If you have COPD, then you know that getting sick can wreak havoc on your daily life. Even common illnesses like the cold or flu can significantly increase your COPD symptoms and, in serious cases, even land you in the hospital.
That's why many doctors see the prevention of illnesses and infections as a primary treatment goal for COPD. Even the most minor illnesses can lead to exacerbations, which can be life-threatening or cause permanent worsening of lung function and COPD symptoms.
In this article, we'll show you how to avoid illnesses like the flu, pneumonia and the common cold if you have COPD. That way, your body can focus all of its energy and resources on keeping you and your lungs as healthy and strong as possible.
First, we'll explain how common viruses like the flu and common cold spread and how they can affect your COPD. Next, we'll introduce you to a variety of practical tips and techniques you can use to stay healthy and boost your immune system during the cold and flu season this year.
Even though COPD puts you more at risk for getting sick, there are many simple actions you can take in your daily life to stave off illnesses and infections. If you learn how to protect yourself and how to put those steps into action, you can significantly reduce your likelihood of getting sick and making your COPD worse.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Why Common Illnesses Are More Serious for COPD Patients

People with COPD have weakened immune systems, which makes them more likely to get sick if they get exposed to viruses or bacteria. It also makes COPD patients more likely to get secondary illnesses and infections, and more likely to experience serious complications when they get sick.
For instance, if you have COPD, getting a common cold makes you thirty times more likely to experience an exacerbation, which can cause life-threatening symptoms and hospitalization. Even when they don't cause exacerbations, illnesses take precious energy and resources away from your lungs and make it more difficult to breathe.
If you have COPD, any kind of illness or infection can weaken your lungs and cause you to have an acute exacerbation. However, illnesses that affect your respiratory system, like the flu, common cold, and pneumonia, are often the most threatening because of their symptoms and how quickly they can get worse.
Let's go through each of these sicknesses to better understand how they work and how they affect people with COPD.
The Common Cold
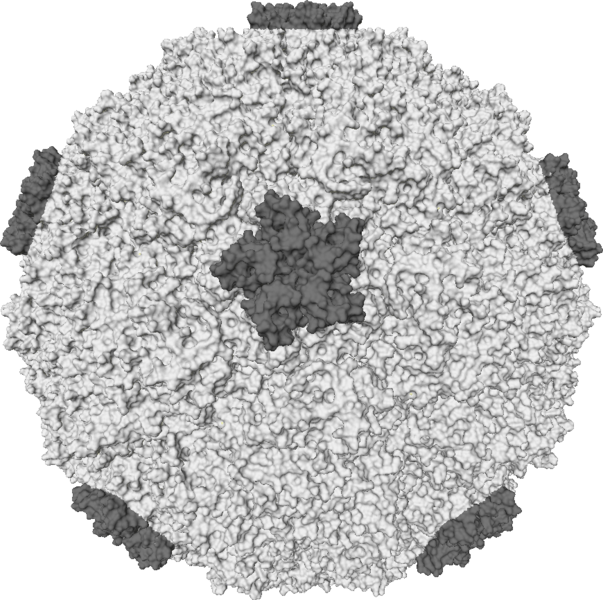
The common cold is caused by a virus, or, more precisely, a group of viruses that are constantly changing and adapting. Common cold viruses (known as Rhinoviruses) generally affect your nose and throat, causing a variety of respiratory symptoms like coughing, sneezing, and excess mucus production that make COPD symptoms much worse.
There are more than 200 types of cold viruses and they are all tricky and evasive. Rhinoviruses evolve very quickly, which is one of the reasons why the common cold is so difficult to treat and prevent. By the time researchers can identify and analyze a particular strain of cold virus, there's a completely new set of rhinoviruses getting passed around.
Because of this, there are no targeted vaccines or treatments that are effective for the common cold. Instead, simple prevention through proper hygeine is still the most effective way to protect yourself from contracting a rhinovirus.
Most people start showing cold symptoms 2-3 days after being exposed to a rhinovirus. Most common colds only last about a week to ten days, but they can sometimes last longer or leave lingering symptoms, like a persistent cough.
Symptoms of the Common Cold:
- Coughing
- Sneezing
- Sore throat
- General malaise (not feeling well)
- Runny nose or congestion
- Thickened mucus
- Mild headache
- Mild body aches
- Low-grade fever
If you think that you are coming down with a cold, consult your COPD treatment plan to figure out what to do next. Your doctor might recommend increasing how frequently you take certain medications or starting a course of corticosteroids or antibiotics to prevent secondary infections.
It's a good idea to call your doctor whenever you start to feel sick, and to check back in if your symptoms don't improve in a few days. If your symptoms start to get significantly worse, or you are experiencing an acute exacerbation, don't hesitate to talk to your doctor or seek medical attention.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
The Flu

Influenza (also known as the flu) comes with many of the same symptoms as the common cold. However, unlike the common cold, which is generally very mild, the flu can make you severely sick. It is particularly dangerous for the young, old, and people with chronic diseases to get the flu, as it has the potential to cause serious complications and even death.
The flu is also a common cause of pneumonia and a variety of other secondary infections, including sinus infections and ear infections. People with COPD are particularly likely to develop pneumonia if they get the flu, which is why disease prevention is so important for COPD patients.
Most healthy adults who get the flu are able to recover relatively quickly and don't experience any serious complications. However, the flu can be much more serious and even deadly for people with chronic diseases like COPD, diabetes, and asthma. People over the age of 65 are also at a much higher risk of serious complications from the flu.
Telling the flu apart from the common cold can be tricky, which is why you should always call your doctor if you feel sick during the flu season. Your doctor can give you a test to see if you have the flu and determine how to treat you based on the results.
Common Symptoms of the Flu:
- Fever
- Chills
- Cough
- Runny nose or congestion
- Headaches
- Body aches
- Fatigue
- Sore throat
During flu season, you should take extra precautions and monitor your health more carefully. Take any respiratory or flu-like symptoms very seriously, and call your doctor earlier when you start feeling sick.
If you think you are starting to get the flu, you should follow the appropriate treatment plan recommended by your doctor and talk to your doctor immediately. There are certain medications, like Tamiflu, that can significantly reduce the length and severity of the flu if taken early enough.
Pneumonia
Another particularly dangerous illness for people with COPD is Pneumonia, a type of respiratory infection that causes inflammation in the air sacs in your lungs. Pneumonia happens when the air sacs (or alveoli) in your lungs fill up with fluid, leading to symptoms like coughing, fever, and breathing difficulties.
Pneumonia is more likely than the cold or flu to cause serious complications, especially for people with COPD. In severe cases, pneumonia can cause lung abscesses, fluid build-up in the lungs, respiratory failure, and death.
Pneumonia can be caused by viruses, bacteria, and even fungi, and most commonly occurs as a result of respiratory infections like the flu. Pneumonia is most common in people over the age of 65 and people with chronic respiratory conditions.
When you have COPD and experience respiratory symptoms on a regular basis, it can sometimes be difficult to tell the difference between a minor COPD flare-up and signs that you're getting sick. That's why it's important to remember and recognize the symptoms of the common cold, flu, and pneumonia.
Pneumonia tends to come with symptoms that are similar to the common cold or regular COPD symptoms. It's common to feel chest tightness, shortness of breath, and experience thicker, darker mucus in your airways.
Common Symptoms of Pneumonia:
- High fever
- Chills
- Worsened chest pain and tightness
- Headaches
- Body aches
- Fatigue
- Shaking
- Shortness of breath
- Rapid breathing
- Thick, dark-colored mucus
If you have cold or flu symptoms that last more than a week or if you believe you might have pneumonia, you need to call your doctor immediately. Pneumonia can often be diagnosed through a simple examination, chest x-ray, or by testing sputum that you cough up from your lungs.
If you have pneumonia, your doctor will determine whether it's caused by a virus, bacteria, or fungus, and start you on the appropriate medication. It's important to get proper medical treatment immediately and as early as possible in order to prevent serious and life-threatening complications.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
How to Avoid Getting Sick

Now that you know how dangerous even mild illnesses can be, you're probably eager to know what you can do to protect yourself from getting sick. Fortunately, there's plenty you can do to reduce your chances of catching contagious illnesses, but unfortunately, no matter how careful you are, it's no guarantee.
Most respiratory illnesses, including the common cold and flu, are very contagious and can spread in many ways. You can catch a cold or flu simply by breathing in the virus from the air or from touching a contaminated doorknob.
That's why it's so important to know what to watch out for and how to protect yourself from the viruses and bacteria in your environment. Read ahead to learn how proper hygiene, vaccination, and other precautions you can take in public can reduce your chances of exposure to disease-causing germs lower your chances of getting sick to a minimum.
Wash Your Hands

Most of the things you touch, including food, people, animals, plants, and anything outdoors is a potential source of germs that could make you sick. That doesn't mean you should be afraid of everything, but it highlights why it's so important to wash your hands often.
Hand-washing is probably the most effective way to protect yourself from illnesses and infections. That's why the CDC calls it a “do-it-yourself vaccine” and uses the slogan, “Clean Hands Save Lives.”
Hand washing works because soap and water is generally enough to remove the vast majority of harmful viruses and bacteria that your hands pick up throughout the day. Washing your hands will not only keep you healthy, but it helps protect other people from getting sick as well.
How and When to Wash Your Hands

In general, you should wash your hands anytime they come into contact with anything that could harbor harmful bacteria or viruses. You should scrub your hands immediately after touching anything visibly dirty or unclean, and anytime you arrive home from an outing.
While you should never wash your hands obsessively, you should wash them often, especially when you're out in public. Here is a guide to some situations in which you should always wash your hands:
-
When cooking: It's very important to always wash your hands frequently while prepping and cooking foods, especially after touching raw or cooked meats. Washing your hands in-between handling different ingredients and before you eat will prevent food cross-contamination and exposing yourself to harmful germs.
-
After visiting a public place: Wash your hands whenever you get home from an outing. You risk exposure to harmful bacteria and viruses anytime you go in public or around other people; this includes going to the grocery store, a friend's house, the park, library, movie theater, or a restaurant.
-
After using the bathroom: Always wash your hands thoroughly after using the bathroom, even in your own home. If you're in a public place, use a paper towel instead of your bare hands to touch the doorknob on your way out. You should also always wash your hands after changing a diaper.
-
After touching surfaces in public: Anything that many people use or touch can potentially harbor dangerous viruses and bacteria. You should always wash your hands after touching public doorknobs, pens, counters, sink faucets, credit card machines, and more. You can also bring sanitizing wipes with you to wipe down certain items, like public phones or the handle on your grocery cart, before you use them.
-
After shaking hands: Even if you are careful to wash your hands, the people you meet on a daily basis might not be so hygienic. Always wash your hands after meet-and-greets and anytime you touch another person's hand.
-
After cleaning or handling trash: You're bound to get some nasty dirt and germs on your hands whenever you clean, gather up garbage around the house, or take out the trash. You should wash your hands after anytime you clean your house or touch any trash or garbage receptacles.
-
When visiting a doctor's office or hospital: Contagious illnesses and infections are ever-present in hospitals and doctor's offices, which make them risky places for patients with compromised immune systems. Take care not to touch public handrails, arm rests, counters, and pens if possible, and wash your hands immediately after if you do. Bring your own pen to sign yourself in instead of using the public pen provided at the front desk.
-
Before touching a newborn: Newborn babies don't have fully developed immune systems yet, and are thus especially susceptible to viruses and bacteria that you might have on your hands.
- Before you eat: Whenever you eat, you're using your hands or utensils to put things directly into your mouth. This puts you at risk of transferring germs from your hands or utensils to your food, then putting it into your body where it could make you sick. Whether you have COPD or not, everyone should wash their hands right before eating, without exception. Make it a habit in your household to have everyone wash up before meals.
How to Practice Proper Hand-Washing Technique

While hand-washing is a very effective way to prevent disease, it only works if you do it right. Unfortunately, most people don't know how to wash their hands properly and do a lazy or inadequate job of cleaning their hands.
How to Wash Your Hands Properly
- Wet: Run your hands under clean, running water from a faucet.
- Lather: Turn off the water and put soap on your hands. Then rub your hands together until it forms a frothy lather.
- Scrub: Use the lather to scrub your hands from top to bottom for about twenty seconds. Scrub your hands thoroughly, including your fingers, palms, wrists, and the backs of your hands. Don't forget to scrub between your fingers and under your fingernails. Use a nail brush if your hands are very dirty or there is dirt caught under your nails.
- Rinse: Turn on the tap again and rinse your hands under the clean, running water until all the soap is gone.
- Dry: Use a clean washcloth, towel, or paper towel to pat your hands dry. If you don't have a towel, shake the excess water off your hands and let them air dry.
Stay Away from Anti-Bacterial Soaps At All Costs
 |
| Image courtesy of Mike Mozart. |
As a final piece of hand-washing advice, you should stay away from antibacterial and antimicrobial soaps at all costs. They're not just ineffective, but potentially dangerous for both individual people and the environment.
While the term “anti-bacterial” in the name might make you think they work better, antibacterial soaps are actually less healthy for you than plain soaps that don't contain antibiotics. They don't clean your hands any better than regular soap and water, and they don't make you any less likely to get sick.
In fact, according to the FDA, antibacterial soaps don't offer any extra protection against illnesses and might even “give people a false sense of security.” Antibacterial soaps also encourage the growth of antibiotic-resistant bacteria, a problem that has grown along with popularity of antibacterial soaps.
Because of this, you should always check the label on any soap you buy and reject anything that says “antibacterial,” “antimicrobial,” or has a “drug facts” section on the label. Instead, opt for regular, plain soap and warm water whenever you wash your hands.
Don't Touch Your Face

While it helps to wash your hands every so often while you're out and about in a public place, there's no need to go overboard. You don't want to be a total germaphobe, and it's not possible or practical to wash your hands every single time you touch a doorknob or another potentially-contaminated surface.
Instead, simply keep your hands away from your face in-between hand washings. This will prevent you from accidentally inoculating yourself with whatever viruses and other pathogens your hands have picked up.
Germs on the surface of your skin can't infect you unless they find another way in; your tough skin is an effective barrier for keeping viruses and bacteria out of your body. But if you touch your face, germs on your hands can find their way into your eyes, nose, or mouth, where they can enter and infect your body.
But as long as you keep your hands away from your face, you're not likely to get sick from any pathogens your hands pick up. Just remember not to rub your eyes or nose, chew your nails, or let your fingers touch your tongue or lips.
Face-touching is a common thing that many people do without even realizing it, so it might take some concentrated effort to break the habit. You'll have to keep it in mind when you go out and get used to catching yourself in the act in order to reprogram absent-minded behaviors, like rubbing your face, that put you at risk.

Start the new habit at home and start training yourself to keep your hands at your sides and avoid touching your face unnecessarily. If you need to touch your eyes, blow your nose, or touch your face for any other reason, make sure you remember to wash your hands or use hand sanitizer first.
The other way that germs get into your body is through wounds and broken skin, which is why it's important to wash and cover any scratches, scrapes, burns, or other lesions you have. Otherwise, you could get a serious infection that weakens your immune system and causes you to get sick.
Use Hand Sanitizer
Hand sanitizer is a great option when you need to wash your hands but don't have access to a bathroom or sink. Although not quite as effective as hand-washing, hand sanitizers can kill the vast majority of viruses and bacteria on your skin and can be indispensable in a pinch when you're out in a public place.
But you have to look out for quality if you want a hand sanitizer that's safe and effective. Alcohol is the active ingredient in sanitizers that kills pathogens, but some don't contain a high enough percentage to reliably kill the bulk of the germs on your skin.
Always check the label and make sure that any hand sanitizer you buy contains at least 60 percent alcohol. Any less is hardly better than using plain water, and can even be dangerous for offering false protection.
You can keep a small bottle of hand sanitizer in your purse or pocket for anytime you need a quick, easy way to get rid of germs on your hands. It's useful for when you're out shopping or when you touch surfaces in high-traffic areas like doorknobs, hand rails, and credit card machines.
It is possible to have too much of a good thing, however, and you should only use hand sanitizer when you really need it. Excess hand-washing and hand-sanitizer use is bad for your skin, and using sanitizer too often can even breed super-strong, resistant bacteria. In moderation, hand sanitizer can keep you healthy, but too much can hurt your immune system and actually make you more likely to get sick.
Avoid Large Crowds

Lots of fun events and activities involve being around hundreds or thousands of other people. This includes most public events like parades, conventions, and holiday festivals. Unfortunately, cramming lots of people into small spaces comes with a lot of disease risks, which makes these situations especially dangerous for people with COPD.
While crowded, public events can be fun to attend, patients with compromised immune systems should avoid them during cold and flu season. No matter how many precautions you take, contagious illnesses can spread through crowds like wildfire, and the risk of picking up harmful germs from common areas increases significantly.
Here are some examples of crowded places you should try to stay away from during cold and flu season:
- Large festivals and events
- Sporting events
- Concert halls
- Convention centers and other entertainment venues
- Places with lots of children, including preschools, grade schools, and day cares
- Busy shopping malls
- Busy college campuses

If you can, skip out on busy winter festivals and try to attend public events during other times of the year, when the risk for contagious illnesses is not so high. If you must go to a crowded event, take every precaution you can to reduce your exposure to public surfaces and airborne germs.
Here are some tips for protecting yourself in crowded places:
- Wear a surgical mask or a CDC-certifie
%20(1).png)
Around 70 million people in the United States suffer from some form of sleep disorder such as narcolepsy, insomnia, or obstructive sleep apnea (OSA). These conditions can appear anytime during our lives and they have a significant impact on our general health and well-being.
Unfortunately, there are many obstacles that prevent people from receiving the treatment they need for sleep disorders. Chief among them is the fact that many people don’t even realize they have a problem in the first place. Symptoms such as daytime sleepiness, restlessness, or difficulty concentrating are often shrugged off as an inevitable part of life.
Another obstacle preventing sleep disorder patients from getting the help they need is confusion about their disease and the treatment options that are available to them. People hear terms like CPAP, BiPAP, EPAP, or APAP, but they never actually receive a simple explanation of what these terms mean and how they relate to each other.
In this post, we’re going to clarify any confusion about these terms as well as how they pertain to other types of respiratory therapy like supplemental oxygen. Remember to check in with your doctor if you have any questions or if you are thinking of making any changes to your treatment plan.
What is Obstructive Sleep Apnea (OSA)?
There are several types of sleep apnea, but one of the most common is obstructive sleep apnea. OSA occurs when the muscles in your throat relax intermittently at night causing you to stop breathing and lose sleep. It’s estimated that about 22 million Americans have some form of sleep apnea.
.jpg)
Obstructive sleep apnea is notoriously difficult to self-diagnose because the patient will likely have no recollection of what caused them to lose sleep or wake up frequently at night. In fact, many undiagnosed OSA patients believe that they get great sleep each night. This is why it’s important to speak with your doctor about having a sleep study done so that a medical specialist can examine your sleep patterns and determine if OSA is present.
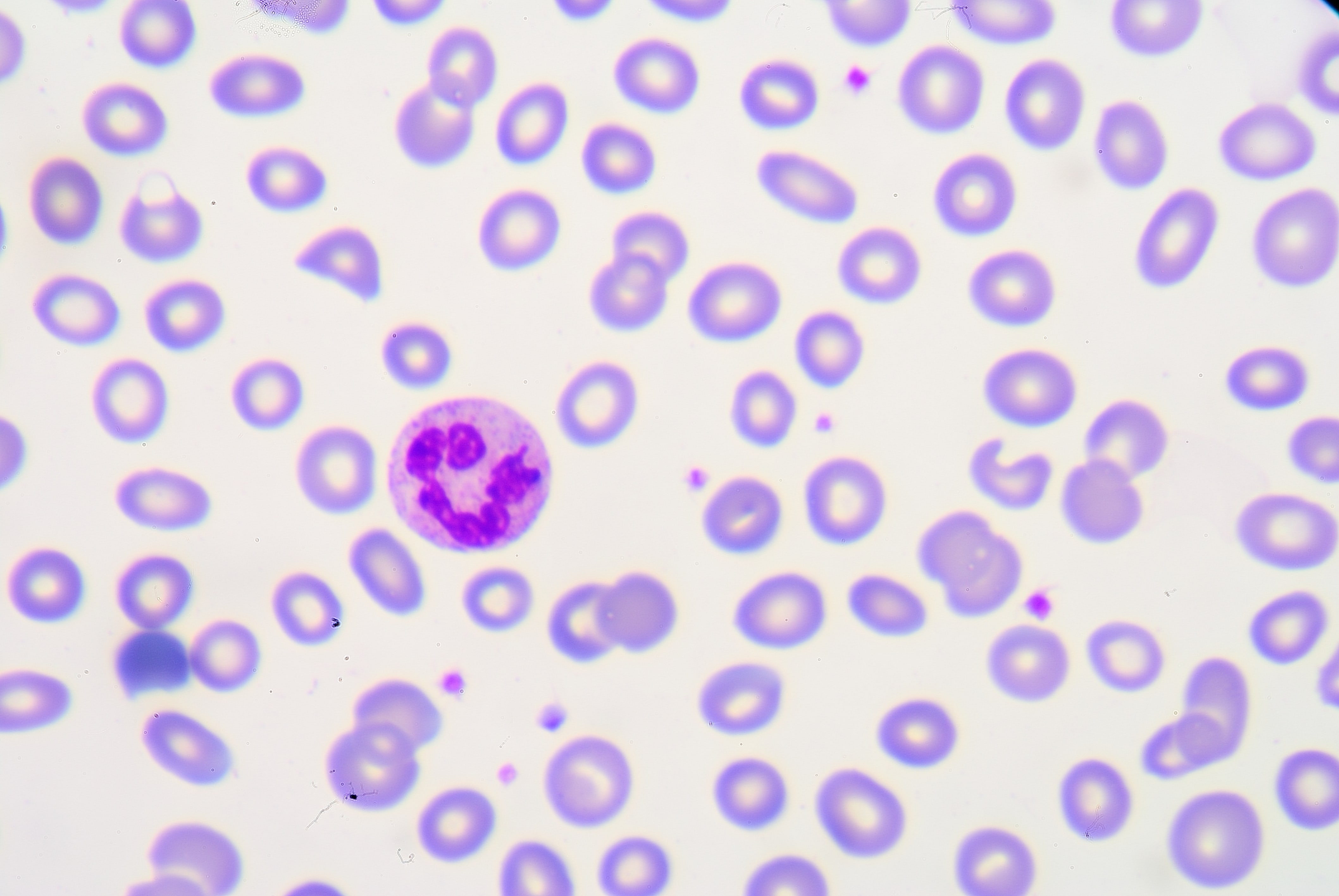
A sleep study (polysomnography) is a non-invasive exam where you will stay in a sleep center overnight. During this study, electrodes will be placed on your head that measure brain activity, you will have a pulse oximeter attached to your finger which measures blood oxygen levels, and a belt will be wrapped around your chest to monitor breathing.
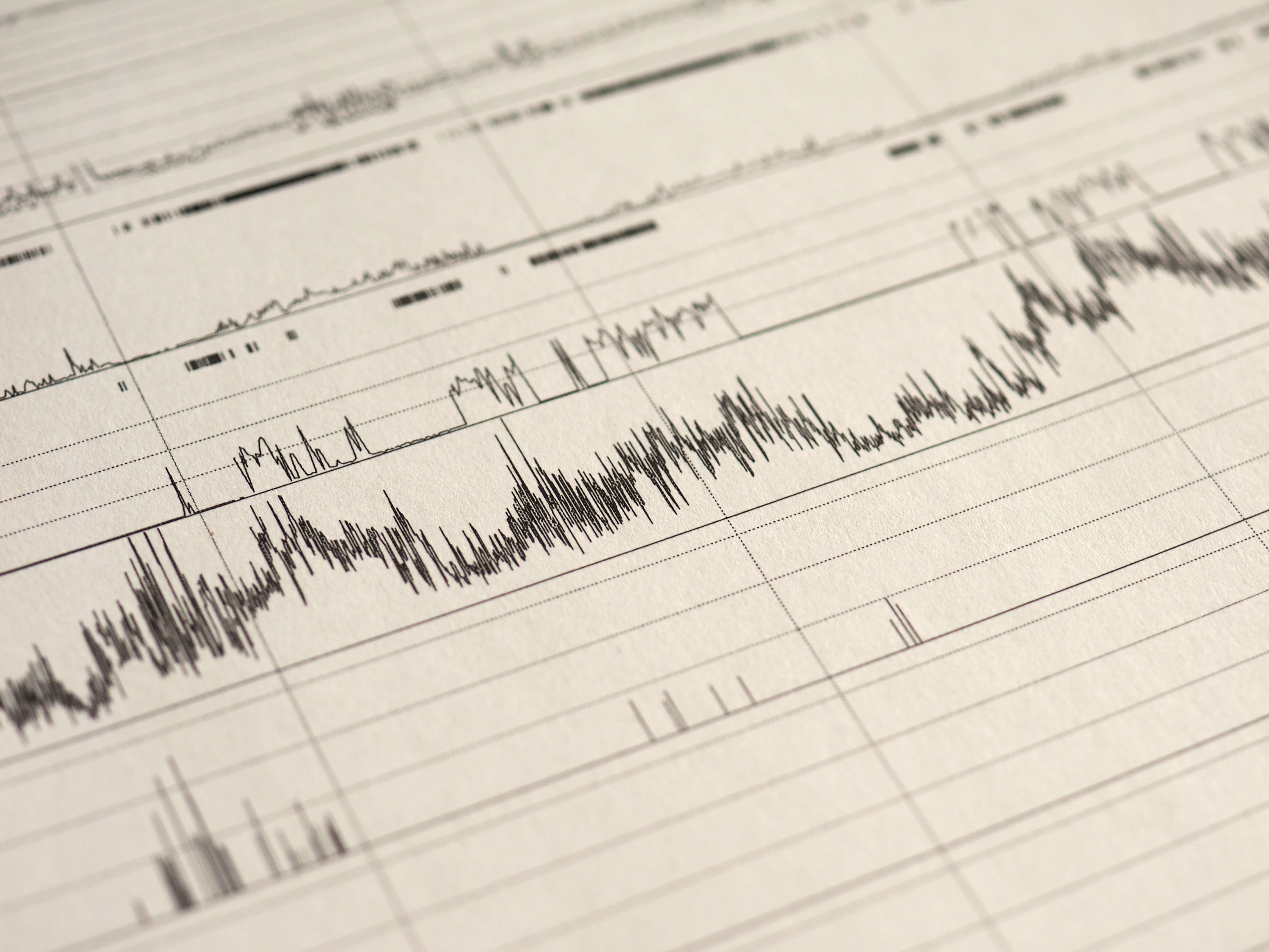
This is one of the most effective ways for a health professional to diagnose OSA because it will show them exactly what’s going on in your body during sleep. For example, if your breathing is interrupted, your blood oxygen levels will likely drop and you’ll wake up. Occasional sleep interruptions are normal, but if it’s happening frequently throughout the night there is a more serious underlying issue at play. According to worldsleepday.org, patients with severe sleep apnea may wake up more than 30 timers each hour.
Why is it Important to Treat Sleep Disorders?
For many people, the term “sleep disorder” doesn’t bring about a huge amount of urgency. You may be thinking that a sleep disorder can be cured with an extra cup of coffee in the morning or an energy drink for lunch, but the issues extend far beyond a little extra drowsiness in your day-to-day life.
Not only can a sleeping disorder sap your energy, but it’s a risk factor for many different life-threatening illnesses as well. According to the Mayo Clinic, complications of obstructive sleep apnea (OSA) include high blood pressure, heart problems, metabolic syndrome, and liver problems.
Furthermore, a medical report published in the Journal of Clinical Sleep Medicine states that sleep apnea increases the risk of heart failure by 140 percent and the risk of stroke by 60 percent. What’s more, it states that obesity is by far the most significant risk factor with about 60 to 90 percent of sleep apnea patients being obese. Other risk factors include cigarette smoking, alcohol consumption, and diabetes mellitus.

Knowing this information, it’s not hard to see how sleep disorders are a much more serious condition than most people realize. While it may only manifest itself with minor symptoms in your daily life, its impact on your long-term health is far worse. It can also contribute to other unhealthy lifestyle choices such as a poor diet or exercise routine, so it’s important to seek out appropriate treatment options.
What is Continuous Positive Airway Pressure (CPAP)?
Continuous positive airway pressure is a therapy that is used to treat obstructive sleep apnea. It’s considered the first non-invasive treatment because, prior to the 1980s, the only effective treatment for OSA was tracheostomy, a surgical procedure that involves making an incision into the trachea in order to bypass an obstructed airway.

The first CPAP machine was invented by Dr. Colin Sullivan in 1981. It works by administering a gentle stream of pressurized air through oxygen tubing that’s connected to the patient’s nose. At night, the patient can breathe freely while the pressurized air prevents the throat from closing up during sleep. Although modern CPAP machines use the same principles as the one created in 1981, they are much quieter and more comfortable, allowing the patient to get a better night’s sleep.
One important thing to note is that CPAP is not the same thing as oxygen therapy. While CPAP does blow air into the nose, it uses ambient air including oxygen, nitrogen, and all the other gases that we normally breathe rather than medical grade oxygen. The sole purpose of CPAP therapy is to keep the airways open while you sleep.

While CPAP machines deliver constant pressure, this pressure can be changed when you aren’t using the device. All CPAP devices use the measurement centimeters of water (cmH20) which is the same unit that lung pressure is measured in. Most patients require between 6 and 14 cmH20 and the average setting is 10 cmH20, however, the setting you use will depend entirely on your condition and the setting that your doctor prescribes. It’s also important to note that every CPAP machine has different capabilities, so you’ll want to make sure it meets your needs before purchasing it.
What is Bilevel Positive Airway Pressure (BiPAP)?
Although CPAP is still the most widely used PAP therapy device to this day, one of the major complaints about it is that it’s difficult to exhale against the air put out by the device. This typically isn’t a problem for someone with healthy lungs, but if you suffer from a low FEV1/FVC ratio, this could be a different story. In simple terms, FEV1/FVC ratio measures your lungs’ ability to exhale effectively. Low FEV1/FVC is often a sign of obstructive lung diseases like chronic bronchitis or emphysema.

BiPAP or Bilevel positive airways pressure is an alternative to CPAP which has two different pressure settings: one for inhalation (inspiratory positive airways pressure) and one for exhalation (expiratory positive airway pressure). The BiPAP machine will automatically detect whether you’re inhaling or exhaling and administer the pressure accordingly. Typically, a higher pressure will be applied when you’re inhaling.
CPAP With C-Flex versus BiPAP
Many people get confused when they hear about C-Flex which is a special feature that comes with some newer CPAP machines. This setting will help decrease the expiratory pressure by up to 3 cmH20. So, in other words, it’s more of a comfort feature that doesn’t completely eliminate the expiratory pressure. On some devices, this feature is called “expiratory pressure relief” or “EPR” for short.
What is Automatic Positive Airway Pressure (APAP)?
APAP is the third and final category of positive airway pressure device. Unlike CPAP and BiPAP, APAP machines automatically adjust airway pressure depending on what is needed at any given time. For example, if the APAP machine detects that your airways have closed, it will increase the pressure to open them up. Similarly, it can detect other episodes like hypopnea (slow and shallow breathing), flow limitation (when an increase in esophageal pressure is not accompanied by a flow increase), or snoring which can also disrupt sleep.
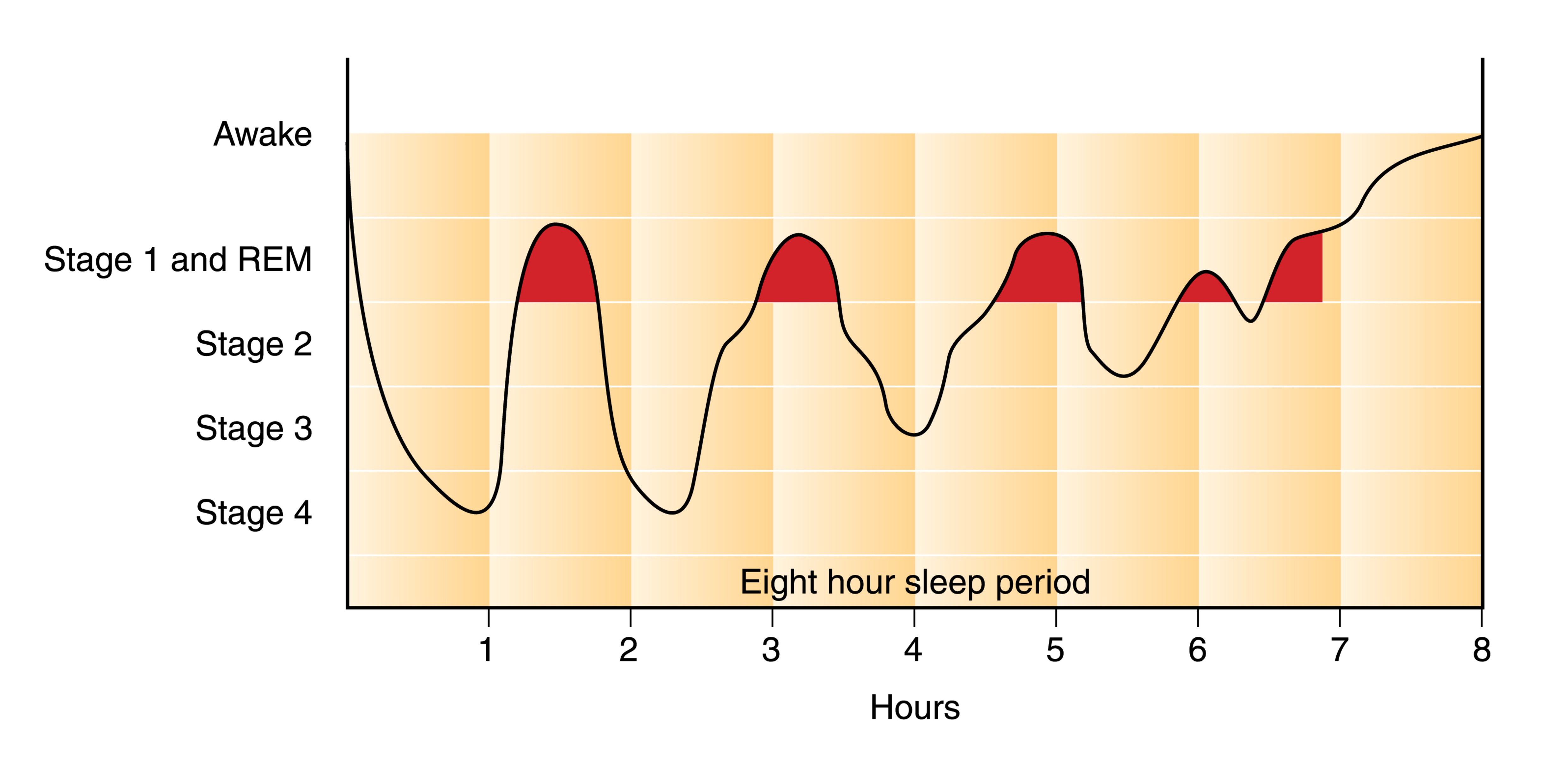
One of the obvious benefits of APAP is that it’s significantly more adaptable than CPAP or BiPAP. It contains a lot more technology and as a result, it’s often better for treating complex sleep apnea conditions. One complex form of apnea, REM-related obstructive sleep apnea occurs specifically during the rapid eye movement (REM) phase of sleep.
Another type of apnea that can be remedied with APAP is positional apnea. This is when your apneic episodes can be attributed to one or more specific sleeping positions. If you tend to move around a lot at night, the APAP machine will recognize this and adjust accordingly.
What is Supplemental Oxygen Therapy?
While supplemental oxygen therapy is often confused with CPAP, BiPAP, and APAP, it is an entirely different therapy that is used to treat respiratory conditions rather than sleep disorders. Oxygen therapy is the administration of medical grade (high purity) oxygen via a nasal cannula. Oxygen therapy ensures the lungs are fully saturated so that a patient can maintain oxygen levels in their blood.

Most commonly, oxygen therapy is used to treat chronic obstructive pulmonary disease (COPD). This is an umbrella term used to describe two different chronic diseases: emphysema and chronic bronchitis. Emphysema is characterized by swollen and damaged alveoli. These are the small air sacs in the lungs that are responsible for the transfer of oxygen and carbon dioxide to and from the blood. Chronic bronchitis is characterized by inflamed and swollen bronchial tubes, the small airways in the lungs.
COPD is one of the most common progressive lung diseases in the world, affecting an estimated 328 million people. Although it’s primarily caused by cigarette smoking, some people contract COPD due to a rare condition called alpha-1 antitrypsin deficiency. COPD is characterized by a chronic cough, chest pain, increased phlegm and sputum production, and exercise intolerance.

Depending on the severity of COPD that a patient has, they will need different flow rates of oxygen. Supplemental oxygen is measured in either liters per minute (LPM) or milliliters per minute (ml/min) depending on the oxygen device that is being used.
What Kind of Oxygen Devices Are There?
There are several different types of oxygen device: oxygen tanks, liquid oxygen tanks, stationary oxygen concentrators, and portable oxygen concentrators. Oxygen tanks are the oldest type of oxygen therapy and they work by storing oxygen at high pressures inside of an aluminum tank. Liquid oxygen tanks are similar to regular oxygen tanks but they’re stored in liquid form meaning they need to be kept at very low temperatures.

Oxygen concentrators are electronic oxygen therapy devices that take in ambient air and remove unnecessary gases like nitrogen and argon, then it puts out medical grade oxygen through a nasal cannula. Stationary oxygen concentrators need to be plugged into a wall outlet at all times but portable oxygen concentrators run off lightweight batteries that can be taken anywhere.
Pulse Dose versus Continuous Flow
There are two different delivery methods for oxygen: continuous flow and pulse flow. The best way to think of these is like the difference between a drinking fountain and a water bottle. Drinking fountains are like continuous flow oxygen concentrators because they put out a constant stream of water irrespective of how much you drink. On the other hand, pulse flow concentrators are like water bottles because you’re drinking all of the water that comes out of the bottle.

Pulse dose oxygen concentrators are more advanced than their continuous flow counterparts because they are able to detect your breathing rate and deliver oxygen at the right moment similar to how an APAP machine changes the pressure in your airways based on your breathing and sleep patterns. However, in certain situations, your doctor may advise you to only use continuous flow oxygen machines. One of the best pulse flow portable oxygen concentrators currently available is the Caire FreeStyle Comfort and one of the best continuous flow portable oxygen concentrators is the Respironics SimplyGo.
How are PAP Therapy and Supplemental Oxygen Therapy Related?
Although PAP therapy and oxygen therapy are used to treat entirely different diseases, that doesn’t mean that they aren’t related. Both therapies are used to improve breathing and to promote lung health as well as general well-being. And in certain situations, you may need to use both CPAP and oxygen therapy at the same time.
What is COPD-OSA Overlap Syndrome?
Just like the name suggests, COPD-OSA overlap syndrome is when symptoms of both COPD and OSA are present. In other words, a patient can have both damaged lungs and airways that collapse during sleep. As you can imagine, this is a pretty bad combination and it can lead to a lot of complications when it comes to getting a good night’s sleep.

There is no evidence to suggest that OSA causes COPD or vice versa, but a COPD patient who is obese or smokes will be at a higher risk of also contracting OSA. It’s important to remember that COPD is an “obstructive” lung disease, not a “restrictive” lung disease. What this means is that it affects the lung’s ability to expel air rather than inspire air. This is why COPD patients with OSA will likely be prescribed an APAP machine rather than a CPAP machine because it doesn’t add any unnecessary strain on their lungs when they expel air.
They Both Require a Prescription
Another similarity between oxygen therapy and PAP therapy is that they both require a prescription. Under the U.S. Food and Drug Administration, CPAP, BiPAP, and APAP machines are considered “Class II Medical Devices.” This means that these devices have potential risks and you’ll need a prescription to purchase one.

Similarly, oxygen is considered a controlled substance by the FDA, and as such, any device that puts out high purity or medical grade oxygen is regulated. If you decide to purchase an oxygen tank, liquid oxygen tank, stationary or portable oxygen concentrator, you will need to provide a prescription from your doctor.
How to Connect an Oxygen Machine to CPAP
If you have COPD-OSA overlap syndrome, you may need to use both oxygen therapy and PAP therapy at the same time. If this is the case, you’ll need to make sure that your PAP device and oxygen device are compatible. Most CPAP machines are compatible with oxygen machines, but you’ll need to make sure you have a continuous flow oxygen concentrator. Pulse dose concentrators like the Inogen One G5 rely on your breathing to deliver oxygen correctly and CPAP will mess with this.

Your oxygen tubing will connect to the CPAP between the mask and the input valve, but if there is no place to connect them, then you will need to purchase an oxygen bleed adapter. Once the devices are connected you should make sure both devices are on before you go to sleep at night. If your nasal passages get dry while using both the CPAP machine and oxygen machine, you can typically purchase a humidifier for either unit that will allow you to sleep more comfortably.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Conclusion
Although CPAP therapy and oxygen therapy are commonly confused, they are not the same thing. CPAP, BiPAP, and APAP are used to treat obstructive sleep apnea, one of the leading sleep disorders in the country. Oxygen therapy, on the other hand, is used to treat COPD and other chronic respiratory diseases.
However, under certain conditions such as COPD-OSA overlap syndrome, your doctor may advise you to use both of these therapies. It can be confusing trying to pick out the right CPAP machine or oxygen concentrator, especially if you want to ensure that they’re compatible with each other. To make this process as easy as possible, reach out to our respiratory specialists here at LPT Medical and we’ll walk you through it and get you the exact device you’re looking for.
Even though COPD is a chronic respiratory disease, its effects aren't limited to your lungs and airways. COPD can affect many parts of the body over time and lead to a variety of complications.
If you have COPD, then you are probably concerned about what kinds of health problems the disease can cause and how you can protect yourself from them. The good news is that, by effectively managing your symptoms and living a healthy lifestyle, you can significantly reduce your risk for a variety of COPD complications.
While you cannot stop COPD from progressing altogether, you can make choices that slow the rate at which your symptoms become more serious. By doing so, you reduce your likelihood of developing more serious health complications that result from reduced lung function and the other effects of COPD.
In this article we're going to give you a thorough overview of some of the most common COPD complications and show you how you can prevent them. We'll also explain how each of these complications is treated so you will know what your options are if you happen to develop any of these conditions.
Here are some of the most common complications of COPD:
- Exacerbations
- Pneumonia
- Collapsed Lung (Pneumothorax)
- Osteoporosis
- Hypoxemia & Hypoxia
- Sleep Apnea
- Heart Complications
Most of these conditions are serious and can lead to more health problems, a severely reduced quality of life, or even death over time. By learning the risk factors and causes of potential COPD complications, you can make better decisions about your health and lifestyle that can protect you from these unpleasant and potentially life-threatening conditions.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Exacerbations

Perhaps the most common complication that COPD patients experience is a COPD exacerbation. Exacerbations happen when your COPD symptoms get noticeably worse than normal for an extended period of time.
More serious than a minor flare-up, an exacerbation can cause worsened symptoms that last for days or even weeks. Some exacerbations can be treated at home, while more serious exacerbations require medical attention or even extended hospitalization.
COPD exacerbations are most often caused by illnesses and infections, but they can also be caused by asthma, allergies, or exposure to respiratory irritants. Even a minor sickness, like a cold, can cause someone with COPD to end up with a nasty, prolonged exacerbation.
Unfortunately, one side effect of COPD is that it depresses your immune system and makes it more difficult for your lungs to fight off viruses and bacteria. That means COPD patients are especially prone to getting sick, especially with respiratory illnesses, and have a constant risk of experiencing an exacerbation.
The first sign of an exacerbation is a minor up-tick in symptoms like coughing, wheezing, breathlessness, and fatigue. If these symptoms don't quickly get better on their own, then you are likely experiencing an exacerbation.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Common Symptoms of a COPD Exacerbation:
- Irregular breathing
- Worsened coughing
- Worsened breathlessness
- Noisy breathing (wheezing or rattling may indicate fluid in your lungs)
- Increased mucus in your airways and coughing up phlegm
- Reduced appetite
- Fatigue
- Fever
- Increased difficulty sleeping
- Signs of low blood oxygen levels, including: morning headaches, swollen ankles or legs, a bluish tint to your skin or nails, or an inability to speak or catch your breath
How to Prevent a COPD Exacerbation

The best way to prevent an exacerbation is to avoid getting sick and protect your lungs from respiratory irritants like allergens and pollution. That's why it's so important for people with COPD to wash their hands, keep up with vaccinations, and avoid exposure to germs and sick people, especially during cold and flu season.
Here are some of the best ways to prevent a COPD exacerbation:
-
Stop smoking.
-
Drink plenty of fluids. This helps thin your mucus, preventing it from building up in your airways and harboring viruses and bacteria.
-
Avoid large crowds and busy public spaces during cold and flu season.
-
Wash your hands often and use hand sanitizer when you don't have access to a sink.
-
Always follow your COPD treatment plan carefully, especially when your symptoms flare up.
-
Don't skip or miss any doses of your prescribed medications.
-
Make sure you've received all your recommended vaccinations, including the pneumococcal vaccine and a yearly flu shot.
-
Eat a healthy diet and get plenty of sleep to keep your body and immune system in top shape.
- If you are prescribed supplemental oxygen, always use it as directed.
The next best thing from prevention is early treatment and management to prevent illnesses and exacerbations from getting worse. Because of this, learning to recognize the early warning signs of an exacerbation is a vital skill for anyone who has COPD.
If an exacerbation isn't quickly managed and kept under control, it can cause a permanent damage to your lungs and a permanent worsening of COPD symptoms. However, exacerbations are sometimes difficult to detect when you experience COPD symptoms daily.
This is why it's so important to pay careful attention to your body and look out for times that your symptoms get worse or more frequent than they are on a normal day.
When you notice your symptoms become elevated above your usual baseline for more than a short period of time, you should consult your doctor and your treatment plan for what to do next.
In the most serious cases, severe exacerbations can cause life-threatening complications, like pneumonia, a collapsed lung, or even respiratory failure and death. Because of this, preventing COPD exacerbations is one of the primary goals of COPD treatment.
How to Treat a COPD Exacerbation
How you treat an exacerbation depends on its severity and your unique medical condition. If you have COPD, you should already have a detailed treatment plan from your doctor that includes what medications to take when your symptoms flare up and when to call your doctor.
As soon as you notice the signs or symptoms of a COPD exacerbation, you should immediately consult the instructions laid out in your COPD treatment plan. You may need to use your inhaler more often, reduce your activity levels, or start taking a course of steroids or antibiotics.
One of the most important things to note in your COPD treatment plan is how long you should wait before consulting your doctor or seeking medical attention. The guidelines outlined in your plan should tell you when your symptoms are bad enough to warrant medical attention and how to recognize an emergency.
Here are some general guidelines for managing a COPD exacerbation:
-
Use airway clearance techniques (like huff coughing and chest percussion) to clear excess mucus out of your lungs and airways.
-
Your may need to increase how often you use your short-acting bronchodilators to manage your symptoms effectively.
-
Your doctor may put you on a short course of corticosteroid medications to help decrease inflammation and reduce the chances of more serious complications.
-
Your doctor may prescribe you antibiotics to help you recover and reduce the chances of a secondary infection and further complications.
- Get plenty of rest and drink plenty of fluids.
As we've discussed, early detection and treatment for exacerbations is key for maintaining your health and quality of life with COPD. That's why you should always be monitoring your symptoms and paying special attention to how you feel. Then, when something goes wrong, you will notice right away and be able to begin treatment as early as possible.
Pneumonia

Another common COPD complication is pneumonia, a respiratory infection that causes severe inflammation in the lungs. Pneumonia can be caused by a variety of things, including bacteria, viruses, and fungi, and is particularly dangerous for people with COPD.
Pneumonia often occurs as a secondary infection that happens as a result of another illness, like a cold or (most often) the flu. The symptoms of COPD put patients with the disease at a higher risk for pneumonia because of symptoms like thick, excess mucus, a weakened immune system, and frequent upper respiratory infections.
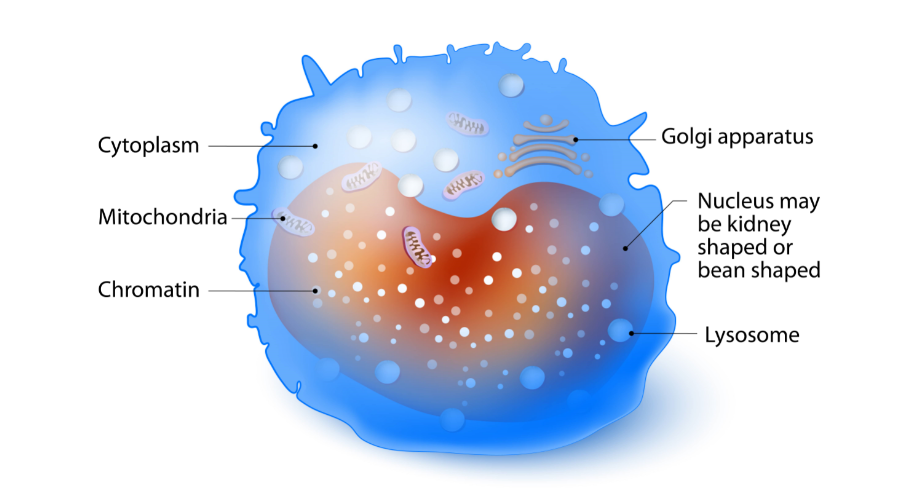
Pneumonia occurs when the lungs become so inflamed that fluid and pus collect in the lungs. This fluid fills up many of the lung's air sacs, preventing them from absorbing oxygen and transferring it to your blood.
With many alveoli incapacitated, your lungs' have difficulty absorbing enough oxygen with its remaining functional alveoli. For people with COPD, whose lungs have already sustained damage and struggle to absorb enough oxygen, this can severely limit airflow and cause permanent damage to their lungs.
Pneumonia is most commonly diagnosed with a physical exam and chest x-ray. Your doctor may also test a sample of fluid or mucus from your lungs to determine exactly what kind of bacteria, fungus, or virus is causing your illness.
Here are some of the most common symptoms of pneumonia:
- High fever
- Shaking
- Chills
- Fatigue
- Worsened chest pain
- Worsened shortness of breath
- Worsened cough
- Headache and body aches
Although relatively common, pneumonia is not a disease to take lightly; it normally takes up to three weeks to recover and as many as twenty percent of pneumonia cases (about 1 million people each year) require hospitalization. Also, people with COPD who contract pneumonia are at a much higher risk for life-threatening respiratory symptoms such as hypoxia and potentially fatal respiratory failure.
Pneumonia can also lead to other complications, including hypoxemia, sepsis, pleural effusion (fluid in the chest or lungs), respiratory failure, and death. Older adults above the age of 65 and people who have lung diseases like COPD are more prone to contracting and experiencing serious complications from pneumonia.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
How to Prevent Pneumonia
You can lower your risk of contracting pneumonia by avoiding getting sick and treating respiratory illnesses promptly and aggressively. However, the best first line of defense against pneumonia is vaccination.
While not 100% effective, the pneumococcal vaccine protects at least 45 out of 100 older adults from pneumococcal pneumonia. Most people in the US receive the pneumococcal vaccine as children. However, a second dose is usually recommended for people who smoke or who are over the age of 64.
How to Treat Pneumonia

Treatment for pneumonia depends on its cause and how serious the symptoms are. Viral pneumonia can sometimes be treated with antiviral medicine, while fungal and bacterial pneumonia are treated with anti-fungal and antibiotic medications, respectively.
Along with antibiotics, anti-viral, and anti-fungal drugs, rest and home care is often enough to support recovery from pneumonia. Recovery can take time, and until you feel better you should take a break from daily chores and responsibilities and give yourself plenty of time to rest.
Drinking plenty of fluids is also important, because it helps thin and loosen up the mucus so it's easier to cough phlegm up and out of your lungs. It's usually fine to take asprin or NSAIDs for a fever, but you should avoid cough suppressants since coughing to clear the phlegm from your lungs is important for recovery.
If your symptoms are severe, you may need to receive treatment in a hospital until you recover. There, you may receive more targeted antibiotic treatments, supplemental oxygen, intravenous fluids, and general medical support. If your condition is very severe, you may need more intensive treatments in an intensive care unit and breathing support through a ventilator.
You are more likely to require hospitalization if you have one or more of the following conditions:
- You are over the age of 65.
- You have other health problems or chronic diseases like asthma, diabetes, or COPD.
- Your blood oxygen levels drop too low.
- You are so ill that you cannot eat or care for yourself.
- You have severe chest pain.
- You are unable to cough up mucus and clear your lungs on your own.
- You are unable to eat or keep food or fluids down.
- Your pneumonia is not getting better with normal treatment at home.
Collapsed Lung (Pneumothorax)
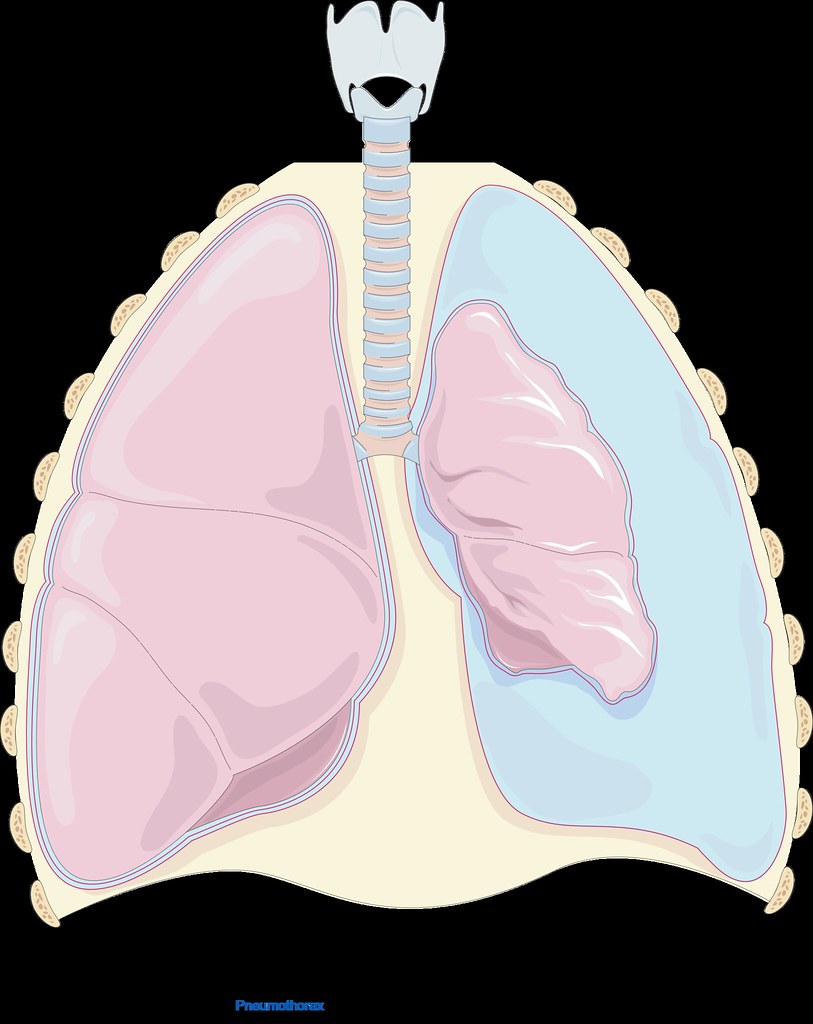
Lungs damaged by COPD are more prone to collapsing because the damaged tissue can leak air into the open space in between your lungs and your chest wall (your chest cavity). The pressure that the trapped air puts on your lung can cause your lung to collapse (also known as pneumothorax).
A collapsed lung can happen suddenly and spontaneously, without any warning. It is usually accompanied by sudden, sharp pain in the chest and worsened shortness of breath.
Pneumothorax is more common in patients with COPD because damaged, weakened lung tissue is both more likely to leak air and more likely to collapse under pressure. A collapsed lung is a medical emergency, especially for patients with COPD whose lung function is poor. If one lung collapses, the other lung may be unable to supply the body with enough oxygen, causing severe hypoxemia or hypoxia.
Here are some of the most common symptoms of a collapsed lung:
- Sudden chest pain (often described as sharp or stabbing)
- Shortness of breath
- Difficulty breathing
- Rapid breathing
- Rapid heart rate
- Coughing
- Bluish tint to the skin
How to Prevent a Collapsed Lung
The first step to preventing a collapsed lung is always to quit smoking. Smoking is one of the greatest risk factors for pneumothorax and quitting can significantly decrease your risk.
The more advanced your COPD, the more likely you are to experience a collapsed lung. That means that the next best way to prevent a collapsed lung is to follow your COPD treatment plan.
If you manage your COPD symptoms well and protect your lungs from further damage, your lungs will be less likely to leak air into your chest cavity and cause a collapsed lung. That's why it's so important to get regular check-ups from your doctor and follow the diet, exercise plan, and medication schedule that your doctor recommends.
How to Treat a Collapsed Lung
If you suspect that you might have a collapsed lung, you should go to a hospital immediately. A collapsed lung can sometimes be fatal without immediate medical attention.
At the hospital, you will likely receive treatment to remove the air in your chest cavity. This is usually done by inserting a small tube between the ribs and into the chest cavity to allow the trapped air to escape.
In some cases, if the collapse is minor, your lung may recover and re-inflate on its own. However, this determination must be made by a doctor and you should never try to treat a collapsed lung on your own at home.
Osteoporosis

Another complication that affects a large number of COPD patients is osteoporosis. Osteoporosis occurs when your bones become thin and brittle as a result of bone density loss, which significantly increases the risk of bone breaks and injuries.
Osteoporosis can be caused by a variety of factors related to COPD, including poor nutrition, lack of exercise, and increased inflammation throughout the body. All of these factors can result in a loss of bone density in patients with COPD; in fact, studies show that nearly seventy percent of all people with COPD have osteoporosis or at least some level of bone density loss.
Many people with COPD, for example, struggle to maintain a healthy weight and get enough nutrients from their diet. This is in part because people with COPD need extra calories and nutrients to support their over-strained lungs, and in part because COPD symptoms like breathlessness interfere with their ability to eat.
This causes some patients to lose weight and become malnourished, resulting in dangerous nutrient deficiencies that lead to osteoporosis. If you fail to get enough calcium and vitamin C in your diet, your body can no longer strengthen and maintain your bones, and will even cannibalize your bones to get the calcium it needs for other bodily functions.
Lack of exercise, too, can lead to bone density loss and disfigurement of your skeleton. That's because your bones are living tissue, and your body is constantly breaking down bits of your bones and building them back up.
Your body balances this process based on the amount of activity and strain your bones experience, taking density away from bones that are used less often and adding density to the bones that experience the most wear and tear.
When you stop exercising, your body takes bone density away from important bones in your limbs and other places in your body that you aren't using much. This leads to osteoporosis and changes to your skeletal structure so that it becomes even more difficult to stay active and avoid injury.
Finally, COPD patients have other characteristics that put them at a heightened risk of osteoporosis. People with COPD tend to be older, have a history of smoking, and use corticosteroid medications to treat their disease. All of these characteristics are also risk factors for osteoporosis and contribute the high incidence of bone density loss in patients with COPD.
Osteoporosis can be dangerous, painful, and interfere with your ability to exercise and stay active. It can cause even minor bumps and falls to bruise and fracture your bones, and recovery can take much longer than normal.
Here are some of the most common symptoms of osteoporosis:
- Bones that fracture easily from minor injuries or falls
- Loss of height over time
- Stooped posture
- Back pain (often caused by a fractured or collapsed vertebra)
- Receding gums (from reduced bone density in your jaw)
- Weakened grip strength
- Weak and brittle fingernails
How to Prevent Osteoporosis

Quitting smoking is one of the most important things you can do to prevent your COPD from getting worse, and it can help prevent osteoporosis as well. Getting regular physical exercise is also necessary to keep your bones healthy and strong.
It's also important to maintain a healthy diet full of whole, nutritious foods. It's particularly important to ensure that you eat plenty of foods rich in calcium and vitamin D; this ensures your body has the building blocks it needs to build thick, strong bones.
Even though COPD symptoms like breathlessness and fatigue can make it difficult to live a healthy lifestyle, it's important to follow your diet and exercise treatment plan, even when it's hard. It's not only necessary for healthy bones, but for maintaining your muscle strength, lung function, and physical mobility with COPD.
If you are struggling to get enough physical activity or need some extra help managing you disease, talk to your doctor about joining a pulmonary rehabilitation class, where you can learn all about how to better manage your diet, exercise, medications, and daily life with COPD.
How to Treat Osteoporosis
Unfortunately, once you begin losing bone density, it is usually impossible to get it back. Once you have osteoporosis or the early stages of bone density loss, the only thing you can do is manage it and keep it from getting worse.
The good news is that it usually only takes adjusting your diet and increasing exercise to manage osteoporosis and prevent further damage to your bones. Your doctor might also prescribe you a bisphosphonate medication which reduces the rate at which your body naturally breaks down your bones.
Other things you can do to prevent worsening of osteoporosis is to stop smoking and avoid drinking excessive amount of alcohol, which can impair your body's ability to build and repair your bones. You may also need to take special measures to prevent falls that could result in serious injury, for example, taking a fall prevention class or removing fall hazards in and around your home.
COPD is a disease usually associated with smokers, which makes sense when smoking is the cause of approximately eighty to ninety percent of COPD cases. However, smoking is certainly not the only way you can get COPD, and there are many other lesser-known causes.
Being exposed to just about any kind of respiratory irritant over long periods of time can cause you to develop COPD. Things like dust, smog, mold, fine airborne particles, and toxic gases can result in serious lung and airway inflammation that, over the years, can cause COPD.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
People who suffer from certain diseases, such as asthma and alpha-1 antitrypsin deficiency, also have a greater risk of developing COPD. These diseases have the potential to cause permanent damage to your lungs, leading to breathing problems later in life.
Even if you develop COPD related to smoking, it is possible that smoking is not the sole cause. If you suffer from asthma, have a history of frequent respiratory infections, or had frequent exposure to other respiratory irritants, these factors could combine with the damage caused by smoking and result in COPD.
It's important to know that COPD has many different causes, and that not everyone who develops COPD is a current or former smoker. The risks of pollution, dust, and other respiratory irritants are very real, and they can cause people who have never smoked or touched tobacco to develop the disease.
If more people are informed about the non-smoking causes of COPD, then more people will have the knowledge they need to protect their lungs from respiratory irritants and make lung-healthy choices throughout their lives. This could not only prevent thousands of new cases of COPD, but could also foster more understanding and compassion for those who already suffer from the disease.
Characteristics that Raise Your Risk for COPD
One of the first things that crosses many people's minds when they get a COPD diagnosis is, “how did this happen?” or “why did this happen to me?” While you may not ever be able to answer that question definitively, understanding all the potential causes may help give you some insight and closure.
Aside from the diseases and respiratory irritants we've mentioned, there are other factors that can put you at risk for COPD. For a variety of different reasons, things like your age, sex, medical history, genetics, and other personal characteristics can increase your likelihood of developing COPD.
While these things may raise your risk of sustaining lung damage and developing COPD later in life, these are usually not direct causes of COPD. These factors in combination with exposure to other COPD causes (such as smoking or exposure to toxic gases) is what ultimately causes you to get COPD.
If you or a loved one is already suffering from COPD, then understanding the causes of the disease can help you prevent the existing COPD from getting worse. If you are lucky enough to be untouched by COPD, then knowing the causes can help you avoid taking risks that increase your chances for developing the disease.
COPD Results from Cumulative Lung Damage Over a Lifetime
There are many different causes of COPD, and many of them are preventable. That's why it's important to understand what they are and what you can do to avoid them.
But first, it's important to understand that COPD is caused by repeated, long-term exposure to things that irritate and damage your lungs. These irritants can be things like smoke, chemical fumes, and even simply dust, but what causes COPD is accumulated damage over time.
That's why there is often not just one culprit, but a collection of potential causes that leads someone to develop COPD. Because of this, preventing COPD is a matter of making hundreds or thousands of small, healthy choices and making an effort to avoid harmful substances throughout a lifetime.
For instance, sitting around a campfire on occasional camping trips is very unlikely to cause long-term damage to your lungs. However, sitting around a campfire every night for months at a time, or working a job that requires you to be around a fire for hours a day, could cause permanent lung damage and significantly raise your risk for developing COPD later in life.

In the following sections, we're going to take a closer look at some of the most common non-smoking causes of COPD. We'll cover everything from toxic substances and respiratory irritants to diseases that are known to damage your lungs and cause COPD.
As you read through these next sections, remember that a single exposure or even years of exposure to any of the risk factors below does not mean that you will develop COPD. It goes the other way, too; if you have COPD, the fact that you were exposed to one of these risk factors does not necessarily mean that it is what caused your disease.
COPD is a complex disease that is difficult to diagnose and it is often difficult to find the root cause of specific cases. The causes listed below are not definitive triggers for COPD, but rather risk factors that increase your likelihood for developing COPD in the future.
Causes of COPD: Exposure to Air Pollution

In the modern age, pollution is everywhere; it comes from your car, local businesses, industrial activity, and even appliances in your home. We all know that air pollution is unhealthy, but many people underestimate the damage it can do to your lungs.
What we usually think of as “air pollution” or “smog” is actually a mixture of a variety of harmful gases and particles that irritate your lungs when you breathe them in. These pollutants can destroy healthy lung tissue, cause chronic respiratory problems, and cause you to develop COPD over time.
Studies show that these environmental and indoor pollutants can cause serious damage and may play a larger role in COPD than previously thought. That's why it's important to know the common sources of air pollution and how to keep your lungs safe.
Local Air Quality
.jpg)
When most people think of air pollution, the first thing they think of is smog, or the smoky haze that often fills dense cities and industrial areas. While everyone knows that air pollution is bad for your health, many people underestimate the damage that breathing polluted air can have on your lungs over a lifetime.
Smog is made up of harmful gases and tiny airborne particles that get lodged deep in your lungs when you breathe. Over time, this can cause serious respiratory symptoms and permanent lung damage that results in COPD.
Here is an overview of some of the major respiratory irritants found in smog:
- Ozone gas
- Tiny airborne particles (from dust, smoke, and other sources)
- Volatile organic compounds (VOC's)
- Nitrogen oxides
- Sulphur dioxide
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
One of the most dangerous pollutants is ozone, which is created when fumes from cars, factories, and other sources react with sunlight in the earth's atmosphere. The ozone that forms then sinks to the ground, sometimes miles away from the original source of pollution.
Ozone is a very reactive, volatile gas that “aggressively attacks” healthy tissue when it enters your lungs. Even relatively small amounts of ozone can be dangerous, raising your risk of heart disease, stroke, and respiratory disorders like COPD.
People who live in areas like big cities that have poor outdoor air quality have a significant higher risk of COPD, lung cancer, and other respiratory disorders as a result. However, your local air quality is affected by a variety of different factors, including temperature and humidity, and it may vary significantly from day to day.
Smog is most common in urban areas with lots of traffic, commercial activity, or industrial pollution. However, things like forest fires and weather patterns can spread polluted air far away from its source.
To protect yourself from poor outdoor air quality, make sure you check your local air quality forecast on a regular basis, especially before spending an extended period of time outside. On days when pollution is high, try not to plan any outdoor activities, and close up your house to prevent your indoor air from becoming polluted as well.
For more tips on how to avoid the harmful gases and particles that pollute the air outdoors, check out our comprehensive guide on protecting your lungs from air pollution and smog.
Indoor Air Pollution
There are many different ways that the air in your home can get polluted, and most of them are avoidable. Things like smoke, particle pollution, and allergens like mold and pollen can all build up in your house and irritate your lungs when you spend time indoors.
Indoor pollution is an especially dangerous form of pollution because it collects in such a confined place and you get exposed to it for so many hours a day. If there are are any significant sources of pollution in your home, it can lead to serious lung damage and other health problems over time.
Appliances like stoves, gas-powered appliances, and fireplaces can also pose a problem if they aren't properly installed and maintained. That's why it's important to inspect your appliances regularly for malfunctions or improper venting and get them repaired promptly whenever you notice a problem.
It's also important to install enough smoke detectors and carbon monoxide detectors to detect harmful gases and smoke in every space in your house. To ensure your home is protected, it's important to keep them in good repair, which includes checking their batteries occasionally to make sure they still have charge.
The simplest ways to make sure your indoor air is healthy to breathe is to make sure your home is well-ventilated and free from mold, allergens, airway-irritating chemicals, and all forms of smoke. It's also important to keep all of your appliances maintained and avoid using fireplaces and wood-burning stoves as much as possible.
Here are some of the most common sources of indoor air pollution you should look out for:
- Stoves, heaters, fireplaces, and furnaces
- Small particulate matter (from dust and other sources)
- Secondhand smoke
- Carbon monoxide
- Allergens like pollen, dust mites, pet dander, bacteria, and mold
- Asbestos
- Radon
- Pesticides
For more practical tips, check out our comprehensive guide on how to improve the air quality in your home.
Wood-burning Stoves and Combustion Fumes

Using a wood-burning stove, fireplace, or furnace to heat your house is extremely risky because of the harm it can do to your lungs. Even when they are properly installed and vented, these appliances can still release harmful amounts of toxic chemicals and respiratory irritants into your home.
Wood smoke contains tiny particles that inflame your lungs when you breathe them in, which can lead to lung cancer and other breathing disorders like COPD with repeated exposure. Burning wood also releases toxic gases like carbon monoxide, nitrogen oxides, hydrocarbons, volatile organic compounds, formaldehyde, dioxins, acrolein, and more—all of which can damage your lungs and hurt your overall health.
Other common and oft-overlooked sources of combustion fumes include bonfires, fire pits, and BBQ grills. While these can be dangerous over a long period of time, you are unlikely to experience any long-term health effects from normal exposure; you are most at risk for COPD if you work around bonfires or grills for a living.

Burning wood or coal to heat your home is particularly dangerous because the fumes are contained indoors and present all day every day for extended periods of time. People who use a fireplace too often or rely on a wood-burning stove for heat are at serious risk for permanent lung damage and getting COPD later in life.
If you use a stove to heat your home, consider switching to a conventional gas or electric heating system for your house. If you do not have that option, there are special precautions you can take in order to reduce the amount of pollution that your stove leaks into your home.
Here are some tips to help you make your wood-burning stove more safe:
-
Use an EPA-certified wood-burning stove, furnace, or fireplace insert to reduce the amount of harmful fumes. This could reduce the pollution released into the air by up to 90% and make your wood go further, too. Check out this guide from the EPA's website to learn more about how to find a safer appliance for burning wood.
- Always use firewood that has been properly dried and seasoned because it produces much less smoke than wet wood. To be extra safe, you can check your wood by using a moisture meter, which you can find online or at some hardware and woodworking stores.
-
Always burn hardwoods instead of softwoods because they produce less smoke, burn slower, and make better firewood overall. To learn more about how to identify good firewood and soft versus hard types of wood, check out this helpful guide.
- Never burn wood that has been exposed to salt water or has been painted, processed, or treated with chemicals. That includes plywood, particle board, varnished wood, and trees exposed to pesticides.
-
Get your chimney, stove, and ventilation system inspected every year for build-up, leaks, and other problems. A blocked up chimney will cause more smoke to leak into your home and can even cause deadly fires and carbon monoxide poisoning.
- Don't use your wood-burning stove or furnace any longer than you need to. Turn it off when it is warm enough and do your best to keep your home insulated so you don't have to use it any more than necessary.
- Always make sure you have working smoke and carbon monoxide detectors installed all throughout your home. Always replace the batteries immediately when they go out and check them a couple times a year to ensure that they are functioning.
Even if you use an EPA-certified stove and follow all of the recommendations above, you could still be putting yourself and your family's health at risk by burning wood or coal in your home. For more information about the dangers of wood smoke, you can check out the Families for Clean Air website or this fantastic guide from the state of Washington's Department of Ecology.
Radon
Radon is a toxic, radioactive gas that seeps out of the ground and can be harmful to your lungs in large amounts. Because the gas is invisible and has no smell, the only way to detect it is to use a special radon detector.
Radon gas is most often associated with lung cancer, as it is the most frequent cause of lung cancer among people who don't smoke. However, many people don't realize that radon exposure can also damage the air sacs in your lungs, which can lead to respiratory problems and breathing disorders like COPD.
Children are more sensitive to radon than adults, even though the effects don't show up until much later in life. Smokers' lungs are also particularly sensitive to the damaging effects of radon, and a smoker's risk for lung cancer and COPD will be much higher than a non-smoker who is exposed to the same levels of radon gas.
Radon can be found anywhere, although levels vary significantly from place to place. Most people are exposed to radon when it leaks into their homes from the surrounding earth through their foundation or water pipes.
The best way to protect yourself from this toxic gas is to buy a radon testing kit or have a licensed radon inspector come to your home. It is also important to keep your home well-ventilated so that radon and other pollutants don't have a chance to build up to harmful levels indoors.
Because radon levels can fluctuate significantly over time in reaction to weather, seasons, and changes in the ground. Because of this, you have to monitor radon levels over several months or years in order to get an accurate picture of how much radon gas you get exposed to in your home.
Causes of COPD: Exposure to Dust, Chemicals, and Fumes
Besides common air pollutants, there are a variety of other substances that can irritate and damage your lungs. Things like cleaning chemicals, dust, and exhaust fumes can all cause COPD if you're exposed to them too often over a lifetime.
Workplace Exposure

There are many different jobs and occupations that can expose you to toxic chemicals, dust, and fumes that cause COPD. Because your job requires you to be around these harmful substances for dozens of hours a week, occupational exposure poses a substantially higher risk to your health than other forms of exposure.
Any job that exposes you to fine particles or noxious chemicals can put you at risk for COPD. Certain types of dust, including silica dust, mineral dust, coal ash, and dust from flour and grains are particularly dangerous for your lungs.
Here is a list of some of the harmful dusts and fumes found in workplaces that can do permanent damage to your lungs:
- Cadmium Dust
- Mineral Dust
- Silica Dust
- Organic Dusts
- Grain and Flour Dusts
- Cadmium Fumes
- Welding Fumes
- Petroleum and Diesel Exhaust Fumes
- Pesticides and Herbicides
Many of theses dusts and fumes come from vehicles, machinery, mining, materials, and manufacturing processes. Working in versatile fields like construction, manufacturing, and agriculture may expose you to several of these lung-irritant sources on a regular basis.
If you work in a high-risk occupation, you should take extra safety measures to protect your lungs. Make sure your workplace follows all the guidelines and requirements from the Occupational Safety and Health Administration (OSHA) and wear a dust mask or respirator around dust and machine fumes.

Even if you don't develop COPD, occupational exposure to lung irritants can cause a variety of other health problems. It may raise your risk for lung cancer, breathing problems, occupational asthma, and respiratory infections like pneumonia.
Here is a list of occupations that put you most at risk for COPD:
- Mining Workers
- Agriculture Workers
- Quarry Workers
- Brick-making
- Stonemasonry
- Rubber and Plastics Manufacturing
- Petroleum Workers
- Foundry Workers
- Dock Workers
- Cadmium Workers
- Welders
- Textile Workers
- Pottery and Ceramics Workers
Chronic obstructive pulmonary disease (COPD) is a disease that causes lung irritation and therefore challenges breathing.
According to the Centers for Disease Control and Prevention (CDC) it’s the fourth most common cause of death among people in the United States. Getting treatment and developing healthy lifestyle habits are essential to improving your quality of life with this condition.
In addition to breathing difficulties, coughing, and lack of energy, COPD can also lead to other weird symptoms that are not as commonly talked about. In this article we will talk about some of these symptoms and what you can do to relieve them.
Irritation, mood swings, and depression
It might not be your first connection when it comes to how COPD will affect your life, but your emotions play an important role in your breathing patterns and vice versa.
People with COPD will sometimes experience emotional problems that they previously didn’t have before they were diagnosed with COPD. They also may be found to have started having symptoms of depression not long before the COPD diagnosis that can be attributed to COPD because their diagnosis might be well after they actually started to have COPD. People who have anxiety or depression even before they have COPD are more at risk for having frequent and severe exacerbations. This is simply because emotions have a big impact on your breathing.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Some of the lifestyle changes and hardships that come with COPD can lead to feelings of loss, frustration, or sadness and if you can’t do the things you once did it is easy to get caught up in depression and anxious feelings. You may even experience a mood disorder that causes you to feel irritated and disinterested.
When you’re depressed, you can get stuck mourning life as you knew it before COPD. One study from The National Center for Biotechnology Information estimated that 40 percent of those with COPD suffer from depression.
So what can you do?
While the physical challenges are hard to face, it is the mental challenges of COPD that are hard to portray to caretakers and your loved ones. The best way to get better is to express your feelings and speak with a professional about how you can communicate these feelings better. You can also talk to your doctor about antidepressants and COPD.
If it is fitting, your doctor might want to prescribe a medication to help alleviate your depression. It’s crucial to find the right medication for you because many antidepressants can interfere with medications you may already take for your COPD.
Two medications that doctors prescribe for depression in people with COPD are sertraline (Zoloft) or citalopram (Celexa). Do not be discouraged if the medication does not work right away, It can take up to 8 weeks for an antidepressant to take full effect.

If you are trying to avoid taking additional medication, but are still suffering from depression, you might find relief by seeing a mental health specialist. You can learn from others in group therapy or find individual help with one on one therapy, both of which can help you learn how to cope with your disease and adapt to your life with COPD.
Ask your pulmonologist or primary care doctor for a reference for a well reviewed therapist who helps people in your particular condition or with similar backgrounds.
Support groups may also be beneficial for people with COPD who are experiencing depression. Being in a setting with others who are facing many of the same problems can help you feel less alone. You may discover some real life tips and advice for taking better care of yourself by talking to others. With the right combination of treatments and communication, you’ll be better able to cope with your COPD and your changing lifestyle.
A variety of online support groups are also available for people with COPD. You can simply search on Facebook “LPT Medical COPD & Respiratory Support Group” and find a community of people willing to help others with COPD. There are many other popular sites that have forums or discussion groups where members can share their feelings to an understanding group of peers.
Always remember that you aren’t the first person to feel this way and someone out there might have found a way of handling their emotions effectively. Taking the time to talk with someone from the comfort of your home can be a great first step to reaching out for help with depression.

How to manage showering
Showering with COPD can be very difficult and leave patients feeling exhausted just by simply standing in the water. Usually people use hot water to shower, and that humidity builds up creating a difficult breathing environment for yourself if you have COPD. You can also be exerting a lot of energy just standing for long periods of time in the heat, so your breathing will be affected by that.
So what can you do?
Here are a few suggestions to help conserve your strength and not become so short of breath while you shower.
1. Use a shower chair
If you have COPD it can take a lot of energy just to stand, bathe, and hold your arms above your head when washing your hair.
Using a shower stool can help you avoid exacerbating your condition. Sitting down alleviates the cost of energy you would exert by standing and bending over. By conserving energy, you are lowering the risk of injury from a fall or slip.
2. Keep a fan in the bathroom
Steam from a shower increases the humidity level in the room. This can also exacerbate COPD, triggering coughing and shortness of breath.
To avoid worsening symptoms, only shower in well-ventilated bathrooms either using a fan or keeping the door open or both. If you have a window in your bathroom you can keep that open as well.
You can also place a portable fan in the bathroom with the door open to ventilate the room, and minimize the humidity.
3. Use your portable oxygen concentrator in the shower

It is ok to use your oxygen in the shower, and it might make it so that you are able to handle the energy it takes to do so.
If you use a portable oxygen concentrator, make sure it is not plugged in to charge, and then you can always add an extension to the cannula tubing so that your concentrator does not get wet.
4. Take less hot showers
This one is easier said than done, because most people love a good hot shower, however this might be the reason you don't feel energized enough to take a shower comfortably.
The heat from the water creates steam so not only is the hot air harder to breath in, the humid steam also poses a lot of issues for people with trouble breathing.

Extreme or Sudden Weight Loss
Weight loss is a sign of severe COPD.
When the damage to your lungs becomes so severe your lung volume will expand in size, which leads to flattening your diaphragm, thereby reducing the amount of space between your lungs and stomach.
You might have noticed that before you were diagnosed with COPD, that you had lost a lot of weight without really doing anything. This is because people with COPD use more calories to breathe than people who don’t have the disease.
So, If you don’t know that you have COPD, this can be perplexing, especially if you’ve tried to gain the weight back and nothing works to do so. This can lead to feeling very run down and weak.
So what can you do?
Try not to eat too fast or eat certain foods that may trigger bloating or indigestion. Doing so can make it harder to breathe and being uncomfortable might discourage you from eating regular, healthy meals as well.
Try to avoid these common triggers:
- salty foods
- spicy foods
- fried foods
- high-fiber foods
- carbonated drinks
- caffeine

To increase your body weight while making sure you get the proper nutrients, it may help to:
- Eat small but frequent meals throughout the day
- Find ways to eat higher calorie foods, such as full-fat milk (“whole milk”) products instead of low fat milk products
- Reduce your intake of fluid during meals to allow more space in your stomach for food
- Drink more fluids in between meals
- Avoid foods and drinks that trigger bloating
- Eat while using oxygen treatments
- Rest before you eat
- In some cases, your doctor or dietitian may encourage you to add a nutritional supplement to your diet.
- Simplify your snacks and meals
- Find ways to prepare snacks and meals more easily might also help you meet your nutritional needs.

For example, you can reduce some of the physical work cooking involves by buying:
- Precut produce
- Microwaveable meals
- Other packaged products
- Cut back on sodium
- When you’re shopping for pre prepared or packaged food products, look for low-sodium options. Eating too much sodium causes your body to retain water, which puts more pressure on your lungs.
It is also important to pay attention to your mental health if you notice that you’ve lost weight around the same time that you’ve been experiencing feelings of depression, anxiety, or stress, consider asking your doctor about ways to improve your mental health.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Antidepressants and other treatments may help you manage your weight while improving your mood and outlook on life.
For more tips and support, your doctor may refer you to a registered dietitian or other specialist. A registered dietitian can help you develop ways to adjust your diet while coping with COPD.
Feet swelling
If you have COPD, you may develop peripheral edema (fluid retention), This causes swelling of the feet, ankles, and legs. This lower body swelling can limit your activity and can be very uncomfortable. It is also a sign of advancing COPD.
As COPD begins to negatively impact your lungs and heart, your blood circulation is eventually affected as well, which causes edema. There are other causes of edema, so you will need a medical evaluation to determine if it is caused by your COPD.

So what can you do?
Medications and lifestyle changes can help reduce leg edema, both of which we will discuss in detail. The important thing is that since edema is a sign that your COPD may be progressing, you might also need to adjust your COPD treatments, for example, your doctor may increase your oxygen therapy prescription.
If you have a hard time doing physical activity due to COPD, it can be difficult to distinguish edema from weight gain.
If you are experiencing lower body swelling from your COPD, fluid management is an important part of the treatment, and it involves lifestyle strategies as well as medication.
Medications that can help reduce edema include diuretic prescriptions, which trigger the elimination of fluid in the urine.
Other methods you should try to minimizing leg swelling include:

- Rest with your feet up: By lifting your feet up at the same level as your heart (or higher) you are reducing the blood flow into your legs which should bring down the swelling.
- Wear compression stockings: Supportive socks may also help bring down the swelling of blood in your feet and ankles. These can normally be purchased at any drugstore.
- Keep up with hydration: You must closely follow your doctor's instructions when it comes to fluids because your fluid intake can be tricky when you have COPD-associated leg edema. Drinking too much fluid can cause edema if your kidneys can't catch up with urine production and on the other hand not drinking enough water may also cause swelling if your kidneys retain excess fluid to prevent dehydration.
- Reduce salt: Your salt intake can influence the edema in your legs. Salt concentration managed by your kidneys, so too little or too much salt can result in swelling or dehydration.
- Get regular exercise: Staying active can help your lungs and heart function properly even if you have COPD it is important to maintain healthy circulation.
Oxygen therapy as treatment for COPD
When you start to get extra oxygen into your system while taking oxygen therapy it can help you have fewer intense bursts of being breathless.

It can also:
- Helps you to sleep better
- Increases your energy and ability to exercise
- Helps you focus
- Boosts your mood
- Improves sex
- Lowers your chance of heart failure (when your heart doesn’t pump enough blood to your body)
- Even prolongs your life expectancy
If your doctor prescribes you oxygen therapy at any point, it is crucial to work with a oxygen supply company that is a licensed distributer and has a dedicated team of experienced respiratory specialist that can connect you with a portable oxygen concentrator that fits into your life with ease.
Overview
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
There are a lot of other random feelings and discomforts that people can attribute to their COPD, and because this disease effects everyone differently, you might also experience something completely different than someone that is you same age and gender with COPD. Therefore, there is not one single treatment plan that works for everyone.
For the most part, the COPD diagnosis means a few things across the board. It is time to take control of your lifestyle, eat healthy foods and eat consistently to maintain a healthy weight, you should continue or start to exercise as much as possible, and you need to quit smoking if you do.
After you have incorporated these healthier lifestyle choices in your daily life, you might recognize other aspects of your life that you need to work on or you need help to mange. These weird symptoms in this article are just a few of the realities COPD patients face, and you might experience one, some, or none of these, but whatever you do, remember you are not alone and there are almost 30 million people in the United states alone with this incurable disease, however you can choose to live a well-balance life or not.
If your doctor prescribes you oxygen therapy at any point, it is crucial to work with a oxygen supply company that is a licensed distributer and has a dedicated team of experienced respiratory specialist that can connect you with a portable oxygen concentrator that fits into your life with ease.
.png)
No matter where you are or what you’re doing, you’re always being exposed to disease-causing pathogens. And while this may seem like a scary concept, you'll be happy to know that your immune system is working around the clock to fight off this bacteria and keep your body healthy. At least, that’s what it’s supposed to do…
Immunodeficiency, also called immune deficiency, is a state in which the body’s ability to fight infectious disease is compromised. Primary immune deficiency is one that’s inherited through genetic mutations while secondary, or acquired immune deficiency is one that’s caused by environmental factors, i.e., bacteria, viruses, or immunosuppressive drugs like cigarettes.
Recently, researchers have focused their sights on understanding the effect of chronic obstructive pulmonary disease (COPD) and other respiratory conditions on the immune system and what role the immune system plays in causing COPD. While COPD is not classified as an autoimmune disease (a disease that causes the immune system to attack the body), it’s still linked to the immune system in a number of ways. According to a study published in the American Thoracic Journal, COPD patients are more prone to respiratory infection and they’re less likely to recover from it than those without the disease.
While the correlation between immune deficiency and COPD is complex, it’s important for you to understand because it has a profound effect on your health and wellbeing. For most people, getting sick is just a part of life. However, for someone with COPD, getting sick could mean being at a higher risk for life-threatening exacerbations.
In the following sections, we’ll discuss how the immune system works, the various types of immune disorders, and most importantly, where COPD fits into all of this. Your pulmonologist and primary physician should be your first line of contact when it comes to improving and maintaining your immune system, so be sure to reach out to him/her if you have any questions or concerns.
How Does the Immune System Work?
Just like the name suggests, the ‘immune system’ isn’t one specific entity; it’s a whole host of processes that occur throughout the body that work in tandem to protect you from disease-causing microorganisms. In a healthy person, these processes are all running at full force and working together effectively as the body’s first line of defense.
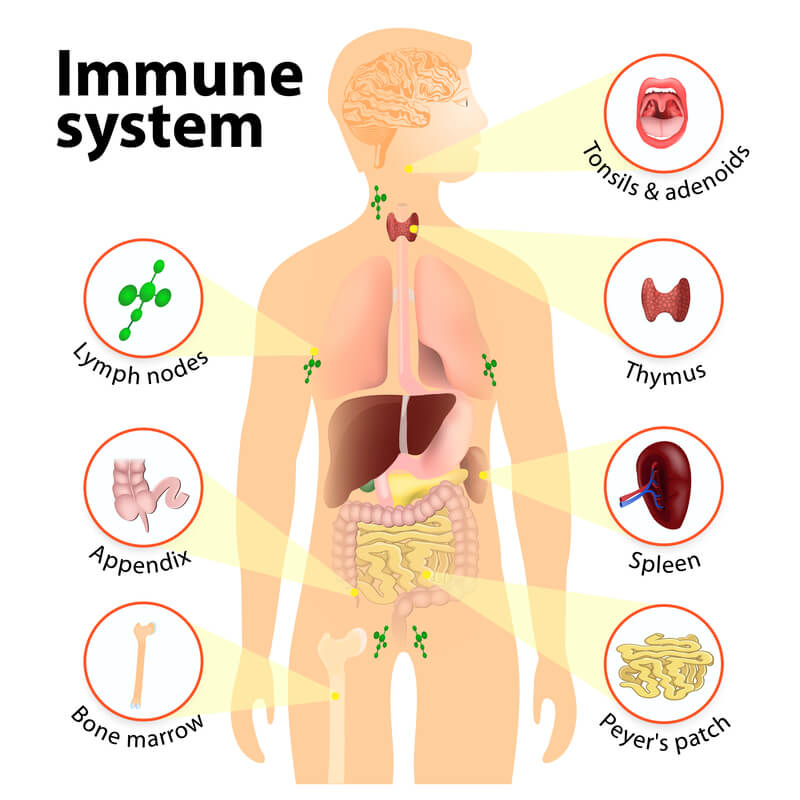
The immune system is one of the most complex parts of the body because it’s made up of a variety of different organs, cells, and proteins. There are three main tasks that the immune system is responsible for in the body:
-
Recognizing harmful substances in your environment and keeping them out of the body.
-
Neutralizing harmful pathogens inside the body such as parasites, fungi, viruses, and bacteria, then removing them.
- Fighting cancerous cells in the body.
Innate Immune System
All immune responses in the body can be divided into one of two different categories: innate or adaptive. The first of which, innate, is characterized by the body’s natural ability to fight harmful substances. Most of the components that make up you innate immune system are present at birth, but they can still develop and adapt over time.
Physical Barriers
While you may not think of your skin, eye lashes, and nose hair as part of the immune system, all of these are considered “physical barriers” and keep harmful substances from entering the body. The skin, for example, has a very low permeability, meaning it’s difficult for foreign substances to enter the body through it. However, other parts of the body like the mouth, nose, ears and eyes are open entry points to the rest of the body, this is why they need extra layers of immune protection.
Defense Mechanisms
Other innate immune responses in the body include things like saliva, mucous, tears, sweat, and secretions. Saliva, for example, plays an important role in managing bacteria in the mouth that causes gum disease. You may simply think of saliva as “water,” which is mostly what it is. However, saliva also contains a number of other substances like electrolytes, mucus, antibacterial compounds and various enzymes, all of which play a number of roles in protecting your oral health.

One important thing to note about your body’s natural defense mechanisms is that there’s a balance to all of it. When your body produces the ideal amount of saliva, mucous, tears, and sweat, you feel good. However, if something alters these processes, the defense mechanisms may be working against you. For example, smoking cigarettes results in high mucus production in the body. While mucus typically helps the body, too much of it can lead to airway obstruction and difficulty breathing.
Another way smoking affects the innate immune system is through the destruction of cilia. Cilia are tiny hair-like protuberances found in the lungs and wave back and forth to keep mucus and other substances out of the lungs. Smoking temporarily disables cilia, and long-term smoking can damage them meaning you’ll be more likely to get sick or experience difficulty breathing.
Inflammation
Inflammation is another key component of the innate immune response. Think of inflammation as a sort of signal that something is wrong. If you get an injury or an infection, inflammation occurs and white blood cells are sent to deal with the issue. Inflammation is a normal reactionary process for your body, but when it goes on for too long it may result in a chronic illness. What’s more, if inflammation never occurs, a seemingly harmless infection could become much more serious.
Adaptive Immune System
The adaptive immune system is your body’s ability to evolve and adjust based on its circumstances. Whenever you contract a disease, your adaptive immune system “remembers” it, making it much easier to fight off the next time it’s exposed to it. Unlike the innate immune system which reacts to general threats in the body, the adaptive immune system is activated when it’s exposed to pathogens. The adaptive immune system is also a lot slower to react than the innate immune system.
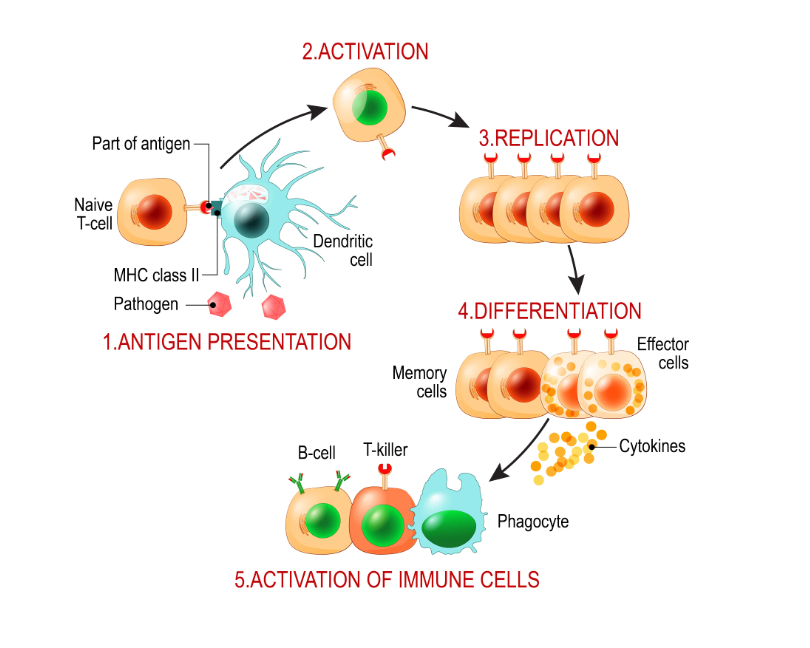
Self vs Non-Self Antigens
In order for the immune system to work effectively, it first needs to be able to differentiate between self and non-self substances, organs, and cells. Self-antigens are ones that originate in the body and should not be attacked while non-self antigens are foreign and can often cause harm to the body if they aren’t neutralized.
Your immune system is largely coordinated by white blood cells called lymphocytes. When these cells come across a non-self antigen in the blood, they produce something called an antibody that allows them to detect and bind to the antigen. After binding to the antigen, the antibody engulfs and digests it with macrophages through a process called phagocytosis.
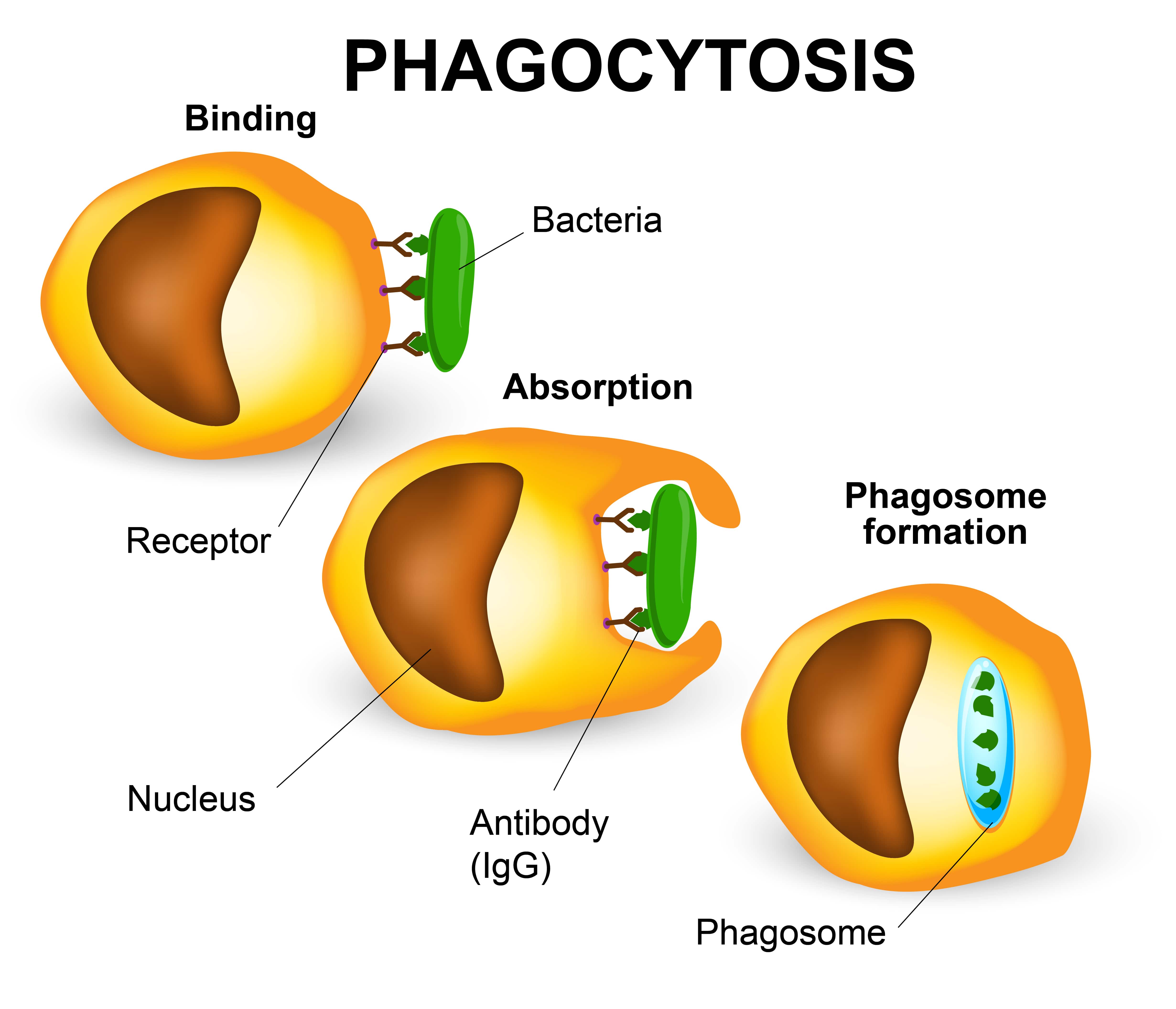
If the body has encountered a substance before, it may have stored “memory” cells that remember the microbe, allowing it to create an antibody more quickly. This is why people are less likely to contract a disease if they’ve already had it, because their immune system is better equipped to fight it off before it becomes a problem. However, an antibody that recognizes one antigen will not be able to recognize another.
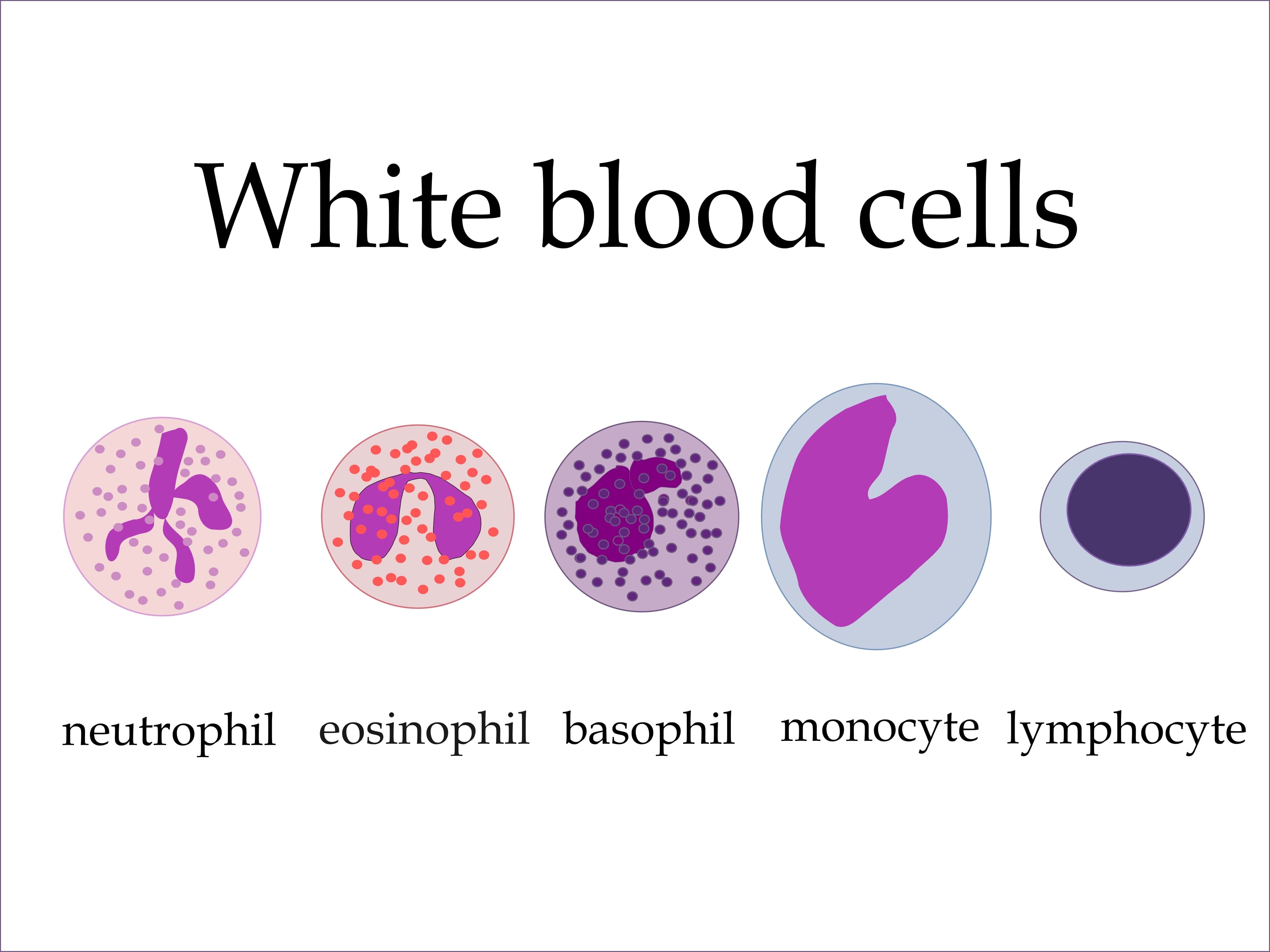 Types of White Blood Cells
Types of White Blood Cells
Lymphocytes
There are three different types of lymphocytes: T cells, B cells, and natural killer cells. T cells got their name because they’re produced in the thymus gland, a pinkish-gray organ in between the lungs. T cells are able to recognize foreign bodies and attach to them while ignoring self antigens.
B cells, produced in bone marrow, are another important type of lymphocyte. These cells have a protein on them called the B-cell receptor which generates the antibodies necessary to neutralize an antigen. B cells are part of the adaptive immune system because they develop when they’re introduced to a foreign substance.
NK cells, or natural killer cells, are the third type of lymphocyte. They got the name “natural” killers because they are part of the innate immune system. While T and B cells need to be primed by antigen presenting cells, NK cells have natural immune capabilities. NK cells are known for fighting cells that show early signs of cancer as well as virally infected cells.
Monocytes
Monocytes are the largest type of white blood cell. They’re produced in bone marrow like many leukocytes and become a macrophage when it travels to different tissues of the body via the bloodstream. These cells ingest foreign material, kill microorganisms, and remove dead cells.
Granulocytes
Basophils
Basophils are a type of white blood cell referred to as granulocytes. A granulocyte white blood cell secretes substances called granules that play an important role in the immune system. When basophils are exposed to an allergen, they release a compound called histamine that causes dilation of capillaries and the contraction of smooth muscles.
Neutrophils
Neutrophils are usually the first white blood cells to arrive at the sight of infection because there are more of them than any other type of immune cell. Neutrophils neutralize bacterial infections through either phagocytosis or endocytosis.
Eosinophils
These are proinflammatory cells that contain two different lobes and a cytoplasm that contains up to 200 granules. These granules contain proteins and enzymes that are needed to destroy foreign substances. While eosinophils play similar roles to other white blood cells, they also have a physiological role in the formation of organs such as the postgestational mammary gland.
Humoral vs. Cellular Immunity
Humoral and cellular immunity are the two main mechanisms within adaptive immunity. Humoral comes from the Latin word “humor” meaning “fluid” or “moisture.” So, humoral immunity refers to immune responses occurring within the body’s fluids, especially the blood. In humoral immunity, the antibody will destroy viruses through either immune cytolysis or phagocytosis.
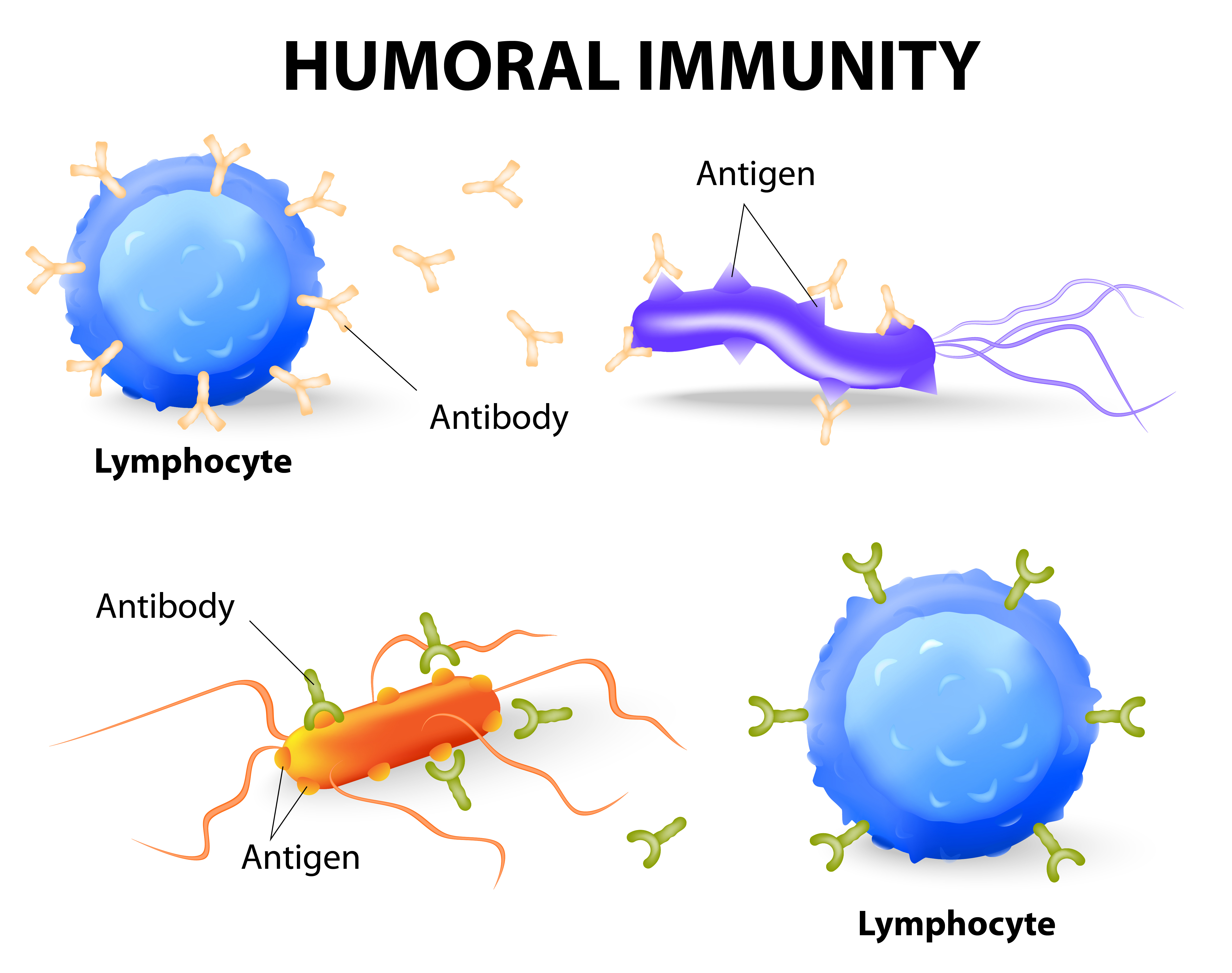
Unlike humoral immunity, cellular immunity does not use antibodies. Instead, phagocytes, antigen-specific cytotoxic T-lymphocytes, and cytokines are released in response to antigens. When there is a viral infection, cell-mediated immunity can help prevent it from spreading but also results in an inflammatory response which can damage vital tissues surrounding the virus, resulting in chronic disease.
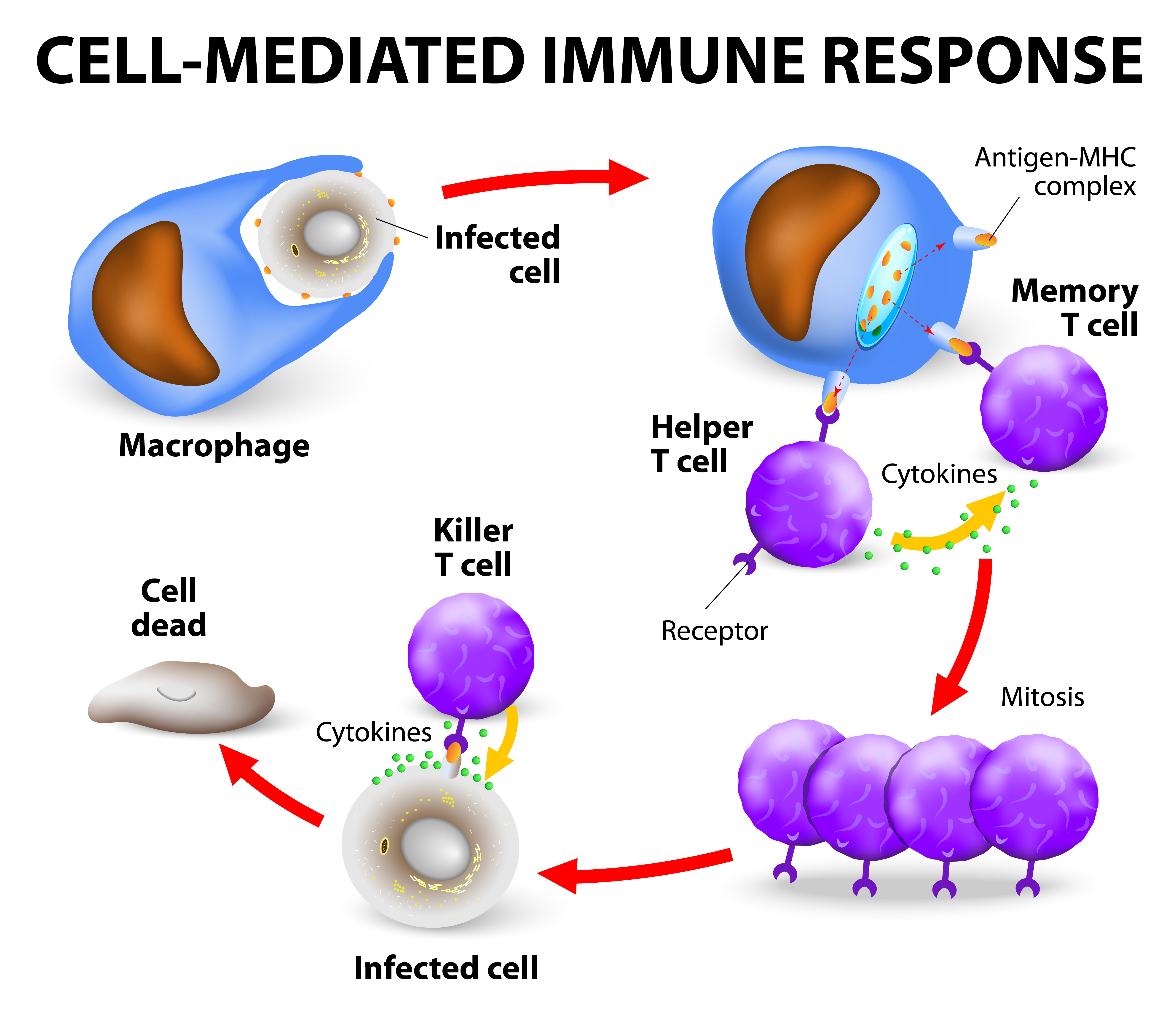
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Autoimmune Disease
An autoimmune disease is one that causes the immune system to be overactive and attack the body's tissues rather than pathogens or cancerous cells. Some autoimmune disease you may recognize include rheumatoid arthritis, multiple sclerosis, psoriasis, and vasculitis. There are more than 80 types of autoimmune disease, so it can be difficult to diagnose and differentiate each one.
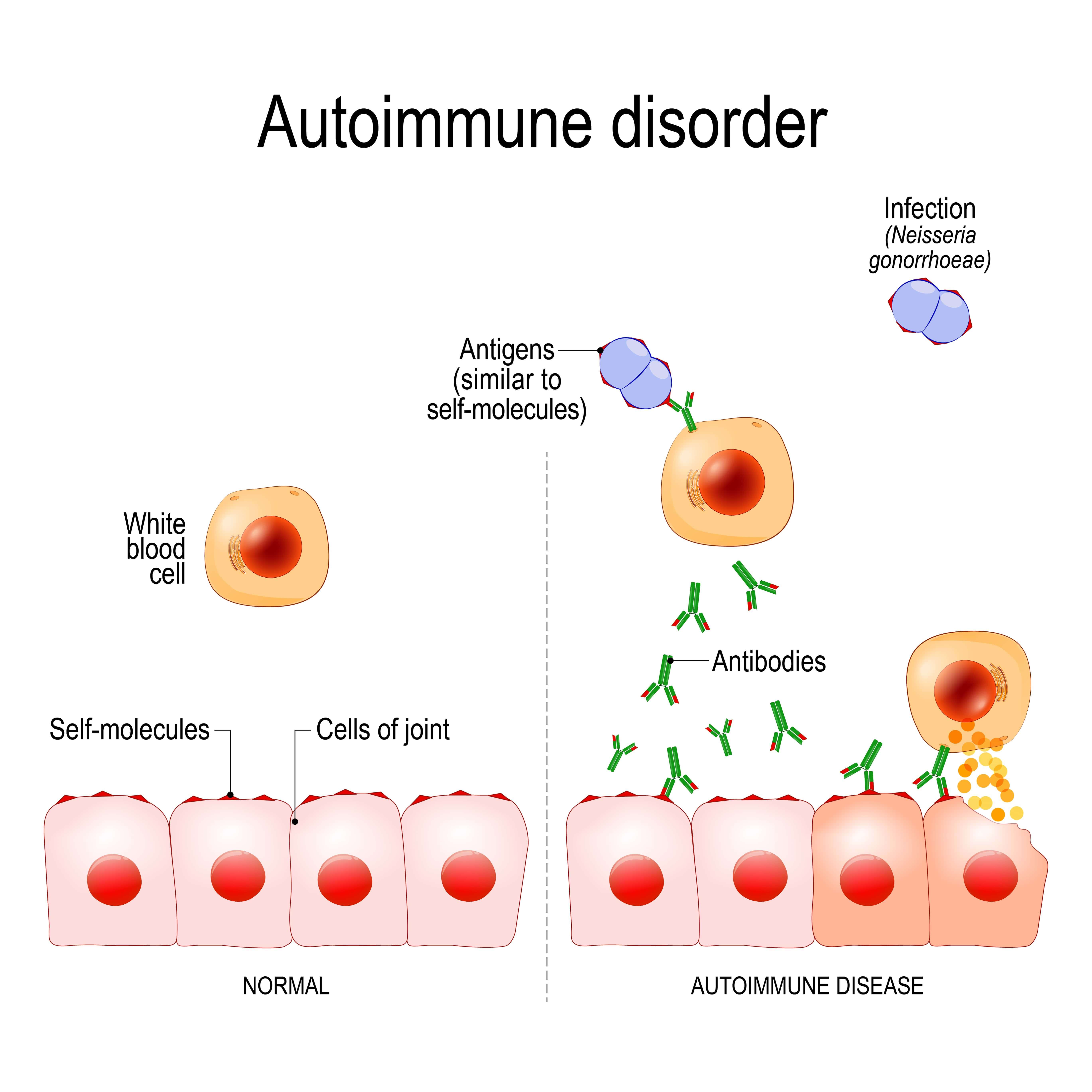
Because autoimmune diseases cause increased immune system activity, they're often characterized by inflammation in the body. When treating these diseases, the goal is usually to reduce inflammation and reduce immune system activity. Your doctor may prescribe corticosteroids or other steroids that can help with this.
COPD and The Immune System
You may recall from earlier that inflammation is one of the key functions of the innate immune system. When cigarette smoke or other airborne irritants enter the lungs, structural and inflammatory cells in the lung begin to release proinflammatory mediators. These mediators create an inflammatory microenvironment that damages the lungs and leaves the immune system in a state of disrepair. Many researchers have found that this lung state leads to more frequent and severe respiratory infection as well as a host of problems throughout the body.
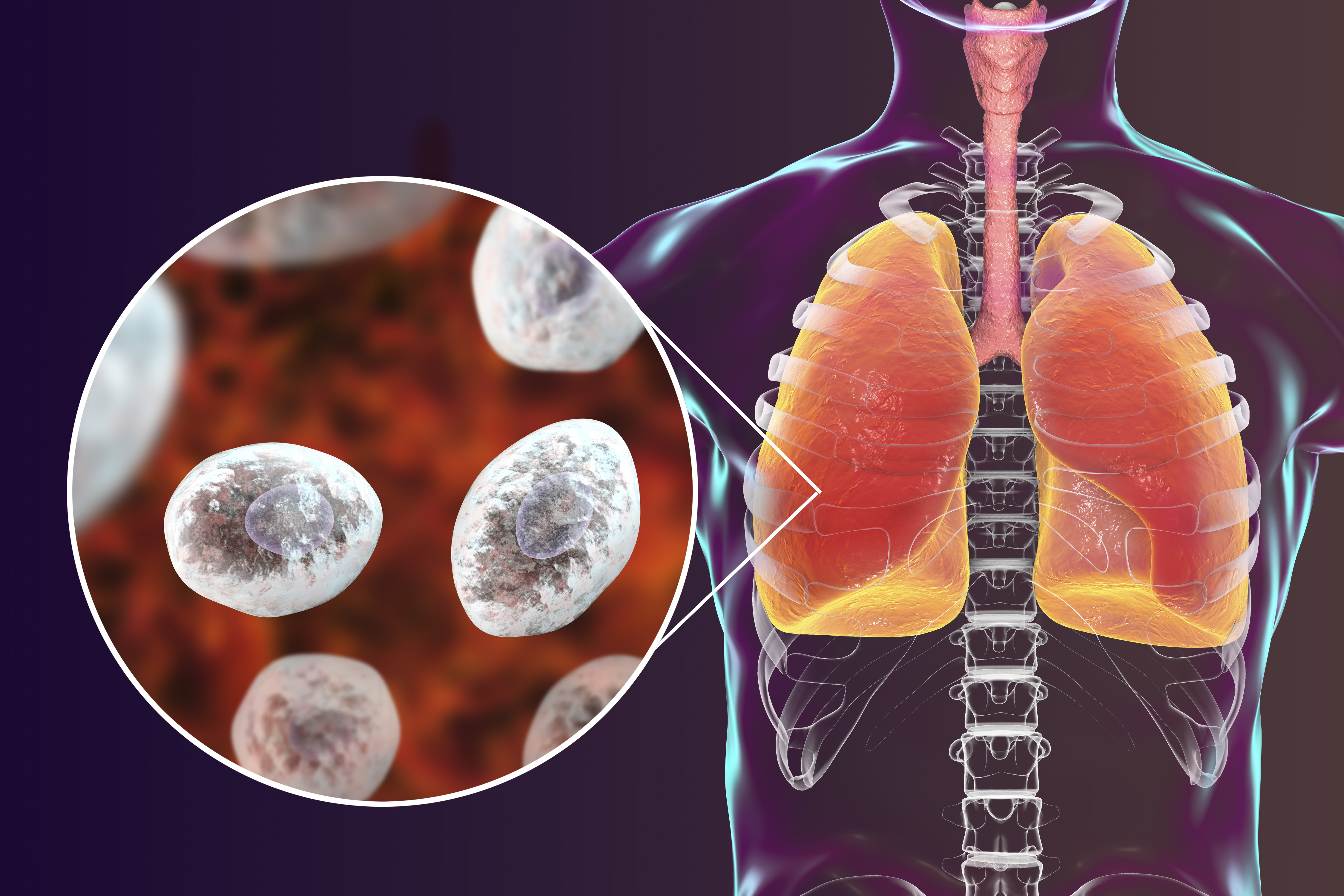
While most medical professionals don’t label COPD as an autoimmune disease, most acknowledge that it has autoimmune components. Think of inflammation as a catalyst for adverse side-effects throughout the body. Because your immune system is preoccupied with chronic inflammation in the lungs, it has fewer resources to use in other areas of the body that may need it.
Immune Dysfunction and COPD are a Two-Way Street
Another important thing to note about COPD and the immune system is that they’re a two-way street. In other words, a compromised immune system will lead to increased COPD symptoms, and COPD symptoms will lead to a compromised immune system. Like we mentioned before, smoking is the primary cause of COPD making up about 90 percent of COPD patients. Continuing to smoke with COPD will not only increase inflammation in the lungs, it will also weaken both your innate and adaptive immune system.
On the other hand, you should remember that only a small percentage of people who smoke actually develop emphysema or chronic bronchitis. This means that there are other factors at play in determining whether a smoker or someone exposed to lung irritants develops COPD. Researchers have found that both genetic makeup and the immune system play a role in determining whether someone develops the disease.
Mucus Hypersecretion
Mucus is a substance created by mucosal glands lining the nasal passages. Its function is to lubricate, moisten, and filter debris that enters the airway, preventing it from reaching the lungs. But mucus isn’t the only substance secreted in the upper body. There are also fluids created by cell membranes in the nose and sinuses. When you get sick or your immune system is compromised by something like smoking or seasonal allergies, these substances are thrown off balance. This means you may experience thicker mucus in the airways making it much more difficult to breathe.
Damaged Cilia
Unfortunately, many of the same things that cause COPD simultaneously damage your immune system. Cilia, tiny hair-like protrusions in the airways are one of the innate immune functions of the body that’s affected by cigarette smoking and air pollution. Much like mucus, cilia are part of a large ecosystem in your body that’s designed to prevent infection. While people who have never smoked or been exposed to a significant amount of pollution may have healthy cilia, most people who have COPD already have damaged cilia.
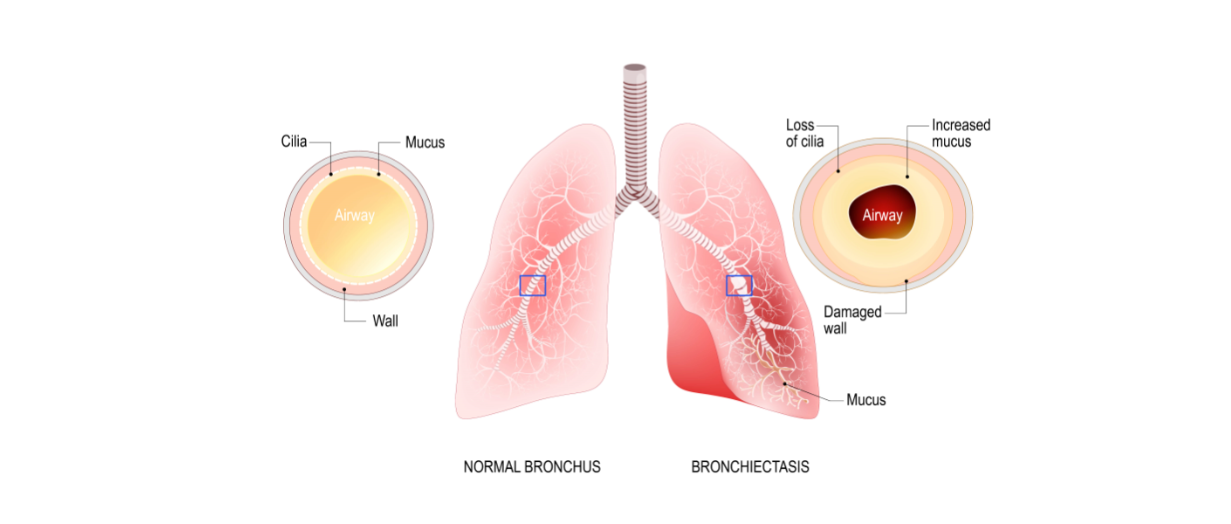
Another function of the cilia is to remove mucus and other substances from the airways. So, when the airways are inflamed due to bronchitis or the cilia are damaged and aren’t able to flow freely, congestion symptoms are likely going to stick around longer in someone with COPD and they may be more severe. This is one of the things that trigger a seemingly never ending cycle of sickness in people with chronic bronchitis and emphysema.
Overactive Immune System
If you’ve ever heard the term “progressive disease,” you may have wondered exactly what that means. What this means is that the disease can’t be cured or reversed. While COPD is a progressive disease, it is still very treatable, meaning symptoms can be reduced and you are able to slow the progression of inflammation in the lungs.
Normally, you think of the immune system as something that protects your body from infection and harm. However, when you have COPD, your immune system is overactive. Something that may cause temporary airway inflammation in a healthy person may cause permanent and irreversible damage to a COPD patient’s lungs because the slightest irritant may result in prolonged inflammation.
High White Blood Cell Count
While a high white blood cell count in and of itself is not harmful, it is a sign of inflammation, chronic disease, and other symptoms. Since white blood cells are what combat infections, cancerous cells, and viruses in the body, a high WBC count is an indication that your body perceives a threat and is trying to eliminate it.
A study published in the National Center for Biotechnical Information looked at WBC counts between 1,227 COPD patients and 8,679 non-COPD adults over the age of 40. It concluded that high WBC counts were negatively associated with forced vital capacity (FVC) and forced expired volume in one second (FEV1), both of which are crucial for quality of life in COPD patients.
When an inflammatory response is triggered, phagocytes are what accelerate the amount of inflammation needed to treat the infection. They recruit alveolar macrophages that combat and control the inflammation. While alveolar macrophages are increased in patients with COPD, their ability to fight infection is impaired. This, along with a high survival rate of neutrophils leads to a high neutrophil load in the airway and a higher white blood cell count.
Reduced Number of Dendritic Cells
Dendritic cells are responsible for processing antigens and presenting it to the T cells. They are also the primary line of communication between the adaptive and innate immune system. While researchers have yet to determine exactly how dendritic cells are affected by COPD, some studies have shown that nicotine exposure can reduce the number of dendritic cells in the body while reducing their functionality, thus compromising both the innate and adaptive immune systems and their ability to work together effectively.
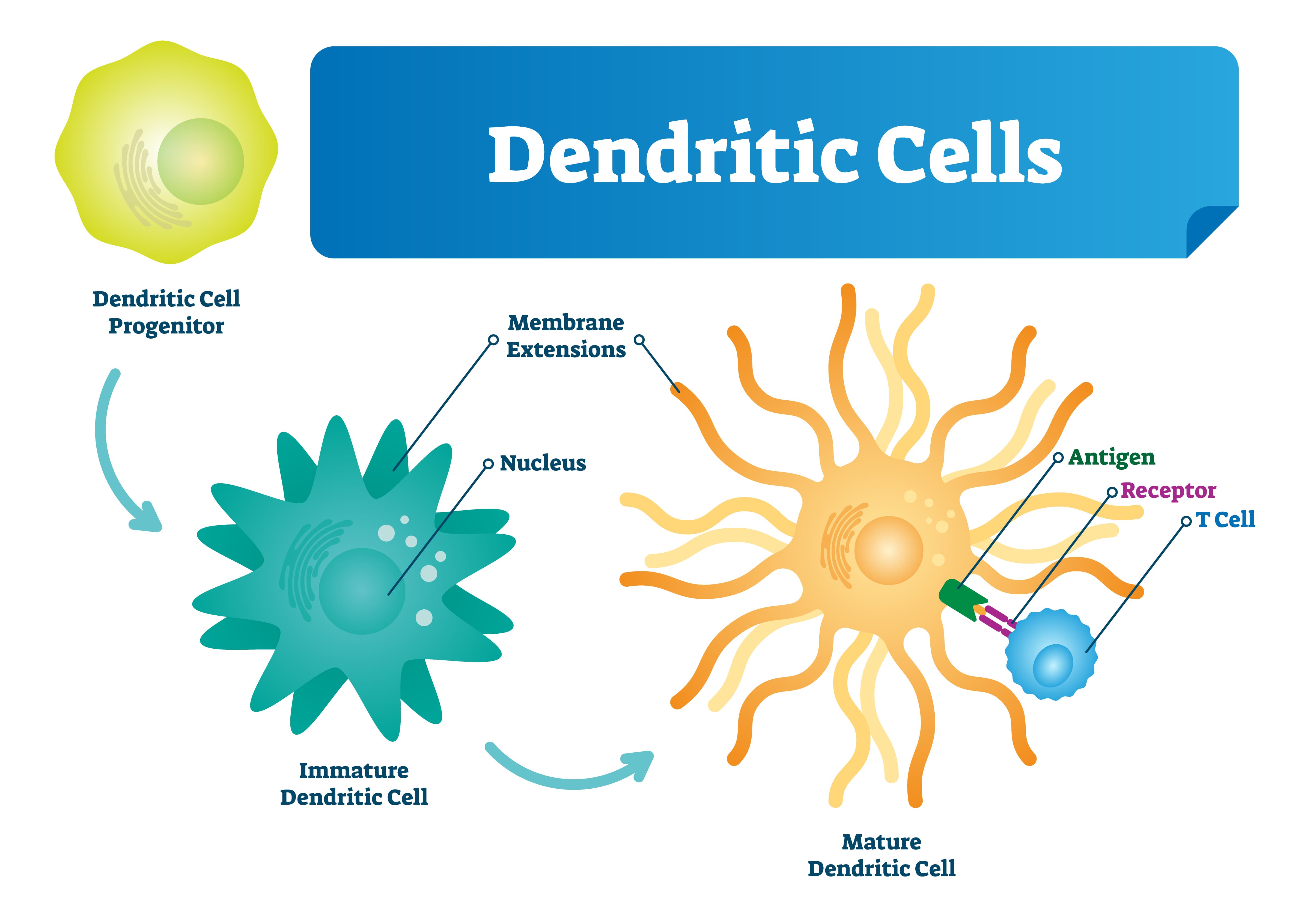
The Immune System and Acute Exacerbations
An acute exacerbation of COPD is a sudden worsening of respiratory symptoms and can last as short as two days or as long as a week. Acute exacerbations are more common in later stages of the disease and exhibit signs such as increased sputum (a mixture of saliva and mucus), breathlessness, coughing, wheezing, and more. Acute exacerbations are typically triggered by environmental factors such as air pollution, dirt, dust, or pollen, and infectious disease
Studies have shown that the majority of exacerbations are caused by respiratory illness like the human rhinovirus, influenza, and respiratory syncytial virus. More specifically, around half of the infective exacerbations caused by bacteria are the result of Haemophilus influenzae (NTHi) which, despite its name, is not the same thing as influenza (the flu). Due to a changing lung microbiome, impaired airway system, and unusual inflammatory response, this provides an ideal environment for it to survive in the lower respiratory area.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
How To Avoid Getting Sick
Now that you know a little bit about how the immune system works and how COPD impairs your immune system, you need to know what you can do about it. No matter what stage of COPD you are in, your age, or your overall health, you should adhere to a strict routine that will keep you from getting sick and keep you breathing freely and effortlessly. While you should be doing everything you can to prevent respiratory infection, you’ll need to know how to react if you do get sick.
Quit Smoking
Smoking cessation should always be your first step in getting healthy and preventing respiratory infection. Cigarettes are what’s called an “immunosuppressive drug.” What this means is that when you smoke cigarettes, your immune system is weakened, and your body will be less prepared to fight off harmful viruses and bacteria.
 According to a study published in the Oncotarget Open Access Journal, cigarette smoke damages adaptive immune cells like regulatory T cells, B cells, and memory T/B lymphocytes while damaging innate immune cells such as natural killer cells, macrophages, and dendritic cells. What’s more, smoking increases mucus production and makes it more difficult to clear meaning harmful pathogens are more likely to build up in the lungs.
According to a study published in the Oncotarget Open Access Journal, cigarette smoke damages adaptive immune cells like regulatory T cells, B cells, and memory T/B lymphocytes while damaging innate immune cells such as natural killer cells, macrophages, and dendritic cells. What’s more, smoking increases mucus production and makes it more difficult to clear meaning harmful pathogens are more likely to build up in the lungs.
Get Plenty of Sleep
A great night’s sleep every night helps ensure your immune system is working its best. According to the National Sleep Foundation, sleep deprivation mainly affects one protein in the body: cytokines. This protein targets and prevents infection and inflammation in the body and they’re mainly produced and released while you’re sleeping.
If that’s not enough, when you slack on sleep, you’ll be more sleepy and less prepared to handle any symptoms of breathlessness or fatigue related to COPD. Getting enough sleep will give you the energy you need to follow your treatment plan to a T without making any mistakes.
Stay Hydrated
There’s no understating the importance of hydration for COPD patients. Although everyone, regardless of whether they’re healthy or sick should be getting enough water, it’s especially important for anyone with a respiratory condition. Every cell in the body needs water in order to function, including all of the immune cells that we discussed above. The human body is made of more than


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!