.png)
Mental illness is a growing problem in the United States. According to Mental Health America (MHA), 1.5 million more Americans experienced mental health issues in 2017 than the previous year. What’s more, surveys from the Centers for Disease Control and Prevention (CDC) indicate a sharp increase in self-reported behavioral health symptoms since the beginning of the COVID-19 pandemic. While there are many possible factors that are contributing to these issues, one of the lesser discussed factors is social isolation.
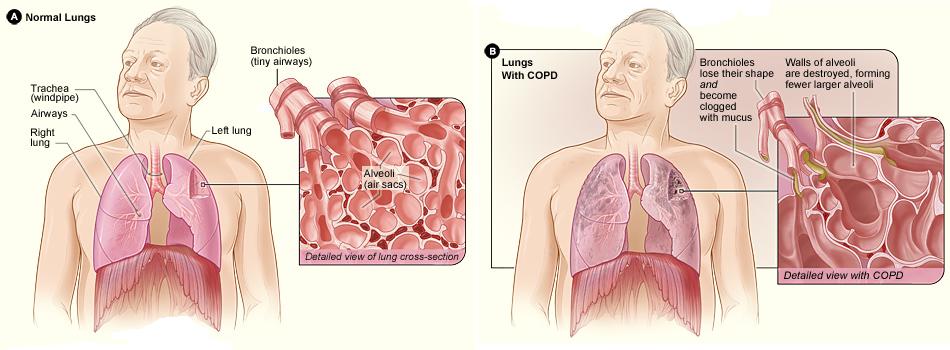
Social isolation is defined as either a partial or total disconnect from social networks. According to a report from the National Academies of Sciences, Engineering, and Medicine (NASEM), one-third of adults aged 45 and older feel lonely, and nearly one-fourth of adults aged 65 and older are considered to be socially isolated. Additionally, people with chronic illnesses — especially debilitating illnesses like COPD — can lead to a higher risk of social isolation and loneliness.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
COPD is often labeled as an “invisible illness” because it’s not always possible for an outside observer to fully understand what COPD patients are experiencing. While some COPD patients may be able to get around just fine and keep up with their friends, that doesn’t mean they aren’t experiencing adverse physical or psychological symptoms. In this post, we’re going to bring some awareness to social isolation and loneliness in COPD, why it happens, and how it can be prevented.
What are the Effects of Social Isolation?
According to a national survey conducted by Cigna, nearly half of the 20,000 participants reported feeling lonely. These numbers are concerning because there are a number of mental and physical health risks associated with loneliness. A study from Brigham Young University found that social isolation has as many health risks as having an alcohol use disorder or smoking 15 cigarettes a day and that it’s as harmful to mental health as obesity.

While the outlook for people experiencing social isolation and loneliness may seem grim, there is actually a growing amount of awareness surrounding the issue. People are beginning to associate the growing loneliness in society with the excessive use of technology and social media which is taking people away from face-to-face interactions. On the other hand, many people believe that social media is giving people experiencing loneliness an outlet to discuss these issues.
Why Do COPD Patients Experience Social Isolation?
Social isolation isn’t always as clear-cut as many people believe. While you may have an idea of a socially isolated person as someone who lives alone and doesn’t go out to visit people, this is only half of the story. There are many COPD patients who have close family members and belong to close-knit communities, but still, feel socially isolated. In order to understand this, let’s take a look at some of the reasons why COPD patients experience social isolation.

Chronic Pain and Fatigue
Chronic obstructive pulmonary disease affects an estimated 16 million people in the United States alone. However, no two cases of this disease are the same. While some COPD patients may be able to get out and do anything they want, others are held back by symptoms like chronic pain, fatigue, and persistent breathlessness. When this is the case, people often struggle to find the motivation to work through these challenges in order to get out and spend time with friends and family members.
![]()
COPD is a disease that develops slowly over the course of many years. So, it’s unlikely that will find yourself suddenly deciding to stay in rather than going out to meet people. Although, in many ways, this can be even worse than the alternative because you might not realize that you’re changing your lifestyle. Some studies estimate that about 70% of COPD cases are undiagnosed meaning millions of people could be experiencing social isolation due to a condition that they’re not even aware of. Oftentimes, the symptoms are shrugged off as a normal sign of aging.
Risk of Exacerbation or Infection
If we’ve learned anything from the past year it’s that viruses can spread quickly and they don’t affect all demographics in the same way. The novel coronavirus (COVID-19) hit the COPD community in a way that nobody could’ve predicted, and even now, over a year later, people are still feeling the effects of it. The Centers for Disease Control and Prevention (CDC) lists COPD as “high risk” for experiencing severe symptoms from COVID-19 and this rings true for many other viruses as well like the flu and viral pneumonia.
Another reason the COPD community has been hit so hard by the virus is due to the average age of people with this disease. It’s estimated that most people are at least 40 years old by the time they start experiencing COPD symptoms. But since COPD develops slowly, many people don’t start experiencing severe symptoms until they’re in their 60s. The CDC also states that people over the age of 65 are at high risk for severe COVID-19 symptoms, so this is a major factor at play too.

On top of the ongoing pandemic, COPD patients also have to worry about air quality. Highly polluted areas or places with a lot of allergens like pollen can result in respiratory exacerbation and even hospitalization. Because of this, it’s recommended that COPD patients plan their day so that they aren’t outside when air pollution is at its worst. Airnow.gov is a great tool if you want to quickly learn about the air quality in your area. Simply input your city or zip code and you will be provided with a number between 0 and 500 with 0 being no pollution and 500 being severely polluted. It’s recommended that COPD patients do not go outside if the air quality index (AQI) is above 100.
A Changing Lifestyle
Being diagnosed with COPD can be a life-changing moment. One day you’re following your normal routine, and the next your doctor is asking you to make a number of lifestyle changes to improve your health. A typical COPD treatment regime involves an improved diet, a pulmonary rehabilitation plan, and supplemental oxygen therapy which helps to keep oxygen levels stable. This can be somewhat overwhelming at first and will take some time to get accustomed to but it’s well worth the effort in the end.

One major lifestyle change that many people are unprepared for is moving into an assisted living facility or receiving in-home care. As COPD patients age, it becomes increasingly more difficult for them to maintain their independence, and oftentimes, friends and family members don’t have the means to be a full-time caretaker. While assisted living can be a convenient option for most people, it leaves open the possibility of social isolation and loneliness.
Social Stigmatization
The term “stigma” is the disapproval of someone based on their perceived characteristics. And although it’s a harsh reality to face, some people view people with chronic conditions as “less capable” even when these claims are completely baseless. The stigma surrounding COPD usually has to do with physical symptoms like coughing or wheezing or medical equipment like oxygen tanks or inhalers. But the bottom line is that it can make people with COPD feel like they don’t belong or aren’t able to keep up with the people around them.

What Can be Done to Prevent Social Isolation in COPD Patients?
Be Open About Your Experiences
The first step to solving problems like isolation and loneliness is to be more open about your experiences with your friends and family members. It’s not always easy putting into words exactly how COPD makes you feel and how it affects your mental health because you may not even be fully aware of how it has. However, by at least trying, you’ll make the people around you more aware of what you’re going through. What’s more, there’s a chance that your friends and family are thinking about the same thing but aren’t quite sure how to ask you about it.
Speak With Your Doctor
Another person you should be open with about your experiences is your doctor or pulmonologist. The reason it’s so important to tell your doctor is that he/she may be able to make adjustments to your treatment plan in order to help you get back on your feet and spend more time with loved ones. At the end of the day, there is no such thing as a “silly question” when it comes to your health. Chances are, many other COPD patients are dealing with a similar situation to yours, so opening up about your social isolation and loneliness will have a positive effect on the COPD community as a whole.

Your doctor might also be able to connect you with a mental health professional who can work with you step-by-step on how to prevent loneliness. Cognitive behavioral therapy (CBT) is a popular form of psycho-social intervention that aims to pinpoint and correct negative or inaccurate thinking patterns that can lead to loneliness. Of course, if the only thing holding you back is your physical symptoms, CBT won’t do much for you. However, if you feel like it’s mainly your mindset holding you back, CBT can work wonders. Many people around the world with chronic illnesses make use of CBT, so you’re not alone.
Embrace Online Communities
Like we mentioned earlier, there are many downsides to online communities. However, it’s impossible to deny the benefits as well. Older generations of Americans are becoming increasingly proficient with computers and social media which can be a great benefit for someone with COPD. Online communities such as COPD360Social hosted by the COPD Foundation or COPD.net’s help center are great for anyone who wants to share advice with other like-minded COPD patients. You might also consider Facebook groups which are free to join and participate in.
.jpg)
Make Use of Technology
In this day and age, we’re completely surrounded by technology wherever we go. While this can definitely be overwhelming at times, it can also be extremely beneficial if we take the time to learn how to use it. As a COPD patient, there are many technologies out there that can make your life much easier, it’s usually just a matter of finding what’s right for your lifestyle and budget. Mobility aids are a great example of a technology that can help you get back out and become a member of the community again. Walking canes, manual wheelchairs, electric scooters, and stairlifts all help you get around with more ease and also help prevent you from overexerting yourself and experiencing an exacerbation. Read this post to learn more about mobility aids for COPD.
.jpg)
Another technology you should consider investing in if you’re a COPD patient is a portable oxygen concentrator. These concentrators work similarly to your supplemental oxygen tank, however, they’re much lighter, smaller, and easier to use. Portable oxygen concentrators are electronic devices so you’ll never need to call an oxygen company to come refill them. You simply need a full battery and you’ll have access to oxygen wherever you go. Another benefit of POCs is that they don’t have the same social stigma attached to them as do oxygen tanks so you’ll feel more confident and secure with your new POC.
Conclusion
COPD is a chronic respiratory disease characterized by breathlessness, chronic pain, and fatigue. It’s the leading cause of morbidity and mortality in the world. Despite this, many people with COPD are suffering from “invisible” symptoms like anxiety, depression, and loneliness. In this article, we took a close look at how social isolation can affect both COPD patient’s mental and physical well-being, as well as offering some insight into how to remedy this. Fortunately, there are many steps that someone can take to prevent loneliness with COPD.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
If you’re looking for more great information that will help you manage the symptoms of your COPD, stay tuned to our blog here at LPT Medical. We try to cover a lot of topics that are under-discussed in the COPD community like the mental health aspects of the disease. If you have any questions or thoughts, feel free to leave them in the comment section below. And in the meantime, if you’re looking for an oxygen device that meets all your needs, take a look at our portable oxygen concentrators. We offer some of the top-rated concentrators on the market including but not limited to the Caire FreeStyle Comfort, Inogen One G5, and Respironics SimplyGo.
If you’d like to speak with an oxygen concentrator specialist please call us or send us an email.
.png)
Supplemental oxygen therapy is a foundational part of most COPD treatment plans. The ultimate goal of oxygen therapy is to provide the lungs with a higher concentration of oxygen which helps ensure that your blood oxygen levels remain normal. While most COPD patients need to use supplemental oxygen at some point in their lives, the experience tends to vary from person to person.
If you’ve been on oxygen for some time, you know that there are good days and there are bad days. One day, everything may be working exactly as it should and you forget that you’re even on oxygen. However, the next day, you might experience discomfort with your nasal cannula, dryness in your nose, equipment failure, or any other number of issues. It’s during times like these that we begin to wonder if supplemental oxygen is too intrusive to be worth our time and effort.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
And while it’s true that oxygen therapy can be intrusive sometimes, the alternative can be far worse. Having low blood oxygen levels (hypoxemia) for prolonged periods of time can have devastating effects on the body including breathlessness, dizziness, confusion, and eventual organ damage or failure. Your body absolutely needs oxygen, so if you’re thinking about reducing your oxygen flow, be sure to consult your physician beforehand.
To help you cope with the unpredictability of oxygen therapy, we’re going to offer seven tips to get you back on the right track and experience peace of mind again.
Start With Choosing the Right Oxygen Device for Your Needs
If you get the sense that oxygen therapy is always an uphill battle, there’s a good chance that you have the wrong oxygen device for your needs. Unfortunately, the greatest strength of the oxygen industry is also its greatest weakness — there are too many options. Traditional oxygen tanks, liquid oxygen tanks, stationary oxygen concentrators, and portable oxygen concentrators are just a few of the options out there. And even once you decide which one is best for you, you’ll have many different brands and devices to choose from, all of which vary greatly in terms of what they offer the patient.

Take traditional oxygen tanks, for example. These devices have been around for many decades and they’ve provided millions of COPD patients with reliable oxygen. However, since the early 2000s, they’ve become nearly obsolete due to technological advancements in the oxygen industry. While oxygen tanks are still popular, most people prefer having a portable oxygen concentrator instead. Rather than being heavy, bulky, and intrusive like oxygen tanks, portable oxygen concentrators are ultra-lightweight, comfortable, and convenient. And most importantly, they provide patients with reliable medical-grade oxygen.

One of the most popular types of POC is a pulse dose POC. These concentrators closely track your breathing rate and administer oxygen only when you’re inhaling. In other words, your concentrator battery will last much longer than it would with a standard continuous flow concentrator because it isn’t having to constantly work to put out oxygen. The Inogen One G5 and the Caire FreeStyle Comfort are two of the most popular pulse dose units because they both weigh under 5 pounds, they have low failure rates, and they’re backed by some of the most reputable brands in the industry.
Choosing the Right Nasal Cannula
Aside from having the right concentrator, having the right nasal cannula is one of the best things you can do to make supplemental oxygen less intrusive. The nasal cannula is the part of the oxygen tubing that allows the oxygen to flow freely into your nose so that you can inhale it. However, as you can imagine, it can be quite annoying having the cannula in your nose all the time. Many people report experiencing irritation or dryness in their nostrils. Also, many people report experiencing irritation on their ears where the oxygen tubing rests.

The simplest solution to this problem is to use an ultra-soft nasal cannula that isn’t as abrasive as the standard cannulas. Many oxygen concentrators also have the option to add a humidifier to the device which prevents the nostrils from drying out after extended periods of use. There are also many different types of nasal sprays and lubricants on the market that you can apply before and after using your oxygen concentrator. However, be sure not to use petroleum-based skin products because these are highly flammable and will be made even more flammable as medical-grade oxygen is applied.
Find the Right Oxygen Accessories for Your Lifestyle
Everyone has a different lifestyle. Some people prefer to stay at home while others prefer to be out of the house as much as possible. So, it goes without saying that not everyone has the same oxygen needs. The amazing thing about portable oxygen concentrators is that they can be customized to different lifestyles with the use of different accessories. For example, if you own the Caire FreeStyle Comfort, you’ll be able to choose between the standard carrying case and the backpack. The former is better for people who want to minimize the amount of weight they’re carrying while the latter is great for anyone who wants to carry a lot of extra personal belongings.

Another decision you’ll have to make is what size of batteries you will need. Most portable oxygen concentrators out there come with several different sizes of battery and you can make a decision based on how long you typically stay out of the house. For example, the Inogen One G5 offers two different battery options — 8-cell and 16-cell. If you just take a quick trip out of the house to go to the grocery store, you might only need the 8-cell battery. However, if you travel around a lot, you might want the 16-cell battery which offers about twice the battery life.

If you’re someone who likes to take road trips, a DC charging cable is a must-have accessory. DC charging cables allow you to charge your POC via a car outlet which is incredibly handy if you’re going to be in the car for hours on end. The best part is that many POCs can be used while they’re charging, so whenever you leave the car to sightsee, you’ll have a fully charged battery to work with.
Take Some Time to Read the User Manual
Think of your portable oxygen concentrator user manual as your all-in-one guide for using your new device. It will teach you everything you need to know from turning the device on to adjusting the flow rate and understanding the different visual and audible alarms. While it may be tedious to sit there and read through the whole manual in one sitting, you should at least sift through it in order to learn the basics of how to operate it. This way, if you’re out of the house, you won’t be left to wonder what a specific button or function does.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Another important thing you’ll learn from the user manual is how to troubleshoot your portable oxygen concentrator. Troubleshooting refers to the steps that you take if something should go wrong in order to remedy the issue. You’ll be surprised to find that the majority of issues that portable oxygen concentrators have can easily be solved with a quick fix. Since POCs are electronic devices like computers, simply turning the device off and then on again can solve a lot of issues, so it’s often the first thing you should try when something goes wrong.
Keep Up With Device Maintenance
Like with any oxygen therapy device, it’s important to take care of your portable oxygen concentrator. The good news is that maintaining a POC is much easier than many people realize and it won’t cost you an arm and a leg to do it either. One thing you should do regularly is clean your device. As you can imagine, when you’re carrying your POC with you everywhere, it can start to gather dirt and germs which could make you sick or even damage the device. Simply wipe your device down with a disinfectant wipe once or twice a week and make sure you don’t get any of the electrical components wet. You should also be sure to take off the particle filter occasionally, wash it off, and replace it because this protects the internal components of the POC and also purifies the air you breathe.

Two other components you should replace regularly are your nasal cannula and your sieve beds. The nasal cannula needs to be replaced regularly because it can get worn out over time and starts to get really dirty. The sieve bed is a special filter inside your POC that removes specific gases from the air like nitrogen which enables you to receive medical-grade oxygen. If the sieve beds are in poor condition, you may not be receiving the oxygen you need to stay healthy. Every device is different, but generally speaking, you should replace the sieve beds every year or two. Ideally, your nasal cannula should be replaced every two weeks.
Plan Your Trips Carefully
You would not be making full use of your portable oxygen concentrator if you didn’t get out of the house and enjoy the freedoms that you used to before starting oxygen therapy. There are near endless possibilities when you own a POC, but it’s still important to be prepared every time you leave the house. For example, if you leave the house without fully charged batteries, you might find yourself in a difficult situation where you either have to find a place to recharge them or return home earlier than expected. The best way to prevent this is to always know how long you will be out of the house. Make sure you have enough battery life to get you through the day plus a few extra hours to account for any change of plans.

One thing that’s really handy to have on long trips away from home is an external battery charger. Most portable oxygen concentrator batteries need to be attached to the unit in order to be charged. This means that you can only charge one battery at a time. However, with an external battery charger, you’ll be able to charge two batteries at once. This is very useful if you’re going to be on the go a lot and don’t want to sit around waiting for your batteries to charge.
Speak With Your Doctor
Last but certainly not least, you should speak with your doctor if you’re having trouble incorporating oxygen therapy into your life. Your doctor should be the first person you contact if you’re thinking about making changes to your oxygen treatment plan because he/she will be able to tell you whether or not it is safe to do so. Many people believe that if there are no immediate symptoms caused by reducing their oxygen flow, then it’s safe to do so. Unfortunately, this is not the case. Although you may feel fine at first, prolonged hypoxemia can cause a lot of harm to your body including dizziness, confusion, and even organ damage. By talking to your doctor you may be able to work out a treatment plan that takes into consideration both your comfort and your long-term health goals.

Conclusion
Having a reliable supply of medical-grade oxygen is essential for any COPD treatment plan. Unfortunately, many people end up purchasing the wrong oxygen device for their needs and find that it’s too intrusive for it to be worth their time and effort. This is why it’s recommended that COPD patients use small, lightweight, and convenient portable oxygen concentrators like the Caire FreeStyle Comfort or the Inogen One G5. After using a POC for the first time, many patients realize that oxygen therapy doesn’t have to be intrusive or cause stress in their lives.
Here at LPT Medical, we take your oxygen needs very seriously. We don’t want you to be stuck with an oxygen device that you’re unhappy with or that isn’t meeting your needs. This is why we have a team of oxygen concentrator specialists who will take the time to understand what you’re looking for, then align you with the oxygen device that will best suit your individual needs. We also have a number of financing and buying options available. Contact us either by phone or email to learn more.
.png)
No matter what stage of life you are in, it’s always a good idea to find new ways to save money. If you’re someone with chronic obstructive pulmonary disease (COPD) or a similar lung disease, one of the best ways you can cut costs is by looking for ways to save money on medication, medical equipment, and other medical expenses. This study found that the average annual healthcare cost per COPD patient is around $4,147 and that increased disease severity is associated with higher healthcare costs.
Unfortunately, many people find that it’s not as easy as they thought it would be to save money on medical expenses. While there are many ways to save on medications, things like doctor’s visits, hospital visits, and pulmonary rehabilitation are pretty set in stone. And trying to avoid these things all together to save money could put your long-term health at risk. Be sure to visit a medical specialist whenever you need to, and find other ways to save such as on your medical oxygen equipment.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
If you’re just getting started with oxygen therapy, it might not be immediately evident how many options you have available to you and that just a few considerations could save you hundreds, if not thousands of dollars when it comes to purchasing and maintaining your oxygen device. In this post, we are going to highlight some tips for getting the best deal on an oxygen concentrator and avoiding some of the common pitfalls many people experience as a first-time oxygen buyer. If you have any questions, be sure to leave them in the comments or reach out to us by phone or email.
Find the Right Retailer to Buy From
By far the most important thing to remember if you’re looking for a good deal on an oxygen concentrator is to find a reputable retailer to buy from. The internet has made it easier than ever before to find the exact product you’re looking for and have it delivered on your porch within a matter of days. However, the internet has also opened the door for scammers and dishonest companies to get your money. This is why it’s so important to be prudent when it comes to the company that you work with.
![]()
Possibly the biggest scam you should be aware of when buying oxygen is companies that don’t ask to see your supplemental oxygen prescription. In the United States, oxygen is a “controlled substance” meaning it can’t simply be bought and sold freely without proof of medical necessity. If a company sells you oxygen without having you provide a prescription from your doctor, they are either doing so illegally, or they’re selling you low grade oxygen that will not meet your medical needs. Either way, these are deceptive business practices and they could be deceiving you in other ways as well.
Another thing to watch out for is something called “recreational oxygen.” This is not necessarily a scam or deceptive but it can lead to confusion when you’re trying to buy an oxygen concentrator to treat your COPD. Essentially, recreational oxygen is a type of low-grade oxygen used by hikers, climbers, or people traveling to higher altitudes than they’re used to. Allegedly, using these cylinders periodically can help you prevent breathlessness and altitude sickness, but there is little evidence to suggest this is the case. The important thing to remember is that “recreational” oxygen does not equate to “medical” oxygen.
.png)
Ultimately, the reason you should focus on finding a reputable oxygen retailer to work with is because purchasing the wrong device will set you back even further financially. Many people are ecstatic to find an oxygen device for a couple hundred dollars only to find out that it’s not going to meet their medical needs and that the company they bought it from doesn’t accept returns. Aside from breaking the bank, buying an oxygen device from a shady company can compromise your health and leave you without oxygen when you need it the most.
Decide Between New, Used, and Refurbished
Another way to get a great deal on an oxygen concentrator is to consider different buying options like new, used, and refurbished units. We wrote a post discussing all of the different buying options for portable oxygen concentrators in a different post, so be sure to check it out for more information. However, we’ll summarize the main points here for your convenience.
A “new” oxygen concentrator is one that has never been opened, turned on, or used in any way since it was manufactured. The obvious benefit to having a new concentrator is that the unit has no wear and tear and that you can expect it to last many years without needing repairs. What’s more, most new concentrators come with a manufacturer warranty which will cover you for several years if anything is wrong with the unit. Although rare, manufacturing defects are a possibility, so having the warranty will guarantee you repairs or a full replacement if your unit doesn’t work.

A “used” oxygen concentrator is one that has been owned by another oxygen patient in the past. The great news though is that “used” doesn’t mean that the unit is old and worn out. Some oxygen patients never use a unit or it is only lightly used before returning it. What this means is that you’ll be paying a discounted price on an item that is in “near mint” condition. When you purchase a concentrator from LPT Medical, you can rest assured that it’s been tested beforehand to ensure full functionality.
A “refurbished” portable oxygen concentrator differs slightly from a used unit in that repairs or replacements have been done to it. One of the common part replacements you’ll see in a refurbished oxygen concentrator are the sieve beds. These are specialized filters that remove unwanted gas from the air, allowing you to receive medical-grade oxygen. Over time, sieve beds can become worn out and need to be replaced.

One final option for you to get your hands on an oxygen concentrator is through renting one. This is not always the most practical option, but if you know you will only be needing one for a few days or weeks, it may be your most cost-effective option. Renting an oxygen concentrator is ideal for people who typically use an oxygen tank or stationary concentrator at home, but want to be able to go on a trip without having to hassle with lugging their tank around or finding a place to refill it.
Overall, there are benefits to each of the buying options, it’s just a matter of your individual situation. Be sure to ask our oxygen concentrator specialists here at LPT Medical if you have any questions or concerns.
Take Advantage of Package Deals
Package deals are one of the best ways to save money on an oxygen concentrator. A package deal is when you buy accessories alongside your oxygen concentrator unit and get a discount on your final price. This means you’ll be able to save a lot of money if you buy everything up front rather than buying each accessory separately. Package deals are not always going on, so be sure to talk with your oxygen concentrator specialist who can let you know what’s available.

One package deal many people enjoy is one that offers a carrying case, battery, and DC charging cable. This way, you will have the ultimate freedom to move around the minute you receive your oxygen concentrator instead of having to order additional accessories later on down the road. Most oxygen concentrators come with the standard size battery but if you think you will need a battery that lasts longer, you can always upgrade it and maybe even get some additional savings that way.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Another reason to take advantage of package deals is that it could help you save money on shipping. With very few exceptions, it’s almost always cheaper to ship everything in one box rather than individually. While it may not seem like that much extra to ship a couple of accessories, the costs can really start to add up.
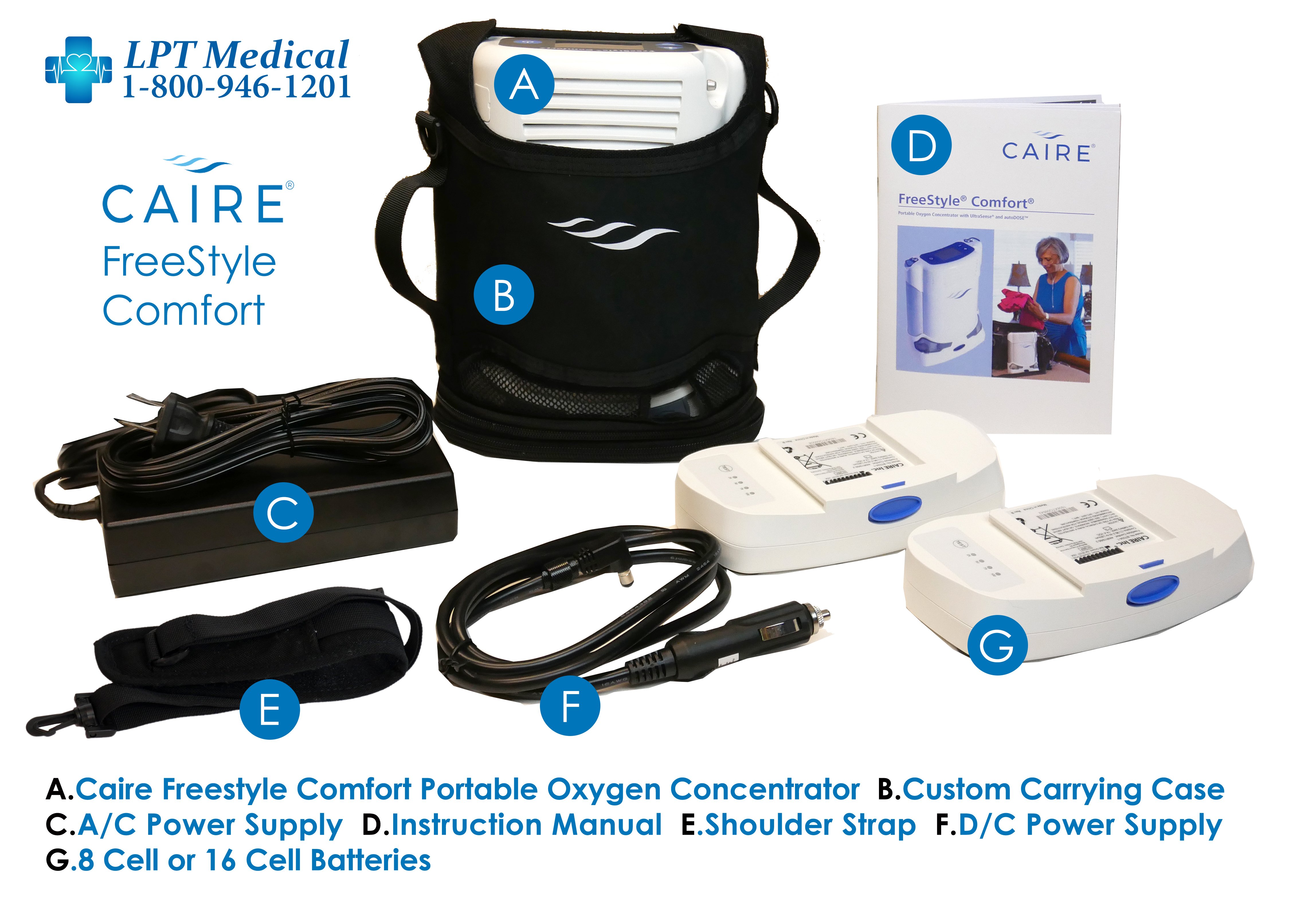
Two package deals we highly recommend are the Caire FreeStyle Comfort package and the Inogen One G5 package. These are some of the top-performing concentrators currently on the market, and when you consider everything that comes with them, you’ll see why they’re so popular. Just the base packages include an 8-cell battery, AC and DC charging cables so that you can charge your device anywhere, a carrying case, oxygen tubing, and a 3-year manufacturer warranty. Speak with one of our oxygen concentrator experts to see which one of these would be best for you.
Take Advantage of Sales
Sales are another thing you should keep an eye out for when you’re shopping for a portable oxygen concentrator. We offer a lot of oxygen concentrator sales here at LPT Medical because we want to get these devices to as many COPD patients as possible, even people who are on a tight budget. Currently, we are running a deal where you can get a free online pulmonary workshop course with the purchase of a new portable oxygen concentrator.
.jpg)
This program is called Thrive eLearning and it provides access to one-on-one counseling, support groups, and online courses that help you slow the progression of COPD. One of the important things you’ll learn during this course is breathing exercises which are a powerful tool for alleviating symptoms of breathlessness, fatigue, and chest pain which are commonly associated with COPD. You’ll also be able to connect one-on-one with doctors, caretakers, and other healthcare professionals, saving you time and money.

Sales are pretty common in the oxygen industry because the market is always changing. For example, we might offer a sale on one concentrator because a newer concentrator has hit the market. This is the perfect opportunity to get a great deal on a slightly older unit that still meets your needs perfectly. One of the best ways to keep up with these sales is to join our mailing list by filling out the form at the side of the page. You’ll be notified immediately whenever we have a new promotion going on!
Consider Your Financing Options
“Financing” an oxygen concentrator means splitting the payments up into more manageable monthly payments. While financing typically doesn’t save you money in the long run, it does lead to more financial security, because you won’t see the full cost of the concentrator come out of your bank account all at once. If at any time, you decide you want to pay off the rest of the concentrator all at once, you can do so without incurring any additional fees. Before committing to the financing terms, however, you should make sure that the company doesn’t charge a bunch of interest on top of the original price. Make sure you know what the exact amount of interest is and not just the monthly payments.

Conclusion
Oxygen concentrators are the ideal oxygen therapy device for most COPD patients. They’re very lightweight, compact, versatile, and most importantly, they provide you with medical-grade oxygen that you need to stay healthy. But if you want to get the best deal on an oxygen concentrator, you need to make several considerations first. Most importantly, you need to work with an oxygen concentrator retailer that you can rely on.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Here at LPT Medical, we take your oxygen needs seriously, and as such, we will take the time and diligence to understand both your medical and financial needs, then use our knowledge of the industry to align you with the perfect concentrator for you. It’s our goal to get an oxygen concentrator in the hands of any and all COPD patients who need them, so we will work with you to provide you with the best deal and we’ll even work with your healthcare provider to ensure you have all the necessary paperwork to buy an oxygen concentrator legally.
To get started, simply give us a call or shoot us an email.
There are five big respiratory diseases that are the most common causes of severe illness and death worldwide- COPD, asthma, acute lower respiratory tract infections, tuberculosis and lung cancer. There are other forms of lung disease that also impact large populations around the world like occupational lung disease, pulmonary hypertension, sleep apnea, pulmonary embolism.
Chronic obstructive pulmonary disease, or COPD affects 16.4 million adults and accounts for two main groups of lung diseases, emphysema and chronic bronchitis, each contributes to the obstruction of air flow that interferes with a patient’s normal breathing.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
If you have been diagnosed with COPD, understand that your condition will worsen over time. However, you can take the necessary treatment that can improve your quality of life and slow down the progression of your disease and you can do so by overcoming hardships and challenges that your disease will inevitably present you. Its called a fight for a reason!
Early and accurate diagnosis of COPD is a huge factor in treating your disease, this may seem obvious, how can you treat a disease if you don’t know that you have it? But it is not that simple, inaccurate diagnosis of COPD happens all of the time, and it is important that you and your doctor are aware of the signs of COPD so you can catch it early on!
Testing for COPD
Doctors should use spirometry for the diagnosis of COPD according to a GOLD report that was released in 2020. This test is helpful in avoiding misdiagnosis and determining the severity or stage of your COPD.
When diagnosing COPD, a doctor is looking at things like:
- Symptoms
- Severity of airflow limitation
- History of exacerbations
- Presence of other health conditions
Looking Out for Early Signs of COPD

Looking out for COPD symptoms is not the easiest way to prevent COPD because oftentimes symptoms don't appear until lung damage has already occurred to the point of no return. The best way to look out for yourself and avoid getting COPD or at least be sure that you are slowing the progression of the disease if you already have it, is to reduce and eliminate your exposure to respiratory irritates, number one being cigarette smoke. Quit smoking!
If you have COPD you’ll start to notices signs and symptoms of COPD like:
- Shortness of breath, especially during physical activities
- Wheezing
- Chest tightness
- Chronic cough
- Excess production of mucus that may be clear, white, yellow or greenish
- Frequent respiratory infections
- Lack of energy
- Unintended weight loss (if your disease has progressed into more severe stages)
- Swelling in areas of your legs
All of these COPD symptoms can inflict pain and suffering on your day to day life, so treating your disease properly can help ease these discomforting symptoms.
Treating COPD Symptoms

COPD affects everyone differently, you might experience more shortness of breath throughout the day and someone else may have a chronic cough, COPD is not a straight laid out treatment plan, it requires you to be flexible and listen to your body.
You also have to listen to your doctor and take the medication and oxygen therapy as prescribed in order to reduce the chances of experiencing an exacerbation and hospitalization, and to slow down the progression of your disease.
Oxygen Therapy

Long term oxygen therapy is one of the most effective treatments for COPD if your blood oxygen levels are low enough, and is the only treatment that will actually add years to your life.
This is because once your COPD has infiltrated your lungs to the point where they can no longer function properly enough to provide your body with the oxygen it needs to survive, supplemental oxygen can oxygenate your blood for you.
If your blood oxygen levels are low enough, and your doctor prescribed you supplemental oxygen therapy, a portable oxygen concentrator is your ticket to a healthier lifestyle. With the help of your oxygen device you should be able to sleep better, exercise more, and breathe easier.

Overcoming Challenges Presented with Supplemental Oxygen Therapy
Overcoming challenges with your oxygen therapy will come with time, patience, and practice. As with anything, it will take time to get used to using your device.
Tubing
Using the tubing during the day and at night while you sleep is a learning process, but eventually it will be second nature.
If you feel like the tubing is rubbing uncomfortably on your ear or your face, try wrapping the tubing in fabric or foam. This is a great solution for irritated skin caused by the friction of a nasal cannula sitting against your face or on top of your ears. Because you have to wear this tubing all day and night, the constant contact can cause soreness and skin irritation over time, which can make oxygen therapy very uncomfortable.
Dryness and irritation
Sometimes, you will notice your supplemental oxygen can cause dryness and irritation, common areas that might be affected are your lips, the skin under the nose, and other areas of the face that are near or in contact with your nasal cannula, oxygen, mask, or tubing.
This can be the result of rubbing, chafing, or the constant flow of air drying out your skin. When you use oxygen continuously, it is common that your skin will dry out in the areas where air escapes the tubing.
A simple solution for dryness and irritation that can help your skin heal and reduce the chances of future inflammation is to start using water-based moisturizers on your face and lips. If that does not help, your skin irritation could be a sign that your oxygen mask or nasal cannula isn't fitting you properly. If it's too tight, too big, or sits too loosely on your face, it can cause unnecessary friction and chaffing.
If you are having chronic problems with soreness or irritation, talk to your doctor or your oxygen supply company about getting a new nasal cannula or oxygen mask. You might need to try a different size, a different design, or a different brand in order to find one that fits your face more comfortably.

For more tips and trick to make you oxygen therapy more comfortable, read this blog:
How to Make Supplemental Oxygen More Comfortable
Medication

Common COPD medication consists of long-acting and short-acting bronchodilators, inhaled steroids, combination inhalers, oral steroids, phosphodiesterase-4 inhibitors, theophylline, and antibiotics.
All of these mediations have some kind of set back or side effect that can disturb your day to day life. Managing your medication and taking it properly is one of the only ways you can combat these issues.

Overcoming Challenges Presented with Medication
First of all, if one of your medications is giving you horrible side effects, talk with your doctor about trying a different medication with the same purpose but perhaps a different medication will not have such great side effects.
There is a lot of research being done surrounding COPD, and new innovative medications become available from time to time, so be sure you stay up to date with COPD news and experiential treatments either by doing your own research online or speaking with your doctor.

There are many efforts to develop new drugs for COPD. A research team from NIH’s National Institute of Environmental Health Sciences (NIEHS) in Rome, Italy, investigated the use of hyaluronan. Hyaluronan is naturally produced by many of the tissues in your body, including your lungs. The idea of utilizing hyaluronan as a new drug for treating COPD wound be for healing and reducing inflammation. In animal studies, inhaled hyaluronan treatment was shown to reverse some types of COPD, so watch this space and others like it for new COPD clinical trials.
Exercise

If you have COPD, you already know that exercise is a huge aspect of your treatment plan, and finding a time to exercise everyday will help you manage your COPD and slow the progression of your disease. But you also must know how hard it is to find the motivation to exercise.
Overcoming Challenges Presented with Exercise
If your disease has progressed, and you are required to be on oxygen therapy, having the right oxygen equipment can help you find motivation to exercise more than any other one thing. A lightweight portable oxygen device will give you the ability to bring your oxygen with you for a long walk or bike ride so you can stay oxygenated during your exercise session.

If you need continuous flow oxygen, the Respironics SimplyGo is the lightest continuous flow device available today, and it is a great option for any oxygen patient that is looking for more range of motion and freedom to exercise.
Of course, even with the help of your oxygen device, exercise can still be challenging.
Here are a few tips for getting in shape with COPD:
- Start with small increments and time, and build from there.
- Write down an attainable goal everyday that involves moving your body or an exercise that you can do. Check off the goal once you’ve accomplished it.
- If you feel tired one day, try to go for a short walk instead of taking the day off
- Drink plenty of water and stay hydrated
- Eat a healthy and balanced diet that give you energy
- Join a pulmonary rehabilitation course to learn new exercise and be around people going through similar trials and tribulations as you

Mental Health and Depression
Dealing with a chronic illness will take its toll on your mental health because you are not always capable of doing the things you once loved. Not to mention that diseases like COPD can be intrusive and uncomfortable to live with.
Emotional health is just as important to take care of on top of your physical health that you treat with medication and oxygen therapy. One of the best ways to treat mental health issues is to seek out meaningful and helpful social interactions.
Try talking to support groups and opening up in your pulmonary rehabilitation courses, it is likely that someone in your COPD community is going through similar issues. If you have trouble opening up about your mental health in person, try joining facebook and online forums and talking to people online. Also don’t forget that confining in friends and loved ones may seem hard at first, but it can really help them understand your mood swings and symptoms that are not always as obvious.
Beyond social interaction, you can also talk to your healthcare team about your mental state. Asking for help is sometimes the only way to get your emotions under control, so ask your health care providers to work with you to understand the cause of your feelings, and to identify coping strategies that will work for you. They may recommend you speak with a mental health professional such as a counselor, psychologist or psychiatrist.
There are also medications available to help with anxiety and depression, but they have not always been found to be effective for people with COPD. Counseling, or talk therapy, can successfully help people living with COPD change patterns of negative thinking and behaviors, improve quality of life and reduce anxiety and depression.
Overview

Dealing with challenges is a guaranteed part of having a chronic illness like COPD, overcoming these challenges is left up to you.
There are active steps you can take to get through the obstacles, and if LPT Medical can help you get the oxygen device you need to combat supplemental oxygen related challenges, just call 1(800)-946-1201.
You can also find a plethora of respiratory disease resources on our website where you can get information about everything and anything you need to learn more about your condition and how to manage it!
.png)
Whether you have chronic obstructive pulmonary disease (COPD), asthma, cystic fibrosis, or any other type of respiratory ailment, your doctor may prescribe you with a device called a nebulizer. Nebulizers are one of many different types of inhaled therapy devices and can provide you with considerable relief from respiratory symptoms such as shortness of breath, coughing, and wheezing.
While nebulizers are an effective treatment option, they aren’t for everyone. A nebulizer should only be used if and when your doctor prescribes it and should only be used for its intended purposes. Since nebulizers use medication, incorrect usage of the device could pose a serious risk to your health, especially if you’re using it too frequently.
In the following sections, we’re going to provide you with all the information you need to get started with nebulizer therapy like how to use a nebulizer, how to clean it, and other things you should consider before getting started. If you have any questions, feel free to leave them in the comment section or speak with your doctor.
How Do Nebulizers Work?
A nebulizer is a form of inhalation therapy, meaning you’re inhaling medication instead of taking it orally or intravenously. For someone with a respiratory condition, inhalation therapy is considerably more effective than the alternatives because the medication reaches the affected area almost instantaneously. This is especially important for someone experiencing a COPD exacerbation or asthma attack because expedited treatment could have life-saving results.

When you use a nebulizer, liquid medication is transformed into a fine mist called aerosol. The aerosol lingers in the mouthpiece or face mask so you can simply breathe normally to receive the treatment. If someone has severe COPD or asthma, other inhaled therapy like metered-dose inhalers (MDIs) may be ineffective because they require a deep and coordinated inhalation for the medication to reach the lungs. With a nebulizer, however, even shallow breathing will help.
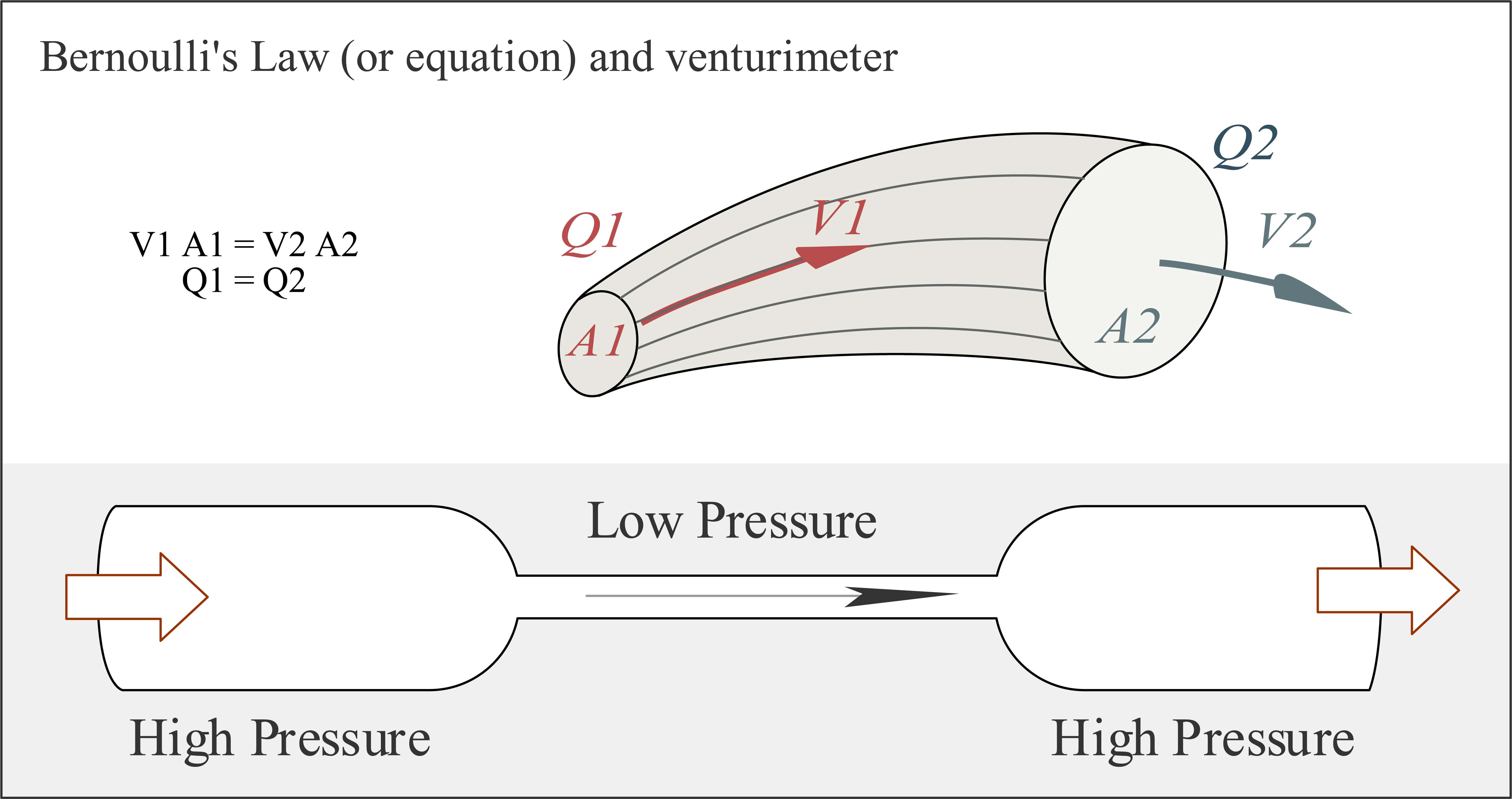
In aerosol therapy, there’s something called the Bernoulli Principle. This principle says that when a pressurized flow of air is directed through a small outlet, its velocity increases creating a jet stream. When this jet stream is created, it makes a sub-atmospheric pressure zone, also known as a vacuum. This vacuum is used to pull the medicine up a capillary tube and into the jet stream which then creates the aerosol that you inhale. This is the same principle that’s used to create jet engines.
Components of a Nebulizer
Unlike inhalers, nebulizers are electronic devices, so they’ll need a source of power in order to operate. Home nebulizers will have a power cord that you can plug into the wall outlet and portable nebulizers will have either replaceable or rechargeable batteries for you to use. While home nebulizers are still rather small and can be transported easily, you may need a portable one if you want to perform inhalation therapy on the go.

Another component of a nebulizer is the mask or mouthpiece which may be a part of the nebulizer device or attached to it via a tube. You will also have a medication cup and measuring device that’s used to administer the correct dosage of medicine and a filter will be attached that removes contaminants from the air before it’s put through the device. These filters should be replaced every once in a while to ensure the compressor stays clean and that you are inhaling fresh, clean air.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Types of Nebulizers
Nebulizers are generally divided into two different categories: jet nebulizers and ultrasonic nebulizers. Each of these units comes with their own pros and cons and each can be purchased in either a home (tabletop) or portable version. While each type of nebulizer is effective, you’ll want to speak with your doctor to decide which one will be best for you. Let’s take a look at each one to see how they work.
Jet Nebulizers
Also known as an atomizer or compressor nebulizer, these are the most common type and are considered the “traditional” nebulizers because they’ve been in use longer. This device uses compressed air at a high velocity in order to turn medicine into an aerosol. While jet nebulizers can be noisy, they’re often used in hospitals for patients with serious cases of respiratory disease.

Pros:
- Wide range of particle sizes
- No restrictions on medication
- Durable and reliable
- Tabletop or portable options available
- Low operational cost
Cons:
- Tend to be very loud
- Tabletop versions are bulky and difficult to move
Ultrasonic Nebulizers
Ultrasonic nebulizers use high-frequency sound waves to turn liquid medicine into an aerosol. In order to create the sound waves, they use a vibrating metal plate at ultrasonic frequencies. Because these sounds are undetectable by the human ear, ultrasonic nebulizers are much quieter and also tend to be easier to move around.
Another technology contributing to the development of ultrasonic nebulizers is called the Vibrating Mesh Technology (VMT). These types of nebulizers have thousands of laser-drilled holes that vibrate in order to produce the mist, which is much more efficient than other ultrasonic nebulizers, however, it tends to produce more heat and liquid waste.

Pros:
- Most technologically advanced nebulizers
- Much quieter than jet nebulizers
- Light and compact
Cons:
- More expensive than other nebulizers
What Medication Do Nebulizers Administer?
Nebulizer medications are divided into two different categories: long-term control medications and quick relief. Long-term medications are used to treat the symptoms of asthma, COPD, and other respiratory ailments, while quick-relief medications are used for emergencies like an asthma attack or COPD exacerbation. Not everyone with a chronic lung condition will be prescribed inhaled medication, but if you are, your doctor may decide that a metered-dose or dry powder inhaler will work better for you.
Depending on the severity of your disease, your age, and the type of condition that you have, your doctor will determine the amount of medication that’s needed. You may also be instructed to mix two different types of medication or to only use it in certain situations. Ensure you follow his/her instructions exactly in order to experience the most relief from your symptoms. Below are just a few of the medications you may be prescribed for nebulizer therapy.
Ipratropium Bromide

This is a type of bronchodilator that can help alleviate acute respiratory symptoms by preventing muscle constriction in the airways. According to the National Institutes of Health (NIH), severe asthma attacks can often be treated with ipratropium in combination with other short-acting drugs like levalbuterol and albuterol, but your doctor may be able to provide you with a premixed combination of these drugs. Potential negative side-effects of ipratropium include an upset stomach, dizziness, and dry mouth.
Cromolyn Sodium
While not as effective as budesonide, cromolyn sodium has some use as a long-term asthma control medication. Cromolyn sodium is used to prevent the chemical release and activation of inflammatory cells in the airways and lungs. This drug is also commonly used to treat seasonal allergies because it stabilizes mast cells, the cells that release histamine and other inflammatory chemicals. Potential side-effects of this drug include throat irritation and coughing.
Albuterol and Levalbuterol
Both levalbuterol (Xopenex) and albuterol (AccuNeb) are used as a quick-relief drug for asthma. They are labeled as such because they are bronchodilators meaning they open the airways making it easier to breathe during an asthma attack of COPD exacerbation. While there are a number of potential side effects to combining these two drugs, the benefits may outweigh them. Be sure to follow your doctor’s instructions carefully.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Budesonide
Budesonide (pulmicort respules) is an inhaled steroid that reduces the number of inflammation-inducing cells in the lungs. It is the only corticosteroid administered through inhalation therapy and has proven extremely useful in reducing asthma symptoms. According to the 2015 Global Initiative for Asthma (GINA) guidelines, budesonide is one of the most effective drugs for long-term asthma control. Potential side-effects of budesonide include oral thrush, a yeast infection in the mouth, and a hoarse throat.

Acetylcysteine
Mucus is a substance secreted by mucous membranes. It plays an important role in the body by trapping particles like airborne allergens and viruses and keeps them from entering the lungs. Unfortunately, many respiratory diseases lead to an overproduction of mucus which can have negative effects like airway obstruction. Acetylcysteine is a drug that breaks up mucus and makes it less viscous allowing it to be cleared more easily.
Diseases Treated With Nebulizers
While browsing the web or watching television, you may have noticed that nebulizers are usually advertised towards kids with asthma. While they’re certainly most commonly used by children, many adults and seniors use them as well. What’s more, nebulizers can be used to treat many different respiratory conditions, not just asthma. Children may benefit from nebulizers if they don’t know how to use an inhaler and those with severe lung disease may not be physically capable of inhaling deeply enough to make inhalers an effective option.
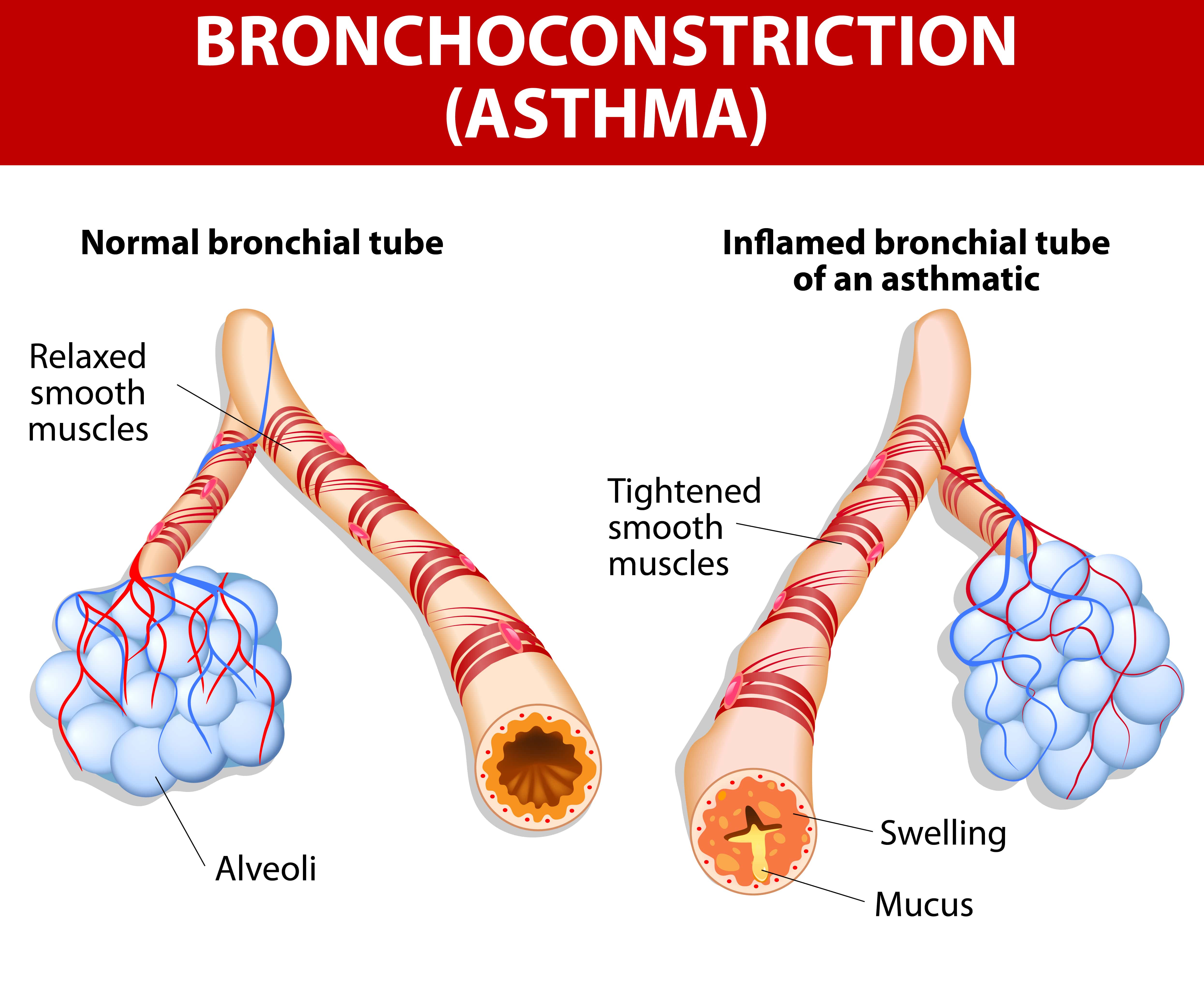
Asthma
Asthma is a lifelong lung condition that leads to inflamed and narrowed airways. Symptoms can range from mild to severe and happen frequently or in rare instances. Medication administered through inhalation therapy can help to reduce this inflammation, open up the airways, and help the patient breathe more easily and cough less.
Chronic Obstructive Pulmonary Disease (COPD)
COPD is an umbrella term that includes both chronic bronchitis and emphysema. Chronic bronchitis is similar to asthma in that it’s characterized by inflamed airways, more specifically in the bronchial tubes that lead to the lungs. However, bronchitis is caused by environmental factors like pollution, cigarette smoke, or a virus, whereas asthma is an increased responsiveness of the airways to irritants. This is a subtle difference, but it could mean having an entirely different treatment plan.
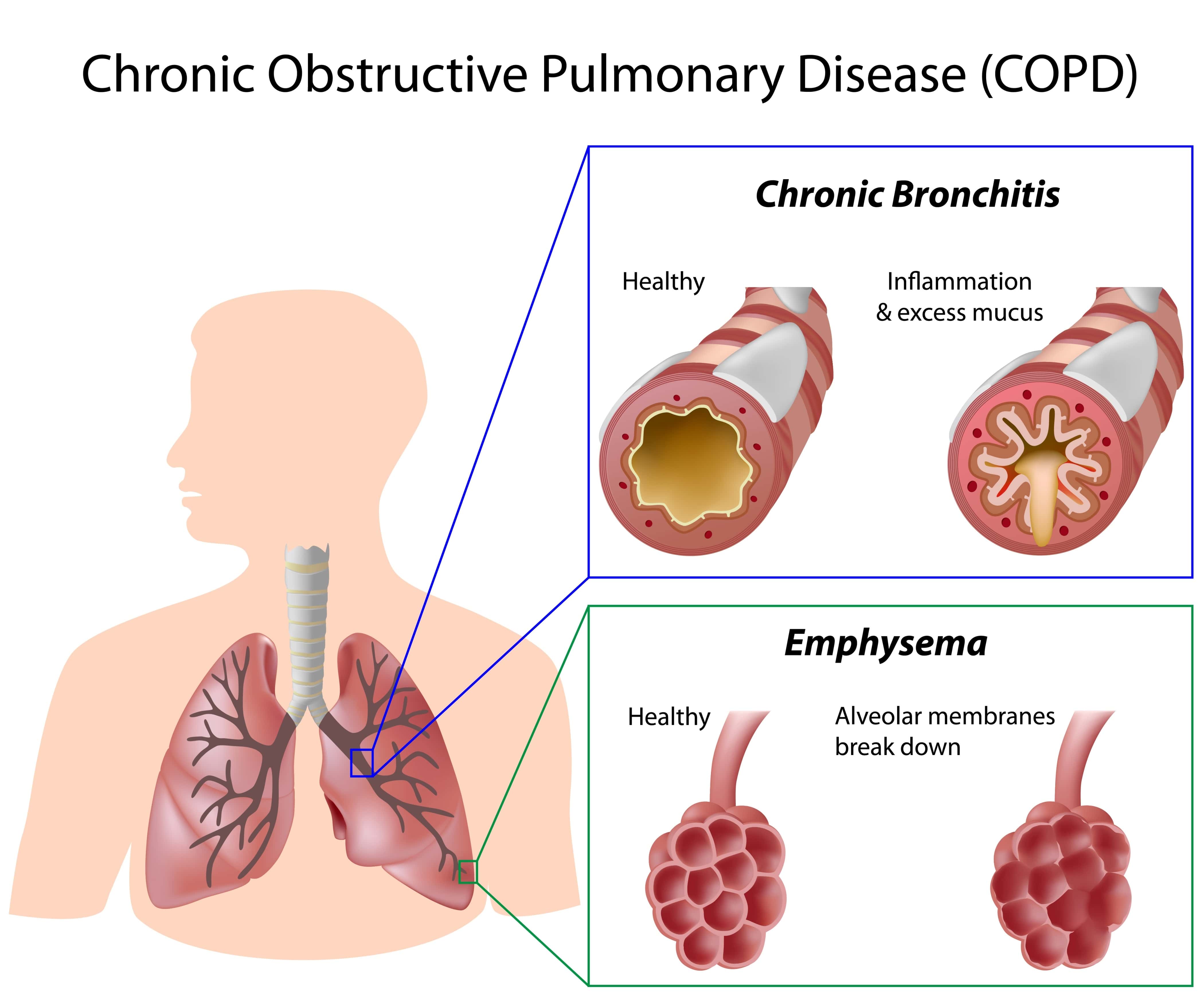
Emphysema, on the other hand, results in inflammation of the alveoli or tiny air sacs that are responsible for the exchange of oxygen and carbon dioxide in the lungs. Emphysema results in coughing, wheezing, increased mucus production, and an increased risk for acute respiratory illness, all of which can be treated with nebulizer therapy.
Cystic Fibrosis
This is a lung disease that causes mucus to be thicker and more viscous than normal. According to Medical News Today, 75 percent of cystic fibrosis cases are diagnosed before the age of 2 making it a significant concern among children. Acetylcysteine is one drug that will help to thin the mucus and make it easier for someone with CF to breathe.
Pneumonia
Nebulizers aren’t just effective in treating chronic lung conditions, they can be helpful for acute illnesses like pneumonia as well. In this disease, the tiny air sacs in the lungs fill with fluid resulting in an infection, chills, and difficulty breathing. In bacterial pneumonia, your doctor may prescribe you antibiotics that can be used through your nebulizer.
How To Properly Use a Nebulizer
The good thing about nebulizers is that they’re very easy to use. While all nebulizers will work slightly differently, they all have the same components and if you have any questions you can easily just consult the user’s manual or speak with your doctor.
- Clean your hands thoroughly — dirt or dust can damage the nebulizer.
- Attach the hose to either an air compressor or an oxygen supply
- Adjust the mouthpiece or mask on your face so that it fits snuggly
- Breathe normally through your mouth until all the medication has been administered. Usually, this takes around 10 to 15 minutes.
- Once you’re done, turn off the device, wash the mouthpiece and medicine cup, then leave it to dry.
How To Clean a Nebulizer
It’s very important that you take the time to clean your nebulizer regularly. If the components aren’t cleaned thoroughly or often enough you may spread bacteria which can lead to sickness. If you have COPD, getting sick could mean experiencing more frequent and severe exacerbations.
- Always use your nebulizer in a dust-free and smoke-free area
- Wash the hose and face mask or mouthpiece after each use and leave it to air dry.
- Remove the medication cup and rinse it thoroughly
- After several uses, take a bowl and put in it one part vinegar and three parts water. Soak the mouthpiece in it for 20 minutes then rinse and dry.
- When storing your nebulizer, always keep it in a bag, case, or covered in a towel to keep it clean.
- Keep extra filters on hand and check it at least once a month.
Nebulizers vs Inhalers
The most immediate and obvious difference you’ll notice between an inhaler and a nebulizer is that nebulizers are much bulkier. Even the portable nebulizers are bigger and heavier than inhalers because they have the electrical components, battery, and compressor, whereas inhalers are just the medicine container and a plastic cover to protect it. Some inhalers have something called a spacer that’s attached to the mouthpiece. This makes it a little easier for children or people with impaired lung capacity to inhale the medicine deeply and allow it to enter the lower lungs.

Nebulizer Therapy vs Oxygen Therapy
It’s important to understand the difference between nebulizer therapy and oxygen therapy. Whereas nebulizer therapy is used to administer medication to the lungs, oxygen therapy simply delivers pure oxygen to the lungs. Oxygen therapy is prescribed to patients who have impaired lung function and aren’t able to take in enough air or process oxygen as efficiently as a healthy person’s lungs. If you’re undergoing nebulizer (inhaled) therapy, you won’t necessarily be prescribed medical oxygen and vice versa.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Oxygen-Driven vs Air-Driven Nebulization
Normally, your nebulizer will be attached to an air compressor. However, depending on the doctor’s specifications, you may need to use a compressed oxygen tank instead. This is usually only beneficial if the patient is already oxygen dependent. For example, they may carry around an oxygen tank or oxygen concentrator to ensure their blood oxygen levels remain normal.. In these instances, doctors typically titrate the oxygen amount, meaning they adjust the amount of oxygen that’s administered through the nebulizer for the best results. However, too much oxygen could be dangerous.
According to a study published by BMC Pulmonary Medicine, high administration of oxygen may lead to hypercapnia (carbon dioxide retention) or increased mortality in patients experiencing an acute COPD exacerbation. Supplemental oxygen is usually adjusted to achieve an oxygen saturation of 88 to 92 percent.
Conclusion
Hopefully, this guide provided you with some helpful information that you can use to get started with nebulizer therapy. While nebulizers are extremely effective at administering medication for asthma, COPD, and other respiratory patients, it’s important that you also keep up with every other aspect of your treatment plan.
While respiratory disease is one of the most common afflictions on the planet, each case is unique. Be sure to maintain open lines of communication with your doctor and that you understand exactly when and how you should use your nebulizer in order to have the best results.
It’s been just over two months since we first heard reports of the coronavirus (COVID-19) entering the United States. During this time, we’ve learned an astonishing amount of information about where the virus came from, what it does to the body, and most importantly, how to protect ourselves and our loved ones.
While there’s still no cure in sight and it will likely be some time before medical specialists fully understand COVID-19, we have been given five clear and strict rules by the World Health Organization (WHO) that each and every person should follow.
- Wash your hands often with soap and water for at least 20 seconds
- Avoid touching your face
- Stay home when possible, especially if you’re sick
- Cover your cough with your shoulder or a kleenex
- Practice social distancing
Unfortunately, the above list does not take into account age, medical conditions, or susceptibility; these are simply guidelines that everyone should follow in order to slow the spread of the coronavirus. So, if you’re someone who’s suffering from a chronic illness that makes you more vulnerable to the effects of the virus, you’ll need to take extra precautions.
In this post, we’ll take a look at seven facts you should know about the coronavirus if you or a loved one is coping with chronic obstructive pulmonary disease (COPD). COPD is an illness that affects around 15.7 million Americans, so it’s imperative that these people are fully aware of how the COVID-19 pandemic affects them. If you have any questions, be sure to leave them in the comment sections or fill out the contact form so we can reach out to you.
What is the Coronavirus?
SARS-CoV-2 is a type of coronavirus that causes coronavirus disease 2019, also called COVID-19 for short. This new type of coronavirus was first discovered in Wuhan, China, a large city in the province of Hubei last December. Since then, it has gone on to infect more than 1,000,000 people worldwide and is responsible for over 70,000 deaths. Since COVID-19 has spread across the whole world at this point, it has earned the title “pandemic.”
In the past, coronaviruses have only been known to infect animals. However, a few have been known to pass onto humans and these are referred to as “alpha” and “beta” coronaviruses. The term “SARS” in SARS-CoV-2 stands for “severe respiratory distress syndrome” which is the primary symptom of most coronaviruses.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
It’s a “Novel” Disease
One of the most important things to know about COVID-19 is that it is considered “novel.” What this means is that it’s a new type of coronavirus that has never been seen before. In other words, we don’t have the decades of experience dealing with it like we do with influenza and other common diseases.
Another problem with it being a new disease is that we don’t have an immunity built up for it. Your body has two types of immunity that it uses to protect your body from harm; these include natural or “innate” immunity and “adaptive” immunity. Innate immunity is something that you’re born with. An example of this is mucus, a sticky substance that lines your sinuses, throat, and lungs which protects your body from infection.

Adaptive immunity, on the other hand, is immunity that your body develops over the course of your life. At a young age, you’re very vulnerable to infections like strep throat and ear infections, but as you age, your body develops a natural immunity to these things. Unfortunately, since COVID-19 is new to everyone, nobody has had the chance to build up an immunity to it.
Typically, when there is an outbreak of any type of disease in a particular region, there is enough scientific data from previous outbreaks in order to direct resources and efforts effectively. However, in the case of a new type of disease like COVID-19, it becomes very difficult for medical professionals to make decisions about where and when to divert their resources. We can see this in the United States through the shortage of ventilators and medical face masks which could help to prevent the spread of the virus.

Lastly, the fact that COVID-19 is a new virus means that it’s difficult to accurately depict its severity. While we now know that there are over 370,000 cases and over 12,000 deaths in the United States, back in January when it first entered the country, it would have been impossible to predict just how bad it would get. With that being said, it’s difficult for us to predict how much damage COVID-19 will cause in the near and distant future, so it’s best to be prepared for the worst.
COPD Patients are at a Higher Risk
Since COVID-19 is a respiratory illness, it goes without saying that people who already suffer from a chronic respiratory disease will experience more severe symptoms. Chronic obstructive pulmonary disease (COPD) is primarily caused by smoking and it’s characterized by symptoms such as shortness of breath, chest pain, coughing, and wheezing. Millions of Americans already have COPD but experts estimate that as many as 81% of cases worldwide may be undiagnosed.
One of the primary ways COPD affects a patient’s ability to cope with the novel coronavirus is through lung inflammation and a weakened immune system. Most COPD patients develop a condition called immune dysfunction which puts them at a higher risk for exacerbations and compromises their ability to fight off common lung infections. When it comes to a virus that has never been introduced to the general population like COVID-19, the risk of contracting it is even more pronounced.

COPD News Today advises that patients with chronic lung illnesses take the following precautions in addition to the preventive measures listed by the World Health Organization:
- If you are using any type of medication like corticosteroids, bronchodilators, or methylxanthines, you’ll ideally want to stock up on these as much as possible. The more you can limit leaving the house to refill a prescription, the better. Doctors aren’t always able to prescribe a large quantity of a particular drug, but due to the circumstances, they might make an exception. Prescription deliveries are also becoming more common, so those might be worth considering as well.
- Secondly, COPD News Today advises that all COPD patients avoid unnecessary travel and large crowds. Necessary travel means leaving the house to get food or other essential supplies or to visit a friend or loved one. However, COPD patients should have their groceries delivered if at all possible and practice social distancing when visiting family.
- When it comes to medical treatment, it’s important to seek help as soon as possible and be prepared in case of an emergency. COVID-19 exhibits some of the same symptoms as COPD, so if you notice an unusual flare up or you shouldn’t wait to receive medical attention. Keep a list of emergency contacts on hand at all times.
- Last but certainly not least, you should take care to disinfect your home regularly. According to a study published in the New England Journal of Medicine, SARS-CoV-2 can live on surfaces for several days depending on the surface and the climate. This study found that it can survive 3 hours in the air, 4 hours on copper, 24 hours on cardboard, 48 hours on stainless steel, and 72 hours on plastic. You should take time to disinfect surfaces like door handles, computer keyboards, your cellphone, and tables or counters at least once a day. Also, be sure to use organic cleaners rather than ones filled with chemicals that can exacerbate COPD symptoms.
It’s worth noting that anyone with a chronic health condition is more prone to severe coronavirus disease, not just COPD patients. While there is still limited information on the risk factors of COVID-19, the Centers for Disease Control and Prevention (CDC) warns that people with moderate to severe asthma are more likely to experience an asthma attack, pneumonia, or acute respiratory disease.

The CDC lists several other conditions that could lead to a higher risk of experiencing severe symptoms from COVID-19. They include the following:
- People with serious heart conditions
- People with diabetes
- People with liver or kidney disease
- People with an immunosuppressive condition (many conditions can lead to a compromised immune system)
- People with a body mass index of 40 or higher
Older Adults Experience More Severe Symptoms
Another risk factor we’ve been told to watch out for is age. According to CDC reports, fatality is highest among people 85 years of age and older, from 10% to 27%. People between the ages of 65 to 85 had between a 1% and 5% fatality rate and people under the age of 65 have under 1% fatality rates.

You’ve likely heard about fatality rates being unusually high in places like Italy, and this is largely due to the fact that the general population is much older than in other parts of the world. Stat News, a health and medicine news website, notes that the median age in Italy is 47 which is the highest in Europe. What’s more, 23% of the population is over the age of 65 and Italy has reported that 7.2% of people who contracted COVID-19 have died. This is significantly higher than the 1.8% to 3.4% fatality rate reported in the United States.

In many instances, fatality among the older population has less to do with their age and more to do with the fact that older people are more likely to have a chronic illness. According to the National Council on Aging, about 80% of older adults have at least one chronic disease and 77% of older adults have at least two chronic diseases. What’s more, four illnesses cause two-thirds of all deaths in any given year — diabetes, stroke, cancer, and heart disease. When you look at these numbers, it’s not hard to see why COVID-19 is such a significant threat to older generations.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Safety Compliance is Important Regardless of Age
Despite the fact that COVID-19 is more severe in older adults with chronic illnesses, that doesn’t change the fact that slowing the progression of the virus is the responsibility of everyone. While you may have heard individual cases of younger people contracting the virus and not experiencing any symptoms, these people are definitely the minority, so people of all ages and health conditions should take it seriously.

In addition to COVID-19 being a threat to younger generations, contracting the virus could mean passing it on to older generations, because the majority of cases are passed from person-to-person rather than from objects to people. Hospitals and nursing homes are particularly vulnerable to outbreaks so if younger people want to visit their parents or grandparents, it’s best to do so through video conference programs like Skype or Facetime.
Your COPD Treatment Plan is Still Important
We understand that times like these can be stressful and filled with uncertainty. And even when we don’t have a pandemic to deal with, it can be challenging to keep up with everything in your COPD treatment plan including pulmonary rehabilitation, an improved diet, and oxygen therapy. However, if history has taught us anything, it’s that we can achieve better outcomes if we focus on a healthy daily routine.
If your pulmonologist has already set you up with a COPD treatment plan, it’s best to stick with it unless he/she tells you to make adjustments. The reason it’s so important to do this is because it gives you the best odds of coping with COVID-19 if you were to contract it. It’s important to note, however, that simply following your COPD treatment plan won’t prevent the virus; you’ll still need to follow all the safety precautions listed above to prevent getting sick.
Pulmonary rehabilitation is the backbone of any good COPD treatment plan. Most often, your pulmonologist will set you up with a one-on-one exercise training course with a physical therapist. However, due to the current circumstances, it’s unlikely that you will be set up with an in-person pulmonary rehab program. Instead, you will likely be offered some type of online pulmonary rehab like Thrive eLearning where you’ll have access to important information for managing your disease. You’ll also be able to speak with respiratory therapists wherever and whenever you need.

Another aspect of your COPD treatment plan, your diet, can be very difficult to maintain with the spread of COVID-19. Grocery stores are a bad place to be right now because they are full of people and it’s difficult to maintain good social distancing practices. What’s more, grocery stores are on low supply of a lot of foods, so it can be difficult to find exactly what you’re looking for. Sites like Fresh Direct are great options for anyone with a chronic health condition like COPD because you can have groceries delivered directly to your door. If online grocery shopping is not an option, you may want to get a friend or loved one to go shopping for you.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Last but certainly not least, you’re going to want to continue with your oxygen therapy treatment program as advised by your pulmonologist. Oxygen therapy helps to keep your respiratory condition stable, reduce feelings of breathlessness, and most importantly, helps prevent exacerbations and hospitalization due to COPD symptoms. There are many types of oxygen generator on the market, but most doctors recommend portable oxygen concentrators like the Inogen One G5, because they’re lightweight, easy to use, and provide a high oxygen output.

Pay Attention to the News
Whenever there’s a pandemic or any other type of national emergency, you often get two different types of people: the ones who have the news on 24/7 and the ones who try to avoid the news as much as possible in order to avoid anxiety. While we certainly don’t want anyone to sit at their TV all day and stress about the current circumstances, it is important to keep up with what’s going on and understand what the recommended safety guidelines are for dealing with COVID-19.

If you don’t want to tune into the news everyday, that’s understandable. However, be sure to bookmark these pages by the Centers for Disease Control and Prevention and the World Health Organization. Check these sites regularly and they will provide you with up-to-date information about COVID-19 prevention, travel guidance, as well as correcting some misinformation that’s out there in the public.

Conclusion
For many people, these are difficult times. The novel coronavirus has taken a pretty large toll not just on the health of the public but on the economy as well. It’s imperative that everyone — young or old, healthy or not — does their part to limit its spread. This means practicing good hygiene, keeping at least 6 feet of space between you and the nearest person, and staying home as much as possible.
As a COPD patient, you’ll need to take some additional precautions like stocking up on medical supplies, disinfecting your home regularly, and avoiding any form of unnecessary travel. You should continue to follow your COPD treatment plan unless otherwise advised by your pulmonologist.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













