Nowadays, we rely on our devices for just about everything. Cellphones, for example, are used for everything from making calls and sending text messages to tracking our fitness progress or staying connected with online communities. If you’ve been diagnosed with COPD or another chronic respiratory ailment, this reliance on technology doesn’t go away. In some cases, you might even be more dependent on technology than previously. This isn’t necessarily a bad thing though as long as you’re using devices that are reliable and match your lifestyle.
In this post, we’re going to take a look at seven of the most important devices you can own with chronic obstructive pulmonary disease (COPD). Whether you’ve just been diagnosed or you’ve been living with COPD for some time, these devices are considered to be essential by many or at the very least, incredibly convenient to have. If you have any questions, be sure to leave them in the comment section below, and don’t forget to bookmark our blog page so that you never miss our latest articles.
Portable Oxygen Concentrator
At one point or another, most COPD patients will need to use supplemental oxygen. When the lungs are impaired due to chronic inflammation, supplemental oxygen ensures that the oxygen levels in your blood are normal; and in turn, every organ in your body receives the oxygen it needs to function properly. Supplemental oxygen not only improves your longevity as a COPD patient, but it can also help you feel better in the moment. Oxygen therapy will reduce breathlessness, fatigue, and lightheadedness associated with low oxygen levels.

However, many people falter when it comes to actually choosing the oxygen device that they will use. Patients and healthcare providers often default to oxygen tanks or liquid oxygen tanks because they are cheap and thus have a low barrier of entry. However, when it comes to the patient’s long-term health and well-being, they often find that these oxygen devices are lacking in many ways. First and foremost, they have to be refilled once the oxygen in them is depleted. This can be costly and takes your time and attention away from more important things like spending time with friends and family.

Another problem with oxygen tanks is that they are heavy and bulky. Chances are, you’ve seen people walking around while lugging around a big green tank behind them. The reason these tanks are so big is that they contain compressed oxygen gas which takes up a lot of space. This problem is somewhat mitigated by using a tank that stores oxygen in its liquid form but this still has a lot of problems associated with it. In most cases, the best alternative is to use something called a portable oxygen concentrator.
Unlike oxygen tanks which limit your freedom and mobility, portable oxygen concentrators are designed for people who are on the go frequently and need something reliable. Rather than storing oxygen within the unit, POCs draw in ambient air and remove unnecessary gases, then put out medical-grade oxygen. POCs are electronic devices that run off of powerful lithium-ion batteries. In other words, you simply need access to either a wall or car outlet to charge the batteries, then you will be set for the rest of the day!
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Nebulizer
Another important device to own as a COPD patient is a nebulizer. What a nebulizer does is crush up your COPD medication into a fine mist called aerosol so that it can be inhaled more easily by the patient. This helps the medication reach your lungs faster and thus is faster-acting than medication that is taken orally. You should be sure to speak with your doctor to see if nebulizers are right for you.

Many people think of nebulizers as devices that they can only use at home, however, there’s been a sudden emergence of portable nebulizers that you can take with you if you go on a trip. Nebulizers differ from inhalers in that they put out a constant stream of aerosol whereas inhalers put out “puffs.” This is beneficial for people with severe COPD who may not be able to inhale deeply or sharply enough to bring the medication into their lungs. With a nebulizer, however, you can simply breathe naturally and be sure that the medication is reaching your lungs.

Much like portable oxygen concentrators, nebulizers are usually electronic devices that either run off of a battery or they need to be plugged into an electrical outlet. It should be noted that not all medications can be administered through a nebulizer. Most likely, your doctor will only have you use medication known as bronchodilators which open up your airways in the event of a COPD exacerbation. Bronchodilators include Pulmicort, Xopenex, albuterol, and more.
Pulse Oximeter
A pulse oximeter is a device that measures the level of oxygen saturation in your blood. Pulse oximeters are very small and lightweight and they’re the least invasive way to check whether you’re getting enough oxygen or not. One of the only other alternatives is arterial blood gas (ABG) analysis which requires your doctor to draw blood in order to determine your oxygen saturation level. While these readings are oftentimes more accurate than pulse oximetry they require you to be at the doctor’s office in order to get your results. Pulse oximeters can be used anywhere and anytime.
Pulse oximeters work by passing light through the finger and measuring the amount of light that comes out the other side. This determines the amount of oxygenated and deoxygenated blood cells and thus your blood oxygen saturation. Many people are surprised to find that these devices cost under $20. However, if you want a more advanced one that connects to your cellphone or smart device, it could run you over $100. Either way, this is something that all COPD patients should have so that they can ensure that they’re receiving enough oxygen. It can also help you determine whether your oxygen device is working properly.
High-Frequency Chest Wall Oscillation Vest
Mucus plays a very important role in the body. It coats the lining of your lungs and airways and if you inhale irritants or bacteria, the mucus traps it so that it can be cleared before it leads to an infection. Unfortunately, many COPD patients aren’t able to create an expiratory force great enough to clear mucus, and as a result, it becomes lodged in the airways. Years of smoking can also damage the cilia in the airways which are small cells that help pass the mucus out of the lungs. Most COPD patients are taught about airway clearance techniques but these can become very exhausting to do on a daily basis.

Alternatively, COPD patients can invest in something called a high-frequency chest wall oscillation vest. This looks just like a life jacket but it attaches to a machine that vibrates the vest at a high frequency. This causes the mucus in your chest to loosen, and after a few minutes, you can remove the vest and try a huff cough to expel the mucus. The main downside to these vests is that they can run you a pretty penny so it’s best to speak with your doctor before investing in one. What’s more, they aren’t very portable so you should plan to buy one for in-home use only.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Positive Expiratory Pressure Device
A positive expiratory pressure (PEP) device has a similar function to that of a high-frequency chest wall oscillation vest which we discussed above. However, the PEP device is much smaller and lighter so you can carry it in your purse, handbag, or pocket when you leave the house. With the PEP device, you will blow into a mouthpiece that creates air resistance. This air resistance will keep your airways open as you exhale meaning the mucus can move more freely without obstruction.

If you’ve ever tried the technique called pursed-lip breathing, you know what to expect with a PEP device. During pursed-lip breathing, you inhale deeply through your nose and then out through pursed lips. This helps to reduce chest tightness and get more air into your lungs. The PEP device makes this a little easier because you don’t have to control the amount of resistance so you can focus more on your breathing. PEP devices are also fairly cheap at around $30 to $50 apiece.
Mobility Devices
Words cannot express how important it is to maintain your mobility as you get older. Unfortunately, someone with COPD will likely begin to lose their mobility sooner than most due to reduced lung capacity, however, the good news is that there are plenty of mobility aids to keep you on your feet and moving. Probably one of the more popular mobility devices for people with respiratory ailments is a rollator. This is like a walker but it has wheels on the bottom and brakes so that you have better control. In the middle, there is a small platform where you can put your oxygen device your sit on if you get fatigued.

Another mobility aid that many COPD patients use is an electric scooter. These are best for people with very advanced lung disease who may not be able to walk more than a short distance on their own. Electric scooters offer a lot of storage room for your portable oxygen concentrator as well as personal belongings. However, the downside is that they need to be recharged after a certain amount of use and they are difficult to transport from place to place. Unless you have a caretaker who can help you out with these things, an electric scooter may not be the best option for you.

Last but certainly not least, there are in-home mobility devices like stairlifts. A stairlift is essentially an elevator designed for people who have trouble walking up and down the stairs. While these devices are very safe to use and can save you a lot of hassle, they are also pretty expensive because a professional will need to come to your home to install them. What’s more, they can wear out over time so you may need to call someone to have it repaired or replaced at some point.
Smartphone or Tablet
Most people have some type of smart device but for the few who do not, it’s worth upgrading, especially if you have COPD or another respiratory condition. Many portable oxygen concentrators like the Inogen One G5 and Caire FreeStyle Comfort make use of smartphone applications to enhance the user’s experience. These apps allow you to do things like track your oxygen usage, check the device user manual and even remotely check your oxygen flow and battery life.

There are many other applications that can make your life easier with COPD. For example, AirNow.gov has a mobile application that allows you to quickly and easily check the air quality in your area which is useful for planning trips. There are apps that can help you plan your diet and exercise routine with COPD as well. Be sure to check out this post where we take a look at some of the best mobile applications for COPD patients.
Conclusion
Being diagnosed with COPD can be life-changing. You’ll need to take steps to slow the progression of your disease like improving your diet, exercise routine, and taking regular trips to the doctor’s office. While this may seem overwhelming at first, it’s helpful to know that there are many resources at your disposal. Not least of which are devices like portable oxygen concentrators, nebulizers, and pulse oximeters. If you have any questions about what you read here, please don’t hesitate to leave a comment. If you’re on the market for a portable oxygen concentrator be sure to reach out to our respiratory specialists by phone or email.
.png)
With the advent of the novel coronavirus earlier this year, most people in the country have undergone drastic lifestyle changes in order to prevent putting themselves and others at risk. And while many businesses are beginning to open back up and we’re seeing things go back to normal, policies like “social distancing” and “safer at home” are likely to continue for quite some time.
Although these policies are intended to keep people safe, sometimes they can have the opposite effect. Spending too much time at home and away from people has well-documented adverse side-effects and some people are combating this by spending more time than normal outside exercising — this wouldn’t be a problem if it weren’t for the heatwave that’s currently spreading across much of the country.
Under normal circumstances, people could go to public areas like theaters or restaurants to seek relief from the heat, but instead, they’re being forced to choose between being cooped up in a non-air conditioned home or being outside under the hot sun. This issue is amplified for people with COPD and other chronic respiratory illnesses because the heat can lead to many different complications.
In order to help you prepare for the hot summer ahead, we’re going to give you 7 helpful tips for preventing heat-related COPD complications. If you still have concerns about coping with the change of weather, be sure to contact your doctor immediately to see if he/she has any additional recommendations for you. Remember that any changes to your treatment plan should first be approved by your doctor.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
How Heat Affects COPD
Your body works around the clock to maintain a normal temperature. The ideal temperature for most people is between 97°F (36.1°C) and 99°F (37.2°C), but it may vary slightly depending on the person’s age and gender. If someone’s body temperature goes above this threshold, it’s usually a sign of an infection, illness, or heatstroke.

When someone is exposed to high temperatures for prolonged periods of time, it can result in something called a heat injury. This may result in symptoms such as confusion, disorientation, and cramps. If the heat is sustained for long enough, it could result in serious health complications like heat exhaustion, heatstroke, or heat edema (swelling of the hands and feet due to water retention).
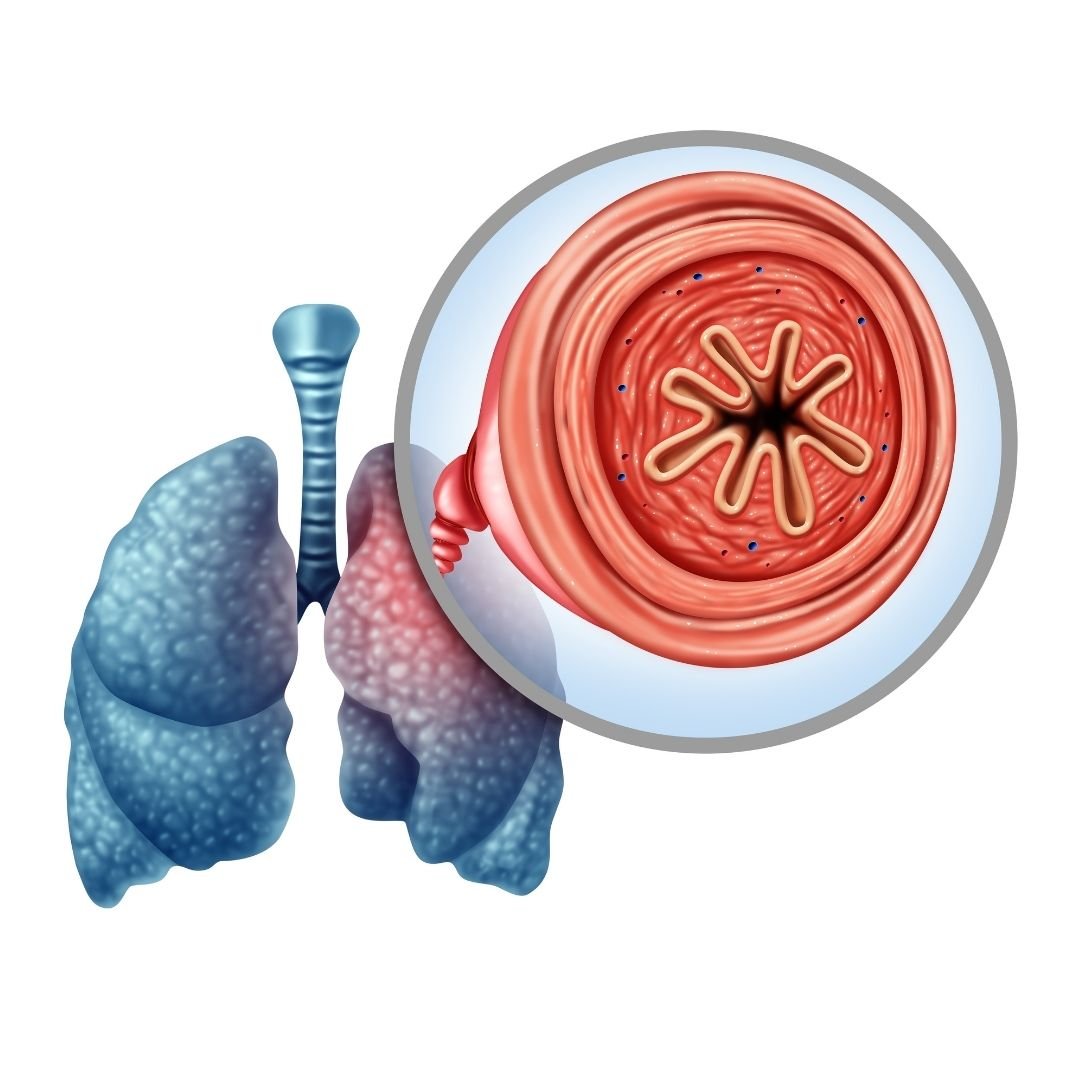
One heat-related illness that’s of particular concern to people with COPD is heat tetany. This refers to a short period of stress characterized by hyperventilation (breathing very heavily and quickly), respiratory problems, and muscle spasms as a result of heat exposure. This can even cause something called bronchospasm which is a sudden constriction of the muscles in the walls of the bronchioles in the lungs.

Another way the heat can affect your COPD is through high humidity which often accompanies it. If you’ve traveled to or live in the south, you’re probably well-acquainted with the feeling of being in a hot and humid climate, but the truth is, humidity can be found anywhere depending on the time of year. Humidity has some beneficial effects on the body, but due to its density, it can increase airway resistance and even make it harder for your body to stay cool making it a nightmare for anyone with COPD.
How to Prevent Heat-Related COPD Complications
Stay Hydrated
Proper hydration is one of the most important things you can do for your health and it’s especially important for COPD patients who live in a hot environment. COPD is characterized by excess mucus production which often becomes thick, sticky, and difficult to clear. If you’re dehydrated, it can make it even harder to remove this problematic mucus from the lungs and airways.

Another reason to stay hydrated is because water is the most important substance involved in maintaining our body temperature. When we start to overheat, our bodies secrete sweat which evaporates and lowers our body temperature. While more than half of the human body is water, we lose up to 3 quarts of water each day from breathing, urinating, and sweating, so it’s imperative that we drink enough to maintain every important function in the body.
Schedule Your Walks
Walking is one of the best exercises you can do for COPD. It helps to increase your pulmonary function, build muscles in your legs and arms and gives you the opportunity to practice your breathing techniques. However, walking outside during the hottest time of day can put you at a higher risk of experiencing a heat stroke or other heat-related injuries.

Fortunately, with some careful planning, you can be sure to avoid this. In the summer, the hottest time of day tends to be from noon to around 3 or 4:30, so it’s best to schedule your walks around this. Try to schedule your walks for early in the morning when the sun is up but hasn’t been out long enough for it to get too hot.
Another thing you should do is keep an eye on your local forecast. Although you can go for a walk when the skies are clear, it’s even better to go when there’s some cloud coverage. Clouds block a lot of the UV rays from the sun, especially the most harmful UV-B rays which put you at a lower risk of overheating or getting sunburned. However, you should still be sure to wear sunscreen every time you go out.

One final reason to schedule your walks is to avoid the busiest times of the day. As aforementioned, there are a lot of people outside trying to enjoy the nice weather. Some people are out mowing the lawn or doing other yard work which can cause a lot of allergens to mix into the air. You can also keep an eye on the pollen count forecast to avoid allergy triggers in your area. Ultimately, avoiding these airborne irritants will help you manage your COPD symptoms more easily.
Don’t Over Exercise
While exercise is a very important part of treating COPD, it’s also imperative that you learn to recognize the signs of overexercising. This is especially true when it’s so hot outside because it may happen a lot faster than you’re expecting it to. As a result, it’s a good idea to keep a close eye on exactly how much time you spend exercising.

According to the Cleveland Clinic, COPD patients should gradually work up to exercising around 30 minutes a day, at least three days a week. Exercise will help improve your circulation, strengthen your heart, lower blood pressure, improve COPD symptoms and much more.
If you enjoy exercising outside, be sure to check the weather at the beginning of the week and plan out what days and time you will exercise. It’s recommended that you follow each workout day with a day of rest, but if you need to workout two days in a row to avoid the heat, this can be considered too.
Another thing you should do is play it by ear. Heat exhaustion is characterized by fatigue, restlessness, dizziness, and muscle cramps. So, if you experience any of these symptoms throughout the week, it’s a good idea to change up your workout schedule in order to recover. If these symptoms continue, be sure to consult your doctor.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Change Your Wardrobe
Believe it or not, the clothes you wear can have a huge impact on your ability to stay cool on a hot day. First and foremost, you should wear loose-fitting clothing. Cotton t-shirts and shorts tend to be your best bet because they are lightweight, breathable, and won’t make you feel like you’re suffocating.

When it comes to footwear, sandals or a more breathable pair of tennis shoes are great options. Sandals are great if you don’t want to wear socks and retain extra heat. But if you want a little more arch support, you can wear a light pair of tennis shoes with thin socks.
To top off your wardrobe, try wearing a baseball cap or gardening hat which will help to keep the sun off your head, face, and neck. These areas tend to be the most vulnerable to heat injury and you’re more prone to feel delirious, noxious, or even lose consciousness if your head is exposed to too much sun and heat.

Keep an Ice Pack Handy
One simple way to keep cool during the summer is to keep an ice pack handy to lay on your skin if you feel like you’re overheating. It’s best to have multiple ice packs so that you can have a backup. Then when one melts, you can simply go to the freezer and swap it out with another one. If you don’t have an ice pack, you can fill a bag with ice and this will work just as well.

One thing to note before trying this is that ice can cause frostbite or ice injury if it’s applied directly to the skin for prolonged periods of time. This can lead to numbness, itchiness, or pain and can even lead to damaged blood vessels and reduced blood flow. To prevent this, try wrapping the ice pack or bag of ice in a cloth towel. Ultimately, the goal is to lower your body temperature slightly, you don’t want the ice to be so cold that it stings or causes numbness on your skin.

If you don’t have access to ice or ice packs, cold water can be an effective alternative. Simply rub some water on your legs, arms, chest, or face, and rather than wiping it off with a rag, let it evaporate off. If you do this too much, however, it could dry out your skin, so be sure to do it in moderation and keep some lotion handy to help your skin retain moisture.
Avoid Hot Foods and Beverages
While it may be tempting to indulge in burgers, hot dogs, or barbeque during this time of year, it’s generally best to avoid them if you want to keep your body temperature down. Hot foods and beverages are comforting all times of the year, but they don’t help when it comes to managing your body temperature and they can make COPD symptoms worse.
Another reason to avoid hot foods is because they can increase the temperature of your home. Running the stove or the oven for a long period of time not only raises the temperature in your kitchen, but it can raise the temperature of your whole home. If you’re looking for great food to eat in the summer, it’s better to reach for something like fruits or vegetables which tend to have high water content meaning they’re refreshing and they’ll keep you hydrated.

Hot drinks like coffee or tea are another thing to avoid this time of year. While this little boost of caffeine may help you wake up in the morning, there are better ways to do this that won’t have potential side-effects on COPD.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Quit Smoking Immediately
According to the Centers for Disease Control and Prevention (CDC), about 38 percent of COPD patients report being current smokers. This is astonishing considering that about 80 percent of deaths due to COPD could have been avoided without smoking. One thing that many people don’t realize is that smoking when it’s hot out may amplify the negative effects.

While hot weather and humidity can already put a lot of strain on your body, making it harder and harder to breathe, smoking increases your body temperature and irritates the airways which are already irritated. Smoking also alters mucus production in the body which could make it more difficult to clear respiratory irritants like pollen. It also gives you withdrawals which decrease your mood and make you less likely to follow through with your COPD treatment routine.
One of the main reasons people get back into smoking is out of boredom or they’re looking for quick relief from stress or anxiety. While smoking may seem like an easy solution, over time, it will only cause more harm than good. It’s understandable why someone would have a craving for cigarettes when they’re stuck at home, but the truth is, there are plenty of things to keep your mind busy without taking up smoking again. Check out this post where you’ll learn about 7 COPD-friendly activities to keep you busy during the quarantine.
![]()
Conclusion
Temperature and climate might not always be something you think about when it comes to managing a respiratory illness. However, according to the Environmental Protection Agency (EPA), there are 1,300 deaths per year due to heat-related illnesses and there are far more than that who are admitted to the hospital from things like heat stroke, heat edema, or heat exhaustion.
Unfortunately, due to the nature of chronic respiratory illness, COPD patients are much more likely to experience heat-related injuries. Follow some of the tips above to help you prepare for the heatwaves we’re experiencing across the country, and if you have any further concerns or you’re thinking about changing your treatment plan, be sure to reach out to your doctor or pulmonologist for guidance.
In the meantime, take some time to look at our portable oxygen concentrators. If you’re a COPD patient who loves to exercise, these devices will allow you to do so while maintaining your oxygen saturation and preventing COPD symptoms such as breathlessness, chest pain, and fatigue. Fill out the form at the side of the page and one of our respiratory specialists will reach out to you shortly.
Chronic obstructive pulmonary disease (COPD) is a term that categorizes a few chronic lung conditions: chronic bronchitis, refractory asthma, and emphysema all of these conditions restrict airflow in some way.
There are about 15.7 million people in the United States who have reported that they have been diagnosed with COPD. This is a progressive disease that gets worse overtime especially if the patient does not treat it properly.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Treating COPD is a lifelong journey comprised of doctors visits, respiratory tests, exercise, oxygen therapy, changing eating and drinking habits, and taking vitamins and supplements.
In this article we are going to focus on how COPD patients can develop a healthy eating habits and take vitamins and supplements in order to help ease the symptoms of COPD.
COPD Information
If you have COPD, it is likely that you find it increasingly difficult to breathe, and this can impact so many aspects of your life. The other symptoms you may experience are coughing, wheezing, excess mucus production, feeling of tightness in your chest, and fatigue.
COPD does not only affect your ability to breathe, but can cause a lot of other problems due to the lack of oxygen in your blood. Many COPD patients need supplemental oxygen therapy, and these patients have to use a device called a portable oxygen concentrator or an oxygen tank in order to get the right amount of oxygen. Oxygen will be prescribed to you if you need it.

In conjunction with your oxygen therapy, you can do a number of things to treat your respiratory condition, one of those treatments is eating healthy and getting the right amount of nutrition. If your diet doesn't give you the vitamins and nutrients you need, it could be helpful to take supplements and vitamins that would support any deficiencies you may have.
Nutrition and Eating Healthy for COPD

Nutrition is a crucial part of treating COPD, and oftentimes one of the hardest things to keep up with, vitamins and supplements can help you get the nutrients your diet is lacking or important vitamins that your body is craving.
Vitamins and minerals give you energy and stamina, and you get vitamins form food and water, if you are not eating the right foods, you may have vitamin deficiencies. If you have COPD, it is likely that you require 430–720 more calories per day than healthy people.
Calories are the fuel that gives your body energy to function. You can get healthy calories from grains, vegetables, fruits, proteins, and fats you eat. COPD patients often require these extra calories because of the added effort they need to breathe. Therefore, malnutrition is also something many people with COPD struggle with. Malnutrition can affect you for a long time, and can negatively impact your disease progression.
It is recommended that eating a high fat, low carbohydrate diet can help people with breathing problems.
Best Eating Habits for People with COPD

Building healthy eating habits is an essential part of treating your COPD. Many people with COPD do not have an appetite or have a hard time finding the energy to cook and eat, and therefore suffer from malnutrition. Follow these following tips to make eating easier.
- Try making food easier to chew, you can do this in a number of ways. When you are cooking vegetables, cook them fully until they are soft. You can mince or grind the meat down and make bowl styled dishes. You can also focus on eating foods that are already easy to chew like pasta, mashed potatoes, thick soups, creamed soups, and casseroles fruit smoothies.
- If you feel short of breath while you are eating you should try to rest 30 minutes before meals. Start practicing pursed-lips breathing and other breathing exercises daily that will improve your breathing endurance.
- While you eat, make sure your body is in a position to expand your lungs, try sitting upright and lean forward with your elbows on the table and keep your feet on the floor.
- Ask your healthcare provider, if you are using a pulse flow oxygen device or a continuous oxygen device, if you should increase your flow rate during meals but do not adjust your oxygen flow without talking with your doctor first.
- Eating and cooking can be exhausting for lung patients, to avoid fatigue, try the “Meals on Wheels” in your community or a similar service that will provide you with nutritious, low-cost meals. By using a service like this, you won’t have to prepare meals.
- Eating too much too often will make you feel tired, instead try eating six small meals each day instead of three big ones. This will also keep your metabolism from slowing you down. The key to maintaining energy throughout the day is to conserve oxygen, and digestion takes up your energy and therefore takes up your valuable oxygen. If you eat smaller meals, you use less oxygen.
- If you enjoy cooking, try to find easy-to-make recipes, and if you don’t enjoy cooking as much, ask family or friends to help with making meals. Even though sugar can sometimes give you a small burst of energy, sweets, cookies, cakes, and other deserts, also known as simple carbohydrates will hold carbon dioxide inside of you causing tiredness.

- Bloating is extremely uncomfortable for lung patients because your stomach is pushing on your diaphragm making it even more difficult to breathe. To avoid this bloating feeling, do not rush your meals, and no not eat when you are short of breath, by doing so, you can simultaneously swallow air making your bloating worse.
- Spread out the amount of fluids you drink, and try drinking one hour before and one hour after a meal in order to decrease the amount of stuff in the stomach at one time.
- Onions, cabbage, sauerkraut, broccoli, Brussels sprouts, and beer all cause bloating, so try to avoid these foods when you can. Fried, fatty food and other high-fat foods are hard to digest and can only be processed in your body very slowly slowly, causing a feeling of bloating.
- Lactose may cause bloating, if you feel bloated after eating or drinking milk, yogurt, cottage cheese, or other dairy products, try avoiding dairy.
- By adding lots of fiber and fluid to your diet you can avoid constipation and bloating.
Supplements and Vitamins

Beyond developing a healthy respiratory diet that works to mitigate your COPD symptoms and helps give you energy, there are also many different supplements and vitamins that you can try to support your medical treatment and help manage your symptoms.
Various vitamins (vitamin C, D, E, A, beta and alpha carotene) can help improve COPD symptoms, exacerbations and pulmonary function and high vitamin intake would probably reduce the annual decline of FEV1.
Vitamins you Need if you Have COPD

COPD flares or exacerbations are episodes of escalated symptoms. When you experience a flare up, you may need to use your rescue inhaler or medication, increase the oxygen output on your portable oxygen concentrator if your doctor recommends it, and in some cases seek emergency medical attention.
In order to avoid COPD exacerbations all together you can do a number of things:
- Take your oxygen as prescribed everyday
- Practice breathing exercises to increase your endurance
- Avoid allergens
- Avoid chemicals and harsh cleaning product
- Avoid bad air quality, and get a home air purifier
- Exercise regularly
- Eat a respiratory friendly diet as mentioned in the beginning on this blog
- Take supplements and vitamins that are good for your health
LPT medical has a COPD resource center on our website where you can go to find information regarding all of these actions you can take to avoid COPD exacerbations and how to take the best care of your condition.

Continue reading this blog for information about how certain supplements can help improve your condition.
Vitamin D
Research shows that many people with COPD also have very low vitamin D, therefore taking vitamin D supplements can help your lungs function better.
The main reason people with COPD can have Vitamin D deficiencies is due to the lack of sun contact, resulting in lack of vitamin D production in skin.
Taking vitamin D-3 supplements for COPD can help protect you from experiencing moderate or severe flare-ups.
Vitamin C
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Research shows that having low levels of vitamin C can lead to symptoms like shortness of breath, mucus, and wheezing, all of which are already symptoms of COPD, and avoiding excess
Vitamin E

Vitamin E is important for your vision, reproduction, your blood, brain and skin.
Studies have shown that long-term use of Vitamin E can help prevent COPD because it has antioxidant properties, which may protect your cells against the effects molecules that are produced when your body is exposed to tobacco smoke and radiation.
If you experience consistent flare-ups of COPD, it is likely that you have lower levels of vitamin E than normal. Taking a vitamin E supplement can help your body get back to normal vitamin E levels.
Vitamin A

Vitamin A is crucial to the functioning of your immune system and plays a vital role in your cells to growth. Taking Vitamin A supplements may help you lungs function at a high capacity if you have a vitamin A deficiency.
Magnesium
Some COPD medications can interfere with your body’s ability to absorb magnesium, this can be harmful for COPD patients because magnesium supports lung function. Taking a magnesium supplement could cause side effects. If you do take magnesium supplements be sure to monitor yourself carefully.
Calcium

There are some COPD medications that may cause you to lose calcium and calcium can help your lungs function. You should try to intake more calcium-rich foods in your diet and if you are still unable to reach your calcium requirements, it may be necessary to take a calcium supplement.
Omega-3 fatty acids

Omega-3 fatty acids can reduce the inflammation in your lungs from COPD. You can eat more fish, seeds, and nuts, to get Omega-3 fatty acids, but you can also take fish oil supplements to make sure that you are getting enough.
Overview
COPD is a chronic illness, and there is no cure, however you can treat your disease. If you maintain a strict COPD treatment regimen you can regulate you symptoms. By taking your medication, adhering to your oxygen prescription, eating healthy and getting the nutrients you body needs you can slow down the progression of your COPD.
If you have issues eating, and find it hard to maintain a healthy diet, we hope that you found some of the ideas listed in this article that will help you get the nutrients you need in order to help relieve your COPD symptoms.
If you have COPD it is likely that your body is lacking in vitamins you needs, and if you are experiencing certain signs of vitamin deficiencies, you should speak with your doctor about taking specific supplements.
Getting the right amount of nutrients and taking supplements can help you better manage you COPD symptoms and helps you body function optimally.
If you learned anything in this blog, or feel as though someone in you life could benefit from any of this information, please leave a comment or share this blog with your friends and family!
Having a dry mouth is a symptom that many COPD patients experience, although it is often overlooked. Compared to more visible or more serious ailments, like coughing and shortness of breath, many patients consider their dry mouth symptoms to be low priority or never bring them up with their doctor at all.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
However, a dry mouth is an extremely uncomfortable symptom, and it is likely to only get worse if you leave it untreated. If ignored for too long, it can even lead to more serious problems like gingivitis, oral thrush, and tooth decay.
That's why in this post we're going to show you what to do if you experience a dry mouth because of your COPD. We'll introduce you to a variety of products and techniques that can treat dry mouth symptoms and show you how to prevent them from returning in the future.
If you or someone you know is suffering from a dry mouth, then this guide will give you the tools you need to track down both the cause and the solution. A dry mouth can happen for a variety of different reasons, and by better understanding the causes and potential treatment options you'll be much more likely to find a solution that works effectively for you.
Dry Mouth Symptoms
The clinical term for a dry mouth is xerostomia, and it happens when your mouth can't produce enough saliva to keep itself moist. It can happen for a variety of reasons, including stress, breathing through your mouth, and taking certain medications.
COPD patients are particularly likely to get a dry mouth as a result of COPD medications and symptoms. It's nothing to worry about if it only happens every once in a while, but you'll need to find a solution if it happens more often than that.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Having a dry mouth can make a variety of things difficult, including eating, chewing, and swallowing. A dry mouth can also make it difficult to talk or make your voice sound scratchy and hoarse.
A dry mouth is often accompanied by a dry throat, nose, or sinuses. This can cause the lining of your nose and upper airways to become irritated and sore, and even lead to nosebleeds and infections.
Here are some of the common symptoms of dry mouth (xerostomia):
- Dry or sticky feeling in your mouth
- Thick, stringy saliva
- Dry tongue
- Dry or sore throat
- Hoarse voice
- Trouble chewing, swallowing or speaking
- Changes in your ability to taste food
- Problems with dentures
Risks and Complications of Not Treating Dry Mouth

Having a dry mouth is more than just unpleasant; it can actually be bad for your health. If it happens frequently, it can cause a variety of other symptoms in your mouth, nose, and throat.
That's why it's important not to ignore dry mouth symptoms if they don't go away quickly on their own. Left untreated, a dry mouth can accelerate tooth decay and lead to other infections and problems.
Tooth Decay
To stay healthy, your mouth should produce enough saliva to stay moist all of the time. However, when you are sick, take certain medications, or suffer from a respiratory disorder like COPD, it can dry out your mouth so much that your saliva glands can't keep up.
This is bad for your oral health, because saliva plays an important role in keeping your teeth and gums clean. It washes bacteria and food particles off of your teeth and has anti-bacterial and anti-fungal properties.
Keeping your mouth moist prevents bacteria from taking hold and prevents tartar build-up on your teeth. If not managed effectively, having a frequent dry mouth leads to tooth decay and cavities.
Mouth Infections and Gum Disease

If left untreated for too long or not properly managed, a dry mouth can lead to bacterial and fungal infections in your gums and other surfaces in your mouth. This can cause your gums to become inflamed, leading to gingivitis and full-blown gum disease.
Symptoms of gingivitis include swollen, sensitive or bleeding gums, bad breath, and pain when you chew. If you experience any of these symptoms along with a dry mouth, you should go see your dentist right away.
A dry mouth can also allow fungus to flourish in your mouth, causing a yeast infection known as candidiasis or oral thrush. Thrush appears as white patches on your tongue, throat, and roof of your mouth.
A dry mouth can also cause sores by leaving you vulnerable to bacterial infections on the surface of your mouth. It can also cause your lips and the skin around your mouth to crack, which is painful and puts you even more at risk for infection.
What is Causing Your Dry Mouth?
Many COPD patients suffer from a dry mouth for a variety of different reasons. Many COPD symptoms can dry out your mouth and throat, as can many different medications used to treat COPD.
If you know what is causing your dry mouth, then it will be easier to find an effective solution that can treat it. To help you understand the cause of your dry mouth, let's take a look at some of the different ways that living with COPD can dry out your mouth and throat.
COPD Medications

Many of the medications used to treat COPD can cause your mouth to get dry. It is a common side effect of inhalers, steroids, and several other drugs used to manage COPD symptoms.
Short-acting bronchodilators are one of the worst culprits and one of the biggest medicinal causes of dry mouth in people with COPD. Most people with COPD have to take bronchodilator medications via an inhaler at least once a day to keep their airways open and their symptoms under control, which can leave them with uncomfortable dry mouth symptoms every day.
Many COPD patients also use steroid inhalers to treat inflammation and prevent exacerbations. Steroid medications are known to dry out your mouth, especially when you take them with an inhaler.
Along with a dry mouth, steroid inhalers, bronchodilator inhalers, and especially combination inhalers (steroid plus bronchodilator) can cause throat irritation, hoarseness, and complications like yeast infections and cavities. If you have COPD, it's important to know how to manage these and other dry mouth symptoms to avoid permanent damage to your oral health.
Another medication many COPD patients take frequently is antibiotics, which are used to treat COPD exacerbations and treat infections in the lungs and upper airways. Many antibiotics can also cause dry mouth symptoms, including Azithromycin, a common antibiotic used to treat COPD.
Luckily, most courses of antibiotics are short, so even if you experience a dry mouth, you shouldn't have to manage it for more than a week or two. However, you should talk to your doctor anytime you experience side effects from your medications, including dry mouth. Your doctor may even be able to give you a slightly different medication to see if your symptoms improve.
Other Medications

Many other medications can also cause a dry mouth, including antidepressants, antacids, quit-smoking medications, and anti-inflammatory drugs. While these drugs are not necessarily COPD medications, they are frequently used by people with COPD to treat other conditions and complications related to or worsened by their disease.
Oxygen
Supplemental oxygen is also a medication, but it deserves a category of its own for its role in causing dry mouth. The majority of oxygen patients suffer from mouth and throat dryness occasionally, and, for some patients, it's a constant struggle to keep their mouth from getting dry.
Often, mouth dryness comes from having a continuous flow of oxygen forced through your mouth and throat, which can dry up the saliva in your mouth after a while. Pulse-flow oxygen is less harsh and less likely to dry you out, but many patients are unable to use pulse-flow technology to meet their oxygen needs.
You are more likely to experience a dry mouth while using oxygen at night, especially if you sleep in a dry room or breathe through your mouth when you sleep. Your mouth and throat are especially likely to get dry if air has an opportunity to leak out of your mouth or nose. This can happen if your oxygen mask doesn't form a tight enough seal or if your mask uses a pillow cushion under the nose.
Using a CPAP or BiPAP machine to treat sleep apnea can have the same drying effect as using supplemental oxygen. Since many people with COPD also have sleep apnea, this is a common cause of dry mouth in COPD patients.
COPD Symptoms That Cause Dry Mouth
COPD wreaks havoc on your respiratory system, causing a variety of uncomfortable symptoms, including a dry mouth. Whenever you have a bout of coughing, wheezing, or shortness of breath it can leave your mouth and throat feeling scratchy and dry.
Your mouth and throat are integral parts of your respiratory system and get directly affected by the conditions in your airways. And as an entry point through which air enters your body, it is one of the parts most affected when you breathe in dry, irritating air.
Whenever you experience a flare-up or exacerbation, it can make a dry mouth even worse, and put you at a higher risk of illness and infection. That's why you should avoid allergens, germs, and respiratory irritants like perfumes and air pollution that could make your symptoms worse.
Here are some of the symptoms and conditions that can cause a dry mouth with COPD:
- Coughing
- Wheezing
- Mouth breathing
- Flare-ups and exacerbations
- Exposure to dry air
- Exposure to smoke, pollution, and irritating particles
- Exposure to allergens, mold, and dust mites
Solutions to Treat a Dry Mouth
Make Adjustments to Your Oxygen Delivery System
The best way to treat a dry mouth is to treat the underlying problem. For many people with COPD (but not all), the main underlying cause of mouth dryness is supplemental oxygen therapy.
Luckily, there are a variety of things you can do to minimize dryness from oxygen therapy and make it more comfortable for your mouth, nose, and throat. These include things like using the right kind of oxygen mask or nasal cannula and getting a humidifier for your oxygen device.
Get a Humidifier Bottle for Your Oxygen Delivery System or CPAP/BiPAP Machine

If you use supplemental oxygen, then you know that the flow of air from your oxygen delivery device can severely dry out your mouth and throat. Higher oxygen flow rates tend to cause worse dryness and may even irritate your lungs and airways.
That's why many oxygen patients get a humidifier bottle to attach to their oxygen delivery system. All you have to do is fill it with distilled water and connect it to the tubing to bubble the air from your oxygen source through. This moisturizes the air to make it less dry by the time it reaches your mouth or nose.
If you experience a dry mouth, nose, or throat more than occasionally while using oxygen, talk to your doctor about getting a humidifier to attach to your oxygen delivery device. However, whether or not you can use a humidifier may depend on your personal oxygen requirements, and it won't work with pulse flow oxygen.
You can also get a humidifier for your CPAP or BiPAP machine if you use one to treat sleep apnea. Talk to your doctor about getting a humidifier for your machine if you often find yourself waking up with a dry mouth or throat during the night.
Using a humidifier bottle can make a huge difference in your comfort and dry mouth when you use oxygen. To learn more about how to make supplemental oxygen more comfortable, visit our previous post here.
Don't Let Your Oxygen Mask Leak

If you have a humidifier for your oxygen but still experience a dry mouth or throat, then it could be because your oxygen mask is leaking. If there is a gap between the edges of the mask and your skin, it allows the humid air from your oxygen supply to escape while letting dry, outside air in.
This can cause severe dryness and is most likely to happen if you use a nasal pillow mask or a mask that doesn't fit correctly. In that case, you may need to replace your mask with one that fits your face better and doesn't allow air to leak out.
Get a More Comfortable Oxygen Mask or Nasal Cannula
Sometimes you can reduce mouth, throat, and nasal dryness from oxygen therapy just by using the right kind of nasal cannula or mask. For example, you can get high-flow nasal cannulae that help by simply reducing the speed at which the air rushes into your nose.
Nasal cannulae and masks come in a wide variety of designs and materials you can choose from. You might have to try out a few different types before you find the one that's most comfortable and convenient for you.
Using the right mask can make all the difference in how comfortable oxygen therapy is and how dry your mouth, nose, and throat feel. To learn more about all the different options for oxygen masks and nasal cannulae, visit our previous post here.
Rinse Out Your Mouth

When your mouth is dry, simply rinsing it out with water once every hour or two can help you keep it moist. You can rinse your mouth out with plain tap water or use a solution of water with added salt or baking soda, if you like.
You can also use oral rinses like Biotene mouth wash whenever your mouth feels dry. These rinses add extra moisture and protect your teeth from harmful bacteria and fungi.
Some oral rinses can even soothe your mouth if it's irritated or strengthen your teeth to fortify them against bacteria and decay. However, it's important to find a mouthwash or oral rinse that is alcohol-free, because alcohol can irritate your mouth and dry it out even more.
Here is a list of some alcohol-free mouth rinses you can use to treat a dry mouth:
- Biotene Mouthwash (made by GSK)
- Oasis Moisturizing Mouthwash (made by GlaxoSmithKline)
- Eco-DenT Ultimate Natural Daily Rinse (made by Eco-DenT)
- Crest Pro-Health Rinse (made by Procter and Gamble)
Use Saliva Substitutes and Oral Gels
There are a variety of saliva substitutes and oral gels on the market that you can use to moisturize your mouth when it gets dry. While they only provide temporary relief from dryness, they tend to be more effective than simply rinsing your mouth with water or mouthwash.
Saliva substitutes mimic the salinity and acidity of natural saliva and come in sprays and liquid solutions. You can buy them over the counter at most drug stores, although you may need to ask a pharmacist for help hunting them down.
You can use your saliva substitute as often as you like throughout the day as long as you have permission from your doctor. However, you are not supposed to eat or drink for fifteen minutes after use.
Oral gels use a special gel solution to lubricate the inside of your mouth and are also available over the counter. Oral gels are great for sealing in moisture and can last for up to four hours after application.
Here is a list of oral gels and saliva substitutes you can use to treat dry mouth:
- Biotene Oral Balance Moisturizing Gel and Dry Mouth Liquid (made by GSK)
- Mouth Kote (Parnell Pharmaceuticals)
- Oasis Moisturizing Mouth Spray (made by GlaxoSmithKline)
- Saliva Substitute (made by Roxane Laboratories)
- Sprey Rain Oral Mist Spray (made by Xlear)
Get Prescription Medication

There are a couple of prescription-only medications that can stimulate extra saliva production and relieve dry mouth symptoms. However, these medications, called secretogogues, are usually only available for patients with chronic, severe dry mouth caused by head and neck radiation therapy.
However, if you experience a frequent dry mouth from oxygen therapy or other medications, you should still talk to your doctor to see if you have any prescription medication options. If your dry mouth is severe and poses a threat to your oral health, your doctor may consider prescribing you a saliva secretogogue medication.
If your dry mouth is causing a bacterial or fungal infection, your doctor or dentist may also prescribe you an antibacterial or antifungal medication. These types of infections are more common when you don't have enough saliva to neutralize bacteria and fungi in your mouth.
Rinse Your Mouth After Using Your Inhaler

Whenever you use an inhaler, you should always rinse out your mouth immediately afterward. Most inhalers include this as part of their instructions, but many patients ignore this step or get lazy over time.
Some studies show that only about half of the medication you inhale ends up actually making it to your lungs and airways; the rest ends up coating your mouth. That's why rinsing your mouth out after using your inhaler is so important, especially if you use it every day.
Swishing water around your mouth removes the residue of the medication, which is what causes dry mouth when you use your inhaler. Washing it off helps your mouth stay moist and prevents cavities, oral thrush, and bacterial infections like gingivitis.
However, you have to remember to rinse your mouth out immediately after you use your inhaler in order for it to be effective. Studies show that putting it off for even one minute gives the medication enough time to absorb into your mouth, causing dryness and other complications.
Use Moisturizers and Creams

While these aren't for your mouth exactly, moisturizers and creams are a godsend for chapped lips and skin. After all, if your mouth is dry and dehydrated, there's a pretty good chance that your skin and lips are on the dry side, too.
Oxygen therapy, in particular, can cause your lips and the skin around your mouth to get dry, irritated, and cracked. Luckily, all it takes is regular moisturizer application to keep your skin smooth and moist.
Since oxygen is highly flammable, oxygen patients should always avoid using chapsticks and moisturizers that contain petroleum, which is also a very flammable substance. Instead, you should only use water-based lubricants and lip balms when you use supplemental oxygen.
If you don't use oxygen, then you are free to use whatever kind of skin or lip moisturizer you prefer. However, moisturizing creams tend to be thicker and work better than lotions, and simple petroleum jellies like Vaseline work exceptionally well for chapped lips and skin.
You can also use water and petroleum-based lubricants to lubricate the outside of your nose and just inside your nostrils if they get dry. If you experience nasal dryness, a saline nasal spray or nasal gel can give you temporary relief.
If you use supplemental oxygen, Surgilube is a great water-based lubricant used by many oxygen patients and hospitals. It's an inexpensive, all-purpose lubricant that can come in handy for a variety of moisturizing needs.
Make Hydration a Priority

Dehydration is a common problem in people with COPD, and it can cause your mouth to dry out, too. Even if your dry mouth is caused by a medication or any other reason, getting dehydrated can make it much worse.
If you struggle with a dry mouth often, then you should be making drinking enough water a top priority in your daily routine. Not only will it help with your dry mouth, but it can reduce a variety of symptoms caused by COPD.
However, it can be difficult to remember to drink enough water throughout the day, even if you know that it's a healthy thing to do. Fortunately, there are plenty of tried-and-true ways to help yourself build healthy hydration habits.
Use Water Bottles

Supplemental oxygen therapy, or simply oxygen therapy, is a treatment that has been around since the late 1800s. It was primarily used to treat the symptoms of pneumonia, but doctors were uncertain how much to administer, how long to keep patients on oxygen, and if there were any serious side-effects. It wasn’t until the late 1900s that there was a significant amount of research on the use of medical oxygen and doctors became more aware of how to use it.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
But the usage of medical oxygen is not the only thing that developed over this time. There were also a number of scientific advancements that revolutionized the way oxygen was administered. For example, the invention of the lithium-ion battery in 1991 made it possible for oxygen manufacturers to produce extremely small, lightweight, and powerful oxygen devices called portable oxygen concentrators. These devices replaced the heavy and bulky oxygen tanks that came before them.
In this post, we’re going to help you understand supplemental oxygen better by outlining some of the conditions that may require its use. Remember that oxygen is a controlled substance in the United States, so if you believe you may need it for medical purposes, you’ll need to get a prescription from your doctor first. If you have one of the following conditions, reach out to your doctor to find out what your oxygen requirements are. Then you can look into the various oxygen devices on the market.
Chronic Obstructive Pulmonary Disease (COPD)
COPD is probably the first condition you think of when you hear the words “supplemental oxygen.” Not only because most COPD patients are on oxygen, but because COPD is one of the most common chronic respiratory conditions in the world. According to the Centers for Disease Control and Prevention (CDC), there are around 16 million people with COPD in the United States alone. Worldwide, there are more than 65 million people with COPD.

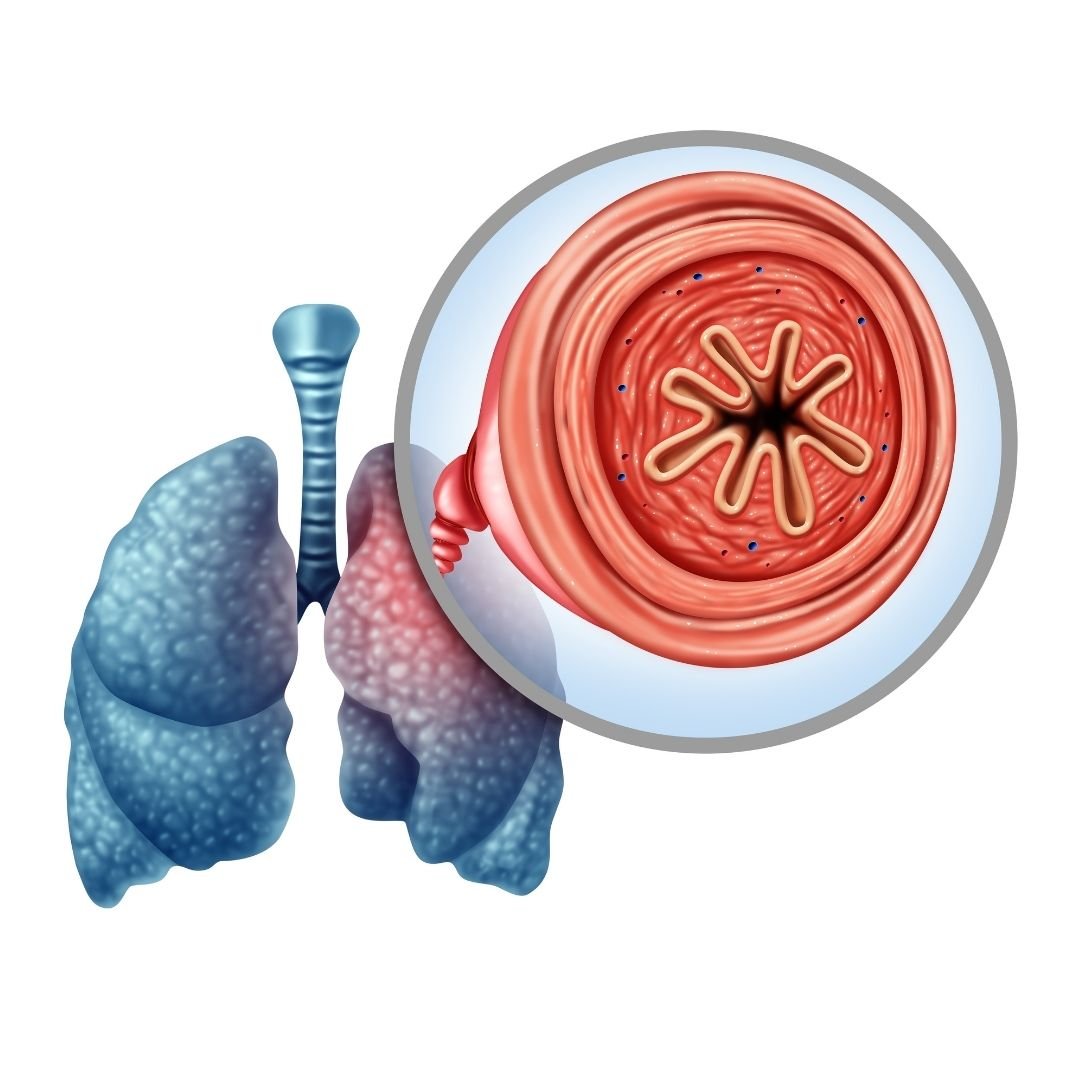
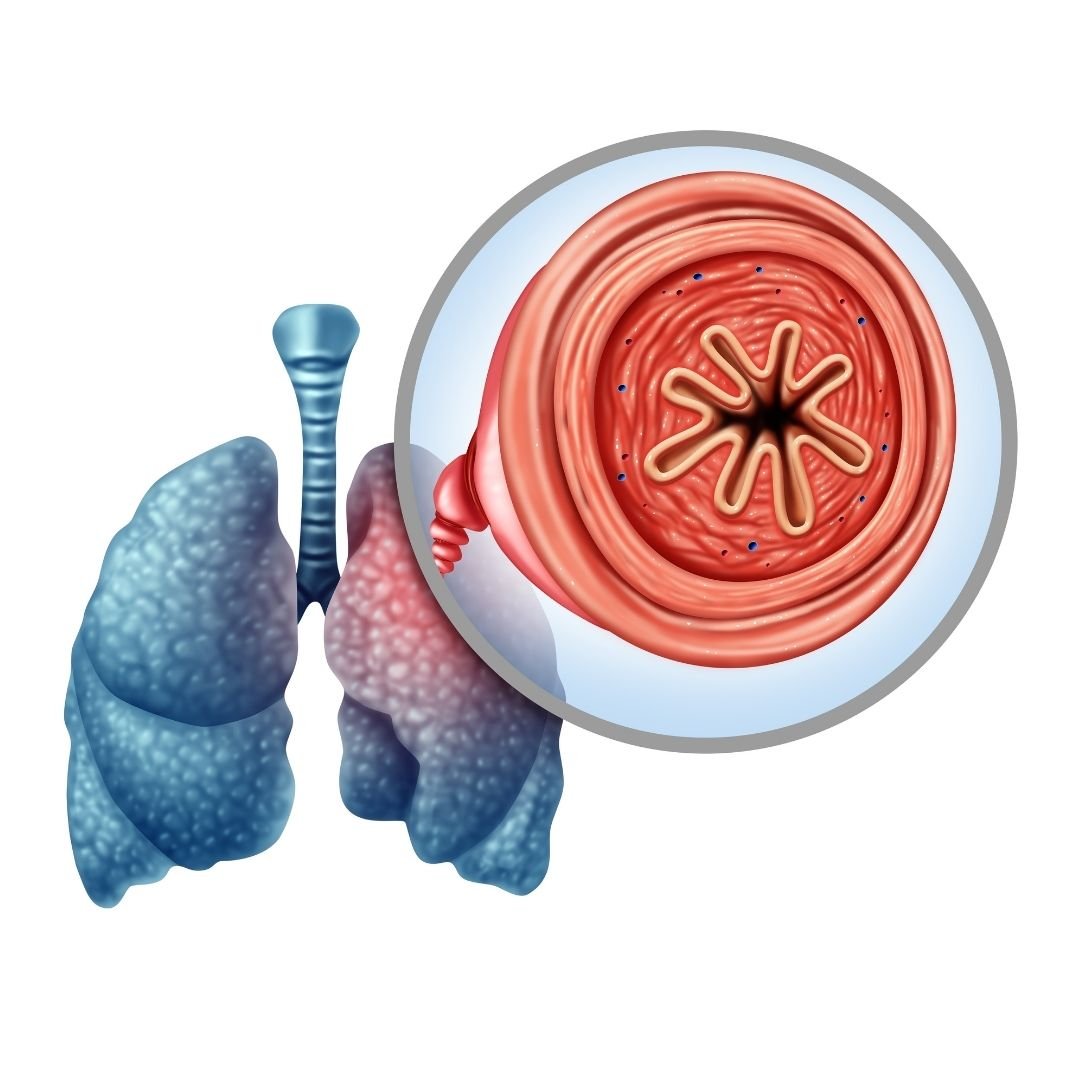
COPD is actually an umbrella term that denotes two separate but similar diseases: chronic bronchitis and emphysema. The former is a disease that affects the airways leading to the lungs called bronchioles. These airways become inflamed and hardened making it difficult to breathe and to clear mucus out of the lungs and throat. Trapped mucus can lead to frequent and recurring lung infections. Chronic bronchitis differs from acute bronchitis in that the damage is permanent and irreversible.
Emphysema, the other condition under the COPD umbrella, is characterized by damage to the alveoli. These are the tiny air sacs in the lungs where the exchange of oxygen and carbon dioxide takes place. When lung damage occurs, usually due to cigarette smoking or the inhalation of air pollution, the alveoli begin to swell and fill with fluid. This makes the lungs much less efficient at transferring oxygen to the blood and the lungs also become less elastic meaning it’s physically harder to breathe.
When is Supplemental Oxygen Needed?
COPD is a disease that develops slowly over the course of many years. In fact, the disease is divided into four different stages, each marked by progressively worsening symptoms. Stage one COPD is very mild and may even go unnoticed by the patient. Many people ignore the signs of stage one COPD because they simply view it as a sign of aging. According to COPD.net, it’s estimated that about 12 million people have COPD that has not been diagnosed. Most of whom are in stage one COPD.

What this means in terms of supplemental oxygen is that most people will not need it during the early stages of the disease. However, as your symptoms progress, you’ll need to communicate closely with your doctor so that he or she knows when it’s best for you to begin oxygen therapy. Before giving you a prescription for oxygen, your doctor will likely perform a test called an arterial blood gas analysis (ABG test). This test will tell you and your doctor the amount of oxygen and carbon dioxide in your blood so that you can determine if supplemental oxygen will benefit you or not.

Since arterial blood gas analysis requires you to draw blood, there is another less invasive option called pulse oximetry. A pulse oximeter is a small device that slips over your finger. It passes rays of light through your finger in order to approximate your blood oxygen saturation levels. While these tend to be less accurate than ABG tests, they can be extremely convenient, especially for checking your oxygen levels at home without the help of a doctor.
Cystic Fibrosis (CF)
Cystic fibrosis is a disease that’s characterized primarily by damage to the lungs and digestive system. It’s a hereditary condition meaning that it’s passed on from parents to their offspring. Around 75 percent of people diagnosed with CF are diagnosed under the age of two. This is in stark contrast to COPD where most cases are diagnosed in patients over the age of 40. According to Medical News Today, all newborns in the United States are screened for cystic fibrosis.
Cystic fibrosis patients have a mutation in the gene that creates the cystic fibrosis transmembrane conductance regulator (CFTR). This is a protein that helps regulate fluids and salt throughout the body. This is why CF patients often struggle with overproduction of mucus and sweat inside and outside their body which can lead to blockages and frequent infections, especially in the lungs and the digestive tract. Like COPD, CF is a progressive disease meaning there is no cure and will likely get worse without effective treatment.
When is Supplemental Oxygen Needed?
Supplemental oxygen therapy is a very common treatment option for cystic fibrosis patients. Unfortunately, since cystic fibrosis is so rare, there are far fewer studies to go off of when determining if supplemental oxygen is right for each patient. However, clinical trials have shown that oxygen therapy can stabilize CF and allow patients to sleep better, exercise effectively, and maintain an otherwise normal life. But since CF causes thick mucus, treating this disease is usually focused on reversing these effects. So, mucus thinners are usually the most important treatment option for CF patients.
.png)
Supplemental oxygen can be prescribed for either short- or long-term use in cystic fibrosis. If the patient is experiencing chronic low blood oxygen levels, you might be required to use oxygen for several hours a day or more. On the other hand, if your low blood oxygen levels are intermittent and caused by things like flare-ups you might be prescribed the use of oxygen only when your respiratory symptoms are elevated.
Pulmonary Fibrosis (PF)
Pulmonary fibrosis is a condition that is commonly confused with chronic obstructive pulmonary disease, but they are not the same thing. While they certainly exhibit some of the same symptoms, they differ greatly in terms of what causes them, the type of damage that’s done to the lungs, and the long-term outlook for patients. Like the name suggests, COPD is an “obstructive” disease. This means that it impairs your ability to expel air from the lungs. Pulmonary fibrosis, on the other hand, is a restrictive lung disease meaning it prevents the lungs from fully expanding.
Another difference between the two is that COPD results in inflammation in the lungs due to exposure to cigarette smoke whereas pulmonary fibrosis is characterized by fibrosis or “scar tissue” in the lungs from years of exposure to pollution. In COPD, the airways become narrowed preventing you from expelling air and leading to a buildup of carbon dioxide in the blood. In pulmonary fibrosis, the lungs themselves may be stiff or too weak to inhale and exhale fully. On the surface, these things are indistinguishable, but there are some significant differences in the way they are treated.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Whereas COPD is mainly caused by cigarette smoking or alpha-1 antitrypsin deficiency, there are many potential causes of pulmonary fibrosis. Idiopathic pulmonary fibrosis (IPF) is the most common type. The term “idiopathic” simply means that the disease developed with no known cause. IPF is most common among people between the ages of 50 and 70. Pulmonary can be caused by other diseases, most commonly autoimmune diseases like rheumatoid arthritis, Sjogren’s syndrome, or scleroderma. Gastroesophageal reflux disease (GERD) and viral infections can also lead to an increased risk of contracting pulmonary fibrosis.
There is also a genetic component to cystic fibrosis. Studies have shown that genes play a role in determining whether someone contracts pulmonary fibrosis. But more research is needed to say exactly how it contributes. Pulmonary fibrosis that is believed to have genetic cause is referred to as “familial PF.”
![]()
Lastly, pulmonary fibrosis can be caused by exposure to hazardous materials. Occupational hazards like silica and asbestos are most likely to cause PF. It can also be caused by radiation treatments and certain types of medications. Cigarette smoking is not a cause of pulmonary fibrosis but it can be a risk factor meaning it makes someone more likely to contract pulmonary fibrosis.
When is Supplemental Oxygen Needed?
As you can imagine, prescribing supplemental oxygen for pulmonary fibrosis can be a little more challenging than with other conditions. There are many different causes of fibrosis in the lungs so it’s more difficult to determine if additional oxygen is needed. Regardless, supplemental oxygen is still widely in use by people with pulmonary fibrosis and many people say that it helps them live an active lifestyle and feel better in their day-to-day lives.

According to UCSF Health, pulmonary fibrosis patients need oxygen when their saturation falls below 89 percent or arterial oxygen pressure falls below 60 mmHg. This is regardless of whether the patient is at rest, active, or asleep. Oxygen is a vital resource for your body and it’s used by every organ in the body so maintaining the proper oxygen levels in the blood at all times can go a long way towards preventing pulmonary fibrosis symptoms.
Severe Asthma
Asthma is the world’s most common respiratory condition. According to the Asthma and Allergy Foundation of America, 7.7 percent of American adults and 8.4 percent of American children have it. The number of people who have it has also been increasing since the 1980s likely due to an increase in environmental pollutions like airborne pollens, car pollution, and even changes in the climate.
Asthma is a condition where a patient’s airways become narrowed, inflamed, and filled with mucus which makes it difficult to breathe as well as causing chest pain and fatigue. While COPD and asthma attacks are very similar events, the main difference between the two is that asthma is not a progressive disease so the airways typically go back to normal after an attack rather than becoming increasingly more inflamed like they would in a COPD patient. Asthma is also not caused by smoking, however, it is a risk factor.
-jpg.jpeg)
The good news when it comes to asthma is that only about 5 to 10 percent of cases are severe and life-threatening. The majority of asthma patients find themselves limited in their exercise ability and they might experience more frequent and severe allergic reactions, especially to seasonal allergies. But most people with asthma are able to live normal lives without a major reduction in their life expectancy.
When is Supplemental Oxygen Needed
Unlike with the other conditions listed above, supplemental oxygen is really only prescribed in rare cases of asthma. In chronic bronchitis, the airways are always inflamed and damaged and in emphysema, the lungs are always inflamed, so this explains why many COPD patients need to be on oxygen 24 hours a day. However, in asthma, the airways are mostly healthy when the patient is not experiencing an asthma attack.

Generally, rescue inhalers and nebulizers are used to treat asthma attacks. These medications are designed to open up the airways and reduce inflammation so that the patient can breathe normally. However, there is a type of asthma attack often referred to as “acute severe asthma” or a “severe asthma exacerbation” where supplemental oxygen is almost certainly needed. These types of asthma attacks do not react the same way to traditional asthma medications like bronchodilators so patients need to receive supplemental oxygen in order to maintain healthy blood oxygen saturation.
Congestive Heart Failure
Congestive heart failure, also known as heart failure, is a disease where your heart doesn’t pump blood in the way that it should. This is usually brought on by a number of conditions such as narrowed heart arteries (coronary artery disease) or high blood pressure. What results in your heart muscle being too weak or stiff to pump blood as effectively as it did when you were healthy. According to the Cleveland Clinic, heart failure is the leading cause of hospitalization in people 65 years and older.

Just like your lungs, your heart plays an important role in your systemic health. When your body isn’t able to pump blood effectively, other areas of your body may suffer just as greatly. Edema is one sign that you’re experiencing heart failure. This is when your extremities such as your hands, feet, or legs begin to fill with fluid, usually turning a purple color. And while edema on its own is not usually a serious problem, it’s a sign that you could be suffering from heart failure or some other heart-related problem.
Another area of the body that’s affected by your heart health is your lungs. This is because your heart and lungs work together to circulate oxygen-rich blood throughout your body. When your heart is unable to circulate blood properly it can lead to symptoms like shortness of breath, problems exercising, and chronic fatigue. This is often caused by either congestion in the lungs or a lack of oxygen in the tissues throughout your body which can make you feel tired and weak. You might also experience dizziness, confusion, or problems concentrating.
When is Supplemental Oxygen Needed?
Since congestive heart failure is a disease that affects the heart, it’s hard to compare to the other diseases on this list which are all lung diseases. However, despite this fact, congestive heart failure still sometimes requires the use of supplemental oxygen. More often than not, your doctor will prescribe you with supplemental oxygen when your heart failure causes low levels of oxygen in your blood. According to Web MD, you’re less likely to be prescribed oxygen if you just have mild symptoms because too much oxygen can be very dangerous in heart failure patients.

All things considered, supplemental oxygen is not a cure-all when it comes to heart disease. In reality, it won’t do a lot to help you manage heart disease symptoms. What it aims to do is prevent collateral issues caused by heart disease. In other words, it prevents further damage from being done to your body.
Conclusion
Supplemental oxygen therapy is a treatment with a long history. It’s been used for hundreds of years to help pneumonia patients manage their symptoms and over the years, researchers have discovered many other conditions that can benefit from supplemental oxygen. If you have one of the conditions listed above, it may be worth asking your doctor if you could benefit from using supplemental oxygen.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
If your doctor prescribes you supplemental oxygen, you’re going to need an oxygen device that’s right for you and your needs. Here at LPT Medical, we have a wide selection of stationary oxygen concentrators, portable continuous flow oxygen concentrators, and portable pulse dose oxygen concentrators. These devices are significantly less bulky and heavy than traditional oxygen delivery methods such as oxygen tanks and liquid oxygen tanks, but they provide you the same medical-grade oxygen. Feel free to reach out to us either by email or by phone to speak with an oxygen concentrator specialist.
For people who have COPD, living in a clean environment should be a top priority. Because the disease makes the lungs hyper-sensitive to irritants, even small amounts of dust and allergens can set off coughing fits and make daily COPD symptoms worse.
Unfortunately, there are many places in your home that can trap particles that irritate your lungs, and it can be difficult to track them all down. Harmful particles can accumulate in your carpet, furniture, and all the nooks and crannies of your home, where they lie in wait until they get stirred up into the air you breathe.
One of these hidden sources of respiratory irritants could be your bedding, which is an oft-overlooked hot spot for dust and allergens. Many people don't realize how quickly their pillows, mattresses, and bed sheets can accumulate hazardous particles that can trigger COPD symptoms.
In this article, we're going to show you how to get rid of dust, mold, dust mites, and other particles in your bedding and keep them away for good. That way, you can rest assured every night knowing your lungs are protected while you sleep.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
A Very Real Hazard
_Lorryia_formosa_2_edit.jpg)
It's easy to underestimate the dangers that respiratory irritants in your sheets, pillows, and mattress can pose for your lungs if you have COPD. However, based on how much time you spend in and around your bed, it should not be difficult to imagine how being exposed to them night after night could affect your lungs on a daily basis.
Because you spend so much time in your bedroom, keeping it clean and lung-friendly should be one of your top priorities. Most people spend a minimum of seven to eight hours in their bed every night, and it can have a significant affect on your ability to breathe if you are surrounded by hazardous particles and allergens while you sleep.
If you don't take special precautions, dust, mold, pollen, and other irritants that live in your bed enter your lungs at night when you breathe. This can inflame your lungs, causing you to wake up with worse symptoms that can last throughout the day.
That's why it's so important to give your bedding some extra attention if you have COPD. Just being more careful and deliberate in the types of fabrics you use and how you care for them can go a long way toward improving your COPD symptoms.
The Hazards Hiding in Your Sheets

According to a microbiologist from the New York School of Medicine, beds are uniquely prone to collecting all kinds of nasty and potentially hazardous substances. “You have spores of fungi, bacteria, animal dander, pollen, soil, lint...” he says, along with skin cells, oils, cosmetics, and bodily secretions, among others.
While some of these are simply gross, others can actually be dangerous for your lungs, especially if you have COPD. Dust mites, mold, pollen, and pollutant particles, in particular, can inflame your lungs, cause uncomfortable symptoms, and exacerbate your COPD.
Dust Mites

Wherever there's fabric, there's a good chance there is an invisible army of dust mites living in the fibers. Dust mites live off of dead skin, dust and fibers, and thrive in places like your carpet, furniture, and—you guessed it—your bedding.
Dust mites particularly like anything that's made with plush or layered fabrics like pillows, comforters, mattresses, and thick blankets. These items tend to trap lots of dust and dead skin for the little bugs to to munch on.
While they don't affect everyone, dust mites cause many people to experience symptoms like coughing, sneezing, and nasal congestion when they're around. If you have COPD and are sensitive to dust mites, exposure to the mites in your mattress and bedding can inflame your lungs and airways and make your COPD symptoms worse.
Mold

Mold is another respiratory irritant that could be lurking in your pillows, mattress, or bed sheets. Exposure to mold can irritate your lungs and cause a variety of uncomfortable symptoms, including coughing, wheezing, nasal stuffiness, eye irritation, and even skin irritation in some cases.
Some people are more sensitive to mold than others, but patients with COPD should be careful to steer clear of damp, moldy environments. That includes looking out for mold growth in your home, including in your fabrics and bedding.
Bed sheets, blankets, and other fabrics can get moldy after you wash them if you leave them sitting in the washer too long or don't dry them out quickly enough. You can usually tell if they've grown any mold because they'll have a musty, mildew odor, even after they've dried.
Your mattress and pillows can collect mold, too, if they get get wet for any reason. That's why it's important to avoid spilling water in your bed and to dry up any damp spots immediately.
If you live in a humid climate, things will get damp easier and dry out more slowly, which means you'll need to be even more on the lookout for mold and mildew. It's also important to know that mold is almost guaranteed to grow in any place that stays damp for more than 24 hours, no matter where you live.
Keeping your bed free from mold is important for protecting your lungs and keeping respiratory symptoms at bay. If you have musty sheets or hidden mold in your mattress, it can cause your COPD symptoms to flare up and hurt your ability to breathe every day.
Pollen, Pollution, and Other Particles
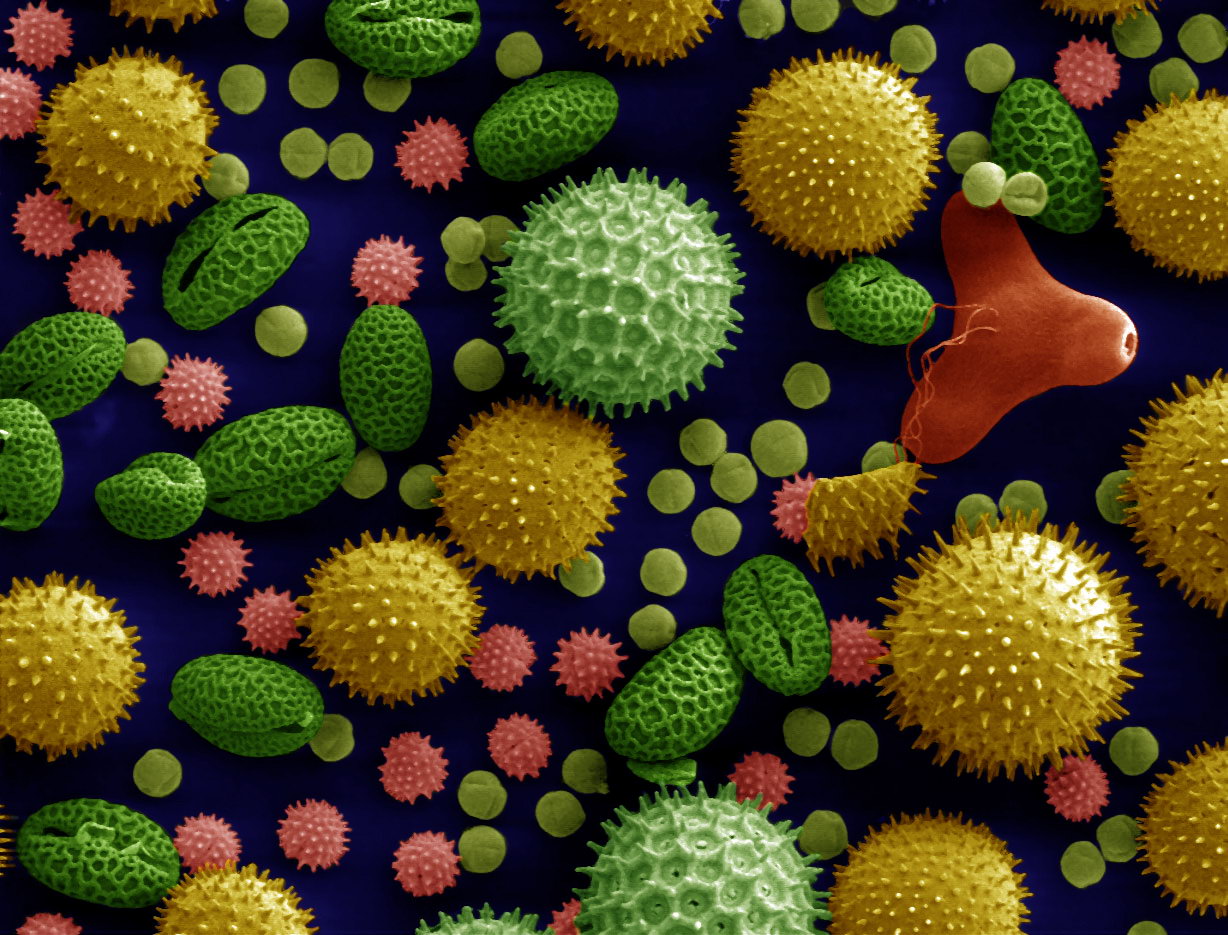
When you go outside or spend time in a place with poor indoor air quality, any dust, pollen, or particle pollution you encounter sticks to your hair, clothes, and skin. If you aren't careful when you go home or get into bed, you can scatter these harmful particles around your home, into the air, and in your sheets.
Pollen and pollution levels tend to fluctuate between seasons and even from day to day, so your risk may change depending on where you live and the time of year. The particles can get in by hitching a ride on your person or by blowing in through open windows throughout the day.
If you have COPD, these allergens and pollutants can be especially dangerous, making it difficult to breathe and triggering COPD symptom flare-ups. Because the disease makes your lungs more sensitive to even small amounts of these irritants, it's important to take steps to minimize them in your bed and in your home.
How to Know if Your Bedding is the Problem

Many people experience worsened COPD symptoms at night and in the morning because they have trouble breathing while they sleep. In many cases, changing your sleeping position, using nighttime oxygen, or getting diagnosed and treated for sleep apnea can solve this problem.
However, sometimes worsened nighttime and morning COPD symptoms is a sign that there's something in your house or bedroom that's irritating your lungs while you sleep. This can cause you to experience worsened breathlessness during the night, which can make it difficult to fall asleep and deprive you of oxygen when you do.
As a result, you may wake up congested, fatigued, and feeling like your lungs and airways are inflamed. You might notice that your COPD symptoms are worse in the mornings and get better as the day goes on.
If this happens to you, make sure you talk to your doctor to make sure that you don't need nighttime oxygen or have an underlying sleep disorder or other problem. If the problem persists, it could be a sign that your bedding is exacerbating your COPD symptoms at night.
If so, then following the tips in this article to clean and care for your bedding could make a huge difference in how you feel every day. By removing a major source of respiratory irritants, it could make a significant difference in your ability to breathe and keep your COPD symptoms under control.
If you've taken care of your bedding, talked with your doctor, and you still notice your symptoms getting worse after spending time in your bedroom or at home, the air inside your house might be polluted. It could be a sign that you need to do a deep, whole-house cleaning and maintenance check to eradicate any other hidden sources of lung irritants in your home.
Here are some of the major symptoms of exposure to indoor respiratory irritants. If you experience these symptoms when you're at home, especially if they get worse after sleeping in your bed, it could be a a strong sign that your bedding is making your COPD worse:
Symptoms of exposure to indoor irritants (e.g. mold, dust mites, and other particles in your bedding):
- Nasal congestion
- Coughing
- Wheezing
- Shortness of breath
- Sneezing
- Itchy or runny nose
- Itchy and watery eyes
- Irritated, itchy skin or rashes
How to Keep Your Bedding COPD-Safe
Clean Your Sheets Often

The best way to get rid of the bulk of allergens and respiratory irritants is to wash your sheets, blankets, and covers often. It generally takes a week or more for them to accumulate in significant amounts, so a thorough wash once a week should be sufficient.
However, if you're like most people, you probably only change your sheets every couple weeks at most, or maybe even less often. Even though most people know they should wash their sheets more, it's an easy task to forget and neglect.
If you tend to put off washing your sheets or struggle to keep up with laundry, try to carve out a specific time in your schedule every week to throw all your bedding in the wash. Just be sure to use very hot water so it sanitizes the fabric and kills any mites or mold spores.
However, comforters and duvets can be washed less often since they don't usually come into direct contact with your skin. It's usually fine to wash these heavier top blankets about once every month or so.
Get an Extra Bedding Set

It's difficult to wash your sheets, pillow cases, and blankets often if you only have one set. To reduce the hassle, invest in a second bedding set so you can simply switch them out when one needs to be cleaned.
This makes it easier to change your sheets frequently and can really come in handy when there's an unexpected mess or spill in your bed. Just make sure to store your extra set of sheets and blankets away in a cool, dry place, preferably in a sealed container or linen bag.
Avoid Materials that May Trigger Allergies
Certain types of blankets and pillows are more likely to cause respiratory symptoms than others. For example, pillows and duvets stuffed with down feathers can trigger respiratory symptoms and breathing problems in people who are sensitive to the material.
If you experience worsened breathlessness or other COPD symptoms at night, you might want to check whether or not you are allergic to any of the materials or stuffing in your bed. If any of your pillows or blankets contain down or other allergy-triggering materials, try removing and replacing them with cotton-stuffed versions to see if your symptoms improve.
However, if you've removed any potential allergy-causing materials and still feel worse at night, then it's a good sign that something else is irritating your lungs. It could also be a sign that you are particularly sensitive to dust mites and need to dust mite-proof your bed.
Purchase Mattresses and Pillows that are Resistant to Dust Mites and Other Allergens

The types of fabrics and materials used in your bedding can make a big difference in how susceptible they are to dust mites and mold. Some materials tend to attract these respiratory irritants more readily, while others are more resistant.
If you have COPD, you might consider replacing your mattress and pillows with hypo-allergenic, dust mite-resistant versions. These products are made with materials designed to keep dust mites and other hazardous, lung-irritating particles from ever getting into their fibers in the first place.
Especially if you suffer from allergies, asthma, or are sensitive to dust mites and particles, getting hypo-allergenic products could help eliminate many of the irritants that trigger COPD symptoms at night. You may find that you sleep better, breathe better, and feel better during the day when you're not breathing in inflammatory particles all throughout the night.
Many hypoallergenic pillows and mattresses are made of allergy-resistant materials like latex, bamboo, and silk. You can often find them at department stores, mattress retailers, and in many shops online.
Choose Hypo-Allergenic Sheets and Blankets
Unfortunately, putting hypo-allergenic covers on your mattress and pillows won't do anything to protect you from irritants in your blankets and sheets. Aside from regular washing, the only way to have irritant-free sheets is to get them in an allergy-proof material.
For example, silk is naturally resistant to a variety of allergens and respiratory irritants, including dust mites, mold, and mildew. Wool is another great bedding material that repels dust mites and other allergens, and it's perfect for keeping your bed warm during the cold, winter months.
If you tend to sweat or overheat at night, you should also look for fabrics that are breathable and good at wicking moisture away so your bedding doesn't get musty. Wool is fantastic at wicking away moisture and can help keep your mattress dry at night.

Here is a list of some the best hypo-allergenic and COPD-friendly bedding materials:
- Bamboo: anti-microbial and resistant to mold and mildew
- Latex: anti-microbial and anti-bacterial
- Silk: resistant to dust mites, mold, and mildew
- Wool: resistant to dust mites and great at wicking away moisture
- Down and Hypodown: naturally dust mite-repellant and lightweight (Do not use down if you have a down allergy; use synthetic down alternatives or hypodown instead.)
Protect Your Mattress and Pillows

The next best thing to buying a new, allergen-resistant mattress and pillow is getting dust mite-resistant covers for your bed. Sometimes called allergy covers or hypo-allergenic covers, they provide an extra barrier to prevent dust mites from infesting the inside of your bed.
Dust mite-resistant covers work because they use a finely-weaved fabric that's so tight that dust mites can't crawl through. This can be especially useful for preventing dust mites from proliferating in your mattress and pillows when the weather turns humid and damp.
For the best results, you should keep the cover tightly zipped on your mattress and pillows all of the time from the minute you bring them into your home. It's important to use the covers consistently, because thy will do nothing against any dust mites that take up residence in the fibers when the cover is not in place.
While some research casts doubt on the effectiveness of hypo-allergenic mattress and pillow covers, other studies show that they can reduce symptoms and complications in people with allergies and asthma. This indicates they are also effective for people with other breathing disorders, including patients with COPD.
In fact, the Lung Institute Recommends that COPD patients use zippered, dust-mite proof cases on their pillows and mattress to reduce their symptoms at home. Especially if you know that you are sensitive to dust mites, dust mite covers can be a simple and effective way to eliminate another COPD trigger from your bedroom.
Be Careful What You Track In to Bed

While cleaning your covers and replacing your pillows regularly is important, there is plenty you can do to minimize the number of hazardous particles that make it into your sheets in the first place. You can do this by being especially careful about what you track into your bedroom and what you wear when you go to bed.
The clothes you wear accumulate all sorts of particles throughout the day no matter where you go. Even if you avoid pollution and do your best to stay away from respiratory irritants, the fibers in your clothes are bound to trap a certain amount of dust, pollen, mold spores, and particle pollution.
That's why you should always remove your clothes before getting in your bed unless they're fresh, clean bedclothes that you just slipped on. Never get into bed wearing anything you've gone out in or even worn about the house.
Instead, always remove your clothes and/or change into fresh clothing before you crawl under your shets. That's the only way you can make sure that none of the hazardous particles in your clothes get transferred onto your sheets.

Here are some more tips for keeping respiratory irritants out of your bed:
- Try showering at night before bed, instead of in the morning, to remove any dust, pollen, or other particles from your skin and hair.
- If you like to wear any clothes to bed, make sure they are clean and wait to put them on until right before you get in.
- Don't allow your pets to sleep with you or get in your bed, especially under the sheets.
- Don't put clutter, dirty clothes, jackets, shoes, or other items on your bed.
Keep Your Bed and Bedding Dry

If you're sensitive to mold or dust mites, then it's important to keep your sheets, blankets, pillows, and mattress as dry as possible at all times. Damp and humid environments encourage dust mites to multiply and mold spores to grow in your sheets.
Because moldy fabrics don't usually look moldy, it can be easy to miss or underestimate. And since dust mites are invisible, you won't know if they've infested your sheets until they start triggering your COPD.
The first sign of mold growth is usually a damp, musty smell that may be very faint at first. It's a good idea to smell your blankets and sheets—or any clothing and fabrics, for that matter—for any hint of a moldy or mildewy smell before you put them on your bed.
Clean up any spills in your bed quickly and get damp spots to dry as fast as possible before mold has a chance to sprout up. Whenever you wash your blankets or sheets, make sure to put them in the dryer or hang them up to air dry immediately.
You should also avoid anything that makes your bedroom too humid, which could encourage mold and dust mites to multiply. If your shower is attached to your bedroom, make sure to close the door and run the ventilation fan or open a window to vent the humid air outside.
It should go without saying that you should dry your skin and hair off as much as possible before getting into bed, and that you should never set a damp towel on your sheets after you shower. If your hair is still damp at bedtime, wrap it up in a towel or put a thick towel over your pillow to protect it from getting wet.
If you do notice a moldy or musty smell in your bed or sheets, wash all of your bedding thoroughly with hot water and detergent to remove the mold. You can also add a cup or two of vinegar to the load during the rinse cycle to get rid of the musty smell.
For very moldy clothes or blankets, soak them in vinegar before putting them in the wash to kill most of the mold first. You can also wash your clothes with bleach or borax, although these methods can ruin or discolor fabrics if you are not careful.
Mold in your mattress can be more difficult to spot, but it can sometimes be identified by smell or by looking for spotting on the surface. If you find a small amount of mold or mildew on the surface of your mattress, you can usually take care of it by scrubbing it off with a mix of warm water and a cleaning solution like rubbing alcohol, vinegar, or bleach; just be sure to dry it off immediately after.
Laying your mattress out in a sunny spot can also help once you've removed all visible signs of mold. The sun's rays and heat will kill any leftover mold on or just under the mattress's surface.
Control the Humidity in Your Room
Many people with COPD struggle to breathe in humid weather, in part because humid air is hard on your lungs. However, many of the respiratory symptoms that COPD patients experience in high humidity could be the result of other respiratory irritants, like dust mites and mold.
That's because warm, humid weather creates ideal conditions for mold and dust mites to thrive and multiply in your home. Humidity also makes everything take longer to dry, further increasing the chances for mold growth on damp towels, sheets, and clothes.
If you live in a humid climate, or get a bout of humid weather, you should be extra diligent about inspecting your house for mold and keeping things like your clothes and sheets dry. You


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!












