Anyone who reads our articles regularly should be pretty well-acquainted with the term chronic obstructive pulmonary disease (COPD). It’s one of the leading causes of death in the United States and it’s largely caused by preventable risk factors like cigarette smoke and air pollution. But there’s another common lung disease that’s often overlooked due to its many similarities with COPD. This disease is called bronchiectasis (brong-kee-EK-ta-sis).
Bronchiectasis is a condition that leads to permanent damage in the bronchial tubes, the main passageway leading to the lungs. As the airways widen and thicken, bacteria and mucus begin to build up leading to frequent infections and blockages. While there is no cure for bronchiectasis, it can be managed effectively and further damage can be prevented with a proper treatment plan.
While bronchiectasis has a lot in common with COPD, asthma, and cystic fibrosis (CF), these are all different conditions. In this post, we’ll tell you everything you need to know about bronchiectasis including symptoms, risk factors, treatment options, and more. We’ll also help you clarify these conditions so that you don’t get them confused. If you have any questions, be sure to fill out the contact form at the side of the page so that one of our respiratory specialists can reach out to you.
What is Bronchiectasis?
The respiratory system is much more complicated than it appears on the surface. While its primary function is to bring oxygen into the body and remove carbon dioxide, the lungs rely on a whole host of other factors in order for this process to work as it should.
One of the most important functions is the production and use of secretions like mucus, phlegm, and sputum. While you may know these as the annoying substances you cough up when you’re sick, they also play a vital role in the respiratory process.
Mucus — a sticky and slimy substance — is part of your innate immune system, your body’s natural defense against foreign invaders. It’s produced by the mucous membranes in the nose and sinuses. Phlegm is a similar substance but it’s produced in the lungs and the lower respiratory tract airways.

In a healthy person, mucus lines the throat, lungs, and nasal passages keeping it from drying out or becoming inflamed. It also acts as a sort of filter by trapping dust, pollen, and other airborne particles that could damage your lungs. It even has antibodies in it that work to locate and neutralize bacteria that enter your body.
Normally, mucus is able to flow freely throughout the respiratory system, but in a patient with bronchiectasis, it becomes stuck in the lungs due to abnormal dilation of the bronchi. This results in what the American Thoracic Society refers to as the “vicious cycle hypothesis” of bronchiectasis. Here’s an overview of what this looks like:
- Abnormal mucus clearance
- Bacterial colonization
- Neutrophil inflammation (proteases)
- Airway destruction (bronchiectasis)
- Repeat
Let’s take an in-depth look at each one of these steps.
Abnormal mucus clearance
Mucociliary clearance is one of the most essential innate defense mechanisms of the lungs. During this process, the protective mucus layer, cilia, and the airway surface liquid layer work to remove mucus and potentially harmful foreign substances from the lungs.
The cilia are specialized organelles found in the respiratory tract. They move in a rhythmic pattern that keeps mucus and harmful substances from getting trapped. However, a condition known as primary cilia dyskinesia (PCD) results in abnormal cilia and an inability of the body to clear mucus properly — as a result, this is often the first step in the development of bronchiectasis.
.png)
Asthma and Cystic Fibrosis (CF) are two other conditions associated with the pathogenesis of abnormal mucociliary clearance. Studies have found that asthma patients who have a difficult time managing their disease are more likely to experience complications that can lead to bronchiectasis.
Another factor that impacts the clearance of mucus is the contents and viscosity of the mucus itself. Cystic fibrosis (CF) is a genetic condition caused by a mutation in the cystic fibrosis transmembrane regulator (CFTR). This gene is responsible for providing instructions for creating a channel that transports particles into and out of the cells. This often impairs the flow of water in tissues, leading to viscous mucus that doesn’t flow freely.
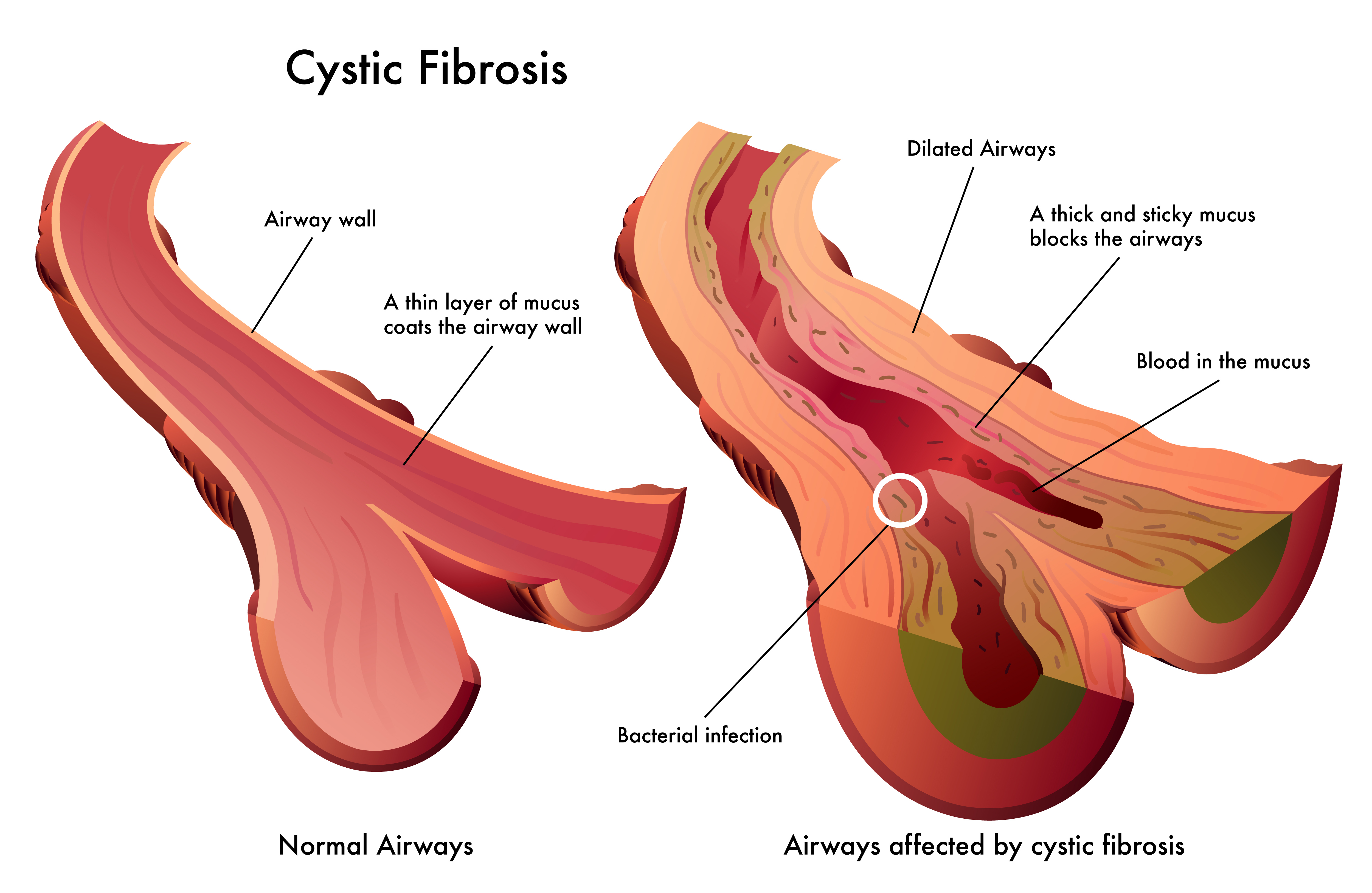
Oftentimes, medical experts will categorize bronchiectasis into one of two groups: cystic fibrosis bronchiectasis (CFB) or non-cystic fibrosis bronchiectasis (NCFB). CFB patients will likely need to be treated for their underlying cystic fibrosis symptoms in order to see notable improvements whereas NCFB patients may require any number of treatments depending on what is causing the abnormal mucus clearance.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Bacterial colonization
The term “colonization” simply refers to the gathering of bacteria on a surface such as the airways, skin, mouth, or intestines. In the case of bronchiectasis, bacteria begin to colonize in the bronchial tubes, the airways that lead to the lungs. If the immune system isn’t able to neutralize the bacteria, it could lead to an infection.
.jpg)
Neutrophil inflammation (proteases)
A neutrophil is a white blood cell that fights infections and heals damaged tissue in the body. A low neutrophil count in the body (neutropenia) is associated with an increased risk of infection, whereas a high neutrophil count (neutrophilia) is typically caused by infection or injury.
Airway destruction (bronchiectasis)
The final part of the cycle is airway destruction. Repeated instances of infection and airway inflammation eventually lead to permanent and irreversible damage to the airways. Normally, the bronchial tubes narrow smoothly towards each lung allowing for air to easily transfer into and out of the body. However, inflammation caused by bronchiectasis will eventually cause the bronchial tubes to become scarred and ineffective. The cilia which help to move mucus will also be damaged.
Symptoms of Bronchiectasis
Bronchiectasis symptoms can take months or years to develop making it a difficult condition to detect. Like many lung conditions, bronchiectasis is often shrugged off as natural signs of aging or it’s confused with other conditions like asthma or COPD. Regardless, there are a number of symptoms you should look out for if you think you have bronchiectasis:

- A persistent, chronic cough
- Frequent production of sputum
- Chest pain
- Recurring chest infections
- shortness of breath
- Fatigue
- Weight loss
-
Coughing and wheezing
Since bronchiectasis is a progressive disease, you may notice symptoms becoming worse over time. For example, after getting sick, you may notice more chest pain, tightness or breathlessness. Severe bronchiectasis may lead to more serious conditions such as low oxygen levels, collapsed lung, respiratory failure, or even heart failure.
Common Causes of Bronchiectasis
Pneumonia
Pneumonia is an infection that can occur in one or both lungs. It causes inflammation in the alveoli, tiny air sacs at the end of the bronchial tubes that are responsible for transferring oxygen and carbon dioxide to and from the blood. Pneumonia can be caused by bacteria, viruses, and fungi.
Tuberculosis
Tuberculosis is another common cause of bronchiectasis. This is a highly contagious infection that typically attacks the lungs, but it can spread to other parts of the body too including the spine and the brain. In the early 1900s, it was a leading cause of death, but it has a much better survival rate now because of the widespread use of antibiotics to treat it.
Aspiration
The term “aspiration” refers to a substance such as saliva, food, or medicine entering the lungs. Sometimes, this can be harmless, but other times it can lead to choking or even a serious infection known as aspiration pneumonia. This is typically not contagious and is usually treated with antibiotics.
Obstructive airway disease
Obstructive airway diseases like asthma, COPD, and cystic fibrosis can all be significant contributors to the onset of bronchiectasis because they impair a person’s ability to clear mucus and may even contribute to compromised immunity. Your doctor will closely monitor your condition to ensure that all underlying conditions are accounted for.
Risk Factors of Bronchiectasis
Risk factors of bronchiectasis include the following:

- Age — bronchiectasis can be contracted at all ages, but it’s much more common in people over the age of 65.
- Gender — bronchiectasis is more common in women due to hormone types and hormonal events such as menstrual cycles, pregnancy, and menopause.
- Cystic fibrosis — while only about half of bronchiectasis cases are caused by CF, 50 to 70 percent of children with CF have bronchiectasis by 3 to 5 years of age.
- Allergic bronchopulmonary aspergillosis
- Cilia function disorders
- Autoimmune disease
-
Immunodeficiency
How is Bronchiectasis Diagnosed?
Unfortunately, bronchiectasis is commonly underdiagnosed or misdiagnosed due to the fact that it has so many similar symptoms to conditions like asthma, bronchitis, and COPD. In these situations, it may go months or years without being treated effectively. To avoid this, your doctor may perform any number of tests that can rule out other conditions.
First and foremost, your doctor will take a look at your medical history. The following may indicate that you’re at a higher risk of contracting bronchiectasis:

- Family history of bronchiectasis
- A history of childhood respiratory symptoms or infection
- Smoking history
- Evidence of an inflammatory disorder (muscle pain, skin rashes, or joint problems)
- Frequent infective exacerbations
Next, your doctor will perform a clinical examination. This includes the following:
- Pulmonary function tests (PFT) such as spirometry or peak flow
- Testing for the presence of sputum
- Tests for a systemic inflammatory disorder
- Stethoscope testing to check for irregular noises in the lungs
-
Blood or sweat tests can be used to rule out different types of bronchiectasis (CF bronchiectasis or non-bronchiectasis)

Last but not least, your doctor may use high-resolution computed tomography (HRCT) to check for bronchiectasis symptoms. He/she will look for the following:
- Bronchial wall dilation
- Lack of bronchial tapering
- Lobar collapse
- Mycetoma formation
-
Aspergillus fumigatus

HRCT tends to be the most conclusive diagnostic tool for determining the type and severity of bronchiectasis. However, your doctor will likely use many of the methods above in order to more accurately diagnose your condition.
How is Bronchiectasis Treated?
Bronchiectasis treatment is varied and depends on the underlying cause of the condition. In general, it can be treated with physical therapy, hydration, and medicines. However, if the bronchiectasis is isolated, your doctor may recommend surgery. Conversely, if the bronchiectasis is widespread and you risk respiratory failure, he/she may recommend oxygen therapy.
The objective of bronchiectasis treatment is to remove mucus from the lungs, treat infections quickly, treat underlying conditions that could be causing bronchiectasis, and to prevent any life-threatening complications. While bronchiectasis is a progressive disease, breaking the “vicious cycle” we discussed earlier can prove extremely effective in slowing the progression of the disease.
Antibiotics
An antibiotic is a type of medicine that helps prevent and stop infections that are caused by bacteria. If you’re suffering from a viral infection, your doctor will not prescribe antibiotics because they will not be effective.

Mucus Thinners
Because bronchiectasis patients have poor mucociliary clearance, they usually need to take medication that can assist with removing mucus from the lungs. Expectorants are a type of medication that loosens mucus so that it can be coughed up. Mucus thinners like acetylcysteine can also help with this process.
Hydration
Hydration is important for everyone, but for bronchiectasis patients, it could be a matter of life and death. Your doctor will likely put you on a strict diet requiring you to drink a certain amount of water each day. You might need to avoid alcohol and food that’s high in sodium as well.

Physical Therapy
Chest physical therapy (CPT) or physiotherapy is a chest percussion technique that’s used to loosen and dislodge mucus that gets stuck in the lungs. More often than not, this procedure is done by your doctor or a trained professional but self-treatment is sometimes advised with the use of tools like inflatable therapy vests. These use high-frequency airwaves to force mucus into your upper chest making it easier to clear.
Other Treatments
The above treatments are commonly used to treat bronchiectasis but in rare cases, other treatment options may be advised. These include bronchodilators that relax muscles in the airways; corticosteroids used to reduce inflammation; and oxygen therapy to raise blood oxygen levels. In very rare cases, surgery may be advised.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Bronchiectasis Prevention Methods
While bronchiectasis is largely brought on by genetics, there are several lifestyle changes that you can make to reduce your chances of contracting it.

- Maintain proper hygiene, i.e. wash your hands, sanitize your home and workplace.
- Ensure you are up-to-date on annual influenza and pneumonia vaccines.
- Seek immediate treatment for lung symptoms like a chronic cough, chest pain, and chest tightness.
- Avoid harmful airborne irritants like car exhaust, fumes, and cigarette smoke.
As with most chronic lung conditions, early prevention and diagnosis are key. The sooner you can implement these prevention techniques, the better your outcome will be.
Bronchiectasis Versus COPD
While bronchiectasis and COPD may produce some similar symptoms, they’re very different diseases. COPD is one of the most common morbidities, affecting about 16 million people in the United States alone. It’s primarily caused by preventable means such as the inhalation of cigarette smoke and other harmful airborne contaminants — about 85 to 90 percent of COPD patients have smoked.
Bronchiectasis, on the other hand, is far less common than COPD. It’s estimated that 110,000 people have bronchiectasis in the United States and it affects people of all ages. Unlike COPD, lung damage from bronchiectasis is the result of severe and recurrent lung infections that damage the bronchial tubes, and in turn, lead to more infections. Studies have shown that comorbidities of COPD and bronchiectasis are common, but researches don’t yet know all the details about their correlation.
Conclusion
Bronchiectasis receives far less media attention than conditions like COPD, asthma, and lung cancer, but it’s one that everyone should be aware of regardless of your age. The good news is that, with early diagnosis and proper lifestyle changes, bronchiectasis patients will see a huge improvement in their quality of life and life expectancy.
Ultimately, your best course of action is to make healthy lifestyle choices like exercising frequently, maintaining a healthy diet, and avoiding cigarettes or other drugs. If you experience chest pain, frequent lung infections, or any of the symptoms listed above, be sure to visit your doctor or pulmonologist immediately.
Getting diagnosed with COPD and watching your body change can be a disheartening thing to go through. This, along with the symptoms of COPD, make depression a reality for a large number of COPD patients.
It's not too difficult to see why; COPD can lead to weight loss, fatigue, sleep disorders, poor nutrition, and a variety of other uncomfortable symptoms. These ailments can be distressing on their own, leading to health anxiety, a negative outlook, and a feeling of loss of control over one's life.
According to some studies, up to forty percent of COPD patients suffer from depression. What's worse, many cases go untreated, which makes patients more likely to suffer a quicker physical decline and death.
But, while COPD can be difficult to cope with, there are plenty of options for support and treatment that can help you take back control over your life. Even though depression can make obstacles seem too difficult to face, the truth is that you can find the power within yourself to overcome them.
It is important to remember that it's more than possible to live a happy and fulfilling life despite the hardships that come along with COPD. If you can shake yourself free of anxiety and depression, you'll find that you have the ability cope in healthy ways and confidently meet any challenges that come your way.
It's hard to see the light when you are in the midst of depression and everything seems hopeless and bleak. That's why it's so important to recognize the signs of depression and seek treatment, and in this article we're going to show you how.
In the next sections, we'll show you how to identify depression and explain how it affects people with COPD. Then, we'll show you how to utilize available mental health resources and how to use a variety of practical techniques to help yourself out of depression.
What is Depression?
The term “depression” is often used loosely in casual conversation, but in reality, it is a serious medical illness. It is much more than just feeling a little down for a few days; it's a deep state of sadness and helplessness that affects many aspects of sufferers' lives.
Depression is often marked by hopelessness, lack of motivation, and lack of interest in activities that you used to enjoy. Depression often interferes with your ability to function and participate in activities at work, home, and with friends.
People who are depressed are also more at risk for a variety of other health problems, including obesity, substance abuse, and premature death. In general, people who are depressed have difficulty maintaining healthy habits and lead a significantly reduced quality of life.
Depression should always be taken very seriously and should never be ignored. If you or someone you know is showing the warning signs of depression, you should encourage them to seek help as soon as possible.
Symptoms of Depression

The main characteristics that separate clinical depression from normal sadness or negative moods is its severity and its duration. Everyone has a bad day or bad week every once and awhile, but people who suffer from depression often experience weeks or months of despair along with a variety of noticeable physical symptoms.
Here are some of the most common symptoms of depression:
- Sadness
- Emptiness
- Hopelessness
- Anxiety
- Helplessness
- Feelings of worthlessness
- Feelings of guilt
- Difficulty concentrating
- Difficulty sleeping
- Irritability
- Loss of appetite or increase in appetite
- Fatigue
- Lack of interest in hobbies and activities you used to enjoy
- Thoughts of death or suicide
How Depression Affects People with COPD

If left untreated, depression in people with COPD can significantly increase their risk for physical decline. It can increase patients' risk of exacerbations, loss of physical mobility, malnutrition, and even death.
There are many reasons for these risks, most of which have to do with changes in behavior and motivation that happen to COPD patients who are depressed. For example, depression can affect both your appetite and your sleep quality, leading to malnutrition and sleep deprivation. This, in turn, weakens your body, makes COPD symptoms worse, and depresses your immune system, making you more prone to exacerbations and hospitalizations.
Studies also show that people with COPD who are depressed are more likely to be hospitalized, less likely to adhere to COPD treatments, and have a much higher risk of death. They are also more likely to smoke and suffer from an overall decreased quality of life.
One of the most damaging effects of depression is how it can take away your motivation to do things that make you healthy and happy. Many people who are depressed stop exercising, eating, and socializing, which are important to living a healthy life with COPD.
There is hardly anything more essential for keeping yourself healthy with COPD than following your treatment plan, eating a healthy diet, and, especially, getting plenty of exercise. However, depression can take away your motivation to do all of these things, causing you to skip meals, workouts, and medication doses. This is a large part of the reason why many depressed COPD patients suffer a more rapid physical decline.
Another reason is the fact that being depressed can make it much more tempting to reach for unhealthy coping mechanisms like cigarettes and other drugs. Since smoking is one of the most damaging things you can do to your body when you have COPD, depression can be even more damaging to patients who are former smokers or who are currently trying to quit.
For all of these reasons, it's vitally important for COPD patients who suffer from depression to seek support and treatment as early as possible. It's certainly not something you should ever take lightly or ignore, as it could have huge and irreversible effects on your health.
Everyday Techniques for Reducing Depression for People with COPD

Everyday activities like diet and exercise can have a huge impact on how you feel. Building healthy habits in these areas is an important first step to breaking free from depression and getting yourself back on track to living a healthy, fulfilling life.
Exercise More

When you are feeling depressed, exercising and being active might sound like the last thing in the world that you want to do. However, getting out of bed every day and doing some physical activity can actually improve your depression, not to mention that it's absolutely necessary to prevent early death from COPD.
It can be difficult and disheartening to exercise when you're experiencing COPD symptoms like breathlessness and wheezing, which on its own can contribute to depression and exercise avoidance. However, skipping exercise will only make that same problem worse, making your body weaker and your lungs decline quicker.
On the other hand, forcing yourself to get out, move your body, and increase your fitness can do wonders for both your body and mind. It not only stimulates your brain and promotes a more positive mood, but it can also increase your physical strength and mobility, allowing you to breathe better, do more, and have more energy.
Here are some of the benefits of exercise for people with COPD:
- More efficient use of oxygen
- Stronger breathing muscles and using less energy to breathe
- Reduced shortness of breath
- Reduced anxiety and depression
- Improved self-esteem and self-image
- Increased physical endurance
- Increased energy levels and reduced fatigue
- Improved sleep quality and reduced insomnia
- Increased cardiovascular health and fitness
- Improved muscle strength

It's not hard to see how getting regular exercise can help with depression caused by COPD. As you see your physical strength and condition improve, you are bound to feel more confident and more optimistic about your future.
Committing to exercising even when you feel down will also allow you to stave off some of the most devastating effects of depression for people with COPD—loss of physical strength and quicker lung function decline. It can also put you in a much better place both physically and mentally to cope with and manage your disease.
That's why it's so important to exercise according to your COPD treatment plan, even when it's hard and you don't feel like it. As soon as you start to neglect your exercise plan, you can quickly fall into a negative downward spiral, where it becomes more and more difficult to exercise.
If you find exercise difficult or don't know where to start, talk to your doctor about joining a pulmonary rehabilitation program. There are also many resources online, such as the Cleveland Clinic, that offer advice and ideas for specific exercises for people with COPD.

Here are some general tips and resources to help you exercise with COPD:
-
Start small and work your way up. Start by walking short distances or doing low-impact strength exercises, and increase the distance you walk and the number of repetitions you do by just a little bit every week. The improvements you make will motivate you to keep going and help you work up to more activity over time.
-
If you have limited strength or physical mobility, try starting out with some chair exercises. These allow you to work out different parts of your body while sitting in a chair, which helps with balance and reduces the amount of strength you have to expend while still toning your muscles. Check out this comprehensive guide for a huge list of chair exercises with accompanying illustrations and instructions for how to perform them.
-
Stretching exercises are easy to do and can improve your strength, mobility, and range of motion. You should always stretch before you workout, but you can also try stretching in the mornings and evenings to get some extra activity and keep yourself limber throughout the day. Check out this guide from Lung Foundation Australia that includes instructions for how to do a variety of different stretches.
-
Use breathing exercises, such as pursed-lips breathing and diaphragmic breathing to help with breathlessness and wheezing when you work out. You should also keep your bronchodilator, supplemental oxygen, and any emergency medications with you in case you need them. Check out this guide from the Cleveland Clinic on how to manage your breathing while you exercise.
- Try joining a fitness class or trying an exercise like yoga or Tai Chi. Having instruction (at a gym or from an exercise tape) can help you get started more easily and keep you motivated to continue. Yoga and Tai Chi are especially good exercises for people with COPD because they incorporate breathing control and meditation in their routines.
Eat Well

When you are depressed, you might not feel like eating as much as you should. It can also make you feel sluggish and unmotivated, making you more likely to reach for convenient, unhealthy options, like fast food, instead of making nutritious meals at home.
But when you have COPD, proper nutrition is vital for keeping your body and lungs healthy. Lungs affected by COPD use up more energy when you breathe, meaning that many patients actually need extra calories to keep their lungs working efficiently.
Eating well is also important for improving depression, as the foods you eat can have a huge impact on both your body and your mind. If you eat unhealthy foods or let yourself become malnourished, you will feel even more tired, fatigued, and depressed.
A variety of nutritional deficiencies and imbalances can contribute to depression, including deficiencies in fats, amino acids, Vitamin D, and blood sugar imbalances. However, proper nutrition can help restore balance to your body and mind, giving your brain the vitamins and nutrients it needs to keep you happy and healthy.

Unfortunately, the symptoms of COPD often make it difficult to maintain a healthy weight and get enough nutrition. However, having a healthy BMI is important for managing the disease; obese COPD patients face a wide variety of health risks, while underweight patients are also more likely to experience more rapid physical decline and other health complications.
Some COPD patients find it difficult to get enough to eat because of COPD symptoms like breathlessness, which often are worse on a full stomach. If you are also depressed, you may experience a reduced appetite, reduced motivation, and reduced enjoyment from the taste of food, which makes it even more difficult to get enough calories and nutrients every day.
If you have COPD, you should think of every meal as an opportunity to strengthen your body and support the health and function of your lungs. Even though it can be difficult and time consuming, it's important to eat whole, home-cooked foods as much as possible so you have maximum control over what nutrients you put in your body.

Even though it might be difficult and require some adjustments to your schedule, you can find ways to eat healthy with minimal effort and discomfort. Here are a variety of tips and techniques for eating well to improve your depression and your COPD:
-
Increasing your intake of certain foods has been shown to help fight depression. These include foods containing Vitamin D, omega-3 fatty acids, vitamin D, vitamin C, magnesium, selenium, and B vitamins.
-
Avoid sugary drinks, caffeine, and fried foods, which can contribute to depression. Instead, increase your intake of water, healthy fats, complex carbohydrates, and whole fruits and vegetables. Here is a guide from Healthline to help you choose healthy, nutrient-rich foods for your kitchen.
-
To avoid feeling uncomfortable and breathless when you eat, have several smaller meals throughout the day instead of large ones. This will help you eat enough calories without ever feeling too full.
- Prepare meals and freeze them ahead of time to eat on days when you feel especially depressed or fatigued. That way, even when you don't have the energy or motivation to cook, you can eat a nutritious, home-cooked meal with hardly any effort at all.
Get Out, Socialize, and Have Fun

Being depressed tends to cause people to isolate themselves and give up on the hobbies and activities that used to make them happy. This is partially due to a lack of energy and motivation, and partially due to a feeling of helplessness and a perceived inability to enjoy things that used to be fun.
However, even when things seem bleak, it's important not to neglect the people, hobbies, and productive activities that used to make you happy. Even if it doesn't feel satisfying right away, being social and active can improve your depression and will likely feel more satisfying with time.
Depression has an uncanny ability to make you avoid the very things that you need the most in order to break free from depression. Just remember that, even though things may seem hopeless right now, you will be much worse off if you give up and drop out of life's activities.
When you feel like staying indoors and avoiding the world, try calling up a friend or family member instead. Often, simply talking to someone else can help to pull you out of the fog and give you a more positive perspective on life.
It's okay to take days off and focus on self-care, but it's important not to let yourself stay in bed all the time and avoid the people who care about you. If you make an effort to get out of the house and spend time with family and friends, you will find it much easier to cope with depression and COPD.

And remember, it's okay to talk to your friends and family about your depression and let them know that you need support. Most people who care about you will understand and be willing to support you when you really need them.
Having a support group of family and friends and activities will give you something to get out of bed for and live for everyday. So don't let yourself become isolated from the people and things that matter in life; once you break out of your bubble, you might just start to notice all the many things that make life worth living.

Getting enough sleep can help your well being in a number of ways, your mental health, your physical capabilities, and so much more. But if you have sleep apnea, falling asleep, let alone sleeping through the night is an impossible task.
There are many reasons why people have sleep apnea, and understanding why you have sleep apnea is a critical step in treating it. Once you understand the root of the issue and what is causing it, you will be able to actively target the issue and hopefully get back to bed!
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In this blog we will discuss why sleep is so important, especially as you get older. We will also talk about sleep apnea diagnosis and the telltale signs that you should talk to your doctor about your sleep. Once you are diagnosed with sleep apnea, you may need to start using a portable oxygen concentrator while you sleep, so we will discuss your oxygen therapy options as well.
7 Reasons Sleep is so Important
![]()
1. Sleep Boosts your Immune System
It is important for your body to get the sleep it needs so that your immune cells are rested and strong to fight off allergies, germs, viruses and whatever aliment comes their way. Avoiding sickness like colds or the flu reduces your chance of ever experiencing a COPD exacerbation. The American Academy of Sleep Medicine suggests that sufficient sleep can also enhance vaccines effectiveness, which is obviously a plus, especially now that the COVID-19 vaccine has been rolled out in the United States, and it is crucial for COPD patients health.
2. More Sleep Will Help Shed the Extra Weight
Getting a full eight hours of sleep doesn’t mean you will wake up and lose the weight you need to, but sleeping can help your body from packing on extra pounds. Without sleep, your body produces something called ghrelin, a hormone that will boost your appetite, not great if you want to lose weight. Without sleep your body also will not produce leptin, a hormone that helps you realize that you are full, also not great for loosing weight. Not to mention, stress increases the likelihood that you will stress eat, and you might not have the energy to fight craving if you are stressed and under slept.
3. Sleep Can Strengthen Your Heart
Your heart loves sleep. Lack of sleep can cause your body to release something called cortisol which can lead to high blood pressure and heart attacks. Cortisol is a stress hormone that triggers your heart to work harder. Your heart also needs rest to function properly.
4. Better Sleep Means a Happier You
Good sleeping can lead to good moods. Simply waking up feeling rested helps your energy levels soar. This gives you energy to deal with whatever life throws at you, or it at least helps you deal with the obstacles and challenges in everyday life. Having the ability and energy to manage and deal with your emotions will help focus on the happier emotions.
5. Sleeping Can Increase Productivity
Getting enough sleep cultivates a healthy attention span and promotes concentration. Sleep also helps several other aspects of thinking including memory, problem-solving, creativity, emotional processing, and judgment, all of which promote success at work!
7. Sleep Can Increase Exercise Performance
Exercise is essential if you have COPD. Exercise promotes your lung and muscle capacity so you are able to do more everyday activities and tasks, and it also helps to slow down the progression of your COPD. Sleep is a form of exercise recovery, and recovery helps your hand-eye coordination, reaction time and muscle recovery. Plus, depriving yourself of sleep can have a negative impact on your energy level, and decrease your strength and power, both of which you will need to have a healthy COPD exercise regime.

When Should You Talk to Your Doctor About your Sleep
You should talk to your doctor about your sleep if you are not sleeping through the night on a consistent basis. If your lack of sleep is affecting your life while you are awake, you should contact your doctor to set up an evaluation. Your doctor will look at your signs, symptoms, and a sleep history. If you have a partner who shares a bed with you, their insight into your sleeping patterns could be helpful to know!

From there, you could be referred to a sleep disorder center. A sleep specialist can determine your need for further evaluation.
Diagnosing Sleep Apnea

To diagnose sleep apnea test will be conducted:
Nocturnal polysomnography is a test where you will be hooked up to equipment that monitors your heart, lung and brain activity, breathing patterns, arm and leg movements, and blood oxygen levels while you sleep.
Home sleep tests provide you with tools to diagnose sleep apnea at home. These tests usually measure your heart rate, blood oxygen level, airflow and breathing patterns.
Based on the results of these tests and how abnormal they are, your doctor might be able to prescribe a therapy without further testing. However, these tests do not always doesn't detect all cases of sleep apnea, and if your results are normal, your doctor might still recommend polysomnography to understand your sleeping condition further.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
If you have obstructive sleep apnea, you may have to go see an ear, nose and throat doctor to rule out blockage in your nose or throat.
However it is more likely that you have central sleep apnea because this is much more common, and if you have COPD it is likely that your sleep apnea can be tied to your respiratory condition.
Tips and Tricks for Sleeping Better if you have Central Sleep Apnea

People with chronic obstructive pulmonary disease (COPD) face distinct challenges getting enough sleep. COPD symptoms including coughing, pain and shortness of breath, all make it difficult to sleep. But as we mention in the section above, sleep is essential for COPD patients because sleep is important for resting your pulmonary muscles — and for simply functioning at a reasonable capacity.
COPD is not the only reason you are not sleeping well, there could be a number of reasons beyond these symptoms that induce sleeping problems. Understanding what these reasons are could help you find your way to a better night’s sleep.
Cut out mid day coffee or tea

Even though you may be tired from not resting enough the night before, that afternoon cup of coffee could be keeping you up. Having a cup of coffee or tea may help the afternoon crash problem you experience, but the extra caffeine late in the day could be impacting your ability to fall asleep that night, and that is a very counterproductive cycle.
Cultivate healthy sleeping habits
Make adjustments to your schedule and the ambiance of your bedroom to help improve your sleep. Start by limiting you napping because too much sleep during the day can disrupt regular sleeping patterns at night. Your naps should be no longer than20 minutes, this should help support your much needed night time rest.
![]()
Stick to a routine, this means going to bed and getting up at the same time every day. This will help reinforce natural sleep/wake cycles.
Elevating yourself by sleeping in a slightly upright position helps reduce stress on your lungs. It also can reduce acid reflux symptoms if you have trouble sleeping due to that.
Adjust your lifestyle
Adjusting your lifestyle means creating healthy habits.
First and foremost, if you smoke, get help to quit. Do not let anyone in your home smoke in order to keep your house free of secondhand smoke, dust, and pollutants. Your breathing is directly impacted by what you breathe in and when you inhale smoke, your air passages get smaller, which makes it harder to breathe.
Start an exercise program, you can join a pulmonary rehabilitation course to learn how to exercise effectively and safely. If you have COPD you can often experience drops in oxygen levels at night and in some cases you may need oxygen therapy while you sleep, but to avoid having to get on oxygen therapy, physical activity will help you build up your oxygen supply. Aim for 30 minutes of exercise a day, three times a week.
A sleep diary is very helpful for COPD patients who have trouble sleeping because it reminds you what works and what doesn’t. Write down what you ate that day, medicines you took, and activities for the day and then write down when you went to bed and woke up. Take a look at it after a few days and you will be able to see what helps you sleep better.
Getting ready for bed prepares you for sleep, even if you are not tired yet, start doing your bedtime routine at the same time every night, this will remind your body that it is time to start relaxing. Try these tips for relaxation:
- Take a warm bath to help your body reach a nice temperature for rest
- Journal or write a to-do list for the next day to clear your mind
- Relax your muscles with light stretching
- Listen to soothing music or a hypnosis recording
- Shut off your electronic devices an hour before bed
- Create a comfortable and cool space with a temperature between 60-71 F.
- Get rid of clutter as it can cause stress
- Aromatherapy with lavender can make it easier to fall asleep
Your sleep position is very important in terms of your lung capacity. Having a good sleeping posture helps open your airways making it easier to breathe. Sleep with your head slightly higher than the rest of your body rather than laying your head completely flat. If you sleep on your side, place a pillow between your knees and keep your back straight. When you sleep on your back, bend your knees slightly with a pillow placed under them.
Sleeping with an Oxygen Concentrator

Sleeping with a portable oxygen concentrator is something you will have to get used to doing. Your breathing pattern changes while you sleep, and you may breathe deeper when you sleep, or it is possible you have a shallower breathing pattern. That is why, if you use oxygen therapy while sleeping, your nighttime oxygen solution may differ from what you use for supplemental oxygen during the day.
Pulse dose portable concentrators can be an effective nighttime solution for some patients, and you can check with your doctor if your pulse flow device is sufficient in ensuring you have adequate blood oxygen levels while sleeping. But your doctor might determine your specific needs require a continuous flow portable oxygen concentrator. Your doctor will be able to perform a series of tests and studies in order to determine exactly what flow-setting you’ll need while you sleep, allowing you to choose your nighttime oxygen machine accordingly.

Once you know what nighttime oxygen machine you need, you can call 1(800)-946-1201 to speak with a respiratory specialist at LPT Medical. We will help you get the device that will cover your oxygen needs at the best possible price.

There are several portable oxygen options to choose from. If you have trouble sleeping, you can look into specific portable oxygen units that have certain features that make them better suited for overnight use. As long as they meet your prescribed oxygen needs, the concentrators discussed here are ideal for your nighttime oxygen solutions.
Best Pulse Flow and Continuous Flow Oxygen Concentrators for Sleeping in 2021

The Respironics SimplyGo is the most flexible option for you in order to satisfy both daytime and nighttime oxygen demands. This device was engineered with your travel needs in mind, so it comes equipped with three modes of oxygen delivery – Continuous Flow Mode, Pulse Mode, and Sleep Mode!
The SimplyGo can run off power from a wall outlet, a cigarette lighter or a charged battery, so you can transport your device with you anywhere. This is the most popular oxygen solution for those that who use sleep therapy equipment, such as a CPAP machine, in conjunction with oxygen.
The SimplyGo is ideal for your 24/7 usage and with its advanced ‘Sleep Mode’ technology you will be delivered a pulse dose of oxygen for a longer duration for a comfortable sleep. If you begin to breathe shallowly or through your mouth, the SimplyGo will automatically switch to the continuous flow mode, and deliver oxygen at 2 LPM to ensure you are adequately oxygenated.
This is something oxygen tanks and canisters will never have the capacity to do. This feature gives you peace of mind that you are being oxygenated throughout the night and getting better sleep for an overall better life.
Here are the SimplyGo specs:
- Pulse Settings: 1 to 6
- Continuous Liter Flow: 0.5 to 2 LPM
- Battery life: Up to 3 hours (on the setting of 2)
- Weight: 10 lbs (with battery included)
- Dimensions: 11.5 W x 10 H x 6 D (inches)
The Inogen One G5 may be a good option for your nighttime use if you are prescribed nighttime supplemental oxygen and approved pulse dose delivery. This is a smaller and lighter machine conducive to an active person’s lifestyle, or simply designed with ease and comfort in mind. The Inogen One G5 weighs 4.8 lbs and will give you 13 hours of pulse dose oxygen when paired with a 16-cell One G5 battery.

Beyond the benefits of its small and compact design, long lasting battery life, and powerful pulse flow settings, is the benefit of owning an oxygen device that provides extremely quiet operation, rated at 38 decibels. That means it won’t disturb you or anyone around you, while you’re asleep.
Here are Inogen One G5 Specs:
- Pulse Settings: 1 to 6
- Battery life: Up to 6 hr 30 min (with single battery)
- Weight: 4.8 lbs (with single battery)
- Dimensions: 3.26 x 8.15 x 7.19 (W x H x D in inches, with single battery)
Overview
The bottom line: you need to sleep well. Sleep is your beginning and the end of each day, so it is a massive part of your life and it should be treated as such, and pay mind to it. If you have trouble sleeping, speak to your doctor about steps you should take to sleep better. People who get less sleep tend to be heavier and are more likely to be diabetic. On top of that they are less energetic, experience bad moods, and lower productivity.
There are so many ways that you can get into a healthier rhythm of sleep, but if you have central sleep apnea, you will need to take added measures to start sleeping again beyond changing your daily habits and creating a sleep routine.
It may be necessary for you to go on oxygen at night. If so, you can get set up with a portable oxygen concentrator that is approved for nighttime use by calling 1(800)-946-1201.
Summer is the season that most people associate with sunny days, bathing suits, and a plethora of outdoor sports and activities. But if you have COPD, summer can also be a difficult time marked by struggles with respiratory irritants and difficulty breathing.
Part of living with COPD is having to be extra careful about protecting your body, and especially your lungs, from harm. That means doing everything you can to avoid illnesses, exacerbations, and any environmental conditions that could weaken your lungs or make your symptoms worse.
Unfortunately, with every new season COPD patients have to adjust to new hazards and challenges that come with the change in weather. And with the summer on its way, it's important to know what to expect and how you can prepare yourself for the shift.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The summer weather, in particular, is especially hard for many people with COPD, bringing with it a variety of atmospheric conditions that can be dangerous for your lungs. The extra humidity, smog, and the plethora of new allergens that come in the summer can worsen your symptoms and make it much more difficult to breathe.
The summer weather can also sap your energy and interfere with your ability to exercise and do other activities during the day. The poor air quality and high temperatures can wreak havoc on your lungs, forcing you to be extra cautious about spending time or exercising outdoors.
It's important to keep your lungs working as efficiently as possible when the air is hot and damp, which means protecting yourself from harsh temperatures and pollution in the air. You have to know when to stay indoors, how to keep your home comfortable, and how to keep your symptoms under control.
In this article, we're going to help you get ready for the summer by alerting you to all the unique summer hazards you should be prepared for. We'll show you how to reduce your risk of flare-ups, better manage your symptoms, and even prepare for summer storms.
With some knowledge and preparation, you can make it through the summer without exposing your lungs to toxic irritants or making your COPD worse. By taking some basic, practical precautions, you can keep your symptoms under control, rock the season, and enjoy this summer to the fullest.
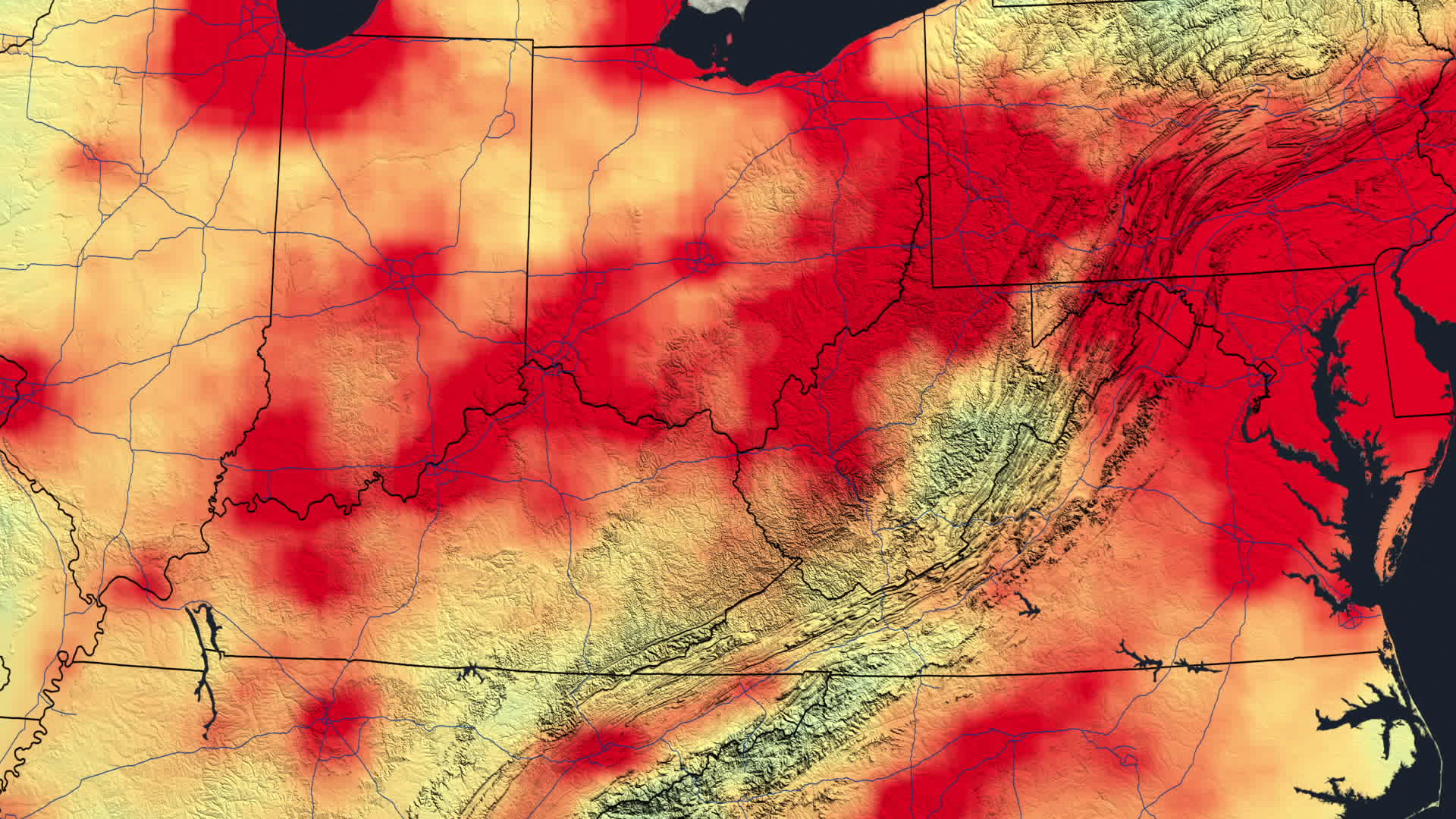
Prepare for Poor Air Quality
Heat, air pollution, and humidity all spike during the summer months, and all of these conditions can make it more difficult to breathe. For patients with lung diseases, these hazards can make respiratory symptoms significantly worse, and often make it both difficult and dangerous to spend time outdoors.
For example, according to the Environmental Protection Agency, high levels of particle pollution, which includes smoke and smog, increases the number of hospitalizations among people with heart and respiratory conditions. It also causes a variety of serious symptoms in people with COPD, including coughing, chest pain, and shortness of breath.
However, living with COPD doesn't mean you have to forego the outdoors and all the fun activities you can do in the summer. You can still enjoy swimming, hiking, and other outdoor activities as long as you know your limits and plan them right.
In this section, we're going to help you learn how to spend time outside while minimizing your symptoms when you're outdoors. We'll show you how to monitor your local weather and air quality so you can make safe and healthy decisions about when to go out and when it's best to stay indoors.
Enjoy the Outdoors During Cooler Times of Day

Spending too much time out under the hot, summer sun can worsen COPD symptoms like breathlessness, coughing, and fatigue. This happens because, as your body overheats, your lungs have to work extra hard to help your body cool down.
The warm environment alone can make breathing a challenge, especially when you suffer from a respiratory condition like COPD. Hot air can irritate your lungs and cause them to spasm, constricting your airways and blocking oxygen from flowing through. This can cause bouts of coughing and wheezing and make it much more difficult to breathe.
When you have COPD, it's important to avoid the heat so you can keep your body and your lungs running at maximum possible efficiency. Otherwise, symptoms like fatigue and shortness of breath may get the better of you and lead to flare-ups or even serious exacerbations.
In the summer, this means staying indoors and limiting your physical activity when the weather outside is too hot. However, that doesn't mean you have to trap yourself indoors all day during the summer.
The trick is to avoid going out during the hottest time of day and during especially bad heat spells. Instead, plan outdoor activities and exercise during the early mornings and early evenings, instead of in the middle of the day.
To plan ahead, you can check your local weather archives and find patterns in how the temperature changes throughout the day. Using records of past year's weather and paying attention to hourly temperature forecasts, you can pin-point the best and coolest times of day to go outside at different points during the season.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Find a Good Source for Weather and Air Quality Forecasts
Besides paying attention to the temperature, you should also watch out for days with high humidity or air pollution. Summer is usually the most humid time of the year, and it's also the prime season for pollen, mold, and smog.
Your local air quality can vary significantly from day to day, depending on the temperature, wind patterns, and other environmental factors. Even allergens vary in severity throughout the season and can spike unexpectedly depending on the weather.
Luckily, you can always monitor your local air quality conditions by watching your local weather channel or by checking the forecast daily online. There are a variety of websites that provide detailed reports, including levels of pollution, humidity, and allergens, to help people like you avoid hazardous conditions.
To prepare for this summer, you can even take a look at past weather and air quality archives to get a better idea of what the summer will be like where you live. You will likely notice patterns in how humidity, allergens, and pollution levels vary throughout the season that you can use to plan your summer activities.
Here are some online resources you can use to check the daily air quality and humidity in your area:
- Visit airnow.gov to check your local air quality index. This website is run by the EPA and uses an intuitive scale (from “good” to “hazardous”) to help you quickly understand the risk.
- Visit pollen.com for local allergy and pollen forecasts. There, you can get a general allergen rating (from low to high allergen risk) and even a list of the top allergens (e.g. oak, ragweed, etc.) in your area.
- You can check the weather and temperature history for your zip code by using this tool from Weather Underground. It can give you detailed information about temperatures and weather from past years, and even includes graphs showing you hour-by-hour temperatures from past dates. You can use this information to figure out the coolest times of day for different parts of the summer and get a better idea of what kind of weather to expect.
Set Up Weather and Air Quality Alerts
There are a variety of Android and iPhone apps you can use to track weather and air quality on your phone. These apps give you a convenient way to monitor outdoor conditions on the go or from your home.
Having the weather and air quality on a mobile app can help you remember to check and plan around poor conditions. Some apps will even push alarms to your phone to warn you of air and weather hazards in real time.
There are dozens of apps on both the Google and iTunes app store dedicated to weather, pollen, and air quality forecasts. Here are a few examples of apps that can be particularly useful for people with COPD.
Plume Air Report
Plume Air Report is an app available for both Android and iPhone mobile devices that gives you real-time data on air pollution for any city in the world. It also tells gives you basic information on the local temperature, wind, and humidity levels.
Plume is simple, straightforward, and easy to use and navigate. It's a great all-in-one app for weather and air quality to help you determine whether it's safe to spend time or exercise outdoors.
WebMD Allergy App
The WebMD Allergy App tells you everything you need to know about pollen and other allergens in your area. It is available for both iPhone and Android and provides up-to-date data on weather and allergen levels.
This app is great for people with seasonal allergies and even people with allergies to dust and mold. It even separates allergens by category, showing you the concentrations of different types, including allergens associated with grass, trees, weeds, dust, dander, and mold.
The WebMD Allergy App also lets you record your allergy symptoms every day to help you monitor your health. This is a great way to track the severity of your symptoms, learn what you're most sensitive to, and get a better idea of how your allergies affect your COPD.
BreezoMeter Air Quality Index
The BreezoMeter app gives you detailed air quality reports you can use to plan outdoor activities and minimize your exposure to airborne pollutants. It includes current air quality data, future air quality forecasts, and detailed air quality maps that can show you the air conditions down to the street level.
The BreezoMeter map even provides personalized, practical health tips based on your local air quality to help you avoid hazards and plan your day. It can also send you alerts when the air quality changes and allows you to monitor the air in multiple locations at once.
Avoid Hazardous Temperatures, Weather, and Pollution

Depending on where you live, the temperature and air quality might vary vastly from day to day or even between morning and evening. But once you've found some good sources for air quality, allergens, and weather alerts, you can begin to work your days and summer plans around the hazards.
Air pollution and extreme heat or humidity can have a significant effect on your COPD, worsening your symptoms and even leading to serious exacerbations. In fact, even if you don't notice its effects in the short term, polluted air alone can make you more prone to getting respiratory infections, raise your risk of heart attack, and increase your chances of needing to be hospitalized.
The dangers of heat, humidity, and poor air quality go up depending on three main factors: the severity of the weather or pollution, the length of time you spend outside, and how much physical exertion you do. For example, taking a short walk or sitting outside on a hot or humid day isn't nearly as dangerous as doing vigorous exercise or spending an extended amount of time in the heat.
Use local forecasts to help you plan outdoor exercise, sports, and activities for times when the temperatures are expected to be mild, humidity is low, and the air quality is good. That might mean limiting outdoor activities in the afternoons and going out during cooler times of the day.
You can use the trends from past years to help you plan things further out, such as sporting leagues, exercise schedules, and vacations. For shorter-term plans, you can use week-long weather and air quality forecasts to figure out what days and times you should avoid spending time outdoors.
Here are some tips for planning your activities around hazardous weather and air conditions:
- Check your air quality forecast every week and note any days that are supposed to be particularly bad. As you plan activities and outings, avoid planning anything on hazardous days that involves physical activity outdoors or requires you to spend too much time outside.
- Protect yourself from the heat by figuring out what parts of the day are the coolest and planning any outdoor exercise, work, or other activities during these times.
- Take care when doing lengthy outdoor activities or heavy exercise, in particular. Make an effort to plan them on days with the most favorable conditions.
- Save lengthy walks, gardening, lawn work, outdoor sporting events, and other activities that keep you outdoors for extended periods of time for cooler days. They are too risky to do in hot, humid, or polluted air.
- Always check the allergen and pollution levels in your area before opening up windows and doors in your house. Airing out your home is a great way to let in cool, fresh air, but if the air quality is poor, you'll just end up filling your home with pollen and airborne irritants.
- During heat spells or very hot days, make sure you have an air-conditioned, indoor place to spend time in. If you don't have air conditioning or it stops working during the heat, leave the house and go somewhere public that has A/C (such as the library, mall, movie theater, a restaurant, or a coffee shop).
- If you like to exercise outdoors, shorten the length of time you spend outside in the heat and take more frequent breaks. You may need to break up your exercise into smaller chunks and spread them out during different times of the day.
- On days with high pollution or allergens, exercise indoors instead. For example, you could go the gym, do aerobics in your living room, or find a large, indoor place to take a walk.
Talk to Your Doctor About Preparing for Summer Hazards

As you prepare for the summer weather and the various respiratory hazards it brings, you should talk to your doctor about any concerns you have. For instance, if you are worried about allergies, flare-ups, or how much exercise you should do in the heat, your doctor is the best source of advice.
To help you get physical activity, your doctor can help you work out a feasible exercise schedule for the summer that takes the weather and heat into account. Your doctor can also help you find activities that are safe and healthy for you to do based on your personal medical history and physical condition.
You can also ask your doctor to help you prepare for allergies and flare-ups so you can minimize your symptoms when the summer respiratory irritants come. He may also be able to give you a prescription allergy medication or an emergency inhaler if you are prone to serious flare-ups.
By working with your doctor, you can make sure you have everything you need to keep your symptoms under control when it gets hot, humid, or the smog rolls in. If your doctor prescribes you s rescue inhaler, keep it and any other quick-relief medications with you at all times in case you encounter poor air conditions or experience a surprise flare-up.
Prepare for High Temperatures and Humidity

Exposure to extreme temperatures can be hard on your body, especially when you suffer from a chronic disease. That's why people with COPD should avoid going outside when the weather is especially hot and humid.
Regulating your body temperature is taxing on your body and puts extra strain on your respiratory system in particular. To keep your lungs working as efficiently as possible, you have to be extra careful to protect yourself out in the heat.
There are many ways to do this while still enjoying the warm summer sun and and your favorite outdoor activities. The following tips will help you keep breathlessness and fatigue at bay without having to shutter yourself in the whole summer.
Know the Signs of Heat Stroke
The symptoms of heat exhaustion and heat stroke can be subtle and easy to miss, especially if you have COPD. Symptoms like fatigue and shortness of breath can be mistaken for normal COPD symptoms instead of a dangerous sign of heat exhaustion.
Heat stroke can strike suddenly, which is why it's so important to know the signs and symptoms and pay close attention to your body whenever you're out in the heat. Be on the look out for symptoms in yourself and others and take care not to exert yourself too much.
Heat exhaustion is not as severe as heat stroke, and the symptoms can be mild or severe. However, experiencing heat exhaustion when you have COPD puts you at a higher risk for serious complications.
Luckily, avoiding heat exhaustion is a simple matter of monitoring your body and taking care of yourself in the heat. Drinking plenty of water, replenishing your electrolytes regularly (with salty food or sports drinks), and taking frequent breaks in the shade can all significantly reduce your chances of heat stroke.
Here are some of the most common symptoms of heat exhaustion and heat stroke:
- Dizziness or feeling faint
- Nausea or vomiting
- Headache
- Fatigue
- Fainting
- Pale or flushed face
- Weak, rapid pulse
- Muscle cramps or weakness
- Heavy sweating with cold, clammy skin
Wear Appropriate Clothing

How you dress can significantly affect your temperature and how you feel outside in the heat. Clothes that are tight or heavy will make you overheat more quickly, while light, loose clothes will help you stay cool.
When you go outside on hot days, make sure to wear light-colored, loose-fitting clothes that give you space to move and room to breathe. Clothes that cinch or are too tight will be very hot under the sun and make it more difficult for you to move freely and breathe comfortably.
To prepare for the summer, fill your wardrobe with light, airy fabrics and pale colors that reflect light rather than absorb it. It may also be a good time to go through your old clothes and get rid of items that don't fit or restrict your breathing.
A hat is another great clothing accessory to have when you're out in the summer heat. A wide-brimmed hat gives you the most protection from the sun, but a visor or baseball cap can help you stay cool as well.
Stay Hydrated
When you're outside in the heat, it's easy to get dehydrated without even realizing it. If you don't make a special effort to drink plenty of water, you could end up with worsened shortness of breath, coughing, and fatigue.
Dehydration strains both your body and your lungs, and also dries out the mucus in your airways. This worsens airway obstruction and makes it even more difficult to breathe, which makes physical exertion dangerous in the heat.
It's important to take dehydration seriously when you suffer from COPD, because it can severely exacerbate existing breathing troubles. Make it a goal to drink extra water during the summer and bring a water bottle with you anytime you leave the house.
Take Breaks
When you're outside in not-ideal weather, such as excessive humidity or heat, it pays to be extra cautious. You may need to limit your physical exertion or take more frequent breaks to keep your COPD symptoms under control.
As soon as you feel too fatigued or feel like you are having trouble catching your breath, stop whatever activity you are doing and retreat to a sheltered place where you can rest. Use any rescue medication you have if needed and don't exert yourself again until your respiratory ailments have passed.
If you feel overheated, find a shaded or air conditioned spot immediately, and drink some cold water to cool down. Don't go outside again until you are well-hydrated, rested, and your body temperature feels normal again.
It's important to stay in tune with your body and be able to recognize the signs of a flare-up. If you catch your symptoms worsening early and take appropriate action, you are much less likely to experience serious symptoms or have to be hospitalized for an exacerbation.
Keep Your House Cooled
Depending on where you live and how your house is designed, it can be a challenge to cool your house during the worst of the summer heat. Sometimes, the A/C just can't keep up with the sweltering heat and the hot sun beating down on your house.
If you have COPD, it's very important for your lungs to keep your house at a cool, comfortable temperature when you're at home. Fortunately, there are a variety of simple techniques you can use to keep the heat out and take give your A/C unit a break.
Short-Term Strategies
First of all, when the sun is beating down, make sure you keep your window blinds and shutters closed. This will prevent the sunlight from shining through and warming up the air inside your home.
You can also cool down and air out your house at night by opening up the windows after the sun goes down. However, you have to be strategic about which windows you open and close to make this method effective.
Since hot a
If you have COPD, then you know that clean air is a necessity for both comfort and health. It follows, then, that the quality of the air you breathe in your home on a daily basis can have a large impact on how you feel.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Part of having COPD is being extra cautious about the air your breathe and the environments you choose to spend your time in. However, many COPD patients don't realize that they could be breathing heavily polluted air inside their own home.
Since most people spend most of their time indoors, poor indoor air quality can cause even more problems than outdoor pollution. Particulates, pollutants, and biological contaminates—including mold, allergens, toxic gases, dust, and a variety of other irritating particles—can all be found indoors.
If you suffer from COPD, these contaminants can cause serious irritation and inflammation in your lungs. Exposure to poor air quality for even short periods of time can make your COPD symptoms worse and even lead to exacerbations.
That's why it's important to take charge of your indoor environment and keep the air in your house as clean and healthy as possible. You'll likely find that you feel better, breathe better, and can be more active at home as a result.
In this article, we'll help you improve your indoor air by explaining what causes poor indoor air quality, why it matters, and what you can do to prevent it. We'll explain how airborne particulates affect your COPD and how to hunt down and eliminate potential sources of respiratory irritants in your home.
There are lots of different ways to reduce indoor pollution, and it's not difficult to do once you identify the main sources of airborne irritants in your home. So if you want to breathe the freshest, cleanest air possible, this article is for you.
How Indoor Pollution Affects COPD

When you talk about air pollution, many people only think about outdoor pollution caused by industry, cars, and weather. But, in reality, smog, pollen, mold spores, and other airborne particles can pollute indoor air as well.
Contaminates in the air, whether indoor or outdoor, can worsen COPD symptoms like breathlessness and fatigue and even cause the disease to progress more quickly. Studies show that prolonged exposure to poor air quality can even increase your risk of being hospitalized or experiencing a COPD exacerbation.
That's why it's so important to pay attention to the quality of the air you breathe both indoors and outdoors. If you don't make an effort to keep particulates and other airborne contaminates out of your home, you could be doing even more permanent damage to your lungs.
Common Symptoms of Exposure to Airborne Particulates:
- Shortness of breath
- Chest tightness and discomfort
- Coughing or wheezing
- Dry, irritated throat
- Excess mucus in lungs and airways
- Dry, itchy nose
- Itchy, dry, or watery eyes
Pollution in Your Home

As important as it is to avoid air pollution outdoors, it can be even more important to avoid poor indoor air. That's because houses tend to be well-sealed and circulate the same air over and over.
New contaminants can easily come in through your windows and doors, but they won't make it back of your home unless you make a deliberate effort to get rid of them.
Because of this, everything from dust, pollen, bacteria, and mold tend to build up in the air and inside the ventilation system over time. Since most people spend the majority of their time indoors, most people are consistently exposed to all of the irritating airborne contaminants that manage to get trapped inside their homes.
Indoor pollution comes in a variety of forms, including toxic gases, airborne particles, and biological contaminants like mold. Some of these airborne particles and pollutants originate from sources indoors, while others are brought in from outside.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Here is a list of common respiratory irritants and pollutants you might find in your home:
- Smog
- Smoke (from tobacco, fireplaces, barbecues, incense, etc.)
- Toxic gases (e.g. radon and carbon monoxide)
- Household Chemicals
- Pollen
- Mold
- Dust Mites
- Pet Dander

For most healthy people, poor quality indoor air only causes minor respiratory irritation or no symptoms at all. However, prolonged exposure over time can lead to serious health complications, including lung diseases like COPD later in life.
For people who already have COPD, exposure to contaminated indoor air for even a short period of time can cause serious respiratory irritation. It can worsen COPD symptoms, cause a decrease lung function, and in general make daily activities more difficult.
How to Reduce Indoor Air Pollution

If you have COPD, you know that your lungs are particularly sensitive to contaminants in the air. That's why, in order to keep yourself healthy, you should take special care to keep all forms of dust, smoke, allergens, and other pollutants out of the air in your home.
The first step to cleaner indoor air is to develop new household habits and cleaning regimens that will prevent particles from building up in the nooks and crannies in your house. The next step is to invest in any of a variety of air filters, purifiers, and other appliances that can remove airborne particulates and moisture from the air.
Avoid Tracking Particulates into Your Home

Many people don't realize that humans and pets are the source of many of the airborne particulates and biological contaminants that make it into their homes. That's because open windows and foot traffic in and out of the house tends to bring in dust, pollen, mold, and other particles from outside.
Every time you go outdoors, particulates in the air have the opportunity to settle on your shoes, clothes and hair. Then, when you come back inside, those contaminants get shaken off as you go about your business at home.
The dust, pollen, and other particles float loose in the air and eventually settle into your carpet, furniture, drapes, and other surfaces. These pollutants stay in your house and get kicked back up into the air every day, triggering allergies and worsened COPD symptoms whenever you spend time indoors.
To prevent this, here are some tips for reducing the amount of harmful particles you and others track into your home:
-
Get a large mat to put outside every entrance to your house. Wipe your feet before you come indoors and ask guests to do the same.
-
Take off your shoes immediately after coming indoors. Never wear shoes while walking on carpet or rugs.
-
Shake off outerwear like coats, jackets, hats, and scarves before coming indoors. Launder these items often to remove any allergens or other irritating particles that they pick up outside.
-
Take a shower after doing yard work, gardening, or spending extended periods of time outdoors to get any pollen or other particles off of your skin and out of your hair. This will prevent contaminates from outdoors getting in your nose, in the air, and on your furniture and bedsheets.
- On days when the outdoor air quality is good, open all your windows and air out your house. This will allow built-up gases and particles in your home to escape and get replaced with fresher, cleaner air.
Protect Yourself on High-Pollution Days
Check Local Air Quality

If you aren't already in the habit, you should make it a point to check your local air quality every day. Most local weather programs offer daily reports and forecasts on the levels of smog and other airborne particulates in their region.
In order to make sense of your local air quality report, you'll need to be able to understand the Air Quality Index (AQI). The AQI scale goes from 0-500, with 500 being the most hazardous and zero being the least.
If you have COPD, an AQI above 100 can be dangerous and make your symptoms worse.
Here's a brief overview of the AQI scale and what it means:
- 1-50 AQI: good air quality
- 51-100 AQI: moderate air quality
- 101-150 AQI: unhealthy for people who are sensitive to air quality (e.g. people with COPD)
- 151-200 AQI: unhealthy for everyone
- 201-300 AQI: very unhealthy air quality
- 301-500 AQI: very hazardous air quality
Most cities have an average AQI below 100 on the scale most of the time, but that average can get higher in large cities and during certain times of the year. AQI values above 300, however, are very uncommon and only happen under extreme circumstances such as when there is a forest fire nearby.

To keep track of your local conditions, you can go to airnow.gov for detailed air quality reports and visit pollen.org for allergen forecasts. There are also a variety of Android and iPhone apps (e.g. Smog Report or AIRNow) that you can use to conveniently check the air quality where you live.
If you want to get really high-tech, you can even get a portable, personal pollution monitor. While it might be overkill, it can be useful to have a reliable way to quickly check the air quality wherever you go, especially if you have advanced COPD or you are particularly sensitive and susceptible to poor air.
Watch the Weather

It is useful to pay attention to certain weather conditions, like heat and humidity, when determining whether or not you should go outside. High temperatures and high humidity alone can make COPD symptoms worse, but they can impact allergies and air quality, too.
Here are the main weather factors that affect outdoor air quality:
-
Humidity: Air quality tends to be worse on high-humidity days because water droplets in the air trap airborne contaminants. Humidity also encourages the growth of dust mites, mold, and other fungi that can cause respiratory symptoms.
- Temperature: The warm summer months tend to be much worse than the cooler winter months in terms of air quality. This is partially because of increased humidity on warm days and the presence of allergens like pollen and mold. It's also the time of year that people are most likely to be outdoors and active.
Plan Accordingly

Pollution and pollen forecasts are useful for identifying days and times when you should be particularly careful to stay indoors. They can also help you plan outdoor activities and excursions for days that are less hazardous to your lungs.
Here are some tips for avoiding exposure on days with high pollution:
-
Make sure to check your local air quality report every day, especially during the summer.
-
When the air quality is considered “unhealthy,” stay inside as much as possible and keep all doors and windows closed.
-
Avoid spending time outdoors on high-humidity days and shut your doors and windows to keep the moisture out of your house.
-
Don't exercise or do any heavy physical activity outdoors on high-pollution days.
-
Avoid spending too much time on busy roads, in inner cities, and in parking lots where car and industry emissions are more dense.
-
If you have the option, set your car's ventilation system to recycle the air in your cabin instead of pulling in air from outdoors while you're on the road.
- Never smoke indoors! Also avoid other common sources of smoke in the home, including fireplaces, barbecues, wood burning stoves, candles, and incense.
Filter Your Air
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Cleaning regularly and airing out your house can only do so much to improve your indoor air quality. If you are extremely sensitive to airborne irritants, then you'll need some extra equipment to remove the finest particulates and biological contaminants from the air.
The first thing you should consider is a high-quality HVAC filter for your main ventilation system at home. There are dozens of options to choose from, but pay attention to the label since they can vary greatly in quality and effectiveness.
Avoid cheap HVAC filters that only catch the largest dust particles because they let all sorts of other respiratory irritants through. Instead, look for filters that can trap smaller particles like pollen, mold, and other microscopic particles.
While an HVAC filter will passively remove a certain amount of irritating particulates, they are not nearly as effective or thorough as a high-quality electronic air purifier. A multi-step HEPA purifier, for example, can filter out 99 percent of particles as tiny as .3 microns.
You can find small, portable air purifiers as well as more expensive whole-house air purification systems. Whole-house systems are expensive, but they can give you the most value of any air filtration product you can buy.
If you decide against a whole-house air purification system, you can also get portable air purifiers that work great for single rooms and small spaces. Portable purifiers are a perfect way to clean the air in your bedroom while you sleep, or you can place them in other rooms in your home that you spend a lot of your time in.
When looking for the right air filter or purifier, make sure to pay attention to what sizes of particles the product is rated for. Purifiers that filter large particles generally remove dust, pollen, and mold spores, while ones that filter smaller particles can remove smoke, soot, and bacteria from the air.
Watch Out for Pets

Unfortunately, furry pets that spend time outdoors track in even more pollutant particles than humans do. Dogs and cats both have thick fur that is capable of collecting a great deal more pollen, dust, and grime than human clothes do.
If you have a cat, the best solution is to keep it indoors. If you have a dog or outdoor cat, you should enforce a “no pets on the furniture” rule to keep your upholstery as clean and pollutant-free as possible.
Here are some other tips to keep your pets from making your indoor air quality worse:
-
Brush your pets often to remove excess hair, dust, pollen, and other particles. Just make sure you brush them outdoors so contaminants don't get loose in the air in your home.
-
Give dogs regular baths to wash allergens and pollutants out of their fur.
-
Consider getting hardwood floors instead of carpet and limiting the number of rugs and other fabric surfaces in your home.
-
Clean your pet beds and blankets often. Most dog and cat beds have removable covers that you can conveniently throw in the wash.
- Always keep your pets off of your bed, couches, and other upholstered furniture. Consider getting your pet their own designated chair, pet bed, or other comfortable spot to lounge on instead.
Prevent Mold Growth

Mold is another contributor to poor indoor air quality that can make your COPD symptoms worse. Every indoor space is bound to have at least some mold, but it can spread and get out of hand in moist, humid conditions.
To prevent excess mold from contaminating your home, make sure to clean up water from leaks and spills as quickly as possible. If anything—including carpets, walls, ceilings, and furniture—stays damp for more than 24 hours, you're guaranteed to get mold.
Sometimes mold grows stealthily in out-of-sight places, especially in bathrooms and basements. It's a good idea to have your house inspected every so often for hidden mold growth, especially if you notice you have allergies or worsened COPD symptoms at home.
When hunting for mold, look out for the sure-fire signs of mold growth: visible moisture, water stains, and a musty stench. If you locate any mold spots, clean them up immediately with soap and warm water and check the area thoroughly for any mold you might have missed.

If you have mold that covers more than ten square feet or is in a hard-to-reach area (e.g. in your walls or ceiling) you should call in a professional to help.
Besides promptly drying up leaks and spills, controlling the humidity and airflow in your house is the best way to prevent mold from contaminating your home. Even in the absence of mold, humidity on its own can make it difficult to breathe if you have COPD and encourage the growth of other respiratory irritants like dust mites and bacteria.
That's why you should ensure that there is adequate ventilation all throughout your house, especially in your kitchen and bathrooms. Running the shower, for instance, generates a great deal of humidity that has nowhere to go unless you turn on a vent fan or open a window. Other appliances, like your dishwasher or clothes dryer can contribute to excess humidity, too.
You can also get a dehumidifier to pull excess moisture out of the air if you struggle with high indoor humidity or live in an area with a very humid climate. For optimal results, most doctors recommend keeping indoor humidity below fifty percent.
Clean Surfaces Often

Dust and allergens can collect on any surface: tables, counters, curtains, carpet, shelving, and just about everything else. Carpets and fabric, in particular, tend to trap and hold particles and let them build up.
All it takes is a little activity or airflow to kick these allergens and pollutants back up into the air where they can make it into your lungs. But if you make it a habit of cleaning your house and furniture carefully, you can prevent irritating particulates from accumulating and contaminating the air in your house.
The most important areas to clean are your floors and upholstered furniture. Start by dusting any counters, shelves and other horizontal surfaces and then vacuum your couches, carpets, and rugs.
Hardwood floors are much easier to clean and don't hold on to tiny particles like fabrics do. If you have the choice, avoid carpeting your floors and decorating with fabrics like curtains and rugs. If you do, make sure to wash all your fabrics regularly and steam clean your carpets at least once or twice a year.
Get Your Home Inspected

Asbestos, mold, and radon gas are common household pollutants that are difficult to find and address without professional help. But, if left un-managed, they can cause serious symptoms and health problems.
Despite having been banned because of its dangerous respiratory effects, many houses still have asbestos to this day. It was a common component in a variety of building materials that were still in use in the very recent past, including attic insulation, flooring, roof shingles, and certain types of paint.
Radon gas, on the other hand, is a colorless, odorless gas that comes from contaminated soil and is sometimes found around houses. It is one of the leading causes of lung cancer in the US, and hiring an inspector is the only way to find out if it's there.
Most home inspectors offer a variety of different services, including radon, asbestos, and mold testing. If you have COPD, you should definitely consider hiring a professional inspector to check your house for the presence of these and other harmful chemicals that could make your disease worse.
The EPA recommends that all households have their homes inspected for Radon gas, and recommends mold and asbestos inspections before doing any kind of home renovation. This is especially important to do if you live an older house, or if you notice worsened respiratory symptoms when you're at home.
Avoid Household Products and Chemicals That Contain Respiratory Irritants

Many cleaning products, paints, and varnishes contain chemicals that cause respiratory irritation. These products can be particularly irritating to people with COPD, which is why doctors recommend that patients enlist help rather than use these products themselves.
If possible, it's better to have friends, family, or hired help do any heavy cleaning that requires bleach, ammonia, or other noxious-smelling products. For everyday cleaning, avoid irritating your lungs by switching to milder, natural cleaning products that don't contain inflammatory chemicals.
Many people with COPD find that other scented products, like perfumes, hairsprays, antiperspirants, and other hair and skin-care products make their COPD symptoms worse. Luckily, if you find that fragrant products irritate your airways, you can almost always find unscented alternatives. If you are very sensitive, you might need to ask others who visit or live in your home to use unscented products as well.
Conclusion
Living with COPD requires taking on a lot of extra responsibility for your health and lifestyle. Part of that responsibility is creating a healthy living environment, which includes paying attention to the air quality in your home.
Proper HVAC filtration and ventilation are key, since closed indoor HVAC systems tend to circulate the same irritants and pollutants over and over. You should also pay attention to humidity, check for mold, and get your home inspected for toxic gases and asbestos.
But what takes the most work is regular, thorough cleaning and keeping outdoor contaminants out of your home. It takes time and effort to build the right habits, but it's an effort that truly pays off.
Chances are, you won't be able to do all of this on your own. You might need to ask for

Some would say it is as certain as death and taxes... allergies. They cannot be avoided, and it's something many people dread every year. If you suffer from any respiratory illness like COPD, asthma, or cystic fibrosis, allergy season is a bearer of bad news.
If you have respiratory issues, allergy season is not something you can take lightly. Breathing in allergens can influence COPD exacerbations or if you have another form of chronic pulmonary respiratory disease allergies cause increased discomfort and worse symptoms.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
COPD is one of the most common pulmonary diseases and it affects 16 million Americans. Allergies impact more than 50 million Americans every year, and many of those people also have COPD or other respiratory conditions that makes allergy season even more unbearable.
Allergy season starts in the spring and continues until the fall. Different allergens and the substances that trigger allergies, appear at different times of the year. Allergies also affect people differently, and in some cases one trigger, will not affect another.
During the spring months in March and April, tree pollen is the most common allergen, then by weeds and grasses.

From May-July all the trees, grass and weeds are creating allergens at the same time, making it a bad time for allergy sufferers. May is the beginning of peak allergy season which continues throughout July.
July to September is when ragweed starts to flower. This flowering plant is a lead cause of seasonal allergies, with 75% of all sufferers allergic to it.
October marks the end of allergy season, as the temperatures drop, and plants start to die, the air starts to rid itself of allergens, bringing an end to outdoor allergy season. While your normal respiratory symptoms will persist to some degree, at least they are not exaggerated by outdoor aliments.
![]()
Surviving allergy season
The best thing for respiratory patients to do is to minimize your exposure to allergens as best as possible. This means do not go outside when the pollen count is high or when the allergen you are allergic to is in bloom. You can utilize this Interactive Allergy Map to see what allergy conditions are in your area and get forecasts for tree, grass and ragweed pollen.
You can also try:
- To keep your pets in the house on high-pollen days so they do not drag pollen into your house.
- If you have an air filter already, be sure the screen is clean and change it often
- When you have allergy symptoms, such as itchy eyes or a runny nose, talk to your doctor about allergy medication. Taking an over-the-counter antihistamine may work for you.
- Medications such as diphenhydramine (Benadryl) and cetirizine (Zyrtec) can stop your immune response to allergy triggers and potentially lessening breathing difficulties
- You may need nasal steroids, decongestants, and inhalers to decrease your inflamed airway
- Buy a cabin air filter for your car that’s specifically designed to keep allergens out

Keep you home free of allergens by
- Install a good filtration system in your air conditioner
- Keeping your windows closed during allergy season or when the allergen forecast suggest the air is saturated with allergens
- Vacuum and dust regularly to get rid of any pollen or mold spores that may have gotten in from outside
- Get an air filter for inside your home
Talk to your doctor about your allergy symptoms and how seasonal allergies affect your COPD They may suggest a variety of options, which could include:
- trying a prescription allergy medication
- using your inhaler more often during peak allergy season
- getting an allergy test to see which allergens are causing your reactions
- trying allergy shots (immunotherapy) to reduce allergy symptoms
- Change your clothes when you go inside on high pollen days
- Keep windows and doors closed to reduce pollen entering the house
Continuing to Treat your Respiratory Illness

The most important thing you can do during allergy season is to continue to treat your condition to the best of your ability.
Treating your condition starts with you and ends with you, it is your responsibility to go to the doctors and get tested should your condition change. You should have the best oxygen equipment available to treat your condition in order to reap the many benefits of oxygen therapy. You can buy a portable oxygen concentrator with a built in filtration system that will help you breathe pure medical grade oxygen for the duration of allergy season.

You can purchase a new or used portable oxygen concentrators at LPT Medical, an oxygen equipment company based in Denver, Colorado.
Treating your COPD means continuing to exercise. You can find manageable home workouts that you are able to do indoors when high allergen counts are high.
Tacking your symptoms throughout allergy season is also important, so keep a detailed diary that explains when you took your COPD medications and your allergy medication, and note how it affects you. This will also help you keep track of whether or not your medication is giving you side effects.
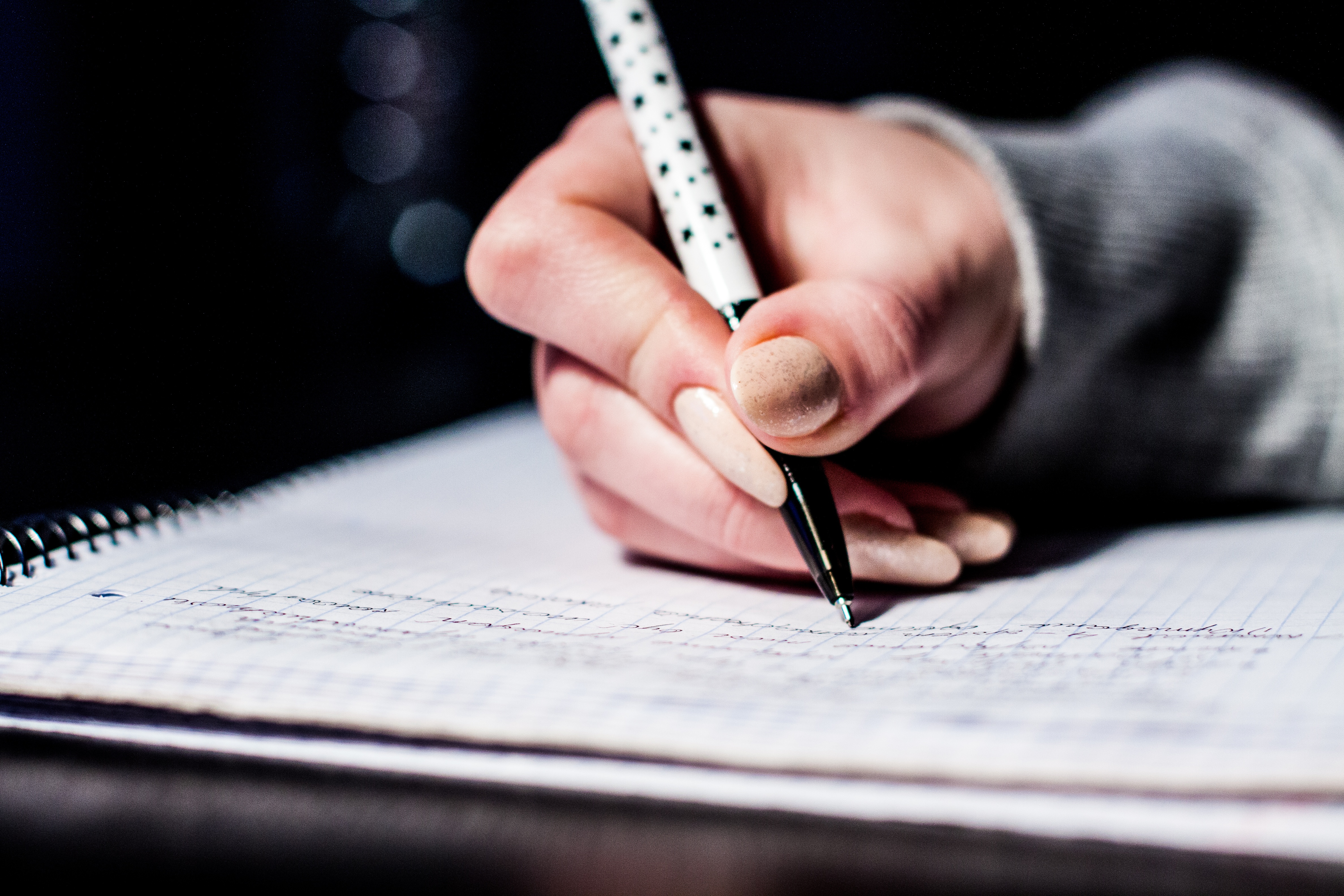
Talking to your doctor is always a great place to start when it comes to your health, they will likely understand your condition the best, and be able to prescribe you allergy medication if you need it or recommend over the counter drugs that will help you manage allergies in conjunction with your disease.
Start by explaining your allergy symptoms and how seasonal allergies affect your COPD symptoms. They may suggest a variety of options, which could include:
- trying a prescription allergy medication
- using your inhaler more often during peak allergy season
- getting an allergy test to see which allergens are causing your reactions
- trying allergy shots (immunotherapy) to reduce allergy symptoms
Allergy Medication: Functions, Side Effects, and COPD
There are a lot of allergy medications, and it is important you discuss with your doctor before taking any medications because there could be side effects that negatively impact your COPD or other respiratory issues you may have.
Allergy medications can be taken as pills, liquids, inhalers, nasal sprays, eyedrops, skin creams and shots. There are over-the-counter medications and others that are prescription only, be sure you discuss with your doctor before using over-the-counter medications as well.

Here an overview of the types of allergy medications and why they're used and how they will affect you if you have COPD or another chronic respiratory illness.
Antihistamines
The purpose of antihistamines is to block histamine. Histamine is a symptom-causing chemical released by your immune system during an allergic reaction, and the goal of medication would be to suppress this reaction and make you more comfortable around allergens.
Antihistamines come in pill and liquid form and in over-the-counter and by prescription.
The function of antihistamine medications is to ease your runny nose, itchy or watery eyes, hives, swelling, and other signs or symptoms of allergies.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The side effects can make you feel drowsy and tired, and it should be taken with caution when you need to drive or do other activities that require alertness.
Antihistamines that tend to cause drowsiness include:
- Diphenhydramine
- Chlorpheniramine
These antihistamines are much less likely to cause drowsiness:
- Cetirizine (Zyrtec, Zyrtec Allergy)
- Desloratadine (Clarinex)
- Fexofenadine (Allegra, Allegra Allergy)
- Levocetirizine (Xyzal, Xyzal Allergy)
- Loratadine (Alavert, Claritin)
Antihistamine also comes in nasal spray forms to help relieve sneezing, itchy or runny nose, sinus congestion, and postnasal drip and does not normally cause drowsiness.

Side effects of antihistamine nasal sprays might include:
- a bitter taste
- In some cases drowsiness
Prescription antihistamine nasal sprays include:
- Azelastine (Astelin, Astepro)
- Olopatadine (Patanase)
- Eyedrops
Antihistamine eye drops are available over-the-counter or by prescription, and are used to treat itchy, red, swollen eyes. The drops can be made of antihistamines and other medicines.
Side effects of eye drops might include:
- headache and dry eyes.
If your antihistamine drops cause stinging or burning, you can put them in the refrigerator before you use them. The types of eye drops include:
- Ketotifen (Alaway, Zaditor)
- Olopatadine (Pataday, Patanol, Pazeo)
- Pheniramine and naphazoline (Visine, Opcon-A, others)
Antihistamines and COPD

Pretty much all nonprescription products have drawbacks, especially for those with respiratory problems such as COPD, asthma, wheezing, emphysema, or chronic bronchitis. It is prudent of the pharmacist to be aware that as a patient you have been diagnosed with a respiratory problem, and they can advise against the use of products including antihistamines, unless your physician has suggested that you do use them.
If you have COPD pharmacists can recognize your COPD through your profiles, and past prescriptions which may include inhaled bronchodilators, inhaled steroids, or other medications to treat your COPD.
All first-generation antihistamines are labeled asking patients to seek the advice their doctors before using this medication if they have COPD.
Antihistamines are not considered a treatment option for COPD but they are often used for seasonal allergies.
The benefits of taking on antihistamine could be outweighed by the negative impacts it has for patients with COPD, because drying effects of first-generation antihistamines, could dry out your mucus and inhibit the your ability to remove it.
Click here to read about coughing and clearing techniques for COPD patients
Decongestants

Decongestants are used for immediate yet temporary relief of nasal and sinus congestion that could be caused by allergies. There are side effects that can cause trouble sleeping, headache, increased blood pressure and irritability.
Decongestants come in pills and liquid form.Many decongestants, such as Sudafed, are available over-the-counter but should still be taken with caution.
Several oral allergy medications have both a decongestant and an antihistamine. Examples include:
- Cetirizine and pseudoephedrine (Zyrtec-D 12 Hour)
- Desloratadine and pseudoephedrine (Clarinex-D)
- Fexofenadine and pseudoephedrine (Allegra-D)
- Loratadine and pseudoephedrine (Claritin-D)
- Nasal sprays and drops
Nasal decongestant sprays and drops relieve nasal and sinus congestion but you can only use these for a short period of time. If you use these drugs for more than three consecutive days it could result in a cycle where your congestion gets worse. Examples of nasal decongestants include:
- Oxymetazoline (Afrin)
- Tetrahydrozoline (Tyzine)
Respiratory Disease and Decongestants
Decongestants are not recommended for people with high blood pressure, cardiovascular disease, glaucoma or hyperthyroidism. Experts will also advise against COPD patients taking antihistamines and decongestants because these medications can thicken your mucus, making it even more difficult to cough up.
Decongestants also can raise blood pressure, and some of the drugs that you may use to treat your COPD also raise your heart rate and the combination of this can be harmful.
Bottomline is these allergy medications should be used with caution. And it is a good idea to talk with your doctor about the best treatments for your allergies.
Overview
It stands to reason that if you’re experiencing a lot of coughing and sneezing due to seasonal allergies, it could be more difficult to cope with your day-to-day symptoms attributed to your COPD.
That being said, it is crucial you continue to treat your COPD, on top of taking care of seasonal allergies.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
If you suffer from seasonal allergies and have COPD, it’s important to follow your doctor’s orders regarding how best handle your seasonal allergies.
There is no cure for seasonal allergies, they can be managed. Reducing your exposure to allergens is by far the healthiest and most effective way to deal with allergy symptoms.
Beyond that, you can keep your home dust and allergen free by using an air filtration system, keeping your doors and windows closed, and minimizing the time your pets stay outside.
Your doctor may also be able to recommend an allergy medication that would help you manage your seasonal allergies if it is safe for you.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!














