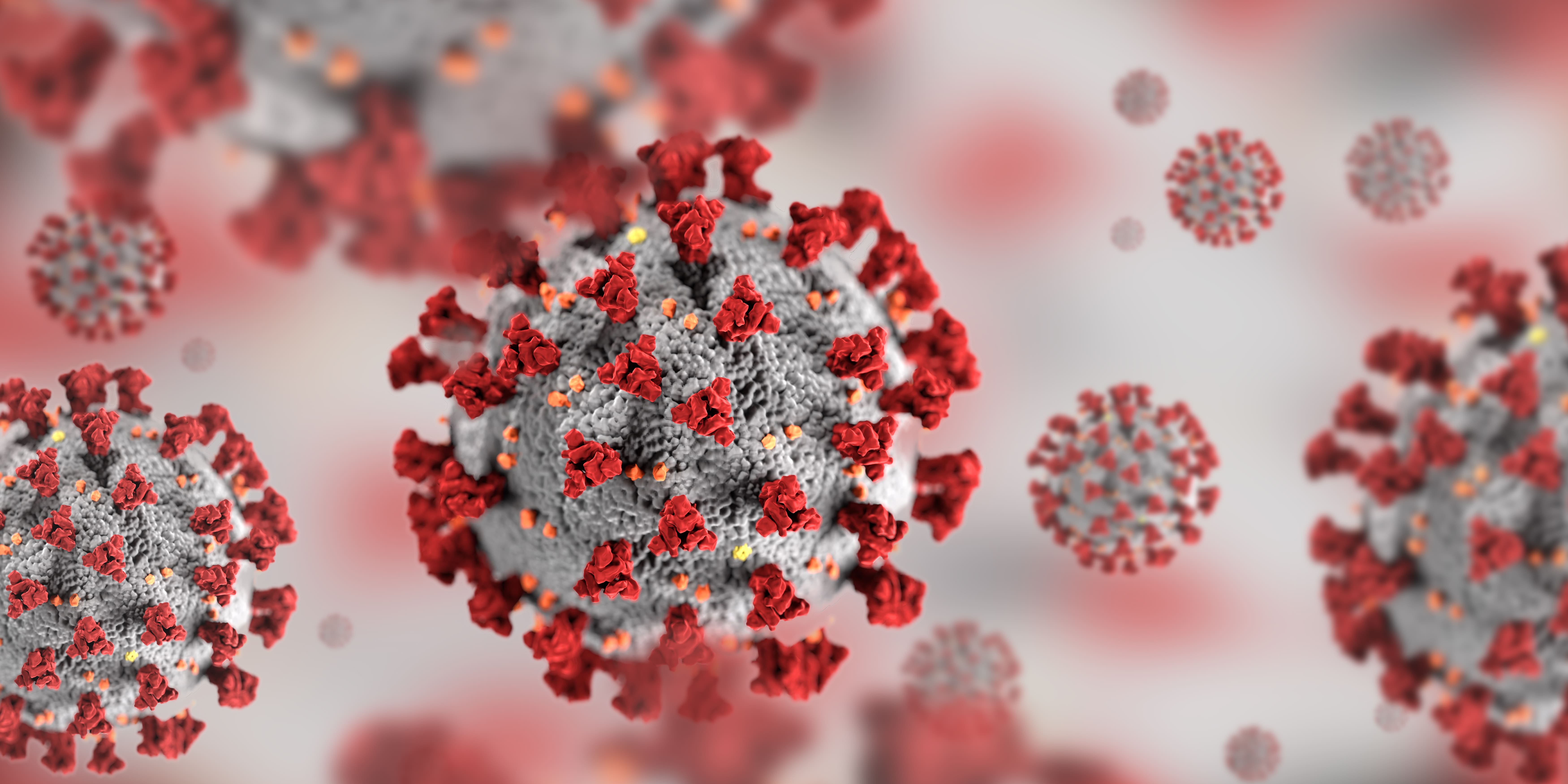
COVID-19 and lung damage is still a very new problem, and while research so far can tell us some of the impacts of COVID-19 on respiratory disease there is still a lot of uncertainty. That being said, it is important to fact-check information that you see on the internet, especially when it comes to something as serious as COVID-19 and lung damage.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
COVID-19 is a respiratory illness that is fast spreading and highly contagious, and while the vaccine is rolling out in the United States and internationally, catching COVID-19 is still cause for concern.
Here is a summary of the blog you are about to read:
- COVID-19 has lasting effects on your respiratory system
- People with lung disease have a high chance of experience harsher symptoms from COVID-19 than a person with no pre-existing conditions
- Don’t be fooled, if you are vaccinated you can still catch COVID-19, yet the effects of covid are much more mild than if you are not vaccinated, and this includes the damage to your lungs
How Does COVID-19 Affect your Lungs
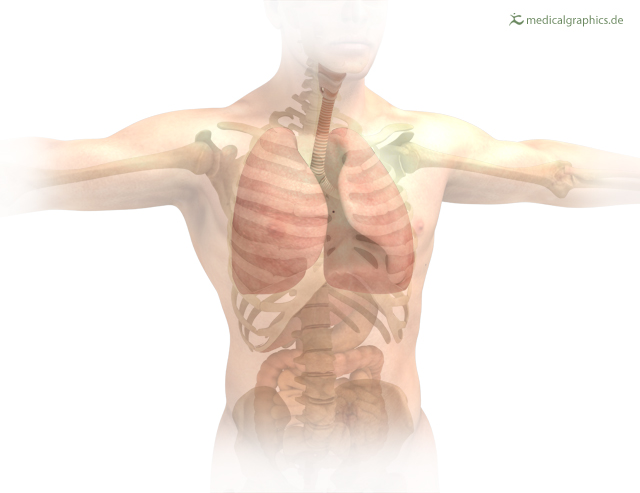
COVID-19 can affect your lungs in mild and sometimes severe ways, and a lot of this depends on your health prior to catching the virus. If you have a relatively healthy respiratory system and have no pre-existing conditions COVID-19 can still hurt your lungs but not as badly as someone who already suffers from a chronic illness.
One of the most common implications caused by COVID-19 is pneumonia and in the most severe cases, acute respiratory distress syndrome. There is also the possibility of Sepsis as a complication of COVID-19, and this can also cause lasting damage to your lungs and other organs.
COVID-19 and Pneumonia
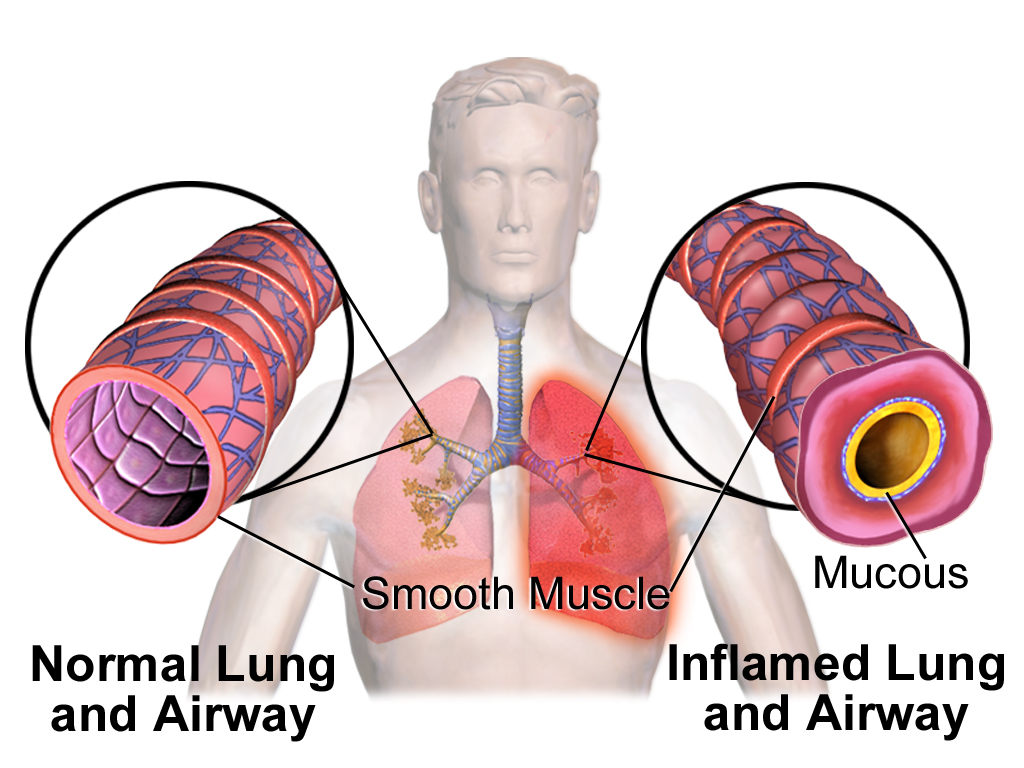
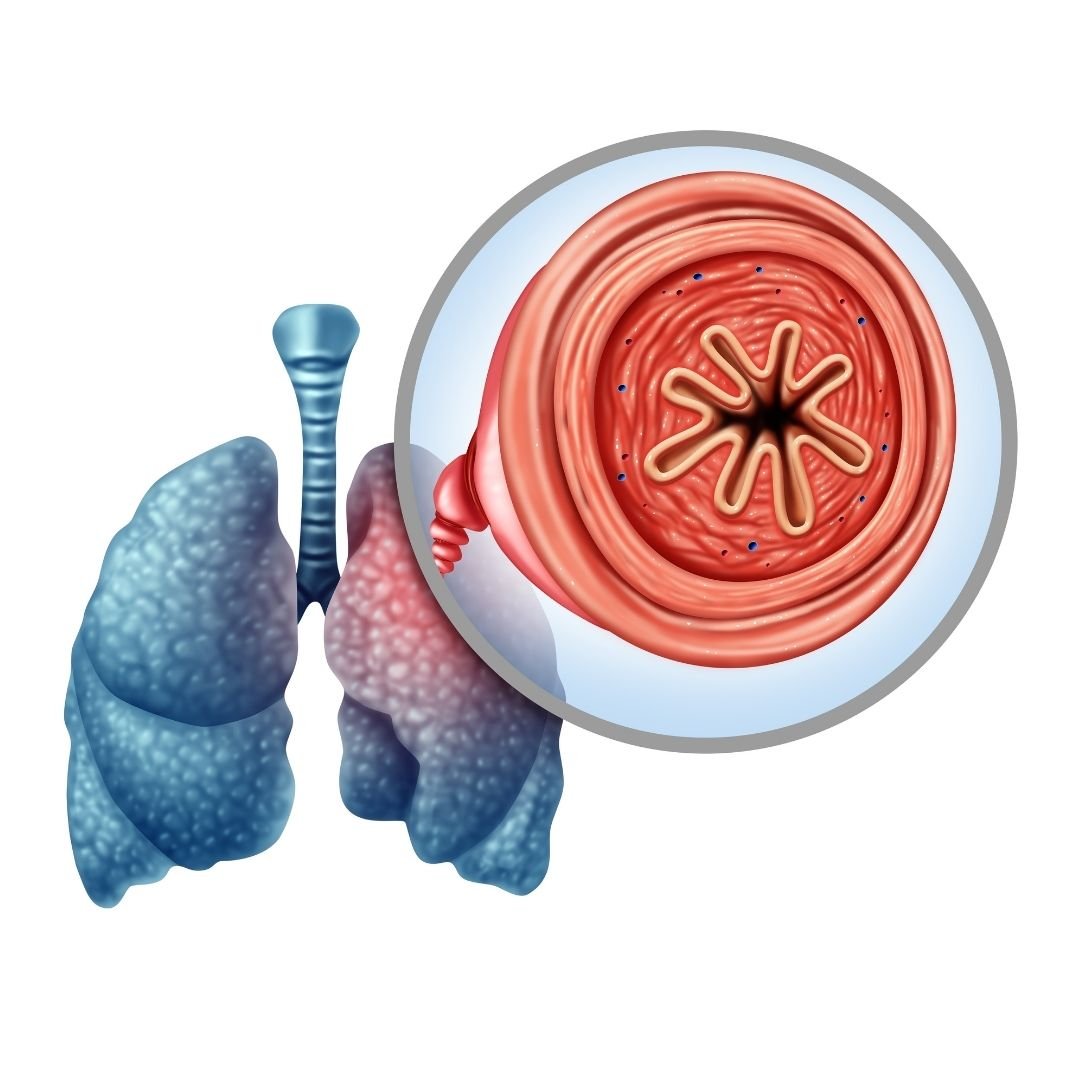
When you get pneumonia, your lungs fill with fluid and become inflamed, leading to breathing difficulties, this is extremely painful for lung patients who have diseases like Chronic Obstructive Respiratory Disease (COPD). When someone with COPD gets COVID-19 the symptoms can become so severe they require treatment at the hospital with a portable oxygen concentrator or even a ventilator.
Pneumonia occurs when your air sacs in your lungs fill with fluid, this limits their ability to take in oxygen and causes shortness of breath, a persistent cough and other symptoms.
While most people recover from pneumonia without any lasting lung damage, the pneumonia associated with COVID-19 can be severe, and people with lung disease have an even harder time healing from this.
Even after the disease has passed, the damage to your lungs may result in breathing difficulties that take a lot of time to heal completely, and with chronic conditions, it is unlikely the damage will heal completely.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Acute Respiratory Distress Syndrome (ARDS) and COVID-19
COVID-19 that causes pneumonia can progress further into a more severe state, and the air sacs which become filled with fluid start to leak from blood vessels in your lungs. Inevitably, breathlessness occurs, which can cause acute respiratory distress syndrome. ARDS is essentially a version of lung failure.
Patients with ARDS are usually unable to breath by themselves and may require a ventilator to help their bodies circulate oxygen through their body.
Sepsis and COVID-19
In severe cases of COVID-19 and people who also suffer from preexisting conditions, sepsis is another serious complication. Sepsis is a fast spreading infection that moves through the bloodstream, causing tissue damage everywhere it goes.
Sepsis causes long-lasting lung damage and also affects other organs in the long term.
Reducing the Chance of Lung Damage from COVID-19

If you have chronic medical conditions, such as diabetes, COPD or heart disease, its crucial for you to continue taking your medication and treating your disease optimally.
Take your oxygen as prescribed and monitor your health status and report to your doctor over the phone regularly. You can also use a pulse oximeter to measure when and if you are breathing appropriately.
Everyone, especially lung patients, need to maintain adequate nutrition by eating healthy and staying hydrated, this will keep your immune system healthy. Also double check that you are up to date with all of your vaccinations, even just getting the common flu can weaken your immune system and leave you more susceptible to catching COVID-19.
Also, be wary of any information you read on the internet that's not supported by researchers and institutions which require a peer review process in order to be published. Because COVID is relatively a new virus, the research is still in progress meaning that most results from studies over the past year and a half are not conclusive yet.
For example, you might have seen reports of vitamins, minerals and prophylaxis medications that can prevent/ or reduce lung damage, however there are no peer reviewed studies that are supporting it at this time.
The best way to avoid COVID-19 and worsening lung damage is to get the COVID-19 vaccine.

Is the vaccine safe for people with lung conditions?
There have been a plethora of studies that have concluded the vaccine is safe for people with lung conditions. The vaccine has been tested on people with long-term conditions and people from all age groups including older people.
In fact, it has been decided that people who are at high-risk should be prioritized to get the vaccine first. At this time, there is no reason to think the vaccine interferes with any medications and therefore, your treatment for your lung condition should continue as normal.
If you have asthma and you use biologics (otherwise known as mAbs, or monoclonal antibodies), talk to your doctor to discuss the timing of your vaccine and your asthma biologic. There is no evidence to show the vaccines are unsafe for you, however it’s advisable that there should be 7-day gap between your vaccine and your next asthma biologic.
Do not stop taking or change any of your medicines without speaking to your doctor first.
So how do we know the vaccine is safe?

Any approved vaccines must meet a strict criteria of safety, quality and effectiveness. And so all of the approved coronavirus vaccines go through certain clinical trials and they are checked that same way as any licensed medicines are checked. Other vaccines are being developed, but they will only be available to the public once they’ve been thoroughly tested.
A vaccine can not be given to people until the FDA oversees extensive lab testing of the vaccine. Usually this can take many years in order to ensure it is safe and effective. Because the COVID-19 vaccine was only developed and tested in a short period of time, some risk is involved, however data indicates that all of the available COVID-19 vaccines are safe.
Also the risk of COVID-19 is far greater than the small risk of the vaccine.
We know this because we can look at the rate of severe or life-threatening reactions to the COVID-19 vaccine, which is estimated to be about 1 in 100,000 patients, whereas the risk right now of dying from COVID-19 is substantially higher than that.
There are many deadly diseases that have been technically eradicated with the introduction of a vaccine. For example, Polio, Tetanus, The Flu (Influenza), Hepatitis B and A, Measles, Whooping Cough, and so many others have a vaccine that is successful in reducing the contamination and spread of the disease, and save millions of lives. COVID-19 can be added to this list eventually!
Overview
The risk of COVID-19 having long term effects and damaging your lungs is high for any person, but extremely high for someone with a pre-existing lung condition. If you have lung disease already, catching COVID-19 could mean hospitalization and it can be life threatening.
There are a number of ways to avoid catching COVID-19 by social distancing, washing your hands, and wearing a mask, and on top of all of those recommendations is to get vaccinated.
If you are still wary of getting the vaccine, talk to your doctor, they can go over your medication that you take and reassure you that the vaccine will not interfere with your medical condition nor your treatments.
Side effects of the vaccine are very normal, and oftentimes unavoidable and even uncomfortable. That being said, these short-lived side effects are much less dangerous than being exposed and unprotected against the coronavirus.
If you have a lung condition like asthma, COPD, of cystic fibrosis, continue to treat your disease during the pandemic. It is important that you stay healthy and get stronger so that your body is capable of fighting ailments including COVID-19. While exposure to coronavirus is extremely dangerous due to the virus and its contagious properties, the healthier you are the better.
If you need oxygen, be sure you have a portable oxygen concentrator that is reliable and durable. For all of your oxygen accessories needs, head over to the LPT Medical website or call 1(800)-946-1202 to speak with a respiratory specialist.

If you are prescribed an oxygen concentrator for chronic health problems and you experience symptoms of COVID-19, call your doctor. Do not change your oxygen levels on your own, unless you have been told to do so by your doctor.
Over 16 million Americans knowingly have COPD, meaning they have been diagnosed with COPD and are currently treating their COPD. The harsh reality for all of these people is the COPD has no cure, this progressive disease will stick with you, and if gone untreated take years off of your life. That being said, treating COPD has been heavily researched, and following a treatment plan for your personal diagnosis will increase your life expectancy.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
This blog is an informative read for anyone who has COPD no matter how severe or mild. It's also a great read for you if you are perfectly healthy and are a caregiver for a COPD patient, or you are just curious about your respiratory health, this blog is a great read for people who are curious about how COPD affects life expectancy.
Treating COPD to Increase Life Expectancy
The only way someone with COPD can add years to their life is by using oxygen therapy. Oxygen therapy is when you need to use a supplemental oxygen device like a portable oxygen concentrator in order to maintain a healthy oxygen level. Once your oxygen levels are stable, you can begin to treat COPD in other ways that will slow down the progression of the disease and ease the severity of the symptoms.

The symptoms of COPD you you should be treating can be any of the following:
- Cough
- Breathlessness
- Mood swings
- Fatigue
- Excess production of mucus
If COPD goes untreated, the consequences are extreme, and if you are reading this blog it is likely that you already know you have COPD, or you are in the process of being diagnosed with COPD. If your case is the latter, getting tested for COPD will be the first step towards treating your symptoms. The longer you wait to get tested, the more time goes by where the progression of your disease worsens at a faster pace due to inadequate treatment.

Life expectancy is directly related to how you treat COPD, and because this disease does not have a cure, proper treatment is the only fight against time you have when it comes to living with COPD.
You can treat your symptoms above by following your doctor's recommendations and this will likely include some or all of the following treatments:
- Exercise, try yoga or tai chi for respiratory patients
- Eat foods that promote respiratory health
- Join pulmonary rehabilitation courses
- Follow your oxygen prescription if you have one
- Use you COPD medications as prescribed
- Avoid lung irritants such as allergens, pollution, and smoke
- Stop smoking cigarettes or inhaling secondhand smoke

Even with treatment COPD symptoms will arise in your daily life, you can learn to deal with symptoms by trying some of the following methods for easing discomfort:
- Breathing techniques can be used to open your airway and increase lung strength, this will help with breathlessness
- Meditation particle can help your breathing when you experience a COPD exacerbation, it can also help easy anxiety and stressed caused by breathlessness
- Coughing and clearing techniques can be used daily to removed excess mucus from you airways which can help ease your coughing and breathlessness
COPD Diagnosis
First and most importantly, being diagnosed with COPD is a good thing, and this might sound crazy, but you cannot go back in time and change the course of time in which you developed COPD, so being diagnosed is the next best thing. And here is why: Once you have been diagnosed with COPD, your life begins again, you start to take care of the symptoms that have been impacting your life, you start to ease the pain and discomfort by utilizing tools like medications, oxygen therapy devices, and pulmonary rehabilitation courses.
People with COPD are are more likely to experience the following complications compared to someone without it:
- Being limited in physical activity
- Difficulty walking or climbing stairs
- Be unable to work
- Need special equipment like Inogen brand oxygen devices
- Engages less socially
- Have increased confusion or memory loss
- Have more emergency room visits or overnight hospital stays
- Have other chronic diseases like arthritis, congestive heart failure, diabetes, coronary heart disease, stroke, or asthma
- Have COPD induced depression or other mental or emotional conditions
There’s No way to Predict the Exact Life Expectancy
The obvious question is, “How long can I live with COPD?” but there is no way to predict the exact life expectancy despite the stage of COPD you are in. That being said, it is known that having this progressive lung disease can shorten your lifespan.
But how much this disease shortens your lifespan depends on your overall health, how you treat the disease on the daily, and whether you have other diseases such as heart disease or diabetes.
What is the GOLD System
COPD effects over 16 million Americans, and research about this disease has a long history and is ongoing. There have been numerous studies that assess the health of someone with COPD all of which have contributed to the GOLD system.
The most current assessment is to take a spirometry lung function test results and compare that to a person’s symptoms. The result can help predict life expectancy but more accurately guide treatment choices for those with COPD.
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) is one of the most used systems of classifying COPD and its effect on your health.
GOLD is made up of an international team of lung health experts who look over current research and produce updated guidelines for doctors to use for testing and treating people with COPD.

Recently, doctors started to use the term “grades” rather than “stages” to assess the degree of severity of the disease. Grading is a way to measure the severity of a person's COPD. It uses the forced expiratory volume (FEV1) to determine the amount of oxygen a person can actively exhale from their lungs in one second, this gives the doctor a rather accurate description of the person’s lung health and allows them to categorize the severity of their COPD.
Based on your FEV1 score, you receive a GOLD grade as follows:
GOLD 1: FEV1 of 80 percent predicted or more
GOLD 2: FEV1 of 50 to 79 percent predicted
GOLD 3: FEV1 of 30 to 49 percent predicted
GOLD 4: FEV1 of less than 30 percent predicted
The second part of the GOLD system is to compare the FEV1 score to the patient's symptoms. Doctors will analyze your symptoms of dyspnea, or difficulty breathing, and degree and amount of acute exacerbations, which are flare-ups that may require hospitalization.
How these aspects of health compare will categorize people in one of four groups: A, B, C, or D.
Grouping COPD Severity, Examples:
Here are some examples of how COPD patients are put into groups.
- Patients X experiences no exacerbations or maybe one and they did not require hospitalization in the past year. Their breathing assessment or their FEV1 score was GOLD 1 and the amount they only experience a few symptoms they have would be in group A.
- Patient Y has had one exacerbation that required hospitalization, or possibly two exacerbations that did or didn’t require hospital admission in the past year. They also scored GOLD 3 and had several breathing symptoms that would be in group C.
Under the most current GOLD guidelines, someone who scored a GOLD Grade 4, Group D, is someone that has the most serious classification of COPD. And they’ll technically have a shorter life expectancy than someone with a label of GOLD Grade 1, Group A.
What is the BODE index
There are other measures that can be taken to determine the severity of COPD by using more than just the FEV1, it is called the BODE index.
BODE stands for:
B - body mass
O - airflow obstruction
D- dyspnea
E - exercise capacity
This is a measure of the overall way COPD affects your life. Keep in mind that while the BODE index is used by some doctors, its value or meaning behind the results may be less accurate than what it was once considered due to the amount we know about the disease now.
Body mass
By looking at you body mass index (BMI), a measurement based on your on height and weight, it can be known if you are overweight or obese, or too thin. Someone who is very thin and has COPD has a lower outlook.
Airflow obstruction
This refers to the FEV1, which is the same test as in the GOLD system that you read in the section above.
Dyspnea
Having trouble breathing is something that can be noted in order to assume the outlook for someone with COPD.
Exercise capacity
Being more tolerant of exercise and having the ability to be physically active suggest you have a better outlook. It’s often measured by a test called the “6-minute walk test.”

Mortality Rates in COPD Patients
COPD is a serious disease and similarly to cancer, the predicted life expectancy is based largely on the severity or stage of the disease which for COPD can be estimated using the GOLD system or BODE.
One of the best ways to explain the mortality rate in COPD is to give an example:
In study that was in the International Journal of Chronic Obstructive Pulmonary Disease, a 65-year-old man with COPD who currently smokes tobacco has the following reductions in life expectancy, depending on stage of COPD:
GOLD 1: 0.3 years
GOLD 2: 2.2 years
GOLD 3 or 4: 5.8 years
For this same group, if the 65 year-old man were to continue smoking they would be reducing thier life expectancy by an additional 3.5 years, rather than those who never smoked and didn’t have lung disease.
For former smokers, the reduction in life expectancy from COPD is:
GOLD 2: 1.4 years
GOLD 3 or 4: 5.6 years
This is just one article that was published and while there is a lot of research on this subject, the mortality rate for COPD patients is still just an estimate.
Continue Treating COPD for the Best Outlook

What’s the goal of these methods to predict life expectancy? The more you are able to treat your disease the slower you will progress to a higher grade of COPD.
The first step towards slowing down the progression of COPD is to stop smoking if you smoke. Also, avoid secondhand smoke or other irritants such as air pollution, dust, or chemicals.
Maintaining a healthy weight and eating small, frequent meals can help your breathing immensely. Learning how to improve breathing with exercises such as pursed lip breathing will also help.
Pulmonary rehabilitation program is another great way to learn about your disease as well as how you can implement exercise into your life safely and effectively, all while connecting with other people that can relate to your health condition.
One of the very best things you can do for you lung health is to exercise, and while physical activity may be challenging it really helps your lungs and the rest of your body.
The bottomline is that, the more you can do to improve your overall health, the longer and fuller your life can be.
Dealing with equipment issues as a chronic obstructive pulmonary disease (COPD) patient is just a part of the process. The equipment can be the most top of the line quality and you still may have malfunctions or trouble getting the equipment to work within your lifestyle.
The truth of the matter is that, once you start to use equipment to help you treat symptoms associated with COPD your lifestyle will be affected. Whether this is in a positive way or a negative way will depend on the equipment you have, and how well you know how to use it.
It is important to learn how to use your equipment correctly as well as know how to troubleshoot issues associated with the equipment.

COPD Equipment
There are therapies you rely on every day to help you breathe. There are a variety of medical devices from inhalers to oxygen concentrators that are designed to treat symptoms associated with COPD either by giving you additional oxygen supply or medication.
Therapies like these allow you to live better with COPD than if you were to live without them, but using the equipment and taking medication everyday does require a bit of a learning curve.

Take the time to learn about all of the common devices prescribed for COPD plus info on how they work in this blog.
In this blog you will learn about portable oxygen concentrators and how to troubleshoot common problems users have with these devices. We will also talk about common problems people have with oxygen tanks, both liquid and compressed oxygen.

Inhalers are a common form of medication for people with COPD, to use these effectively is important so you get the right dosage of medication, we will discuss how to use your inhalers properly.
Beyond inhalers and supplemental oxygen we will also talk about how to use and take advantage of other common COPD equipment!
Supplemental Oxygen
![]()
Supplemental O2: Compressed Oxygen
Even though there are more modern and sleeker forms of oxygen therapy nowadays, when people think of “supplemental oxygen”, the cylindrical metal-tank system typically comes to mind.
The oxygen from this tank is delivered through a thin plastic hose attached to a cannula. These cylindrical tanks come in various sizes, depending on the amount of oxygen you need.
Your doctor will prescribe you the most beneficial amount of oxygen by giving you a flow rate to set your oxygen device.

It is important for your healthcare team to show you how to adjust gauges on the tank to control the oxygen flow rate, it is common for you to need to adjust the “flow rate” depending on your activity status.
You will also need a system to refill the tanks whether you get new tanks delivered weekly from a supply company, or have someone come to refill the tanks.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Streamlining the process of getting your oxygen tanks refilled is challenging because you are dependent and at the will of the oxygen supply companies. Having patiences but also having a full back-up canister is crucial here. Running low on oxygen is a stressful situation you should try to avoid at all costs.
Supplemental O2: Liquid Oxygen
The benefit of a liquid oxygen system is that it doesn't need to be plugged in because it doesn't run off of electricity or batteries, however, it is not the easiest form of supplemental oxygen therapy because it must be refilled, and in doing so it must be handled with caution.
Liquid oxygen is extremely cold— 200 degrees Fahrenheit— it can burn your skin if you’re not careful while handling the equipment for refilling.
Oxygen must be compressed and cooled to a level that it becomes highly concentrated oxygen that you are able to breath in and process in your body easily.

It is likely you will have a stationary storage unit that is a large reservoir of oxygen and a different smaller portable container to bring when you’re moving around.
To streamline this process, you will have to get very good at refilling your portable oxygen canisters, and maintaining sustainable levels of oxygen in the reservoir so you never run low on oxygen. This will require a relationship with an oxygen supply company for deliveries and refills.
Supplemental O2: Oxygen Concentrator

If you are an active person, a traveler, independent, or simply enjoy user-friendly equipment you will need a portable oxygen concentrator as your supplemental oxygen therapy device.
A new generation of lightweight, portable oxygen concentrators, like the Inogen One G5 and the Caire Freestyle Comfort among others, have made it possible to have an active life while using oxygen support like never before.

An oxygen concentrator draws in air from the room around you, purifies it, compresses it, stores it in a tank, then delivers the fresh air via cannula to your waiting lungs. It sounds like a big job for a small compact device! And it is!
Modern technology has allowed for oxygen manufacturers like Inogen to create small lightweight oxygen devices with batteries to last for hours! Meaning you can carry your device with you whenever you go, and simply charge the device as you would a cell phone so you never run low on oxygen.

There are now smaller, more compact portable oxygen concentrators that also have powerful pulse flow settings and long lasting battery life. The rechargeable batteries make it easy to use your device all day and night.
Inhalers

One of the very first things your doctor prescribed to you once you were diagnosed with COPD was some prescription medications to help you manage your symptoms.
There are two types of inhalers that are most common for COPD management, one for daily maintenance meds and another “rescue” inhaler for symptom flare-ups.
Inhaled bronchodilators, for example, work to open airways for easier breathing as needed or long-term, while corticosteroids are used to fight airway inflammation.
How to Use your Inhaler properly
 Every inhaler comes with its own instructions. In general, here’s how to use one:
Every inhaler comes with its own instructions. In general, here’s how to use one:
- Remove the cap from the inhaler.
- With the mouthpiece facing down, shake the inhaler for about five seconds to mix the medicine.
- Then use one of these techniques:
- Open-mouth technique: Hold the mouthpiece 1 1/2 to 2 inches from your mouth.
- Closed-mouth technique: Put the mouthpiece between your lips and close your lips tightly around it.
- With a spacer: Place the MDI inside the spacer and close your lips around the spacer.
- Gently breathe out.
- Press the inhaler and, at the same time, take a deep breath in through your mouth. Keep breathing in for 3 to 5 seconds.
- Hold your breath for 5 to 10 seconds to get the medicine into your airways.
- Relax and breathe out slowly.
- Repeat the process if you need more puffs of the medicine.
Benefits of Inhalers

They are easy to use and can be used with many different types of COPD drugs, including steroids, bronchodilators, and combination medicines. You also get the same dose of medicine each time you use them.
Drawbacks of Inhalers
require you to coordinate between activating the medicine and breathing it in. It’s also necessary that you breathe in slowly and deeply. If you breathe in too quickly, the medicine will hit the back of your throat, and much of it won’t reach your lungs. You may also need to use a spacer to get the medicine into your lungs.
Nebulizers

Nebulizer can be an easier option for people with COPD who find it difficult to take their meds via inhaler.
Nebulizers are machines that convert liquid medicine into a mist. The drug particles are contained in tiny aerosol droplets inside this mist, which you can then inhale through a mouthpiece or mask.
A great advantage of a nebulizer is that it gets the medication deep into your lungs where it's needed most.
For nebulizers to work, you must use it correctly, however patients with COPD using nebulisers at home experienced problems functioning these devices. Talk to your healthcare team and be sure they are effectively supporting you in the use of your nebulisers at home.
Smartphone Apps
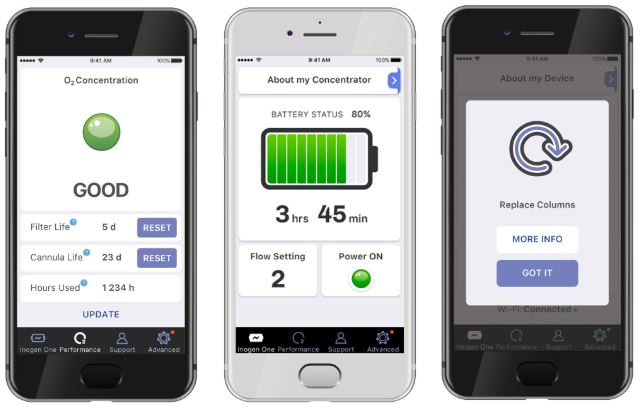
COPD patients can use their smartphones as educational sources and use it to help monitor your COPD symptoms. Your phone is able to alert you when you are experiencing exacerbations that might warrant a call to your pulmonologist.
There are apps you can download that offer a daily questionnaire to rate your symptoms.
You can also check local air quality to avoid airborne irritants via the Environmental Protection Agency’s AirNow app.
CPAP or BiPAP

Often used to treat sleep apnea, continuous positive airway pressure (CPAP) and bi-level positive airway pressure (BiPAP) machines open your airways for better breathing normally while you are sleeping.
Both a CPAP and BiPAP device have a mask that is applied over your face. Then pressure is supplied to open up your airways.
A CPAP machine delivers constant pressure, this pressure can be changed when you aren’t using the device. Most patients require between 6 and 14 cmH20 and the average setting is 10 cmH20, however, the setting you use will depend entirely on your condition and the setting that your doctor prescribes.
![]()
It’s also important to note that every CPAP machine has different capabilities, so you’ll want to make sure it meets your needs before purchasing it.
A BiPAP machine is less common than the CPAP, and it has two different pressure settings: one for inhalation and one for exhalation. The BiPAP machine will automatically detect whether you’re inhaling or exhaling and administer the pressure accordingly. Typically, a higher pressure will be applied when you’re inhaling.
Mucus-Loosening Devices
Mucus build up is a common symptom of COPD. It can affect your breathing by clogging your airways, and it can also induce an uncontrollable cough that lasts the day and night.
A high-frequency chest wall oscillator is an inflatable vest that massages your chest wall to loosen the excess mucus. This will help you cough out the mucus while also using proper coughing and clearing techniques.
Positive expiratory pressure therapy (PEP) is another method to clear mucus. PEP is where you inhale through a mouthpiece, then exhale against a one-way valve that provides resistance. This creates a pressure in your airways to move up mucus.
Overview
We hope that you learned about the equipment that you, as a COPD patient, may need.
A lot of equipment you will need to use everyday, and having the best equipment that you also know how to use is very important for managing this chronic disease.
For instance, a portable oxygen concentrator will be your companion for the rest of your life, therefore it should be reliable and easy to use! Call 1+(800)-946-1201 if you are in the market for a new oxygen device!
Speak with your healthcare team about the other equipment you use, and make sure you are reaping the benefits of the medications and other management tools in your COPD treatment routine!

Flu season is just about in full swing here in the northern hemisphere. October through March are the coldest months of the year, creating a viable environment for the flu virus to spread and infect peoples' immune systems. Many people are wondering if they should get a flu shot this year, and you might be curious about the same thing.
Considering the state of the world, and our continued efforts to mitigate, manage, and survive the COVID-19 pandemic, some people may be hesitant to get a flu shot this season, especially those who are immunocompromised and ones with pre-existing conditions.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
However, catching the common flu can be just as scary and harmful as catching COIVD-19 for people who suffer from COPD and other respiratory illnesses. So the flu vaccine is imperative for people who are trying to stay away from the hospital this season, and to help minimize their impact on the already influx of hospital admissions due to COVID-19.

It is also concerning for healthcare workers and infrastructures going into this flu season because the flu and COVID-19 have similar symptoms and oftentimes, cases require similar equipment from hospitals and health labs, which makes the COVID-19 pandemic during another flu season even more concerning.
As one of the leading local medical oxygen equipment company in Boca, Raton Florida and a long-time established medical equipment company in Denver, CO, we are dedicated to keeping our communities safe and protected while we continue to offer our customers alternative oxygen therapy devices.

In this article we are going to talk about the flu vaccines, and why it is so important for our community of respiratory patients and COPD caregivers to get a flu shot this season. We will answer a few questions that will clear up any uncertainties about getting the flu vaccine. If you use a portable oxygen concentrator, you already have an advantage in staying healthy throughout the flu season, but getting a flu shot is still
But first, we want to give some of our reader the local web-pages where the Center for Disease Control (CDC) tracks the flu season in a particular area weekly. You can stay up to date about the severity of the flu in your state, simply by clicking on the state you live in on this map:
Here is the Florida Flu Review
Here is the Colorado Flu Review
COPD and the Flu
If you have COPD, preventing acute exacerbations is crucial to reduce your disease severity and to prevent and slow down COPD progression. Avoiding exacerbations also means reducing the frequency of hospitalizations, and other high costs associated with the illness. Habits such as smoking, illnesses like bronchiectasis, factors including severe airflow limitation, and lastly infection are all identified as exacerbation triggers for people with COPD.
In order to avoid the misfortunes of dealing with a COPD exacerbation, and to limit both the short and long term effects, means getting your annual flu vaccine, and sooner rather than later.
Limiting your potential to catch influenza as a COPD patient is important, so you must wash your hands, avoid large crowds, disinfect often, exercise, sleep well, and most importantly get the flu vaccine. We know there are some hesitations when it comes to vaccination, so we gathered a few of the most frequently asked questions, so you feel confident getting you flu shot this year, and every year afterwards.
What is the flu vaccine? Why do I need one every year?

The flu vaccine can be taken as a shot that is injected into your arm or the flu nasal spray (which is not available every year). The vaccine is new every year, because the nature of viruses is how they quickly adapt and change in order to survive, therefore the vaccine must stay up to date with the newest most invasive virus strains.
The flu shot is a dead virus, when you get a shot your immune system creates the antibodies against the dead viruses, and your antibodies are able to protect you from being infected by the live virus.
When is the best time to get vaccinated?

There is no bad time to get vaccinated, but October-December is when the flu season starts to pick up, and getting the shot within this window will protect you through the flu season. Earlier is great too.
Even if it seems too late to get the flu shot, remember that if you’re being offered the flu shot, it’s because there’s the flu virus is still around. So definitely don’t hesitate if you have the opportunity to get the vaccine.
How is the flu vaccine made every year?
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
In order to keep track of the changing viruses, flu experts around the world within more than 100 influenza centers around the world research the different flu variations,. They go through intensive experiments to identify which strain will be the most common in a given season. Whichever strain they find to be the prevalent, will determine the flu vaccines “ingredients” that year.
This research process helps create a flu vaccine that’s specific to the common flu strains expected that winter, however it is not always a perfect science. This is why some years the vaccine will protect against the flu more effectively than other years.
Some years the vaccine does not provide your antibodies with the correct protections for your immune system to combat the virus, in which case the flu season will be worse overall.
.jpg)
Is it possible to get the flu from the flu vaccine?
This is probably one of the more frequent and concerning questions that people commonly mis-understand. This is cause for concern because mis-information can lead to less and less people getting the flu vaccine.
There are a lot of people who would argue that there is no point in getting the flu vaccine, and the strongest defense against the flu, are healthy habits like washing your hands, eating healthy, sleeping more, and exercise, which might be true for young adults in good shape with no health conditions.
However, people who suffer from a chronic illness, autoimmune disease, and people in poor health should try to practice these healthy habits, but also get the flu vaccines.
The bottomline is that, the flu shot is an inactivated or “killed” virus, which means you can’t get sick from the shot. The flu shot is a dead virus, when you get a shot your immune system creates the antibodies against the dead viruses, and your antibodies are able to protect you from being infected by the live virus.
The nasal spray flu vaccine does contain a weakened live virus — but it is not strong enough to cause the flu for most people.
However, like we mentioned before, sometimes the strain of the flu vaccine does not protect against that winter’s particular virus strain perfectly. That being said, for those who are vaccinated against flu and still get the flu, their symptoms are typically milder due to their vaccination.

Are there side effects from the flu vaccine?
While the flu vaccine cannot give you the flu, it can cause a few symptoms. The most common side effects are tenderness, redness, or a bit of swelling at the injection site.
You might not experience any of these symptoms but you can prepare to experience a few days of muscle soreness in whichever arm you get the vaccine, so you can opt to get the shot in your non-dominant arm.
It’s also possible to develop a low-grade fever, headache, or nausea, but these symptoms should go away within a couple days.
The nasal spray flu vaccine could also cause a runny nose, sore throat, and cough, however serious adverse effects are not common. In fact the risks you take to get a vaccine are far lower than the risks you’d run from getting the flu itself.
You should contact your doctor if you experience a high fever or signs of a severe allergic reaction like difficulty breathing, dizziness, or a rapid heartbeat. These types of reactions would most likely happen within a few minutes to hours after getting the vaccine, and can be treated with medical attention.
Are allergic reactions to the flu shot common?
Some people do have an egg allergy, and if you have a severe allergic reaction to eggs, you should avoid flu vaccination. If you’re mildly allergic, talk to your doctor because you still might qualify for the vaccine.
If you have a mercury allergy you shouldn’t get the shot either. Some flu vaccines contain trace amounts of mercury to prevent vaccine contamination.
If I got sick from the flu vaccine before, should I get one again?
Many types of viruses can cause cold and flu-like symptoms, but the flu shot only protects against the influenza virus, which is the common flu that we all try to avoid come winter because it is the most severe. It may be possible that you catch a different virus that the vaccine does not protect against, but you can rest assured that the virus you caught is much less severe than the influenza virus you might have caught without the flu vaccine.
Getting vaccinated is the best way to protect yourself and the ones you love from influenza. While you cannot get influenza from a flu shot, it is not rare to feel a little under the weather after receiving it. This only means that your immune system is responding to the vaccine, and it is actually a good thing.
How do you get vaccinated without using a needle?
There is a flu mist nasal vaccine. The difference between the shot and the nasal spray is that the flu nasal spray vaccine is a live "weakened" virus, while the shot is a “dead” virus. The nasal spray is a severely weakened virus that will cause a small brief infection in your nasal passages but most people don’t even notice it.
If you have a condition that affects your immune system may not be able to take the nasal spray because it is a live virus and it may cause you to get ill. The flu nasal spray has been approved for healthy people ages 2 through 49 years old.
There is also a CDC-approved list of people who shouldn’t get the live flu nasal spray vaccine.
How do I get vaccinated if I don’t have health insurance?

This is a serious question, and just because you don’t have insurance doesn’t mean you are not able to get a flu shot. You have a few options. You can pay out of pocket, in most places a flu shot will cost about $40, and slightly more for the senior dose.
Before you pay out of pocket, you can research websites like Blink Health or GoodRx and try to find discounts for vaccines available in your area. For example, if you live in Boca Raton, FL flu shots will be available at a pharmacy near you, to find one you can type you can your zip code into VaccineFinder.
Sometimes there are ways that you can get a free or discounted flu shot. Some schools and workplaces will hold events to offer a flu shot to members within their communities. For instance, in Boca Raton, Florida the Boca Helping Hands mission took place in partnerships with Walgreens and the Boca Raton Regional Hospital to off free flu shots to clients, volunteers and staff that are eligible to receive them.
Overview
The flu shot is an essential societal duty that everyone should partake in to help protect themselves and the people around them from the common flu. Even if you are a perfectly healthy adult, getting the flu might not seem like a very big deal, and you might miss a couple days off work. But for a super healthy person to spread the flu to others greatly increases the chances of a a chronically ill patient coming down with the flu, this is a far bigger deal.
People with COPD are often times hospitalized because they caught the flu and have severe COPD symptoms, or even an exacerbation as a result. If you have COPD be sure that the people in your life that you interact with have gotten the flu vaccine for your own sake, and if you haven't gotten vaccinated yet, be sure to schedule an appointment at you doctor or local pharmacy to get a flu shot as soon as possible.
For more expert advice about the flu shot, you can click here to read this HealthLine article, that touches on even more topics so you feel confident going in for a flu shot every year.

COPD, or chronic obstructive pulmonary disease, is a group of progressive lung diseases, the most common being emphysema and chronic bronchitis.
There are several benefits of mind-body exercise for people with chronic conditions, and even more specific exercise can be done if you have a chronic respiratory disease like COPD that are designed to stretch your muscles and open your airways.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In studies done looking at the benefits of yoga and tai chi for COPD patients showed how yoga postures, breathing exercises, and tai chi movements gave COPD patients overall improvement to their quality of life, and physical tests showed that their lung function improved!
Tai Chi

Tai chi may be the best exercise for you If yoga feels too hard and meditation feels too easy. Tai chi is a good balance between the two. Studies show that Tai Chi has a number of benefits for people with chronic obstructive pulmonary disease (COPD).
How can tai chi help with COPD?
Tai chi is a combination of slow flowing movements linked with breathing, and it is an ancient Chinese martial art. This is a great practice for COPD patients in any stage of the disease, because Tai chi exercises can be done standing or sitting.
This is also a great exercise option if you have limited resources, because no special equipment is needed. You just wear loose clothing, you need about a yoga mat's worth of space to preform the movements!
It may seem as if these movements are extremely easy, but the power you generate from the motion of the poses and the connection with your breath cultivates strength. It's great too, because these exercises are low-impact.

Not only does tai chi help strengthen your body, it can reduce stress, anxiety, and depression.
There has been a lifetime of experiments and research that explains how tai chi can help people with medical conditions like heart disease, osteoarthritis, and Parkinson’s disease. And now it is known that tai chi has significantly improved the quality of life for people with COPD.
It is also very likely that if you decide to join a pulmonary rehabilitation program that tai chi will be an effective part of your program.

Research about tai chi and COPD
Tai chi is commonly known to help many people with certain chronic conditions, and so there were additional studies done that would prove whether or not tai chi could improve the quality of life for people with COPD.

In an experiment, they tracked 120 people with COPD, half of the people were put on a traditional pulmonary rehabilitation program, and the other half were enrolled in a tai chi class.
In conclusion, the group of COPD patients who did tai chi had better scores in a survey about their respiratory health and they also performed better during a respiratory walking test.
Do you want to start doing tai chi?
If you think tai chi sounds interesting, the first step will be to get in contact with your doctor, talk to them about tai chi and whether or not this is a good exercise for you personally. Talking with your health care team is also a great way to learn about tai chi classes in your local area, and they may be able to recommend one.
They can also recommend online classes that would be a good fit for your respiratory level!

Tai chi has become very popular and during the pandemic, online workout courses became much more common, so if you like to exercise in the comfort of your home rather than go to a class, you could find classes to take online. Try searching for “beginner tai chi” or “tai chi basics” or “tai chi for people with respiratory health issues”.
There are usually tai chi classes at your local health club or gym, at community centers, or senior citizen organizations. You can also check your local hospital or healthcare center for a tai chi program.
Yoga

Yoga can be a great form of exercise if you have COPD because it is low-impact and can help to improve both your mental and physical health.
Yoga stands to benefit your health by:
- Lowering blood pressure
- Increasing relaxation and self-confidence
- Reducing stress and anxiety
- Improving fitness
Yoga will help you stay fit, flexible, and relaxed. There are different degrees of yoga classes, and there are specific yoga classes taught for people who are diagnosed with health conditions like COPD.
Yoga is a combination of physical postures and breathing techniques. Meditation and relaxation can be a big part of certain yoga practices as well.
The Physical Yoga Postures
Performing the physical postures of yoga can help improve your body’s ability to perform physical activity and will increase your:
- range of motion
- balance
- flexibility
- strength
Yoga postures can ultimately improve your energy levels and clear your mind from worry, and they also cultivate strength in your muscles and lungs.
Breathing Techniques
Breathing techniques can help utilize your breath more efficiently and teach you how to use your lungs more fully. Yoga is so great for COPD patients because these breathing exercises as you do the postures encourages your breath work outside of yoga and in your everyday life.
Benefits of Yoga for People with COPD
If you have COPD, taking a regular yoga class could be too much physically, and so modified versions of yoga have been developed so that you are capable of the practice without over-exercising.
Modified yoga classes are created with the health needs of people with COPD in mind and should provide you with a gentle, easy, and effective way to manage your health and emotional well-being.

The gentle stretches help to improve fitness and flexibility, while breathing exercises give you skills to manage any attacks of breathlessness. The techniques you learn should also be easy enough so you can practice at home.
Breathing techniques can help you manage symptoms of breathlessness by strengthening your respiratory muscles even when you are not doing yoga! The benefits of yoga spread into your daily life, and help you breathe better but will also help you manage stress and anxiety.
Yoga teaches you how to indulge in deep relaxation through breathing and meditation techniques. This helps to relieve stress and tension.

Before taking any yoga class, even if it is a class for people with your health condition, always consult your healthcare provider to get clearance before practicing any form of exercise. If your class is a normal yoga class that was not designed for people with COPD, check that your yoga teacher understands your needs as a person with COPD.
The right yoga teacher will show you how to breathe correctly in order to enhance your yoga practice and will give you modifications of poses that you are capable of doing.
You can try some of these yoga postures which can help you build strength and encourage healthy breathing:
Standing Mountain Pose
Stand tall to open up your chest. Your arms can be raised. or left at your sides.

Standing Backbend
This pose also helps to open up the muscles of your chest but needs to be practiced carefully to avoid muscle strain and breathlessness.

Seated Forward Folds
These poses help strengthen your respiratory system.

Standing Side Bends
These bends will help strengthen your diaphragm while also improving the flexibility of your rib cage.

Breathing exercises
Breathing correctly brings more oxygen into your blood and cultivates vital energy for your muscles and brain. Good breath helps your mind and body.
Pursed-lip breathing and diaphragm breathing are two of the most common breathing techniques for COPD and both have roots in yoga. They are often taught to people with COPD as part of their pulmonary rehabilitation program.
Exercising safely with COPD

Yoga and Tai Chi are generally safe ways to get in shape, but there are always things to be aware of, and if you have COPD be sure to take these precautions just to be sure.
Ask your doctor before performing any new exercise, they will have advice for practicing your exercise safely and considering your oxygen levels be able to recommend how much exercise you should be getting, so you get enough but also not too much. Your healthcare team may also have yoga classes or tai chi classes for COPD in your area.

Check the credentials of any yoga instructor or tai chi teacher before you begin classes and make sure they know about your condition and health needs before beginning the class.
The best thing about yoga and tai chi, is that you are practicing your own exercise, and there are no expectations to do anything that is uncomfortable or harmful to your body. Therefore, you should avoid any poses that restrict your breathing and put pressure on your diaphragm. Examples of yoga poses you should avoid are Child’s Pose or the Plough.
Yoga and tai chi are exercises meaning your heart rate could increase and your breathing can also speed up. Be prepared for this, and keep your inhalers or portable oxygen device close by when practicing tai chi, yoga, or any form of exercise.

Stop exercising immediately if you experience shortness of breath while exercising, taking breaks and allowing yourself to catch your breath is a helpful tool to use when you are experiencing an exacerbation or flare up. Use your medication and rest until you feel well enough to begin again.
Exercise for COPD Patients
It is way too common for COPD patients to not get enough exercise, and this is because they think that feeling breathless and tired is bad for their lungs, but this is not true. For COPD patients, it is crucial to get some exercise daily. Without exercise you will become less physically fit, and your breathing will get worse.
Overview

Exercises that are incredibly important for COPD patients include aerobic exercises, strength and conditioning, and breathing exercise. Yoga and tai chi are two forms of exercise that help with all of those aspects of exercise and they also help improve flexibility and mental health!
Tai Chi and yoga are two forms of exercise that can help COPD patients improve their blood pressure, help with relaxation and self-confidence, reduce stress and anxiety, and will help improve their overall fitness.
Keep an open mind and if your doctor agrees that yoga or tai chi would be a good option to improve your health, give it a try!
.png)
Activities of daily living (ADL) is a term that was first coined by Sidney Katz in 1950. Essentially, it refers to the basic functions that an individual must perform on a daily basis in order to be considered self-sufficient. By better understanding the level of independence of patients with debilitating illnesses like COPD, osteoporosis, or Alzheimer’s Disease, medical professionals are able to make better decisions for their patient’s well-being such as recommending medical equipment or an assisted living facility. Activities of daily living are generally divided into five distinct categories:
Personal Hygiene - bathing, grooming, hair care, and oral health
Continence - using the bathroom
Dressing - the ability to select clothing and dress for different occasions
Feeding - the ability to eat and drink
Ambulating - the ability to walk and move around independently
When it comes to managing your daily life with chronic obstructive pulmonary disease (COPD), it’s very important to consider how your condition affects your ability to live independently. Studies have shown that ADLs can be very challenging for respiratory patients because they can lead to dyspnea (shortness of breath) and oxygen desaturation, meaning the percentage of oxygen in the blood is lower than what it should be.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In this post, we’ll take a look at the importance of supplemental oxygen for carrying out activities of daily living. We’ll also show you why portable oxygen concentrators are the best device to use for maintaining your freedom and independence. If you have any questions about these units, please feel free to leave a comment or reach out to our respiratory specialists.
What is a Portable Oxygen Concentrator?
A portable oxygen concentrator is an electronic device used to administer medical-grade oxygen. POCs are the most state-of-the-art oxygen units on the market because they’re extremely lightweight and versatile. Using a POC, you’ll be able to go more places and do more things than if you had a standard compressed oxygen tank or liquid oxygen tank. Since they’re electronic devices, you simply need to have access to a source of power in order to recharge your batteries. You’ll never have the need to reach out to an oxygen company ever again to refill or deliver new tanks to your home!

One of the greatest benefits of owning a portable oxygen concentrator is that they’re approved by the Federal Aviation Administration (FAA) for in-flight use. What this means is that you can take your POC with you on any commercial flight within the United States. This is a freedom that COPD patients never had in the past because compressed oxygen tanks and liquid oxygen tanks are not allowed on flights for safety reasons. Upgrading your old outdated oxygen device to a portable oxygen concentrator quite literally opens up a world of possibilities! Without further ado, let’s take a look at why activities of daily living are so much easier when you have a portable oxygen concentrator.
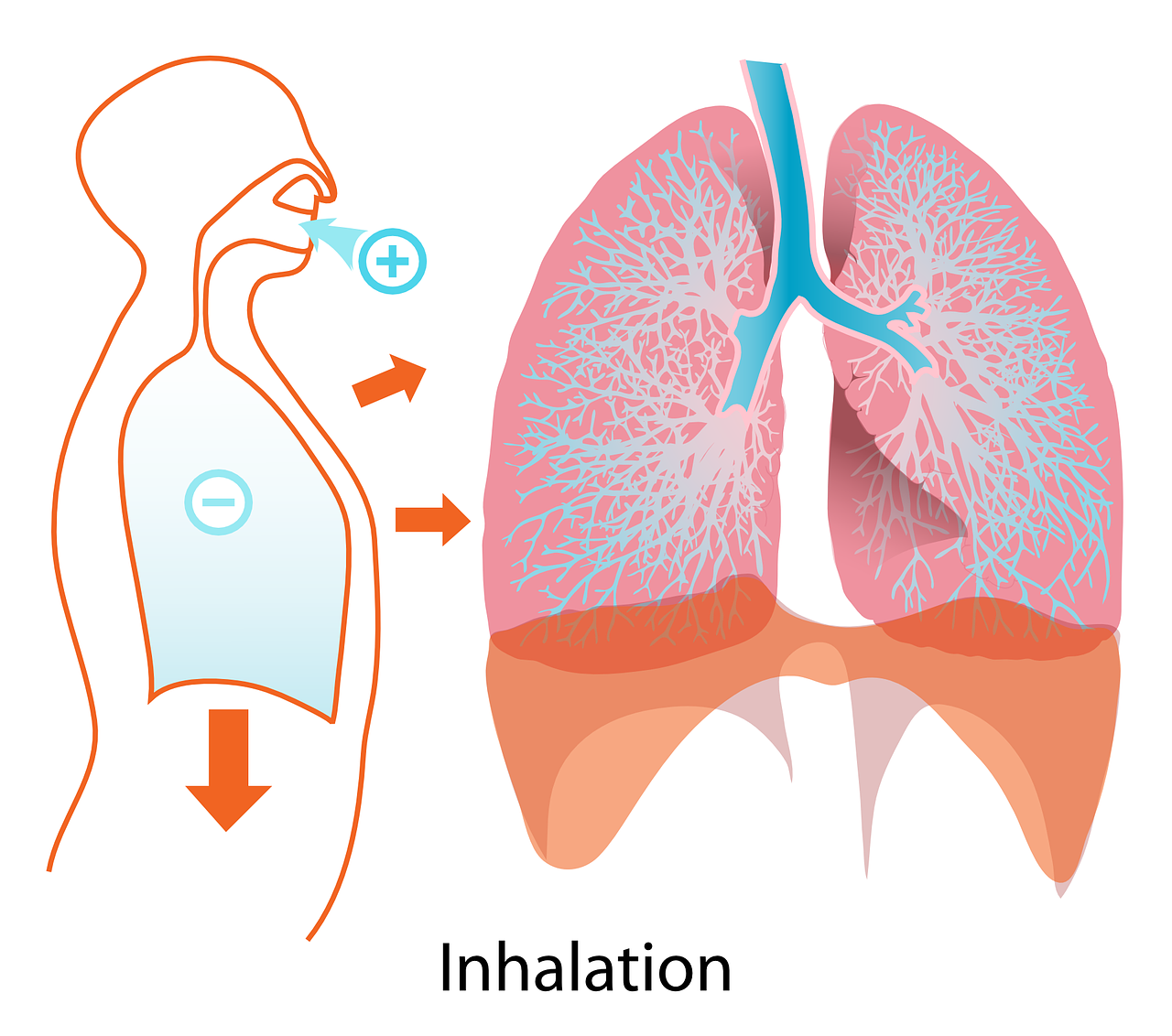
Reduced Shortness of Breath
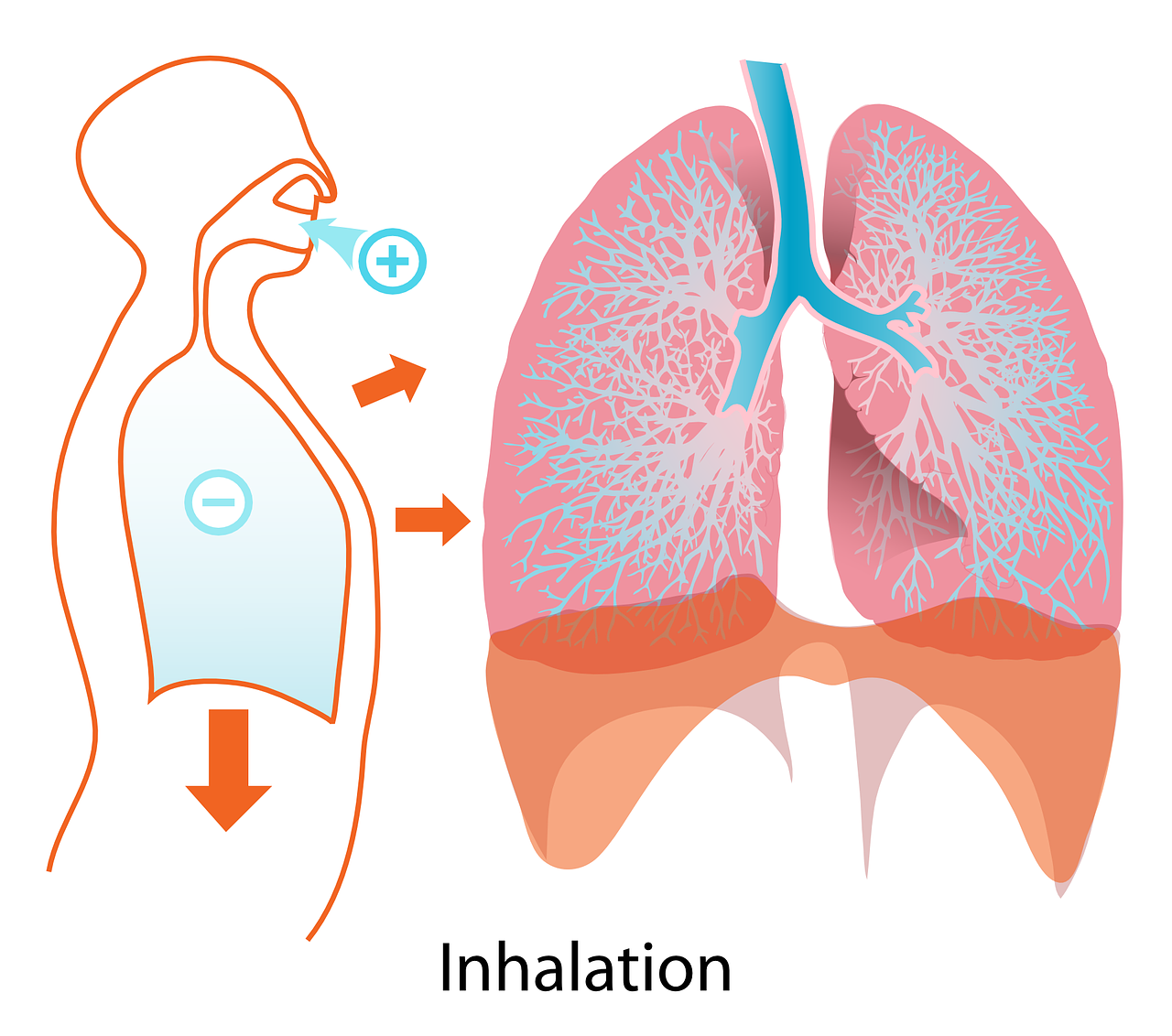
The human body has a complex system for managing breathing rate and breathing depth. Breathing is part of something called the autonomic nervous system which regulates involuntary physiologic processes like heart rate and blood pressure. However, you also have the ability to take control of your lungs through voluntary breathing. Exercises like deep breathing or controlled breathing are great for teaching you how to use your lungs more effectively.
![]()
One of the primary factors that affect respiratory rate is how much carbon dioxide is in the blood. When you are unable to expel air from the lungs fully — a problem that’s common among COPD patients — CO2 begins to build up in the bloodstream. This change in CO2 levels is detected by chemoreceptors which send a message to the medulla oblongata (the control center for the lungs) to increase respiratory rate. Other factors that affect respiratory rate and depth include atmospheric pressure, intra-alveolar pressure, and body temperature.
If you have COPD, interstitial lung disease, or any number of other respiratory conditions, the best way to reduce feelings of breathlessness is by increasing the concentration of oxygen in the lungs. By doing so, you will stabilize CO2 levels in your blood and the chemoreceptors will never send a message to your brain that you need to breathe quicker or more heavily. What this means when it comes to activities of daily living is that you won’t need to stop to catch your breath so frequently.

Using a portable oxygen concentrator throughout the day will prevent you from becoming breathless and thus reducing your chance of experience a COPD exacerbation. Many people find it difficult to keep up with their friends or loved ones because they need to stop to rest frequently. But with a portable oxygen concentrator, you can easily adjust the amount of oxygen you’re receiving based on how you’re feeling. It’s important to speak with your doctor, however, who will tell you what oxygen levels are acceptable.
Improved Mental Alertness
Your ability to complete daily tasks like eating, bathing, and cooking is equally reliant on your mental ability as it is your physical ability. When the oxygen levels in your blood are low this may result in brain hypoxia, also known as cerebral hypoxia, or low oxygen levels in the brain. Symptoms of brain hypoxia include temporary memory loss, impaired motor functions, confusion, lightheadedness, and more.
![]()
Maintaining a “sharp” mind with age is notoriously difficult and living with a respiratory condition like COPD can make it even more challenging. However, by carrying a portable oxygen concentrator with you wherever you go and keeping your oxygen saturation at a healthy level, you’ll be able to rule out one potential cause of cognitive decline as you go about your daily life. Studies have found that there is a correlation between disease severity and cognitive decline, so the more you can do to slow the progress of COPD, the better off you will be in terms of your mental health as well.

A portable oxygen concentrator will provide you with a convenient and reliable source of oxygen as you go about your day. POCs like the Inogen One G5 and Caire FreeStyle Comfort simply need to be turned on and then you can adjust the flow setting however you need it. Then all you need to do is set it and forget it. Your POC will provide you with a steady supply of oxygen all day allowing you to go about your day with your oxygen needs out of mind. This will afford you the freedom to focus your attention on what you’re trying to accomplish rather than worrying about whether your needs are met.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Another reason mental alertness is so important is for your safety. People experiencing cognitive decline, more specifically dementia, are at a higher risk of experiencing a fall. Like we discussed in a previous blog post, experiencing a fall, whether it’s inside or outside your home can be dangerous. Studies have also found that dementia patients are at a greater risk for car accidents. Whether you’re driving to the store or just doing chores around the house, maintaining your oxygen levels will keep your mind sharp so that you can navigate safely.
Improved Exercise Tolerance
As you’re likely already aware, a healthy exercise routine is paramount to any COPD treatment plan. While exercise is important for everyone, it’s especially important for people with chronic lung conditions who need their lungs to perform as optimally as possible. Studies show that exercise increases the strength and function of muscles meaning that they require less oxygen. In other words, any form of exercise will benefit you in the long run. But if you want the best exercise routine, speak with your doctor about pulmonary rehabilitation. This is a type of exercise routine that focuses on your lungs and respiratory system as a whole.
When you’re exercising, the rate and depth of your breathing increase because your muscles need more oxygen. What’s more, your heart rate and blood flow increase in order to get that oxygen to the parts of the body that are being worked the most. Not only do your muscles need this oxygen in order to provide them with energy, but oxygenated muscles tend to recover and rebuild faster than muscles that do not get oxygen. So your body will feel more prepared to go through a strenuous exercise the next day.
.png)
Without a doubt, portable oxygen concentrators are the best oxygen device for exercising. Most pulse dose concentrators weigh around 5 pounds and are no bigger than a handbag or purse, so taking one with you when you do your exercise routine is hassle-free. Concentrators like the Caire FreeStyle Comfort also have a lot of carrying options available for them so you can find one that works best for the type of workout you’re doing. The custom carrying case, for example, is great for walking or hiking, but if you’re doing something more involved like weight lifting, you might want to go for the FreeStyle Comfort backpack.
Improved Mobility
Mobility is oftentimes one of the most discussed issues when it comes to aging, and for good reason. The older we get, the more likely we are to suffer from debilitating conditions like osteoporosis, arthritis, impaired strength or balance, or dementia. COPD only makes these conditions worse by adding breathlessness, chest pain, and chronic fatigue to the mix. Sometimes, there isn’t one particular way of dealing with these issues, but instead, COPD patients should work with their doctor and loved ones to find the best solution for them.
![]()
While portable oxygen concentrators certainly don’t “solve” mobility issues, they can definitely help. Old outdated oxygen devices like oxygen tanks are extremely heavy and awkwardly shaped making it nearly impossible to navigate your home with ease. But when you upgrade to a POC, you’ll have a machine that you can carry around the house all day while completing chores and never feeling the need to set it down for a rest. If you use a mobility aid like a walker, wheelchair, or electric wheelchair, you can easily set your POC on your mobility for even more convenience and comfort.

Another benefit of having a portable oxygen concentrator is that it’s easier to prevent your oxygen tubing from getting tangled or tripping over it as you walk. Whether you carry your POC on your shoulder or your back, you won’t need to use long oxygen tubing. But since oxygen tanks are so heavy, you’ll need to use a rolling cart, meaning you’ll need to use much longer oxygen tubing. Many people find that their oxygen tubing gets tangled and wrapped around things while using an oxygen tank which is not only frustrating but dangerous as well.
Conclusion
Activities of daily living are essential tasks that we need to perform each day in order to be independent. If COPD prevents you from doing one or more of these tasks, then you may need to consider hiring a part-time or full-time caretaker. Alternatively, you could invest in a medical oxygen device like a portable oxygen concentrator which allows you to extend your freedom and independence. Many COPD patients feel like they’re taken back in time when they get their first POC because they are able to do things they never thought would be possible after being diagnosed with COPD.
One important thing to note is that oxygen is a controlled substance in the United States. In other words, you will need to have a prescription for medical oxygen from your doctor in order to purchase a portable oxygen concentrator. Whether you have a prescription or not, your best course of action is to give our respiratory specialists a call here at LPT Medical. If you don’t have the required paperwork to purchase a POC, we can reach out to your doctor for you. We’ll also walk you through the process of choosing a portable oxygen concentrator from start to finish. We’re also happy to announce that we now offer assistance with Medicare and medical financing so you can save as much money as possible on a new, used, or refurbished unit.
Give us a call or email us today for more information!


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













