There are about 16 million people in the United States alone who have chronic obstructive pulmonary disease (COPD). This condition is characterized by slow but persistent lung function decline that leads to breathlessness, chest pain, and fatigue. Several lifestyle changes can significantly reduce the rate at which COPD progresses including an improved exercise routine, a refined diet, inhaled medications, and most importantly, oxygen therapy. Every case of COPD is different, however, so patients should consult with their doctor to learn which lifestyle changes will benefit them.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
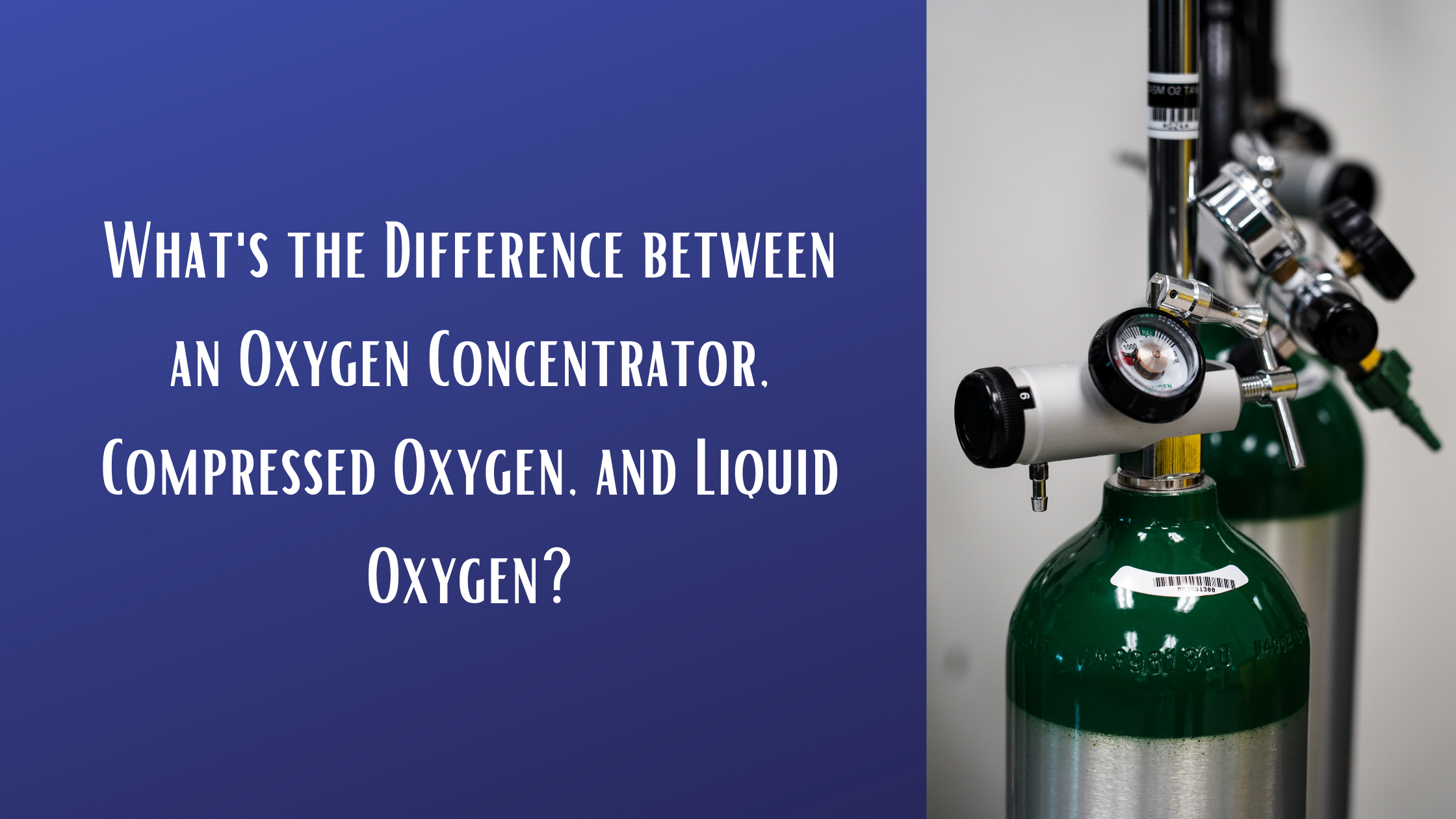
When it comes to supplemental oxygen therapy, there tends to be a lot of confusion over the different devices that are available to COPD patients. Many people are told that they need medical oxygen, but they’re never provided with instruction on finding an oxygen device that meets their needs. In this post, we’ll discuss three different types of medical oxygen: compressed oxygen, liquid oxygen, and oxygen concentrators. You’ll learn the differences between them and you’ll receive some guidance for choosing one that fits your lifestyle.
If you still have questions after reading, be sure to reach out to our oxygen device specialists here at LPT Medical. We’ll walk you step-by-step through choosing an oxygen device, getting the best deal, and even helping you to receive the necessary medical paperwork. Give us a call at 1-888-416-3855 or email us at info@lptmedical.com.
What is Compressed Oxygen Gas?
Compressed oxygen gas refers to oxygen that has been stored within a tank or a cylinder. Oxygen has been stored in this way since 1868 and it’s still considered a viable method to this day; albeit, the technology has certainly evolved. Compressed oxygen gas is used for a variety of purposes, but it’s primarily used for industrial and medical settings. Many COPD patients use oxygen tanks on a daily basis to maintain the oxygen levels in their blood. For the most part, oxygen tanks are reliable for oxygen therapy, but there are some downsides that you should be aware of.

One of the most notable downsides of oxygen tanks is that they are heavy and bulky. Chances are, you’ve seen people carrying an oxygen tank around in public, and it’s not hard to see how much they struggle. Portable oxygen tanks can weigh as much as 20 pounds and they have a very oblong shape that makes them difficult to carry at your side or on your back. Most people choose to put their oxygen tank on a rolling cart but this comes with problems of its own. They take up a lot of space and they’re difficult to maneuver around obstacles or up a flight of stairs. Home oxygen tanks can weigh well over 100 pounds meaning you will need professional help just to move one.

Another glaring problem with oxygen tanks is that they need to be refilled constantly. For example, an “E” tank that is about 3 feet tall and weighs 8 pounds will only last 5 hours if it’s used continuously. At this point, you are going to either have to run home and use your home fill station or find a dependable oxygen company that can refill or replace your oxygen tank for you. All of this takes time and money, all while distracting you from what you care about most. It’s important to remember that the only way to extend the duration of your oxygen supply is to carry a bigger and bulkier oxygen tank or purchase a device called an oxygen conserver.
What is Liquid Oxygen?
Liquid oxygen is similar to compressed oxygen in that the oxygen is stored in a tank. The difference is that these devices store the oxygen in its liquid state rather than as a gas. This is preferable over compressed oxygen because once oxygen enters its gaseous state it expands and thus takes up more space. Liquid oxygen canisters tend to be much smaller and lighter than compressed oxygen and they last longer without needing to be refilled. There are some downsides to these units, however, so let’s take a look.

Likely the first thing you’ll notice about liquid oxygen devices is that they are more expensive than traditional oxygen tanks. This is because — in order for oxygen to be stored in a liquid state — it needs to be kept at very low temperatures. And in order to do that, you need a special type of storage container. Liquid oxygen cylinders work like a thermos in that they keep the liquid oxygen at around -297 degrees Fahrenheit. For safety reasons, liquid oxygen cylinders have decompression vents that release oxygen as the unit warms up. This means you should use it right after filling it up to ensure no oxygen is lost.

One of the problems many people encounter with liquid oxygen is that it’s extremely difficult and expensive to refill. You’ll need to either have a special home fill reservoir or you’ll need to outsource to an oxygen company. Even then, you may be hard-pressed to find a company that is able to fill a liquid oxygen device. While liquid oxygen tanks provide many benefits over traditional oxygen tanks, they aren’t as popular simply due to the high barrier of entry.
What is an Oxygen Concentrator?
The third and final oxygen device we’ll discuss is oxygen concentrators. Unlike traditional and liquid oxygen tanks which hold oxygen inside the unit, oxygen concentrators draw in ambient air, remove gases like nitrogen and argon, and output medical-grade oxygen. Another thing that sets concentrators apart is that they are electronic devices. What this means is that they need a reliable source of energy in order to operate. There are three different types of oxygen concentrators so we’ll break each one down.
Stationary Oxygen Concentrators
Also called home oxygen concentrators, stationary oxygen concentrators need a constant source of power in order to operate. The unfortunate downside to this is that you won’t be able to leave the house without there being an interruption in your oxygen delivery. On the other hand, you can still use things like extension cords or extra long nasal cannulas in order to move around the room freely. Despite the name “stationary,” most of these oxygen devices have wheels on the bottom that make them easier to move around the house. However, they tend to weigh a lot (usually upwards of 30 pounds).

One of the main reasons stationary oxygen concentrators are still in use today is because of their high oxygen output. Some concentrators like the NewLife Intensity 10 can put out up to 10 LPM (liters per minute) of oxygen which is enough for people with severe COPD. They’re also extremely reliable and they can run 24 hours a day and 7 days a week without a problem. Stationary concentrators are not ideal for people who want to get out and about but they’re a good choice for people who stay around the house.
Continuous Flow Portable Oxygen Concentrators
A portable oxygen concentrator works the same way as a stationary oxygen concentrator, but instead of being plugged into a wall outlet 24/7, POCs run off of rechargeable batteries. Most POCs use lithium-ion batteries which are some of the most powerful and reliable batteries in use today. You can find them inside cellphones, laptops, and other electronic devices. The term “continuous flow” refers to the way that oxygen is administered to the patient. It simply means that the oxygen is being released in a constant stream regardless of your breathing rate.

As you can imagine, there are several disadvantages to this. Since the device is working around the clock to administer oxygen, your battery life is going to suffer. Most continuous flow concentrators will only run for a couple of hours before the batteries need to be recharged or replaced. This can really be problematic if you want to get out of the house for an extended period of time in order to visit a friend or take a vacation.

Since continuous flow units are so bulky, taking your oxygen device into public areas or walking up long flights of stairs is out of the question. Unless you’re able to carry the machine on your back, the nasal cannula will dangle down quite a bit which can be a tripping hazard for you and others. To mitigate this risk, some people resort to using mobility aids that they can rest the device on while walking. This way, there’s no chance that the oxygen tubing will get caught on anything. The obvious downside of this is that you’ll have yet another thing to keep track of as you’re out and about.
Pulse Dose Portable Oxygen Concentrators
The final type of oxygen concentrator is a pulse dose portable oxygen concentrator. The term “pulse dose” refers to the way that oxygen is administered to the patient. Rather than being released in a constant stream, the device closely monitors your breathing rate and only delivers oxygen at the optimal moment. What this means is that no oxygen is wasted and you’ll have a lot more battery life to work with. Another major benefit of this technology is that it enables manufacturers to make their devices much lighter and smaller.

The Caire FreeStyle Comfort is one of the top pulse dose portable oxygen concentrators currently on the market. It weighs in at just 5 pounds and the 16-cell battery lasts up to 8 hours on a setting of 2. It also has a maximum oxygen output of 1,050 ml/min which is more than enough for the vast majority of oxygen patients. The great thing about the FreeStyle Comfort and most other pulse dose POCs is that it’s approved by the Federal Aviation Administration (FAA) meaning you’ll be able to take it on any commercial airline with you.

Ultimately, using a pulse dose portable oxygen concentrator as opposed to one of the other oxygen devices listed above, you’ll have more freedom to go where you please and spend more time doing the things you love. They’re very simple to use straight out of the box so you don’t have to worry about spending hours reading through the user manual or researching online. There is also a wide range of accessories available for them in order to help you customize and make the most of your new device.
Conclusion
In this post, we took a look at three of the main oxygen devices on the market: oxygen tanks, liquid oxygen tanks, and oxygen concentrators. Each of these devices is widely used by oxygen patients across the world and they are each viable in their own way. However, all things considered, pulse dose portable oxygen concentrators provide some pretty distinct advantages over the other options. Most importantly, they’re extremely lightweight meaning you can take them anywhere in the world with comfort and ease.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
The GCE Zen-O Lite, for example, is a pulse dose portable oxygen concentrator that weighs in at just 5.5 pounds. With both batteries inserted into the device, you’ll get up to 8 hours of battery life on one charge! That’s enough to last you the whole day and then some. It’s also one of the most powerful pulse dose units offering up to 1,050 ml/min (milliliters per minute ) of oxygen on one charge.
There are many incredible pulse dose concentrators on the market, so be sure to contact our respiratory specialists to discover which one is best for you. We’ll walk you through the whole process from choosing a device to choosing a buying option. We’ll even help you collect all the necessary paperwork and assist you with being reimbursed through Medicare or another health insurance company. Give us a call at 1-(800)-946-1201 or email us at info@lptmedical.com to get started.
Respironics is a company that was founded in 1976 by Gerald E. McGinnis. At first, they primarily focused on sleep apnea products like CPAP machines, but in the early 2000s, they began to branch out and started producing oxygen delivery systems as well. Since their acquisition by Philips in 2008, they’ve been able to expand their oxygen device manufacturing significantly, providing better products and reaching millions of customers around the world.
Some of the most notable Respironics oxygen products include the EverFlo and EverFlo Q stationary oxygen concentrators, the Respironics SImplyGo continuous flow portable oxygen concentrator, and the SimplyGo Mini pulse dose portable oxygen concentrator. Respironics products are known for their outstanding build quality, reliability, and ease of use. Watch the video above as we unbox and review a SimplyGo Mini.
In this post, we’re going to be taking an in-depth look at the Respironics SImplyGo Mini and how it sets itself apart from other concentrators on the market. We understand that trying to find the right concentrator for your needs can be time-consuming and even confusing at times, so be sure to reach out to our oxygen concentrator specialists for a free consultation. We’ll walk you through everything from choosing a device, to obtaining your medical paperwork, and receiving financial compensation through Medicare.
A New Generation of Oxygen Devices
Throughout the history of oxygen therapy devices, healthcare professionals have struggled to find an effective way to provide their patients with the oxygen they need while also helping them maintain their freedom. Oxygen tanks have been used for many decades and they’ve proven to be an effective tool for managing chronic respiratory conditions. However, they’re incredibly difficult to use whether you’re inside the home or outside the home.

In the 1970s, home oxygen concentrators started hitting the market. The major benefit these devices had over oxygen tanks is that they never needed to be refilled with oxygen. As long as you had a reliable source of power, you would have access to medical-grade oxygen. This was also the biggest disadvantage of home concentrators because you would be unable to leave your home while using them.

The Respironics SimplyGo Mini is part of a new generation of oxygen devices that combines the benefits of oxygen tanks and stationary oxygen concentrators. The SimplyGo Mini is a portable oxygen concentrator meaning it uses the same technology as stationary concentrators but instead of having to be plugged into the wall 24/7, it runs off of powerful lithium-ion batteries that you can take anywhere. It also uses something called pulse dose technology which closely monitors your breathing, administering oxygen at the optimal moment. This results in extended battery life so that you can stay out and about longer.
Meeting the Needs of the Modern Oxygen User
In this day and age, we expect more from our electronic devices. Our cellphones and laptops are smaller, lighter, and more powerful than ever before, so why shouldn’t we expect the same from our oxygen device? The good news is that the SimplyGo Mini fully delivers in every way. This machine weighs in at only 5 pounds making it one of the lightest portable oxygen units currently on the market. And the dimensions are just 9.4” H x 3.6” D x 8.3” W making it no bigger than a small handbag or purse.

What this means for you and other oxygen users is that you can do all of the activities you used to do without feeling like you’re being held back by your oxygen device. Whether you simply enjoy going for a stroll through the park or you want to be able to take a flight across the world, the SimplyGo Mini has got you covered. This machine is approved by the Federal Aviation Administration (FAA) meaning you’ll be able to take it on any commercial flight. Just make sure you contact your airline 48 hours in advance to learn about more specific regulations regarding in-flight oxygen use.

Another way that the SimplyGo Mini excels is in terms of battery life. There’s nothing worse than getting out of the house, looking down at your oxygen concentrator, and realizing that you’re almost out of battery power. What this means is that you’ll need to stop whatever you’re doing and rush back home or to the nearest electrical outlet to charge your device. The SimplyGo Mini, however, offers considerable battery life that will allow you to stay out and about longer.

On a flow setting of 2, you’ll get up to 4.5 hours out of the 8-cell battery and up to 9 hours with the 16-cell battery. For most people, this is more than enough battery life to get through the day. However, if you still need more, you can always purchase an additional battery and keep it in the accessory pouch then just replace the battery that’s on your unit whenever it runs out.
A Simple Design That’s Easy to Operate
Another thing that people expect nowadays are devices that are easy to operate. Life can be complicated enough, so there’s no need to overcomplicate it with an oxygen device that’s difficult to learn and use. From the video above, you’ll see just how easy it is to pull the SimplyGo Mini out of the box and start using it right away. One of the unique features it offers is a full touch interface meaning you won’t have to hassle with any buttons that are difficult to depress. It also makes it a lot easier to clean the device than it would be otherwise.

In order to prevent downtime in your oxygen delivery, Respironics has also made it very easy to swap out batteries on the fly. When your battery starts to run low, simply press the tab and slide the battery off of the side of the unit. You can then slide on a fully charged battery until it clicks into place. This can all be done in a matter of seconds so you can get back to using your oxygen device as quickly as possible.
A Plethora of Oxygen Accessories to Choose From
One of the greatest things about buying a Respironics product is that you can rest assured you will have many accessories to choose from that help you make the most of your purchase. Whenever you purchase a SimplyGo Mini from us, you’ll receive the following items:
- Respironics SimplyGo Mini Portable Oxygen Concentrator
- 8-Cell Battery
- AC Power Supply
- DC Power Supply
- Custom Carrying Case
- Padded Shoulder Strap
- Padded Handle Strap
- Tubing
- Manual
- 3 Year Warranty

In addition to all of these items, you can purchase a whole host of accessories that are sold separately like the external battery charger. Normally, you would have to charge your batteries when they’re attached to the concentrator, but this accessory allows you to charge them separately. In other words, you’ll be able to charge two batteries at the same time.
Another accessory sold separately is the battery packs. If you’re someone who’s away from home frequently you can always purchase an additional 8-cell or 16-cell battery in order to effectively double your battery life. The SimplyGo Mini accessory bag and backpack are also great options if you want to be able to carry all of your accessories more easily.
Conclusion
While the SimplyGo Mini is one of our top picks as one of the best portable oxygen concentrators, it’s important to find the oxygen device that’s right for you and your needs. That’s why our oxygen concentrator specialists are always on hand to answer any questions you may have about POCs. If you’re not sure where to begin, we’ll guide you through the whole process from choosing a concentrator, to discussing your buying options, and even collecting medical paperwork like your oxygen prescription. Either give us a call at 1-888-416-3855 or reach us by email at info@lptmedical.com to get started.
Respironics SimplyGo Mini Specs:
|
Weight |
5 Pounds |
|
Dimensions |
9.4” H x 8.3” W x 3.6” D |
|
Flow Rate |
Pulse Flow Settings 1-5 |
|
Battery Life |
Up to 9 Hours |
|
Power |
100-240 VAC, 50/60 Hz; 19 VDC |
|
FAA Approved |
Yes |
|
Warranty |
3 Years |
Oxygen Output
|
Flow Setting
|
Oxygen Output
|
| 1 | 220 ml/min |
| 2 | 440 ml/min |
| 3 | 660 ml/min |
| 4 | 880 ml/min |
| 5 | 1000 ml/min |
Over 16 million Americans knowingly have COPD, meaning they have been diagnosed with COPD and are currently treating their COPD. The harsh reality for all of these people is the COPD has no cure, this progressive disease will stick with you, and if gone untreated take years off of your life. That being said, treating COPD has been heavily researched, and following a treatment plan for your personal diagnosis will increase your life expectancy.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
This blog is an informative read for anyone who has COPD no matter how severe or mild. It's also a great read for you if you are perfectly healthy and are a caregiver for a COPD patient, or you are just curious about your respiratory health, this blog is a great read for people who are curious about how COPD affects life expectancy.
Treating COPD to Increase Life Expectancy
The only way someone with COPD can add years to their life is by using oxygen therapy. Oxygen therapy is when you need to use a supplemental oxygen device like a portable oxygen concentrator in order to maintain a healthy oxygen level. Once your oxygen levels are stable, you can begin to treat COPD in other ways that will slow down the progression of the disease and ease the severity of the symptoms.

The symptoms of COPD you you should be treating can be any of the following:
- Cough
- Breathlessness
- Mood swings
- Fatigue
- Excess production of mucus
If COPD goes untreated, the consequences are extreme, and if you are reading this blog it is likely that you already know you have COPD, or you are in the process of being diagnosed with COPD. If your case is the latter, getting tested for COPD will be the first step towards treating your symptoms. The longer you wait to get tested, the more time goes by where the progression of your disease worsens at a faster pace due to inadequate treatment.

Life expectancy is directly related to how you treat COPD, and because this disease does not have a cure, proper treatment is the only fight against time you have when it comes to living with COPD.
You can treat your symptoms above by following your doctor's recommendations and this will likely include some or all of the following treatments:
- Exercise, try yoga or tai chi for respiratory patients
- Eat foods that promote respiratory health
- Join pulmonary rehabilitation courses
- Follow your oxygen prescription if you have one
- Use you COPD medications as prescribed
- Avoid lung irritants such as allergens, pollution, and smoke
- Stop smoking cigarettes or inhaling secondhand smoke

Even with treatment COPD symptoms will arise in your daily life, you can learn to deal with symptoms by trying some of the following methods for easing discomfort:
- Breathing techniques can be used to open your airway and increase lung strength, this will help with breathlessness
- Meditation particle can help your breathing when you experience a COPD exacerbation, it can also help easy anxiety and stressed caused by breathlessness
- Coughing and clearing techniques can be used daily to removed excess mucus from you airways which can help ease your coughing and breathlessness
COPD Diagnosis
First and most importantly, being diagnosed with COPD is a good thing, and this might sound crazy, but you cannot go back in time and change the course of time in which you developed COPD, so being diagnosed is the next best thing. And here is why: Once you have been diagnosed with COPD, your life begins again, you start to take care of the symptoms that have been impacting your life, you start to ease the pain and discomfort by utilizing tools like medications, oxygen therapy devices, and pulmonary rehabilitation courses.
People with COPD are are more likely to experience the following complications compared to someone without it:
- Being limited in physical activity
- Difficulty walking or climbing stairs
- Be unable to work
- Need special equipment like Inogen brand oxygen devices
- Engages less socially
- Have increased confusion or memory loss
- Have more emergency room visits or overnight hospital stays
- Have other chronic diseases like arthritis, congestive heart failure, diabetes, coronary heart disease, stroke, or asthma
- Have COPD induced depression or other mental or emotional conditions
There’s No way to Predict the Exact Life Expectancy
The obvious question is, “How long can I live with COPD?” but there is no way to predict the exact life expectancy despite the stage of COPD you are in. That being said, it is known that having this progressive lung disease can shorten your lifespan.
But how much this disease shortens your lifespan depends on your overall health, how you treat the disease on the daily, and whether you have other diseases such as heart disease or diabetes.
What is the GOLD System
COPD effects over 16 million Americans, and research about this disease has a long history and is ongoing. There have been numerous studies that assess the health of someone with COPD all of which have contributed to the GOLD system.
The most current assessment is to take a spirometry lung function test results and compare that to a person’s symptoms. The result can help predict life expectancy but more accurately guide treatment choices for those with COPD.
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) is one of the most used systems of classifying COPD and its effect on your health.
GOLD is made up of an international team of lung health experts who look over current research and produce updated guidelines for doctors to use for testing and treating people with COPD.

Recently, doctors started to use the term “grades” rather than “stages” to assess the degree of severity of the disease. Grading is a way to measure the severity of a person's COPD. It uses the forced expiratory volume (FEV1) to determine the amount of oxygen a person can actively exhale from their lungs in one second, this gives the doctor a rather accurate description of the person’s lung health and allows them to categorize the severity of their COPD.
Based on your FEV1 score, you receive a GOLD grade as follows:
GOLD 1: FEV1 of 80 percent predicted or more
GOLD 2: FEV1 of 50 to 79 percent predicted
GOLD 3: FEV1 of 30 to 49 percent predicted
GOLD 4: FEV1 of less than 30 percent predicted
The second part of the GOLD system is to compare the FEV1 score to the patient's symptoms. Doctors will analyze your symptoms of dyspnea, or difficulty breathing, and degree and amount of acute exacerbations, which are flare-ups that may require hospitalization.
How these aspects of health compare will categorize people in one of four groups: A, B, C, or D.
Grouping COPD Severity, Examples:
Here are some examples of how COPD patients are put into groups.
- Patients X experiences no exacerbations or maybe one and they did not require hospitalization in the past year. Their breathing assessment or their FEV1 score was GOLD 1 and the amount they only experience a few symptoms they have would be in group A.
- Patient Y has had one exacerbation that required hospitalization, or possibly two exacerbations that did or didn’t require hospital admission in the past year. They also scored GOLD 3 and had several breathing symptoms that would be in group C.
Under the most current GOLD guidelines, someone who scored a GOLD Grade 4, Group D, is someone that has the most serious classification of COPD. And they’ll technically have a shorter life expectancy than someone with a label of GOLD Grade 1, Group A.
What is the BODE index
There are other measures that can be taken to determine the severity of COPD by using more than just the FEV1, it is called the BODE index.
BODE stands for:
B - body mass
O - airflow obstruction
D- dyspnea
E - exercise capacity
This is a measure of the overall way COPD affects your life. Keep in mind that while the BODE index is used by some doctors, its value or meaning behind the results may be less accurate than what it was once considered due to the amount we know about the disease now.
Body mass
By looking at you body mass index (BMI), a measurement based on your on height and weight, it can be known if you are overweight or obese, or too thin. Someone who is very thin and has COPD has a lower outlook.
Airflow obstruction
This refers to the FEV1, which is the same test as in the GOLD system that you read in the section above.
Dyspnea
Having trouble breathing is something that can be noted in order to assume the outlook for someone with COPD.
Exercise capacity
Being more tolerant of exercise and having the ability to be physically active suggest you have a better outlook. It’s often measured by a test called the “6-minute walk test.”

Mortality Rates in COPD Patients
COPD is a serious disease and similarly to cancer, the predicted life expectancy is based largely on the severity or stage of the disease which for COPD can be estimated using the GOLD system or BODE.
One of the best ways to explain the mortality rate in COPD is to give an example:
In study that was in the International Journal of Chronic Obstructive Pulmonary Disease, a 65-year-old man with COPD who currently smokes tobacco has the following reductions in life expectancy, depending on stage of COPD:
GOLD 1: 0.3 years
GOLD 2: 2.2 years
GOLD 3 or 4: 5.8 years
For this same group, if the 65 year-old man were to continue smoking they would be reducing thier life expectancy by an additional 3.5 years, rather than those who never smoked and didn’t have lung disease.
For former smokers, the reduction in life expectancy from COPD is:
GOLD 2: 1.4 years
GOLD 3 or 4: 5.6 years
This is just one article that was published and while there is a lot of research on this subject, the mortality rate for COPD patients is still just an estimate.
Continue Treating COPD for the Best Outlook

What’s the goal of these methods to predict life expectancy? The more you are able to treat your disease the slower you will progress to a higher grade of COPD.
The first step towards slowing down the progression of COPD is to stop smoking if you smoke. Also, avoid secondhand smoke or other irritants such as air pollution, dust, or chemicals.
Maintaining a healthy weight and eating small, frequent meals can help your breathing immensely. Learning how to improve breathing with exercises such as pursed lip breathing will also help.
Pulmonary rehabilitation program is another great way to learn about your disease as well as how you can implement exercise into your life safely and effectively, all while connecting with other people that can relate to your health condition.
One of the very best things you can do for you lung health is to exercise, and while physical activity may be challenging it really helps your lungs and the rest of your body.
The bottomline is that, the more you can do to improve your overall health, the longer and fuller your life can be.

Flu season is just about in full swing here in the northern hemisphere. October through March are the coldest months of the year, creating a viable environment for the flu virus to spread and infect peoples' immune systems. Many people are wondering if they should get a flu shot this year, and you might be curious about the same thing.
Considering the state of the world, and our continued efforts to mitigate, manage, and survive the COVID-19 pandemic, some people may be hesitant to get a flu shot this season, especially those who are immunocompromised and ones with pre-existing conditions.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
However, catching the common flu can be just as scary and harmful as catching COIVD-19 for people who suffer from COPD and other respiratory illnesses. So the flu vaccine is imperative for people who are trying to stay away from the hospital this season, and to help minimize their impact on the already influx of hospital admissions due to COVID-19.

It is also concerning for healthcare workers and infrastructures going into this flu season because the flu and COVID-19 have similar symptoms and oftentimes, cases require similar equipment from hospitals and health labs, which makes the COVID-19 pandemic during another flu season even more concerning.
As one of the leading local medical oxygen equipment company in Boca, Raton Florida and a long-time established medical equipment company in Denver, CO, we are dedicated to keeping our communities safe and protected while we continue to offer our customers alternative oxygen therapy devices.

In this article we are going to talk about the flu vaccines, and why it is so important for our community of respiratory patients and COPD caregivers to get a flu shot this season. We will answer a few questions that will clear up any uncertainties about getting the flu vaccine. If you use a portable oxygen concentrator, you already have an advantage in staying healthy throughout the flu season, but getting a flu shot is still
But first, we want to give some of our reader the local web-pages where the Center for Disease Control (CDC) tracks the flu season in a particular area weekly. You can stay up to date about the severity of the flu in your state, simply by clicking on the state you live in on this map:
Here is the Florida Flu Review
Here is the Colorado Flu Review
COPD and the Flu
If you have COPD, preventing acute exacerbations is crucial to reduce your disease severity and to prevent and slow down COPD progression. Avoiding exacerbations also means reducing the frequency of hospitalizations, and other high costs associated with the illness. Habits such as smoking, illnesses like bronchiectasis, factors including severe airflow limitation, and lastly infection are all identified as exacerbation triggers for people with COPD.
In order to avoid the misfortunes of dealing with a COPD exacerbation, and to limit both the short and long term effects, means getting your annual flu vaccine, and sooner rather than later.
Limiting your potential to catch influenza as a COPD patient is important, so you must wash your hands, avoid large crowds, disinfect often, exercise, sleep well, and most importantly get the flu vaccine. We know there are some hesitations when it comes to vaccination, so we gathered a few of the most frequently asked questions, so you feel confident getting you flu shot this year, and every year afterwards.
What is the flu vaccine? Why do I need one every year?

The flu vaccine can be taken as a shot that is injected into your arm or the flu nasal spray (which is not available every year). The vaccine is new every year, because the nature of viruses is how they quickly adapt and change in order to survive, therefore the vaccine must stay up to date with the newest most invasive virus strains.
The flu shot is a dead virus, when you get a shot your immune system creates the antibodies against the dead viruses, and your antibodies are able to protect you from being infected by the live virus.
When is the best time to get vaccinated?

There is no bad time to get vaccinated, but October-December is when the flu season starts to pick up, and getting the shot within this window will protect you through the flu season. Earlier is great too.
Even if it seems too late to get the flu shot, remember that if you’re being offered the flu shot, it’s because there’s the flu virus is still around. So definitely don’t hesitate if you have the opportunity to get the vaccine.
How is the flu vaccine made every year?
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
In order to keep track of the changing viruses, flu experts around the world within more than 100 influenza centers around the world research the different flu variations,. They go through intensive experiments to identify which strain will be the most common in a given season. Whichever strain they find to be the prevalent, will determine the flu vaccines “ingredients” that year.
This research process helps create a flu vaccine that’s specific to the common flu strains expected that winter, however it is not always a perfect science. This is why some years the vaccine will protect against the flu more effectively than other years.
Some years the vaccine does not provide your antibodies with the correct protections for your immune system to combat the virus, in which case the flu season will be worse overall.
.jpg)
Is it possible to get the flu from the flu vaccine?
This is probably one of the more frequent and concerning questions that people commonly mis-understand. This is cause for concern because mis-information can lead to less and less people getting the flu vaccine.
There are a lot of people who would argue that there is no point in getting the flu vaccine, and the strongest defense against the flu, are healthy habits like washing your hands, eating healthy, sleeping more, and exercise, which might be true for young adults in good shape with no health conditions.
However, people who suffer from a chronic illness, autoimmune disease, and people in poor health should try to practice these healthy habits, but also get the flu vaccines.
The bottomline is that, the flu shot is an inactivated or “killed” virus, which means you can’t get sick from the shot. The flu shot is a dead virus, when you get a shot your immune system creates the antibodies against the dead viruses, and your antibodies are able to protect you from being infected by the live virus.
The nasal spray flu vaccine does contain a weakened live virus — but it is not strong enough to cause the flu for most people.
However, like we mentioned before, sometimes the strain of the flu vaccine does not protect against that winter’s particular virus strain perfectly. That being said, for those who are vaccinated against flu and still get the flu, their symptoms are typically milder due to their vaccination.

Are there side effects from the flu vaccine?
While the flu vaccine cannot give you the flu, it can cause a few symptoms. The most common side effects are tenderness, redness, or a bit of swelling at the injection site.
You might not experience any of these symptoms but you can prepare to experience a few days of muscle soreness in whichever arm you get the vaccine, so you can opt to get the shot in your non-dominant arm.
It’s also possible to develop a low-grade fever, headache, or nausea, but these symptoms should go away within a couple days.
The nasal spray flu vaccine could also cause a runny nose, sore throat, and cough, however serious adverse effects are not common. In fact the risks you take to get a vaccine are far lower than the risks you’d run from getting the flu itself.
You should contact your doctor if you experience a high fever or signs of a severe allergic reaction like difficulty breathing, dizziness, or a rapid heartbeat. These types of reactions would most likely happen within a few minutes to hours after getting the vaccine, and can be treated with medical attention.
Are allergic reactions to the flu shot common?
Some people do have an egg allergy, and if you have a severe allergic reaction to eggs, you should avoid flu vaccination. If you’re mildly allergic, talk to your doctor because you still might qualify for the vaccine.
If you have a mercury allergy you shouldn’t get the shot either. Some flu vaccines contain trace amounts of mercury to prevent vaccine contamination.
If I got sick from the flu vaccine before, should I get one again?
Many types of viruses can cause cold and flu-like symptoms, but the flu shot only protects against the influenza virus, which is the common flu that we all try to avoid come winter because it is the most severe. It may be possible that you catch a different virus that the vaccine does not protect against, but you can rest assured that the virus you caught is much less severe than the influenza virus you might have caught without the flu vaccine.
Getting vaccinated is the best way to protect yourself and the ones you love from influenza. While you cannot get influenza from a flu shot, it is not rare to feel a little under the weather after receiving it. This only means that your immune system is responding to the vaccine, and it is actually a good thing.
How do you get vaccinated without using a needle?
There is a flu mist nasal vaccine. The difference between the shot and the nasal spray is that the flu nasal spray vaccine is a live "weakened" virus, while the shot is a “dead” virus. The nasal spray is a severely weakened virus that will cause a small brief infection in your nasal passages but most people don’t even notice it.
If you have a condition that affects your immune system may not be able to take the nasal spray because it is a live virus and it may cause you to get ill. The flu nasal spray has been approved for healthy people ages 2 through 49 years old.
There is also a CDC-approved list of people who shouldn’t get the live flu nasal spray vaccine.
How do I get vaccinated if I don’t have health insurance?

This is a serious question, and just because you don’t have insurance doesn’t mean you are not able to get a flu shot. You have a few options. You can pay out of pocket, in most places a flu shot will cost about $40, and slightly more for the senior dose.
Before you pay out of pocket, you can research websites like Blink Health or GoodRx and try to find discounts for vaccines available in your area. For example, if you live in Boca Raton, FL flu shots will be available at a pharmacy near you, to find one you can type you can your zip code into VaccineFinder.
Sometimes there are ways that you can get a free or discounted flu shot. Some schools and workplaces will hold events to offer a flu shot to members within their communities. For instance, in Boca Raton, Florida the Boca Helping Hands mission took place in partnerships with Walgreens and the Boca Raton Regional Hospital to off free flu shots to clients, volunteers and staff that are eligible to receive them.
Overview
The flu shot is an essential societal duty that everyone should partake in to help protect themselves and the people around them from the common flu. Even if you are a perfectly healthy adult, getting the flu might not seem like a very big deal, and you might miss a couple days off work. But for a super healthy person to spread the flu to others greatly increases the chances of a a chronically ill patient coming down with the flu, this is a far bigger deal.
People with COPD are often times hospitalized because they caught the flu and have severe COPD symptoms, or even an exacerbation as a result. If you have COPD be sure that the people in your life that you interact with have gotten the flu vaccine for your own sake, and if you haven't gotten vaccinated yet, be sure to schedule an appointment at you doctor or local pharmacy to get a flu shot as soon as possible.
For more expert advice about the flu shot, you can click here to read this HealthLine article, that touches on even more topics so you feel confident going in for a flu shot every year.
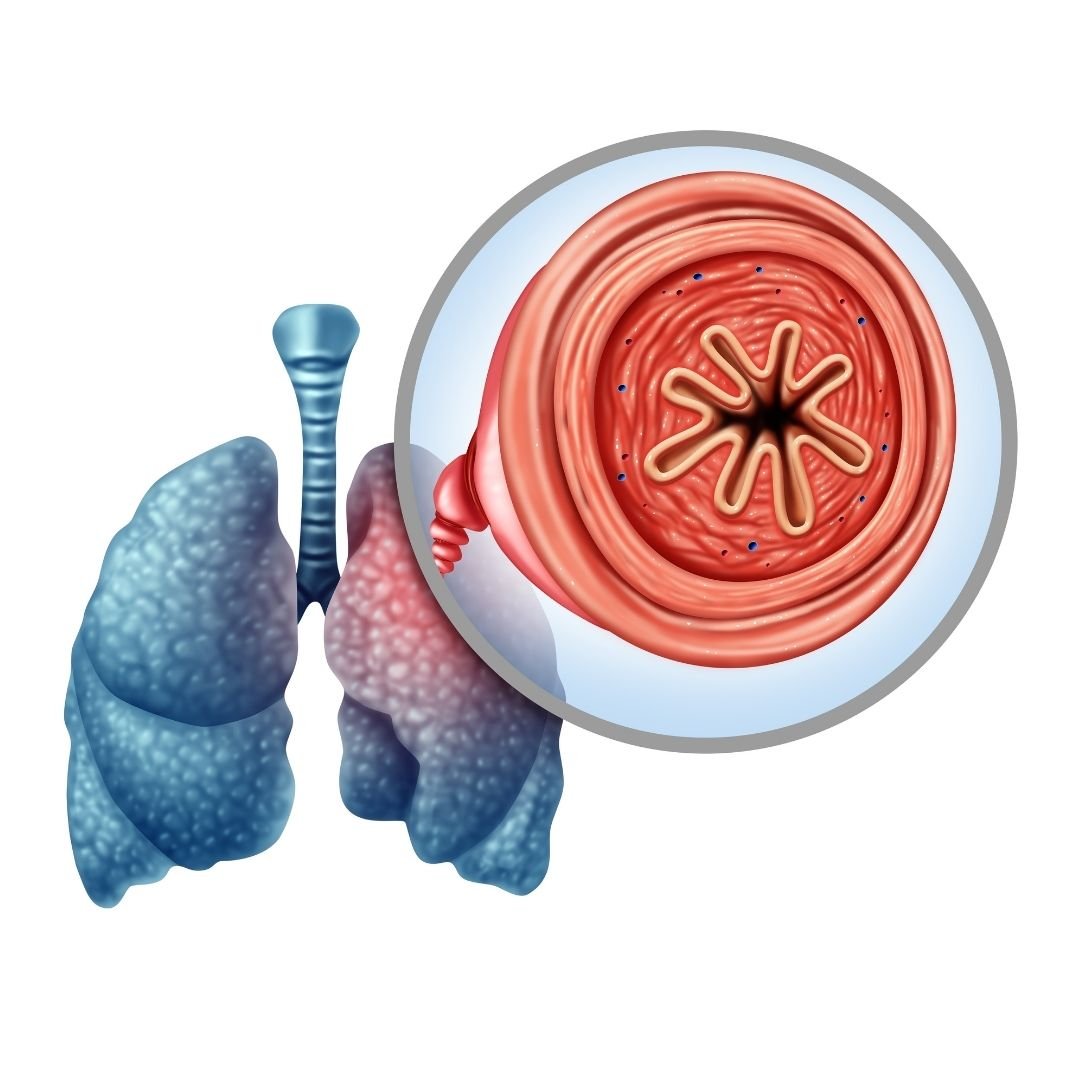
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease. COPD is an umbrella term for diseases like emphysema and chronic bronchitis. COPD comes in stages with stage one being mild and four being the very last stage. There is a need to improve the quality of life and slow down progression into subsequent stages.
To do this, it is imperative that a patient goes through pulmonary rehabilitation. This program arms you with the necessary skills to participate in everyday activities without a struggle by teaching you how to properly exercise and diet among other important aspects.
You will also learn breathing techniques and how to get the most out of your inhalers among other useful tidbits.The result of attending pulmonary rehab is less frequent and shorter periods of hospitalization. Faster recovery after exacerbation has also been noted. The exercise is good for consequent anxiety and depression due to the production of endorphins. The program, if ordered by a doctor will be covered by medical insurance.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2')}}
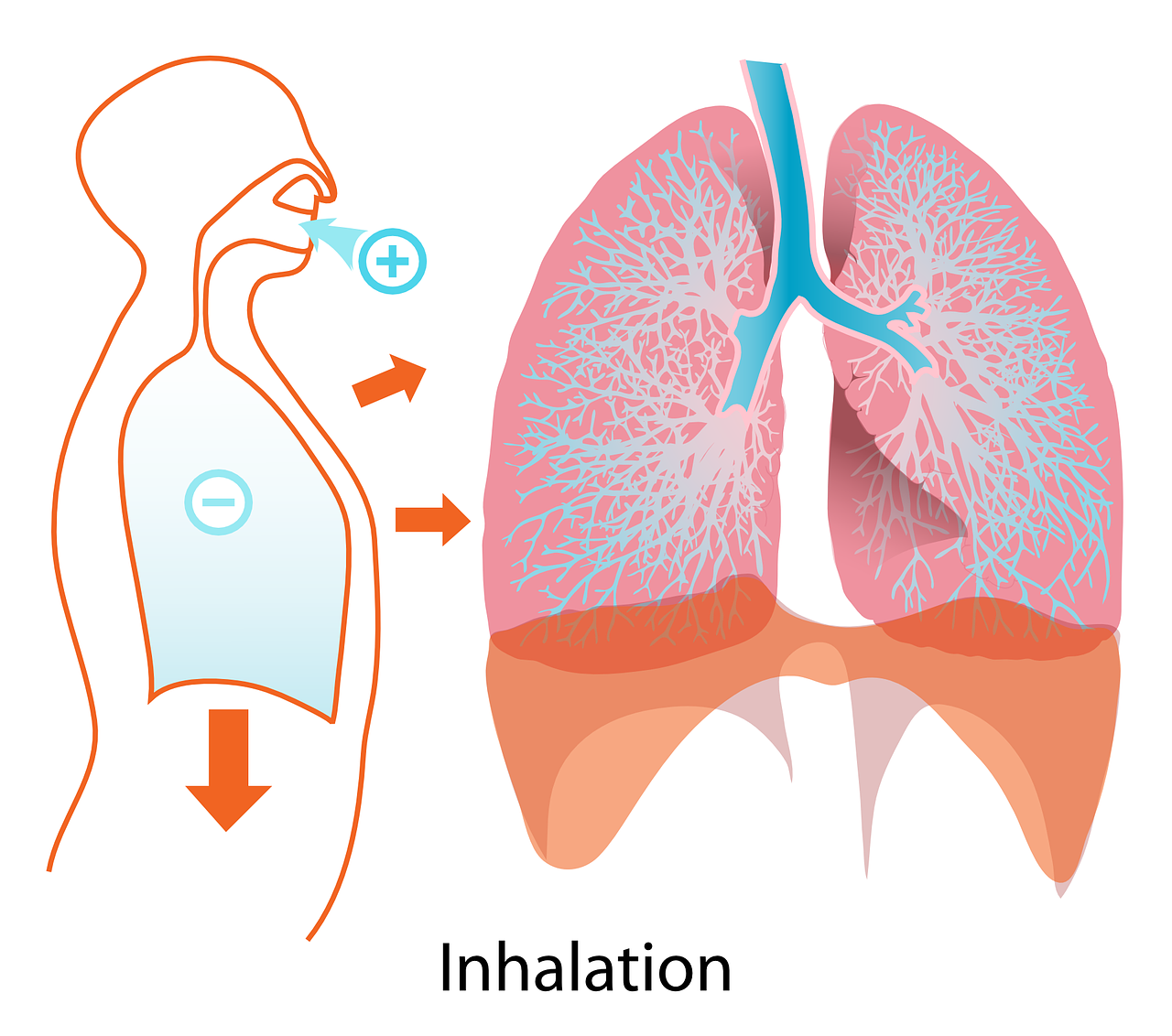
Exercise

Physical activity can be strenuous for a person with COPD. They will often suffer shortness of breath after a short walk and other simple activities.This is because the disease decreases lung function and weakens respiratory muscles. The program arms the patient with tips on how to exercise successfully.
With time, the patient is able to tolerate more activity that is physical. It is advisable that a patient starts small, then gradually increases the intensity of exercise. A good exercise has three parts: a warm up, conditioning and a cool down. The warm up prepares the body for the impending calorie burn. It also prevents muscle injury and increases range of motion.
The conditioning stage is where the party truly starts. In this stage, cardiovascular exercises like walking, jogging, water aerobics, cycling and jumping rope will be good. The cool down can last five minutes and stretching would be enough to allow the body recovery time.
General exercise guidelines may be followed. Like not exercising less than one and half hours after a meal. It is advisable to exercise in the morning because that is when the body is at its peak. Exercise for twenty minutes a day, three times a week is a good place to start. The patient is advised to exhale twice as often as they inhale through pursed lips.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Stop Smoking

It is estimated that 10-15% of smokers will develop COPD. After cessation, the difference can be felt within 24 hours. Improvement on blood pressure and heart rate is significant.
In a year, cardiovascular events are less probable by half. Naturally, lung function declines with age. Smoking heightens the rate. To reduce the progress of COPD into advanced stages, a patient should stay away from the cloud permanently.
This is the number one way to modify the natural course of COPD. Studies have shown that women gain the most from tobacco treatment than men. This is not deterrent though as both parties do enjoy a reduced rate of decline of lung function.
What to Eat

After metabolism, the body gains energy and carbon dioxide. The carbon dioxide is waste. COPD patients use a lot more energy when breathing and therefore need up to ten times more calories in their diet.
A prescribed diet will keep the weight optimal. Too much weight will put pressure on the lungs and respiratory muscles. Too little weight will make the patient frail and weak.
A good diet also helps long term bronchodilators work better and reduces the use of rescue medication. One should take plenty of fluids to keep the mucus thin and easy to cough up. Mucus will block airways and cause exacerbation.
Patients should not overeat and should opt for more frequent and smaller meals instead of the traditional three meals. High fiber foods are also recommended. It is important that a patient exercise sodium control. Before using other salt supplements, they should consult. The same applies to alcohol intake. They should take smaller bites to ease breathing and eat while sitting up.
Arsenal of Information

The quality of life of a COPD patient can be significantly influenced by their self-management capabilities. The only way for patients to manage themselves successfully is to have a lot of information about their condition. The program also avails the same information to family members. This ensures that proper care is taken and exacerbations are attended to appropriately.
Often, sleeping position might affect breathing. This can be quite alarming but after going through the program a patient will know that all they have to do is sleep on their side with the head elevated to keep airflow smooth. Patients are also made aware of trials like those involving use of stem cells to repair damaged lungs.
Support
Living everyday knowing that something as minute as strong cologne might set off an exacerbation and quite possibly death is depressing and soul crashing. It is easy to just curl up and wait for death. In addition to medical support, patients will often need emotional and psychological help. There are many blogs where people post their stories and words of encouragement for those on the same COPD boat.
There are also support groups where one can find solace for the bad days. The pulmonary rehabilitation program will direct the patient to these. They will also connect them with excellent COPD specialists. Support might not heal the disease but it will make them feel a little better.
After a patient has completed the program, it is paramount that they stick to the prescribed diet and exercise schedule. Exercise may be as simple as walking up and down the stairs for ten or twenty minutes every day or taking a walk in the park.
This is the only way to ensure continuation of wellness and long term positive effects. Morbidity and mortality, though still quite pronounced, is pushed further away from the patient’s mind. With pulmonary rehabilitation, a COPD patient can live life without letting the impending doom falter their steps.

Winter and cold season are right around the corner, and it's important if you have chronic obstructive pulmonary disease (COPD) that you avoid pneumonia and remain healthy this season.
COPD is the third leading cause of death in the United States, and pneumonia is the eighth leading cause of death in the U.S. Contracting pneumonia could be deadly for someone with COPD. Check out the following information to stay healthy this upcoming fall and winter!
Who is most at risk for developing pneumonia?
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Young children, cigarette smokers, and adults over the age of 65 with certain medical issues, including COPD, are at the highest risk of developing pneumonia.
How do you contract pneumonia?
Pneumonia is most normally caused by the exchange of bacteria, viruses, and on occasion, but less commonly, fungi. Often those individuals who contract pneumonia due to a fungi struggle with suppressed immune systems.
Many of these viruses and bacteria exchanges are preventable with a plethora of helpful vaccines such as vaccinations for:
- Influenza
- Pneumococcus
- Measles
- Pertissis, or Whooping Cough
- Haemophlilus influenza type b (Hib)
How do I know if I have pneumonia?

Symptoms of pneumonia appear very similar to symptoms of COPD. It is extremely imperative that if you struggle with COPD you are aware of the symptoms of pneumonia.
Such symptoms include:
- A fever over 100.5 degrees Fahrenheit
- Shaking chills
- Changes in breathing patterns (shortness of breath or more rapid breathing)
- Nausea, vomiting, or diarrhea
- A cough with an increased amount of sputum (mucus)
- A cough with a change in color of sputum (mucus)
- More rapid heart rate
- Pain in one area of the chest from deep breaths
As you can see, if you have COPD, many symptoms of pneumonia look similar to those of COPD. Oftentimes people with COPD aren't sure if the symptoms they are showing are from pneumonia or worsening or exacerbated COPD.
Unfortunately, many individuals will wait to seek treatment which can be fatal or lead to longer hospitalizations. If your COPD symptoms change slightly or worsen, contact your doctor immediately. This preventative action could stop the pneumonia in its early stages and thwart further health complications and even death.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
What are some ways I can avoid pneumonia?

There are several ways you can avoid pneumonia when you suffer from COPD. The following list consists of comprehensive methods you can carefully apply to avoid contracting pneumonia:
-
Be sure to check in with your doctor or healthcare provider for your regularly schedule appointment so you both can keep a close eye on your COPD and if it potentially worsens.
-
Every year, get a flu shot at your local pharmacy or grocery store. They can administer flu shots easily and often for free.
-
Check with your doctor or healthcare provider to see if you are due for a pneumonia shot. A pneumonia shot can help considerably reduce one's risk of developing pneumonia.
-
Wash your hands regularly with soap and water and carry hand sanitizer with you if you don't have regular access to soap and water throughout your day.
-
Be sure to especially avoid crowds during cold and flu season.
-
When you are in public areas and crowded spaces, avoid touching your eyes, mouth, and nose to prevent the spread of germs throughout entire body.
-
Make sure to get adequate sleep. When the body is well rested, you are at a lower risk of getting sick. Aim for at least 7-8 hours per night.
-
Regular exercise can benefit your body in multiple ways, especially in boosting your immune system, which can help in avoiding pneumonia.
-
Eating a healthy diet filled with plenty of fruits and vegetables is beneficial in avoiding infection.
- Don't smoke. If you haven't already, work on quitting. Smoking makes it much harder for your lungs to ward off infections like pneumonia. Smoking may also impact one's awareness of worsening COPD symptoms that may in fact be pneumonia.
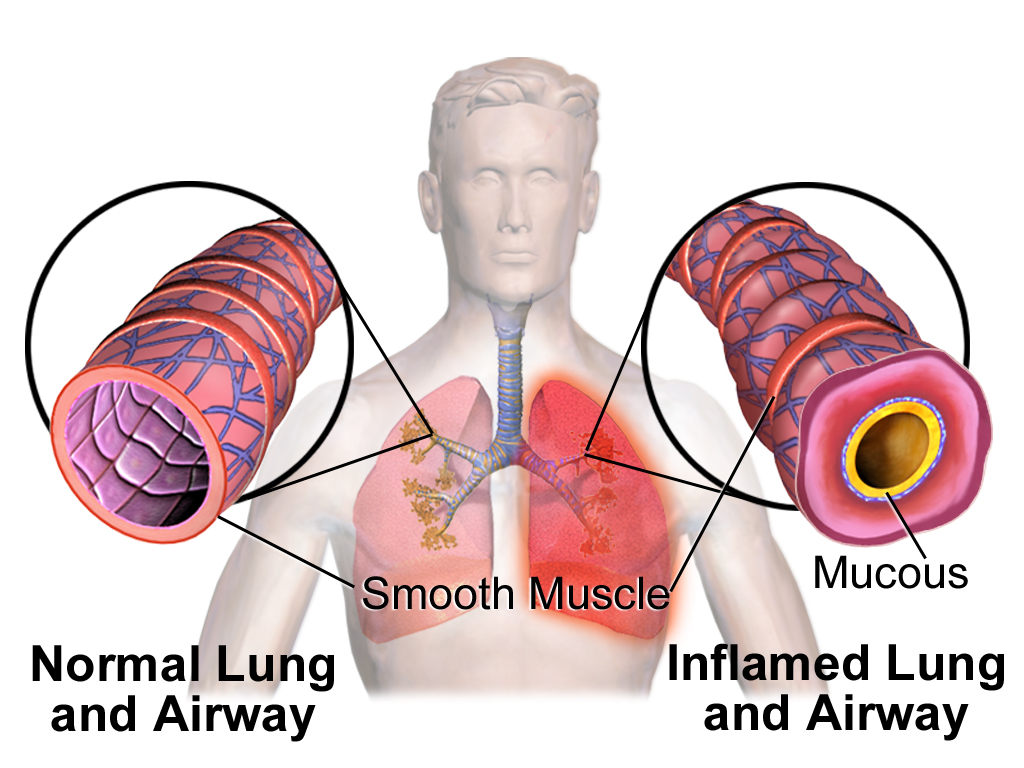
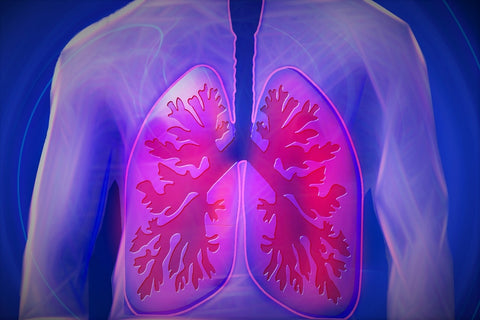
Complications with your COPD do arise if you develop pneumonia. Long term and permanent damage may occur; however, early treatment can aid in decreasing these potential outcomes. It is imperative that you know how pneumonia can affect your lungs.
Indeed, inflammation from pneumonia can limit airflow throughout the lungs which can further damage lungs; thus, if you have COPD and pneumonia you are at a notably greater risk of respiratory failure. Respiratory failure is a response from the body it isn't obtaining enough oxygen or expelling enough carbon dioxide.
A deprivation in oxygen, or what is known as hypoxia, can lead to additional complications for individuals diagnosed with COPD such as:
- Damage to kidneys
- Various cardiovascular issues including stroke and heart attack
- Irreversible brain damage
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
So how is pneumonia treated in patients with COPD?

-
To begin, the patient with symptoms of pneumonia and/or worsening COPD will be admitted immediately to a hospital
-
Your doctor may order chest-x-rays, CT scans, blood work, and/or may take a sputum (mucus) sample in order to diagnose the patient properly.
-
A doctor may prescribe the patient antibiotics which are administered intravenously at the hospital. Added antibiotics may also be prescribed for you to take at home.
-
A doctor may prescribe glucocorticoids, a medication taken via an inhaler, a pill, or an injection. This medication helps to reduce inflammation in the lungs, thus assisting your breathing.
-
A doctor may prescribe other medications in nebulizers and/or inhalers to help you breathe better and manage their own COPD symptoms.
- Supplemental oxygen and ventilators may also be prescribed for you to utilize in order to increase your body's oxygen flow.
Symptomatic awareness and precautions can help you treat and avoid contracting pneumonia. With early detection of pneumonia, you will experience fewer complications and hopeful outcomes if diagnosed with pneumonia.
Tune into your body and keep a close eye on your COPD symptoms as the temperature drops and the weather transitions towards winter. Use some of the aforementioned prevention methods to evade pneumonia as cold and flu season approaches! As always, keep in contact with a trusted doctor or healthcare provider as you continue to monitor your COPD.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













