Chronic obstructive pulmonary disease (COPD) is one of the most common lung diseases in the world. It’s estimated that about 16.4 million people in the United States alone have COPD and millions more are either undiagnosed or at high risk of contracting it. Despite this fact, many people are woefully unaware of what causes this disease and how it should best be managed.
In short, COPD is an umbrella term that denotes two conditions: chronic bronchitis and emphysema. While the symptoms and pathogenesis of these two diseases are slightly different, they are both primarily caused by cigarette smoking. However, in rare instances, someone who has never smoked can contract COPD through something called alpha-1 antitrypsin deficiency (AAT deficiency).
One of the symptoms of COPD that’s particularly vicious is something called an exacerbation. This is similar to an asthma attack in that it causes respiratory symptoms such as breathlessness, chest pain, and sputum production to suddenly become worse, oftentimes requiring you to seek immediate medical attention. In this post, we will help you better understand COPD flare-ups and exacerbations, as well as how to avoid being hospitalized as a result.
If you have any questions or concerns, feel free to leave them in the comment section so we can address them.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What’s the Difference Between a Flare-Up and an Exacerbation?
Generally speaking, the terms “COPD flare-up” and “COPD exacerbation” are used interchangeably. They both refer to respiratory symptoms becoming worse due to environmental causes, infections, or any number of other things. However, when it comes to discussing these symptoms, it’s important to be precise not only about what’s causing them but how severe they are as well.

A mild COPD exacerbation is one that could lead to increased discomfort but is unlikely to cause any serious long-term consequences. These can typically be treated with short-acting bronchodilators (SABD) or “rescue inhalers” which work to quickly open up the airways allowing you to breathe better. Moderate COPD exacerbations should be supplemented with oral corticosteroids which suppress inflammation and antibiotics which can help fight inflammation.

The final type of exacerbation is a severe exacerbation, sometimes called an “acute” exacerbation. This type of exacerbation requires immediate medical attention and can even be life-threatening if it’s not treated appropriately. Ideally, the best way to prepare for this type of exacerbation is to have an action plan and ensure you always have someone on hand to either take you to the hospital or call an ambulance.
Why it’s so Important to Avoid Hospitalization With COPD
According to the American Journal of Respiratory and Critical Care Medicine, COPD is responsible for $72 billion a year in direct healthcare expenditures. The majority of these costs come from hospital visits which range from 4.5 to 8.8 days on average. Around two-thirds of all COPD hospitalizations are due to COPD exacerbations, and the majority of COPD exacerbations are caused by infections — specifically viral infections.

The primary reason it’s important to avoid hospitalization for COPD is because of the risks for your health. According to another study by the aforementioned medical journal, after testing over 2 million patients, the 1-year readmission rate was 64.2% and the 1-year mortality rate was 26.2% both of which were significantly higher than rates among the general COPD population. Readmission and mortality rates are also much higher among patients who were hospitalized with severe exacerbation of COPD.
The second most important reason to avoid hospitalization due to COPD is cost. Frequent or long-term admissions can pose a significant financial burden on people with COPD which can also lead to stress, anxiety, and even depression. In our last post, we highlighted some key ways that you can avoid unnecessary financial costs due to COPD so check it out if you’re interested in learning more.
Have a Plan to Deal With Exacerbations
First and foremost, if you want to avoid hospitalization due to COPD exacerbation, you need to have a plan of action before an emergency occurs. An action plan is a sort of written outline that you will follow in order to accomplish a certain goal. This way, if you notice your COPD symptoms starting to worsen, you can refer to your sheet instead of worrying about making difficult decisions at the moment.

In order to prepare your COPD action plan, you should first consult your doctor. He/she will likely already have a template that you can fill out to make this process a little easier. On this action plan, you will need to create an “action” for every symptom you experience. For example, if the symptom is a gradual decrease in your blood oxygen levels, you might make a note to increase your oxygen flow setting or contact your doctor. If you experience sudden shortness of breath, you might make a note to use your rescue inhaler.
Another important thing to know about your COPD action plan is that it should not be private information. You should make it a priority to go over your plan with friends and family, especially if they spend a lot of time with you. This way, if you are in a situation where you are unable to act out your action plan, they will be able to help. In this post, we discuss how you can prepare for medical emergencies and hospital visits with COPD, so check it out if you want to know more.
![]()
Change Up Your Diet
Diet can be a very difficult topic to discuss in this day and age. Most people have access to more types of food than ever before and there is a near endless list of diets that people swear by. As a result, it can feel like an insurmountable task trying to find something that keeps you happy and healthy. The good news, however, is that many years of research have been dedicated to COPD diets, so you shouldn’t have to do much scrambling to make sense of it all.
![]()
Generally speaking, COPD patients should maintain a diet that’s high in protein, fiber, and fat, but low in carbohydrates. The reason for this is that the metabolism of carbs produces the highest amount of carbon dioxide in the body while the metabolism of fat produces the least. Adequate protein ensures your respiratory muscles stay strong and efficient, and fiber helps to control blood glucose levels and reduce cholesterol in the blood.
Another reason to keep your diet healthy, natural foods rather than processed ones is because weight management is vital to COPD management. Most often, people tend to become underweight after contracting COPD due to a loss of appetite or other factors. Sometimes, people experience a loss of appetite because consuming food is more physically exerting than it was previously, and bloating can contribute to breathing difficulties. COPD patients who are underweight may find that they lack the energy or endurance to make it through the day.
On the other hand, being overweight with COPD can contribute to breathing problems as well. While it is less common for a COPD patient to become overweight than underweight, the problems associated with it can be just as severe. Simply put, having a higher body mass index (BMI) can be obstructive to your breathing by putting more strain on your lungs when you inhale. However, some studies have found mixed results when it comes to being overweight/obese with COPD.
Be Consistent With Your Exercise Routine
Consistency is unbelievably important when it comes to treating COPD and preventing exacerbations. For example, your diet is much more likely to benefit you if you keep up with your goals week in and week out. But if you do well one week then cheat the next, you’re going to put yourself at a much higher risk of COPD complications like exacerbations. This works pretty much the same way when it comes to your exercise routine.

Oftentimes, exercise specialists will talk about getting into a “routine.” In other words, you do the same exercise each day for an allotted period of time. By doing so, it will be much easier to track your progress and catch yourself when you fall back on your plan. This works well for most people who want to commit to an exercise routine, but it’s especially useful for COPD patients who benefit more from consistent moderate exercise rather than high-intensity exercise.
Avoid Getting Sick
Lung infection is both the number one cause of severe COPD exacerbation and the number one cause of hospitalization due to COPD. With that being said, staying healthy and avoiding infection (especially lung infections) is vital. One of the best things you can do right now to avoid getting sick is to quit smoking or avoid second-hand smoke if you live around smokers.
It’s been known for quite some time that smoking reduces the immune response in the body and also makes the smoker more likely to have exaggerated responses to viral infections. During influenza outbreaks and with the current situation we face involving COVID-19, smokers have a much lower survival rate when compared to the general population. Not to mention that smoking and second-hand smoke can trigger COPD exacerbations even if an infection isn’t present.

Another thing you can do to avoid getting sick is to be more conscious of your daily habits. For example, do you wash your hands frequently throughout the day? Do you take care to avoid places that are unclean or unsanitary? Do you stay away from people who exhibit symptoms of the cold or the flu? Do you clean surfaces in your home like door handles, coffee pot handles, or faucet handles? Are you following all the precautions recommended by the World Health Organization (WHO) in order to prevent contracting the novel coronavirus?
Last but certainly not least, you should be getting the doctor-recommended eight hours of sleep each night in order to avoid getting sick. According to WebMD, sleep deprivation suppresses the immune system and puts you at a higher risk of contracting colds, the flu, and other ailments. This is an especially difficult topic for many COPD patients because respiratory symptoms can make it difficult to maintain a healthy sleep schedule. In this post, we take a look at some actionable tips to improve your sleep if you have COPD.
Avoid Environmental Triggers
It can be a scary world out there for anyone who values their lung health. From wildfire smoke to car exhaust and pollen, it’s easy to feel like no place is safe. The Environmental Protection Agency (EPA) even reports that indoor air can be two to five times more polluted than outdoor air. Fortunately, it’s not all grim news for COPD patients who want to avoid exacerbation triggers. Just by following a few simple steps, you’ll be well on your way to avoiding the most common triggers.

Despite summer ending last week, we are still in the midst of wildfire season. As a result, COPD patients need to be aware of when they go outside, especially when it concerns exercising outdoors. Air quality index (AQI) is the measurement we use to determine how safe outdoor air is to breathe. Each day before you go outside, be sure to check AirNow.gov for the AQI in your area. If the AQI is above 100, this is a sign that the air quality is too poor for people with lung diseases like COPD, asthma, or pulmonary fibrosis.
Another thing you should be wary of is seasonal allergies. Contrary to popular belief, allergies are a reality during all times of the year as opposed to only being active during certain seasons. In September and October, allergens like ragweed are typically at their peak. According to WebMD, if you get allergies in the spring, you are about 75% likely to have reactions to ragweed. So, if you’re outside this trying to enjoy the fall colors and cool weather this year, just be aware that allergies are still a reality.

The final airborne COPD exacerbation triggers we’d like to talk about are the ones found in your home. Like we mentioned earlier, indoor air can potentially be more dangerous than outdoor air. This is because the air in your home is extremely concentrated, so if you track things in like dust, allergens, or smoke, it will likely start to build up in one area of your home unless you take the time to clean regularly. While it may not seem that important, taking the time to vacuum, dust, and wipe down surfaces every day can go a long way to preventing COPD exacerbations. What’s more, it will help you get your daily exercise.
Use a Reliable Portable Oxygen Machine
Last but certainly not least, having a reliable portable oxygen device that you can take anywhere will put you in the best position to avoid COPD exacerbations and hospitalization. For the vast majority of COPD patients, supplemental oxygen therapy is a medical necessity. Not only does it stabilize your lung condition, but it also ensures your blood oxygen levels are normal, which in turn saturates every organ in your body with the oxygen it needs to function properly.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
For the foreseeable future, portable oxygen concentrators are your best bet for reliable portable oxygen. Unlike oxygen tanks or liquid oxygen tanks, portable oxygen concentrators are electronic devices. So, instead of having to go out of your way constantly to have your tanks refilled by an oxygen specialist, you simply need to carry batteries with you. Fortunately, these batteries are lightweight and don’t take up very much space in your backpack or handbag.

Currently, the best portable oxygen concentrator on the market is the Caire FreeStyle Comfort. It weighs in at only 5 pounds and it offers 5 different flow settings that you can adjust on the fly as needed. One of the unique features of the FreeStyle Comfort is its ergonomic design which keeps the device comfortably at your side rather than jostling around as some other concentrators do.

Another portable oxygen concentrator we’d like to recommend is the Inogen One G5. While this POC came out last year, it’s still very relevant and a great choice for anyone who needs a reliable 24/7 medical oxygen supply. The Inogen One G5 has one more pulse flow setting than the FreeStyle Comfort and it weighs slightly less at just 4.7 pounds. Inogen is one of the top brands in the medical oxygen industry and they take pride in customer satisfaction.
In rare instances, your doctor may require you to use a continuous flow concentrator. If this is the case, we recommend the Respironics SimplyGo portable oxygen concentrator. This unit is twice as heavy as the Caire FreeStyle Comfort, but since it puts out a continuous flow of oxygen, it can be used with your CPAP or BiPAP machine if you have sleep apnea or another related sleeping disorder. If you’re looking for affordable portable oxygen concentrators, don’t hesitate to visit our online oxygen store.

Conclusion
Unfortunately, exacerbations and flare-ups are a reality for COPD patients. But that doesn’t mean that you can’t take steps to reduce your risk of experiencing hospitalization due to an exacerbation. Above all, following your treatment plan as closely as possible and preventing sickness like the cold or flu will be your best bet if you want to avoid hospital visits.
If you would like to learn more about managing chronic respiratory conditions such as COPD, stay tuned to our blog. We aim to equip our readers with the knowledge they need to combat breathlessness, chest pain, and fatigue in their daily lives, as well as learning how to cope with the mental aspects of chronic disease like anxiety and depression. Feel free to leave a comment below if you have any questions or concerns.
So, you recently found out you have COPD and you're not sure what to do. You might be feeling scared, lost, overwhelmed, or anxious about what will come next.
First of all, take a deep breath and remind yourself that you will be okay. COPD is a serious disease, but it doesn't mean your life as you know it is over. Many people go on to live many long, happy years after getting diagnosed with COPD.
Even though the news can come as a shock, it's important not to not panic or get too discouraged about your diagnosis. COPD is treatable, even if it's not curable, and the next steps you take can have a major impact on your disease and how quickly your symptoms get worse.
One of the worst things you can do is get stuck in the trap of dwelling on what-ifs and feeling hopeless about things you can't change. Instead, you should do your best to focus on what you can change in order to keep yourself healthy and live the longest, best life possible in spite of your disease.
That's why we created this guide to help you figure out what to do after you've been diagnosed with COPD. In the sections below, we'll walk you through 11 vital steps you can take right away to preserve your health and take charge of your disease.
Learning how to manage COPD is a complicated journey, and it helps to have a roadmap to point you in the right direction. Luckily, there are plenty of resources to help you get started, including the one you're reading now, and you will find links to many more all throughout this guide.

The Next Steps: What to Do After Your COPD Diagnosis
Stop Smoking!

Don't make the common mistake of believing that it's not a big deal to keep smoking just because you already have COPD. The truth is, continuing to smoke after your COPD diagnosis is extremely dangerous; it can shorten your lifespan, make your symptoms more severe, and make your quality of life significantly worse.
One of the major effects of COPD is that it makes your lungs extra vulnerable to inflammation. Anything you breathe that irritates your lungs, including dust, allergens, and smoke, can make your symptoms worse for hours or even days at a time.
Even worse, inflammation can lead to permanent lung damage and accelerated loss of your remaining lung function. It can also make you more likely to have a COPD exacerbation, which is a prolonged episode of worsened respiratory symptoms that requires special treatment—and sometimes even hospitalization—to cure.
But studies show that if you quit smoking, it can reduce your COPD symptoms, make it easier to breathe, and reduce your risk for other health complications. It can even improve the overall function of your heart and lungs, reducing shortness of breath and making it easier to do physical activities.
Most importantly, research suggests that quitting smoking is the most effective thing you can do to slow down the progression of COPD. It can help you live longer, live better, and suffer from less severe symptoms over the course of your disease.
Of course, stopping smoking is almost never an easy thing to do. Many people need help quitting, which is why there are a wide variety of smoking cessation resources available to assist you if you need them.

U. S. Air Force photo by Beverly Joyner
Don't be discouraged if you've tried and failed before; most smokers make many quit attempts before it finally sticks. You might be more likely to succeed if you use one or more quit smoking medications, such as nicotine replacement patches or pills.
Other helpful resources include quit smoking counseling (which is generally free with medicare), quit smoking hotlines, and online smoking cessation programs. The first step is deciding that you want to make the firm commitment to quit, and then you can set up a plan including a quit date and a strategy for gathering the support, medication, and any other tools you need to help you succeed.
Learn Anything and Everything You Can About COPD
In order to manage your COPD effectively, you need to understand your disease and what it takes to minimize further damage to your lungs. The more you know, the better you can manage your symptoms, make healthy choices, and maintain your quality of life.
That's why it's important to learn everything you can about COPD and how to live responsibly with the disease. That includes learning how COPD affects your body, how it progresses over time, and the myriad ways you can improve the health of your heart and lungs. COPD oxygen therapy treatment is one of the best ways to reduce symptoms regardless of whether you have mild or severe COPD.
There are many online resources you can use to research COPD and learn practical strategies for managing the disease. We have a variety of helpful guides on our Respiratory Resource Center blog to help you get started, all of which include numerous links to helpful information from doctors, researchers, and other COPD experts.
https://blog.lptmedical.com/
You can start with following guides which cover a variety of vital COPD topics:
- Learn About the 4 Stages of COPD
- 15 Tips for Reducing Your Risk for COPD Exacerbations
- How to Prevent COPD-Related Heart Attacks
- How COPD Affects Your Immune System
- The Importance of Following Your COPD Action Plan
- How to Avoid Common Mistakes New COPD Patients Make
COPD-Proof Your Environment
One of the first things you should learn about COPD is that many common chemicals, microbes, and airborne particles can worsen your COPD. That includes common household allergens like pollen, dust, and mold, as well as other respiratory irritants like fragrances and smoke.
In order to minimize your symptoms and keep your COPD under control, it's important to minimize your exposure to these and other respiratory hazards. That means avoiding air pollution both outside and inside, but especially within your own home.
Indoor air quality is important, and one of your immediate priorities should be to create a lung-friendly climate inside your house. There are many ways to do this, including eliminating sources of air pollution and maintaining ideal temperature and humidity conditions indoors.
The first step is to deep clean your house to remove dust, mold, and other contaminants that can make it more difficult to breathe. This can make a noticeable difference in your daily symptoms and make your COPD easier to manage at home.
Next, you may need to make some changes to household habits and routines. You can reduce the amount of hazardous VOC's you breathe in, for example, by taking care to set up proper ventilation anytime you cook or clean.
It's especially important to eliminate any sources of smoke in your house, including cigarettes, incense, and wood-burning fireplaces. You should also avoid certain common household products, including many commercial cleaning chemicals and aerosol sprays, that can irritate your lungs and contribute to indoor air pollution.
On days when your local air quality is poor, you can shield your home from outdoor air pollution by keeping your doors and windows closed. You can also optimize your indoor air purity by using high-quality air filters, humidifiers, or electric air purifying appliances (such as a certified HEPA filtration system).
Check out the following guides to learn more about how to COPD-proof your home:
- How to deep clean your house to reduce COPD symtpoms
- Practical tips for improving your indoor air quality
- How to reduce your exposure to noxious cleaning products (and find lung-safe alternatives)
Learn COPD Breathing Techniques
One of the earliest and most prevalent symptoms of COPD is shortness of breath, which often appears during exercise and other physical activities. This tends to get worse with time, and it can seriously interfere with your ability to do daily activities and live an active, healthy life.
Fortunately, there are many strategies you can use to reduce shortness of breath; in fact, that is one of the major goals of COPD treatment. One of these strategies is practicing deep breathing techniques, which is proven to be an effective short-term solution to breathlessness.
Unlike many other COPD treatments, breathing exercises are simple, immediate, and they're available for you to use anytime and anywhere. Breathing techniques also teach you how to be aware of your breathing and control your breaths in beneficial ways.
Because of this, breathing exercises are an early skill that every person with COPD should learn soon after diagnosis. It works as a first-line solution to breathlessness that is effective in a wide range of different situations, including when you walk, exercise, or exert yourself in any way.
Even if you have mild COPD and don't experience breathlessness often yet, learning to control your breathing is still an important skill. The more you practice now, the easier and more natural it will feel to use these techniques as your disease progresses and it becomes more difficult to breathe.
Learn COPD Airway Clearance Techniques

Just like breathing techniques, airway clearance techniques are basic, vital skills for every COPD patient. Their purpose is to get rid of excess mucus that builds up in and blocks your airways as a result of your COPD.
Simply put, airway clearance techniques are exercises you can do to deliberately move mucus up and out of your lungs and airways. Once the mucus reaches your upper airways and mouth, you simply cough or spit it out to remove it from your respiratory tract completely.
While this might sound gross at first, this is exactly what happens anytime you have a wet cough, which often happens during minor respiratory infections like the flu. Unfortunately, people with COPD tend to produce lots of extra mucus all the time, where it blocks airflow through their airways and makes it more difficult to breathe.
Fortunately, airway clearance techniques can help you manage this problem and minimize its effect on your life. You can use include tool-assisted strategies as well as simpler techniques as-needed throughout the day.
Techniques like controlled coughing, positional drainage, and strategic tapping on the chest and back can all help you get rid of stubborn mucus at home. If you work with your doctor, you may also get to use specialized mucus-clearing tools and equipment, such as vibrating chest vests (high-frequency chest wall oscillation) and medical lung flutes.
Many people with COPD experience reduced respiratory symptoms when they use airway clearance techniques regularly. They can reduce shortness of breath, prevent coughing fits, and minimize the amount of wheezing when you breathe.
To learn more about airway clearance techniques, including methods you can use at home, check out our guide on the topic here.
Get Your Flu & Pneumonia Vaccinations
Vaccinations are important for everybody, but they are especially important for people with COPD and other chronic diseases. It is very dangerous to get sick when you have COPD because it can cause severe COPD exacerbations and other complications.
COPD actually depresses your immune system, making you more likely to get sick with infectious illnesses like the flu. It also makes your lungs more prone to infection and inflammation, so that even a minor illness can lead to life-threatening breathing problems in people with advanced COPD.
Now that you've been diagnosed with COPD, you can't take the risk of leaving your immune system unprotected. Avoiding illnesses and exacerbations is a key part of managing your disease, especially since exacerbations can cause irreversible lung damage and permanent lung function loss.
Because of this, getting vaccinated for the flu—and possibly pneumonia—is usually one of the first recommendations doctors give to someone recently diagnosed with COPD. In general, all adults aged 65 or older, or who have a chronic disease, should get the pneumonia vaccine; however, your doctor can tell you if you need it for sure.
The flu vaccine is particularly important, because influenza is a serious respiratory illness that kills up to 79,000 people every year and causes even more hospitalizations. In people with COPD, the flu can cause severe COPD exacerbations, and frequently leads to secondary lung infections like pneumonia.
While the pneumonia vaccine is a one-time thing, you will need to get a new flu vaccine every year to stay protected. Don't take this duty lightly; after all, it may only take one serious illness to make your COPD symptoms worse forever.
Even minor exacerbations can affect your ability to breathe and do daily activities for weeks, and it can take even longer to get back to baseline after a serious one. If you have severe COPD, exacerbations put you at risk for hospitalization, respiratory failure, and possibly even death.
Learn How to Manage Your New Medications
After your COPD diagnosis, your doctor will likely put you on a strict medication regimen. You are likely to receive, at the very least, a maintenance inhaler to use every day and a quick-relief inhaler to use as-needed when you find it difficult to breathe.
If your COPD is more severe, you will likely have a variety of additional medications to keep track of. This might be difficult to get used to at first, especially when some medications are regular, some are as-needed, and some you only use during a COPD exacerbation.
However, it's vital that you understand each medication as well as exactly how you're supposed to use it. If you haven't received one already, ask your doctor to give you a detailed COPD action plan, which will serve as a vital resource for you as you learn to manage your disease.
Your COPD action plan should detail each of your medications and the conditions for their use. It should explain when to take each medication, how much you're supposed to take, and if any other factors—such as bad symptom flare-ups—change how you should use it.
Once you fully understand your medications, it's important to set up a schedule and a routine to help you take them consistently and correctly. You can use whatever methods are available to keep yourself on track, such as sticky notes, phone reminders, or pill containers labeled with each day of the week.
Kickstart Healthy Daily Habits

When you're a healthy adult, it's all too easy to brush off the fact that you have a bad diet or have put on excess weight. However, these unhealthy habits become much too dangerous to ignore if you get diagnosed with COPD.
COPD patients who live an unhealthy lifestyle have worse symptoms and a much worse quality of life. This is especially true for people who have bad eating habits, don't get enough exercise, or have an unhealthy BMI.
Unfortunately, COPD symptoms like breathlessness, depression, and fatigue can make it difficult to stay healthy. However, it's important to work through these problems so that you can work out, stay active, and cook healthy, balanced meals.
It's okay if you need help; there are many diet, nutrition, and exercise specialists out there who can show you how to get on track. It's also good to start small, with simple steps and modest goals to help you move forward without feeling overwhelmed or burnt out.
Major lifestyle changes don't happen overnight, but it's important to get started as early as possible. The longer you wait to improve your habits, the worse your COPD symptoms will become, and the harder it will be to change.
However, making improvements in your diet and exercise can go a long way towards improving your COPD symptoms and your overall quality of life. It can even improve your ability to breathe and slow the rate of lung function decline over time.
If you're not sure whether or not your lifestyle needs to change, talk to your doctor about your current habits related to diet, exercise, and health. He can help you spot any unhealthy behaviors and give you pointers for how to improve.
To learn more, check out our following guides about COPD-healthy exercise and nutrition:
- Tips for Exercising at Home with COPD
- Learn which Foods You Should Eat and which Foods You Shouldn't Eat if you have COPD
- How to Reduce COPD-Related Fatigue
Ask Questions and Work With Your Doctor

Living with COPD is no simple matter, and you're bound to have a lot of questions after getting diagnosed. When you do, don't be afraid to talk to your doctor and ask him to explain anything you don't understand.
Asking questions is a good thing; it shows you want to be involved in your treatment and learn how to manage your COPD. Your doctors are some of the best resources you have, so don't be afraid to ask for—or even insist on—answers to any questions that come up.
Working with your doctor should be an two-sided dialogue, and you should feel comfortable asking your doctor to provide you with explanations and clarifications. That's why it's important to work with a doctor you get along with and who you can trust to keep you informed.
If you're not quite sure how to open up a dialogue, take some time to think about any questions or concerns you have about your health and your disease. Write down everything that comes to mind, including any topics you and your doctor have already discussed that have you worried, confused, or unsure.
This exercise will expose gaps in your knowledge and help you figure out what you need to know. Then, the next time you talk to your doctor, bring this list of questions and concerns with you so you don't leave anything out.
If you need some ideas to get started, check out our guide with 16 questions you should ask your doctor about your COPD.
Get Support and Assistance from Family and Friends
Nobody should have to cope with a COPD diagnosis all on their own. As soon as you've processed the news and feel ready to discuss it, you should consider telling your family and friends about your disease.
The reasons for doing so are two-fold: First of all, the emotional support you get from the people who love you can be a huge relief and allow you to cope with your diagnosis in a healthier way. Second, it gives your family and friends the chance to offer physical and practical support, which you may need as you go through treatment.
For example, you could ask your loved ones to help you make the lifestyle changes needed to keep yourself healthy for as long as possible. You may also need to ask them for help with daily tasks, like cooking, cleaning, and making it to doctor's appointments in the more severe stages of COPD.
In many cases, friends and family members are more than happy to do what they can, even if it's just little things here and there. Having someone to help you go shopping, pick up your medications, or simply call to check up on you when you're not feeling well can make life just a little easier to manage when you're living with COPD.
Take the Time to Look After Your Mental Health
Oxygen therapy has evolved to the point where the oxygen user should not only be getting the oxygen they need to breathe, but the freedom and independence to do more activities, travel, and find happiness in everyday comforts. The demand for oxygen to be user friendly, portable, and noninvasive is hugely due to the fact that every year, about 1.5 million patients in the United States utilize long term oxygen therapy.
However, not every oxygen device can give patients the freedom they deserve. In fact, many oxygen devices tether its user to their home, making travel impossible and exercise unbearable. We are lucky enough to live in an age of innovation and growth, oxygen therapy is no exception. The technology that is used to design and manufacture modern oxygen devices has improved drastically and has come a long way from the heavy and bulky oxygen reservoirs used in the past.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Shopping for oxygen
It is important to note, that with the growth and demand for new forms of oxygen technology, came a lot of cheaply made replicas and non-licensed distributors selling malfunctioning oxygen machines. It is important for people shopping for oxygen therapy devices to speak with their doctors and find the most trusted oxygen brands and suppliers that they can work with.
If you are looking into buying your first or a new oxygen device, it is not only important to do your research, but you also should not go with the cheapest option you find on Google. Your oxygen device is going to be your trusty companion all day and all night for the rest of your life, so making sure you get the right device for your oxygen needs that also fits into your lifestyle is essential for your wellbeing.
In this article we talk about a number of aspects surrounding oxygen therapy:
- We look at the evolution of oxygen
- Understanding flow rates
- We will go over your oxygen therapy options
- We will give you a list of the most trusted names in oxygen manufacturing companies
- We will discuss our best selling portable oxygen concentrators
- How to make the most of your oxygen therapy
Evolution of Oxygen Devices

Long term oxygen therapy (LTOT) is prescribed to patients with chronic obstructive pulmonary disease (COPD) and other chronic lung diseases. LTOT increases survival and improves the quality of life of users with hypoxia, it can be very dangerous if used incorrectly, which is why oxygen is prescribed to patients by their doctors after taking a series of pulmonary function tests.
In the beginning, pressurized cylinders were the only available option for long term oxygen therapy. Then in 1965, the first home based liquid oxygen system was invented which gave the oxygen user both an immobile and portable oxygen system. This presented a great advantage, where the oxygen user finally had the ability to refill their portable liquid oxygen system and their smaller portable system whenever needed.
In 1973 home oxygen concentrators became readily available, these devices operated by filtering nitrogen from the air and producing medical grade oxygen. Oxygen concentrators provided an unlimited supply of oxygen, and it ran off of electricity. While this oxygen system was safe and efficient it was stationary, and tethered its users to their home where there was electricity.
Today, there are combinations of oxygen devices:
- Compressed gas canisters
- Liquid oxygen tanks
- Concentrators
- Liquid oxygen portable canisters
- Battery operated portable oxygen concentrator

Every home oxygen system has a different performance characteristic, with its own set of capabilities and applications. Your doctor should be aware of product variability in performance when identifying specific systems that would work for you.
Your Oxygen Therapy Options
There are so many home oxygen therapy options to choose from that to the point where it is notoriously difficult to know what equipment is right for you, what is available and the capabilities and drawbacks of each device.

So while your doctor will typically prescribe you a flow rate and frequency for home oxygen therapy based on the results of your pulmonary function, the oxygen provider is expected to supply the necessary equipment based on your prescription and recommendations from your doctor. Therefore, it should be evident that it is important to work with the most trustworthy oxygen providers that supply the most trusted names in oxygen manufacturing.
Flow rates
At one point in time, there were only continuous flow oxygen devices, until intermittent-flow devices were introduced in 1983. The continuous flow devices distribute the oxygen at a consistent rate, even while you exhale. Intermitted-flow devices were created to conserve the oxygen that is wasted while exhaling. Intermittent-flow devices only admit oxygen when the user inhales, and it will pause during the exhale.
Both continuous flow devices and intermittent-flow also known as pulse flow devices, are still used today and the flow rate you use will depend on your oxygen requirements that will be established by your doctor. From there it will be the responsibility of your oxygen supplier to adhere to your oxygen requirements and match you with a device that will meet these needs.
There are three main forms of home oxygen therapy that offer both continuous and pulse flow operations listed in the following sections.
Oxygen gas
.jpg)
Oxygen gas can be stored in a portable tank also known as compressed gas systems. You would use a larger stationary concentrator while you are at home, and you would have a smaller oxygen tank that can be taken with you outside the home.
The portable oxygen tanks are very small and only deliver oxygen in pulses, not continuously in order to save oxygen, so you will not run out. This is of course not an option for everyone, because many people do need the continuous flow of oxygen in order to reap the benefits of oxygen therapy.
Liquid oxygen
Liquid oxygen can be stored in a portable tank, but the difference between the gas and liquid oxygen is how the liquid form is more highly concentrated, and more oxygen can fit in a smaller tank. Active people would prefer this method because it is much more portable, but it will still need to be refilled often.
Most people with liquid oxygen and oxygen gas systems are able to get their oxygen delivered to their home, and this will depend on your location.
Portable oxygen concentrators

Portable oxygen concentrators are the most portable option. An oxygen concentrator is a device that takes oxygen from the room, filters out impurities, and concentrates the air into medical-grade oxygen. The most obvious advantages of portable oxygen concentrators is that they are less expensive and don’t require refilling.
So while there are only 3 main forms of oxygen therapy, the diversification between each method is vast, and you may want to read more about the comparison between oxygen device systems, you can do so by clicking here to read Oxygen Concentrators vs. Oxygen Tanks: A Simple Comparison Guide.
A lot like buying a car, the next step, is deciding which brand of POC you will choose and then deciding on the model you want, luckily your choice are limited by your oxygen prescription, but for most people they will have more than one option, and picking the right device can be overwhelming.
Here are a few of the most trusted names in oxygen manufacturing.
Oxygen Manufacturing Companies
Of all of the oxygen manufacturers out there there are a few that continuously outperform their competitors, bringing oxygen users the most efficient, cost effective, overall best oxygen equipment to the market every year, for more reasons than one.
- Inogen
- ResMed
- Philips Respironics
- Drive Medical
At LPT Medical, quality is the only option. Which is why, LPT Medical offers products from all of the most reputable manufacturers in the industry. These are the companies that are pushing the boundaries of what’s possible for patients suffering with a debilitating respiratory condition. And by offering these brands, we ensure that more people around the country have access to the most state-of-the-art oxygen therapy equipment in the world.

Best Selling Portable Oxygen Concentrators
The make and model of your device will be narrowed down based on your oxygen requirements. From there, one of our knowledgeable respiratory specialists at LPT Medical reviews your needs and matches you with a variety of devices that vary in weight, battery life, and other factors. Our customers have reviews our specialists ability to pick out the best device, and we are thrilled with our performance.
Our selective and integrated process working with every customer on a personal level has given us worldwide recognition as one of the most trusted names in the world of oxygen therapy products offering home oxygen concentrators, portable oxygen concentrators, CPAP and BiPAP machines, and all the accessories you need to make the most of them.
That being said, we know which devices work for many people and for those who do qualify for the following portable oxygen concentrators, are always our happiest customers!
Inogen One G5 and the Inogen One G3
The Inogen One G5 portable oxygen concentrator in the best selling pulse flow oxygen device there is because it meets mostly every oxygen patient’s needs. It is powerful enough to cover a user’s oxygen prescription, by going up to a level 6 which is 1260 ml or oxygen per minute.
The battery life of the Inogen One G5 is unbeatable, the Inogen One G5 Double Battery provides the same reliability as the G5 Single Battery but adds up to 13 hours of additional battery life on a single charge.

So this device can go with you anywhere, and last for hours, but it is also very lightweight. You can carry the One G5 with you in the One G5 backpack or the custom carrying case, but with either method you will barely notice the 4.7 pounds.
The Inogen One G3 goes up to a level 5 in pulse flow output, and weighs the same as the One G5. it is a great option for people who don’t mind having older generations that are still high quality and reliable. The One G3 is still rated the number one pulse flow oxygen concentrator because of its long-standing record and dependable results. Not to mention the carrying case is designed in a classic and sleek style, so it doesn't look like a medical device

The 8-cell battery that comes with the One G3 is very powerful, but you can also get the Inogen One G3 16-Cell Battery if you value that extra long lasting battery life.
The G3 is also one of the quietest portable oxygen concentrators available, but it also help you pay attention with audible alerts in case of a power outage, no breath detected alarms, and oxygen purity checks. If your oxygen level ever falls below required levels, the One G3 will let you know immediately.

Caire Freestyle Comfort
The Caire Freestyle Comfort portable oxygen concentrator has been compared to the Inogen One G5 in similar respects to its long lasting battery life and lightweight design. The Freestyle Comfort is even lighter than the One G5 but the battery doest last quite as long.
Similarly to the One G5 and One G3, the Freestyle comfort has two battery options, the Caire Freestyle small battery, and the Caire Freestyle large battery.

Respironics SimplyGo
The Respironics SimplyGo is the most lightweight portable oxygen concentrator that offers both pulse flow and continuous flow, making this device a hot commodity for people who switch between flow settings.
The long lasting battery life is another huge selling point because people can go longer without having to plug in their oxygen to the car or outlet. When the machine does need to be recharged it is as easy as changing your cell phone, and you can continue to use it as it charges.

Making the Most Out of Your Oxygen Device
In order to take advantage of all of our devices, including the ones not listed above, you can purchase extra batteries, external chargers, backpacks and carrying cases, and more. Oxygen accessories are designed to make using oxygen therapy easier and more comfortable, and you will quickly learn what aspects of oxygen therapy you want to make more comfortable.

For example, if you notice that the oxygen tubing is putting a lot of pressure on your ears, there are ear pads available to accommodate that pain.
If you notice that your battery is dying too quickly, you can upgrade to the larger battery for extended use.
Devices like the the Inogen one G3 have backpacks and rolling backpacks available, to make carrying the 5 pound device even easier, you can find those items by following the links below:
Inogen One G3 Rolling Backpack by Portablez
GO2 Carryall Inogen One G3 Carrying Bag
If you notice that your tubing tends to get tangled there are Tidy Tubs Oxygen Supply Tubs available to stop this from happening
Here are 4 other ways to take advantage of your oxygen concentrator

1. Consider buying additional oxygen concentrator batteries.
Having an additional oxygen concentrator battery is extremely important for people who enjoy spending extended time away from their home or car. An extra battery can be the difference between having to worry about leaving an event early versus living stress free knowing you have plenty of time with pure medical grade oxygen. This particularly applies to patients who do not get as much battery life, either due to their high-flow rate, or their device just doesn't have that long lasting battery that some do.
2. Keep your spare batteries fully charged and do not forget to rotate them.
Keeping an extra battery without a charge for extended periods of time can actually damage the battery. Oxygen users should always store spare batteries that are fully charged. this is not only better for the battery life overall, but keeping batteries fully charged and ready, allows you to switch batteries at any time without having to worry about damaging them or your POC. You should also rotate batteries if you have more than two and always switch to a fully charged battery.
Tip: If you aren't going to use your spare batteries, store them at a 50% charge to ensure you don't damage any battery cells.

3. Utilize the accessory bag that comes with the package
Most units will come with a custom carrying case, few do not. Theses accessory bag vary in size and color based on the type of concentrator you have has. The accessory bag is an excellent organizational tool that helps you arrange the unit accessories in one particular location without having trouble finding them or risk losing them. Accessory bags usually have padding, zipper or velcro, and easy access to keep the contents safe.
4. Utilize the DC Power Supply.
All POCs come with a DC power supply that can be plugged into the cigarette lighter of a car. Small pulse flow units are totally functional on the DC power supply, which means you can use your device on any flow rate settings, and recharge the battery at the same time. However, the constant flow units carry a few limitations when using the DC power supply. Generally, uninterrupted flow units will continue to work and charge on pulse flow settings 1-4 as well as continuous flow settings as much as 2 LPM.
Overview
Oxygen can be a life saving therapy if you are adhering to your oxygen prescription correctly. If you start to take advantage of you oxygen device, you can find even more independence and more freedom than you had before you needed oxygen. All this requires in knowledge and trust in the process that this life saving therapy, can make a huge difference in the quality of you life.
.png)
There are three main types of respiratory disease: airway diseases, lung tissue diseases, and circulatory diseases. The first type, airway diseases, affect the tubes called bronchioles, usually causing them to narrow, swell, or become filled with a slimy substance called mucus. Airway diseases include asthma, a specific type of chronic obstructive pulmonary disease (COPD) called chronic bronchitis, and bronchiectasis, a condition that results from recurrent lung infections.
The second type of respiratory disease, lung tissue disease, specifically affects the tissue within the lungs. Oftentimes, these diseases cause the lungs to become inflamed and lose their elasticity which is why they’re usually categorized as “restrictive” lung diseases because they prevent the lungs from expanding fully. Pulmonary fibrosis is one common type of lung tissue disease and it results from the formation of irreversible scar tissue in the lungs.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The final type of respiratory disease is lung circulation disease. This type is a little more complicated in that it affects the complex interactions between your lungs and the rest of your circulatory system. These diseases prevent the lungs from processing oxygen from the air you breathe and releasing carbon dioxide, resulting in an imbalance of gases in the body. As you can imagine, these diseases are closely linked with cardiovascular issues.
Believe it or not, COPD has elements of all three of these categories, so it’s more complicated than most people think. In the following sections, we’ll take a look at 7 interesting facts that you may not know about COPD. After reading this, we hope that you are more aware of the global burden of COPD and that you’ll feel inclined to share this information with friends and family members who may be at risk of contracting COPD.

It’s One of the Most Preventable Chronic Illnesses
When we say a disease is “preventable,” we mean that personal lifestyle choices most often cause the disease to take hold. For example, acute illnesses like the flu or the common cold can be prevented with vaccinations and proper hygiene. But when it comes to COPD, this is not quite so simple. According to lung.org, 85 to 90 percent of all COPD cases are caused by cigarette smoking, but there are also other risk factors at play such as environmental pollution and genetics which makes COPD a difficult disease to prevent.
![]()
When you compare COPD to some of the other leading preventable illnesses in the world, it’s not hard to see why COPD is so difficult to prevent. Heart disease, cancer, and diabetes are some of the most discussed diseases and more often than not, this results in a high level of funding while other prominent diseases like COPD are left behind. According to a survey published in ScienceDaily, 38 percent of people with COPD were unaware of the disease before being diagnosed. This often leads to people referring to COPD as a “silent disease,” because it can feel like patients don’t have much of a voice in the community at large.

Perhaps, one of the reasons that COPD has such a lack of awareness is because of how slowly the disease develops. Typically, COPD takes many decades to progress from its early stages to its later stages. This is in stark contrast to diseases like lung cancer which tend to come on more quickly. Unfortunately, this leads to people underestimating the risk of COPD and not taking it as seriously as it should be. Another thing that can overshadow COPD is the fact that lung cancer shares the same awareness month, November. Since lung cancer has more funding in the first place, many people overlook COPD funding and support.
COPD Cannot Be Reversed
COPD is what’s known as a “progressive disease.” What this means is that symptoms related to this respiratory condition get worse over time. While symptoms may subside after a flare-up or exacerbation, these events usually result in a permanent drop in lung function. This is in contrast to conditions like asthma which exhibits similar symptoms, but after experiencing an asthma attack, most people fully recover and don’t maintain any permanent damage to their lungs.
As a result, the most important thing you can do to prevent your disease from progressing, or at the very least, slow its progression is to avoid common COPD triggers. We discuss in detail in this post how you can avoid COPD exacerbations, but we’ll summarize the points here for your convenience. First and foremost, infections are the cause of around 51% of all COPD exacerbations, so preventing them should be your top priority.
When you were young and didn’t have any chronic conditions, you probably weren’t too concerned about the flu or the common cold. These are infections that our body has adapted immunity towards allowing us to fight them off quickly, with or without the use of medications. However, the older we get older, these seemingly harmless things become a lot more serious, especially for people with chronic respiratory illness. It’s estimated that bacterial infections are the cause of 40 to 50 percent of all COPD exacerbations and a significant portion of hospitalizations as well.

Another major cause of COPD flare-ups and exacerbation is air pollution. No matter where you are and what the time of year is, there is air pollution. And if you want to slow the progression of COPD, you should be careful to check the quality of air wherever you go. AirNow.gov is a great resource for anyone who wants an accurate and up-to-date description of the air quality in their area. It’s recommended that COPD patients avoid going outside if the AQI (air quality index) is over 100.
Smoking Cessation is Still Important
There’s a strong belief among many people who have been diagnosed with COPD that “the damage has been done” and that “smoking cessation won’t help.” However, this could not be farther from the truth. While there is no cure for COPD, smoking will most certainly make your symptoms worse. In fact, cigarettes are an immunosuppressant drug meaning they inhibit the body’s innate and adaptive immune system. This puts you at a higher risk of infection and hampers your body’s ability to heal.

According to reports from the Centers for Disease Control and Prevention (CDC), about 38 percent of Americans who have COPD are current smokers. This is pretty astonishing considering that smoking is entirely counterproductive to a COPD treatment plan. Unfortunately, everyone is different so there’s no set smoking cessation plan you should follow. Your best bet will be to speak with your doctor who can help you find something that will work for you.
![]()
Another thing that will help is being away from a household where people have smoked or currently smoke. Secondhand smoke can be equally as dangerous as smoking yourself and experts estimate that the harmful chemicals in cigarettes can linger in a room for as long as five hours. In other words, if you smell cigarettes, you’re probably inhaling harmful chemicals that could lead to a COPD exacerbation. If you live with someone who smokes, try asking them to do it outside.
Every Case of COPD is Different
While around 16 million Americans have COPD, every case is unique. COPD is an umbrella term that’s used to denote two different chronic illnesses: chronic bronchitis and emphysema. And while these conditions might exhibit similar symptoms such as a chronic cough, breathlessness, and fatigue, they’re very different in terms of their causes, risk factors, and prognosis. These conditions can also occur in different parts of the respiratory system and work in tandem with co-morbidities which further complicates treatment and outlook.

Emphysema is what many people think of as the “smoker’s disease.” It’s a condition that affects the alveoli, the tiny air sacs that scatter the lungs. These air sacs are responsible for the exchange of oxygen and carbon dioxide to and from the bloodstream, so they play a key role in our systemic health. In someone with emphysema, the alveoli begin to lose their shape and fill with fluid meaning the transfer of gases is less efficient.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
In many cases, doctors will prescribe supplemental oxygen therapy which can help reduce the burden on the lungs. But it’s important to understand exactly how much you should be receiving because too much oxygen can lead to oxygen toxicity. This can result in symptoms such as coughing, difficulty breathing, and in severe cases even death. Make sure you’re clear on when to use oxygen and how much to use and don’t assume that increasing your oxygen intake will help you feel better.
The treatment options for emphysema also vary based on where the emphysema is located. For example, if the emphysema is located in one specific area of the lung, you may be a candidate for lung volume reduction surgery. This is a procedure that involves removing the damaged tissue in the lungs which prevents air from getting trapped and causing difficulty breathing. While it may sound counterintuitive to remove part of your lungs in order to help you breathe better, sometimes the benefits outweigh the negatives.
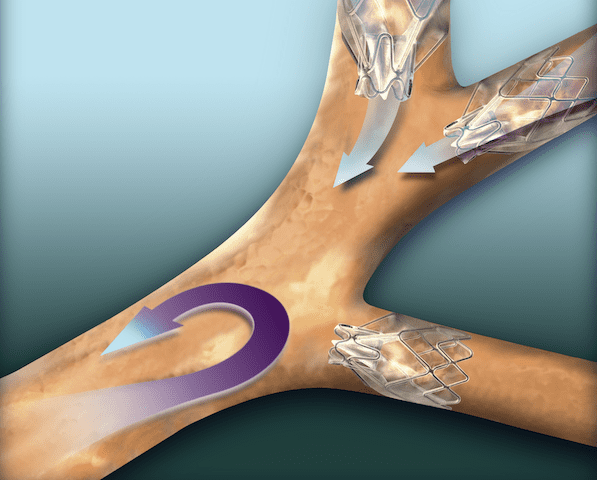
In other cases, emphysema patients may be a candidate for something called endobronchial valves. This is a less intrusive alternative to lung volume reduction surgery and involves inserting one-way valves into certain airways. The end result is that air won’t get trapped in areas of the lungs with emphysema and you’ll be able to breathe easier.
Lastly, COPD can be complicated when co-morbidities such as sleep apnea are involved. Sleep apnea is a condition where the airways close up as you sleep resulting in disruptions in your sleep and more serious long-term effects such as an increased risk of high blood pressure (hypertension) and heart attack. When COPD and sleep apnea occur together it is referred to as overlap syndrome, and studies have found that this phenomenon is common, especially as COPD progresses.
There is a Genetic Component to COPD
There is a small group of COPD patients that are often excluded from larger discussions about COPD and its causes. These are people who contracted COPD without ever picking up a cigarette or spending time around smokers. While alpha-1 antitrypsin deficiency (A1AD) is rare, it is the number one cause of COPD in non-smokers and people who live otherwise healthy lives.

A1AD occurs when the liver does not produce the correct amount of the alpha-1 protein. This protein is responsible for protecting the lungs from damage due to inflammation and it also prevents damage due to scar tissue in the liver. In these people, even something as simple as exposure to poor air quality or higher than normal levels of air pollution can lead to permanent lung damage and even COPD.
While there is no cure for alpha-1 antitrypsin deficiency, there are treatment options available. It’s also very important to recognize it at an early age so awareness is key. One possible treatment option is called augmentation therapy (replacement therapy). This is where the patient receives replacement alpha-1 from a donor once a week through an IV treatment. While this is not a cure-all, it can play an important role in delaying damage to the lungs. This is another reason it’s important to start as soon as possible.
COPD is More Common in Women
For many decades, COPD was primarily a disease that affected men. This is largely due to the fact that women did not smoke very frequently before the 1950s. However, since then, the gap between men who smoke and women who smoke has narrowed significantly. With that being said, the number of smokers, in general, has decreased from 40 percent in the 1970s to around 14 percent in 2017.

Another reason COPD is more common among women is that women are proven to have a faster rate of decline in FEV1 (forced expiratory volume in one second) than men despite smoking less heavily. Studies have also shown that women have higher hospitalization rates and deaths due to respiratory failure or comorbidities.
COPD Patients Can Live a Long and Healthy Life
It’s so easy to fall into a line of thinking where being diagnosed with a chronic condition means it’s the end, but this couldn’t be farther from the truth. While receiving a COPD diagnosis should act as a wake-up call for heavy smokers, it is far from “the end.” Many COPD patients are able to live long, happy lives as long as they make a serious effort to change their lifestyle for the better.

According to Medicinenet.com, the five-year life expectancy for newly diagnosed COPD patients is 40% to 70%. This is despite the fact that as many as 38% of people diagnosed with COPD continue to smoke and many don’t follow through with the treatment plan that their doctor set forth for them. On the other hand, people who immediately quit smoking and implement healthy choices like supplemental oxygen therapy, a healthy diet, and a consistent exercise routine see much better results. Some people with COPD have lived well into their 70s and 80s.
Conclusion
COPD is a leading cause of death in the United States and it’s also one of the most preventable illnesses in the world. Despite this fact, many people are woefully unaware of what exactly it is and how it affects the body. In comparison to other chronic illnesses like lung cancer or heart disease, COPD receives a lack of funding. This has led to many people referring to it as an “invisible illness.” — many people are affected, yet many suffer in silence.
The good news is that everyone can play a role in the treatment and prevention of COPD. if you have COPD, you can take part in clinical trials which helps to pave the way for researchers and doctors. If you have a friend or loved one with COPD, you can take time out of your day to help them manage their disease. And if you don’t have any connection to COPD, you can still get involved by donating or volunteering with organizations like the American Lung Association or the COPD Foundation.
.png)
According to Philip Tierno, director of clinical microbiology at NYU, humans come into contact with around 60,000 germs every day. However, only about one to two percent of these are potentially harmful. Our body also has innate and adaptive immunity which helps to protect us from these dangerous bacteria. Innate immunity is the defense system that’s in place when we’re born, and adaptive immunity is our body’s defense which develops over time as we’re exposed to more and more bacteria.
With the advent of the novel coronavirus, people have been much more conscious about their exposure to bacteria and viruses. The World Health Organization (WHO) has put forth a list of best practices for avoiding exposure to COVID-19 such as social distancing practices, mask-wearing, and other hygiene measures. And at the end of last year, we saw the first COVID-19 vaccine being tested on high-risk patients.
Despite the urgency of the COVID-19 vaccine, many people still have doubts about getting vaccinated due to the perceived risks. Older adults with chronic illnesses such as chronic obstructive pulmonary disease (COPD) or other respiratory diseases are proven to be at the highest risk of both contracting and experiencing severe reactions to the virus, yet many of these people choose not to get the vaccine.
In this post, we’re going to go over everything you need to know about getting vaccinated as a COPD patient, why it’s important, and settle any doubts or fears that you may have about the process.
What is a Vaccine?
Aside from safe hygiene practices, vaccines are the best tool that we have to fight bacterial and viral infections. Vaccinations are made from the same germs that cause the disease, but they are either weakened or killed so they don’t actually make you sick. What this does is causes your immune system to produce antibodies that can be used to fight off the disease if you come into contact with it. In other words, you’re developing immunity to the disease without actually contracting it.

Vaccines are not a new concept by any means, but the practice of vaccinology has evolved over time. According to healthaffairs.org, the first successful vaccine is credited to Edward Jenner, an English physician. In 1796, he administered a vaccine to a small child which prevented smallpox. While this vaccine was effective in the general population, there were limitations when it came to administering the vaccine to large groups of high-risk people.
With modern technology, however, administering vaccines has become much easier and more effective. While the first COVID-19 vaccine was administered this past December, there are already over 39 million people worldwide who have been fully vaccinated and over 120 million who have received at least one dose. What’s more, the vaccine is being administered to high-risk patients and front-line healthcare workers before everyone else which will increase its effectiveness in the long term.
Why Do COPD Patients Need Vaccines?
Most COPD patients are considered “high risk” when it comes to transmittable diseases like COVID-19 and influenza. According to Healthline, COPD is most common in people over the age of 40, and studies have shown that the average age of death for COPD patients is around 77.4 years of age. According to the Centers for Disease Control and Prevention (CDC), seniors over the age of 65 are at the highest risk of COVID-19, making up about 80% of the total deaths. They also report similar trends with influenza and other infectious diseases.

Another factor that contributes to COPD patients being “high risk” is that many of them are smokers. According to Very Well Health, 38% of adults with COPD continue to smoke. Nicotine, one of the most harmful chemicals found in cigarette smoke, alters the immune response in your body putting you at a higher risk of contracting an infection. According to news-medical.net, carcinogens are the main immunosuppressive agents in cigarette smoke. One of the worst effects of nicotine is that it inhibits the release of reactive oxygen species (ROS) which weakens the ability of neutrophils to kill pathogens (a microorganism that causes disease).
Infection is the Most Common Cause of Exacerbation
A COPD exacerbation is a period of time where your respiratory symptoms suddenly worsen. For example, if you normally experience mild breathlessness and chest pain throughout your day, an exacerbation could cause you to experience more severe symptoms that prevent you from going about your day. Exacerbations can range in severity from mild to severe. They can also have varying time frames from several hours to several days depending on what caused it.
While many things can cause an exacerbation such as air pollution, over exercising, or allergies, lung infections are by far the most common cause. Although infections like pneumonia can be mostly harmless in younger people with healthy lungs, they can be much more serious in COPD patients. COPD, especially chronic bronchitis, is associated with swelling and increased mucus production in the airways. Infections like influenza can contribute to this issue making it even harder to catch a breath.
Infection Can Cause Hospitalization
Not only does infection result in COPD exacerbations, but it’s also the most common cause of hospitalization in COPD patients. Hospitalization is something that you want to avoid at all costs, not only because it’s an indication you’re suffering from something severe, but also because it’s a very heavy financial burden. In 2016, the average cost of a hospital stay was $11,700 meaning it’s the most costly healthcare spending in the country. For more information on avoiding hospitalization due to COPD, read through this post.

Another reason it’s important to avoid hospitals is because they’re not a safe place for you to be during a pandemic. While doctors want anyone and everyone who’s experiencing a medical emergency to feel safe going to a hospital, there’s no reason to risk it if you don’t have to. Not every hospital has the same policies or safety practices when it comes to COVID-19 prevention, so it’s important to research hospitals and do what you can to prevent being hospitalized.
It Protects Other People
Last but certainly not least, getting vaccinated plays an important role in protecting people around you. Infectious diseases are often passed from person-to-person via physical contact or simply breathing the same air. While getting vaccinated is not a surefire sign that you won’t carry a disease or pass it onto someone else, it can help. Even if you are vaccinated for COVID-19, however, you’ll still need to wear a mask and maintain safe social distancing.

Are There Risks to Getting a Vaccine?
Unfortunately, the risks of getting vaccinated are often blown out of proportion. People hear of friends or family members experiencing symptoms of the disease they’re being vaccinated for and this turns them off of receiving the vaccination themselves. But this is a perfectly natural reaction to the vaccination and it’s actually a good sign that the vaccine is working as it should. This is because your body is creating an immune response that leads to the creation of antibodies which inevitably prevents you from getting sick.
![]()
Which Vaccines Should COPD Patients Receive?
Influenza Vaccine
The influenza vaccine is possibly one of the most important vaccines you can receive because hundreds of thousands of people are hospitalized due to the flu every year. Flu symptoms include.
- Headache
- Runny nose
- Sore throat
- Fatigue
- Shortness of breath
- Cough
-
Fever

It’s recommended that you receive a flu vaccine every year because your body’s defenses will diminish over time. Another reason to keep up to date with your flu vaccines is that there are different strains of this virus. The vaccines may be updated from year-to-year in order to ensure that people have immunity to all of these changing strains.
Pneumococcal Vaccine
Pneumococcal disease is the name for infections caused by Streptococcus pneumoniae. You might have never heard of this type of vaccine and that’s because it’s not recommended for everyone. However, the reason it’s often recommended for COPD patients is to prevent pneumonia. This is a respiratory infection that attacks the alveoli, the tiny air sacs in the lungs that are responsible for the exchange of oxygen and carbon dioxide to and from the blood. COPD patients are more susceptible because they often struggle to clear mucus from the lungs which can carry bacteria.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Tdap Vaccine
Pertussis, or whooping cough as it’s more commonly known, can lead to pulmonary hypertension (high blood pressure in the lungs), brain damage, seizures, and even pneumonia. Even the mildest cases of whooping cough can exacerbate COPD symptoms, potentially leading to hospitalization. It’s recommended that adults receive one dose of the Tdap vaccine and they also have the option of getting a booster shot every 10 years which strengthens its effects.
Zoster Vaccine
Chickenpox is a highly contagious infection that’s characterized by rashes on the skin. If you’ve had this condition earlier in life you might experience a recurrence called shingles. This is because, after you recover from chickenpox, the virus moves to your nerve tissue where it can emerge later in your life. Fortunately, if you have never contracted chickenpox during your life, you are not at high risk for shingles.
Studies have shown that COPD patients who have had chickenpox are twice as likely to contract shingles as healthy individuals who have had chickenpox. This is most likely due to the widespread inflammation and immune system disruptions caused by the disease. Be sure to speak with your doctor about getting a zoster vaccine if you believe you’re at risk of contracting shingles.
COVID-19 Vaccine
The coronavirus is at the top of everyone’s minds at the moment, and rightfully so. Since early last year, people have been scrambling to find ways to live normal lives without putting themselves and others at risk of contracting this virus. Miraculously, healthcare professionals were able to test out the first-ever COVID-19 vaccine at the end of the year and now it’s being mass-administered all over the world.
As we’ve learned, the people who are at the highest risk of contracting and experiencing severe symptoms from COVID are older adults with chronic conditions, especially pulmonary disease, heart disease, and diabetes. If you fit any of these descriptions, it’s time to reach out to your doctor and ask about receiving a COVID vaccine.
Speak With Your Doctor First
Before going out to get a vaccine, it’s important to first speak with your doctor. Since vaccines are such an important part of COPD management, you’ll want to have a plan to follow before taking any action. Your doctor will recommend vaccinations based on your age, medical history, as well as the expected prognosis of COPD or any other chronic condition you have. In rare cases, your doctor may advise you to not receive a vaccine due to the perceived risks.

Other Safe Practices to Prevent Infection
Social Distancing
Social distancing, also known as physical distancing, is the practice of maintaining distance between yourself and others. While it’s debated exactly how much space you need in order to prevent the spread of illness, the World Health Organization (WHO) recommends six feet. However, it’s also important to consider the type of environment that you’re in. If you’re indoors where ventilation is poor, you may need to maintain more physical distance in order to be safe. Another thing you should do is be sure to cover your coughs and sneezes in your shoulder.

Wearing a Mask
Surgical masks and cloth face coverings are not designed to filter out viruses, but this doesn’t mean they aren’t helpful when it comes to preventing the spread of disease. Face coverings are effective at preventing large droplets of saliva or mucus from exiting or entering the mouth as well as helping to prevent germs from escaping when you cough or sneeze. It’s important to make sure you’re wearing your mask correctly by ensuring that it covers both your mouth and your nose. Also, make sure the ear straps are tight enough that you don’t have to constantly adjust the mask with your hands which can increase your risk of getting sick.
.jpg)
Practicing Good Hygiene
Hygiene is something that you can always work at to improve and it’s especially important during a pandemic. You should be washing your hands with soap and water periodically throughout the day especially before eating, drinking, and going to bed at night. Cleaning surfaces in your home such as door handles, tables, chairs, keyboards, and countertops will also help to prevent the spread of bacteria.

Follow Your COPD Treatment Plan
At the end of the day, following your COPD treatment plan is just as important as getting vaccinated. Smoking cessation, supplemental oxygen therapy, a consistent exercise routine, and a well-balanced diet will all promote a healthy immune system which is essential for warding off disease, including the novel coronavirus. It will also keep your symptoms in check so that if you do end up getting sick it will be less severe and easier to cope with.
.jpg)
While COPD is not a disease that can be stopped or reversed, a carefully planned treatment regime will significantly reduce adverse symptoms and slow the rate of respiratory decline. It can be overwhelming trying to completely overhaul your lifestyle so you should take things day-by-day and don’t be afraid to reach out to your doctor when you have any questions. Family and friends are also the best people to rely on when you’re facing challenges caused by your disease.
Conclusion
Like anything healthcare-related, vaccinology is a field that continues to grow and evolve. As new infectious diseases are discovered and others mutate, we need new technology and inventions in order to cope with them. Since the advent of the novel coronavirus in 2019, there’s been an increased emphasis on protecting high-risk individuals such as those with COPD and other chronic conditions as well as people over the age of 65 who have a less-active immune system.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
While there are occasionally risks associated with vaccines, for the most part, they play a crucial role in keeping people safe and healthy, especially those with chronic obstructive pulmonary disease. Fortunately, COVID-19 vaccines are being distributed all across the world for high-risk individuals, so it’s the perfect time to get one if you haven’t already.
Lastly, you should continue to follow your COPD treatment plan and speak with your doctor regarding your concerns. Supplemental oxygen therapy, pulmonary rehabilitation, and a balanced diet all play a crucial role in maintaining your health so it’s important to take a holistic approach to your health.
.png)
From managing short- and long-term goals to exercising, eating right, and making it to doctor’s appointments, living with COPD is not easy by any means. Whether you are still working or you’ve already retired, being diagnosed with COPD means taking on a whole new set of responsibilities — some of which can be overwhelming at times.
Sometimes, it’s a good idea to take a step back and try to figure out some ways to simplify your daily routine. This will help you experience more peace of mind and provide you with some reassurance that you’re taking the steps necessary to treat your condition effectively. It can also make it much easier to cope with the mental and emotional aspects of COPD such as anxiety management.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
If you’re in the market for a supplemental oxygen device such as an oxygen tank, liquid oxygen tank, or oxygen concentrator, read on, because we’re going to be taking a look at how the Caire FreeStyle Comfort, one of the most popular portable oxygen devices on the market, will simplify your life with COPD. If you have any questions, please feel free to leave them in the comment section below and we’ll get back to you.
What is the Caire FreeStyle Comfort?
The Caire FreeStyle Comfort is a portable oxygen concentrator. What this means is that, instead of storing oxygen like an oxygen or liquid oxygen tank would, it draws in ambient air, removing any impurities, and puts out medical-grade oxygen. This is defined as a type of controlled gas, over 90% purity, that’s used to treat respiratory illnesses. While oxygen concentrators are much safer than oxygen tanks, you will still need a prescription from your doctor in order to purchase one.

Another difference between the Caire FreeStyle Comfort and oxygen tanks is that the former is battery operated whereas the latter is not. In other words, by using an oxygen tank, you are restricted by how much oxygen can be compressed into one container — the more oxygen you need, the bigger the tank you’ll need to use. With the FreeStyle Comfort, you simply need to replace the battery.
The FreeStyle Comfort is one of the latest portable oxygen concentrators released, and objectively speaking, it’s one of the best. It has relatively little competition when it comes to its weight, size, oxygen output, and general reliability. The only comparable portable oxygen concentrator in terms of specifications is the Inogen One G5. And while this device surpasses the FreeStyle Comfort in terms of oxygen output, the battery is less powerful, which leads many people to prefer the former.
.png)
Another thing to note about the Caire FreeStyle Comfort is that it uses pulse dose technology rather than continuous flow. What this means is that it closely monitors your breathing rate and only delivers oxygen when you’re inhaling. This is what enables manufacturers to make their oxygen devices so small and yet still provide you with hours upon hours of medical-grade oxygen on one battery charge.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Continuous flow portable oxygen concentrators, on the other hand, tend to be much bulkier and they have batteries that won’t last you more than a couple of hours. This is problematic if you’re someone who wants to be able to stay out of the house for extended periods of time without having to run home and charge your device.

1.) You’ll Have a Hassle-Free Oxygen Device
Quite possibly the most common complaint about oxygen tanks is how much of a hassle they can be. Oxygen tanks need to be refilled constantly meaning you need to have an oxygen company deliver them to your home or you can drive to an oxygen company and have them refilled. This is incredibly inconvenient if you don’t live near a company that is able to refill your tanks and it can also be very expensive to pay someone to deliver your oxygen. What’s more, you’re likely going to want to have backup oxygen tanks meaning you’ll have to find a place to store them.

To counteract this issue, many oxygen patients choose to buy something called a homefill oxygen station. This is similar to an oxygen concentrator but it’s designed to refill your oxygen tanks. This can be extremely costly, though, and it requires you to know how to use it. If you’re going this route, you might as well just purchase a home oxygen concentrator and you’ll never have to worry about refilling oxygen tanks ever again. Home oxygen concentrators are also much more compact and easy to maneuver around your home than oxygen tanks are.

Alternatively, you could use the Caire FreeStyle Comfort which is one of the most hassle-free oxygen devices money can buy. When you’re at home, simply plug your FreeStyle Comfort into the wall and you’ll have access to an infinite supply of oxygen. Once you’re ready to go, simply unplug it and the device will begin to run off the powerful lithium-ion battery. There’s no need to constantly be in touch with oxygen companies because the device does all the work for you.
2.) You Can Exercise With Ease
If you have COPD, you know how important it is to maintain a consistent exercise routine. Exercise is what keeps your lungs and body strong so that you can reduce symptoms of breathlessness, fatigue, and chronic pain. But how can you exercise effectively if you’re lugging around a heavy and bulky oxygen device? Fortunately, the Caire FreeStyle Comfort weighs in at just 5 pounds and it’s small and compact enough to sling over your shoulder as you exercise. If you want, you can even use accessories like the FreeStyle Comfort backpack to spread the weight between your shoulders as you work out.

One unique feature of the FreeStyle Comfort is its ergonomic design. Unlike oxygen concentrators in the past which tend to be box-shaped, the FreeStyle Comfort has a curved design that prevents the unit from wobbling around too much as you’re walking and exercising. While this is only a minor difference, it just goes to show how far Caire has gone to make a portable oxygen concentrator that meets everyone’s needs.
3.) You Can Plan Trips More Easily
Before portable oxygen concentrators were invented there was no way for supplemental oxygen patients to take a flight. Oxygen tanks and liquid oxygen tanks are banned on all commercial airlines because they’re an explosive hazard. Instead, people who needed medical-grade oxygen were relegated to road trips. And while there’s nothing wrong with road trips, it takes a lot longer to get where you’re trying to go. And even if you were in the mood to drive somewhere, you would need to make sure you had enough backup tanks to last you the duration of the trip.

Traveling with a portable oxygen concentrator like the Caire FreeStyle Comfort, however, is incredibly simple because it’s approved by the Federal Aviation Administration (FAA) for use on all commercial airlines in the United States. All you need to do is check in with your airline 48 hours before your flight and be sure to bring 1.5 times the duration of your flight in battery life. This will help to account for any potential delays during the flight. You might also consider investing in other accessories like the external battery charger so that you can charge batteries more quickly while you’re on vacation.

Unsurprisingly, using other modes of transportation also become much easier when you’re using a Caire FreeStyle Comfort. This machine comes with a DC charging cable that allows you to charge your device in any car outlet. In other words, if you’re taking a long road trip, you’ll never have to worry about stopping to charge your POC or carrying tons of extra batteries. You can even continue using your POC while it’s charging in the car.
4.) You’ll Save Money Over Time
Many people are surprised to find that portable oxygen concentrators are actually one of the most affordable options for oxygen therapy. While POCs do have a higher upfront cost, the longer you have them, the more they pay for themselves. And since the Caire FreeStyle Comfort is built to be reliable and durable, you won’t need to worry about having to send it in to get repaired or maintained. Aside from replacing the columns, there aren’t any major repairs that you will need for many years to come.

This is in stark contrast to oxygen tanks which have significant recurring costs associated with them. While you might only spend a couple of hundred dollars on a tank, you’ll need to pay to refill them on a weekly or biweekly basis which can add up really quickly. And realistically, you’ll want to have multiple tanks as a backup. On the other hand, if you want to rent tanks and have someone deliver full tanks when you run out, this can be even more expensive.

If you choose to refill your own tanks, you’ll need to purchase an oxygen refill station. These devices alone will run you several thousand dollars and they’re largely unsupported by most oxygen manufacturers so you will likely need to pay exorbitant prices to fix one if anything goes wrong. At this point, it would make a lot more sense to invest upfront in a portable oxygen concentrator rather than dealing with the recurring costs and hassle of owning oxygen tanks.
5.) You’ll be More Independent
Maintaining your independence as you get older is very important. According to Vantage Aging, independence in older adults helps them find a sense of purpose and fulfillment and even have physical benefits like improved strength, balance, and memory skills. Unfortunately, it can feel downright impossible to maintain your independence when you’re using a heavy, bulky oxygen tank. Even if you’re making every effort possible to do things on your own, you may find yourself relying on others to help you manage your oxygen tank.

One example of this is going up a flight of stairs. It would be unreasonable to expect anyone to carry oxygen concentrators up a flight of stairs by themselves because it’s dangerous and can cause you to overexert yourself. However, the Caire FreeStyle Comfort portable oxygen concentrator is very lightweight and small. What’s more, it comes with accessories that make it safer and more convenient to carry. The FreeStyle Comfort backpack which we mentioned earlier keeps the unit close to your back as you walk so that there’s no added stress on your body, even when you’re going up a flight of stairs.
6.) You’ll Experience More Restful Sleep
If your doctor has prescribed you with 24 hours of oxygen, you’re going to need to use your oxygen device while you sleep. While this may sound like a huge pain, it’s actually made very easy by pulse dose portable oxygen concentrators. Like other oxygen devices, the FreeStyle Comfort is capable of detecting even the faintest breaths. This is important because when you’re sleeping, your breathing rate changes significantly, so you want to ensure that you’re inhaling the correct amount of oxygen despite this.

The Caire FreeStyle Comfort has a built-in UltraSense® technology that ensures optimal oxygen delivery throughout the day and night. Unlike oxygen tanks which can run out while you sleep, you can keep your FreeStyle Comfort plugged into the wall outlet all night long so that you never run out of oxygen supply. Caire understands that many of their patients use oxygen 24/7 so they built this device with these people front of mind.
7.) You’ll Keep Your Symptoms in Check
Last but certainly not least, using a Caire FreeStyle Comfort will help you manage your symptoms and keep your thoughts off of your disability and instead focus them on what you’re trying to accomplish. Far too many people have trouble living in the moment with COPD. Instead of focusing on what they’re trying to accomplish, many people are overcome with regrets about the past or anxiety about the future.

Most people find that when they make the switch to a POC, they’re much less self-conscious about using an oxygen device. Some people even say they forget they’re using a medical oxygen device making them feel much more confident in their own abilities. Since the FreeStyle Comfort adjusts to your needs there aren’t too many things for you to be concerned about.
Conclusion
No matter what your age is or what stage of life you’re in, simplifying your lifestyle is an invaluable skill to have. If you have COPD, making the switch from an oxygen tank or liquid oxygen tank to a portable oxygen concentrator like the Caire FreeStyle Comfort can make a world of difference, especially when it comes to managing your disease effectively.
Here at LPT Medical, it’s our goal to get a portable oxygen concentrator into the hands of anyone who wants and needs one. However, it’s also important to us that you get a device that aligns with the prescription that your doctor created for you. Reach out to us either by phone or email and you’ll be connected with a respiratory specialist who can answer all of your questions and get you the best deal possible on a new, used, or refurbished portable oxygen concentrator.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













