.png)
Chronic obstructive pulmonary disease (COPD) is a debilitating lung condition that affects around 16 million people in the United States. While there are many symptoms of COPD, shortness of breath, chest pain, and chronic fatigue are among the most crippling. In the early stages of COPD, these symptoms are mild and sometimes even go unnoticed by the patient. However, as time goes by, these symptoms become progressively worse and become even more of a burden for the victim.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Unfortunately, there is no magic wand that you can wave to reverse the effects of COPD. Treatment for this disease is aimed at slowing the rate that it progresses, reducing the risk of exacerbation, and managing chronic pain. And since every case of COPD is different, you’ll need to rely on information from your doctor and make lifestyle changes accordingly in order to achieve the best results.
But many COPD patients are left to wonder if there are other methods that can be used to ease the physical, emotional, and financial burdens of their disease. In our last post, for example, we took a look at some tips for living in the moment with COPD. Doing so will help you settle your regrets about the past and concerns about the future, instead, focusing them on things that you can change in the here and now.

Another thing you should be doing is applying for disability benefits which will help you out with some of the financial difficulties of managing a chronic disease. In this post, we’ll take a look at everything you need to know about Social Security Disability Insurance (SSDI) and how you can apply if you have COPD. If you have any questions, be sure to leave them in the comment section below so we can get back to you.
What is Social Security Disability Insurance (SSDI)?
SSDI is one service offered by the Social Security Administration (SSA). The SSA is a government-run agency that is responsible for assigning Social Security numbers and administering services related to their various insurance programs as well as the Supplemental Security Income (SSI) program for the aged, blind, and disabled. While most people in the country pay social security taxes, not everyone is eligible to receive benefits from it.

When you apply for social security disability, your condition will be compared to the disability “listing” found in the Social Security “Blue Book.” This book is accessible to anyone online and COPD is found under Section 3.02, under the title “Respiratory Disorders” and the subsection “Chronic Pulmonary Insufficiency.” However, when the claimant first requests disability benefits, it will be examined by local SSA field offices or state agencies who will verify non-medical requirements such as employment status, marital status, and age.
Unfortunately, there’s a lot of gray area when it comes to qualifying for SSDI. While the Blue Book clearly states what conditions you need to meet, there is some interpretation required, so it’s very important to fully understand how the process works before you file a claim. Another reason to be meticulous is that the turnaround time is generally quite long and might be even more backed up considering the COVID-19 pandemic. According to Nolo.com, 62% of people receive an answer within three months of filing an application.

What are the Requirements for COPD Patients to Qualify?
According to the SSA, a disability is defined as an inability to participate in something called “substantial gainful activity.” Essentially, what this means is that you are unable to work or make less money than the monthly income limits set by the SSA. This can either be due to a physical or mental disability that’s expected to last or has lasted 12 months or more.

The first thing you will need to gather to apply for benefits is a complete medical history of your COPD. In other words, you’ll need records of every medical event since you were diagnosed with COPD and even future medical procedures or tests if they apply. This should include things like the progression of your lung disease, symptoms, and any other physical examination that’s relevant. Below is a list of some of the test results you should include:
- Pulse oximetry
- Spirometry results
- Records of hospitalizations
- ABG tests
- Pulse Oximetry Levels
- Arterial Blood Gas
- Pulmonary (Lung) Function Tests
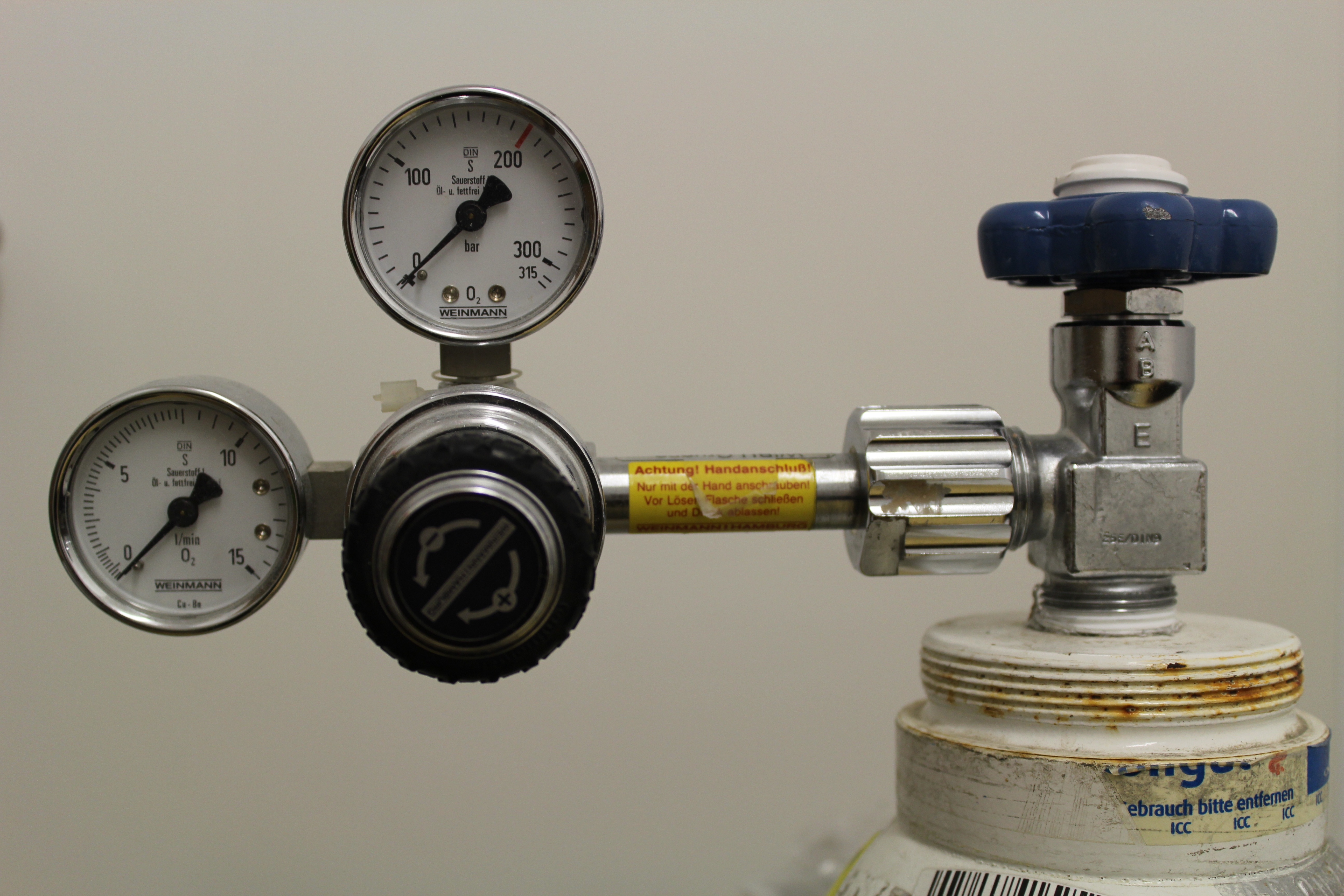
- Supplemental oxygen records (including your flow rate)
- CT scans or chest x-rays
Evidence of Comorbid Conditions
Like with many chronic conditions, COPD doesn’t just affect the lungs. The longer someone has COPD, the more likely they are to experience comorbid conditions such as sleep apnea, heart disease, high blood pressure, and even mental health conditions such as anxiety and depression. It’s important to include documented evidence of comorbid conditions because it will increase your chances of receiving benefits. The following are some examples of things you can include:
- Electrocardiogram (ECG) tests
- Heart stress test results
- Echocardiogram results
- History of heart attack, chest pain, or fainting
- Sleep tests
- Blood pressure tests
Evidence of COPD Treatment
Just like your medical history, it’s important to have full documentation of your COPD treatment history as well. Basically, this will show the SSA that you have been making every effort to improve the quality of your life despite the fact that COPD is an incurable disease. You will have the best chance of receiving disability benefits if you can prove that you still experience severe symptoms despite your treatment plan and you are unable to work as a result. Below are a few of the things you should include in this category:
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
- All medications that you are currently taking or have used in the past. Some common examples include inhaled steroids or bronchodilators, nebulizer treatments, antibiotics, or supplemental oxygen therapy. Be sure to include how your body reacted to these treatments.
- Pulmonary rehabilitation: including the duration and results
- Any medical procedures you’ve received such as endobronchial valve placement, lung volume reduction, or any other type of surgery.
- Include any complications related to these procedures
What Benefits Do COPD Patients Receive?
The amount of compensation that someone receives from SSDI will depend entirely on your lifetime earnings, so it’s very difficult to predict the exact amount that you will receive. According to DisabilitySecrets.com, most people receive between $800 and $1,800 each month with the 2021 average being $1,277. Another thing that will affect your earnings is whether or not you are receiving benefits from any other sources. The condition that you have and its severity will not affect how much compensation you receive.

The Social Security Administration uses a very complex formula to determine what your disability benefits will be, but it is possible to estimate your earnings by using an online social security disability payment calculator. In 2021, your disability benefits are based on the amount of income that you have paid Social Security taxes on. These are called “covered earnings.” Over the course of a year, the average covered earnings are called the average indexed monthly earnings (AIME).
.jpg)
The primary insurance amount (PIA) is calculated by applying a formula to your AIME which is the base figure that the SSA uses. If you want to learn more about how this is calculated, refer to this PDF document from the SSA. Alternatively, you can email or call your local SSA office where you will be connected with a representative who can help you predict the amount of your expected benefits.
Tips for Winning Your Disability Claim
Like we mentioned earlier, the amount that you will earn from Social Security benefits is pretty set in stone, so your focus should be on winning your case rather than earning as much as possible. Unfortunately, the burden of proving that your COPD is severe enough for benefits is largely in your hands. This is why you’ll need to be accurate and concise about the way you apply for benefits. The turnaround time for an SSDI application is several months at best, so you should be prepared to submit a thorough application the first time around rather than having to risk waiting for them to process your application a second time. Follow the tips below to get you started.
Speak With Your Pulmonologist
When it comes time to gather medical documents such as evidence of COPD treatment, procedures, or symptoms, it’s always best to get them from your pulmonologist rather than your primary care physician whenever possible. The reason for this is because the SSA may weigh this information more heavily since it’s coming from someone who specializes in COPD and other respiratory conditions.

Another reason to consult your pulmonologist ahead of time is that he/she may be able to provide you with more specific information about your disease including more thorough notes about the type of COPD you have and its expected prognosis. While pulmonologists are not specialists when it comes to disability benefits, they will help you to make the most convincing argument possible so that you can win your SSDI claim.
Hire an SSDI Attorney or Advocate
While your pulmonologist will provide you with information about your disease, SSDI attorneys and advocates are people who understand how the SSA works and how you can present the best case. While attorneys and advocates will provide you with mostly the same services, there are a number of differences between them that you should be aware of. First and foremost, an attorney is someone who is trained and has a degree in law whereas a non-attorney advocate does not have a law degree.
.jpg)
In order for someone to become an attorney, they need to have a bachelor’s degree, a Juris Doctorate (JD) degree and be admitted to a state bar. Attorneys are bound by professional conduct rules, they have many years of specialized training, and they have the ability to appeal your claim to the federal level if you want to dispute the SSA’s decision. If you decide to hire an attorney to help you with your SSDI claim, you should first ensure that they specialize in disability law.

A disability advocate (also called a legal representative, claimant representative, or disability representative) needs to pass an exam administered by the SSA, a background check, need professional liability insurance, and a bachelor’s degree. While disability advocates are highly educated on disability claims, they are not held to the same professional standards as attorneys are, and as a result, you will have less legal recourse if something doesn’t go as planned. In terms of payment, neither attorneys nor advocates are paid unless you win your case and they are entitled to the same fee which is paid directly by the SSA.
Take Your Time and be Thorough
Ultimately, the best way to win the SSDI benefits that you deserve is to be thorough with the application process. You want to provide an overview of your medical history and make it clear that you are taking the initiative to treat your COPD in the way that your pulmonologist advises. Before submitting your application, be sure to review it with a specialist who can point out any potential pitfalls. If your application is declined, the SSA will store your information in the event that you decide to dispute it.

Conclusion
Applying for benefits with COPD is not always an easy process. You need to be able to prove that your lung condition prevents you from participating in “substantial gainful activity” and you need to meet other requirements as well. Gathering the necessary medical information and knowing the right place to acquire it will give you the best chance of receiving benefits upon submitting your first application. You should also be consulting the Blue Book which outlines the exact requirements for qualifying for disability with COPD.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
COPD is one of the most common chronic conditions in the world and it represents a serious financial burden on individuals, especially in the latter stages of the disease. If you have any further questions about SSDI benefits, be sure to speak with your doctor or a disability attorney or advocate. Alternatively, you can leave your questions in the comment section below and we’ll get back to you as soon as possible.
.png)
Oxygen is one of the elements that’s essential for human life. Earth’s atmosphere is composed of about 20% oxygen which is the perfect amount for someone with healthy lungs to breathe easily. However, the farther you go up in altitude, the thinner the air becomes meaning you have to inhale more air to get the same amount of oxygen. This is why many mountain climbers use special devices that allow them to get the oxygen they need.
In much the same way, someone with chronic obstructive pulmonary disease (COPD) or other respiratory conditions may need to use oxygen at high altitudes. If you’re not yet prescribed oxygen, you may need to rent an oxygen device before traveling. And if you’re already on oxygen, you may need to increase the flow rate of your device in order to account for the change in altitude.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
No matter which camp you’re in, you’re going to need an oxygen device that can operate at high altitudes and enables you to get around easily without becoming breathless or fatigued. In this post, we’ll take a look at why it’s important to use oxygen at high altitudes and list some of the best portable oxygen concentrators for use at high altitudes.
The Importance of Having Access to Reliable Oxygen at High Altitudes
If you’re traveling to a higher altitude to visit a mountain town, or to do some skiing or hiking, you need to first consider how the altitude will affect you. Altitude sickness is a condition that can affect anyone, regardless of their age or health. But it’s more likely to occur in people who have either lived close to sea level or they have a lung condition such as COPD, asthma, or pulmonary fibrosis (PF).

Essentially, altitude sickness is what happens when you quickly go from low altitude to high altitude. It occurs when your body has a difficult time adjusting to the lack of oxygen and it can result in symptoms such as breathlessness, nausea, confusion, and fatigue. There are three different types of altitude sickness: acute mountain sickness (AMS), high-altitude pulmonary edema (HAPE), and high-altitude cerebral edema (HACE).
Acute mountain sickness is the most common and mildest form of altitude sickness. HAPE often comes on more quickly and severely than AMS and it’s the number one cause of death due to altitude sickness. Lastly, HACE is a type of altitude sickness that results in cerebral edema. This is when fluid builds up in the brain causing confusion, nausea, and can even cause a coma.

Having a reliable source of oxygen is very important if you’re a COPD patient. Even the mildest form of altitude sickness, AMS, can be serious for COPD patients because it can result in exacerbations and low blood oxygen levels. In addition to a reliable portable oxygen concentrator, you should plan your trip in a way that gives you time to acclimate to the change of altitude. Another thing to note is that any exercise you do, such as hiking or skiing will further increase your breathlessness.
Without further ado, let's take a look at the top 5 portable oxygen concentrators for high altitude...
5.) Caire FreeStyle Comfort (10,000 feet)
The Caire FreeStyle Comfort is one of only a few portable oxygen concentrators to be released in the past couple of years. And, unsurprisingly, it’s also one of the best. While Caire Inc. is a brand you might not recognize, they’re actually one of the top oxygen manufacturers in the world, selling products under the name “SeQual” and “AirSep.”

The Caire FreeStyle Comfort is a pulse dose portable oxygen concentrator meaning it only puts out oxygen when the user inhales. What this means is that this device is very efficient with long battery life and a lightweight design that won’t cause you any unneeded strain as you go about your day. It’s one of only a handful of concentrators that weighs under 5 pounds and it’s currently the most reliable portable oxygen concentrator on the market.

The FreeStyle Comfort has a maximum oxygen output of 1,050 ml/min and it has a maximum pulse flow setting of 5. This offers you plenty of room to adjust your oxygen flow as you move up and down in altitude. You’ll never have to stress about running out of oxygen either since this device offers up to 16 hours of battery life on one charge using the 16-cell battery. You can always carry an extra battery too if you want an extra safety net.

This mobile oxygen generator provides users with an ergonomic design. Unlike many other oxygen devices, it has a curved shape that fits comfortably at your side. When you walk around it will stay at your hip rather than swaying around causing you to lose balance. This is a small detail but it just goes to show that Caire Inc. has gone the extra mile to ensure oxygen patients are as comfortable as possible.
4.) Inogen One G5 (10,000 feet)
The Inogen One G5 has been neck-in-neck with the Caire FreeStyle Comfort since it was first manufactured. Inogen Inc. has been a household name when it comes to reliable lightweight oxygen devices, and the G5 is their latest and greatest product. One of the unique things about the G5 is that it combines all the best features of its previous generations of oxygen concentrators.

While the Inogen One G4, the last generation of Inogen units, was the second lightest portable oxygen concentrator ever produced, it lacked the oxygen output to satisfy the needs of the majority of oxygen patients. Much like the FreeStyle Comfort, the G5 weighs under 5 pounds, but it also offers a higher oxygen output at 1,260 ml/min or 6 pulse flow settings. What this means is that more oxygen patients — even those who have high oxygen demands — can experience the freedom of owning a portable oxygen concentrator.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Another unique feature of the Inogen One G5 is Inogen Connect, a mobile application that affords you more control over how you use your oxygen concentrator. This application connects your phone wirelessly to your concentrator and enables you to check your battery life and adjust your flow setting without ever touching your oxygen device. This is especially useful for people who use the Inogen G5 backpack and don’t want to take it off constantly to check their G5.

When it comes to using medical oxygen at high altitudes, most people will find that the G5 has just as much, if not more to offer than the Caire FreeStyle Comfort. It has the same maximum operational altitude at 10,000 ft and it offers a little more oxygen output in case your blood oxygen level drops and you need to move up a couple of flow settings. You can also rest easy knowing you own a mobile oxygen machine manufactured by one of the most trusted names in the industry.
3.) Respironics SimplyGo (10,000 feet)
The Respironics SimplyGo is a continuous flow portable oxygen concentrator released by Philips in 2012. The term “continuous flow” indicates that it puts out a constant stream of oxygen irrespective of the user’s breathing rate. This is problematic because it means oxygen is coming out of the device even when the user isn’t inhaling. In other words, the SimplyGo is less efficient than the two devices listed above.

With that being said, the Respironics SimplyGo is still an excellent portable oxygen delivery device for certain people. For example, if your doctor requires that you use continuous flow oxygen rather than pulse dose, the SimplyGo will be one of your best options. It’s the lightest continuous flow unit, weighing in at 10 pounds, and it also has the same maximum operational altitude as the FreeStyle Comfort and Inogen G5 at 10,000 ft above sea level.

While the Respironics SimplyGo is light enough to be carried on your shoulder or back, you’ll probably be more comfortable using a carrying cart and wheeling it around. And since the batteries are placed in the top of the unit, you won’t have to flip the device over or remove your carrying case in order to replace them. This is very convenient when you’re traveling and don’t have much time to stop.
2.) AirSep FreeStyle 5 (12,000 feet)
AirSep is a brand that’s been in the oxygen industry for a long time, and it shows. Over the years, they’ve manufactured oxygen concentrators that are trusted by millions of people. They always show a constant desire to innovate their products and adapt them for a new generation of people who expect more portability and comfort from their oxygen devices.

Much like Inogen’s “G” line of POCs, AirSep has their “FreeStyle” line of POCs. The FreeStyle 5 was released quite a few years ago. But despite its age, the FreeStyle 5 still stands out as one of the best wearable oxygen concentrators on the market. It provides oxygen users with 1,000 ml/min of pulse dose oxygen and 5 different pulse dose options. What’s more, it only weighs 6.7 pounds meaning it’s significantly lighter than the lightest continuous flow portable oxygen concentrator.
The FreeStyle 5 is an outstanding option for anyone who wants to travel to high altitudes because its maximum operating altitude is 12,000 feet above sea level. Considering the city in the United States with the highest altitude is just over 10,000 feet, the FreeStyle 5 will more than suit your needs.

Like all oxygen concentrators on this list, the FreeStyle 5 comes equipped with both AC and DC charging options. In other words, you’ll be able to charge your POC at home or in hotels via a wall outlet as well as in a vehicle via the electrical outlet. If you’re traveling to another country you can purchase a charging adapter. However, be sure to check the user manual before doing this to make sure you’re using the right voltage.
1.) SeQual Eclipse 5 (13,123 feet)
The SeQual Eclipse 5 is known for offering the highest oxygen output of any portable oxygen concentrator. It can put out a maximum of 3 liters per minute of continuous oxygen and it has 9 different pulse flow settings as well. But what many people don’t know is that the SeQual Eclipse 5 also holds the record for the highest operational altitude of 13,123 feet above sea level.

Despite how powerful the Eclipse 5 is, it is very heavy. It weighs around 18.4 pounds which is nearly four times as much as the FreeStyle Comfort and Inogen One G5. It’s also extremely bulky, so if you’re looking to do some hiking or skiing, the Eclipse 5 is not the oxygen concentrator for you. This unit is best for people with high oxygen demands who still want to be able to travel or live at high altitudes.

Since the SeQual Eclipse 5 has both continuous flow and pulse dose you’ll have enough options to suit whatever situation you’re in. If you have obstructive sleep apnea (OSA) and you need to use a CPAP machine while you sleep, you can switch to continuous flow on your Eclipse 5 and use it simultaneously with positive airway pressure. On the other hand, if you’re out and about and you want to conserve battery life, you can switch over to the pulse dose setting.
Conclusion
Whether you’re going to high altitude for a short vacation or to live, you need to ensure that your oxygen device will function properly. Not all oxygen devices have the same maximum operational altitude, and you should take into account other factors such as the device’s portability, battery life, and reliability. All of the devices on this list are approved by the Federal Aviation Administration (FAA) meaning you’ll be able to fly on any commercial flight within the United States while using your POC.
No matter whether you’re traveling to high altitude soon or you’re trying to plan for the long term, be sure to reach out to our respiratory specialists here at LPT Medical. It’s our highest priority to find you a portable oxygen concentrator that meets both your wants and your needs. We start by asking you about what oxygen flow you need. We then start to narrow down your options based on your lifestyle.
If you have any questions, feel free to leave them in the comment section so that we can get back to you. And if you’re ready to learn more about oxygen concentrators, give us a call or email us.

If you are ill with a chronic lung disease, you have likely experienced hypoxemia or hypoxia or both, these conditions limit the amount of oxygen your body is able to generate and so it greatly impacts your health. Breathlessness, fatigue, and insomnia are three of the prime symptoms associated with hypoxemia and hypoxia but all of the symptoms can be mitigated and managed with the help of supplemental oxygen therapy.
Not everyone who experiences hypoxia or hypoxia requires supplemental oxygen there are a series of tests that will inform your doctor of the serenity of your condition, and whether or not you require oxygen in order to treat your disease.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Everyone is different and everyone's disease can impact their health in different ways, therefore as a respiratory patient it is important to understand your disease to the best of your ability so you are able to treat it to the best of your ability.
While reading this article, bear in mind that everyone is different, and some things in this blog may apply to you while other aspects of your disease do not. Talk with you pulmonary health specialist, whether that is your doctor or pulmonary rehabilitation health care team to understand your disease better.
In this blog we are focusing on the contrast between hypoxia and hypoxemia and how these conditions can be treated with the help of oxygen therapy.
Oxygen therapy

There are many ways people utilize oxygen therapy. LPT Medical highly recommends some kind of portable oxygen concentrator for oxygen patients who are medically qualified for one. These devices are lightweight and run on batteries, meaning you can bring them anywhere (even on an airplane) and they will never have to be refilled.
If you are interested in the oxygen devices LPT Medical offers, call 1(800)-946-1201 to speak with a respiratory specialist. They will ask you a series of questions about your health and lifestyle in order to narrow down your options to buy a portable oxygen concentrator.
You can also take a look at these 3 other blogs that go into detail about some of LPT Medical’s best selling portable oxygen concentrators.
Comparing the Three Best Portable Oxygen Concentrators of 2021
7 Reasons to Replace Your Liquid Oxygen Tank with a Caire FreeStyle Comfort
Inogen Portable Oxygen Concentrators and You: A Match Made in Breathlessness
Having an oxygen device that you enjoy using makes life so much easier, and spending the money upfront actually saves you money in the long run, so portable oxygen concentrators are the way to go if you are on a budget.
COPD Treatments
COPD treatment consists of lifestyle changes, medication, and oxygen therapy if needed. Not every COPD patient needs long term oxygen therapy (LTOT), but if you and your doctor decide it is time to take that course of action, LTOT is a beneficial treatment that can enhance the quality of life and even add years to your life.
Hypoxemia vs. Hypoxia
Hypoxemia and hypoxia do not always coexist.
Hypoxemia

Typically, patients with hypoxemia have blood oxygen levels at or lower than 92% which is a decrease in partial pressure of oxygen blood vessels, oxygen therapy is typically a go to treatment for hypoxemia.
Many people with chronic obstructive pulmonary disease have hypoxemia. If you do, supplemental oxygen treatment can improve your well-being; alternatively, in some, this can lead to hypercapnia, which is the adverse effect of elevating the carbon dioxide content in the blood to toxic levels.
This is why it is important to only take oxygen when directed to by your doctor. Too much oxygen or taking supplemental oxygen when you do not need it is toxic for your system.
The adverse effect of oxygen on chronic obstructive pulmonary disease is to cause increased carbon dioxide retention.
Carbon dioxide retention can look like:
- Drowsiness
- Headaches
- In severe cases lack of respiration, which may lead to death
Hypoxia
Hypoxia means you have reduced levels of tissue oxygenation. Hypoxia can be attributed to a defective delivery of oxygen or your tissues are defective in utilizing oxygen, either way this condition will affect individuals differently based on the condition’s cause and severity.
Generally, symptoms include:
- Coughing
- Wheezing
- increased heart rate
- Headache
- bluish color in the skin, lips, or fingernails (called cyanosis)
Severe cases might even cause:
- Fainting
- Seizures
- Confusion
- Difficulty speaking
- Temporary memory loss
- Difficulty moving
- Coma
Chronic or less severe cases of hypoxia can cause general fatigue and shortness of breath, especially after physical activity.
Causes of hypoxia could be Asthma attacks and lung diseases. Both of these conditions restrict your oxygen supply thereby causing hypoxia directly.

Heart diseases can also impair your cardiac output, and decrease the blood flow to and from your organs, this is ineffective oxygen transport that causes hypoxia.
Since coronavirus (COVID-19) has emerged, this sickness has also been known to cause hypoxia.
Many people experience hypoxia when there is low oxygen concentration in the surrounding air for example at high altitudes. This is especially true for individuals with pre-existing risk factors like COPD or asthma.
Testing for Low Oxygen Levels

To test for Hypoxemia and Hypoxia, doctors will first give you a physical exam to evaluate your heart and lungs. If they recognize signs of hypoxia or hypoxemia, they can confirm these signs with other tests.
If they see signs, they will try tests like pulse oximetry which is a non-invasive test used for measuring oxygen saturation or the percentage of hemoglobin saturated with oxygen in your blood.
You can also use a pulse oximeter monitor in your everyday management of chronic obstructive pulmonary disease to check up on your pulmonary function, or how well your lungs are working.
An arterial blood gas test is a blood sample test used to measure the partial pressure of oxygen, oxygen saturation, the partial pressure of carbon dioxide, and blood pH levels within your blood. This means the test is looking at the levels of oxygen in your blood, and whether or not they are healthy.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
After all of this, your doctor may order other tests like an MRI, CT scan, echocardiogram, or electroencephalogram (EEG) in order to ensure your diagnosis, and to understand its severity. These tests will also determine the course of action your doctor will recommend you to take and any prescription medication ro oxygen therapy you may need.
Once you have been tested and it is confirmed that you are experiencing Hypoxemia and Hypoxia, either due to a chronic condition or an environmental aliment, you may require the utilization of oxygen therapy. If you have a chronic illness, you may need long term oxygen therapy.
How Does Supplemental Oxygen Help Hypoxemia and Hypoxia
Supplemental oxygen therapy improves your lungs and oragn’s ability to function, thereby reducing your symptoms, improving your well being, and even adding years to your life.
Supplemental oxygen therapy can help treat hypomania and hypoxia in many ways…
Treating Shortness of Breath

First and foremost, oxygen therapy helps you to be less short of breath, breathlessness is one of the most prevalent symptoms of lung disease, and one of the most notably uncomfortable symptoms. Relieving breathlessness can open up a lot of doors for oxygen patients to become more active and to have more energy.
Everyday activities become easier, and with the help of a lightweight portable oxygen device you can find the will to exercise which is very important to do if you have a respiratory illness.
Treating Fatigue
-jpg.jpeg)
With the help of oxygen therapy, you will feel less fatigued because oxygen will be circulating your bloodstream and rejuvenating your organs. Once your oxygen levels are back to a normal rate, your mind and body will both feel more energized.
Treating Insomnia

People with lung disease often have a hard time sleeping. This is because of the lack of oxygen your body is receiving from your lungs with every breath if you have hypoxemia or hypoxia.
Everyone for the most part, has trouble sleeping if there is a lack of oxygen, for example, people will have trouble sleeping at higher altitudes, where there is less oxygen in the air to begin with. When you spend the night at higher altitudes than you are accustomed to, for instance in Denver, Colorado, every lungful of air you take provides fewer oxygen molecules to your body.
Lack of oxygen for long periods of time can induce insomnia, so visiting high altitude areas, or having a lung disease that impairs your bodies ability to process and use oxygen increases the risk of experiencing headaches, fatigue, digestive issues and nausea.
The lack of oxygen initiates unstable breathing patterns while you sleep, so your body works overtime to try and restore normal oxygen levels. Rather than sleeping through the night, your body will go through periods of breathing, not breathing, waking up, and dozing off, and overall you do not get good rest.
Oxygen therapy gives your body the oxygen you need so that your system does not have to struggle to oxygenate your blood and organs. Even if you do not require oxygen therapy at night while you sleep, using supplemental oxygen during the day stabilizes your oxygen levels, so when you do go to sleep you will not suffer from lack of oxygen induced insomnia.
If you do need oxygen while you sleep, it is important to have portable oxygen concentrators that can cover your oxygen requirements at night. For instance, the Respironics SimplyGo portable oxygen concentrator is CPAP/BiPAP compatible and it is equipped with both pulse flow and continuous flow oxygen delivery modes to cover you 24/7. It offers pulse flow settings 1-6 and continuous flow settings 0.5-2.0 LPM.
To learn more about this device, and the others that could help you get to sleep and stay asleep, call 1(800)-946-1201 to speak with a respiratory specialist at LPT Medical.
Overview

Oxygen is life, and not getting the oxygen you need is debilitating. Taking care of yourself means adjusting to a proper oxygen therapy regime and adhering to your treatment.
Chronic illnesses, such as COPD, are not curable, but they can be treated, and you can live a healthy and long life with these conditions.
That being said, feeling the effects of hypoxemia and hypoxia will be very uncomfortable and addressing these conditions is crucial for your wellbeing. You can address the symptoms of breathlessness, fatigue, and insomnia by utilizing your oxygen therapy.
If you are not happy with your oxygen therapy method, there are ways to make oxygen therapy more comfortable and suitable for your lifestyle. You can start by understanding your options when it comes to oxygen therapy methods, there are three different oxygen devices and depending on your oxygen prescription you can fit the requirements laid out by one or all three of these devices.
People with a high oxygen output prescriptions normally need to use an oxygen tank or a home oxygen concentrator because these devices can emit a lot of oxygen at one time, that being said there are downsides to these devices, and if you do not have to use one, there are better more mobile devices available today.
Overall it is important that you do not wait to address symptoms associated with hypoxemia or hypoxia, and that you get tested right away, because it is possible that you are experiencing signs of a chronic illness like COPD. If this is the case, treating the disease in a timely manner can be the difference between experience very severe symptoms and managing your symptoms before they get worse.
Planning a big trip is never a simple task, but it can be especially difficult if you use supplemental oxygen. It can be complicated, stressful, and even feel overwhelming to travel when you have to bring oxygen everywhere you go.
Cruises can be even more daunting than other types of travel, since they are relatively long and remote excursions. They take you far from home and in to foreign places, which requires some extra planning and care.
However, you shouldn't let your oxygen therapy get in the way of enjoying all that a cruise line vacation has to offer. You'll find that, as long as you plan ahead, you can have a perfectly safe and enjoyable cruise even if you're dependent on oxygen.
But unless you are a frequent cruiser, planning a cruise is probably an unfamiliar and intimidating task on its own, even without considering your medical needs. That's why we've created this guide to help you navigate the tricky waters of taking a cruise on oxygen.
The goal of this guide is to give you a thorough overview of everything you need to know and consider if you have to use oxygen on your cruise. We'll explain all the steps you should take both before and during your trip to ensure a safe, fun, and hassle-free vacation.
We'll show you how to plan ahead, avoid common problems, and make sure you have all the oxygen, equipment, and care that you need during your cruise. We'll also show you how to work with your doctor and your cruise line to ensure that all of your personal and healthcare needs are taken care of along the way.
How to Prepare for Your Cruise with Supplemental Oxygen

If you are planning a cruise for yourself or someone else who is dependent on supplemental oxygen, it's important to pay extra attention to the details. You not only have to plan the basics, but you also have to figure out how to procure, transport, and store all of your oxygen supplies along the way.
You also have to consider the cruise line's policies and processes for handling medical equipment and serious medical conditions. You'll need to work with your doctor, your cruise line, and likely even your insurance provider to make sure all your medical needs are fully covered on your cruise.
It might seem like a lot to think about, but it's important to cover all of these bases if you want a safe and successful cruise. Skipping any of these steps could cause major problems, such as difficulty boarding the ship or, even worse, put your health in danger while you're out on the open seas.
On the other hand, planning well ahead of time will help you avoid unnecessary hassle and give you peace of mind. By working out all the details ahead of time, you'll feel more secure about your trip and your access to oxygen during your cruise.
Here is a list of some major factors to consider as you prepare to take a cruise on oxygen:
- What kind of oxygen sources you will bring (tanks, portable oxygen concentrator, etc.)
- How much oxygen you should bring, including extra for emergencies and delays
- Cruise line policies and requirements for oxygen and other prescription medications
- How to transport your oxygen supplies onto the cruise ship
- How to ensure you won't run out of prescription or non-prescription medications on your trip
- Cruise line amenities and accommodations for people with special needs and medical conditions
- Respiratory hazards and other adverse conditions you may encounter on your cruise
In the rest of this guide we're going to discuss how to handle each of these issues and much more in greater detail. We will explain everything you need to know to plan a successful cruise on oxygen and how to avoid unexpected roadblocks along the way.
This guide offers plenty of useful tips you can use to prepare for your cruise and make on-board oxygen therapy as hassle-free as possible. That way, you can have a wonderful, relaxing, and memorable vacation while taking the best possible care of your health.
Check Your Cruise Line's Policies and Accommodations

If you use oxygen, one of the things you must do before booking your cruise is check the cruise line's policies on oxygen therapy and other medical concerns. If you don't, and you show up without the right equipment, information, or forms, then you could get turned away from the ship.
To save yourself the heartache of missing your trip, get as much information as you can about the cruise line's rules and accommodations early on in your planning process. That means looking up their policies on medical equipment, prescription medications, and special medical needs.
Don't Forget to Give Advance Notice & Submit Required Forms

All cruise lines require you to notify them ahead of time if you use oxygen or have a serious medical condition. Some even limit you to certain types of oxygen equipment or limit the number of tanks you can bring.
At the very least, your cruise line will ask you to give them some basic information about your medical condition and the equipment you plan to bring. Many cruise lines have a special form for this, which you will need to fill out and submit a few weeks before your trip.
Your cruise line will likely need know much oxygen you're bringing and the dimensions of each oxygen tank. Some might even ask for paperwork from your doctor detailing your prescription medications and special medical needs.
As an example, here is a link to the medical “special services” form that you have to fill out for Disney Cruise Line.
You will also need to know the cruise line's rules for bringing oxygen on your person when you first come on board. For example, Disney Cruise Line allows you to bring two oxygen cylinders with you to your room, but all others must be delivered to the ship by a third-party supplier.
Most of the time, you can find general information about your cruise line's policies from their website. However, you should also contact the cruise line directly to verify the information and make sure you don't miss any necessary steps or forms.
Communicating with your cruise directly is the best way to ensure that your trip goes smoothly and the crew is prepared to accommodate your needs. It is important to give them information that is as accurate and complete as possible to avoid unnecessary hassle and potentially serious problems.
Here are some things you might want to ask your cruise line when you call:
- Am I allowed to bring liquid or compressed gas tanks on board if I need them for oxygen therapy?
- Are there any restrictions on the type of oxygen tanks (e.g. liquid or compressed-gas), size of oxygen tanks, or number of tanks I can bring?
- What forms do I need to fill out in order to bring my own oxygen supply and equipment on board?
- Do I need to fill out any forms in order to bring my prescription medications on board?
- Do I need to provide any documents from my doctor related to my oxygen therapy, prescription medications, or medical condition?
Cruise Line Medical Services

If you depend on oxygen therapy, then it's important to have access to healthcare during your cruise in case you experience a medical problem or emergency. That's why it's important to look into what kinds of medical services are available on the ship.
All cruise ships have a medical staff on board, but you can ask your cruise line about their specific services if you are concerned. They can answer any questions you have about their medical clinic or pharmacy, and verify that they have the proper equipment and staff to take care of you in an emergency.
You should also check with your medical insurance provider to make sure that you will be covered on the ship and at all your travel destinations. You may need to purchase extra travel or medical insurance to cover any special care you need during your cruise.
Accessibility Accommodations and Amenities
 |
| Photo by ironypoisoning on Flickr. |
Some cruise lines offer accessibility and disability services for guests with special medical needs. This can be helpful if you have limited mobility, as many people who use oxygen do.
You might even have the option of booking an “accessible” room that's designed to accommodate special physical needs. Every cruise line is different, so make sure to ask yours about their accessibility options before you book your room.
For example, Disney Cruise Line offers a range of accommodations, including:
- Rooms with wider doorways for mobility aids
- Shower seats and transfer benches
- Raised toilet seats
- Bathroom grab bars
- Sharps containers
- Threshold ramps
- Adjustable shower heads
- Emergency call buttons
Stocking Up on Oxygen Before Your Cruise
The vast majority of cruise ships do not have on-board oxygen available except in the case of emergencies, which means you will have to bring your own. That's why the the most vital part of planning your cruise is making sure you bring enough oxygen to last the whole trip.
How you should do this depends on how much oxygen you need and what kind of oxygen supply you use. It's important to consider the pros and cons of different options ahead of time, so you can secure your oxygen and arrange delivery in time to make your cruise.
Choosing an Oxygen Supply
Many people who use oxygen use a stationary oxygen concentrator in their home as their primary oxygen supply. However, you will need a more portable oxygen source to take with you when you go on your cruise.
There are two main types of oxygen you can use on a cruise ship:
- Liquid or compressed-gas oxygen tanks
- A portable oxygen concentrator
The easiest way to travel with oxygen, by far, is to use a portable oxygen concentrator. These devices are smaller, lighter, and significantly more convenient than other types of oxygen supplies.

Since it generates concentrated oxygen from normal, ambient air, a portable oxygen concentrator will never run out of oxygen as long as you keep the battery charged. This eliminates the need to stock up on heavy, bulky oxygen tanks.
If you cannot get a portable oxygen concentrator, you will need to make sure you have enough liquid or compressed-gas oxygen tanks to last the duration of your cruise. To do this, you will need to coordinate with your doctor and your oxygen supply company to get the right amount of oxygen delivered.
Oxygen tanks can be difficult during travel, since they take up a lot of space and require careful handling. Depending on the cruise line you use, you might be limited to a certain number of tanks, a certain size of tank, or a particular type of oxygen device.
This is why it's so important to look up your cruise line's policies and contact them before you book your trip. You can't be too careful or too thorough when it comes to planning this part of your cruise.
Making Sure You Have Enough Oxygen: Liquid and Compressed-Gas Oxygen Tanks
Since liquid and compressed-gas oxygen tanks hold a limited amount of oxygen, you have to be very careful to make sure you bring enough. Once you know exactly how long your cruise will be, talk to your doctor to figure out exactly how much oxygen you will need to make it through the trip.
It's worth taking the time to double-check your plans and verify your arrangements with the oxygen supplier a few days before your cruise. Don't be afraid to go over your oxygen supply estimate with your doctor more than once to catch any oversights or mistakes.
Additionally, you should make sure you have more than the minimum amount of oxygen you think you will need. You should bring enough extra oxygen to last at least a day or two beyond the expected length of the cruise.
This will ensure you can continue your oxygen therapy uninterrupted even in the case of an unexpected emergency or delay. It may also help you feel more secure to know you don't have to worry about pushing the limits of your oxygen supply.
However, if you use a portable oxygen concentrator, then you don't need to worry about running out of oxygen at all. The only thing you need to worry about is bringing enough battery power to keep your portable concentrator running the whole time.
Getting Your Oxygen Tanks on the Ship

Because they are heavy and difficult to move, you will probably need arrange special transportation to get your liquid or compressed-gas oxygen tanks onto the cruise ship. You might be able to do this through your usual oxygen supply company, but you might need to find a different supplier that can deliver directly to the ship.
Your oxygen supplier will also need to pick up the empty oxygen tanks once you get back from the cruise. Make sure to ask them about any delivery or pick-up fees they charge and make sure they can guarantee on-time delivery and pick-up from the ship.
If you can transport the oxygen supply on your own, the cruise line might allow you to bring them to the ship yourself. However, some cruise lines will only accept oxygen tanks delivered by a third-party supplier, so be sure to verify their rules ahead of time.
You should also talk to your cruise line about how you are supposed to retrieve your oxygen tanks once aboard. For instance, you might need to call a specific number to have a crew member deliver a new oxygen tank to your room.
Making Sure You Have Enough Oxygen: Portable Oxygen Concentrators

Portable oxygen concentrators are convenient for just about any use, but traveling is where their benefits get a chance to really shine. First of all, they never run out of oxygen. Second, they are much smaller and much easier to transport than unwieldy oxygen tanks.
Taking a portable oxygen concentrator on your cruise saves you the hassle of having to stock an entire trip's-worth of oxygen tanks on the ship. That means no need to coordinate with an oxygen supply company, no need to arrange a large delivery of oxygen, and no worries about not bringing enough.
Instead, you just have to bring your portable oxygen concentrator, charger, a couple extra batteries, and then you're good to go. That way, you can spend more time planning the fun parts of your cruise and less time worrying about how to procure enough oxygen to last the entire trip
Don't Forget to Bring Your Charger and Extra Batteries
When you use a portable oxygen concentrator, you never have to worry about your oxygen supply as long as you keep the batteries charged. At a minimum, you should bring two sets of batteries to ensure you always have power when you need it.
You should also bring a separate, external battery charger to place the batteries in when they are not in use. This will allow you to use one set of batteries in your portable oxygen concentrator while the other set of batteries charge up.
Especially if you use oxygen 24/7, it's important to be diligent about switching out the batteries and remembering to keep one set charging at all times. If your concentrator uses up battery more quickly than your charger can charge the second set, then you may need to bring more than two.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
To help you determine how much battery power you will need, you can refer to your portable oxygen concentrator's manual. It will tell you how long the battery will last on each flow rate the concentrator offers, which you can use to determine how often you'll need to switch the battery out.
If you do end up running out of battery, you can always continue to use your portable oxygen concentrator by plugging it directly into an outlet. While this limits your ability to move around, it's a safe back-up option to use while you wait for your extra batteries to charge.
Ideally, you should bring enough battery power to keep your portable oxygen concentrator going 24/7 while allowing them enough time to charge between rotations. To compare the battery life and other features on some of the top portable oxygen concentrators, you can take a quick look at this guide.
Don't Forget ALL Your Oxygen Delivery Equipment
In all the fuss over planning and packing for your trip, don't forget to bring all the oxygen supplies and accessories that you normally use. That includes your nasal cannula or oxygen mask, extension tubing, and any other accessories like your humidifier bottle or equipment cleaning supplies.
Since you'll be cut off from the rest of the world for potentially days at a time on your cruise, you may even want to bring some extra supplies. For instance, even if your nasal cannula will last the whole trip, bring an extra one along just in case.
When you're in a new, strange place like on a cruise ship, your things are more likely to get lost, damaged, or misplaced. Even if you are usually very good at keeping track of your things, you might find it more difficult when your routine and environment change.
That's why it's best to be over-cautious and bring along some extra oxygen supplies. You should always hope for the best, but you should also plan for the worst when your lungs and your health are at stake.
Here is a list of supplies you might want to include in your cruise packing list:
- Nasal cannula or oxygen mask (plus one extra)
- Extension tubing (plus one extra)
- Humidifier bottle
- Tubing clips
- Tubing tape or soft covers
- Swivel connectors
- Sanitizing wipes
- Sanitizing solution
- Your CPAP/BiPAP machine and related equipment (bring a travel sized machine for extra convenience)
- Any other prescription or over-the-counter medications you need
Don't Forget Your Medications

While most cruise lines have an on-board pharmacy, they usually only stock a small selection of medications. If you take any prescription or over-the-counter medicine, you should bring it with you to your cruise.
First of all, make sure you will have enough medication to last the entire length of your trip. If you are due for a refill before the end of the cruise, talk to your doctor about getting enough extra medication to last until you return.
Remember to check your cruise line's policies on prescription medications to make sure that you bring any necessary documents or forms. Even if the cruise line doesn't require it, it's a good idea to have your doctor print out a complete list of your medications, dosages, and treatment regimen to keep with you during your trip.
Protect Your Lungs from Environmental Conditions on Your Cruise

Along with all the logistics of bringing your oxygen, equipment, and medication on board, it's a good idea to look in to the specific conditions you will encounter on your cruise. Whether in your cabin, in the main ship, or at port destinations, it's important to make sure you can keep yourself and your lungs as safe and comfortable as possible.
Prepare for Irritants on the Ship

If you are sensitive to dust, allergens, or other respiratory irritants, check with your cruise line to make sure the environment in your cabin won't irritate your lungs. Make sure you book a non-smoking room and ask to be placed as far away from smoking areas as possible.
Fortunately, most cruise ships take cleanliness very seriously and follow strict sanitation guidelines set by the Center for Disease Control and Prevention (CDC). The CDC even has a vessel sanitation program that performs regular cruise ship inspections and publishes their results for the public to read online.
However, if your lungs are very sensitive to mild irritants, you may be able to request special bedding or other accommodations. Some cruises even offer special hypo-allergenic rooms if you're willing to pay the extra cost.
If you're bothered by mild fragrances and fumes, don't forget to pack your own fragrance-free shower and personal care products to bring with you on board. If you have a quick-relief medication prescribed by your doctor, always keep it close by during the cruise.
Once again, you can always discuss any concerns you have with your cruise line. They can more thoroughly explain their cleaning practices, room options, and help you make special arrangements if they are
.png)
It seems like no matter where we go these days or what we’re doing, we’re always using technology. While several decades ago, it may have been possible to avoid using a cell phone or the internet, this becomes increasingly difficult as nearly everything around us is moving digital. According to the Pew Research Center, 95% of adults between the ages of 50 and 64 own a cell phone, and 79% of people in the same age group own smartphones. These numbers are only expected to increase over the years.
Although the pros and cons of smartphone use are hotly debated, it’s fair to say that they’ve afforded us easier access to information than ever before. And if you’re someone with a respiratory illness like chronic obstructive pulmonary disease (COPD), you know that technology enables you to stay connected more easily with friends and loved ones, and research information about managing and treating your disease. What’s more, most of these resources are free and easy to use.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
If you’re a COPD patient who’s interested in technology that allows you to interact with your disease in unique and beneficial ways, stick around. We’re going to be taking a look at some of the best mobile applications you can have on your smartphone. In the meantime, if you’re in the market for a portable oxygen concentrator, feel free to reach out to our respiratory specialists in Denver, Colorado. LPT Medical offers the lowest prices on the latest portable oxygen concentrators including the Caire FreeStyle Comfort, Inogen One G5, and the Respironics SimplyGo.
AirNow Mobile Application (Android and Apple)
If you’ve read any of our blog posts here at LPT Medical, you know how important air quality is to us. While cigarette smoking is still the primary cause of COPD, exposure to outdoor air pollution, and indoor irritants is still a significant risk factor for contracting COPD. this is why it’s of the utmost importance to be conscious about the air we breathe and take steps to plan our life around these issues. While there will always be poor air quality due to wildfires and carbon emissions, we can take steps to live healthier lives.

If you read our post about wildfires, you know that we discussed a very important component of air quality: the air quality index (AQI). This is a broad term used to describe the overall quality of air outdoors. It’s an aggregate score of five major types of pollutants including carbon monoxide, particle pollution (PM2.5 and PM10), ground-level ozone, sulfur dioxide, and nitrogen dioxide. The AQI scale runs from 0 being perfect air quality and 500 being the absolute worst. Generally speaking, COPD patients should not be outside if the AQI is over 100, but this will depend on the severity of your symptoms.
.jpg)
Rather than having to go to the AirNow website to check the AQI in your area, the AirNow Mobile application allows you to do it anywhere in the world from the convenience of your smartphone or tablet. You can save a variety of different locations to easily check the AQI all over the country and you can even view the AQI forecast in your area to make it easy to plan your week. Since all of the information is pulled straight from AirNow.gov, you can rest assured that it’s up-to-date and factual.
Breathe2Relax (Android and Apple)
Most people give very little or no thought to the way they breathe — but they should! The way we breathe is directly linked to many of the body’s functions including, sleep, digestion, and cognitive function. Simply by becoming more self-aware of our breathing habits and implementing techniques like deep breathing and diaphragmatic breathing, we can begin to reverse the negative effects of shallow, ineffective breathing. This is imperative for COPD patients who have significantly reduced lung function compared to the general population.
Another problem with ineffective breathing is that it can cause anxiety. The Breathe2Relax app was created specifically to target this type of breathing and correct it so that you can feel more at peace and relaxed in your day-to-day life. One of the techniques it focuses on is diaphragmatic breathing which teaches you how to breathe using the diaphragm muscles below the lungs rather than using the chest muscles to breathe. Many people find it difficult to learn this technique from simply reading about it, so this app is more interactive to ensure you do the exercises correctly. Another great feature of this app is that it can connect with your Apple Watch to measure your heart rate and provide you even more detailed information about your health.
If you’d like to learn more about breathing exercises for COPD, we’ve created a great comprehensive guide. In this post, we take a look at 6 key breathing exercises that all COPD patients should know about including:
- The stop, rest and continue technique
- Pursed lips breathing
- Coordinated breathing
- Deep breathing
- Diaphragmatic breathing
-
And a relaxed posture
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
NCI QuitGuide (Android and Apple)
According to the American Lung Association, 85 to 90 percent of COPD patients contract their disease through cigarette smoking. While not all people continue smoking after being diagnosed with COPD, you may be surprised to find that around 38% do. Unfortunately, many people believe that the damage has already been done, and continuing to smoke will not affect them, however, this couldn’t be further from the truth. Any amount of smoking, whether it’s one cigarette a week or a pack a day will contribute to lung inflammation, and thus, increase the rate at which COPD progresses.

Another problem with smoking as a COPD patient is that it significantly increases your risk of experiencing a flare-up or exacerbation. In short, an exacerbation is a sudden increase in respiratory symptoms such as breathlessness, chest pain, coughing, or wheezing. Acute exacerbations can be severe and even lead to hospitalization if they aren’t dealt with swiftly and efficiently. Smoking also impairs your immune system’s responsiveness making you more likely to contract a lung infection. Infections are also the most common cause of COPD exacerbations. For a more detailed look at the importance of smoking cessation, please visit our article titled: 15 Important Things That Happen When You Quit Smoking.
While there are many “quit smoking” apps out there, we chose NCI QuitGuide because it was created by the National Cancer Institute. This is one of 11 government organizations that makes up the Department of Health and Human Services (HHS) in the United States. NCI QuitGuide is not necessarily designed to be an all-in-one smoking cessation tool, but it can be used in tandem with other methods like nicotine replacement therapy and cognitive-behavioral therapy (CBT). Be sure to consult with your doctor to determine which method is best for you.

QuitGuide is a simple mobile application that allows you to track cigarette cravings, mood, and your reasons for quitting. It also displays information about your smoking cessation including the amount of money you’ve saved, days smoke-free, and provides you with milestones to reach. This app is perfect for anyone who wants to see the tangible effects of smoking cessation. The best part of all is that it’s free. There’s no need to worry about paying an upfront fee or paying a subscription of any kind.
The COPD Pocket Consultant Guide (Android and Apple)
We’ve referenced the COPD Foundation many times and you’re likely familiar with COPD360social, a free social networking site for people with COPD. However, you may be less familiar with their mobile application, the COPD Pocket Consultant Guide. This app has tools for healthcare providers, caretakers, and patients, so it’s important that you select the option that applies to you when you first open it. Once you have it set up, however, you’ll find that you have a variety of resources at your disposal.

The “For My Next Visit” section is designed to help you prepare for your next doctor’s visit. This is a simple tool that displays a bunch of “questions” and “symptoms.” You can then go through and select the questions you’d like to ask your doctor upon your next visit, along with any symptoms that have changed since your last one. You can then either save your results or print them out to show your doctor.
The “Wallet Card” section is designed to work like a digital version of your medical information card. Through this tool, you can save important information about your oxygen concentrator flow setting, CPAP or BiPAP settings, and a whole host of other things such as your physician contact information and insurance provider information. The best part about this feature is that it allows you to secure all of this important information using face identification technology. This way, you ensure that only you can view this information.

The third feature of this app is the training video section. Pulmonary rehabilitation, inhaler therapy, and nebulizer therapy are key components of most COPD treatment plans, and these videos will show you exactly how to do these things effectively. Believe it or not, studies show that many people do not follow their treatment plan, especially when it comes to using an inhaler. This app provides the easiest solution to this with all the training videos in one area.
The next feature of this app is the “Activity Tracking” section. This section lists out a bunch of daily activities such as cleaning, making the bed, and brushing your teeth, then you get to choose the level of difficulty you have doing these things. Fill out this form once a month and then print it out to see what kind of progress you’re making in your day-to-day life.
![]()
An action plan is a series of steps you will take if you encounter a specific problem. The COPD Pocket Consultant Guide divides your symptoms into three different categories: green, meaning you feel good; yellow, meaning you feel worse than normal; and red, meaning you are experiencing serious and disruptive respiratory problems. Go over this section of the app with your doctor so that you’re prepared for days where your symptoms increase.
Last but certainly not least, there is a section titled “more” that has additional resources for you to view. This includes links to COPD360social, the COPD Foundation blog, the COPD Patient-Powered Research Network (COPD PPRN), a COPD Assessment Test (CAT), and a help page if you’re experiencing any issues with the app or you have any questions about managing your disease.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
All Respiratory Disease and Treatment (Android)
The last mobile application we’re going to go over is not necessarily specifically designed for COPD patients, but it’s more of an educational resource about all respiratory diseases — chronic and acute — and how they’re treated. This is a useful app if you’re someone who simply enjoys learning about the lungs and how to take care of them. It can also help you put COPD into perspective and clarify any confusion about its similarities and differences when it comes to other lung diseases.
The best advantage of using this app is that you won’t have to waste time scouring the internet for information about COPD and other lung diseases. Simply open up the app and you’ll be able to view a substantial amount of information about COPD like a definition, risk factors, symptoms, causes, home remedies, and much more. It’s also handy to have on-the-go if a question comes to mind while you’re away from your computer at home. The only downside is that this app is only available on Android.
Conclusion
The world is a more connected place than ever before. One of the biggest benefits of this is that we can have easier access to information in the palm of our hands, pretty much wherever we go. If you’re a COPD patient, you need to stay up to date on how to treat your disease, as well as how to use things like inhalers, nebulizers, and oxygen devices. The apps listed above are just a few of the free resources you have available to you if you use a smartphone like an Android or an iPhone.
Looking for more ways to stay connected? Telehealth technology is reshaping the way we view healthcare and it’s becoming increasingly more accessible for COPD patients like you. Check out this blog post where we feature portable oxygen concentrators like the Caire FreeStyle Comfort and the Inogen One G5 and the unique technologies they’re bringing to the oxygen industry. And in the meantime, stay tuned to our blog where we discuss helpful information about COPD and COPD management.
Happiness, an emotional state of being that humans are innately attracted to. Happiness overall embodies positivity and satisfaction, yet it is a subjective well-being that makes an individual truly happy. This means that everyone's happiness is rooted in something unique to them, and their journey through life is fueled by their own desires, and while society can inflict its bias on everyone and sway people into believing there is only one way to be happy, in reality happiness is limitless.
But how can you be happy if you are suffering? If you have COPD, it is fair to say that you are spending a lot of time in discomfort and even in pain, both physical and emotional, so seeking out happiness throughout you COPD diagnosis can seem like a daunting and even impossible task.
In this blog, we look into your COPD symptoms and how you can ease some of these uncomfortable feelings associated with your disease. Beyond treating your disease there are a few ways that you can begin to feel happy again, and we hope that some of these concepts resonate with you so you can start implementing them into your life.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
At LPT Medical, our goal is to help respiratory patients nationwide by giving them the oxygen equipment they need at the most affordable price. We offer the very best portable oxygen concentrator on the market that gives respiratory patients the freedom and independence many people crave in order to be happy! Again, happiness is subjective, and unique to every individual, which is why we supply many different brands, makes, and models on POCs, check out our inventory on our website LPTmedical.com, or reach a respiratory specialist based in Denver, CO by calling 1(800)-946-1201
Happiness is Reliable and Easy Oxygen Equipment

For many respiratory patients happiness is having oxygen equipment that is not only reliable but helpful. Studies have proven that oxygen therapy prolongs life in patients who are a certain level of hypoxic. So while the oxygen therapy is giving you a quantity of years back, remember that the type of oxygen equipment you are using can impact the quality of those years you are getting back.
If you utilize oxygen therapy you are most likely using one of these three methods:
- Portable oxygen concentrators
- Liquid oxygen tanks
- Gas oxygen tanks

There are several reasons why POCs give oxygen patients a quality of life that tanks cannot.
Portability

First and foremost, is the portable aspect of a POC compared to the two alternative methods. POCs were designed with the active oxygen patient in mind. We wanted to give oxygen patients who were looking to be more active the opportunity to do so without being weighed down by heavy machinery.
POCs like the Caire Freestyle Comfort weight just under 5 pounds and have an ergonomic shape that makes this device easy to carry with you in a Caire Freestyle backpack, or its Caire Freestyle custom carrying case. Have the accessibility to move freely around your home is happiness in itself. But in addition to this you will have the capabilities to exercise more frequently which is known to increase happiness and promote healthy emotional responses, and for many people more exercise means more happiness.

Battery powered
If you have an oxygen tank, you have to spend a lot of time and money waiting for your oxygen to be delivered to you weekly. Spending all of this cash and waiting around for a delivery service would weigh on anyone. There are often delivery delays that cause unnecessary stress, not to mention additional fees and price jumps for oxygen services that you have been using for years.
With a POC you are cutting off all dependability you have on other aspects outside of your control. Instead you are responsible for charging your device, and that's it. The Respironics SImplyGo POC is a pulse flow and continuous flow device, and its battery can last up to 3.4 hours, and when it needs to be charged you can do so almost anywhere. With the AC and DC charging cable you will be able to plug in your device at home, in the car or RV, even a boat!
Because POCs are not oxygen reservoirs, you can travel with your POC on an airplane. And it is no surprise that travel promotes happiness in so many people! If you love to travel, but are limited by your oxygen tanks, it could be very beneficial to you and your happiness to buy a portable oxygen concentrator.

Happiness is Treating your COPD with Care and Attention
For many people happiness is keeping their COPD symptoms at ease and treating their disease diligently in order to maintain a healthy lifestyle. Since we already discussed oxygen therapy, there are 6 other main treatments for COPD that can make a very big difference in the quality of life and happiness you are experiencing throughout your diagnosis. All of these treatments can go a long way in easing some of your symptoms and supporting your mental health.
- Medication
- Quit smoking
- Eating a COPD healthy diet
- Taking supplements if you have deficiencies
- Pulmonary Rehabilitations
- Therapy and/or support groups

Happiness is Appreciating the Little Things
Life is hard, and it's harder if you have COPD. The simplest thing in life, breathing, is being stripped away from you. It is uncomfortable and disheartening. Life seems unfair, and it is in the hardest and most painful moments you have to be strong enough to appreciate the small things in your life that are positive.
This is so much easier said than done, and it takes effort and time to be able to accomplish this practice. Here are some steps into focusing on the positive things:
1. Start a journal and write down one thing a day that you are grateful for. This can be easy because you can write down something as small as being grateful for a cup of coffee, or the support of a loved one. Try to think of something different everyday.

2. Drink more water and eat healthy. Staying hydrated and good gut health is directly related to our emotional responses in our brains, so what you eat has a large impact on how you feel emotionally.
3. Connect with your family and friends.Even if you can only do this virtually, try to call and speak with someone that you love once a day, even if it's just for a small amount of time. Humans are very social creatures, and social interaction can promote happiness if you value togetherness.
4. Try mediation. Mediation is the practice of being in the here and now, which is something everyone struggles with from time to time, and if you have COPD or another chronic illness it is even harder to be present. It is very possible that you are thinking about your next doctor's visit, or how you once love to do something that you are incapable of doing now that you are sick. Thinking about the past and future can cultivate a negative headspace. Mediation helps bring you back to this moment, so you can start to focus on your life right in front of you rather than the past and future moments that are out of your control.
5. Treat yourself. Understanding that you are in a difficult position and giving yourself credit for going through the trials and tribulations of your disease is a useful way to promote a little bit of happiness in your life here and there. Think about what brings you joy whether it is scoop of ice cream or a new pair of shoes, and go out and get it!! Remember that these little gifts to yourself are sometimes a form of instant gratification, and the happiness you gain from these types of endeavors can be fleeting, but every so often we all need a little pick me up!
Happiness is Being Empathic

Empathy is an interesting thing, and often confused with sympathy. As a person with COPD, it is easy to forget that the people around you are going through their own challenges, and as small as those hardships may seem to you compared to what you are going through, people’s challenges are relative to them and their experiences.
If you can find the energy to be empathic to a loved one in your life, you will gain a sense of understanding and more importantly perspective.
Perspective is the lens in which we see and react to certain situations, the broader and more complex your perspective is the more in control of your emotional state you will be. This means that by taking a step back from the issue or circumstance in front of you you will be able to see the bigger picture and deal with the issue reasonably rather than being intimidated and stressed out by your situation.

Empathy helps you broaden your perspective by connecting with other people on a level deep enough where you understand that everyone has hardships and while you are suffering and COPD is a very invasive disease, you have the ability to get stronger and deal with your disease and life in general.
Overview
COPD patients have to be some of the strongest and most willful people on the planet. They are constantly struggling to breathe and experiencing other symptoms on top of that daily. The mental and physical exhaustion is something that a healthy person would ever understand. Yet, here you are, alive!
Happiness is attainable, and as hard as it may seem, if you can find happiness in the simple things if you are able to change your perspective and focus on more positive things. You can also do a lot for your well-being by getting oxygen equipment that promotes a healthy lifestyle. Lastly, being diligent and treating your COPD can make a huge difference not only for your physical wellbeing but your mental state of mind!


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













