Whether you've been recently diagnosed with COPD or have been living with the condition for years, you are bound to have lots of questions. These might include questions about your health, your disease, your medications, your treatment options, and more.
As these questions come up over the course of your COPD treatment, your doctor will be your primary source for answers. But in order to get the right answers and the information you need, you first have to know what questions to ask.
Communication between doctors and patients should never be one-way; it's just as important for you to communicate with your doctor as it is for him to explain information to you. In order to get the best treatment possible, you need to keep track of all your questions, articulate your concerns, and remember to bring them up with your doctor when you have the chance.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
However, it can be easy to get distracted or forget any questions you have once you're actually in the office with your doctor. That's why it's a good idea to think about your questions and concerns ahead of time, before you get to your doctor's appointment.
In this post, we're going to go over a variety of questions that you can ask your doctor about your COPD. The answers to these questions can help you better understand your disease, how to keep yourself healthy, and how to take a more active role in your COPD treatment.
You can use these questions as a guideline when you visit your healthcare providers or as a jumping-off point to open up an ongoing dialogue with your doctor. As you read through the questions in this guide, they may even remind you of other questions and concerns you want discuss.
Questions to Ask Your Doctor About COPD
What Kind of COPD Do I Have?

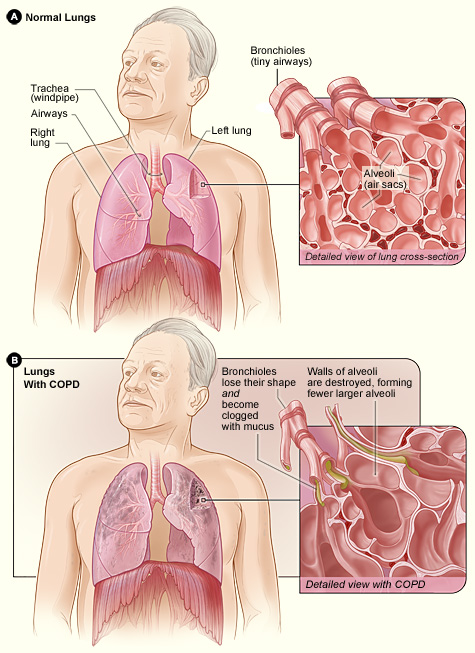
COPD is an umbrella term that encompasses two distinct, but related lung conditions: emphysema and chronic bronchitis. Some people with COPD have just one of these conditions, while others have a combination of both.
Even people who show signs of both emphysema and chronic bronchitis often have one condition that is dominant. For instance, your lungs could be primarily affected by emphysema but also show signs of mild chronic bronchitis.
Before your doctor diagnoses your COPD, he will likely use a variety of tests, including spirometry (a basic lung function test), a chest X-ray, and pulse oximetry (a way to measure blood oxygen saturation). He will then consider the results of these tests along with your symptoms and medical history to come up with a diagnosis.
When you get diagnosed with COPD, ask your doctor to take the time to thoroughly explain your condition, including the difference between emphysema and chronic bronchitis and what kind of COPD you have. If there is anything you don't quite understand, don't hesitate to ask your doctor for more examples and details.
How Serious is My COPD?
COPD is a chronic disease that slowly gets worse over time. How severe your COPD is depends on how badly your lungs are damaged and how serious your symptoms are.
When you first get diagnosed, your doctor will likely place your disease within one of four distinct stages. Stage 1 COPD is the most mild, while stage 4 COPD is the last, most serious stage of the disease.
However, every person is different, and COPD affects different people in different ways. For instance, two people who are diagnosed with the same stage of COPD could have different symptoms and complications, and their diseases could progress at different speeds.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
That's why it's important to ask your doctor to give you a thorough explanation of your health, your disease stage, and your prognosis. Ask him to explain your test results, how exactly he made his diagnosis, and where you fit on the spectrum of COPD severity.
Continue to ask questions and get as much information as you can as your symptoms change and your disease progresses. Even if your doctor has explained something already, don't be afraid to ask him to go over it again or provide you with some helpful context.
How Did I Get COPD?

Although smoking is by far the most common cause of COPD, many other things can cause the disease. In general, just about anything that repeatedly irritates and damages your lungs over time can cause COPD.
This includes things like air pollution, chemical fumes, and occupational exposure to dangerous respiratory toxins. Other health conditions that affect the lungs, like asthma, cystic fibrosis, and AAT deficiency, can also cause COPD later in life.
If you and your doctor can figure out what caused your COPD, it can help you avoid exposing your lungs to the same hazard in the future. Unfortunately, in some cases, the exact culprit is difficult to find.
It is not always possible to pinpoint a single cause of COPD; you could be exposed to many different things over the years—such as air pollution, wood smoke, and cooking fumes—that damage your lungs. Still, discussing your medical history, occupational history, and any other possible causes with your doctor may help you better understand your disease.
Here are some things your doctor might want to know when discussing the cause of your COPD:
- When did your breathing symptoms first start?
- Have you ever smoked tobacco? (And do you still smoke tobacco?)
- Have you ever been diagnosed with asthma?
- Have you ever been frequently exposed to second-hand smoke (in childhood or adulthood)?
- Have you ever worked in an occupation where you might have been exposed to exhaust fumes, chemical fumes, wood smoke, dust, or fine particles?
- Have you ever lived in an area with heavy pollution?
- Do you use a wood-burning stove in your home?
- Has anyone in your family ever been diagnosed with a lung disease?
What Do My Test Results Mean?

If you have COPD, you will go through many different types of tests both before and after your diagnosis to help your doctor monitor and treat your disease. In fact, your doctor will likely do lung function tests (spirometry) and a blood oxygen saturation test (pulse oximetry) at every regular visit.
These tests reveal some very important things about your lungs, your heart, and your overall health. Your doctor will use the results of these tests to better understand your disease and find the best ways to treat it.
Your doctor will do some tests, like spirometry, at every check-up appointment to help him monitor changes in your lung function over time. As you go through treatment, it is important for you to understand what these tests are and what their results mean for your health.
Whenever your doctor does a test, he should show you the data and take the time to explain your results in terms you can understand. However, not all doctors take the time they should to explain things to their patients, and some doctors are simply not very skilled at explaining tough concepts in layman's terms.
That's why you should never be afraid to ask your doctor for more details and information about any of your medical test results. You shouldn't feel nervous to ask questions or feel embarrassed to admit when there is something you don't understand.
If you don't quite get it the first time around, ask your doctor to re-explain. Tell him which things you don't understand and don't hesitate to ask for more details, examples, and clarification if you need to.
Make it your goal to never leave the doctor's office with unanswered questions or concerns. Also, remember that if anything comes up later, you can call up your doctor on the phone to ask any additional questions you have.
Here are some examples of questions you can ask your doctor to better understand test results:
- What exactly does this test measure?
- How reliable are the test results?
- What do the test results say about my COPD?
- Do the test results indicate there is anything I should or should not be doing for my health?
How Do I Use My Medications?

Once you've been diagnosed with COPD, your doctor will prescribe you a variety of medications that will help you keep your symptoms under control. These may include quick-relief inhalers, maintenance inhalers, anti-inflammatory medications, corticosteroids, antibiotics, and more.
The combination of medications your doctor prescribes is your most powerful tool for managing your symptoms and keeping your COPD from getting worse. That's why you should take the time to make sure you know exactly how to use them correctly.
First, you will need to ask your doctor to explain what each of your medications are and what they are supposed to do. Then, you need to know when to take each medication and how to get the correct dose.
Your doctor should provide you with a COPD action plan that explains, in brief, your daily medications along with which medications to take when your symptoms get worse. However, in order for you to be able to use this resource effectively, your doctor needs to thoroughly explain how it works and how to use it to manage your symptoms every day.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
You should also ask your doctor to demonstrate for you the proper way to use your inhaler. Even if you've used an inhaler before, it's important to review the correct technique and make sure you know how to use your particular type of inhaled medication.
An alarming number of COPD patients don't use their inhalers correctly, which is why it's so important to double-check your technique. You can ask either your doctor or pharmacist to demonstrate it for you, and you can ask them to evaluate your technique as well.
You should also ask your doctor to give you a printed and signed list of all the medications you take, both prescription and over-the-counter. You should keep this list handy for a variety of reasons.
You may need to present this doctor's note when you travel with prescription medications, especially if you board a plane or train. Your medication list can also come in handy as a reference for yourself, your pharmacist, or other medical professionals you see.
What are the Potential Side-Effects of My Medications?

All of the medications prescribed for COPD have the potential to cause side effects. As you go through treatment, it's important to understand the potential side effects of every medicine you take.
For example, doctors often prescribe oral corticosteroid medications to help COPD patients recover from exacerbations. But even though corticosteroids are very effective at managing COPD symptoms, they can have serious side effects; because of this, most doctors only prescribe them when absolutely necessary and only for short-term use.
That's why it's important to ask your doctor to explain the side effects of every medication he prescribes or recommends. That way, you can fully evaluate the medication's benefits and risks and more easily recognize any side effects that occur.
It's also important to keep in touch with your doctor whenever you start a new medication. Let your doctor know how well the medication is working and alert him to any side effects right away.
Some side effects are merely uncomfortable, while others are more difficult to manage or can cause serious damage to your health. Depending on the type and severity of side effects you experience, your doctor may advise you to stop the medication, reduce your dosage, or switch to a different type of medicine.
Keep in mind that side effects are much more likely when you don't follow the correct dosage. That's just one of many reasons why it's so important to use your medications exactly as directed. This includes your as-needed inhalers, which you should take care not to use more often than your doctor recommends.
Here are a few examples of common COPD medications along with their potential side effects:
- Bronchodilator Medications:
- Increased heart rate
- Shakiness
- Camping in hands, legs, and feet
- Dry mouth
- Inhaled Corticosteroid Medications:
- High blood pressure
- Thrush
- Hoarse voice
- Dry or sore mouth
- Mouth and throat infections
- Oral Corticosteroid Medications:
- Weight gain
- Weakened bones
- Weakened skin
- Elevated blood sugar
- Muscle weakness
- Increased risk for Pneumonia
- Cataracts
- Changes in mood
What COPD Triggers Should I Watch Out For?

And important part of learning to manage your COPD symptoms is knowing about COPD triggers. A COPD trigger is anything that irritates your lungs and makes your respiratory symptoms worse.
A wide variety of different things can be COPD triggers, including fragrances, air pollution, allergens, and certain weather conditions. Depending on your lifestyle and the climate you live in, you may need to take special precautions to protect yourself from these and other things that irritate your lungs.
That's why you should ask your doctor to tell you all about COPD triggers. He should give you a thorough briefing on the many respiratory irritants and environmental triggers you may encounter, as well as tips for how to avoid them.
Your doctor can also alert you to common triggers that are specific to your geographical area, such as air pollution, high humidity, or seasonal allergens. He can also give you advice for reducing indoor air pollution so you can breath fresher air and manage your symptoms better at home.
You should also tell your doctor all about your lifestyle and home environment so he can help you identify any activities or conditions in your life that might trigger your symptoms. Every person is different, and which triggers your lungs are sensitive to depends on your unique biology and lifestyle as well as the severity of your disease.
What Changes Should I Make to My Diet?
In order to work at their optimum level, your lungs need lots of nutrients for fuel. Unfortunately, many COPD patients don't get enough nutrients—or don't get enough of the right kinds of nutrients—to keep their lungs and bodies strong.
The truth is that what and how much you eat can have a noticeable effect on your COPD. Too few calories and nutrients can reduce your lung function, while eating too much of the wrong things can also make breathlessness and other COPD symptoms worse.
That's why it's important to talk to your doctor about your diet and ask him what you can do to improve. That way, he can help you identify unhealthy eating habits and set better nutritional goals.
Your doctor is a great resource for learning what a proper diet looks like and how to maintain a healthy weight. He can also tell you what kinds of foods support healthy lungs and warn you against foods that may make it even more difficult to breathe.
Like all adults, it's important for people with COPD to eat a well-balanced diet full of whole foods, lean meats, and lots of fruits and veggies. However, there are some unique dietary requirements and sensitivities that many COPD patients have.
If you, like many other COPD patients, suffer from any diet-related complications, your doctor can help you resolve those issues as well. If you experience heartburn, acid reflux, weight gain, weight loss, or worsened shortness of breath after meals, you should bring these issues up with your doctor right away.
If you need more guidance, your doctor can also refer you to a nutritionist or dietitian to help you get on track. These specialists can help you develop a more detailed and personalized diet plan that takes your personal lifestyle and unique health needs into consideration.
What Kind of Exercise Should I Get?

Exercise is not only safe, but extremely beneficial, for the vast majority of people with COPD. While it may be difficult at first, getting enough physical activity improves your overall health and may even improve your ability to breathe over time.
Even if you suffer from symptoms that make exercise difficult, it's important to do what you can to keep yourself active. You just have to take it slow, start with light activities you can manage, and gradually do more as your physical abilities improve.
Getting started is often the most difficult part, especially if you aren't used to exercising on a regular basis. That's why you should ask your doctor to help you put together an exercise plan that is feasible and suitable for you.
Your doctor can tell you what kinds of exercises are safe and help you find activities that are appropriate for your level of fitness. He can also give you tips for reducing shortness of breath and managing your symptoms during physical activity.
If you have very severe symptoms, limited mobility, or just need some extra help getting started, your doctor can also refer you to another specialist that can help. Many patients are able to overcome obstacles and get on the track to better physical fitness by working with a personal trainer, physical therapist, or joining a pulmonary rehabilitation class.
Will I Need to Use Supplemental Oxygen?

As your disease progresses and your lung function gets worse, you may need to use supplemental oxygen to help your lungs meet your body's oxygen needs. Many, but not all, COPD patients end up needing oxygen therapy eventually.
Oxygen therapy isn't usually needed unless your lungs get to the point that they are no longer able to keep your blood saturated with oxygen on their own—a condition known as chronic hypoxemia. If your blood oxygen concentration begins to frequently drop below about ninety percent, your doctor may decide it's time for you to start using supplemental oxygen.
Once you start oxygen therapy, it is likely that you will need to continue using it for the rest of your life. However, some patients end up only needing oxygen for a short period time while recovering from a serious COPD exacerbation.
It's a good idea to discuss the possibility of oxygen therapy with your doctor early on in case you need it at some point during treatment. That way, he can explain how oxygen therapy works and how he will determine if and when you need to use supplemental oxygen.
Talking to your doctor ahead of time can help you feel more prepared if the time to begin oxygen therapy eventually comes. He can also clear up any questions or worries you have about using supplemental oxygen.
Your doctor can also help you take a more active role in your treatment by teaching you to recognize symptoms that indicate your blood oxygen levels are low. That way, you can alert your doctor if you notice the signs of worsening hypoxemia.
If you do use oxygen therapy, make sure your doctor takes the time to explain how to use it, when to use it, and how to get the dosage right. He should also go over basic safety precautions for handling your oxygen equipment to prevent dangerous fires and other accidents.
Before using your oxygen equipment, ask your doctor as many questions as you can think of to make sure you thoroughly understand how to use oxygen therapy safely and correctly. Oxygen is a medicine, and, like other medicines, it can be dangerous if you don't use it as directed.
How Can I Slow Down the Progression of My COPD?
Unfortunately, there is no actual cure for COPD. However, research shows that there are certain things you can do that may be able to extend your life and slow down the progression of the disease.
For example, if you smoke, quitting can reduce how quickly your lung function declines and allow you to live longer. Making other lifestyle changes, such as being more active and improving your diet, may also slow the rate at which your COPD worsens.
However, every case of COPD is different, and how quickly your symptoms progress dep
