.png)
Telehealth is defined as “the use of telecommunications to provide long-distance administration of healthcare services for patients.” if you’re having trouble putting this into perspective, you’ve likely already used some form of telehealth services in the past. Scheduling a doctor’s visit by phone or through the internet is one example because you’re using a digital medium to make healthcare more convenient and accessible.
While telehealth is all around us, it’s still in its infancy when it comes to the technology that makes it possible. For example, services like Doctors On Demand allow you to speak with a board-certified health specialist in a matter of minutes via video chat in the comfort of your own home. However, there’s little more these health specialists can do for you than discuss your symptoms. Without patients in their office, they won’t have the ability to diagnose or treat a patient with an illness.

If you have chronic obstructive pulmonary disease (COPD) or any other respiratory condition that requires you to use oxygen, there are some interesting prospects on the horizon in terms of telehealth technology. Oxygen manufacturers like CAIRE Inc. and Inogen are already hard at work on new software and devices that make oxygen therapy more accessible for patients all over the world. Let’s take a look at 7 things oxygen patients can look forward to with emerging telehealth technology.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Improved Early Diagnosis of COPD
According to the American Lung Association, millions of people around the world may be suffering from undiagnosed COPD. Despite going to the doctor frequently and maintaining an otherwise healthy lifestyle, many people ignore the symptoms of COPD or they shrug them off as a natural part of aging. This happens with a number of chronic illnesses, but it’s especially prominent with COPD because it’s a disease that progresses slowly.

Another reason for undiagnosed COPD is that patients have a fundamental misunderstanding about what COPD is and what causes it. Many people believe that the only way to contract a lung disease is by smoking cigarettes or being exposed to some other harmful substance for a long period of time. Unfortunately, this is not always the case. According to Medical News Today, around 1 in 6 people with COPD have never touched a cigarette. Many people with undiagnosed COPD have a condition called Alpha-1 deficiency.
Alpha-1 antitrypsin (AAT) deficiency is an inherited condition. It’s known for contributing to the onset of liver disease and lung disease in otherwise healthy people. Normally, the liver produces the alpha-1 protein and distributes it throughout the blood. It’s responsible for protecting the lungs from inflammation, either resulting from airborne irritants like cigarette smoke or infections. So, even if you’ve never smoked, being in an environment with smoke or getting sick frequently could greatly increase your risk of contracting COPD.
.jpg)
At the end of the day, there is no cure for Alpha-1 deficiency. Your doctor won’t be able to provide you with a medication or procedure that will return your AAT levels back to normal. However, there are many ways to treat the condition including lifestyle changes and augmentation therapy. This procedure is done by infusing AAT into your blood through an IV tube which can be used to help slow the progression of COPD. Since the effects are temporary, you’ll likely need to repeat this procedure weekly for the rest of your life.
Now that you know how difficult it can be to detect COPD early on, you’re probably wondering how telehealth technology will help mitigate this. Since undiagnosed COPD is largely the result of people not being open or honest about their symptoms, it goes without saying that being more digitally connected to your healthcare providers will make people more likely to open up about how they’re feeling. In this day and age, people are often so busy that they neglect scheduling doctor’s visits. This will ensure that people have no reason not to speak about their symptoms. While it’s unlikely doctors will be able to diagnose something like COPD through video chat, simply speaking about your symptoms may be enough for your doctor to know if you should be scheduled for an in-person appointment. At this point, your doctor will be able to test for and diagnose any health conditions normally.

Last but certainly not least, the practice of telepulmonology (telespirometry) may lead to higher rates of COPD diagnosis. These terms refer to a general practitioner (GP) consulting a pulmonologist via telecommunication for advice on interpreting spirometry results. As opposed to the old days where you’d be referred to a respiratory therapist if you had a cough or chest pain, your general practitioner may be able to diagnose you more quickly with a quick and simple video chat. According to a study published in pubmed.gov, telepulmonology reduced physical referrals by 22 percent and 90 percent of general practitioners reported learning from their consultation with a pulmonologist.
Tracking Disease Progression More Easily
COPD is a progressive disease. This means that, as time goes by, symptoms like breathlessness, coughing, and chest pain tend to get worse. But that doesn’t mean that COPD patients don’t have the ability to live full and rewarding lives. Many patients can even significantly reduce the severity of their symptoms as long as they follow a strict treatment plan including dietary adjustments, pulmonary rehabilitation, and oxygen therapy.
Most pulmonologists recommend scheduling 2 or 3 doctor’s visits each year. However, people with later stages of the disease will likely need to schedule even more than that. Over long periods of time, this can really get exhausting for COPD patients, and if they have caretakers, they may find it difficult to take the time to schedule and attend all of these office visits — this is where telehealth technology could come into play.

Although you’ll still have to schedule meetings with your doctor, telehealth technology will enable patients to have more frequent checkups without the need to drive to the doctor’s office and sit in a waiting room. Frequent checkups are more beneficial anyway because it will give your doctor the ability to keep tabs on how your disease is progressing and what adjustments you can make to improve your outcome.
Ultimately, infrequent doctor’s appointments are ineffective when treating a disease like COPD. One day, respiratory patients may feel energetic, healthy, and alert, whereas other days they may feel sick and unmotivated. If the doctor only sees you three times a year, they’re not getting the full picture and they won’t understand your condition as well as they could. If you’re able to see your doctor once a month, for example, he/she may be able to prevent things like exacerbations.
Tracking Oxygen Usage
One of the most common symptoms of COPD is a below-normal blood oxygen level. Your body needs an arterial oxygen level of about 75 to 100 milliliters of mercury (mm Hg) in order for you to be considered “healthy.” Low blood oxygen level (hypoxemia) has many adverse side-effects including shortness of breath, a chronic cough, and confusion. Since every organ in your body relies on oxygen, long-term hypoxemia can lead to organ damage and even organ failure.
Typically, a COPD patient is prescribed oxygen when they have a blood saturation level below 60 mm Hg. At this point, you should start looking for a medical oxygen device that matches your lifestyle. In the past, oxygen tanks were the only option for people who needed medical-grade oxygen, but they’ve since been replaced with portable oxygen concentrators which are much lighter, smaller, and safer to use. We recently wrote a guide about finding the perfect portable oxygen concentrator which you can find here
Aside from portable oxygen concentrators making oxygen therapy much safer and accessible for COPD patients, they’ve also made some significant breakthroughs when it comes to telehealth technology. CAIRE Inc., an oxygen equipment manufacturer based out of Georgia recently released its most advanced portable oxygen concentrator called the FreeStyle Comfort. This POC has the longest battery life of any machine on the market and also offers an outstanding oxygen output and lightweight design. However, the most interesting thing about this concentrator is the new CAIREView Telehealth Application.
Each Caire FreeStyle Comfort portable oxygen concentrator has built-in technology that allows it to connect with your mobile device such as a cell phone, tablet, or laptop, and upload important data about your oxygen usage. What’s more, this data can be sent off to the oxygen manufacturer, giving them live updates about your oxygen settings and daily oxygen usage. The best part of all of this is that it’s done on a secure network so you can rest assured that your privacy will always be protected.

While many oxygen patients likely don’t know what CAIREView is, it indicates a significant step forward for both oxygen therapy and telehealth technology. Just twenty years ago, most oxygen patients relied on bulky oxygen tanks and home oxygen concentrators which significantly stunted their freedom and independence. However, in 2020, oxygen patients not only have access to lightweight oxygen devices that they can take everywhere, but they have the comfort of knowing that their doctor or oxygen manufacturer will have live updates about their oxygen use. And this application has just scratched the surface of what’s possible. Since the Caire FreeStyle Comfort is such a popular portable oxygen concentrator, we’re likely to see other manufacturers following suit by creating new and innovative telehealth technologies to accompany their oxygen machines.

Remotely Troubleshooting Oxygen Devices
Purchasing a new electronic device like a smartphone, tablet, or laptop can be a nerve-racking experience. On one hand, you want to always have the latest and greatest model of your favorite device, but you also don’t want to have to deal with any problems that arise if it were to malfunction. Most device manufacturers require you to ship off your device to have it repaired at a warehouse somewhere. This can be costly and it can leave you without a device for weeks or months on end.

But what if the manufacturer had the ability to connect to your device and troubleshoot it remotely without you having to lift a finger? This would save you a lot of time, money, and hassle. Amazingly, this is what CAIRE Inc. has been able to accomplish with their CAIREView application. While you’re out and about enjoying your day, your Ciare FreeStyle Comfort will send periodic updates about your oxygen usage and the integrity of your portable oxygen concentrator. If they detect that you are not receiving oxygen or that it’s not being used as prescribed, they can contact you quickly to fix the issue. If the device malfunctions, they can provide you with the necessary steps to troubleshoot it quickly and easily.

This new telehealth technology could immensely improve the lives of COPD patients all over the world. Since oxygen is a clear and odorless gas, you would normally have no idea if your device stopped putting out oxygen. The only indication you would have is if you started feeling lightheaded, out of breath, or noxious, all of which could be avoided if you had live updates about how the device is functioning. Losing your oxygen supply while you’re out can ruin your day or worse, leading to a severe COPD exacerbation that can put you in the hospital.
Improved Freedom and Independence
One of the most considerable concerns of COPD patients is their ability to maintain their freedom and independence. The lungs play an important role in our capacity to remain mobile, so naturally, a chronic disease that causes significant inflammation in the lungs and airways may cause people to revert to a sedentary lifestyle. At the same time, many COPD patients rely heavily on friends or loved ones to help them with day-to-day tasks like cooking, cleaning, or taking a trip to the doctor’s office.

Before portable oxygen concentrators, it was even more difficult for COPD patients to retain their freedom. Oxygen tanks can weigh upwards of 100 pounds and need to be refilled regularly. Stationary oxygen concentrators were lighter but they needed to be connected to a wall outlet in order to run. This meant that oxygen patients could only travel as far as their nasal cannula would permit them to. In the early 2000s, portable oxygen concentrators were introduced and COPD patients were able to experience some of the freedom they had before they contracted the disease.
In 2020, portable oxygen concentrators are more advanced than ever before. POCs like the Inogen One G5 offer over 13 hours of battery life on one charge, a lightweight design, and 1,260 ml/min of oxygen — more than enough for the majority of oxygen patients. Modern POCs are also incredibly easy to use meaning you can start using it straight out of the box without having to memorize a bunch of commands or buttons. Since these devices are so advanced and innovative, you may be wondering how telehealth technology can add to this.

One of the ways telehealth will improve freedom and independence is by making oxygen patients see their therapy device as less of a burden. Rather than having to fear whether their POC will hold up throughout the day, POC patients can relax knowing that their doctor or oxygen manufacturer has an eye on their oxygen machine. Oxygen patients can focus more on the important things in their life like spending time with family or taking a trip to a place they’ve never been before.

Another benefit of telehealth technology is that it will make patients less reliant on caretakers and loved ones. Instead of having someone at your side to troubleshoot your oxygen machine if something goes wrong, most oxygen patients will feel comfortable fixing their own device. What’s more, you won’t have to carry your POC manual around with you because you’ll have access to all of that information on your phone or another mobile device.
Reduced Medical Costs
According to Investopedia.com, healthcare spending in the United States in 2017 was reported at $3.5 trillion and it’s expected to rise to $6 trillion by 2027. Medical costs are a growing problem in the country especially for people who already struggle to pay their bills. While it would be unwise to sit around and wait for reasonable healthcare reform, telehealth technology has already proven to be a major driving force in reducing medical costs.

According to High Point Solutions, the average cost of a telehealth appointment costs $79 whereas an in-person doctor’s office visit costs around $146. First and foremost, telehealth appointments cut costs for patients. Instead of having to drive to the doctor’s office and in some cases, skip a day of work, patients can have access to medical services and education in the comfort of their own homes. On the healthcare provider’s side, telehealth technology can cut costs by reducing the need for clinical workspace and making appointments go quicker and more smoothly. Ultimately, some of these savings will make it back to the patient as well.

Another way telehealth technology cuts medical costs is by reducing hospital admissions. According to studies done by Cardinal Health, telehealth services are able to eliminate nearly 1 in 5 emergency room visits. This is substantial considering the fact that one day in a hospital costs an average of $3,949. When it comes to COPD, periodic appointments via telehealth technology could result in significant health savings for many patients. Since telehealth appointments enable patients to have more frequent checkups, doctors will have a higher chance of catching exacerbation symptoms before they become serious.
Increased Accessibility
Lastly, the accessibility of medical services is another major issue facing COPD patients. While healthy patients have the means to get themselves to the doctor’s office, many people with COPD are physically incapable of doing so. COPD patients who are immobile or struggle with mobility issues may need to rely on caretakers or loved ones meaning that appropriate healthcare, in general, is less accessible.

Furthermore, people who tend to forget things that they discussed with their doctor will have the added security of being able to record every appointment they have with their doctor. Instead of having to write everything down and take notes on what your doctor says, you can simply use video recording software to keep an archive of all your telehealth appointments. This will also ensure that you follow your doctor’s instructions as closely as possible.
Conclusion
Health specialists and health equipment manufacturers have barely scratched the surface of what’s possible with telehealth technology, however, we’ve already seen many of its benefits come to light. Video conferences are one simple way doctors can offer their patients more accessible, cost-effective, and reliable services and all it requires is a computer and a video camera. For COPD patients, this could mean less frequent admittance to hospitals due to exacerbations.
Oxygen device manufacturers like Caire Inc. and Inogen are also hard at work on telehealth technologies that allow for better communication between oxygen users, oxygen providers, and practitioners. CAIREView is an easy-to-use application that connects to all Caire FreeStyle Comfort devices. It provides the oxygen manufacturer with up-to-date information about the patient’s oxygen usage and allows them to assist with troubleshooting your device anywhere in the world.
-min.png)
All medication prescribed to patients in the United States is approved by the Center for Drug Evaluation and Research (CDER), a branch of the U.S. Food and Drug Administration (FDA). This program acts as a watchdog for all genetic and biological therapeutic drugs being tested throughout the country, ensuring that only safe and effective ones are administered to the general public.
Contrary to the name, however, the CDER doesn’t spend a lot of time researching new drugs. Instead, the organization receives applications from drug makers and evaluates their efficacy through a four-phase approval process. Once the phases are complete, the drug is considered “FDA approved” and is distributed to pharmacies throughout the country. If the side-effects or risks posed by the drug ever outweigh the benefits, the FDA may recall a drug that has already been distributed.
As a patient, this drug approval process provides you with a unique opportunity called a clinical trial. These clinical trials play a crucial role in evaluating the safety and effectiveness of a drug and may be the perfect opportunity for you to seek relief from your respiratory symptoms — but they’re not for everyone.
In the following sections, we’ll take a look at what clinical trials are, how they work, and why you may want to consider participating in one. As always, if you have any questions about your current treatment plan, clinical trials, or any other COPD-related concern, be sure to consult your doctor as soon as possible.
What is Clinical Research?
In medical terms, the word “clinical” refers to the observation and treatment of real patients as opposed to theoretical or laboratory studies. They act as a sort of real world experiment for medication without the risks associated with immediately releasing it to the public. Generally, clinical research is divided into two categories: observational studies and clinical trials.
 Observational Studies
Observational Studies
During an observational study, researchers observe people in a normal setting. Through medical exams, questionnaires or other tests, they can help reveal common health trends throughout a community and provide new opportunities for clinical trials.
Clinical Trials
Clinical trials are similar to observational studies, but instead of taking a hands-off approach, they aim to test a specific medical, surgical, or behavioral intervention. While a drug may work in theory or in practice in a petri dish or on animals, a clinical trial allows researchers to test their effects on actual patients. Because clinical trials are completed by sponsors and not the FDA, there are certain criteria that need to be met before a drug can be tested and drug sponsors need to submit an Investigational New Drug (IND) application that outlines the results of their testing, the composition of the drug, and a plan for its development — this is called the pre-clinical stage.

All clinical trials have a purpose which can be part of one of the following categories:
Diagnostic - finding new procedures, techniques, and methods for diagnosing diseases more effectively or sooner.
Screening - testing different methods for improving screening procedures that could reveal signs of a disease.
Prevention - examining vaccines, vitamins, medicines, minerals, or lifestyle changes that could prevent the development or recurrence of disease.
Treatment - testing new drugs, combinations of drugs, surgery, or therapy that reduces the effects of a disease.
Supportive Care - Evaluating the effectiveness of procedures used to increase the comfort and quality of life of a patient.
Health Services - Examines the financial aspects of health care, access to care, organization, and delivery methods.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The Four Phases of a Clinical Trial
Phase 1
20-80 participants
The first phase of the clinical trial process is focused on safety. Most drugs, regardless of how effective they are, have some form of negative side effect associated with them. The goal of the first phase is to test the way the drug is metabolized and processed by the body. Typically, phase 1 is performed on healthy recipients without an illness.
Phase 2
100’s of participants
Unlike phase 1, phase 2 is all about effectiveness. As a result, this stage usually requires participants with a condition the researchers are trying to treat. Researchers may also compare the effects of these drugs to other similar drugs that are being used to treat their condition. Phase 2 won’t begin until the perceived benefits are greater than the risks uncovered in phase 1.
Phase 3
1000’s of participants
Phase 3 studies both safety and efficacy further. Researchers may study different demographics, dosages, or using it in combination with other drugs. Participants may be divided into different groups so the results can be compared. Oftentimes, phase 3 clinical trials can last several years depending on the type of drug that’s being studied.
Phase 4
Post-approval risk assessment
At phase 4, the drug has been approved by the FDA and doctors can begin administering it to patients. However, in certain cases, the sponsor may need to continue studying the effects of the drug. This is especially the case if the sponsor wants to be able to sell the medication for a new purpose such as treating a different disease.
The Clinical Trial Process
For many people, the most intimidating part of clinical trials is the process. First and foremost, you should know that you will never be a part of a clinical trial without your knowledge. In order to be a part of one, you’ll need to first sign an informed consent form. This differs from a regular consent form in the following ways.
- Participants must be given the necessary information to make an informed decision about their involvement in the trial.
- Participants must be allotted an adequate amount of time to discuss the clinical trial with friends and family.
- Researchers must be open and honest about all questions regarding the clinical investigation.
- Researchers continue to provide information about the trial as it progresses.
After meeting with the staff and signing an informed consent form, you will be screened to ensure you qualify for the trial. This is done through what’s called a “baseline” visit where researchers will conduct both physical and cognitive tests.
Once all the consent and qualification processes have been completed, you will be assigned to a control group and given specific instructions like when you need to come in for a checkup. If there are any forms that you need to fill out daily or weekly, they will go over this with you to ensure you understand what needs to be done. Note that you should continue to visit your regular primary care physician throughout this process and keep them updated with information about the clinical trial.
Who Can Participate?
Because clinical trials are used to study a specific group of people, it’s not unusual for an application to be declined. Criteria will differ from study to study, however, the age of the patient, disease stage, gender, genetic profile, and family history could all play a role. Your ability to participate could also be affected by other medications you are currently taking that may interfere with the study.
Diversity of test subjects is very important when conducting clinical trials. The objective is to find drugs that are effective for a wide group of people, so the more people that are involved, the better idea researchers will get of the potential risks and benefits. If you think you’ll get turned down because of a specific condition you have or your age, it’s best to contact them anyways because you may be just the person they’re looking for.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Benefits of Clinical Trials
For some COPD patients, clinical trials are a great option, allowing them to receive treatment for their condition outside the traditional means of doing so. However, for others, it may add an extra burden to their healthcare routine that’s unwanted and unneeded. It’s important to take your time and determine if it’s something worth pursuing.
A ccess to New Medication
ccess to New Medication
Possibly the most common reason people join a clinical trial is that they get access to medication that’s not yet available to the general public. This is especially beneficial to people who don’t like the side-effects of medication they’re currently taking or they’re simply interested in trying something new.
Assisting in Research
Another common reason for participating in clinical trials is to assist in the process of researching new solutions for your disease. While it may sound like you’re playing a small role, researchers would not be able to test their medication without the help of people who have the condition they’re trying to treat.
Back Out at Any Time
One common misconception about clinical trials is that once you sign up, you won’t be able to back out. Fortunately, this is not the case.
Anyone who signs up for a clinical trial can back out at any time and for any reason. It is, however, recommended that you notify the research company of your decision and consult with your doctor immediately to get back on your regular treatment plan.
Potentially Reduced Costs
While you or your insurance company will still need to pay for the medication you receive, many costs associated with clinical trials like checkups and evaluations are paid for by the company that is performing the test. So, you may be getting some additional checkups or medical services for free that you would normally be paying for with your primary care physician.
Disadvantages of Clinical Trials
Medication is Not Approved by FDA
While there are many benefits to being part of a clinical trial, there are several downsides as well, one of which is that the drug likely hasn’t been approved by the FDA yet. If you refer back to the list of phases above, you’ll see that only one phase, the 4th, is FDA approved. So, if you’re part of a clinical trial that’s in the first, second, or third phase, you’ll be using medication that hasn’t been fully tested yet.
Fortunately, the FDA maintains regulations for clinical trials that protect patients’ safety and security, you can view the full list of regulations on their website. In short, however, these documents require researchers to take a number of precautions when it comes to your safety and notify you about every detail of the procedure.
Frequent Checkups
Another thing that may be seen as a disadvantage to clinical trials is that you have more frequent checkups and more responsibilities. During a clinical trial you may be required to go to the testing center weekly to check your progress and document the effect of the medication on your body. Additionally, you may be asked to fill out forms or questionnaires that ask about your symptoms. All of this takes extra time, so if your goal is to save time, you may want to avoid clinical trials.
Placebo-Controlled Studies
Last, but certainly not least, placebo-controlled studies may be seen as a disadvantage to clinical studies depending on what your goals are.
When researchers start a clinical trial, they want to do everything they possibly can to ensure the results of the study are accurate and have a very low margin of error. As a result, they may use something called a “placebo” or an inactive substance that’s designed to look exactly like the actual medication. Oftentimes, even the person administering the medication doesn’t know whether the medication is real or a placebo; this is known as a double-blind, placebo-controlled clinical trial.

Placebos are used to account for the “placebo effect.” In other words, if you tell someone that they’re receiving medication for their condition, they may perceive that they benefited from the drug even if there was no actual benefit. When researchers divided test subjects into placebo and non-placebo groups, it allows them to account for this psychological effect.
Generally, placebos can be seen as a negative because you won’t know whether or not you’re actually receiving treatment for your condition. Although researchers are required to notify you if placebos are a part of the trial, they won’t tell won’t tell you as an individual that you’ll be given placebos.
Insurance Coverage for Clinical Trials
Fortunately, most health insurance companies are required to offer coverage for clinical trials under federal law. However, the coverage you receive will depends on three things:
- You must be approved and eligible for the trial
- The trial must be approved
-
Out-of-network doctors or hospitals will not be covered unless otherwise stated in your plan
Approved Clinical Trials
An approved clinical trial is one that includes the following:
- It tests ways to treat, detect, or prevent life-threatening conditions
-
It’s been approved by the FDA by submitting an IND application is not required to submit one.
What Costs are Covered?
Some of the costs your insurance will cover include:
- Lab tests
- Office visits
- Procedures and services needed in trial
-
Supportive care drugs
Costs that are typically not covered include:
- Data collection used for the trial
- The cost of the procedure or treatment studied by the clinical trial
Before you commit to a clinical trial it’s important that you understand what your insurance does and does not cover. If the research team has out-of-network doctors or facilities, you may be liable for these costs. Costs such as data collection and treatment may be covered by the research company, however, unless specifically stated, it’s best to assume they aren’t.
Current Clinical Trials for COPD
If you’re a patient who is currently undergoing treatment for COPD, you may want to consider being part of a clinical trial. Clinical trials for COPD help researchers understand better ways to prevent, screen for, and treat symptoms of the disease. Remember, however, that your ability to participate in a trial will depend on your current health condition, age, gender, ethnic profile, and a variety of other conditions. What’s more, there may or may not be a clinical trial in your area for you to apply to.
COPD Patient-Powered Research Network
The COPD PPRN is a network of 75,000 COPD patients that’s designed to connect them with researchers who perform clinical trials. According to the COPD Foundation, while COPD is the 3rd leading cause of death, there are only 780 clinical trials, a small fraction of the nearly 41,000 trials taking place for cancer research. The COPD PPRN is not a clinical trial in and of itself, but it is a directory that can provide you with more information on finding local clinical trials for COPD.
ACRC Clinical Trials for COPD
The Airways Clinical Research Centers (ACRC) is run by the American Lung Association and is dedicated to researching both asthma and COPD. Around 6,900 patients have participated in clinical trials in 15 clinical research centers throughout the country. There are several clinical trials currently underway including an asthma BMI baseline study, anxiety andd COPD evaluation, losartan effects, and much more. You can view a full list of current studies and their stages here.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Conclusion
Clinical trials are a crucial component of medical research. They afford researchers all over the country an opportunity to test the safety and efficacy of their medication while allowing patients to make a difference as well. There are many benefits to being a part of a clinical trial, but there are also several disadvantages.
If being a part of a clinical trial interests you, it’s best to start by speaking with your doctor and signing up for one of the research networks listed above. If you decide it’s not for you, there are still a number of ways you can get involved like attending events, providing health information, or recruiting friends to a research program. Click the links below for more information on clinical trials for COPD.
Finding a Clinical Trial
COPD Patient-Powered Research Network
Airways Clinical Research Centers (ACRC)
CenterWatch COPD Clinical Trials
Other Resources
Studies show that people with COPD are about twice as likely to experience chronic pain compared to people with no chronic disease. In fact, researchers found that the pain experienced by many COPD patients is severe enough to rival arthritis pain and often requires opiate medications to manage.
If you have COPD it's important to understand that the disease doesn't just affect your lungs; it has many direct and indirect effects on the body. COPD can spawn several types of temporary and chronic pain, including pain in your chest, spine, muscles, joints, and even your bones.
Some chronic pains are the result of respiratory strain and lung damage, while others are caused by poor exercise, malnutrition, and even medication. Many COPD patients struggle to eat enough and get enough physical activity, and neglecting these vital habits is a common reason for chronic muscle and joint pain.
If you or someone you love has COPD, then you'll need to know what kinds of pains COPD can cause and how to treat them. More than 45% of COPD patients are plagued by chronic pain, and some of those pains can be relieved with professional support, proper diet, exercise, and other at-home therapies.
COPD is a difficult disease to manage, and it's even harder when you have to deal with chronic aches and pains. That's why, in this article, we're going to help you understand how COPD causes pain in different parts of the body and what you can do to manage and relieve these pains.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
What Kinds of Chronic Pains are Caused by COPD?
COPD can cause many different types of pain, and every patient's experience with chronic pain is different. However, there are a few particularly prominent causes of chronic pain that affect a large percentage of COPD patients.
Disuse Syndrome
 |
| Photo by Kristina on Flickr |
COPD symptoms like coughing, wheezing, and shortness of breath can be very hard on your body. These symptoms are unpleasant on their own, but they can also cause a variety of chronic and acute pains.
Struggling for air during exercise or bouts of breathlessness is a common cause of chest pain and tightness for COPD patients. Coughing, especially a chronic cough, can also cause serious chest pain and strain the muscles in your shoulders, neck, and back.
However, the most damaging effect of these symptoms is that they make physical activity challenging and uncomfortable. Breathlessness, coughing, and chronic pains all discourage people with COPD from exercising, practicing breathing exercises, and participating in other forms of physical therapy.
Unfortunately, these physical activities are necessary to reduce COPD-related pain and improve patients' ability to breathe. Avoiding exercise only accelerates muscle wasting, loss of mobility, and serious physical decline.
What's worse, inactivity on its own causes even more chronic pain and discomfort due to a phenomenon known as disuse syndrome. Disuse syndrome refers to a variety of chronic pains, illnesses, and even mental disorders that result from a lack of physical activity.
Disuse syndrome occurs as a result of muscle wasting, cardiovascular disease, and nervous system changes that happen when you live a sedentary lifestyle and don't use your body enough. Luckily, disuse syndrome can be reversed with regular exercise and a healthy lifestyle.
Osteoporosis

At least 20 percent of people with COPD also suffer from osteoporosis, a condition that occurs when your bones become thin, weak, and prone to breaking. This is a result of a variety of COPD-related factors, including malnutrition, lack of exercise, chronic inflammation, and even corticosteroid medications.
Your bones are made of living tissue that is constantly being worn down and built back up again, but age and illness can hurt their ability to fully regenerate. Osteoporosis occurs when your body lacks the nutrients it needs to build up your bones at the same rate as old bone tissue is broken down.
Often osteoporosis is “silent,” having no outward signs or symptoms. Many people don't realize that their bones are weakened until they get a minor injury that fractures a bone.
However, once osteoporosis becomes severe it can lead to frequent injuries that cause chronic aches and pains. People with osteoporosis are particularly prone to spinal compression fractures, which can cause severe back pain and spine disfigurement.
If you have osteoporosis even minor actions like twisting, lifting, or minor falls can cause bone fractures that take months or longer to mend. Until they heal, fractures cause chronic pain that often requires prescription pain medication to manage.
Osteoporosis is more common than usual in all subsets of the COPD patient population, but it becomes more likely with age and in the later stages of the disease. COPD patients who have had many exacerbations, have a history of smoking, or who take inhaled or oral corticosteroids are most at risk than others for osteoporosis.
Chest Pain

Moderate to severe chest pain is common ailment that affects COPD patients, especially emphysema patients, day after day.
Emphysema is a common form of COPD that results from damage to the air sacs (alveoli) in the lungs. Over time, emphysema causes your lungs to balloon and over-inflate, which hurts their ability to push all of the air out when you exhale.
Emphysema patients' lungs can become so large that they press on their rib cage and diaphragm, which causes severe pain. The pain can strike at any time and can be triggered by activities as light as walking.
Although lung over-inflation is one of the most common reasons for chest pain, another common cause is muscle tightness and fatigue. COPD symptoms like coughing and shortness of breath over-exert the muscles in your chest that you use to breathe, making them tired and sore.
Chronic coughing and gasping for air can also strain the muscles in your neck, shoulders, and back. Luckily, chronic chest, neck, and back pain can often be lessened with regular exercise, good posture, breathing techniques, and proper symptom management.
Muscle Cramps and Soreness

Muscle soreness and cramps are also common pains that affect people with COPD. These pains can result from a variety of COPD-related conditions, including malnutrition and a sedentary lifestyle.
Because COPD is an age-related disease, many patients are elderly with muscles that can't stand up to the same amount of activity and strain that they used to. This puts COPD patients at a much greater risk for muscle weakness, cramps, and pain, especially when combined with a greater risk of muscle wasting due to the disease.
Muscle cramps can also be caused by poor blood circulation, which can occur along with other cardiovascular complications in the later stages of the disease. And since COPD makes it very difficult to exercise, many patients avoid physical activity, which makes muscle weakness and pain even worse.
What's more, certain medications like corticosteroids can cause vitamin and mineral imbalances in your body that starve your muscles of the nutrients they need to function. This can lead to severe muscle cramping and weakness, adding yet another risk factor for muscle problems in people with COPD.
While muscle cramps tend to be sudden, acute pains, rather than chronic pains, they can come as an indirect consequence of chronic pain. It happens like this:
-
Chronic muscle soreness and weakness makes it difficult to exercise, leading to inactivity.
-
Lack of physical activity and stretching exercises causes your muscles to get even more stiff and painful to move.
-
You then become even more prone to getting additional muscle injuries and pains, including cramps, because your muscles are stiff and under-used.
- This can then lead to even more exercise avoidance out of fear that you will experience more painful muscle cramps and soreness.
Muscle pains are very important to treat because they make it more difficult to exercise, leading to an even more unhealthy and sedentary lifestyle. This compounds the problem, making your muscles and joints even more stiff and cramped from inactivity.
In fact, strengthening your leg muscles and treating chronic pains that make it difficult to move around are some of the most important things you can do for your COPD. Any intervention that makes your body stronger and improves your capacity for exercise has the potential to significantly improve COPD symptoms and even delay the progression of the disease.
Treatment for muscle cramps and soreness usually includes pain relievers, gentle stretching, and physical activity to reduce stiffness and improve limb mobility. We'll go into these treatments in more detail in the next sections so you can learn how to treat muscle pains and stay active with COPD.
General Treatments for Pains Caused by COPD
Over the Counter Pain Relievers
 |
| Photo by Briana Jones |
Over-the-counter pain relievers like Ibuprofen and Aspirin aren't usually strong enough for severe pains, but they can be very effective for minor ailments. If you experience muscle cramps, chest pain, sore joints, or other small pains, these non-prescription medications could help.
For example, you could use mild pain relievers to treat sore muscles after a workout or a particularly active day. You could also use them to reduce mild chronic joint pains and muscle cramps so that you can exercise and perform daily activities without significant discomfort.
If you have COPD, you should always talk to your doctor before taking any new medication, even over-the-counter medications. Your doctor can ensure that they won't interfere with any of your other prescriptions or treatments and warn you about any side effects or complications you should look out for.
Mental Health Support

It's well-known that people who are anxious and depressed experience more aches and physical pains than people with good mental health. Therefore, one way to reduce chronic physical pain is to treat the emotional pain that amplifies it.
It's not difficult to understand why mental health support is so important for people living with COPD. A COPD diagnosis is extremely distressing to receive and can cause a great deal of fear, anxiety, sadness, and regret. Most people need as much extra support as they can get, both practical and emotional, to get through this difficult time.
Even after the initial diagnosis, people with COPD have to devote a significant amount of time and mental effort to managing their disease and its symptoms, which can cause even more worry and stress. Without professional help, the severe anxiety and emotional distress that many COPD patients feel can develop into more serious conditions like chronic anxiety and clinical depression.
If you feel depressed, anxious, or are struggling with increased chronic pain, don't hesitate to seek help from a therapist or psychiatrist. They can give you emotional support, help you manage negative thoughts and emotions, and prescribe you medication like antidepressants if you need them.
Once you take care of your mental health, you will likely notice that your chronic aches and pains have lessened as well. And without the burden of chronic emotional distress, it is much easier to stick to an exercise schedule and treatment plan to properly manage your disease.
Pulmonary Rehabilitation
Pulmonary rehabilitation is a special class designed to help people with respiratory diseases like COPD take charge of their health. It includes instruction on how to exercise right, breathe better, and use medications effectively, along with a variety of other practical advice for managing chronic lung diseases.
Pulmonary rehab is a great opportunity to practice effective exercise techniques and breathing exercises that can improve your endurance for physical activity. It includes COPD-specific physical therapy lessons and tailored exercise classes that can help you reduce a variety of chronic pains, especially chest and muscle pain.
Pulmonary rehab also teaches you to strengthen the muscles in your chest and abdomen that you use to breathe, which can reduce chest tightness and pain that comes from over-inflated lungs and struggling to breathe. You can reduce muscle strain, cramps, and joint aches over the course of pulmonary rehab by learning exercise techniques that strengthen your muscles and joints.
Physical Therapy
 |
| Photo by Tech. Sgt. Kristopher Levasseur |
If aches and pains in your muscles and joints are preventing you from exercising, you might need some physical therapy before you start working out on your own. Especially if you've been sedentary for awhile, your body might not be ready to jump into action just yet.
That's what physical therapy is good for; it helps you work with and around any physical conditions that limit your ability to move. A good physical therapist will teach you how to safely stretch and move the parts of your body that ache and help you recover from injuries and pains.
Through physical therapy, you can improve your muscle strength, flexibility, and overall range of motion. In many cases, this is enough to significantly reduce aches and pains in your muscles and joints and make it much easier to tolerate exercise and daily activities.
If you're suffering from any of the chronic aches, pains, or mental effects of disuse syndrome, physical therapy is one of the best ways to jump-start your recovery. Anything that makes it easier to exercise and move your body, like physical therapy and pulmonary rehab, can help you fight chronic pains and other symptoms caused by COPD.
Massage

There's no doubt that massages are relaxing and feel wonderful, but research shows that it's an effective treatment for muscle and joint pain, too.
Massage therapy is great for COPD because it helps relax sore muscles, limber up stiff joints, and reduce chronic pain. It can also help improve your range of motion, which makes it easier to exercise and do other everyday activities.
If you suffer from chronic pain in your muscles and joints, consider getting a massage once or twice a month. Depending on your insurance provider, your policy might even cover some of the expense. Just make sure to tell your massage therapist about any and all of your health conditions so that you can have a safe and pleasant experience.
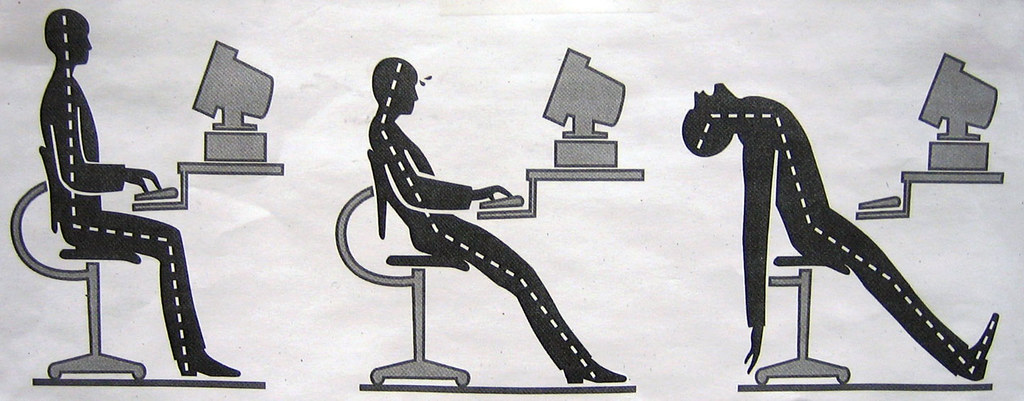
Better Posture

Poor sitting, standing and sleeping posture can lead to a variety of chronic aches and pains. If you have COPD, it's especially important to practice a healthy, straight posture to keep your spine, muscles, bones, and joints healthy.
Bad posture leads to muscle and tendon strain that can severely limit your mobility and physical endurance. Since people with COPD are especially prone to sedentary living and exercise avoidance, they are also more prone to bad posture and the negative consequences that come with it. These negative effects include muscle wasting, stiffness, chronic pain, and permanent changes to the shape and curvature of the spine.
To practice good posture, you should always keep your back straight, your chin up, and your shoulders parallel with your hips. This will prevent you from leaning, slouching, and hunching, which put enormous strain on your spine, shoulders, and neck.
To learn more about how posture affects your COPD, visit our previous article here. It will show you in more detail what good posture looks like and give you a variety of tips and advice for building better postural habits.
Targeted Treatments for Pains Caused by COPD

Now that you've read some general tips for reducing chronic pains and keeping your body strong, we're going to introduce you to some targeted treatments and techniques for treating specific aches and pains. We'll show you techniques for relieving a variety of common COPD pains, including chest pain, joint aches, and muscle cramps.
Breathing Exercises

One of the best ways to prevent COPD-related chest pain is to strengthen the muscles in your chest and improve your breathing efficiency. Exercise is the most effective way to do this, but breathing exercises can help, too.
There are a variety of breathing exercises designed to help people with COPD and other respiratory illnesses breathe easier and more efficiently. Some of the most common are pursed lips breathing and diaphragmic breathing, which you can read about in more detail here.
Practicing these breathing exercises every day can help you change how you breathe on a daily basis and help you better control other respiratory symptoms like breathlessness and wheezing. Both techniques also reduce the amount of strain that breathing puts on your chest muscles, reducing chest pain and making it easier to breathe
Mucus Clearance Techniques
A chronic cough is a major source of chest pain for people with COPD. If you find yourself sore because of a chronic cough, especially if your cough usually brings up mucus, there are a variety of mucus clearance techniques that can help.
Although it may seem counter-intuitive at first, taking the time to cough intentionally can actually prevent more painful, more exhausting coughing fits later. Controlled coughing and huffing techniques clear the same mucus out of your lungs that is often the culprit behind a chronic cough. This allows you to breathe better and exercise better without worrying about excess phlegm triggering another coughing fit.
Common mucus clearance techniques include huff coughing, chest physiotherapy, and the active cycle of breathing technique. You can also use medical devices like positive expiratory pressure (PEP) devices, high-frequency chest wall oscillation, and lung flutes.
To learn about these and other ways to reduce mucus in your lungs and airways, visit our article on mucus clearance techniques here.
Heat Therapy

Heat therapy is a favorite home remedy used to treat a variety of aches and pains. It's one of the most simple ways to reduce bone and joint pain, and it works on stiff and sore muscles, too.
Heat therapy works by increasing blood flow to the affected bone or joint, which allows the body to transport extra oxygen and nutrients to the area. This can help the injury heal faster and also provides a soothing, warming sensation that temporarily reduces pain.
To apply this treatment, you'll first need a convenient, portable source of heat, such as a hot water bottle. Then, wrap your heat source in a towel to protect your skin from the extreme temperature. Next, press the hot pack on to the affected muscle, bone, or joint for up to thirty minutes at a time. With any luck, you should experience pain relief after only fifteen or twenty minutes.
What makes heat therapy so great is that it is simple, convenient, and has an immediate soothing effect. And if you don't have a heat pack at home, you can easily make one with items around the house.
Here are some ideas for heat sources you can use to relieve pain in your muscles, bones, and joints:
- Electric heating pad
- Hot water bottle
- Single-use heat packs (e.g. Hot Hands packets)
- A hot shower or bath
- Fill a sock or other fabric pouch with rice, then microwave for a couple minutes until hot.
Increase Calcium and Vitamin D in Your Diet

A major contributor to osteoporosis is a lack of calcium in your diet. It can also be caused by too little Vitamin D, which your body requires in order to absorb and utilize the calcium your eat.
While extra calcium is not a cure for osteoporosis, it can help prevent osteoporosis and reduce bone density loss. If you have COPD, you are at a very high risk for osteoporosis and you should be especially careful to get the recommended amount of calcium in your diet, which is usually about 500-1000 mg.
Here are some good sources of calcium you can add to your diet to protect against osteoporosis:
- Dairy (e.g. milk, cheese, and yogurt)
- Collard greens
- Kale
- Salmon
- Sardines
- Foods fortified with calcium (e.g. tofu, orange juice, cereal, and almond, rice, or soy milk)
Here ar
Breathing comfortably is a constant struggle for people living with COPD, and bad posture can make it even more difficult to breathe. Unfortunately, many people with COPD do not practice good posture, and the disease itself can lead to unhealthy slouching habits.
The good news is that, if you do struggle with bad posture, you might be able to improve your COPD symptoms simply by changing how you position your body. By paying attention to how you sleep, sit, stand, and lie down, you can make adjustments that reduce the strain on your lungs and muscles and make it easier to breathe.
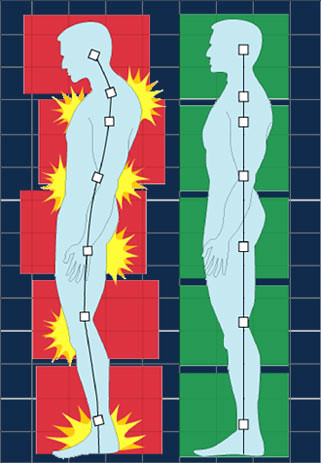
How Posture Affects COPD

Some of the main symptoms of COPD include reduced lung function, chest discomfort, shortness of breath, and difficulty breathing. Because of this, the lungs of people with COPD need all the help they can get to function efficiently and take in enough oxygen.
However, when you assume a hunched posture, it compresses your chest cavity and pushes your rib cage against your lungs and diaphragm. This constricts your diaphragm and makes it more difficult for your lungs to expand.
As a result, you take shallower breaths and get less oxygen when you slouch than you do when you stand or sit up straight.
In this way, poor posture can cause chest discomfort and breathlessness that can make it very difficult and uncomfortable to breathe. Getting into the habit of hunching forward for significant periods of time can significantly affect your respiration and lower your blood oxygen levels, which can be dangerous day after day.
You can see the difference for yourself by comparing how comfortably you can breathe in an upright versus hunched over position.
First, sit and lean forward with your shoulders drooped forward and your neck bent toward your chest. Try to take a few deep breaths. You should notice that your chest feels compressed and your breaths feel restricted.

Next, sit up straight. Hold your chin up parallel to the ground and put your shoulders back, so your back is straight and your shoulders are parallel with your hips. Now, try to take a few deep breaths again. Do you notice that your chest feels more open, and it's much easier to breathe?
If you did this right, the difference should be obvious; a poor, hunched posture puts a great deal of strain on your ability to breathe, while an upright posture takes off the pressure and makes it much easier for your lungs to expand. This difference is apparent after only a few moments of holding a hunched posture, so you can imagine how much strain it puts on your lungs if you have bad posture all the time.
Even though it's clear that body posture can have a significant effect on COPD symptoms, some doctors are beginning to believe that it can go the other way, too. They think that simply having COPD can directly affect your posture and can lead people with the disease to develop negative postural habits.
How COPD Affects Your Posture

If you have COPD, take a moment to think about what you do when you have difficulty breathing. Do you tilt your body forward when you try to catch your breath?
Whether or not this is your reaction to breathlessness, many doctors have noticed that this is a common posture people with COPD assume when they have difficulty breathing. They believe that, in the short term, this forward-leaning position might help relieve the feeling of breathlessness.
This is a learned posture that many people with respiratory illnesses get in the habit of doing. In the short term, this can be helpful and make it easier to breathe when you're having trouble.
However, if you do this often, it's important to tilt your body forward while keeping your back straight and your shoulders relaxed. You could end up putting even more strain on your lungs and the rest of your body if you aren't careful.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The Effects of Bad Posture
Bad posture hurts more than just your breathing. It can cause stiffness, pain, and other complications elsewhere in your body that can affect your ability to exercise and do daily activities.
When your body is not aligned the way it was designed to be, it forces other muscles and joints to have to take over. These muscles aren't designed to hold up your body's weight, and they become sore and strained when you don't practice good posture.
Here are some of the major effects that bad posture can have on your body:
-
Shoulder, Neck, and Back Pain: Slouching forward can put enormous strain on the muscles in your neck, back, and shoulders. This results in soreness, stiffness, and joint damage, and over time can cause permanent disfigurement.
-
Jaw and Head Pain: Bending your neck forward often, as many people do when working at a desk or computer, can strain the muscles, tendons, and joints in your neck and jaw. It can cause muscle tightness that radiates to the head, which leads to jaw tension and headaches.
-
Gastrointestinal Pain: Hunching forward puts pressure on your stomach and intestines, making it harder for them to function and move food through your digestive system. This can lead to stomachaches, pain, and indigestion.
-
Reduced Lung Function: As we discussed before, hunching forward puts pressure on your lungs and reduces their capacity by up to thirty percent. This makes it difficult for your lungs to get enough oxygen, which can be especially troublesome for people with respiratory conditions who already have reduced lung function.
- Reshaping Bones and Joints: Extra pressure on certain bones and joints that aren't suited for the role can actually cause them to change shape. Certain muscles and tendons get shorter or longer over time due to improper posture that positions your body unnaturally. This can lead to stiffness, soreness, decreased mobility, and, in the worst cases, a permanently hunched-over posture.
|
|
| Image courtesy of Aidan Jones on Flickr. |
The strain that bad posture puts on your muscles, organs, and joints only makes it more difficult to move and exercise. And the more your physical activity is limited, the more likely you are to experience worsened COPD symptoms and quicker disease progression.
Since living with COPD already weakens your muscles and makes physical activity difficult, the last thing you need is to be even further hindered by the effects of bad posture.
What Good Posture Looks Like

In general, good posture is a straight posture. Your back should form a straight line connecting your hips, shoulders and head.
That means no slouching or bending for extended periods of time. Pay attention to your normal posture and look out for habits like leaning back, hunching forward, and pulling your shoulders or neck toward your chest
Here's a list of bad postural habits to watch out for:
-
Shifting your weight to one foot or the other, which puts extra strain on your hips and spine. You should try to distribute your weight evenly between both feet instead.
-
Bending forward over your phone, laptop, or desk. This strains your neck, back, and shoulders and reduces your flexibility.
-
Using your shoulder to prop your phone against your ear puts strain on your shoulders, neck, and upper back. Hold your phone in your hand or use a hands-free device like a bluetooth earpiece, instead.
-
Bending your neck back and your chin up in order to look up at a screen. Make sure your screen is positioned in such a way that you can keep your back and neck straight while viewing it.
-
Standing with your pelvis pushed back and your chest pushed forward, a position that exaggerates the curve in your lower back.
- Standing with your back flat, which forces you to pull your pelvis forward and hunch slightly. In a proper posture, your spine should have three curves: it curves in at your lower back, out at your chest, and back in again at your neck.
It can be hard to break bad posture habits like these because, over time, they start to feel natural and comfortable. You have to be diligent about catching yourself slouching or practicing bad posture, and make an effort to correct it every time to successfully break the habit.
Over time, you can train yourself to hold a better posture that will help your muscles, joints, and lungs stay healthy. In fact, there is a wide variety of benefits that you can gain if you dedicate yourself to practicing good posture.
Here are some of the greatest benefits you can gain from good posture:
-
Prevent muscle strain and soreness in your back, neck, shoulders, and limbs
-
Reduce strain on joints and ligaments throughout your body, especially your spine.
-
Prevent bone and spine stiffness and disfigurement
-
Increase the efficiency of your muscles, which increases physical endurance and reduces fatigue
-
Prevent abnormal wear and tear on your joint surfaces
-
Reduce your risk of arthritis
- Improve your confidence and physical appearance
How to Practice Good Sitting Posture

Poor sitting posture is extremely common. And now that most people in the developed world do at least 75% of their work sitting down, learning proper sitting posture is more important for health than ever before.
A hunched posture while sitting is one of the worst positions for someone with COPD because it constricts your chest and makes your lungs have to work extra hard to breathe. If you stay in a hunched position for prolonged periods of time, it can even reduce your blood oxygen saturation and contribute to hypoxia.
Good sitting posture, however, opens up your chest and takes pressure off of your lungs and diaphragm. You should keep your back as straight as possible (while maintaining the curvature of your spine) and keep your neck and shoulders aligned with your hips. Any bending or leaning forward or backward should happen at your waist, not your chest or back.
It's okay to tilt your chest forward if needed, as long as you keep your back straight and refrain from tensing your neck and shoulders. In fact, research shows that leaning forward slightly while sitting or standing can actually make it easier for people with respiratory conditions to breathe.
Here are some general guidelines for proper sitting posture:
-
Keep your back straight at all times and your feet flat on the floor.
-
Your back should always have three curves: at your lower back (lumbar curve), chest (thoracic curve), and neck (cervical curve). Your spine, when viewed from the side, should look roughly like an elongated “S” shape.
-
Your knees should form a right angle (approximately) when you sit.
-
Scoot all the way back into your seat when you sit down. In general, the back of your buttocks should be touching the back of your chair when you sit.
-
Always keep your weight evenly distributed between both hips so you don't put extra pressure and strain on one side.
-
Use a chair with back support when possible. If you are sitting in a straight-backed chair, you can place a rolled-up towel between the chair and your lower back to support the natural curve of your spine.
-
Don't sit still in one place for more than thirty minutes at a time. Take breaks to stand, stretch, and move around whenever possible.
- Use an office chair with a seat that can spin, that way you can turn the whole chair when you need to turn left or right. This helps you keep your back straight instead of twisting at your waist all the time.

It's easy to get in the habit of hunching your body forward, and sitting upright probably won't feel right at first. But if you put forth a conscious effort to practice proper sitting posture, it will start to feel much more natural and more comfortable with time.
Here is an example of a good sitting posture you can use to breathe better with COPD:
-
Keep both feet flat on the floor at all times to keep your hips and back supported.
-
Keeping your back straight, lean forward slightly and rest your elbows on your knees. You may also rest your elbows on a table or flat surface in front of you.
-
If you need extra support, you can rest your chin in the palms of your hands.
- Make sure your neck and shoulders are relaxed. Do not tense them or allow them to slump forward.
How to Practice Good Standing Posture

Even if you spend most of your day sitting down, it's important to pay attention to your posture when you stand, too. If you develop the habit of using correct, upright standing posture you can increase your standing endurance, breathe easier, and reduce muscle soreness and fatigue.
Here are some general guidelines for proper standing posture:
-
Keep your shoulders back, relaxed, and aligned with your hips.
-
Keep your chin up and parallel to the ground. Don't lean forward or bend your neck forward when standing or walking.
-
Bend your knees slightly and keep your feet about shoulder's-width apart.
-
Tuck your stomach in and keep your back straight; don't lean back or push your hips forward when standing.
-
Wear comfortable shoes with good arch and ankle support.
- Don't stand still for long periods of time. Move around, walk, stretch, and shift your weight to prevent soreness and strain.
 |
| Image courtesy of Beth Scupham on Flickr. |
Here are two examples of proper standing positions you can practice to improve your posture.
Standing Posture 1:
-
Stand with your feet spread about shoulder's width apart.
-
Make sure your weight is distributed evenly between both feet, so you're not leaning on one leg or another.
-
Lean your hips back against a wall for support if needed and rest your hands on your thighs.
-
Keep your shoulders relaxed and parallel with your waist.
- You can lean forward slightly and let your arms hang in front of you as well.
Standing Posture 2:
-
Stand with your feet spread about shoulder's width apart.
-
Make sure your weight is distributed evenly between both feet, so you're not leaning on one leg or another.
-
Rest your hands or arms on a chair, table, or another piece of furniture in front of you that's below shoulder height.
- Rest your head on your hands or forearms if needed.
How to Practice Good Sleeping Posture
|
|
| Image courtesy of Esther Max on Flickr. |
Many people don't think about how they position themselves when they sleep, but bad sleeping posture can significantly affect your body. Most people spend 6-9 hours every night in bed, and how you position your body during that time can significantly affect your muscles and your ability to breathe.
Here are some general tips for good posture while you sleep:
-
Choose a mattress that is medium firmness. You want it to be soft, yet not so soft that it doesn't support the curves of your body.
-
Use a lumbar support for your lower back if needed.
-
As always, it's important to keep the natural curvature of your spine intact. Here's how you can do this while you sleep.
-
If you sleep on your back, put a pillow or rolled towel under your knees. You can also place a lumbar support roll under your lower back.
-
If you sleep on your side, bend your knees slightly at the knee. Don't pull your knees up toward your chest.
- Avoid sleeping on your stomach, which can strain your back and neck.
Here are two examples of good sleeping positions you can practice for better posture:
Proper Sleeping Posture 1:
-
Sleep on your back and put a pillow under your head to support your head and neck.
- Bend your knees slightly and place a pillow or rolled-up towel under your knees. This will help keep your spine straight and relieve pressure on your lower back.
Proper Sleeping Posture 2:
-
Sleep on your side with your knees slightly bent, but not pulled up toward your chest.
-
Put a pillow under your head to keep your head elevated and your neck supported.
-
Tuck a pillow in-between your knees.
- Do your best to keep your back straight while you sleep. Don't curl up your body or tuck your chin in.
Improving Flexibility

Unnatural postures causes stiffness and a variety of imbalances in your muscles, tendons, and joints. If you have had bad posture for a long time, chances are your body needs some work to restore natural balance and flexibility.
Regular exercise and physical activity is one of the best ways to restore strength and flexibility to your muscles and joints, but it's important to take time to stretch as well. There are a variety of simple stretching exercises you can do at home and before workouts that can help you improve your posture and flexibility.
Here are some stretching exercises you can do to support better posture:
-
Chin tucks (Neck Flexion): Sit or stand up straight and tilt your neck down toward your chest and hold. Follow up this stretch with neck extensions
. -
Neck extensions: Sit or stand up straight, tilt your head straight back, and hold. Keep your shoulders as relaxed as possible.
- Chin retractions: Sit or stand up straight and push your chin forward. Then pull your chin back and tuck it in slightly—but not too much—keeping it parallel to the floor. Hold for a moment and repeat.

Shoulders
-
Shoulder rolls: Sit or stand with your back straight and roll your shoulders backward. Start by pulling your shoulders up (like a shrug) and then pushing them backward, down, then forward again. Repeat ten times, then reverse the direction by rolling your shoulders forward another ten times.
- Arm stretch: Straighten your right arm and cross it over your chest. Place your left hand on your upper-left arm to hold it in place and pull it closer to your chest. Hold, then repeat with your left arm.
-
Upper back stretch: Sit up straight and clasp your hands together in front of you with your fingers interlaced. Then, turn your palms facing away from your body and push out, extending your arms all the way, and hold.
- Lower back stretch: Lie on your back on a flat, firm surface. Bend your knees slightly and place both feet flat on the floor. Reach up with both hands and grasp your thigh behind one knee. Pull your knee in toward your chest until you feel the stretch in your lower back and hold. Then, lower your foot back to the ground and repeat with your other leg.
Chest
- Open chest stretch: Stand with your side facing a wall or doorway. Extend one arm and place it on the wall or doorframe, then twist at the waist, turning your body away from the wall. Twist until you feel the stretch in your chest and shoulder and hold. Next, turn so that your other side faces the wall or doorframe and repeat with your other arm.

You can do most of these stretching exercises while sitting in a chair to save energy. You should hold each stretch for about 20-30 seconds at a time (unless otherwise indicated) and repeat 2-3 times.
If you still find it difficult to perform light exercises like these, talk to your doctor. You might need to take physical therapy or a pulmonary rehabilitation class to help you get into good enough shape to exercise on your own.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Conclusion
Managing breathlessness and difficulty breathing is one of the most important skills you can learn if you have COPD. Learning to have better posture is an effective and simple means to better control your symptoms.
By practicing a straighter, more natural posture, your body will be in a better position to breathe without extra pressure or strain. Not only that, but good posture will also reduce aches, pains, and cramps in the rest of your body.
But just as important as knowing good posture is knowing what positions to avoid. Breaking negative postural habits can be tricky, but with enough attention and diligence you can get to the point that you use good posture without even having to think about it.
It can be difficult to get in the habit of sitting, sleeping, and standing in the right way, but you get to reap the benefits of feeling better, breathing better
For many people with COPD, a chronic cough is an ever-present feature in their lives. This can be very disruptive to daily life and leave you feeling tired and fatigued.
COPD causes a chronic cough for two main reasons: First, COPD causes inflammation in your throat, lungs, and airways, making them much more sensitive to getting triggered to cough. Second, COPD causes you to produce extra mucus, which obstructs your lungs and airways and triggers a phlegmy cough.
People with COPD also tend to suffer more often from other conditions that cause coughing, like pneumonia, asthma, and GERD.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Along with breathlessness, coughing is one of the most uncommon and unpleasant symptoms of COPD. Some people have a chronic cough that they have to deal with day in and day out, while others only experience severe coughing during exacerbations.
But whether you struggle with coughing every day or just when your symptoms get worse, you should know that you don't have to suffer hopelessly. While you probably won't be able to rid yourself of your cough for good, there are many effective cough suppression techniques that can reduce your cough and make it easier to manage.
In this article we're going to show you a variety of cough suppression techniques for COPD. We'll introduce you to an assortment of home remedies, lifestyle changes, and mucus reduction techniques that can help you control your cough and breathe unobstructed
Not All Coughing is Bad
![]()
Before we get into the cough suppression techniques, it's important to know that there are times when you shouldn't try to suppress your cough. Oftentimes, COPD causes a productive cough, which is a cough that produces sputum (a mixture of mucus and saliva).
A good rule of thumb is that if you can cough up mucus, then you should try to cough up as much as you can. You don't want to stop or suppress the coughing, otherwise the mucus will build up in your airways and make it even more difficult to breathe. The mucus has to come out at some point, so you might as well deal with it now!
If you have a wet cough that produces sputum, you can use controlled huffing and coughing techniques to move the mucus up and out of your airways and into your mouth, where you can spit it out. You can read more about controlled coughing techniques in our previous post here, and learn about other methods to loosen and get rid of mucus in your airways.
Controlled, productive coughing is important because it's the only way to clear your airways of mucus and prevent uncontrolled coughing later. Uncontrolled coughing, however, can be disruptive, uncomfortable, and even painful.
If you have COPD, uncontrolled coughing can leave you feeling exhausted and leave you with less energy for other activities. In this next section, we'll show you how you can reduce and suppress coughing with simple activities and home treatment methods.
Simple Activities to Reduce Coughing
Avoid Coughing Triggers

COPD makes your lungs and airways especially sensitive to airborne irritants. That includes particulates likes smog, dust, and barbecue smoke as well as biological molecules like bacteria, pollen, and mold.
These airborne irritants are common causes of coughing, and breathing clean, pure air is one of the best ways to prevent it. If you smoke, live in an area with high air pollution, or are sensitive to airborne allergens like pollen, you're much more likely to experience a chronic cough and other worsened COPD symptoms.
To avoid coughing as a result of exposure to contaminated air, its important to keep airborne irritants and allergens from building up in your home. Since most people spend a lot of time indoors, it's worth putting in some extra effort into cleaning and buying a high-quality air filter to remove particulates from the air indoors.
You should also avoid going any place where you might be exposed to smoke or other forms of air pollution. Stay away from wood-burning stoves, avoid breathing car exhaust on busy roads, and stay indoors when your local air quality or allergen report indicates caution.
Finally, scented products like perfumes, lotions, and other body products are irritating to many people who have COPD. If you notice that certain products and fragrances are making you cough or causing other respiratory symptoms, make sure to use only unscented products. You might consider asking other people who share your home or work space to do the same.
Avoid Foods that Worsen Symptoms

There are certain foods, like dairy, that you should avoid if you often have thick or excess amounts of mucus in your airways. For some people, dairy seems to increase mucus production and changes their mucus' consistency to be thick and sticky.
Not everyone is sensitive to this effect, however. But if you regularly experience thick mucus and coughing, it's worth testing whether dairy is a culprit by reducing your dairy consumption and paying attention to how it affects your congestion and cough.
Another category of foods to avoid is foods that contain a lot of salt. Too much salt can make you dehydrated, thickening the mucus in your airways and making you more likely to cough. It can also cause bloating, which increases chest discomfort and makes it even more difficult to breathe.
Drink Plenty of Water
If you have COPD it's important to avoid dehydration. If you don't drink enough water, it can make several COPD symptoms worse, including chest discomfort, coughing, and difficulty breathing.
This happens because, when you don't get enough water, the mucus in your lungs and airways dries up and becomes more thick and sticky. This thick mucus gets stuck in your lungs and airways, blocking airflow and triggering the need to cough.
Proper hydration prevents this by keeping your mucus thin and watery, that way it is less likely to cause blockages. Thin, runny mucus is also easier to cough up and drain out of your airways using postural drainage techniques (discussed later in this article).
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Get Plenty of Exercise
If you have COPD, then you know that exercise is important. It's the only way to stay healthy and keep your body strong, and it's an effective way to reduce coughing, as well.
Regular exercise can improve many COPD symptoms and can make it much easier to breathe on a daily basis. That's because, in the long run, physical activity strengthens the muscles in your chest that you use to breathe.
This overall reduction in symptoms, increased ability to breathe, and increased tolerance for activity means less coughing and wheezing, too. However, exercise can also help your cough in the short term by helping mucus drain.
For some people, exercise helps their mucus flow and makes it easier to clear out of their airways. However, some people find that exercise actually increases their mucus production and makes coughing worse. To figure out how exercise affects you, pay attention to how you feel and how much you cough during and after moderate to light aerobic activity.
Practice Breathing
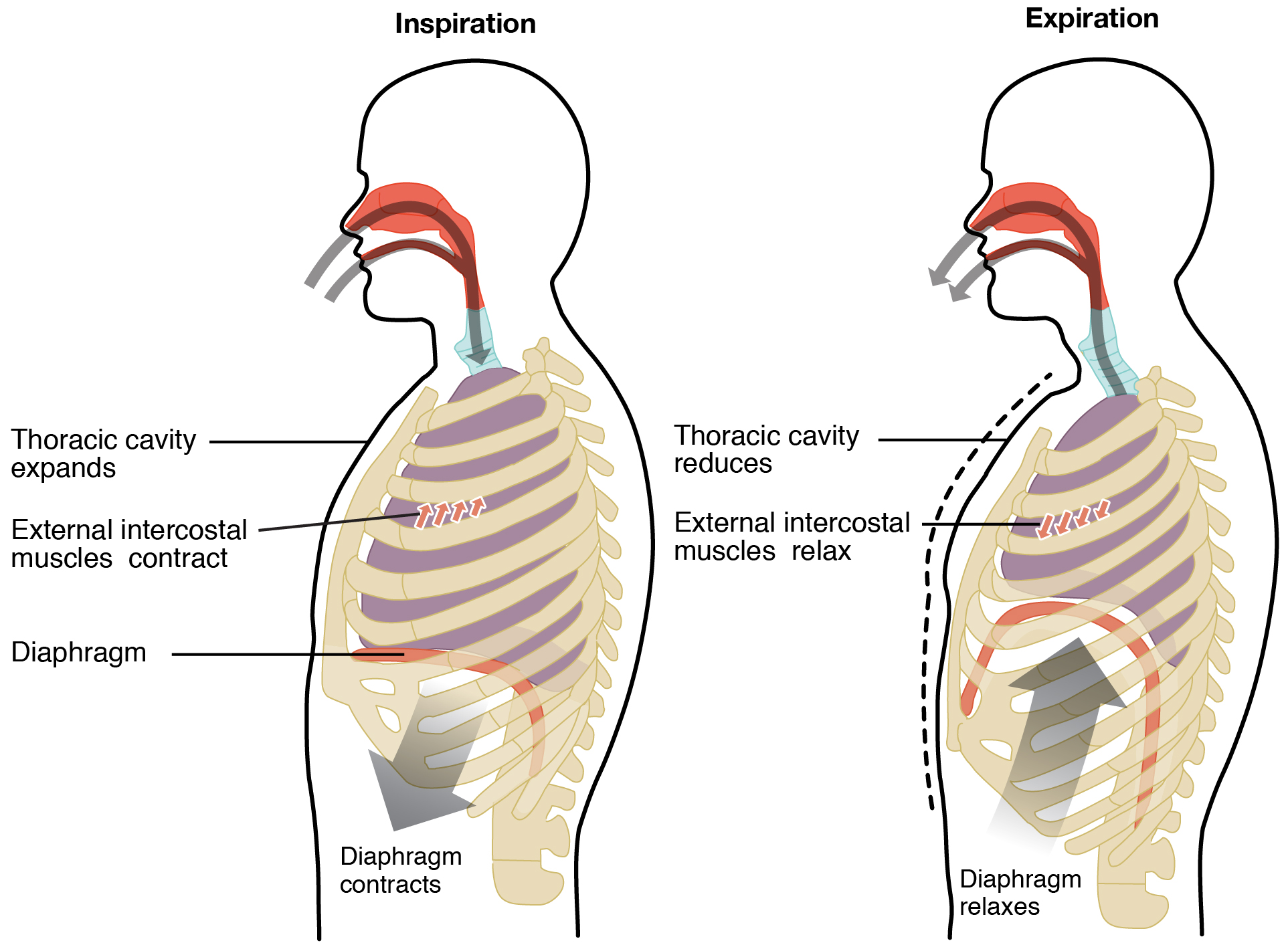
Shortness of breath, wheezing, and coughing can all make you more likely to cough. That's right, coughing itself causes more coughing because it irritates your airways and makes them even more sensitive to irritants and other coughing triggers.
This is why, when you have a coughing fit, it can be so difficult to stop coughing and get your symptoms back under control. The best way to break out of this negative cycle is to practice controlled breathing techniques.
Breathing techniques help you slow your breathing and get it back into a natural rhythm. Doctors recommend that you practice breathing exercises like diaphragmic breathing and pursed lips breathing every day, that way you can use them when needed to recover from periods of wheezing, breathlessness, and coughing.
Position Yourself for Proper Drainage

Excess mucus production is a major cause of coughing in people with COPD. One way to prevent this and reduce coughing is to position yourself so that the mucus drains out of your lungs and airways.
Postural drainage is a specific mucus-draining technique used to help COPD patients and people with other respiratory conditions breathe better. It involves positioning your body in specific ways that allow mucus to flow out of your lungs and airways and into your mouth, where you can spit it out.
There are several recognized postural drainage positions, and each helps drain a different section, or lobe, of your lungs. Most positions require lying down on a soft surface and using pillows to elevate certain parts of your body.
Here is a link to more information on postural drainage positions.
Chest and Back Percussion
Percussion is a method used to loosen up mucus in the lungs so you can more easily cough it up. This allows you to clear out phlegm that might obstruct your breathing or cause a fit of coughing later.
To do chest percussion, you lie flat on your back and have someone tap firmly and rhythmically on specific places on your chest. After a few minutes, you sit up and do controlled coughing techniques until you are able to get the dislodged mucus out of your lungs.
Back percussion is similar to chest percussion, except you lie on your chest and have someone tap on specific points on your back. To learn more about chest percussion and the correct spots to tap, see this guide to chest physiotherapy from the Cystic Fibrosis Foundation.
Elevate Your Head at Night

Keeping your head and neck elevated at night is an effective way to prevent coughing and breathing difficulties while you sleep. It helps mucus drain out of your airways so it doesn't pool in your throat and obstruct your breathing at night.
Before you go to sleep, prop up your head and neck with a pillow or two to keep mucus from building up in your throat and upper airways. This will help you avoid nighttime coughing and help you and your family sleep more comfortably.
Home Remedies for Coughing
Get a Humidifier

Dry air is a very common trigger for coughing, especially if you have COPD. If you live in a dry climate or experience worse coughing in the winter, the cold weather could be what's making your cough and other COPD symptoms worse.
When you breathe air that is too dry it irritates your airways and triggers a coughing reaction. When you breathe in moist air, however, it lubricates your airways and allows air to pass through without discomfort.
The best solution to dry indoor air is to get a humidifier for your home. Running a humidifier increases the amount of moisture in the air and makes it easier and more comfortable to breathe.
You can get either a whole-house humidifier for your entire home or a smaller, portable humidifier for a single room or small area. Just make sure to read the information on the box to make sure that the humidifier you get is big enough for your space.
Many people find that using a humidifier in their bedroom at night reduces their COPD symptoms and makes it easier to breathe while they sleep. However, if the humidity gets too high then it can actually make your symptoms worse. Most doctors recommend that you keep the humidity in your home at about forty percent for the best results, and to not let the humidity rise above fifty percent indoors.
Breathe Moist Air
If you're suffering from an acute coughing fit due to an irritated throat or airways, try taking a hot shower or bath. This helps suppress coughing by moistening and soothing your airways so they are less irritated and sensitive to coughing triggers.
If you don't want to go through the hassle of taking a whole shower or bath, you can breathe in moist air from other sources. You can inhale the steam rising from a hot drink or by standing over a pot of simmering water to get the same effect as a steamy shower.
Breathe Still Air
Moving air, like wind or air stirred up by a fan or heater, can sometimes make coughing worse. Moving air can tickle and irritate your throat and nasal passages, which are particularly sensitive to irritation in people with COPD.
To prevent this, turn off any overhead fans, HVAC ventilation, heaters, or other air-stirring appliances whenever you feel particularly sensitive to coughing. If you remove the air currents indoors and stay out of the wind, you will be less likely to cough and experience other respiratory symptoms.
Drink the Right Stuff

Along with drinking water, there are certain foods that might be able to suppress coughing by reducing the amount of mucus in your airways. For example, one group of researchers found that drinking pineapple juice can help your body get rid of mucus in your lungs, although no other scientists have yet verified these results.
Lemon and honey is another common and potentially effective home remedy for coughing. The acidity from the lemon helps kill bacteria clinging to the walls of your throat and the honey acts as a thick, soothing liquid that soothes your throat and prevents irritation.
Eat to Clear Your Throat
Sometimes thick mucus gets stuck in the folds and the walls of your throat and just won't let go. This gives you an uncomfortable, phlegmy feeling and can obstruct airflow when you breathe.
Sometimes a few gulps of water or a warm drink like coffee or tea can loosen mucus and clear it up, but it's often not enough to do the job. Extra fluids will thin your mucus if you wait and give it time, but you can sometimes get more immediate relief by using solid food to physically brush it off.
Toast is a perfect food for this purpose. It's soft and spongy, and yet rough enough scrape stubborn mucus from the back of your throat. So if you have a phlegmy throat that's bothering you and won't go away, try eating a piece of toast to clear it up.
Medical Remedies for Coughing

When all else fails, you might need to turn to pharmaceutical medications to manage your cough. If you talk to your doctor, he can prescribe daily bronchodilators, recommend over-the-counter medications, or suggest other treatments to help you reduce coughing.
Bronchodilators
Bronchodilators help widen your airways so that it's easier to get mucus out. They relax and open up your airways, bypass blockages, make it easier to breathe, and make it easier to move mucus up and out of your lungs when you cough. Many doctors recommend using bronchodilators before trying other mucus clearance techniques like percussion or postural drainage.
Cough Suppressants

Some studies show that cough suppressant medications like codeine can help people with COPD better control their chronic cough. However, cough medications are not always effective, and you should always talk to your doctor before taking any over the counter medicine.
VapoRub
This is a common remedy for congestion and coughing that could help reduce coughing for people with COPD. You simply rub the thick, menthol-infused cream on your back, throat, and/or chest, and you should feel its effects within minutes.
Throat Lozenges
Throat lozenges, or cough drops, are often an effective way to suppress coughing when you have an irritated throat. Cough drops coat your throat to prevent irritation and usually contain a soothing compound like menthol which can reduce congestion and soothe your throat.
Positive Expiratory Pressure
If you have trouble with breathlessness and coughing while you sleep, you might need to use a positive expiratory pressure device at night. This is a medical device with a tube that connects to a breathing mask that fills your airways with pressurized air.
This pressurized air helps keep your airways open so they don't collapse and obstruct your breathing while you sleep. The widened airways also make mucus less likely to build up and block your airways, preventing coughing and making it easier to breathe.
High Frequency Chest Wall Oscillation
This is a technique for which you need a special vest that inflates and vibrates against your chest and back. This works similarly to chest percussion by loosening mucus in your lungs and airways to make it easier to cough up.
You can do high-frequency chest wall oscillation for several sessions of several minutes each. In-between each session, use controlled coughing techniques to dislodge the loosened mucus and cough it up and out of your body.
Conclusion
Dealing with a chronic cough is hard. It makes it difficult to exercise, sleep, and participate in the activities that you enjoy.
Luckily, with these techniques and home remedies you can reduce your coughing and prevent it from taking a major toll on your life. If you eat a healthy diet, use mucus-draining techniques, and try the other tips in this article you'll likely find your cough much easier to manage.
Treating your cough makes it easier to exercise, breathe, and get more joy and fulfillment out of your life. Start using these cough suppression techniques today to get yourself back on the road to feeling better.
.png)
Creating an effective financial plan is essential no matter who you are or what stage of life you’re in. According to brightplan.com, having organized financials can help you improve your confidence, peace of mind, and reach both long-term and short-term goals. However, if your life becomes complicated by a chronic condition like COPD, you might find that financial planning is a lot more time-consuming and less straightforward.
Not only does COPD come with a lot of added costs like doctor’s visits, medications, and oxygen devices, but it also leads to added stress, anxiety, and worry; all of which can make it feel overwhelming to create a financial plan. Luckily, the more you educate yourself about your disease and the common financial mistakes that COPD patients make, you’ll be well on your way towards creating a more secure long-term plan.
Here at LPT Medical, we take pride in offering cost-effective long-term solutions for your supplemental oxygen needs. We offer a wide selection of portable pulse dose and continuous flow oxygen concentrators, stationary oxygen concentrators, as well as oxygen accessories that help you get the most out of your purchase. Read on to learn about some actionable tips for saving money as a COPD patient and be sure to reach out to us if you’re interested in an oxygen machine.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Reduce Living Expenses
If you think about it, a lot of your money goes into essential things like your monthly rent, food, gas money, car repairs, and insurance. But just because these things are necessary does not mean that you can’t save money on them. In fact, according to a CNBC article from last year, on average, people spend $143 more than their budgeted weekly allowance. And while this may not sound like a whole lot, that adds up very quickly accounting for over $7,000 each year.

Another thing associated with living expenses is that many people assume they only affect younger people. People that are just out of high school or college are oftentimes more aware of their monthly living expenses because they don’t have that much money saved up. As a result, they need to be more frugal in the way that they use things such as utilities or how much they use their car. As we age, however, it’s easier to overspend on living expenses because we have more of a financial safety net.
One popular trend that’s being embraced by many seniors is something called “downsizing.” Simply put, this is the process of significantly reducing your expenses by getting rid of things that you don’t need. In some cases, downsizing could even mean moving from your current home into one that is physically smaller and less costly. By doing so, you’ll be able to save up more money each month for things like doctor’s visits and COPD medication.

Another living expense that COPD patients may struggle with is the prospect of applying to a nursing home. According to AARP, a nonprofit organization designed to support people over the age of 50, the cost of long-term care options like nursing homes is skyrocketing. Because of this, many people with disabilities are opting for cheaper options that don’t break the bank.
Reduce Unnecessary Spending
Unnecessary spending differs from living expenses in the fact that they are not essential. This includes things like subscription services, gym memberships, cigarettes, or any other type of “luxury” product or service. The problem is that nowadays it’s so easy to spend money. Online shopping has become such a common way for people of all ages to pass their time but it’s also very easy to lose track of how much you’re actually spending.

Cigarette smoking is another expense that can really add up over time. Believe it or not, around 38 percent of people with COPD still smoke despite the fact that 85 to 90 percent of COPD cases are the result of smoking. What’s more, smoking a pack a day can run you around $2,292 each year. Not to mention the fact that continuing to smoke while you have COPD will increase your risk of experiencing an exacerbation and cause your diseases to progress more quickly. Inevitably, this will lead to more medical expenses.
Another unnecessary expense that many people fall victim to is subscription services. It seems like just about every product or service nowadays is bound to a subscription payment in hopes that consumers will start one and forget they have it. Unfortunately, this is usually what happens. Take some time to go through your bank statements and identify any recurring costs, and if they aren’t absolutely necessary then you should eliminate them.

Limit Hospital Visits
By far the biggest expense for anyone with a disability like COPD is a hospital visit. You may be surprised to find that the average hospital visit costs the patient $10,000 and hospital stays are responsible for 60% of all bankruptcies. With this information in mind, it should be your number one priority to prevent medical emergencies that facilitate a need to visit the emergency room.

The best way to prevent medical emergencies related to COPD is to follow your COPD treatment plan and avoid exacerbation triggers such as smoke, pollution, and other airborne particles. And due to the fact that infections are the most significant cause of exacerbation, you should also take safety precautions like getting your annual flu shot and staying up-to-date about COVID-19.
The most essential components of your COPD treatment plan include supplemental oxygen therapy and pulmonary rehabilitation. Oxygen therapy will help you keep your blood oxygen levels stable wherever you go which can prevent respiratory failure and pulmonary rehabilitation will keep your lungs and muscles working efficiently making it easier to breathe.
Learn About Social Security Disability Benefits
Old-age, Survivors, and Disability Insurance (OASDI) is the official name for “social security benefits” in the US. This program is funded by the Federal Insurance Contributions Act (FICA) taxes made by employees and matched by employers. According to the official Social Security website, Social Security benefits play a crucial role in the economic well-being of millions of Americans. So, when it comes to managing your finances with COPD, it’s important to know what your social security benefits allowance is.

The social security administration defines a disability as any condition that prevents you from participating in “substantial gainful activity” for 12 months or more. In other words, if you are unable to work due to severe respiratory symptoms you should start collecting social security in order to help you pay for medical expenses. However, in order to determine whether COPD is severe enough to warrant SS benefits, they use something called the “Blue Book.” COPD is listed under section 3.02.
In order to qualify for social security benefits, you also need evidence of your COPD diagnosis. First and foremost, you’ll have to provide a full history of your COPD including symptoms, prognosis, and physical examination results. Below are some of the test results that you should provide:
- Pulse oximetry
- Hospital records
- Spirometry results
- Lung function tests
- Supplemental oxygen prescriptions
- Imaging tests such as CT scans
- Arterial blood gas tests
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Remember that it is possible for them to deny your social security benefits claim for COPD. Because of this, it’s important to gather all the medical information you can before filling out the claim. It takes around 3 to 5 months to process your documents and let you know the results, so if you are careless in how you go about the process, you may be waiting a lot longer than expected to start receiving your benefits. Here are some tips to ensure that you’re doing the process correctly:
Fully Understand the Blue Book
The Blue Book also called the “Disability Evaluation Under Social Security” highlights medical conditions and the symptoms that need to be specified in order to receive benefits. You can either view an updated version of this book online or you can receive one in the mail which may take several weeks. This document is used as a guide book for agency officials when determining the validity of your application, so it’s important to read and understand it, especially the section that pertains to your condition.
Receive Up-to-Date Lung Function Tests
One good way to ensure that you’re receiving your full allowance is to get up-to-date tests. For example, if you received a spirometry test several years ago, you may want to consider having another test done. COPD is a progressive disease meaning it tends to get worse over time, so you want the documents you send to the SSA to reflect that.

Learn About Medical Vocational Allowance
In certain situations, it is possible for someone with severe disability to not qualify for social security benefits. However, there is something called a medical vocational allowance which can make this possible. What you’ll need to do to qualify for this is to prove that your disability has prevented you from working a job that you’ve been trained to do. Since COPD significantly impairs lung function, you should have no problem proving this if you are involved in manual labor work.
Contact a Social Security Attorney or Advocate
If you’re worried about qualifying for social security benefits or you believe you have been wrongly denied for benefits, you may consider working with a social security attorney or advocate. One of the greatest benefits of contacting an SSDI attorney is that you’re protected by something called a contingency fee arrangement. What this means is that your attorney is only allowed to charge you a fee if you win the case. What’s more, the fee is capped at 25 percent of the past-due benefits awarded to you, up to a maximum of $6,000.

Cut Costs on Medication
Medication is another area that COPD patients tend to overspend in. There are a large variety of medications that you may be required to take for COPD including bronchodilators to prevent shortness of breath, antibiotics that prevent infection and exacerbations, and anti-inflammatories which reduce flare-ups. Unfortunately, many COPD patients purchase these expensive medications without taking the time to consider how they can save money. We discussed this topic in detail in a previous post, but we’ll go over it again for your convenience.

Order Prescriptions Online
Most peoples’ gut reaction after being given a prescription is to go to their local pharmacy. While there’s nothing wrong with this approach, it will likely mean spending significantly more money on your medications. Rather, it’s often a better option to research online pharmacies because there is more competition meaning they will offer lower prices. Many online pharmacies also offer free shipping and quick turnaround times, so you shouldn’t have to wait too long to receive your medication.
Purchase Generic Brands
While you’re probably constantly bombarded with advertisements of name-brand medications, these are not the only options out there. In fact, many generic brands offer the same exact product for a much lower price. If you want to save some money, ask your doctor about generic brand medications to see if they will work for you.

Use a Patient Assistance Program (PAP)
Believe it or not, many pharmaceutical companies offer patient assistance programs designed to help low-income people pay for their medication. Oftentimes, these programs require you to make below a certain income, you must be a US citizen, and you can’t be a part of any other patient assistance program with a different pharmacy.
Ask Your Doctor for Advice
Last but certainly not least, you should always consult your doctor before making decisions about your medication. Not only will he/she have advice for you to save money on your medications, but he/she may also warn you of common pitfalls of the pharmaceutical industry. Medication is expensive these days so it’s important to take the time to understand your options.

Participate in a Clinical Trial
A clinical trial is a program designed to test the safety and efficacy of new medications and treatments before they hit the market. Clinical trials are carefully designed by medical professionals and they must be approved by the US Food and Drug Administration (FDA). These research programs depend on volunteers, so it’s very easy for anyone to sign up for one and get involved.

The benefit of participating in clinical trials for COPD is that you may be able to test new medications for free and in some cases, researchers will even pay you to participate. What’s more, the researchers will thoroughly examine your medical history to ensure the new medication doesn’t negatively interfere with your condition. Generally speaking, clinical trials are safe and they can save you hundreds or thousands on your medical expenses. It’s also nice knowing that you have the power to help researchers test new drugs and treatment procedures. If you’re interested in researching COPD clinical trials, visit clinicaltrials.gov.
Invest in a Long-Term Oxygen Therapy Solution
Supplemental oxygen therapy is a reality for most COPD patients. Whether you have stage one COPD or stage four COPD, medical oxygen helps to ensure that your blood oxygen levels remain stable and that you can breathe easily. Unfortunately, many COPD patients take the wrong approach when it comes to purchasing a medical oxygen device and it often costs them more in the long run.

Oxygen tanks are a very popular oxygen for oxygen therapy because they are accessible and have low upfront costs. The problem, however, is that the costs add up very quickly because you have to keep refilling them. Since they run out of oxygen so quickly most people keep two or more on hand at any given time. They’re also really heavy, bulky, and dangerous to use.
Alternatively, you could invest in a long-term oxygen therapy solution like a portable oxygen concentrator. Rather than refilling oxygen concentrators as you would with an oxygen tank, these devices draw in ambient air and output medical-grade oxygen. Since these are electronic devices, all you need to do is have access to a power outlet in order to charge the batteries. Additionally, portable oxygen concentrators are extremely lightweight and easy to carry making them perfect for traveling and getting out of the house.

If you’re looking to save money in the long term and you want a powerful, reliable oxygen device, we recommend either the Caire FreeStyle Comfort or the Inogen One G5. Each of these units is 5 pounds or under, they offer over 10 hours of battery life, and they can last you between 5 and 7 years with minimal maintenance. They also have 3-year warranties which will protect you from rare occurrences like manufacturing defects.
.png)
The above portable oxygen concentrators are pulse dose delivery, meaning they deliver oxygen whenever the user inhales. In certain situations, your doctor may require you to use continuous flow instead. In this case, we recommend using the Respironics SimplyGo. This oxygen machine is not quite as light as the other two but it is the most reliable and trusted continuous flow portable oxygen concentrator on the market.

While portable oxygen concentrators have a larger upfront cost, they are always the best long-term solution. Another benefit of owning one is that if you ever decide you want to upgrade to a newer model or your doctor tells you that you no longer need oxygen, many oxygen retailers will buy back your oxygen concentrator. This is usually not possible with oxygen tanks because most oxygen companies just rent them out rather than selling them.
Speak With a Financial Advisor
Seeking out the help of a financial advisor is usually a last resort for the average person. Some financial advisors charge a pretty penny for their work and some people simply have nothing to gain from it. However, if you’re overwhelmed with financial decisions after being diagnosed with COPD and you can find the right financial expert to go to, it’s always something to consider.

A financial advisor will walk you through all of your financials and put together a long-term plan that will help you meet your goals. Oftentimes, they will tell you where to invest your money and give you a monthly allowance for what you’re allowed to spend. They’ll also help you better understand how to deal with the increasing number of medical expenses that you’re having to deal with.
Conclusion
Financial planning is something that we all have to deal with throughout our life. Taking the time to understand how much money you have and understanding where you should invest that money is crucial to living comfortably. Unfortunately, if you’re coping with a chronic lung disease like COPD, asthma, or pulmonary fibrosis, the process of planning your finances may be difficult and time-consuming.
On a positive note, if you take the time to understand your condition and some common mistakes that COPD patients make, you can avoid some major financial pitfalls. Hopefully, some of the tips listed in this article got you started on the right foot, and if they did, be sure to share it with a friend or loved one who may be struggling with the same issue.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!
















