Emphysema

Severe emphysema is another major cause of CO2 retention in people with COPD. Emphysema causes your lungs to become enlarged and less stretchy (a condition known as lung hyperinflation), which makes it more difficult to push all of the air out of your lungs when you exhale.
Lungs with emphysema tend to trap lots of air, which makes it difficult to breathe and absorb enough oxygen as well as expel enough CO2. This puts patients with emphysema at an increased risk of hypercapnea, especially during heavy exercise, which forces your lungs to get rid of even more CO2.
That's why doctors recommend breathing exercises like pursed-lips breathing and diaphragmic breathing to help you train yourself how to empty your lungs more completely when you exhale. These can be especially helpful during exercise and physical activity to reduce and prevent shortness of breath.
It is also important to follow your COPD treatment plan carefully to minimize your symptoms. The better you keep your symptoms and breathing under control, the better you can prevent air from getting trapped in your lungs, reduce hyperinflation, and prevent hypercapnea.
Some patients with severe emphysema may be eligible for lung reduction surgery if their lungs are significantly enlarged. By reducing the volume of the lungs, the surgery makes it easier to push all the air out when you exhale, preventing CO2 retention and making it easier to breathe.
To learn more about breathing exercises you can practice to improve your COPD, see our previous article on COPD breathing techniques here.
Eating Too Many Carbohydrates

Believe it or not, the foods that you eat can have a significant effect on CO2 retention in your lungs. That's because, whenever your body digests food, it turns it into two main things: energy, and carbon dioxide waste.
The carbon dioxide waste has to be processed through your lungs so that you can exhale it out of your body. Some foods, however, create extra carbon dioxide waste that puts unnecessary strain on your lungs.
The main culprits for this are foods high in carbohydrates, which create more CO2 waste than other foods when your body breaks them down. When you have COPD and your lungs are already struggling to function efficiently, this excess CO2 can be enough to tip the balance in your lungs and cause you to retain too much CO2.
Because of this, doctors often recommend that people with COPD limit the amount of carbohydrates in their diets. That includes grains, pastas, breads, and especially simple sugars and processed foods high in carbs.
While a certain amount of carbs are still healthy, you should try to limit yourself to healthy sources of complex carbohydrates and be careful not to eat more than you need. Instead, replace carbohydrates in your diet with more foods that are high in lean protein and healthy fats.
According to US dietary guidelines for older adults, you should eat about 5-7 ounces of grains every day, at least half of which should come from whole-grain sources. However, it is easy to exceed this amount if you eat a lot of breads, pastas, cereals, or processed foods.
Shallow Breathing

When you take too short or too shallow of breaths, your lungs have a hard time getting rid of enough CO2. That's why it's important to keep your breathing under control and practice breathing exercises if you have COPD.
Many COPD patients tend to take more shallow breaths whenever they feel like they're having trouble breathing, such as during bouts of breathlessness or coughing. Unfortunately, that just makes the problem worse by making it easier for air and CO2 to stay trapped in your lungs.
This happens because shallow breathing only uses the upper part of your lungs, which is why it is sometimes referred to as “top breathing.” As a result, stale air stays in the lower parts of your lungs, which leads to CO2 retention and makes it harder to breathe.
You can counteract this, however, by practicing breathing exercises in your spare time and remembering to use them when you feel short of breath. Exercises like diaphragmic breathing and pursed-lips breathing are especially helpful for training yourself to take deep, full breaths and push all the air out of your lungs when you exhale.
It also helps to strengthen your breathing muscles, which you can also do with aerobic exercise, wind instruments, and other forms of physical activity. You can even join special COPD exercise and therapy classes designed to help you improve your breathing, including pulmonary rehabilitation and music therapy courses.
Conclusion
COPD is a complicated breathing disorder that can lead to a variety of different symptoms and health complications. Because of the complex nature of the disease, many patients struggle to understand how their blood oxygen levels, blood CO2 levels, and their symptoms are all connected.
Hopefully, after reading this article, you have a better understanding of how your lungs function and how CO2 retention works. You should also be better able to recognize the signs of hypercapnea and how to protect yourself from factors that put you at risk.
If you use supplemental oxygen therapy, it's particularly important to know the symptoms of CO2 retention and the dangers of getting too much oxygen. If you catch the early signs, you can work with your doctor to adjust your oxygen delivery before it causes any serious problems. It's important to fully understand oxygen therapy benefits and oxygen therapy side effects before you get started.
COPD is sometimes a difficult disease to manage, but with the right knowledge, a good treatment plan, and the support of a good medical team, you can successfully keep your symptoms and CO2 retention under control. That's why it's important to learn everything you can about COPD and what you can do to keep your lungs as healthy as possible.

We’ve all experienced what it’s like to be burnt out on something. Whether it’s your job, chores, or health routine, it’s not always easy to find a way to stay on track to meet your goals. What complicates this even further is that everyone experiences this for a different reason. For some people, it’s just a matter of learning how to stick to a routine, but for others, it could be a lack of mental or physical energy that’s holding them back.
Oftentimes, when people are trying to stick to a COPD treatment plan, the latter is true. After all, fatigue is the second most common symptom of COPD with about 50% of patients experiencing it. Knowing this information, it’s not hard to see why it can be difficult to stick to a routine. If you’re hit with a sudden wave of fatigue, grogginess, or breathlessness, it can make simple tasks seem overwhelming. Eventually, your health goals will seem unattainable and unrealistic.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In this post, we’re going to provide you with some tips for having a fresh perspective on your COPD treatment plan. Regardless of the stage of COPD that you’re in, it’s never too early or too late to hit the reset button and start managing your COPD symptoms proactively. If you have any questions, feel free to leave them in the comment section below and we’ll get back to you.
Change Up Your Exercise Routine
As a COPD patient, you know how important your exercise routine is. While exercise does not magically reverse the effects of lung damage, it improves the efficiency of your body and lungs which inevitably leads to less breathlessness, less chronic pain, and a longer life expectancy. But you know as well as anyone that exercise routines are difficult to stick to, especially if you viewed it as a “chore” in the first place.

More often than not, COPD patients are taught how to exercise through a pulmonary rehabilitation program. These programs are aimed at educating patients about their lungs and disease, then applying exercise techniques that allow them to lead a happier life. Unfortunately, pulmonary rehabilitation programs don’t teach you how to make your exercise routine “interesting” or “engaging.” They simply tell you what needs to be done. As a result, many people find themselves in a situation a year or two down the road where they don’t have the motivation to continue.

At some point, you’re going to want to try new exercises that hold your interest. The important thing to remember is that you still need to follow the guidelines that you learned in pulmonary rehabilitation because this will ensure that you are making the most of your time and avoid injury. For example, if you implement a new exercise, you need to make sure it works the same muscle group and that it’s a similar intensity as your original exercise. If you have any doubts about it, you can always reach out to your doctor with any questions you may have.
Make Adjustments to Your Diet
What you eat also has a major impact on your ability to live a comfortable life with COPD. Unfortunately, your diet is also something that can become mundane if you’re eating the same things every day. Like with exercising, it’s okay to make changes to your diet, you just need to make sure that you’re getting the right nutrients. You also need to ensure that you aren’t increasing or decreasing your caloric intake too much. According to the COPD Foundation, breathing with COPD takes more energy than for a healthy individual, so you need to maintain your caloric intake.

Most COPD patients need a high protein intake. Protein plays an essential role in the structure, function, and regulation of body tissues. Most notably, protein helps you build muscle and counteract muscle atrophy which is common in COPD patients. Maintaining muscle mass is important for respiratory patients because strong muscles take less oxygen to function, thus reducing the burden on your lungs. While you probably get most of your protein through meat, there are many other great sources of protein, including but not limited to fish, eggs, dairy products, nuts, and beans.
You might think of fats as being “unhealthy.” But you may be surprised to find that many COPD patients are prescribed high-fat diets. The problem is that many people don’t know the difference between healthy fats and unhealthy fats. Unhealthy fats like saturated fat or trans fat include things like beef or pork fat, margarine, butter, and shortening. Eating too many of these things can lead to increased blood cholesterol levels and LDL cholesterol levels. Healthy fats, on the other hand, like monounsaturated fats and polyunsaturated fats include avocados, olives, nuts, olive oil, and more. Fatty fish like salmon is also a great source of healthy fats like omega-3.
While it may seem like COPD diets are pretty restricted, this is not necessarily the case. It’s important to avoid foods that are high in added sugars, sodium, and unhealthy fats. However, aside from that, you simply need to meet your minimum caloric intake for the day and any other requirements that your doctor sets. You still have plenty of freedom to choose what you eat and switching up your meals can even keep you on track for meeting your goals by preventing burnout.
Upgrade to a Portable Oxygen Concentrator
After being prescribed oxygen, many people choose the first oxygen device they think of — oxygen tanks. Most people know about oxygen tanks and they’ve seen people use them. But that doesn’t mean they’re the best option for you and your lifestyle. Although oxygen tanks are a popular choice, they tend to be heavy and bulky meaning they are difficult to maneuver. Fortunately, there is an alternative known as portable oxygen concentrators.

A portable oxygen concentrator is unlike an oxygen tank in that it doesn’t hold oxygen within the unit. Rather, it takes in ambient air, removes nitrogen and argon, and puts out medical-grade oxygen. POCs are electronic devices and they run off of powerful lithium-ion batteries, so you simply need to charge the battery via a car or wall outlet and you’ll be on your way. The most notable benefit of this is that you won’t have to keep going out of your way to refill or replace your oxygen tanks when they run out.
Another benefit of portable oxygen concentrators is their lightweight and compact design. Unlike oxygen tanks which are oblong-shaped, POCs are small enough and light enough to be carried on your shoulder. This opens up a world of possibilities and enables you the freedom to live life on your own terms without being defined by your disease. Inevitably, this leads to more options for you and a lower chance of experiencing burnout with your COPD treatment plan.
Reduce the Clutter
Sometimes it’s not our COPD treatment plan itself that’s causing us to feel burnt out, but all the extra clutter around us. The term “clutter” can be defined as anything that complicates our lives and occupies our thoughts but doesn’t provide any real benefit to us. If you live with clutter too long it can really start to become exhausting and you’ll notice yourself losing motivation in other areas of life such as your exercise routine, diet, and making it to doctor’s visits.

For some people, this might imply clutter within the home. For example, having a messy bedroom, bathroom, or kitchen can lead to a lot of discomfort in your daily life, and as a result, you might find yourself too distracted to follow your COPD treatment plan. Eliminating physical clutter like this is as simple as taking the time each day to organize your home and avoid getting to the point where it’s too much to manage. If you’re too busy to clean, you might consider hiring a caretaker who can help out around the home.

Another type of clutter is “mental clutter.” Think of this as the opposite of mental clarity. Instead of being able to concentrate on what you’re doing in the current moment, your thoughts are always wandering to something else. Mental clutter can certainly be caused by things like a messy home, but it’s more likely to be caused by something that takes your focus off of what you’re doing in the present moment. For example, watching the news for too long or spending too much time on social media are both things that can take your focus off the present moment.

Cognitive behavioral therapy (CBT) is one way of dealing with problems related to mental clarity. This is a type of therapy that’s focused on reversing negative or unproductive thought processes. CBT has become very common among people with chronic conditions like COPD as awareness around mental health problems has increased. During CBT, you will work one-on-one with a certified therapist who will guide you through the process.
Practice Meditation
Meditation comes in many different forms. However, in most cases, the goal is always to achieve a state of mental clarity and well-being. Meditation helps train your mind to think clearly and without distractions. It also promotes emotional well-being while reducing anxiety and in some cases even improving physical well-being. By far the most popular form of meditation for COPD patients is Tai Chi. This practice combines traditional meditation principles with martial arts. It’s popular for COPD patients because it teaches you to control your thoughts, breathing, and balance, all of which are important if you’re trying to improve your health. Read through this post we made about Tai Chi to learn more.

Speak With Your Doctor
Your doctor should be your first point of contact when it comes to anything related to your COPD treatment plan. If you know that you need to make changes, your doctor will be able to tell you what changes are acceptable and which are not. He/she may also be able to provide you with additional resources or direct you to another specialist who can help you deal with issues related to COPD burnout and fatigue. Sometimes burnout is due to poor sleep quality, so he/she may recommend that you get tested for obstructive sleep apnea (OSA) and other sleep disorders.

Another change your doctor may be able to do is make changes to your medication routine. Corticosteroids are one of the most common drugs used to treat COPD because they reduce inflammation in the lungs. However, these drugs are also known to have adverse psychiatric effects such as mania, depression, and cognitive impairments, all of which can contribute to burnout and a negative outlook of your disease. Your doctor may be able to reduce your dosage or prescribe you a different medication altogether.
Conclusion
Being “burnt out” on your COPD routine can be exhausting. On one hand, you may be tempted to revert to your old way of living and entirely forget about your COPD treatment plan. However, on the other hand, you understand that the best way to deal with the symptoms of your disease is through persistence and consistency. If you feel like you’ve reached this point, be sure to try some of the tips above to get back on track.
Ultimately, you will want to consult your doctor if you’re struggling to keep up with your treatment plan. It’s not unusual for someone to struggle, especially if they’ve had COPD for many years. Here at LPT Medical, we strongly believe that a portable oxygen concentrator can help you regain much of the freedom that you lost after being diagnosed with COPD. As a result, you’ll be able to approach your treatment plan from more angles and prevent burnout.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
We sell some of the top-rated portable oxygen concentrators in the industry such as the Caire FreeStyle Comfort, Inogen One G5, and the GCE Zen-O Lite. When you contact one of our oxygen concentrator specialists, they will work with you one-on-one to understand your needs and align you with a concentrator that matches them. We also have many different buying and financing options to help you manage payments in a way that works with your budget. To get started, simply give us a call or send us an email.
.png)
If you’ve already read our blog on treating and overcoming sleep apnea, you know that sleep apnea is a common disorder with potentially serious implications. While sleep apnea symptoms may seem mild at first, over time, obstructive sleep apnea may eventually lead to increased blood pressure, heart disease, liver disease, depression, and more.
But when sleep apnea is combined with other conditions like chronic obstructive pulmonary disease (COPD) , it’s often a two-way road. According to a new study called Canadian Cohort Obstructive Lung Disease (CanCOLD), sleep disruptions — like those experienced in sleep apnea — could lead to a greater risk of long-term COPD exacerbations.
Led by researchers at Montreal’s McGill University, this ongoing study aims to analyze over 2,000 Canadians with mild to severe COPD. Whereas previous trials have shown that COPD symptoms may lead to sleep disturbances, this study will help medical professionals better understand the characteristics of COPD and how they’re affected by a poor night’s sleep.
Using the Pittsburgh Sleep Quality Index (PSQI) and negative binomial regression, the team observed data from 480 participants over an 18-month assessment period. During this time, 185 of the participants experienced at least one exacerbation and 203 had a baseline PSQI score over five, indicating that the participant had a poor night’s sleep. The study also concluded that both symptom- and event-based exacerbation risks were associated with a higher PSQI score.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What We Can Take Away From The Study
When it comes to other major causes of death like cancer and heart disease, COPD awareness remains low both in the United States and around the world. Studies on COPD are often overshadowed by discussions about lung cancer and other respiratory conditions. However, this study may help bring some much-needed awareness to a condition that so many people suffer with.
Unlike acute illnesses, chronic conditions like COPD progress slowly and oftentimes without any cause for concern. You may have started to develop COPD years ago but brushed off your symptoms as “getting old” or “being out of shape.” This study reaffirms the importance of getting checked regularly for both healthy lung function and sleep quality.
Sleep Quality Matters
It’s easy to dismiss a bad night’s sleep as unimportant or insignificant, but when this issue persists, it’s almost always linked to an underlying condition. And even when it isn’t, feelings of restlessness and chronic fatigue can have an impact on the severity and frequency of your COPD symptoms and exacerbations. What’s more, if you’re sleepy frequently, it will make it significantly more difficult to deal with the daily struggles of managing COPD.

As such, it’s important to take all necessary precautions to ensure that you sleep well and aren’t disturbed. First and foremost, you should make sure that you get an adequate amount of sleep each night. According to the National Sleep Foundation, adults between the ages of 24 and 64 should get between 7 to 9 hours of sleep and anyone older than 65 should get at least 7 to 8 hours of sleep. Let’s take a look at some tips for getting a better night’s sleep.
Sleep-Wake-Time Consistency
Researchers have studied sleep extensively and one of the most common rules they stress is creating a sleep routine and sticking with it. Many people will tell you that you need to get up as early as possible and that staying up late is a problem. But in reality, you simply want to pick a schedule and follow it every day of the week.
Avoiding Screens Before Bed
Technology helps us all lead more productive lives and has allowed us to learn more about the world than any other time in human history. But staring at a screen right before bed may have the opposite effect. According to the National Sleep Foundation, using electronics before bed delays the circadian rhythm in your body and slows the release of melatonin (the sleep-inducing hormone in the brain) making it harder to fall asleep when you need to.
Calcium and Magnesium Levels
Magnesium is an essential mineral that’s responsible for 300 biochemical reactions in the body. It’s one of the most important minerals in the body, helping to maintain a healthy immune system, strong bones, and muscle function. And if there isn’t enough magnesium in the body to absorb calcium, it can lead to weak bones and digestion problems. Additionally, calcium is responsible for tightening and tensing muscles and nerves while magnesium calms and relaxes them. So, having this balance is essential for deep and restful sleep.

Some foods high in magnesium include:
- Whole wheat
- Spinach
- Quinoa
- Peanuts, cashews, and almonds
- Dark chocolate
- Black beans
- And avocado
Functioning Adrenal System
A well-functioning adrenal system is essential to good sleep and overall well-being. The adrenal glands are located on top of each kidney and produce hormones that your body needs. In a healthy body, these hormones help manage stress, regulate metabolism, control blood pressure, and more. However, there are a variety of disorders that can negatively affect the adrenal glands resulting in an adrenal deficiency. Junk food, sugar, and caffeine are known to reduce adrenal function making you feel groggy and restless after waking up.
Blood Sugar Levels
In what is often a vicious cycle, blood sugar levels affect your sleep, and poor sleep affects your blood sugar as well. Blood sugar is regulated by what you eat and when you eat it. While it’s not a good idea to eat a heavy meal late in the day, eating too early and then not eating all evening can cause a dip in blood sugar in the middle of the night. Low blood sugar can cause you to wake with a headache or feel out of sorts, making it difficult to go back to sleep.
On the other hand, if your blood sugar is too high, your body is likely to try to rid itself of excess sugar through the kidneys causing you to wake up to use the bathroom. Many people who are trying to lose weight feel that bedtime snacks add unnecessary calories but weight loss isn’t just about calorie counting. In order to maintain a healthy metabolism, good sleep, hormone regulation, and stable blood sugar are essential.
Awareness Is Key
Maintaining a healthy sleep schedule, eating right, and avoiding sugar and caffeine before bed are all great habits to get into, but without being tested, it’s difficult to diagnose and treat any sleep disorder you may be struggling with. If you have COPD, you should speak with your doctor about having both a sleep study and an exercise test.
Sleep Studies
The easiest way to detect sleep apnea and other sleeping disorders early on is through a sleep study. Also known as a polysomnogram, a sleep study is a non-invasive procedure doctors use to analyze sleep patterns, heart rate, and brain activity in order to diagnose sleep disorders. Aside from sleep apnea, these disorders include narcolepsy, insomnia, restless leg syndrome, and more.
No matter whether you have bronchitis, emphysema, or any other lung condition, a sleep test will provide both you and your doctor with critically important information about your body, mind, and overall health. Using the test results and your medical history, your doctor will be able to narrow down the source of your sleep disruptions and determine if any actions need to be taken on your part to get a better night’s sleep.
Exercise Tests
Similar to how a sleep study will reveal crucial information about your breathing patterns while you sleep, an exercise test is useful for monitoring how your lungs function while undergoing physical exertion. If you have COPD, an exercise test will reveal the condition's effects on your physical abilities and help your doctor set up an exercise routine that’s right for you.
There are two main types of exercise test: laboratory tests and field walking tests. Patients who already have a chronic pulmonary condition may opt for a field walking test because they are able to stop and take a break, whereas laboratory tests are usually better for someone who still retains most of their physical abilities. Some exercise tests include the 6-minute walk test, the incremental shuttle walk test, the endurance shuttle walk test, and the cardio-pulmonary test. Your doctor will help you determine which one is best for you.

When used in tandem with a sleep study and your medical history, an exercise test will provide your doctor with a wide range of information about your overall health. For example, if your doctor discovers disruptions in your sleep pattern, he/she may be able to link it to an issue you experience while exercising or vise versa. This will make it easier to create a treatment plan that’s best for you.
Sleep Affects Your Overall Health
One of the major mistakes people make when approaching an issue like sleep apnea or sleep deprivation is that they treat it as an isolated issue. These people assume that the fatigue or restlessness that they feel is the extent of the effect it’s having on their bodies. Unfortunately, as the study suggests, this is not the case.

Aside from short-term symptoms like decreased performance and alertness, long-term sleep deprivation can put you at a higher risk for heart disease, high blood pressure, depression, and more. Chronic sleep deprivation can also significantly reduce your quality of life and put a strain on your relationships.
You’re at a Higher Risk With COPD
Above all, this study shows us that you’re at a higher risk of experiencing and being hospitalized for COPD exacerbations when you get poor sleep. Whether you’re suffering from chronic sleep apnea or you’re experiencing poor sleep due to anxiety or depression, you should take these issues seriously in order to avoid respiratory complications.
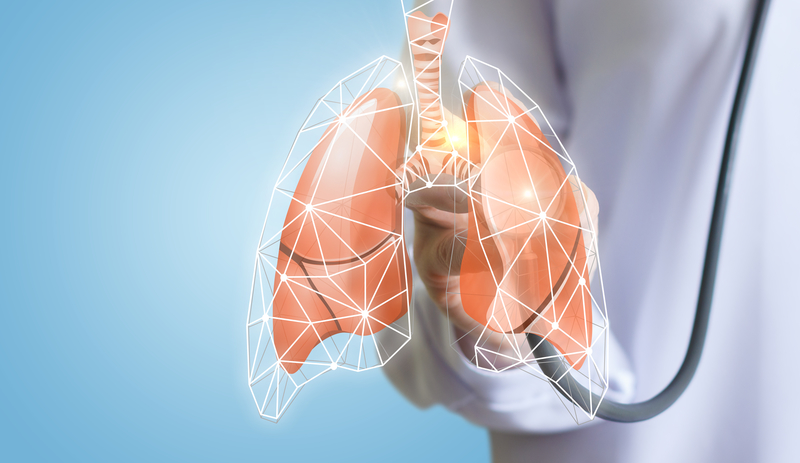
Most people tend to think of COPD exacerbation triggers as air pollutants and irritants or sicknesses like the flu or the common cold. However, according to the study, the quality of sleep you get also has an impact on when exacerbations occur and how severe they are. While COPD is manageable on its own, frequent exacerbations can take a serious toll on your health and can even be fatal.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Sleeping Disorders That Can Cause Exacerbations
Unfortunately, it’s not just poor sleep quality that increases your risk of exacerbations; sleeping disorders like sleep apnea and insomnia can also play a role while simultaneously contributing to poor sleep. Many people who have a sleeping disorder are never diagnosed because they either don’t realize they have a problem or they believe nothing can be done.
Like maintaining healthy sleep habits, diagnosing and treating sleep disorders starts with awareness. Sleep constitutes a third of our lives. And during this time, many important processes occur that are necessary for us to lead happy and healthy lives. Sure, preventing that grogginess and sleepiness when you wake up is part of it, but sleep is vital for the rest of the body as well.

According to the Mayo Clinic, your immune system is affected by lack of sleep. Proteins called cytokines are released by the immune system when your body is experiencing inflammation, stress, or infection. However, less cytokines are produced when you’re deprived of sleep. What’s more, cells and antibodies that fight infection are reduced when you don’t get enough sleep.
As a COPD patient, getting sick could lead to a serious flare up in your symptoms and even result in exacerbations due to increased mucus production and difficulty breathing. We’re going to take a look at just a few of the most common sleep disorders so that you know when to seek help.
Sleep Apnea
Sleep apnea is a condition characterized by disrupted breathing while sleeping. There are three main types of sleep apnea that you should be aware of.
- Obstructive sleep apnea is one of the most common forms of the condition and it results when throat muscles relax and block your airways.
- Central sleep apnea is the result of the muscles that control breathing not receiving proper signals from your brain.
- Complex sleep apnea is the result of having both these conditions simultaneously.
As you can imagine, these two disorders are treated in very different ways. Continuous Positive Airway Pressure (CPAP) machines are one of the most common treatment methods for obstructive sleep apnea. Unlike a normal in-home oxygen therapy device, a CPAP machine is designed to blow at a pressure that will keep your airways open and free of obstruction while you sleep. When the device is on, it creates a cushion along the upper airway preventing the tongue, uvula, and soft palate from interfering with the airway.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
When it comes to central sleep apnea, medication is often the only effective solution. Medication like theophylline or acetazolamide are used to stimulate breathing while you sleep. And if you’re on any opioid medications, your doctor may take you off these to prevent any complications.

Insomnia
Insomnia is another common sleep disorder affecting around 60 million Americans. Insomnia is defined as difficulty falling asleep or feeling dissatisfied with the quality of sleep that you do get. Many people who have insomnia are unable to fall asleep even when they’re tired and often wake up feeling groggy, fatigued, and unable to concentrate.
Depending on what is causing the insomnia, both medical and non-medical treatment methods may be used. Cognitive behavioral therapy (CBT), counseling, and group therapy may be beneficial non-pharmacological treatments while relaxation techniques, breathing exercises, and changes to your sleep schedule may help as well. Medication for insomnia includes both benzodiazepine sedatives and non-benzodiazepine sedatives.
Narcolepsy
Narcolepsy is a neurological disorder that results in an irregular regulation of sleep and wakefulness. Someone with narcolepsy may fall asleep frequently during the day and may feel sudden muscle weakness as well during any type of activity. People who experience narcolepsy may also have difficulty falling asleep or staying asleep at night due to their circadian rhythm being disrupted during the day. Although this disorder usually starts at a young age, it often goes undiagnosed in many people.
Restless Leg Syndrome (RLS)
RLS results in unpleasant feelings in the legs such as aches, tingling, burning, or general discomfort. It’s considered a neurological movement disorder and is commonly associated with periodic limb movements of sleep (PLMS), which is a similar condition that occurs while the person is asleep. For some people, this condition doesn’t have a significant impact on their ability to get a restful night’s sleep. However, restless leg syndrome almost always does.
Circadian Rhythm Disorders
We’ve talked before about the importance of the circadian rhythm in managing your sleep-wake cycle and getting a good night’s sleep. And in a circadian rhythm disorder, a person’s biological clock is out of sync, especially when it comes to external time cues like the natural dark-light cycle.

Although your sleep cycle will never be completely in sync with external cues, someone with these disorders may feel completely restless and sleepy in the middle of the day and wide awake at night making it difficult to find a sleep schedule that works for them. These disorders may eventually lead to insomnia or hypersomnia (excessive sleepiness).
What You Can Do To Avoid COPD Exacerbations
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Now that you understand how poor sleep quality and sleep disorders can lead to COPD exacerbations, you need to know exactly what steps you should take to avoid complications. While chronic sleep disorders and general sleepiness are dangerous on their own, for someone with COPD, they could lead to a life-threatening exacerbation. Fortunately, you don’t have to leave anything up to chance when it comes to your health and you can get started right away improving your sleep quality. Simply follow the steps below.
1.) Make A List of Your Symptoms
As you’re probably well aware, living with COPD or any chronic illness can be challenging. You may be following a strict diet, exercise routine, sleep schedule, and work schedule. And it’s easy to get confused as to what you should be doing and when. As such, the more you can write down on paper, the better.

One reason to make a physical list is because you may forget when it comes time to see your doctor. COPD has a long list of symptoms and most people with the condition experience them all at one point or another. The more information you have about what symptoms you’re experiencing and when, the better you and your doctor will be able to pinpoint what’s causing the exacerbation. On your list, be sure to thoroughly describe what symptoms you experienced, the date, the time, as well as details about your sleep schedule and sleep quality.
2.) Visit A Doctor
The second step in this process is to visit a doctor. As aforementioned, awareness is key when it comes to being able to effectively treat sleep disorders and COPD symptoms. If there’s any information about your symptoms that your doctor isn’t aware of, he/she may not be able to treat them effectively. Since COPD exacerbations are linked to your diet, sleep patterns, and overall health, you should try to provide a thorough overview of your symptoms.
3.) Don’t Be Afraid to Ask Questions
Chances are, you’re going to have a few questions about your symptoms and how your sleep quality may be affecting them — don’t hesitate to ask them. Although doctors have your best interest in mind, they aren’t infallible. There’s a chance they may have overlooked something when coming up with your treatment plan. And it’s important for you to understand your condition as well as possible after leaving the exam room.

For example, if you’re curious about sleep studies, exercise tests, or medication that you heard about online, it never hurts to ask your doctor if they might be a viable option. The worst that can happen is they suggest a better option and you become more educated about the condition you’re coping with.
Conclusion
For better or for worse, the quality of sleep you get at night affects the frequency and severity of COPD exacerbations you experience. Conversely, COPD symptoms like shortness of breath, coughing, and wheezing may prevent you from achieving a good night’s sleep. Understanding this two-way relationship is the first step in learning how to overcome it and live a healthier and more fulfilling life.
Although you will likely always experience some COPD symptoms, you can avoid exacerbations by making some simple lifestyle changes and being open and honest with your doctor. Additionally, taking the time to educate yourself on what triggers exacerbations will make it easier to manage the condition on a daily basis.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













