.png)
Whether you have chronic obstructive pulmonary disease (COPD), asthma, cystic fibrosis, or any other type of respiratory ailment, your doctor may prescribe you with a device called a nebulizer. Nebulizers are one of many different types of inhaled therapy devices and can provide you with considerable relief from respiratory symptoms such as shortness of breath, coughing, and wheezing.
While nebulizers are an effective treatment option, they aren’t for everyone. A nebulizer should only be used if and when your doctor prescribes it and should only be used for its intended purposes. Since nebulizers use medication, incorrect usage of the device could pose a serious risk to your health, especially if you’re using it too frequently.
In the following sections, we’re going to provide you with all the information you need to get started with nebulizer therapy like how to use a nebulizer, how to clean it, and other things you should consider before getting started. If you have any questions, feel free to leave them in the comment section or speak with your doctor.
How Do Nebulizers Work?
A nebulizer is a form of inhalation therapy, meaning you’re inhaling medication instead of taking it orally or intravenously. For someone with a respiratory condition, inhalation therapy is considerably more effective than the alternatives because the medication reaches the affected area almost instantaneously. This is especially important for someone experiencing a COPD exacerbation or asthma attack because expedited treatment could have life-saving results.

When you use a nebulizer, liquid medication is transformed into a fine mist called aerosol. The aerosol lingers in the mouthpiece or face mask so you can simply breathe normally to receive the treatment. If someone has severe COPD or asthma, other inhaled therapy like metered-dose inhalers (MDIs) may be ineffective because they require a deep and coordinated inhalation for the medication to reach the lungs. With a nebulizer, however, even shallow breathing will help.
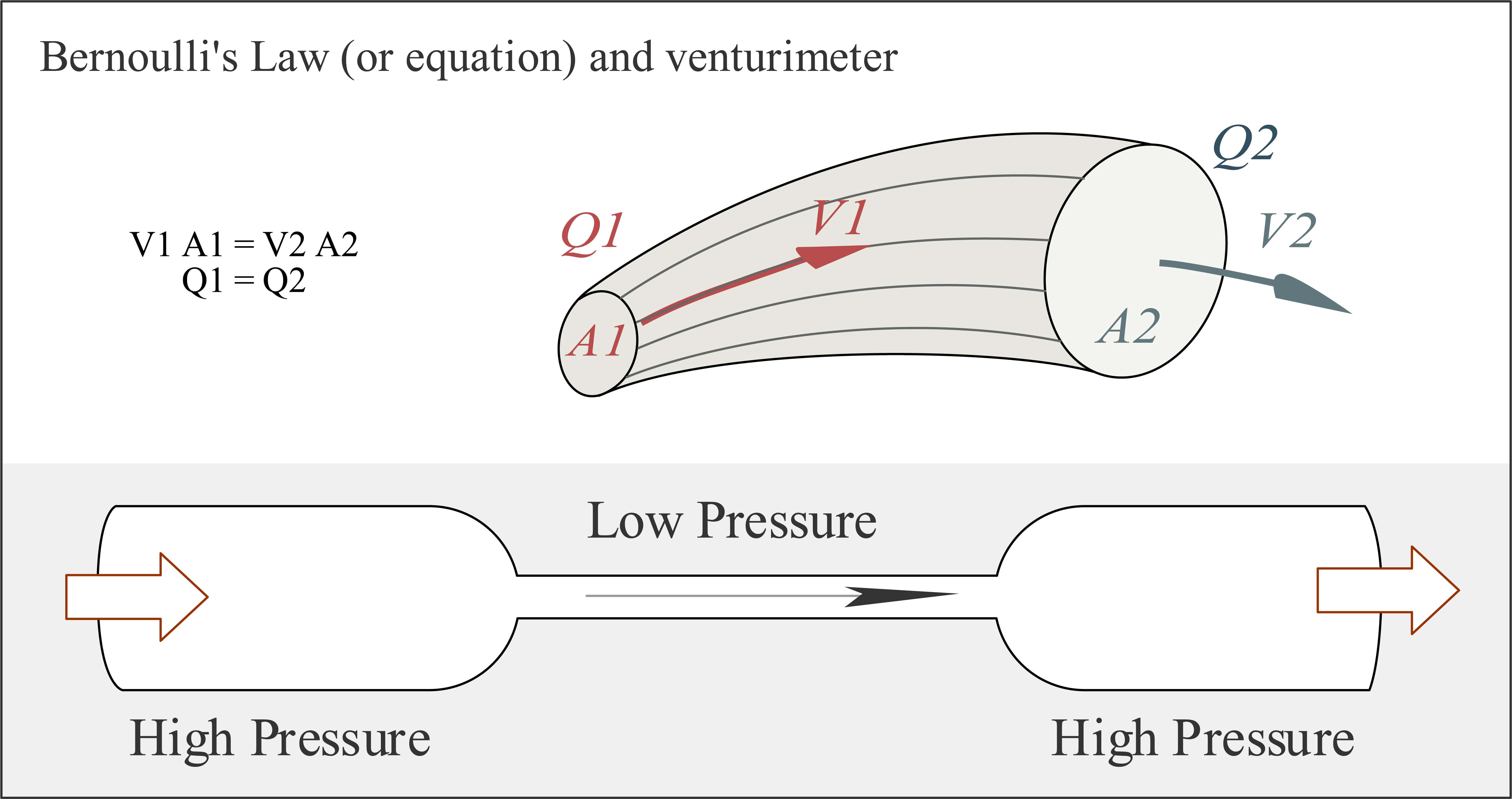
In aerosol therapy, there’s something called the Bernoulli Principle. This principle says that when a pressurized flow of air is directed through a small outlet, its velocity increases creating a jet stream. When this jet stream is created, it makes a sub-atmospheric pressure zone, also known as a vacuum. This vacuum is used to pull the medicine up a capillary tube and into the jet stream which then creates the aerosol that you inhale. This is the same principle that’s used to create jet engines.
Components of a Nebulizer
Unlike inhalers, nebulizers are electronic devices, so they’ll need a source of power in order to operate. Home nebulizers will have a power cord that you can plug into the wall outlet and portable nebulizers will have either replaceable or rechargeable batteries for you to use. While home nebulizers are still rather small and can be transported easily, you may need a portable one if you want to perform inhalation therapy on the go.

Another component of a nebulizer is the mask or mouthpiece which may be a part of the nebulizer device or attached to it via a tube. You will also have a medication cup and measuring device that’s used to administer the correct dosage of medicine and a filter will be attached that removes contaminants from the air before it’s put through the device. These filters should be replaced every once in a while to ensure the compressor stays clean and that you are inhaling fresh, clean air.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Types of Nebulizers
Nebulizers are generally divided into two different categories: jet nebulizers and ultrasonic nebulizers. Each of these units comes with their own pros and cons and each can be purchased in either a home (tabletop) or portable version. While each type of nebulizer is effective, you’ll want to speak with your doctor to decide which one will be best for you. Let’s take a look at each one to see how they work.
Jet Nebulizers
Also known as an atomizer or compressor nebulizer, these are the most common type and are considered the “traditional” nebulizers because they’ve been in use longer. This device uses compressed air at a high velocity in order to turn medicine into an aerosol. While jet nebulizers can be noisy, they’re often used in hospitals for patients with serious cases of respiratory disease.

Pros:
- Wide range of particle sizes
- No restrictions on medication
- Durable and reliable
- Tabletop or portable options available
- Low operational cost
Cons:
- Tend to be very loud
- Tabletop versions are bulky and difficult to move
Ultrasonic Nebulizers
Ultrasonic nebulizers use high-frequency sound waves to turn liquid medicine into an aerosol. In order to create the sound waves, they use a vibrating metal plate at ultrasonic frequencies. Because these sounds are undetectable by the human ear, ultrasonic nebulizers are much quieter and also tend to be easier to move around.
Another technology contributing to the development of ultrasonic nebulizers is called the Vibrating Mesh Technology (VMT). These types of nebulizers have thousands of laser-drilled holes that vibrate in order to produce the mist, which is much more efficient than other ultrasonic nebulizers, however, it tends to produce more heat and liquid waste.

Pros:
- Most technologically advanced nebulizers
- Much quieter than jet nebulizers
- Light and compact
Cons:
- More expensive than other nebulizers
What Medication Do Nebulizers Administer?
Nebulizer medications are divided into two different categories: long-term control medications and quick relief. Long-term medications are used to treat the symptoms of asthma, COPD, and other respiratory ailments, while quick-relief medications are used for emergencies like an asthma attack or COPD exacerbation. Not everyone with a chronic lung condition will be prescribed inhaled medication, but if you are, your doctor may decide that a metered-dose or dry powder inhaler will work better for you.
Depending on the severity of your disease, your age, and the type of condition that you have, your doctor will determine the amount of medication that’s needed. You may also be instructed to mix two different types of medication or to only use it in certain situations. Ensure you follow his/her instructions exactly in order to experience the most relief from your symptoms. Below are just a few of the medications you may be prescribed for nebulizer therapy.
Ipratropium Bromide

This is a type of bronchodilator that can help alleviate acute respiratory symptoms by preventing muscle constriction in the airways. According to the National Institutes of Health (NIH), severe asthma attacks can often be treated with ipratropium in combination with other short-acting drugs like levalbuterol and albuterol, but your doctor may be able to provide you with a premixed combination of these drugs. Potential negative side-effects of ipratropium include an upset stomach, dizziness, and dry mouth.
Cromolyn Sodium
While not as effective as budesonide, cromolyn sodium has some use as a long-term asthma control medication. Cromolyn sodium is used to prevent the chemical release and activation of inflammatory cells in the airways and lungs. This drug is also commonly used to treat seasonal allergies because it stabilizes mast cells, the cells that release histamine and other inflammatory chemicals. Potential side-effects of this drug include throat irritation and coughing.
Albuterol and Levalbuterol
Both levalbuterol (Xopenex) and albuterol (AccuNeb) are used as a quick-relief drug for asthma. They are labeled as such because they are bronchodilators meaning they open the airways making it easier to breathe during an asthma attack of COPD exacerbation. While there are a number of potential side effects to combining these two drugs, the benefits may outweigh them. Be sure to follow your doctor’s instructions carefully.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Budesonide
Budesonide (pulmicort respules) is an inhaled steroid that reduces the number of inflammation-inducing cells in the lungs. It is the only corticosteroid administered through inhalation therapy and has proven extremely useful in reducing asthma symptoms. According to the 2015 Global Initiative for Asthma (GINA) guidelines, budesonide is one of the most effective drugs for long-term asthma control. Potential side-effects of budesonide include oral thrush, a yeast infection in the mouth, and a hoarse throat.

Acetylcysteine
Mucus is a substance secreted by mucous membranes. It plays an important role in the body by trapping particles like airborne allergens and viruses and keeps them from entering the lungs. Unfortunately, many respiratory diseases lead to an overproduction of mucus which can have negative effects like airway obstruction. Acetylcysteine is a drug that breaks up mucus and makes it less viscous allowing it to be cleared more easily.
Diseases Treated With Nebulizers
While browsing the web or watching television, you may have noticed that nebulizers are usually advertised towards kids with asthma. While they’re certainly most commonly used by children, many adults and seniors use them as well. What’s more, nebulizers can be used to treat many different respiratory conditions, not just asthma. Children may benefit from nebulizers if they don’t know how to use an inhaler and those with severe lung disease may not be physically capable of inhaling deeply enough to make inhalers an effective option.
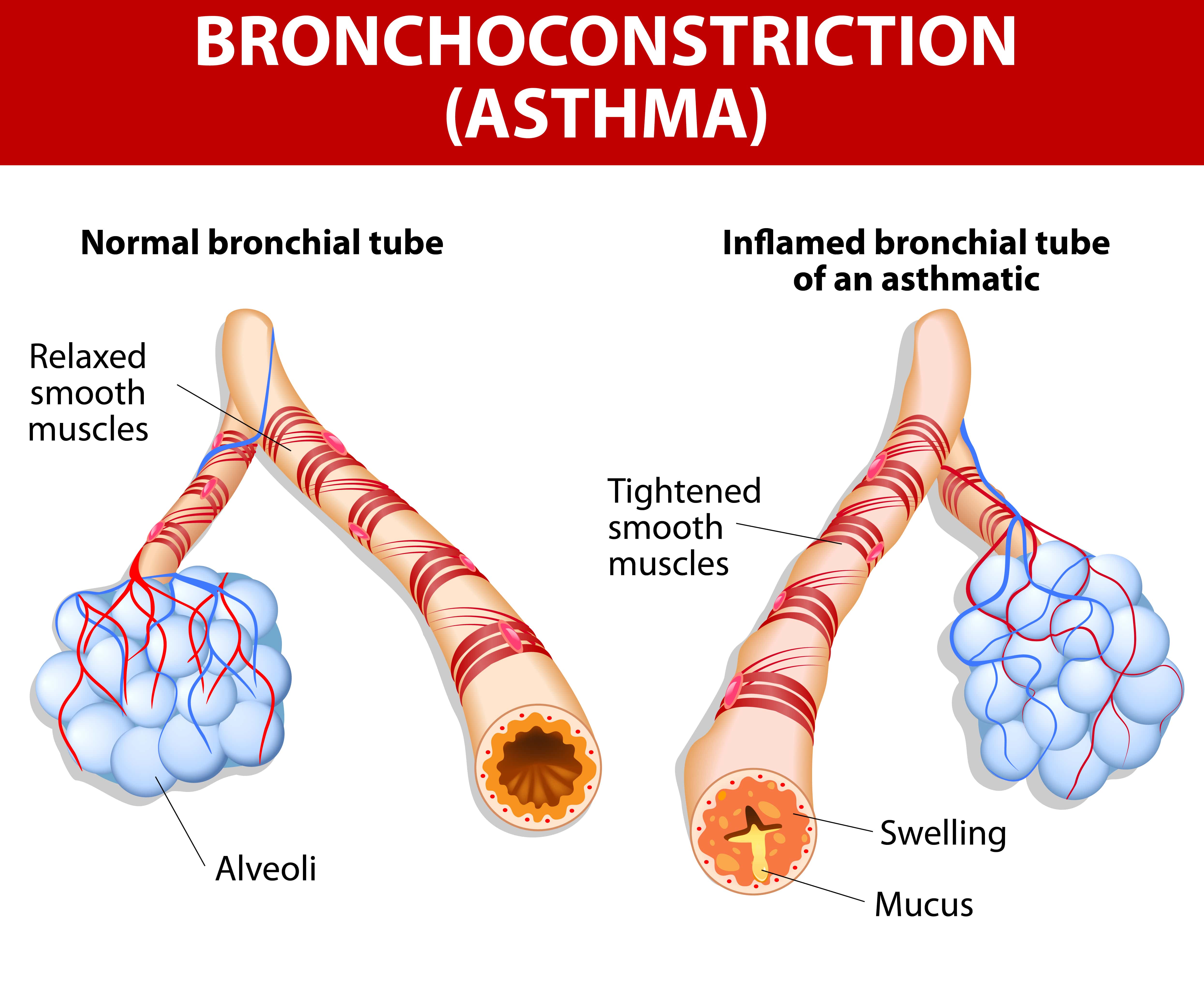
Asthma
Asthma is a lifelong lung condition that leads to inflamed and narrowed airways. Symptoms can range from mild to severe and happen frequently or in rare instances. Medication administered through inhalation therapy can help to reduce this inflammation, open up the airways, and help the patient breathe more easily and cough less.
Chronic Obstructive Pulmonary Disease (COPD)
COPD is an umbrella term that includes both chronic bronchitis and emphysema. Chronic bronchitis is similar to asthma in that it’s characterized by inflamed airways, more specifically in the bronchial tubes that lead to the lungs. However, bronchitis is caused by environmental factors like pollution, cigarette smoke, or a virus, whereas asthma is an increased responsiveness of the airways to irritants. This is a subtle difference, but it could mean having an entirely different treatment plan.
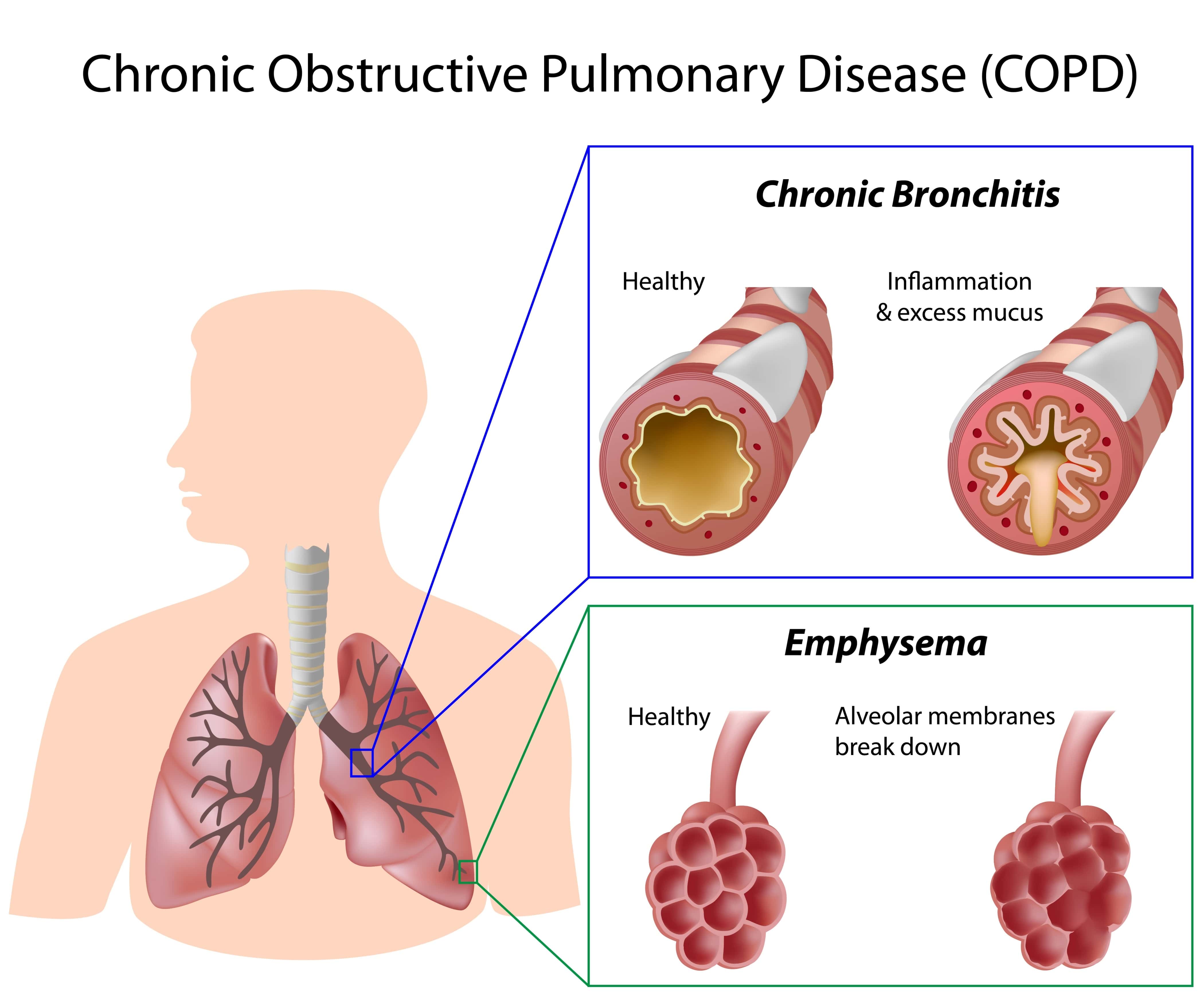
Emphysema, on the other hand, results in inflammation of the alveoli or tiny air sacs that are responsible for the exchange of oxygen and carbon dioxide in the lungs. Emphysema results in coughing, wheezing, increased mucus production, and an increased risk for acute respiratory illness, all of which can be treated with nebulizer therapy.
Cystic Fibrosis
This is a lung disease that causes mucus to be thicker and more viscous than normal. According to Medical News Today, 75 percent of cystic fibrosis cases are diagnosed before the age of 2 making it a significant concern among children. Acetylcysteine is one drug that will help to thin the mucus and make it easier for someone with CF to breathe.
Pneumonia
Nebulizers aren’t just effective in treating chronic lung conditions, they can be helpful for acute illnesses like pneumonia as well. In this disease, the tiny air sacs in the lungs fill with fluid resulting in an infection, chills, and difficulty breathing. In bacterial pneumonia, your doctor may prescribe you antibiotics that can be used through your nebulizer.
How To Properly Use a Nebulizer
The good thing about nebulizers is that they’re very easy to use. While all nebulizers will work slightly differently, they all have the same components and if you have any questions you can easily just consult the user’s manual or speak with your doctor.
- Clean your hands thoroughly — dirt or dust can damage the nebulizer.
- Attach the hose to either an air compressor or an oxygen supply
- Adjust the mouthpiece or mask on your face so that it fits snuggly
- Breathe normally through your mouth until all the medication has been administered. Usually, this takes around 10 to 15 minutes.
- Once you’re done, turn off the device, wash the mouthpiece and medicine cup, then leave it to dry.
How To Clean a Nebulizer
It’s very important that you take the time to clean your nebulizer regularly. If the components aren’t cleaned thoroughly or often enough you may spread bacteria which can lead to sickness. If you have COPD, getting sick could mean experiencing more frequent and severe exacerbations.
- Always use your nebulizer in a dust-free and smoke-free area
- Wash the hose and face mask or mouthpiece after each use and leave it to air dry.
- Remove the medication cup and rinse it thoroughly
- After several uses, take a bowl and put in it one part vinegar and three parts water. Soak the mouthpiece in it for 20 minutes then rinse and dry.
- When storing your nebulizer, always keep it in a bag, case, or covered in a towel to keep it clean.
- Keep extra filters on hand and check it at least once a month.
Nebulizers vs Inhalers
The most immediate and obvious difference you’ll notice between an inhaler and a nebulizer is that nebulizers are much bulkier. Even the portable nebulizers are bigger and heavier than inhalers because they have the electrical components, battery, and compressor, whereas inhalers are just the medicine container and a plastic cover to protect it. Some inhalers have something called a spacer that’s attached to the mouthpiece. This makes it a little easier for children or people with impaired lung capacity to inhale the medicine deeply and allow it to enter the lower lungs.

Nebulizer Therapy vs Oxygen Therapy
It’s important to understand the difference between nebulizer therapy and oxygen therapy. Whereas nebulizer therapy is used to administer medication to the lungs, oxygen therapy simply delivers pure oxygen to the lungs. Oxygen therapy is prescribed to patients who have impaired lung function and aren’t able to take in enough air or process oxygen as efficiently as a healthy person’s lungs. If you’re undergoing nebulizer (inhaled) therapy, you won’t necessarily be prescribed medical oxygen and vice versa.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Oxygen-Driven vs Air-Driven Nebulization
Normally, your nebulizer will be attached to an air compressor. However, depending on the doctor’s specifications, you may need to use a compressed oxygen tank instead. This is usually only beneficial if the patient is already oxygen dependent. For example, they may carry around an oxygen tank or oxygen concentrator to ensure their blood oxygen levels remain normal.. In these instances, doctors typically titrate the oxygen amount, meaning they adjust the amount of oxygen that’s administered through the nebulizer for the best results. However, too much oxygen could be dangerous.
According to a study published by BMC Pulmonary Medicine, high administration of oxygen may lead to hypercapnia (carbon dioxide retention) or increased mortality in patients experiencing an acute COPD exacerbation. Supplemental oxygen is usually adjusted to achieve an oxygen saturation of 88 to 92 percent.
Conclusion
Hopefully, this guide provided you with some helpful information that you can use to get started with nebulizer therapy. While nebulizers are extremely effective at administering medication for asthma, COPD, and other respiratory patients, it’s important that you also keep up with every other aspect of your treatment plan.
While respiratory disease is one of the most common afflictions on the planet, each case is unique. Be sure to maintain open lines of communication with your doctor and that you understand exactly when and how you should use your nebulizer in order to have the best results.

