Because COPD is a breathing disorder, most of the symptoms of the disease are caused by not being able to get enough oxygen when you breathe. However, there is another, equally serious breathing problem that COPD patients face, which is not exhaling enough carbon dioxide (CO2) when they breathe—known as CO2 retention.
When this happens, it allows excess carbon dioxide to build up in your blood, which can cause serious symptoms and make it more difficult to breathe. Although it is most likely to happen to patients suffering from severe COPD, anyone with the disease, especially those using supplemental oxygen, are at risk for CO2 retention.
In this post, we're going to explain how carbon dioxide retention happens and how it affects your health and your COPD. We'll also give you tips on how to avoid CO2 retention and how to recognize the signs in case it ever happens to you.
How Does CO2 Retention Happen?
COPD causes your airways to get narrowed and obstructed, which makes it more difficult for air to flow through. This, along with the damage to the air sacs in your lungs, causes the majority of COPD symptoms like coughing, wheezing, and shortness of breath.
Sometimes, the same airway obstruction that makes it difficult to inhale enough oxygen in also makes it difficult to exhale effectively. And because you release carbon dioxide—a waste product—when you exhale, breathing out is just as important as breathing in.
How Your Lungs Process Oxygen and Carbon Dioxide
Breathing is about maintaining a balance between oxygen and carbon dioxide; you take in oxygen when you inhale, and breathe out carbon dioxide when you exhale. These gases are both carried by your red blood cells, which cart them to and from your lungs.
The first, oxygen, is an important fuel that all the cells in your body need a constant supply of in order to survive. The other, carbon dioxide, is a waste product that your body gets rid of in order to make room for more oxygen.
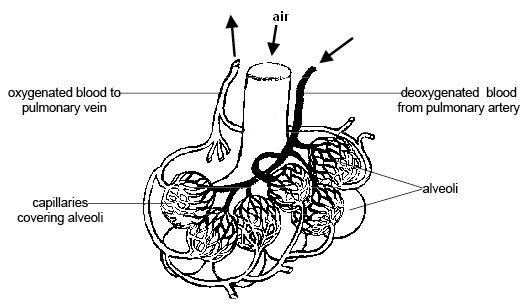
When you breathe in, empty-handed red blood cells pick up oxygen molecules from your lungs before beginning their journey to carry that oxygen all around your whole body. This exchange between your blood and the oxygen in your lungs happens in the alveoli, or the tiny air sacs in the lungs.
As the oxygen gets used up by the different organs and cells in your body, it gets turned into the waste product carbon dioxide. Then, the cells hand off this CO2 to empty-handed red blood cells in your bloodstream, which then carry the CO2 back to the air sacs in your lungs.
Then, before you exhale, all of those CO2-carrying red blood cells release their carbon dioxide into your lungs. When you breathe out, you exhale all of that CO2, and the red blood cells, empty-handed once more, are ready to pick up more oxygen the next time you inhale.
Why COPD Causes CO2 Retention

COPD can disrupt the process described above by preventing you from getting rid of enough carbon dioxide when you breathe. It does this in two ways: by destroying the tiny air sacs in your lungs, and by preventing you from pushing all of the air out of your lungs when you exhale.
COPD can make it difficult to breathe out because of airway narrowing, blockage, and other changes in the lungs. This leaves excess CO2 trapped in your lungs after you exhale, which takes up space that is needed to hold oxygen-rich air when you breathe in.
COPD also damages and destroys your air sacs, or alveoli, which is where oxygen and carbon dioxide is passed between your blood and the air in your lungs. When you have COPD, there are fewer healthy alveoli and fewer places for this exchange to happen, which makes it difficult to get enough oxygen into your blood and also difficult to get enough CO2 out of your blood and into your lungs.
Over time, as your COPD progresses and your lung function declines, you may retain more and more carbon dioxide as you breathe. As that excess CO2 builds up in your blood, it causes an imbalance between your blood oxygen and carbon dioxide levels, which can cause serious symptoms and oxygen deprivation.
Co2 retention also happens through a phenomenon known as ventilation-perfusion mismatch. This happens when your body gets confused about which parts of your lungs to prioritize, which reduces the efficiency of gas exchange in your lungs.
Usually, your lungs constrict your blood vessels in such a way that they decrease the amount of blood that flows to poorly functioning air sacs that have been damaged by COPD. At the same time, they increase blood flow to the most healthy alveoli so they can absorb as much oxygen (and release as much carbon dioxide) as possible.
However, this ventilation-perfusion ratio can get thrown off, usually because of high-flow oxygen therapy, COPD exacerbations, or other COPD symptoms. That causes this blood flow strategy in the lungs to break down; less blood flows to the parts of the lungs that function efficiently, and more blood flows through damaged alveoli that are less capable (or completely incapable) of exchanging oxygen and carbon dioxide efficiently.
The result is low blood oxygen levels (hypoxemia) and high blood carbon dioxide levels (hypercapnea) that make it more and more difficult to breathe. When mild, this can often be corrected with supplemental oxygen therapy and other COPD medications, however, it can be caused by improperly-dosed oxygen therapy, as well.
Why CO2 Retention is Dangerous

When too much CO2 is trapped or “retained” in your lungs after you exhale, it makes it much harder to breathe. This is partially because oxygen-rich air that enters your lungs when you inhale mixes with the leftover CO2, diluting the oxygen concentration of the air in your lungs and making it more difficult for the air sacs to absorb enough oxygen.
Another problem is that the excess CO2 gets picked up by empty-handed red blood cells and re-absorbed back into your blood. Since red blood cells can only hold one gas at a time, it leaves fewer red blood cells free to pick up oxygen when you breathe in.
The problem can get worse as more and more CO2 builds up in your bloodstream, making it harder and harder to absorb oxygen from your lungs. If your blood CO2 gets too high, it's known as hypercapnea, and it can lead to serious breathing problems and dangerously low levels of oxygen in your blood.
Because of this, the main symptoms of hypercapnea overlap with the symptoms caused by hypoxemia, which happens when your blood oxygen saturation gets too low. If left untreated for too long, hypercapnea-related hypoxemia can cause serious health complications, including respiratory failure and death.
However, CO2 retention poses a more immediate risk of making your COPD more difficult to manage and making symptoms like coughing, wheezing, and shortness of breath worse. You are more likely to experience hypercapnea during symptom flare-ups, respiratory illnesses, and COPD exacerbations, but CO2 retention can also happen slowly and gradually over time.
In fact, the early symptoms of CO2 retention may be so mild or non-existent that you don't notice them until it gets much worse. That's why it's important to understand what CO2 retention is, how it happens, and how to recognize it; the sooner you realize it's happening, the sooner you can seek treatment and get your COPD back under control.
Left unchecked for too long, CO2 retention deprives your body of oxygen, which can cause serious health problems like heart disease, pulmonary hypertension, and cognitive dysfunction. If it gets too bad, severe hypercapnea can cause respiratory failure, organ damage, and death.
Respiratory failure happens when you have so much CO2 in your blood that it raises your blood's acidity beyond healthy levels. This is a condition known as acute respiratory acidosis, and it is is a life-threatening medical emergency.
A less severe form of respiratory acidosis, known as chronic respiratory acidosis, can happen gradually over time. It does not pose as immediate a risk as acute respiratory acidosis, and, because it happens little by little, the body adapts to the blood's acidity. This makes the symptoms are subtle, if noticeable at all.
If you have COPD and are worried about CO2 retention, hypercapnea, or chronic respiratory acidosis, then ask your doctor to take another look at your blood oxygen, CO2 levels, and your lung function tests (he should already do this at your regular appointments). Always tell your doctor about any new symptoms you have, even if they are mild, and don't be afraid to discuss any concerns you have about your health.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The Symptoms of CO2 Retention and Hypercapnea

The first symptoms of CO2 retention or hypercapnea are usually headaches, breathlessness, drowsiness, and lack of energy. These symptoms happen because you can't absorb enough oxygen and your blood oxygen saturation gets low.
As it gets worse, hypercapnea can cause difficulty thinking and concentrating, confusion, and muscle twitches. In serious cases, it can cause severe oxygen deprivation which leads to swelling in the hands and feet (edema), a bluish tint to the skin (especially fingers and lips), seizures, coma, respiratory failure, and death.
Here is a list of some of the general symptoms of CO2 retention:
- Mild headaches
- Feelings of drowsiness, fogginess, or sleepiness
- Lack of energy or fatigue
- Inability to focus or think straight
- Feeling dizzy or disoriented
- Shortness of breath
Here is a list of the more severe symptoms of hypercapnea:
- Unexplained confusion
- Abnormal muscle twitching
- Abnormal depression or paranoia
- Irregular heartbeat
- Bluish tint to the skin and lips
- Swollen hands and feet (edema)
- Hyperventilation
- Seizures
- Loss of consciousness
These symptoms can occur quickly or happen gradually over time. If you experience mild symptoms for more than a couple of days, then you should schedule an appointment to see your doctor. If your symptoms are severe, then you should seek medical attention at an emergency room immediately.
Causes of CO2 Retention for People with COPD
As we discussed, CO2 retention is often caused by airway obstruction, damaged lung tissue, and ventilation-perfusion mismatch in the lungs. However, there are a variety of other things that can make CO2 retention worse.
Oxygen Therapy

A common cause of CO2 retention is supplemental oxygen therapy. If your oxygen dosage is wrong or you get too much oxygen for any other reason, it can cause too much CO2 to build up in your blood.
This happens because, when you get excess oxygen with every breath, it can cause red blood cells to drop carbon dioxide to pick up oxygen instead. As a result, the dropped CO2 dissolves into your blood instead of getting released into your lungs for expulsion.
This dramatically throws off the balance of oxygen and carbon dioxide exchange in your lungs, causing more and more CO2 to build up in your bloodstream. In this way, portable or home oxygen therapy can make CO2 retention much worse and cause hypercapnea when prescribed or used incorrectly.
Another way that oxygen therapy can worsen CO2 retention is by causing ventilation-perfusion mismatch. Although researchers aren't sure exactly why, this happens when you get more oxygen at a time than what you actually need.
The best way to avoid oxygen therapy-induced CO2 retention is to follow your oxygen prescription exactly. To reduce the chances of hypercapnea, your doctor should prescribe you enough oxygen to keep your blood oxygen saturation at about 90 percent, but not much higher.
If you are worried about CO2 retention, you can always have your doctor check to make sure your flow rate is adjusted correctly and that you are using your equipment properly. Then, it's up to you to follow your doctor's instructions and only use your oxygen as often as your doctor recommends.
Emphysema

Severe emphysema is another major cause of CO2 retention in people with COPD. Emphysema causes your lungs to become enlarged and less stretchy (a condition known as lung hyperinflation), which makes it more difficult to push all of the air out of your lungs when you exhale.
Lungs with emphysema tend to trap lots of air, which makes it difficult to breathe and absorb enough oxygen as well as expel enough CO2. This puts patients with emphysema at an increased risk of hypercapnea, especially during heavy exercise, which forces your lungs to get rid of even more CO2.
That's why doctors recommend breathing exercises like pursed-lips breathing and diaphragmic breathing to help you train yourself how to empty your lungs more completely when you exhale. These can be especially helpful during exercise and physical activity to reduce and prevent shortness of breath.
It is also important to follow your COPD treatment plan carefully to minimize your symptoms. The better you keep your symptoms and breathing under control, the better you can prevent air from getting trapped in your lungs, reduce hyperinflation, and prevent hypercapnea.
Some patients with severe emphysema may be eligible for lung reduction surgery if their lungs are significantly enlarged. By reducing the volume of the lungs, the surgery makes it easier to push all the air out when you exhale, preventing CO2 retention and making it easier to breathe.
To learn more about breathing exercises you can practice to improve your COPD, see our previous article on COPD breathing techniques here.
Eating Too Many Carbohydrates

Believe it or not, the foods that you eat can have a significant effect on CO2 retention in your lungs. That's because, whenever your body digests food, it turns it into two main things: energy, and carbon dioxide waste.
The carbon dioxide waste has to be processed through your lungs so that you can exhale it out of your body. Some foods, however, create extra carbon dioxide waste that puts unnecessary strain on your lungs.
The main culprits for this are foods high in carbohydrates, which create more CO2 waste than other foods when your body breaks them down. When you have COPD and your lungs are already struggling to function efficiently, this excess CO2 can be enough to tip the balance in your lungs and cause you to retain too much CO2.
Because of this, doctors often recommend that people with COPD limit the amount of carbohydrates in their diets. That includes grains, pastas, breads, and especially simple sugars and processed foods high in carbs.
While a certain amount of carbs are still healthy, you should try to limit yourself to healthy sources of complex carbohydrates and be careful not to eat more than you need. Instead, replace carbohydrates in your diet with more foods that are high in lean protein and healthy fats.
According to US dietary guidelines for older adults, you should eat about 5-7 ounces of grains every day, at least half of which should come from whole-grain sources. However, it is easy to exceed this amount if you eat a lot of breads, pastas, cereals, or processed foods.
Shallow Breathing

When you take too short or too shallow of breaths, your lungs have a hard time getting rid of enough CO2. That's why it's important to keep your breathing under control and practice breathing exercises if you have COPD.
Many COPD patients tend to take more shallow breaths whenever they feel like they're having trouble breathing, such as during bouts of breathlessness or coughing. Unfortunately, that just makes the problem worse by making it easier for air and CO2 to stay trapped in your lungs.
This happens because shallow breathing only uses the upper part of your lungs, which is why it is sometimes referred to as “top breathing.” As a result, stale air stays in the lower parts of your lungs, which leads to CO2 retention and makes it harder to breathe.
You can counteract this, however, by practicing breathing exercises in your spare time and remembering to use them when you feel short of breath. Exercises like diaphragmic breathing and pursed-lips breathing are especially helpful for training yourself to take deep, full breaths and push all the air out of your lungs when you exhale.
It also helps to strengthen your breathing muscles, which you can also do with aerobic exercise, wind instruments, and other forms of physical activity. You can even join special COPD exercise and therapy classes designed to help you improve your breathing, including pulmonary rehabilitation and music therapy courses.
Conclusion
COPD is a complicated breathing disorder that can lead to a variety of different symptoms and health complications. Because of the complex nature of the disease, many patients struggle to understand how their blood oxygen levels, blood CO2 levels, and their symptoms are all connected.
Hopefully, after reading this article, you have a better understanding of how your lungs function and how CO2 retention works. You should also be better able to recognize the signs of hypercapnea and how to protect yourself from factors that put you at risk.
If you use supplemental oxygen therapy, it's particularly important to know the symptoms of CO2 retention and the dangers of getting too much oxygen. If you catch the early signs, you can work with your doctor to adjust your oxygen delivery before it causes any serious problems. It's important to fully understand oxygen therapy benefits and oxygen therapy side effects before you get started.
COPD is sometimes a difficult disease to manage, but with the right knowledge, a good treatment plan, and the support of a good medical team, you can successfully keep your symptoms and CO2 retention under control. That's why it's important to learn everything you can about COPD and what you can do to keep your lungs as healthy as possible.

We’ve all experienced what it’s like to be burnt out on something. Whether it’s your job, chores, or health routine, it’s not always easy to find a way to stay on track to meet your goals. What complicates this even further is that everyone experiences this for a different reason. For some people, it’s just a matter of learning how to stick to a routine, but for others, it could be a lack of mental or physical energy that’s holding them back.
Oftentimes, when people are trying to stick to a COPD treatment plan, the latter is true. After all, fatigue is the second most common symptom of COPD with about 50% of patients experiencing it. Knowing this information, it’s not hard to see why it can be difficult to stick to a routine. If you’re hit with a sudden wave of fatigue, grogginess, or breathlessness, it can make simple tasks seem overwhelming. Eventually, your health goals will seem unattainable and unrealistic.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In this post, we’re going to provide you with some tips for having a fresh perspective on your COPD treatment plan. Regardless of the stage of COPD that you’re in, it’s never too early or too late to hit the reset button and start managing your COPD symptoms proactively. If you have any questions, feel free to leave them in the comment section below and we’ll get back to you.
Change Up Your Exercise Routine
As a COPD patient, you know how important your exercise routine is. While exercise does not magically reverse the effects of lung damage, it improves the efficiency of your body and lungs which inevitably leads to less breathlessness, less chronic pain, and a longer life expectancy. But you know as well as anyone that exercise routines are difficult to stick to, especially if you viewed it as a “chore” in the first place.

More often than not, COPD patients are taught how to exercise through a pulmonary rehabilitation program. These programs are aimed at educating patients about their lungs and disease, then applying exercise techniques that allow them to lead a happier life. Unfortunately, pulmonary rehabilitation programs don’t teach you how to make your exercise routine “interesting” or “engaging.” They simply tell you what needs to be done. As a result, many people find themselves in a situation a year or two down the road where they don’t have the motivation to continue.

At some point, you’re going to want to try new exercises that hold your interest. The important thing to remember is that you still need to follow the guidelines that you learned in pulmonary rehabilitation because this will ensure that you are making the most of your time and avoid injury. For example, if you implement a new exercise, you need to make sure it works the same muscle group and that it’s a similar intensity as your original exercise. If you have any doubts about it, you can always reach out to your doctor with any questions you may have.
Make Adjustments to Your Diet
What you eat also has a major impact on your ability to live a comfortable life with COPD. Unfortunately, your diet is also something that can become mundane if you’re eating the same things every day. Like with exercising, it’s okay to make changes to your diet, you just need to make sure that you’re getting the right nutrients. You also need to ensure that you aren’t increasing or decreasing your caloric intake too much. According to the COPD Foundation, breathing with COPD takes more energy than for a healthy individual, so you need to maintain your caloric intake.

Most COPD patients need a high protein intake. Protein plays an essential role in the structure, function, and regulation of body tissues. Most notably, protein helps you build muscle and counteract muscle atrophy which is common in COPD patients. Maintaining muscle mass is important for respiratory patients because strong muscles take less oxygen to function, thus reducing the burden on your lungs. While you probably get most of your protein through meat, there are many other great sources of protein, including but not limited to fish, eggs, dairy products, nuts, and beans.
You might think of fats as being “unhealthy.” But you may be surprised to find that many COPD patients are prescribed high-fat diets. The problem is that many people don’t know the difference between healthy fats and unhealthy fats. Unhealthy fats like saturated fat or trans fat include things like beef or pork fat, margarine, butter, and shortening. Eating too many of these things can lead to increased blood cholesterol levels and LDL cholesterol levels. Healthy fats, on the other hand, like monounsaturated fats and polyunsaturated fats include avocados, olives, nuts, olive oil, and more. Fatty fish like salmon is also a great source of healthy fats like omega-3.
While it may seem like COPD diets are pretty restricted, this is not necessarily the case. It’s important to avoid foods that are high in added sugars, sodium, and unhealthy fats. However, aside from that, you simply need to meet your minimum caloric intake for the day and any other requirements that your doctor sets. You still have plenty of freedom to choose what you eat and switching up your meals can even keep you on track for meeting your goals by preventing burnout.
Upgrade to a Portable Oxygen Concentrator
After being prescribed oxygen, many people choose the first oxygen device they think of — oxygen tanks. Most people know about oxygen tanks and they’ve seen people use them. But that doesn’t mean they’re the best option for you and your lifestyle. Although oxygen tanks are a popular choice, they tend to be heavy and bulky meaning they are difficult to maneuver. Fortunately, there is an alternative known as portable oxygen concentrators.

A portable oxygen concentrator is unlike an oxygen tank in that it doesn’t hold oxygen within the unit. Rather, it takes in ambient air, removes nitrogen and argon, and puts out medical-grade oxygen. POCs are electronic devices and they run off of powerful lithium-ion batteries, so you simply need to charge the battery via a car or wall outlet and you’ll be on your way. The most notable benefit of this is that you won’t have to keep going out of your way to refill or replace your oxygen tanks when they run out.
Another benefit of portable oxygen concentrators is their lightweight and compact design. Unlike oxygen tanks which are oblong-shaped, POCs are small enough and light enough to be carried on your shoulder. This opens up a world of possibilities and enables you the freedom to live life on your own terms without being defined by your disease. Inevitably, this leads to more options for you and a lower chance of experiencing burnout with your COPD treatment plan.
Reduce the Clutter
Sometimes it’s not our COPD treatment plan itself that’s causing us to feel burnt out, but all the extra clutter around us. The term “clutter” can be defined as anything that complicates our lives and occupies our thoughts but doesn’t provide any real benefit to us. If you live with clutter too long it can really start to become exhausting and you’ll notice yourself losing motivation in other areas of life such as your exercise routine, diet, and making it to doctor’s visits.

For some people, this might imply clutter within the home. For example, having a messy bedroom, bathroom, or kitchen can lead to a lot of discomfort in your daily life, and as a result, you might find yourself too distracted to follow your COPD treatment plan. Eliminating physical clutter like this is as simple as taking the time each day to organize your home and avoid getting to the point where it’s too much to manage. If you’re too busy to clean, you might consider hiring a caretaker who can help out around the home.

Another type of clutter is “mental clutter.” Think of this as the opposite of mental clarity. Instead of being able to concentrate on what you’re doing in the current moment, your thoughts are always wandering to something else. Mental clutter can certainly be caused by things like a messy home, but it’s more likely to be caused by something that takes your focus off of what you’re doing in the present moment. For example, watching the news for too long or spending too much time on social media are both things that can take your focus off the present moment.

Cognitive behavioral therapy (CBT) is one way of dealing with problems related to mental clarity. This is a type of therapy that’s focused on reversing negative or unproductive thought processes. CBT has become very common among people with chronic conditions like COPD as awareness around mental health problems has increased. During CBT, you will work one-on-one with a certified therapist who will guide you through the process.
Practice Meditation
Meditation comes in many different forms. However, in most cases, the goal is always to achieve a state of mental clarity and well-being. Meditation helps train your mind to think clearly and without distractions. It also promotes emotional well-being while reducing anxiety and in some cases even improving physical well-being. By far the most popular form of meditation for COPD patients is Tai Chi. This practice combines traditional meditation principles with martial arts. It’s popular for COPD patients because it teaches you to control your thoughts, breathing, and balance, all of which are important if you’re trying to improve your health. Read through this post we made about Tai Chi to learn more.

Speak With Your Doctor
Your doctor should be your first point of contact when it comes to anything related to your COPD treatment plan. If you know that you need to make changes, your doctor will be able to tell you what changes are acceptable and which are not. He/she may also be able to provide you with additional resources or direct you to another specialist who can help you deal with issues related to COPD burnout and fatigue. Sometimes burnout is due to poor sleep quality, so he/she may recommend that you get tested for obstructive sleep apnea (OSA) and other sleep disorders.

Another change your doctor may be able to do is make changes to your medication routine. Corticosteroids are one of the most common drugs used to treat COPD because they reduce inflammation in the lungs. However, these drugs are also known to have adverse psychiatric effects such as mania, depression, and cognitive impairments, all of which can contribute to burnout and a negative outlook of your disease. Your doctor may be able to reduce your dosage or prescribe you a different medication altogether.
Conclusion
Being “burnt out” on your COPD routine can be exhausting. On one hand, you may be tempted to revert to your old way of living and entirely forget about your COPD treatment plan. However, on the other hand, you understand that the best way to deal with the symptoms of your disease is through persistence and consistency. If you feel like you’ve reached this point, be sure to try some of the tips above to get back on track.
Ultimately, you will want to consult your doctor if you’re struggling to keep up with your treatment plan. It’s not unusual for someone to struggle, especially if they’ve had COPD for many years. Here at LPT Medical, we strongly believe that a portable oxygen concentrator can help you regain much of the freedom that you lost after being diagnosed with COPD. As a result, you’ll be able to approach your treatment plan from more angles and prevent burnout.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
We sell some of the top-rated portable oxygen concentrators in the industry such as the Caire FreeStyle Comfort, Inogen One G5, and the GCE Zen-O Lite. When you contact one of our oxygen concentrator specialists, they will work with you one-on-one to understand your needs and align you with a concentrator that matches them. We also have many different buying and financing options to help you manage payments in a way that works with your budget. To get started, simply give us a call or send us an email.
.png)
For the majority of people, summer is the best time for being active. No matter what type of physical exercise you like to do, everything tends to be more enjoyable and productive when it’s done outside rather than inside. What’s more, studies have shown many health benefits to being outdoors including lowering blood pressure, reducing stress, and preventing insomnia, a sleep disorder that often results from a lack of sunlight during the day.
On the other hand, if you have COPD or any number of chronic respiratory conditions, you may find it difficult to exercise during the summer. Hot weather can exacerbate your respiratory symptoms and sap your energy making you feel unmotivated to face the challenges of your disease. Additionally, several allergens such as pollen, mold, and insect bites are at their peak in the summer months, which can lead to a whole host of problems for COPD patients as well.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Despite the challenges of staying active during the summer, it’s imperative that COPD patients do so. Exercise is a key part of any treatment regime because it strengthens the lungs and makes your body more efficient at using oxygen, thereby reducing symptoms of breathlessness and fatigue. By having strong stabilizing muscles that you enhance by exercising, you’ll be able to reduce your risk of experiencing a fall or any other type of physical injury. In the following sections, we’re going to take a look at a couple of tips for staying active in the summer if you have COPD. Please don’t hesitate to leave a comment at the end of the article if you have any questions or concerns.
Plan Your Trips Carefully
The first, and probably the most crucial tip to help you stay active during the summer is to plan your trips carefully. Depending on where you are in the country, weather can be variable and sometimes even unpredictable. You should get in the habit of checking the weather regularly and comparing it across multiple sites so that you have a good picture of what the weather will be like. Even then, weather forecasts are never perfect so you should always plan for the worst-case scenario.

Generally speaking, the hottest time of the day is in the afternoon, so ideally, you’ll want to plan your outdoor activities in the morning or in the evening. However, this can vary if there is cloud coverage or precipitation. Since everyone with COPD has different severities of respiratory symptoms, it’s difficult to say what temperature is “too hot.” Most people know their limits and you may have a higher tolerance for hot weather if you’ve spent most of your life in a hot climate. According to Science Direct, about 4% of the population is heat intolerant. This means that they are not able to acclimate to high degrees of heat stress.

Aside from checking the weather before you leave the house, you should also check the air quality in your area. Summer is wildfire season in much of the country and there’s also a high risk of allergens like pollen and mold. And although car exhaust tends to dissipate better in the summer than in the winter, it’s still possible for there to be a lot of pollution during the summer, especially if it’s a little cooler and overcast.
Dress for the Weather
The way you dress can have an immense impact on how you tolerate heat while you’re outdoors. Short-sleeve, loose-fitting clothing is always ideal if you’re going to be outside for an extended period of time and you should be sure to wear lighter colors that reflect more heat. Another important thing to consider is the material of clothing that you wear. Breathable materials like cotton, polyester, and nylon are very light and perfect for a hot summer day. But you should be sure to avoid heavy materials like wool and insulated clothing like rain-resistant shirts or pants.

Another must-have article of clothing for a sunny day is a hat. If your face and head are exposed to too much sunlight you’ll feel fatigued much quicker and you might start to get a bad headache. You’re going to want to wear a wide-brimmed hat that keeps the sun off your face, head, and neck, but just like your shirt, it should be made of breathable material. According to the University of Michigan, 50% of the body’s heat is released from the scalp and face.
Stay Hydrated
When it’s hot out, your body releases more sweat in order to keep you cool. And since sweat is 99% water, you can become dehydrated very quickly by being out in the sun. The CDC recommends drinking at least 8 ounces of water every 20 minutes while you’re outside. And ideally, you should be drinking in consistent intervals so that your body isn’t working so hard to process it all at once. But you should also take care to stay hydrated before you exercise outdoors, not just during your exercise.
.jpg)
Equally important as drinking enough water is avoiding drinks or food that can dehydrate you. While salty foods may sound tempting while you’re outside exercising, be aware that you will have to drink more water to accommodate this. And while sugary sports drinks or energy drinks may give you a nice boost before exercising, they can also dehydrate you and you’ll experience an energy crash after its effects wear off. Ideally, you should stick with water and unsalted foods while exercising in the heat.
Keep Medications on Hand
Just like any other time you leave the home, you need to make sure you have all of the medications you need. Many COPD patients use fast-acting bronchodilators which are designed to quickly release tension in the chest and airways if you’re experiencing a flare-up or exacerbation of your symptoms. These are especially important to have on hand when you’re exercising and away from home because you won’t have many other options for alleviating your symptoms.

Know the Warning Signs of Heat-Related Illness
The easiest way to prevent heat-related illness is to simply know the warning signs. The sooner you realize that your body is overheating, the sooner you can make it to a shaded area or air-conditioned building so that you can begin to recover. Heat exhaustion can happen slowly over the course of a couple of hours or it can come on very quickly so you should always be on the lookout for any symptoms. According to Healthline, there are three different stages of heat emergency: heat cramps, heat exhaustion, and heatstroke.

Heat cramps are more common in older people who have been physically active. They’re also more common in people who are overweight or who have been drinking alcohol recently. The primary symptoms of heat cramps are muscle pain and tightness. The second stage of heat emergency is heat exhaustion which comprises a list of potential symptoms including:
- Headache
- Dizziness
- Mild confusion
- A fast heart rate or fast breathing
- Extreme thirst
- Nausea
- Heavy sweating
-
Muscle cramps
Heatstroke is the most severe form of heat emergency and it can include all of the aforementioned symptoms in addition to:
- Confusion
- Irrational behavior
- A body temperature over 104°F
- Rapid breathing or heart rate
- Loss of consciousness
- Seizures
If you’re outside exercising with a friend make sure that they are also aware of these symptoms and don’t be afraid to check up on each other regularly.
Focus on Moderate Exercise
One of the key mistakes many people make when starting their pulmonary rehabilitation routine is believing that they need to practice high-intensity exercise in order to stay healthy. However, for most COPD patients, high-intensity exercise is not necessary and it can even lead to a respiratory exacerbation if you’re not careful. What’s more important than anything is that you’re consistent with your exercise and that you don’t stay sedentary for long periods of time. Walking, hiking or moderate weight lifting exercises can all be beneficial for lung health.
![]()
Have a Safety Net in Place
A safety net is a must when you leave the house during the summer. Before you do anything, make sure to tell at least one person where you will be going and how long you will be gone. This way, if there’s an emergency, your friend or loved one will know exactly where to look for you. Secondly, you should create a list of contacts of people that you can call if you experience a flare-up in your symptoms and don’t feel comfortable driving or walking home alone. However, if you believe you’re experiencing a medical emergency, you should always call 9-1-1 first.
Use a Portable Oxygen Concentrator
There comes a time when oxygen tanks become too much to manage. While supplemental oxygen is a medical necessity for most COPD patients, oxygen tanks are extremely heavy and bulky making it difficult to get out of the house and enjoy the outdoors. Fortunately, there are alternatives to traditional oxygen tanks and they’re called portable oxygen concentrators. A portable oxygen concentrator puts out medical-grade oxygen just like a tank, but the difference is that it’s an electronic device that runs on batteries. Simply have a fully charged battery on hand and you’ll have access to an infinite supply of oxygen.

Another great thing about portable oxygen concentrators is that they’re very easy to operate so you won’t have any problems making adjustments to your flow setting on the go. POCs like the Caire FreeStyle Comfort and Inogen One G5 only have a few buttons on them so you can have it up and running in just a few minutes and feel confident about using it outside of the home. Both of these concentrators offer a high flow setting and they weigh under 5 pounds meaning they’re incredibly versatile. Most POCs also have a DC charging option available, so you won’t have to worry about running down your battery while you’re driving to whatever destination you’re going to.

All things considered, portable oxygen concentrators are a much more financially sound and practical long-term investment. While they do cost more money upfront than oxygen tanks, the important thing to remember is that you don’t have to keep paying to refill them. In the long term, this could save you hundreds if not thousands of dollars. What’s more, POCs often come with manufacturer warranties which will have you covered if anything goes wrong with your unit within the first couple of years after your purchase.
Speak with Your Doctor
As always, if you have any concerns about being able to cope with the hot weather this summer, you should address them with your doctor. Heat-related illness is a potentially serious condition. According to the CDC, there are about 702 heat-related deaths in the United States each year. Unfortunately, due to the symptoms of COPD including chronic breathlessness and fatigue, COPD patients are oftentimes at a higher risk of experiencing heat-related illness than the general public. This study found that hospitalization in COPD patients increased by 7.6% for each degree Celcius over 29°C (84°F).
As aforementioned, no two cases of COPD are the same so it’s impossible to say what advice your doctor will have for you. If you have more severe stage 3 or 4 COPD and heat-related illness runs in your family, he/she will likely recommend that you use a high degree of caution when it comes to exercising outdoors. But if you’re stage 1 or 2 and you don’t use oxygen regularly, your doctor’s guidelines might be a little more lenient.
Conclusion
As a COPD patient, consistent exercise is very important for your well-being. But severe weather conditions like high heat or excessive dryness or humidity can make this seem like an insurmountable task. So, if you want to exercise outdoor this summer, you should take some time to plan ahead, and as always, if you have any questions about coping with extreme weather, be sure to address them with your doctor or pulmonologist as soon as possible.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
If you’re looking for a brand new, used, or refurbished portable oxygen concentrator to help you get on your feet this summer, look no further than LPT Medical. We proudly offer pulse dose and continuous flow oxygen concentrators from some of the most reputable manufacturers on the market including but not limited to Caire, Inogen, and AirSep. While there are many different concentrators out there, our respiratory specialists will take the time to understand your wants and needs and recommend the perfect device for you. We also have a variety of different financing options available to help you pay off the device in a more manageable way. Reach out to us either by phone or email to speak with an oxygen concentrator specialist.
.png)
If you’ve already read our blog on treating and overcoming sleep apnea, you know that sleep apnea is a common disorder with potentially serious implications. While sleep apnea symptoms may seem mild at first, over time, obstructive sleep apnea may eventually lead to increased blood pressure, heart disease, liver disease, depression, and more.
But when sleep apnea is combined with other conditions like chronic obstructive pulmonary disease (COPD) , it’s often a two-way road. According to a new study called Canadian Cohort Obstructive Lung Disease (CanCOLD), sleep disruptions — like those experienced in sleep apnea — could lead to a greater risk of long-term COPD exacerbations.
Led by researchers at Montreal’s McGill University, this ongoing study aims to analyze over 2,000 Canadians with mild to severe COPD. Whereas previous trials have shown that COPD symptoms may lead to sleep disturbances, this study will help medical professionals better understand the characteristics of COPD and how they’re affected by a poor night’s sleep.
Using the Pittsburgh Sleep Quality Index (PSQI) and negative binomial regression, the team observed data from 480 participants over an 18-month assessment period. During this time, 185 of the participants experienced at least one exacerbation and 203 had a baseline PSQI score over five, indicating that the participant had a poor night’s sleep. The study also concluded that both symptom- and event-based exacerbation risks were associated with a higher PSQI score.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What We Can Take Away From The Study
When it comes to other major causes of death like cancer and heart disease, COPD awareness remains low both in the United States and around the world. Studies on COPD are often overshadowed by discussions about lung cancer and other respiratory conditions. However, this study may help bring some much-needed awareness to a condition that so many people suffer with.
Unlike acute illnesses, chronic conditions like COPD progress slowly and oftentimes without any cause for concern. You may have started to develop COPD years ago but brushed off your symptoms as “getting old” or “being out of shape.” This study reaffirms the importance of getting checked regularly for both healthy lung function and sleep quality.
Sleep Quality Matters
It’s easy to dismiss a bad night’s sleep as unimportant or insignificant, but when this issue persists, it’s almost always linked to an underlying condition. And even when it isn’t, feelings of restlessness and chronic fatigue can have an impact on the severity and frequency of your COPD symptoms and exacerbations. What’s more, if you’re sleepy frequently, it will make it significantly more difficult to deal with the daily struggles of managing COPD.

As such, it’s important to take all necessary precautions to ensure that you sleep well and aren’t disturbed. First and foremost, you should make sure that you get an adequate amount of sleep each night. According to the National Sleep Foundation, adults between the ages of 24 and 64 should get between 7 to 9 hours of sleep and anyone older than 65 should get at least 7 to 8 hours of sleep. Let’s take a look at some tips for getting a better night’s sleep.
Sleep-Wake-Time Consistency
Researchers have studied sleep extensively and one of the most common rules they stress is creating a sleep routine and sticking with it. Many people will tell you that you need to get up as early as possible and that staying up late is a problem. But in reality, you simply want to pick a schedule and follow it every day of the week.
Avoiding Screens Before Bed
Technology helps us all lead more productive lives and has allowed us to learn more about the world than any other time in human history. But staring at a screen right before bed may have the opposite effect. According to the National Sleep Foundation, using electronics before bed delays the circadian rhythm in your body and slows the release of melatonin (the sleep-inducing hormone in the brain) making it harder to fall asleep when you need to.
Calcium and Magnesium Levels
Magnesium is an essential mineral that’s responsible for 300 biochemical reactions in the body. It’s one of the most important minerals in the body, helping to maintain a healthy immune system, strong bones, and muscle function. And if there isn’t enough magnesium in the body to absorb calcium, it can lead to weak bones and digestion problems. Additionally, calcium is responsible for tightening and tensing muscles and nerves while magnesium calms and relaxes them. So, having this balance is essential for deep and restful sleep.

Some foods high in magnesium include:
- Whole wheat
- Spinach
- Quinoa
- Peanuts, cashews, and almonds
- Dark chocolate
- Black beans
- And avocado
Functioning Adrenal System
A well-functioning adrenal system is essential to good sleep and overall well-being. The adrenal glands are located on top of each kidney and produce hormones that your body needs. In a healthy body, these hormones help manage stress, regulate metabolism, control blood pressure, and more. However, there are a variety of disorders that can negatively affect the adrenal glands resulting in an adrenal deficiency. Junk food, sugar, and caffeine are known to reduce adrenal function making you feel groggy and restless after waking up.
Blood Sugar Levels
In what is often a vicious cycle, blood sugar levels affect your sleep, and poor sleep affects your blood sugar as well. Blood sugar is regulated by what you eat and when you eat it. While it’s not a good idea to eat a heavy meal late in the day, eating too early and then not eating all evening can cause a dip in blood sugar in the middle of the night. Low blood sugar can cause you to wake with a headache or feel out of sorts, making it difficult to go back to sleep.
On the other hand, if your blood sugar is too high, your body is likely to try to rid itself of excess sugar through the kidneys causing you to wake up to use the bathroom. Many people who are trying to lose weight feel that bedtime snacks add unnecessary calories but weight loss isn’t just about calorie counting. In order to maintain a healthy metabolism, good sleep, hormone regulation, and stable blood sugar are essential.
Awareness Is Key
Maintaining a healthy sleep schedule, eating right, and avoiding sugar and caffeine before bed are all great habits to get into, but without being tested, it’s difficult to diagnose and treat any sleep disorder you may be struggling with. If you have COPD, you should speak with your doctor about having both a sleep study and an exercise test.
Sleep Studies
The easiest way to detect sleep apnea and other sleeping disorders early on is through a sleep study. Also known as a polysomnogram, a sleep study is a non-invasive procedure doctors use to analyze sleep patterns, heart rate, and brain activity in order to diagnose sleep disorders. Aside from sleep apnea, these disorders include narcolepsy, insomnia, restless leg syndrome, and more.
No matter whether you have bronchitis, emphysema, or any other lung condition, a sleep test will provide both you and your doctor with critically important information about your body, mind, and overall health. Using the test results and your medical history, your doctor will be able to narrow down the source of your sleep disruptions and determine if any actions need to be taken on your part to get a better night’s sleep.
Exercise Tests
Similar to how a sleep study will reveal crucial information about your breathing patterns while you sleep, an exercise test is useful for monitoring how your lungs function while undergoing physical exertion. If you have COPD, an exercise test will reveal the condition's effects on your physical abilities and help your doctor set up an exercise routine that’s right for you.
There are two main types of exercise test: laboratory tests and field walking tests. Patients who already have a chronic pulmonary condition may opt for a field walking test because they are able to stop and take a break, whereas laboratory tests are usually better for someone who still retains most of their physical abilities. Some exercise tests include the 6-minute walk test, the incremental shuttle walk test, the endurance shuttle walk test, and the cardio-pulmonary test. Your doctor will help you determine which one is best for you.

When used in tandem with a sleep study and your medical history, an exercise test will provide your doctor with a wide range of information about your overall health. For example, if your doctor discovers disruptions in your sleep pattern, he/she may be able to link it to an issue you experience while exercising or vise versa. This will make it easier to create a treatment plan that’s best for you.
Sleep Affects Your Overall Health
One of the major mistakes people make when approaching an issue like sleep apnea or sleep deprivation is that they treat it as an isolated issue. These people assume that the fatigue or restlessness that they feel is the extent of the effect it’s having on their bodies. Unfortunately, as the study suggests, this is not the case.

Aside from short-term symptoms like decreased performance and alertness, long-term sleep deprivation can put you at a higher risk for heart disease, high blood pressure, depression, and more. Chronic sleep deprivation can also significantly reduce your quality of life and put a strain on your relationships.
You’re at a Higher Risk With COPD
Above all, this study shows us that you’re at a higher risk of experiencing and being hospitalized for COPD exacerbations when you get poor sleep. Whether you’re suffering from chronic sleep apnea or you’re experiencing poor sleep due to anxiety or depression, you should take these issues seriously in order to avoid respiratory complications.
Most people tend to think of COPD exacerbation triggers as air pollutants and irritants or sicknesses like the flu or the common cold. However, according to the study, the quality of sleep you get also has an impact on when exacerbations occur and how severe they are. While COPD is manageable on its own, frequent exacerbations can take a serious toll on your health and can even be fatal.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Sleeping Disorders That Can Cause Exacerbations
Unfortunately, it’s not just poor sleep quality that increases your risk of exacerbations; sleeping disorders like sleep apnea and insomnia can also play a role while simultaneously contributing to poor sleep. Many people who have a sleeping disorder are never diagnosed because they either don’t realize they have a problem or they believe nothing can be done.
Like maintaining healthy sleep habits, diagnosing and treating sleep disorders starts with awareness. Sleep constitutes a third of our lives. And during this time, many important processes occur that are necessary for us to lead happy and healthy lives. Sure, preventing that grogginess and sleepiness when you wake up is part of it, but sleep is vital for the rest of the body as well.

According to the Mayo Clinic, your immune system is affected by lack of sleep. Proteins called cytokines are released by the immune system when your body is experiencing inflammation, stress, or infection. However, less cytokines are produced when you’re deprived of sleep. What’s more, cells and antibodies that fight infection are reduced when you don’t get enough sleep.
As a COPD patient, getting sick could lead to a serious flare up in your symptoms and even result in exacerbations due to increased mucus production and difficulty breathing. We’re going to take a look at just a few of the most common sleep disorders so that you know when to seek help.
Sleep Apnea
Sleep apnea is a condition characterized by disrupted breathing while sleeping. There are three main types of sleep apnea that you should be aware of.
- Obstructive sleep apnea is one of the most common forms of the condition and it results when throat muscles relax and block your airways.
- Central sleep apnea is the result of the muscles that control breathing not receiving proper signals from your brain.
- Complex sleep apnea is the result of having both these conditions simultaneously.
As you can imagine, these two disorders are treated in very different ways. Continuous Positive Airway Pressure (CPAP) machines are one of the most common treatment methods for obstructive sleep apnea. Unlike a normal in-home oxygen therapy device, a CPAP machine is designed to blow at a pressure that will keep your airways open and free of obstruction while you sleep. When the device is on, it creates a cushion along the upper airway preventing the tongue, uvula, and soft palate from interfering with the airway.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
When it comes to central sleep apnea, medication is often the only effective solution. Medication like theophylline or acetazolamide are used to stimulate breathing while you sleep. And if you’re on any opioid medications, your doctor may take you off these to prevent any complications.

Insomnia
Insomnia is another common sleep disorder affecting around 60 million Americans. Insomnia is defined as difficulty falling asleep or feeling dissatisfied with the quality of sleep that you do get. Many people who have insomnia are unable to fall asleep even when they’re tired and often wake up feeling groggy, fatigued, and unable to concentrate.
Depending on what is causing the insomnia, both medical and non-medical treatment methods may be used. Cognitive behavioral therapy (CBT), counseling, and group therapy may be beneficial non-pharmacological treatments while relaxation techniques, breathing exercises, and changes to your sleep schedule may help as well. Medication for insomnia includes both benzodiazepine sedatives and non-benzodiazepine sedatives.
Narcolepsy
Narcolepsy is a neurological disorder that results in an irregular regulation of sleep and wakefulness. Someone with narcolepsy may fall asleep frequently during the day and may feel sudden muscle weakness as well during any type of activity. People who experience narcolepsy may also have difficulty falling asleep or staying asleep at night due to their circadian rhythm being disrupted during the day. Although this disorder usually starts at a young age, it often goes undiagnosed in many people.
Restless Leg Syndrome (RLS)
RLS results in unpleasant feelings in the legs such as aches, tingling, burning, or general discomfort. It’s considered a neurological movement disorder and is commonly associated with periodic limb movements of sleep (PLMS), which is a similar condition that occurs while the person is asleep. For some people, this condition doesn’t have a significant impact on their ability to get a restful night’s sleep. However, restless leg syndrome almost always does.
Circadian Rhythm Disorders
We’ve talked before about the importance of the circadian rhythm in managing your sleep-wake cycle and getting a good night’s sleep. And in a circadian rhythm disorder, a person’s biological clock is out of sync, especially when it comes to external time cues like the natural dark-light cycle.

Although your sleep cycle will never be completely in sync with external cues, someone with these disorders may feel completely restless and sleepy in the middle of the day and wide awake at night making it difficult to find a sleep schedule that works for them. These disorders may eventually lead to insomnia or hypersomnia (excessive sleepiness).
What You Can Do To Avoid COPD Exacerbations
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Now that you understand how poor sleep quality and sleep disorders can lead to COPD exacerbations, you need to know exactly what steps you should take to avoid complications. While chronic sleep disorders and general sleepiness are dangerous on their own, for someone with COPD, they could lead to a life-threatening exacerbation. Fortunately, you don’t have to leave anything up to chance when it comes to your health and you can get started right away improving your sleep quality. Simply follow the steps below.
1.) Make A List of Your Symptoms
As you’re probably well aware, living with COPD or any chronic illness can be challenging. You may be following a strict diet, exercise routine, sleep schedule, and work schedule. And it’s easy to get confused as to what you should be doing and when. As such, the more you can write down on paper, the better.

One reason to make a physical list is because you may forget when it comes time to see your doctor. COPD has a long list of symptoms and most people with the condition experience them all at one point or another. The more information you have about what symptoms you’re experiencing and when, the better you and your doctor will be able to pinpoint what’s causing the exacerbation. On your list, be sure to thoroughly describe what symptoms you experienced, the date, the time, as well as details about your sleep schedule and sleep quality.
2.) Visit A Doctor
The second step in this process is to visit a doctor. As aforementioned, awareness is key when it comes to being able to effectively treat sleep disorders and COPD symptoms. If there’s any information about your symptoms that your doctor isn’t aware of, he/she may not be able to treat them effectively. Since COPD exacerbations are linked to your diet, sleep patterns, and overall health, you should try to provide a thorough overview of your symptoms.
3.) Don’t Be Afraid to Ask Questions
Chances are, you’re going to have a few questions about your symptoms and how your sleep quality may be affecting them — don’t hesitate to ask them. Although doctors have your best interest in mind, they aren’t infallible. There’s a chance they may have overlooked something when coming up with your treatment plan. And it’s important for you to understand your condition as well as possible after leaving the exam room.

For example, if you’re curious about sleep studies, exercise tests, or medication that you heard about online, it never hurts to ask your doctor if they might be a viable option. The worst that can happen is they suggest a better option and you become more educated about the condition you’re coping with.
Conclusion
For better or for worse, the quality of sleep you get at night affects the frequency and severity of COPD exacerbations you experience. Conversely, COPD symptoms like shortness of breath, coughing, and wheezing may prevent you from achieving a good night’s sleep. Understanding this two-way relationship is the first step in learning how to overcome it and live a healthier and more fulfilling life.
Although you will likely always experience some COPD symptoms, you can avoid exacerbations by making some simple lifestyle changes and being open and honest with your doctor. Additionally, taking the time to educate yourself on what triggers exacerbations will make it easier to manage the condition on a daily basis.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
For many decades, being prescribed oxygen has meant sacrificing your freedom and independence. Oxygen tanks were the only way for respiratory patients to receive reliable medical-grade oxygen, but they were heavy, bulky, and a pain to refill. Fortunately, oxygen manufacturers like O2 Concepts came around and came up with unique innovations in order to solve the issues that oxygen patients were facing. Most notably, we saw the advent of lightweight portable oxygen concentrators in the early 2000s.
Unlike oxygen tanks which hold oxygen within the unit, portable oxygen concentrators are electronic devices that derive oxygen from the surrounding air while removing unnecessary gases like nitrogen and argon. Oxygen manufacturers are able to make these devices much smaller and compact than oxygen tanks, and as a result, oxygen patients are able to go more places and do more things without being held back by their oxygen device.
Watch the video above as we unbox and review one of the top-rated portable oxygen concentrators on the market: the Oxlife Freedom. Then continue reading below for more specific details about this revolutionary oxygen device. Once you’re ready to start your search for a portable oxygen concentrator that meets your needs, reach out to our oxygen concentrator specialists here at LPT Medical. We’ll answer any questions you have and get you the best deal on a new, used or refurbished unit.
Pulse Dose Oxygen Delivery on the Go
One of the first things you’ll notice about Oxlife Freedom is that it has pulse dose oxygen delivery as opposed to continuous flow oxygen. So, instead of putting out oxygen in a constant stream it carefully monitors your breathing rate through the nasal cannula and delivers oxygen at the optimal moment. This has a number of advantages including extending the battery life and helping to keep the device lightweight and manageable.

To put this into perspective, the Oxlife Freedom weighs just 6 pounds. On the other hand, a typical continuous flow portable oxygen concentrator weighs over 10 pounds and sometimes even as much as 20 pounds. Generally speaking, most people are able to carry a portable oxygen concentrator on their shoulder if it’s under 10 pounds. Anything over that, however, and you’ll likely need to resort to a rolling cart which only adds more weight and bulk to your device.
Another great benefit the Oxlife Freedom has going for it is its small form factor. The dimensions of the Oxlife Freedom are as follows: 9.4 inches tall, 3.4 inches deep, and 9 inches wide. Whether you’re relaxing at home or out for a walk, you’ll find that the Oxlife Freedom is small enough that it won’t obstruct your movement, and if you’re going for a drive, you can easily put the device in the seat next to you without it getting in the way. Just make sure your Oxlife Freedom is secure before you start driving.
If you’re worried about using your POC while you sleep, don’t be! The Oxlife Freedom intelligent delivery system will closely monitor your breathing while you sleep. This technology even has the ability to detect shallow mouth breaths so you don’t need to worry about getting the oxygen you need while you sleep.
Dynamic Network Analysis® (DNA) Technology
DNA is a system designed by 02 Concepts specifically for use in their Oxlife Freedom and Oxlife Independence oxygen machines. Essentially, DNA connects your concentrator to a secure proprietary network. This network enables oxygen providers and caregivers to use usage data to provide oxygen patients with a new level of customer service and efficiency. The end goal is to ensure that the oxygen patient is using oxygen as prescribed and to prevent COPD readmittance.

There are a host of other services that DNA provides the oxygen user. For example, it will passively monitor your equipment for changes in temperature and purity and make adjustments on the fly. The DNA technology will help you make better decisions about your oxygen concentrator maintenance and repairs so that you can proactively prevent downtime in your oxygen delivery.

While other oxygen concentrators have implemented technologies similar to DNA technology such as Inogen Connect with the Inogen One G5 and CaireVIEW with the FreeStyle Comfort, O2 Concept’s Oxlife Freedom was technically the first “smart portable oxygen concentrator.” What’s more, DNA provides oxygen patients with many features that aren’t available with the G5 or the FreeStyle Comfort.
Sleek and Functional Design
When you’re out and about enjoying your day, the last thing you want to deal with is a complicated piece of technology. Life is busy enough with work, chores, and other responsibilities so it doesn’t make sense to invest in an oxygen device that makes your life harder. Luckily, through much trial and error, O2 Concepts has come up with a design that is sleek, functional, and easy to learn all while providing you with the oxygen you need to stay healthy.

The user interface of the Oxlife Freedom has a transflective display that makes it easy to read whether you’re inside or outside in the sunlight. The interface is also very minimalistic with only four buttons that you need to worry about. Two of them are used to adjust the oxygen flow up or down; one is used to turn the device on and off, and the last button is used for the menu. There are also a variety of different symbols that may pop up on the screen. Simply refer to the user manual that comes with your device to learn what each one means.
Conclusion
The Oxlife Freedom is an oxygen concentrator that’s aptly named. With the Freedom, you’ll be able to get out of the house and do more than you ever thought possible with COPD or any other lung condition. Unlike the oxygen tanks that came before it, the Oxlife Freedom is extremely lightweight, compact, and versatile. It’s also one of the first oxygen concentrators in the world to offer “smart” technology which monitors your oxygen usage, device condition, and much more in order to proactively manage your health. It also keeps you connected with medical specialists and device technicians who can help you out in case of an emergency.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
While the Oxlife Freedom is an amazing portable oxygen concentrator, it’s far from the only device we would recommend to oxygen patients. We understand that it can be overwhelming trying to learn about each and every device on the market — this is why our oxygen concentrator specialists are here. Simply give us a call and we’ll walk you step-by-step in choosing an oxygen device, assisting with financing options, and even helping you collect the necessary medical paperwork.
Oxlife Freedom Specs
Battery Life
| Flow Setting | Hours of Use |
| 1 | Up to 5 Hours |
| 2 | Up to 4 Hours |
| 3 | Up to 3 Hours |
| 4 | Up to 2 Hours |
| 5 | Up to 1.75 Hours |
Oxygen Output
| Flow Setting | Oxygen Output |
| 1 | 160 ml/min |
| 2 | 320 ml/min |
| 3 | 480 ml/min |
| 4 | 640 ml/min |
| 5 | 800 ml/min |
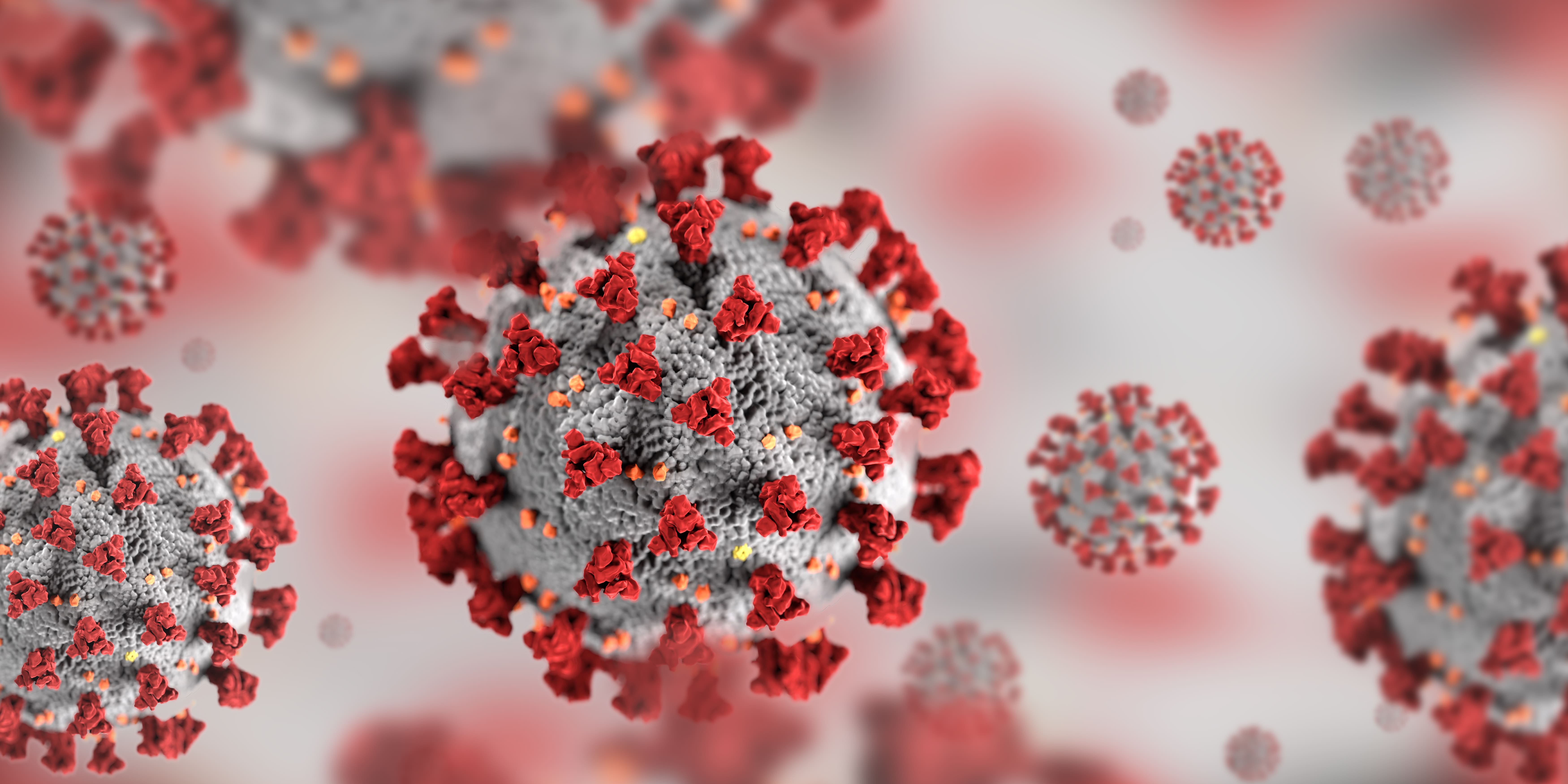
COVID-19 and lung damage is still a very new problem, and while research so far can tell us some of the impacts of COVID-19 on respiratory disease there is still a lot of uncertainty. That being said, it is important to fact-check information that you see on the internet, especially when it comes to something as serious as COVID-19 and lung damage.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
COVID-19 is a respiratory illness that is fast spreading and highly contagious, and while the vaccine is rolling out in the United States and internationally, catching COVID-19 is still cause for concern.
Here is a summary of the blog you are about to read:
- COVID-19 has lasting effects on your respiratory system
- People with lung disease have a high chance of experience harsher symptoms from COVID-19 than a person with no pre-existing conditions
- Don’t be fooled, if you are vaccinated you can still catch COVID-19, yet the effects of covid are much more mild than if you are not vaccinated, and this includes the damage to your lungs
How Does COVID-19 Affect your Lungs
COVID-19 can affect your lungs in mild and sometimes severe ways, and a lot of this depends on your health prior to catching the virus. If you have a relatively healthy respiratory system and have no pre-existing conditions COVID-19 can still hurt your lungs but not as badly as someone who already suffers from a chronic illness.
One of the most common implications caused by COVID-19 is pneumonia and in the most severe cases, acute respiratory distress syndrome. There is also the possibility of Sepsis as a complication of COVID-19, and this can also cause lasting damage to your lungs and other organs.
COVID-19 and Pneumonia
When you get pneumonia, your lungs fill with fluid and become inflamed, leading to breathing difficulties, this is extremely painful for lung patients who have diseases like Chronic Obstructive Respiratory Disease (COPD). When someone with COPD gets COVID-19 the symptoms can become so severe they require treatment at the hospital with a portable oxygen concentrator or even a ventilator.
Pneumonia occurs when your air sacs in your lungs fill with fluid, this limits their ability to take in oxygen and causes shortness of breath, a persistent cough and other symptoms.
While most people recover from pneumonia without any lasting lung damage, the pneumonia associated with COVID-19 can be severe, and people with lung disease have an even harder time healing from this.
Even after the disease has passed, the damage to your lungs may result in breathing difficulties that take a lot of time to heal completely, and with chronic conditions, it is unlikely the damage will heal completely.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Acute Respiratory Distress Syndrome (ARDS) and COVID-19
COVID-19 that causes pneumonia can progress further into a more severe state, and the air sacs which become filled with fluid start to leak from blood vessels in your lungs. Inevitably, breathlessness occurs, which can cause acute respiratory distress syndrome. ARDS is essentially a version of lung failure.
Patients with ARDS are usually unable to breath by themselves and may require a ventilator to help their bodies circulate oxygen through their body.
Sepsis and COVID-19
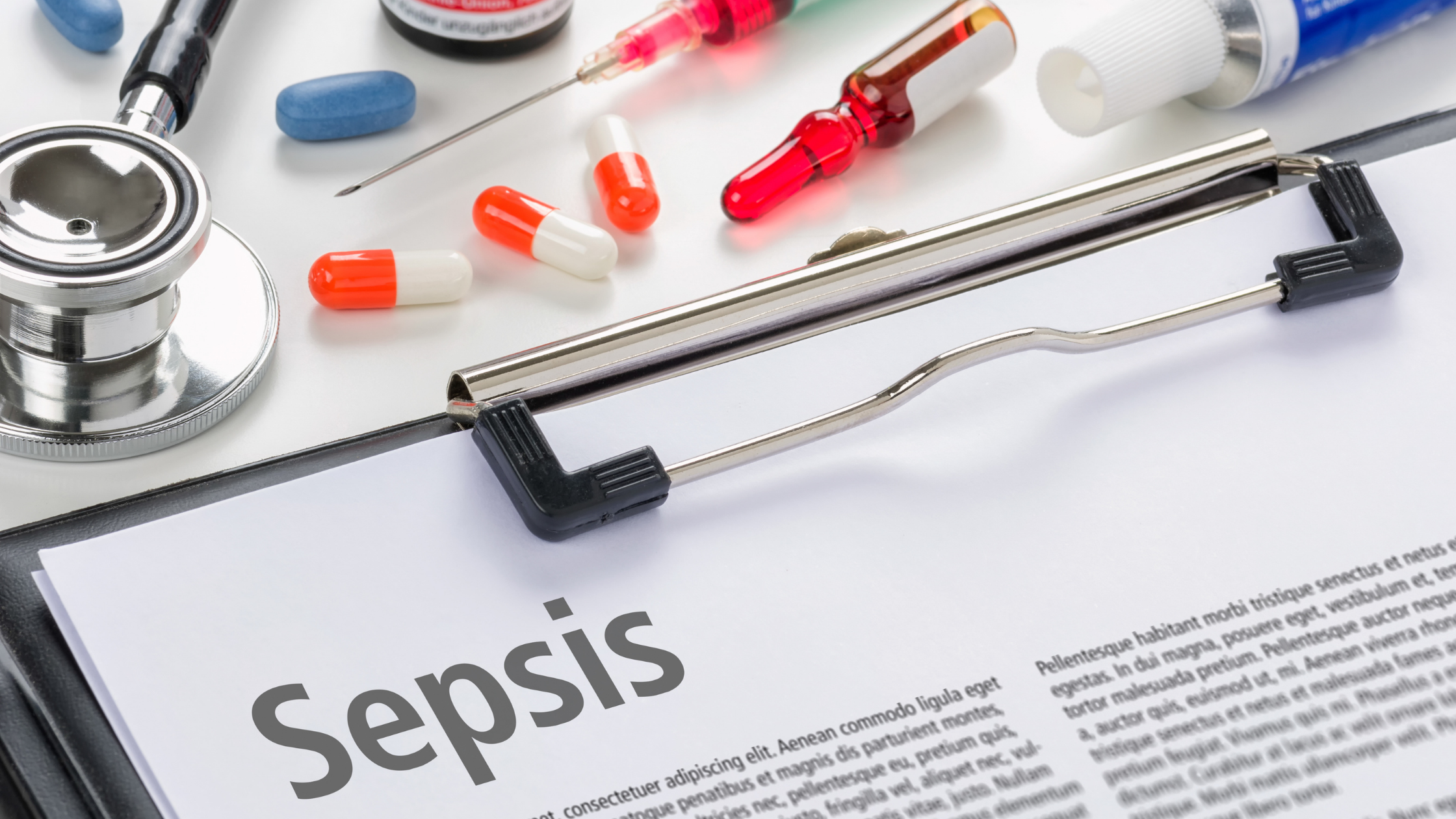
In severe cases of COVID-19 and people who also suffer from preexisting conditions, sepsis is another serious complication. Sepsis is a fast spreading infection that moves through the bloodstream, causing tissue damage everywhere it goes.
Sepsis causes long-lasting lung damage and also affects other organs in the long term.
Reducing the Chance of Lung Damage from COVID-19

If you have chronic medical conditions, such as diabetes, COPD or heart disease, its crucial for you to continue taking your medication and treating your disease optimally.
Take your oxygen as prescribed and monitor your health status and report to your doctor over the phone regularly. You can also use a pulse oximeter to measure when and if you are breathing appropriately.
Everyone, especially lung patients, need to maintain adequate nutrition by eating healthy and staying hydrated, this will keep your immune system healthy. Also double check that you are up to date with all of your vaccinations, even just getting the common flu can weaken your immune system and leave you more susceptible to catching COVID-19.
Also, be wary of any information you read on the internet that's not supported by researchers and institutions which require a peer review process in order to be published. Because COVID is relatively a new virus, the research is still in progress meaning that most results from studies over the past year and a half are not conclusive yet.
For example, you might have seen reports of vitamins, minerals and prophylaxis medications that can prevent/ or reduce lung damage, however there are no peer reviewed studies that are supporting it at this time.
The best way to avoid COVID-19 and worsening lung damage is to get the COVID-19 vaccine.

Is the vaccine safe for people with lung conditions?
There have been a plethora of studies that have concluded the vaccine is safe for people with lung conditions. The vaccine has been tested on people with long-term conditions and people from all age groups including older people.
In fact, it has been decided that people who are at high-risk should be prioritized to get the vaccine first. At this time, there is no reason to think the vaccine interferes with any medications and therefore, your treatment for your lung condition should continue as normal.
If you have asthma and you use biologics (otherwise known as mAbs, or monoclonal antibodies), talk to your doctor to discuss the timing of your vaccine and your asthma biologic. There is no evidence to show the vaccines are unsafe for you, however it’s advisable that there should be 7-day gap between your vaccine and your next asthma biologic.
Do not stop taking or change any of your medicines without speaking to your doctor first.
So how do we know the vaccine is safe?

Any approved vaccines must meet a strict criteria of safety, quality and effectiveness. And so all of the approved coronavirus vaccines go through certain clinical trials and they are checked that same way as any licensed medicines are checked. Other vaccines are being developed, but they will only be available to the public once they’ve been thoroughly tested.
A vaccine can not be given to people until the FDA oversees extensive lab testing of the vaccine. Usually this can take many years in order to ensure it is safe and effective. Because the COVID-19 vaccine was only developed and tested in a short period of time, some risk is involved, however data indicates that all of the available COVID-19 vaccines are safe.
Also the risk of COVID-19 is far greater than the small risk of the vaccine.
We know this because we can look at the rate of severe or life-threatening reactions to the COVID-19 vaccine, which is estimated to be about 1 in 100,000 patients, whereas the risk right now of dying from COVID-19 is substantially higher than that.
There are many deadly diseases that have been technically eradicated with the introduction of a vaccine. For example, Polio, Tetanus, The Flu (Influenza), Hepatitis B and A, Measles, Whooping Cough, and so many others have a vaccine that is successful in reducing the contamination and spread of the disease, and save millions of lives. COVID-19 can be added to this list eventually!
Overview
The risk of COVID-19 having long term effects and damaging your lungs is high for any person, but extremely high for someone with a pre-existing lung condition. If you have lung disease already, catching COVID-19 could mean hospitalization and it can be life threatening.
There are a number of ways to avoid catching COVID-19 by social distancing, washing your hands, and wearing a mask, and on top of all of those recommendations is to get vaccinated.
If you are still wary of getting the vaccine, talk to your doctor, they can go over your medication that you take and reassure you that the vaccine will not interfere with your medical condition nor your treatments.
Side effects of the vaccine are very normal, and oftentimes unavoidable and even uncomfortable. That being said, these short-lived side effects are much less dangerous than being exposed and unprotected against the coronavirus.
If you have a lung condition like asthma, COPD, of cystic fibrosis, continue to treat your disease during the pandemic. It is important that you stay healthy and get stronger so that your body is capable of fighting ailments including COVID-19. While exposure to coronavirus is extremely dangerous due to the virus and its contagious properties, the healthier you are the better.
If you need oxygen, be sure you have a portable oxygen concentrator that is reliable and durable. For all of your oxygen accessories needs, head over to the LPT Medical website or call 1(800)-946-1202 to speak with a respiratory specialist.

If you are prescribed an oxygen concentrator for chronic health problems and you experience symptoms of COVID-19, call your doctor. Do not change your oxygen levels on your own, unless you have been told to do so by your doctor.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













