.png)
Have you ever left a conversation with your doctor confused about their instructions or explanations? It may have been the complicated terminology they were using, or long instructions about a prescription you need to be taking, or a lack of explanations for your treatment. Studies show that there is a gap between patient–doctor communication leading to decreased quality of care.
Education is a vital element of the patient care process and can contribute to successful and effective management of COPD.
Educating yourself about COPD is your job as the patient. This comes down to understanding your COPD symptoms, the testing, and management and treatment options involved. Then, you will be able to effectively ask your doctor questions and confidently understand their answers.
This is a clear and cohesive guide that you can study before your next visit with your doctor to ensure that you understand the information you doctor presents to you, and you can ultimately advocate for yourself!
Effective patient education will enhance your experience dealing with the uncertainties and confusions of having a chronic illness like COPD.
Patient education also lead to:
- Satisfaction with your overall health care
- Understanding COPD and your treatment
- Comfort and skill in managing and monitoring your COPD by yourself
Important aspects of COPD you need to know: Medication, supplements, oxygen therapy, and pulmonary rehabilitation
If you or someone you know has recently been diagnosed with COPD the amount of information about the disease may feel daunting. But remember; information is power, and knowing what your options are will open doors to a personalized treatment plan that is crucial for living with COPD.
The 3 basics of COPD:
- COPD is a chronic illness. This means that you live with it every day.
- COPD is referred to as chronic bronchitis or emphysema.
- You can do a lot of different things to treat and help manage the disease. There are medications you can take, you might try supplements if you have a deficiency, you can start oxygen therapy, and pulmonary rehabilitation, and get involved with social support groups
Medications and Supplements:
Your medications should be geared towards keeping your airways open as much as possible by helping clear mucus from your respiratory tract, and decrease inflammation. No single strategy or medicine is "best" for everyone, so do not settle for a medication that gives you adverse side-effects.
Personalization is key to addressing your COPD and finding the best plan for symptom control. Always be search for the right medication and supplements to to ensure:
- Better breathing
- Participation in the activities you enjoy
- Fewer flare-ups
Bronchodilators
Bronchodilators relax the muscles around your airways, opening your airways, and helping you breathe easier. Most of the time, you take bronchodilators through an inhaler or it can be converted into a fine spray as a nebulizer, so you breathe the medicine straight into your lungs.
Inhalers work in different ways, so make sure to ask your doctor shows you how your specific inhaler works. Be sure that you are getting a full dose of medicine with each breath.

Three main categories of COPD inhalers:
- Rescue inhalers use short-acting bronchodilators, which work quickly so that you get relief from symptoms fast, and these wear off in a few hours
- Maintenance inhalers use medications known as long-acting bronchodilators, they provide relief for many hours, but the effect may act slower.
- Steroid inhalers contain corticosteroid medications, which target the body's immune system to suppress inflammation in the lungs. These are mainly prescribed to treat COPD exacerbations.

Anti-Inflammatory medications
Anti-inflammatory medications decrease swelling and mucus production within your airways making it easier to breathe. These medicines are known as corticosteroids or steroids. They are usually inhaled with an inhaler.
You could also take corticosteroids as a pill but these will usually only be prescribed for short periods of time in special circumstances when your symptoms are getting more severe.
Steroids have serious side effects, such as weight gain, diabetes, osteoporosis, cataracts and increased risk of infection, so you and your doctor should monitor your use carefully.
Antibiotics
If you have COPD, you are more susceptible than others to catching illnesses from bacteria that infects your respiratory system. If your illness is caused by bacterial or viral infections your doctor may prescribe you an antibiotic for you to keep on hand for if you get an infection.
Talk to your doctor about the prescription of your antibiotic. It is imperative that you finish the perception by taking all of the antibiotics for the duration of time it is prescribed, even if you start to feel better and are not experiencing symptoms. If you do not finish your perspiration, the infection and symptoms can come back in full-swing before it's ever really gone.
Vaccinations
If you have COPD, you are especially vulnerable to viral and bacterial pulmonary infections. Infections are major causes of exacerbations, hospitalization, disease progression, and mortality in COPD patients. Effective vaccines reduced the risk of contracting respiratory infections and reducing flare ups COPD patients.
Supplements
Using herbal and nutritional supplements for COPD can also help with managing your symptoms. Before taking any supplements, you should discuss their use with your doctor because it can interfere with some drugs and cause side effects.
All of these vitamins and nutrients can be found in the foods and drinks you consume, but if just eating more nutrient rich food still leaves you with a vitamin deficiency, taking supplements may be a great option for you to get the nutrients your body needs.
Here is a table of vitamins that have been shown to improve lung health:
| Vitamins and minerals: | Commonly found in: | Common benefits: |
| Vitamin D | Fatty fish, like tuna, mackerel, and salmon, some dairy products, orange juice, soy milk, and cereals, beef liver, cheese, egg yolks | Help lungs function better, and protects against moderate or severe flare-ups |
| Vitamin C and E | Salmon, herring and sardines, cod liver oil, canned tuna, egg yolks, mushrooms, cow’s milk, soy milk, orange juice, | Studies show that taking vitamin C and E supplements for 12 weeks may improve the resistance of DNA in whole blood white blood cells against oxygen related challenges. Meaning there are beneficial effects vitamin C and E have on slowing the decline of lung function in patients with COPD. |
| Vitamin C | Broccoli, brussels sprouts, cauliflower, green and red peppers, spinach, cabbage, turnip greens, and other leafy greens, sweet and white potatoes., tomatoes and tomato juice winter squash. | Studies show that vitamin C can relieve skeletal muscle fatigue that impacts COPD patients. They also provide further evidence that oxidative stress plays a critical role in the skeletal muscle dysfunction that many COPD patients experience. They suggest that antioxidants could eventually be used as a treatment for these problems |
| Vitamin A | Carrots, cantaloupe, spinach, sweet potato, papaya, margo,dried apricot, grapefruit, salmon | Vitamin A can help COPD patients because the body uses vitamin A to build and repair lung tissue. But the relationship with vitamin A and lung health starts before diagnosis, and people with healthy amounts of vitamin A intake had a 52% lower risk of COPD. |
| Magnesium | Black-eyed peas (cooked). tempeh (cooked), soy nuts, cooked beans (black, lima, navy, pinto, chickpeas), tofu, almonds, cashews, flaxseed. | Supports healthy lung function, but some COPD medications may interfere with the body’s ability to absorb it. |
| Calcium | Milk, cheese and other dairy foods, green leafy vegetables – such as broccoli, cabbage and okra, soya beans, tofu, soya drinks with added calcium, nuts, bread | Can help the lungs function. Come COPD medications may cause people to lose calcium. This makes it even more important for people with COPD to consider increasing calcium-rich foods in their diet, or taking a calcium supplement. |
| Omega-3 fatty acids | Fish and other seafood (especially cold-water fatty fish, such as salmon, mackerel, tuna, herring, and sardines), nuts and seeds, plant oils (such as flaxseed oil, soybean oil, and canola oil) | Increasing the intake of omega-3 fatty acids may reduce inflammation for people with COPD. |
| Dietary fiber | Raspberries, pears, apples with skin, raw carrots and cauliflower, boiled sweet corn and broccoli, bake potato with skin | Eating more dietary fiber may lead to a lower risk of COPD. |
| Curcumin | Turmeric |
A natural anti-inflammatory. Some research suggests that it may help treat the inflammation of the airways that characterizes COPD. |
| Ginseng | Ginseng root can be consumed in many ways: eaten raw or lightly steamed to soften it. It can also be stewed in water to make a tea | Helps to build lung strength. |
Oxygen therapy facts for COPD patients
Oxygen therapy is a great option for you if you have moderate to severe COPD and it is something that your doctor will need to prescribe to you. Oxygen therapy can improve your quality of life in a number of ways and it is one of the few treatments that can extend lung health as COPD progresses.
Research shows that even though oxygen is the foundation of treatment for severe COPD patients, many people may not be using it as often as recommended because it can restrict your ability to do certain activities.

You should have a conversation with your doctor if you've been reluctant to use oxygen for any reason. And you should know that there are many streamlined portable oxygen designs available that allow you to get out of the house and be active with far less shortness of breath and risk.
You have a lot of different options when it comes to choosing an oxygen concentrator, and like your treatment for COPD your oxygen concentrator should be personalized to your needs, and meet your requirements.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Some oxygen concentrators are lightweight, others have longer battery life, others have stronger pulse/continuous flow rates, and there are a few concentrators that embody a variety of these aspects in one
So choosing an oxygen concentrator is something that you should discussed in great detail with your doctor. This way when you get in contact with one of our specialists, they are able to accommodate all of your medical demands and physical goals with the best unit for you.

You and your doctor should discuss what type of oxygen concentrator you will need to full-fill your oxygen demands:
- Pulse Flow Oxygen Concentrators deliver oxygen in puffs of air called “boluses.” A bolus of oxygen is only administered when the patient is inhaling. Pulse flow units tended to be much lighter, allowing you to carry them on your shoulder or in a bag
-
Continuous Flow Concentrators produces a constant stream of oxygen despite the patient’s breathing rate. continuous flow units are heavier but offer more options and often much higher oxygen output.

After you determine what type of flow will full-fill you oxygen needs bests, you can then make a list of priorities base on what you should look for in an oxygen concentrators. You can access this guide by clicking here.
Pulmonary therapy and rehabilitation
Pulmonary rehabilitation can be an essential tool throughout your lifetime management of COPD. It requires the coordinated action of a multiple healthcare professional in order to deliver you a rehabilitation program that best fits your needs.
The most important components of pulmonary rehabilitation are exercise and self-management education. Studies have been shown that these are the most beneficial aspects for improving health-related quality of life.
By joining a pulmonary rehabilitation program, you are signing up for more than just physical therapy. The classes will often take place in a group setting, giving you the opportunity to meet others with COPD, you will develop physical strength while both giving and receiving emotional and mental support from and to others.

Social support groups
While this may not be a topic that comes up with your doctor, it is something you should consider if you are living with COPD. In the midst of a global pandemic its is ill-advised to spend time regular socializing with others, or joining group pulmonary rehab classes, however you are still not alone.
By joining Facebook groups or online forums, you are immediately welcomed into a community of people who are going through similar challenges and confusions as you. There may be an option to take a pulmonary rehabilitation classes online, and maintain connections with others through live videos and streaming.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
-1.png)
Oxygen is essential for maintaining human life. Each time you inhale, your lungs begin a chemical process called cellular respiration where oxygen is removed from the air and is used to convert nutrients into energy that our bodies can use. Without oxygen in the atmosphere, our bodies would have no way to process and digest the food we eat.
However, what many people don’t realize is that oxygen is not always beneficial to the body. Earth’s atmosphere is made up of a variety of gases including nitrogen, argon, and carbon dioxide. Only about 21 percent of the atmosphere is oxygen, so it’s not just the presence of oxygen that makes human life possible, but the fact that there’s a perfect balance of oxygen to keep us healthy.
When the partial pressure of O2 that you inhale is above 0.45 ATA (atmospheres absolute) you’ll start to experience symptoms of oxygen toxicity. Extended exposure to this level of oxygen can lead to pulmonary oxygen toxicity which is characterized by chest pain, shortness of breath, and a chronic cough. Short-term exposure to even higher partial pressures of oxygen can lead to oxygen toxicity of the brain which causes lightheadedness, nausea, and confusion.
In short, your body is designed to process a certain amount of oxygen at a specific partial pressure. When these needs aren’t met, you may begin to experience adverse side effects. These side-effects can be treated with oxygen therapy. In this post, we’ll take a look at 4 different types of oxygen therapy in use today and how they work.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Hyperbaric Oxygen Therapy
The term “hyperbaric” is used to describe a gas at a higher partial pressure than it’s normally found at. Therefore, “hyperbaric oxygen therapy” is the use of higher partial pressure of oxygen in order to treat a variety of conditions. One of the most common conditions treated by hyperbaric oxygen therapy is decompression sickness, commonly experienced by scuba divers and other people who breathe with the help of an oxygen tank.

The ultimate goal of hyperbaric oxygen therapy is to get more oxygen in the blood. By inhaling pure oxygen at pressures 1.5 to 3 times higher than normal, it can promote healing in areas of the body that are deprived of oxygen. As such, it can be a useful therapy for treating wounds and infections that are not healing normally. Risks of hyperbaric oxygen therapy include oxygen toxicity, ear trauma, and eye damage.
How Does the Procedure Work?
There are two common types of hyperbaric oxygen therapy (HBOT): monoplace chambers and multiplace chambers. Monoplace chambers resemble MRI machines and they’re able to hold one person. Once the patient enters the chamber, the doors are sealed and it’s slowly pressurized with 100 percent oxygen. The patient is typically required to lie down in order to use a monoplace hyperbaric chamber.
Multiplace chambers perform the same function as monoplace chambers but they are able to treat multiple patients at one time. Once the patients enter the room, they wear a mask that delivers the oxygen and the room is then pressurized. One of the key benefits of this type of hyperbaric oxygen therapy is that the patients have more space and the room is often climate-controlled which could be helpful to people who get claustrophobic easily.

The important thing to remember about this procedure is that it’s carefully controlled by medical professionals. It’s not something that can be done on a whim because your doctor will first need to carefully consider your health and determine whether or not you will benefit from it. If you’re exposed to highly pressurized oxygen for an extended period of time, you could pose a serious risk to your health.
Key Benefits of HBOT
Wound healing
Chronic wounds are wounds that take a long time to heal. Oftentimes, the reason for this slow healing is due to poor circulation or hypoxia (lack of oxygen in the tissue). During HBOT treatment, the supply of oxygen to these tissues will increase which will promote a faster and smoother healing process. Diabetes patients commonly use HBOT because they often suffer from neuropathy (nerve damage) which slows or prevents wound healing.
Skin Cell and Collagen Development
Hyperbaric oxygen therapy has many different anti-aging effects. Collagen is a component of your skin that’s largely responsible for the healing and recovery of wounds, but it also affects the condition of your skin. Skin with a lot of collagen will look more youthful, elastic, and won’t become damaged or scar as easily. Oxygen therapy can help with the production and management of collagen in the body.
Strengthening the Immune System
Innate and adaptive immunity are two of the most important functions of your body. When you ingest any type of foreign bacteria your body is at constant war to protect you from these harmful substances. HBOT is known for being able to disable the toxins of certain bacteria, effectively making them less of a threat to the immune system and the body as a whole. What’s more, oxygen therapy helps white blood cells find and destroy foreign invaders. In some cases, neutrophils even use oxygen radicals to kill invading pathogens.

Preventing Reperfusion Injury
Reperfusion injury is a phenomenon that occurs when oxygen-rich blood returns to a tissue that was previously deprived of oxygen. Reperfusion can result in damage to the tissue, inflammation, and even cause blood vessels to clamp, reducing blood flow to the area. HBOT works to generate scavengers that destroy oxygen radicals which are responsible for tissue damage.
Curing Decompression Sickness
Decompression sickness is a condition commonly contracted by divers who return to the surface too quickly. Due to the rapid change of pressure, bubbles of gas can form in the blood causing symptoms such as dizziness, rashing, fatigue, and chest pain. While decompression sickness is uncommon, it can be serious or even fatal if it isn’t treated swiftly. HBOT is the only effective treatment for decompression sickness because it reduces the size of the gas bubbles, fills the tissues with oxygen, and reduces swelling.

Disadvantages of HBOT
The only disadvantage of HBOT is overexposure. Patients should not be in a hyperbaric chamber for more than 2 hours at a time and they should not be exposed to pressure that is greater than 3 times that of the atmosphere. People with certain lung conditions, a cold or fever, or those who have recently had ear surgery should not consider HBOT.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Compressed Oxygen Gas
Compressed oxygen tanks are commonly used in both hospitals and in homes. Despite being thrown in with hyperbaric oxygen therapy, oxygen tanks are used in very different situations. Whereas HBOT is used to repair tissue damage and cure decompression sickness, oxygen tanks are commonly used to treat lung conditions such as chronic obstructive pulmonary disease (COPD), cystic fibrosis, pneumonia, and more.
-min.png)
Another significant difference between oxygen tanks and HBOT is that oxygen there is no compression aspect. While oxygen is compressed inside the tank, you won’t need to be in a pressurized room or use a special pressurized facemask. Oxygen therapy is commonly administered through the nose via a nasal cannula but face masks can be used as well depending on the situation.
How Do Oxygen Tanks Work?
Oxygen tanks — typically made of aluminum — are filled with medical-grade oxygen. The process that oxygen manufacturers use to fill these tanks maximizes their oxygen concentrator and limits any impurities that could affect the patient’s health. The pressure inside these aluminum tanks reaches about 2,200 pounds per square inch (PSI). To put this into perspective, the average car tire has a PSI of about 32 to 35, so oxygen tanks are considerably more than this. As you can imagine, this makes them pretty dangerous to keep around unless you avoid dropping them or bumping into them.
.jpg)
Compressed oxygen comes in two forms: home oxygen tanks and portable oxygen cylinders. Since oxygen can only be compressed so much, the size of an oxygen tank directly correlates to the amount of oxygen it can hold. Home oxygen tanks are large and bulky but they can hold quite a bit of oxygen. Portable oxygen cylinders like the “E” cylinder, however, weigh around 8 pounds and they can carry up to 6 hours worth of oxygen.
Key Benefits of Compressed Oxygen
Reduced COPD Symptoms
COPD is characterized by symptoms such as breathlessness, chronic fatigue, chest pain, coughing, and wheezing. All of which are very difficult to live with, especially in later stages of the disease. Using compressed oxygen for the amount of time prescribed by your doctor will ensure that your oxygen levels remain stable and symptoms are kept at a minimum.

Reduced Hospital Admissions
High hospitalization rates are a major problem for COPD patients. No matter where you are or what you’re doing, there’s always a chance that you could experience a COPD exacerbation that could put you in the hospital for days or even weeks. Not only do hospital admissions cost a fortune, but they’ll take you away from what you’re doing. Studies show that long-term oxygen therapy reduces the risk of hospitalization.
Disadvantages of Compressed Oxygen
The most notable disadvantage of compressed oxygen is how bulky, heavy, and dangerous it is. Even the smallest and lightest ones on the market are typically too heavy to carry by hand. Most people prefer to either put them in a backpack or use a rolling cart to transport them. What’s more, they aren’t approved by the Federal Aviation Administration (FAA) so you won’t be able to take them on a flight with you.
Liquid Oxygen Tanks
Liquid oxygen is used for the same purpose as compressed oxygen: to support healthy oxygen levels in COPD patients. However, since oxygen takes up less space in its liquid form, liquid oxygen is a better choice for people who want to stay out for longer without having to refill their oxygen tank.

In order for oxygen to be stored in a liquid state, it needs to be cooled to around -297 degrees Fahrenheit. So, in general, liquid oxygen tanks are more advanced and require more training to use than a compressed oxygen tank. As such, liquid oxygen is typically not prescribed for short-term use.
Key Benefits of Liquid Oxygen
Carry More Oxygen Than Compressed Tanks
The main reason someone would choose a liquid oxygen tank over compressed oxygen is that it offers significantly more oxygen. If you have high oxygen flow needs, you can rest easy knowing that you can stay out all day without having to refill the tank. You likely won’t need to resort to something like a pulse dose regulator which is designed to conserve oxygen which is a good thing because they can add weight and make the device more complicated to use.

Much Safer to Use
Another reason to go with liquid oxygen over compressed oxygen is that it’s much safer to use. Compressed oxygen is stored at very high pressures making it very dangerous to carry around or keep in your home. Liquid oxygen, on the other hand, is stored at very low temperatures because it doesn’t expand as much when it’s in its liquid form.
Disadvantages of Liquid Oxygen
The most notable downside to liquid oxygen is the cost. Due to the additional technology needed to keep oxygen at such low temperatures, you should expect to pay significantly more. It’s also a lot harder to find someone who can fill a liquid oxygen tank for a reasonable price. Despite the high costs, many people find that liquid oxygen is worth it due to the amount of freedom it offers.
Oxygen Concentrators
Oxygen concentrators are the newest form of oxygen therapy on the market. They’re used for the same purpose as compressed oxygen and liquid oxygen (treating chronic lung disease) but they’re battery operated. What this means is that as long as you have access to a functional battery, you’ll have an infinite supply of oxygen wherever you go.

Rather than holding oxygen like oxygen tanks, oxygen concentrators draw in ambient air and remove non-essential gases like nitrogen, argon, and carbon dioxide. They then put out pure medical-grade oxygen through the nasal cannula. Since there’s more that can go wrong with an oxygen concentrator, it’s important that you purchase one from a reputable brand like Inogen, AirSep, or Caire Inc.
There are three different types of oxygen concentrators on the market: home oxygen concentrators, portable continuous flow concentrators, and portable pulse flow oxygen concentrators. Home oxygen concentrators (stationary oxygen concentrators) need a wall outlet in order to operate whereas portable oxygen concentrators run off a battery.

Continuous flow oxygen concentrators are similar to oxygen tanks in that they put out a constant stream of oxygen. They tend to be bulky, usually weighing in at over 10 pounds. Pulse flow oxygen concentrators have additional technology built into them that only puts out oxygen when the user inhales. As such, they are more efficient, lightweight, and small.
Key Benefits of Oxygen Concentrators
No Refills
The greatest part about oxygen concentrators is that they never need to be “refilled” like oxygen tanks do. Simply charge the batteries and you’re good to go. Many POCs even come with car chargers so you can feel free to take a road trip or drive long-distance without ever running out of oxygen.
Very Small and Lightweight
By using compressed oxygen or liquid oxygen, you’re significantly restricting your freedom. Most oxygen tanks need to be wheeled around using a rolling cart but pulse flow portable oxygen concentrators can easily be carried at your side. Most pulse flow units weigh under 6 pounds and some are even small enough to fit in a purse or on your belt.

Safe to Use
While liquid oxygen tanks are significantly safer than compressed oxygen, they still can’t compare to pulse flow oxygen. Since oxygen concentrators don’t hold onto any oxygen that they use, there is no chance of them exploding or creating a fire. All of the oxygen that’s administered goes directly to the nasal cannula. Because of this, oxygen concentrators are the only oxygen therapy devices approved by the Federal Aviation Administration (FAA) for in-flight use.

Disadvantages of Oxygen Concentrators
For the vast majority of oxygen patients, oxygen concentrators are the ideal solution. However, there are some potential downsides depending on your situation. If your pulmonologist wants you to use continuous flow oxygen, you’ll have to either use a home oxygen concentrator or a continuous flow portable oxygen concentrator. While you can take these machines just about anywhere, they tend to be bulky and heavy. But most patients would say that they still offer significantly more freedom than oxygen tanks.
Conclusion
There are several different types of oxygen therapy out there so it’s important that you don’t get them confused. Hyperbaric oxygen therapy is a form of short-term oxygen therapy. It can be used to treat conditions like decompression sickness or to prevent reperfusion injury. Hyperbaric oxygen therapy should only be administered by a medical professional under controlled conditions in order to prevent oxygen toxicity.
Oxygen tanks, liquid oxygen tanks, and oxygen concentrators are more commonly used in a long-term setting in order to treat lung conditions like COPD, cystic fibrosis, and pneumonia. These oxygen devices are often prescribed to be used for several hours a day or even 24/7 if the situation demands. Compressed oxygen has been the industry standard for many decades but it’s becoming much less popular due to the freedom and independence liquid oxygen and portable oxygen concentrators have to offer.

If you have a respiratory impairment like chronic obstructive pulmonary disease (COPD) or pulmonary fibrosis, you’re probably used to carefully planning your day-to-day life. From following your treatment plan to scheduling doctor’s appointments, you need to have an acute understanding of your medical needs and how to address them.
One of the medical needs you may struggle with is supplemental oxygen therapy. Depending on how severe your respiratory illness is, your pulmonologist will ask you to use medical oxygen anywhere from several hours a day to 24 hours a day. Either way, this could mean making sacrifices like staying home from activities to ensure your oxygen needs are met.
Fortunately, there is an alternative to standard oxygen therapy methods like oxygen gas cylinders and liquid oxygen devices. Portable oxygen concentrators were invented in the early 2000s and they offer the same medical-grade oxygen as traditional delivery methods, but they offer it in a much more convenient way that allows you to live life freely and on your own terms.
What’s more, if you live in a state like Colorado, the last thing you want is to be stuck at home when there are so many better things you can be doing. In this post, we’re going to take a look at 7 reasons you should be using a portable oxygen concentrator rather than other medical oxygen devices in Colorado. Remember to always consult your pulmonologist before making any changes to your respiratory treatment plan.
They Work Great at Higher Elevations
Whether you’ve lived in Colorado your whole life or you’re an out-of-stater looking to come here for work or retirement, you likely already know the state’s most defining feature: The Rocky Mountains. People come from all around the country to ski, mountain bike, and simply enjoy the fresh mountain air.
Unfortunately, as an oxygen patient, you know there’s one slight problem with this: the air is much thinner at higher altitudes. What this means is that the higher you go in altitude, the less air pressure there is, and in turn, the less oxygen you have to breathe. This doesn’t just apply to the mountains though; even Denver, the Capital of Colorado is a mile above sea level.
If you have lived at sea level most of your life and don’t travel to higher altitudes very often, you might experience something called acute mountain sickness (AMS). This typically happens when you moved to a higher elevation without giving your body enough time to acclimate to the lower oxygen levels. Anyone can experience acute mountain sickness, but it’s more common and oftentimes more severe in people with COPD or other respiratory illnesses.
Some of the symptoms of AMS include:
- Fatigue
- Dizziness
- Breathlessness
- Nausea
- Headache or lightheadedness
If someone experiencing AMS stays at a high altitude or they continue to climb in altitude, they may experience more severe symptoms including confusion, chest pain, and reduced consciousness. Another condition that can result from AMS is something called high-altitude cerebral edema (HACE). This is a neurological syndrome that causes the brain to swell with fluid and can even result in death if it’s left untreated.

Generally speaking, it’s easier for COPD patients to live at lower altitudes where it’s easier to breathe, but if you want to live at a higher altitude, you should consult your doctor in order to learn how to do it safely. He/she will likely recommend that you start supplemental oxygen therapy or alter your current oxygen therapy plan to adjust for the change of altitude. For example, if you want to travel into the mountains, you may need to use oxygen intermittently in order to maintain your blood oxygen levels while at higher altitudes.
While this is not a commonly known fact, portable oxygen concentrators work great at high altitudes. The Inogen One G5, for example, works at altitudes up to 10,000 feet above sea level meaning you’ll have no problems living in Denver and traveling to the mountains. Be aware, however, that there are several towns in Colorado that are higher than 10,000 feet like Leadville and Alma, so you should only travel to these towns if your doctor specifically advises you to.
.png)
Most portable oxygen concentrators manufactured within the last decade or so offer similar results as the G5 in terms of operating altitude. However, you should be sure to speak with an oxygen concentrator expert before making any decisions.
They’re Great for Road Trips
Taking a road trip is about as American as baseball and apple pie. While not everyone enjoys driving for hours on end or putting thousands of miles on their car, it’s hard to deny its benefits when it comes to seeing more of the country. Colorado is packed with landmarks, but you’re going to need to take a lot of road trips in order to see everything the state has to offer.
Unfortunately, traditional oxygen therapy devices like compressed oxygen cylinders and liquid oxygen tanks make road tripping an impossible feat for most oxygen patients. Oxygen tanks only provide several hours of freedom before they need to be refilled or replaced and this simply isn’t feasible for a long road trip. It’s never easy to find a place to refill oxygen tanks while you’re on the road and bringing a bunch of extra oxygen tanks is cumbersome and takes up a lot of room in the car.
Portable oxygen concentrators, on the other hand, were specifically designed with travelers in mind. These oxygen machines run off of electricity and can be charged from any wall outlet or cigarette outlet in a car via a DC charging cable. So, instead of struggling to find a place to refill your oxygen tank or carrying a bunch of backup units, you’ll have access to an infinite supply of oxygen just by plugging your POC into your car. One thing to note, however, is that most POCs will not run on their maximum flow setting while plugged into the car and you should not charge your POC while the car is off in order to prevent the battery from dying. Refer to your user manual for more information on this.
Another reason portable oxygen concentrators are so much better for road trips is that they’re far safer than traditional oxygen devices. In order to drive with an oxygen tank, you need to take a number of safety precautions because they can explode in certain circumstances. They’re also very bulky and heavy so if they end up getting jostled around in the car, they could injure someone. POCs don’t have these problems because they’re lighter, easier to handle, and don’t have any compressed oxygen.
Hiking is a Breeze
In Colorado, hiking is a popular pastime for people of all ages, and for good reason! Just a short hike every day or two can reduce stress levels, reduce the risk of heart disease, lower blood pressure, and most importantly, allow you to explore a new area that you’ve never been to before. But without an oxygen device that’s manageable, you won’t be able to hike, even if you are physically able.

‘Hiking’ implies that you will be away from pathed paths meaning it won’t be easy to wheel your oxygen device around with a rolling cart. Rocks and other obstacles will make this a lot more trouble than it’s worth and you’ll likely need to take your eyes off where you’re going which can be dangerous. On top of all this, your oxygen tubing will need to run all the way down to the oxygen tank which can be a tripping hazard as well.
While continuous flow portable oxygen concentrators like the Respironics SimplyGo are too heavy to carry on your back or shoulder, pulse dose portable oxygen concentrators like the Caire FreeStyle Comfort are not. Weighing in at just 5 pounds, you’ll be able to hike all day without experiencing back or shoulder pain and with the ergonomic curve of the FreeStyle Comfort, it won’t slide around causing you to lose balance as you walk.

Many pulse dose machines like the Inogen One G3 offer plenty of options in the way of accessories in order to make it more comfortable and easy to carry. For example, there is the G3 backpack which has a compartment to hold the G3 and keep it secure and plenty of other pockets to hold personal belongings like keys, your wallet, or a camera. A similar carrying backpack was also available for the Inogen One G5.
If you’d like to learn more about hiking with a respiratory condition, please refer to one of our latest posts titled “You are Never Too Old for A Walk in the Woods.”
They Could Save You Hundreds of Dollars
There’s no denying that Colorado is a great place to live, especially for seniors and others looking to settle down after retirement. However, that doesn’t mean that it’s the cheapest state to live in. In the grand scheme of things, Colorado is actually pretty average when it comes to the total cost of living, but as we age and stop working, we have to get a little creative with how we spend and save our money.

As an oxygen patient, it may seem counter intuitive to look for ways to save money on your oxygen device. After all, you depend on it every day in order to feel better and improve your life expectancy. However, there are ways to reduce the amount of money you’re spending without increasing your risk of experiencing complications like COPD exacerbations.
While portable oxygen concentrators have a higher upfront cost, they’re actually much more affordable in the long run. For example, the Inogen One G4 retails at $2,295. Given that this machine is set to last 5 to 7 years on average, that’s around $0.90 to $1.20 per day of oxygen use. Compare this to oxygen tanks which cost an average of $5 or more a day to refill and maintain.
Another thing to consider is that most portable oxygen concentrators come with 3-year warranties. This will cover you with a full replacement unit in the event that you received one that is defective. And if you want an extra layer of protection, you can typically upgrade to a 5-year or lifetime warranty for an added cost. This will vary based on the unit that you’re purchasing so be sure to consult with an oxygen concentrator specialist.
Improved Self-Image
COPD and anxiety are two closely linked conditions. Physical symptoms such as chest pain and tightness can lead to natural increases in stress within the body, and people who are naturally predisposed to stress may experience even higher degrees of anxiety. Another thing that can lead to anxiety and even depression in COPD patients is their mindset. For example, someone who has a negative view of their disease and its outcome.
Believe it or not, the oxygen device that you use can also impact how much anxiety you experience. Someone who uses an oxygen tank may feel less capable and thus, experience lower self-esteem. On the other hand, someone who uses a portable oxygen machine may feel more confident because they’re thinking less about their oxygen delivery device and concentrating more on what they’re doing. POC users also report feeling more youthful and active than their oxygen tank counterparts.

If you own an Inogen One G3 we highly recommend accessories like the GO2 Carryalls. This is a stylish carrying bag specifically designed to hold your G3 and other personal belongings. The greatest thing about this bag is that it looks like any ordinary purse or handbag so you don’t have to be self-conscious about carrying around a supplemental oxygen device. It has a sleek leather look and comes in either brown or black so it can match with just about any outfit. It also has a conveniently located zipper so that you have easy access to your oxygen cannula and the G3’s user interface.
Conclusion
Colorado has a reputation as one of the most “outdoorsy” and “active” states in the country. If you have COPD or another chronic respiratory illness, that doesn’t mean you need to give these things up; it just means you need an oxygen device that can match your lifestyle.
Portable oxygen concentrators offer significantly more freedom and independence than other oxygen devices because they’re lighter, smaller, cheaper, and they allow you to stay out of the house for longer without having to search for a place to refill.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Pulse dose portable oxygen concentrators like the Inogen One G5 or Caire FreeStyle Comfort tend to be the best option for most people because they’re more reliable than their continuous flow counterparts. If you’re ready to learn more about our portable oxygen concentrators for sale, don’t hesitate to fill out the form at the side of the page or give our respiratory specialists a call.
In the meantime, check out the infographic below to see how pulse dose portable oxygen concentrators stack up against portable oxygen cylinders.
%20(1).png)
.png)
We've long known that the harsh chemicals found in many cleaning products can be dangerous if not handled correctly. However, recent research shows that common household cleaners may be much more dangerous than most people realize.
Studies show that breathing in the fumes from cleaning chemicals can cause both short-term and long-term breathing problems. Even if you don't notice immediate symptoms, years and years of exposure to these fumes can cause permanent lung damage and even life-threatening diseases like COPD.
This means that anyone who uses cleaning chemicals regularly may be putting their lungs at risk. However, the risk is much higher for people who suffer from existing respiratory problems like asthma or COPD.
People with respiratory diseases are particularly sensitive to the damaging effects of respiratory irritants like chemical fumes. That's why it is particularly important to learn how to recognize and avoid hazardous cleaning chemicals if you have a lung condition like COPD.
In this article, we're going to explain everything you need to know about how to protect your lungs from dangerous chemical fumes. We'll tell you which products are dangerous, which products are safe, and how to adjust your cleaning methods to be more lung and COPD-friendly.
We'll also introduce you to a variety of simple, safer cleaning techniques and alternative cleaning products, including lung-healthy cleaning solutions that you can make yourself at home. You will find all kinds of practical tips and tricks in this guide that you can use to significantly reduce your exposure to toxic cleaning fumes.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What Cleaning Fumes Do to Your Lungs
Any time you use a cleaning solution, it emits fumes into the air that you inevitably end up breathing. These fumes are made up of gaseous chemicals and tiny droplets that mist from the solution.
Many chemicals found in cleaning products create fumes that are irritating and toxic to your lungs. As soon as the fumes touch your lung tissue, they can cause inflammation and a variety of respiratory symptoms like coughing, sneezing, and shortness of breath.
These fumes can also inflame your eyes, nose, and upper airways, causing sharp, burning pain when you breathe. If you're exposed to a lot of fumes all at once, you might experience a sore throat, dizziness, headache, nausea, and even stomach pain.
These are the acute, immediate effects, but breathing chemical fumes can cause long-term health problems as well. Breathing in even small amounts of fumes over a long period of time can cause chronic health problems and do permanent damage to your lungs.
This often happens as a result of inflammation in the lungs, which can occur any time you breathe in a respiratory irritant, including chemical fumes. If sustained for too long, the inflammation begins to injure healthy lung tissue.
This kind of lung damage is permanent and cannot be reversed. Over many months or years, as more and more lung tissue gets affected, the damage can add up and cause noticeable lung function decline.
Certain chemicals, such as ammonia, emit fumes that are immediately caustic to your lungs. When these fumes come in contact with the delicate tissue lining the inside of your lungs, they cause immediate cell death, destroying healthy lung tissue and causing inflammation.
Usually, it takes many episodes of chemical exposure and inflammation over the span of many years to cause noticeable long-term damage. Unfortunately, studies show that simply using household cleaning products on a regular basis is enough to cause permanent damage—and even COPD—over time.
That's why you should never assume that your lungs are safe when you clean just because you don't notice any symptoms or the fumes don't burn your nose. You might not realize that cleaning fumes have damaged your lungs until much later in life when it starts to have more obvious effects on your health.
What the Research Says
Researchers have known for some time that exposure to cleaning chemicals can cause asthma and respiratory symptoms, but they had little data on the long-term effects. In the past few years, however, researchers have found strong links between cleaning chemical fumes and chronic respiratory diseases.

This is something scientists have long suspected but, until recently, didn't have the data to prove. Fortunately, two large-scale studies published in the past couple of years have shed more light on the link between cleaning fumes and long-term respiratory problems.
One study from Harvard, published in 2017, found a strong correlation between subjects' use of chemical cleaners and fatal lung diseases like COPD. In a study of more than 55,000 US nurses that spanned thirty years, they found that those who used chemical disinfectants just once per week had a 32 percent higher risk of developing COPD.
A more recent study from the University of Bergen in Norway looked at the effects of cleaning in a typical home environment. After tracking 6,000 subjects for twenty years, they found that women who regularly used chemical cleaning solutions had poorer respiratory function than those who didn't.
In fact, researchers estimated that the amount of lung function these women lost was roughly equivalent to smoking a whole pack of cigarettes every day. Those who were exposed even more often than that experienced more severe lung decline.
Despite including men in the study, they were unable to find any strong evidence of cleaning product-related lung decline in men. However, that doesn't mean that men who get regularly exposed to fumes from cleaning chemicals are any less at risk; the researchers noted that the men in the study just didn't use cleaning products as often as the women subjects, which likely left them with too small a sample to detect such effects among the men.
These studies show that even minimal exposure to chemical fumes can have a significant effect on your lungs over the span of many years. They also indicate that the severity of lung damage is directly related to how frequently you are exposed.
The most important take-away is that you should limit your use of chemical cleaning products as much as possible. And when you must use them, you should be careful to breathe in as little fumes as possible.
How Cleaning Fumes Affect People With COPD

Using household cleaning chemicals puts you at risk whether you're a healthy adult or someone who suffers from a chronic breathing disorder. However, exposure to chemical fumes can be even more dangerous for lungs that are strained due to an existing respiratory problem like asthma or COPD.
People with these conditions have particularly sensitive lung tissue, which means that even small amounts of fumes can trigger inflammation in their lungs. This makes their lungs more vulnerable to permanent damage as a result of exposure to chemical fumes.
Because their lung function is already limited, the damage COPD patients sustain from repeated exposure also has more serious effects. Further damage and inflammation from cleaning chemicals is much more likely to cause noticeable symptoms and measurable lung function decline.
Because of this, repeatedly breathing in respiratory irritants like chemical cleaning fumes can actually cause the disease to progress faster. It can cause quicker lung function decline and cause patients' respiratory symptoms to permanently get worse.
Cleaning fumes are also more likely to trigger immediate respiratory symptoms—like wheezing, coughing fits, and severe shortness of breath—in people with COPD. In some cases, they can even trigger COPD flare-ups that last long after the fumes are gone.
As a result, using household cleaners at all can make your COPD symptoms more difficult to manage on a daily basis. This can be dangerous, since managing your symptoms is a vital part of keeping your lungs healthy, preventing complications, and slowing down the progression of COPD.
In the next sections, we're going to show you a variety of ways you can reduce your exposure to dangerous cleaning chemical fumes. First, we'll take a look at which cleaning products are safe (and not safe) to use, and then we'll show you some specific tips and tricks for keeping your lungs protected every single time you clean.
Which Cleaning Products are the Most Dangerous?
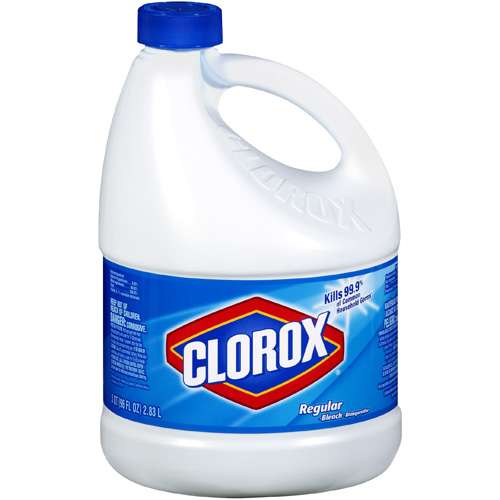
Few commercial cleaning products are completely safe to use, but some seem to be much worse for your lungs than others. Certain harsh cleaning chemicals, like ammonia and bleach, are particularly toxic to breathe.
The 2017 Harvard study, for instance, identified some specific chemical culprits that were most strongly linked to respiratory decline. They found that exposure to cleaning solutions containing bleach and a category of chemicals known as quaternary ammonium compounds (quats) seemed especially likely to cause COPD later in life.
Researchers believe that both types of chemicals can cause significant respiratory problems, even in small amounts, to people who use them regularly. If they are that dangerous even to healthy adults, using these chemicals could have even worse consequences for people with asthma or existing respiratory diseases.
Unfortunately, ammonia and bleach are some of the most common chemicals found in commercial cleaning products. If you don't read the ingredients carefully, you might even use cleaners containing ammonia or bleach without even realizing it.
However, ammonia and bleach are not the only chemicals worth avoiding; most commercial cleaning products contain chemical compounds that can irritate your lungs. A category of chemicals known as volatile organic compounds (VOCs), for instance, are well-known air pollutants and respiratory irritants that are found in all sorts of cleaning solutions.

There are many different types of VOCs, and they are found in a wide array of products, including cleaning solutions, hair spray, and even building materials like plywood and glues. Some VOCs are harmless, while others can hurt your lungs and cause a variety of other health issues, including organ damage and cancer.
In small amounts, VOCs are usually not harmful to healthy adults. However, if you get exposed to too many VOCs over a long period of time, they can cause serious health problems and chronic respiratory symptoms.
VOC's are most likely to cause respiratory symptoms in people with sensitive respiratory tracts, including people with asthma and COPD. Their existing respiratory issues make their lungs more prone to both the short-term and long-term effects of exposure, which is why they should be more careful to avoid VOCs.
If you have asthma or COPD, even mild fragrances in cleaning solutions and air fresheners can irritate your lungs badly enough to cause serious respiratory symptoms. Other VOC-heavy household chemicals, like adhesives, varnishes, and fabric softeners, may also trigger coughing and shortness of breath.
That's why it's important to check the ingredients on any cleaning and chemical products you buy to use in your home. Unless you need them for a very specific purpose, you should always avoid any cleaning solutions that contain ammonia, bleach, VOCs, or other harsh cleaning chemicals.
Sometimes, you can find versions of cleaning products that contain smaller amounts of VOCs and other noxious chemicals. However, it can be difficult to determine whether a product is safe because it's so hard to recognize the names of all the hazardous chemical compounds.
To help you out, we've made a list of some of the most common chemicals in cleaning solutions that can be dangerous to your lungs. We've also included some of their more obscure chemical names so you can more easily pick them out of ingredient lists.

Here are some of the most hazardous chemicals for your lungs and respiratory system:
- Ammonia
- Bleach
- Sodium hypochlorite
- Chemical solvents
- Hydrochloric acid
- Sulfiric acid
- Napthalene
- Propellants
- Formaldehyde (a VOC)
- Hydroxymethylglycinate
- Diazolidinyl urea
- Quaternium-15
- DMDM, aka Glydant
- Bronopol, aka 2-bromo-2-nitropropane-1,3-diol
- Grotan, aka hexahydro-1,3,5-tris(2-hydroxyethyl)-S-triazine
- Quaternary ammonium compounds
- Stearalkonium chloride
- Benzalkonium chloride
- Centrimonium bromide
- Quaternium 1-29
- Didecyl dimethyl ammonium chloride (DDAC)
- “Fragrance” (many products don't list specific chemicals used for fragrance)
- 1,4-dioxane
- Cresol
Here is a list of some specific products that contain hazardous chemicals or emit fumes that can irritate your lungs:
- Drain cleaners
- Disinfectants and sanitizing solutions
- Aerosol sprays (including fragrances and air fresheners)
- Carpet powders
- Dry cleaning powders
- Pain thinners
- Varnishes
- Adhesives
- Paint fumes
- Fabric softeners
If you suffer from chronic respiratory problems, it's worth going well out of your way to protect your lungs from all types of cleaning fumes, not just ammonia and bleach. That's why it's best to avoid commercial cleaning products all-together when possible and make your own lung-healthy cleaning solutions at home.
Which Cleaning Products are Safe?

The vast majority of commercial cleaning solutions are likely to contain noxious chemicals, VOCs, and fragrances that are dangerous to breathe. In order to eliminate the risk of harmful fumes, you will likely have to buy specialized, mild cleaning products or make your own DIY cleaning solutions.
Lung-Safe Commercial Cleaning Products
Unfortunately, products labeled “green” or “environmentally-friendly” may not actually be any safer for your lungs. That's why reading the label is a must; you should always look closely at the ingredients list and warning information before using any commercial chemical.
However, there are some other resources that can help you find safer cleaning products to use in your home. Both the Asthma and Allergy Foundation of America and the EPA have endorsed a multitude of products that are better for your health and the environment.
How to Find Safer Cleaning Products:
- The EPA's search tool for “Safer Choice Standard” products (search by product type to find a variety of products for different cleaning purposes)
- The Asthma and Allergy Foundation of America's list of certified asthma- and allergy-friendly products
DIY Lung-Safe Cleaning Products You Can Make Yourself at Home
 |
| Photo by Abi Porter |
Safe commercial cleaners can be difficult to find and expensive to buy once you do. Luckily, you can make simple and effective cleaning solutions yourself using just a few basic ingredients.
The following DIY recipes for homemade cleaners all use common, mild ingredients like soap, baking soda, vinegar, lemon juice, and borax. If you have asthma or COPD, these solutions won't harm your lungs and shouldn't trigger any respiratory symptoms.
All-purpose Cleaner
Recipe:
- 1 quart warm water
- 4 tablespoons baking soda
Uses: This deodorizing solution is great for cleaning smooth surfaces like appliances, faucets, kitchen counters, door handles, and more.
Instructions: Mix the water and baking soda together in a large container like a bucket, mixing bowl, or a large pot. To use, simply wet a cleaning towel or sponge with the solution and gently wipe down the surface you want to clean. The solution works best while the water is warm, so you should try to use it immediately.
Glass and Window Cleaner

Recipe:
- 2 cups water
- ½ cup white vinegar
Uses: Use to wipe down smooth glass surfaces like windows, glass doors. and glass tabletops.
Instructions: Mix the water and white vinegar together and store the solution in an airtight container or spray bottle. To use, either spray the solution directly on the glass surface and wipe dry, or wipe down the surface with a clean cloth dampened with the solution. You may need to wipe the surface one more time with a dry cloth to remove any moisture and leave the glass streak-free.
Grease-cutting Cleaner
Recipe:
- 1 cup white vinegar
- A few drops of liquid Dawn dish soap
- 1 tablespoon baking soda
- 2-3 cups of water
Uses: This cleaner is great for removing oil and grease from smooth surfaces like your kitchen counters, oven, and sink.
Instructions: Mix the vinegar, dish soap, and baking soda together in a spray bottle or another airtight container. Then add 2-3 cups of water and shake vigorously. Spray the greasy surface directly or dip a sponge in the solution, then wipe the surface clean. You may need to give the surface another wipe with a damp cloth to remove any leftover residue.
Scrubbing Solution

Recipe:
- 2 tablespoons lemon juice
- ½ up borax
Uses: This paste is great for removing rust and stains from porcelain, enamel, or stainless steel surfaces like your bathtub or sink.
Instructions: Mix the lemon juice and borax together to form a gritty paste. Apply the paste to a sponge or scrub brush and scrub the surface you want to clean. Once the stain or rust is removed, wipe the area clean with a damp cloth.
How to Reduce Your Exposure to Cleaning Fumes
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
There are many things you can do when you use cleaning products to reduce your exposure to their fumes. After all, even cleaning products that are safer for your lungs can irritate your respiratory system if it is very sensitive or you suffer from severe COPD.
That's why it's important to learn how to use all cleaning products safely. That includes properly handling chemicals, using noxious cleaners only when necessary, and ensuring that the air is well-ventilated while you clean.
Don't Use Spray Bottles

Spray bottles turn cleaning solutions into a fine mist, much of which ends up in the air rather than on the surface you are spraying. These droplets and fumes mix into the air and get into your lungs when you breathe.
Because of this, any time you use a cleaning spray, you are essentially spraying chemical fumes into the room. It is exposes you to significantly more fumes than plain liquid solutions and can be much more damaging to your lungs.
Instead of using spray bottles, you can simply use a cloth or sponge to absorb the solution and coat the surface you want to clean. Just dip your cloth (or sponge) into the solution, wring it out, and use circular wiping motions to distribute it evenly over the area.
Then, use a clean, damp cloth to wipe off the solution and any residue it loosens up. You may need to do a final wipe with a dry cloth to remove any excess moisture left behind.
Minimize How Often You Use Chemical Cleaners

Having COPD means you are more prone to illnesses and respiratory infections, which means it is very important to keep your environment free of bacteria and other sickness-causing pathogens. However, that doesn't mean that you have to use harsh chemicals and disinfectants every time you clean.
Chances are you don't actually need to use chemical cleaners and sanitizing solutions nearly as often as you think. In fact, the vast majority of cleaning tasks can be completed to satisfaction with nothing more than a clean cloth,
Influenza—also known as the flu—is one of the most common and deadly viruses that spreads throughout the US every year. With the peak of the flu season beginning in January and continuing through March, now is the time to get your flu vaccine if you haven't done so already.
Experts recommend that every person over 6 months old get the flu shot every year, but it is especially important for older adults and people with serious health conditions. This applies particularly to people with chronic respiratory diseases like COPD, who have a much higher risk of experiencing life-threatening complications if they get exposed to the flu.
Unfortunately, most adults fail to get the vaccine, and only about forty percent of American adults get their flu shot in any given year. However, doctors and health experts strongly urge all adults to get vaccine, both for their own health and to protect the health of others.
Still, flu vaccination rates stay low, in part because many people underestimate how serious and deadly the flu can be. This, in turn, causes many people to underestimate the importance of the flu vaccine and assume that skipping the yearly shot is not a big deal.
In this post, we're going to explain why getting your flu shot is vital, whether you are old, young, healthy, sick, or anything in-between. We'll also take a closer look at some of the reasons people decline the flu shot while debunking some of the most common myths and misconceptions.
We'll show you how the flu shot works, why it's recommended, and how it protects the lives of people with COPD and other chronic diseases. With the information in this guide, we hope that you will better understand the flu vaccine and why doctors believe it is so important for public health.
Flu Vaccine Basics: What You Should Know
Who Should Get the Flu Vaccine?

Many people assume that the flu vaccine is meant mainly to protect the young, elderly, and people with serious health conditions. However, this is false; doctors and health experts urge everyone over 6 months of age to get a flu shot every year, with just a few exceptions.
Your doctor will be able to tell you if you should get the flu vaccine and will give you the vaccine that is appropriate for your age. For example, adults over the age of 65 receive a special high-dose flu vaccine that is more effective for older adults.
According to the CDC, the following people should get vaccinated against the flu every year:
- Children 6 months of age and older
- All adults, including pregnant women
- Most adults who have chronic health conditions (talk to your doctor if you are unsure)
However, there are some people who should not get the flu vaccine, including:
- Some people with allergies to eggs or other ingredients in the vaccine (If you are allergic to eggs, you should notify your doctor, but you can most likely still get a flu vaccine.)
- Some people with Gillain-Barre Syndrome
Who Recommends the Flu Vaccine?

Just about every major governmental health organization along with many other expert health organizations recommend routine flu vaccination. They emphasize the importance of vaccination in the young, elderly, and those with chronic health conditions, but also urge healthy children and adults to get the vaccine as well.
Here is a list of some of the major health organizations that endorse the flu vaccine:
- The United States Center for Disease Control and Prevention (CDC)
- The World Health Organization (WHO)
- Canada's National Advisory Committee on Immunizations (NACI)
- The European Center for Disease Prevention and Control
- A large number of leading public health organizations and experts. The following represent just a few:
- American Academy of Family Physicians (AAFP)
- American Academy of Pediatrics (AAP)
- American College of Physicians (ACP)
- American Pharmacists Association (APhA)
- Association of Occupational Health Professionals in Healthcare (AOHP)
- National Foundation for Infectious Diseases (NFID)
- And many more!
Who is Most Vulnerable to Serious Flu Complications?

Certain groups of people are much more susceptible to the flu and flu-related health complications than others. This includes a larger number of people than most tend to realize, including anyone over the age of 65, anyone under the age of 5, and people with common health conditions like heart disease and COPD.
For these people, a flu infection could be deadly or cause serious secondary infections like pneumonia. That's why it's especially important for people who belong to these vulnerable groups to get vaccinated against the flu.
According to the CDC, it is particularly important for people in the following vulnerable groups to get the flu vaccine:
- Children under 5 years old (particularly children under 2)
- Older adults over the age of 65
- Pregnant women
- People in nursing homes and long-term care facilities
- Native Americans and Alaska Natives
- People with chronic respiratory illnesses, including asthma, COPD, and cystic fibrosis
- People with other chronic diseases, including heart disease, kidney disease, liver disease, and metabolic disorders like diabetes
- People with blood disorders (e.g. sickle cell disease)
- People with extreme obesity
- People with neurological and developmental disorders (e.g. cerebral palsy, epilepsy, stroke, and muscular dystrophy)
- People with suppressed immune systems (e.g. people taking steroids, immunosuppresant medications, and people with HIV)
- People receiving long-term aspirin therapy
When Should You Get Your Flu Shot?
The CDC recommends that you get your flu vaccine by the end of October every year. This gives the flu vaccine time to work before flu season begins to pick up in November-December.
In general, you will be protected from getting the flu about two weeks after you get your shot. That's why it's better to get your shot earlier in the season, rather than waiting until the flu has already begun to spread.
However, if you forget to get vaccinated early, you can still get the flu vaccine anytime throughout the winter and early spring. It will still be just as effective later in the season, but it won't be able to protect you from any flu viruses you catch before the vaccine takes effect.
If you are over the age of 65 or suffer from a chronic disease like COPD, then it's especially important for you to be protected from the flu for the entirety of the flu season. You should get your vaccine as early as possible so that your immune system has plenty of time to prepare before the virus begins to spread.
How Much Does the Flu Shot Cost?
If you have health insurance, then it's almost always free to get your yearly flu shot. But even if you don't have insurance, you may still be able to get the shot for free, or at least at a reduced price.
The chances are good that you can find some sort of program or event in your city that offers the flu vaccine for free. At worst, you shouldn't have to pay more than $25-35 out of pocket to get the shot at your local Walmart or CVS.
All Medicare plans also fully cover the flu shot. If you have medicare part B, the deductible doesn't apply to the flu vaccine, so you shouldn't have to pay any out-of-pocket costs.
If you don't have health insurance, click here to see a helpful list of some of the cheapest places you can go to get your flu vaccine.
Where Can You Get Your Flu Shot?

Flu shots are cheap, quick, and readily available all across the United States. You can get the vaccine at a variety of different places, including your doctor and just about any chain-business pharmacy.
Many colleges, employers, and other organizations also give flu shots on-site or offer vouchers to get a flu shot for free. You can also check with local health organizations and city, county, or state health departments to see if they offer flu vaccination programs or incentives.
Here is a list of some of the places you can go to get your flu vaccine:
- Your primary care doctor (you can make a special appointment or get the shot during a routine examination)
- Urgent care centers (these are often more convenient and closer to home than the doctor's office)
- Pharmacies (these are often the cheapest and most convenient option, and it's usually free if you have health insurance)
- Walmart
- Walgreens
- CVS
- Kroger
- Rite Aid
- Target
- Kmart
- Stop & Shop
Why You Should Get the Flu Vaccine: A Matter of Life and Death

The reason you should get your flu shot is twofold: first of all, you want to protect yourself from getting sick with the influenza virus and experiencing potentially life-threatening complications. The second is to prevent you from transmitting the virus to other people around you who could be even more vulnerable to the illness.
Here is a quick summary of the major benefits of getting the flu vaccine before we go into them in more detail.
Benefits of Flu Vaccination:
- Reduces your chances of getting sick with the flu
- Reduces your chances of experiencing a serious health complication (including hospitalization and death) from the flu
- Can reduce the severity of your flu symptoms and your risk of complications even if you end up getting sick with the flu
- Reduces your chances of spreading the flu virus to other people (including infants, who cannot receive the vaccine)
- Reduces the risk of serious complications, hospitalization, and death if you are over 65 or suffer from a serious health condition like COPD
- Protects pregnant women and infants (If a pregnant woman receives the flu vaccine during pregnancy, it can protect their infant child from the flu for several months after giving birth)
Getting the Flu Vaccine Protects Your Own Health

According to the Centers for Disease Control and Prevention (CDC), the flu kills, on average, 12,000 to 56,000 people in the US and puts up to 710,000 people in the hospital every year. The exact number of deaths and hospitalizations can vary significantly from year to year depending on the severity of flu outbreaks.
2017, for instance, was a particularly bad year for the flu in the US. That year, more than 80,000 Americans died from the flu, marking the highest number of flu-related deaths in four decades.
Many of these deaths and hospitalizations could have been prevented if more people had gotten the flu vaccine. Many of those who died were also healthy adults with no other serious medical conditions.
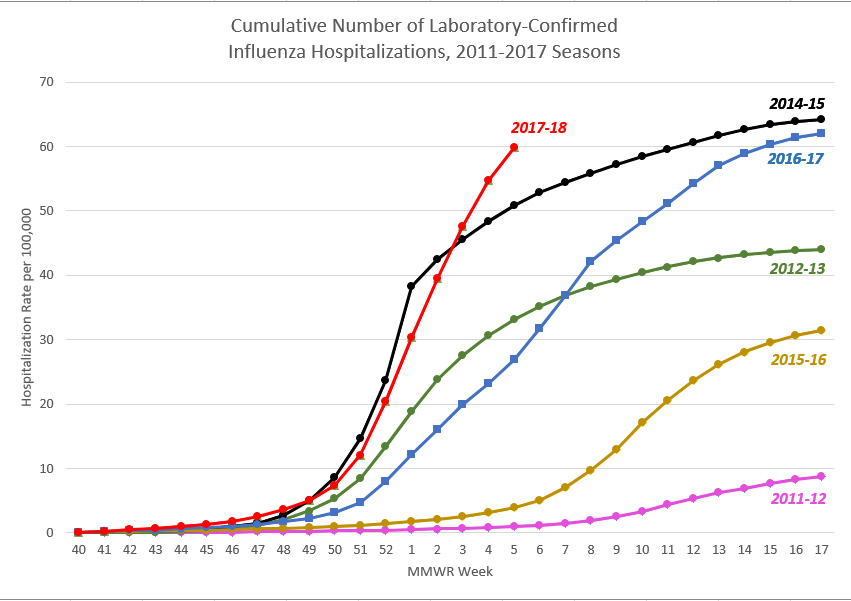 |
| Image created by the CDC |
Just because you've had the flu before and it turned out fine, that doesn't mean you're not at risk in the future. You may have gotten over many flus in your life, but all it takes is one serious infection to put your life and health on the line.
Whether you are 17 or 75, the flu vaccine could save your life and significantly reduce your chances of being hospitalized with the flu. Especially if you have COPD or belong to another high-risk group, there is no reason to take the risk of not getting the shot when the vaccine is so cheap and readily available.
Getting the Flu Vaccine Protects Others Around You and Can Even Save Lives
Even if you are not concerned about getting sick yourself, failing to get your flu vaccine could put the lives of vulnerable people at risk. That's why doctors recommend that everyone, even those with a low risk of flu complications, get the flu vaccine every year.
Chances are, you, a family member, or someone else you know comes into regular contact with someone with a serious health condition who needs extra protection from the flu. More than 11 million people in the US have been diagnosed with COPD alone, and they are certainly not the only ones who are at risk.
Unfortunately, many vaccinations—including the flu vaccine—are not as effective in the elderly and people with compromised immune systems. Even if they get vaccinated, their immune systems may not be able to build up an effective immunity to the virus.
The same applies to infants under the age of 6 months, whose immune systems aren't fully developed. Because of this, infants this young can't generate the immune response necessary to gain immunity from the vaccine.
All of these people who cannot build immunity on their own--from infants to older adults to immuno-compromised individuals--have to rely on the people around them to get vaccinated to protect them from the flu. This relates to a concept known as herd immunity, which we'll discuss more in the sections below.
How Does the Flu Vaccine Work?
Even though the flu vaccine is more effective and more readily available than ever, a large percentage of people in the US still decline this life-saving vaccine. We hope that by learning more about how the vaccine works and the benefits it has to offer, more people—especially at-risk populations like people with COPD—will choose to get their flu vaccine every year.
How Does the Flu Vaccine Protect You From the Flu?

The flu vaccine is essentially a mixture of inactivated flu virus strains. However, instead of getting you sick, the viruses in the vaccine help your immune system prepare to fight similar viruses in the future.
Most simply put, the flu vaccine introduces your immune system to a small sample of the same types of viruses that it might encounter if you get exposed to the flu. Your immune system then “remembers” what those viruses look like by creating an army of tiny molecules—called antibodies—that can recognize what the virus looks like.
That's why, when you get the flu vaccine, it takes a couple of weeks to take full effect. During those two weeks, your immune system is working hard to build up store of antibodies that will lie in wait until you get exposed to the virus again.
The next time one of those viruses (or a similar virus) enters your body, the antibodies will recognize the virus immediately and mark it for destruction. This allows your body to kill the virus so quickly that it never gets the chance to infect you and make you sick.
How Do Researchers Develop the Flu Vaccine Every Year?

The first vaccine able to combat the influenza virus was developed by researchers in the mid 1940's. This first vaccine only worked against one specific strain of the flu virus, but modern flu vaccines offer even greater protection.
The flu vaccine is unique in the sense that it get re-formulated every year. This allows researchers to create a vaccine that targets specific virus strains that are active at the time.
This is necessary because the flu is not just a single virus. There are hundreds of different known flu virus strains, and they evolve and change very quickly.
Right now, it is impossible to develop a vaccine that works against every single flu virus strain. Even if it were, the flu virus changes so quickly that it would evolve to evade the vaccine over time.
That's why researchers work hard every year to predict which strains are the biggest threat. Then, they pick the top 3-4 strains and develop a vaccine that boosts your immunity to those and similar virus strains.

Researchers are pretty good at predicting which strains will be most active, even though their estimations are not always perfect. But even with just 3-4 strains included the vaccine, researchers have been able to develop a vaccine that prevents, on average, up to ninety percent of of targeted flu viruses and about fifty percent of overall flu infections.
However, it's impossible to predict the future with absolute certainty, which means that the flu vaccine might be more or less effective in different years. If the common flu virus strains circulating around don't match well with the strains included in the vaccine, then the vaccine may not be able to prevent as many infections as expected.
How Effective is the Flu Vaccine?
On the surface, a sixty percent overall effectiveness rate might not seem very impressive for a vaccine, but there's a reason that it's endorsed by CDC and leading health organizations. A flu vaccine that prevents more than half of infections is extremely valuable, especially considering how deadly the flu can be.
Consider the fact that, in one of the deadliest flu seasons in America, the flu killed more than 80,000 people and forced Alabama to declare a public health emergency. The flu is no joke, and any vaccine that prevents a noticeable percentage of infections or deaths is absolutely worthwhile to use.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
The flu vaccine doesn't just reduce the number of people who get sick, but also reduces the number of serious flu complications and protects people in vulnerable groups. For example, the vaccine is 30-70% effective at preventing hospitalization with the flu in healthy adults, and 50-60% effective at preventing hospitalization in adults living in long-term care facilities like nursing homes.
The flu vaccine can also dramatically reduce the number of people who die from the flu. For people in long-term care facilities, the flu vaccine reduces death from flu complications by a whopping eighty percent.
The flu shot is also particularly effective at protecting children, which is evidenced by the fact that three out of four children who die from the flu did not receive a flu vaccination. In fact, one study found that getting the flu shot reduced the risk of flu-related death by 65 percent in healthy children and 51 percent in children with high-risk medical conditions.
What is Herd Immunity?

Remember how we mentioned that the flu vaccine not only protects you, but it protects people around you, too? This happens largely because of a nifty phenomenon known as herd immunity.
Simply put, herd immunity is the ability of a large population to resist an illness when a large number of people within that population are immune. It works by “breaking the chain” of infection, because people who are immune to an illness won't pass on that illness to others.
Viruses like the flu cannot spread as quickly when it continually encounters people who are vaccinated and immune. In this way, the flu vaccine can protect even those who are not vaccinated—and are thus not immune—from catching the flu.
Think of it this way: each person who gets the flu is one link in a long, branching chain that represents how the virus spreads from person to person. But if the flu virus reaches someone who is immune, then that particular branch of the chain stops, since the
-png.png)
Being diagnosed with a respiratory illness such as chronic obstructive pulmonary disease (COPD), cystic fibrosis, or pulmonary fibrosis can be life-changing. You’ll have to make adjustments to your daily routine in order to accommodate for doctors visits, pulmonary rehabilitation, supplemental oxygen therapy, and other lifestyle changes.
One hurdle many respiratory patients struggle to overcome after being diagnosed with COPD or similar conditions is maintaining relationships. Whether you like to visit a friend down the street or you have a long-time friend who lives overseas, a respiratory impairment of any kind can make these relationships difficult or impossible to maintain.
The good news, however, is that with enough time and patience, it is possible for respiratory patients to live a normal life. And the more you educate yourself about your condition and the tools at your disposal to help you succeed, the more equipped you will be to deal with problems when they arise.
Possibly the best way for COPD patients to overcome the setbacks of their illness is to invest in a portable oxygen concentrator. Unlike other oxygen delivery devices, portable oxygen concentrators enable patients to regain their freedom and independence while ensuring their oxygen needs are always met. Read on to learn 7 of the most important social benefits of owning a portable oxygen device.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Greater Independence
Independence is something that’s easy to take for granted until it’s gone. Independence is what allows us to get out and do the things we want on our own terms rather than being bound to a person or thing. Unfortunately, many COPD patients lack the independence they need to maintain an active social life.
Traditional oxygen devices like compressed oxygen tanks make it very difficult for respiratory patients to maintain their independence. These tanks can often weigh in excess of 100 pounds and they need to be refilled every time they run out of oxygen. There are portable oxygen tanks available, but they typically only hold a couple of hours worth of oxygen.

Refilling an oxygen tank is a long and tedious process no matter how you do it. If you want a professional to refill your oxygen tanks, you’ll likely need to sign up for an oxygen delivery service which is not only expensive, but it can be very time consuming as well. If you opt to refill your own oxygen tanks, you’ll need to purchase an oxygen refill system. These are very bulky devices that will stay in your home and can take several hours just to refill a small oxygen cylinder.
Aside from being dependent on their oxygen tank, oxygen refill station, or an oxygen provider, many COPD patients are dependent on their friends and loved ones. From making it to monthly doctors appointments or pulmonary rehabilitation appointments, it can be impossible to keep up with all of these things on their own. There’s no understating the work that caretakers put into helping their patients, but the truth is, many COPD patients want to take care of themselves.

This is where portable oxygen concentrators come into play. Unlike with oxygen tanks, you can be entirely self-sufficient when using a portable oxygen concentrator. Since they are electronic devices, all you need is access to a wall outlet in order to charge the batteries. And once they’re charged, you can go wherever you please without having to worry about your oxygen supply.
Ultimately, POCs will give you the independence you need to handle your own life without depending on others. You can make it to doctors appointments, pulmonary rehab, and social gatherings without having to bring a loved one or caretaker along to help out.
Better Health
The goal of supplemental oxygen therapy is to reduce common symptoms associated with COPD. This includes symptoms such as breathlessness, chest pain, coughing, wheezing, and more. Studies have also shown that supplemental oxygen plays a key role in treating COPD exacerbations by preventing hypoxia (deficiency of oxygen in the tissues).
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Whether you’ve been prescribed oxygen for several hours a day or your doctor wants you on oxygen 24/7, your health depends on your ability to receive the right amount of oxygen at the right time. And at the end of the day, portable oxygen concentrators offer much more flexibility when it comes to how your oxygen is administered.
.png)
Portable oxygen concentrators like the Inogen One G5, for example, provides patients with up to 1,260 ml/min of medical grade oxygen. The flow rate can easily be adjusted using the arrow buttons on the top of the unit, allowing you to fine-tune the amount of oxygen you receive. If for some reason a breath isn’t detected and no oxygen is put out of the device, you’ll hear an audible alarm notifying you.

When your health is in check and you’re doing everything you can to prevent COPD exacerbations, you’re likely going to have a much better social life. Whenever you go out with friends or family, you can rest assured that you’re receiving the oxygen you need to stay saturated. Of course, you’ll still want to take precautions such as avoiding polluted or smokey areas that could lead to exacerbations.
Long-Distance Travel is Possible
It’s hard to believe that just several decades ago, it was impossible for oxygen patients to travel long distances safely. Oxygen tanks have never been approved for in-flight use because they’re a fire hazard and they’re highly explosive. However, with the advent of portable oxygen concentrators, oxygen patients can travel freely on most major airlines as instructed by the Federal Aviation Administration (FAA).
.jpg)
The main reason POCs are safe on airplanes is that they contain pressurized oxygen like oxygen tanks do. They simply take ambient air, remove nitrogen, argon, and other impurities, then put out medical-grade oxygen via the nasal cannula. As aforementioned, it will only work when it detects a breath, so if you happen to drop the cannula, it won’t continue to put out oxygen.
Another form of long-distance travel you’ll have available to you are cruise ships. Taking a cruise is one of the best ways to explore an area of the world that you’ve never been to before and it’s also a great way to catch up with friends and family. While oxygen tanks are often permitted on cruise ships, this doesn’t necessarily mean you’ll have a way to refill it. And spending extra time with that means less time that you can spend with your loved ones.

On the other hand, all you’ll need with a POC is a fully charged battery and you’ll be able to stay out all day enjoying your time. Once you settle in for the night, you can charge up all of your batteries and have them ready to go in the morning. With the Inogen One G5, you can even invest in an external battery charger which will allow you to charge a battery separately from your POC.
If flying or taking a cruise isn’t your style, you might want to take a long road trip. Luckily, this is also a breeze when you have a portable oxygen concentrator. Most POCs either come with a DC charging cable or you can purchase one separately which will allow you to charge your device in your car using the cigarette outlet.

All-in-all, owning a portable oxygen concentrator is the best way for respiratory patients to stay connected with their friends and loved ones over long distances. Rather than fussing with an oxygen device that’s difficult to use and could put your health at serious risk, POCs just work, allowing you to spend quality time with your loved ones.
Improved Physical Endurance
Everyone has a friend or two who are constantly on the go. With healthy lungs, this might not be a problem, but if you have a respiratory illness, you may find it difficult to keep up with them. Aside from keeping your COPD symptoms in check, studies have also shown that supplemental oxygen can induce an enhanced physiologic training effect on the muscles which can improve your endurance and strength.

Another way portable oxygen concentrators help with physical activity is that they’re extremely lightweight and easy to carry. The Caire Freestyle Comfort, for example, weighs in at just 5 pounds and it’s still able to put out an outstanding 1,050 ml/min of medical-grade oxygen. Compare this to oxygen tanks or continuous flow portable oxygen concentrators which are too heavy to carry meaning you’ll have to wheel them behind you using a rolling cart.

Ultimately, owning a pulse flow portable oxygen concentrator means you’ll be able to keep up with those active friends in your life. Whether you just want to go for a daily walk in the park or you want to start a new exercise program, you’ll be able to do so without worrying about your ability to keep up.
Reduced Social Stigma
Social stigma is an unfortunate, but very harsh reality that people face on a daily basis. Essentially, a social stigma is a sort of generalized feeling about a certain person or thing. For example, people may see someone in a wheelchair and believe that they’re less capable than someone who can walk.

Similarly, someone who’s carrying or rolling an oxygen tank around with them may be seen as less capable than someone with a portable oxygen concentrator. One of the reasons for this is because most people don’t even know what portable oxygen concentrators are. They also look a lot more high-tech and advanced than oxygen tanks which affect the way people view them.
At the end of the day, we all know that oxygen patients are equally as capable as anyone else. However, owning a portable oxygen concentrator may prevent people from making generalized assumptions about you and your condition. It can also be a great conversation starter because people will be curious about what your POC does and how it works!
Improved Self-Confidence
One thing that’s more important than the way others feel about you is the way you feel about yourself. Confidence is key to maintaining any relationship and portable oxygen concentrators will inevitably make it easier to feel comfortable and confident being yourself.
.jpg)
When it comes to oxygen tanks, there’s very little in the way of customization or personalization. Most oxygen tanks are a drab silver and green color that’s not very appealing to the eye. This can lead to you feeling self-conscious about your oxygen tank, taking your mind off social interactions as a result.
-min.png)
Due to their size and bulkiness, oxygen tanks can also be embarrassing to maneuver in public. Whether you’re walking down a crowded sidewalk or you’re going up a flight of stairs, it’s difficult to be graceful with an oxygen tank.
Portable oxygen concentrators are the polar opposite of this. They’re light enough to carry on your shoulder and small enough to tuck under your arm without bumping into people. You also won’t have to dread taking public transportation or going up a flight of stairs with a portable oxygen concentrator.

When it comes to aesthetics, portable oxygen concentrators are much more stylish than oxygen tanks. While oxygen tanks are very oblong, portable oxygen concentrators are compact and sleek looking. You’ll also have access to more accessories like the Inogen One G5 Custom Carrying Case or the GO2 Carryall for the Inogen One G3 which completely conceals the concentrator.
They’re More Affordable for Long-Term Care
Potentially the most controversial topic surrounding supplemental oxygen is its cost. On one hand, patients need a device that can meet their needs consistently and reliably. On the other hand, they don’t want to break the bank doing it.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
While at first glance, portable oxygen concentrators may seem like they’re the most expensive option, they’re actually far more affordable for long-term oxygen therapy. For example, if you spend $2,000 on an oxygen concentrator that lasts an average of 5 years, that’s just over a dollar a day. What’s more, most POCs come with a 3-year warranty at the very least meaning you’ll have an extra safety net if there happens to be a defect with your unit.

Ultimately, when you invest in a more cost-effective long-term solution for your oxygen needs, you’ll have more money to spend on other things such as a night out with your friends. Since financial struggles are among the top triggers of stress and anxiety, it’s best to always create a long-term financial plan rather than choosing the option that’s the most convenient at the time.
Conclusion
Being diagnosed with COPD or another chronic respiratory illness should not mean sacrificing time spent with friends and loved ones; if anything, the exact opposite is true. COPD patients should be spending more time on their relationships because they’re proven to reduce stress, boost life expectancy, and improve general well-being.
While there are many things you can do to maintain an active social life with COPD, investing in a portable oxygen concentrator is likely one of the most important. With a portable oxygen concentrator, you’ll have the freedom to go where you want, when you want. And you’ll feel significantly more confident and secure with a high-tech medical-oxygen delivery device at your side.
If you have any questions at all about portable oxygen devices for seniors, don’t hesitate to reach out to our respiratory specialists here at LPT Medical. Start by filling out the contact form at the side of the page and we’ll answer any question you may have.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!














