Even though COPD is a chronic respiratory disease, its effects aren't limited to your lungs and airways. COPD can affect many parts of the body over time and lead to a variety of complications.
If you have COPD, then you are probably concerned about what kinds of health problems the disease can cause and how you can protect yourself from them. The good news is that, by effectively managing your symptoms and living a healthy lifestyle, you can significantly reduce your risk for a variety of COPD complications.
While you cannot stop COPD from progressing altogether, you can make choices that slow the rate at which your symptoms become more serious. By doing so, you reduce your likelihood of developing more serious health complications that result from reduced lung function and the other effects of COPD.
In this article we're going to give you a thorough overview of some of the most common COPD complications and show you how you can prevent them. We'll also explain how each of these complications is treated so you will know what your options are if you happen to develop any of these conditions.
Here are some of the most common complications of COPD:
- Exacerbations
- Pneumonia
- Collapsed Lung (Pneumothorax)
- Osteoporosis
- Hypoxemia & Hypoxia
- Sleep Apnea
- Heart Complications
Most of these conditions are serious and can lead to more health problems, a severely reduced quality of life, or even death over time. By learning the risk factors and causes of potential COPD complications, you can make better decisions about your health and lifestyle that can protect you from these unpleasant and potentially life-threatening conditions.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Exacerbations

Perhaps the most common complication that COPD patients experience is a COPD exacerbation. Exacerbations happen when your COPD symptoms get noticeably worse than normal for an extended period of time.
More serious than a minor flare-up, an exacerbation can cause worsened symptoms that last for days or even weeks. Some exacerbations can be treated at home, while more serious exacerbations require medical attention or even extended hospitalization.
COPD exacerbations are most often caused by illnesses and infections, but they can also be caused by asthma, allergies, or exposure to respiratory irritants. Even a minor sickness, like a cold, can cause someone with COPD to end up with a nasty, prolonged exacerbation.
Unfortunately, one side effect of COPD is that it depresses your immune system and makes it more difficult for your lungs to fight off viruses and bacteria. That means COPD patients are especially prone to getting sick, especially with respiratory illnesses, and have a constant risk of experiencing an exacerbation.
The first sign of an exacerbation is a minor up-tick in symptoms like coughing, wheezing, breathlessness, and fatigue. If these symptoms don't quickly get better on their own, then you are likely experiencing an exacerbation.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Common Symptoms of a COPD Exacerbation:
- Irregular breathing
- Worsened coughing
- Worsened breathlessness
- Noisy breathing (wheezing or rattling may indicate fluid in your lungs)
- Increased mucus in your airways and coughing up phlegm
- Reduced appetite
- Fatigue
- Fever
- Increased difficulty sleeping
- Signs of low blood oxygen levels, including: morning headaches, swollen ankles or legs, a bluish tint to your skin or nails, or an inability to speak or catch your breath
How to Prevent a COPD Exacerbation

The best way to prevent an exacerbation is to avoid getting sick and protect your lungs from respiratory irritants like allergens and pollution. That's why it's so important for people with COPD to wash their hands, keep up with vaccinations, and avoid exposure to germs and sick people, especially during cold and flu season.
Here are some of the best ways to prevent a COPD exacerbation:
-
Stop smoking.
-
Drink plenty of fluids. This helps thin your mucus, preventing it from building up in your airways and harboring viruses and bacteria.
-
Avoid large crowds and busy public spaces during cold and flu season.
-
Wash your hands often and use hand sanitizer when you don't have access to a sink.
-
Always follow your COPD treatment plan carefully, especially when your symptoms flare up.
-
Don't skip or miss any doses of your prescribed medications.
-
Make sure you've received all your recommended vaccinations, including the pneumococcal vaccine and a yearly flu shot.
-
Eat a healthy diet and get plenty of sleep to keep your body and immune system in top shape.
- If you are prescribed supplemental oxygen, always use it as directed.
The next best thing from prevention is early treatment and management to prevent illnesses and exacerbations from getting worse. Because of this, learning to recognize the early warning signs of an exacerbation is a vital skill for anyone who has COPD.
If an exacerbation isn't quickly managed and kept under control, it can cause a permanent damage to your lungs and a permanent worsening of COPD symptoms. However, exacerbations are sometimes difficult to detect when you experience COPD symptoms daily.
This is why it's so important to pay careful attention to your body and look out for times that your symptoms get worse or more frequent than they are on a normal day.
When you notice your symptoms become elevated above your usual baseline for more than a short period of time, you should consult your doctor and your treatment plan for what to do next.
In the most serious cases, severe exacerbations can cause life-threatening complications, like pneumonia, a collapsed lung, or even respiratory failure and death. Because of this, preventing COPD exacerbations is one of the primary goals of COPD treatment.
How to Treat a COPD Exacerbation
How you treat an exacerbation depends on its severity and your unique medical condition. If you have COPD, you should already have a detailed treatment plan from your doctor that includes what medications to take when your symptoms flare up and when to call your doctor.
As soon as you notice the signs or symptoms of a COPD exacerbation, you should immediately consult the instructions laid out in your COPD treatment plan. You may need to use your inhaler more often, reduce your activity levels, or start taking a course of steroids or antibiotics.
One of the most important things to note in your COPD treatment plan is how long you should wait before consulting your doctor or seeking medical attention. The guidelines outlined in your plan should tell you when your symptoms are bad enough to warrant medical attention and how to recognize an emergency.
Here are some general guidelines for managing a COPD exacerbation:
-
Use airway clearance techniques (like huff coughing and chest percussion) to clear excess mucus out of your lungs and airways.
-
Your may need to increase how often you use your short-acting bronchodilators to manage your symptoms effectively.
-
Your doctor may put you on a short course of corticosteroid medications to help decrease inflammation and reduce the chances of more serious complications.
-
Your doctor may prescribe you antibiotics to help you recover and reduce the chances of a secondary infection and further complications.
- Get plenty of rest and drink plenty of fluids.
As we've discussed, early detection and treatment for exacerbations is key for maintaining your health and quality of life with COPD. That's why you should always be monitoring your symptoms and paying special attention to how you feel. Then, when something goes wrong, you will notice right away and be able to begin treatment as early as possible.
Pneumonia

Another common COPD complication is pneumonia, a respiratory infection that causes severe inflammation in the lungs. Pneumonia can be caused by a variety of things, including bacteria, viruses, and fungi, and is particularly dangerous for people with COPD.
Pneumonia often occurs as a secondary infection that happens as a result of another illness, like a cold or (most often) the flu. The symptoms of COPD put patients with the disease at a higher risk for pneumonia because of symptoms like thick, excess mucus, a weakened immune system, and frequent upper respiratory infections.
Pneumonia occurs when the lungs become so inflamed that fluid and pus collect in the lungs. This fluid fills up many of the lung's air sacs, preventing them from absorbing oxygen and transferring it to your blood.
With many alveoli incapacitated, your lungs' have difficulty absorbing enough oxygen with its remaining functional alveoli. For people with COPD, whose lungs have already sustained damage and struggle to absorb enough oxygen, this can severely limit airflow and cause permanent damage to their lungs.
Pneumonia is most commonly diagnosed with a physical exam and chest x-ray. Your doctor may also test a sample of fluid or mucus from your lungs to determine exactly what kind of bacteria, fungus, or virus is causing your illness.
Here are some of the most common symptoms of pneumonia:
- High fever
- Shaking
- Chills
- Fatigue
- Worsened chest pain
- Worsened shortness of breath
- Worsened cough
- Headache and body aches
Although relatively common, pneumonia is not a disease to take lightly; it normally takes up to three weeks to recover and as many as twenty percent of pneumonia cases (about 1 million people each year) require hospitalization. Also, people with COPD who contract pneumonia are at a much higher risk for life-threatening respiratory symptoms such as hypoxia and potentially fatal respiratory failure.
Pneumonia can also lead to other complications, including hypoxemia, sepsis, pleural effusion (fluid in the chest or lungs), respiratory failure, and death. Older adults above the age of 65 and people who have lung diseases like COPD are more prone to contracting and experiencing serious complications from pneumonia.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
How to Prevent Pneumonia
You can lower your risk of contracting pneumonia by avoiding getting sick and treating respiratory illnesses promptly and aggressively. However, the best first line of defense against pneumonia is vaccination.
While not 100% effective, the pneumococcal vaccine protects at least 45 out of 100 older adults from pneumococcal pneumonia. Most people in the US receive the pneumococcal vaccine as children. However, a second dose is usually recommended for people who smoke or who are over the age of 64.
How to Treat Pneumonia

Treatment for pneumonia depends on its cause and how serious the symptoms are. Viral pneumonia can sometimes be treated with antiviral medicine, while fungal and bacterial pneumonia are treated with anti-fungal and antibiotic medications, respectively.
Along with antibiotics, anti-viral, and anti-fungal drugs, rest and home care is often enough to support recovery from pneumonia. Recovery can take time, and until you feel better you should take a break from daily chores and responsibilities and give yourself plenty of time to rest.
Drinking plenty of fluids is also important, because it helps thin and loosen up the mucus so it's easier to cough phlegm up and out of your lungs. It's usually fine to take asprin or NSAIDs for a fever, but you should avoid cough suppressants since coughing to clear the phlegm from your lungs is important for recovery.
If your symptoms are severe, you may need to receive treatment in a hospital until you recover. There, you may receive more targeted antibiotic treatments, supplemental oxygen, intravenous fluids, and general medical support. If your condition is very severe, you may need more intensive treatments in an intensive care unit and breathing support through a ventilator.
You are more likely to require hospitalization if you have one or more of the following conditions:
- You are over the age of 65.
- You have other health problems or chronic diseases like asthma, diabetes, or COPD.
- Your blood oxygen levels drop too low.
- You are so ill that you cannot eat or care for yourself.
- You have severe chest pain.
- You are unable to cough up mucus and clear your lungs on your own.
- You are unable to eat or keep food or fluids down.
- Your pneumonia is not getting better with normal treatment at home.
Collapsed Lung (Pneumothorax)
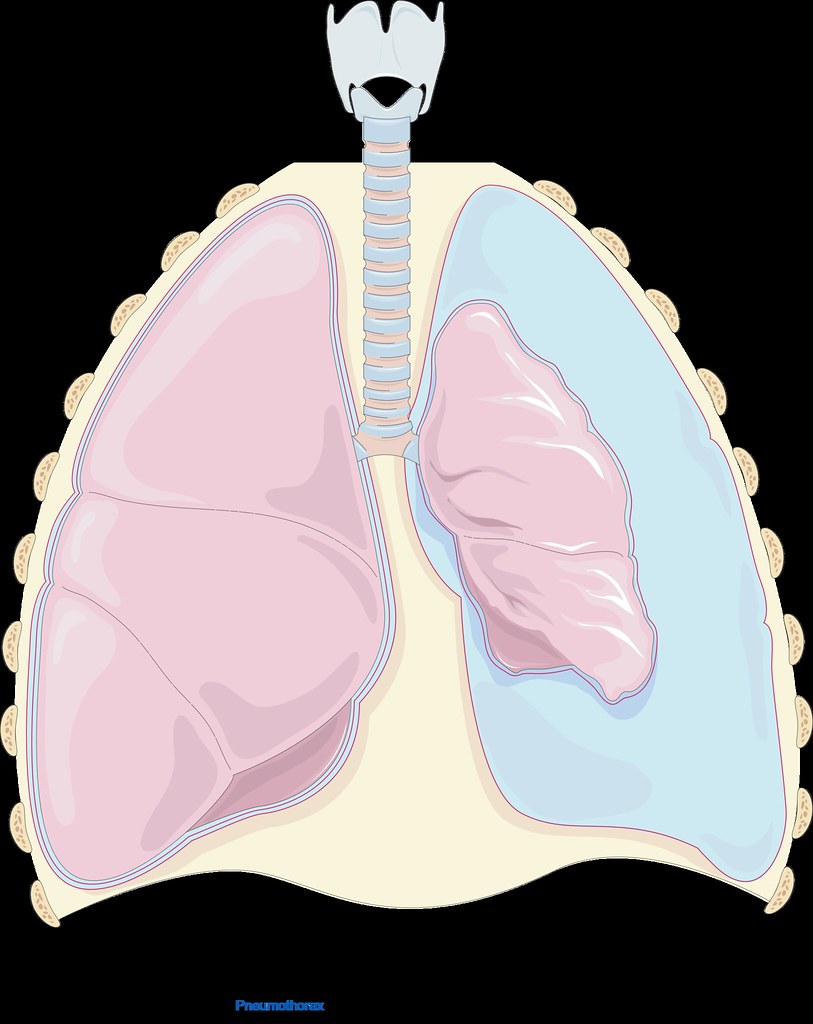
Lungs damaged by COPD are more prone to collapsing because the damaged tissue can leak air into the open space in between your lungs and your chest wall (your chest cavity). The pressure that the trapped air puts on your lung can cause your lung to collapse (also known as pneumothorax).
A collapsed lung can happen suddenly and spontaneously, without any warning. It is usually accompanied by sudden, sharp pain in the chest and worsened shortness of breath.
Pneumothorax is more common in patients with COPD because damaged, weakened lung tissue is both more likely to leak air and more likely to collapse under pressure. A collapsed lung is a medical emergency, especially for patients with COPD whose lung function is poor. If one lung collapses, the other lung may be unable to supply the body with enough oxygen, causing severe hypoxemia or hypoxia.
Here are some of the most common symptoms of a collapsed lung:
- Sudden chest pain (often described as sharp or stabbing)
- Shortness of breath
- Difficulty breathing
- Rapid breathing
- Rapid heart rate
- Coughing
- Bluish tint to the skin
How to Prevent a Collapsed Lung
The first step to preventing a collapsed lung is always to quit smoking. Smoking is one of the greatest risk factors for pneumothorax and quitting can significantly decrease your risk.
The more advanced your COPD, the more likely you are to experience a collapsed lung. That means that the next best way to prevent a collapsed lung is to follow your COPD treatment plan.
If you manage your COPD symptoms well and protect your lungs from further damage, your lungs will be less likely to leak air into your chest cavity and cause a collapsed lung. That's why it's so important to get regular check-ups from your doctor and follow the diet, exercise plan, and medication schedule that your doctor recommends.
How to Treat a Collapsed Lung
If you suspect that you might have a collapsed lung, you should go to a hospital immediately. A collapsed lung can sometimes be fatal without immediate medical attention.
At the hospital, you will likely receive treatment to remove the air in your chest cavity. This is usually done by inserting a small tube between the ribs and into the chest cavity to allow the trapped air to escape.
In some cases, if the collapse is minor, your lung may recover and re-inflate on its own. However, this determination must be made by a doctor and you should never try to treat a collapsed lung on your own at home.
Osteoporosis

Another complication that affects a large number of COPD patients is osteoporosis. Osteoporosis occurs when your bones become thin and brittle as a result of bone density loss, which significantly increases the risk of bone breaks and injuries.
Osteoporosis can be caused by a variety of factors related to COPD, including poor nutrition, lack of exercise, and increased inflammation throughout the body. All of these factors can result in a loss of bone density in patients with COPD; in fact, studies show that nearly seventy percent of all people with COPD have osteoporosis or at least some level of bone density loss.
Many people with COPD, for example, struggle to maintain a healthy weight and get enough nutrients from their diet. This is in part because people with COPD need extra calories and nutrients to support their over-strained lungs, and in part because COPD symptoms like breathlessness interfere with their ability to eat.
This causes some patients to lose weight and become malnourished, resulting in dangerous nutrient deficiencies that lead to osteoporosis. If you fail to get enough calcium and vitamin C in your diet, your body can no longer strengthen and maintain your bones, and will even cannibalize your bones to get the calcium it needs for other bodily functions.
Lack of exercise, too, can lead to bone density loss and disfigurement of your skeleton. That's because your bones are living tissue, and your body is constantly breaking down bits of your bones and building them back up.
Your body balances this process based on the amount of activity and strain your bones experience, taking density away from bones that are used less often and adding density to the bones that experience the most wear and tear.
When you stop exercising, your body takes bone density away from important bones in your limbs and other places in your body that you aren't using much. This leads to osteoporosis and changes to your skeletal structure so that it becomes even more difficult to stay active and avoid injury.
Finally, COPD patients have other characteristics that put them at a heightened risk of osteoporosis. People with COPD tend to be older, have a history of smoking, and use corticosteroid medications to treat their disease. All of these characteristics are also risk factors for osteoporosis and contribute the high incidence of bone density loss in patients with COPD.
Osteoporosis can be dangerous, painful, and interfere with your ability to exercise and stay active. It can cause even minor bumps and falls to bruise and fracture your bones, and recovery can take much longer than normal.
Here are some of the most common symptoms of osteoporosis:
- Bones that fracture easily from minor injuries or falls
- Loss of height over time
- Stooped posture
- Back pain (often caused by a fractured or collapsed vertebra)
- Receding gums (from reduced bone density in your jaw)
- Weakened grip strength
- Weak and brittle fingernails
How to Prevent Osteoporosis

Quitting smoking is one of the most important things you can do to prevent your COPD from getting worse, and it can help prevent osteoporosis as well. Getting regular physical exercise is also necessary to keep your bones healthy and strong.
It's also important to maintain a healthy diet full of whole, nutritious foods. It's particularly important to ensure that you eat plenty of foods rich in calcium and vitamin D; this ensures your body has the building blocks it needs to build thick, strong bones.
Even though COPD symptoms like breathlessness and fatigue can make it difficult to live a healthy lifestyle, it's important to follow your diet and exercise treatment plan, even when it's hard. It's not only necessary for healthy bones, but for maintaining your muscle strength, lung function, and physical mobility with COPD.
If you are struggling to get enough physical activity or need some extra help managing you disease, talk to your doctor about joining a pulmonary rehabilitation class, where you can learn all about how to better manage your diet, exercise, medications, and daily life with COPD.
How to Treat Osteoporosis
Unfortunately, once you begin losing bone density, it is usually impossible to get it back. Once you have osteoporosis or the early stages of bone density loss, the only thing you can do is manage it and keep it from getting worse.
The good news is that it usually only takes adjusting your diet and increasing exercise to manage osteoporosis and prevent further damage to your bones. Your doctor might also prescribe you a bisphosphonate medication which reduces the rate at which your body naturally breaks down your bones.
Other things you can do to prevent worsening of osteoporosis is to stop smoking and avoid drinking excessive amount of alcohol, which can impair your body's ability to build and repair your bones. You may also need to take special measures to prevent falls that could result in serious injury, for example, taking a fall prevention class or removing fall hazards in and around your home.


