.png)
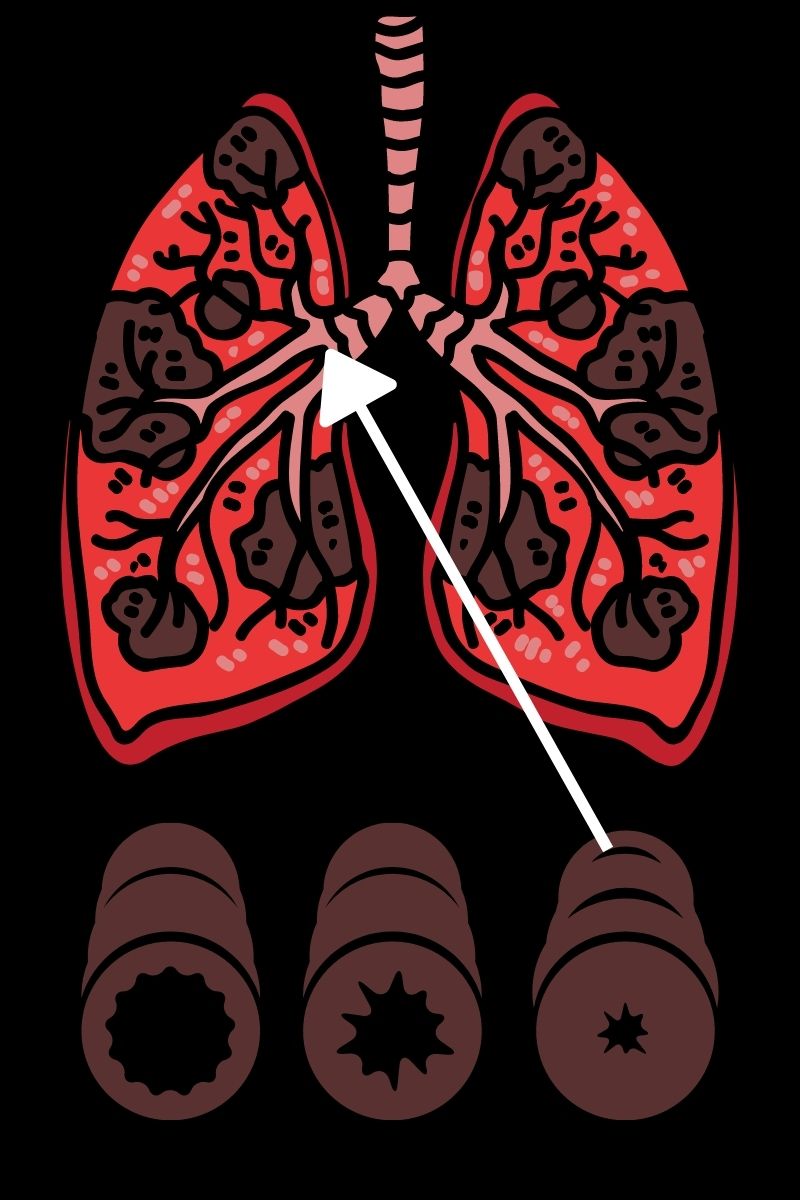
The novel coronavirus has completely reshaped the way that we view sanitation. Over the past year, organizations and individuals alike have taken steps to control the spread of disease, and the population as a whole has become more aware of the impact of infectious disease. Another thing that people have become more aware of is the impact of chronic respiratory diseases such as COPD, asthma, and pulmonary fibrosis. Studies have shown us that these people are “high risk” when it comes to infectious disease, so we need to take steps to protect their health.
Unfortunately, simply telling someone to “clean more often” or “clean more thoroughly” is bad advice. These statements fail to acknowledge that cleaning products themselves can actually put our health at risk. Many household cleaning products are filled with toxic chemicals that can irritate the eyes, skin, and throat. And in the worst cases, they can even contribute to COPD symptoms by exacerbating chest pain, difficulty breathing, and chronic coughing.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
In this post, we’re going to provide you with a comprehensive list of steps for cleaning your home as a COPD patient. We’ll give you advice on choosing cleaning products, how often you should clean, and other things you should take into consideration. If you have any questions, feel free to leave a comment. And if you find this information helpful, don’t hesitate to share it to help us get the word out about safe cleaning habits.
How to Choose Cleaning Products With COPD
The first step in cleaning your home is to choose the cleaning products that you will use. While this may sound like the easiest step, it’s actually the hardest. Cleaning products are rife with volatile organic compounds (VOCs). These are compounds that have a high vapor pressure and low water solubility. Many VOCs are artificial meaning they’re man-made, and they contain chemicals such as methyl tert-butyl ether (MTBE), trichloroethylene, oxygenates, and other industrial solvents.

According to the Environmental Protection Agency (EPA), concentrations of VOCs are up to ten times higher indoors than they are outdoors. This is largely due to the fact that VOCs are found in many household cleaning products and many homes are not ventilated well enough to rid them of harmful chemicals. But VOCs aren’t the only harmful ingredients found in home cleaning supplies. Many of them also contain carcinogens, chemicals that are known to cause cancer.
![]()
As a COPD patient, your goal should be to eliminate all hazardous cleaning products from your home. However, it’s especially important to avoid cleaning products that can exacerbate your respiratory symptoms. Products like air fresheners are particularly harmful to COPD patients because aerosol droplets can remain suspended in the air for long periods of time, meaning they can be inhaled. Generally speaking, “scented” cleaning products should be avoided at all costs. While we may enjoy a fresh smell and equate it with a clean home, most of these products contain harmful chemicals.
Before heading out to the store, create a list of ingredients that you should avoid. The ingredients below are commonly used in cleaning products and should be avoided:
- Perchloroethylene (PERC)
- Formaldehyde
- 2-Butoxyethanol
- Ammonia
- Sodium Hydroxide
- Chlorine
Some common cleaning products you should avoid include:
- Bleach
- Spray cleaners
- Fragrance sprays
- Carpet fresheners
- Fabric softeners
- Varnishes
-
Drain cleaners

Another thing to note is that you should be wary of anything labeled “green,” “organic,” or “eco-friendly.” Just because something is “organic” does not necessarily mean that it is healthy or safe. However, you may see products labeled as “safer choice.” These cleaning products are actually regulated by the Environmental Protection Agency (EPA) and they’re aimed at reducing, eliminating, or preventing pollution at its source. In many cases, these cleaning products can be a safer alternative for COPD patients but many of them still contain chemicals.
How to Make Safe Cleaning Products at Home
Believe it or not, homemade cleaning products can be extremely effective and they can also be much safer to use than store-bought items. When you make your own cleaners, you’ll know exactly what’s in them and you won’t have to worry about reading through and researching a long list of ingredients.

According to Healthline, some of the safest and most effective ingredients you can use to make homemade cleaning products include white vinegar, lemon juice, methylated spirits (denatured alcohol, and baking soda. Unlike the harsh chemicals found in store-bought products, COPD patients typically don’t have any reactions when exposed to these ingredients.

If you want to clean your floor or countertops, combine boiling water with either lemon juice, white vinegar, or methylated spirits. This will make a great degreaser and prove much more effective than a wet rag. If you want to clean a mirror, vinegar and water is a great combination. For removing stains, soda water is your best bet.
Keep Your Home Well Ventilated
Ventilation is imperative when it comes to keeping your home clean. Simply put, ventilation refers to the healthy exchange of air between the inside of your home and outdoors. This prevents harmful chemicals, moisture, and other allergens from concentrating in your home and posing a serious health risk. One of the best ways to ventilate your home is to simply crack a window when you’re cleaning.

If you’re worried about allergens making it into your home through the window, you can install a screen. While this won’t block out all allergens, it will prevent some of the larger particles from entering your home. Another thing you can do is change up the air filters on your HVAC system. The air filter or “particle filter” is designed to remove allergens from the air as it’s circulated throughout your home. However, over time, these filters can become very dirty. Not only will this start spiking your utility bills, but it won’t filter airborne pollutants correctly.
Choose the Right Tool for the Job
Aside from choosing the right cleaning products, you also need to choose the right tools for cleaning your home. COPD is a debilitating condition so you may need to find creative ways of doing things that won’t add any unnecessary strain on your lungs and the rest of your body. For example, if you need to clean in a hard-to-reach area, be sure to use a cleaning device with an extendable handle. This way, you won’t have to strain yourself or risk falling just to clean your home.

If you’ve been prescribed long-term supplemental oxygen therapy, another thing that can help is a portable oxygen concentrator. If you already use a stationary oxygen concentrator or oxygen tank for your oxygen needs, a portable oxygen concentrator will provide you with much more freedom to navigate your home with ease. Rather than having to be plugged into a wall outlet, POCs operate off of powerful lithium-ion batteries so you won’t be relegated to one room of the house.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Portable oxygen concentrators like the Caire FreeStyle Comfort and Inogen One G5 are very lightweight and compact, so you can carry them around all day without feeling exhausted or out of breath. The FreeStyle Comfort even has an ergonomic curve design that will prevent the unit from sliding around at your side while you’re cleaning the house. Once you’re ready for a break from cleaning, simply plug your device into the wall and by the time you’re ready to go again, you’ll have a full battery.

If you’re someone who needs more oxygen to keep you going, the Respironics SimplyGo may be the portable oxygen concentrator for you. This is a continuous flow unit meaning it puts out a constant stream of oxygen rather than “boluses” of oxygen like the FreeStyle Comfort and the Inogen G5. While the Respironics SimplyGo is a bit heavier than these two, it will provide you with more options including the ability to use your POC with your CPAP or BiPAP machine while you sleep.
Don’t Forget to Declutter Your Home
While you’re up and about cleaning your home, it’s also a good idea to spend some time decluttering your home. “Decluttering” simply means reorganizing or getting rid of some of your belongings in order to make your home more comfortable and easy to navigate. This is very important if you’re a COPD patient because having to navigate a messy home can be very challenging and dangerous.

We briefly discussed decluttering in our post about COPD and balance issues, but the basic idea is that you want to create a living space that’s accommodating of your lung condition. First and foremost, you should remove any belongings from the floor that could be a tripping hazard such as clothing, cables, and even furniture. Taking the time to move these things out of the way of where you walk in your home can go a long way toward making your home safer and more accommodating for you and your guests.

If you want to go the extra mile, you might want to consider installing a medical alert system in your home. This consists of a receiver that’s plugged into the wall and a small button that can be worn around your neck. If you take a fall or experience a COPD exacerbation in your home, simply press the button and medical personnel will immediately be sent to your home. These are a must-have for any COPD patient, especially if you don’t have friends or caretakers who visit your home regularly.
Get Outside When You Can
According to the EPA, indoor air pollution can be 2 to 5 times greater than outdoor air pollution. The reason for this is because indoor air pollutants are concentrated in a small area whereas outdoor air pollution can dissipate. While you can and should take the time to clean your home, you should be going outside as much as possible to get some fresh air.

AirNow.gov has a great air pollution map that will give you a good idea of how clean the air is in your area. Simply visit their site and type in your ZIP code. You’ll be given a number anywhere between 0 and 500 with 0 being the least polluted and 500 being the most polluted. It’s recommended that COPD patients avoid going outside if the air quality index (AQI) is over 100. However, people with severe COPD may only want to go outside when it’s below 50 AQI.
.jpg)
While the AQI is a good indication of the air quality in your area, it’s not 100% accurate. If you live in a very urban area with a lot of traffic, the air quality may be lower than what the website tells you. As such, it’s important to use your best judgment before going outside. Try going out when traffic has settled down and try to stay away from the roads as much as possible.
The temperature is another important factor to consider before going outside. Extreme conditions of any kind can lead to exacerbation of COPD. Low temperatures can be particularly difficult for COPD patients because inhaling cold air can thicken your mucus making it more difficult to breathe. Hot temperatures can cause you to feel exhausted more quickly and also exacerbate respiratory problems.
![]()
Schedule a Home Inspection
If you want to take the extra step towards making your home as accommodating as possible for your COPD, you should consider scheduling a home inspection. This is when a professional safety inspector walks through your home and performs a variety of tests designed to determine the safety of your home. While you may think of a home inspector as someone who examines the structural integrity of a home, they also play an important role in determining its cleanliness as well.
One important thing your home inspector will do is evaluate your HVAC system. This includes things like your heater, air conditioner, air ducts, and air filters. He/she will check to ensure that there are no leaks and that your system is circulating clean air throughout your home. The inspector will also look for water damage or plumbing leaks throughout the home that could lead to the growth of mold. Several types of mold, like black mold, can be very hazardous to your health. Black mold poisoning is associated with a chronic cough, fatigue, and irritation in the throat and eyes.

Home inspectors won’t fix these issues within your home. Rather, they provide you with a list of potential problems in your home and advise you on what to do or who to call to get the issues resolved. However, hiring a home inspector is still a very important step because you may be exposed to harmful airborne irritants unknowingly. Many people live with health issues for years only to find out they had a mold or HVAC problem that they were unaware of.
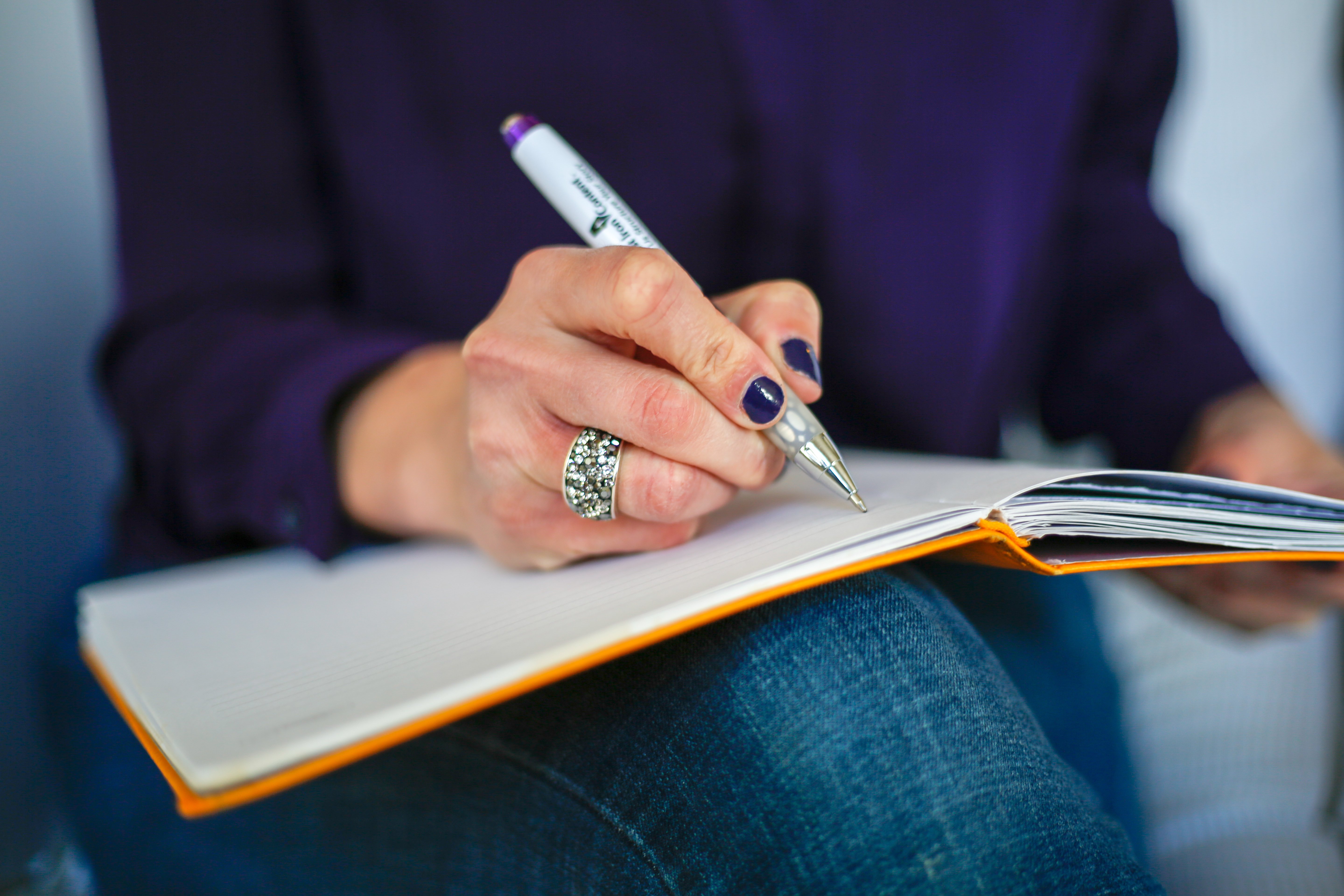
Recruit Help With Cleaning
There’s no doubt about it, cleaning can be exhausting. If you feel like you have a lot to clean and not a lot of time to do it, you may want to start outsourcing work to friends, family, or even a caretaker. While physical exercise is a must for any COPD patient, too much exercise or overexertion can lead to a flare-up in your symptoms, most notably chest pain, breathlessness, and fatigue.
.jpg)
There’s no shame in asking for help with cleaning your home, especially when your well-being is at stake. However, if you decide to recruit help from a friend or family member be sure to let them know about your safe cleaning routine. Let them know that you’re concerned about the chemicals in common store-bought cleaning products and show them how to make the homemade cleaning products we discussed earlier in this post.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Conclusion
Maintaining a healthy living environment is one of the most important things you can do as a COPD patient. Poor air quality in your home will not only irritate your skin and eyes, but it can damage your lungs and lead to flare-ups in your respiratory symptoms. COPD patients who do not breathe clean air are more likely to experience exacerbations that can lead to hospitalization.
Unfortunately, simply cleaning more often or more thoroughly is not the solution. You need to be careful about what cleaning products you’re using and how they affect the quality of air within your home. You should also take additional steps like ensuring your home is well-ventilated and that you’re keeping dust and mold in check.
If you found this post useful, don’t forget to bookmark it so you can refer back to it in the future. And if you have any questions or concerns, please don’t hesitate to leave them in the comment section below
.png)
Chronic obstructive pulmonary disease (COPD) is one of the most prevalent lung conditions, affecting more than 328 million people around the world and an estimated 16 million people in the United States alone.
Despite how common COPD is, it’s often overshadowed by other chronic illnesses like lung cancer, heart disease, and diabetes. A report published by the EMBO Journal found that, while COPD results in about 300,000 deaths per year — nearly double that of lung cancer — it received less than a third of the funding.
While the inequity in COPD research funding can only be addressed through political and social advocacy, healthy lifestyle choices remain the best way to prevent and treat COPD. And in order to make healthy lifestyle choices, you need to stay educated about how your lungs work. There are a lot of things to consider depending on what stage of your life you’re in and whether or not you’ve already been diagnosed with COPD.
In this post, we’re going to address some key facts about aging and how it affects the prognosis of people with COPD and those who are at risk of contracting COPD. In the meantime, if you are interested in getting tested for COPD, be sure to consult your doctor immediately to start discussing your symptoms.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
COPD Takes Several Years to Develop
One of the main differences that sets COPD apart from lung cancer and other chronic illnesses is the rate at which it develops. According to MedicineNet, small cell lung cancer is known to develop extremely quickly and can often result in death within 6 months if it is left untreated.
COPD is very different from this because you’ll see the disease develop over several years or even decades rather than over months. While smoking immediately results in symptoms like coughing, wheezing, and breathlessness, it takes several years before medical professionals can actually associate these symptoms with COPD.

Another factor contributing to the rate of onset of COPD is how many cigarettes you smoke and how frequently you smoke. While researchers aren’t entirely sure what amount of cigarettes will cause COPD, they do agree that even just one cigarette can cause permanent damage to the body.
Many people consider themselves to be “social smokers” because they only smoke when they’re with friends. These people may feel better about their habit because they feel more in control of how much they smoke, but the truth is, they may be at just as high of a risk of contracting COPD as a chronic smoker.

Another risk of being a “social smoker” is that you’re being exposed to a lot more cigarette smoke than you realize. A common myth about smoking is that inhaling second-hand smoke is more dangerous than actually smoking. This is not the case, but it is still equally damaging to inhale second-hand smoke, so you should avoid hanging out around people who smoke.
The key takeaway from this is that your body isn’t going to give you any major warning signs that you have COPD. Long-term symptoms of COPD are similar to the short-term side-effects of smoking which will mask any serious underlying issues you’re facing. The difference, of course, is that the symptoms you experience from COPD are permanent. The best way to avoid COPD is to quit smoking immediately and visit your doctor.
Underdiagnosis and Misdiagnosis are Common in COPD
Diagnostic error is a much more common issue than many people realize. According to Improveddiagnosis.org, an estimated 12 million Americans experience an inaccurate diagnosis in their life, and between 40,000 to 80,000 people die each year as a result of diagnostic errors in hospitals.

These are startling numbers, but you may be surprised to find that people showing signs of respiratory illness are some of the most commonly affected by diagnostic errors. Like we discussed in a previous post, COPD is not always an easy condition to diagnose. Inconsistencies in testing procedures like spirometry can throw off results and miscommunications between doctors and their patients can contribute to this.
One of the most common diagnostic errors is COPD patients being diagnosed with asthma. According to a study published in the National Jewish Health Journal, more than half of COPD patients may be misdiagnosed with asthma. This is not surprising, as both conditions exhibit similar symptoms such as coughing, wheezing, and shortness of breath.

The biggest danger of being misdiagnosed for respiratory symptoms is that you will receive the wrong treatment plan. Asthma is most often treated with fast-acting inhaled medication like bronchodilators which help to open up the airways and prevent asthma attacks. However, COPD treatment is more involved and includes things like supplemental oxygen therapy, long-acting inhaled medication, pulmonary rehabilitation, and an improved diet.
Someone who was misdiagnosed with asthma may live for years without being correctly diagnosed or they may never be correctly diagnosed with COPD. Another way COPD can be misdiagnosed is if a patient is diagnosed with asthma when they’re young. If respiratory symptoms increase with age, they may dismiss them as asthma symptoms, and never seek professional help.

The best way to avoid a missed or delayed diagnosis for COPD is to ensure that you’re always honest and upfront about your symptoms. It’s not normal to have a cough or chest pain that lasts more than a few days and asthma does not necessarily get worse with age. Visit your doctor often and don’t be afraid to ask a lot of questions.
Younger Generations Could be Less Predisposed to COPD
Not all news surrounding chronic obstructive pulmonary disease is negative. You’ll be happy to know that younger generations may be far less predisposed to contracting COPD than their parents and grandparents. This is primarily due to changing regulations surrounding smoking and pollution, and more stigma surrounding smoking at a young age.
![]()
On July 1, 2006, the Colorado Clean Indoor Air Act went into effect which banned smoking in public indoor places. This law was updated in 2019 to include the following:
- E-cigarettes and vaping are now included in the ban
- Originally, smoking was not permitted within 15 feet of a public building; this has been extended to 25 feet
- Exemptions for smoking areas in airports and hotels have been removed
While other states have their own rules and regulations concerning smoking and vaping, generally speaking, the country is moving in the right direction when it comes to lowering the risk of future generations contracting COPD, lung cancer, and other chronic lung conditions.
Another factor to consider is the increased social stigma attached to smoking. In the past, smoking was seen as stylish or cool, but over time, public perception of smoking has changed significantly. A study done by UC San Francisco and Stanford University School of Medicine examined the adolescent perception of smoking in 2001 versus 2015 and found that it’s largely looked down upon.
![]()
This study found that 94 percent of students in 2015 and only 65 percent in 2001 intended not to smoke and that only 17 percent of students believed smoking made them look more mature in 2015, as opposed to 27 percent in 2001.
Changes to environmental regulations could also play a major role in reducing COPD predisposition in future generations. Researchers have found that air pollution like dust, exhaust, fumes, and chemicals can all contribute to the onset of COPD, both in smokers and non-smokers. So, as we see a push towards cleaner or fewer emissions, we should see a corresponding drop in COPD cases all across the country.
Alpha-1 Deficiency Could Lead to Earlier Onset of COPD
Alpha-1 antitrypsin (AAT) deficiency is a genetically transmitted disorder that increases someone’s likelihood of contracting COPD. It occurs when there is a lack of the protein alpha-1 antitrypsin in the blood which the lungs use to reduce inflammation and infection in the lungs. Abnormal genes affect the way that alpha-1 protein is created and excreted from the liver.

Contrary to common belief, alpha-1 deficiency does not cause COPD in and of itself. However, it does make your lungs more susceptible to factors that can cause COPD. In other words, if you have alpha-1 deficiency and you smoke or you’re exposed to high levels of air pollution, you’re more likely to contract COPD, and you’ll likely contract it more quickly than someone without the disorder.
One of the biggest dangers of alpha-1 deficiency is that it’s fairly uncommon with only 100,000 cases in the United States. What this means is that doctors don’t typically test for it and it’s usually only discovered if you happen to have blood drawn for some other reason. AAT plays an important role in breaking down an enzyme called neutrophil elastase which is part of the natural immune response in the lungs. In a healthy person, these enzymes are controlled and cause no threat to the lungs, but in someone with AAT deficiency, it can cause permanent and irreversible damage.
While rare, AAT deficiency simply reinforces the importance of getting tested as early as possible. There are many different treatment options for alpha-1 deficiency including augmentation therapy, which aims to infuse the missing protein directly into the patient’s blood. Other treatment options include vaccinations that prevent infections and an improved diet which promotes healthy lungs and liver.
COPD is Commonly Diagnosed in Late Adulthood
Even when COPD is diagnosed correctly, it’s usually only found in older adults. According to Healthline, of the 8.9 million Americans diagnosed with chronic bronchitis in 2016, 75 percent of them were over the age of 45. There are also stark gender differences with 5.9 million women receiving a diagnosis and only 3 million men receiving a diagnosis.

It’s estimated that about 40 percent of people with COPD have not yet been diagnosed. It’s safe to assume that many of these people are experiencing early stage 1 COPD and they are simply brushing off the symptoms as a sign of aging. However, it’s important to note that chronic coughing or wheezing are never symptoms of normal aging. COPD is often associated with recurring lung infections that can cause this.
No matter what age you’re diagnosed at, COPD treatment will look pretty similar. Since COPD is characterized by progressive lung inflammation and obstruction, your doctor’s primary goal will be to slow the rate of lung decline while simultaneously reduce your risk of exacerbation (a flare-up in your respiratory symptoms).
An improved diet is one of the primary treatments for COPD. Regardless of your age, your body needs a healthy balance of vitamins, minerals, and other nutrients in order to stay healthy. Your lungs depend on these in order to promote healthy blood flow, efficient breathing, and to help control inflammation which can cause chest pain and accelerate the progression of your disease.
Secondly, your doctor will likely set you up with a pulmonary rehabilitation routine. Think of this like a controlled exercise program that’s specifically designed to educate you about your lungs and how to train them for maximum efficiency. Of course, pulmonary rehabilitation will look different based on your age and what your physical abilities are. Ultimately, the goal isn’t to be an all-star athlete, it’s to keep your muscles in shape and improve your endurance so that you don’t feel out of breath so frequently.

Lastly, your doctor will look at medications such as supplemental oxygen, nebulizer therapy, and inhaled corticosteroids. Typically, patients with stage 1 or stage 2 COPD are instructed to use supplemental oxygen for several hours a day, whereas patients with more severe stage 3 or stage 4 COPD will likely need to use oxygen 24/7 in order to receive its full effects. Oxygen is effective at not only reducing COPD symptoms, but it can also reduce the likelihood that you will experience a COPD exacerbation. If you’re looking for an oxygen device for seniors, portable oxygen concentrators tend to be the best option because they offer the most freedom and independence.

A nebulizer is a small device that delivers medication as a mist that can be inhaled. Nebulizers are most often used by younger children or seniors who are not able to effectively time their breathing well enough to use an inhaler. They’re also much easier to use than oral medication which can be difficult to swallow. Some common drugs administered through nebulizer therapy include ipratropium bromide, cromolyn sodium, albuterol, levalbuterol, budesonide, and acetylcysteine.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Managing COPD is More Difficult in Seniors
Potentially the most urgent age-related issue associated with COPD is its effects on seniors. Old age is already associated with a number of issues such as joint pain, muscle pain, fatigue, and chronic health conditions which can only make coping with COPD more difficult. Generally speaking, the older your age, the shorter your life expectancy with COPD will be.
Joint and Muscle Pain
Chronic pain in the joints and muscles is more common than you may think. According to WebMD, about one in three adults have experienced joint pain in the past 30 days and this only gets worse with age. Joint and muscle pain can be brought on by an injury or one of many chronic underlying conditions such as osteoporosis, osteoarthritis, gout, or bursitis.

One of the ways these issues can affect COPD patients, in particular, is through reduced mobility. COPD is considered a debilitating disease meaning it makes you weak and feeble. Osteoporosis, a condition that results in weak, fragile bones, can contribute to COPD symptoms like rib or chest pain.
Respiratory Infections
Influenza and the common cold are two of the most common infections in the world. And as of late, we’ve been introduced to a new type of viral respiratory infection: COVID-19. While anyone can contract these illnesses, they’re more common in older adults and they can be far more deadly, especially when they’re combined with chronic diseases like COPD. According to the American Lung Association, you’re 7.7 times more likely to contract pneumococcal pneumonia (a type of bacterial pneumonia) if you have COPD and you’re over the age of 65.
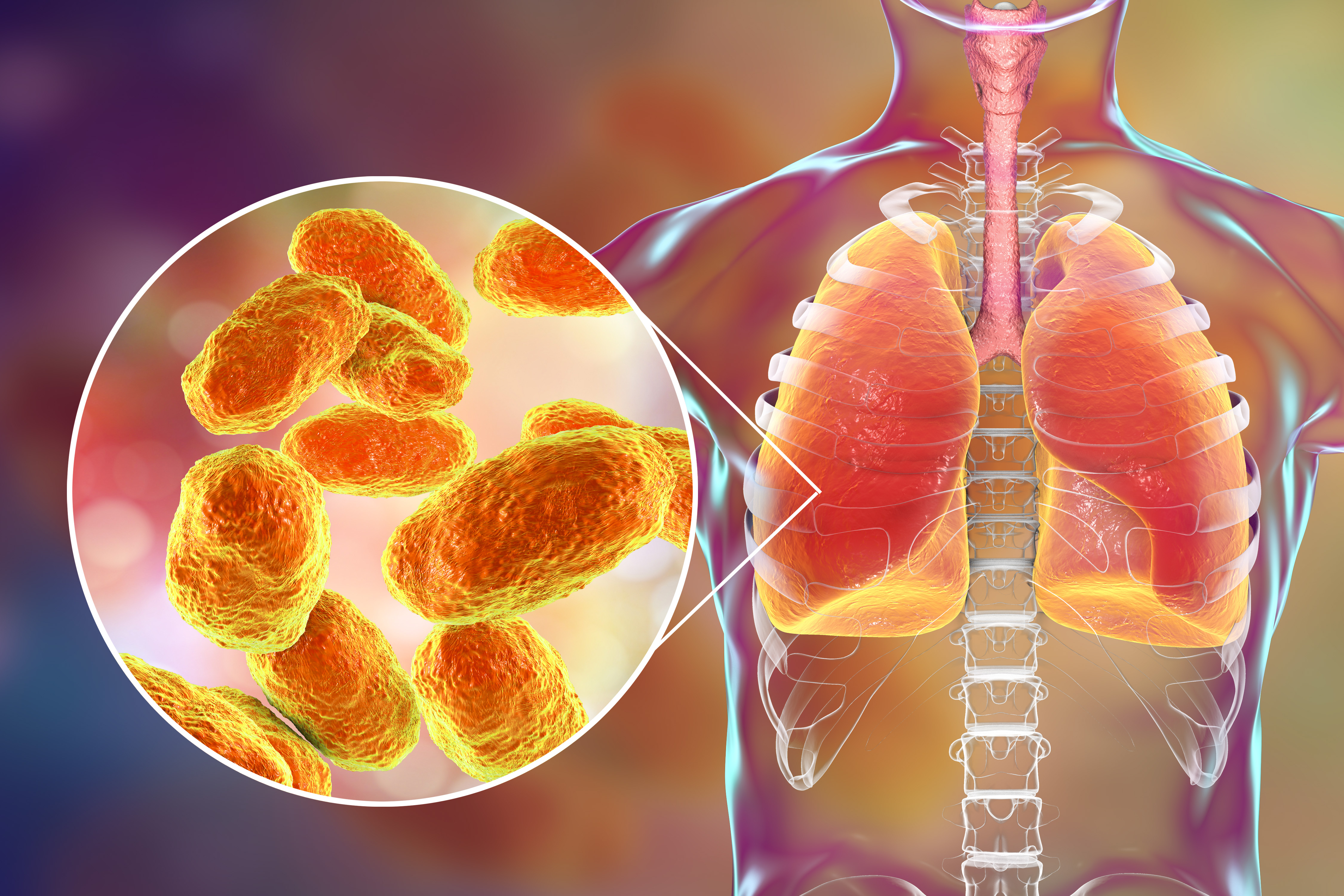
Since bacterial infections are responsible for around 40 to 50 percent of all COPD exacerbations, it is imperative that you do everything you can to avoid acute illness. Cleaning your home regularly with natural and safe cleaners is a great place to start, and you should visit a doctor immediately if you experience any unusual symptoms.
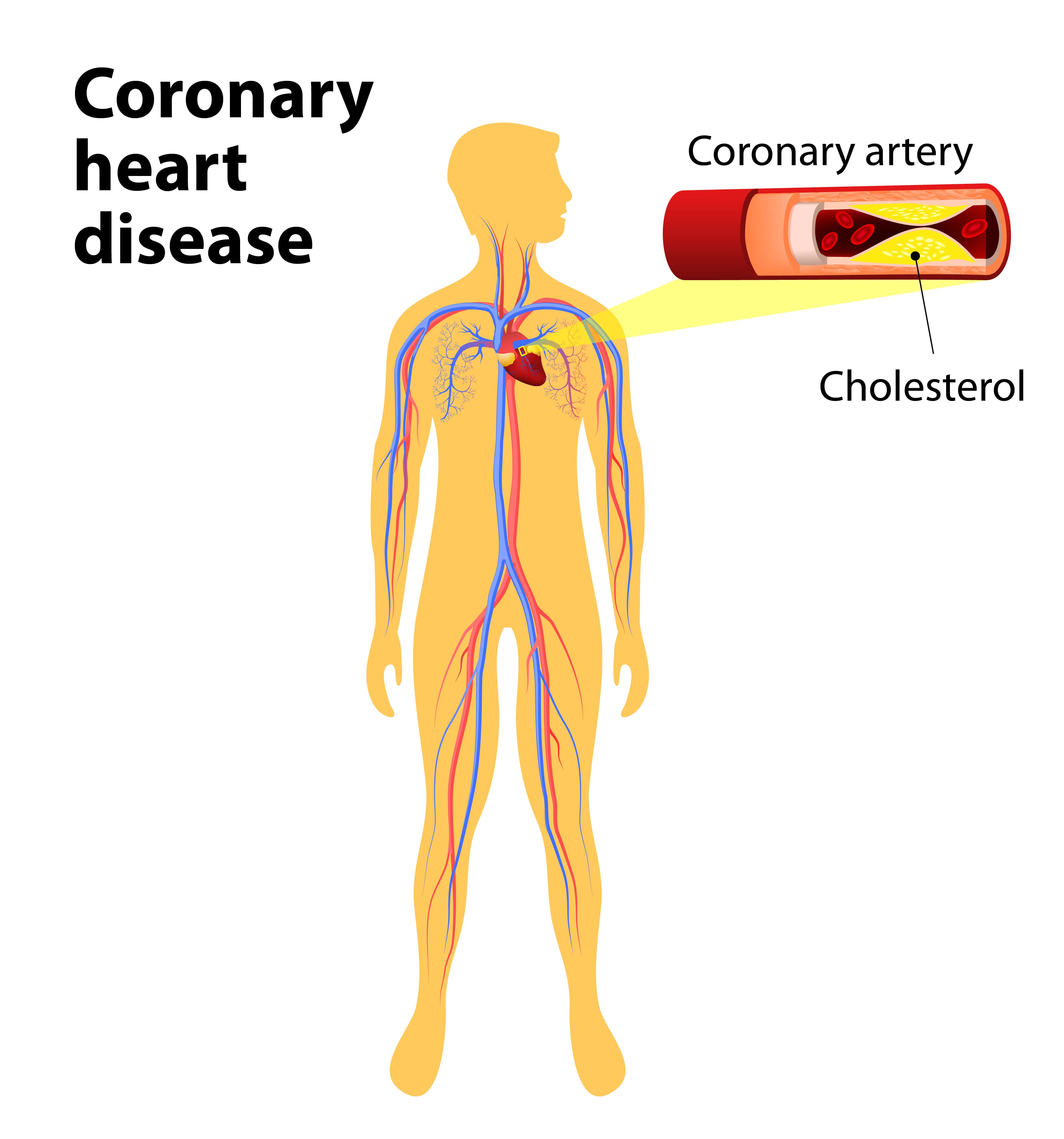
COPD Comorbidities
A comorbidity is a condition that exists alongside another one. Some of the most common comorbidities of COPD include obstructive sleep apnea (OSA), pulmonary hypertension, coronary artery disease, and heart failure. Sometimes, comorbidities can be treated with COPD medication or therapies, but other times, they require a separate treatment plan in order to address the underlying issues.
.jpg)
Obstructive sleep apnea is common. According to sleepapnea.org, between 11 and 19 percent of COPD patients have it and almost half of all COPD patients experience some type of sleep difficulty. If this is the case, your doctor may advise that you use supplemental oxygen therapy, CPAP therapy, or both that night in order to promote restful sleep.
Coronary heart disease is a condition that’s usually caused by the build-up of plaque in the arteries of the heart causing them to narrow and blocking blood flow. Just like COPD, one of the main causes of coronary heart disease is smoking, so it’s not surprising that having chronic bronchitis will raise your risk of contracting it by about 50 percent. Other risk factors of coronary heart disease include high cholesterol, systemic hypertension, and a high body mass index (BMI).
Conclusion
Chronic obstructive pulmonary disease is one of the leading causes of mortality in the world; It’s also one of the most preventable illnesses in the world. Whether you’re a young adult or a senior, it’s important to always make good health decisions and to be more aware of how your lifestyle affects your lungs.
Age has a significant impact on your ability to prevent and treat COPD. Younger generations may be less likely to contract COPD because of the stigma associated with smoking and pollution. On the other hand, seniors with COPD will have a harder time managing their disease than a young person due to comorbidities and other issues caused by aging.
Regardless of your age, your doctor should be the first person you go to if you’re experiencing chronic symptoms. Coughing, wheezing, and chest pain are not normal signs of aging, so if they persist for more than a couple of days, you should schedule an appointment as soon as possible.

We all know that life can be exhausting, but when your exhaustion starts to become chronic, and it feeling tired or fatigued starts to affect other aspects of your life, it is time to take action. There are things you can do to fight off the exhaustion, so you can get back to a more energize state of being.
Exhaustion can impact many aspects of your life including your mood, mental health, physical strength and so much more. Feeling exhausted is not the end all be all, there are habits you can form and habits you can break that can help you get back to feeling more like yourself again.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The first part of fighting off the exhaustion is understanding why you feel this way. If you have chronic respiratory disease like COPD, fatigue is a very common symptom of your disease, but feeling exhausted can also be attributed to other aspects of you habits and daily routine.
Here are some reasons many people find themselves chronically exhausted due to their symptoms:
- Trouble breathing at night
- Excess mucus production while sleeping
- Hypoxemia (low oxygen levels)
However, your fatigue or exhaustion could be attributed to other things unrelated to your respiratory disease.
- Lack of exercise
- Poor diet
- Dehydration
COPD and exhaustion
-jpg.jpeg)
COPD inhibits your lungs from making the proper exchange of gases, therefore your body can’t get the oxygen it needs. With COPD, you develop low blood oxygen levels, a condition called hypoxemia. You can combat the symptoms associated with hypoxemia, like shortness of breath, by using supplemental oxygen. You can administer oxygen with a portable oxygen concentrator or liquid and gas oxygen tank.
Your doctor will write you a prescription that will tell you the exact amount of oxygen you need. It is important that you follow these instructions. If you do not get the oxygen your body needs you will feel tired because fatigue comes more quickly when your lungs can’t properly inhale and exhale air.
Once you start to feel fatigue from a lack of oxygen, you are less likely to engage in physical activity. By avoiding activity, your stamina starts to decline and you can grow tired more easily, this is the toxic cycle exhaustion can manifest in your life, and it is something that you can it avoid or break out of! To get back to a place where you feel more energized and capable, follow the simple steps laid out in this article.
To combat symptoms of fatigued associated with your COPD you will need to follow these 3 basic steps:
- Ask you doctor if you would benefit from using supplemental oxygen at night
- Clear your airways before bed effectively
- Stick to your COPD treatments: Medications, oxygen therapy, diet, and exercise
Supplemental Oxygen

Getting the oxygen you need at night can help you sleep more soundly, thereby helping you feel less fatigued during the day. COPD prohibits you from getting the oxygen your body needs, making it more difficult and laboring to breathe, so taking oxygen therapy during the day can help you feel less fatigued as well.
Depending on your condition, you will be prescribed pulse flow oxygen or continuous flow oxygen. Your doctor will tell you if you need to use your oxygen at night, during the day, or both. This will all be included in your prescription, and you should be diligent to follow the prescription as you would with any prescription medication.
Clearing your Airways
People with COPD and chronic bronchitis often have issues with producing a large amount of mucus. Once mucus starts to collect in your airways, breathing becomes more difficult, and can even result in an infection. There are a few techniques to remove mucus that are often done after using an inhaled bronchodilator medication. The medication helps loosen the mucus and open the airways to make these techniques even more effective. Common techniques used to help remove mucus can be ordered and demonstrated by your doctor.
Clearing your airways of mucus also can help you sleep more soundly allowing you to breathe more easily and reducing the amount of coughing you experience while you sleep.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
There are a number of mucus clearing techniques that you can try that will help you open up your airways.
Deep Coughing: First, take a deep breath. Hold your breath for 2-3 seconds. Forcefully expel your air using your stomach muscles. A deep cough is less tiring and more effective in clearing mucus out of the lungs than merely clearly your throat.
Huff Coughing: Huff coughing, or huffing, is an alternative to deep coughing.. Start by taking a breath that is deeper than a normal breath. Use your stomach muscles to make a series of three rapid exhalations with your airway open, making "ha, ha, ha" sound. Then, perform a series of controlled diaphragmatic breaths followed by a deep cough if you feel mucus moving.
Other Techniques: If you produce a large amount of mucus and huffing nor deep coughing help to clear your airways, your health care provider may recommend other techniques to help clear the mucus.
Your doctor may suggest using a mucus clearing device. There are several types of airway/mucus clearance devices that you can use to remove excess mucus and saliva from your airways. They will come in the form of a mouthpiece, a mask, a vest, etc. and to function they use air pressure, oscillation, or high-frequency sound waves to function.
Postural drainage is a technique that uses gravity to promote drainage of mucus from the lungs.
Any of these airway clearing techniques technique can be ordered and demonstrated by your doctor. Try doing this before bed to sleep without being interrupted by a mucus inducing cough or breathing complications.
Learn Breathing Exercises
One of the reasons COPD patients often feel exhausted, is because they are not getting enough oxygen, yet, you still might not qualify for supplemental oxygen. If this is the case for you, it could be very beneficial to work with a respiratory therapist. These healthcare providers are trained to teach you more efficient ways to breathe, which are often referred to as breathing exercises.
Breathing exercises like pursed lip breathing can improve fatigue by:
- Slowing down your respiratory rate
- Getting rid of the trapped carbon dioxide
- Relieving shortness of breath
A person can try pursed lip breathing during and after any activity that causes shortness of breath and before bed. To do pursed lip breathing work through these 4 steps:
- Breathe through the nose for around 2 seconds
- Purse or pucker the lips, as if blowing out a candle
- Slowly breathe out through the pursed lips for 4–6 seconds
- Repeat the exercise
Follow your COPD treatment plan and Take your Medication
There no cure for COPD yet, but taking the necessary treatment can help reduce your symptoms, including exhaustion. Managing shortness of breath and making it easier to breathe can help you feel less tired during the day and sleep more soundly at night.
Your doctor has probably prescribed medications to help you breathe easier. Common COPD medications include bronchodilator inhalers, which dilate or widen your airways, steroid inhalers, which reduce inflammation in your lungs, and again supplemental oxygen therapy, which relieves shortness of breath if you have low oxygen levels.
Following your own treatment plan along with a healthy diet and regular physical activity or exercise will help combat that feeling of fatigue and exhaustion.
A healthy COPD diet will have all of the nutritional foods that you need to feel more energize. It will exclude foods that make you feel overly full or bloated. Dieting does not mean eating less food, it means eating more food that is good for you, and cutting out foods that make you feel bad. It is still not as easy as it sounds, and dieting takes a lot of practice.
Exercising is the last thing people want to do when they feel weak or fatigued, however without physical actively your muscles and endurance will degrade, making any simple task more of a hassle. Start by doing a small amount of exercise every day, you will notice your stamina start to improve and you will feel a little bit stronger and less tired everyday.
Exercise during the day also promotes a healthier sleep at night, so if you have trouble falling asleep or staying asleep, being more physically active during the day will help.
Other Reasons you Feel Exhausted
Fatigue is one of the most common symptoms of COPD, especially as the disease progresses. Research suggests that about 50 to 70 percent of people with COPD also feel fatigued. Clearly, fatigue often goes hand in hand with COPD, but the reasons for this association are not clear nor does having COPD mean that you will always feel fatigue.

It is important not to chalk up your fatigue to the fact that you have COPD. You can take the necessary action and steps towards a lifestyle where you feel more energized and capable of doing more.
If you are having trouble sleeping for reasons unrelated to your COPD you can start by:
- Getting into a night time routine
- Avoiding caffeine before bed
- Limiting exposure to white light
- Drinking more water throughout the day
- Exercise more regularly
- Eating a balanced diet
- Treating other conditions
Taking action toward these seven steps will help you get on track so that you are sleeping more soundly more often. It is also important to start building up your stamina during the day so you don't feel drained doing everyday activities, you can do this by exercising, eating healthy, and drinking plenty of water.
Overview

As we mentioned above, fatigue is a very common symptom that has been linked to COPD. Excess carbon dioxide, shortness of breath, trouble sleeping, all contribute to feeling exhausted during the day.
By taking action to address other COPD symptoms you are also helping to combat your fatigue. Using your oxygen therapy as prescribed, keeping up with your COPD medication, and treating your COPD effectively will get you back to feeling energized.
While it can be hard to break the toxic cycle the fatigue creates, performing physical activities in some form daily will help you build up your stamina so that eventually everyday activities become doable again. Sleeping better at night will also give your body the refresh it needs to feel more energized during the day.
Sleeping more soundly isn't always easy. Sleeping better all comes down to building healthy habits surrounding your nighttime routine. If you still have trouble sleeping, you should talk to your doctor about your experiences sleeping, they may be able to suggest a remedy that will help you get the sleep you need.
Overall, it is our hope that anyone with COPD can get back to doing what they love. Even in the face of hardship, it is important to stay positive and continue to research ways in which you can improve your wellbeing. It is our goal to get this resource into the hands of people who need it. If you know someone that struggles with COPD and fatigue, please send them this article, and if this helped you in anyway, let us know by commenting below!
%20(1).png)
When we’re younger, we often take for granted our ability to get around with ease. Whether it’s a trip to the grocery store once a week or a month-long trip across the country, there are very few physical limitations setting us back. But as we get older, tasks that used to be second nature to us now become strenuous exercise. This is further complicated by the fact that older adults are more likely to suffer from chronic conditions like osteoarthritis, heart disease, and chronic obstructive pulmonary disease (COPD), all of which are debilitating.
According to Healthline, COPD is most commonly diagnosed in people over 40 years of age. However, the age groups that are most affected by COPD are women between the ages of 65 and 74 and men between the ages of 75 and 84. This is when people tend to struggle the most with mobility because the effects of aging begin to mix with the later stages of the disease. But despite the struggles these patients face, it is possible to regain a significant portion of the mobility that they lost.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
While every case of COPD is different, treatment is usually focused on pulmonary rehabilitation, which is essentially an exercise routine that’s focused on lung strength and education; a refined diet with an emphasis on protein and healthy fats; and finally, supplemental oxygen therapy which is designed to reduce the physical burden on the lungs and maintain blood oxygen levels which leads to improved systemic health.

If you’ve gone ahead and purchased a Caire FreeStyle Comfort, one of the lightest and most powerful portable oxygen concentrators on the market, you’re likely looking to enjoy your newfound freedom by taking a trip of some kind. Since the FreeStyle Comfort is approved by the Federal Aviation Administration (FAA), you’ll be able to fly anywhere in the country or worldwide with your new concentrator. In this post, we’ll go over 7 must-know tips before you travel with your Caire FreeStyle Comfort.
Speak With Your Doctor
Whether you’re taking a flight or a road trip, you should speak with your doctor before you even begin planning. Your doctor will not only provide you with advice on using your oxygen concentrator away from home but he/she will also make sure you understand all other facets of your treatment plan like your diet, pulmonary rehabilitation, and sleep schedule. Be sure to write down any questions you may have before you go in for a doctor’s visit.

Easily the biggest problem many COPD patients face when traveling is falling back or cheating on their new diet. Since your diet is inextricably linked to your lung health, making poor dietary choices can be devastating. Since most people tend to be “on the go” when they’re on vacation, they usually opt for simple snacks or fast food which are usually high in sodium, sugar, and unhealthy fats instead of protein and healthy fats like your COPD diet entails. This can put you at higher risk for exacerbations while you’re away from home.
Another aspect of your COPD treatment plan that might get neglected while you’re traveling is your exercise routine. It can be difficult to find the time to set aside time for important exercises that can boost your strength and improve endurance so your doctor may set you up with a special routine. On the other hand, if you’re going to be up and moving a lot anyways, your doctor may tell you not to worry about pulmonary rehab while you’re gone.
Lastly, you should consult your doctor for information about using your oxygen concentrator while away from home. He/she may have advice for you on adjusting your flow setting based on whether you’re sitting or walking. This way you can conserve battery life and experience more freedom during your trip.
Skim Through Your User Manual
There’s no doubt about it, the Caire FreeStyle Comfort is one of the easiest portable oxygen concentrators on the market to use. There are just three buttons on the user interface: two to control the flow setting up or down and one to turn the device on or off. While you’ll likely get the hang of using this concentrator almost immediately, it’s still a good idea to read the user manual in order to understand its more advanced features.
.jpg)
The user manual will help you get better acquainted with the various audio and visual alarms on the device. For example, there is a symbol when your battery life is getting low or if there is some type of malfunction. By learning these symbols, you won’t have to stress about them while you’re on vacation trying to enjoy yourself. Also, take some time to read through the “troubleshooting” section so that you can fix minor errors on your own while you’re away from home.
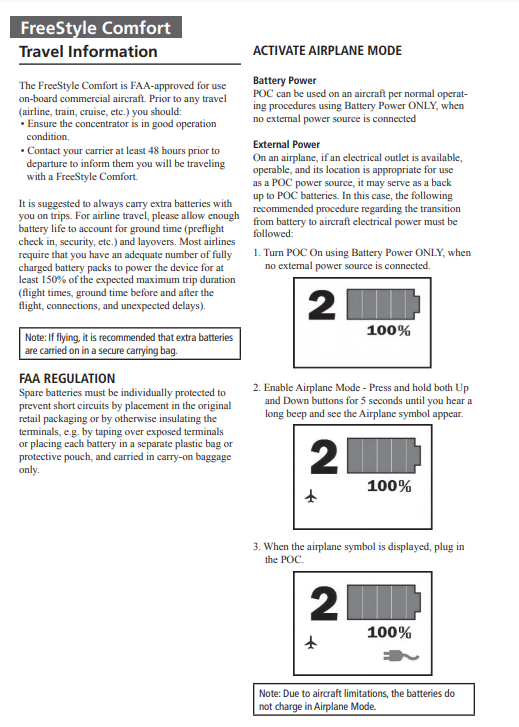
Another section of the Caire FreeStyle Comfort manual that you should pay special attention to is the one titled “Travel Information.” By reading this, you’ll learn some helpful tips for using your portable oxygen concentrator while on a flight including how to put it into airplane mode.
Pack Extra Batteries
Despite the Caire FreeStyle Comfort offering the longest battery life of any pulse dose portable oxygen concentrator on the market, it’s still a good idea to bring extra batteries with you when you travel. With an additional small 8-cell battery for the FreeStyle Comfort, you can double the battery life of your device and only add a small amount of weight. You can even upgrade to a large 16-cell battery and you’ll still be carrying less weight than most portable oxygen concentrators out there.

Another great advantage of these batteries is that they don’t take up very much space. You can easily fit several of them in your backpack or purse while still having room for other personal belongings like your keys or wallet. This is in stark contrast to oxygen tanks which take up significantly more space, not to mention the fact that they’re awkwardly shaped making it difficult to fit them in storage.
Other Accessories to Pack
Aside from extra batteries, there are a lot of other accessories out there for the Caire FreeStyle Comfort that you should consider taking on a trip. First and foremost, you need the AC charging cable. This accessory comes with every FreeStyle Comfort package and allows you to charge your device with any electrical wall outlet. If you’re traveling to another country, be sure to get an adapter to ensure you are able to charge your POC wherever you go.

Secondly, you will need a DC charging cable. This is similar to an AC charging cable but it allows you to charge your Caire FreeStyle Comfort in any car cigarette outlet. Most people don’t realize this, but you’re actually able to use your POC while it’s charging in the car. So, if you’re taking a long road trip you’ll always have a full battery. If you want to get out and stretch your legs or do some sightseeing, you’ll have peace of mind that you have a full battery to work with.

Last but certainly not least, you’re going to want to purchase and bring an external battery charger with you. Normally, you need to have a battery attached to your concentrator in order to charge it, but the external battery charger allows you to charge the battery when it’s not attached. In other words, you’ll be able to charge two batteries at the same time. This is perfect for people who are on-the-go a lot and don’t have much downtime.

For example, if you’re going back to the hotel for an hour or two, the external battery charger will let you charge your batteries much more quickly allowing you have more freedom once you leave. You can also charge two batteries overnight without having to wake up and swap out the batteries on your concentrator.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Learn About CAIREview™ Telehealth Technology
One of the most unique features of the Caire FreeStyle Comfort is its telehealth technology. Telehealth is a practice that’s progressing very quickly in this day and age. Essentially, it means health care professionals providing patients with services over long distances by taking advantage of video communication and other technologies. The Caire FreeStyle Comfort has its own built-in telehealth technology called CAIREview.
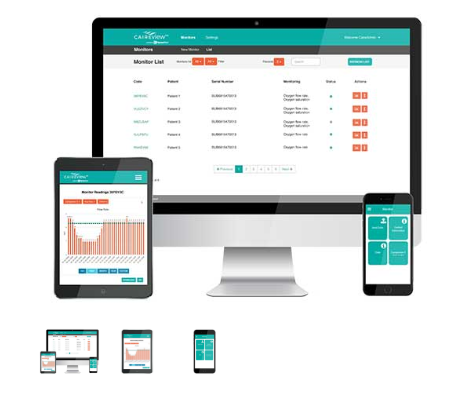
CAIREview is an advanced and cost-effective tracking solution that will help you better understand how you’re using oxygen and how you can improve your treatment. This information can also be shared remotely with your provider who can help you make changes to your routine. What’s more, you can rest assured that this is all done over a secure network that doesn’t share any personal information unrelated to your oxygen usage. To get started, you’ll simply need to install the CAIREview application and connect it wirelessly to your POC.
Decide How You Will Carry Your Device
The way you carry your oxygen device can make a huge difference when it comes to your ability to get around while you’re on vacation. For example, oxygen tanks are so heavy and bulky that the only way to carry them is with a rolling cart. This is not ideal because it can make it very difficult to get up a flight of stairs or move through crowded areas without bumping into people.

If you have a Caire FreeStyle Comfort, however, you will have many different options for how you transport it. Most people choose to use the custom carrying case that comes with the device because it can easily be swung over your shoulder and kept close to your side. The FreeStyle Comfort has an ergonomic curve design to keep it from sliding back and forth as you walk and you’ll have easy access to all the controls on the top of the device.
Another carrying option available to you is the FreeStyle Comfort backpack. With the backpack, you’ll have plenty of extra room to carry things like your keys, wallet, water bottle, or any other supplies you need for traveling. Some people find it more comfortable to carry their POC on their back because it spreads the weight between their shoulders, preventing back pain or soreness. However, it will always come down to your personal preference and what you’re trying to accomplish.

One final way you can carry your oxygen device is with a mobility aid like a wheelchair or rolling walker. Mobility aids are best for older COPD patients who are struggling to get around on their own. If you use a wheelchair, you can hang the concentrator over the back of the chair. Just be sure that there is no slack in the oxygen tubing so it doesn’t get caught on a wheel. Most walkers or “rollators” as they’re often called have a seat that can be used to rest your concentrator on as you walk.
Contact Your Airline Ahead of Time
While the FreeStyle Comfort is approved for all commercial airlines in the United States, you’ll still need to contact your airline of choice 48 hours before your flight. This is because they may have paperwork that you need to fill out about your respiratory condition or your oxygen usage before you can fly. Once you actually arrive at the airport you should also check in with the receptionist at your gate to make sure they’re aware of your oxygen usage. This is just to make sure that there isn’t any confusion or holdups before you have to get on the plane.
.jpg)
Another policy many airlines have is that you need to have 150% of the duration of the trip in battery life. Delays and malfunctions are not uncommon in the airline industry so they simply want to make sure you’re covered in the event that there is a delay. Make sure that you charge some extra batteries the night before you leave and have them in your carry-on bags ready to go.
Conclusion
Supplemental oxygen therapy is one of the most important aspects of a COPD treatment plan. As such, it’s important to be very well prepared before you travel with an oxygen concentrator. This means knowing when to use oxygen, what flow setting to use, as well as following all other aspects of your COPD treatment such as your diet, exercise routine, and sleep schedule.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Fortunately, travel is made a lot easier with a powerful pulse dose portable oxygen concentrator like the Caire FreeStyle Comfort. This POC weighs in at just 5 pounds with the single battery and only 6 pounds with the double battery, it offers up to 16 hours of battery life on a flow setting of 1, and it has a maximum oxygen output of 1,050 ml/min or a flow setting of 5. These are the best specs of any oxygen concentrator on the market, so it’s no wonder that so many people have bought one.

While the Caire FreeStyle Comfort is the best POC for the greatest number of people, we here at LPT Medical understand that everyone has different needs. If you have higher oxygen demands than what the FreeStyle Comfort is able to provide, we are here to help you find exactly what you need. We offer a wide range of continuous flow portable oxygen concentrators such as the Respironics SimplyGo or the Oxlife Independence, as while as a host of stationary oxygen concentrators including the Respironics EverFlo Q and the Inogen at Home.
If you have any questions, please don’t hesitate to contact us by phone or email.
.png)
Whether you have a friend or a loved one with COPD or you have COPD yourself, you can likely attest to the fact that this disease can cause significant problems with mobility. The top causes of mobility issues in COPD patients include poor pulmonary function, leg swelling (peripheral edema), and loss of muscle mass (muscle atrophy). Combined with the effects of aging and other chronic conditions like osteoarthritis, COPD patients can experience a lot of difficulties getting around in their day-to-day life.
Aside from supplemental oxygen therapy, a healthy diet, and pulmonary rehabilitation, another thing that can help you get around are mobility aids. A mobility aid is a device that’s used to help older people and people with chronic conditions walk more easily. They’re often designed to improve balance, reduce physical load, and in COPD patients, they can even help to prevent exacerbations and flare-ups. There is a huge variety of mobility aids and you’re not just limited to choosing one or the other.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In the following sections, we’ll help you better understand the mobility options available to you as well as some other helpful information that will help you maintain your mobility as a COPD patient. As always, if you have any questions, please be sure to address them in the comment section or consult your doctor for more specific information pertaining to your disease and treatment plan.
Why Are Mobility Aids Important for COPD Patients?
According to an article published in the National Center for Biotechnology Information, balance deficit is a common issue among COPD patients. COPD is a progressive disease meaning it becomes worse over time. And as symptoms like breathlessness, chronic fatigue, and chest pain progress, so do issues related to balance and mobility. Believe it or not, studies have shown that COPD is one of the chronic illnesses with the highest rate of falls next to osteoarthritis.
Several months ago, we wrote an article discussing a common complication of COPD called peripheral edema. In short, this is a condition where your legs or feet begin to swell due to a buildup of fluid. One of the root causes of this condition is pulmonary hypertension or high blood pressure in the lungs. High blood pressure in the lungs puts more strain on the heart and prevents oxygen-rich blood from circulating to organs like the liver and kidneys. Since these organs are responsible for removing fluids from the body, swelling of the feet or legs are usually a sign of this happening.
While peripheral edema is a complex condition, it’s one of the issues contributing to the high risk of falls in COPD patients. As the disease progresses, COPD patients don’t just have to deal with increased respiratory symptoms, they have to deal with complications that can result from their disease. Someone with peripheral edema may not even realize they have it because it often comes on slowly and doesn’t cause any pain.
-jpg.jpeg)
Another issue contributing to the high rate of falls in COPD patients is muscle atrophy. In other words, as COPD progresses, patients tend to lose muscle mass from a variety of issues like a changed diet and reduced physical activity. Similar to peripheral edema, a patient may not realize that they are losing muscle mass until they experience a fall. This is why pulmonary rehabilitation is such an important part of any COPD treatment plan.
One final problem that can contribute to the fall rate in COPD is an exacerbation. An exacerbation is an event where respiratory symptoms suddenly worsen. According to COPD.com, the most common cause of exacerbation is a bacterial infection, but air pollution is another common cause. COPD exacerbations can lead to problems walking, balance issues, chest pain, headaches, and confusion, all of which can increase your risk of falls.

While mobility aids are not a replacement for your treatment plan, they play a crucial role in preventing falls, especially in people with late-stage COPD where the disease is the least predictable. Mobility aids don’t need to be prescribed by your doctor so it’s up to you and your loved ones to determine whether you need one or not. Continue reading to learn about some of the mobility options available to COPD patients.
Canes
Walking canes are the oldest type of mobility aid and they’re also one of the simplest. Most walking canes are made of wood or a light metal material meaning they’re easy to carry despite your level of physical impairment. Canes are also widely accessible, and you can buy them just about anywhere, or you could even make your own if you have time. Walking canes are great for taking weight off your joints and providing you with a little extra stability as you walk.

The key to improving your mobility with a cane is to get one that’s the appropriate size. While there is no hard and fast rule as to how you should choose a cane, it should be long enough that you aren’t bending over and straining your back in order to use it and it should be short enough that you can actually lean on it. For most people, this will be somewhere around their hip bone. Luckily, most modern canes are adjustable, so you’ll probably be safe buying one online rather than shopping around for one.

One thing to consider if you want to use a cane is how you will carry your supplemental oxygen device. If you have an oxygen tank and you wheel it behind you using a rolling cart, a walking cane might not be the best option for you because you won’t have any hands free to catch yourself if you fall. A cane is a better option if you carry your oxygen device on your back because it will help you keep a good posture as you walk.
Walkers
Walkers are another mobility option available to COPD patients. There are several different types including traditional walkers, two-wheel walkers, and four-wheel walkers. Traditional walkers tend to be a poor choice for most COPD patients because they need to be picked up as you walk which can be strenuous on your shoulders, arms, and back. Two-wheel walkers provide a little more mobility by allowing you to push the walker rather than lift it. However, for most people, four-wheel walkers, or “rollators” as they’re often called, will be the best option.

Modern rollators are more advanced than other types of walkers because they offer four swivel wheels that afford you more control. They also offer a braking system that’s controlled by two levers on the handlebars on either side of the device. They also provide a padded platform in the middle that you can either sit on or rest your oxygen device, purse, or handbag on as you walk. Some rollators even have a basket in front for added storage.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
It’s a good idea to speak with a mobility aid expert if you want to get a rollator. Since these devices are so popular, there are many different versions and brands available to choose from. What’s more, it’s easier to use one if you’ve been shown how to do so by someone who’s experienced with them. You’ll also need to have one fitted unless you can find one that’s adjustable.
Wheelchairs
When you think of a mobility aid, chances are, wheelchairs are the first thing that comes to mind. They’re commonly used by people who are permanently disabled, but how do they fare when it comes to someone with limited mobility? The answer ultimately depends on your individual circumstances. COPD patients with poor upper body strength may find it difficult to get around in a manual wheelchair, but if you have a caretaker or loved one who can push you around it shouldn’t be a problem.

Another option for you are motorized wheelchairs or “power wheelchairs” as they’re often called. The benefit of investing in a power wheelchair is that you will have the same mobility as a manual wheelchair, but you won’t have to push it with your arms. Power wheelchairs have a joystick that you use to move in any direction. They’re not overly complicated to operate but they can be difficult to transport and you’ll need to keep it charged if you want to stay out of the house for extended periods of time.
Scooters
Mobility scooters are similar to power wheelchairs but they differ in terms of their design. Unlike power wheelchairs which use a joystick, scooters are controlled with handlebars similar to a bike. Scooters can either have three or four wheels depending on what your preferences are. They also have baskets on the front that you can use to store things like your portable oxygen concentrator, a purse, or other personal belongings. Since there are so many options available when it comes to mobility scooters, it’s important to speak with an expert who can align you with the exact product you’re looking for.

Stairlifts
Stairlifts are a mobility aid that many people have never heard of, but they’re incredibly useful. Essentially, a stairlift is a chair that moves up and down a rail that’s installed on a flight of stairs in your home. The chair has a built-in motor that can be controlled with a joystick on the handlebars. This allows you to navigate the stairs in your home without the risk of experiencing a dangerous fall. The one downside to stairlifts is that they can be very expensive and many people can’t justify spending the money to have one installed in their home.

Surprisingly, stairlifts are extremely versatile and can be installed on most staircases regardless of their size or shape. What’s more, if you like to get outside, there are specially designed stairlifts that can be installed on outdoor staircases. They can be installed in several hours so you won’t have to wait days or weeks to start using them.
Will Medicare Pay for a Mobility Aid?
Whenever it comes to medical equipment, questions about health insurance and Medicare are sure to follow. And while it would be nice if Medicare paid for medical expenses like you’d expect them to, it’s never that simple. More often than not, they will cut corners providing you coverage for mobility aids and find any way they can to offer you the bare minimum rather than what you deserve.

In short, Medicare will provide some compensation for manual or power wheelchairs and scooters. Mobility devices like these are covered under Medicare Part B and it is classified as durable medical equipment (DME) the same as oxygen tanks and portable oxygen concentrators. But it’s important to note that not all devices are covered. Medicare has a list of devices that are covered, and some of them require prior authorization. So, it’s best to consult with both the mobility aid supplier and a Medicare representative before you make any decisions.
.jpg)
Another thing to note is that Medicare has a long list of prerequisites that you need to meet in order to qualify for compensation. First and foremost, the doctor that has prescribed you with COPD and the mobility aid supply company needs to be enrolled in Medicare. Additionally, you’ll need a written order from your doctor stating that you have a medical need for a mobility aid. For a full list of requirements, refer to the wheelchair and scooter benefit page of Medicare Part B.
Get a Handicap Parking Permit
Once you have your mobility aid of choice, you may want to consider getting a handicap parking permit. This permit will allow you to park in any handicap spot in the country making it much easier for you to get around. This is especially useful for people who are using electric scooters or power wheelchairs because you won’t have room to unload it in a standard parking spot.

In order to get a handicap parking permit, you’ll need to apply at your local Department of Motor Vehicles (DMV). Every state has different policies but you’ll likely have to provide a doctor’s note which outlines your lung condition and symptoms. You’re more likely to get approved if you can prove that you use an electric scooter or power wheelchair as opposed to a cane or walker so it’s best to put time into finding a mobility aid first.
.jpg)
Last but not least, if you’re given the option between a handicap sticker that goes on your car or a placard that you hang on the mirror, always go with the placard. This is because you can transfer these to any car that you’re in whether it belongs to a family member or friend. Be aware that it is illegal for them to use the placard without you actually being present and most states require you to be recertified for your handicap permit every couple of years.
Conclusion
Making the decision to use a mobility aid is an important step for many COPD patients. People with chronic respiratory conditions are at a higher risk of experiencing falls than the general public, but mobility aids will help to support your balance whether you’re inside or outside the home. Unfortunately, there is no one-size-fits-all solution. Everyone has their own needs and preferences so you should consider all options available to you.
Canes and walkers are a good place to start because they’re affordable and they’re easy to carry. However, you may want to consider a more long-term solution like a mobility scooter or power wheelchair. These devices are generally safe and easy to use, and they will make it easy to carry around your oxygen devices such as your oxygen tank, liquid oxygen tank, or portable oxygen concentrator.
Lastly, you should check with your health insurance to see if your mobility device is covered. This could save you hundreds if not thousands of dollars. You can also file for disability and receive a handicap parking permit which will afford you more convenience and freedom whenever you leave the house. In the meantime, if you’re looking for a lightweight and easy-to-use portable oxygen concentrators such as the Caire FreeStyle Comfort or the Inogen One G5, don’t hesitate to reach out to your respiratory specialists here at LPT Medical.
Whether this is your first time in the market for an oxygen machine or you’re looking to upgrade your old, outdated oxygen tank, there’s never been a better time to look into oxygen concentrators. Unlike oxygen tanks which offer very little in the way of options, you may find yourself slightly overwhelmed by everything that concentrators have to offer.
Usually, the best place to start is to simply understand what you want out of an oxygen device. For example, you may want a unit that you can take on a plane with you or on a road trip across the county. Or you might be looking for an oxygen concentrator that’s quiet enough to take to the library or a church service.
Regardless of your preferences, however, there are certain qualities that everyone should look for in an oxygen concentrator. In this post, we’ll discuss the most important things to look for and why. If you have any questions, be sure to address them in the comments section or fill out the contact form at the side of the screen so that one of our respiratory specialists can reach out to you.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Backed by a Reputable Brand
Easily one of the most important things to look for in an oxygen concentrator is that it’s backed by a reputable brand. In this day and age, it’s possible for anyone to get online and start selling things. While this may be beneficial if you’re wanting to start a business, it makes it much more difficult for buyers to gauge which sellers are reputable and which ones are not.

When it comes to oxygen concentrators, this issue is amplified. Respiratory patients want to find reliable medical equipment that will meet their oxygen needs, but at the same time, they’re unacquainted with the industry and how it works. This can lead to people investing in untrusted or inexperienced oxygen brands.
Fortunately, there’s a great way to avoid this problem: take the time to research reputable oxygen companies before looking at specific oxygen concentrators. The most respected brands tend to be companies with 5 or more years of experience producing medical equipment like CPAP or BiPAP machines, oxygen equipment, and oxygen accessories. They also tend to have positive reviews from customers on their social media pages and the Better Business Bureau (BBB).

If you don’t want to take the time to research each company, you can reach out to an authorized oxygen reseller like LPT Medical. We have an A+ rating with the BBB and we’re committed to only selling oxygen equipment from the most reputable brands in the industry. In fact, our most popular brand, Inogen Inc. is widely considered to be the best portable oxygen concentrator manufacturing company in the industry.

There are many other great oxygen concentrator companies out there such as AirSep, which is known for creating the lightest portable oxygen concentrator in the world. Respironics, inc. is another well-known oxygen concentrator company that got its start in the 1970s selling CPAP and BiPAP machines.
Oxygen Output
The second most important thing to look for in an oxygen concentrator is its total oxygen output. Unlike oxygen tanks which can be adjusted to any oxygen output that you need, oxygen concentrators are slightly more limited. So, when you’re buying an oxygen concentrator, you need to first make sure that the device is able to maintain your oxygen saturation. The good news is that there is an oxygen concentrator for just about everyone out there, no matter how severely their lungs are impaired.
First and foremost, you should ask your doctor or pulmonologist how many liters or milliliters of oxygen you will need per minute. Also, be sure to ask him/her whether continuous flow or pulse flow would be best. A continuous flow oxygen concentrator works similar to an oxygen tank where oxygen is put out in a constant stream, whereas pulse dose concentrators only put out oxygen when you inhale.

Once this is done, you can start to weed out oxygen concentrators based on whether they meet your needs or not. This can be a difficult process, so it’s best to simply call one of our respiratory specialists who will be able to sort it all out for you and provide you with a list of options that will work best for you.
Portability
Portability refers to how easily a device can be moved around and carried. Oxygen concentrators vary widely in terms of portability because they’re all built differently. Home oxygen concentrators, for example, weigh anywhere from 18 to 50 pounds making them impractical for taking with you outside. They also need to be plugged into an electrical outlet in order to be used. However, they do have wheels on the bottom of them so that you can transport them from one place to another.

Continuous flow portable oxygen concentrators are much more manageable, weighing in around 10 to 20 pounds. This makes them much more practical for taking out of the home with you, and since they don’t need to be plugged into the wall at all times, they will provide you with much more freedom and independence.

Finally, pulse dose portable oxygen concentrators are the lightest and most portable oxygen devices on the planet. Due to additional technology inside these devices, oxygen manufacturers can make them much smaller, lighter, and more manageable all around. The average pulse flow portable oxygen concentrator weighs under 6 pounds making them perfect for carrying on your shoulder or in a backpack.
Battery Life
Battery life is another major factor to consider when you’re purchasing an oxygen concentrator. As you can imagine, battery life varies widely based on the size of the concentrator, delivery type, and the oxygen setting that you’re using. Generally speaking, continuous flow oxygen concentrators have a shorter battery life than pulse flow oxygen concentrators because they put out more oxygen. Also, the higher the oxygen setting you’re using, the less battery life you will have.

Everyone will have different needs when it comes to battery life. For example, someone who just wants to be able to go to the grocery store or visit a friend may only need a few hours of battery life. Whereas someone who wants to be able to take long flights across the country will need much more battery life.

Your oxygen needs are also an important factor. The double battery for the Inogen One G5, for example, can last up to 13 hours on a flow setting of 1. However, if you need to use a setting of 6, it will last only about 3 hours. If you want to, you can even carry extra fully charged batteries with you wherever you go and simply replace them when they get low.
Ease of Use
One problem that many oxygen patients report about oxygen tanks is that they’re difficult to use. Components can often be fragile or fidgety making it difficult for patients to know whether they’re getting the oxygen they need. What’s more, if something goes wrong with it, it may be difficult or impossible to fix problems on the fly without the help of an expert.

Fortunately, oxygen concentrators are usually not like this. Depending on the oxygen company that you buy from, you can expect your oxygen device to last anywhere between 5 to 7 years with very little maintenance. Most oxygen concentrators have at the very least a 3-year warranty meaning if there are any defects within that time period, you can send it back for free repairs or a full replacement.

Since oxygen concentrators are electronic devices, you’re going to want to find one that has a simple and easy-to-use interface. The Inogen One G5, for example, only has five buttons on it; two to control the oxygen flow; one to turn the device on or off; one to control the volume; and one to change the alarm settings. This is ideal for people who are always on the go because you never have to hassle with checking the manual constantly to figure out how to operate the device.

Another thing to look out for when it comes to ease-of-use is the battery. Oxygen generators like the Inogen One G3 and Inogen One G4 have very accessible batteries that can easily be replaced when you’re on the go. However, other concentrators have built-in batteries that can be much more difficult to replace.
Cost
Cost is never an easy subject to discuss when it comes to choosing an oxygen concentrator. On one hand, you want to get a high-quality oxygen device that will last you for years to come, but on the other, you don’t want to break the bank and spend more money than your budget allows. Oxygen concentrators differ from oxygen tanks in that they’re a lot more costly to produce, but in the long run, they can save you a substantial amount of money.
.jpg)
Think about it this way: a standard oxygen tank will only run you a couple of hundred dollars, but you’ll need to pay to have the tank refilled several times a week. This can easily run you hundreds or thousands of dollars a year depending on how much oxygen you use. Alternatively, if you choose to fill your own oxygen tanks, you’ll need a home fill station. These can easily run you $2,000 or more depending on where you buy from.

While oxygen concentrators have higher upfront costs, they more than make up for the cost over years of use. Unlike oxygen tanks, oxygen concentrators don’t need to be refilled. Simply recharge the battery and you’ll have access to oxygen wherever you need it. There isn’t much in the way of short- or long-term maintenance for most oxygen concentrators because they’re built to be durable and hassle-free. It is recommended, however, that you clean the air filters regularly because this will ensure the device is free of dirt and grime that could reduce its lifespan.

When you decide that oxygen concentrators are the best choice for you, you’ll have several different ways of saving money. First and foremost, you can purchase a used or refurbished oxygen concentrator. Refurbished machines are typically sent back to the manufacturer or a specialized retailer who can check the machine for damage and make repairs.
Another way to save money on an oxygen concentrator is to wait for a sale. This can be a great way to save a couple of hundred dollars on a new or used machine, but it’s important to remember to keep your health top of mind. It’s not worth waiting months or years for the right sale if it means putting your health at risk.

Lastly, some retailers will give you the option to pay for your oxygen concentrator through financing. This is the perfect way to pay for your oxygen device in a more manageable way through monthly installments. The one catch to using financing is that it usually requires a credit check, so if you have bad credit, you’ll need to find a friend or family member who does.
Additional Features
If you’ve taken the time to narrow down your search to several concentrators, it’s time to look into the additional features that the oxygen concentrator offers. By “additional features” we’re referring to things that aren’t necessary but may offer additional convenience or comfort. For example, the Caire FreeStyle Comfort is a pulse flow portable oxygen concentrator with something called CAIREview™.

CAIREview™ is a telehealth service that allows oxygen patients to stay connected wherever they are in the world. Powered by SynsorMed, this is a cost-effective oxygen tracking method that can be accessed by you, your doctor and your oxygen provider and provides detailed information about your oxygen usage including:
- Tracking the location of your CAIRE oxygen device
- Monitoring oxygen flow rates
- Troubleshoot alerts and email alerts
- Ensure proper equipment utilization
The great thing about CAIREview is that it’s one of the first telehealth options for patients who rely on oxygen throughout their day-to-day lives. In the past, doctors would provide patients with instructions for how much oxygen to use and when, but there was no effective way to ensure this was being done properly. CAIREview allows doctors to have 24/7 up-to-date information about their patient’s usage over a secure network. To get started, simply install the app on your smartphone and follow the instructions to connect to your Caire FreeStyle Comfort.

Another additional feature you may be interested in is the Inogen Connect. Like CAIREview, this is a mobile phone application that you install and connect to your concentrator via Bluetooth technology. Once it’s connected to your Inogen One G4 or Inogen One G5 device, you’ll be able to track realtime information about your oxygen concentrator including battery life and flow setting. You’ll even be able to access your device’s user manual and view troubleshooting information which can be very convenient if you’re away from home. Unlike CAIREview, however, Inogen Connect does not send information directly to your doctor or oxygen provider.
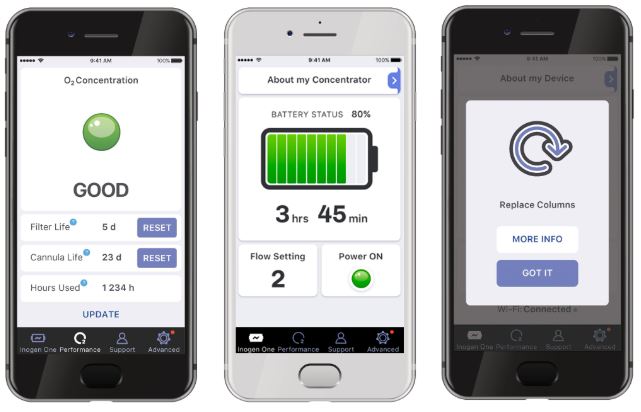
In the grand scheme of things, telehealth is a pretty new concept. However, oxygen companies like Inogen Inc. and Caire Inc. are taking steps to make these services more widely available to oxygen users all over the world. Telehealth services have proven especially useful in ensuring that everyone’s health is accounted for even given the current circumstances. If you’d like to learn more about telehealth services and how they’re improving the lives of COPD patients, check out this blog post.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Conclusion
Choosing the right oxygen concentrator is not always easy. Everyone has different wants and needs, so it’s impossible to provide a one size fits all solution and call it a day. If you’re just beginning your search, it’s imperative that you speak with your doctor or pulmonologist to see exactly how much oxygen you need and how often you need to use it.
Once this is done, you can start researching oxygen companies and retailers to determine which one is the most dependable. Be aware that you need to have a prescription from your doctor in order to purchase any type of oxygen device, so if you’re offered a “cheap” oxygen concentrator without providing proof of oxygen use, it’s likely a scam.
If you’re still having trouble finding the right oxygen concentrator, don’t be afraid to reach out to our respiratory specialists here at LPT Medical. We’ll walk you through all of your options ensuring that both your medical needs and your personal preferences are taken into account. To get started, simply fill out the contact form at the side of the page and we’ll reach out to you.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!












