.png)
Chronic obstructive pulmonary disease (COPD) is a lung condition that affects millions of people across the country. Advanced stages of COPD can lead to debilitating symptoms such as breathlessness, wheezing, and chest tightness. Since there is no cure for COPD, managing its symptoms is the best way to prevent it from progressing.
With that being said, it’s no surprise that many people afflicted with COPD also develop anxiety from their condition. In tandem with physical symptoms, knowing that the condition can’t be reversed can lead to severe anxiety and reduced quality of life. This is a common response and should be taken just as seriously as the disease itself.
In the following sections, we’re going to take a look at how exactly COPD can lead to anxiety, how anxiety can make COPD symptoms worse, and what you can do to prevent this negative feedback loop.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
How COPD Can Cause Anxiety
Much like how you feel hungry when you haven’t eaten all day or thirsty when you’re dehydrated, your body will exhibit symptoms when it’s low on oxygen. Short-term symptoms like the need to stop and rest more frequently while exercising are easy to notice, however, anxiety tends to be more of a long-term reaction that can be more difficult to detect.
It’s normal to experience anxiety to some extent throughout our daily lives and it can even be used to motivate us to make a change. For example, if you have dirty dishes piling up in your sink, you may experience enough anxiety to clean them and put them away, leaving you feeling relieved and accomplished.

On the other hand, chronic and severe anxiety, like what you may experience as a result of COPD, is not healthy and can even contribute to the physical symptoms you’re experiencing.
According to a study published by the Department of Health and Human Services (HHS), instances of anxiety and depression are “generally higher than those reported in other advanced chronic diseases,” and are much higher than the prevalence of anxiety in the general public, especially during later stages of the disease.
We’re going to take a look at just a few of the main reasons COPD leads to anxiety and what you can do about it.
Shallow Breathing
On average, a healthy person takes between 12 to 20 breaths per minute. If you take more breaths than this, it is known as tachypnea or hyperventilation. Although on the surface, this may not seem like a serious issue, for a COPD patient, it may be the root cause of their anxiety.
According to the Yearbook of Intensive Care and Emergency Medicine, patients with COPD demonstrate shallow and rapid breathing that often results in hypercapnia or carbon dioxide retention. This shallow breathing is usually the result of diminishing lung elasticity and general lung function and can result in breathlessness and increased blood pressure.
Whether it occurs as an isolated incident or chronically like in progressive lung disease, hypercapnia causes a stress response in the body that leads to anxiety. It’s your brain’s way of telling you that something’s wrong and your body isn’t getting the oxygen it needs.
COPD Exacerbations
A COPD exacerbation can result from anything that causes COPD symptoms to worsen. For example, inhaling an irritating substance like pollution or contracting an illness that leads to inflammation of the airways.
Exacerbations like these can lead to a sudden onset of anxiety commonly called panic attacks. If you’d like more information on treating and preventing COPD-induced panic attacks, our blog titled COPD and Panic Attacks: How to Manage Your Anxiety will be a great resource for you.
Aside from panic attacks, however, you might have anxiety about experiencing another exacerbation. For example, if you were outside when an exacerbation occurred, you may have a fear of going outside, especially in busy areas where you feel a lack of control. If this persists long enough, you could be missing out on a lot of the things you enjoy doing in your life.
Feelings of Guilt
One of the most common causes of anxiety in people with chronic respiratory conditions is a sense of guilt. Some patients may feel guilty about their increased dependency on loved ones or about an activity that they are no longer able to do with their condition.
Over time, feelings of guilt can lead to COPD patients not asking for the help they need or distancing themselves from friends and family in order to regain some independence.
The Breathlessness-Anxiety Cycle
When COPD and anxiety combine, they can create a cycle of negative feedback. Feelings of breathlessness may provoke panic, causing you to feel more anxious, thus making it harder to breathe. When you get caught up in this cycle, it may be difficult to distinguish the symptoms of anxiety with the symptoms of COPD.

If you believe you’ve found yourself in this breathlessness-anxiety cycle, it’s important that you speak with a doctor before making any decisions about your health. If you take medication for anxiety, it may exacerbate your COPD symptoms or vise versa. Your doctor will help you find the right balance and ensure that you aren’t making symptoms worse.
How To Reduce COPD-Induced Anxiety
Fortunately, there is ample research done on anxiety and many resources out there for you to go to if you’re experiencing COPD-related anxiety. But a good place to start would be to simply try to recognize the signs of anxiety and how they might be affecting your COPD symptoms.
If you notice that you’re stuck in a loop of negative thoughts surrounding your condition, you’re most likely experiencing anxiety and you should speak with a doctor immediately. However, in the meantime, try some of these tips to reduce anxiety, and ideally, improve COPD symptoms at the same time.
Pulmonary Rehabilitation
Pulmonary rehabilitation (PR) is the process of improving lung function and reducing the symptoms of chronic respiratory conditions through exercise and education. In pulmonary rehabilitation, you will learn more about how your lungs work and how to exercise effectively and safely.

By attending pulmonary rehabilitation, you will not only learn techniques for breathing more effectively, but you will be surrounded by a group of people who are facing similar challenges in their lives. This is a great opportunity to meet some new people and socialize which, in and of itself, may help you alleviate feelings of anxiety.
Breathing Exercises
Although it may seem silly to practice your breathing, it’s incredibly important and can help you live a happier and more fulfilling life, especially if you have a chronic respiratory condition like COPD.
Taking the time to understand how your breathing and posture affect your oxygen intake can be hugely beneficial. And as a result, you’ll be able to reduce symptoms of anxiety significantly. There are a lot of different breathing exercises you can try, however, for COPD patients, diaphragmatic breathing, deep breathing, and pursed lips breathing tend to be the most effective.

Diaphragmatic Breathing
The diaphragm is the muscle under the chest cavity that’s responsible for expanding the lungs, allowing air to flow in. Due to the reduced lung function in COPD patients, however, many people develop a rapid, shallow breath that doesn’t use the diaphragm muscle. Diaphragmatic breathing will help you concentrate on “breathing from the stomach” rather than breathing from the chest.
Deep Breathing
Once you’ve mastered diaphragmatic breathing, you may want to give deep breathing a try. Similar to diaphragmatic breathing, deep breathing requires you to take in a lot of air. However, with this exercise, you will breathe in slowly until your lungs are completely filled and then release it slowly. Ideally, you’ll want to be lying on your back to practice deep breathing exercises.
Pursed Lips Breathing
With this breathing technique, you will inhale slowly through your nose and release it slowly through pursed lips. The purpose of the pursed lips is to increase resistance in the airways, keeping them open while you breathe. Breathing in this way will help you calm down and reduce anxiety.
For more detailed information on breathing techniques, check out 6 Effective Breathing Techniques and Exercises for COPD.
Get More Sleep
One of the main causes of anxiety is a lack of sleep. When you don’t get enough sleep each night, your body is not physically, mentally, or psychologically equipped to make it through the day. And when you’re living life with COPD, you’re carrying additional emotional baggage that many people are not dealing with.
Sleep apnea is a condition affecting more than 18 million Americans. Although it’s not any more common among people with COPD, it can be a lot more dangerous for those that do. When someone has both COPD and sleep apnea it’s called “overlap syndrome” which increases your risk for chronic fatigue, high blood pressure, and hypercapnia.
Improve Your Diet
If you’ve already read our blog about 21 Healthy Foods You Should Eat if You Have COPD and 11 Foods You Should Avoid if You Have COPD, then you already have a pretty good idea of what food is good and bad for COPD. However, when it comes to anxiety, there are two in particular that you need to watch out for — sugar and caffeine.
Although sugar may make you feel great when you first consume it, your body will release extra insulin to absorb the glucose and once this happens, you’ll experience a sugar crash. After a sugar crash, you can expect to feel increased levels of anxiety, irritability, and fatigue.

Similarly with caffeine, you’ll get a quick boost of energy, but reduced levels of serotonin (the feel-good chemical) leading to a depressed mood. The bottom line here is that COPD symptoms are already hard enough to deal with and consuming copious amounts of sugar and caffeine will only make them more difficult in the long run.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Practice Positive Thinking
Sometimes, simply changing your mindset is a great way to reduce COPD-induced anxiety. Whenever you start a new medication, exercise routine, or anything else related to your COPD treatment plan, it pays to see things in a positive light and prevent negative thoughts wherever possible.
Although there is no way to cure COPD, if you follow your doctor’s recommendations and you take care of yourself, you’ll be surprised at all the things you can accomplish! Many people with COPD are able to live long and fulfilling lives just by making a few simple lifestyle changes.
If you’ve never tried it before, you may want to consider meditation or other techniques that help to quiet the mind and relieve tension in the body. These techniques often work hand-in-hand with breathing exercises because the more in tune you are with your body’s needs, the more your mind will be at ease.
Aside from meditation, maintaining a positive outlook on your situation can help you immensely in the long run. Instead of focusing on the negative aspects of your condition, try living in the moment and enjoying time spent with friends and family or doing your favorite hobbies.
Get Outside
In this day and age, humans spend the majority of their time indoors. There are a number of ways that this can have a toll on our mental health, especially when coping with a chronic condition like COPD.
In the past, before the invention of the electric light, humans spent more time outdoors. As a result, the human circadian rhythm was in sync with the natural light-dark cycle. However nowadays, we’re often exposed to light immediately before bed, after waking up, and all throughout the day which can disturb our sleep and increase anxiety.
The best way to combat this is to spend more time outside, especially in the morning or at night right before bed. Although many people work indoors throughout the day, the more you can mimic the natural day-night cycle of the earth, the better.

Another important part of this is staying consistent. Your body needs to get into a rhythm where it knows exactly what to expect each day. This will help you get more restful sleep and keep you feeling alert and positive each day you wake up.
Visit A Therapist
If you’ve tried all of the above solutions to anxiety but haven’t seen any success, you should never be afraid to speak with a therapist. Although it may seem like there is no solution to your anxiety, therapists are experienced with treating patients just like you.
Whether you’re experiencing general anxiety disorder or frequent panic attacks, a licensed mental health professional will help you identify and treat the underlying causes. More specifically, cognitive behavioral therapy (CBT) will help increase awareness of negative thinking patterns so that you’re more equipped to take on a challenging situation.

Additionally, your psychiatrist will help you determine if medication may be beneficial such as antidepressants and other anti-anxiety drugs. If you’re having trouble finding a psychiatrist that’s right for you, be sure to speak with your primary care physician.
Follow Your Treatment Plan
COPD is a progressive disease. What this means is that symptoms rarely get better on their own and they tend to get worse unless medical action is taken. Your doctor will set you up with a clear treatment plan for COPD, and it’s important to stick with it.
COPD treatment may involve a variety of things such as oxygen therapy, bronchodilators, or vaccines to prevent illnesses that make COPD worse. Additionally, your doctor may recommend pulmonary rehabilitation and lifestyle changes like a special diet to follow. Be sure to listen carefully, and if you ever have any questions, don’t hesitate to ask them. The more thoroughly you understand your condition, the better you will be able to manage it and the less anxiety you will experience.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Conclusion
When it comes to COPD-induced anxiety, the sooner you take action, the better. It’s not uncommon for someone coping with a chronic disease to experience anxiety, depression, or panic attacks, and there is always something you can do to relieve these symptoms.

By following your treatment plan and making changes to your lifestyle, you’ll be able to experience more peace of mind and assurance throughout your daily life. When you live anxiety free, you’ll be able to enjoy the time you spend with loved ones and doing all of the activities you enjoy.
Additionally, finding ways to relieve anxiety could help reduce COPD symptoms like breathlessness, chest tightness, and exacerbations. Be sure to speak with your doctor immediately if you have any questions.
 Without oxygen, human life would not exist. Much like the water you drink and the food you eat, the oxygen you inhale plays an essential role in helping your body convert nutrients into usable energy, occurring through a process called cellular respiration.
Without oxygen, human life would not exist. Much like the water you drink and the food you eat, the oxygen you inhale plays an essential role in helping your body convert nutrients into usable energy, occurring through a process called cellular respiration.
Every time you take a breath, air passes over tiny air sacs in the lungs called alveoli. Oxygen is absorbed from the air and sent to every part of the body via the bloodstream providing your body with the energy it needs to survive and thrive.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Unfortunately, there are a number of diseases and disorders that can affect the body's ability to process oxygen, transport it throughout the body, or to take in the amount of oxygen that it needs. This results in a condition called hypoxemia or low blood oxygen levels.
In the following sections, we'll take a look at what exactly causes low blood oxygen levels, what symptoms to look for, and what steps you can take to ensure that you maintain healthy blood oxygen levels throughout your daily life.
What Are The Symptoms of Low Blood Oxygen Levels?

The symptoms of low blood oxygen levels can vary widely depending on its severity. It also helps to note whether the hypoxemia is chronic (occurring over an extended period of time) or acute (occurring over a short period of time). Symptoms of acute hypoxemia may include:
- Increased heart rate
- Coughing
- A change in skin color
- Shortness of breath
- Increased breathing rate
Although symptoms of chronic hypoxemia can be just as destructive, they are often more difficult to detect because the body begins to compensate for decreased oxygen over time. Symptoms of chronic hypoxemia may include:
- High blood pressure in and around the lungs (pulmonary hypertension)
- Heart disease brought on by the enlargement and failure of the right side of the heart (cor pulmonale)
- Increased red blood cell count in the blood (polycythemia)
What Causes Low Blood Oxygen Levels?
Although your body naturally works to maintain oxygen levels in your blood, there are a number of conditions that can make it difficult or impossible for your body to do so.
According to an article published by The National Center for Biotechnology Information, there are several different mechanisms through which blood oxygen levels may decrease, thereby resulting in the different types of hypoxemia.
Diffusion Impairment
After entering the lungs, oxygen is absorbed by tiny sacs called alveoli. Capillaries surround these sacs and the oxygen is then diffused into the blood. Diffusion impairment refers to a condition that prevents the oxygen from moving into the bloodstream. Diffusion impairment is usually the result of inflammatory conditions, fibrosis, or granulomas, which can make the condition worse.
V/Q Mismatch
This defect is characterized by a "mismatch" between the air that travels between the lungs and the environment (ventilation), and the blood that passes through the lungs carrying oxygen (perfusion). In other words, anything that interferes with the ventilation of the lungs or the flow of blood to the capillaries can result in a mismatch and reduced oxygen in the lungs. V/Q mismatches are one of the most common causes of hypoxemia.
If there is decreased ventilation and increased perfusion, this will result in a lower V/Q ratio. This could be caused by conditions such as:
- Asthma
- Pulmonary edema
- Airway obstruction
- Chronic bronchitis
If there is decreased perfusion but increased ventilation, this will result in a higher V/Q ratio. This may be caused by conditions such as:
- Emphysema
- Pulmonary embolism
Hypoventilation
This is when there is a reduced amount of air that enters the alveoli in the lungs, resulting in higher levels of carbon dioxide in the blood. Hypoventilation often occurs as a result of breathing that is too slow (bradypnea) or breathing that is too shallow (hypopnea).
Right-To-Left Shunt
The heart is responsible for providing the body with oxygen and nutrients while carrying away waste that could be harmful to it. However, when there's an abnormal communication between the right and left side of the heart, deoxygenated blood may bypass the lungs and be distributed to the rest of the body. This is known as a right-to-left shunt.
How You Can Maintain Safe Blood Oxygen Levels
Visit A Doctor
Whether you know you have low blood oxygen levels or you've experienced one or more of the symptoms above, visiting a doctor should always be your first course of action. Although shortness of breath or increased heart rate may not seem serious at first, they could be the sign of a long overdue condition that needs to be treated.

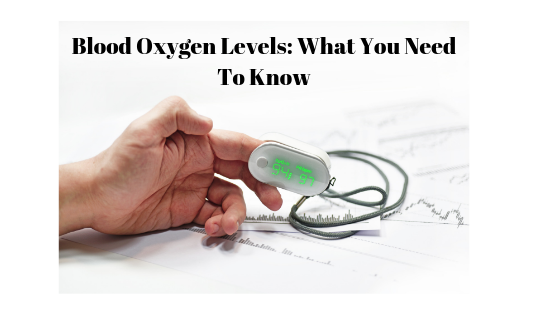
Another reason to visit a doctor immediately rather than waiting is because of the advanced diagnostic methods used to detect low blood oxygen levels. There are three common tests used to check blood oxygen levels including pulse oximetry, arterial blood gas tests, and breathing tests.
Pulse oximetry is a quick, painless, and noninvasive procedure that measures oxygen saturation of your red blood cells. Most pulse oximeters attach to the finger, but can also be attached to the forehead, feet, toes, or ears. Pulse oximeters can be purchased for in-home use. However, it's recommended that you learn from your doctor how to use it first.

Another form of blood testing, arterial blood gas analysis (ABG) can be used to determine the amount of carbon dioxide and oxygen in the blood as well as its pH level. However, unlike pulse oximetry, an ABG test requires drawing blood and should only be done by an experienced medical professional.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Get Outside And Exercise
Generally, getting out of the house and getting some fresh air is a great way to increase your blood oxygen levels. If you live in a home without any plants, you're likely living in a low-oxygen environment that could be unsafe, especially if you already have a condition that affects your blood oxygen levels.
According to the Environmental Protection Agency, we spend about 90 percent of our time indoors, and oftentimes, the air we breathe can be even more polluted than the air outdoors. Ensuring that your home is clean and ventilated properly can have an immense impact on your health.
The two most important organs for maintaining high blood oxygen levels, the heart and the lungs, are strengthened through exercise. So naturally, getting more exercise will be beneficial for you. Additionally, strong muscles are more efficient and require less oxygen to operate.

If you have a severe respiratory condition, it's important to check in with your doctor before starting an exercise routine. Conditions like Chronic Obstructive Pulmonary Disease (COPD) can't be cured with exercise, but your doctor may be able to set you up with a routine that can help alleviate some of the symptoms.
Reinforce Good Habits
Regardless of the condition you want to treat or avoid, reinforcing good habits is always a great place to start. Maintaining a healthy diet, consuming enough fluids, and getting enough sleep will all help you maintain healthy blood oxygen levels. Common COPD diets are high in protein and healthy fats, but require you to avoid a high intake of salt, certain fruits, and dairy products.
Like exercise, a healthy diet and restful sleep won't cure COPD, but they can certainly reduce the symptoms and help you live a more full and productive life. Your doctor may refer you to a dietitian or other experienced medical professional to set up a plan that works for you.

Using Oxygen as Prescribed
If you are currently undergoing oxygen therapy, be sure to use your oxygen concentrator as it was prescribed by your doctor. The purpose of oxygen therapy is to help people with conditions like COPD, asthma, lung disease, and more cope with their condition more easily. However, if you aren't using it frequently enough, you may not experience the full benefits.
If you're having trouble maintaining your blood oxygen levels while on a trip or otherwise away from home, portable oxygen concentrators may be a great option for you. There are plenty of options out there, so be sure to consult a professional before committing to anything.
What Is A Healthy Blood Oxygen Level?
Now that you know a little bit about blood oxygen levels, you're probably wondering what a healthy level actually is. A blood oxygen measurement is often referred to as the oxygen saturation level. For healthy lungs, this will fall between 80 and 100 millimeters of mercury (mm Hg).
If you had a pulse oximetry reading, it should be between 95 and 100 percent. However, when you're living with a respiratory disease like COPD, anything between 88% and 92%, is still considered safe and average.
Anything below these results is considered hypoxemia and could be a sign of a progressive disorder. If you experience any drops or fluctuations in your blood oxygen levels, you should consult your doctor immediately.
Conclusion
Although low blood oxygen levels could have serious implications, the sooner you act, the better chance you will have to reverse them. It’s normal to have an occasional cough or shortness of breath, but if the issues persist, you should take action sooner rather than later.
Your doctor will be able to help you pinpoint exactly what is causing your symptoms, diagnose your condition, and help you set up a plan to improve your blood oxygen levels. And if you already have a respiratory condition like COPD, never hesitate to speak with a professional about the issues you're facing.
Did you know that living with COPD can make it more difficult to think, make decisions, and remember things? It's true; studies show that COPD can cause mild cognitive impairment, a condition that affects your memory and other mental functions.
Unfortunately, many people are unaware of, or underestimate, the effect that COPD can have on your brain. Because of this, many COPD patients experience mental decline without ever realizing that their disease could be the cause.
This is a shame, especially because COPD-related mild cognitive impairment is both treatable and preventable. But in order to avoid it or minimize its symptoms, you have to understand what it is and what is has to do with COPD.
That's why, in this post, we're going to explain how COPD causes mild cognitive decline and how to recognize it if you have it. We'll also explain what you can do to prevent COPD-related memory loss and how to treat it if it appears.
Many people with COPD have to deal with mild cognitive impairment at some point or another, and it's important to know what you can do about it and what to expect if it happens. That's why we've included a wealth of practical knowledge, helpful advice, and effective techniques in this guide to help you manage memory problems and other cognitive symptoms caused by COPD.
What Does Mild Cognitive Impairment Mean?
In general, mild cognitive impairment (MCI) is a condition that causes minor problems with memory, focus, problem-solving, and attention. It happens to many people as they age, but respiratory diseases like COPD can both trigger and accelerate the condition.
Many people who experience forgetfulness or worry their brain is not as “sharp” as it used to be are actually experiencing the symptoms of mild cognitive impairment. However, MCI is slightly worse than the normal changes to memory and cognition you'd expect to see with age alone.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Mild cognitive impairment happens when the brain's cognitive functions are slightly lower than they should be. It can result from both temporary problems (e.g. oxygen deprivation) and permanent changes (e.g. structural damage) that happen to the brain.
Mild cognitive impairment is very common, affecting about 10-20 percent of people over the age of 65 and about 36 percent of people with COPD. Fortunately, it is a treatable, and sometimes even reversible, condition that can improve with diet, exercise, and other lifestyle changes.
It's important to note that the symptoms of mild cognitive impairment are often very subtle. Some people notice these symptoms on their own, but many don't recognize the signs of MCI until a friend or family member points it out.
Here are some of the most common signs and symptoms of COPD-related memory loss and MCI:
- Forgetting things like events and appointments often
- Forgetting words or struggling to come up with the right vocabulary more often
- Losing or misplacing things more often
- Feeling overwhelmed when faced with problems, making decisions, or making plans
- Difficulty understanding instructions or doing activities that require multiple steps
- Struggling to focus on simple tasks like reading, watching a movie, or having a conversation
- Difficulty finding your way around familiar places or environments
- Increased impulsive behavior or poor judgment
Sometimes, mild cognitive impairment is split into two distinct categories: memory-related or “amnestic” MCI, and MCI that affects thinking skills like decision making and completing tasks with several steps. Some people with MCI experience just one or two symptoms, while others experience a wider rage of cognitive problems.
 |
| Image from www.amenclinics.com |
In the words of Charles Emery, a COPD researcher from Ohio State University, “COPD-related cognitive impairment usually isn't noticeable to the untrained eye, but it can be a serious problem.” That's why people with COPD should be more aware of their risk for cognitive impairment and more familiar with what it looks like in everyday life.
Even if you don't realize it's happening, mild cognitive impairment can make daily living more difficult and have rippling negative effects. Even minor memory problems, like misplacing bills or forgetting to turn off the stove, can cause serious problems in everyday life.
Minor cognitive impairment can also make it difficult to manage your disease and keep track of your medications and other treatments. For example, it could cause memory problems that lead you to use your medications incorrectly or skip doses accidentally, making you more vulnerable to life-threatening exacerbations, quicker disease progression, and other disease complications.
Experiencing difficulties with memory and concentration can also cause you to feel frustrated and stressed, even if you aren't aware that your symptoms are caused by MCI. This can lead to mental disorders like anxiety and depression, especially if the condition is left untreated for too long.
Luckily, COPD-related cognitive impairment can be treated and managed to minimize the symptoms and its effect on your quality of life. With healthy lifestyle changes and proper treatment, you may even be able to regain some or all of the cognitive ability you've lost, especially if you catch it early on.
Importantly, early treatment for mild cognitive impairment can prevent future cognitive decline and more serious conditions like dementia. Because it often results from low blood oxygen levels, recognizing mild cognitive impairment can also alert you to other problems that you need to address in order to better manage your COPD.
The Relationship Between COPD and Memory Loss

At first, it might seem strange that COPD, which is primarily a respiratory disease, could cause mental deficiencies and memory problems. However, a variety of studies have confirmed that there is a direct link between lung function and cognitive decline.
Research from the Mayo Clinic, for instance, found that having COPD can double your risk for mild cognitive impairment, including memory loss. The risk is even higher for people with more advanced COPD and people who use supplemental oxygen therapy.
Some people experience general cognitive impairment that affects many areas of cognition, while others only experience difficulties in one or two areas. Specific cognitive abilities that tend to be affected are memory, information processing, attention, concentration, executive function, and self-control.
However, research also shows that people with COPD—even advanced COPD—only show very slight cognitive decline. According to one study, people with severe COPD scored, on average, just one point less than people who didn't have the disease on a 35-point scale of cognitive ability.
But even though this amount of cognitive decline might seem trivial, it is not something you should ignore. Mild cognitive impairment is enough to affect everyday life and impair your ability to manage your COPD.
That's why it's important to look out for even minor symptoms, especially since cognitive impairment is much more treatable in the early stages. Recognizing the earliest signs of MCI and taking them seriously is a necessary step toward making the changes that can minimize your symptoms and prevent more serious cognitive issues in the future.
How COPD Causes Cognitive Impairment
To understand why COPD causes cognitive impairment, you have to realize that COPD is not just a simple breathing disorder. It is a disease that causes inflammation, strains your heart, and starves your body of oxygen.
One of the key links between COPD and MCI is low blood oxygen levels, known as hypoxemia, which gets worse in the later stages of the disease. This lack of oxygen affects every organ in your body, but it is especially harmful to your heart and brain.
The brain is particularly sensitive to the effects of hypoxemia because it needs so much oxygen; the brain uses up a large amount of energy and needs a continuous flow of oxgen-rich blood in order to function. Because of this, low blood oxygen levels are particularly bad for your brain, and they can lead to brain hypoxia and cognitive impairment.
As a result, memory and cognition problems are much more common in people with more advanced and severe COPD. As the the lungs lose more and more of their ability to function, blood oxygen levels drop lower and more often than they did before, increasing the risk for cognitive symptoms.
However, hypoxemia is not the only reason that people with COPD experience mild cognitive impairment. Researchers believe that a lack of physical activity could also be a cause.
After all, many studies have shown a strong link between regular exercise and better cognitive function. There are many reasons for this, but improved cardiovascular health and circulation seems to play a major role.

Unfortunately, inactivity is a huge problem among people with COPD because their breathing symptoms make exercise very difficult. However, this lack of physical activity worsens COPD symptoms and causes the disease to progress more quickly.
The result is that it becomes harder for your body to supply enough oxygen to your brain and the rest of your body. This can lead to a variety of complications including cognitive impairment and dementia.
COPD also significantly increases your risk for cardiovascular disease for many different reasons, including hypoxemia, lack of exercise, and other disease complications. Cardiovascular disease is a well-known cause of cognitive impairment, in part because it causes poor circulation and damages the blood vessels in your brain.
COPD also causes chronic inflammation, which is a major risk factor for both heart disease and cognitive decline. Researchers believe this happens in part because long-term inflammation causes harmful changes to the blood vessels and tissues in the brain.
Researchers also suspect that a history of smoking—which the vast majority of people with COPD have—can make you more prone to mild cognitive impairment. One study showed, for instance, that MCI is much more common among people who have smoked, are currently smoking, or who are exposed to secondhand smoke for at least one hour per week.
COPD and Dementia
Studies show that both COPD and mild cognitive impairment can significantly raise your risk for dementia. That's because the same conditions that cause COPD-related cognitive impairment can also cause long-term damage to your brain.
Dementia is a general, umbrella term that is used to describe a variety of different types of cognitive decline. It is much more severe than mild cognitive impairment, but it often starts with MCI that gets worse and progresses to dementia over time.
Here are some of the major signs and symptoms of dementia:
- Memory loss that significantly interferes with daily life
- Difficulty completing simple, familiar tasks
- Confusion about dates, places, and how much time has passed
- Difficulty making plans, solving problems, and keeping up with responsibilities
- Difficulties with language, including speaking, writing, keeping track of conversations, and coming up with words
- Frequently misplacing things and forgetting about major events
- Social withdrawal, including giving up on hobbies or work
One of the main ways that COPD leads to dementia is by depriving your brain of oxygen. If your blood oxygen levels stay too low for too long, it can cause permanent damage to the blood vessels and tissues in your brain.
Other COPD-related symptoms and complications can also cause dementia, including chronic inflammation and heart disease. Basically, most of the conditions that can cause mild cognitive impairment have the potential to also cause dementia if they are severe enough or happen frequently enough.
However, it's important to note that, even though mild cognitive impairment and memory loss can be early signs of dementia, they don't necessarily mean that you will develop the disease. For many people with the condition, MCI stays stable or even improves with time.
 |
| The appearance of a normal brain versus a brain with severe Alzheimer's Disease, a form of dementia. |
On the other hand, cognitive problems could be a sign that your COPD could cause, or is causing, serious damage to your brain. This is more likely to happen if your symptoms are severe or you suffer from frequent, severe hypoxemia.
If you have COPD and experience any symptoms of cognitive impairment, you need to be particularly diligent about managing your disease. By taking your medications, getting regular checkups, and living a healthy lifestyle, you can minimize your COPD symptoms and keep your blood oxygen levels high.
In many cases, it is possible to prevent COPD-related cognitive impairment and dementia with healthy living and proper COPD treatment. However, in order to do this, you might need to make some serious changes to your diet, your lifestyle, and how you manage your disease.
How to Prevent & Minimize Memory Loss Caused by COPD

If you have COPD, the best way to prevent memory loss and cognitive impairment is to keep your heart and lungs in the best shape possible. That means managing your COPD properly and building healthy habits that help you keep your body strong.
If you already have mild cognitive impairment, these same methods may even help you reverse your cognitive symptoms. At the very least, making healthy changes can prevent more severe cognitive issues and make a noticeable difference in your health and quality of life.
In the next sections, we'll show you a variety of simple things you can do in your daily life to boost your cognitive ability and prevent cognitive decline. The earlier you take action the healthier your brain will be as you continue to manage your COPD.
Exercise Your Body

Exercise is an irreplaceable tool for keeping your heart, lungs, and brain healthy, especially if you have COPD. It can improve your circulation, improve your ability to breathe, and help your body get more oxygen to your brain.
Studies show that physical fitness reduces cognitive decline caused by aging and even improves general cognitive ability. Other studies on people with COPD even suggest that exercise alone can improve at least some symptoms of cognitive impairment.
On the other hand, lack of physical activity weakens your heart and lungs, worsens breathing problems, and leads to a variety of other health complications. Inactivity is particularly hard on your cardiovascular system, leading to high blood pressure, heart disease, and worsened hypoxemia.
That's why it is so vitally important to get regular physical activity if you have COPD. That means getting at least 20-30 minutes of exercise, including light to moderate-intensity aerobic exercise (e.g. walking, swimming, or jogging), at least 3-4 times per week.
While this might seem daunting at first, don't let it scare or discourage you. You don't have to jump in all at once; you can start small and work at your own pace.
You can start with simple, low-impact activities like walking, stretching, and doing light aerobic exercises. Anything you can do to add more physical activity to your schedule will help, including hobbies like gardening.

You could also join a gym, try a sport, or take regular walks in a park you enjoy nearby. There are many different ways to exercise, and all you have to do is find a few activities that you can stick with and enjoy.
Building the habit can be difficult, but it is certainly worth the effort it takes. It can not only significantly reduce your risk for cognitive decline, but it can also strengthen your heart, reduce your symptoms, and delay the progression of your COPD.
To help you get started, we've put together several guides full of practical tips and tricks for exercising with COPD. Take a look at any of them by clicking the links below:
- Hobbies and activities that are well-suited for people with COPD
- Exercises you can do at home to improve your COPD
- How Pulmonary Rehabilitation can improve your ability to exercise with COPD
- Breathing techniques you can use to reduce shortness of breath when you exercise
Exercise Your Brain
Much like physical exercise helps keep your body strong, mental exercise can help you keep your brain and cognitive functions strong. That's why it's important to keep your brain active as you age, and especially if you suffer from COPD.
Research shows that one of the best ways to do this is by learning new things and doing activities that require mental focus. These kinds of activities strengthen important neural pathways in your brain and can even improve your mental function.
Activities that exercise your brain include things like reading, social activities, and creative endeavors like writing and painting. Other hobbies like playing chess or doing puzzles can also help keep your brain sharp.

Studies show that learning a new skill like playing an instrument or speaking a new language is particularly effective at preventing cognitive decline. You can also pick up new skills by taking a class at a local college or community center, or by joining an activity club.
In general, making an effort to use your brain in new ways and learn new things can help you preserve your memory and cognitive skills as you live with COPD. It can also reduce your chances for developing more serious forms of cognitive impairment, including dementia.
Maintain a Healthy Weight

Being underweight or overweight is bad for your brain and can increase your risk for cognitive issues, including memory problems and MCI. Unfortunately, many people with COPD struggle to
COPD affects more than 11 million people in the US, both men and women alike. However, there are some noticeable differences between how men and women are affected by the disease.
For example, in recent years, significantly more women than men have been diagnosed with COPD. Men and women can also have different COPD symptoms, and gender can even affect how quickly the disease progresses and gets worse.
Other differences show up in the doctor's office, when doctors give different care to men and women with early symptoms of the disease. This results in many women having to wait longer to get tested and diagnosed for COPD.
While these differences don't apply to every man and woman, they play a role in many people's experiences with COPD. That's why, in this post, we're going to explain this gendered phenomenon and shed some light on why it matters.
In the following sections, we'll show you how COPD affects people of opposite sexes differently and take a closer look at where these differences come from. We'll also explain what these differences actually mean for men and women who have—or who are at risk for developing—COPD.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Differences Between COPD in Women and Men
It is possible for just about anyone to get COPD, but the disease does not affect all groups of people equally. This is reflected in the fact that people from different regions, nationalities, and sexes tend to get the disease at different rates.
However, this is not because the disease is fundamentally different in different types of people. Rather, it's because COPD is linked to secondary factors that tend to affect people in certain groups more than others.
In other words, when it comes to gender, COPD is associated with traits that tend to differ between men and women. Some of these differences are rooted in biology, but many of them are instead rooted in lifestyle and behavior.
In general, you can divide these differences into three main categories:
- Differences in risk, or how likely men and women are to develop COPD
- Differences in disease, or how COPD affects men's and women's bodies differently
- Differences in psychological symptoms
Differences in Risk
In general, women seem to have a higher risk of developing COPD than men. There are many potential reasons for this, but hormones and physical traits, like smaller airways in women, likely play a role.
This difference seems to be significant, especially among people who smoke tobacco, which is the number one cause of COPD. Research shows that women who smoke less than men actually tend to experience worse lung function decline.
This means that women who smoke are more likely to develop COPD and other lung diseases. Women are also more likely to develop symptoms of COPD at an earlier age.
Statistics show that about 58 percent of people who have COPD are women, and that women make up a slightly higher percentage—53 percent—of those who die from COPD. When you consider that about 15.5 million people in the US have been diagnosed with the disease, that adds up to about 9 million women and 6.5 million men with COPD.
However, this is a relatively recent phenomenon that is strongly tied to an increase in the number of women who smoke. Before the mid-1950's, it was largely men who smoked tobacco and later developed COPD.
Differences in Disease
A person's biological sex plays a role in how COPD affects their lungs. Because of this, men and women sometimes experience different COPD symptoms, and even differences in the overall severity of their disease.
For instance, COPD seems to progress more quickly in general in women than in men. This means that women with COPD often experience earlier and more severe lung function decline.
As a result, women's symptoms tend to be more severe—sometimes significantly more severe—and also tend to show up earlier in the disease. Women tend to experience worse shortness of breath, more frequent exacerbations, and are also more likely to die from COPD.
Men and women with COPD also tend to experience slightly different types of COPD (e.g. emphysema or chronic bronchitis), which can lead to different symptoms.
Men, for example, are more likely to have COPD dominated by emphysema, which tends to cause more fatigue-related symptoms. Women, on the other hand, tend to have worse chronic bronchitis, which causes more coughing and airway obstruction from mucus.
Additionally, while the death rate for men with COPD has fallen in recent years, the death rate for women has remained the same. While researchers aren't exactly sure why this is, declining smoking rates in men and quicker disease progression in women are the most likely culprits.
Women with COPD are also more likely to experience certain COPD complications like osteoporosis. This is partially due to the fact that osteoporosis is more common in women in general, but worse COPD symptoms in women also play a role.
Differences in Psychological Symptoms
Anxiety and depression are extremely common side effects of COPD. In fact, researchers estimate that up to 40 percent of people with COPD suffer from clinical depression while up to 20% suffer from clinical anxiety.
However, studies show that women with COPD are much more susceptible (PDF link) to these psychological disorders than men. This is likely influenced by a combination of several different factors, including the severity of COPD symptoms and high rates of anxiety and depression in women overall.
For instance, the fact that women experience worse symptoms and disease outcomes than men is enough on its own to explain much of this difference. More severe symptoms would naturally lead to more health-related stress, causing a higher incidence of anxiety and depression in women.
It is also worth noting that women, in general, tend to have significantly higher rates of anxiety and depression across the board. It is likely that the same factors that cause this general predisposition also apply to women with COPD.
Why Does Gender Affect COPD?
As you can see, there are a variety of important differences between how men and women are affected by COPD. However, while the facts and statistics are relatively straightforward, they don't exactly explain why these differences exist.
But before you can understand the reasons, you need to know how people develop COPD in the first place. Once you understand that, it's easier to see why certain groups of people (e.g. women) tend get COPD more often—and more severely—than others.
To put it simply, COPD is a breathing disorder caused by lung damage. It causes two main things to happen: it reduces the lungs' ability to absorb oxygen, and it narrows the airways so less air can flow through the lungs at a time.
This lung damage can be caused by many different things, namely diseases or substances that cause repeated irritation and inflammation in the lungs. For example, smoking, noxious chemicals, and other diseases like asthma can all cause COPD.
So, what does all this have to do with differences between the sexes? It's simple: COPD is caused by physical traits and patterns of behavior. Since men and women have different physical traits and different patterns of behavior, this naturally leads to differences in how likely men and women are to develop COPD.
For instance, in a biological sense, women tend to have smaller airways, which makes them more susceptible to damage. From a lifestyle perspective, however, men are more likely to work in occupations that could expose them to dangerous respiratory toxins.
Because of this, the differences between men and women with COPD are not always 100% consistent or clear cut. And, as men and women's habits and lifestyles change, so does their relative likelihood of developing COPD.
It is also important to realize that men and women do not always receive the same kind of medical care. This is another factor that could account for some of the differences we see between men and women with COPD.
Biological Differences

Men and women have different biological traits that affect their experiences with COPD. As we mentioned earlier, these differences can influence how likely someone is to develop COPD, what symptoms they have, and how quickly the disease progresses.
A person's biological sex influences both their physical traits and important hormones that regulate their health. Both of these factors can influence your likelihood of developing COPD as well as how your body responds to the disease.
The Effect of Airway Size
Studies show that women tend to have smaller airways than men, but not smaller lungs. This is a factor that could make some people more likely to develop COPD than others, and could partially explain why women seem to be more prone to COPD.
First of all, smaller airways could make women more sensitive to respiratory toxins like smoke. Because women have less total airway tissue, each bit of tissue gets exposed to proportionally more toxins when they breathe.
Compare a male smoker and a female smoker, for instance, who both have similarly-sized lungs but differently sized airways. When the man inhales smoke, the smoke will come into contact with a larger amount of airway tissue, since he has larger airways than the woman.
On the other hand, when the woman inhales smoke, the smoke comes into contact with a smaller surface area of tissue overall. However, she still inhales the same amount of smoke and toxins, meaning that the woman's airways are exposed to a higher “dose” of toxins per area than the man's airways.
This could explain part of the difference between men's and women's risks for developing COPD. Since women have smaller airways, they could be more prone to the damaging effects of cigarette smoke and other respiratory irritants.
The Influence of Hormones
Some researchers believe hormone activity could play a major role in how COPD progresses differently in women than in men. Having more estrogen, in particular, could make women's lungs more susceptible to damage from things like air pollution and smoke.
Researchers believe that estrogen worsens oxidative stress in the lungs, which could explain why smoking tends to affect women more severely. Oxidative stress occurs anytime the lungs and airways get inflamed by a respiratory irritant or infection.
Too much oxidative stress can damage the delicate tissue in the lungs, causing permanent scarring over time. COPD makes the lungs particularly sensitive, causing them to experience oxidative stress more frequently and severely.

Researchers have long noticed that women with COPD seem to have more lung scarring than men, and that the scarring tends to happen earlier on in the disease. This is true even for men and women with similar smoking histories who have lived with the disease for the same amount of time.
Because of this, women tend to have worse lung function and respiratory symptoms by the time they are diagnosed with COPD. The disease also progresses faster and causes death sooner in women than in men.
More recent studies have revealed that this effect could be caused by estrogen. Research shows that estrogen can significantly increase oxidative stress in the lungs, and experts believe this could make women more prone to both the risk factors and effects of COPD.
Since women produce more estrogen, their lungs and airways get exposed to extra oxidative stress any time they breathe in a respiratory irritant like smoke. This leads to worse and earlier airway tissue scarring in women with COPD compared to men.
This could also explain why women who smoke seem to experience quicker lung function decline than men. Estrogen could make their lungs more sensitive to respiratory irritants in general, putting women smokers at a higher risk for developing COPD and making women's COPD symptoms worse.
Genetic Diseases and Traits
Certain genetic traits might give some people a higher risk of developing COPD than others. However, while researchers know that genetics play some role in COPD, they still are not sure which genes those are or how they work.
It is certainly possible, for instance, that certain genes could predispose either men or women to develop COPD more easily. This is an ongoing area of COPD research, and more answers are likely to come in the future as researchers continue to untangle the genetic complexities of the disease.
Lifestyle Differences
On average, men and women tend to live different lifestyles, with different hobbies, occupations and household roles. While no man or woman is the same, there are, statistically, certain jobs, habits, and activities that either men or women are more likely to do.
These different lifestyles that men and women tend to choose have a significant effect on how likely they are to get exposed to harmful substances. And, as we know, how much someone is exposed to respiratory toxins is directly related to their likelihood of developing COPD.
Smoking

Cigarette smoking is the number one cause of COPD. As such, it is the most important factor in an individual person's risk for developing COPD.
One of the clearest ways to see this effect is to look at the changing rates of COPD among men and women over the years. In the mid-1900's, the vast majority of people with COPD were men; however, this changed in the late 1900's, as more women than men started to get diagnosed with the disease.
This change might seem strange until you realize that it is directly correlated to a major cultural phenomenon: more and more women started to smoke. Before then, a much larger percentage of smokers were men, and COPD was considered a male-dominated disease.
However, once this new generation of women smokers began to age, more and more cases of COPD began to show up in women. In fact, since 1980, the number of women who die from COPD every year has more than quadrupled in size (PDF link).
This made it clear that COPD wasn't a man's disease, but rather a smoker's disease, instead. Today, there is less of a gap between the percentage of men and women who smoke, and about 18 percent of men and 14 percent of women in the US are smokers.
This is the perfect example of how rates of COPD in a group can reflect lifestyles and habits that people in the group tend to share. After all, COPD used to be considered a “man's disease,” but this was almost entirely due to the fact that most cigarette smokers at the time were men, not any biological factor.
The Snowball Effect of Having Worse COPD Symptoms

People who experience worse COPD symptoms also have a reduced ability to exercise and do activities that require physical strength. This makes them less likely to get enough physical activity and more prone to sedentary lifestyle.
This can create a snowball effect that has significant consequences for both mental and physical health. Since women with COPD generally have worse lung function and symptoms, they are also more likely to succumb to this negative cycle.
The consequences can be serious: studies show that not getting enough exercise can significantly worsen both the physical and psychological symptoms of COPD. Studies on the general population also support the idea that physical activity is a powerful tool for combating anxiety and depression.
For both men and women, COPD and depression have a circular, or “bi-directional” relationship. This means that worse COPD symptoms can lead to depression, and that depression can lead to worse COPD symptoms.
This happens for many reasons that have to do with living a healthy lifestyle in general. People who are depressed are more likely to live unhealthy, sedentary lives, and people who live unhealthy, inactive lifestyles are more likely to be depressed.
For instance, studies show a very strong correlation between COPD patients' lung function and their likelihood of being depressed. Worse lung function leads to worse shortness of breath, which in turn leads to higher rates of depression.
As we've discussed already, women with COPD tend to have worse symptoms and worse lung function than men. Thus, it makes sense that women with COPD are also more likely to suffer from depression.
Worse symptoms leads to less physical activity and fewer opportunities to benefit from the protective psychological effects of exercise. This leads to a generally unhealthy and sedentary lifestyle that speeds up psychological, physical, and lung function decline.
Losing strength and endurance also makes it more difficult, or even impossible, to participate in many kinds of normal activities. As a result, many people with severe COPD start to give up on hobbies and other things they enjoy in life, leading to social isolation and depression.
The snowball effect of worse symptoms, less exercise, and worse health also seems to make women more prone to certain COPD complications. It leads to more frequent lung infections, more frequent exacerbations, and puts women even more at risk for other health conditions like osteoporosis.
Occupation

In general, more men than women work jobs that put them at risk for COPD. These jobs include any occupation that exposes workers to dangerous levels of respiratory irritants such as noxious chemicals, smoke, and dust.
Studies show that the jobs that put you most at risk for COPD include coal mining, hard-rock mining, concrete manufacturing, tunnel work, non-mining industrial work, welding, and construction. As it so happens, the vast majority of employees who work in these occupations are men.
Some studies suggest that particular air pollutants, such as chlorine, silica dust, cement dust, and welding fumes pose a greater risk than others. Overall, researchers estimate that occupational exposure causes up to 21 percent of all COPD cases.
Household Tasks

While men tend to dominate many occupations that cause COPD, there are other hazardous jobs and activities that more women than men tend to do. This includes household tasks like cooking and cleaning, which, despite changing gender norms, are still done more often by women than men.
Many studies have shown that both cooking and cleaning expose your lungs to harmful respiratory irritants. Cooking exposes your lungs to aerosolized oils and other toxic chemicals, while common cleaning chemicals emit noxious fumes that can damage your lungs.
This puts men and women who cook and clean frequently for many years at a significantly higher risk of developing COPD. One study, for example,
Pulmonary nodules—or spots on the lung—are the source of a great deal of worry and stress for the thousands of people who are diagnosed with them every year. Despite the fact that pulmonary nodules are relatively common, the majority of people don't really understand what they are or how they work.
Many people's first thought is that pulmonary nodules are cancer—but this is not always true. In reality, most pulmonary nodules are harmless, and only a very small percentage of them turn out to be cancerous.
If you or someone you love has been diagnosed with lung spots, then you might be worried and you might have a lot of questions. In this guide, we hope to answer these questions and give you all the information you need to better understand pulmonary nodules and the level of risk they pose.
In the following sections we'll explain what pulmonary nodules are, what causes them, and what they mean for your health. We'll also take a closer look at the connection between pulmonary nodules and cancer, as well as how pulmonary nodules are related to other lung conditions like COPD.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
What Are Pulmonary Nodules?

A pulmonary nodule is simply a small, circular-shaped patch of irregular tissue on the lungs. These patches usually show up after something, like an infection, irritates or damages part of your lung.
Pulmonary nodules are relatively common and often harmless, but they can be cancerous in some cases. You can have just one pulmonary nodule, or you could have several or many nodules on your lungs
Most pulmonary nodules are healed-over wounds—scar tissue, essentially—left behind after a period of inflammation. This inflammation can be caused by a variety of things, including lung infections and certain inflammatory diseases like sarcoidosis and rheumatoid arthritis.
On the other hand, some pulmonary nodules are not created by patches of inflamed tissue, but rather cancerous cells. These cancerous pulmonary nodules are essentially tumors, made up of mutated cells that quickly grow and spread.
Pulmonary nodules are often referred to as “coin lesions,” “spots,” or “shadows” on the lungs, since that's how they appear on scans. On a chest x-ray, for instance, a pulmonary nodule shows up as a small, light-colored or grey-ish spot on the lungs.
Most pulmonary nodules are very small, usually between about ½ inch to a little more than 1 inch wide. They usually don't cause any symptoms, but symptoms are more likely to show up if the nodule grows into a larger lesion (greater than 3cm), known as a mass.
In rare cases, pulmonary nodules can cause respiratory ailments similar to a cold or mild flu. In severe cases, they can cause wheezing, shortness of breath, coughing (or coughing up blood), and respiratory infections.
Are Pulmonary Nodules Serious?

Generally, pulmonary nodules are nothing to worry about. Research shows that they are surprisingly common, asymptomatic, and only carry a “minimal risk” for cancer.
In fact, it is not unusual for someone to have pulmonary nodules for years without even knowing. Since they don't cause any symptoms, most people don't figure out they have spots on their lungs until they show up on an unrelated chest scan.
If you are diagnosed with a pulmonary nodule, don't panic; chances are good that—like most pulmonary nodules—the spot on your lungs is benign. Even cancerous pulmonary nodules tend to be very treatable, since they usually represent an early stage of cancer.
Types of Pulmonary Nodules

There are several different varieties of pulmonary nodules you can get. They are generally differentiated by their cause and whether they are cancerous or benign.
Pulmonary Nodules Caused by Inflammation
A common cause of benign pulmonary nodules is infections and inflammation in the lungs. These can be caused by a variety of things, including:
- Bacterial, fungal, or parasitic infections in the lungs
- Inflammatory diseases like rheumatoid arthritis
- Repeated exposure to lung irritants like smoke
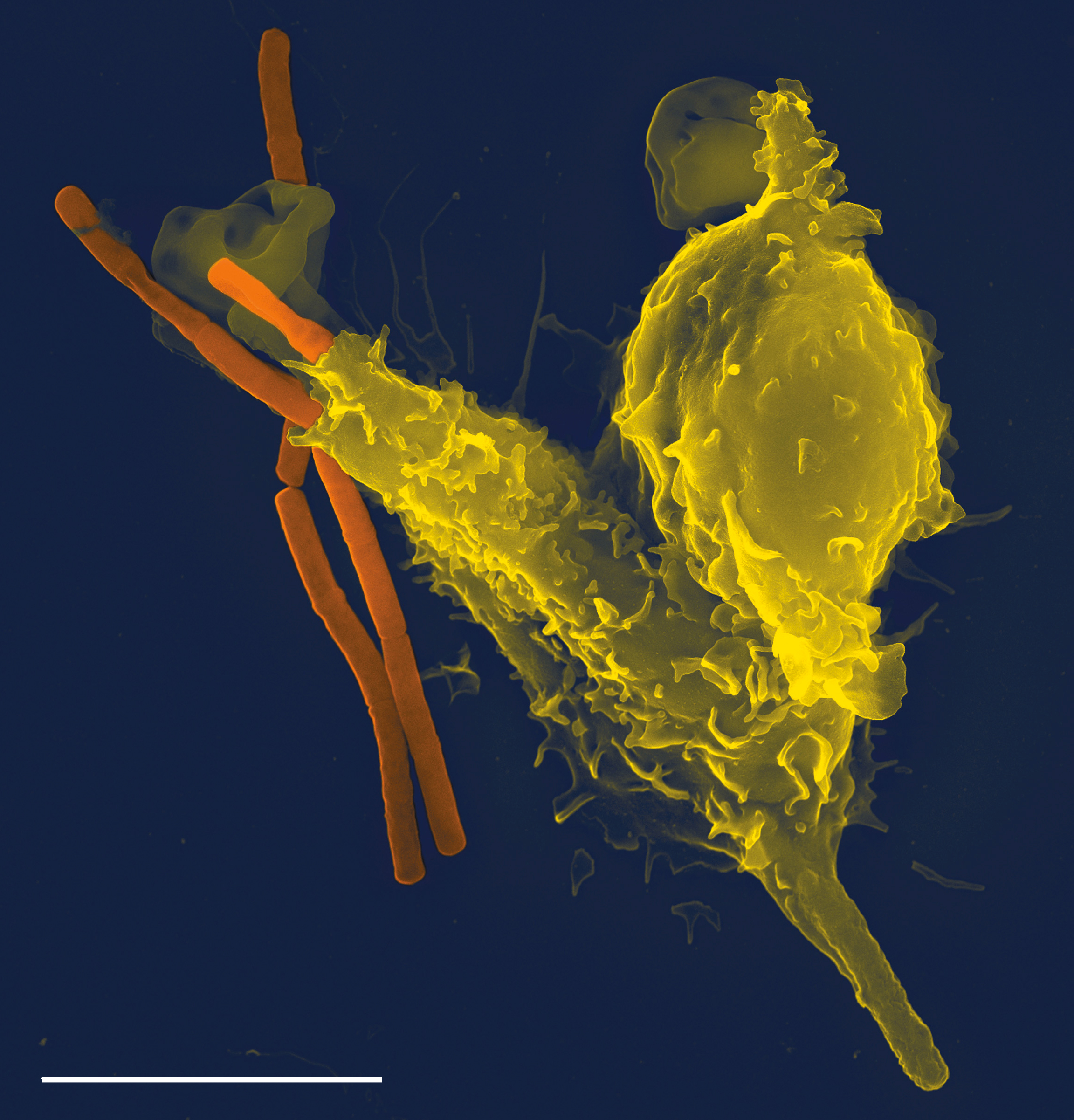
This kind of pulmonary nodule forms as a side-effect of your body's inflammatory response. This response gets triggered whenever your body detects irritation or infection in your lungs, and it helps your immune system fight off the invader.
As part of the inflammatory response, a granuloma, or a small patch of inflamed tissue, can form at the site of irritation or infection. Granulomas are your immune system's way of isolating the infection and preventing it from spreading to surrounding areas.
However, over time calcium deposits can form in the granuloma, leaving behind a permanent spot of calcified tissue. That spot is now a pulmonary nodule that can show up on chest scans long after the original source of irritation is gone.
This type of of pulmonary nodule is usually harmless, asymptomatic, and doesn't grow or change. It is like a scar; just a patch of tissue that's healed over but looks slightly different than it did before.
However, it's difficult to know if inflammation is the cause of a pulmonary nodule without doing further testing. If your doctor has any doubt that it could be cancerous, he will need to monitor the spot to make sure it doesn't grow.
Here is a list of some infections that can cause pulmonary nodules:
- Tuberculosis
- Mycobacterial infections
- Histoplasmosis
- Blastomycosis
- Aspergillosis
- Coccidiobycosis
- Roundworms (ascariasis)
- Hydatid cysts (echinococcus)
- Liver flukes (paragonimous)
Here is a list of some of the common inflammatory conditions that lead to pulmonary nodules:
- Rheumatoid arthritis
- Sarcoidosis
- Granulomatosis with polyangiitis
- Pneumoconioses
Pulmonary Nodules Caused by Cancer

Cancerous pulmonary nodules usually represent a very early form of cancer. They are essentially small, cancerous tumors that, without treatment, would grow larger and spread throughout the lungs.
Luckily, finding a cancerous pulmonary nodule means that you've caught the cancer at it's smallest stage, before it has the chance to grow into a larger tumor, or mass. In fact, the survival rate for most people with a single cancerous nodule is extremely high, up to 70-80 percent.
In rare cases, however, pulmonary nodules can be caused by a metastatic cancer. Metastatic cancers are aggressive forms of cancer that spread between organs in the body, and they can cause cancerous pulmonary nodules if they spread to the lungs.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Nodules that are caused by metastatic cancers are usually numerous rather than a single isolated spot. Unlike early-stage pulmonary nodules, nodules caused by metastases are the result of a more serious, later-stage cancer.
Cancerous pulmonary nodules tend to be larger and have more irregular shapes. They are also more likely to appear on a scan as a spot with hazy margins rather than solid, defined edges.
Here is a list of some of the common cancers that cause pulmonary nodules:
- Lymphomas
- Sarcomas
- Carcinoid tumors
Pulmonary Nodules Caused by Benign Tumors
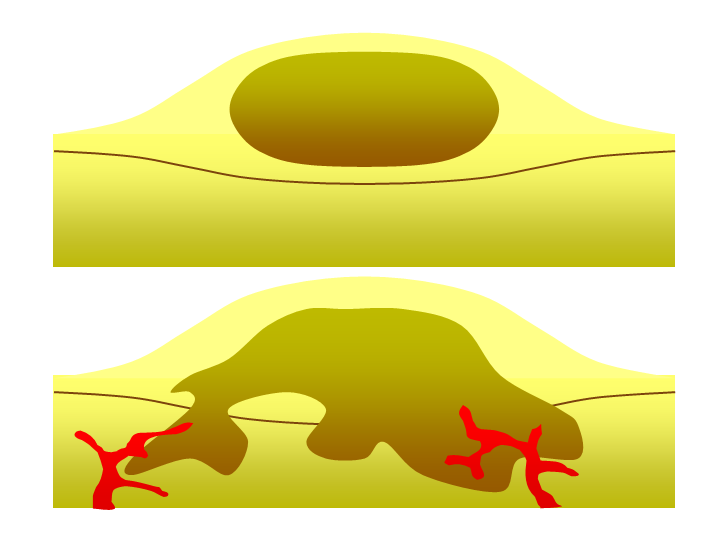
Benign tumor (top) versus malignant tumor (bottom).
Certain types of benign (non-cancerous) lung tumors can show up as pulmonary nodules on scans. These tumors are generally made up of a disorganized mass of cells, but but they do not grow or spread like cancerous tumors do.
Because they are so small, pulmonary nodules caused by benign tumors don't usually cause any symptoms. Most are harmless growths that can be left alone without any further treatment.
However, if a nodule forms in certain places in the lung (e.g. near an airway opening), it can obstruct airflow and cause respiratory symptoms. If this happens, or the tumor causes other symptoms, you may need to have it removed through surgery.
Here is a list of some of the most common types of benign tumors that cause pulmonary nodules:
- Hamartomas (the most common type)
- Blastomas
- Fibromas
- Neurofibromas
- Bronchial adenomas
- Hemangiomas
Other Causes of Pulmonary Nodules

Some types of pulmonary nodules don't fit easily into the any of the categories above. These include nodules caused by blood vessel abnormalities, protein deposits, and other lung conditions.
Here is a list of some of the miscellaneous potential causes of pulmonary nodules:
- Blood vessel abnormalities: e.g. AV malformations
- Amyloidosis: a condition that causes abnormal protein deposits in tissues
- Pulmonary Fibrosis: a serious lung condition resulting from scarred lung tissue
- Atelactasis: the partial collapse of a lung
Who Gets Pulmonary Nodules?

It is not uncommon for someone who develops pulmonary nodules to have an existing respiratory disease such as COPD. However, many people who are diagnosed with pulmonary nodules have had no other respiratory problems up to that point.
People who have a history of smoking are also more likely to have pulmonary nodules than people who have never smoked. Smoking also increases the risk that a pulmonary nodule is cancerous.
However, just about anyone can get a pulmonary nodule, both smokers and non-smokers alike. Basically, if you have lungs, then that means you can get pulmonary nodules.
In fact, so many people have spots on their lungs that they show up on about 50 percent of all chest CT scans and 0.2% percent of chest x-rays. In fact, some estimate that more than half (PDF link) of all adults over the age of 50 have nodules on their lungs.
Is My Pulmonary Nodule Cancerous?

While some pulmonary nodules are cancerous, the vast majority of them are not. (PDF link). In fact, several studies suggest that only about 5 percent of pulmonary nodules found via CT scan turn out to be cancer; the other 95% of the time, they are benign.
However, certain factors can increase the likelihood that your pulmonary nodule is cancerous. For instance, the risk of cancer is higher if the nodule is large, if you are over the age of 40, or you have a history of smoking.
Nodules found via chest x-ray also have a higher risk of being cancerous, simply because only larger pulmonary nodules show up on x-ray scans. X-ray technology is not as sensitive as a CT scan, meaning smaller pulmonary nodules—which are more likely to be harmless—are much more likely to show up on a CT scan than a chest x-ray image.
Most of the time when someone is diagnosed with a pulmonary nodule, doctors recommend simple monitoring to see if the spot grows. That means taking additional scans of the lungs—usually about six months apart—and comparing the images to look for any changes.
If the nodule doesn't get larger over time, then it's likely that it is benign. In fact, there is usually no need to continue doing scans if the images show that the spot hasn't grown for two full years.
However, if the nodule does grow, there is a higher chance that it could be cancerous. But in order to know for sure, you will need to get the spot analyzed through a biopsy, which we'll discuss this more in sections below.
Fortunately, cancerous pulmonary nodules are most often a very early, very treatable stage of lung cancer. It is much better to catch lung cancer at this stage rather than later, when the cancer has grown, spread, or begun causing symptoms.
Factors that increase the risk that a pulmonary nodule is cancerous:
- The pulmonary nodule is large (e.g. more than 30 millimeters across)
- The pulmonary nodule grows over time (as tracked via chest scans)
- The pulmonary nodule's borders are irregular, spiky, or blurry (instead of rounded and well-defined)
- The nodule is not calcified (calcified nodules are usually benign)
- The nodule is located in an upper lobe of the lung
- You have a history of smoking
- You are over the age of 40
- You have COPD
- Your have a family history of cancer (especially lung cancer)
- You have been repeatedly exposed to substances that can cause lung cancer, especially through your occupation (e.g. diesel fumes, chemical solvents, second-hand smoke, etc.)
Pulmonary Nodules and COPD

Many people with COPD also have pulmonary nodules. However, the two conditions are not directly related; COPD does not directly cause pulmonary nodules and pulmonary nodules do not cause COPD.
Instead, it is likely a combination of shared risk factors that causes pulmonary nodules to be more common in people with COPD. Both conditions are the result of damage to the lungs, which can occur for a variety of health and lifestyle reasons.
Smoking, for instance, is perhaps the most significant risk factor that both COPD and pulmonary nodules share. Both conditions can be caused or worsened by the repeated inflammation that occurs when you smoke for many years.
Put simply, the same things that cause lung damage that leads to COPD can also cause lung damage that leads to pulmonary nodules. This is the most likely reason that pulmonary nodules are more common in people with COPD.
The fact that COPD is, in part, an inflammatory condition, could also be a factor. Lungs affected by COPD are much more prone to inflammation than healthy lungs, which creates more opportunities for granulomas, cancer, and pulmonary nodules to form.
Lung infections are another cause of pulmonary nodules that are also linked to COPD. It is common for people with COPD to experience frequent respiratory infections, which can in turn raise their risk for developing nodules on their lungs.
Unfortunately, lung nodules in people with COPD also carry a higher risk of being cancerous. That's because COPD is itself an independent risk factor for lung cancer, even when you ignore the common risk factor of smoking.
How Pulmonary Nodules are Treated
Most people first find out they have pulmonary nodules when they get a CT scan. Often, the scan is being done for an unrelated reason when a doctor notices a lung spot (or spots) on the image.
After discovering the nodule, your doctor will likely ask you some questions about your health and lifestyle. This allows him to look for any factors that could indicate a higher risk of lung cancer.
Your doctor will use this information as well as the characteristics of the spots on the scan to estimate the risk that the nodule is cancerous. Then your doctor will likely decide to do one of three things: ignore the nodule, do a biopsy, or monitor the nodule to see if it grows.
Often, the next step is simply to keep an eye on the spot to see if anything changes. However, your doctor may want to test the spot for cancer right away if it shows cancerous characteristics, if you have symptoms, or your have other significant risk factors for lung cancer.
Monitoring the Spot
After getting diagnosed with a pulmonary nodule, your doctor may choose to take a “wait and see” approach. That requires taking more CT scans in the future—often about 6 months apart—to monitor the spot over time.
Your doctor will compare the new scans with previous images of your lungs to look for signs of cancer. If the nodule grows or shows cancer-like changes, then you will need further testing to figure out if it's cancerous or benign.
Most of the time, however, pulmonary nodules do not grow between scans and turn out to be benign. If it shrinks or shows no change over the span of two years, then it means the spot is most likely cancer-free and there's no need to monitor it anymore.
Testing Pulmonary Nodules for Cancer
If your doctor suspects that your pulmonary nodule is cancerous, then he will order a biopsy of the spot. That means taking a small sample of the tissue to analyze it more thoroughly for signs of cancer.
There are three main ways to do this: by inserting a needle through the chest wall, by performing chest surgery, and by using a bronchoscope. A bronchoscope is the least invasive method, and it works by inserting a scope down the throat and into the airways to take the sample directly in the lungs.
Once they get the tissue sample from the lung nodule, an expert will then take a closer look at the tissue to look for signs of cancer. Even if the nodule appears to be benign, your doctor might decide to monitor it for awhile just to be sure. If it is cancerous, then your doctor will refer you to an oncologist who will put together a full cancer treatment plan.
Treatment for Benign Pulmonary Nodules
If your doctor confirms that your pulmonary nodule is benign, then you probably won't need any further treatment. However, you might need medication if your nodule is the result of a current infection.
If an inflammatory disease is the cause of your pulmonary nodule, then you may need treatment to get the underlying condition under control. For example, your doctor may prescribe anti-inflammatory medications like corticosteroids to reduce inflammation in your lungs.
What You Can Do: Don't Panic
If you or someone you love has just been diagnosed with pulmonary nodules, you should do your best not worry. Remember that most lung spots are not cancerous and won't do any harm.
Unfortunately, evaluating pulmonary nodules is often a waiting game. Your doctor will likely need time to monitor the spot and look for growth or other changes.
This “wait and see” approach can be frustrating and scary when you're anxious to know the results. But if you can manage not to panic, the wait will be much easier to bear.
Of course, it's only natural to worry after you get diagnosed with a pulmonary nodule. It can help to talk to your doctor, who can help you understand the condition and tell you more about your personal risk.
Learning more about pulmonary nodules can also help you feel less worried. The knowledge can eliminate the fear that comes from facing the unknown and help you feel more secure.
After reading through this guide, you should know much more about pulmonary nodules, how they get diagnosed, and how they're connected to COPD and other health conditions. This should help you understand your diagnosis and what having a spot on your lungs actually means.
COPD is a chronic respiratory disease that impairs your breathing capabilities, and due to the deprivation of oxygen, the disease will affect other aspects of your life beyond the function of your lungs. If your body cannot process the oxygen in the air enough for your body, parts of your brain will, in some cases, be affected by this.
This is not something that should frighten you, however, many people will chalk up forgetfulness to be associated with older age, or being too busy, or having too much on their mind. Every time you think to yourself, “Where did I put that” or “ What was I about to do?” you should also think about becoming more aware of what this means for you.
Especially if you have COPD, mindfulness and attention to details can go a long way in creating a more habitable living space both physically but also inside your mind.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Similarly to COPD, Mild Cognitive Impairment (MCI) has no cure, however, there are ways you can work to prevent it from affecting you severely.
Cognition is associated with learning, memory, and thinking. So, cognition is about your language, memory, how you learn, reasoning, recognizing, and categorizing. It is how we see our environment and how we adapt to it. All of which will progress, change, and be affecting by time and your age.
However, if you have COPD, age may not be the main factor in your cognitive decline. Due to the symptoms associated with COPD there is a risk that you will experience MCI and other memory issues.
In general, mild cognitive impairment (MCI) is a condition that causes minor problems with memory, focus, problem-solving, and attention. It happens to many people as they age, but respiratory diseases like COPD can both trigger and accelerate the condition.

If you experience forgetfulness or worry that your mind is not as “sharp” as it used to be, you are actually experiencing the symptoms of mild cognitive impairment. However, MCI is slightly worse than the normal changes to memory and cognition you'd expect to see with age alone.
Mild cognitive impairment happens when your brain's cognitive functions are slightly lower than they should be. It can result from both temporary problems like oxygen deprivation and permanent changes that occur when you experience structural damage to your brain.
The National Center for Biotechnology Information advances science and health journal suggests that mild cognitive impairment is very common, affecting about 10-20 percent of people over the age of 65 and about 36 percent of people with COPD.
Fortunately, mild cognitive impairment is a treatable, and sometimes even reversible, condition that can improve with diet, exercise, and other lifestyle changes.
How to improve Mild Cognitive Impairment

Exercise:
You need to exercise every day with COPD, we have talked about exercise in almost every blog post about COPD since the beginning of time. And while it does help to strengthen your lungs, exercise does more than that.
Many studies including work from the JAMA Network, suggests exercise can provide better blood flow to your brain releasing molecules that could repair your brain and prevent it from getting worse. By exercising, your body will release serotonin and endorphins that will help make you want to exercise more frequently, which is a very healthy cycle!
Diet:

The National Center for Biotechnology Information published a study that concluded there are significant associations with the risk of MCI and a person’s diet. This means that a moderate intake of cooked white rice and an adequate intake of whole grains, fruits, milk, and dairy products were associated with reduced risks of MCI among adults aged over 50 years.
Having a diet rich in vitamins and minerals keeps our brain happy and allows you to be more active.
Mindfulness and Meditation:
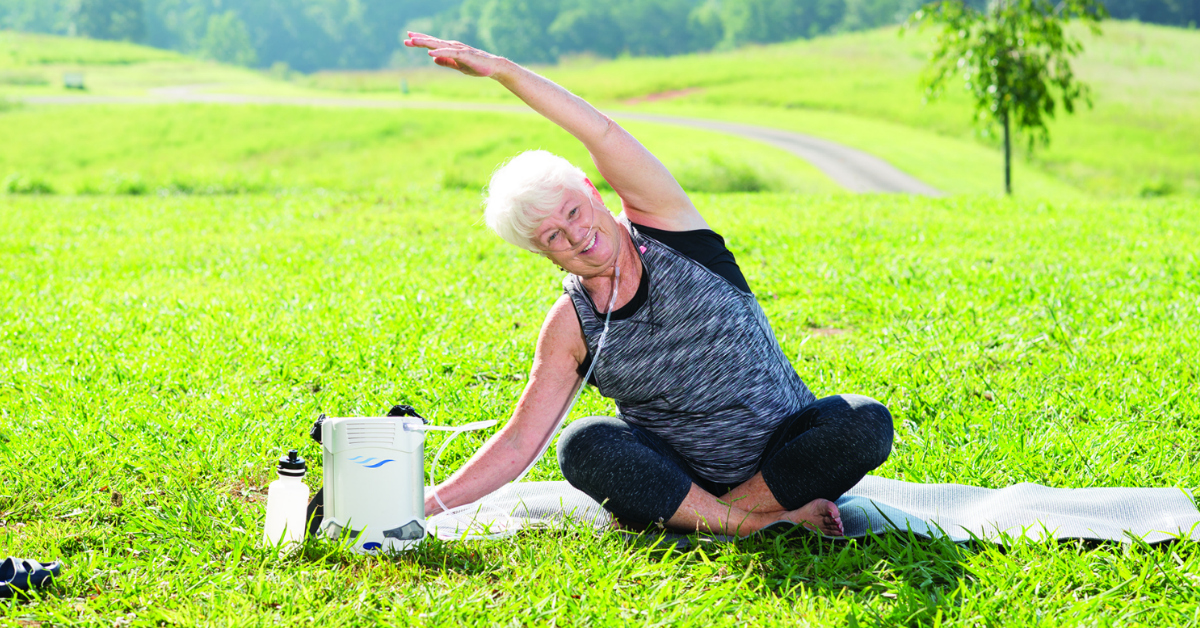
Medication and other mindfulness exercises can help calm your mind and allow you the space you need to keep things in perspective. Findings in a De Gruyter publishcation study recommended that there be future studies on meditation-based treatment for MCI and stress management because of how influential the practice was when used to treat these cognitive impairments, and more information should be processed to understand this phenomenon further.
Games and puzzles:
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Engaging in mentally stimulating games and puzzles can make a huge difference in the prevention and treatment of MCI. Just like exercise for your muscles so they get stronger, it is important to work out the neurons in your brain. By doing mind games and puzzles, your brain will be able to make connections and you can work to keep those connections and neurons strong and firing.
COPD, MCI, and oxygen therapy

So the connection between COPD and MCI is very strong, and studies showed that patients with COPD had an increased risk for MCI by about 83 percent. These patients who had COPD for more than five years had a greatest risk for MCI.
The reason behind the connection is still not completely understood, and research suggests that COPD is associated with risk of MCI. The next step for researchers is to understand the exact mechanisms by which COPD increases the risk of MCI.
Until then, oxygen therapy, either by utilizing oxygen tanks or portable oxygen concentrators, can be beneficial for improving memory and other symptoms associated with COPD induced MCI.
If your blood oxygen saturation is below 90 percent, that means you're not getting enough oxygen to meet your body's needs and you likely need supplemental oxygen therapy. If you already use supplemental oxygen, experiencing mild cognitive impairment could be a sign that your oxygen prescription needs to change and you should discuss this with your doctor as soon as possible.

In this case, your doctor may decide to increase your oxygen dosage or instruct you to use supplemental oxygen more often. You might also need to start using oxygen while you sleep, since nighttime oxygen deprivation is a common cause of MCI.
Understanding COPD and MCI
If you have been diagnosed with COPD, it is crucial that you take daily notes of your symptoms and which aspects of your life are being affected. By understanding what is happening in your body and mind, you and your doctor, will be able to set up a treatment plan that is special for you whether that means beginning on oxygen therapy, or starting a pulmonary rehab course.
If you begin to realize that your memory or aspects of your cognition are worsening, this could be attributed to your COPD, and there are ways that you can begin to reverse or slow down mild cognitive impairment from advancing into a more severe state.
If you focus on treatments that will help your MCI, you are also working towards a healthier lifestyle with COPD. These treatments over-lap, like eating brain healthy foods, exercising regularly, meditating, and doing puzzles and playing mind games, while also being prudent to use supplemental oxygen therapy will all contribute to slowing down the progression of both COPD and MCI.
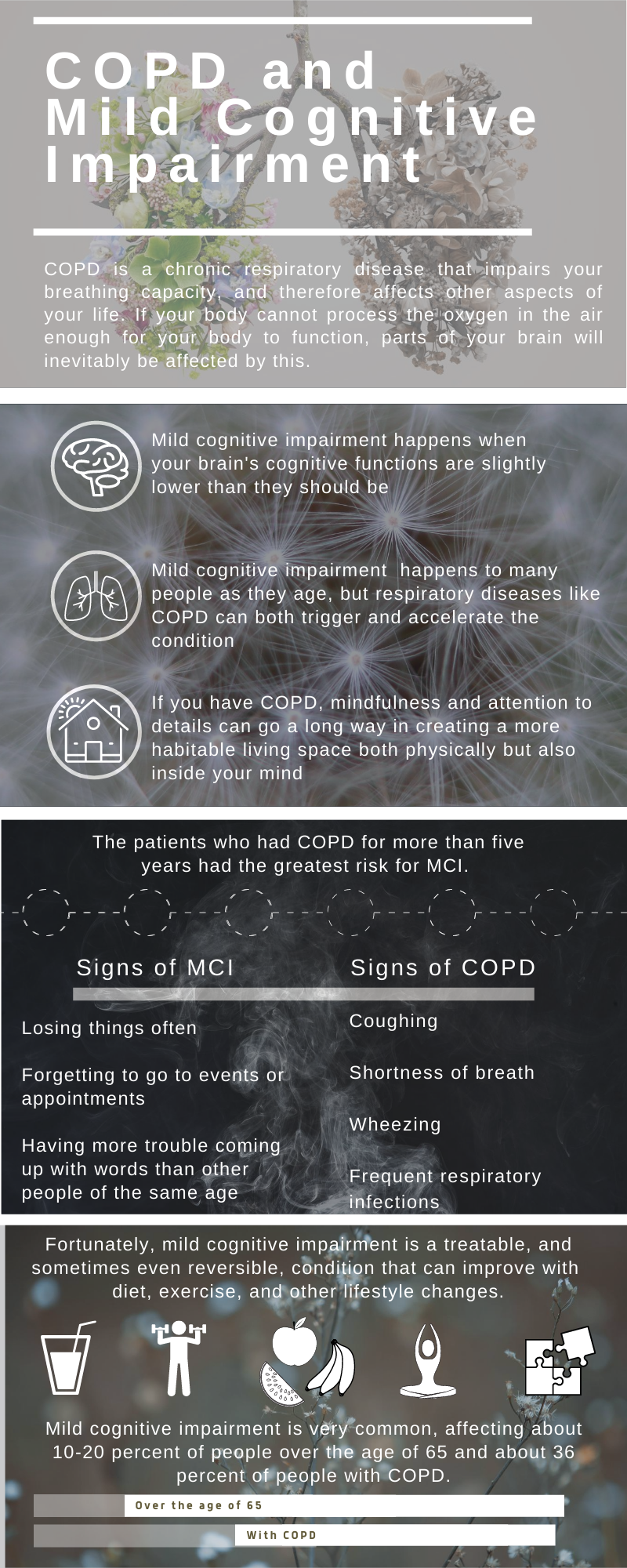


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













