Because COPD is a breathing disorder, most of the symptoms of the disease are caused by not being able to get enough oxygen when you breathe. However, there is another, equally serious breathing problem that COPD patients face, which is not exhaling enough carbon dioxide (CO2) when they breathe—known as CO2 retention.
When this happens, it allows excess carbon dioxide to build up in your blood, which can cause serious symptoms and make it more difficult to breathe. Although it is most likely to happen to patients suffering from severe COPD, anyone with the disease, especially those using supplemental oxygen, are at risk for CO2 retention.
In this post, we're going to explain how carbon dioxide retention happens and how it affects your health and your COPD. We'll also give you tips on how to avoid CO2 retention and how to recognize the signs in case it ever happens to you.
How Does CO2 Retention Happen?
COPD causes your airways to get narrowed and obstructed, which makes it more difficult for air to flow through. This, along with the damage to the air sacs in your lungs, causes the majority of COPD symptoms like coughing, wheezing, and shortness of breath.
Sometimes, the same airway obstruction that makes it difficult to inhale enough oxygen in also makes it difficult to exhale effectively. And because you release carbon dioxide—a waste product—when you exhale, breathing out is just as important as breathing in.
How Your Lungs Process Oxygen and Carbon Dioxide
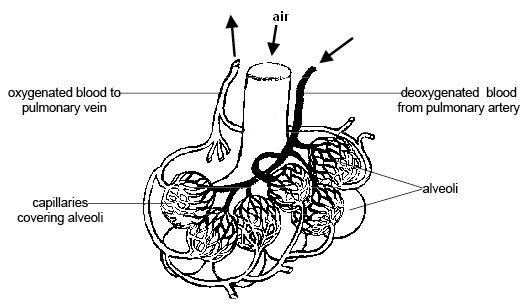
Breathing is about maintaining a balance between oxygen and carbon dioxide; you take in oxygen when you inhale, and breathe out carbon dioxide when you exhale. These gases are both carried by your red blood cells, which cart them to and from your lungs.
The first, oxygen, is an important fuel that all the cells in your body need a constant supply of in order to survive. The other, carbon dioxide, is a waste product that your body gets rid of in order to make room for more oxygen.
When you breathe in, empty-handed red blood cells pick up oxygen molecules from your lungs before beginning their journey to carry that oxygen all around your whole body. This exchange between your blood and the oxygen in your lungs happens in the alveoli, or the tiny air sacs in the lungs.
As the oxygen gets used up by the different organs and cells in your body, it gets turned into the waste product carbon dioxide. Then, the cells hand off this CO2 to empty-handed red blood cells in your bloodstream, which then carry the CO2 back to the air sacs in your lungs.
Then, before you exhale, all of those CO2-carrying red blood cells release their carbon dioxide into your lungs. When you breathe out, you exhale all of that CO2, and the red blood cells, empty-handed once more, are ready to pick up more oxygen the next time you inhale.
Why COPD Causes CO2 Retention

COPD can disrupt the process described above by preventing you from getting rid of enough carbon dioxide when you breathe. It does this in two ways: by destroying the tiny air sacs in your lungs, and by preventing you from pushing all of the air out of your lungs when you exhale.
COPD can make it difficult to breathe out because of airway narrowing, blockage, and other changes in the lungs. This leaves excess CO2 trapped in your lungs after you exhale, which takes up space that is needed to hold oxygen-rich air when you breathe in.
COPD also damages and destroys your air sacs, or alveoli, which is where oxygen and carbon dioxide is passed between your blood and the air in your lungs. When you have COPD, there are fewer healthy alveoli and fewer places for this exchange to happen, which makes it difficult to get enough oxygen into your blood and also difficult to get enough CO2 out of your blood and into your lungs.
Over time, as your COPD progresses and your lung function declines, you may retain more and more carbon dioxide as you breathe. As that excess CO2 builds up in your blood, it causes an imbalance between your blood oxygen and carbon dioxide levels, which can cause serious symptoms and oxygen deprivation.
Co2 retention also happens through a phenomenon known as ventilation-perfusion mismatch. This happens when your body gets confused about which parts of your lungs to prioritize, which reduces the efficiency of gas exchange in your lungs.
Usually, your lungs constrict your blood vessels in such a way that they decrease the amount of blood that flows to poorly functioning air sacs that have been damaged by COPD. At the same time, they increase blood flow to the most healthy alveoli so they can absorb as much oxygen (and release as much carbon dioxide) as possible.
However, this ventilation-perfusion ratio can get thrown off, usually because of high-flow oxygen therapy, COPD exacerbations, or other COPD symptoms. That causes this blood flow strategy in the lungs to break down; less blood flows to the parts of the lungs that function efficiently, and more blood flows through damaged alveoli that are less capable (or completely incapable) of exchanging oxygen and carbon dioxide efficiently.
The result is low blood oxygen levels (hypoxemia) and high blood carbon dioxide levels (hypercapnea) that make it more and more difficult to breathe. When mild, this can often be corrected with supplemental oxygen therapy and other COPD medications, however, it can be caused by improperly-dosed oxygen therapy, as well.
Why CO2 Retention is Dangerous

When too much CO2 is trapped or “retained” in your lungs after you exhale, it makes it much harder to breathe. This is partially because oxygen-rich air that enters your lungs when you inhale mixes with the leftover CO2, diluting the oxygen concentration of the air in your lungs and making it more difficult for the air sacs to absorb enough oxygen.
Another problem is that the excess CO2 gets picked up by empty-handed red blood cells and re-absorbed back into your blood. Since red blood cells can only hold one gas at a time, it leaves fewer red blood cells free to pick up oxygen when you breathe in.
The problem can get worse as more and more CO2 builds up in your bloodstream, making it harder and harder to absorb oxygen from your lungs. If your blood CO2 gets too high, it's known as hypercapnea, and it can lead to serious breathing problems and dangerously low levels of oxygen in your blood.
Because of this, the main symptoms of hypercapnea overlap with the symptoms caused by hypoxemia, which happens when your blood oxygen saturation gets too low. If left untreated for too long, hypercapnea-related hypoxemia can cause serious health complications, including respiratory failure and death.
However, CO2 retention poses a more immediate risk of making your COPD more difficult to manage and making symptoms like coughing, wheezing, and shortness of breath worse. You are more likely to experience hypercapnea during symptom flare-ups, respiratory illnesses, and COPD exacerbations, but CO2 retention can also happen slowly and gradually over time.
In fact, the early symptoms of CO2 retention may be so mild or non-existent that you don't notice them until it gets much worse. That's why it's important to understand what CO2 retention is, how it happens, and how to recognize it; the sooner you realize it's happening, the sooner you can seek treatment and get your COPD back under control.
Left unchecked for too long, CO2 retention deprives your body of oxygen, which can cause serious health problems like heart disease, pulmonary hypertension, and cognitive dysfunction. If it gets too bad, severe hypercapnea can cause respiratory failure, organ damage, and death.
Respiratory failure happens when you have so much CO2 in your blood that it raises your blood's acidity beyond healthy levels. This is a condition known as acute respiratory acidosis, and it is is a life-threatening medical emergency.
A less severe form of respiratory acidosis, known as chronic respiratory acidosis, can happen gradually over time. It does not pose as immediate a risk as acute respiratory acidosis, and, because it happens little by little, the body adapts to the blood's acidity. This makes the symptoms are subtle, if noticeable at all.
If you have COPD and are worried about CO2 retention, hypercapnea, or chronic respiratory acidosis, then ask your doctor to take another look at your blood oxygen, CO2 levels, and your lung function tests (he should already do this at your regular appointments). Always tell your doctor about any new symptoms you have, even if they are mild, and don't be afraid to discuss any concerns you have about your health.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The Symptoms of CO2 Retention and Hypercapnea

The first symptoms of CO2 retention or hypercapnea are usually headaches, breathlessness, drowsiness, and lack of energy. These symptoms happen because you can't absorb enough oxygen and your blood oxygen saturation gets low.
As it gets worse, hypercapnea can cause difficulty thinking and concentrating, confusion, and muscle twitches. In serious cases, it can cause severe oxygen deprivation which leads to swelling in the hands and feet (edema), a bluish tint to the skin (especially fingers and lips), seizures, coma, respiratory failure, and death.
Here is a list of some of the general symptoms of CO2 retention:
- Mild headaches
- Feelings of drowsiness, fogginess, or sleepiness
- Lack of energy or fatigue
- Inability to focus or think straight
- Feeling dizzy or disoriented
- Shortness of breath
Here is a list of the more severe symptoms of hypercapnea:
- Unexplained confusion
- Abnormal muscle twitching
- Abnormal depression or paranoia
- Irregular heartbeat
- Bluish tint to the skin and lips
- Swollen hands and feet (edema)
- Hyperventilation
- Seizures
- Loss of consciousness
These symptoms can occur quickly or happen gradually over time. If you experience mild symptoms for more than a couple of days, then you should schedule an appointment to see your doctor. If your symptoms are severe, then you should seek medical attention at an emergency room immediately.
Causes of CO2 Retention for People with COPD
As we discussed, CO2 retention is often caused by airway obstruction, damaged lung tissue, and ventilation-perfusion mismatch in the lungs. However, there are a variety of other things that can make CO2 retention worse.
Oxygen Therapy

A common cause of CO2 retention is supplemental oxygen therapy. If your oxygen dosage is wrong or you get too much oxygen for any other reason, it can cause too much CO2 to build up in your blood.
This happens because, when you get excess oxygen with every breath, it can cause red blood cells to drop carbon dioxide to pick up oxygen instead. As a result, the dropped CO2 dissolves into your blood instead of getting released into your lungs for expulsion.
This dramatically throws off the balance of oxygen and carbon dioxide exchange in your lungs, causing more and more CO2 to build up in your bloodstream. In this way, portable or home oxygen therapy can make CO2 retention much worse and cause hypercapnea when prescribed or used incorrectly.
Another way that oxygen therapy can worsen CO2 retention is by causing ventilation-perfusion mismatch. Although researchers aren't sure exactly why, this happens when you get more oxygen at a time than what you actually need.
The best way to avoid oxygen therapy-induced CO2 retention is to follow your oxygen prescription exactly. To reduce the chances of hypercapnea, your doctor should prescribe you enough oxygen to keep your blood oxygen saturation at about 90 percent, but not much higher.
If you are worried about CO2 retention, you can always have your doctor check to make sure your flow rate is adjusted correctly and that you are using your equipment properly. Then, it's up to you to follow your doctor's instructions and only use your oxygen as often as your doctor recommends.
Emphysema

Severe emphysema is another major cause of CO2 retention in people with COPD. Emphysema causes your lungs to become enlarged and less stretchy (a condition known as lung hyperinflation), which makes it more difficult to push all of the air out of your lungs when you exhale.
Lungs with emphysema tend to trap lots of air, which makes it difficult to breathe and absorb enough oxygen as well as expel enough CO2. This puts patients with emphysema at an increased risk of hypercapnea, especially during heavy exercise, which forces your lungs to get rid of even more CO2.
That's why doctors recommend breathing exercises like pursed-lips breathing and diaphragmic breathing to help you train yourself how to empty your lungs more completely when you exhale. These can be especially helpful during exercise and physical activity to reduce and prevent shortness of breath.
It is also important to follow your COPD treatment plan carefully to minimize your symptoms. The better you keep your symptoms and breathing under control, the better you can prevent air from getting trapped in your lungs, reduce hyperinflation, and prevent hypercapnea.
Some patients with severe emphysema may be eligible for lung reduction surgery if their lungs are significantly enlarged. By reducing the volume of the lungs, the surgery makes it easier to push all the air out when you exhale, preventing CO2 retention and making it easier to breathe.
To learn more about breathing exercises you can practice to improve your COPD, see our previous article on COPD breathing techniques here.
Eating Too Many Carbohydrates

Believe it or not, the foods that you eat can have a significant effect on CO2 retention in your lungs. That's because, whenever your body digests food, it turns it into two main things: energy, and carbon dioxide waste.
The carbon dioxide waste has to be processed through your lungs so that you can exhale it out of your body. Some foods, however, create extra carbon dioxide waste that puts unnecessary strain on your lungs.
The main culprits for this are foods high in carbohydrates, which create more CO2 waste than other foods when your body breaks them down. When you have COPD and your lungs are already struggling to function efficiently, this excess CO2 can be enough to tip the balance in your lungs and cause you to retain too much CO2.
Because of this, doctors often recommend that people with COPD limit the amount of carbohydrates in their diets. That includes grains, pastas, breads, and especially simple sugars and processed foods high in carbs.
While a certain amount of carbs are still healthy, you should try to limit yourself to healthy sources of complex carbohydrates and be careful not to eat more than you need. Instead, replace carbohydrates in your diet with more foods that are high in lean protein and healthy fats.
According to US dietary guidelines for older adults, you should eat about 5-7 ounces of grains every day, at least half of which should come from whole-grain sources. However, it is easy to exceed this amount if you eat a lot of breads, pastas, cereals, or processed foods.
Shallow Breathing

When you take too short or too shallow of breaths, your lungs have a hard time getting rid of enough CO2. That's why it's important to keep your breathing under control and practice breathing exercises if you have COPD.
Many COPD patients tend to take more shallow breaths whenever they feel like they're having trouble breathing, such as during bouts of breathlessness or coughing. Unfortunately, that just makes the problem worse by making it easier for air and CO2 to stay trapped in your lungs.
This happens because shallow breathing only uses the upper part of your lungs, which is why it is sometimes referred to as “top breathing.” As a result, stale air stays in the lower parts of your lungs, which leads to CO2 retention and makes it harder to breathe.
You can counteract this, however, by practicing breathing exercises in your spare time and remembering to use them when you feel short of breath. Exercises like diaphragmic breathing and pursed-lips breathing are especially helpful for training yourself to take deep, full breaths and push all the air out of your lungs when you exhale.
It also helps to strengthen your breathing muscles, which you can also do with aerobic exercise, wind instruments, and other forms of physical activity. You can even join special COPD exercise and therapy classes designed to help you improve your breathing, including pulmonary rehabilitation and music therapy courses.
Conclusion
COPD is a complicated breathing disorder that can lead to a variety of different symptoms and health complications. Because of the complex nature of the disease, many patients struggle to understand how their blood oxygen levels, blood CO2 levels, and their symptoms are all connected.
Hopefully, after reading this article, you have a better understanding of how your lungs function and how CO2 retention works. You should also be better able to recognize the signs of hypercapnea and how to protect yourself from factors that put you at risk.
If you use supplemental oxygen therapy, it's particularly important to know the symptoms of CO2 retention and the dangers of getting too much oxygen. If you catch the early signs, you can work with your doctor to adjust your oxygen delivery before it causes any serious problems. It's important to fully understand oxygen therapy benefits and oxygen therapy side effects before you get started.
COPD is sometimes a difficult disease to manage, but with the right knowledge, a good treatment plan, and the support of a good medical team, you can successfully keep your symptoms and CO2 retention under control. That's why it's important to learn everything you can about COPD and what you can do to keep your lungs as healthy as possible.

