.png)
Oxygen therapy, pulmonary rehabilitation, and inhaled medication are the most common treatment options for COPD. They’re proven to significantly reduce respiratory symptoms like coughing, wheezing and shortness of breath, while simultaneously reducing the rate at which COPD progresses.
But if there’s one lesson you can learn about medical conditions, it’s that there’s no “one-size-fits-all” solution. Many patients suffering with COPD have overlapping conditions that may prevent them from experiencing relief using traditional treatment methods, or they might simply be dissatisfied with the results that they experience. At this point, it’s not out of the question to try a different approach like lung surgery.
Lung surgery, especially highly invasive lung surgery, often gets a bad rap in the medical community because it can be dangerous, costly, and time consuming. However, you should never be too quick to write them off, especially when it comes to treating a life-threatening condition like COPD. Millions of people around the world can attest to the effectiveness of surgery for COPD and it’s an area that’s seen some major advancements in recent years.
Whether you’re considering surgery for COPD or you’re just curious what your options are, you’ve come to the right place. In the following sections we’re going to take a look at each of the surgical procedures currently available for COPD, helping you to weigh their advantages, disadvantages, risks, and more.
Who Needs Surgery for COPD?

According to the National Heart, Lung, and Blood Institute, surgery is usually a last resort for someone suffering with COPD. While surgery is an option in all four stages of COPD, it’s most commonly advised only in stage four or “end-stage” COPD. Oftentimes, medical professionals are put in a difficult situation because the patient’s respiratory ailments need to be bad enough to warrant surgery but the patient also needs to be healthy enough for the procedure to go as planned.
Some considerations your doctor will make include:
- Your overall health and health history. Your doctor will want to ensure that you are strong enough to recover after the surgery and that you have a healthy body weight. If you have other conditions that may affect the surgery, you may not be approved for the procedure.
- Your ability and willingness to participate in pulmonary rehabilitation programs. These programs aren’t only great for teaching you how to breathe and exercise correctly, but they provide your doctor with important information about your progress.
- Your age. Surgery is not recommended for patients over the age of 75.
- You’re not a smoker. Smoking is known to cause a number of complications with surgery. It reduces blood flow, slowing the healing process after surgery and puts you at a greater risk of contracting pneumonia and other acute respiratory illnesses.
These are the general guidelines your doctor will use to determine if you’re right for surgery, however, there may be other requirements you have to meet. For example, your doctor may have to perform tests to locate the damaged area of the lung. If the damage is in the wrong area or it’s not localized, you may not benefit from surgery.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What Types of Lung Surgery Are There?
There are four main types of surgery used to treat COPD including bullectomy, lung volume reduction surgery (LVRS), endobronchial valves, and lung transplants. While each of these procedures is very different, they all have the same purpose: to allow the patient to breathe easier, reduce coughing and wheezing, and increase life expectancy and quality of life.

Lung Volume Reduction Surgery (LVRS)
Just like the name suggests, the goal of LVRS is to reduce the size of the lungs. While this may seem counterintuitive since you’re trying to make it easier to breathe, this procedure is used for COPD patients with a very specific type of ailment called hyperinflation where the lungs are in a perpetual state of overinflation. When this happens, it can be difficult to breathe because you won’t be able to fully expel air from the lungs.
How Emphysema Causes Hyperinflation
While hyperinflation can be caused by a number of lung conditions, it’s primarily caused by emphysema. About 3.5 million Americans have emphysema, a condition that causes damage to the alveoli (tiny air sacs) within the lungs. After years of exposure to cigarette smoke and other airborne chemicals, these air sacs begin to expand and become inflamed, impairing their ability to transfer oxygen and carbon dioxide to and from the blood.
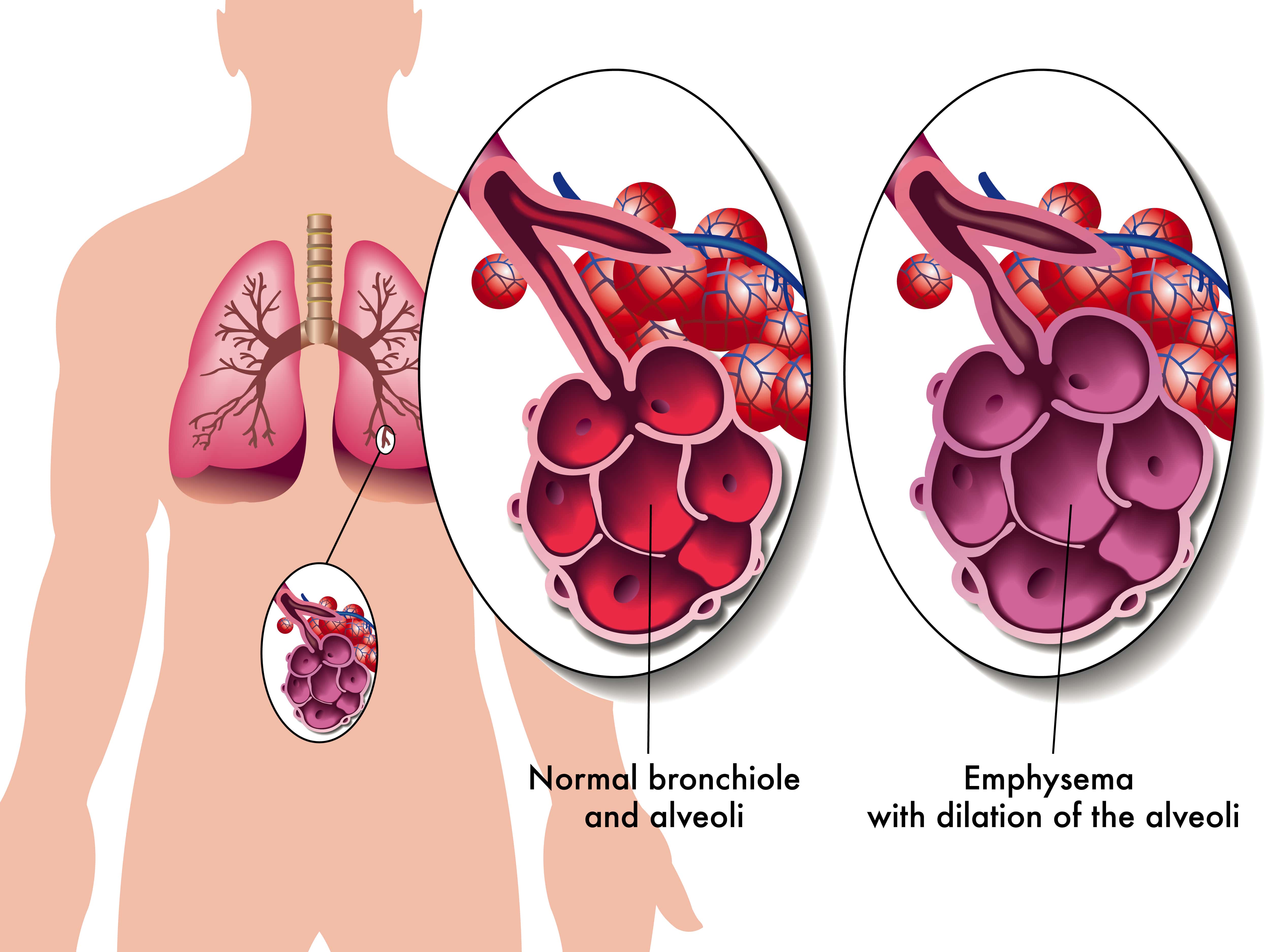
In a healthy person, the alveoli are elastic, allowing gasses to flow in and out of them easily. However, in an emphysema patient, these air sacs are baggy and air can get trapped in them, blocking healthy alveoli that surround it. This is known as “static” hyperinflation and can make it very painful to breathe and causing you to trap carbon dioxide within the lungs.
“Dynamic” hyperinflation is another type of overinflation of the lungs that can either work in tandem with or independently from static hyperinflation. Dynamic hyperinflation is caused by hyperpnea (the increased depth and rate of breathing) or exercise and results in an increase in end-expiratory lung volume (EELV).
Despite every emphysema patient having damaged alveoli, only about 1 - 2% of COPD patients qualify for LVRS. This procedure is typically only advised for patients with severe symptoms like if your FEV1 value (the amount of air you can expel in one second) is below 50%.
Your doctor will likely recommend LVRS if you have upper lobe predominant emphysema. This is a type of centrilobular emphysema that progresses upward, damaging both the upper lobes of the lungs and bronchioles (respiratory passageways).
How Lung Volume Reduction Surgery Works
While it may seem like the bigger the lungs are, the better they are for breathing, it’s not quite this simple. Think of the lungs like a giant sponge. When the lungs expand, they draw in air until they reach their max capacity. Oxygen and carbon dioxide are exchanged in the blood through the alveoli and then you can fully expel the carbon dioxide in the lungs.
Having bigger lungs wouldn’t help you unless you had more functioning alveoli to perform the exchange. So, if part of your lungs is severely damaged, it can actually be causing more harm than good. In the case of hyperinflation, the damaged part of the lungs is actually acting as dead weight that you have to deal with every time you breathe.

The goal of LVRS is to remove that section that’s causing problems and leave only the optimal, high-functioning parts of the lungs. This is typically about 30 percent of each lung, however, it depends on individual circumstances. There are two methods used to complete lung volume reduction surgery:
Sternotomy
This is the preliminary process in many types of heart and lung surgery. During this procedure, an incision is made down the center of the chest wall and the breastbone is separated. After the damaged tissue is removed and the lungs are resealed, the breastbone is put back into place to heal.
Thoracoscopy
Another less invasive method for completing lung volume reduction surgery is a thoracoscopy. During this procedure, several small incisions will be made between the ribs. The surgeon will use a videoscope to monitor what’s going on inside the chest. A stapler and grasper are used to remove the damaged tissue and reseal the lungs.
Bullectomy
A bullectomy is a type of lung surgery used to remove bullae from the lungs. A bulla is a small air bubble that is at least 1 cm in size, but it differs from other abscesses in the body in that it usually forms on the lungs due to something called bullous lung disease. However, occasionally, they can be found in otherwise healthy lungs.
Bullae usually grow over time and the bigger they get, the more they obstruct the function of the lungs. While in most patients bullae are harmless and dissipate with time, in severe cases, medical professionals may resort to a bullectomy to remove the pockets of air on the lungs.

Similar to hyperinflation, bullae affect the alveoli in the lungs. However, in this case, bullae result when the walls of the air sacs break down and form larger ones. These new air sacs don’t assist in transferring oxygen to the blood, and instead end up suppressing and weighing down on surrounding tissue.
Classification of Bullous Lung Disease
If you have COPD, there are two categories of bullous lung disease that you should know about: bullous emphysema and vanishing lung syndrome.
- Bullous emphysema is the classification of bullae that form in emphysematous lung parenchyma. This is characterized by the formation of multiple adjacent bullae which are the result of the progressive loss of alveolar attachments. 80 percent of patients with bullae have associated pulmonary emphysema.
- Vanishing lung syndrome got its name because on X-ray, it makes it look like the lungs are disappearing. This condition commonly affects young male smokers and is characterized by a large emphysematous bullae on the upper lobes of the lung. VLS is uncommon and usually requires a bullectomy for treatment.
When bullae form in normal lungs, they usually form on their own and are surrounded by healthy tissue. Although health experts are not quite sure what causes this type of bullae, it’s likely caused by some type of focal anatomic defect that causes progressive air trapping. Even with bullae, many patients still experience normal lung function.
How a Bullectomy Procedure Works
If the bullae found on your lungs are progressing quickly or they’re obstructing your breathing, you may qualify for a bullectomy. This procedure is much less intrusive than other types of lung surgery and can be completed using video assisted thoracoscopic surgery (VATS), also known as videoscopic surgery.
Endoscopic Lung Volume Reduction
While not technically “surgical,” valve therapy (endoscopic lung volume reduction) is often used as an alternative for lung volume reduction surgery. The basic premise of these valves is to prevent air from entering diseased areas of the lung while allowing air to exit freely. By doing so, the patient will be able to maintain an equilibrium with each breath and prevent hyperinflation of either lung.
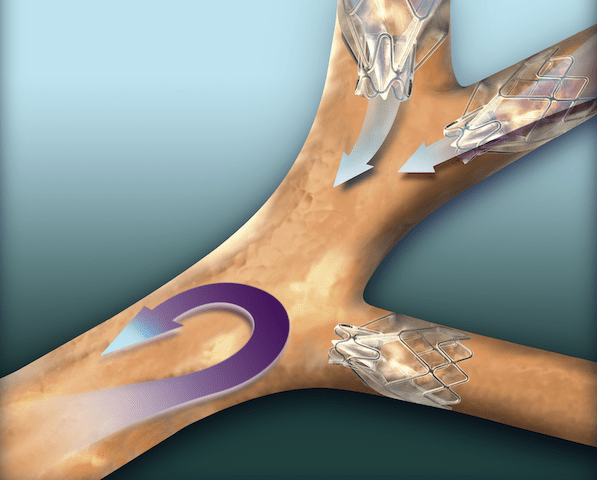
Zephyr valves, produced by PulmonX, are the most widely accepted and successful endobronchial valves on the market. And since the first successful implant in 2001, the company has developed a number of technologies to assess emphysema patients and provide better treatment.
Aside from being minimally invasive, one of the major benefits of endobronchial valves is that they can be repaired, removed, or adjusted as needed. Whereas lung volume reduction surgery is permanent, specialists are able to easily remove and repair endobronchial valves, move them around, or replace them entirely with a simple procedure.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}Lung Transplant Surgery

Last but certainly not least, we have lung transplant surgery. Despite being one of the most discussed surgery options for COPD, it’s far from being a common procedure. According to the 2015 report from The Registry of the International Society for Heart and Lung Transplantation, just over 17,000 patients had lung transplants for COPD between 1995 and 2014. This is a small fraction of people with COPD.
Because lung transplants are some of the most invasive and complicated procedures surgeons can perform, there is a long list of criteria that must be met before a patient will even be considered. Patients must be screened before the operation to ensure they don’t have any active infections or other health issues that could lead to complications.
When are lung transplants advised?
Permanently damaged lungs can significantly reduce someone’s quality of life. There are many treatment options like oxygen therapy and pulmonary rehabilitation which can increase your quality of life and help you live normally again. However, when all these other options fail and your doctor knows you won’t get better without surgery, he/she may recommend a lung transplant. Some of the most common reasons to have a lung transplant include:
- Cystic fibrosis
- Pulmonary hypertension (high blood pressure in lungs)
- Lung scarring (pulmonary fibrosis)
- Chronic obstructive pulmonary disease
Lung transplants are almost always a last resort option for treating these conditions. Your doctor may perform a number of tests to determine if other surgeries or medications are an option. Surgeries like lung volume reduction are far less invasive, costly, and time consuming, and they may provide you with the same or comparable benefits.
Risks of lung transplant surgery
Due to the intensiveness of lung transplant surgeries, there are many risks associated with them. Your doctor will be very precise and thorough when describing how to prepare for the procedure in order to reduce risks and leave as little room for error as possible. Before you even consider lung transplant surgery, it’s important to understand the risks involved.
Lung Rejection

Your body is naturally equipped to fight infections and foreign substances using both your adaptive and innate immune system. While everyone’s immune system has its strengths and weaknesses, most tend to recognize the transplanted organ as a “foreign object.” When this happens, it can lead to organ failure. This is more likely to happen immediately after surgery and becomes less frequent as time goes on.
There are several different types of lung rejection that can happen after a lung transplant. Acute rejection is an immediate reaction to the new lung or lungs and is fairly common. As such, your doctor will be closely monitoring your progress after the surgery and you should ensure that you’re taking the immunosuppressive drugs that you’re given which will help your body accept the new lungs.
Another type of rejection is chronic lung allograft dysfunction (CLAD), or long-term lung rejection. This condition usually results in airflow restrictions or obstructions and can have symptoms ranging from mild to severe. One of the most common types of chronic lung rejection is bronchiolitis obliterans syndrome (BOS), a condition causing inflammation that affects the bronchioles, the smallest airways in the lungs.
Infection
Infection is another risk after lung transplant surgery. Your doctor will provide you with a plan that suppresses your immune system so that the lungs aren’t rejected, but this will also make you more likely to get sick. Contracting acute respiratory illness may also exacerbate any issues your body is having with accepting the new lungs, so it’s important to stay healthy.

Fortunately, lung transplants have become much safer within the past several decades. According to the U.S. Department of Health and Human Services, the one-year survival rate of a lung transplant patient was 45 percent in 1990. Since then, survival rates have risen to 83 percent, meaning transplants are a much more viable option than they were in the past.
How To Get Started
COPD is a debilitating respiratory condition that affects millions of people across the world. For some, COPD symptoms are not bad enough to warrant lung surgery, but for others, especially those in stage 4, surgery may be the only effective way of seeking relief. Whether you’re preparing for an upcoming surgery or surgery is something you may be considering in the near future, there are a few things you can do right now to prepare.
Speak With Your Doctor
Before you do anything else, it’s important to first consult with your primary care physician and pulmonologist. Many patients tend to rush into things only to be disappointed when they find out they don’t need or qualify for surgery. On the other hand, some people are terrified by the thought of surgery and try to avoid it meaning they could be missing out on a great opportunity to seek relief from their symptoms.

The more open and honest you can be about how you’re feeling and what symptoms you’re experiencing, the better your doctor will be able to align you with a treatment plan that works for you. Because surgery is so costly and time consuming, your doctor will likely try many other options before resorting to surgery.
Quit Smoking
Smoking is the primary cause of some of the world’s deadliest lung diseases including COPD and lung cancer — but the problems don’t end there. Smokers are also at a much higher risk of contracting type 2 diabetes, cataracts, strokes, heart disease, and complications during lung surgery.

According to the Truth Initiative, an organization dedicated to promoting tobacco-free living, smoking decreases blood flow and alters the immune system making it difficult for your body to heal properly. And because surgery is such a precise process, doctors will want to eliminate any potential risks they can before they begin. While some surgeons may operate on someone who has smoked recently, it’s in your best interest to stop as soon as possible.
Exercise

Pulmonary rehabilitation is an effective method of reducing shortness of breath, fatigue, and depression in COPD patients. And according to a study by the Journal of Thoracic Disease, preoperative pulmonary rehabilitation is also an important process increasing exercise tolerance before surgery. The study concludes that exercise capacity reduces both postoperative complication risk and the amount of time patients spend in the hospital after a surgery. Additionally, preoperative exercise increases muscle mass and reduces fatigue which can also help with the healing process post-surgery.
Eat Right
Your diet plays a crucial role in your body’s ability to manage and treat COPD symptoms like breathlessness, fatigue, and chest pain. Many COPD patients report feeling weighed down and weak when they don’t get the right nutrients in their body, and this is no different when it comes to preparing for a surgery.


