Lung function decline is a defining characteristic of COPD, and it gets worse as the disease progresses. Because of this, most COPD patients eventually have to begin using supplemental oxygen to help their lungs once they become too weak to absorb enough oxygen on their own.
The purpose of supplemental oxygen is to deliver extremely oxygen-rich air to your lungs, usually using a pressurized oxygen tank or an oxygen concentrator. This air, generally about 85-95 percent pure oxygen, allows your lungs absorb more oxygen with every breath.
Supplemental oxygen is a very important part of COPD treatment because it helps your lungs take in enough oxygen to supply your organs and tissues with the oxygen they need. Without it, your blood oxygen saturation can fall to unhealthy levels—a condition called hypoxemia—which can lead to serious, life-threatening complications over time.
Supplemental oxygen is also important for treating acute COPD symptoms, and can help you when you feel breathless from exercising or when your symptoms flare up. Many patients also use supplemental oxygen when they sleep to treat low blood oxygen levels during the night.

Despite how often supplemental oxygen is used and prescribed, it can be dangerous if you don't understand the risks. Oxygen is highly flammable, and you have to take special precautions when you use it to reduce the risk of a fire.
Even though they are rare, oxygen leaks and major fires can happen if you don't practice proper oxygen safety. High oxygen levels can make objects that wouldn't usually be a risk highly flammable, such as grease and oily creams. It also causes fires to burn hotter and spread faster than they normally would.
Even small sparks or flames can can cause combustion when there's excess oxygen in the air, which is why it's so important to understand how to use your oxygen safely and minimize the risks.
In this article we're going to show you how to practice proper oxygen safety so you can avoid accidents, injuries, or fires from using supplemental oxygen. We'll explain the benefits and risks of oxygen therapy, how to minimize fire hazards, and tell you how to follow proper safety protocols when using, storing, and transporting your oxygen.
If you or a loved one uses oxygen therapy to treat COPD or another respiratory condition, then it's important for you to know how to use supplemental oxygen as safely as possible. This guide will teach you the basics and provide you with a variety of valuable tips you can use in your everyday life if you are prescribed supplemental oxygen.
The Potential Dangers of Using Supplemental Oxygen

Before we discuss how to use oxygen safely, it's important to understand the potential risks. If you know what to look out for, you're less likely to make a dangerous mistake.
The main immediate danger that supplemental oxygen poses is its flammability. When oxygen leaks out into the air from your tank, nasal cannula, or mask, it can raise oxygen levels in the room or in your immediate area, which significantly increases the flammability of everything nearby.
A certain amount of leakage from your nose and nasal cannula is inevitable, meaning there is a constant flammability risk when you use your supplemental oxygen. That's why you have to take a variety of fire-safe precautions any time oxygen is in use, even if your oxygen tank isn't nearby.
It is also important to make sure that all the oxygen from the tank goes straight into your lungs through your mask or nasal cannula instead of leaking into the air. Leaky tanks, faulty valves, and carelessness when opening and closing the valve can make the surrounding air extremely flammable, putting you, your belongings, and others nearby at risk.

Standard oxygen tanks, the most common type of equipment used to provide supplemental oxygen, pose hazards of their own, as well. The oxygen must be highly pressurized when it's stored in the tank, which means oxygen tanks can explode violently or “take off like a rocket” if the container is somehow damaged and ruptured.
You can avoid this danger by using an oxygen concentrator machine, but they tend to be pricier and harder to come by. Many patients don't have access to anything other than pressurized or liquid oxygen tanks because their budget, insurance, or medicare provider won't cover it.
The Benefits of Using Supplemental Oxygen

Despite the risks, supplemental oxygen is generally very safe to use as long as you use it carefully and as directed. It's also a very important part of treatment for people with COPD and other respiratory conditions who can't get enough oxygen to stay healthy on their own.
By raising your blood oxygen levels and taking some of the strain off your lungs, supplemental oxygen therapy can significantly improve COPD symptoms like breathlessness, coughing, wheezing, and fatigue. It can also help you be more active and participate in more of life's activities by making it easier to walk, exercise, and keep your symptoms under control.
Here are some more of the benefits you can gain from supplemental oxygen therapy:
- Improved mood and mental alertness
- Improved exercise ability and exercise endurance
- Improved energy and reduced fatigue
- Improved cardiovascular function
- Reduced hypoxemia and risk of hypoxia
- Improved sleep
- Reduced breathlessness
- Reduced risk of COPD complications including pulmonary hypertension and heart failure
- Overall improved quality of life
It's hard to overstate the importance of supplemental oxygen for COPD. If you doctor prescribes oxygen to you, it's vital that you use it exactly as directed according to your treatment plan.
Many patients don't follow their supplemental oxygen treatment regimen well enough because of inconvenience, aesthetics, or discomfort, but not using your oxygen as directed can worsen your COPD and lead to life-threatening complications, including heart failure. Talk to your doctor if you are having trouble using your oxygen or sticking to your treatment plan.
Tips for Using Oxygen Safely

Now that you better understand the benefits and potential risks of oxygen therapy, we're going to show you how to practice proper oxygen safety. There are many important precautions that everyone who uses supplemental oxygen must take in order to reduce the likelihood of fires and burns.
In the next sections, we'll give you a variety of tips for preventing oxygen leaks and minimizing fire hazards in your home. We'll explain all the different flammable substances and spark risks that you should look out for and how to safely cook while using oxygen at home.
We'll also give you advice on how to store and transport your oxygen tanks so they won't leak or get damaged. To learn all of this and more, continue reading to learn all about how to practice proper oxygen safety in and outside of your home.
Prevent Oxygen Leaks

One of the most important parts of supplemental oxygen safety is to prevent oxygen from leaking out of your tank or mask. If too much oxygen escapes into the air, it poses a serious fire hazard.
Even a small spark or heat from a stove burner can cause oxygen in the air to ignite and set fire to you or objects nearby. That's why it's important to know how to handle your equipment safely when you use supplemental oxygen.
Here are some tips for preventing oxygen leaks:
-
Always exercise care when turning the valve on your oxygen tank. Turn the valve slowly so you don't release too much pressurized oxygen at once.
-
Do not forget to close the valve on your oxygen tank when you are not using it. Take the time to double check if you aren't sure that it is closed all the way.
-
Visually inspect any oxygen tanks you have, including the valves, regularly. Check the outside of the tank for noticeable wear, tear, or damage, and check for any noticeable leaks.
-
Always store your tanks in a secure place where they won't tip, fall, or get damaged.
-
Liquid oxygen tanks will leak if laid on their sides, so it's particularly important to store liquid tanks upright with a cart or chains.
- Always use clean, undamaged tubing during oxygen therapy. Never use damaged equipment or tubing with holes or tears.
No matter how careful you are to prevent leaks from your tank and tubing, a small amount of oxygen will inevitably leak out near your nose and mouth while you use supplemental oxygen.
That's why it's so important to stay away from heat, sparks, and anything else that could cause the oxygen to combust. We'll go into this in more detail in the following sections.
Keep Heat and Flame Away From Your Oxygen

If you remember nothing else about oxygen safety, you should make sure you remember this: never, ever use your oxygen around an open flame. Doing so could quickly and easily cause a fire, which is why it's so important to keep your oxygen away from flames at all costs.
Open flames aren't the only hazard, however; even everyday heat sources like stoves and space heaters can also be dangerous. Anything with a heating element can pose a fire risk when you are using supplemental oxygen.
Here are some tips for avoiding heat and flame hazards when you use oxygen:
-
Be very cautious when using supplemental oxygen while you cook. Always move at least five feet away from the stove to use your supplemental oxygen, and never wear your nasal cannula near a gas stove or open flame.
-
Your oxygen tank and other equipment should also be kept at least five feet away from the stove and other heat sources at all times.
-
When you are using oxygen, beware of all sources of open flames: this includes lighters, matches, candles, fireplaces, cigarettes, gas burners, etc. Do not use any of these items or allow anyone near you to start a flame while oxygen is in use.
-
Do not smoke or use an electronic cigarette or vaping device while using oxygen. E-cigarettes contain heating elements that could potentially ignite the oxygen that collects around your nasal cannula, causing severe facial burns.
-
Place “oxygen in use” signs in visible places near all of the entrances to your home (these are usually provided by your oxygen supplier). This will ensure that visitors and emergency personnel know to be cautious of the high flammability risk.
-
Make sure to inform people around you of the risks of heat and open flame when you use oxygen. If needed, place a "no smoking, oxygen in use" sign nearby so others remember to be cautious.
- Take the same precautions that you would when using supplemental oxygen when you are near where you store your oxygen and extra tanks. Make sure you and everyone in your home knows where you keep your oxygen tanks and equipment and understand how to exercise proper fire safety.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Keep Your Oxygen Equipment Away from Electronics, Static Electricity, and Flammable Substances
|
|
| . |
While they don't pose as much of a risk as heated appliances and open flames, faulty electronic devices can also pose a fire hazard when you use supplemental oxygen. Some electronics and mechanical toys can also create tiny sparks that can cause fires in the presences of excess oxygen, which is why you shouldn't use them at the same time as you're using supplemental oxygen.
Another risk is static electricity build-up, the kind that happens when you drag your socks across the carpet or rub a balloon on your clothes. The "shock," or spark, that results when the static electricity dissipates can pose a fire risk when you are using supplemental oxygen. While it's impossible to avoid static electricity altogether, especially during the dry, winter months, you can reduce the risk of static sparks by avoiding certain types of clothing and fabrics.
Here are some tips for reducing the risk of fire from electronics and static electricity:
-
Don't use electronic appliances when using oxygen. This includes electric razors, mechanical toys, heating pads, electric blankets, electric toothbrushes, and electronic hair dryers, hair curlers, and hair straighteners.
-
Don't use any electronic device that produces heat when using supplemental oxygen. This includes electronic cigarettes.
-
Avoid static-producing fabrics like wool, nylon, and synthetic fabrics (e.g. polyester). Instead, choose clothing and bedding made of cotton, which is much less likely to produce static electricity.
-
Don't use any flammable products on your skin and hair, including flammable lotions, hair products, and hair sprays that could ignite due to heat or a static spark in the presence of oxygen. Especially watch out for products that contain petroleum and choose water-based ones instead.
-
Avoid using chapstick and oil-based lotions on your body, and especially your face, when using your supplemental oxygen, as they can cause severe burns if they ignite.
-
Avoid other flammable substances when using oxygen, including gasoline, paint thinner, cleaning fluids, aerosols, and sprays that contain alcohol.
-
Never use any aerosol sprays while using supplemental oxygen. This includes air fresheners, spray deodorants, and hairsprays.
-
Don't use alcohol-based hand sanitizers while using supplemental oxygen. If you use hand sanitizer before using oxygen, make sure that it has dried off of your hands completely before starting the oxygen or touching any of your oxygen equipment.
-
Using a humidifier during dry weather can reduce the amount of static build-up that occurs in your home. Keeping your house at an ideal humidity level (usually around 40 percent humidity) may reduce your fire risk when using supplemental oxygen and can also help your COPD symptoms.
- If you use an oxygen concentrator, always plug it into an empty, grounded outlet (an outlet with three holes instead of two). Never plug it into an extension cord, a faulty outlet, or an outlet that has other electronics plugged into it.

Even if you don't want to switch out your wardrobe for cotton-based clothes, consider at least switching to cotton bed sheets and blankets, especially if you use nighttime oxygen.
Static electricity from other types of fabric poses a much greater risk while you are asleep; this is partially because you are more likely to build up a static charge while shifting under your sheets, and partially because you might not be able to respond as quickly if a fire starts while you are asleep.
Use Your Oxygen in a Well-Ventilated Area
Using oxygen in a well-ventilated space is another important precaution that you can take to reduce your flammability risk and avoid fires. That means using your oxygen in an area with plenty of airflow and open space whenever possible.
Proper ventilation ensures that any extra oxygen in the air can quickly dissipate and leave the room before it builds up to the point of posing a significant fire risk. Beware of small, enclosed spaces; you should always try go outside or seek a more open area before beginning supplemental oxygen treatment.
Here are some tips for making sure you use your oxygen in well-ventilated places:
-
Make sure the ventilation system in your home is in good working order.
-
Crack the windows in your car if you are using supplemental oxygen while driving or transporting an oxygen tank.
-
Never place anything on top your oxygen tank. Doing so could cause any oxygen that leaks out to become trapped and build up to extremely flammable levels.
- Keep your oxygen tanks clean and in an open space where air can freely flow around them. Never store your oxygen tanks in an enclosed space or anywhere that doesn't have ventilation.
Prepare Your Home for Fire Emergencies

Even if you are very careful when using your supplemental oxygen, accidents can still happen. That's why, if you use oxygen in your home, you should be extra prepared in case a fire starts.
Here are some tips for home fire preparedness and precautions you should take if you or someone in your home uses supplemental oxygen:
-
Make sure your house has the recommended number of smoke detectors and they are all in good working order. Check the batteries often and replace them promptly when needed.
-
Make sure there is always a smoke detector in or right outside the room whenever you use supplemental oxygen.
-
Always keep a fire extinguisher in your home and within easy reach, especially while you are using oxygen.
-
Make sure your fire extinguisher is in good working order and replace it promptly when it expires.
-
Make sure you and everyone else in your household knows how to operate your fire extinguisher correctly.
- Have an evacuation plan and escape route planned in case of a fire emergency. Make sure everyone in your household knows what to do, where to go, and where to locate any safety equipment such as window escape ladders.
Keep Oxygen Equipment Away from Children

Now that you understand how dangerous supplemental oxygen can be if not properly handled, it should be clear why you should keep children away from your oxygen equipment. Many children are not old enough to understand the dangers of oxygen or to be trusted to treat the equipment gently.
If you have children in your home, you should keep your oxygen equipment secured and out of reach whenever possible. Large oxygen tanks can be particularly tempting for little children to play with and climb on, so it's important to instruct kids that they are off limits and keep a close watch to ensure that they stay away.
Large, heavy oxygen tanks can also be very dangerous to children and cause injuries if they fall. This is yet another reason to store your tanks properly and securely so they can't be tipped or knocked over.
Always Store and Transport Tanks Securely
 |
It's very important to make sure that you keep your oxygen tanks stored safely in a place where they won't be bumped or disturbed. You should keep any extra tanks in a stand or cart to ensure that they do not fall or get knocked over.
This is especially important when you are traveling with oxygen tanks, as there is a higher risk of the tanks getting jostled and tipped. Always keep your equipment carefully secured and protected any time you transport them from place to place.
Here are some tips for storing and transporting your oxygen:
-
Use an oxygen cart, stand, or chains to secure any extra oxygen tanks that you are not using. Never store them loose or unsupported.
-
Make sure all tanks are stored flat on the ground. Do not put them up on shelves or in any elevated place.
-
Transport oxygen tanks in your car by securing them in the main cabin of your car, not in the trunk. Open your car windows slightly to ensure that you have adequate airflow and ventilation.
- Keep your tanks in a moderately temperature-controlled space, like an air conditioned room. Do not leave your equipment in the sun, in a hot car, or allow them to be exposed to temperature extremes.
Exercise Care When Handling Your Equipment

Overall, it's important to always handle your equipment gently and with care. It's important to protect your tanks from damage to prevent leaks and dangerous explosions.
Here are some tips for handling and using your oxygen equipment with care:
-
Be careful not to drop your oxygen tanks. Use a stand, cart, or another safe container to secure your tanks when you move them from place to place.
-
Never handle your tanks roughly or carelessly.
-
Never drag or roll your tanks across the floor, set them down too hard, or let them bang against walls or other objects.
-
Always lift your oxygen tanks by holding the bottom or sides of the tank; do not lift or carry your tanks by holding the cap or valve.
-
Never cover your oxygen equipment, including tanks, tubing, and electrical cords. Do not put them underneath fabric, furniture or bedding.
-
Do not use an oxygen tank that has been dropped or damaged.
Conclusion
Knowing how to use oxygen safely is extremely important for anyone with COPD. Most patients end up using supplemental oxygen at some point over the course of their life, and knowing what precautions to take can prevent devastating fires and injuries.
Even though most people who use supplemental oxygen don't have any problems, all it takes is one poorly-timed mistake or a stroke of bad luck to cau
Whether you've been recently diagnosed with COPD or have been living with the condition for years, you are bound to have lots of questions. These might include questions about your health, your disease, your medications, your treatment options, and more.
As these questions come up over the course of your COPD treatment, your doctor will be your primary source for answers. But in order to get the right answers and the information you need, you first have to know what questions to ask.
Communication between doctors and patients should never be one-way; it's just as important for you to communicate with your doctor as it is for him to explain information to you. In order to get the best treatment possible, you need to keep track of all your questions, articulate your concerns, and remember to bring them up with your doctor when you have the chance.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
However, it can be easy to get distracted or forget any questions you have once you're actually in the office with your doctor. That's why it's a good idea to think about your questions and concerns ahead of time, before you get to your doctor's appointment.
In this post, we're going to go over a variety of questions that you can ask your doctor about your COPD. The answers to these questions can help you better understand your disease, how to keep yourself healthy, and how to take a more active role in your COPD treatment.
You can use these questions as a guideline when you visit your healthcare providers or as a jumping-off point to open up an ongoing dialogue with your doctor. As you read through the questions in this guide, they may even remind you of other questions and concerns you want discuss.
Questions to Ask Your Doctor About COPD
What Kind of COPD Do I Have?

COPD is an umbrella term that encompasses two distinct, but related lung conditions: emphysema and chronic bronchitis. Some people with COPD have just one of these conditions, while others have a combination of both.
Even people who show signs of both emphysema and chronic bronchitis often have one condition that is dominant. For instance, your lungs could be primarily affected by emphysema but also show signs of mild chronic bronchitis.
Before your doctor diagnoses your COPD, he will likely use a variety of tests, including spirometry (a basic lung function test), a chest X-ray, and pulse oximetry (a way to measure blood oxygen saturation). He will then consider the results of these tests along with your symptoms and medical history to come up with a diagnosis.
When you get diagnosed with COPD, ask your doctor to take the time to thoroughly explain your condition, including the difference between emphysema and chronic bronchitis and what kind of COPD you have. If there is anything you don't quite understand, don't hesitate to ask your doctor for more examples and details.
How Serious is My COPD?
COPD is a chronic disease that slowly gets worse over time. How severe your COPD is depends on how badly your lungs are damaged and how serious your symptoms are.
When you first get diagnosed, your doctor will likely place your disease within one of four distinct stages. Stage 1 COPD is the most mild, while stage 4 COPD is the last, most serious stage of the disease.
However, every person is different, and COPD affects different people in different ways. For instance, two people who are diagnosed with the same stage of COPD could have different symptoms and complications, and their diseases could progress at different speeds.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
That's why it's important to ask your doctor to give you a thorough explanation of your health, your disease stage, and your prognosis. Ask him to explain your test results, how exactly he made his diagnosis, and where you fit on the spectrum of COPD severity.
Continue to ask questions and get as much information as you can as your symptoms change and your disease progresses. Even if your doctor has explained something already, don't be afraid to ask him to go over it again or provide you with some helpful context.
How Did I Get COPD?

Although smoking is by far the most common cause of COPD, many other things can cause the disease. In general, just about anything that repeatedly irritates and damages your lungs over time can cause COPD.
This includes things like air pollution, chemical fumes, and occupational exposure to dangerous respiratory toxins. Other health conditions that affect the lungs, like asthma, cystic fibrosis, and AAT deficiency, can also cause COPD later in life.
If you and your doctor can figure out what caused your COPD, it can help you avoid exposing your lungs to the same hazard in the future. Unfortunately, in some cases, the exact culprit is difficult to find.
It is not always possible to pinpoint a single cause of COPD; you could be exposed to many different things over the years—such as air pollution, wood smoke, and cooking fumes—that damage your lungs. Still, discussing your medical history, occupational history, and any other possible causes with your doctor may help you better understand your disease.
Here are some things your doctor might want to know when discussing the cause of your COPD:
- When did your breathing symptoms first start?
- Have you ever smoked tobacco? (And do you still smoke tobacco?)
- Have you ever been diagnosed with asthma?
- Have you ever been frequently exposed to second-hand smoke (in childhood or adulthood)?
- Have you ever worked in an occupation where you might have been exposed to exhaust fumes, chemical fumes, wood smoke, dust, or fine particles?
- Have you ever lived in an area with heavy pollution?
- Do you use a wood-burning stove in your home?
- Has anyone in your family ever been diagnosed with a lung disease?
What Do My Test Results Mean?

If you have COPD, you will go through many different types of tests both before and after your diagnosis to help your doctor monitor and treat your disease. In fact, your doctor will likely do lung function tests (spirometry) and a blood oxygen saturation test (pulse oximetry) at every regular visit.
These tests reveal some very important things about your lungs, your heart, and your overall health. Your doctor will use the results of these tests to better understand your disease and find the best ways to treat it.
Your doctor will do some tests, like spirometry, at every check-up appointment to help him monitor changes in your lung function over time. As you go through treatment, it is important for you to understand what these tests are and what their results mean for your health.
Whenever your doctor does a test, he should show you the data and take the time to explain your results in terms you can understand. However, not all doctors take the time they should to explain things to their patients, and some doctors are simply not very skilled at explaining tough concepts in layman's terms.
That's why you should never be afraid to ask your doctor for more details and information about any of your medical test results. You shouldn't feel nervous to ask questions or feel embarrassed to admit when there is something you don't understand.
If you don't quite get it the first time around, ask your doctor to re-explain. Tell him which things you don't understand and don't hesitate to ask for more details, examples, and clarification if you need to.
Make it your goal to never leave the doctor's office with unanswered questions or concerns. Also, remember that if anything comes up later, you can call up your doctor on the phone to ask any additional questions you have.
Here are some examples of questions you can ask your doctor to better understand test results:
- What exactly does this test measure?
- How reliable are the test results?
- What do the test results say about my COPD?
- Do the test results indicate there is anything I should or should not be doing for my health?
How Do I Use My Medications?

Once you've been diagnosed with COPD, your doctor will prescribe you a variety of medications that will help you keep your symptoms under control. These may include quick-relief inhalers, maintenance inhalers, anti-inflammatory medications, corticosteroids, antibiotics, and more.
The combination of medications your doctor prescribes is your most powerful tool for managing your symptoms and keeping your COPD from getting worse. That's why you should take the time to make sure you know exactly how to use them correctly.
First, you will need to ask your doctor to explain what each of your medications are and what they are supposed to do. Then, you need to know when to take each medication and how to get the correct dose.
Your doctor should provide you with a COPD action plan that explains, in brief, your daily medications along with which medications to take when your symptoms get worse. However, in order for you to be able to use this resource effectively, your doctor needs to thoroughly explain how it works and how to use it to manage your symptoms every day.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
You should also ask your doctor to demonstrate for you the proper way to use your inhaler. Even if you've used an inhaler before, it's important to review the correct technique and make sure you know how to use your particular type of inhaled medication.
An alarming number of COPD patients don't use their inhalers correctly, which is why it's so important to double-check your technique. You can ask either your doctor or pharmacist to demonstrate it for you, and you can ask them to evaluate your technique as well.
You should also ask your doctor to give you a printed and signed list of all the medications you take, both prescription and over-the-counter. You should keep this list handy for a variety of reasons.
You may need to present this doctor's note when you travel with prescription medications, especially if you board a plane or train. Your medication list can also come in handy as a reference for yourself, your pharmacist, or other medical professionals you see.
What are the Potential Side-Effects of My Medications?

All of the medications prescribed for COPD have the potential to cause side effects. As you go through treatment, it's important to understand the potential side effects of every medicine you take.
For example, doctors often prescribe oral corticosteroid medications to help COPD patients recover from exacerbations. But even though corticosteroids are very effective at managing COPD symptoms, they can have serious side effects; because of this, most doctors only prescribe them when absolutely necessary and only for short-term use.
That's why it's important to ask your doctor to explain the side effects of every medication he prescribes or recommends. That way, you can fully evaluate the medication's benefits and risks and more easily recognize any side effects that occur.
It's also important to keep in touch with your doctor whenever you start a new medication. Let your doctor know how well the medication is working and alert him to any side effects right away.
Some side effects are merely uncomfortable, while others are more difficult to manage or can cause serious damage to your health. Depending on the type and severity of side effects you experience, your doctor may advise you to stop the medication, reduce your dosage, or switch to a different type of medicine.
Keep in mind that side effects are much more likely when you don't follow the correct dosage. That's just one of many reasons why it's so important to use your medications exactly as directed. This includes your as-needed inhalers, which you should take care not to use more often than your doctor recommends.
Here are a few examples of common COPD medications along with their potential side effects:
- Bronchodilator Medications:
- Increased heart rate
- Shakiness
- Camping in hands, legs, and feet
- Dry mouth
- Inhaled Corticosteroid Medications:
- High blood pressure
- Thrush
- Hoarse voice
- Dry or sore mouth
- Mouth and throat infections
- Oral Corticosteroid Medications:
- Weight gain
- Weakened bones
- Weakened skin
- Elevated blood sugar
- Muscle weakness
- Increased risk for Pneumonia
- Cataracts
- Changes in mood
What COPD Triggers Should I Watch Out For?

And important part of learning to manage your COPD symptoms is knowing about COPD triggers. A COPD trigger is anything that irritates your lungs and makes your respiratory symptoms worse.
A wide variety of different things can be COPD triggers, including fragrances, air pollution, allergens, and certain weather conditions. Depending on your lifestyle and the climate you live in, you may need to take special precautions to protect yourself from these and other things that irritate your lungs.
That's why you should ask your doctor to tell you all about COPD triggers. He should give you a thorough briefing on the many respiratory irritants and environmental triggers you may encounter, as well as tips for how to avoid them.
Your doctor can also alert you to common triggers that are specific to your geographical area, such as air pollution, high humidity, or seasonal allergens. He can also give you advice for reducing indoor air pollution so you can breath fresher air and manage your symptoms better at home.
You should also tell your doctor all about your lifestyle and home environment so he can help you identify any activities or conditions in your life that might trigger your symptoms. Every person is different, and which triggers your lungs are sensitive to depends on your unique biology and lifestyle as well as the severity of your disease.
What Changes Should I Make to My Diet?
In order to work at their optimum level, your lungs need lots of nutrients for fuel. Unfortunately, many COPD patients don't get enough nutrients—or don't get enough of the right kinds of nutrients—to keep their lungs and bodies strong.
The truth is that what and how much you eat can have a noticeable effect on your COPD. Too few calories and nutrients can reduce your lung function, while eating too much of the wrong things can also make breathlessness and other COPD symptoms worse.
That's why it's important to talk to your doctor about your diet and ask him what you can do to improve. That way, he can help you identify unhealthy eating habits and set better nutritional goals.
Your doctor is a great resource for learning what a proper diet looks like and how to maintain a healthy weight. He can also tell you what kinds of foods support healthy lungs and warn you against foods that may make it even more difficult to breathe.
Like all adults, it's important for people with COPD to eat a well-balanced diet full of whole foods, lean meats, and lots of fruits and veggies. However, there are some unique dietary requirements and sensitivities that many COPD patients have.
If you, like many other COPD patients, suffer from any diet-related complications, your doctor can help you resolve those issues as well. If you experience heartburn, acid reflux, weight gain, weight loss, or worsened shortness of breath after meals, you should bring these issues up with your doctor right away.
If you need more guidance, your doctor can also refer you to a nutritionist or dietitian to help you get on track. These specialists can help you develop a more detailed and personalized diet plan that takes your personal lifestyle and unique health needs into consideration.
What Kind of Exercise Should I Get?

Exercise is not only safe, but extremely beneficial, for the vast majority of people with COPD. While it may be difficult at first, getting enough physical activity improves your overall health and may even improve your ability to breathe over time.
Even if you suffer from symptoms that make exercise difficult, it's important to do what you can to keep yourself active. You just have to take it slow, start with light activities you can manage, and gradually do more as your physical abilities improve.
Getting started is often the most difficult part, especially if you aren't used to exercising on a regular basis. That's why you should ask your doctor to help you put together an exercise plan that is feasible and suitable for you.
Your doctor can tell you what kinds of exercises are safe and help you find activities that are appropriate for your level of fitness. He can also give you tips for reducing shortness of breath and managing your symptoms during physical activity.
If you have very severe symptoms, limited mobility, or just need some extra help getting started, your doctor can also refer you to another specialist that can help. Many patients are able to overcome obstacles and get on the track to better physical fitness by working with a personal trainer, physical therapist, or joining a pulmonary rehabilitation class.
Will I Need to Use Supplemental Oxygen?

As your disease progresses and your lung function gets worse, you may need to use supplemental oxygen to help your lungs meet your body's oxygen needs. Many, but not all, COPD patients end up needing oxygen therapy eventually.
Oxygen therapy isn't usually needed unless your lungs get to the point that they are no longer able to keep your blood saturated with oxygen on their own—a condition known as chronic hypoxemia. If your blood oxygen concentration begins to frequently drop below about ninety percent, your doctor may decide it's time for you to start using supplemental oxygen.
Once you start oxygen therapy, it is likely that you will need to continue using it for the rest of your life. However, some patients end up only needing oxygen for a short period time while recovering from a serious COPD exacerbation.
It's a good idea to discuss the possibility of oxygen therapy with your doctor early on in case you need it at some point during treatment. That way, he can explain how oxygen therapy works and how he will determine if and when you need to use supplemental oxygen.
Talking to your doctor ahead of time can help you feel more prepared if the time to begin oxygen therapy eventually comes. He can also clear up any questions or worries you have about using supplemental oxygen.
Your doctor can also help you take a more active role in your treatment by teaching you to recognize symptoms that indicate your blood oxygen levels are low. That way, you can alert your doctor if you notice the signs of worsening hypoxemia.
If you do use oxygen therapy, make sure your doctor takes the time to explain how to use it, when to use it, and how to get the dosage right. He should also go over basic safety precautions for handling your oxygen equipment to prevent dangerous fires and other accidents.
Before using your oxygen equipment, ask your doctor as many questions as you can think of to make sure you thoroughly understand how to use oxygen therapy safely and correctly. Oxygen is a medicine, and, like other medicines, it can be dangerous if you don't use it as directed.
How Can I Slow Down the Progression of My COPD?
Unfortunately, there is no actual cure for COPD. However, research shows that there are certain things you can do that may be able to extend your life and slow down the progression of the disease.
For example, if you smoke, quitting can reduce how quickly your lung function declines and allow you to live longer. Making other lifestyle changes, such as being more active and improving your diet, may also slow the rate at which your COPD worsens.
However, every case of COPD is different, and how quickly your symptoms progress dep
.png)
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease that affects around 16 million people in the United States alone. While there is no “cure” for COPD, the rate that it progresses can be slowed significantly with healthy lifestyle choices and therapy options such as pulmonary rehabilitation, oxygen therapy, and nebulizer therapy. COPD is a debilitating condition meaning it can affect your ability to get around. But despite this, many people with COPD have been able to live active lives.
One activity in particular that many COPD patients may have trouble doing is grocery shopping. Many people enjoy going to the store because it can be therapeutic and it allows them to plan their own meals. However, on the other hand, grocery shopping requires a lot of walking and lifting which can be made more challenging by increased breathlessness, chest pain, and chronic fatigue.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In this post, we’ll take a look at some actionable tips for making grocery shopping a little bit easier and accommodating of your lung condition. And if you are unable to make it to the grocery store, we’ll provide you with some interesting alternatives that you can try. As always, if you have any questions or concerns, please feel free to leave them in the comment section below.
Speak With Your Doctor
Before you start planning your trip to the grocery store, it’s very important that you speak with your doctor. While it would be nice if there was one simple dietary plan that every COPD patient could follow, the truth is, no two people have the same nutritional needs. Your doctor will work closely with you to determine what foods you should be eating based on the severity of your COPD, your age, and whether or not you have any comorbidities like diabetes, sleep apnea, or cardiovascular disease.

Diet and respiratory health are inextricably linked. Whenever you eat, the food consumed is used as raw materials in a process called cellular respiration. This is when the oxygen that you take into your lungs is used to break down food and turn it into usable energy for your entire body. If you eat unhealthy foods or you don’t have the proper balance of nutrients, your lungs will not have the energy and strength they need to function properly.
You not only need to know what to eat but how much to eat as well. If you don’t eat enough food and you’re malnourished, you likely won’t have the energy to go about your daily life and do things like grocery shopping or cooking. Many COPD patients are underweight because eating can lead to bloating, chest pain, and fatigue. If this is the case, your doctor may closely manage your diet to ensure you’re getting enough protein and healthy fats in your diet. He/she may also prescribe you medication that helps you cope with bloating and fatigue after eating.

On the other hand, being overweight can also cause a lot of problems in COPD patients. While overweight is far less common in COPD patients, the added weight can lead to obstructed breathing. If you are overweight, your doctor will likely make adjustments to your fitness routine to ensure you’re getting the right amount of exercise. Spreading meals throughout the day and implementing portion control can also help alleviate weight problems. Atrophy (muscle wasting) is a common cause of weight loss in COPD patients, so it’s important to lose weight in a healthy way that burns fat rather than muscle.

Last but certainly not least, you should not hesitate to address any questions or concerns you have about grocery shopping, cooking, and diet with your doctor. If you think you have a “weird” question, chances are, there are many other people out there who have the same question, so it’s best to just speak your mind. One good way to do this is to keep a notepad handy as you go about your day and write down any questions you have as you think of them. Once it comes time to visit your doctor, simply hand him/her the notepad.
Take Time to Plan Ahead
Going to the grocery store with COPD is all about planning. The more prepared you are, the better you will be able to deal with complications as they arise. Before heading out the door, you might want to create a list of emergency contacts that you can call if you experience a flare-up in your symptoms and need someone to come get you. According to Healthline, the average COPD patient experiences between 0.85 and 1.3 exacerbations a year so it’s best to be prepared no matter where you’re going or what you’re doing.
COPD is an invisible disease in many ways meaning nobody is going to know that you have COPD just by looking at you. This is why it’s important to have a plan rather than relying on strangers in the grocery store if you experience a flare-up. If you’re able to, you might consider reaching out to a friend and schedule days to go to the grocery store together. This could be another person with COPD or a healthy individual, but what matters is that they understand your disease and how to deal with a flare-up or exacerbation.
Research Nutritional Information and Brands
One thing you should get in the habit of doing is being more careful about the brands you buy and the nutritional labels on the back of each product. Unfortunately, there is a lot of deceptive advertising out there to make you think that you’re eating healthy food when you’re really not. According to Truth in Advertising, 70 percent of consumers make buying decisions while they are in the store making them more susceptible to false advertising.
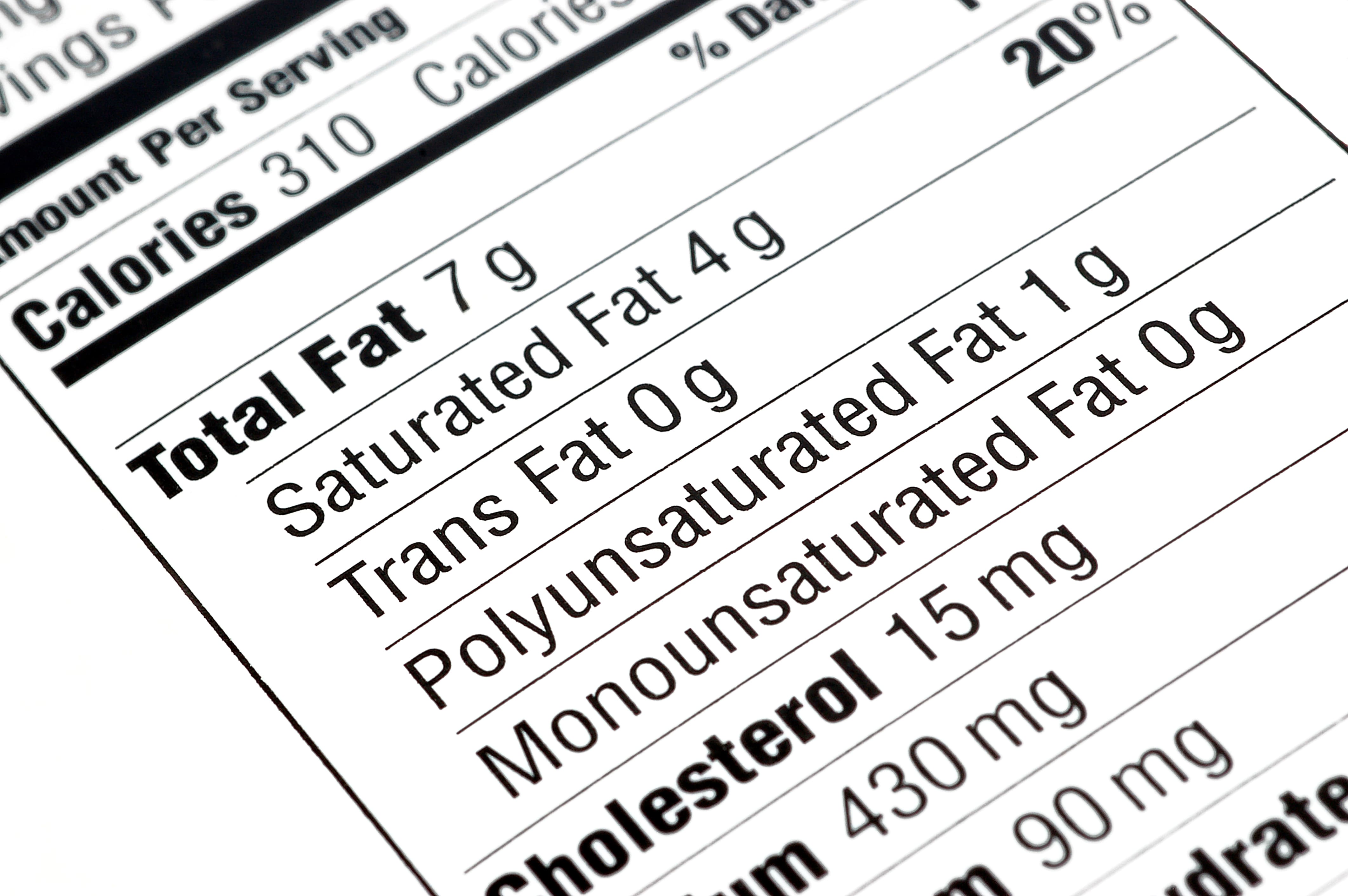
Remember that stores are specifically designed to get shoppers like you to spend more money. But “spending more money” doesn’t always mean getting healthy and nutritional food. If you’re in the store looking at a wall of different products, don’t just take the first one you see. Take some time to read the nutritional label on each of them and determine which one is best suited for your dietary needs. Also, be sure to write down which ones you choose so that you know for next time.
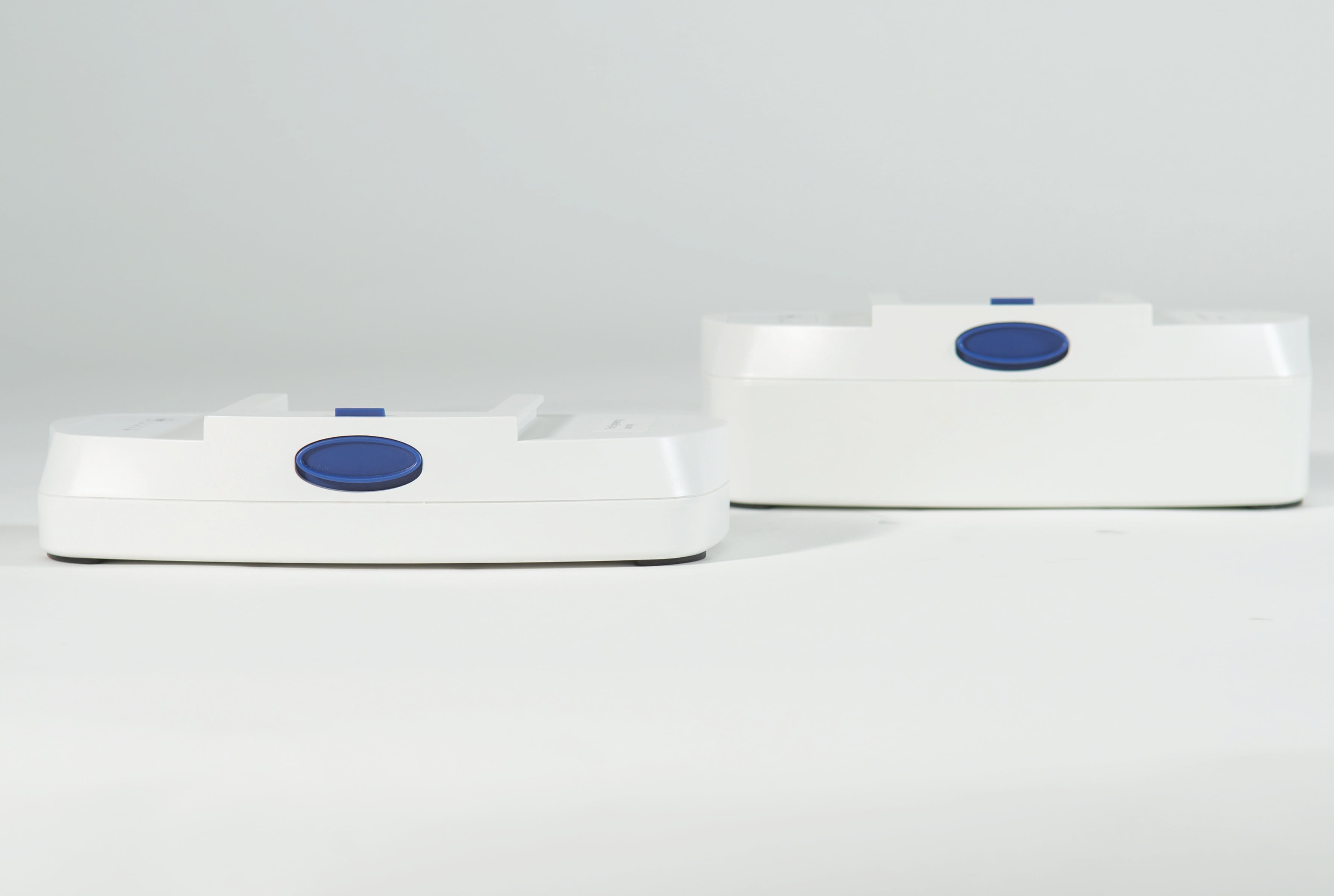
Find the Right Portable Oxygen Concentrator
Medical oxygen is a core aspect of most COPD treatment plans. Using supplemental oxygen throughout the day as prescribed allows COPD patients to keep their blood oxygen levels stable while preventing breathlessness, chest pain, and coughing. The problem, however, is that oxygen tanks are very bulky and the longer you want to stay out of the house, the heavier your tank will be.

Fortunately, there is a better alternative to oxygen tanks called portable oxygen concentrators. Unlike oxygen tanks which store compressed oxygen, oxygen concentrators are electronic devices that take in ambient air, remove nitrogen, argon, and other gases, then put out medical-grade oxygen. The benefit of this is that you don’t need to buy a large, heavy oxygen tank just to get out of the house, you just need enough batteries to last the duration of your trip.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
One of the most popular portable oxygen concentrators on the market in 2021 is the Caire FreeStyle Comfort. This unit weighs in at only 5 pounds making it one of the lightest portable oxygen concentrators ever produced. But that’s not all that it has going for itself. The FreeStyle Comfort has a maximum oxygen output of 1,050 milliliters per minute (ml/min) of medical grade oxygen (5 pulse flow settings) and offers up to 16 hours of battery life on one charge while using the 16-cell battery.

Another great affordable portable oxygen concentrator is the Inogen One G5. Much like the FreeStyle Comfort, the G5 is lightweight, weighing in at only 4.7 pounds. It also has the highest oxygen output of any pulse dose portable oxygen concentrator with 1,260 ml/min of medical-grade oxygen. Last but not least, it offers up to 13 hours of battery life on one charge using a 16-cell battery.

Needless to say, there are plenty of options available to you in terms of portable oxygen concentrators. Rather than going with the first one you find, you should take the time to speak with a respiratory specialist who will be able to align you with the POC that best meets your wants and needs. Remember that you will need a prescription from your doctor or pulmonologist in order to purchase or rent a medical-oxygen device.
Bring Your Rescue Inhaler
A rescue inhaler is a small portable device used to administer inhaled medications. Most respiratory patients including people with asthma and COPD are prescribed an inhaler because it provides quick relief during respiratory exacerbations. Fast-acting bronchodilators act quickly to open up the airways, clear mucus, and alleviate breathlessness so it’s important to carry yours with you and keep it handy whenever you go to the grocery store.

Unfortunately, inhalers are notoriously difficult to use. Unlike nebulizers which deliver medication in a constant stream, allowing you to breathe at your own pace, inhalers require you to inhale sharply in order for the medication to reach your lower respiratory system. This can be really challenging for some COPD patients, especially people with more severe lung impairment. One great way to combat this is to use an inhaler spacer. A spacer is a plastic piece that attaches to your inhaler mouthpiece and holds the medication for longer, giving you more time to inhale it. If you’d like more information on using an inhaler more effectively, please read this article.
Use Mobility Aids
A mobility aid is a device that helps you get around more easily. Devices like walking canes, walkers, manual wheelchairs, and electric scooters can be invaluable tools for anyone with COPD. Many grocery stores have electric scooters at the door to make it more accessible for people with disabilities. These scooters usually have a basket on the front or back so that you can store your groceries, so be sure to take full advantage of these if you see them in your store.

Choose the Right Time and Day
Choosing the right day and the right time to go to the store can make a world of difference. Going during peak hours will mean spending more time in lines and you might be forced to rush through your grocery shopping. For someone with COPD, this is not ideal because you need to be careful about the products that you’re buying. Additionally, there’s usually added stress and anxiety when you go during the busiest hours.

According to Thrillist, the busiest times at grocery stores are Saturday afternoons between 1 pm and 3 pm and weekdays after 4 pm or 5 pm. The least busy time is Monday mornings and any weekday before noon. Planning your grocery store trip during these times will make your shopping experience much more pleasant and you won’t feel the need to rush through what you’re doing just to get out of someone’s way.
Learn the Store’s Layout
As you go through the store for the first time, you should take note of where everything is located. You don’t need to write down everything, but you should keep track of what isle number your favorite products are located in. This will make it much easier to plan your shopping list next time you go to the store.

Consider Grocery Delivery Services
Last but certainly not least, you may want to consider either doing grocery pickup or have your groceries delivered to your home. Grocery pickup is where you order your groceries online and then you simply have to drive to the store to pick them up. This will save you a lot of time and you won’t need to worry about walking around the store to find the groceries you need. Simply pull up, load the groceries into your car, and you’re all set.

Another option is grocery delivery. Grocery delivery is usually done by third-party companies like Instacart or Shipt and will provide you with even more convenience than in-store pickup. However, the one downside to having your groceries delivered is that you will have to pay a delivery fee, so this is not a great option if you just need a few things.
Conclusion
Grocery shopping and cooking are two activities that many people love to do. However, if you’re living with COPD or any other type of chronic lung disease, you may find it difficult to find the energy to do these things. What’s more, you might worry about not having enough medical oxygen to last the duration of your trip to the store. Follow the tips above to get you started with grocery shopping in a way that’s safe and accommodating for your respiratory illness.
Here at LPT Medical, we strive to provide as many oxygen patients as possible with high-quality, lightweight, and easy-to-use portable oxygen concentrators. Unlike old outdated oxygen tanks, portable oxygen concentrators enable you to go wherever you please without restriction. With long-lasting lithium-ion batteries, you’ll never have to worry about running out of oxygen while you’re out of the house. And taking a trip to the grocery store will be a breeze with POCs like the Inogen One G5 or Caire FreeStyle Comfort.
Whether you simply have a question about portable oxygen concentrators or you’re looking for a great deal on a new or used portable oxygen concentrator, don’t wait to reach out to our respiratory specialists here in Denver, Colorado. You can reach us by phone at 1-888-416-3855 or by email at info@lptmedical.com. Alternatively, you can leave a comment below expressing your interest in an oxygen concentrator and we will reach out to you with more information.

The holidays can be a stressful time for everyone and people with COPD should take extra precautions to avoid over-exerting themselves mentally and physically, over-eating, and stressing. If you are one of the 16 million Americans with COPD, avoiding these COPD triggers over holidays will make everything more enjoyable and you will run a lower risk of getting sick or experiencing a COPD exacerbation.
However, this holiday season, 2020 and going into 2021, the global COIVD-19 pandemic is making this holiday season even more difficult, especially for our family and friends that have COPD.
With COVID-19 cases increasing as we are getting more into the holiday season, public health experts are encouraging people to be even more stringent about social distancing, and limiting travel.
These unprecedented circumstances have changed almost everything, including the ways we interact with people. Connecting virtually with loved ones and family members is one of the only ways to safely spend this lovely time of year together, even in the weeds of a pandemic.
If you have never tried FaceTime, Zoom, Skype, Google Hangouts or any other form of face to face virtual communication, there is no better time to do so! Also, stay on the look out for a new LPT Medical blog about connecting with family and friends digitally!
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The Importance of Holidays and Social Connection
Holidays give us a sense of belonging, and they bring our most loved people together into one place. This tradition should continue into this year in some way shape or form. So, start spreading the idea that creating new traditions amongst your family members can be very joyful and fun.
That being said, holidays can be exciting and fun, but for people who suffer from Chronic Obstructive Pulmonary Disease (COPD) holidays can also initiate stress and other COPD triggers.
In this article we are going to discuss how you can avoid COPD exacerbations throughout the holidays, and minimize your chances of getting sick.

COPD and the Holidays
If you have COPD, be prepared this holiday season. It is unfortunate, but living carefree and enjoying the holidays can be difficult for those that suffer from ongoing medical conditions, such as COPD. The extra effort it takes to just to breathe can cause any holiday to be just that much more stressful, not to mention the added stress of a global pandemic. However, there is relief, and we have compiled some helpful COPD tips for the holiday!
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Helpful COPD Tips for the Holidays
The holiday season is famously the time of year we get to relax and spend quality time with loved ones, but it does pose real risk for additional anxiety and increased stress, which can be triggering for patients with COPD. So here some helpful tips for you!
Traveling

Of course it is recommended not to travel for the holidays this year, but if you are traveling, be prepared, be prepared more than you have ever been before.
You don't only need to remember all of your medications and be sure you have your portable oxygen concentrator (POC) or oxygen tank, you also have to make sure that you have an extra POC battery, and your POC AC and DC charger cables. Should your POC start to run low, you want to avoid having to stop into a location to charge your oxygen device in order to avoid contact with strangers and surfaces. If you do not have an extra battery or other oxygen accessories, all of those items can be found on our website.
Watch What you Eat
If you have COPD it is important to avoid overeating. This is much easier said than done especially during the holidays, but portion control can be the difference between enjoying your holiday versus spending it in the hospital
Medically, a full stomach can press on the diaphragm. This will increase the regular symptoms of COPD that include breathlessness, and can often induce a COPD exacerbation.

Eating healthy foods that help with COPD symptoms is a must during the holidays, especially if cold weather is a factor in your area. Minimizing the chances of triggering a COPD exacerbation is key to enjoying the holidays, and if you can’t control the cold weather, you can control what you eat, so eat healthy.
Everything may look delicious, but go with the fresh veggies, greek yogurt dip, whole grain items, potatoes and smoked turkey (in small portions) because these are all great options to choose from. You can even suggest these dishes in advance, some people love to have ideas before they decide on what food they will bring to the potluck.
Save money
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Limit shopping to what’s absolutely necessary. This year is more financially taxing for most people than any year in the past, so there is no absolutely no shame in expressing your gratitude in other ways rather than in material gifts.
As a person with COPD, it is never advisable to be out shopping among large groups of people, especially during the COVID-19 pandemic and flu season. Luckily, you can do much of your shopping from the comfort and safety of your home!

Even small local businesses have developed their online platform as a result of COVID-19 restrictions in many areas. So you will still have the option of buying thoughtful gifts that only your favorite local stores supply rather than buying from bulk operations like Amazon.
Our small family owned business, LPT Medical, invites you to shop with us online or over the phone at 1-800-946-1201 for any of your oxygen therapy necessities or accessories. From portable oxygen concentrators like the Caire FreeStyle Comfort, The Inogen One G5, or the Respironics SimplyGo, to any and all of the accessories you need to make the most of them we have some great holiday deals that our respiratory specialists would be happy to discuss with you. If you would like to know how much portable oxygen concentrator costs please call us at 1-800-946-1201, for all of your oxygen inquires and questions.

Watch What you Carry

If you do decide to venture out to go shopping, don’t be afraid to use a cart! And make sure you clean the handles of the cart with an antibacterial cleaner before you use it. If you don't already have a portable oxygen concentrator backpack, you might find it useful for carrying your oxygen device along with your other essentials everywhere you go this holiday season, to ensure you do not forget anything.
The Inogen One G4 backpack has also been reviewed as one of the easiest ways to transport your oxygen with you wherever you go, and it is also user friendly, so if you need to adjust your oxygen flow or mess with the settings, the POC is conveniently located so you can get to it without rummaging through your bag! There are also custom backpacks for the One G3 and One G5.

Stay Warm
If you haven't already read our LPT Medical blogs about avoiding COPD exacerbations, cold weather and COPD are not the perfect combination, so dressing warm for both the expected outdoor temperatures and the indoor ones is essential for maintaining your health over the holidays.
Here is a tip if you use supplemental oxygen keep your oxygen tubing under a layer of clothing so that the air you breathe will be warmer. Also, consider wearing a scarf or a CT face mask to make breathing colder air easier while you are outside!
A CT mask is the perfect holiday gift for a loved one with COPD it converts the cold dry air into moist warm air, and help respiratory patients breathe in cold air, just take note these masks do not protect against COVID-19

Be Prepared
Have all of the tools you need for everyday activities, including medications, daily inhalers and fast-acting inhalers for emergencies. If you use supplemental oxygen, make sure that you have an adequate oxygen supply by either ensuring that you have enough oxygen left in your tanks or an extra portable oxygen concentrator battery to keep your POC charged all day and night.
Trust Yourself

This holiday season is not the same as many others, where gatherings and events could go on for a long period of time, and someone with COPD might have to step out for the night due to feeling overwhelmed and tired. This is normally when we would recommend trusting this instinct and leaving when you know you have had enough rather than over-extending yourself, and weakening your immune system to the point where you are more susceptible to illness.
But this season, you might be feeling lonely, anxious, or even frightened, and it is important to recognize these emotions as valid, and understand that millions and millions of people are feeling similarly. Click here for a guide about encouraging mental health for people with COPD.
This is why it is so important for mental health to stay connected with your family and loved ones during this holiday season even if you cannot be together in person.
Overview
These suggestions for staying safe and sane during the holidays may seem like common sense, but oftentimes a reminder to trust your instincts, eat healthy, stay warm are positive health checkups we do not do enough!
Also, we wrote this article mainly as a reminder, that even if you do struggle with breathing problems, due to a chronic illness or other ailment, that does not mean that you should not experience the joy that comes with sharing the holidays with those we love.

If you are struggling with staying connected, subscribe to our daily newsletter to be updated every time we post a new blog, Or you can join our facebook group, by searching LPT Medical COPD & Respiratory support group on the Facebook App. Our emails and our Facebook group connect you with the best resources and information for anyone that suffers from a respiratory disease, or chronic illness like COPD. Our readers utilize this information to make valuable life changing decisions.
We like to write about changing your habits, your medical oxygen supply needs, tips and tricks to get through just about any obstacle life throws at you. So if you need the gift of connection, please comment below this article with any inquiries, questions, or happy holiday wishes. From LPT Medical’s family to you and yours, we are wishing you a safe and joyful holiday season.
The lungs are one of five vital organs in the human body along with the brain, heart, kidneys, and liver. Every breath you take helps to produce and distribute nutrients in the bloodstream that provide you with energy, heal your wounds, and maintain every other organ throughout the body. And while most people understand the basics of maintaining healthy lungs i.e., getting enough exercise, eating healthy foods, and not smoking, many people aren’t aware of how specific lung diseases differ from one another and how they’re diagnosed by medical professionals.
There are many lung diseases, but each one affects a different part of the respiratory process. For example, one condition may affect your physical ability to take in air while another could affect your lung’s ability to absorb oxygen from that air. While the symptoms you experience may be similar in these two situations, the way they’re diagnosed and treated could be very different.
If you’re diagnosed with a lung disease, it’s important that you’re educated about its unique characteristics because, while your doctor will provide you with medication and information regarding your disease, your body’s ability to heal will inevitably depend on the lifestyle changes you make.
In the following sections, we’re going to break down each category of lung disease to help you demystify them and eliminate any confusion you may have. Then, we’ll take a look at how exactly respiratory diseases are diagnosed by doctors. Keep in mind that if you have any questions or concerns about your respiratory health, don’t hesitate to discuss them with your pulmonologist or in one of the many online forums designed to support those suffering with respiratory disease.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
The Importance of Respiratory Health
Despite lung disease being one of the leading causes of death worldwide, many people are unaware of the role their lungs play in their overall health. While asthma and lung cancer are household names in the health world, they are far from the only conditions you should be aware of or concerned about.
Unfortunately, as we age, most things become more difficult and that includes breathing and maintaining healthy lungs. If you’ve smoked in the past or lived in a polluted area, you’re going to be at a much higher risk for a variety of different respiratory conditions so the best way to stay healthy is to get started as soon as possible with protecting your lungs.
Generally, raising awareness is a great way to stress the importance of lung health and prevent many diseases before they take hold. Simply discussing the topic with a friend and striking up a conversation on a blog, online forum, or among your friend group will get people talking and cause them to be more conscious about their lung health.
How The Lungs Work
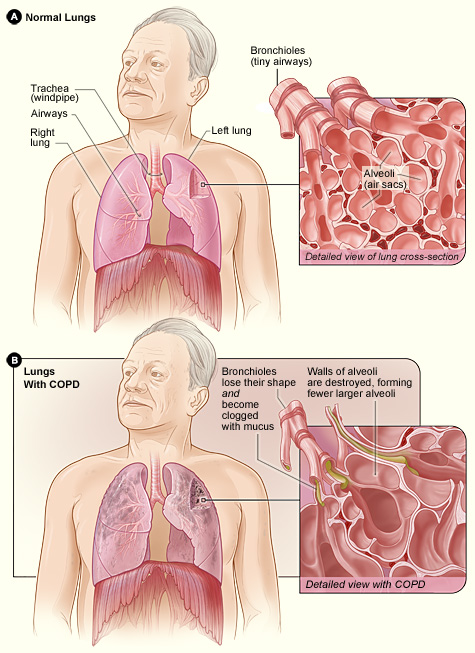
The lungs are one piece of the respiratory system and are responsible for bringing oxygen into the body and removing carbon dioxide. The respiratory process begins when the diaphragm (the muscle between the lungs and the abdomen) contracts, expanding the lungs and causing air to flow down the windpipe to the trachea where it is divided into the bronchial tubes and into the lungs.
As air enters the lungs it’s divided into smaller air passages called bronchioles. At the ends of these bronchioles are alveoli, tiny air sacs with blood vessels and capillaries on them. The walls of the alveoli absorb oxygen where it passes into the blood. Simultaneously, carbon dioxide is released from the blood and sent out of the body when you exhale.
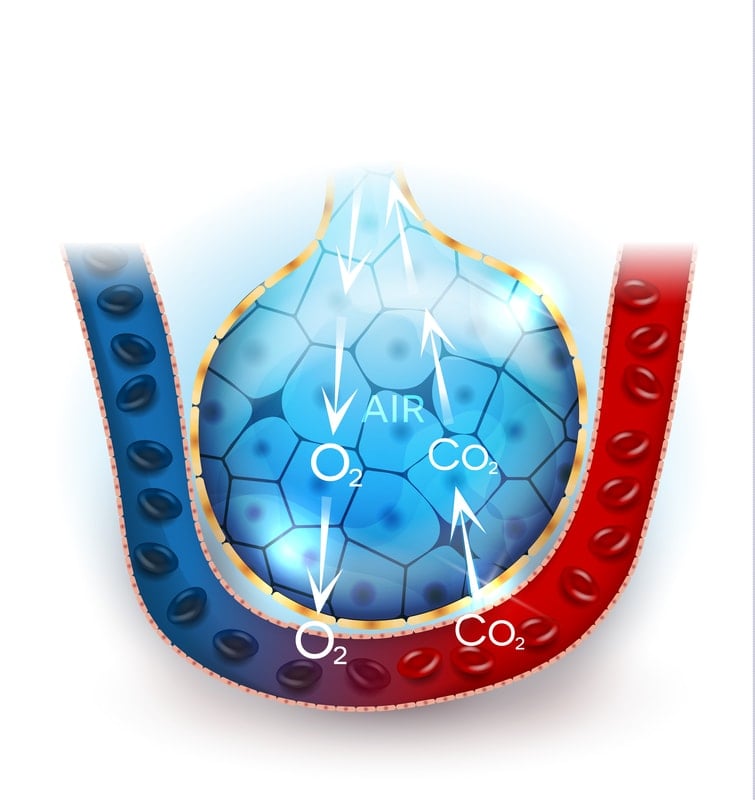
Your red blood cells need oxygen to complete a process called metabolism. This is where nutrients taken from the food you eat are broken down using oxygen to create usable energy for your body. The heart then pumps this blood throughout the body reaching every organ in the body.
Your respiratory system has a number of “defense mechanisms” that it uses to prevent irritants and harmful substances from entering the lungs and bloodstream. Tiny hairs in the nose called cilia help to prevent larger particles from entering your lungs. Additionally, mucus in the bronchial tubes and trachea help prevent viruses and bacteria from reaching the lungs. However, if these impurities do reach the lungs, they can sometimes be brought up through mucus.
The Different Types of Respiratory Disease
The majority of lung disease in the United States are the result of smoking, infections, and genetics. They can be classified into six different categories. Each category impacts a different part of the lungs. Because each of these categories can overlap in terms of symptoms, causes, and risk factors, it’s often difficult to diagnose them without the appropriate diagnostic tests and a thorough examination of symptoms. Read on to learn more about each category of respiratory disease.
Diseases Affecting the Airways
The airways are all parts of the respiratory system that transport air from one point to another. It starts at the nose and mouth, passes through the pharynx and larynx, and into the trachea. After reaching the trachea, it passes into the left and right bronchi and then the three lobes in each lung.
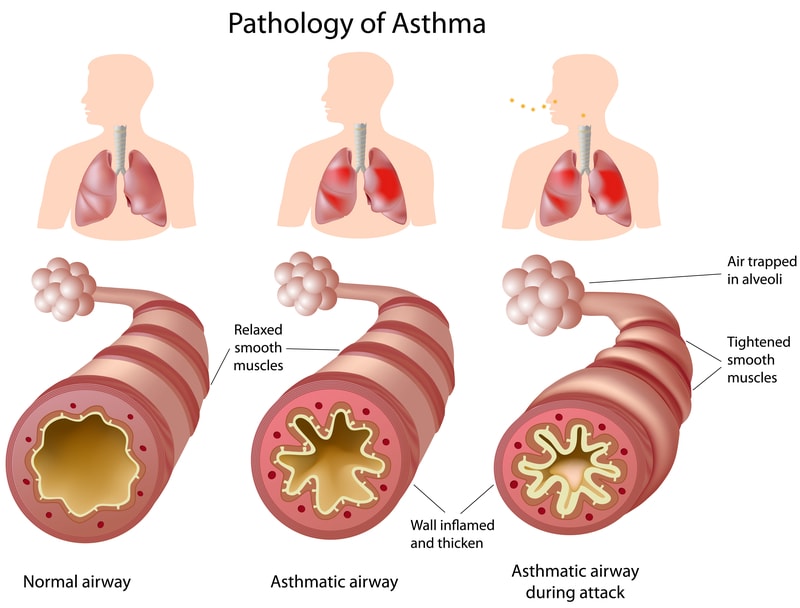
Asthma
Asthma is one of the most common respiratory diseases affecting the airways. It’s characterized by persistent inflammation and spasms that result in shortness of breath and wheezing. During an asthma attack, muscles near the airways contract and they become swollen causing the bronchial tubes to narrow. 1 in 13 people have moderate to severe asthma according to the Centers for Disease Control (CDC).
Asthma is classified into two different categories: allergic asthma (extrinsic) or non-allergic asthma (intrinsic). Allergic asthma is caused by external factors or irritants that come from outside the body such as pollution, cigarette smoke, pollen, exhaust, or airborne chemicals. Non-allergic asthma is the result of internal triggers such as bacterial and viral inflammations of the airways. Emotional or physical stress can also induce an asthma attack.
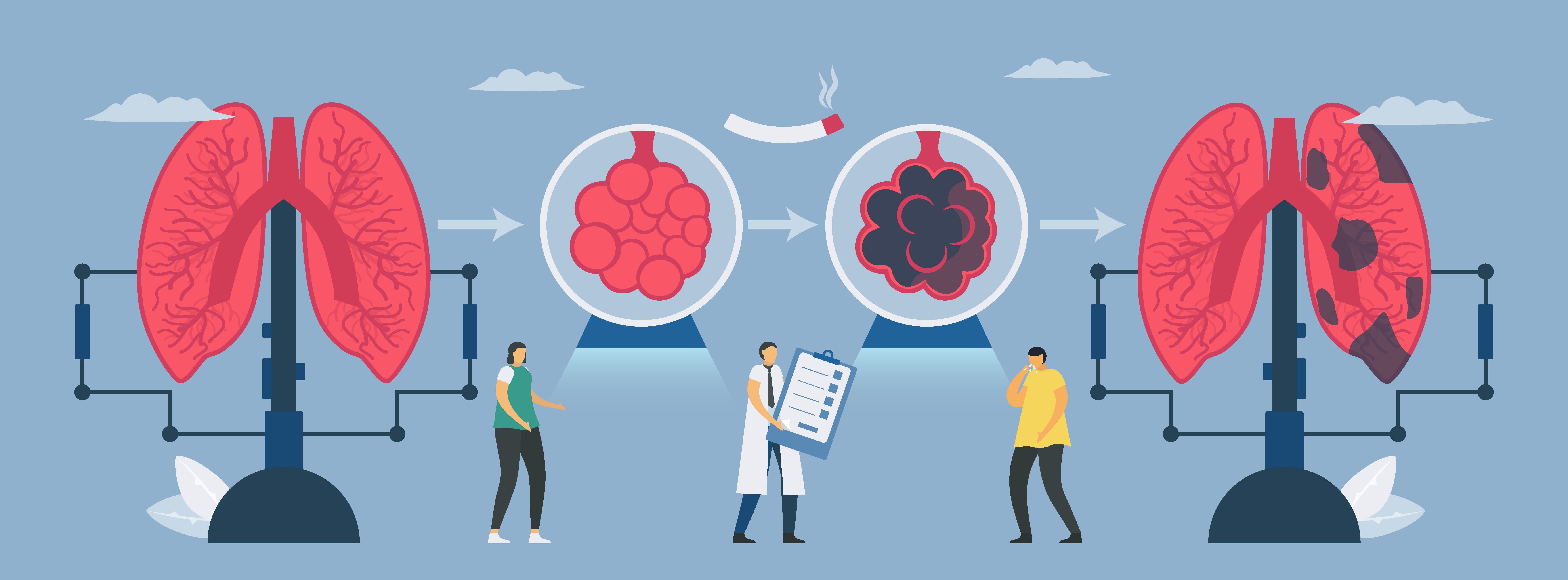
Chronic Obstructive Pulmonary Disease (COPD)
COPD is one of the leading causes of death in the United States. It’s an umbrella term that includes emphysema (damage to the alveoli) and chronic bronchitis (damage to the bronchial tubes). 90 percent of instances of COPD are the result of smoking.
COPD isn't a disease that takes hold overnight; it develops gradually over years like many lung conditions. As a result, many people don't realize they have COPD until their symptoms get bad enough for them to see a doctor. Like an asthma attack, a COPD exacerbation is a sudden onset of symptoms. These symptoms include:
- Breathlessness - especially during physical activity
- Chronic cough that tends to get worse over time
- Wheezing or other breathing sounds
- Coughing up mucus (phlegm)
- Symptoms that get worse with sickness such as a cold or the flu
Acute Bronchitis
Also known as a chest cold, acute bronchitis is the temporary inflammation of the bronchi. This is usually accompanied by a fever, shortness of breath, wheezing, and excess mucus production. While acute bronchitis is not usually a huge health concern, combined with other more serious respiratory conditions, it can cause an exacerbation that could be fatal. This is why it's so important to avoid getting sick if you have any type of lung disease.
Cystic Fibrosis
Cystic fibrosis differs from the above conditions in that it’s genetic. Someone with with cystic fibrosis will have difficulty clearing mucus from the airways because the disease causes it to become sticky and thick. These people typically have frequent lung infections and a chronic cough and it's often detected in childhood so it can be treated early on.
Cystic fibrosis alters a protein in the body called the cystic fibrosis transmembrane (CFTR). This protein manages the flow of salt and water in and out of cells in the body. Because the balance of salt and water is altered, mucus becomes thicker which can affect a number of systems throughout the body, especially the respiratory, digestive, reproductive systems, and sweat glands.
Diseases Affecting the Air Sacs (Alveoli)
There are millions of alveoli in the lungs. Each balloon-shaped air sac is only one cell thick and are the “endpoint” of the respiratory system where oxygen enters the bloodstream. There are a number of disorders affecting the alveoli that can result in inflammation, overdistention, or surfactant which prevents the alveoli from deflating entirely between breaths.
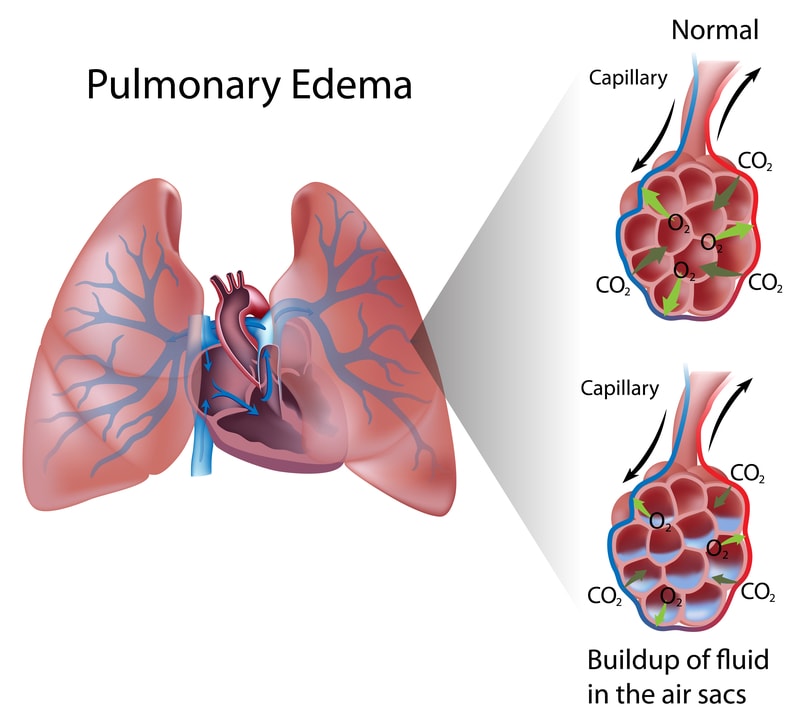
Pulmonary Edema
A pulmonary edema occurs when the alveoli begin to fill with fluid preventing the exchange of oxygen and carbon dioxide. This disease can often occur as a result of congestive heart failure and can be deadly.
In situations where pulmonary edemas are not caused by the heart, this is called noncardiogenic pulmonary edema. This results when the capillaries in the lungs become leaky or more permeable. This may happen as a result of high-altitude pulmonary edema (HAPE), acute respiratory distress syndrome (ARDS), a viral infection or more.
In order to prevent pulmonary edemas, you should focus on your cardiovascular health. Eat a heart-healthy diet low in salt, sugar, and solid fats, exercise regularly, and never smoke. Pulmonary edemas can be fatal so it's important that you visit a cardiologist and pulmonologist regular to monitor your heart and lung health.
Pneumonia
This condition results when the alveoli become inflamed and infected, usually filling with pus and making it difficult to breathe. While pneumonia can range from mild to life-threatening, it's more dangerous for people with a weakened immune system or people with other health problems.
Pneumonia can be acquired from a number of sources including hospitals, long-term care facilities, or other healthcare facilities. In order to prevent pneumonia, you should get vaccinated, practice good hygiene, and keep your immune system strong by eating right and not smoking.
Tuberculosis
Tuberculosis is a contagious disease resulting from a bacteria called mycobacterium tuberculosis. This disease begins in the lungs but bacteria is known to travel to other parts of the body like the spine, brain, and kidney. People who have active tuberculosis may experience symptoms like shortness of breath, fatigue, and coughing up blood-tinged phlegm. To some, tuberculosis is known as the "disease of poverty" because it is far more common in developing countries that are often overcrowded.
Lung Cancer
While lung cancer can occur in any part of the lungs, it occurs more frequently in or around the alveoli. Lung cancer is the most common form of cancer but it's also the most preventable with up to 90 percent of all cases being caused by smoking. While there are more than 20 different types of lung cancer, the two most common are small cell and non-small cell lung cancer.
Acute Respiratory Distress Syndrome (ARDS)
ARDS occurs when the alveoli in the lungs begin to fill with blood from surrounding blood vessels. Because ARDS leads to low blood oxygen levels and breathing failure, it can often be a fatal disease and while two thirds of ARDS patients survive, some may never fully recover from their symptoms.
Diseases Affecting the Interstitium
Between the alveoli in the lungs, there is a thin lining containing blood vessels that are responsible for the exchange of oxygen and carbon dioxide between the blood and the air sacs. This delicate layer is called the interstitium.
Diseases that affect the interstitium are classified under the umbrella term “interstitial lung disease” (ILD) and include things like autoimmune disease, sarcoidosis, and idiopathic pulmonary fibrosis. Other diseases that can affect the interstitium include pulmonary edema and pneumonia.
Diseases Affecting Blood Vessels
It’s important to remember that what affects one part of the body often has an effect on another party of the body — this is often the case with diseases affecting blood vessels. When the right side of the heart receives deoxygenated blood, it goes to the lungs through the pulmonary arteries. These arteries may become damaged by disease as well.
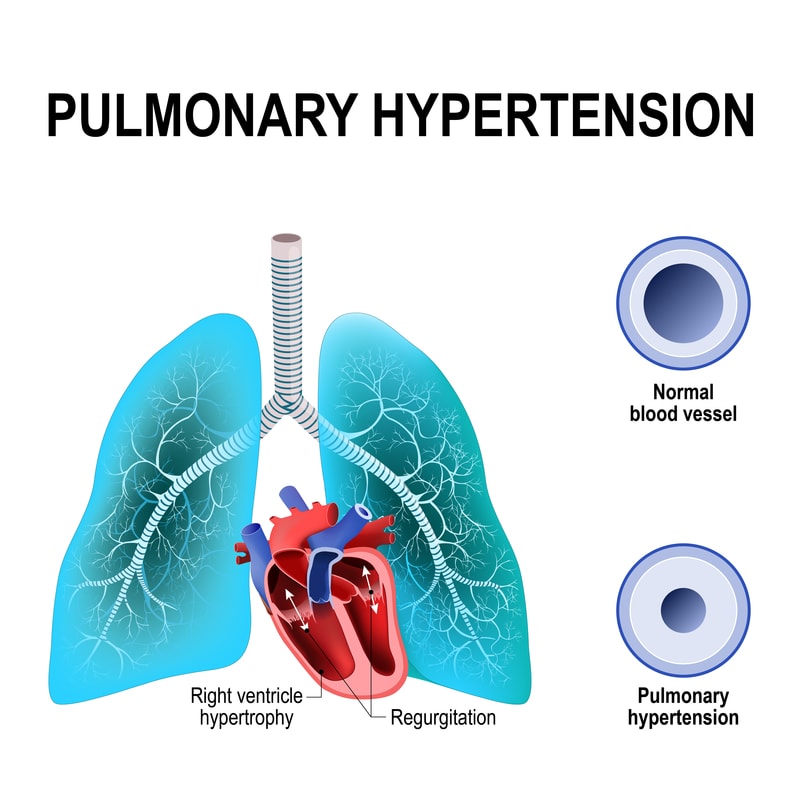
Pulmonary Hypertension
Idiopathic pulmonary arterial hypertension (high blood pressure in the lungs) can result in chest pain and shortness of breath. The primary concern with pulmonary hypertension is heart failure as it puts a strain on the right ventricle of the heart.
High blood pressure usually results when capillaries and pulmonary arterioles are damaged, clogged, or narrowed in some way. When this happens, the right side of your heart will have a harder time pumping blood through the lungs. Eventually, the patient will experience heart failure.
Pulmonary Embolism (PE)
Also known as a blood clot, a PE may be pumped into the lungs resulting in low blood oxygen levels and difficulty breathing. It can also result in damage to the lungs or other organs within the body and can even be fatal. Common signs of a pulmonary embolism are a chronic cough, chest pain, and shortness of breath. Treatment options for PE include blood thinners, compression clothing, and physical activity.
Diseases Affecting the Pleura
The pleura is the outer lining of the lungs made up of the parietal pleura and the visceral pleura. The pleura as a whole assists the lungs as you inhale and exhale by producing a fluid that lubricates them and allows them to move easily.
Pleural Effusion
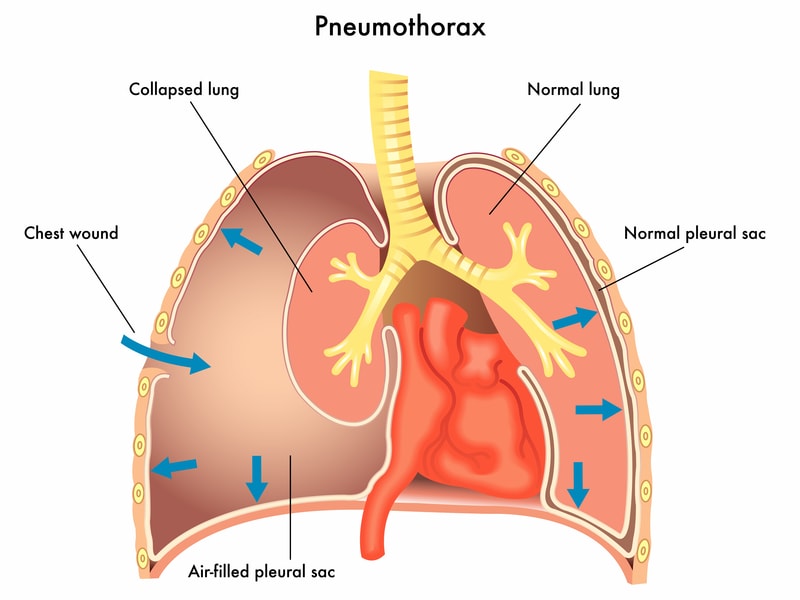
Heart failure or pneumonia can sometimes result in what’s called a pleural effusion. This is when an excess amount of fluid builds up in the space between the chest wall and the lung. Draining the fluid can help the patient regain their breathing.
The two types of pleural effusion are exudative and transudative. Exudative pleural effusions are the result of an excess of white blood cells that have reached the pleural fluid. Cancer, infection, and inflammation are usually the cause of this type of pleural effusion. On the other hand, transudative effusion is usually caused by kidney disease, liver disease, and cardiac failure. It's usually pale and yellow in color.
Pneumothorax
Pneumothorax, also known as a collapsed lung, results when air leaks into the area between the lung and the chest wall (pleural cavity). There are a number of things that can cause pneumothorax like chest injury, lung disease, or lung procedures. Depending on how severe the event was, pneumothorax can fix it self or it may require medical attention. To treat it, doctors insert a needle or tube between the ribs and remove excess air.
Mesothelioma
This is a rare type of cancer that’s typically caused by exposure to asbestos, a fibrous mineral often used in the building and construction industry. Years of exposure can significantly damage the lungs and can be life threatening. In order to prevent mesothelioma, it's a good idea to have the air quality in your home tested regularly.
This cancer attacks mesothelial cells found in the abdominal cavity and membranes lining the chest. This forms a tissue called mesothelium which lubricates organs and prevents them from becoming damaged as they move up against one another. Peritoneal mesothelioma occurs in the abdomen while pleural mesothelioma occurs in the chest cavity.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Diseases Affecting the Chest Wall
In order to take in as much air as possible, your lungs, diaphragm, and chest wall need to be as flexible as possible. When any one of these is obstructed it can result in difficulty breathing and other respiratory disorders.
Obesity Hypoventilation Syndrome
Obesity is common and can have numerous adverse effects on the body. Extra weight on the abdomen and chest, however, can lead to serious breathing problems, especially if other respiratory diseases are involved. In most cases, respiratory patients will undergo some form of exercise in order to prevent fat from building up in the chest.
Neuromuscular Disorders
Myasthenia gravis and amyotrophic lateral sclerosis are two neuromuscular disorders that may affect the lungs. These conditions affect the nerves that control the muscles in your chest wall resulting in difficulty breathing. This can’t be cured but it can be managed and treated.
Diagnostic Tests for Lung Conditions
Because so many lung conditions have overlapping symptoms, it can be difficult to diagnose them. According to WebMD, between 25 and 50 percent of people in the United States visit a doctor with a concern about shortness of breath every year. Lung diseases are by no means uncommon, but they can range in severity from mild to life-threatening.

While your doctor will likely ask you about the symptoms you’ve been having, he/she will likely have to perform some type of test to accurately diagnose your condition. A physical examination is usually where they will start along with studying your medical history. If these bring up any concerns, your doctor will have a better idea of what test to perform.
Spirometry
If your doctor believes you are exhibiting signs of COPD, asthma, or pulmonary fibrosis, he may perform a spirometry test. These tests can also be used if you already have a lung disease in order to see how well your treatment is working.
During a spirometry test you will exhale into a tube that’s attached to a spirometry device. This will result in two measurements: forced vital capacity (FVC), the amount of air you can exhale, and forced expiratory volume (FEV), the amount you can exhale in one second.
Chest X-Rays
A chest X-ray can reveal a number of things about your pulmonary health. Because they produce images of your heart, lungs, blood vessels, and airways, your doctor will be able to see how your lungs are functioning with the rest of the body. Your doctor will be able to identify cancer, emphysema, pneumonia, collapsed lungs, and heart issues that could be affecting your lungs.

Blood Gas Tests
This is a type of blood test used to determine your blood oxygen levels. Blood gas tests or blood gas analysis will provide your doctor with crucial information about the function of your lungs and can be used to diagnose a wide range of respiratory diseases. It will measure your oxygen saturation level, partial pressure of oxygen and carbon dioxide, bicarbonate, and arterial blood pH. If you already have a lung disease, pulse oximetry is a quick and noninvasive way to check your blood oxygen levels. Your doctor may recommend this, especially if you are using supplemental oxygen like an oxygen tank or oxygen concentrator.
Chest CT Scan
A CT Scan is a more advanced form of X-ray allowing your doctor to see more detailed images of the chest and its internal organs. A CT scan can be used to reveal tumors and evaluate heart and lung diseases. The main benefit of a CT scan over a traditional X-ray is that it’s much easier to see subtle details in the internal organs which could be crucial for accurately diagnosing a lung diseases like pneumonia, tuberculosis, interstitial diseases, and detect inflammation of the pleura covering the lungs.

Bronchoscopy With Biopsy
A bronchoscopy is a procedure where a thin tube with a camera on the end is inserted through the nose or mouth in order to view the airways and the lungs. The biopsy part involves taking a small amount of tissue for testing which is not always necessary depending on what your doctor is testing for. Bronchoscopies are typically used to look for blockages in the airways, diagnose shortness of breath or a chronic cough, or to follow up on a CT scan that revealed a lung infection.
Electrocardiography (EKG)
Electrocardiography is a noninvasive test that can help your doctor determine if blood flow to the heart is being impaired. During this procedure, several electrodes will be attached to your chest and monitor your heart rhythm which is displayed on a screen. This type of test can be used to diagnose lung disorders that affect the blood vessels and heart.
How To Maintain Healthy Lungs
Respiration is one of the most important processes that your body performs and your lungs are at the center of it. Fortunately, you don’t have to leave your lung health up to chance. According to the Centers for Disease Control and Prevention, 39 percent of chronic lower respiratory diseases cases (the fourth leading cause of death in the U.S.) are preventable. What this means is that making healthy lifestyle choices will significantly decrease your chance of being diagnosed with a lung disease.
What’s more, many of the lifestyle changes you can make are very simple and will have far reaching effects beyond just your respiratory health. Heart health is very closely linked to lung health, so chances are, if you’re taking good care of your heart, you’re also helping your lungs. Let’s take a look at some simple things you can do to improve your health.
Avoid Airborne Pollutants
The scary thing about airborne pollutants is that we’re surrounded by them constantly, sometimes without us even knowing.
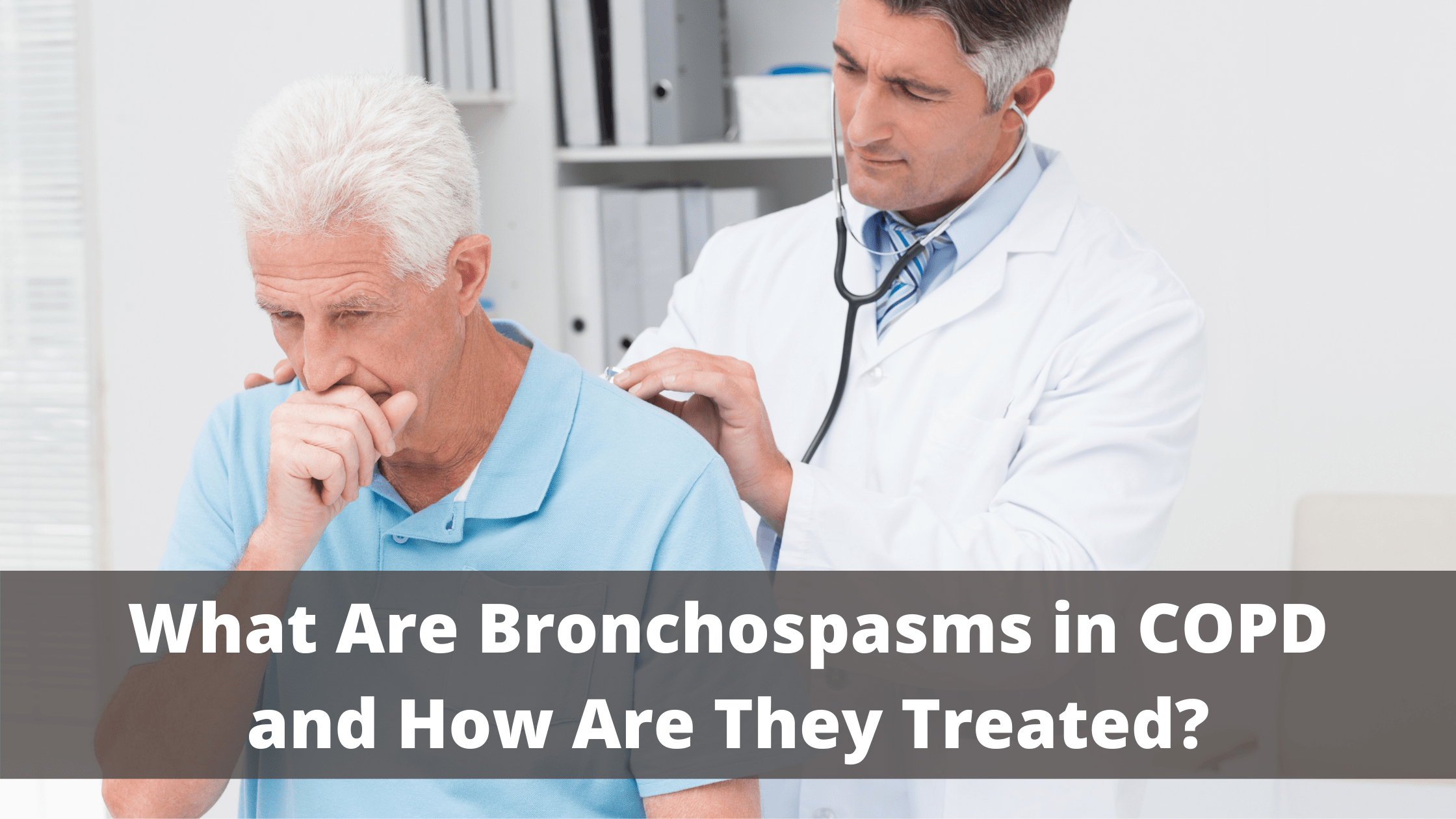
If you’ve just been diagnosed with chronic obstructive pulmonary disease (COPD), you’re probably just beginning to learn about some of the common symptoms associated with this disease. Most people — whether they’re early stage, late stage, or anywhere in between — will experience breathing difficulties, chest pain, and a chronic cough. And as it progresses, COPD patients are more likely to experience complications like hypertension, recurring respiratory infections, and heart problems.
Unfortunately, it’s not always easy to identify the root cause of COPD symptoms. For example, you might wake up one day feeling more chest pain or stiffness than usual. This could be caused by many things such as changes in environmental factors, your diet, exercise routine, or medication. If you experience an unusual or recurring symptom, be sure to take note of it and address it with your doctor during your next appointment.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
One fairly common symptom of COPD you should know about is bronchospasms. This occurs when your airways narrow, leading to difficulty breathing, chest pain, and coughing. If you’d like to learn more about bronchospasms, read on to discover what causes them, how they can affect your respiratory health, and much more. If you have any questions or concerns, don’t hesitate to leave them in the comment section below or reach out to us.
What are Bronchospasms?
Bronchospasms (also called bronchial spasms) result when your airways constrict making it difficult to breathe. As the name suggests, bronchospasms affect the bronchial tubes or the “bronchioles” in the lungs. These tubes are responsible for the transfer of air to and from the lungs. However, when they begin to constrict they don’t allow air to be transferred properly, often causing wheezing and chest pain. The bronchioles contain what’s called “involuntary” smooth muscle fibers. This means that you can’t consciously control these muscle functions similar to how you can’t control when your heart pumps blood.
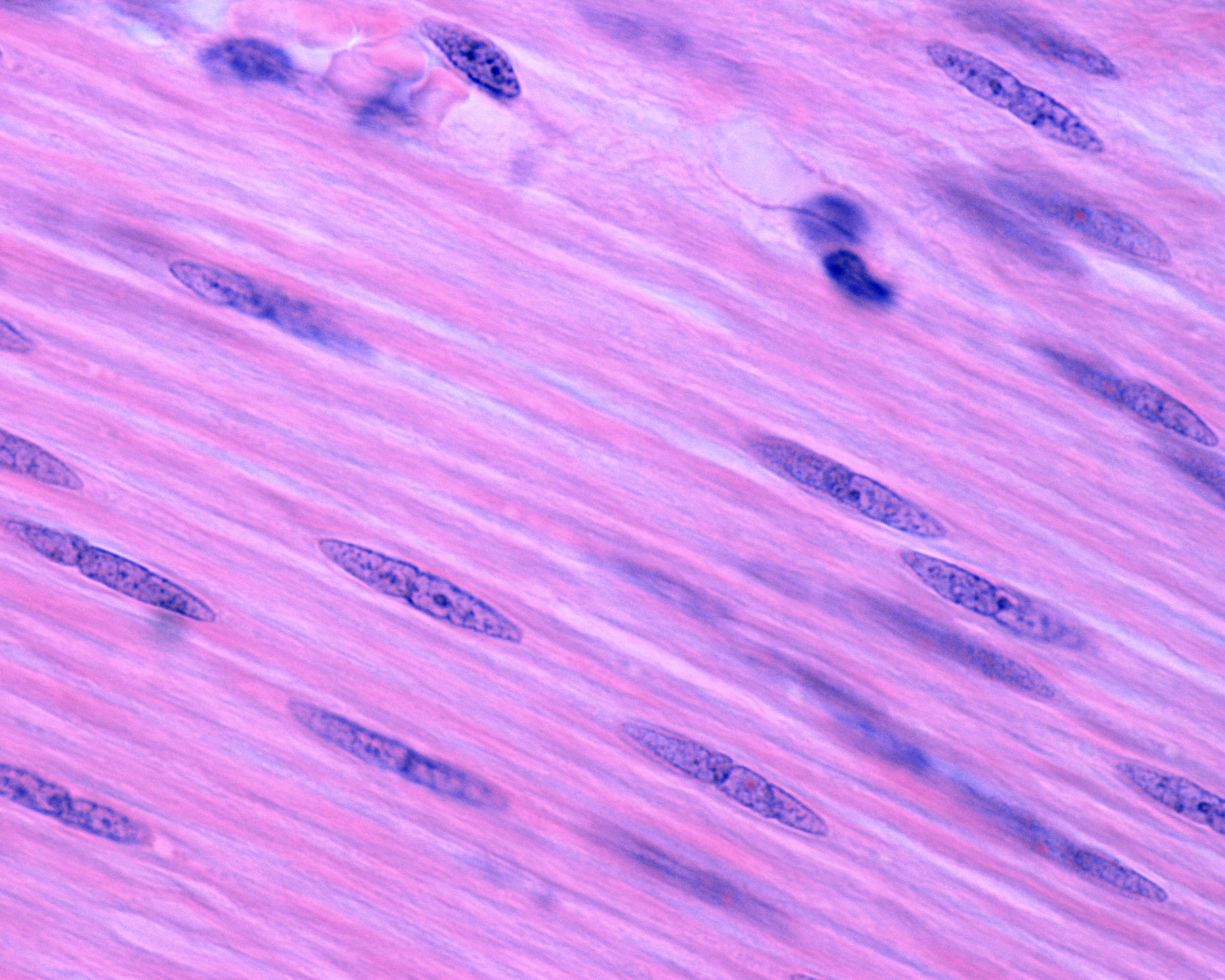
Your ability to take oxygen-rich air into your lungs and expel carbon dioxide-rich air is imperative for your overall health and well-being. Oxygen that enters the lungs is transferred to the blood through the alveoli, tiny air sacs that scatter the lungs. From there, your blood vessels carry oxygen to every organ in your body. Oxygen is an essential resource for every organ and tissue because it breaks down food so that your body can use it as energy. When tissues or organs don’t have the oxygen they need to function properly, it is called hypoxia.
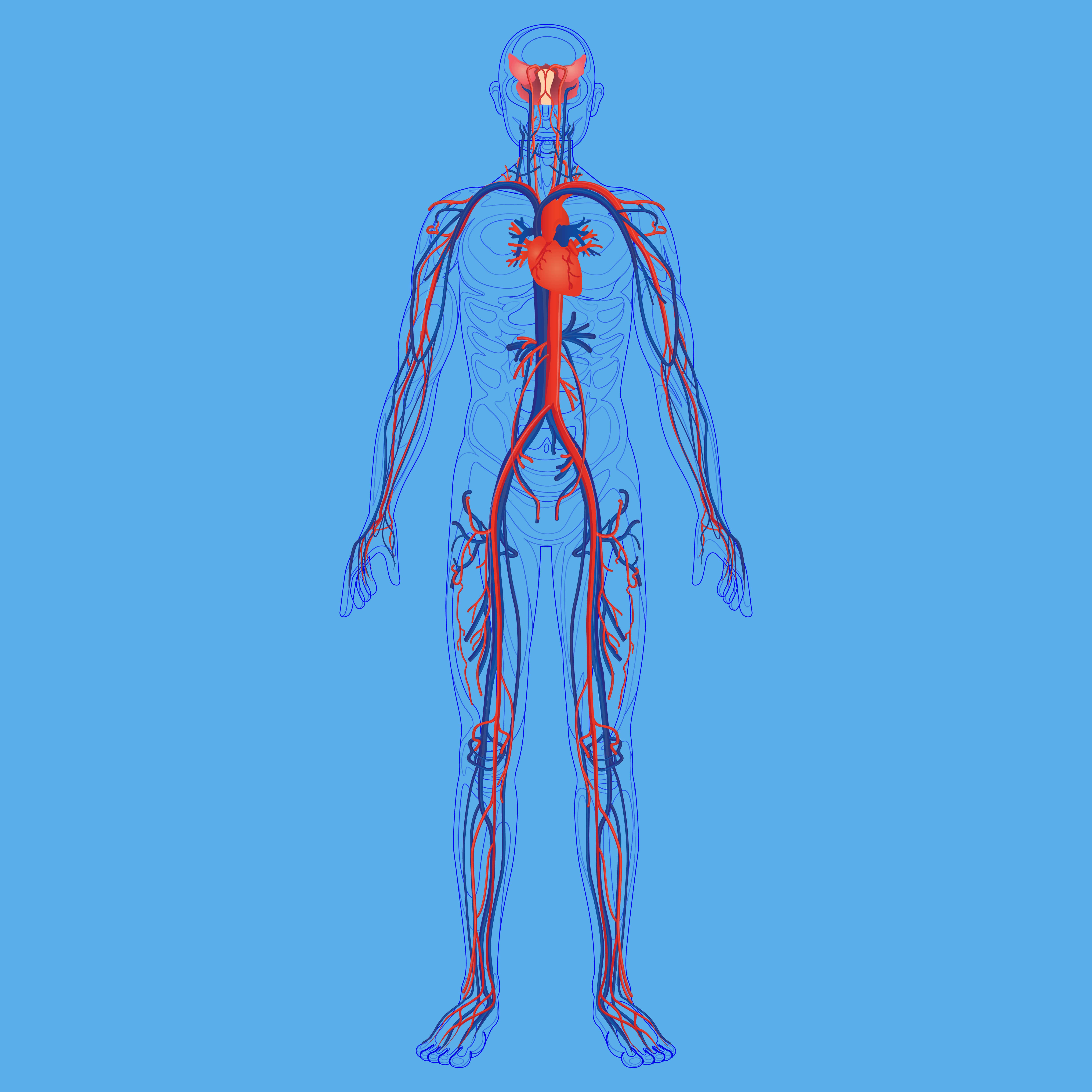
Not only do bronchospasms block air from coming into the lungs, but they can also block air from going out. This is equally problematic because your lungs need to be able to replace carbon dioxide-rich air with oxygen-rich air, otherwise carbon dioxide will begin to build up in the blood. Too much carbon dioxide in the blood is called hypercapnia and it can result in many of the same symptoms as a lack of oxygen like shortness of breath, fatigue, and dizziness.

Bronchospasms primarily occur in patients with chronic bronchitis or asthma. Chronic bronchitis is one of two chronic respiratory diseases under the umbrella term “COPD.” The other being emphysema which affects the alveoli in the lungs. While chronic bronchitis and asthma share many symptoms such as wheezing, shortness of breath, and chest tightness, they have different causes. Chronic bronchitis is primarily caused by cigarette smoking and asthma is mostly hereditary. Bronchospasms can also be induced by anaphylaxis (a severe allergic reaction) or exercise.
What Causes Bronchospasms?
There are many different causes of bronchospasms so it will be challenging to narrow down what’s causing your symptoms without speaking with your doctor. There may be one specific thing that’s causing your bronchospasms or there could be multiple things involved. Let’s take a look at some of the potential causes of these symptoms.
Air Pollution
Pollutants are one of the most common and avoidable causes of bronchospasms. According to the Centers for Disease Control and Prevention (CDC), there are six criteria of air pollutants including particle pollution, sulfur oxides, ground-level ozone, nitrogen oxides, lead, and carbon monoxide. All of these types of pollution can lead to respiratory exacerbations including bronchospasms, chest pain, coughing, and wheezing.
![]()
The best way to avoid hazardous air pollution is by checking the air quality in your area before you go outdoors. AirNow.gov is an excellent resource for asthma and COPD patients who want to be more conscious about the quality of air they’re breathing. Simply type in your area code or city and you will be provided with a forecast of the air quality in your area. It will specify the types of pollutants that are currently present so you can plan your day accordingly.
.jpg)
Air quality index (AQI) is the unit of measurement for air quality. It runs from 0 to 500 with 0 being the best air quality and 500 being the worst. Generally speaking, COPD and asthma patients should not go outside if the AQI is above 100.
Airborne Allergens
An allergen is a type of antigen that causes a severe immune response to something that would normally be harmless. Allergens can be airborne such as pollen or mold, or they can be food-based such as nuts, shellfish, or soy. If you have COPD or asthma, avoiding these triggers is imperative if you want to avoid bronchospasms and other potentially life-threatening symptoms.

There are many sites that can keep you up to date on the active allergens in your area, but Pollen.com is probably one of the most accurate and easy to use. Just like AirNow.gov, you simply have to type in your area code and you’ll have access to current information about the allergens that you should be concerned about. This is a great resource if you want to figure out what allergens affect you the most and how to avoid them.
Infections
COPD and asthma patients can have what’s called a disruption to the epithelial lining which makes them more likely to contract infections like the flu or COVID-19. Essentially, many of the immune cells in the throat and lungs become compromised due to chronic inflammation. Over time, the body loses its ability to fight off bacteria or viruses that enter the body.
Bronchiectasis is another condition that can lead to infections in COPD patients. While bronchiectasis is not caused by COPD, it is more common among COPD patients, especially in later stages of the disease. Bronchiectasis causes mucus and bacteria to build up in the lungs and prevents it from clearing properly meaning you’ll experience frequent and recurring lung infections.

Lastly, cigarette smoking will put you at a greater risk of contracting a lung infection. While many COPD patients are able to quick smoking after receiving a diagnosis, as many as 38 percent of COPD patients continue smoking. Smoking suppresses the immune system making you more likely to get sick and even causing infections to be more severe and longer-lasting. Immediate smoking cessation will help you prevent lung infection and stay healthy.
Medication
The use of certain medications can result in drug-induced bronchospasms. A few of them in particular, such as non-steroidal anti-inflammatory drugs (NSAIDs) are very well-known and widely used. For example, ibuprofen and aspirin are both NSAIDs.These drugs are used as painkillers to treat things like headaches, toothaches, and soreness. However, for some people with asthma, they can cause bronchospasms.

According to Healthline, NSAIDs inhibit a protein called cyclooxygenase and many asthma patients are sensitive to these effects. One possible reason for this is due to the overproduction of leukotrienes. These are chemicals that are released into the bronchial tubes and cause the bronchial muscles to constrict and spasm. To be safe, it’s best to consult with your doctor before using any type of medication, even if it is an over-the-counter medication.
How are Bronchospasms Diagnosed?
Your doctor may use a number of different methods to diagnose you with bronchospasms depending on your medical history and whether or not you’ve already been diagnosed with asthma or COPD. He/she will likely start by using a stethoscope to listen for any irregularities in your breathing. And if any are detected, you may be administered one of the following tests to determine if you have bronchospasms.
Spirometry
During a spirometry test, you will be blowing into a device called a spirometer. There are two different readings that your doctor will derive from this: forced vital capacity (FVC) which is the total amount of air you can exhale and forced expiratory volume in one second (FEV1) which is the total volume of air you can push out of your lungs in one second.

Pulse Oximetry
If you have COPD and you’re on oxygen, you likely already know what a pulse oximeter is. It’s a small device that attaches to your finger and reads your blood oxygen level. Your doctor may use one of these devices to see if your bronchospasms are reducing the amount of oxygen that is making it into your blood.

Arterial Blood Gas Analysis
Arterial blood gas tests are similar to pulse oximetry but they are more invasive by requiring you to draw blood. They also provide your doctor with a lot more information about your blood composition which can assist in diagnosing bronchospasms and other respiratory problems.
Eucapnic Voluntary Hyperventilation (EVH) Test
This is a type of test that attempts to simulate the effects of prolonged exercise. In other words, it allows your doctor to understand how your lungs and airways react when you are at a point of physical exertion. This test can take between 60 and 90 minutes to complete but it can be convenient in diagnosing bronchial spasms.
How Are Bronchospasms Treated?
Bronchospasms can be treated with a combination of home remedies and treatment methods prescribed by your doctor. Below are just a few of the ways your doctor may treat these respiratory symptoms.
Short-Acting Bronchodilators
Short-acting bronchodilators are used in asthma and COPD patients to provide quick relief from respiratory symptoms. They work by opening up the airways when you’re faced with severe breathing problems, chest pain, or coughing. Short-acting bronchodilators are taken with either an inhaler or a nebulizer so that the medication reaches the lungs faster.

Long-Acting Bronchodilators
If your bronchospasms are less severe, your doctor may prescribe you long-acting bronchodilators. These medications will take much longer to start working but they will also provide a much longer period of relief. Long-acting bronchodilators are typically administered orally.

Corticosteroids
If your bronchospasms were induced by an allergic reaction, your doctor may advise corticosteroids. These types of steroids will reduce inflammation in the airways and suppress the immune system which could be causing them to constrict. He/she may use any combination of the above treatment options to help you cure your bronchospasms.
What Can Be Done to Prevent Bronchospasms?
Since bronchospasms put you at a higher risk of experiencing severe complications from COPD, it’s important to do what you can to prevent them. For most people, preventing bronchospasms simply means following the treatment plan that your doctor has already created for you. If you believe that you aren’t doing enough to prevent them, consult with your doctor for more information.
Oxygen Therapy
Supplemental oxygen therapy is one of the foundational treatments for COPD and it can also help you prevent bronchospasms. The goal of oxygen therapy is to maintain a healthy blood oxygen level in your body when your lungs aren’t able to do so on their own. For some patients, this could mean using oxygen intermittently, but for others, it could mean using oxygen 24/7. Your doctor will help you decide what’s best for you.
.png)
We recommend using a portable oxygen concentrator such as the Caire FreeStyle Comfort or the Inogen One G5 because these units are lightweight and allow you to take your oxygen supply anywhere in the world with ease. They’re also extremely reliable, so you don’t have to worry about losing access to your oxygen when you need it the most.
Exercising Safely
Exercise is a fundamental aspect of any COPD treatment routine. Pulmonary rehabilitation (PR) is used to increase the strength and efficiency of the lungs while helping COPD patients maintain their weight and promote healthy circulation. However, if you exercise too much or you don’t exercise in a way that’s advised by your doctor, you might experience exercise-induced bronchospasms (EIB).

To avoid exercise-induced bronchospasms, be sure to avoid exercising in the cold. Cold, dry air can cause your mucus to become thick and difficult to clear. Air that’s filled with pollen or other allergens can also irritate your airways causing bronchospasms. Lastly, you should be careful not to overexercise. High-intensity exercise is not typically recommended for treating COPD and it can put you at a higher risk for experiencing exacerbations or other serious complications. Stick to a moderate, but consistent exercise routine.
Diet
Your dietary habits can make the difference between a healthy and unhealthy respiratory system. As aforementioned, consuming food that you’re allergic to can exacerbate your respiratory symptoms and cause bronchospasms. COPD patients tend to retain sodium, so you should avoid food with added salt and drink plenty of water. Being well-hydrated means your mucus will be less viscous and easier to clear from your airways. Foods to avoid include coffee, sugary drinks, fried foods, and milk.

Another thing to be wary of is dietary supplements. While dietary supplements are often hyped-up through advertising and word of mouth, they have negative side-effects just like over-the-counter and prescription drugs. The problem is that dietary supplements are registered as “food products” through the Food and Drug Administration (FDA) so companies can often get away with overexaggerating the benefits of their supplements without discussing the potential side-effects.
Conclusion
Bronchospasms are a common symptom of COPD and asthma, but under certain circumstances, they can also occur in healthy people. Severe allergic reactions, air pollution, and medications can all cause bronchospasms and they can range in severity from moderate to life-threatening. While there are several home remedies that can help alleviate the symptoms of bronchospasms, your best bet will be to speak with your doctor as soon as possible.
In the meantime, your best course of action is to follow your COPD treatment plan. Using supplemental oxygen as prescribed, following a strict diet, and maintaining a healthy and consistent exercise routine will all promote healthy lungs and airways, thus helping you to prevent bronchospasms and other respiratory complications. You should also take the time to check the air quality in your area before going outside so that you can avoid air pollution.
Here at LPT Medical, our goal is to provide as many COPD patients as possible with durable and reliable portable oxygen concentrators. With a portable oxygen concentrator at your side, you’ll have the freedom to go about your daily life without having to worry about not having medical oxygen that meets your respiratory needs. If you need help choosing an oxygen concentrator, please feel free to give us a call at 1-888-416-3855.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













