Many people with COPD also struggle with anxiety. It's an understandable reaction to the daily worries and hardships of living with a chronic disease. However, for patients who don't find ways to treat their anxiety and manage it in healthy ways, that anxiety can grow to the point that it causes serious problems and affects many aspects of their lives.
One result of this chronic anxiety is panic disorder, or frequent panic attacks. A panic attack is, according to the Mayo Clinic, “a sudden episode of intense fear that triggers severe physical reactions when there is no real danger or apparent cause.”
Although they can be frightening and overwhelming, panic attacks are just that—panic. They aren't actually dangerous or life-threatening, even though they can trick your brain into thinking they are.
However, even though they are harmless in the short term, panic attacks are incredibly unpleasant to experience and can take a serious toll on your mental health. That's why treating anxiety and looking after your mental and emotional health is so important if you have COPD.
COPD patients are more prone to panic attacks for a variety of reasons, and the symptoms of COPD can make them even more difficult to manage and prevent. In this article, we're going to help you understand how panic attacks affect people with COPD and what you can do to recognize, manage, and prevent panic attacks in your own life.
What is a Panic Attack?

Panic attacks are explosive episodes of anxiety that often have no obvious cause. While they usually only last a short period of time—usually about ten minutes—those minutes can be absolutely agonizing.
In fact, the fear and physical symptoms of a panic attack are often so intense that panic attack sufferers believe they are experiencing a life-threatening problem like a heart attack. However, even though the symptoms can be terrifying, panic attacks are almost always harmless.
Panic attacks and panic disorder tend to run in families, and are often triggered by intense anxiety. They are more likely to happen after experiencing stressful or traumatic life events and changes, such as diagnosis of a chronic disease, divorce, or the death of a loved one.
Panic attacks often come suddenly and unexpectedly, and nobody knows exactly why they happen. We do know, however, that panic attacks are inextricably linked with anxiety, and, in at least some cases, are the result of chronic anxiety building up to a breaking point.
The most obvious symptoms of panic attacks include a rapid heartbeat, chest pain, shortness of breath, and intense fear. A panic attack is triggered in part by your body's fight or flight response and is meant to help you respond to real danger. However, when you suffer from anxiety, panic attacks can happen when there is no real threat of danger.
In people who have COPD, panic attacks can happen as a result of health anxiety caused by living with the chronic disease. Episodes of wheezing and shortness of breath caused by COPD can be terrifying, and it's easy to mistake panic attack symptoms for the symptoms of a COPD.
In fact, COPD patients are up to ten times more likely to suffer from panic attacks than people without the disease. And while panic attacks are generally harmless in the immediate term, they can interfere with the treatment and management of COPD symptoms and make your COPD worse if not properly treated.
Here are some of the most common symptoms of a panic attack:
- Rapid, pounding heartbeat
- Shortness of breath
- Dizziness or light-headedness
- Headache
- Nausea
- Sweating
- Chills
- Hot flashes
- Abdominal pain or cramping
- Trembling or shaking
- Tightness in the chest and throat
- Chest pain
- Feelings of dissociation or detachment
- Feelings of fear or terror
- Sense of impending doom
- Fear of death or of going crazy
- Numbness or tingling sensations
The Panic Feedback Loop

A panic attack can start unexpectedly at any time, and it is particularly frightening if you don't recognize it for what it is. Some people in the midst of a panic attack feel as though they are having a heart attack or like they are suffocating and can't breathe.
You might be driving down the road, making a sandwich, or lying in bed when a panic attack hits. They usually come with very little warning, and they can happen frequently or only on rare occassions.
As you can imagine, having COPD can make a panic attack even more frightening, since COPD is life-threatening disease that already makes it difficult to breathe. A panic attack can worsen COPD symptoms like wheezing and shortness of breath, causing even more panic as you struggle to breathe.
Because of this, many COPD patients who experience panic attacks assume that they are experiencing a medical emergency related to their COPD. It can be difficult to tell the difference between COPD symptoms and panic symptoms, which makes panic attacks harder to recognize.
This can cause a panic feedback loop, a downward spiral of anxiety, panic, and breathlessness that can make panic attacks more intense and more frequent. It's a difficult spiral to get out of, and the longer you are stuck in it, the harder it becomes to break free.
Here's what the panic feedback loop looks like:
- You start to feel anxious, fearful, and short of breath.
- When you notice those feelings, it causes you to become even more anxious.
- The increased anxiety triggers and even stronger fight-or-flight response, making the physical and emotional panic attack symptoms even worse.
- The worsened symptoms make you feel even more panicked and anxious, and the cycle continues.
When you're stuck in the panic feedback loop, the only way out is to seize back control over your body and mind. You can do this by using breathing techniques, mental techniques, and therapy to train yourself to respond to react to panic in more healthy, calming ways.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
How to Prevent Panic Attacks

At this point, you probably have a much better understanding of the mechanisms behind panic attacks and why they are so problematic for people with COPD. Now, you can build on that understanding by learning new skills and techniques to help you prevent panic attacks and manage them if they come.
Even though COPD symptoms like shortness of breath make panic attacks more likely and more difficult to control, you can still manage them effectively with the right knowledge and skills. If you can learn to recognize a panic attack when one hits, keep yourself calm and collected, and know what treatment options to seek, then you will find it much easier to manage your anxiety and your COPD.
Mind Over Matter
Panic attacks are self-feeding monsters, as we discussed with the panic feed-back loop. If you let fear and panic take over, it will only escalate your symptoms and make the panic attack even worse.
That's why slowing down and taking the time to get your thoughts back under control is one of the most important things you can do to stop a panic attack. It's difficult when you can hardly breathe and your mind is racing, but it's possible if you practice the following strategies:
Separate Yourself from Your Panic

When your heart is pounding and you feel paralyzed by fear, it is difficult to think clearly and rationally. To overcome the chaotic panic, you have to step back from it and find a way to ground yourself in reality.
It can help to remember that the emotions you feel during a panic attack are essentially irrational; they are unnecessary, out-of-proportion feelings triggered by an exhausted brain. When you're in the midst of a panic attack, remind yourself that you're not actually in danger, but simply experiencing a symptom of chronic anxiety.
It may feel like you're dying, or that your world is falling apart, but remember that the feeling is only temporary. Remind yourself that the panic will disappear soon, and even sooner if you can manage to calm yourself down.
Re-frame Your Panic

Instead of fighting against the panic, which can make you feel even more anxious and afraid, try to relax and let it wash over you instead. Remember that you have nothing to fear, that you are simply experiencing the symptoms of a panic attack, and accept the anxiety as an unavoidable symptom.
Although it might seem counter intuitive, struggling against the panic and telling yourself you need to calm down can actually make your panic attack worse. Instead, tell yourself that it's okay to feel anxious, and you will be able to help yourself feel less distressed.
Instead of thinking about the anxiety as a bad thing, re-frame it as something more positive and less scary. For example, you can use the panic attack as an opportunity to learn more about yourself and practice all the healthy coping mechanisms you've learned.
Positive Visualization

Positive visualization is a powerful tool that you can use to calm and redirect your mind away from anxiety and fear. It's basically a way to trick your brain into feeling more calm and letting go of distressing thoughts.
To practice positive visualization, all you have to do is picture yourself in a calm, pleasant, serene environment far away from unpleasant feelings and sensations. You might visualize yourself in a cozy, safe spot in front of a flickering fireplace, or relaxing in a warm, lush field far away from civilization and all of the stressors of modern life.
To be effective, your visualization needs to go beyond a simple image and should engage all of your five senses. Think about what it would actually feel like to be in your calming scene, including what you would hear, touch, smell, and taste if you were actually there.
Visualization can be as simple as taking a few minutes to sit quietly and reflect or as involved as a longer meditation session. For more information on positive visualization and instructions on how to start, you can use this comprehensive guide from the Calm Clinic.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Try the 5-4-3-2-1 Grounding Technique
Panic attacks can be overwhelming, filling your mind with so much fear that it's impossible to think clearly. It can make you feel like you are suffocating, going crazy, or like your life is in immediate danger.
In order to calm down, you need to pull your head out of the panic and convince yourself that you are safe. One way to do this is with the 5-4-3-2-1 grounding technique, a simple exercise you can use to reel in your fear and bring your mind back to the present.
Here's how you do it:
-
First you need to pause, take a deep breath, and look around you at your present environment.
-
Then, name five objects you can see in the space around you. It could be anything; a chair, a light switch, or a stain on the wall.
-
Next, name four things that you can feel or touch around you. For example, you might be able to feel your hair tickling your face, your clothes brushing your skin, or feel the smooth texture of your cell phone with your fingers.
-
Name three things that you can hear in your environment (not in your head). You might be able to hear a ticking clock, the whir of air through a vent, or the soft sound of your own breathing.
-
Name two things that you can smell. It could be a stale smell of dust in the air, the smell of your perfume or cologne, or the smell of an object in the room.
- Finally, name one thing you can taste, whether it's the neutral taste of your tongue, a strong fragrance in the air, or the remnants of the last thing you ate or drank.
The point of this exercise is to force your brain to focus on what's real instead of the fear inside your head. It can be even more effective if you name the things out loud so you can hear them audibly as recite them in your head.
By forcing yourself to acknowledge the present and the physical environment around you, it's easier to stay calm and grounded. It helps you to convince yourself that you are safe and in no immediate danger in the midst of irrational panic.
Distract Yourself from Your Panic

Finally, once you've reeled in your panic a bit and put things in perspective, you should try to take your mind off of the anxiety. Sometimes, simply distracting your brain from the physical and emotional sensations caused by the panic attack is enough to make the panic subside.
For example, try some simple mental exercises like counting up by multiples of three or reciting the alphabet backward. You can also try reciting a favorite poem, song, or bible passage to help keep your mind busy.
If you have the opportunity, you can also distract your brain with outside stimulation, such as listening to music or watching a video online. Anything that re-focuses your mind on something besides your anxiety can help you regain your sense of calm and control.
Tune in To Your Body

The earlier you can recognize a panic attack, the easier it is stop it. Sometimes you can even feel the signs before the panic hits, but recognizing those signs requires you to pay special attention to your body.
First, study the symptoms of panic attacks until you are confident that you can recognize them. Then, the next time you experience one, pay special attention to how your body feels and how the symptoms manifest for you personally.
Staying tuned in to your body and mind can help you recognize the first signs when something goes wrong. This is not only a way to recognize panic attacks, but also a good general habit to have to look after your mental health.
As soon as you recognize the warning signs or the symptoms of a panic attack, you can then begin to mentally fortify yourself against the panic. You can tell yourself that it is only a panic attack, and use mind-over-matter techniques to keep yourself calm.
Control Your Breathing
The most noticeable and frightening symptoms of panic attacks are the ones that make it difficult to breathe. Shortness of breath, hyperventilating, and light-headedness caused by a panic attack can cause you to panic even more, which only worsens the symptoms further and makes it more difficult to calm down.
This is especially true for people with COPD, who struggle with breathing difficulties on a daily basis. Patients who are already anxious about their life-threatening respiratory disease can easily fall into the panic feedback loop and get caught in the cycle of ever-escalating panic.
That's why one of the most effective things you can do when you're experiencing a panic attack is to get back control over your breathing. It's not always easy to do, but it's almost guaranteed to help you stay calm and make the panic pass sooner.
Rapid, frantic breathing sends panic signals to your brain, while breathing slow and steady signals your brain to calm down. One of the best ways to slow and control your breathing is with a technique called pursed-lips breathing, a common strategy recommended for managing breathlessness for people with COPD.
 |
| Image courtesy of hans van den berg on Flickr. |
ThePursed-Lips Breathing Technique:
-
Sit or stand up straight in a comfortable position. Relax your neck, shoulders, and chest.
-
Take a deep breath in through your nose lasting about two seconds.
-
Purse your lips, as if you were about to blow a kiss, and then breathe out slowly through your mouth for about two seconds (twice as long as the inhale).
- Repeat
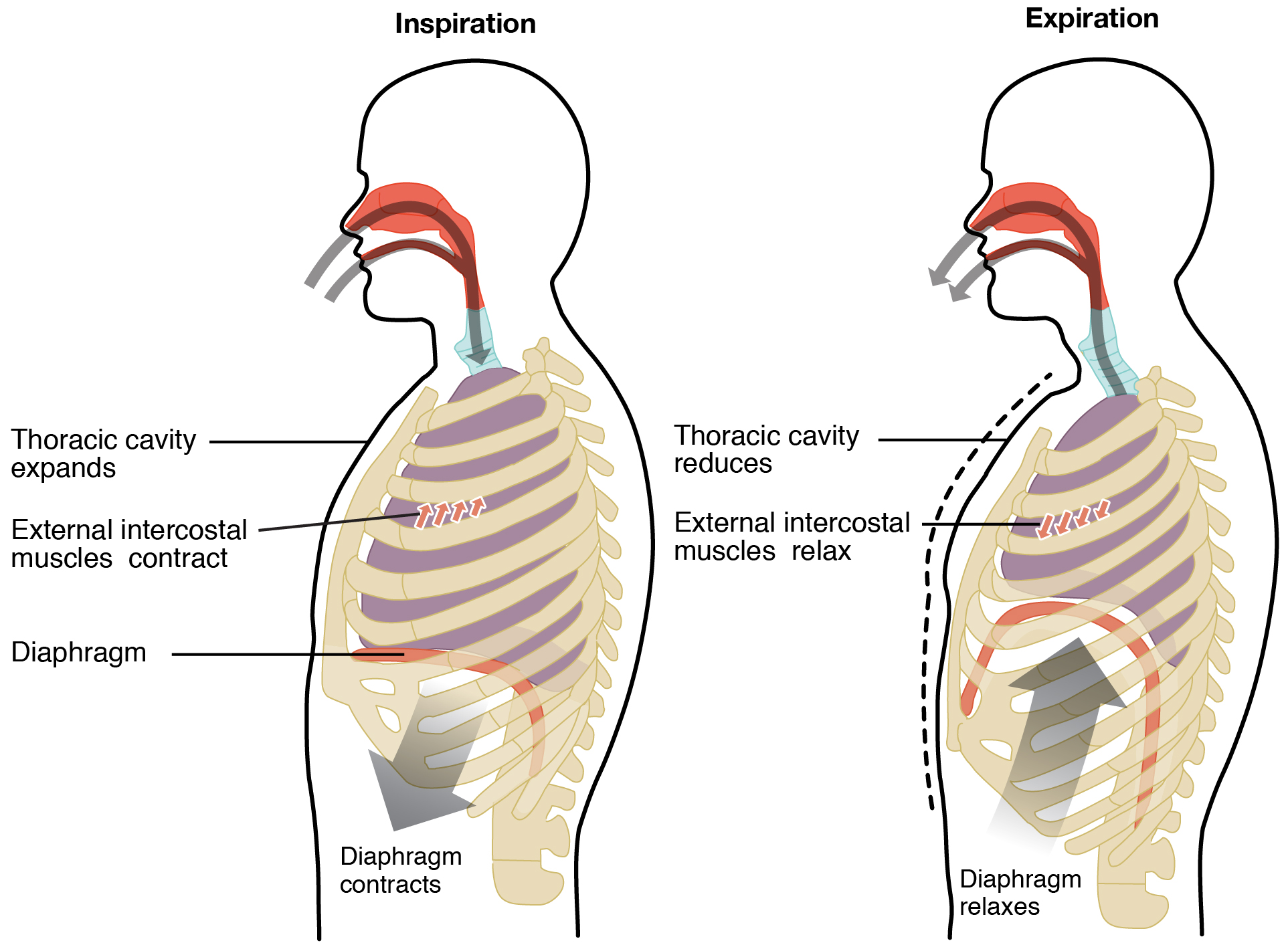
Another helpful breathing technique is diaphragmic or abdominal breathing. It helps you learn to breathe with your diaphragm, rather than your chest muscles, which allows you to breathe more deeply and evenly. This not only helps with anxiety, but can also improve COPD symptoms by allowing you to breathe with less energy and strain.

The Diaphragmatic Breathing Technique:
-
Lie down flat on your back or sit in a comfortable, upright position. Keep your neck, shoulders, and chest relaxed.
-
Place one hand on your chest and one hand on your stomach so you can feel when they rise and fall. The goal of diaphragmatic breathing is to feel your stomach, but not your chest, expand and fall as you breathe in and out.
-
Next, take a deep breath in through your nose, using your diaphragm instead of your chest muscles. You should feel the hand on your stomach rise while the hand on your chest stays still.
- Finally, breathe out slowly through your mouth. You should feel the hand on your stomach fall while the hand on your chest doesn't move at all.
- Repeat for several minutes.
Even though it is hard to think straight when you're in the midst of a panic attack, try to remember these simple, easy breathing exercises to help you stay calm. It can help to purposefully practice pursed-lips and diaphragmatic breathing when you're not anxious, that way it will be easier to remember how to do it when you feel panicked.
Do a Relaxing Activity

When you're experiencing a panic attack, it can be difficult to think about anything besides the frightening symptoms and the terror that's taken over your body. But sometimes, giving yourself a positive physical sensation or activity to focus on can take your mind away from your anxiety.
Simple, relaxing activities like reading, doodling, watching a favorite TV show, or coloring in a coloring book help give your hands and your mind something else to do besides focusing on the panic attack. You can also try activities that are tactile or give you a pleasant physical sensation, such as taking a warm shower, wrapping yourself in a soft blanket, or curling up with a hot cup of tea or hot chocolate.
Think Twice About Using Your Bronchodilator Medication
![]()
When you are having trouble breathing during a panic attack, it can be tempting to reach for your inhaler like you do when your COPD symptoms flare up. However, since the breathlessness is caused by panic, not COPD, your bronchodilator is unlikely to be much help.
In fact, bronchodilators act like stimulants and can make the panicked feeling more intense. They can end up increasing your heart rate, cause trembling and shaking, and make you feel even more anxious than you did before.
That's why it's important to learn other calming techniques to help you cope with the symptoms of panic attacks. Try using breathing techniques, meditation, or other relaxation techniques to bring your breathing back under control.
Mindfulness Meditation

Mindfulness meditation is a kind of mental exercise that helps you let go of worry and focus on the present. It's a technique that's highly regarded in the mental health field and is a common treatment recommended to people struggling with anxiety.
To practice mindfulness, you simply sit quietly for a set period of time and try to keep your mind calm and focused on the present moment. Try not to think any conscious thoughts, and let any worries or negative thoughts wash over you like water.
Mindfulness coaches often suggest focusing on your breathing and your body sensations as a way to keep your brain focused on the here and now, instead of what's going on in your head. It's a great way to learn how to stay calm when panic attacks strike and to cope with general breathing problems caused by COPD.
It's often easiest to begin practicing mindfulness meditation by following along with a written or audio-based guide. The University of California, Los Angeles has several free guided meditation audio classes you can use, or you can use the written guide at mindful.org that contains loads of useful tips and advice for getting started.
Seek Emotional Support

When you're in the midst of a panic attack, it can be extremely difficult to think straight, let alone calm yourself down. That's why it can help to call a close friend or family member for support.
It can help to tell your confidant ahead of time about your panic attacks and what they can do to help. Sometimes, just having someone there to ground you in reality and assure you that everything will be okay is enough to make a difference.
In fact, it helps to have someone you can go to for support anytime you feel anxious or depressed, even if it's not a full-blown panic attack. Having someone you can trust and talk to about your feelings is a wonderful form of therapy, and it can help you to begin healing your anxiety, which is the root cause behind most panic attacks.
Another great way to get emotional support is to join a support group for people with anxiety or people with COPD. Group therapy sessions are an opportunity to share your worries, struggles, and successes while learning from others who are facing similar har
Despite affecting more than 11 million people in the United States, many people do not understand COPD. Even people who have been diagnosed with COPD often have a poor understanding of how the disease actually works.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
COPD is a relatively complex condition and it affects different people in different ways. Not everyone experiences the same symptoms, which can be confusing for patients and lead to misconceptions about the disease.
Unfortunately, myths and misconceptions about COPD can be dangerous and misdirecting. They lead to false ideas about what causes COPD and how severe the condition is, and may even discourage people with the disease from seeking treatment or listening to their doctor.
If you or someone you love has COPD, then it's vitally important to have an accurate understanding of the disease and how to treat it. Without accurate information, you may not be able to make the healthy choices and lifestyle changes that are necessary for you to manage your COPD and live a good quality of life.
In this article, we're going to take a look at some of the most common myths and misconceptions that people have about COPD. Chances are you've heard a few of these inaccurate claims before, and now it's time to set the record straight.
Common Myths and Misconceptions About COPD
Myth: COPD is a Rare Disease

According to the World Health Organization, more than 65 million people worldwide suffer from moderate or severe COPD, and that number is steadily increasing every year. But because the disease mostly affects older adults and seniors, it doesn't get the same attention as other, more visible diseases.
However, researchers estimate that up to two-thirds of COPD cases are not diagnosed, meaning that tens of millions of people have COPD and don't even know it. That's because COPD symptoms can be very mild and difficult to recognize in the early stages, and many people assume they are just normal signs of aging.
However, symptoms like frequent breathlessness and fatigue during activity are not normal aging symptoms, and are often the result of early-stage COPD. But due to misinformation and lack of awareness about the disease, many of these people go without treatment until their condition declines.
What's more, the symptoms of COPD are not always obvious to others, so many people may not realize that a friend, family member, or coworker is suffering from the disease. Because of this, many people underestimate how common it is and assume COPD is a rare disease.
Myth: COPD is Just Like Asthma

While both COPD and asthma are breathing disorders, they are very different diseases. COPD happens as a result of lung damage that accumulates over time, while asthma often occurs in otherwise healthy lungs that are extremely sensitive to irritants in the air.
Asthma can be present from birth or show up later in life as a result of exposure to respiratory irritants. It can cause episodes of wheezing and shortness of breath, often known as asthma attacks, but lung function usually returns to normal after the attack subsides.
On the other hand, COPD is a disease that usually comes later in life as a result of long-term damage to your lungs. People with COPD have permanently reduced lung function and also experience episodes of breathlessness and wheezing, known as COPD flare-ups and exacerbations.
Interestingly, COPD and asthma are somewhat connected in the sense that having asthma may put you at a greater risk of developing COPD later in life. However, COPD and asthma are distinctly separate conditions, even if some of their symptoms are similar.
Myth: COPD is Just a Breathing Disorder
While shortness of breath and difficulty breathing are the main and most common symptoms of COPD, they are definitely not the only ones. COPD can cause a variety of different symptoms including a chronic cough, wheezing, frequent respiratory infections, fatigue, depression, and more.
Although COPD primarily affects the lungs, it affects many other parts of the body as well. For example, your lungs are inextricably connected to your heart and cardiovascular system; because of this, COPD can lead to a variety of heart complications including cardiovascular disease and stroke.
COPD is also an inflammatory disease, and people with COPD show signs of elevated inflammation in their lungs, blood vessels, and elsewhere in their bodies. This alone can increases COPD patients' risk for a variety of other conditions including lung cancer and heart disease.
Myth: You Can Only Get COPD from Smoking

Although most people think of COPD as a smoking-related disease, it is not always caused by smoking. COPD is a condition that results from irreversible damage to the lungs, which can be caused by many different things, including air pollution, toxic gases, and certain health conditions.
Many people who develop COPD from non-smoking causes get it from exposure to chemicals in their workplace. For instance, people who work in manufacturing and construction can develop COPD from exposure to airborne toxins, dust, and other particulates in the air.
You can also get COPD outside the workplace from long-term exposure to things like cleaning chemicals, indoor and outdoor air pollution, and toxic gases. For example, Radon, a colorless, odorless gas known as the largest environmental cause of deadly cancers in United States, can also cause COPD.
COPD can also be caused by other medical conditions like asthma, alpha-1 antitrypsin deficiency, and frequent respiratory infections during childhood. There are many different things that can damage your lungs throughout your life and eventually cause COPD, not just smoking as many people believe.
However, smoking is still by far the most common cause of COPD, accounting for approximately 90 percent of COPD cases. That means avoiding tobacco and quitting smoking are still the most important things you can do to protect yourself from COPD.
Myth: Only Very Old People Ever Get COPD
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Most people develop COPD in their 50's and 60's after a lifetime of exposure to smoke or other substances that are toxic to their lungs. However, it is certainly possible to develop COPD earlier, and many people do.
In fact, although it's rare, some people are diagnosed with COPD before they even turn 40. You are much more likely to develop COPD at a young age if you have another condition like asthma or Alpha-1 antitrypsin deficiency.
Myth: Only Men Usually Get COPD

In the early 1900's, COPD was considered a “man's disease,” mostly because men were more likely to smoke tobacco. However, the number of women smokers skyrocketed in the 50's, leading to a huge increase in women diagnosed with COPD in more recent years.
Studies also show that women may be more sensitive to the irritating effects of smoke and other airborne contaminates. Because they tend to have smaller lungs, women tend to get a larger “dose” of these harmful irritants, making their lungs more susceptible to damage.
However, that doesn't mean that COPD is a “women's disease” either; COPD is still one of the leading causes of death for both men and women in the United States. While your genetics do play a role in how susceptible you are to the disease, every person still has the potential to develop COPD from long-term exposure to smoke and other respiratory irritants.
Myth: If You Stop Smoking, COPD Will Go Away
Some people mistakenly believe that once you quit smoking, the symptoms of COPD will go away. While quitting smoking can reduce some of your symptoms, it cannot reverse the damage to your lungs that has already been done.
Unfortunately, there is no known cure for COPD; it is a chronic, life-long disease. Once you have COPD you are stuck with it, and the best thing you can do is seek treatment and try to prevent it from getting worse.
Although this is a heartbreaking reality to accept, understanding the severity of the disease is important for taking your lung health seriously. In order to prevent further damage to your lungs and maintain a good quality of living, you need to diligently follow your COPD treatment plan for the rest of your life.
The good news is that by following an effective treatment plan and taking an active role in managing your disease, you can minimize your symptoms and live an active life for many years to come. However, it takes a lot of hard work and dedication to living a healthy lifestyle every day.
Myth: COPD is Not Treatable

On the opposite end of the spectrum there is the misconception that COPD cannot be treated at all. And, while it's true that there is no real cure for COPD, there are many medications, treatments, and lifestyle changes that can significantly reduce COPD symptoms.
In fact, early detection and treatment for COPD is vital for maintaining your health and quality of life. The sooner you get diagnosed, the sooner you can begin treatment and prevent further damage to your lungs.
Every person who is diagnosed with COPD should receive a detailed health assessment and a personalized treatment plan from their doctor. The standard course of treatment includes using inhalers, steroids, antibiotics, lifestyle changes, and sometimes supplemental oxygen to manage respiratory symptoms and infections.
An effective COPD treatment plan will help you keep your symptoms under control and can even slow down the disease's progression. You can breathe easier, be more active, and live a better quality of life when you work with your doctor to effectively manage your symptoms.
Myth: There's No Point in Quitting Smoking if You Already Have COPD

Even though quitting smoking will not cure your COPD, it can help protect your lungs from further decline. If you have COPD, you should try to stop smoking immediately to prevent the disease from rapidly getting worse.
It's never too late to quit smoking, and it has the potential to significantly improve your quality of life. It can also help reduce COPD symptoms like coughing and wheezing and lower your risk for life-threatening respiratory infections and exacerbations.
Research shows that people with COPD who quit smoking have fewer COPD flare-ups and are less likely to be admitted into a hospital for their symptoms. It also reduces your chance of dying from COPD.
What's more, quitting can improve your health in other ways that are unrelated to COPD. It can improve your exercise endurance, your cardiovascular health, and reduce your risk for other smoking-related diseases like lung cancer, heart disease, and stroke.
It's important to understand that, if you continue to smoke after your COPD diagnosis, then you are aggravating your disease and gambling with your life. Smoking can even make certain COPD treatments (such as corticosteroid medications) less effective, which puts your lungs and your health at even greater risk.
Myth: It Doesn't Matter if You are Overweight and Have COPD
Being overweight puts extra strain on your body, including your heart and lungs. It also puts extra weight on your chest when you lie down, which can make it much more difficult to breathe if you have COPD.
Maintaining a healthy BMI is important for keeping all of your organs healthy, including your heart and lungs. Studies show that being obese can also increase inflammation in your body, which can make COPD-related inflammation in your lungs and other organs even worse.
Obesity also increases your chance of developing other chronic conditions that can worsen COPD, including heart disease, diabetes, and obstructive sleep apnea. It also makes it more difficult to exercise and stay active, which is vital for keeping your lungs and body healthy when you have COPD.
Myth: Your Diet Doesn't Affect Your COPD

What you eat is directly related to your overall health, and this is especially true for people with COPD. Eating the right foods and maintaining a healthy weight can boost your energy levels and make it easier to breathe.
In fact, because they have to use more energy to breathe, people with COPD often need more calories and nutrients per day to meet their body's needs. On the other hand, eating too much can lead to being overweight or obese, which makes it both harder to exercise and harder to breathe.
The most important thing to do for a healthy, balanced diet is to eat meals full of vitamin-rich fruits and vegetables, whole grains, healthy fats, and lean proteins. However, you should limit the amount of carbohydrates you eat, because studies show that breaking down carbohydrates can actually put extra strain on your lungs.
People with COPD are particularly prone to malnutrition and fatigue, both of which can be combated with a healthy diet. Eating right will give you the energy you need to stay active and supply your lungs with the fuel they need to operate efficiently.
To learn more about how your diet affects your COPD, check out our previous post on healthy foods for COPD patients. You can also get some more useful diet tips from our article on foods to avoid if you have COPD.
Myth: Exercising is Dangerous if You Have COPD
People with COPD often experience symptoms like coughing and shortness of breath when they exercise. This leads some to believe that exercise is dangerous and that they should avoid physical activity.
In reality, though, exercise is one of the best things you can do to improve your health and quality of life if you have COPD. All good COPD treatment plans include regular exercise, and staying active can help prevent your COPD from getting worse.
While you shouldn't exert yourself too much and you should always give yourself time to rest when you feel extremely short of breath, exercise is safe and healthy for the vast majority of COPD patients. It can strengthen your heart, breathing muscles, and skeletal muscles, and reduce your chances of developing other age-related and COPD-related diseases.
If you are worried about exercising, talk to your doctor to see what kinds of activities are safe and effective for you to do. Your doctor can also help you better manage your symptoms, which can help you breathe better when you exercise.
There are even special exercise programs—known as pulmonary rehabilitation classes—that are developed specifically to help people with COPD learn how to exercise while keeping their breathing and other COPD symptoms under control. If you struggle with exercise and staying active because of your disease, talk to your doctor about enrolling in a pulmonary rehabilitation class.
Myth: You Cannot Have a Satisfying Sex Life with COPD

Many people believe that because COPD makes breathing and exercising more difficult, it will inevitably hurt their sex life as well. However, while it may make certain sexual activities a little more difficult, you can still have a healthy and fulfilling sex life with COPD.
Even if you struggle with shortness of breath, you can keep your symptoms under control with diet, exercise, medications, and other COPD treatments. You may even be able to attend a pulmonary rehabilitation class if you have significant trouble breathing during physical activity.
Also, it's important to remember that there are countless ways to experience sex and intimacy, and it's normal for your sex life to change as you age. That doesn't mean that it has to be any less exciting or satisfying than it was before; it just means you might have to be more flexible or willing to try new positions that are more comfortable with COPD.
Myth: Once You Start Oxygen Therapy, There is No Going Back

May COPD patients are afraid to start supplemental oxygen therapy because they fear that once they start, they will be tethered to their oxygen machine for life. While it is true that some COPD patients have to use Oxygen 24/7, this is not the case for most patients.
You might need to use oxygen occasionally as a supplement to other COPD treatments, or you may only need it for a short period of time while you are recovering from an exacerbation. You can also use supplemental oxygen to help you breathe when you exercise and reduce shortness of breath throughout the day.
Most patients start out using supplemental oxygen less frequently, and slowly increase their oxygen use as their disease progresses. For many patients, this starts with using oxygen during physical activities or at night to make it easier to breathe during sleep.
While some people see supplemental oxygen as a limitation, in reality, it can actually enable you to do more and improve your quality of life. Supplemental oxygen helps you breathe better, sleep better, have more energy, and can reduce your risk of serious COPD complications like heart disease and pulmonary hypertension.
Myth: You Cannot Live a Healthy, Fulfilling Life with COPD

While COPD is a serious disease, it is not a death sentence or an end to your life as you know it. You can still live a healthy, happy, and active life even if you have COPD.
You may have to make some serious lifestyle changes to protect your lungs and treat your disease, but that doesn't mean you can't live a normal life. In fact, if you follow your treatment plan carefully, including eating a healthy diet and exercising, you may even find that you have more energy and feel better than before you were diagnosed.
The more you care for your health and adhere to your COPD treatments, the amore likely you are to maintain the lung function you still have for longer. While COPD inevitably gets worse over time, you can live comfortably with the disease for many years and continue to do all of the things you enjoy.
Conclusion
If you have COPD, then you know that your lungs are particularly sensitive to the environment and the quality of the air you breathe. Even minor irritants like dust, smog, or cold air can worsen your symptoms and make it even more difficult to breathe.
The cold weather and harsh, dry air is irritating to anyone's respiratory system, but it can cause debilitating symptoms for people with weakened and sensitive lungs. That's why the winter months tend to be particularly challenging for people with COPD.
Cold weather and COPD has been a topic of interest to researchers for some time, and many studies have proven that winter weather can significantly worsen COPD symptoms. In fact, studies show a very strong link between extended periods of cold weather and increased hospitalizations for people with COPD.
Because of this, doctors and health organizations like the Lung Institute urge people with COPD and other respiratory conditions to be especially cautious in cold weather. It's important to protect yourself and prepare yourself for the winter to prevent dangerous and even deadly COPD exacerbations.
If you're heading into the winter months and want to know how the weather will affect your COPD, then this article is for you. In the following sections, we'll help you understand why cold weather tends to make COPD worse and give you a variety of tips to help you better manage your disease this winter.
How Cold Weather Affects Your Respiratory System

Although most people have experienced coughing or inflamed airways in cold weather, it's easy to underestimate how severely the cold air can affect your respiratory tract. According to the Lung Institute, cold air can have an “extreme” effect on your lungs and “cause dramatic changes to the respiratory system.”
One of the most immediately noticeable changes is narrowed airways that restrict airflow and make it difficult to breathe. This can be dangerous for people with severe COPD and trigger bouts of serious breathlessness, coughing, and wheezing.
Another way cold weather affects your body is by triggering a sudden increase in breathing rate followed by a sudden drop in breathing rate when you get cold. This effect is a major cause of cold-related deaths in the elderly and can happen even when the weather is only mildly cold, in temperatures as high as forty degrees Fahrenheit.
Another effect of cold weather is an increase in blood pressure, which is hard on your heart and lungs. This happens when extremely cold air causes your blood vessels to narrow, which forces your heart to work harder to circulate blood and oxygen throughout your body.

In most healthy people, these changes only cause minor symptoms and discomfort. But for people with COPD and other serious conditions, these respiratory changes that happen in response to cold air can cause serious problems and even be life-threatening.
However, it's not just the temperature that causes increased respiratory strain in the winter. Cold air also happens to be drier than warm air because it can't hold as much moisture. This can cause humidity to drop far below the ideal level.
Dry air is generally more difficult to breathe, especially for people with COPD and other respiratory conditions that make their airways sensitive to irritation. Cold air dries out and irritates your airways, causing airway constriction and inflammation that makes it difficult to breathe.
Cold, dry air also tends to increase mucus production, which can worsen coughing and breathlessness in people with COPD. The density of the air also plays a role; cold air is denser than warm air, which means cold air creates more resistance in your airways and makes it harder to breathe.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Other Winter Hazards

Another major problem many COPD patients have during the winter is getting enough physical activity. Having to stay indoors can disrupt your usual exercise routine and make it easy to get out of the habit of being active.
The wintertime is also the peak season for colds, the flu, and other contagious illnesses. Cold weather is also a friendly environment for bacteria that cause respiratory infections and exacerbations.
Since most COPD exacerbations are caused by contagious illnesses and infections, it's particularly important for people with the disease to avoid getting sick. Combined with all the other complications that cold air can cause, contracting any kind of respiratory illness puts you at an extremely elevated risk for serious and even life-threatening exacerbations.
But even though the wintertime can be dangerous for people with COPD, there are plenty of things you can do to protect yourself and your lungs from the hazards of the cold air. There's no reason to worry if you prepare and take the right precautions.
In the next sections we'll show you all the steps you can take this winter season to stay healthy and keep your COPD symptoms under control. Continue reading for a plethora of practical tips and advice for staying warm, breathing easier, and avoiding worsened symptoms and exacerbations this year.
How to Protect Yourself from Cold Weather
Breathing Techniques for Cold Weather

If you have COPD, you've probably noticed that it's harder to control your breathing when the weather is cold. All it takes is a sudden breath of cold air to shock your respiratory system and cause you to lose your breath.
This makes it more difficult for people with COPD to breathe normally and catch their breath in the cold winter air. However, if you practice proper breathing techniques you can reduce the shock of the cold air on your lungs and get your breathlessness under control.
The pursed lips breathing technique is recommended for any situation when you find it difficult to breathe, but it can be particularly helpful in the cold. The technique is simple: make sure you breathe in through your nose for a couple of seconds count, and then exhale slowly for twice as many seconds while pursing your lips together (as if you were blowing a kiss).
Breathing in through your nose protects your lungs because it gives the cold air time to warm up slightly and absorb moisture it as it travels through your nasal passages. If you breathe in through your mouth, the cold, dry air goes straight to your lungs and causes much more irritation.
It's a good idea to practice the pursed lips breathing technique at home when you have full control of your breathing and your symptoms aren't acting up. That way it will feel more natural when you use it in a breathing crisis, and it will be easier to get your breathing back under control.
There are a variety of other breathing techniques you can use to control your breathing whenever cold air or anything else triggers a bout of breathlessness or coughing. Visit The Lung Institute here to learn more about effective breathing exercises and techniques.
Cover Up Your Nose and Mouth

If you have to be out in the cold, there are a couple of things you can do to make the air you breathe less harsh. In addition to wearing warm clothes and a coat, you can also wrap a scarf around your nose and mouth.
This warms up the air before it reaches your nostrils and is a great way to protect your lungs and make the harsh air easier to breathe. Wearing a scarf over your face also traps the moisture from your breath, which helps humidify the air slightly before you breathe it in.
Another option is to get a cold-weather mask, like a CT Mask, designed for people with respiratory illnesses like COPD. Like a scarf, CT masks trap the warmth and moisture from your breath when you exhale in order to warm and humidify the next breath of air you breathe in.
CT masks are reusable, washable, and made from soft, flexible materials for comfort. Although more pricey than a scarf, CT masks are often more comfortable, more effective, and more convenient for keeping your lungs warm when you go outside.
Cover Your Oxygen Tank and Tubing
If you use supplemental oxygen, you have to consider how to keep your oxygen warm when you go out and about in the winter. If the air in your oxygen tank or the tubing gets too cold it can be uncomfortable and difficult to breathe.
If you take your oxygen supply with you out in the cold weather, make sure to insulate the tank and tubing from the cold air. You can do this by keeping your portable oxygen tank in an insulated bag or case that protects it from the cold air and elements.
Another option—better for shorter jaunts—is to hold the tank under your coat so your body heat keeps it warm. Whatever you do, you should always try to keep your tubing secured under your coat or jacket so it doesn't cool down the oxygen coming from your tank.
Avoid Sick People and Crowded Places

When you have COPD, you are particularly susceptible to respiratory illnesses and even minor infections can be devastating to your health. That means you have to be especially careful to avoid germs and stay away from people who are sick.
It's best to avoid extremely crowded places and events during the winter when colds, the flu, and other respiratory illnesses are at their peak. When you do go to public places, make sure to wash your hands often and use hand sanitizer when needed.
Avoid touching your nose, mouth, or any part of your face when you're out in public unless you wash your hands first. That way you don't infect yourself with germs picked up from all the surfaces you've touched.
Keep Your Medications Handy

When the weather is cold and the air is dry, you're likely to experience more severe symptoms than usual. That means you will probably need to use your inhaler and other medications more often during the winter months.
You should always bring your inhaler, supplemental oxygen (if you use it), and any prescribed quick-relief medications with you, especially if you will be spending any amount of time outdoors. That way you'll have everything you need to get your symptoms back under control if the cold air starts to bother you.
You might even find that your usual prescription medications and therapies aren't enough to control your symptoms during long periods of cold weather. If this is the case, you should talk to your doctor right away so he can adjust your prescriptions or treatment plan to better manage your symptoms.
Watch Air Quality Forecasts

Extreme temperatures, both hot and cold, tend to worsen air quality. Because of this, air pollution is a major culprit behind increased COPD symptoms in the winter.
This is partly because people tend to generate more pollution in the winter by using fireplaces, wood-burning stoves, and leaving their cars running idle. But another cause of poor winter air quality is the cold air itself, which tends to trap smog and other particulates close to the ground instead of letting them disperse into the atmosphere.
If you have COPD, you should always avoid spending time outdoors when the air quality is poor, no matter the time of year. You can check your local air quality forecast daily at airnow.gov and plan your outings and activities for days when the air quality is good.
If you don't already know how, it's important to learn how to interpret air quality warnings and how they apply to COPD. For example, “moderate” quality air is considered acceptable for healthy individuals to breathe but can be harmful to people with COPD, especially in the latter stages of the disease.
Don't Neglect Indoor Air Quality

While it's a good idea to stay indoors on days when the outdoor air quality is poor, it won't do you much good if your indoor air is polluted, too. Many people don't realize that indoor allergens and pollutants can actually get worse in the winter and exacerbate your COPD symptoms.
For example, many appliances utilize combustion and can emit harmful fumes into your home. Many of these, including fireplaces, stoves, water heaters, and dryers, tend to be used more often in the winter months, too. It's important to make sure all of your appliances are well-ventilated and working properly to minimize the amount of pollution they leak into your home.
The winter months also coincide with holidays like Halloween and Christmas, which usually means digging for seasonal clothes and decorations. This often involves moving old boxes in your attic or basement and digging in the back of your closets. Unfortunately, moving around items in storage tends to unleash dust and other allergens from their resting place, which can hurt your indoor air quality and make COPD symptoms worse.
Since there are fewer opportunities to open the windows and air out your house in the winter, it's important to be especially vigilant about cleaning up dust, removing mold, and changing the air filters in your house's ventilation system. These are simple steps, but they can make a huge difference in the air quality in your home and how you feel.
Extra Tips for Staying Warm in the Cold

If you have COPD, keeping out of the cold should be a top priority in the winter. However, you can't always stay indoors, so you should be prepared to bundle up and protect yourself from the cold weather when it can't be avoided.
Dressing for the cold weather might seem like a no-brainer, but it's something you should really think about if you have COPD. The disease makes your body particularly susceptible to dangerous cold-weather reactions like increased blood pressure and irregular breathing. This is why it's so very important to keep your body warm
If you do have to go out on cold days, you should always take extra time to make sure you have everything you need to stay warm. You should check the temperature forecast daily and make sure to take wind chill, precipitation, and other weather conditions into consideration.
You should also never forget to bring your inhaler or rescue medications with you in case your symptoms get much worse in the cold. Here are some more general tips and techniques you can use stay warm and protect your lungs this winter:
-
Dress in layers so you can always adjust to different temperatures. You can simply add an extra jacket or sweater if you get cold, and if you get too hot later, all you have to do is remove a layer.
-
Wear long-sleeved undershirts, long underwear, or leggings for an extra under-layer in extremely cold weather.
-
Don't forget about other pieces of important winter outerwear like scarves, hats, and gloves. It's also a good idea to keep an extra set of gloves in your car or handbag in case you forget when you leave the house.
-
Always check your local weather forecast and plan around harsh weather and temperatures. Make sure to take humidity, air pollution, and wind chill into consideration too.
-
Always cover and insulate your oxygen tank and tubing in cold weather.
- Consider wearing a CT mask or other cold weather mask to warm up the air as you breathe.
Stay Hydrated

Cold, dry air tends to irritate your airways and thicken the mucus in your lungs. Both of these things lead to increased coughing and breathlessness, especially for people with COPD.
One of the ways to combat this is to drink extra water during the winter. Dehydration thickens mucus and makes COPD symptoms worse, while proper hydration keeps your airways moist and your mucus thin. This it much less likely that phlegm will obstruct your breathing or trigger a coughing fit, and makes it much easier to get mucus out with controlled coughing techniques.
You should always drink at least 6-8 glasses of water per day to stay hydrated, possibly more if you exercise. If you tend to forget, it helps to keep a couple of re-usable water bottles filled in places around your house. Keep a filled bottle in key, noticeable places like your fridge, living room, and nightstand for convenience.
Staying Active During the Winter
One indirect yet dangerous effect of cold weather on COPD is that it makes it more difficult to get enough physical activity. It's not just because the cold air makes breathing during exercise more difficult, but also because it often means staying indoors and giving up outdoor activities that help you stay active.
However, if you have COPD then you know that exercising is one of the healthiest, most important things you can do to treat your disease. It can improve your lung function, strengthen your breathing muscles, reduce COPD symptoms like coughing and breathlessness, and even slow down the progression of your disease.
Because of this, most doctors recommend getting as much exercise as you can, and that includes during the winter months. Even though the cold weather makes physical activity more difficult, it's still just as important for your health to find ways to stay active.
In this next section, we're going to help you out by showing you a variety of convenient ways you can stay active this winter. We'll and show you a variety of indoor activities and exercises you can do to avoid the cold weather and give you tips for handling the cold air when you can't avoid it.
Join a Gym

The gym is an obvious option for getting physical activity during the winter. Even if you don't go to a gym any other time of the year, it might be your best option when the weather is too cold to exercise outside.
Nearly all gyms have treadmills, exercise bicycles, stair steppers, and other machines for light to moderate aerobic activities. Some even have indoor tracks for a more natural walking or jogging experience.
Gyms also give you access to a variety of weights and strength training machines that you can use to build muscle more easily. Weight machines are often easier for less experienced people and those with limited mobility to use.
Gyms also have employees on hand that can teach you how to use the equipment and help you with any questions you have. Some gyms even host group exercise classes you can join, although you often have to pay an extra fee.
Find Alternative Places to Walk

Many people with COPD use walking as a primary source of exercise. It's a popular way for people with respiratory illnesses to stay active and is often recommended by doctors for being low-impact, effective, and less likely than many other exercises to make you feel out of breath.
Unfortunately, the cold winter weather makes it unpleasant, and even dangerous, to exercise outside if you have COPD. If you usually like to stroll around your neighborhood or an outdoor park, you'll have to find another way to get that exercise indoors, instead.
One of the most obvious and popular options for indoor walking is to join a gym. However, treadmills, indoor tracks, and monthly membership fees aren't for everyone. As an alternative, you can look for large, public buildings that have plenty of room to walk around.
Walking laps around an indoor shopping mall, for example, is a great option for exercising when it's too cold to walk outside. There are plenty of long, flat hallways to stroll down and plenty of interesting things and people to look at to stave off boredome.
You can also bring along a friend or two to make your indoor walks more fun. Some malls even have community walking groups or stay open after-hours to promote public walking indoors.
Other places that often have enough floor-space for walking include large community centers, department stores, and warehouse stores like Ikea. These places are generally open to the public most of the day and have plenty of space for walking laps.
When all else fails, you can get in your daily steps in by walking around your own home, instead. If you have enough space, you can do laps through the halls and climb up and down stairs for exercise. You can also walk or jog in place while listening to music or watching your favorite TV show.
Invest in a Pedometer

If you're used to walking outdoors during the warmer months, you probably measured your progress based on the distance of your walking route. But when you're forced to change your routine in the winter and move your walking indoors, it can be much more difficult to estimate how much exercise you got.
That's why you should consider getting a pedometer to help you keep track of how much walking you do this winter. That way, if you walk laps around your home, local mall, or another indoor place you can always know exactly how far and how many steps you walk. It's a great way to track your steps if you walk in place, too.
But pedometers aren't just for tracking your steps; they're a fantastic tool for motivation, too. Using a pedometer to track your progress helps you set goals, celebrate improvements, and challenge yourself to get in as many steps as you can every day.
Try At-Home Strength Training Exercises

Strength training is very important for people with COPD because it helps you build muscle and exercise endurance. In fact, many COPD patients who have trouble exercising say that muscle weakness and soreness holds them back even more than breathing difficulties do.
If the winter weather is disrupting your exercise routine or making it difficult to go to the gym, there are plenty of options for exercising at home. You don't even need weights or special equipment in order to tone and build strength, although a small set of light free-weights can make it easier build muscle and open up even more options and exercise techniques.
Many exercises you can do in your home are simple and take minimal equipment. All you have to do is clear out a space large enough to move around in and you can begin practicing a variety of strength training exercises right away.
To learn more, visit our previous article on how to effectively exercise at home here. It will teach you about a variety of different strength training exercises and other physical activities you can do without ever having to set foot outside.
Get Into Stretching

As a respiratory disease, COPD comes with many symptoms, but the most serious and uncomfortable of these symptoms is difficulty breathing. These breathing problems have a variety of interconnected causes, including airway obstruction, reduced lung function, and a reduced capacity for exercise that are all caused by COPD.
In fact, almost every COPD treatment is, ultimately, aimed at managing your breathing. Bronchodilator medications, supplemental oxygen, and even diet and exercise regimens are all meant to help relieve airway obstruction and help you breathe as efficiently as possible.
But there's another type of COPD treatment that is invaluable for managing COPD symptoms and keeping your breathing under control: practicing breathing exercises. You've probably heard about breathing exercises from your doctor, but you might not yet understand how handy and effective they can be.
Breathing exercises are perhaps the most convenient and useful techniques that any COPD patient could add to their toolbox. They're absolutely safe, surprisingly effective, simple enough for anyone to learn quickly, and one hundred percent cost-free.
In this article, we're going to teach you about all of the breathing techniques that doctors and researchers recommend for people with COPD. We'll not only introduce you to the most effective breathing exercises and teach you how to practice them but also help you understand how they work and what the best times are to use them.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Breathing Exercises for COPD

One thing that makes breathing exercises such a valuable treatment option is the fact that you can use them anytime and anywhere as long as you remember the steps. So, if you'd like to add some new techniques to your COPD treatment tool set, continue reading to learn how to use several different breathing exercises to help you breathe easier and better manage your COPD symptoms.
The Stop, Reset, and Continue Technique

When you have trouble breathing it can be a very scary experience. However, if you let yourself become too anxious or distracted by worry, it will make it even harder for you to catch your breath.
Once breathlessness starts, it can easily cascade out of control, becoming worse and worse if you don't manage it quickly. That's when you need to stake a step back, pause, and regroup so that you can begin using proven strategies to get your breathing back under control.
Simply worrying about feeling breathless can even trigger a bout of breathlessness or hyperventilation on its own, especially if you suffer from chronic anxiety or panic disorder. Whatever the cause of your breathlessness, it's important to keep a level head whenever the symptom strikes.
That's why the "stop, reset, continue" technique is such a valuable tool for any person who has COPD. It helps you stay calm, re-focus, and then begin steadying your breathing until it returns to normal.
Here is how you practice the stop, reset, and continue technique:
-
Stop whatever activity you are doing and sit or lie down whenever you start to feel short of breath.
-
Reset your breathing by relaxing the muscles in your shoulders and chest and practicing a breathing exercise (such as pursed lips breathing, which we'll discuss in the next section below) until you are able to catch your breath.
- Continue whatever activity you were doing before, at a slower pace if necessary, while continuing to consciously control your breathing.

You can use this technique if you get breathless from physical activities like walking, exercising, or doing chores around the house. It can also work when you feel short of breath for other reasons, such as when you experience an exacerbation or when your symptoms flare up because of exposure to allergens, pollution, temperature extremes, and other respiratory irritants.
The "stop, reset, continue" method works because it keeps you in clear-headed command of your thoughts and your breathing. It helps cut through anxiety, reminds you not to panic, and allows you to concentrate on practicing breathing exercises and other treatments that can help you recover.
This may seem like a simple technique, but it can be surprisingly effective in the moment. The next time you have trouble catching your breath, just repeat the simple steps "stop, reset, and continue" to remind yourself that you have the ability to bring your breathing back under control.
As you do your breathing exercises, you might need to remind yourself to stop, reset, and continue multiple times as you lose control or focus. Reset as many times as you need until your get your symptoms under control.
When you feel short of breath, you should also use your quick-relief medications--such as your bronchodilator, supplemental oxygen, or inhaled corticosteroids--as directed by your doctor. Using these in combination with breathing exercises can be more effective than just practicing breathing exercises alone.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Pursed Lips Breathing
Pursed lips breathing is the number one, staple breathing technique that everyone with COPD should know how to use. It's probably the most simple, effective, and versatile method for preventing and treating breathlessness caused by COPD.
If you don't have this method memorized yet, then now is the time to learn it by heart. Once you have the basic steps down, you can use pursed lips breathing to aid you in a multitude of situations and circumstances.
That's because pursed lips breathing isn't just something you use when you feel breathless to get your breathing back under control. It's also a technique for preventing breathlessness when you exert yourself and helping you breathe easier in any situation.
Research shows that using pursed lips breathing helps open up your airways, reduces airflow resistance, and uses less effort and energy to breathe. It also makes your breaths easier to control when you exercise or when you experience a flare-up that makes your symptoms worse, which can prevent breathlessness from ever occurring in the first place.
One study showed that COPD patients who practiced pursed-lips breathing while exercising had increased exercise endurance and were able to take in more oxygen as they worked out. Pursed-lips breathing also helped steady patients' breathing rates, reduced rapid breathing, and even increased the levels of oxygen in their blood.
Pursed lips breathing can be particularly helpful for people with emphysema, who often have trapped air in their lungs that makes it difficult to breathe. Pursed lips breathing helps push the trapped air out, allowing you to take deeper breaths and absorb more oxygen every time you inhale.
How to Practice Pursed Lips Breathing
Pursed lips breathing is simple to learn and easy to do, but that doesn't mean you don't need to practice. You should take the time to practice pursed lips breathing every day until it becomes second nature. To do that, you need to concentrate on the steps and the process, not just go through the motions.
Here is how you perform the pursed lips breathing technique:
-
Lie down or sit upright in a chair and relax the muscles in your shoulders and chest.
-
Take a slow, deep breath in through your nose (not your mouth) for two seconds. You can repeat the words in your head, "Inhale, one, two" to help you keep rhythm if you like.
-
Next, purse your lips as if you were about to whistle or blow out a candle.
-
Then, breathe out slowly and steadily for a count of four (twice as long as your inhale) through your pursed lips. You can repeat the words "Exhale, one, two, three, four," in your head to help you keep pace.
- Repeat.
The are a couple of key things to remember while practicing pursed-lips breathing: First, inhale only through your nose and exhale only through your mouth. Second, make sure to exhale for about twice amount of time that you spent inhaling.
You can use the pursed lips breathing technique any time you like, and it can even help you breathe easier when you're not experiencing any acute COPD symptoms. However, pursed lips breathing is especially effective to use when you exercise or exert yourself in any way.
For example, you can use pursed lips breathing when you climb stairs, do housework, or get up from a chair to keep your breathing even and steady. This can prevent fits of coughing and breathlessness, help you increase your endurance and tolerance for physical activities, and live a more comfortable, active life.
If you would like to see a visual demonstration of how to practice pursed lips breathing, check out this video from National Jewish Health.
Coordinated Breathing
Coordinated breathing is a technique for keeping your breathing controlled and steady when you exercise or do any other kind of physical activity. It makes it easier to breathe, reduces shortness of breath, and helps you stay focused on your breathing as you exercise.
"Coordination" is the key part of coordinated breathing, because it helps you time--or coordinate-- your breaths to keep pace with the rhythm of your movements. This helps you breathe steadily and deeply while you perform physical activities and prevents you from holding your breath, which is a common, but counterproductive reaction that many people have when they exert themselves or feel breathless.
How to Practice Coordinated Breathing
 |
| Photo by Ilke Cole |
The purpose of coordinated breathing is to help you remember to breathe steadily while you exercise instead of breathing erratically or holding your breath. You should practice coordinated breathing any time you work out or do a tiring physical activity.
Coordinated breathing is, more or less, a modified version of pursed lips breathing that helps you match the breathing technique with your movements as you exercise. If you haven't yet memorized and mastered pursed lips breathing, you will probably need to practice it while resting first to let it sink in before you can rely on it to help you in the middle of physical activity.
Here's how you perform the coordinated breathing technique:
-
Before you start a movement that's part of your exercise or activity, take a deep breath in through your nose for a couple of seconds.
- Begin doing your activity and, as you reach the most difficult or exerting part, purse your lips and exhale slowly for twice the number of seconds that you breathed in.

It can help to count your breaths in your head or out loud while you exercise to help you focus on coordinated breathing and keep the correct rhythm. Counting out loud also keeps you from holding your breath and helps you remember to stop or slow down if you get too breathless to speak.
Here are a couple examples of what coordinated breathing looks like in practice when you use it during everyday exercises and activities:
Coordinated Breathing While Climbing Stairs:
-
Start by taking a deep breath in for about two seconds.
-
Then, while breathing out slowly through pursed lips for about four seconds, climb 1-4 steps up.
- Pause, then repeat.
Coordinated Breathing While Vacuuming:
-
Before you start, take a deep breath in for about two seconds.
-
Next, push the vacuum forward while you breathe out slowly through pursed lips for about four seconds.
-
Inhale again for two seconds as you pull the vacuum back toward you.
-
Then, exhale again for about four seconds as you push the vacuum forward once more.
- Repeat.
Another great way to practice coordinated breathing is through certain types of yoga, like Vinyasa, which focus on combining breathing with fluid movements. Tai chi is another type of healthy exercise you can do that utilizes coordinated breathing as part of its routines.
 |
| Photo by Airman 1st Class J. Zuriel |
Check out this video for a helpful demonstration of how to use coordinated breathing during Vinyasa yoga. Even if you don't practice yoga, this video provides a practical example of how to coordinate your breathing with body movements that you can apply to any kind of activity you do.
Deep Breathing
Deep breathing is an effective method for getting trapped air out of your lungs and getting bigger, fuller breaths. Deep breathing can also help you stay calm and reset your breathing pattern when you feel short of breath.
This breathing technique works by filling your lungs up to maximum capacity and then slowly deflating them until every last bit of air is pushed out. This helps gets rid of any stale air that has been trapped in your lungs, which then allows you take in more fresh, oxygen-rich air with every breath.
Deep breathing can also help you relax your body and mind when you feel anxious or stressed. And, since anxiety is a common precursor to worsened shortness of breath, it might even help you preempt bouts of breathlessness triggered by anxiety.
How to Practice Deep Breathing
Deep breathing is a great exercise to practice along with other breathing techniques like pursed-lips breathing and diaphragmatic breathing (discussed in the next section below). When you feel short of breath, it might help to try deep breathing first, that way you can push any trapped air out of your lungs before moving on to other techniques.
Here is how you perform the deep breathing technique:
-
Find a comfortable place to stand or sit and relax your shoulders and chest muscles.
-
Push your elbows back slightly to open up your chest cavity and give your lungs more room to expand.
- Take a deep breath in through your nose until your lungs are fully inflated.
-
Hold your breath for about five seconds. You can count the seconds off in your head to help you stay focused.
- Exhale slowly through your mouth until you have pushed all of the air out of your lungs.
Diaphragmatic Breathing

Diaphragmatic breathing, also known as belly breathing (and sometimes "deep breathing"), is a versatile breathing exercise that can help you breathe more fully, steadily and slowly. It not only prevents breathlessness caused by COPD, but it can help you relax your chest, make it easier to breathe, and allow you to more quickly catch your breath when your symptoms act up.
Diaphragmatic breathing is a classic techniques that has long been recommended to patients with COPD. It is a breathing exercise meant to train your body to breathe from your belly (using your diaphragm) instead of using your chest muscles to breathe.
This is beneficial to people with COPD because their lungs and chest muscles already have to work overtime to make up for the fact that they can't absorb oxygen efficiently. This can cause chest soreness and discomfort, making it more difficult and uncomfortable to breathe.
The idea behind diaphragmatic breathing, however, is that it takes the work of breathing off of your chest muscles and puts it on your diaphragm, which is better designed to handle the work. This can help you breathe easier, get more oxygen to your lungs, and prevent the muscles in your chest, shoulders, and back from getting sore and worn out from breathing.
 |
More recently, however, experts have begun questioning the long-term effectiveness of diaphragmatic breathing for people with COPD. While it can help you breathe from your diaphragm in the short term, more recent research suggests that it may not have the expected long term effects.
For example, some studies show that even when you practice diaphragmatic breathing regularly, it usually doesn't stick. It may not be possible to "retrain" your muscles because, as soon as you're not consciously thinking about breathing with your diaphragm, you'll likely go right back to using your chest muscles to breathe.
However, even if you can't retrain your body to use diaphragmatic breathing all the time, it can still have immediate, short-term benefits. Consciously practicing diaphragmatic breathing when you do activities or experience worsened COPD symptoms can provide some relief and reduce the amount of effort it takes to breathe.
For example, if you have severe COPD or experience a flare-up or exacerbation, you might experience worsened chest pain or sore chest muscles from coughing and wheezing. At times like these, you may be able to take some of the strain off of your chest and temporarily relieve some discomfort by practicing diaphragmatic breathing.
How to Practice Diaphragmatic Breathing

To practice diaphragmatic breathing, it's best to lie on your back in a quiet, comfortable place. However, you can also practice this technique while sitting or standing if needed.
Here is how you practice diaphragmatic breathing:
-
Sit down in a chair or lie down in a comfortable position. Make sure to relax the muscles in your shoulders, neck, and chest.
-
Then, place one of your hands on your chest and one on your belly so you can feel them expand as you breathe.
-
Take a deep breath in, concentrating on using your belly (diaphragm) to breathe. You should feel your stomach inflate and the hand resting on your belly should rise as you inhale. Focus on keeping your chest still.
-
Next, exhale slowly though pursed lips, focusing on using your belly to push the air out while keeping your chest still. You should feel your belly deflate and the hand on your stomach should fall as you breathe out.
- Repeat.
The key part of diaphragmatic breathing is keeping your chest muscles relaxed while you breathe with your stomach (or diaphragm). Placing your hands on your stomach and chest helps you focus on this goal and easily identify which muscles you are using to breathe.
For more information and a demonstration of how to practice this technique, check out this video on diaphragmatic breathing from the American Lung Association. This video will help you better understand the benefits of diaphragmatic breathing and how to use the exercise to improve your breathing in everyday life.
The Power of a Relaxed Posture

You might have noticed that the first step to practicing any of these breathing techniques is to relax your body. That is because it's common to tense up the muscles in your shoulders, neck, and back when you are struggling to breathe.
This tense posture happens naturally, but it can make it even more difficult to breathe when you feel short of breath. Instead, you should always do your best to keep your body relaxed, even when you're feel like you can't breathe.
Keeping the muscles in your neck, chest, and shoulders relaxed can help relieve airway obstruction and make it easier to catch your breath. It not only relaxes the muscles in your chest cavity, giving your lungs more room to expand, but also relaxes the muscles in your throat and airways so air can more easily flow through.
Relaxing your body can also help you feel more calm, as tense muscles send signals to your brain that make you more aroused and anxious. The more calm you are, the easier it is to slow your breathing rate and stay focused on productive breathing exercises that can make the breathlessness pass.
Pulmonary Rehabilitation
Pulmonary rehabilitation is like a special health class designed to help people with COPD and other respiratory diseases improve their breathing and better manage respiratory symptoms like shortness of breath. Taking a pulmonary rehabilitation class is a fantastic way to learn more about breathing techniques and how to use them during exercise and in your everyday life.
In pulmonary rehab, you will get plenty of opportunities to learn and practice practical breathing strategies and exercises along with other patients who have COPD. You'll also learn how to use your medications to control your symptoms, how to make lung-healthy lifestyle choices, and how to exercise while coordinating your breathing and keeping your symptoms under control.
Pulmonary rehabilitation is often recommended to COPD patients who have trouble exercising, doing daily activities, or managing their symptoms on their own. If you would like to join a pulmonary rehabilitation class you will need to talk to your doctor to get a referral first.
Practice Makes Perfect!
If you have COPD, there's no excuse for not learning and utilizing these extremely simple, yet surprisingly powerful, techniques for controlling your breathing. They're not only easy to learn, but easy to practice compared to other COPD treatments because they take such a little amount of effort and time out of your day.
After studying this article, you should know how to practice the most effective COPD breathing exercises and understand when each is most helpful to use. If you put in the time to study and practice these techniques, you'll be better able to catch your breath and keep your breathing steady in the midst of difficult COPD symptoms.
As we've mentioned before, practicing breathing techniques regularly, especially when you're not having trouble breathing, is key for reaping maximum benefits from the exercise. After
Getting enough sleep is a daily challenge for many people with COPD. Between coughing, breathing troubles, and shortness of breath, it's no wonder that the disease makes it difficult to relax and sleep soundly at night.
Up to fifty percent of people with COPD report sleeping problems, which makes it a major concern for COPD treatment. Good quality, adequate sleep is necessary for a healthy body and immune system, and constant sleep disturbances can make COPD patients much more prone to illnesses, exacerbations, and other dangerous complications.
What's more, COPD patients are disproportionately affected by sleep disorders. For example, people with COPD are more likely to have sleep apnea, a dangerous condition that occurs when your airways collapse and restrict your airflow when you sleep.
In this article, we're going to show you a variety of different ways to improve your quality of sleep at night. But first, you need to understand why getting enough sleep is so important for your mental and physical state.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Why it's Important to Get Enough Sleep
Sleep deprivation can have devastating effects on your ability to concentrate, remember things, and deal with the pressures of everyday life. It also weakens your physical state, making you more prone to getting sick and having an acute COPD exacerbation.
If you have trouble getting enough sleep or wake up often during the night, it actually suppresses your immune system and makes you more likely to get sick. Some studies have shown that COPD patients who get poor sleep are up to fifty percent more likely to experience an acute exacerbation.
Lack of sleep also contributes to a variety of other health issues and chronic diseases including diabetes, high blood pressure, obesity, mood disorders, and inflammation. It also affects your mental state, making it more difficult to focus, problem-solve, and remember things. It can even lead to anxiety and depression over time.
To avoid these problems and keep your body healthy, getting enough sleep is a must. If you are having difficulty sleeping on a regular basis, you should start trying new ways to get better sleep right away.
Even though COPD can make sleeping challenging, there are plenty of ways to reduce and manage nighttime symptoms and make yourself more comfortable at night. Instead of giving up on good sleep, take some time to learn about the variety of medications, medical tools, and lifestyle changes that are proven to help you sleep better.
In this article, we'll show you many different techniques you can use to make it easier to fall and stay asleep every night. If you want to learn how to get better sleep, reduce your COPD symptoms, and experience the benefits of being well-rested, continue reading this article for a variety of practical tips you can use to get better quality sleep with COPD.
Why COPD Makes it So Difficult to Sleep

There are many reasons that a large percentage of COPD sufferers find it difficult to relax and get good quality sleep at night. COPD symptoms on their own often interfere with rest, but other, indirect effects of COPD can also make it difficult to sleep.
Many people with COPD experience disease-related anxiety or depression, or are at a higher risk for other conditions that affect sleep, including GERD and sleep apnea. In addition, medications used to treat COPD symptoms can cause poor sleep as well.
Here are a few major factors that contribute to sleep problems in people with COPD:
-
Disruptive COPD symptoms: It's not hard to imagine how feeling short of breath or having a coughing fit can make it difficult to relax and fall asleep at night. Shallow breathing at night can also cause blood oxygen levels to drop, which can cause you to wake up abruptly and frequently as a result.
-
Anxiety and mental health problems: COPD is a difficult chronic disease to live with, and it can take a huge toll on your emotional and mental health. It's common for people with COPD to experience anxiety disorders, depression, and general emotional distress, all of which can make it difficult to sleep.
-
Medications used to treat COPD: Some COPD medications, especially bronchodilator medications, can make it more difficult to sleep. Some medications have indirect side effects that can affect your ability to sleep as well, such as medications that cause nightmares or cause frequent urination during the night.
-
Obstructive Sleep Apnea: Obstructive sleep apnea is a breathing-related sleep disorder that affects a large percentage of COPD patients. It causes frequent lapses in breathing during sleep and causes people with the condition to startle awake frequently at night. Sleep apnea can still affect your sleep even if you don't know you have it and if, like most sufferers, you don't remember waking up during the night.
-
GERD (Gastroesophageal Reflux Disease): This is a condition that occurs when stomach acid leaks into your throat, and it affects a large number of people with COPD. GERD symptoms tend to be most noticeable at night while lying down, and it can affect your quality of sleep.
- Difficulty sleeping in a comfortable position: COPD-related breathing problems can make it difficult to breathe while lying down. As a result, many people with COPD end up sleeping in uncomfortable, unhealthy positions, such as sitting up in a chair.

While COPD can make getting adequate, good-quality sleep a challenge, it's a challenge that can be conquered with simple solutions and adjustments to your daytime and nighttime routines. In this article, we're going to show you how to conquer each of these COPD-related sleeping problems so you can get the rest and energy you need to enjoy your life to the fullest.
There are a variety of practical ways to conquer the most common emotional, physical, and environmental causes of poor sleep in people with COPD. With this guide, you can begin addressing your sleep barriers today and start building a sleep-healthy lifestyle that will give you the consistent, restful sleep you've always wanted.
How to Get Better Sleep if You Have COPD
Change Your Bedtime Routine
Many sleep problems in the modern world result from poor habits. Even if COPD is the main cause of your sleeping difficulties, looking at your overall bedtime routine is still wise.
For example, habits like exercising in the evening or spending time on your phone or computer late at night make it much more difficult for your body to feel tired at bedtime. Also, running errands, doing chores, and working late in the evening doesn't put you in a good mindset for sleep.

Many of these habits are simple to change and can be surprisingly effective at improving your quality of rest. One of the most important things you can do is establish a relaxing, consistent bedtime routine that allows you to gradually wind down in the evenings.
For example, try planning relaxing activities like reading, yoga, or listening to music close to the time that you go to sleep. Work these kinds of activities into a routine you can follow every night, that way, when you follow your bedtime routine, your brain and your body will know it's time to rest and start preparing to go to sleep.

Here are some general tips for nighttime habits that can improve your ability to sleep:
-
Dim the lights at least an hour or so before you go to bed. That will help your brain and body start to feel drowsy so it's easier to fall asleep when it's time.
-
Don't do stressful or mentally taxing activities before bed. Try to find relaxing, idle activities that allow your mind to wind down and let go of worries.
-
Go to bed at the same time every night and set your alarm for the same time every morning, even on weekends. This will help your body adjust to your sleep pattern and fall asleep naturally at the right time every night.
-
Practice relaxation exercises like mindfulness meditation, breathing exercises, or yoga in the evenings to help your body and mind relax.
-
Try taking a warm shower or bath near bedtime; warming up your body will help you feel more sleepy.
-
Try drinking warm milk or decaffeinated tea to relax and wind down before bed. Just don't drink anything with caffeine and avoid drinking too close to bedtime if it will make you have to get up to go to the bathroom during the night.
-
Never use your computer, phone, or laptop in your bed or too close to bedtime. The light from the screen tricks your brain into thinking it's still daytime and makes it more difficult to go to sleep.
-
Use your bed for two things only: sleeping and sex. That way your body will know it's time to sleep and feel drowsy when you get in bed. Don't read books, browse the internet, or watch TV in your bed. It's a hard habit to break, but it can save you from many restless nights.
-
Clear your airways before bed to reduce symptoms like coughing and shortness of breath. Use proven mucus clearance techniques like chest percussion and huff coughing.
- Don't sleep with pets in your bed, no matter how much you like to have them by your side. Studies show that pets can severely disturb your sleep, even if you're not aware of it. Get your pet a nice warm bed of their own to keep next to yours. Don't worry, both you and your pet will adjust quickly and you'll have more energy to give them in the mornings.
Stay Away from Alcohol and Caffeine at Night

While caffeine is an obvious cause for poor sleep, many people don't realize that alcohol can hurt your quality of sleep as well. Caffeine affects your brain and makes it difficult to fall asleep, while alcohol affects your brain and muscles, making it more difficult both to breathe and to stay asleep through the night.
One way that alcohol affects your sleep is by causing the muscles lining your throat and airways to relax too much when you sleep. This causes your airways to collapse or sag and obstruct airflow, which affects your ability to breathe and absorb oxygen at night.
This is a greater risk for people with COPD, who already tend to suffer from sleep disorders and nighttime breathing problems. Alcohol also affects your brain and your sleep cycles, and drinking alcohol too close to bedtime leads to worsened sleep quality.
Caffeine is a stimulant that can also affect your ability to fall asleep at night, especially if consume it too close to bedtime. For the best possible sleep, you should avoid caffeine for at least eight hours before you go to bed or cut it out of your diet altogether.
Avoid Foods that Trigger GERD
Gastroesophageal reflux disease (GERD) is a common digestive issue in people with COPD. In fact, by some estimates, up to fifty percent of COPD patients also suffer from GERD.
Some of the common symptoms of GERD are indigestion and difficulty breathing at night, which is particularly uncomfortable for people with respiratory diseases. These symptoms are most noticeable during the night because, when you're lying down, it's easier for stomach acid to leak into your esophagus. This causes heartburn and throat irritation that make it difficult to sleep and can leave you with a sore throat in the morning.
The best way to prevent nighttime GERD symptoms is to eat a GERD-friendly diet. If you suffer from GERD, be careful not to eat foods, like acidic foods, that might trigger your GERD symptoms, especially at night before bed.
Another thing that can help is to eat something bland and absorptive before going to sleep. Try eating a few light crackers, like plain saltine crackers, before bed to keep your hunger and stomach acid at bay.
If you still struggle with GERD symptoms after adjusting your diet, talk to your doctor about medications and antacids you can take to keep your symptoms under control. In severe cases, you might need stronger medications or surgery to treat your GERD.
Don't Eat too Close to Bedtime

Many people with COPD find that a full stomach makes them feel extra breathless. This happens when your stomach expands and presses on your lungs and diaphragm, making it more difficult to breathe.
This can make you very uncomfortable, especially if you're trying to rest. Feeling bloated and breathless makes it hard to relax and will likely hurt your quality of sleep at night.
The best way to prevent this is to eat several smaller meals throughout the day, instead of three large ones. Also, be careful not to eat too much too close to bedtime, otherwise, you'll be at risk for breathlessness and indigestion as you try to sleep.
You don't want to go to bed hungry, though, so have a light, healthy snack ready in case your appetite kicks in before you go to sleep. Saltine crackers, a bit of cheese, or another small, quick, low-sugar snack will do.
Make Your Bedroom More Pleasant

Many people underestimate the impact that their environment has on their ability to sleep. If the bed and the room you sleep in doesn't feel comfortable, it makes it much more difficult to relax and rest at night.
Take a moment to look around your bedroom, and ask yourself, “Is this a place I look forward to sleeping in?” Is the room cozy and comfy, quiet, and free from clutter?
It's important to sleep in an environment that is quiet, dark, and comfortable, otherwise, it will be difficult to sleep undisturbed. Your sleep environment should be free from messes, bright screens and electronics, and anything else that could be distracting or stressful while you're trying to sleep.
Here are some tips for making your bedroom environment more cozy and comfortable:
-
Save up for a better mattress or more comfortable bedding. Lying on a luxurious mattress or wrapping yourself in soft, silky sheets can help you relax at night and even look forward to going to bed.
-
Clean up messes and clutter and organize your space. Make sure every item in your bedroom has a proper place so it's easy to keep clean.
-
White noise can be very effective at blocking sounds that come from outside your room. Get a white noise machine to place near a noisy window or door to drown out disruptive sounds while you sleep.
-
If bright light comes in through your window in the morning, consider getting a blackout curtain to keep your room dark. You could also hang a thick blanket in front of the window or get a comfortable eye mask to block the sun from your eyes.
-
Keep anything that reminds you of work or responsibilities out of your bedroom. Keep your bills, work documents, and other task-related items somewhere else, so they don't trigger anxiety before bed.
- It's easier to sleep if you keep your room cool at night. You can do this by setting your AC to a comfortable temperature, opening a window, or aiming a fan at your bed.

It's easy to ignore messes and environmental annoyances in the bedroom, but it's not a part of your house you should neglect. It's worth taking some time to personalize, organize, and turn your bedroom into a place where you can actually be comfortable and enjoy sleeping.
Take Care of Your Mental Health

If you're having trouble relaxing and sleeping at night, it might be because of mental distress. It's normal and common for people with COPD to experience negative emotions or psychological disorders like anxiety and depression, all of which can severely interfere with your ability to sleep.
Living with a chronic disease is hard; it can be exhausting, frightening, and take a huge toll on your life. It's natural to experience anxiety, depression, and emotional distress as your symptoms worsen and you lose your physical independence.
That's why it's so important to look after your mental health and see a mental health professional if you can't cope on your own. Instead of withdrawing or letting anxiety eat away at your life, turn to your family, friends, and pets for joy and comfort. Do your best to continue doing the hobbies and activities you enjoy and don't let your disease define your life or who you are.
Part of looking after your mental health includes setting aside time for quiet and relaxation every day. Proven techniques like mindfulness meditation or creative hobbies are a great way to unwind and refuel your mental resources.

A healthy diet, healthy sleep schedule, and regular exercise can also do wonders for your mental health. Getting regular aerobic exercise, in particular, is a very effective treatment for anxiety that will also help you feel tired enough to go to sleep at night.
If you suffer from severe anxiety or depression that disrupts your daily life, talk to your doctor about treatments or medications that can help. Your doctor might refer you to a psychologist or psychiatrist or prescribe anti-depressant medications to help you improve your mental health and quality of life.
Consider Therapy

People with COPD often feel isolated, disconnected, and find it difficult to ask for support. But everyone needs mental and emotional help now and then, especially when going through a difficult time like managing a chronic disease.
Many people find that counseling and talk therapy help them confront their anxiety, depression, and other negative emotions related to their disease. Individual therapy provides a safe, intimate setting to unpack personal thoughts, worries, and fears and work through mental barriers that make it difficult to fully enjoy life.
You can also find COPD therapy groups where you can connect with other people who understand what you're going through. There are a variety of both online and local therapy groups designed specifically for people with COPD and other chronic diseases.
Talking with other COPD patients and sharing your challenges and successes is a great way to regain confidence and a feeling of control over your disease. You can also get useful advice, emotional support, and new friends through group therapy that you would never have gotten if you tried to cope on your own.
Keep a Journal

If you suffer from anxiety or depression, then you know how they can take a toll on your ability to sleep. Many people with COPD experience hopelessness, despair, fear, and worry, which often intensify and are difficult to ignore at night.
That's why it's important to quiet your mind and let go of your worries and fears before bed. One method for doing this is journaling, an activity researchers have proven time and time again is a powerful and effective tool for mental health.
There are no hard rules for journaling; a huge part of its benefits come from the freedom that journaling gives you to write and express yourself freely, without strict guidelines or judgment. All you have to do is spend at least a few solid minutes writing something—anything—about yourself, your life, or your thoughts.
Journaling before you go to bed is a great way to unload all the distressing thoughts and worries that have accumulated in your head during the day. Recording your hopes, your fears, or even your to-do list in your journal can help you let go of heavy thoughts and feel calm enough to sleep.
Here are some general tips to help you get the most out of journaling:
-
Try to write in your journal regularly, ideally every day. That way it becomes a habit and something you can look forward to that will help you relax before bed.
-
Don't edit, scrutinize, or judge yourself as you write. Let the words flow freely and uncensored; it's about the action of writing, not how eloquent or pretty it looks on paper.
-
It's okay not to write in full sentences. It's okay to write stories, lists, and streams of consciousness. You don't have to be grammatically correct, and you don't even have to make sense. A journal is about expressing yourself in whatever way you please.
- Your journal is, primarily, for you and you alone. However, if you desire, you can share pages or passages with others. Sometimes it's easier to express yourself and communicate on paper, and sharing your thoughts and feelings with others can be therapeutic.
Progressive Muscle Relaxation
Another technique that can help to quiet nighttime anxiety and restlessness is progressive muscle relaxation. It is a method for reducing muscle tension and relaxing your body before you sleep, and it's often recommended for people who suffer from insomnia.
Anxiety and mental distress affect more than just your emotional state; they have noticeable physiological effects, too. Anxiety, in particular, tends to manifest in your body as muscle tension and jitters that can make relaxation all but impossible.
Progressive muscle relaxation addresses anxiety from the outside in; that is, by relaxing your muscles and reducing the physical effects of anxiety, it helps to reduce the feeling of anxiety that you experience on the inside, as well. It also helps prevent muscle spasms and tightness, so you can relax and feel more comfortable in bed.
Y

It’s pretty amazing to think about how quickly health care advances these days. Just in the past couple of decades, medical specialists have made significant strides with everything from mapping the human genome to improving telemedicine and even introducing robotic surgery. According to Singularity Hub, we’re likely to see medicine advance more in the next 10 years than it did in the past 100 years.
If you have a respiratory condition such as asthma, COPD, or cystic fibrosis, you might also be surprised to find that your treatment plan would have looked very different 100 years ago than it does today. Using modern testing procedures and techniques, doctors are able to provide a more accurate diagnosis than ever before and help patients plan their life accordingly.
With all that being said, the way we treat COPD will likely look very different in another 10 years than it does today. As we speak, researchers are working on a number of different medicines, tests, and surgeries that may prove to be breakthroughs in the way that we treat and diagnose one of the world’s most prevalent illnesses.
In this post, we’re going to take a look at several different emerging medical breakthroughs that COPD patients should keep an eye on in the coming years. While these procedures show promise, it’s important to remember that they’re still in a developmental stage. Currently, your best bet for reducing COPD symptoms and slowing the progression of your disease is to follow your doctor’s instructions.
Stem Cell Therapy
Stem cell therapy is possibly one of the most talked-about medical breakthroughs, not just for COPD, but also for a variety of other conditions such as macular degeneration, spinal cord injury, stroke, burns, heart disease, and more. Also known as “regenerative medicine,” the goal of stem cell therapy is to generate healthy cells in the body to replace diseased ones.
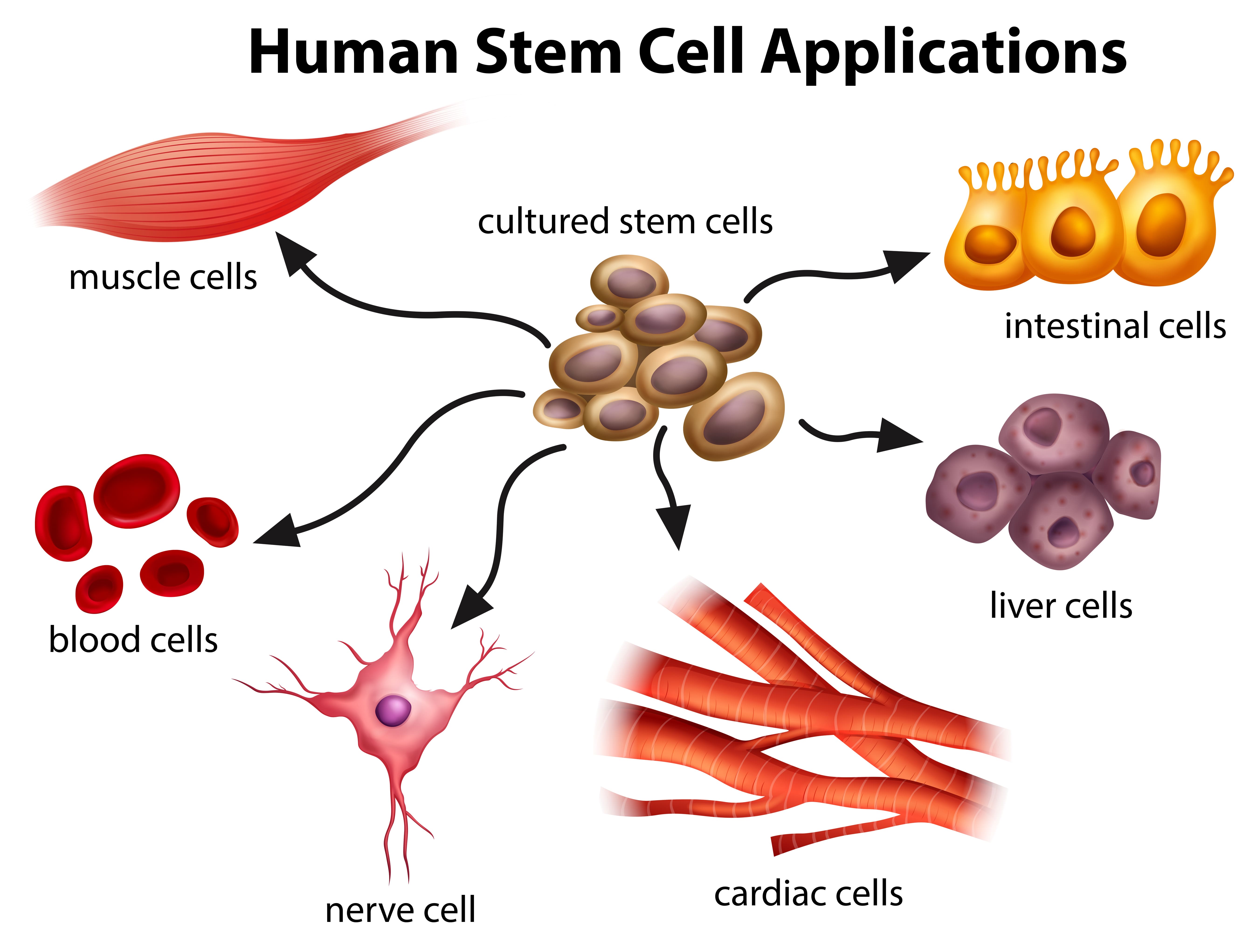
In essence, a stem cell is a sort of canvas on which all other types of cells are made. When they’re exposed to the right conditions — either in the body or in a lab — stem cells divide into “daughter cells” which are more specialized and suited to accomplish a certain task or goal. For example, white blood cells can be produced to help fight and dispose of foreign invaders in the body.
The reason there is so much talk around COPD and stem cell therapy is that COPD is a “progressive disease.” What this means is that once inflammation starts to develop in the airways of the lungs, the damage cannot be reversed. In order to slow the disease progression, you’ll need to follow a strict treatment plan created by your pulmonologist.
According to DVCStem, stem cells can repair damaged lung tissue to combat either emphysema or chronic bronchitis, the two diseases that makeup COPD. A study conducted by the Lung Institute showed a number of positive results, stating that patients “averaged an increase of 35.5% to their Quality of Life (QLS) score within three months of treatment.” It also found that 84% of patients saw an increase in their quality of life after 3 months.
However, since stem cell therapy is such a new procedure, more tests are needed to verify its efficacy using larger sample sizes and other factors such as exercise tests, hospital visits, the use of oxygen therapy, and more. Periodic patient follow-up will also help researchers better understand the long-term benefits of stem cell therapy on COPD. So far, these studies have shown no negative side-effects to using stem cell therapy.
Endobronchial Valves
Endoscopy is the process of inserting a tube with a camera into the body in order to view certain organs in more detail. In certain situations, health professionals may need to look inside a patient’s airways either to examine signs of damaged tissue or to take samples. This is known as a bronchoscopy.
One of the more recent advancements in endoscopy is something called an endobronchial valve (EBV). This is a small implantable medical device that can help people with lung disease (primarily emphysema) breathe easier. While endobronchial valves were approved by the U.S. Food and Drug Administration in 2018, they’re still considered a developing technology, and studies are being done to improve their efficacy.
According to the Cleveland Clinic, about 3 million people have emphysema in the United States. It’s one of the diseases under the umbrella term “COPD” and it’s characterized by swollen and damaged alveoli, the tiny air sacs in the lung that are responsible for the transfer of oxygen and carbon dioxide to and from the blood.
One of the primary symptoms of emphysema is breathlessness. As the air sacs in the lungs become inflamed, they lose a lot of their elasticity and they begin to trap air inside the lungs. This stagnant air, also known as “dead-space ventilation,” prevents new, oxygen-rich air from entering the lungs making it very difficult to get the oxygen your body needs.
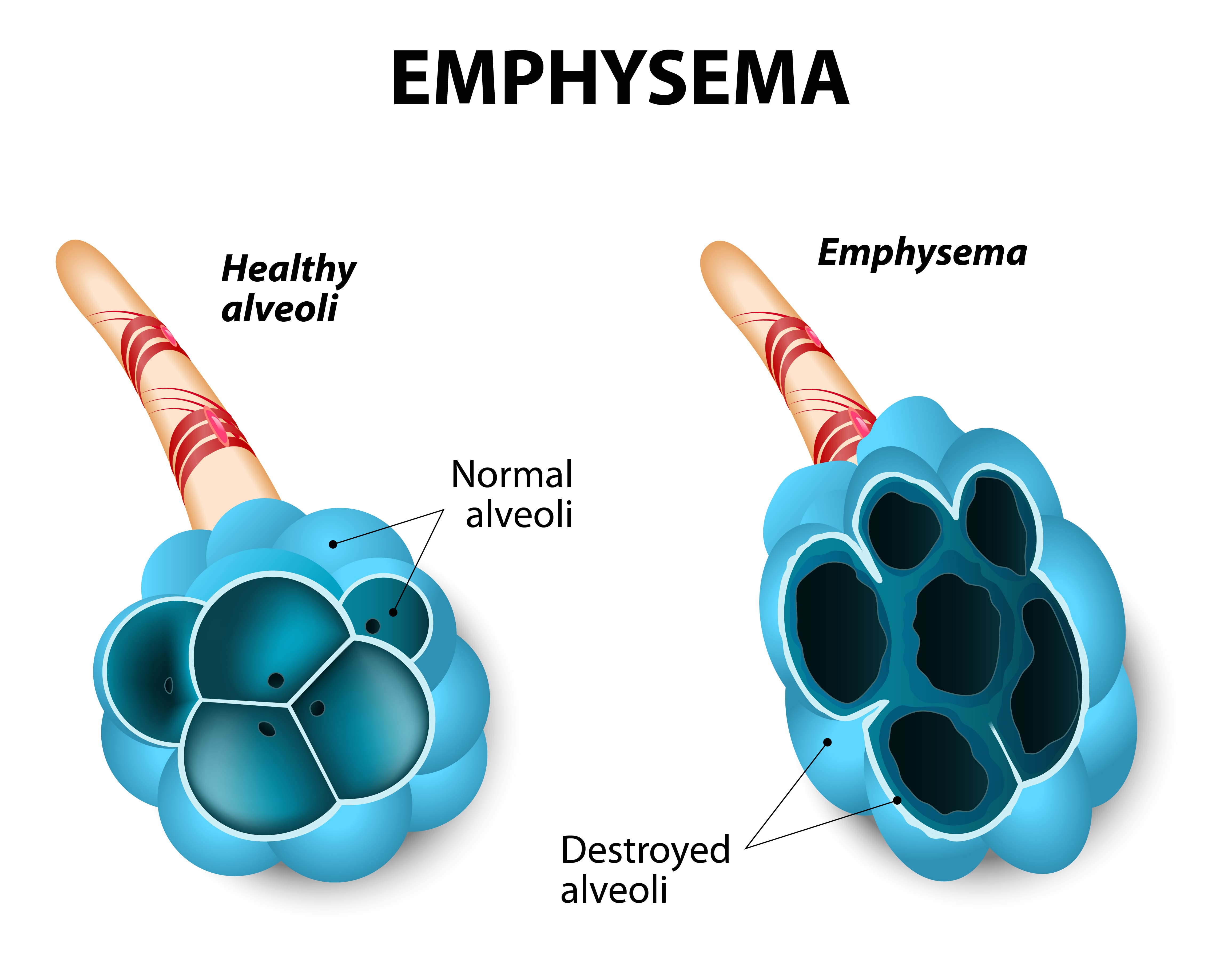
While it may sound counterintuitive, endobronchial valves actually block off a portion of the lungs that are most damaged by emphysema. By doing so, medical professionals can actually improve the mechanical efficiency of the lungs meaning it will take less energy and effort to breathe. Endobronchial valves are one-way, meaning inspired air is redirected to healthy parts of the lungs but carbon dioxide-rich air is still able to escape from the damaged part.
One of the greatest benefits of endobronchial valves is that they are an effective alternative to other more invasive procedures such as lung volume reduction surgery and lung transplant surgery. Lung volume reduction is a procedure that surgically removes the damaged tissue in the lungs while lung transplants are a full replacement of both lungs. Either way, these procedures are extremely invasive and they can be very costly as well.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
With that being said, endobronchial valves are not without their problems as well. While they have been proven to increase Forced Expiratory Volume (FEV1) for many patients, there isn’t enough information to verify its efficacy for all patients. The number one complication associated with these valves is pneumothorax, a condition where the lungs partially or fully collapse. The good news is that endobronchial valves can be quickly and easily removed if this risk is identified.
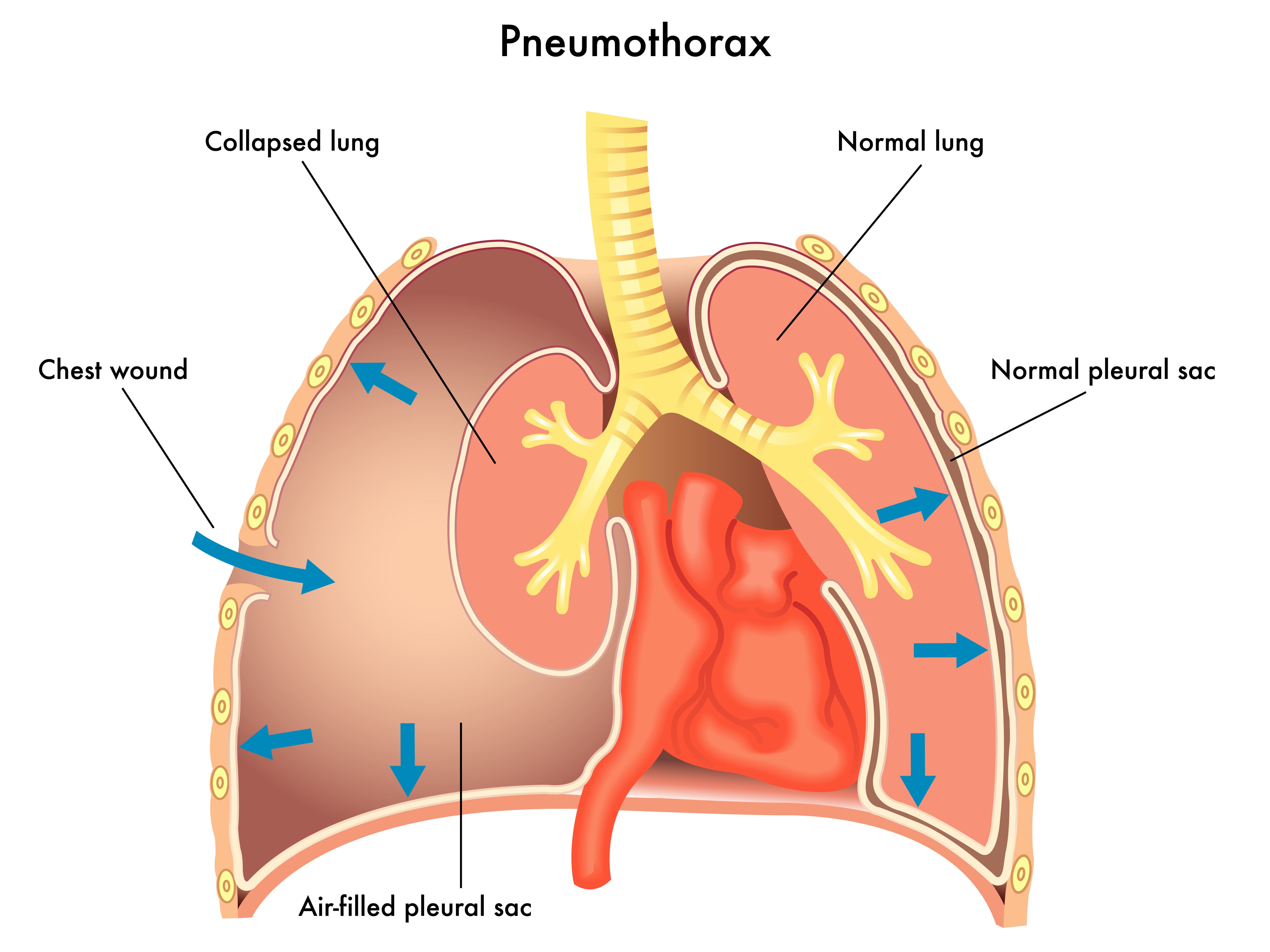
There are several other implantable medical devices that can be used for lung volume reduction in emphysema patients. Endobronchial coils, for example, are implanted through a similar process as endobronchial valves, and they’re intended to prevent hyperinflation of the lungs. Intrabronchial valves are another device with a similar function to endobronchial valves but they’re typically used to manage post-operative air leaks and allow mucus to clear correctly.
Targeted Lung Denervation (TLD)
Targeted lung denervation is another type of bronchoscopic therapy that can be used to treat COPD. During this procedure, a specialized catheter is inserted into the main bronchial pathway. At the end of this catheter is an electrode that emits RF frequency. Ultimately, the goal is to interrupt nerve transmissions which has a permanent bronchodilatory effect. It also reduces mucus production and decreases airway inflammation through the reduction of acetylcholine. This neurotransmitter is known to affect mucus secretion, inflammation, and muscle tone.
According to studies published in Healio, a medical journal, targeted lung denervation is associated with a lower risk of COPD exacerbation and lower hospital admittance after a 1-year period. Another study found that targeted lung denervation therapy was just as effective as long-acted inhaled anticholinergic therapy (drugs that block these neurotransmitters) and there were no noted adverse side-effects either. We’ll likely need to see more thorough studies of this procedure before it becomes a major treatment option for COPD patients.
Bronchoscopy Thermal Vapor Ablation (BTVA)
Yet another lung volume reduction technique, bronchoscopy thermal vapor ablation helps to limit hyperinflation in emphysema patients. Studies have shown that this method can be particularly useful in treating patients with upper lobe-predominant emphysema by improving lung function, exercise capacity, and quality of life.
Prior to the procedure, medical specialists will use a specialized program that’s designed to target the most emphysemic areas of the lungs. Once these areas are located, a catheter is applied that delivers heated water vapor. This results in a thermal reaction and immune response which leads to permanent fibrosis and atelectasis. This has a similar effect to other lung volume reduction techniques by reducing tissue and air volume and improving lung mechanics.
Typically, BTVA is done under deep sedation or general anesthesia and patients are monitored for a minimum of 24 hours after the procedure. Periodic checkups are advised for at least three to six months after the procedure to ensure no complications occur. While future studies are needed, BTVA has been proven to have a favorable benefit-risk in patients with heterogeneous emphysema.
Bronchial Rheoplasty
Not all bronchoscopy therapies are aimed at lung volume reduction. Bronchial rhinoplasty, for example, is used for patients with chronic bronchitis who are experiencing increased mucus production. Mucus can be a serious problem for COPD patients because the cilia which typically clear mucus from the airways is usually impaired or damaged due to chronic inflammation. Additionally, many patients, especially those with stage 3 or stage 4 COPD, are unable to perform mucus clearing techniques such as huff cough.
.jpg)
Bronchial rhinoplasty is a procedure that involves targeting cells that are producing excess mucus and applying electrical currents. This results in mucus-producing cells dying off and being replaced with healthier ones. In the fall of 2019, the RheOx Bronchial Rheoplasty system was granted Breakthrough Device Designation by the FDA, representing a significant step forward for bronchial rhinoplasty.
Robotic Lung Volume Reduction Surgery
In early 2019, the first-ever robotic lung volume reduction surgery was performed in Northwestern Memorial Hospital using the da Vinci Xi Surgical System. This system was developed by Intuitive, a company that’s been at the forefront of surgical robotics for over 20 years.

The reason this is such a significant breakthrough is that it is far less invasive than traditional lung volume reduction surgery. According to OR Today, RLVRS requires only three 8-millimeter incisions on the chest in order to remove damaged tissue in the lungs. This is much smaller than the incision required in the traditional surgery meaning it can effectively reduce scarring and pain for the patient.
Another benefit of robotic surgery is that it significantly reduces the risk of collateral damage. According to the Journal of Robotic Surgery, robotic surgery provides surgeons with a number of benefits over traditional surgery like improved depth perception and steadier incisions. Robotic surgery enables surgeons to work around tissues or organs rather than having to cut through them.
Interleukin-5 (IL-5) Antagonists
Oftentimes, standard COPD treatment options don’t work on certain patients. In this case, doctors need to perform more tests in order to better understand their condition. For example, your doctor can use blood tests to determine if you have eosinophilia or not. This results when there are a high number of white blood cells called eosinophils in your blood. According to this report, one-third of all COPD patients show signs of eosinophilia.
The problem with a high eosinophil count is that it is likely a significant contributor to airway inflammation. They have been associated with an increased risk of exacerbations as well as reduced lung function in both COPD and asthma patients. Interleukin-5 (IL-5) antagonists are a developing class of drugs that are specifically designed to target the IL-5 receptor in the body, thus reducing the release of eosinophils.
Like with most of the therapies on this list, we will need to see more evidence before IL-5 antagonists become a major part of COPD treatment plans. IL-5s have been used to treat asthma for several years, but we don’t have a significant enough body of evidence to prove its efficacy and safety when treating COPD.
Conclusion
As you can see, there are a number of exciting medical breakthroughs for emphysema and chronic bronchitis patients to follow. In the past, respiratory patients have typically been prescribed a standardized treatment plan. However, with more advanced testing methods, doctors are able to divide their patients into smaller groups with more specialized treatment regimens.
Whether you’ve just been diagnosed with COPD or you’re well-acquainted with your COPD treatment plan, it’s worth addressing these new therapies with your doctor. There may be additional opportunities for further testing, allowing you to better understand your disease and benefit from treatments that are not yet widely available. Clinicaltrials.gov is another great resource if you’d like to learn about getting involved with new therapies and medications.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













