.png)
Most people don’t put a lot of thought into the way that they get around. As humans, we learn to walk from a very young age and we use our basic motor skills all the time. So, for most people, it’s difficult to imagine being in a situation where these basic functions are impaired. However, for someone with COPD, problems with mobility, balance, and coordination can be a daily struggle. Healthy, functioning lungs are essential for physical exertion, no matter how little it may be.
A study on pubmed.gov followed COPD patients over the course of six months and found that about one-third of them experienced a fall at some point. The same study also states that COPD is one of the chronic conditions with the highest fall rates, right behind osteoarthritis, a very common degenerative joint disease that’s caused by the wearing down of cartilage on the bones.
Unfortunately, the high risk of falls in COPD patients is very much an under-discussed topic. That’s why, in this article, we’ll take a look at the main causes of falls and how you can avoid them. If you have any questions, please feel free to leave them in the comment section below and we’ll get back to you as soon as possible.
What Causes Balance Issues in COPD Patients?
COPD balance and coordination issues aren’t limited to one cause. There are many different factors that need to be considered in order to pinpoint and mitigate your risk of experiencing a fall. Comorbidities, age, COPD stage, and environmental factors can all play a role, so it’s important to be open-minded about possible prevention methods.
Low Blood Oxygen Levels
Oxygen is a vital resource for your body. It’s used to break down stored energy that you get from food and convert it into usable energy for every cell in your body. Since COPD patients have impaired lung function due to excessive inflammation, medical oxygen can be used to lessen the load on the lungs and ensure that your blood oxygen levels stay within a normal range. Contrary to what many people believe, there are no “side-effects” of medical oxygen. As long as you’re using it as prescribed, medical oxygen will only benefit you.

When it comes time to buy an oxygen device, you’ll have several options. Oxygen tanks, liquid oxygen tanks, and oxygen concentrators are all popular options. However, portable oxygen concentrators will be the best option for most oxygen patients because they’re lightweight, small, and easy to carry as you go about your day. The Inogen One G5 and Caire FreeStyle Comfort, for example, are two of the most popular options because they have a high oxygen output, and they both weigh under 5 pounds.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Another great option if you have higher oxygen demands is the Respironics SimplyGo. This is the lightest continuous flow portable oxygen concentrator and it offers up to 2 liters per minute (LPM) of oxygen. The Respironics SimplyGo can either be carried on your shoulder with the adjustable strap, or it can be wheeled behind you using the rolling cart. Be sure to speak with one of our respiratory specialists here at LPT Medical to learn which portable oxygen concentrator is right for you.
Peripheral Edema
"Edema” is a term that refers to swelling, usually due to the buildup of fluid. Peripheral edema occurs when fluid begins to accumulate in an extremity away from the heart such as the hands, feet, or legs. While this condition can happen to anyone, it’s more common among COPD patients and it can be a warning sign of several serious medical conditions including pulmonary hypertension (high blood pressure in the lungs) and cor pulmonale (right-sided heart failure).

Another problem that can be caused by edema is problems with balance and coordination. This condition often develops slowly and without the patient knowing, so you might start losing control of your balance without knowing it as well. Oftentimes, people first notice that there’s a problem when their shoes or clothing don’t fit anymore. In order to avoid this situation, check your legs and feet daily for swelling, redness, or pitting. This is when you press your skin and it leaves an indentation.
Malnutrition
COPD patients are more likely to experience malnutrition than the general public. There are many possible reasons for this, but a loss of appetite, changing food preferences, and problems with digestion are among the most common causes. COPD patients often find themselves in a difficult situation where they’re hungry but aren’t in the mood to eat because it can leave them feeling bloated and exhausted.

One significant concern is something called muscle atrophy (muscle wasting). Many people are under the impression that they’re losing fat, but it’s actually muscle weight that they’re losing. Inevitably, this can lead to problems with balance, coordination, and exercise tolerance. This is why it’s so important for COPD patients to consume enough protein. Today’s Dietician recommends you get at least 20 percent of your calories from protein.
Medication Side-Effects
Every medication has side-effects, including those used to treat COPD. One of the most common inhaled COPD medications, bronchodilators, are used to open up the airways helping you to breathe easier. However, bronchodilators have a number of adverse side-effects including but not limited to trembling, muscle cramps, and nausea, all of which can contribute to balance problems and even result in serious falls.

Just like with oxygen, it’s important to use medication only as it’s prescribed by your doctor. What’s more, you should be cautious about the way you use it. For example, if you’re using a bronchodilator, try sitting down beforehand. This way, if you start feeling dizzy or lightheaded, you won’t run the risk of falling down. Bronchodilators are fast-acting, so if you feel okay after a couple of minutes, you can stand up and go about your business.

Corticosteroids are another popular medication used to treat COPD. These are a type of steroid that is used for the long-term treatment of COPD and asthma, and they help to reduce inflammation and tightening in the airways and lungs. However, corticosteroids used in large doses can contribute to bone deterioration and the development of osteoporosis. This condition not only increases your risk of falls, but it also increases your risk of experiencing bone fractures after falling.
Sedentary Lifestyle
Living a “sedentary lifestyle” means not getting up and moving around very often. Many people become more sedentary the older they get and developing a chronic condition like COPD can cause someone to become sedentary as well. The problem with this is that it can lead to a lot of health issues, one of which is an increased likelihood of experiencing a fall. This study found that physical activity is associated with better balance and slowing the rate of physical deterioration in older adults.
Environmental Factors
All of the issues above are caused by the symptoms of COPD and COPD treatment. But you also need to consider how your environment is contributing to your risk of falls. Living in a home that is cluttered or not designed to accommodate someone with a chronic respiratory disease can put you at a higher risk of falling.

Since it’s winter, there are also environmental factors related to the weather. According to the World Health Organization (WHO), 56 percent of all falls occur outside the home such as in the yard, on the sidewalk, or in a public area. So before you go anywhere, you should consider what obstacles will be presented and how you can navigate them safely without experiencing a fall.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
What Can Be Done to Prevent Falls With COPD?
Although falls are very common in COPD patients, the good news is that they’re highly preventable. Just a few small adjustments to your lifestyle could make a huge difference but you need to know what’s causing them in the first place.
Carry a Pulse Oximeter
A pulse oximeter is a small electronic device that slips over your finger and tells you your blood oxygen levels. It is a non-invasive device, meaning you won’t need to draw blood in order to use it. It works by passing light through your finger and calculating your blood oxygen levels based on the amount of light that’s absorbed by oxygenated or deoxygenated blood. Pulse oximeters are lightweight and portable medical devices.

The reason it’s so important to have a pulse oximeter is to be able to check your blood oxygen levels and heart rate, especially when you’re away from home. Just a quick pulse oximeter reading and you’ll know exactly what adjustments you need to make to your oxygen therapy device. Pulse oximeters are usually recommended over arterial blood gas analysis (ABG) because they’re less intrusive and you receive your results almost instantaneously. The quality of the device matters too, so be sure to spend some time looking for a pulse oximeter with good reviews.
ABG analysis and pulse oximetry also differ in terms of the information they provide. While a pulse oximeter just reads the percentage of hemoglobin in the blood that is saturated with oxygen (SpO2), ABG tests will provide you with a whole host of information including blood alkalinity, the partial pressure of CO2 and oxygen (PaCO2 and PaO2), and much more. This information is useful for other reasons, but it’s not necessary if you’re just trying to maintain your blood oxygen levels.
Carry a Medical Alert System
A medical alert system or personal emergency response system (PERS) is a small device that’s worn around your neck or on your wrist. If you ever experience an emergency like a fall or a COPD exacerbation, simply press the button on the device and a notification will be sent to a 24/7 call center. Once the notification is received they will call 911 and emergency medical personnel will be sent to your home immediately.

Adjust Your Eating Habits
As aforementioned, many COPD patients are underweight. As respiratory symptoms get worse, many people find it difficult to eat a full meal without feeling bloated and tired. One of the best ways to deal with this is to spread your meals throughout the day rather than having one or two bigger meals. This will give your body lots of time to digest rather than having to do it all at once.
![]()
Another reason to spread your meals out is that it helps you avoid the temptation to eat unhealthy foods. When you’re feeling hungry and lacking energy, you’re more likely to give in to foods that will provide you with a quick energy boost. These foods are usually high in sugar and other unhealthy ingredients which can exacerbate COPD symptoms and leave you feeling drained.
Get Active
Many people are under the impression that the sole purpose of pulmonary rehabilitation is to improve lung function. And while that may be the most important reason, it’s not the only reason. Even a moderate form of exercise can provide some major benefits as long as it’s done consistently. According to the Mayo Clinic, regular exercise helps prevent a whole host of health problems, including but not limited to high blood pressure, type 2 diabetes, depression, and heart disease.

Another reason for COPD patients to exercise is that it increases their muscle tone, thus increasing their oxygen efficiency. As a COPD patient, you want every muscle in your body to be strong not only to improve balance and posture but to reduce the amount of oxygen required for getting around. Exercise also improves blood circulation which is very important for maintaining your mobility.
Create a Safe Living Space
No matter whether you live alone or with friends or family, making adjustments to your living space can go a long way towards preventing falls. Keeping your home organized and free of debris will give you fewer obstacles to trip over or navigate around as you go about your daily life. Many falls occur in the bathroom, so that might be the best place to start with. Another way to create a safe living space is to install mobility aids such as hand railings, stairlifts, or ramps.

Address Your Concerns With Your Doctor
Anxiety is associated with an increased risk of falls, so if you have concerns about balance or coordination issues caused by COPD or your COPD treatment plan, you should address them with your doctor immediately. Chances are, the feelings you’re experiencing are perfectly normal and your doctor might be able to make changes to your medication, exercise, or diet plan in order to improve your balance. As the saying goes, there’s no such thing as a “stupid question” especially when your health is concerned.

Conclusion
Although COPD is a leading morbidity in the United States, many people are not fully aware of what it’s like to live with this disease. Balance and coordination issues are pervasive among COPD patients and they become more prevalent with age and as the disease progresses. The tips outlined above will help you mitigate the risks of falls.
Here at LPT medical, we want you to be educated about your disease so that you can make the best decisions for your long-term health. We carry a wide range of portable oxygen concentrators from popular brands like Caire Inc., Inogen, and Respironics. And we take pride in providing oxygen patients all over the country with reliable lightweight devices that help them get around more easily while limiting the risk of a fall.
If you’re interested in our portable oxygen concentrators for sale, please reach out to us either by phone or by email.
.png)
Supplemental oxygen therapy, or simply “oxygen therapy,” is the use of medical-grade oxygen to treat a variety of conditions. In hospitals, short-term oxygen therapy is used to help patients recover from surgery or acute conditions, but oxygen can also be administered for long-term in-home use in people with chronic lung diseases like COPD and cystic fibrosis.
No matter what your reason is for using supplemental oxygen, it’s important that you’re using it correctly because it can be a fire hazard. While oxygen itself cannot burn, it is what’s called an oxidizer meaning it makes everything it comes into contact with more flammable. What’s more, improper use of oxygen can lead to oxygen toxicity or lung damage that results from inhaling too much oxygen.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In the following sections, we’re going to take a look at some of the most common mistakes new oxygen users make and tell you how to avoid them. If you have any questions about using oxygen safely and effectively, be sure to address them with your doctor. And if you have questions about what you read here, leave them in the comment section and we’ll get back to you.
Choosing the Wrong Oxygen Device
Oxygen therapy has been used since the 1950s to treat conditions like pneumonia. However, as you can imagine, it has evolved over the years as researchers have learned more about how supplemental oxygen can be used safely and effectively. In the past, oxygen tanks were the only option for people suffering from respiratory conditions. But nowadays, there are many other types of oxygen devices at peoples’ disposal like liquid oxygen tanks and oxygen concentrators.

The first mistake many patients make when they’re first prescribed medical oxygen is choosing the wrong oxygen device. What happens is that many people rush into choosing something rather than taking the time to do research and figure out what options are available to them. And while oxygen tanks are certainly a popular choice for long-term oxygen therapy, they are not the only one.
Liquid oxygen, for example, is a common alternative to traditional oxygen tanks. Rather than storing oxygen in its gas form, these oxygen tanks are kept at very low temperatures in order to keep the oxygen in its liquid form. The reason for this is because oxygen expands significantly in its gaseous state meaning it takes up a lot more space. What’s more, it’s stored at much higher pressures making it more dangerous to use.

While liquid oxygen enables oxygen patients to experience more freedom, they’re not without their downsides. In order to keep oxygen in its liquid form, you need a special container. For safety reasons, these containers need to be vented so that as the heat increases, the pressure can also be released. What this means is that you will slowly lose your oxygen supply over time if you aren’t using it. According to the Lung Institute, liquid oxygen will evaporate after a week or two.
Another downside to liquid oxygen is that it’s more expensive than traditional oxygen tanks. Not only do the units themselves cost more, but they cost more to maintain and refill. As a result, Medicare and other healthcare providers may not help you pay for them like they do with compressed oxygen. Luckily, liquid oxygen and compressed oxygen are not the only supplemental oxygen options available to you.
.png)
Oxygen concentrators are a newer more advanced form of oxygen therapy. As opposed to storing oxygen like the aforementioned devices, oxygen concentrators are electronic devices that draw in ambient air and put out pure medical-grade oxygen. Home or stationary oxygen concentrators need to be plugged into the wall but portable oxygen concentrators run off of batteries, allowing you to go wherever you please.
Not Using Oxygen As It’s Prescribed
Like we mentioned earlier, oxygen is a controlled substance in the United States. Oxygen sales are regulated by the U.S. Food and Drug Administration to ensure that only respiratory patients have access to medical oxygen. But being prescribed oxygen does not mean you should use it however you please. You need to follow your doctor’s instructions for using it safely and effectively.
More often than not, people begin to fall back on their oxygen routine as time goes on. It’s not unusual to feel exhausted always being connected to your oxygen device and many people experience discomfort with the nasal cannula. If you’re falling back on your oxygen therapy plan because of irritation or dryness in your nose, please read this post to get a few tips for alleviating these issues.
If the reason you’re not using enough oxygen is because of your oxygen device, following the instructions above to get the oxygen device that’s right for you may be your best option. Unfortunately, since oxygen tanks only provide a limited amount of oxygen, people find themselves turning down their flow rate in order to have more freedom. This is a bad idea because it means your blood is not saturated with the right amount of oxygen to keep you healthy. Fortunately, portable oxygen concentrators help you to ensure that you have access to oxygen wherever you are in the world so that you don’t have to turn down your flow rate.

Although less common, it is possible for someone to use more oxygen than they’re prescribed. For example, if you’ve been exercising and you’re feeling out of breath, you might feel tempted to turn up the flow setting on your oxygen device. Before doing any form of exercise, you should consult with your doctor and ask him/her what an acceptable flow rate is while you’re sedentary and while you’re exercising. Also, be sure to carry a pulse oximeter with you when you exercise so that you can ensure that you stay at the correct blood saturation level.
Another reason you might be using too much oxygen is if you’re unaware of the harmful effects of having too much oxygen in your system. While oxygen is vital for the healthy functioning of every organ in our bodies, having too much of it in your blood can lead to oxygen toxicity. This condition will result in coughing, difficulty breathing, and chest pain. Prolonged exposure to high partial pressures of oxygen can even result in death. Before taking the initiative to increase your oxygen flow rate if you’re feeling out of breath, be sure to consult your doctor. There could be any number of reasons that are causing a flare-up in your symptoms. For more information on preventing COPD flare-ups, check out this blog post.
Not Cleaning Your Oxygen Therapy Device
In this day and age, the saying “cleanliness is next to godliness” has taken on a whole new meaning. With the advent of the novel coronavirus, our society as a whole has been more conscious of the spread of bacteria, germs, and viruses. What many people don’t acknowledge or even realize is that COPD patients and other respiratory patients are at a higher risk of both contracting and experiencing severe symptoms from infections.
One of the added health risks that COPD patients experience is having to carry around an oxygen device that can collect bacteria. Even if you’re careful not to set your oxygen concentrator or oxygen tank down in a dirty place, it’s inevitable that it will collect germs. Aside from the concentrator or tank itself, the nasal cannula and oxygen tubing can also get dirty so you should be sure to clean them often.
COPD patients are sensitive to certain cleaning products, especially ones with bleach, ammonia, and fragrances. So, when you go to clean your oxygen concentrator, be sure to not use any products that could exacerbate your symptoms. Cleaning products marked as “safer choice” are regulated by the Environmental Protection Agency (EPA) and they don’t contain as many harmful chemicals as standard cleaning products. You can also make your own cleaning products so that you know exactly what’s in them.

Whenever you leave the house, be sure to take your cleaning product of choice with you. Clean the unit once or twice a day and make sure to get all sides including the bottom. The nasal cannula and oxygen tubing should be cleaned as well. The Lung Institute recommends washing them in 10 parts water one part vinegar and then rinsing them and leaving them to dry completely. Oxygen tubing should be replaced after several months of use.
Smoking Around An Oxygen Device
Smoking is the number one cause of chronic obstructive pulmonary disease. But did you know that many people (around 38 percent) continue to smoke even after being diagnosed? Unfortunately, being unable to kick this bad habit means you’re unlikely to make much progress on your COPD treatment plan. After all, the purpose of using oxygen is to help limit and prevent symptoms like breathlessness, chest pain, and a chronic cough. But smoking regularly will just cause these problems to resurface.

Another reason to avoid smoking is that it could damage your oxygen device. Oxygen concentrators work by taking in ambient air and removing nitrogen and other gases. If you’re smoking near your concentrator, the smoke could damage the internal components. Most concentrators have particle filters but these won’t stop smaller particles from entering the device. However, you should remove the particle filters regularly and clean them off so that they’re as effective as possible.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
The third and final reason you should avoid smoking near an oxygen device is for safety reasons. While your oxygen tank or concentrator won’t explode or catch fire like many people believe, they are still a fire hazard. According to the National Fire Protection Association (NFPA), 5 percent of all home fires between the years of 2012 and 2016 were caused by smoking materials. That’s around 19,000 fires each year that could be prevented if cigarettes were not a concern.

Fires that are exposed to medical oxygen will burn faster and be harder to put out. Since supplemental oxygen is a medical necessity, cigarette smoking is really the only variable in this scenario. We wrote a whole guide on smoking cessation so be sure to check it out if you’re struggling to drop the habit.
Not Enjoying Your Newfound Freedom
Last but not least, you need to be able to enjoy the newfound freedom that your oxygen device has afforded you. This means getting out of the house, exercising, exploring, and visiting friends and family. Far too many COPD patients believe that being prescribed supplemental oxygen means giving up all of the things that you love to do, but this couldn’t be farther from the truth.

While you can live a sedentary lifestyle if you choose, the main purpose of oxygen therapy is to help you get back on your feet and moving again. Portable oxygen concentrators like the Caire FreeStyle Comfort and Inogen One G5 have pushed the boundaries of what’s possible for oxygen patients because they weigh under 5 pounds and they supply enough oxygen for the vast majority of COPD patients.

Another major advantage of portable oxygen concentrators is their lithium-ion batteries. These batteries are extremely durable and long-lasting meaning you can stay out and about for longer than ever before. The FreeStyle Comfort allows you to run your oxygen device for up to 16 hours without recharging and the G5 allows you to run your oxygen device for up to 13 hours without recharging.
Conclusion
All things considered, it can be somewhat overwhelming being prescribed supplemental oxygen therapy. You need to understand exactly what your prescription entails and you need to find an oxygen device that will meet your needs. While this will certainly take some trial and error, however, you can always rely on experts such as your doctor or pulmonologist if you need help.
If you’re interested in learning more about using a portable oxygen concentrator for supplemental oxygen therapy, you need to ensure that you receive a device that is capable of meeting your medical needs as well as your personal preferences. Rather than taking hours out of your day to research every device on the market, reach out to our oxygen specialists here at LPT Medical. We take the time to understand what your needs are and then we apply our knowledge of oxygen concentrators to align you with the perfect device for your needs.
We offer a wide range of products from stationary oxygen concentrators to pulse dose portable oxygen concentrators and all the oxygen accessories you need to make the most of them. If you have any questions at all or you’re ready to pick out an oxygen machine, you can reach us by phone or email.

Managing chronic obstructive pulmonary disease (COPD) can feel like a balancing act a lot of the time. On one hand, you want to do everything you can to reduce the symptoms and prevent the progression of your disease. However, on the other hand, you don’t want to use any treatments that could cause serious side-effects. It’s not always easy to find a balance between these two things and create a routine that works for you.
This has never been more true than with home remedies. Simply put, a home remedy is an easy and accessible treatment option for an ailment that you can do at home. Home remedies are not prescribed by a doctor and they typically have more anecdotal evidence to prove their efficacy than hard scientific fact. What’s more, home remedies aren’t always focused on treating a specific disease like COPD. Instead, they could be focused on improving your health in general which, in turn, could help you treat your COPD.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Rather than taking a risk with home remedies you may find on social media or elsewhere on the internet, we’re going to outline some COPD home remedies that are proven to be safe and effective. Just remember that home remedies should never be put before the treatment plan prescribed by your doctor including but not limited to supplemental oxygen therapy, pulmonary rehabilitation, and an improved diet. As always, if you have any questions about what you read here, don’t hesitate to leave a comment and we’ll get back to you as soon as possible.
Dietary Supplements
Dietary supplements are commonly misunderstood in today’s world. Many people are under the impression that dietary supplements can replace a healthy diet and others are convinced that dietary supplements do nothing at all. However, the truth is somewhere between these two points of view. Supplements can potentially enhance your diet, but there are also a few things you need to be aware of in order to use them safely.

Dietary supplements are not considered “medication” by any means. In fact, the Food and Drug Administration (FDA) classifies them as a “food product.” The good news is that this means they are widely available and you won’t need a prescription in order to buy them. But the bad news is that supplements are not regulated the same way as medication. It also means you’ll have to do your due diligence and research supplements, as well as the company selling them before you make any commitments.
Vitamin D Supplements
It’s a well-known fact that many people develop vitamin D deficiency after contracting COPD. According to the National Emphysema Foundation, over half of all COPD patients develop vitamin D deficiency because they consume fewer foods that are high in vitamin D and they are less likely to spend time outside in the sunlight which is a major source of vitamin D for many healthy people.

The main problem associated with vitamin D deficiency is osteoporosis, a condition where the bones become weak and brittle. Vitamin D plays an important role in the absorption of calcium which gives the bones their structure and strength. Vitamin D also plays an important role in the growth and function of muscles which is also very important for COPD patients.
Ginseng
Ginseng has a long history of use in Chinese medicine. It’s an herb that’s believed to improve pulmonary function as well as respiratory endurance. It’s known for both its antioxidant and anti-inflammatory effects as well as being able to regulate blood sugar levels. While the benefits of ginseng look promising, it’s important to discuss with your doctor before using it because it’s known to interfere with certain COPD medications.

N-Acetylcysteine (NAC)
This is an antioxidant supplement that’s shown potential when it comes to thinning mucus, reducing phlegm, and clearing the airways. Like ginseng, NAC is a widely available supplement that can be bought without a prescription. However, it is also known to interfere with certain medications, so it’s important to consult with your doctor before using it to treat your COPD.
Smoking Cessation
The vast majority of people who have COPD have smoked in the past and about 38 percent of current COPD patients are also smokers. Many people believe that, since they’ve already contracted COPD, there is no reason to put in the effort to quit smoking. But this could not be farther from the truth. The main reason to quit smoking is to slow the progression of COPD, but there are a whole host of other reasons as well.

Smoking increases your risk of conditions like heart disease, heart attack, diabetes, and more. What’s more, current evidence suggests that smoking is associated with increased severity of disease and a higher likelihood of death in COVID-19 patients. Smokers are known for having impaired immune systems which could also put you at a higher risk of contracting respiratory infections.
While there are many prescription medications you can use to quit smoking such as Chantix or Zyban, there are also many natural methods for quitting smoking. One thing you should know about smoking and other types of addictions is that you need it in order to feel normal. If you’re deprived of it for too long, you will likely start to experience feelings of withdrawal. When this happens, you’ll experience intense cravings, along with headaches and a change of mood. This is when you’re most likely to fall back into your smoking habits.
In order to avoid these intense feelings, you may have to slowly wean yourself off cigarettes or use a common technique like nicotine replacement therapy. Unfortunately, many smokers feel like they’re up against impossible odds when it comes to smoking cessation. Maybe you’ve seen others around you fail at losing cigarettes or you just don’t feel like you have it in you. But the truth is, it takes many attempts to quit smoking. This study suggests that it could take anywhere between 8 and 14 attempts to drop a smoking habit for good.
Cleaning Your Home
For most people, cleaning the house is a chore. But for someone with COPD, it can be a lifesaver. There are two reasons you should clean your home on a daily basis: first and foremost, it helps to eliminate airborne allergens and bacteria from your home, and secondly, cleaning is a therapeutic activity that helps you feel accomplished and whole. When your living environment becomes messy or dirty, you’re far more likely to experience issues like anxiety and depression.

Before you start cleaning, you need to make sure you’re using safe cleaning products that don’t contain dangerous chemicals that could exacerbate your respiratory problems. Unfortunately, the cleaning product industry is rife with hazardous chemicals that, if inhaled, can lead to coughing, wheezing, chest pain, shortness of breath, and even permanent lung damage. In COPD patients, inhaled chemicals can even cause severe exacerbations.
Volatile organic compounds (VOCs) are some of the most common hazardous materials you should keep an eye out for. Some common personal and home care items that include VOCs are:
- Disinfectants and cleaners
- Pesticides
- Air fresheners
- Deodorant and cosmetics
- And fuel

Other hazardous things in cleaning products include bleach, ammonia, ethylene glycol, monobutyl acetate, sodium hypochlorite, and trisodium phosphate. If at all possible, you should entirely avoid using cleaning products with these chemicals in them. However, if you absolutely have to use them, you should ensure that the room is well-ventilated, you should always wear a mask, and avoid getting the cleaning product on your hands or near your eyes or mouth. Refer to the Cleveland Clinic for more information on cleaning safely if you have COPD.
Breathing Exercises
Breathing exercises may seem silly to someone who has never tried them. However, the more you look into them, the more you begin to realize the bad breathing habits people develop over the course of their life. As a society, we spend more time sitting and remaining sedentary than ever before. This has caused many people to develop a shallow, ineffective breathing method that can be dangerous for someone with COPD or other respiratory conditions.
Breathing exercises are very easy to practice in the comfort of your own home and they are the perfect thing to incorporate into your daily routine. Not only will breathing exercises help you correct bad breathing habits, but they will also teach you how to reduce and manage anxiety more effectively.
.jpg)
One of the worst habits for COPD patients to develop is chest breathing. This type of breathing is focused on using the chest muscles in order to expand the lungs which can be exhausting with inflamed and obstructed lungs. Chest breathing should be replaced with diaphragmatic deep breathing which is focused on using the diaphragm, the thin sheet of muscle above the stomach to expand the lungs.
Anxiety Management
Cleaning regularly and practicing breathing techniques are both great ways to reduce anxiety, but they aren’t the only ones. The tricky thing about anxiety, depression, and other mental health disorders is that they can be triggered by just about anything. Some people may experience anxiety about their health whereas other people may experience anxiety for reasons that are purely biological.
The first step to preventing anxiety is to simply follow your treatment plan as closely as possible. Your treatment plan is designed with your long-term well-being in mind and that includes your mental health. Things like exercise and a healthy diet will help with full-body wellness and they’re always the first things you should commit to if you want to feel happier and more motivated. If you’ve tried all of this and you’re still experiencing anxiety, cognitive behavioral therapy (CBT) is the best alternative.
Weight Management
COPD is commonly linked with weight loss. Due to the increased energy that it takes to breathe with COPD, a changing immune system, and other factors like a loss of appetite, many COPD patients find themselves losing an unhealthy amount of weight. Oftentimes, this weight can be muscle mass rather than fat which is the most dangerous part about it. Your body needs muscle strength in order to breathe and get around more efficiently, so it’s very important to keep a healthy weight with COPD.

Weight management is something that can be done at home. Your doctor has likely set you up with a new diet plan that includes high protein, fiber, and healthy fats. You should follow this plan as closely as possible. What’s more, you should eat regularly throughout the day instead of eating one or two big meals each day. This will prevent you from feeling exhausted or bloated after eating and keep your energy levels stable throughout the day.
![]()
The second thing you should be aware of is your exercise routine. Pulmonary rehabilitation isn’t just designed to keep your lungs strong, it’s also important for helping you manage your weight by keeping fat off and muscle on. Like your diet, the most critical thing with pulmonary rehab is consistency so try to incorporate fitness into your daily routine.
Healthy Sleep Habits
Your sleep/wake cycle doesn’t just affect your alertness throughout the day, it also affects your energy levels and your ability to take on the challenges that COPD presents. For example, someone with a healthy sleep schedule will have a better mental attitude and a better willingness to make lifestyle changes that will positively impact their respiratory health. A poor sleep schedule can also contribute to anxiety which can further exacerbate COPD.

The key to a healthy sleep schedule is consistency. Adults should be getting between 7 to 9 hours of sleep each night and your sleep schedule shouldn’t vary night-to-night. Try to get to bed and wake up at the same time each day. Doctors also recommend avoiding naps throughout the day, getting plenty of exercise, and avoiding using electronics before you go to bed.
If you’re concerned that you’re losing sleep at night due to low oxygen levels, you may want to speak with your doctor about using supplemental oxygen therapy while you sleep. You are likely already on some form of oxygen therapy, but using an oxygen concentrator while you sleep will ensure that your blood oxygen levels remain stable throughout the night. Portable oxygen concentrators like the Caire FreeStyle Comfort or the Inogen One G5 are great options because they’re small, quiet, and can be plugged into any wall outlet meaning they’ll never turn off on you in the middle of the night.

If you have obstructive sleep apnea (OSA) and need to use a CPAP or BiPAP machine while you sleep, you will need to use a continuous flow portable oxygen concentrator like the Respironics SimplyGo. This concentrator is designed to put out a constant stream of oxygen, so if your breathing is interrupted for any reason while you sleep, you can rest assured that you’ll still be receiving medical-grade oxygen.
Conclusion
When it comes to treating COPD, you need a comprehensive approach that takes into consideration all facets of your life from your sleep schedule to your mental well-being. Home remedies are a great way to make you more conscious about how your lifestyle is affecting your health and what steps you can take to reverse these issues.
At the same time, however, you need to be careful about what home remedies you use. Some people will make unfounded claims about dietary supplements or other remedies which can actually make your symptoms worse. This is why you should always consult your doctor before using a new product or making drastic changes to your lifestyle.
Above all, you should be focusing on the treatment plan that you’ve created with your doctor. Doing so will help you alleviate breathlessness, chest pain, and coughing associated with COPD and you can expect to see a better prognosis for your disease.
.png)
The novel coronavirus has completely reshaped the way that we view sanitation. Over the past year, organizations and individuals alike have taken steps to control the spread of disease, and the population as a whole has become more aware of the impact of infectious disease. Another thing that people have become more aware of is the impact of chronic respiratory diseases such as COPD, asthma, and pulmonary fibrosis. Studies have shown us that these people are “high risk” when it comes to infectious disease, so we need to take steps to protect their health.
Unfortunately, simply telling someone to “clean more often” or “clean more thoroughly” is bad advice. These statements fail to acknowledge that cleaning products themselves can actually put our health at risk. Many household cleaning products are filled with toxic chemicals that can irritate the eyes, skin, and throat. And in the worst cases, they can even contribute to COPD symptoms by exacerbating chest pain, difficulty breathing, and chronic coughing.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
In this post, we’re going to provide you with a comprehensive list of steps for cleaning your home as a COPD patient. We’ll give you advice on choosing cleaning products, how often you should clean, and other things you should take into consideration. If you have any questions, feel free to leave a comment. And if you find this information helpful, don’t hesitate to share it to help us get the word out about safe cleaning habits.
How to Choose Cleaning Products With COPD
The first step in cleaning your home is to choose the cleaning products that you will use. While this may sound like the easiest step, it’s actually the hardest. Cleaning products are rife with volatile organic compounds (VOCs). These are compounds that have a high vapor pressure and low water solubility. Many VOCs are artificial meaning they’re man-made, and they contain chemicals such as methyl tert-butyl ether (MTBE), trichloroethylene, oxygenates, and other industrial solvents.

According to the Environmental Protection Agency (EPA), concentrations of VOCs are up to ten times higher indoors than they are outdoors. This is largely due to the fact that VOCs are found in many household cleaning products and many homes are not ventilated well enough to rid them of harmful chemicals. But VOCs aren’t the only harmful ingredients found in home cleaning supplies. Many of them also contain carcinogens, chemicals that are known to cause cancer.
![]()
As a COPD patient, your goal should be to eliminate all hazardous cleaning products from your home. However, it’s especially important to avoid cleaning products that can exacerbate your respiratory symptoms. Products like air fresheners are particularly harmful to COPD patients because aerosol droplets can remain suspended in the air for long periods of time, meaning they can be inhaled. Generally speaking, “scented” cleaning products should be avoided at all costs. While we may enjoy a fresh smell and equate it with a clean home, most of these products contain harmful chemicals.
Before heading out to the store, create a list of ingredients that you should avoid. The ingredients below are commonly used in cleaning products and should be avoided:
- Perchloroethylene (PERC)
- Formaldehyde
- 2-Butoxyethanol
- Ammonia
- Sodium Hydroxide
- Chlorine
Some common cleaning products you should avoid include:
- Bleach
- Spray cleaners
- Fragrance sprays
- Carpet fresheners
- Fabric softeners
- Varnishes
-
Drain cleaners

Another thing to note is that you should be wary of anything labeled “green,” “organic,” or “eco-friendly.” Just because something is “organic” does not necessarily mean that it is healthy or safe. However, you may see products labeled as “safer choice.” These cleaning products are actually regulated by the Environmental Protection Agency (EPA) and they’re aimed at reducing, eliminating, or preventing pollution at its source. In many cases, these cleaning products can be a safer alternative for COPD patients but many of them still contain chemicals.
How to Make Safe Cleaning Products at Home
Believe it or not, homemade cleaning products can be extremely effective and they can also be much safer to use than store-bought items. When you make your own cleaners, you’ll know exactly what’s in them and you won’t have to worry about reading through and researching a long list of ingredients.

According to Healthline, some of the safest and most effective ingredients you can use to make homemade cleaning products include white vinegar, lemon juice, methylated spirits (denatured alcohol, and baking soda. Unlike the harsh chemicals found in store-bought products, COPD patients typically don’t have any reactions when exposed to these ingredients.

If you want to clean your floor or countertops, combine boiling water with either lemon juice, white vinegar, or methylated spirits. This will make a great degreaser and prove much more effective than a wet rag. If you want to clean a mirror, vinegar and water is a great combination. For removing stains, soda water is your best bet.
Keep Your Home Well Ventilated
Ventilation is imperative when it comes to keeping your home clean. Simply put, ventilation refers to the healthy exchange of air between the inside of your home and outdoors. This prevents harmful chemicals, moisture, and other allergens from concentrating in your home and posing a serious health risk. One of the best ways to ventilate your home is to simply crack a window when you’re cleaning.

If you’re worried about allergens making it into your home through the window, you can install a screen. While this won’t block out all allergens, it will prevent some of the larger particles from entering your home. Another thing you can do is change up the air filters on your HVAC system. The air filter or “particle filter” is designed to remove allergens from the air as it’s circulated throughout your home. However, over time, these filters can become very dirty. Not only will this start spiking your utility bills, but it won’t filter airborne pollutants correctly.
Choose the Right Tool for the Job
Aside from choosing the right cleaning products, you also need to choose the right tools for cleaning your home. COPD is a debilitating condition so you may need to find creative ways of doing things that won’t add any unnecessary strain on your lungs and the rest of your body. For example, if you need to clean in a hard-to-reach area, be sure to use a cleaning device with an extendable handle. This way, you won’t have to strain yourself or risk falling just to clean your home.

If you’ve been prescribed long-term supplemental oxygen therapy, another thing that can help is a portable oxygen concentrator. If you already use a stationary oxygen concentrator or oxygen tank for your oxygen needs, a portable oxygen concentrator will provide you with much more freedom to navigate your home with ease. Rather than having to be plugged into a wall outlet, POCs operate off of powerful lithium-ion batteries so you won’t be relegated to one room of the house.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Portable oxygen concentrators like the Caire FreeStyle Comfort and Inogen One G5 are very lightweight and compact, so you can carry them around all day without feeling exhausted or out of breath. The FreeStyle Comfort even has an ergonomic curve design that will prevent the unit from sliding around at your side while you’re cleaning the house. Once you’re ready for a break from cleaning, simply plug your device into the wall and by the time you’re ready to go again, you’ll have a full battery.

If you’re someone who needs more oxygen to keep you going, the Respironics SimplyGo may be the portable oxygen concentrator for you. This is a continuous flow unit meaning it puts out a constant stream of oxygen rather than “boluses” of oxygen like the FreeStyle Comfort and the Inogen G5. While the Respironics SimplyGo is a bit heavier than these two, it will provide you with more options including the ability to use your POC with your CPAP or BiPAP machine while you sleep.
Don’t Forget to Declutter Your Home
While you’re up and about cleaning your home, it’s also a good idea to spend some time decluttering your home. “Decluttering” simply means reorganizing or getting rid of some of your belongings in order to make your home more comfortable and easy to navigate. This is very important if you’re a COPD patient because having to navigate a messy home can be very challenging and dangerous.

We briefly discussed decluttering in our post about COPD and balance issues, but the basic idea is that you want to create a living space that’s accommodating of your lung condition. First and foremost, you should remove any belongings from the floor that could be a tripping hazard such as clothing, cables, and even furniture. Taking the time to move these things out of the way of where you walk in your home can go a long way toward making your home safer and more accommodating for you and your guests.

If you want to go the extra mile, you might want to consider installing a medical alert system in your home. This consists of a receiver that’s plugged into the wall and a small button that can be worn around your neck. If you take a fall or experience a COPD exacerbation in your home, simply press the button and medical personnel will immediately be sent to your home. These are a must-have for any COPD patient, especially if you don’t have friends or caretakers who visit your home regularly.
Get Outside When You Can
According to the EPA, indoor air pollution can be 2 to 5 times greater than outdoor air pollution. The reason for this is because indoor air pollutants are concentrated in a small area whereas outdoor air pollution can dissipate. While you can and should take the time to clean your home, you should be going outside as much as possible to get some fresh air.

AirNow.gov has a great air pollution map that will give you a good idea of how clean the air is in your area. Simply visit their site and type in your ZIP code. You’ll be given a number anywhere between 0 and 500 with 0 being the least polluted and 500 being the most polluted. It’s recommended that COPD patients avoid going outside if the air quality index (AQI) is over 100. However, people with severe COPD may only want to go outside when it’s below 50 AQI.
.jpg)
While the AQI is a good indication of the air quality in your area, it’s not 100% accurate. If you live in a very urban area with a lot of traffic, the air quality may be lower than what the website tells you. As such, it’s important to use your best judgment before going outside. Try going out when traffic has settled down and try to stay away from the roads as much as possible.
The temperature is another important factor to consider before going outside. Extreme conditions of any kind can lead to exacerbation of COPD. Low temperatures can be particularly difficult for COPD patients because inhaling cold air can thicken your mucus making it more difficult to breathe. Hot temperatures can cause you to feel exhausted more quickly and also exacerbate respiratory problems.
![]()
Schedule a Home Inspection
If you want to take the extra step towards making your home as accommodating as possible for your COPD, you should consider scheduling a home inspection. This is when a professional safety inspector walks through your home and performs a variety of tests designed to determine the safety of your home. While you may think of a home inspector as someone who examines the structural integrity of a home, they also play an important role in determining its cleanliness as well.
One important thing your home inspector will do is evaluate your HVAC system. This includes things like your heater, air conditioner, air ducts, and air filters. He/she will check to ensure that there are no leaks and that your system is circulating clean air throughout your home. The inspector will also look for water damage or plumbing leaks throughout the home that could lead to the growth of mold. Several types of mold, like black mold, can be very hazardous to your health. Black mold poisoning is associated with a chronic cough, fatigue, and irritation in the throat and eyes.

Home inspectors won’t fix these issues within your home. Rather, they provide you with a list of potential problems in your home and advise you on what to do or who to call to get the issues resolved. However, hiring a home inspector is still a very important step because you may be exposed to harmful airborne irritants unknowingly. Many people live with health issues for years only to find out they had a mold or HVAC problem that they were unaware of.
Recruit Help With Cleaning
There’s no doubt about it, cleaning can be exhausting. If you feel like you have a lot to clean and not a lot of time to do it, you may want to start outsourcing work to friends, family, or even a caretaker. While physical exercise is a must for any COPD patient, too much exercise or overexertion can lead to a flare-up in your symptoms, most notably chest pain, breathlessness, and fatigue.
.jpg)
There’s no shame in asking for help with cleaning your home, especially when your well-being is at stake. However, if you decide to recruit help from a friend or family member be sure to let them know about your safe cleaning routine. Let them know that you’re concerned about the chemicals in common store-bought cleaning products and show them how to make the homemade cleaning products we discussed earlier in this post.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Conclusion
Maintaining a healthy living environment is one of the most important things you can do as a COPD patient. Poor air quality in your home will not only irritate your skin and eyes, but it can damage your lungs and lead to flare-ups in your respiratory symptoms. COPD patients who do not breathe clean air are more likely to experience exacerbations that can lead to hospitalization.
Unfortunately, simply cleaning more often or more thoroughly is not the solution. You need to be careful about what cleaning products you’re using and how they affect the quality of air within your home. You should also take additional steps like ensuring your home is well-ventilated and that you’re keeping dust and mold in check.
If you found this post useful, don’t forget to bookmark it so you can refer back to it in the future. And if you have any questions or concerns, please don’t hesitate to leave them in the comment section below
.png)
Chronic obstructive pulmonary disease (COPD) is one of the most common lung conditions in the world. It’s known for developing slowly over the course of many years, leading to increased breathlessness, chest pain, coughing, and wheezing. As this incurable disease progresses, flare-ups and exacerbations become more common, so COPD patients need to pay especially close attention to the treatment plan created by their doctor. Since a core aspect of most treatment plans involves supplemental oxygen therapy, it’s also important for COPD patients to find an oxygen device that serves their long-term goals.
Unfortunately, the medical oxygen industry can be very confusing, especially for someone who’s never had to navigate it before. People who are buying oxygen for the first time often fall victim to false advertising, scams, or they simply end up purchasing an oxygen device that doesn’t meet their needs. As such, we strongly encourage oxygen patients to do their research and understand what oxygen devices there are before buying one. Here at LPT Medical, we take pride in providing oxygen patients with the resources they need in order to make educated decisions about their disease.
In this post, we’re going to take a look at seven reasons someone who uses a liquid oxygen tank or someone who is considering purchasing a liquid oxygen tank may want to upgrade to a pulse dose portable oxygen concentrator: the Caire FreeStyle Comfort. This is one of many oxygen concentrators on the market, so be sure to speak with our respiratory specialists if you’d like to learn about other options. You can reach us at 1-800-946-1201 or you can email us at info@lptmedical.com.
What is a Liquid Oxygen Tank?
A liquid oxygen tank (also called a LOX unit) is a medical device that stores oxygen in a liquid form. They are often seen as an upgrade to compressed oxygen tanks because they are lighter, safer, and store more oxygen. What’s more, you can also purchase portable versions of these tanks, usually called “portable oxygen cylinders.” These tanks are light enough to carry on your shoulder as you walk and they provide you with many hours of oxygen.

While liquid oxygen tanks provide many benefits over compressed oxygen tanks, they still cause a lot of inconveniences for oxygen patients. One of the most glaring problems with liquid oxygen tanks is that, in order to store oxygen in a liquid form, it needs to be kept at very low temperatures (typically around -183°C or -297°F). While the tanks themselves are designed to maintain these temperatures, it’s inevitable that the tank will heat up causing the water to evaporate over time. In other words, you won’t be able to store a liquid oxygen tank for a significant amount of time without the oxygen dissipating.
What is the Caire FreeStyle Comfort?
An oxygen concentrator performs the same function as a liquid oxygen tank by providing the user with medical-grade oxygen. The difference between the two, however, is that oxygen concentrators are electronic devices that run off of batteries. Rather than storing oxygen inside the machine, concentrators take ambient air, remove unneeded gases like nitrogen and argon, then puts out medical-grade oxygen through the nasal cannula.

The Caire FreeStyle Comfort is a pulse dose portable oxygen concentrator meaning it carefully monitors your breathing and only puts out oxygen when you need it. In other words, it conserves energy so that you can go more places and do more things on one battery charge. Much like a liquid oxygen cylinder, the Caire FreeStyle Comfort is very lightweight and easy to carry on your shoulder.

Another thing to note about this portable oxygen concentrator is that it’s manufactured by one of the most trusted brands in the medical oxygen industry. Caire Inc. advertises its products under the names SeQual, AirSep, and Caire, and the FreeStyle Comfort is one of their most advanced oxygen machines yet. Thee Caire FreeStyle Comfort is widely considered to be one of the best portable oxygen concentrators ever made, but many people also believe the Inogen One G5 is the best. Without further ado, let’s take a look at some of the reasons you should upgrade your liquid oxygen cylinder.
Safety
Safety is incredibly important. The reason for using supplemental oxygen therapy in the first place is to maintain oxygen levels in the blood and prevent life-threatening conditions like right-sided heart failure; so, it goes without saying that you don’t want your supplemental oxygen device to add any unnecessary health risks. And despite the fact that liquid oxygen tanks are safer than compressed oxygen tanks, they are still more dangerous to use than a portable oxygen concentrator.

Liquid oxygen tanks are stored at a pressure of around 350 PSIG (pressure per square inch, gauge). While this is significantly less than the 2,000 psi that regular oxygen tanks are stored at, it can still be a safety concern. Liquid oxygen tanks have complex safety mechanisms in place that prevent pressure from building too high, but in reality, there is simply more that can go wrong with these units.
The great thing about portable oxygen concentrators like the Caire FreeStyle Comfort is that you never have to deal with a high-pressure device in the first place. Since oxygen concentrators take ambient air and immediately put it out of the nasal cannula, you never have to feel insecure about using supplemental oxygen. What’s more, if you happen to drop your nasal cannula the device will stop putting out oxygen until a breath is detected.

Convenience
Another point to note about traditional oxygen tanks and liquid oxygen tanks is that they’re extremely inconvenient to use. Because these tanks can’t be simply recharged like an oxygen concentrator, you have to have some way of refilling them. Whether that means having new tanks delivered by an oxygen company or having to refill them with a liquid oxygen reservoir, you’ll need to find something that works for you.

If you decide to have your tanks delivered or drive to an oxygen company to refill them, this could be a huge time sink for you and you may have trouble working your schedule around them. On the other hand, if you decide to purchase your own oxygen reservoir, you’ll only be able to refill your liquid oxygen tank in your home. On top of this, reservoirs tend to be very bulky, heavy, and difficult to move.
Since the Caire FreeStyle Comfort is charged through either a wall outlet or a car outlet, you’ll be able to take your portable oxygen concentrator just about anywhere with you. You’ll be able to charge your machine at your home, in hotels, airports, and in any vehicle that has a power outlet. And the best part of all is that you can use the machine while it’s charging, as long as it’s on a low flow setting.

Long-Distance Travel
In the past, beginning supplemental oxygen therapy meant giving up your freedom to travel long distances. The Federal Aviation Administration (FAA) oversees safety regulations for commercial flights in the United States, and both traditional and liquid oxygen tanks are banned. What this means is that if you’re using one of these oxygen devices, you’ll be relegated to other slower forms of transportation.
However, the Caire FreeStyle Comfort — like most portable oxygen concentrators — is approved by the FAA for in-flight use. All you need to do is call your airline 48 hours ahead of your flight and be prepared to bring at least 1.5 times the duration of your flight in battery life. Once that’s out of the way, you’ll be able to fly anywhere in the country without question. If you’re going out of the country, be sure to check in with the regulations in your destination country before leaving.

Reliability
It’s easy to get caught up in talking about all of the other factors of a portable oxygen machine and forget about one of the most important factors: reliability. Having reliable supplemental oxygen means being able to be out and about at the store, visiting a friend, or on vacation, without ever having to worry about receiving the oxygen you need to maintain your blood oxygen levels. You’ll be able to spend more time focusing on enjoying your day and accomplish your goals rather than worrying about whether or not your oxygen needs are being met.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Like we mentioned earlier, liquid oxygen needs to be kept at very low temperatures in order to prevent it from turning into a gas. While liquid oxygen tanks are designed like a thermos to keep the internal temperature low, it’s inevitable that it will heat up over time, especially if you’re out in the hot sun. Over time, you will begin to lose oxygen from your liquid oxygen device even if you aren’t using it.

Portable oxygen concentrators like the Caire FreeStyle Comfort, on the other hand, are known for their reliability. In fact, back in August, we featured the FreeStyle Comfort as “the most reliable portable oxygen concentrator” ever produced. This is because it has the lowest failure rate of any POC on the market, meaning that, out of the box, it is less likely to have a defect than any other device like the Inogen One G5 or Respironics SimplyGo.
Another wonderful thing about the Caire FreeStyle Comfort — and portable oxygen concentrators in general — is that the vast majority of issues they have can be fixed on the fly. If you experience a glitch or the device isn’t working properly, a hard reset will typically fix the issue right away. We discuss how to perform a hard reset in this post, but if you have any problems either consult the user manual or reach out to our portable oxygen concentrator specialists at 1-(800) 946-1201.

Liquid oxygen tanks are very different from this. Since they aren’t electronic devices like POCs, you can’t simply restart them if they aren’t working properly. Liquid oxygen tanks are a very complex piece of equipment, and if you tamper with them you risk injuring yourself or further damaging the unit. In order to fix your problem, you’ll need to send it to an oxygen specialist and it could take days or weeks to get it back.
Cost
Liquid oxygen is considered to be the most expensive form of oxygen therapy. Some of the more popular portable liquid oxygen units like the HELiOS Plus will run you over a thousand dollars. And remember, you’ll also need to either have a home fill reservoir to fill your own portable units or you’ll have to go to an oxygen supplier regularly. These costs can add up really quickly and there’s a lot more that could go wrong.
On the other hand, the Caire FreeStyle Comfort requires no additional components aside from the battery. Since these batteries are rechargeable, you won’t have to keep investing in your oxygen therapy over time. Simply plug your device into any wall or car outlet and you can charge the battery all the way up.
Ease-of-Use
Most people are very surprised to find just how easy it is to use the Caire FreeStyle Comfort. All you need to know how to do to get started is how to turn on the device, charge it, and adjust the flow settings. Any additional information about notifications, alarms, or warnings can be found in the user manual. However, with a liquid oxygen tank, not only will you need to know how to operate the portable unit, but you’ll also need to know how to refill it using the reservoir. This can be very time consuming and most people admit that it’s a pretty convoluted process.

Additional Features
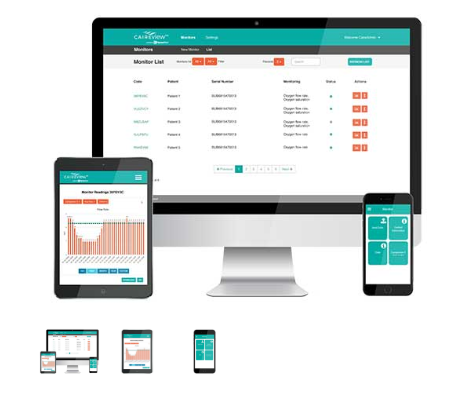
The final reason to upgrade from liquid oxygen to the Caire FreeStyle Comfort is because of all the additional features you’ll get with the latter. The FreeStyle Comfort has something called CAIREview which is a free oxygen tracking application made by SynsorMed. By connecting your phone or computer to your POC, you’ll be able to see up-to-date information about your oxygen usage. Liquid oxygen tanks don’t offer any features like this.
Conclusion
Liquid oxygen tanks are a huge upgrade from traditional oxygen tanks. They’re lighter, smaller, safer, and hold a lot more oxygen. However, they offer few advantages over portable oxygen concentrators like the Caire FreeStyle Comfort. These oxygen machines enable you to have access to an infinite supply of oxygen no matter where you are in the world and they’re far more convenient and reliable than the alternative.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Despite what you read here, we here at LPT Medical encourage oxygen patients to take their time when choosing a supplemental oxygen device. Also, it’s important to be open with your doctor and understand exactly what your oxygen requirements are. If you’d like to learn more about portable oxygen concentrators, don’t hesitate to reach out to our respiratory specialists. You can reach us at 1-800-946-1201 or you can email us at info@lptmedical.com.
Oxygen therapy, also known as supplemental oxygen therapy, is the administration of medical-grade oxygen in order to treat a variety of medical conditions. While oxygen has been used as early as the 1800s, it wasn’t until the late 1900s that doctors were able to nail down the exact conditions that oxygen could treat, and equally as important, when oxygen therapy should be avoided.
Like we discussed in our last post, there are four commonly used types of oxygen delivery: hyperbaric chambers, oxygen tanks, liquid oxygen tanks, and oxygen concentrators. Hyperbaric chambers are a form of oxygen therapy that administers pressurized oxygen in order to treat conditions like decompression sickness and promote healthy blood flow. On the other hand, the other three oxygen delivery methods are usually used to treat chronic lung conditions like COPD, cystic fibrosis, and more.
In this post, we’re primarily going to be discussing portable oxygen concentrators and their benefits when it comes to long-term oxygen therapy. If you have any questions or concerns about what you read here, be sure to leave a comment or fill out the form at the side of the page so that one of our respiratory specialists can reach out to you.
What is Long-Term Oxygen Therapy?
Long-term oxygen therapy (LTOT) is the continuous use of oxygen therapy for patients with low blood oxygen levels (hypoxemia). Patients with early-stage lung disease may be required to use oxygen several hours a day, whereas people with more severe lung disease might need to be connected to their oxygen machine 24/7. According to the American Thoracic Society, the following conditions may indicate the need for LTOT in patients who suffer from chronic lung disease:
- A partial pressure of oxygen less than 55 mmHg (7.3kPa)
- An oxygen saturation of 88% or less
- Signs of tissue hypoxia (lack of oxygen in tissues)
- Pulmonary hypertension (high blood pressure in the lungs)
-
Pulmonary edema (excess fluid in the lungs)
Ultimately, oxygen therapy is one of the most effective ways to return blood oxygen levels back to normal in COPD patients. By doing so, they will maintain a much more stable pulmonary state avoiding common symptoms such as chest pain, breathlessness, and coughing fits. LTOT has also been shown to increase exercise capacity, reduce hospitalizations, and reduce exacerbation rate and severity.
When is LTOT Not Advised?
Contrary to popular belief, not all COPD patients require long-term supplemental oxygen. In fact, certain respiratory patients may experience something called oxygen-induced hypercapnia where a patient’s breathing is negatively affected by the use of supplemental oxygen.

Carbon Dioxide (CO2) is the byproduct of metabolism. Although it’s expelled from the body as a waste product, it does have one important function in the body: respiratory drive. Essentially, when there are higher levels of CO2 in your blood, it releases chemoreceptors to the brain which increases the rate of respiration. Since COPD patients have chronically high levels of CO2 in the blood, the body may become desensitized to these signals. In other words, supplemental oxygen may suppress respiratory drive and cause a COPD patient to retain more CO2.
While long-term oxygen therapy is effective for most COPD patients, it’s imperative that patients see their pulmonologist regularly. Supplemental oxygen is rarely a “black and white” situation, so it’s important to closely monitor things like CO2 levels, partial pressure of oxygen (PaO2), oxygen saturation, and COPD symptoms in order for oxygen to be prescribed effectively and safely. If problems arise, he/she may advise a decrease in oxygen flow rate or remove the patient entirely from supplemental oxygen.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Why Are Portable Oxygen Concentrators Ideal for LTOT?
Now that you know the important role LTOT plays in treating COPD symptoms, you may be wondering why portable oxygen concentrators provide the greatest benefits for someone looking for an oxygen therapy device. While there are several other options like compressed oxygen, liquid oxygen, and stationary oxygen concentrators, portable oxygen concentrators have stood the test of time as the best option for long-term supplemental oxygen therapy.

Oxygen concentrators largely became popular around the 1970s when patients were looking for better alternatives to big, bulky oxygen tanks which needed to be refilled several times a day. Concentrators were revolutionary at this time because they prevented the need for oxygen patients to get up to go refill their oxygen. Simply by plugging the concentrator into the wall, they’d have an infinite supply of oxygen.

Portable oxygen concentrators didn’t become popular until the early 2000s when lithium-ion battery technology had advanced enough to make them practical. To this day, portable oxygen concentrators remain one of the most popular options for LTOT, especially for patients who are more active or want to limit the amount of work they want to put into their daily COPD treatment routine.
They Can Run 24 Hours a Day Without Interruption
Despite what your COPD treatment regimen says, you’re never truly going to be on oxygen 24/7 while using compressed oxygen or liquid oxygen. Running continuously at 2 liters per minute, an E cylinder will only last about 5 hours. D cylinders which are even smaller only last about 3 hours at the same LPM. What this means is that you will need to have a backup tank on hand or deal with a gap in your oxygen treatment while your tank fills up. Not only is there a chance you could experience an exacerbation during this time, but it will waste a lot of your time.

Fortunately, when you own a portable oxygen concentrator, you won’t have to deal with any of these issues. Every component of modern POCs is designed to be run 24/7 including the compressor, battery, and processor. As long as you take care to follow the instructions in your user manual, you will ensure that your device doesn’t overheat or malfunction. The most important maintenance procedure for most POCs is to change the particle filter. This component will prevent airborne contaminants like dust and dirt from getting inside your device and potentially damaging it. This also helps to ensure that the air you breathe through the nasal cannula is clean and doesn’t trigger a COPD exacerbation.

Another reason you can run your POC without interruption is because they run entirely off batteries so you’ll never have to refill it or keep an extra one on hand. Once your battery starts getting low, simply plug your oxygen machine into the wall and you can continue using it while the battery charges. If you want to stay out of the house for longer, you can simply carry an extra battery and swap it out with the other one once it starts to get low.
.png)
Lastly, several newer portable oxygen concentrators like the Inogen One G5 come equipped with something called an “Intelligent Delivery System.” In the G5, proprietary conserver technology ensures oxygen is always delivered within 400 milliseconds of inspiration. This is known as the critical point because it’s the time-frame when you experience the most clinical benefit from inspired oxygen. When you’re sleeping, breathing rates typically slow down significantly. The G5 responds to this by increasing the bolus size and ensuring that you always receive oxygen no matter your rate of breath. What’s more, the G5 can even detect shallow mouth breaths, adjusting oxygen delivery accordingly.
They Afford More Freedom and Independence for Patients
Freedom is a quality that defines everyone. Without freedom and independence, we wouldn’t be able to go where we please, pursue our dreams, or spend time with people that we choose. Unfortunately, many older adults and elderly people suffer debilitating conditions that prevent them from getting out and enjoying their lives — COPD is just one example of these.

Many COPD patients report feeling chest pain or breathlessness just from simply waking up in the morning and getting out of bed. If you’re faced with all of this along with chronic fatigue and the thought of lugging around a heavy oxygen tank, it’s no wonder many COPD patients don’t get out of the house! The good news is that there is a better solution for long-term oxygen therapy that won’t add any burden to your already challenging daily routine.
Portable oxygen concentrators, especially pulse flow ones, are extremely light when compared to other oxygen therapy devices. An average continuous flow portable oxygen concentrator weighs around 10 to 15 pounds while the average pulse flow portable oxygen concentrator weighs around 6 pounds. Pulse flow units are so much lighter because of the technology that’s built into them allowing them to administer oxygen more efficiently. POCs are also more practical in terms of their shape. Whereas oxygen tanks are oblong, POCs are usually box-shaped or rectangular making them much easier to store in small places.

Most continuous flow POCs should be carried with a rolling cart, however, pulse flow POCs are light enough to carry over your shoulder. Amazingly, the lightest portable oxygen concentrator, the AirSep Focus weighs in at just 1.75 pounds which is light enough to clip onto your belt! Other pulse flow POCs like the Inogen One G4 are small enough to fit in a purse or small handbag. However, it’s recommended that you use the official carrying bag that comes with the device to avoid damaging it.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
They Allow Precise Control Over Oxygen Output
As aforementioned, one of the most important things about long-term oxygen therapy is the ability to have precise control over your oxygen delivery. If you aren’t receiving enough oxygen, you may be at a high risk of experiencing a COPD exacerbation or other symptoms like breathlessness, chest pain, or coughing fits. If you’re receiving too much oxygen, you may experience oxygen toxicity or oxygen-induced hypercapnia.
One of the defining features of portable oxygen concentrators is that they allow for precise control over your oxygen delivery. Each POC has what’s called flow settings. Each one has a different number of flow settings and a different oxygen output for each one. So, for example, the Inogen One G5 has 6 flow settings and a total oxygen output of 1,260 ml/min of oxygen. This means that for each flow setting you go up, you’ll be increasing your oxygen by 210 ml/min. You can adjust your flow setting on the fly by pressing the arrow buttons on the device’s control panel.

One of the greatest benefits of being able to change your oxygen flow so easily is that you can ensure that you always get the oxygen you need no matter what you’re doing. Some patients like to use their oxygen concentrator while they’re exercising meaning they’ll likely need to increase their flow rate to accommodate for this. On the other hand, you may be sitting down for a long period of time and want to reduce your flow rate in order to save battery life — you can do this too!
They’re More Affordable Than the Alternatives
Oxygen patients are often surprised when they hear someone say that portable oxygen concentrators are the most affordable method of oxygen delivery. One of the reasons for this is because insurance companies often label them as expensive “luxury” items that are not necessary for a COPD patient’s happiness and well-being. While oxygen concentrators do have a higher upfront cost than most other forms of oxygen therapy, they are much more cost-effective when it comes to long-term oxygen therapy.

Oxygen tanks have very low upfront costs and this is what makes them so appealing to people. A home or portable oxygen cylinder can be bought for a couple hundred dollars. But the problem is that the longer you use it, the more you have to spend on it. If you want to refill your own tank at home, you’re going to need to purchase a homefill oxygen refill system. These machines alone cost as much as a portable oxygen concentrator. If you decide to go the other route and have a professional refill your tanks, you can expect to pay upwards of $10 for each fill. This can add up very quickly if you use oxygen every day.
Alternatively, you can purchase a portable oxygen concentrator. Although they run several thousand dollars upfront, there are little-to-no maintenance costs. Portable oxygen concentrators are designed to be run 24/7, all you’ll need to do is clean and replace the particle filters regularly to ensure that it runs smoothly. Additionally, most portable oxygen concentrators come with a 3-year warranty at the very least. So, if anything goes wrong with your device within that time frame, you can get it repaired at no cost to you.
They Promote a Productive Lifestyle
Productivity is not something that should be restricted by your age or health. Unfortunately, many people with COPD and other debilitating diseases become less motivated to lead a productive lifestyle when they’re dependent on friends and loved ones for support. Oxygen tanks add to this because they keep oxygen patients homebound and in some cases, they even prevent them from moving around the house freely.

On the other hand, portable oxygen concentrators offer more freedom than any other type of oxygen therapy device. With the average pulse flow POC weighing under 6 pounds, you won’t have to dread the thought of walking up a flight of stairs or going into a crowded public area. Ultimately, it will allow you to focus on what you’re trying to accomplish rather than on whether or not your oxygen needs are being met.

Another reason many people don’t like using oxygen tanks is that they can make you feel self-conscious. It’s easy to feel like you’re a burden on other people when you’re wheeling around a bulky and dangerous oxygen tank behind you into public areas. Portable oxygen concentrators don’t have this effect because they’re small enough to fit under your shoulder. They’re also pretty inconspicuous so most people won’t even notice it. And if they do, they likely won’t ask any questions or give you any unwanted attention.
They’re Much Safer to Use
If you remember the last time you went out and bought a car, what was the first feature you looked at? Chances are, it wasn’t the gas mileage, top speed, or color — it was safety. If you’re going to be investing your money in something, it would be unwise to check whether it’s going to be safe or not. And just like with a car, your portable oxygen concentrator is a long-term investment, so there’s a lot at stake.
One of the main reasons oxygen tanks are so dangerous is because they contain many liters of compressed oxygen inside them. Oxygen is not flammable or combustible but it is an oxidizer. What this means is that when something is exposed to oxygen it can catch fire more easily. Additionally, oxygen is stored at very high pressures meaning there’s always the risk that it could explode. Liquid oxygen is stored at much lower pressures, so they’re safer in that regard, but you’ll still be carrying around a canister of medical-grade oxygen.

The main reason that portable oxygen concentrators are so much safer is that they contain no compressed oxygen. Ambient air is drawn into the concentrator and gases like nitrogen, argon, and carbon dioxide are removed. A pulse flow POC will only put out oxygen when you inhale, so if you happen to put down your nasal cannula, oxygen won’t continue to come out of the hose. Instead, it will stop producing oxygen and wait for you to start inhaling again. It’s also much safer that oxygen comes out in boluses rather than continuously.
You’ll be happy to know that the people around you will also feel more secure and safe while they’re around you. Many people are misinformed about the dangers of oxygen, believing that it can catch fire rather than acting as an oxidizer. While you can take the time to explain exactly how it works, it’s best to just use a device like a portable oxygen concentrator that won’t get people on edge.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Conclusion
Long-term oxygen therapy is a core component of most COPD treatment plans. While some patients won’t need any supplemental oxygen, most will need to use it for 18 to 24 hours a day. Portable oxygen concentrators tend to be the best option for people who need LTOT because they’re safer, more cost-effective, lighter, smaller, and easier to use than most other medical oxygen devices. However, before making any decisions about your oxygen usage, be sure to consult your pulmonologist who will be able to make recommendations based on your health condition.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













