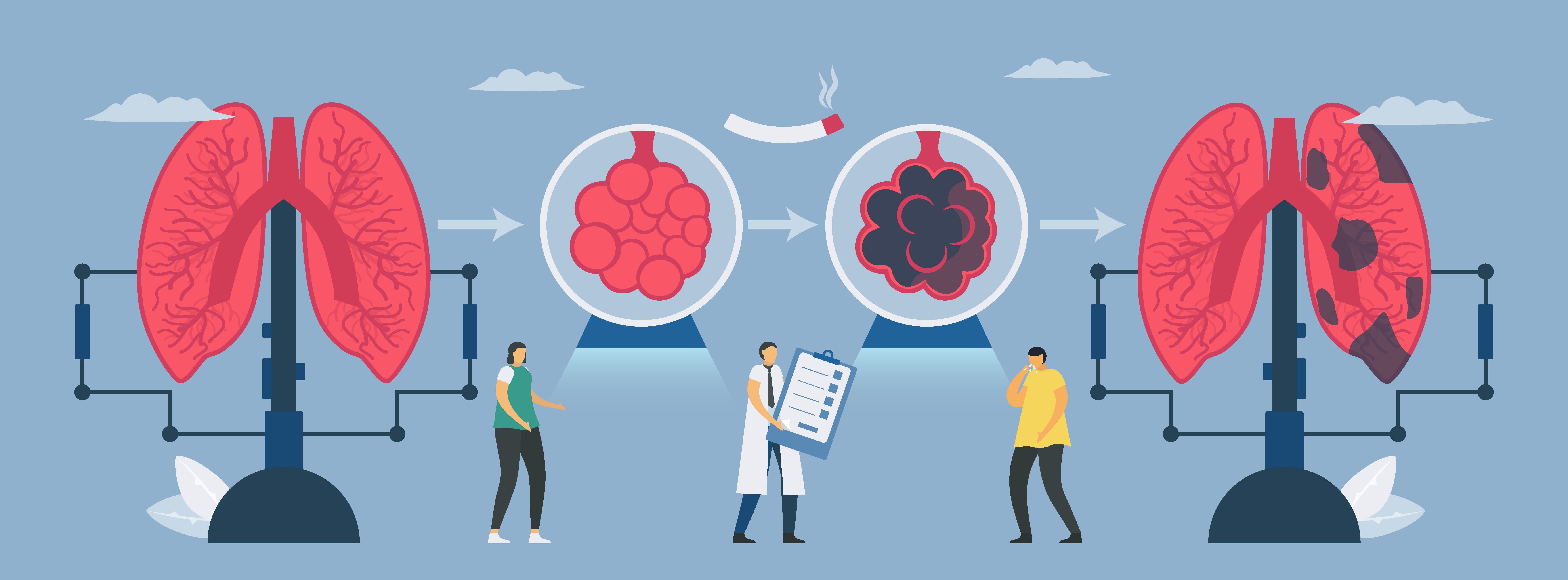
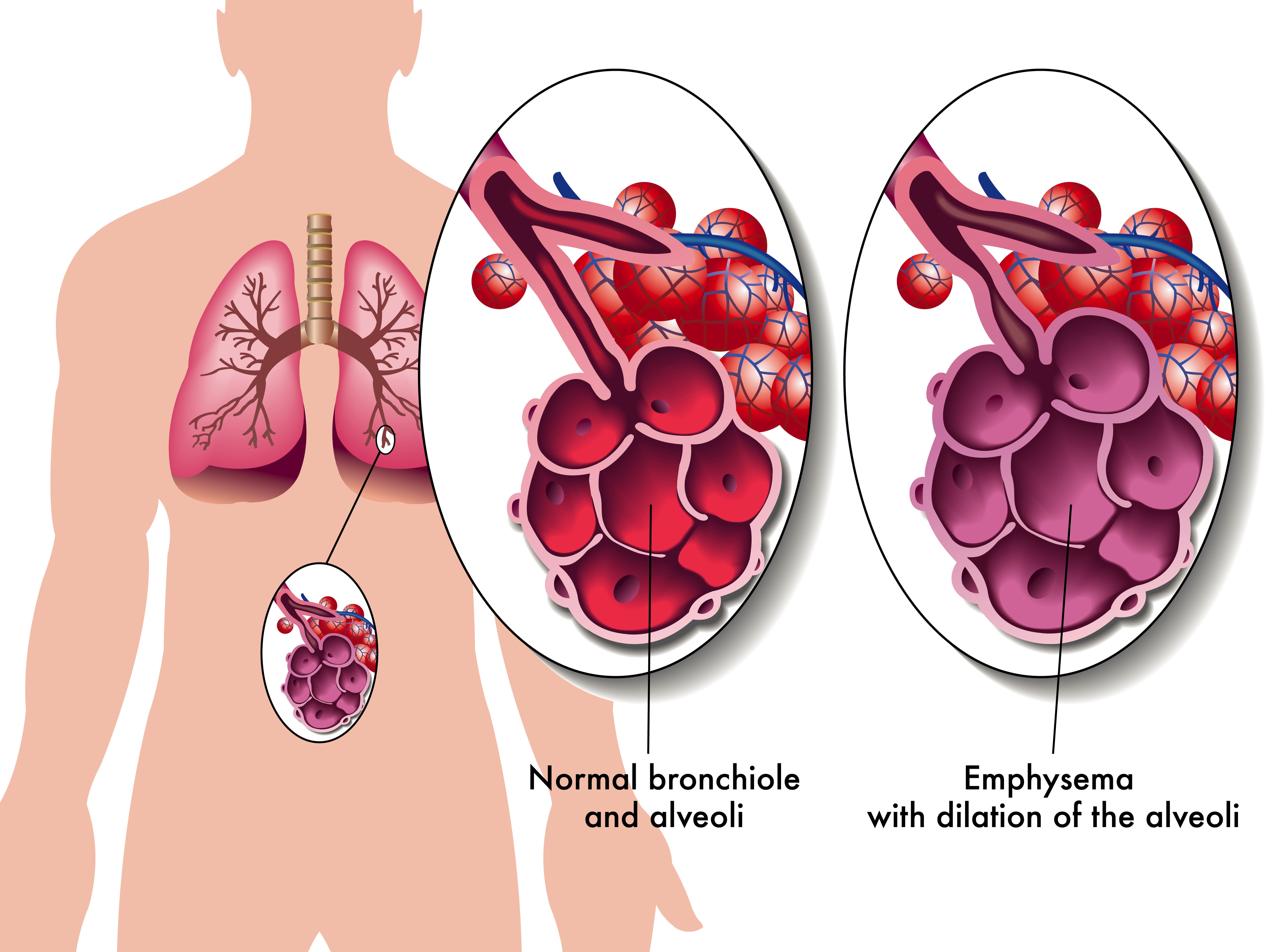
Chronic obstructive pulmonary disease (COPD) is an umbrella term used to define two different types of lung disease: chronic bronchitis and emphysema. The former is a condition that impairs the bronchioles, the airway tubes that lead into the lungs. The latter affects the tiny air sacs in the lungs called the alveoli. These are responsible for the transfer of oxygen and carbon dioxide to and from the bloodstream. Both chronic bronchitis and emphysema are called “obstructive” diseases because they make it more difficult for the patient to expel air from the lungs, thus leading to a buildup of CO2 in the blood.
When a patient is diagnosed with COPD, they’re typically prescribed a standardized treatment plan including but not limited to supplemental oxygen therapy, a specialized diet, pulmonary rehabilitation, and breathing exercises. These are all clinically proven techniques that will help to prevent breathlessness, chest pain, and improve long-term prognosis. While most COPD patients adhere to these well-researched practices, some people look for additional “home remedies” to treat their disease. These are usually referred to as “alternative therapies.”
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Here at LPT Medical, we don’t advise using any type of alternative therapy unless it’s explicitly approved by your doctor or pulmonologist. Some alternative therapies and medications are touted as “cure-alls” or “cheap alternatives” to standardized medications, but more often than not, they don’t live up to their hype and they can even result in further damage to your lungs. In this post, we’re going to tell you all about the alternative therapy called halotherapy, or more commonly known as salt therapy. If you have any questions, please feel free to leave them in the comment section below and we’ll get back to you as soon as possible.
What is Halotherapy and How is it Used?
The term “halotherapy” comes from the Greek word “halos” meaning “salt.” In other words, it’s the use of salt as a therapy for a variety of different ailments. The idea of using salt as a type of therapy is believed to have originated in Europe several hundred years ago. Miners, who are known to contract deadly lung diseases (pneumoconiosis) like black lung and silicosis due to their exposure to mineral dust, did not experience the same effects when they worked in salt mines. Rather, salt mine workers appeared to thrive and experience great lung and skin health.

It wasn’t until 1826 that the first salt therapy facility was opened by a Polish physician named Feliks Boczkowski. At this treatment facility, he offered salt baths from naturally occurring underground brine. After World War II, Dr. K.H. Spannahel created a systemic approach to the climatological conditions of salt caves and attempted to confirm their medical effectiveness. Together, these two physicians helped to lay the foundation of modern speleotherapy (salt cave therapy).
Nowadays, there are many different types of salt therapy used to treat a variety of different conditions. Below are just a few:
Wet Salt Therapy
This therapy got its name because it involves the use of salt combined with water vapor. Wet salt therapy is one of the most common types of salt therapy and it’s also one of the easiest and most accessible for most people. It includes things like salt scrubs, salt baths, salt nebulizers, and saline solutions.

Dry Salt Therapy
This is a type of salt therapy that is completely void of moisture or humidity. This is considered the most “traditional” type of salt therapy and it includes salt caves, salt grottos, salt rooms, and salt chambers. Dry salt therapy is said to have many benefits for the body including improved breathing and softer skin.
Speleotherapy
“Speleo” is derived from the Greek word spḗlaion meaning caves. Speleotherapy is a type of salt therapy that involves going into naturally occurring caves below the earth’s surface. It’s believed that the natural climate and environment of these caves is great for treating respiratory diseases like asthma and chronic obstructive pulmonary disease.

Active Salt Rooms
This type of salt room uses a halogenerator. This is a device that crushes pure sodium chloride into a fine powder that can be dispersed as an aerosol into the room. This is done in a confined room where the amount of salt in the air can be closely monitored by a specialist. The climate and humidity of these rooms are also closely monitored.
%20(2).jpg)
Passive Salt Rooms
This is similar to active salt rooms but there is no halogenerator that puts out salt particles in the air. Rather, a passive salt room simply has blocks of various types of salt including Himalayan, Mediterranean, Caribbean, or Rock salt, and they’re designed to mimic the effects of being in an actual naturally occurring salt cave. Many people claim that having large quantities of salt like this in a confined space creates positive energy frequencies and a clean-air environment. This is also a major selling point for products like salt lamps which are very popular nowadays.
Can COPD Patients Benefit from Salt Therapy?
Now that you know a little bit about what salt therapy is, you’re probably wondering if there are any proven benefits for COPD patients. Unfortunately, there isn’t a simple “yes” or “no” answer to this. Despite being around for hundreds of years, there isn’t a significant amount of research done on the topic, and many health experts have conflicting opinions about how it should be used, or if it should even be used at all.
The reason salt therapy is associated with COPD in the first place is because of its antibacterial and anti-inflammatory properties. Hundreds of years ago, before the invention of refrigerators, salt was used to preserve meat. This worked because salt draws the moisture out and prevents harmful bacteria from forming. Proponents of salt therapy believe this can also benefit the respiratory system of COPD and asthma patients by killing harmful bacteria that could lead to infection.
Proponents of salt therapy also claim that salt can reduce inflammation in the lungs and airways, loosen excess mucus, and reduce immune system oversensitivity, all of which are symptoms of COPD. However, most of these claims have very little evidence backing them up and many studies have even shown that salt therapy can actually exacerbate the issues above rather than help to cure them.
According to the Asthma and Allergy Foundation of America (AAFA), inhaling concentrated salts (hypertonic saline) or any crystalloid solution containing more than 0.9% saline is proven to make asthma and COPD worse by irritating the airways, increasing mucus production, and causing a cough. As such, it’s important to understand the concentration of salt in the therapy you’re receiving.
Another important thing to note is that the popularity of salt therapy does not affirm its efficacy. Just turning on your TV or browsing the internet, you’re likely to see advertisements for salt therapy caves, salt lamps, and salt inhalers, and you likely hear claims that they can cure chronic illness, but this doesn’t make them true. Since salt therapy is not classified as an FDA approved medication, it’s also not regulated the way that your traditional COPD medication is.

That doesn’t make them completely immune to responsibility, however. With the advent of the novel coronavirus (COVID-19), salt therapy companies have been under close watch by the FDA when it comes to the claims they make about their products. Some salt therapy companies have made wild claims about their products curing or treating COVID-19 when there is little or no evidence to suggest this is the case. If you’d like to learn more about how these types of products are regulated, read through our post about dietary supplements.

Last but certainly not least, there’s a problem with a placebo effect concerning salt therapy. A lot of the research on salt therapy has been inconclusive because it’s based on anecdotal evidence. In other words, many patients are reporting that salt therapy is beneficial to their health, but there is little evidence to suggest there was a physical change to their disease. Rather they have an expectation that something will change, so that’s what they believe. This is a great selling point for many salt therapy companies because, generally speaking, people trust the opinion of others.
Should COPD Patients Use Salt Therapy?
The most important thing to remember when it comes to alternative therapies or home remedies is to always consult your doctor first. Your doctor may have additional insight into why you should or should not be using salt therapy and he/she will help you weigh the risks. You should also do research on the specific salt cave that you want to visit. While some of these places are sanitized regularly, others are teeming with bacteria which could increase your risk of respiratory infection.
It’s also important to weigh the risks of different types of salt therapy. For example, salt therapy caves or chambers are designed to have a very high saline concentration, so it’s more likely this type of therapy could exacerbate your symptoms. Conversely, simply having a salt lamp around your home is unlikely to result in a high concentration of salt in the air, so you can assume that they’re safe to use. Just don’t expect there to be any significant benefits for managing your disease.
What Should COPD Patients be Doing Instead of Salt Therapy?
While it may be tempting to join in on a fad like salt therapy, the best way to treat your COPD symptoms is with traditional methods that have been researched for hundreds of years and backed by thousands of different studies. Let’s take a look at each of these treatment options.
An Improved Diet
Your lungs play an extremely important role in a process called cellular respiration. This is a set of metabolic reactions in the cells of your body that convert chemical energy into adenosine triphosphate (ATP). In other words, the oxygen that your lungs take in is directly linked to the breakdown of nutrients in your body and it’s absolutely necessary for your body to produce energy that it can use. One of the most important things to note as a COPD patient is that certain foods create more waste products (carbon dioxide) than others do which can make breathing even more difficult.
![]()
Pulmonary Rehabilitation
Regular exercise is one of the most important things you can do for your health. Whether you’re young, old, sick, or healthy, exercising improves blood flow, heart strength, and reduces your risk of life-threatening conditions like heart disease and diabetes. Pulmonary rehabilitation is a type of exercise that’s specifically designed for people with COPD and other chronic respiratory diseases because it’s focused on strengthening the lungs, reducing breathlessness, managing weight, and preventing exacerbations. Learn more about how pulmonary rehab works in this post.

Supplemental Oxygen Therapy
Another standard treatment for chronic obstructive pulmonary disease is supplemental oxygen therapy. Since COPD patients have less efficient lungs than the general population, oxygen therapy is designed to supply them with a higher concentration of oxygen. In turn, this will alleviate difficulty breathing, ensure blood oxygen levels remain stable and help to prevent exacerbations and other complications. Many people are intimidated by oxygen therapy because they believe it will prevent them from getting around and living life on their own terms.

Fortunately, this is not necessarily the case. While older outdated oxygen devices like oxygen tanks and liquid oxygen tanks can be bulky and difficult to maneuver, they’ve since been replaced by lightweight portable oxygen concentrators. Unlike oxygen tanks, concentrators are battery-powered machines that never need to be refilled by an oxygen company. They’re also fully approved by the Federal Aviation Administration (FAA), so you’ll never have to worry about being restricted in where you can travel. For more information on portable oxygen concentrators, be sure to reach out to our respiratory specialists here at LPT Medical.
Smoking Cessation
Smoking cessation can be one of the greatest challenges for many COPD patients. Some people have smoked for decades, so being faced with a COPD diagnosis and the task of quitting immediately, it can be somewhat overwhelming. However, it’s also the single most important thing you can do to alleviate your symptoms and ensure the best long-term prognosis of your disease. Several months ago, we wrote a three-part guide on smoking cessation and recovery so be sure to check it out if you’re interested.

Inhaled Therapy
It’s important not to confuse “oxygen therapy” and “inhaled therapy.” Oxygen therapy is meant to increase blood oxygen levels whereas inhaled therapy is meant to administer COPD medication via a mist called “aerosol.” By inhaling medication rather than taking it orally, you’ll experience greater benefits and you’ll experience the effects almost immediately. Inhaled therapy is usually administered through either an inhaler or a nebulizer device.

Conclusion
While salt therapy (halotherapy) is a trendy topic these days, that doesn’t necessarily mean it’s an effective treatment option for COPD. Although salt therapy has been around for hundreds of years, it’s surprisingly understudied and there is very little empirical evidence to go off of. With that being said, salt therapy has been found to be rather safe as long as you’re not exposed to it in high quantities.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Regardless of what you’re trying to change with your COPD treatment plan, you should always consult your doctor first. He/she may want to take a look at your medical history before determining if it’s safe for you to use salt therapy, or may completely advise against it if there’s a chance it could make your symptoms even worse. You should also take time to plan your day ensuring that you’re focusing on things that you know will improve your symptoms.
It is 2021, and no matter who you are, your life was most likely impacted by the global pandemic caused by the novel coronavirus first exposed late in 2019 (COVID-19). This virus is the most dangerous for humans when it infects your respiratory system, so this is obviously frightening for people with COPD and other underlying health conditions and immunodeficiencies.
There is much more that is unknown about the virus than there is any information that is definitive. How fast it spreads, how easily transmittable it is, and so much more will be under scientific scrutiny for months even years to come.
COVID-19 and COPD recommendations
This means that if you have COPD or any respiratory aliment or immunodeficiency it is recommended by medical professionals all over the world, that you especially need to take care to adhere to guidelines and other health related advice.
This means limiting your travel or vacation plans, maintaining social distancing recommendations of at least 6 feet apart, among other requirements.
You might have had plans this year to visit the grandkids, or they were coming to visit you, maybe you were embarking on an adventure, or a relaxing getaway, or maybe you had no plans at all, but are finding the reality of a global pandemic lifestyle unfulfilling.
No matter how serious your COPD is, there are ways you can maintain a positive livelihood without being exposed to COVID-19. Here are the best ways to enjoy this year safely in the midst of a global pandemic if you are immunocompromised or suffer from a respiratory illness such as COPD.

Simplify your life
There is no better time than now to simplify your life. This is often called minimalism. The benefits of simplifying your life are substantial especially at a time of pandemic when our minds are filled with anxieties and uncertainty. Ironically, making things simpler can sometimes be more complicated than you think.
Minimalism and simple living can offer anyone, especially seniors and people living with COPD, many benefits. For example, minimalism can help seniors have a much easier life physically.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
With all of your things organized, you will decrease the annoyance of misplacing something. And with less things, you won’t have to deal with moving things around as much, or moving around and clean as often. Overall, with less to physical material to deal with, comes less stress and anxiety.
By reducing the clutter in your home, yard, and work space, you subsequently make room in your mind for peace and mindfulness, something that might have gotten lost since the global pandemic has shifted reality.
It can be difficult to get rid of older things that have sentimental value to you, so start by cleaning out a shed or garage where the items have less emotional attachments.

You will find a powerful feeling of control and liberation in this stage and will be able to make more decisions about getting rid of things closer to you.
Hold yourself accountable for getting rid of things that do not serve you, for example: donate clothing you don't wear, donate plates and bowls that are taking over your kitchen cabinets, give away books you’ve read and don't want to read again. The act of giving to others through donations or gifts is very fulfilling in itself, so this is a bonus.
In order to avoid going to donation centers, ask a less vulnerable family member or friends if they would help you by picking up boxes of stuff from your home for them to bring to donation centers for you.
Start a garden or doing daily yard work
While at first thought, this sounds exhausting, gardening and 10 minutes of yard work each day can be very exciting and addicting. Being outside and getting physical activity everyday is one of the best treatment options if you have COPD, and starting a garden is one way of doing that.
Gardening is a physical challenge, relieves stress, and improves dexterity, and aspects that will encourage healthier lung functions.

If you do not have a yard or a nearby community garden to plant anything, you can buy a plant and leave it on the stoop of your house. Visit your plant everyday in the sunshine and watch it grow!
Yard work can take up a lot of time and give you a fulfilling mindset at the end of each day. You don't have to do a lot at first, but once you start picking weeds one day, you’ll begin to enjoy cleaning the yard and finding creative ideas for an outdoor sanctuary right in your backyard.
Find a new hobby you can do online
There are a lot of indoor activities that can keep you occupied and busy this summer and beyond. And there are a lot of activities you probably don’t know that you enjoy yet.
One way to try a lot of different hobbies is to join a club, and because of COVID-19 rather that gathering in a large group for a weekly meeting, you can do this online.
Right now there are a lot of resources where you can join a book club online, or spend time virtually connecting to people with similar interests, either through video chat or social media.

If you have a favorite hobby already, you can try to expand on that by dedicating more time to that specific activity, and find a way to get involved with others who enjoy that hobby virtually.
If it brings you joy, prioritize the time you spend doing those things.
If you feel you are struggling alone with COPD, try joining a FaceBook group or a supportive online forums where individuals share their stories and resources about their COPD.
Go hiking or walking
Walking is a safe and effective form of exercise for people living with COPD, and there are a number of reasons walking and hiking relive COPD symptoms.
Walking and hiking can help improve your COPD:
- Low impact activity that will improve your body's ability to use oxygen
- Build endurance
- Strengthen muscles
- Enhance an overall sense of well-being
- Being more self-sufficient
- Tolerate exercise better
There are even more benefits of walking for a person with COPD than whats listed above.

While you should not travel too far away from home, there might be a great walking or hiking trail near you. Try to avoid walking on busy trails by going during the week day rather than the weekends.
Hiking gets you into the outdoors and under the sun, but it is important that you do so safely. Be sure to continue wearing a mask if people are present on the trails. If the parking lot is extremely crowded, come back another day.
If you are curious how to find the best trails near you, be sure to do some research and learn more about how you could go walking and hiking even with COPD or other complicated health issues can enjoy hiking and walking.
Invest in a oxygen concentrator
Even though we are expected to “stay in place” there is no better time to become more mobile while doing so.
Receiving oxygen treatment for conditions such as COPD doesn't have to mean being tethered to a bulky canister of compressed oxygen, and you should not be subject to limited mobility and lack of independence.
You do not have to subject yourself to the unnecessary risks of carrying around an atmosphere of pure oxygen. There are safer and more transportable alternatives available today.
You do not have to carry a heavy tank around, instead portable oxygen concentrator extracts and concentrates pure oxygen and give you therapeutic doses of purified oxygen from the air around you.

Being at home unable to move around easily due to a rolling oxygen cart can be frustrating and upsetting, especially when you have no outlet to go out and do something, go on vacation, or look forward to family members and friends visiting you.
The uncertainty of these times leaves people hesitate to make larger purchases, such as a portable oxygen concentrator. However, when it comes to the air you breathe and the peace of mind you gain by being more physically active with less shortness of breath is priceless.
These long-term investments lead to long-term savings both monetarily and with regard to your livelihood.
You have a plethora of choices to make when it comes to buying an oxygen concentrator. One thing you need to know is there are two ways that concentrators deliver nearly pure oxygen from the air around you and into your lungs:
1. Pulse flow
Pulse flow or pulse dos oxygen concentrator sensors measure your breathing rate and automatically deliver a short bursts of oxygen as needed. This is a more popular choice for those with higher-functioning lungs like people in stages 1, 2, or sometimes 3 of COPD or those seeking an oxygen boost for exercise or at higher altitudes.
2. Continuous flow

Continuous flow oxygen concentrator maintains a steady supply of oxygen to you while it is being produced. This model will generally be heavier with more power and lower battery life. This option is best for you if you have stage 3 or 4 COPD and very limited lung capacity or higher oxygen saturation requirements for your body.
Be sure that you purchase your oxygen concentrator from an authorized dealer that carries devices from well-established manufacturers. By working with an authorized dealer you can be sure that your machine will be serviced and that the warranty is valid.
Medical and healthcare professionals do not advise purchasing portable oxygen concentrators from questionable sources such as amazon or online auction websites because the warranties and support may be fraudulent and the device may not be exactly what is represented online.
Plan ahead
Planning ahead has been recognized as a key to success, so even under the impending uncertainties brought on by COVID-19, you should plan your goals through hard work and strategic thinking.
This can mean:
- Planning to a regular walking routine for the next week
- Planning to call your loved ones once a day for the next month
- Planning a budget to purchase a portable oxygen concentrator within the next year
- Planning a diet for healthier eating habits over the next week
- Planning goals to quit smoking
COPD can cause a lot productivity challenges, due to shortness of breath and common depressive moods and anxiety. Nevertheless it is these times of isolation, where planning is more important than ever.
You can combat depressive moods and especially anxiety, by planning beneficial goals that will help you to attain a higher quality of life. And there is no excuse not to give this a try while you have so much extra time on your hands.
Foster new and old social connections
Social interaction is vital for everyone, and if you have COPD connecting with others is essential.
If you are not used to being all alone and without other people, and are eager to to reach out to find ways to connect with others, it is important to do so safely.
When exposing yourself to other people you should stay the recommended 6 feet apart and everyone should be wearing a mask. But this does not mean that you can’t have fun.
Take a trip with friends and family to the local beach, river bed, or lake, bringing a large towel or blanket to establish physical boundaries and make sure others are staying a safe distance away from you.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Try bringing a king sized bed spread and your spot can be right in the middle of it, creating a perfect distance away while still socializing.
You and your neighbors can have small communal cookouts where families bring their grills to their respective front yard to BBQ and eat together.
If you want to be more creative, have a neighborhood talent show where each house takes turns putting on a show, either playing music, dancing, or magic outside for everyone to watch.
In order to have a successful social-distancing get-together you must do your best to be innovative. And if you have COPD and are rightfully concerned about COVID-19 you should become a leader in your community to help people socialize safely amid the ongoing pandemic.

Enjoy
Taking each of these steps in your own personal way will help you to enjoy your summer to the fullest, despite on-going risks associated with COVID-19.
Simplifying your life will give you the space you need to try new things. And by taking pleasure in the simple things, you will appreciate your new found adoration for gardening, or yard work.
You can also start exploring ways to use the computer to start new hobbies, or join an online club that you've always wanted to try but could never find the time or motivation to get out of the house and do so.

If you find yourself stuck inside unwilling or unable to move around without shortness of breath, this is the best time to purchase a portable oxygen concentrator that will give you the freedom and independence you need to get moving around your house and outside safely.
Once you are ready to explore more with a lightweight oxygen concentrator that you can carry around, you can attempt taking a short hike or going for a walk. If this is within the capabilities of your lungs, be sure you go to less busy hiking trails and try to go on weekdays when trails are less busy.
Remain social by getting "together" with you family and neighbors and try putting on a social gathering where everyone stays in their respective yards for a BBQ or talent show.
Do you best to stay motivated by planning ahead and setting goals for yourself in all aspects of you life. By taking all of these measures in 2021, amidst a global pandemic while also managing a chronic lung disease, will lead you to a more fulfilling and satisfying life.
%20(1)-png.png)
If you keep up with our blog here at LPT Medical, you’ll know that last week we crowned the Inogen One G5 with the title “The Best Portable Oxygen Concentrator of 2020.” As you can imagine, we don’t take this title lightly.
With so many medical oxygen machines on the market these days, finding the right one for you may seem like a brain-bending puzzle. Even if you have all the information you need at your disposal, you may not have the experience with POCs to even know what’s important in a machine or what price you should be paying for it — that’s why we’re here to help.
As one of the premier oxygen concentrator distributors in the country, we take your search for the perfect oxygen delivery device seriously. Rather than trying to push the most expensive unit we have to offer, we prefer to start with the patient by asking questions like these:
- Are you someone that likes to get out and about or do you prefer to stay home?
- What level of oxygen delivery has your doctor prescribed for you?
- Are you currently using a CPAP or BiPAP machine at night?
- Have you used a portable oxygen concentrator in the past and what was your experience?
These are just a few of the questions we might ask you in order to better understand your point of view and your needs. Purchasing an oxygen therapy device is no small decision, so we’re here to make it as simple and pain-free as possible.
To add to the list of resources you have to help you pick an oxygen concentrator, we’re going to discuss the Inogen G5 and standard portable oxygen tanks. More specifically, we want to show you just how far portable concentrators have come and why you may need to consider upgrading that old oxygen tank. If you have any questions at all, please feel free to visit our oxygen FAQs page or get in touch with us.
Access to Replacement Parts
The first, and potentially most important reason for choosing an Inogen G5 over an oxygen tank is the reputability of the Inogen brand. Oxygen tank companies have been around for what seems like forever, but in this day and age, they’re being rapidly pushed out by portable oxygen concentrator companies. Why? Because oxygen tanks are an outdated technology.
One of the major concerns that oxygen tank users have is that they have trouble finding a place to buy oxygen accessories from and they have trouble finding someone to send the tank for maintenance or repair. Fortunately, since the Inogen One G5 is the newest and best rated portable oxygen concentrator by Inogen, you won’t have to worry about scouring the internet for parts.

The Inogen brand was founded in 2001 with the sole purpose of providing COPD patients with an alternative to oxygen tanks. During this time, many people used portable oxygen tanks which may sound fine, but oftentimes, the word “portable” was used loosely. What people got instead was a bulky and heavy tank that couldn’t be transported without a struggle.
While Inogen was one of the first companies to start producing high flow portable oxygen concentrators, it remains one of the top manufacturers 20 years later. They understand the needs of their customers perfectly and they consistently release top-rated portable oxygen concentrators on the market.

There’s nothing like the freedom that you get from working with a reputable brand. Inogen One oxygen closely tracks the amount of units they sell and they know how long each unit lasts meaning they’re able to provide support for older generations of machine and continue producing accessories like batteries, carrying cases, and filters.
Durability and Safety
One of the first things many people notice about portable oxygen concentrators is how durable and compact they feel — the g5 is no exception! The amount of technology that Inogen has been able to pack into such a small space is nothing short of revolutionary and you can rest easy knowing that it’s protected by a hard outer shell that keeps everything together.
Oxygen tanks stand in stark contrast to this in that they don’t feel durable whatsoever. If you’ve used a portable oxygen tank before, you know exactly what we’re talking about. Since these tanks are explosive and highly flammable, many patients report feeling insecure around their medical oxygen machines, especially when they take it in public.

While oxygen is an essential gas for humans, it only makes up about 21 percent of the atmosphere. If we lived on a planet with an atmosphere that was 100 percent oxygen, it would be very dangerous, not only because our bodies couldn’t handle it, but because it would be very easy to start a fire and keep it going. The oxygen tank that you wheel around is pure oxygen meaning it’s very dangerous unless it’s used correctly.
The thing that makes portable oxygen concentrators safer is that they don’t have any stored oxygen. They remove ambient air and remove the nitrogen allowing it to output pure oxygen. Even if you do end up bumping your POC or dropping it, you’ll never have to worry about it exploding or catching fire. If you would like more information on oxygen safety tips, check out this blog post.
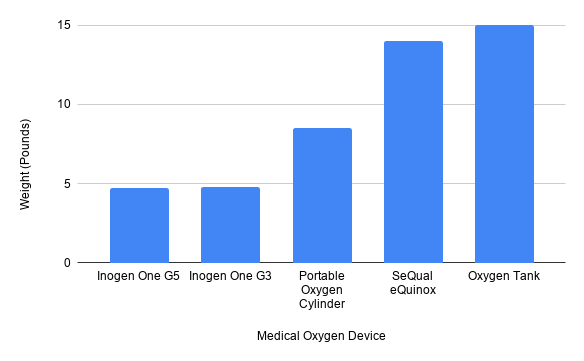
Lightweight Design
When you think of freedom, the first thing that should come to mind is a portable oxygen concentrator like the Inogen G5. This medical oxygen machine weighs in at just 4.7 pounds making it the second lightest POC on the market behind the G4 and lighter than any portable oxygen tank out there. With an Inogen One G5, you’ll be able to go where you want and do what you want without worrying about your oxygen therapy device.

Alternatively, if you opt for a portable oxygen tank or portable oxygen cylinder, the lighter the device, the less oxygen you will have available to you. To put this into perspective, a continuous flow portable oxygen tank offers around 400 liters of oxygen. At a rate of 2 liters per minute (LPM), this will last you just over 3 hours. What’s more, they weigh about 8.5 pounds, about 4 pounds more than the Inogen One G5.
For most people, the weight of the device is the first thing they look at before making a purchase. The lighter the device is, the more personal belongings you will be able to carry with you comfortably and in the case of the G5, the more batteries you can carry with you. If you need extra time with your oxygen cylinder, you’re going to need to carry another one with you. That’s another 8.5 to carry around on your back or on a cart. Alternatively, with a G5, you can double your battery life by upgrading to a 16-cell battery or an additional 8-cell battery.
Intuitive and Easy to Use
Despite being a more complex and high-tech medical oxygen machine, the Inogen One G5 is far simpler to use than an oxygen tank. Oxygen tanks deliver continuous flow oxygen. What this means is that there is a constant flow of oxygen coming through the nasal cannula. Inogen concentrators like the G5, however, use something called pulse dose technology. This technology detects your breathing rate and only delivers oxygen when you’re inhaling.
It is possible to turn an oxygen tank into a pulse dose unit, but you need to purchase something called a pulse regulator and have it installed by a professional. Most oxygen tanks don’t come with pulse regulators and other accessories, so if you want them, you’re going to have to go out of your way in order to find them. What’s more, if something goes wrong with them while you’re out and about, you may not be able to remove it without the help of a professional. In other words, you could be left with a full tank and no way to access the oxygen.

The Inogen One G5 was designed to be intuitive from the control panel to the filters, sieve beds, and battery. Their goal with this line of machines was to offer more freedom by allowing patients to make quick changes to their oxygen delivery on the fly with no hassle. The control panel is easy to use, allowing you to change your flow rating up or down, adjust audio alerts, and check your battery level. If you’re in a poorly lit area, you can even tap the power button to activate the backlight on the screen.
Small Form Factor
While we probably could’ve mentioned form factor under the “lightweight” heading, this is important enough to have a category of its own. “Form factor” doesn’t just refer to the size of the unit, but also its shape and practicality. When you take a look at the G5 next to both portable and home oxygen tanks, it’s not hard to see the benefits the G5 offers.
The Inogen One G5 dimensions are 8.15" H x 7.19" L x 3.26" W. This is comparable to the size of a lunch box or a small portable cooler. But more importantly, it doesn’t have any jagged edges that can get caught on clothing or anything in your environment. The only part that protrudes from the device is the piece that you attach your cannula to. However, this is on the front and top of the device where it’s out of the way.

Oxygen tanks are a huge hassle when it comes to their form factor. The tank itself is long rather than compact meaning you’ll have a hard time fitting it into small areas. Since they’re bulky and heavy, they can be dangerous to store in a closet or in your car. And possibly the worst part about the design of oxygen tanks is that the valves protrude from the tank and they have a lot of jagged edges that can get caught on things. If it does get caught on something, there’s a chance of breaking it and causing a leak. What’s more, if you decide to add additional accessories to your oxygen tank like an oxygen conserver, pulse regulator, or humidifier, it will only add more bulk to it.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
A Variety of Accessories
If you’ve owned an Inogen unit before, you know you can expect high-quality accessories with the release of a new concentrator — the G5 was no exception. Alongside the release of the Inogen One G5 portable oxygen concentrator, we got the custom carrying case, G5 backpack, single and double cell batteries, and the external battery charger.
The great thing about all of these Inogen One accessories is that you know they’re going to be of high quality. Every product Inogen puts out gets their quality seal of approval and if you have any problems with it, you can contact their support and get the issue fixed quickly and typically, with no extra cost to you.

Custom Carrying Case
The G5 custom carrying case is the best way to carry the Inogen One G5. This accessory is simple but offers some extra protection for your device and allows you to carry it on your shoulder without it getting in the way. The leather exterior will protect your POC from scratches, dents, and chips and has mesh material to prevent the device from overheating. If you need to go to the store or visit a friend, this may be the best carrying accessory for you.

G5 Backpack
The G5 backpack is for people who need a little extra space to carry personal belongings and even other G5 accessories. The G5 Backpack is great for anyone who’s going on vacation or taking an extended trip where they’ll need to carry extra batteries and the G5 AC adapter and DC adapter.
External Battery Charger

The external battery charger is another G5 accessory that offers you more freedom wherever you go. Normally, you can only charge your G5 batteries when they’re attached to the concentrator. However, thee external battery charger allows you to charge either the single or double cell battery separately. If you have two batteries, this means you’ll be able to charge them twice as fast!
No Recurring Costs
One of the biggest concerns people have about portable oxygen concentrators is their high upfront cost. While we certainly can’t blame anyone for feeling that way, you’ll be happy to know that there are no recurring costs like there are for portable oxygen tanks. With an oxygen tank, you have to pay every time that you want to refill the unit. This means that you’re going to need to have several backup tanks if you don’t want to go to a refill station every day.
Since a portable oxygen concentrator draws ambient air instead of storing it, you’ll never have to pay to refill it. You may have to replace the sieve bed which removes nitrogen from the air, however, these can last as long as the system itself as long as you take good care of it and wash the filter regularly. Over time, the cost of an oxygen tank will outweigh the initial upfront cost of a portable oxygen concentrator and the high quality and reliability of concentrators is unmatched as well.
Approved For In-Flight Use
As we age, it’s important to make sure we’re able to do all the things we once did. Many people with COPD and other chronic respiratory diseases believe that they need to give up flying if they want to use oxygen therapy. While you cannot, under any circumstances, take an oxygen tank on a plan, most portable oxygen concentrators are approved by the FFA for in-flight use including the Inogen One G5.

The reason oxygen concentrators are safe on a plane and other portable medical oxygen devices aren’t is that they don’t have compressed air. At high altitude, a compressed air tank could explode, injuring anyone near it. What’s more, the Inogen One G5 is small and light enough that it can be stored under the seat during takeoff and landing. The one stipulation is that most airlines require you to have at least 1.5 times the duration of the flight in battery life. This is to account for potential delays in the flight.
Mobile Connectivity
The idea of “connectivity” is a fairly new concept, not just when it comes to concentrators but in general. Essentially what this means is being able to connect your electronic devices such as your laptop, cell phone, or tablet so that they can work together.
Inogen One Oxygen was the first company to apply this concept to oxygen therapy via the Inogen Connect App. This is an easy-to-use app that you can get on any smartphone or tablet device. It allows you to track crucial information about your portable oxygen concentrator without even looking at it. The best part of all? It’s 100% FREE to use!

These are a few of the things you can track through the app:
- Battery status
- Software updates
- cannula and filter maintenance updates
- Column life
- Troubleshooting tips, FAQS, and the user manual
- Oxygen purity status
If you’re someone who’s on the go a lot, there’s no understating the convenience of this app. Instead of having to constantly stop and mess with your concentrator, you can just take a peek at your phone and view this important information. This is especially useful for people with the G5 backpack because the unit will be stowed away out of reach.
Unfortunately, oxygen tanks don’t provide the same connectivity that portable oxygen concentrators do. Since there are no electrical components on these tanks, there’s no way to relay any information to your smartphone or another device. And if there’s something wrong with the tank or the regulator, you won’t know until a professional can inspect it.
Easy Shipping
Another one of the major problems associated with oxygen tanks is how notoriously difficult they are to ship. We already mentioned that they’re not approved for in-flight use, so if you’re planning on going on vacation, you either need to get a portable oxygen concentrator or find an O2 tank at your destination. However, what about when you’re purchasing the unit?
With the G5, you can purchase a unit anywhere in the country and have it shipped to you, no problem. Since it’s such a small and light device, you won’t be paying a hefty fee to have it shipped. On the other hand, many oxygen tank distributors don’t ship their product because of how hazardous it can be. This means you’ll have to drive someplace to purchase an oxygen tank from a local distributor.
.jpg)
Most couriers don’t allow people to ship a full oxygen tank, so if you choose to go that route, you’ll have to go out of your way to get the tank filled up when it arrives. What’s more, since oxygen tanks are so heavy and have such an unusual shape, you may be paying a pretty penny to get it to where you need it to be.
High Oxygen Output
Some oxygen tank owners are anxious when it comes to upgrading to a portable oxygen concentrator because they believe it won’t provide them with the high oxygen output that they’re used to. This is not the case as the Inogen One G5 can go up to a flow setting of 6. That’s the highest flow rate of any POC on the market, and the large majority of COPD patients don’t need that much oxygen.
Since oxygen tanks are measured in liters per minute (LPM) and pulse dose concentrators are measured in flow settings, it’s difficult to compare the two. Ultimately, it will be up to you and your doctor which one will be best for you, but be aware that if a flow setting of 6 isn’t high enough, there are other POCs on the market that go up to a 9.
%20(1).png)
Conclusion
Were you surprised by a few of the things you read on this list? We are too! It’s amazing how far portable medical oxygen has come in the past decade, and it can only get better from here! We chose to take a look at the Inogen One G5 for this list because it’s one of the most advanced and best rated portable oxygen concentrators on the market. However, there are plenty of great POCs out there to choose from so be sure to shop around a bit before making a decision.
You may be wary to invest in an older generation of POC like the Inogen One G3 or G4, but these units have plenty to offer as well. The Inogen One G4, for example, is the lightest portable oxygen concentrator ever produced and the G3 is our pick for the best budget POC on the market. If these are qualities that you’re interested in, take a look and see what else is out there!
If you’re more interested in a device that offers you high flexibility above weight and battery life, you may want to consider continuous flow portable oxygen concentrators. Most continuous flow machines like the SeQual Equinox, SeQual Eclipse 5, and the Respironics SimplyGo also offer pulse flow settings in addition to a higher overall oxygen output. If you’re looking for the full Inogen G5 specs, you can find them here. Otherwise, if you have any questions for us, don’t hesitate to get in touch.
Getting diagnosed with COPD can seem overwhelming, especially when it catches you by surprise. It's often even more overwhelming to get used to all the new treatments, medications and lifestyle changes required to keep your lungs healthy, especially while you're still trying to come to terms with your diagnosis.
As a chronic disease, COPD requires constant work and careful decision-making to keep the symptoms under control. Because of this, it's no surprise that new COPD patients make a variety of mistakes that can affect their health and well-being.
Between making changes to your diet, exercise routine, medications, and many other activities of daily life, there are a lot of opportunities for error. As you adjust to life with COPD, it's important to avoid making mistakes that could serious consequences for your health, or at least catch and correct them early on.

That's why you should learn and pay attention to the mistakes that other new COPD patients tend to make. It helps you learn more about your disease, what to look out for, and how to keep your body and lungs as healthy as possible.
In this guide, we're going to help you avoid common pitfalls by showing you the mistakes that new COPD patients frequently make. Along with each mistake we've provided solutions so you'll know how to avoid that mistake and do the correct thing instead.
By taking the time to learn from others' mistakes, you'll be much less likely to encounter the same problems yourself. In the next sections, we'll give you all the information you need to avoid falling into the same pitfalls that other patients end up in.
However, it's important to remember that mistakes and struggles are inevitable as you adjust to the many changes that getting diagnosed with COPD brings. But if you educate yourself now, you can easily correct these mistakes and avoid serious problems that could permanently affect your health.
A major part of keeping your lungs healthy and keeping your COPD under control is learning everything you can about your disease. It also means being an active, motivated participant in your treatment and knowing what you shouldn't do just as much as the things you should.
The Mistake: Not Using Your Inhaler Correctly

While inhalers may seem like fairly straightforward devices, a surprisingly large percentage of patients don't use their inhaler correctly. This happens to many patients who never learned the proper technique or forgot the correct steps over time. Other patients get too complacent or careless and skip steps to save time, not realizing each step is important.
Most of the mistakes patients make with their inhalers have to do with preparing the inhaler and using the right breathing technique. This is a serious problem, since these steps are necessary for getting the medication into the lungs where it needs to work.
Unfortunately, many doctors don't do their due diligence in training their patients to use their inhalers correctly. Even though doctors are supposed to check patients' inhaler technique at every appointment, it is often rare for them to take the time to do it properly in practice.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
It doesn't help that many doctors don't even know proper inhaler technique themselves, meaning they can't give their patients adequate instruction. Luckily, the medical community has recently acknowledged the extent of this problem and is making efforts to raise awareness among doctors to correct it.
Here are some of the common mistakes to look out for:
- Not shaking the inhaler before each puff
- Not exhaling fully before using the inhaler
- Not holding the inhaler in the correct position
- Not timing your inhale with the spray from the inhaler
- Not inhaling deeply enough
- Not inhaling slowly enough
- Not holding your breath after inhaling the medication
- Inhaling through your nose instead of your mouth
Making any of these mistakes can result in getting too little medication or none of the medication that you need. This can be very dangerous when you suffer from COPD, because you need your full dose to prevent serious symptoms and exacerbations.
The Solution: Learning Proper Inhaler Technique
Because all inhalers are different, the only way to ensure that you're using your inhaler correctly is to re-read your inhaler's instructions and re-evaluate your technique. That means going over all the steps and guidelines in the information packet that comes with your medication.
This is important whether you're a newly diagnosed COPD patient or you have been treating your disease for some time. No matter how well you think you know it, it never hurts to double check.
You should also take your inhaler with you to every doctor's appointment so you can show your doctor exactly how you usually use it. That way, your doctor can identify any mistakes you make and show you the correct technique.
Every time you use your inhaler, make sure you follow every step and don't rush or cut any corners. Don't forget to shake or prime your inhaler if needed, and always remember to exhale before using it.
Timing your inhale with the spray from your inhaler is extremely important, but also difficult, which is why this step tends to cause patients the most problems. It may take some practice to time correctly, and you may need to use a spacer attached to the mouthpiece to help you do it right.

Studies show that when you inhale too early, then you only get about 35% of the full dose you're supposed to get. If you inhale to late, however, you end up spraying the medication in your mouth and throat instead of inhaling it into your lungs. This makes the medication ineffective and puts your lungs at risk.
To make sure you inhale at the right time and get the full dose, start breathing in slowly just before you press the button to release the medicine. Continue inhaling slowly and deeply as you feel the spray to draw the medication all the way into your lungs.
Remember that inhaling the medication isn't the last step; you still have to hold your breath to keep it in your lungs. Most recommend holding your breath for about ten seconds, then you can slowly and gently exhale.
If you are using an inhaler that contains steroid medications, then you still aren't done quite yet. To prevent the medication from drying out your mouth and throat, you need to rinse your mouth out with water before you're done.
If you ever have any questions or concerns about using your inhaler, don't hesitate to talk to your doctor. You can also ask your pharmacist to demonstrate how to use your inhaler(s) or to answer any other questions you have.
You can also find tips and information online for a variety of different types of inhalers. However, this should never be a replacement for the information you can get from your doctor and prescription information.
The Mistake: Not Knowing When to Take Which Medications

Nearly all COPD patients take two major types of medications: maintenance medications and quick-relief medications (also known as rescue medications). Both medications are delivered via inhaler, which is why patients sometimes get them confused.
This can be dangerous, because you need to use both medications correctly in order to treat your COPD effectively and keep your symptoms under control. Mixing up the two medications or forgetting to take them at the right time could make your symptoms worse or cause you to have a serious COPD exacerbation.
Other medications can be confusing to use, too, especially if you are only supposed to take them on certain occasions. For example, many doctors prescribe oral antibiotics and steroid medications for their patients to use as needed to prevent and treat COPD exacerbations.
The Solution: Following Your COPD Action Plan

Every COPD patient should get a COPD action plan from their doctor shortly after getting diagnosed. If you haven't received one yet, ask your doctor to work one up for you, as studies show that they help patients better manage their COPD at home.
A COPD Action plan acts like a set of guidelines for you to follow based on how bad your symptoms are from day to day. For example, most action plans have three major “zones” that correspond to the severity of your symptoms; the first zone is for when you are feeling fine, the second for mild flare-ups, and the third for more serious symptoms and complications.
Click here to see what a sample COPD action plan looks like.
Every day, you should evaluate your symptoms to determine what “zone” to look at. Then, you simply follow the instructions in that zone for what medications and what doses you should take. Most action plans also include guidelines to let you know when its safe to exert yourself and at what point you should call your doctor when your symptoms flare up.
Because most COPD patients have several different medications to keep track of, it's extremely important to take the time to learn all of the important facts about each of your medications. That includes learning their full names, what they look like, and what you are supposed to use them for.

This ensures that you can match your medications with the instructions in your COPD action plan and use them exactly as your doctor directs you to. It also makes you much less likely to mix your medications up, take them at the wrong time, or forget about them altogether.
You should also bring a complete list of your medications with you anytime you go to the hospital or doctor's office. This will make it easier for the medical professionals who look after you to ensure you get the best treatment possible.
It is also important to bring this list with you whenever you travel, especially if you will be taking your medication with you on a bus, train, or airplane. You may need to present your list of medications to travel personnel, and it will come in handy if you need medical attention while you're away from your regular doctor.
The Mistake: Not Quitting Smoking
One of the most important things you can do for your health when you have COPD is to stop smoking. Unfortunately, too many patients believe it's too late for them to quit and continue to smoke even after their COPD diagnosis.
The thing is, even after you've developed COPD, there are still enormous benefits to quitting. In fact, having COPD makes it even more imperative to quit, since continuing to smoke can cause your disease to rapidly get worse.
COPD is a result of reduced lung function, often due to smoking, but continuing to smoke after COPD has set in will only harm your lungs even more. Smoking causes you to lose lung function at an accelerated rate compared to COPD patients who are able to quit.
Reduced lung function will make it even more difficult to breathe, do physical activities, and can significantly reduce your quality of life. If you quit, however, you may even see an improvement in your COPD symptoms, and you can enjoy the lung function and lifestyle you have for much longer.
While quitting smoking cannot reverse the damage that's already been done to your lungs, it can slow down the damage from getting worse. It can also increase your lifespan and reduce the number of exacerbations, flare-ups, and hospitalizations you experience because of your COPD.
Don't forget that quitting can reduce your chances for a variety of other serious health problems as well. For example, you can significantly reduce your risk for heart disease, lung cancer, and stroke if you successfully quit smoking.
The Solution: Making the Decision to Quit

It's important for every COPD patient to understand that it is never too late to quit smoking. Whether you are 25 or 65, you can improve your health and possibly even your lifespan by making the decision to quit today.
It's not an easy decision to make, and it's even harder to actually follow through. However, every year at least 350,000 smokers in the US are able to quit completely, and there's no reason why you can't be one of them.
Although quitting is hard, there are many things you can do to increase your chances of success. For example, using a quit-smoking medication or joining a quit-smoking program can make your quit attempt more likely to succeed.
When you make the decision to quit, remember that you are not alone and there are many ways to get support. First, you should talk to your doctor to see what kinds of medications and support programs are available to help you.
You may want to try nicotine replacement therapy, which is proven to increase smoking cessation rates. There are many different forms available, too, including nicotine gum, skin patches, tablets, oral sprays, and inhalers.
For more information on how to quit smoking, visit the CDC's website for a variety of helpful links and resources. You can also find helpful quit-smoking tips from the American Lung Association's website or from smokefree.gov.
Don't be discouraged if your first, second, or even tenth attempt to quit smoking ends up failing. It takes most smokers at least six attempts to quit smoking, and sometimes up to twenty, before they are able to quit long-term.
As the CDC puts it, “Quitting smoking is a marathon, not a sprint,” and you have to be in it for the long term if you truly want to live smoke free. Even though it is a long and difficult process, it is more than worth the benefits you will receive through improved health, reduced COPD symptoms, and your overall quality of life.
The Mistake: Not Eating a COPD-Healthy Diet

In order to keep your lungs and the rest of your body strong, you need to feed them the nutrients they need. That means eating a healthy, balanced diet every day to give your body fuel to work as efficiently as possible.
Unfortunately, many new patients find that controlling their weight and eating healthy foods is difficult with COPD. The disease can make it difficult to exercise and prepare healthy meals, both of which are vital for a healthy lifestyle.
COPD can make it difficult to lose weight and difficult to gain weight, which is why some patients struggle with being underweight while others struggle with obesity. Either situation is bad for your health and can make it more difficult to breathe.
If you get too few calories and nutrients, then your lungs won't have enough fuel to keep up with your body's needs. However, eating too much and gaining weight puts extra strain on your muscles and lungs, which can also make your COPD symptoms worse.

Also, because COPD makes your lungs less efficient, it means they have to work harder than healthy lungs in order to get enough oxygen to your body. This means that COPD patients need more calories and more nutrients to fuel the needs of their lungs and breathing muscles.
Another danger that many new COPD are unaware of is eating a diet that's too high in carbohydrates. Carbohydrates actually put extra strain on your lungs when digested, because they release large amounts of CO2 that then has to be processed through your lungs.
The Solution: Eating Whole Foods and Balanced Meals

Staying healthy with COPD requires a variety of lifestyle changes, including changes to your diet and eating habits. While this is never an easy thing to do, it can make a huge difference in your mood, your symptoms, and your overall physical well-being.
It helps to work with your doctor or a licensed dietitian to develop a nutrition plan that works for you. However, it is certainly possible to manage a healthy diet on your own by simply eating a balanced diet.
A healthy diet is one that's full of whole foods, which generally means foods made by starting with raw, unprocessed ingredients. These include whole grains, fresh fruits and vegetables, and lean, unprocessed meats like poultry and fish.
To avoid putting extra strain on your lungs, you should also try to limit the amount of carbohydrates you eat to the minimum healthy amount. That means avoiding processed grains, sugary foods, and processed snacks like crackers and chips.
If you want more information on eating a COPD-healthy diet, take a look at any of the several comprehensive guides we've created to help you out:
The Mistake: Not Getting Enough Exercise
It is common for COPD patients to avoid physical activities because it makes it more difficult to breathe. This causes a vicious cycle of inactivity, where the less exercise you get, the weaker your lungs and breathing muscles become, which in turn makes physical activity even more and more difficult to bear.
It doesn't help that COPD can cause fatigue, coughing, depression, and other symptoms that make it difficult to live an active lifestyle. Some patients give up on exercise altogether, which is devastating to their health.
Living a sedentary lifestyle will only end up making your COPD symptoms worse and can even make the disease progress more rapidly. It can also cause you to gain weight, lose mobility, and raise your risk for heart disease and a variety of other COPD complications.
Studies show that COPD patients who exercise and stay active are less likely to experience exacerbations, hospitalizations, and may even live longer than those who don't. That's why it's so important to work through your symptoms and find ways to stay active in spite of your disease.
The Solution: Stick With an Exercise Plan

Even though it may make you feel short of breath, exercise is healthy for your lungs and your overall well-being. It also helps you maintain a healthy weight and keep your physical mobility as you age.
If you have been diagnosed with COPD, then making the decision to stay active is one of the best things you can do for your health. To help keep you on track, work with your doctor to come up with an exercise plan that is realistic and sufficient for you.
If you find yourself struggling for any reason, never be afraid to talk to your doctor or ask for help and advice. If you're finding exercise too difficult because of your symptoms, ask your doctor about attending a pulmonary rehabilitation class, where you can learn how to better manage all kinds of physical challenges that come with COPD.
By keeping up with your exercise plan, you can keep your body toned, your breathing muscles strong, and live a much better quality of life with COPD.
If you need some help getting started, check out the following guides. They contain a variety of practical tips and tricks you can use today to make exercise easier with COPD.
- Home Exercises for COPD
- How Pulmonary Rehabilitation Can Help You Master Exercise with COPD
- Breathing Techniques and Exercises to Help You Manage Your Breathing
The Mistake: Not Conserving Energy

When you have COPD, you have to adjust to certain physical limitations. You will find that, over time, the disease makes many activities that you are used to doing more difficult by making you feel breathless and run down.
Many patients get frustrated when tasks that used to be easy become a struggle, triggering their COPD symptoms and sapping their energy. This can cause significant anxiety, depression, and cause some patients to give up on hobbies and physical activities they enjoy.
However, these problems can be managed by pacing yourself and learning how to better manage your limited energy reserves. Unfortunately, new patients who are still coming to terms with their limitations often deplete their energy quickly during the day, which causes them to live their lives feeling ever breathless and fatigued.
This can be incredibly disheartening for new COPD patients who haven't got the hang of managing their disease. However, by recognizing your limitations and
In this article we are talking about what it means to build new habits, break old ones, and create healthy routines. We will talk about how you can do this successfully, and why it is important for everyone that wants to live a healthy and long life, that cultivating healthy habits is the best way to do it!
The initial steps towards building a healthy routine and good habits can cause a lot of resistance, this is because humans are creatures of habit, therefore any kind of change even if it is good change, is often met with resistance. Resistance starts out as a small hesitation to grow or change, and then you become overwhelmed with it all to the point where you can’t commit to building a healthy routine anymore.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
If you have Chronic obstructive pulmonary disease (COPD) building a health routine includes, taking you medication, accomplishing your oxygen therapy, exercising, eating well, among many other things.
COPD is a progressive and chronic lung disease, and it is treatable. COPD causes breathlessness, either due to inflammation in the airways, excess mucus production, or both. People with COPD are treating their condition to avoid exacerbations, improve quality of life, and of course to reduce the chance of death.
Ironically, COPD is often a result of a lifetime of unhealthy habits, like smoking cigarettes, In fact, the primary cause of COPD is exposure to tobacco smoke. So quitting life threatening habits is one of the steps we will discuss in this article.
In this article we will talk about the steps towards building healthy habits, and if you have COPD, how you can use these techniques to create a routine that helps you maintain your COPD treatment on a daily basis.
The first step to building healthy habits is to “Make it Easy”.
Make it Easy
Successfully implementing lasting changes into your life is hard, period. So, our first pieces of advice is to make it easy. Make the change so small and so easy that you have to do it!
The first step in creating healthy habits that stick, is to make the initial changes very simple. This way, there is no excuse not to do it!
There are two ways you can change, you can work towards quitting a nasty habit or getting in the routine of creating a healthy habit.
For instance, if you want to start exercising more, consider doing a minimal amount of exercise per day, this way you can’t excuse the action one day by saying you’re too tired. This goes back to minimizing the amount of resistance. The amount of exercise you set yourself up to accomplish everyday will be relative to your health, so whatever is doable for you whether that is walking to get the mail, or walking 1.5 miles, make it a point to do it everyday.

If you are working towards cutting something bad out of your life, such as eating fried foods, give yourself as easy alternative. Fried foods can cause bloating and discomfort by pushing on your diaphragm, making it difficult and uncomfortable to breathe. Excessively eating fried food can cause you to gain weight which increases pressure on your lungs. If you eat a lot of fried food, working to eat less fried foods can be a habit that you break.
Make this easy by giving yourself a tasty alternative, that fulfills the craving but isn't as bad for you. For instance, 100 grams of fried and battered chicken breast contains 13.2 g of fat, and over-roasted chicken breast only contains 0.39 g of fat.

Breaking habits along with building healthy ones takes time, start making simple changes to train yourself, and this will help you make bigger changes in the future once you are ready.
The next step to building healthy habits or breaking bad ones, is using incremental steps rather than all at once.
Take Multiple Steps to Reach Your Goals

This is a hugely important step to take when breaking down those sticky habits and in some cases curing addiction. Smoking is one of the leading causes of preventable death worldwide and is responsible for more than 480,000 deaths per year in the United States, which goes to show how quitting smoking is not easy.
if you normally smoke one pack a day, it would be unlikely that within one day you will quit smoking entirely. Nicotine is the most common addiction in the United States, a study by the CDC back in 2015 suggested that while about 70 percent of current adult smokers in the United States wanted to quit, about 55 percent had attempted to do so , but only 7 percent were successful in quitting.

Do not let the statistics deter you from trying! Simply start by quitting a little bit day by day and using supplementary hand and mouth fixation tools. Eventually, you can make a step towards going one full day without a cigarette, and subsequently a few days in a row.
There are thousands of quitting techniques circling the internet, and getting advice from you doctor can help you find a technique that works for you. If you fail the first time, try something else, and just take it one step at a time.
This brings us to the next step, and that is celebrating small victories.
Small Wins and The Snowball Effect

Celebrating the small victories in your journey to create new habits implements self trust into your life. Self trust is saying you are going to do one thing, and having the courage, strength, and honestly to stand by your words with your actions.
Self trust is an important aspect of building healthy habits, and breaking down bad ones. Using healthy routine building tools can help you build a solid foundation of self trust.
To celebrate your small wins you reward good behavior, this generates a snowball effect that can start rolling in a positive direction. The goal is to build a small habit initially, it can be easy at the beginning and by using incremental steps over the course of time, you will succeed. In doing so, you will gain the confidence in yourself and your ability to follow through.
Underwhelm yourself, do not overwhelm yourself. Feeling overwhelmed initiates a stress repose, making it even more challenging to do anything. You can build on the underwhelming feeling, and encourage yourself that more positive change can be done little by little.
Living with COPD is challenging enough, but standing by and not doing anything is worse than challenging yourself to break bad habits and build healthy ones.
As we mentioned above, changing your habits doesn't have to be hard, and in fact, it should be easy when you are first starting to make a change.This means creating an attainable plan of action that is easy to accomplish successfully. From there, you can start taking incremental steps towards a larger goal, this takes time and patience, but it is the best way to stay committed to a goal. Lastly, celebrate the small wins, and encourage yourself to continue doing better.
Health Habits for People With COPD
So now that you know where to start, comes the hard part. Deciding what it is you need in your life, or don’t need, that will improve your livelihood. We drafted a few of the habits that are great for people with any respiratory disease including COPD, you can also discuss with your doctor and decide together what it is you should work towards.

Eating more protein rich foods:
Protein is essential to daily living whether you have a respiratory disease or not. Protein gives you energy, something respiratory patients desperately need in order to get through the day. Protein helps build and repair muscle, tissues, and every cell in your body. It can also strengthen your immune system, making you less susceptible to sickness and infection.
Here are some tips for getting protein into you meals more often:
-
Try to eat 5-6 small meals daily. In each meal make sure that you have protein. You can try these small meal idea to get started:
- Peanut butter and crackers
- Handful of nuts or trail mix
- Apple with string cheese
- Greek yogurt with berries
- Sandwich with hummus and vegetables
- Baked potato with cottage cheese
- Hard boiled egg with whole grain toast
-
Bean burrito
-
Try making a smoothie with protein powder, fruit, and milk, and you can even add peanut or almond butter for an extra serving of protein
- Choose whey, pea, or bean protein for best quality.
- Look at the ingredient list to make sure protein is the main ingredient.
-
Avoid protein powders that have herbs or other foreign or unrecognizable ingredients.
- Try to plan your meals and snacks in advance. This will help if you tend to forget to eat or avoid eating because you do not have a strong appetite.
-
Before bed, have a protein-rich bedtime snack to make sure you meet your daily protein needs
- To increase the protein intake of foods you eat regularly, you can add dry milk powder into milk, oatmeal, overnight oats, or yogurt
Exercise 3-4 Times Per Week
This is a habit that is often met with a lot of resistance, and it is something you should work your way up to before going all in.

If you have COPD and do not exercise regularly, starting to exercise will be a challenge. This is when you have to force yourself to do easy exercise that you can accomplish, rather than setting the bar too high.
If you start exercising too much all at once, you will not feel good, and it can tire you out to the point where you end up quitting entirely.
Depending on your current physical activity, you and your doctor or respiratory therapist can set up an exercise program that will start off slow and steady and gradually gets more intense, until you are at a healthy place, which for people with COPD is often 20 - 30 minutes.
Here is a great resource for exercise options for respiratory patients: Improving Your Exercise Tolerance and Quality of Life with COPD.
Get a Portable Oxygen Device

It is normal for oxygen therapy to start interfering with the quality of your life, and while it is important to cover all of your oxygen therapy needs, you cannot let your oxygen therapy control the quality of your life.
If your oxygen tanks are heavy and bulky, it is harder to exercise.
If you have an oxygen tank you cannot travel with it on airplanes.
You might have difficulty carrying a large oxygen unit on errands and end up spending a lot of time at home.
There are a number of aspects that oxygen therapy has held oxygen patients back from doing, and this does not have to be your reality.
Switching to a lightweight, portable oxygen concentrator unit can make it easier to move around, exercise, travel, and so much more. Activities like going to restaurants, running errands, and even traveling can become a lot more convenient with the help of a lightweight battery powered portable oxygen concentrator.

Education is a very important aspect of buying a portable oxygen concentrator, understanding your condition as well as the device will set you up to succeed throughout your oxygen therapy treatment.
Portable oxygen concentrators costs range in prices, depending on if you need a pulse flow device like the Caire Freestyle Comfort, or a continuous flow device like the Respironics SImplyGo. Prices also depend on the batteries each device is equipped with, its weight, and the technological capabilities.
The best way to learn about your options is to speak over the phone with a respiratory specialist, they can converser with your doctor's office to find out exactly what your oxygen intake is, and from there find the perfect device for you.
Learn Breathing Techniques
Practice implementing breathing techniques into your daily life, it is a great way to control your COPD symptoms.
Pursed-lip breathing can open up your lungs, allowing you to take in more air. The purpose is to strengthen your lungs so you can enjoy more activities without breathlessness.
Follow these simple steps:
- Position your lips as if you’re about to whistle
- Breathe in slowly through your nose and count to two or three
- Breathe out through pursed lips and count to four or five
- Repeat this technique up to five times to control your breathing
- Do this multiple times per day if you have time
You can also discuss with your doctor about the possibility of attending a pulmonary rehabilitation course in your area. This type of rehab teaches you different ways to breathe, and better manage your other symptoms.
Learn Coughing Techniques
Coughing is a common symptom of COPD, however it actually has a useful purpose, if done so correctly.
Oftentimes, your cough can be caused by excess mucus that is trapped in your airways, coughing is the natural reaction your body initiates to clear the mucus. If you work on purposefully coughing correctly to clear your airways, you will experience less involuntary coughing throughout the day a night.
You can work on these techniques in the morning and night, as well as before and after you eat. Hopefully, the more you do it in the beginning, the more productive it becomes.
It is also important to take the necessary steps to prepare for clearing your airways, such as drinking plenty of water which will thin out the mucus, and do not eat food that promotes mucus production, such as having too much dairy in one meal.
Huffing, otherwise known as huff coughing, is a coughing technique that helps move mucus from your lungs and it is similar to exhaling onto a window to steam it up.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Huffing is not as forceful as a cough, but it can work better and be less tiring.
The Huff Coughing Technique:
- Tilt your chin tilted slightly up and mouth open
- Take a slow deep breath to partially fill your lungs
- Hold breath for two or three seconds
- Exhale forcefully, but slowly, in a continuous exhalation to move mucus from the smaller to the larger airways
- Repeat this maneuver two more times
- Follow with one strong cough to clear mucus from the larger airways
- Do a cycle of four to five huff coughs as part of your airway clearance
Accomplishing these huffing techniques enables air to get behind the mucus and separates it from the walls of your lungs so it can be coughed out.
There are a lot of other coughing techniques that can be found in this article: How to Cough Correctly with COPD
Overview
Building healthy habits start with a mind set. You can make positive changes in your life that will greatly impact your ability to do more things, and feel physically and mentally better.
Make the initial changes easy, this way your actions cannot be met with resistance, and accomplishing small goals will lead to your capacity to accomplish large goals.
Develop steps for yourself, when changing a habit or creating a new habit, take incremental steps to get to your desired results.
Lastly, cultivate a sense of achievement, even in your small endeavors. This creates self trust, that will reinforce your ability to change for the better.
.jpg)
If you have COPD, changing your habits may be an essential treatment that your doctor tells you is going to help you live longer, and healthier. Your chronic lung disease will not disappear, but you can take control of it.
We hope that you can use the tactics laid out in this article to make healthy lifestyle changes in all aspects of your life.

Health professionals are some of the most important and trusted members of our society. They’ve gone through many years of schooling and they’ve had to pass rigorous tests that make them qualified to look after our health.
While we can and should hold health professionals in high esteem, it’s important to remember that they aren’t infallible. Just like the rest of us, they are prone to mistakes from time to time.
One mistake health professionals can make is called a “diagnostic error.” This is when a patient receives a delayed diagnosis, wrong diagnosis, or missed diagnosis from a doctor which can lead to a patient using the wrong treatment or no treatment at all.
In this post, we’re going to take a look at how diagnostic errors affect people with lung diseases such as COPD, asthma, and cystic fibrosis (CF). If you have any questions, be sure to leave them in the comment section below and we’ll get back to you as soon as possible.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What is a Diagnostic Error?
According to the National Academy of Medicine, a diagnostic error is the failure to establish a timely and accurate diagnosis of a patient’s health problems or an inability to communicate them effectively. These errors are divided into three groups:
Delayed Diagnosis
This is when a disease is diagnosed much later than it should be. After a delayed diagnosis, patients may have progressed to a point in their disease where it is difficult or impossible to receive certain treatments.
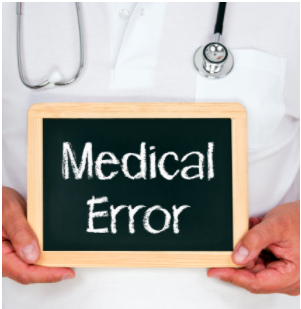
Missed Diagnosis
A missed diagnosis is when a patient has symptoms that are never addressed by a health professional. It’s estimated that 100,000 people in the United States are permanently disabled or die each year due to an illness that was either delayed or missed.
Wrong Diagnosis
A wrong diagnosis or misdiagnosis is when a patient is diagnosed with a condition that they do not have. In a worst-case scenario, a patient is diagnosed with a condition that is less urgent than the condition they actually have. This can lead to the delayed onset of treatment regimes that would improve medical outcomes for the patient.
The Cost of Diagnostic Errors
Diagnostic errors pose a major health risk to people all across the country. According to the Society to Improve Diagnosis in Medicine (SIDM), diagnostic errors are found in 10 to 20 percent of autopsies, meaning that 40,000 to 80,000 people die each year as a result.
![]()
Despite the fact that diagnostic errors affect as many as 12 million Americans every year, there remains a lack of federal funding and research that could help prevent these issues. At this point in time, SIDM is the only organization that is committed to improving the timeliness and accuracy of diagnosis and combating issues associated with diagnostic error.
Another problem with diagnostic error is that it’s very difficult for a patient to take legal action if malpractice is involved. According to Nolo, a legal resource website, medical malpractice cases are some of the most difficult cases a lawyer can take on, especially those involving diagnostic errors.

There are a lot of moving parts in a medical malpractice case and it requires a patient to prove the following:
- A doctor-patient relationship existed
- The doctor did not provide treatment in a timely and skillful manner
- And the doctor’s error resulted in harm to the patient
While this may seem pretty straightforward, there’s a lot of gray area and it requires an attorney to be particularly well-versed in medical jargon and processes. As a result, attorneys often charge a high price for these cases or they will simply turn them down altogether if they believe the case is not worth pursuing. According to the Rosenbaum Firm, even with strong evidence of negligence, patients win an average of 50 percent of medical malpractice cases.
The Role of Diagnostic Error in Lung Disease
Respiratory illness is one of the most common medical conditions in the world. According to the World Health Organization (WHO), chronic obstructive pulmonary disease (COPD) alone accounted for 3 million deaths in 2016, followed closely by lower respiratory infections such as pneumonia.
Not surprisingly, patients suffering from respiratory symptoms can also fall victim to diagnostic error. One of the most common diagnostic errors in terms of lung disease is the overdiagnosis of asthma.and the underdiagnosis of COPD. Since asthma is such a common disease (1 in 13 people have it) it’s not uncommon for health specialists to jump the gun and diagnose it before doing proper testing.
On the other hand, it’s likely that COPD is significantly underdiagnosed because its symptoms are often ignored as a sign of aging. COPD can progress differently depending on the individual, so a patient may experience symptoms for years before finally seeking help. Let’s take a look at some of the top reasons lung disease is often undiagnosed or misdiagnosed.

Similarity of Symptoms
Possibly one of the most common factors affecting the diagnosis of respiratory illness is the similarity of symptoms. For example, the symptoms between asthma and COPD are almost identical making it nearly impossible to diagnose an illness simply based on the symptoms you’re experiencing.
Another problem overlapping symptoms can cause is when comorbidities are present such is the case with cystic fibrosis and bronchiectasis. Cystic fibrosis (CF) is a chronic lung disease that usually begins in early childhood and it’s inherited through genetics. This condition affects the cells that create mucus causing it to become thick and sticky. This leads to coughing, wheezing, and frequent lung infections.
Cystic fibrosis commonly causes a condition called bronchiectasis which occurs later in life. It’s caused by damage and widening of the bronchial tubes which makes it difficult to clear mucus and bacteria from the lungs. If someone has lived with CF their whole life, it may be difficult to recognize the symptoms of bronchiectasis when they appear because they are nearly identical to that of CF.
Errors in Spirometry Testing
Spirometry is a type of lung function test designed to measure how much air you can inhale, exhale, and how quickly you can exhale. While spirometry may seem like a simple test on the surface, it’s actually very difficult to interpret the results correctly. Even a small error in spirometry testing can lead to inaccurate disease diagnosis.

During a spirometry test, patients are asked to exhale for a certain amount of time into a small mouthpiece. This will provide your doctor with two different measurements: forced vital capacity (FVC) and forced expiratory volume (FEV). FVC is the total amount of air you can forcefully exhale and FEV is the amount of air you can exhale in a given period of time.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Once these values are calculated, they are compared to “normal values” based on the patient’s age, gender, height, and weight. If any of this information is entered incorrectly, it could throw off the whole test causing your health specialist to either over exaggerate or under exaggerate the severity of your symptoms.

Aside from issues with interpreting test results, there are also a number of problems that can occur during the test itself. For example, a patient may perform the test incorrectly without the moderator knowing. If the patient does not inhale fully before blowing into the mouthpiece or they have air leaking out the side of their mouth when they exhale, the results could be under interpreted.
Ultimately, there are a lot of different factors involved in getting accurate results from a spirometry test. The test results can easily become skewed if the patient is not aware of how to perform it or the technician conducting the test is careless or inexperienced. When this happens, the results may be misleading or unhelpful when it comes to diagnosing a lung condition such as COPD.
Lack of Appropriate Testing
Another factor that can lead to diagnostic error is a lack of appropriate testing. A medical specialist may not perform the right tests or they may not perform enough tests to get an accurate picture of a patient’s lung condition.
While spirometry is often considered to be the most effective test for diagnosing COPD and asthma, other tests may be more effective when it comes to diagnosing other chronic lung diseases, especially the less common ones.

High-resolution computerized tomography (CT) scanning is one test that can be extremely beneficial in diagnosing lung disease. This is similar to an X-ray, but the computer will take multiple pictures from different angles.
Once the images are collected, the computer uses processing to make cross-sectional images of all the tissues in the lungs. Although X-rays can be useful in diagnosing some conditions, CT scans provide medical specialists with a much more detailed view of what’s going on in your lungs.
CT scans help to provide evidence of things like interstitial lung disease, an umbrella term for diseases that cause scarring (fibrosis) in the lungs. It can also be used to provide additional evidence for COPD and other lung diseases in order to provide a more accurate diagnosis.
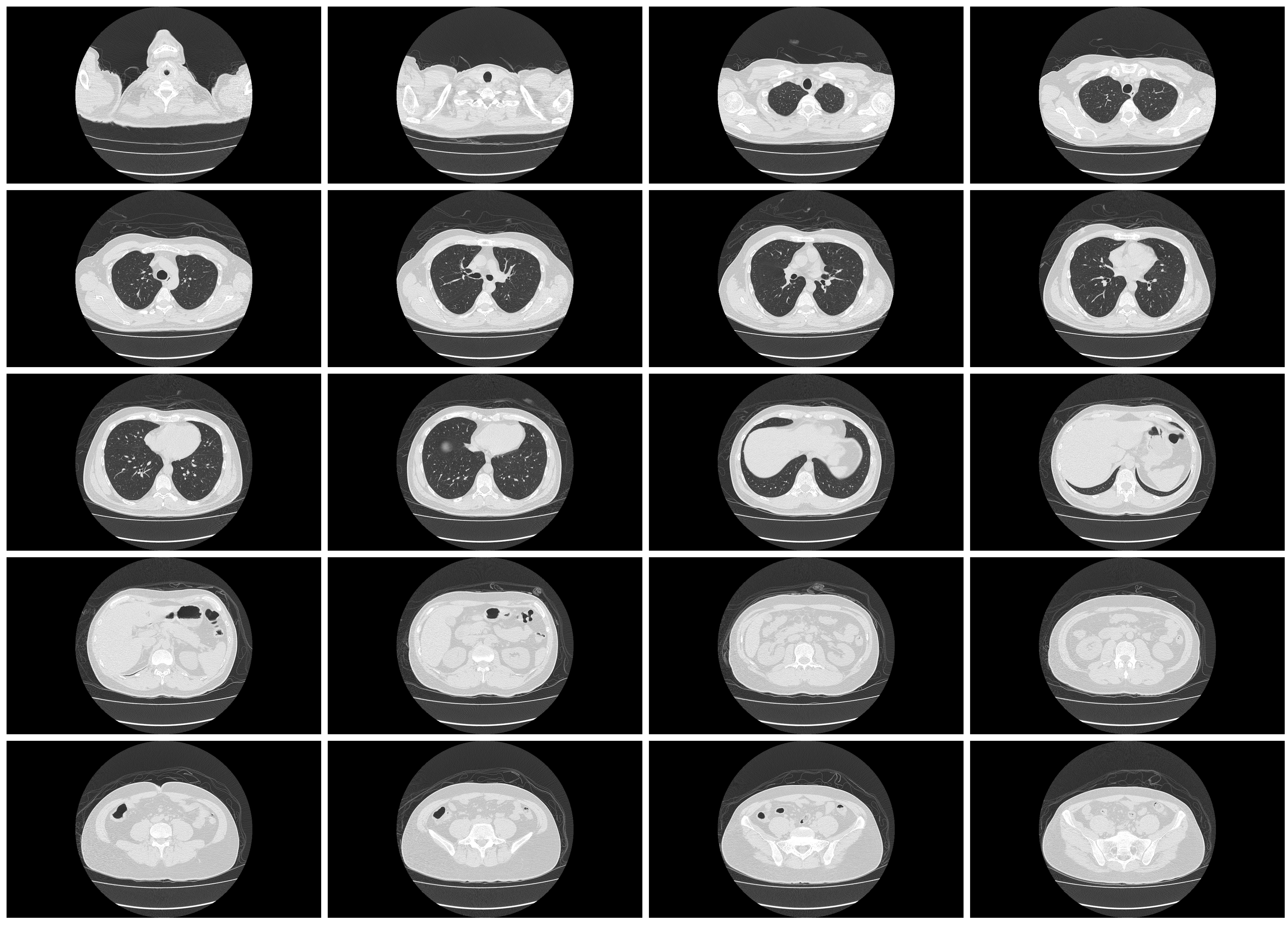
Last but certainly not least, blood gas analysis can be useful in diagnosing many respiratory illnesses. Your doctor will either recommend that you have your blood drawn so that it can be tested in a lab, or he/she might use a pulse oximeter for a less intrusive option. This is a small device that slips over your finger.
Blood tests will provide your doctor with a lot of important information such as your partial pressure of oxygen (PaO2), partial pressure of carbon dioxide (PaCO2), pH, bicarbonate (HCO3), and oxygen content (O2CT).
Threshold for Defining COPD
Threshold is the value that needs to be crossed in order for COPD to be diagnosed. Currently, the threshold for COPD is an FEV1/FVC ratio of 0.70. While this is considered by many to be the most optimal threshold for COPD, there are other methods out there such as the lower limits of normal (LLN) method.

The LLN method uses an additional step of comparing the FEV1: FVC ratio to demographics such as age, height, race, and gender in order to determine a “normal.” A recent study, however, showed that the fixed threshold of 0.70 was consistently more reliable and accurate than LLN and other methods of diagnosing COPD.
If you’re concerned at all about a diagnosis that you did or didn’t receive, it never hurts to discuss them with your doctor. He/she will likely be very open about the methods used to come to a conclusion, and if you still have doubts, there may be an opportunity to get retested or have your doctor double-check the results.
Miscommunication Between Doctor and Patient
Possibly one of the most common reasons for respiratory illness being misdiagnosed is a miscommunication between a doctor and his/her patient. For example, a patient might wait too long to address their symptoms with their doctor or they might forget certain details about their symptoms.

Genetics is also a major determining factor of whether someone can develop a lung disease so if a patient miscommunicates their family’s history of illness, it may be significantly more difficult for their doctor to discover the root of their problems.
There are many mistakes that can occur on the doctor’s side as well. For example, he/she could keep inaccurate information about your height, age, gender, or weight which could skew the results of any test you take.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
What You Can Do to Ensure Accurate Diagnosis
Be Open and Honest With Your Doctor
The best thing you can do in order to prevent diagnostic errors is to be open and honest with your doctor. Unfortunately, when people start experiencing respiratory problems, their first instinct is to shrug them off as a sign of aging or they wait until their symptoms have progressed to a point where they need to seek help.

Alternatively, you should be contacting your doctor as soon as problems arise. Most conditions such as COPD and asthma can be treated more effectively if they are diagnosed early on. These are both progressive diseases, so there is no way to cure them or reduce the damage effects. All you can do is prevent further damage from occurring.
Don’t be Afraid to Ask Questions
Another thing to remember when you go to the doctor is that there’s no such thing as a silly question when it comes to your health. Chances are if there’s something you’re wondering about, there’s always someone else out there wondering the exact same thing. So, when you go in for a doctor’s appointment, don’t be afraid to ask questions, whether they pertain to your symptoms, treatment plan, or anything else.

Another reason to ask a lot of questions is that it gives your doctor a better understanding of your concerns and more importantly, the way your condition is progressing. The more your doctor knows about your respiratory symptoms, the better he/she will be able to prescribe treatments that work for you.
Schedule Regular Doctor’s Visits
Lastly, you’re going to want to schedule more frequent doctor visits. At the end of the day, the more you communicate with your doctor, the easier it will be for him/her to track your progress. And even if you aren’t experiencing severe symptoms, your doctor may be able to diagnose you sooner, leading to better outcomes. It’s recommended that people 30 years old and younger should visit the doctor once every couple of years. But the older you get, the more frequently you should go.
![]()
Conclusion
Diagnostic error is always a possibility. However, you can significantly improve your odds of receiving a timely and accurate diagnosis by scheduling more frequent doctor visits, not ignoring respiratory symptoms, and not being afraid to ask a lot of questions. As a last resort, you always have the option to file a lawsuit if you believe that negligence or malpractice was involved.
Here at LPT Medical, we aim to provide respiratory patients with transparent and helpful resources for managing their disease. If you’re in the market for a lightweight portable oxygen concentrator like the Inogen One G5 or the Caire FreeStyle Comfort, our respiratory specialists would be glad to help you out by answering any questions you may have. Fill out the contact form at the side of the page to get started.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!












