
If you don't already know how beneficial oxygen therapy is for people with COPD and other respiratory chronic conditions this blog post will explain all of the reasons this therapy can make such a big difference their lives.
We understand that it may seem like oxygen therapy is an invasive aspect of your daily routine, however supplemental oxygen offers the user freedom, energy, and livelihood, it also adds years to your life!
That being said, it is important to discuss the side effects of oxygen therapy and how we can work with you to make it more comfortable.
If you are looking at your oxygen device every morning and dreading using it, you are not taking advantage of what this therapy has to offer you.
If done correctly, you could start to see your oxygen device as a ticket to anywhere in the world, as independence from caretakers and hospitals, your breathing device should give you life and excitement for the future.
In order to address all of the positive aspects of oxygen therapy it is essential that we discuss the drawbacks and how you can overcome the negative aspects. Simply put, there are obstacles that you may need to overcome while getting used to your breathing device.
There are some aspects of your day that will become the “new normal”. Lastly, there are certain discomforts and side effects associated with oxygen therapy. That is why we are going to discuss ways to normalize your oxygen therapy and help you adjust to daily life.
How to overcome oxygen therapy obstacles
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
One of the first and biggest obstacles you may face after being prescribed home oxygen, is education, this means learning about your illness and how oxygen will affect you.
It is critical you are willing to handle new and sometimes confusing pieces of machinery along with the medical jargon and language about your condition.
We have a great blog titled “COPD Education is Key: 15 Questions you Need to ask your Doctor” that can help you understand some of the questions about your breathing capabilities and what this means when you are looking to buy an oxygen device.
This is a great place to start if you want to understand more about COPD testing, symptoms, and treatments.
After you are capable of communicating with your doctor effectively, you can begin to understand their reasoning as to why you qualify for oxygen therapy, and how you can get the most out of this COPD treatment method.
The next obstacle you must overcome is choosing the oxygen therapy device that is best for you and your lifestyle. This is complicated because everyone is different and everyone’s COPD affects them differently.
Therefore, it is important you talk to a respiratory specialist who can ask you questions about your lifestyle and your oxygen prescription in order to match the perfect oxygen device to your specific needs and wants.
A specialist works with a number of people everyday, they know oxygen devices inside and out, so once they have an understanding about you and your oxygen prescriptions they will be able to match you with a device that will help you get back to your daily routine!
Our respiratory specialists will connect you with a portable oxygen concentrator because a portable oxygen concentrator (POC) is going to be the most cost-effective way to administer oxygen to manage your COPD. If you purchase your POC there are no recurring costs, you will never have to worry about refilling your oxygen tanks, and they are simple and user friendly!
Simply by utilizing a portable oxygen concentrator rather than an oxygen tank or oxygen canisters, you are saving money while minimizing a lot of the obstacles that come with oxygen tanks.
Portable oxygen concentrators are also much safer to use because there is no reserved compressed liquid or oxygen gas that would otherwise create a fire hazard. Instead, the concentrators extract the surrounding air, purify, and condense it into the medical grade oxygen that you breathe in.
That being said, there are still certain adjustments and challenges that come with you oxygen concentrators.
One of the best ways to overcome any obstacle is to learn more and educate yourself about the subject. Knowledge is power, and that is why we’re now offering a FREE Thrive eLearning Course with the purchase of your Inogen One G5 portable oxygen concentrator.
We know how important pulmonary wellness is, but this means more than just having a great portable oxygen concentrator; it requires you to make other lifestyle changes involving your diet, exercise routine, and more.
In an effort to help you with all aspects of your pulmonary wellness regimen, we wanted to give this immersive learning experience to our customers so they can educate themselves beyond the oxygen therapy and adjust other complicated aspects of life while dealing with COPD or other respiratory diseases.
Thrive is an accessible, all-in-one online training course that aims to provide you with simple, practical, and actionable tips for managing chronic obstructive pulmonary disease (COPD).
With this program, you’ll also have access to one-on-one counseling with certified pulmonary experts, support group opportunities, online learning courses, and much more! Below is a full list of what you’ll receive:
- Direct access to a private support group (patients, caretakers, and experts)
- Years of COPD and respiratory illness knowledge
- Step-by-step disease management regimen
- Best selling e-books and guides
- Step-by-step breathing exercises
- Learn about exacerbations and how to prevent them
- Speak with a nutritionist about refining and improving your diet
COPD symptoms can only be managed with impeccable lifestyle choices. This ePulmonary Advanced Online Workshop will help you get back on track and locate any anomalies in your COPD treatment plan.
The Inogen One G5 will provide you with the oxygen and freedom that you need to live life on your own terms, but this training program will make you unstoppable!
This Thrive ePulmonary Online Training Program is a $497 value, but we’re offering it for FREE! Order your Inogen One G5 today and experience the freedom you want and deserve! Fill out the blue box to the right of your screen, or call a respiratory specialist at 1-800-943-1201 and find out how you can purchase a Inogen One G5 portable oxygen concentrator.
Your goals for oxygen therapy
Your goal when it comes to oxygen therapy should be to continue as many of your usual activities as you can!
You should work with your doctor and oxygen supply company to get oxygen equipment that will allow you to do every activity you still enjoy. Choosing the right type of equipment for you and your lifestyle is crucial — the right portable oxygen equipment can play a major role in improving your quality of life, starting by relieving a lot of your symptoms.
Oxygen therapy works to relieve breathlessness, so that you can exercise and get outdoors more often. Not only does oxygen therapy give you the accessibility to do more it also gives you more time! By this, I mean that oxygen therapy studies from multiple sources suggest that long-term oxygen therapy extends the life expectancy of COPD patients with low blood oxygen levels.
Even though there are a lot of great aspects associated with oxygen therapy, there are side effects that you should be aware of, so that you know how to handle it.
Get comfortable, oxygen therapy is your new normal
Side effects of oxygen therapy may include:
- The skin around the face mask or nasal cannula can get irritated.
- The inside of your nose might become dry.
- You may get nosebleeds once in a while.
- In the morning, you may wake up tired or with a headache.
In some cases, you can avoid these side effects by adjusting the amount of oxygen you get, meaning that you should continue to speak with your doctor about your oxygen prescription.
The equipment you use may need to be changed if you’re having constant problems and irritation, but most of the time there is just a small adjustment period where your body has to get used to the new normal.
If you’ve ever used a bulky and cumbersome continuous flow concentrator or an oxygen tank, you know that they’re anything but user-friendly.
While both methods do offer you the oxygen you need, it doesn’t feel like they were built with your comfort in mind.
If you are looking for a portable oxygen concentrator that was designed to be comfortable, The Caire Freestyle Comfort got its name for a reason; it was specifically designed to be comfortable to wear and use.
This oxygen unit has a curved design that fits the natural shape of your body. While you’re walking, it will stay at your side instead of sliding around and interfering with your natural movements.
All of the buttons for your oxygen control as well as the power switch are conveniently located on the top of the unit and the batteries can be easily pulled off the bottom of the unit for replacement.
The Caire Freestyle Comfort is one of the lightest portable oxygen concentrators on the market, weighing in at just 5 pounds with the 8-cell battery and 6 pounds with the 16-cell battery.
This means you’ll be able to carry your oxygen unit without ever experiencing back pain or unnecessary strain that can ruin your day.
There is some adjusting you have to get used to when you first get started on your oxygen therapy regime, but soon enough your life with your trusted POC will be the new normal. A big part of enjoying life while using oxygen therapy is having the right equipment.
This means having a POC that meets your oxygen requirements but also allows you the freedom and opportunity to travel, exercise, and socialize.
The other aspect, is education and this means learning about you disease and how it should be managed on a daily basis along with your oxygen therapy.
The bottom line when it comes to oxygen therapy is that it is a blessing in disguise. When you are diagnosed with COPD you might think that you should try to go as long as possible before you have to start using oxygen.
But the truth is, once your doctor prescribes you oxygen therapy, if done correctly, you should start to see improvements in your mood, energy, and overall quality of life.
As we mentioned in this article, there are still side effects, but having an oxygen device that is designed to be comfortable and easy to use will help with those adjustment periods where you are learning how to manage and avoid certain irritations.
Also always be patient and kind to yourself, allow yourself time to learn about oxygen therapy before you let yourself hate it. If you need help adjusting or think that your oxygen device is not right for you, give us a call at 1-800-946-1201 or reach out over social media and we will gladly mentor the oxygen user on best practices.
Anxiety can show itself in a number of ways for a multitude of different reasons. If you have COPD or another obstructive respiratory disease that makes breathing difficult, you may also experience anxiety related symptoms due to breathlessness.
Mental health problems are very common in COPD patients: about 60% of patients with COPD have symptoms of anxiety and 40% have symptoms of depression.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Anxiety and depression can heighten COPD related symptoms like breathlessness, physical functioning, quality of life, exacerbation rates, length of hospital stays, and mortality.
Both anxiety and depression amplify hyperventilation and cause panic attacks which will heighten the sensation of breathlessness. Also, if you have COPD and psychological difficulties you are less able to manage symptoms and treat your lung condition for a number of reason, two being that you are less likely to be physically active or attend pulmonary rehabilitation.
However, if you can recognize your mental and physical limitations, the psychological impact of your COPD is very treatable along with your physical COPD symptoms.
Treating COPD

Treating COPD is important not only for your physical health, but it is a step towards better mental health as well. For example, if you need oxygen therapy, following the guidelines of your oxygen perception is a necessary step that will make your life more easily manageable. If you're in the market for a portable oxygen concentrator be sure you are working with an oxygen licensed distributor like LPT Medical so you can have peace of mind that you are getting an oxygen device that will take care of condition in the most effective way possible.
Other treatments include, taking your medication and understanding when and where you need to take certain inhalers through the day. This will help reduce stress and anxiety around your condition.
You should also be exercising, dieting, quit smoking and following other COPD treatments that have been proven to improve the quality of life for patients with COPD.
Treating Anxiety
Not being able to breathe can cause a lot of problems in your physical body but it also impacts your brain! Anxiety causes breathing to get worse, which causes more stress and anxiety, and then your breathing gets worse again, creating a toxic cycle of shortness of breath.
Anxiety disorders, specifically generalized anxiety disorder (GAD) happen at a higher rate in patients with COPD compared with the general population and over 16 million Americans are diagnosed with COPD.
![]()
Not surprisingly, anxiety can have a significantly negative impact on the quality of your life with COPD.
In this blog we are discussing the potential to get help for your anxiety which can help you live a higher quality of life with COPD. If there is one thing you take away from this article, let it be that as a person with a chronic respiratory disease the very best thing you can do for yourself is to become educated about your disease.
First thing is first, it is important that you understand where your anxiety is coming from.
Deciphering Between COPD Induced Anxiety and General Anxiety

It is very possible that you have COPD and anxiety from not being able to breathe properly, but it is also possible that your anxiety disorder is unrelated to your breathing problems, and is rooted in something else.
This would mean that the ideas laid out in this particular article may not be as beneficial as other resources that can explain other sources of anxiety that you are experiencing, but again could be worth the read because education is key.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Your pulmonary health care team can help you find the root of your anxiety by performing certain tests, and with the help of psychologists that are trained in treating mental health disorders.

Generalized Anxiety disorder most often looks like this:
- Persistent worrying or anxiety about a number of areas that are out of proportion to the impact of the events
- Overthinking plans and solutions to all possible worst-case outcome
- Perceiving situations and events as threatening, even when they aren't
- Difficulty handling uncertainty
- Indecisiveness and fear of making the wrong decision
- Inability to set aside or let go of a worry
- Inability to relax, feeling restless, and feeling keyed up or on edge
- Difficulty concentrating, or the feeling that your mind "goes blank\
- Fatigue
- Trouble sleeping
- Muscle tension or muscle aches
- Trembling, feeling twitchy
- Nervousness or being easily startled
- Sweating
- Nausea, diarrhea or irritable bowel syndrome
- Irritability
The tricky part is that COPD related anxiety can and often does look very similar. It is when treating anxiety where you have to be careful about where your anxiety comes from.
Treating COPD induced Anxiety

There are now better methods for treating anxiety related to breathing complications.
Here are the 3 different anxiety treatment options within the context of COPD patients:
- Pharmacological
- Psychotherapeutic
- Pulmonary rehabilitation treatments
Pharmacological

There have been pharmaceuticals called nortriptyline, buspirone, and sertraline all of which have been found to reduce symptoms of anxiety caused by COPD.
In a study, patients with COPD and depression were examined during a 12-week, randomized controlled trial of nortriptyline. Nortriptyline notably helped treat depression and showed valuable improvements in anxiety, certain respiratory symptoms, overall physical comfort, and day-to-day function.
Buspirone (BuSpar) is a nonaddictive anti-anxiety medication that doesn’t interfere with your breathing.
While sertraline has not been proven to improve in forced expiratory volume (FEV1) or depressive symptoms, COPD patients who were given a certain dose of sertraline did show some improvement in their daily activities. The effectiveness of sertraline with COPD or a related obstructive airways disease showed significant improvement in breathing abilities. A few patients in this study also showed some improvement in exercise capacity, depression and anxiety.

Psychotherapeutic
There are now specifically designed cognitive behavior therapy programs that take into account the unique difficulties of COPD patients like yourself. These specifically designed programs are catered to people with breathing difficulties and for many people, it is the best treatment available for COPD related depression and anxiety.

Cognitive–behavioral programs focus on relaxation and mindfulness practices to help reduce anxious symptoms.
Cognitive behavior therapy (CBT), which helps patients develop strategies for coping with anxiety and similar conditions, have been proven to help lower that anxiety and reduce the chances COPD patients will end up in the hospital.

It works best when behavioral therapy is done by nurses with expertise in lung conditions!
It is commonly known now that the importance of psychological treatment in chronic obstructive pulmonary disease (COPD), has great potential benefits, yet clinicians do not always address this important issue.
This therapy is designed to understand patients’ current difficulties by linking a patient's environment, their physical symptoms, thoughts, emotions and behavior.
![]()
Techniques will be used to tackle their current difficulties and teach the patient skills to identify unhelpful thinking or behavior which might be causing vicious cycles of anxiety and/or depression. Having a personal approach can help cultivate an understanding of the patient's problems so they are capable of identifying ways to overcome their problems and identify triggers so they can actively improve their quality of life.
Here are some of the steps a CBT program will go through with COPD patients:
- Identify what triggers a patient's breathlessness: physical activities and/or psychological factors (fear or panic).
- Create a self-management plan to address physical and psychological difficulties.
- Improve medical care, for example, identifying and addressing unhelpful thinking.
- Planning and pacing activities, breathing techniques, distraction and relaxation can all help breathlessness alongside oxygen therapy.
Patients with all levels of COPD severity who also experience symptoms of anxiety and/or depression can benefit from CBT, but it is up to your doctor and team of health professionals to get you the care you need.

You should seek out appropriately trained respiratory healthcare professionals to undertake your CBT if you and your doctor determine that you would benefit from a a cognitive behavior program.
One day, hopefully soon, the healthcare system will be able to provide safe and effective psychological care from an experienced person with the right skills to provide the treatment, but it is still a long process to implement this into a tradition COPD treatment plan. As a patient, being educated about this topic will help you advocate for your needs, and get to the therapeutic help you need.
Pulmonary rehabilitation treatments
.jpg)
Multicomponent pulmonary rehabilitation programs can also hep to improve anxious symptoms.
Pulmonary rehab is a program that was designed to improve quality of life by:
- Decreasing respiratory symptoms and complications
- Encouraging self-management and control over daily functioning
- Improving physical conditioning and exercise performance
- Improving emotional well-being
- Reducing hospitalizations
The focus is partly to reduce physical symptoms of breathlessness by giving the your new exercises, breathing techniques, and dieting and habit forming skills, but these programs are also heavily focused on education and emotional health.
Pulmonary rehab gives you the tools to accomplish goals and strategies for managing your condition in a healthy way both physically and mentally. It is also a social group setting that gives you the chance to talk to other people in similar situations, which is good for your mental health.
Finding Alternatives for Anxiety Medication
People who don’t have COPD but do have anxiety are sometimes prescribed anti-anxiety medications but many of these drugs can negatively impact breathing if you do have COPD.
Anxiety medication can also potentially interact with other medications you use to treat your COPD. Not to mention, these medications can cause dependence and addiction problems as well.
Traditionally the typical treatment for COPD has been inhaled medication with goals to reduce airway obstruction. More recently, it has been recognized that good quality, holistic care of COPD should address all aspects of the condition including mental health and not merely focus on treatments aimed at improving airway obstruction.
If you have COPD and you also struggles with anxiety, some of the ideas laid out in this blog may help you manage these conditions! It could be beneficial for you to think about taking certain pharmaceuticals in order to reduce anxiety caused by COPD. You could also be benefiting from cognitive behavioral therapy and pulmonary rehabilitation courses that are designed with your conditions in mind.
First and foremost, education is a game changer in treating and living with a chronic condition like COPD. Learning about your condition and how it can affect more than just your ability to breathe will give you insight into treating your disease more holistically and in-turn cultivates a healthier lifestyle moving forward.
If you found this blog helpful, please share it with your friends and family and comment to let us know your thoughts!

Caregivers are either naturally selfless people or they becomes selfless as their role of a caregiver develops. Caregivers take on a difficult job that often requires sacrifice in order to care for their loved one. This article is for you, the caregivers out there who need some advice about how they can continue to care for their loved one, but also take care of themselves.
It is so important for you to take care of yourself because only when you first help yourself can you effectively help others. Caring for yourself is one of the most important—and one of the most often forgotten—things you can do as a caregiver. When your needs are taken care of, the person you care for will benefit, too.
We hope that the caregiver and the patient can read this article together and find helpful ways to work through their difficulties managing and treating COPD together.
What is COPD
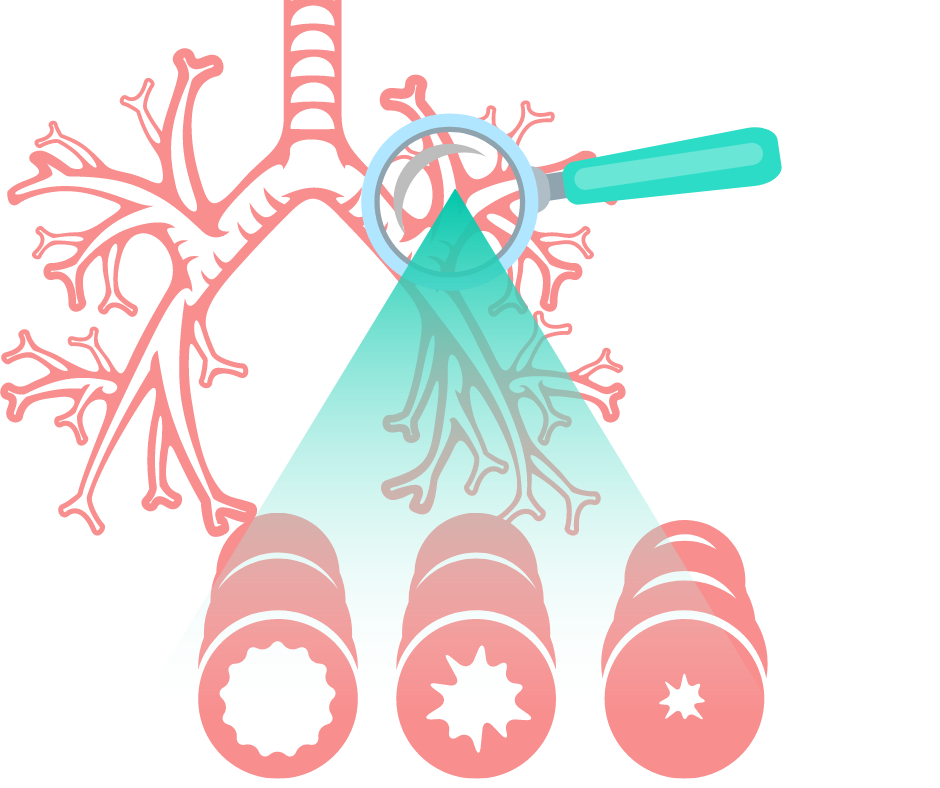
The first thing you must do is to understand what Chronic Obstructive Pulmonary Disease is, and there are three main forms of COPD:
- Chronic bronchitis, which involves a long-term cough with mucus
- Emphysema, which involves damage to the lungs over time
- Some patients have both conditions listed above
All of which make it hard for the COPD patient to breath because their airways become inflamed, damaged, and restricted by excess mucus. This causes a number of other issues throughout their body across all of their systems. With lack of oxygen comes low blood saturation levels, bone decay, added stress on the circulatory system, and a list of other complications.
COPD is treatable, and people can live with this disease for many years despite how severe it gets. There are ways to learn how to manage the disease and even slow down the progression of COPD. It requires a strict treatment plan that the COPD patient and their caregivers can develop with their doctor. Actually executing this treatment is the hard part, and where the caregivers role is essential.
So let's talk about our caregivers.
Being a caregiver
-jpg.jpeg)
There are over 40 million families worldwide in the caregiver role for a spouse, parent, friend, or other loved one, no matter the circumstance this is no easy task but it is an important one. It should not be taken lightly! Both the patients and the caregivers are in a hard position where intense lifestyle changes and everyday norms are flipped upside down.
If the patient has a condition like COPD, the caregiver's role likely evolved over time once their symptoms started progressing and through the diagnosing process, rather than a sudden change like an accident where a patient was healthy one day and hurt the next.
Because COPD is a progressive disease meaning it gets worse over time, both the caregiver and the patient will go through different stages of the disease together changing and altering everyday activities to adjust to a more comfortable lifestyle.
As a COPD caregiver, your main focus will inevitably be your loved one. However, your own health and well-being is important for you and the one you are caring for. This means remembering to take care of your own needs. As we mentioned above, this is not an easy job, and it is easy to feel overwhelmed.

Here are some tips for taking care of yourself as a caregiver:
Some of the most common impacts caregiver experiences are listed below:
- Sleep deprivation
- Poor eating habits
- Failure to exercise
- Failure to stay in bed when ill
- Postponement of or failure to make medical appointments for themselves
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
If you experience any of these lifestyle changes as a caregiver it is important to find tips for managing and adjusting your habits in order to live a more productive and happier life.
Here are some tips you can focus on. These tips were developed to help you get into a sleep scheduled, eat healthier foods, exercise more regularly, taking care of yourself when sick, and to remind you that you should make medical appointments for yourself when necessary.
Tip #1 Reducing stress

Caregivers are under a lot of stress all day long everyday, one of the best easy to avoid feeling stressed is to adjust to a strict sleeping schedule. Studies show the effects of sleep deprivation are related to a person's exposure to severe environmental and operational stress and negatively impacts their cognitive performance. This particular study sourced from Springer Link explains the results of a study that sleep deprivation and environmental stress adversely affects a person’s performance and mood.
You can also work to recognize stress warning signs early. This means realizing your irritability, sleep problems, and forgetfulness early on so it doesn't get worse. You can learn how to recognize your own warning signs, and be capable of making effective changes. Donʼt wait until you are overwhelmed.
You can also begin to identify the sources of your stress. Ask yourself, “What is causing stress for me?”
Sources of stress might include:
- you have too much to do
- family disagreements
- feelings of inadequacy
- the inability to say no
After you can put a source to your stressful feelings identify what you can and cannot change.
Remember, we can only change ourselves and our own behavior, and someone else’s actions are out of our control. When your focus is wrongly adjusted on things you cannot change or control, you will only increase your sense of frustration.
Ask yourself, “What do I have some control over? What can I change?” and even if you can only make a small change, this can make a big difference.
The last thing is to take action. These types of active decisions to reduce stress gives you back a sense of control that you deeply need. Stress reducers can be simple activities:
- Walking
- Other forms of exercise
- Gardening
- Meditation
- Having coffee with a friend
- Identify some other stress reducers that work for you
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Tip #2: Set goals for yourself
You can set a variety of goals all having different timelines, and it's a great way to stay in check with what matters to you.
Some goals you might try to set are:
- Taking a break from caregiving
- Get help with caregiving tasks like bathing and preparing meals
- Engage in activities that will make you feel more healthy
You do not want to get overwhelmed with accomplishing too many goals at once. Instead focus on one of two so that you can work towards those ideas productively.
The next step is to make an action plan, you can do this by asking yourself, “What steps do I need to accomplish to reach my goal?’” Then you can determine which step you will take first, and when.
Here is an example of how to set and make a plan for accomplishing goals:

Tip #3 Finding a solution
Your priority as a caregiver has been to seek solutions for your patients to difficult situations. You also have to do this for yourself!
If there is an issue in your life, for insistence, you are not going to the doctor for your own check ups or you get out of bed while you are sick, you must start taking action to solve this.
Making active choices to change the situation at hand will encourage a positive attitude, also giving you more confidence in your abilities.
Tip #4 Find accurate information

COPD is not always genetic, and it most often caused by smoking or inhaling harmful irritates, therefore, you may have never known anyone with COPD in your life, so understanding this new disease as a caregiver, can come as quite a shock.
A quick google search isn’t always the best way to research aspects about COPD especially because COPD is not a one size fits all diagnosis. This means that whoever you are taking care of with COPD is very different than anyone else with the same diagnosis.
The first thing is creating a strict treatment plan with your doctor, as well as establishing a relationship with your doctor, physical therapist, pulmonary therapist, or other related health care professional. Your doctor will create a specific treatment plan for their COPD and how COPD affects your life. By establishing a relationship you will be able to call and ask questions, seek help, and advice, rather than guessing.
One of the most important parts about a patients COPD treatment regime is long term oxygen therapy. Oxygen therapy is used for COPD who’s oxygen saturation is 92% or below while breathing air. This means the patient has a low enough blood oxygen level, also known as dyspnea, to qualify for a long term oxygen prescription.
The most effective, modern, and cost effective option for long term oxygen therapy, is utilizing a portable oxygen concentrator. These devices are built to last a long time, and they are designed to be portable, and can even be taken on airplanes.
As a caregiver, it is important for you to be able to take time off, and rest.
If your loved one with COPD has their own portable oxygen concentrator, they will be able to take it with them alone to the store, or feel comfortable walking by themselves, because some units like the Caire Freestyle Comfort only weigh 5 pounds! This way if you need to take a break, you can ask for help.
.png)
It gives the person in your life with COPD a sense of independence from you (the caregiver) which is also a very motivating feeling for them!
Finding information about oxygen therapy can be very confusing, the first thing you should know is that not everyone with COPD needs oxygen therapy, only those who have very low blood oxygen levels. You could actually over-saturate your blood with oxygen, which has adverse consequences and can be very dangerous. This is the reason why you will need a written prescription from your doctor in order to buy a portable oxygen concentrator from a licensed distributor.

A reliable place you can speak with a respiratory specialist who knows how to connect any patient with the best portable oxygen concentrator of 2020 is at LPT Medical. You can reach out by phone 1(800)-946-1201 or by email at info@ltpmedical.com.
Tip #5 Effective communication
.jpg)
Being able to communicate as a caregiver is hugely important for yourself, and the one you are caring for. Being able to communicate in ways that are clear, assertive, and constructive, helps you to find the help and support you need.
Communicating is not the easiest thing, but here are some things you can practice to get better at it:
- Try to express your feelings using “I” messages rather than using “you” messages. For example saying “I am angry” rather than “You are making me angry” is much more productive and allows you to speak about your emotions without blaming the other person making them become defensive.
- Accept the emotions of others and respectfully take into consideration their point of view. Avoid intentionally hurting anyone’s feelings by violating their rights, you can do this by recognizing another person’s right to express their feelings.
- Be clear and direct with your words. Speak directly to the person. Do not expect the other person to know how you feel if you haven’t explained your emotions. There are no mind readers. When you are direct about what you need or feel, you are respecting the other person's opinion by directing the conversation in a productive manner. It also allows the other person to speak freely and openly about their emotions and the chances of reaching understanding are greater.
- Be a good listener. Listening is the most important aspect of communication.
Overview
Having COPD is a challenging diagnosis, it requires you to alter your daily lifestyle, break bad habits, and much more. With the help of a caregiver, to comfort and support you, you will be able to stick to a treatment regimen that is healthy and promotes an active lifestyle.
As a COPD patient it is important for you to work with your caregiver in times of hardship, and to frequently do things independently when you can. That means you might need to find innovative ways to do your own chores by carrying your own oxygen device. Even if you need a higher output of oxygen, the Respironics SimplyGO is the lightest pulse and continuous flow concentrator on the market, and give the oxygen user freedom and independence that is healthy for the caregiver and patient's relationship.
We hope all the caregivers and COPD patients can find a rhythm going through their day to day lives living with COPD. We hope these tips are helpful for the caregiver to continue to take care of themselves in order to be the best caregiver for their loved one.
If you have COPD, the first sign that something was not right was likely feeling shortness of breath, to the point that you wanted to see your doctor about it. It also could have been that incessant cough throughout the day and night.
It's easy to blame a cough on allergies or a common cold, but if it persists and becomes a regular thing, you should see your doctor to discuss the possibility of having COPD or another lung ailment. The sooner you find out if it is COPD causing your symptoms the sooner you will be able to treat the chronic illness, thereby slowing down the progression of your COPD.
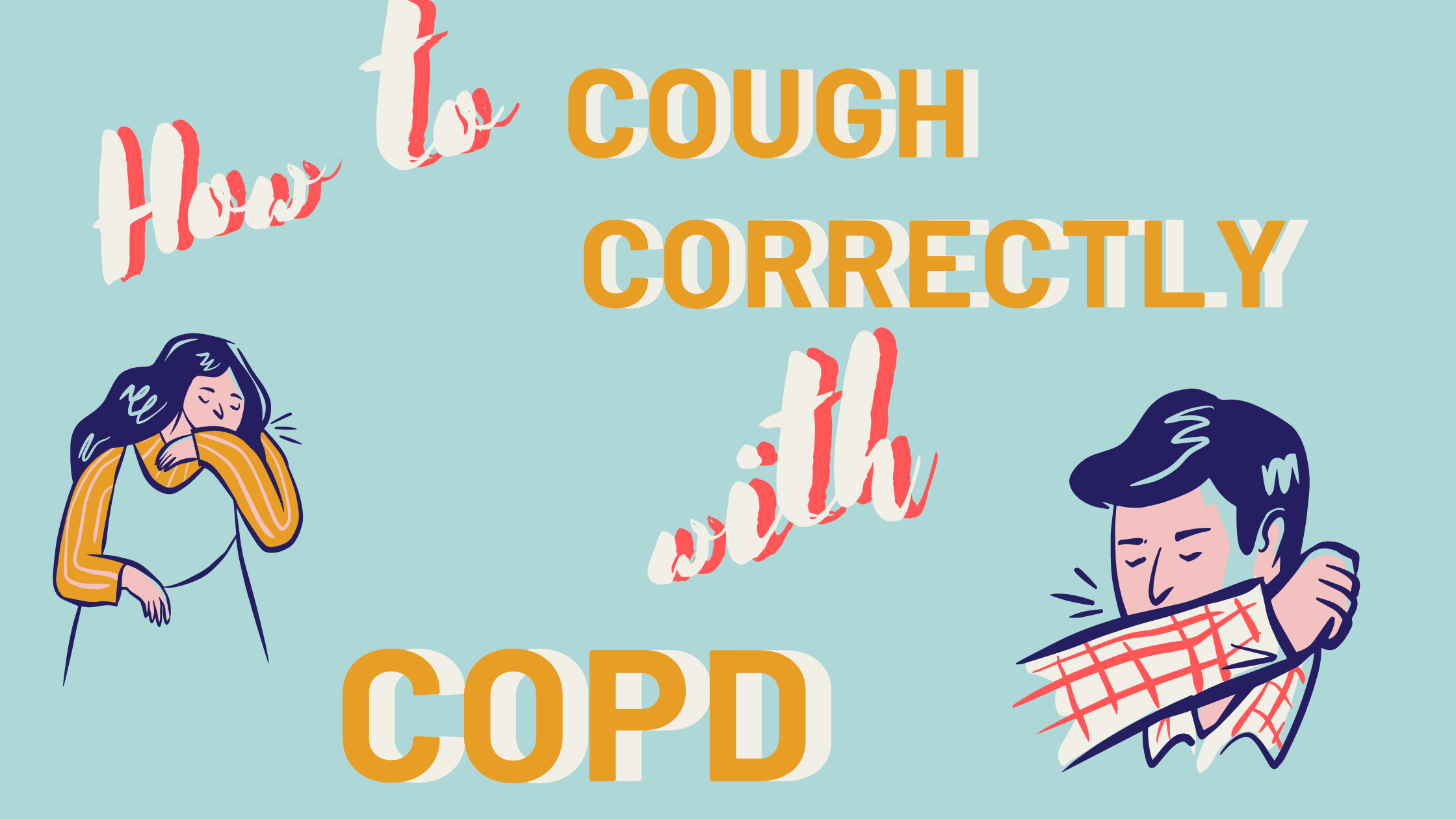
The first thing that you need to understand is that coughing may seem like a symptom you want to relieve, but in the case of COPD, it actually serves a function.
Continue reading to understand how COPD and coughing are related, what you can do to ease a cough, and when to seek medical attention.
How are COPD and Coughing Related
If you have COPD you probably experience a persistent cough. This symptom is related to a condition of COPD called chronic bronchitis, which means that your airways are constantly irritated. This irritation is often caused by smoking or second-hand smoke, but it can also be caused by other irritants and biological factors, such as pollution or genetics.
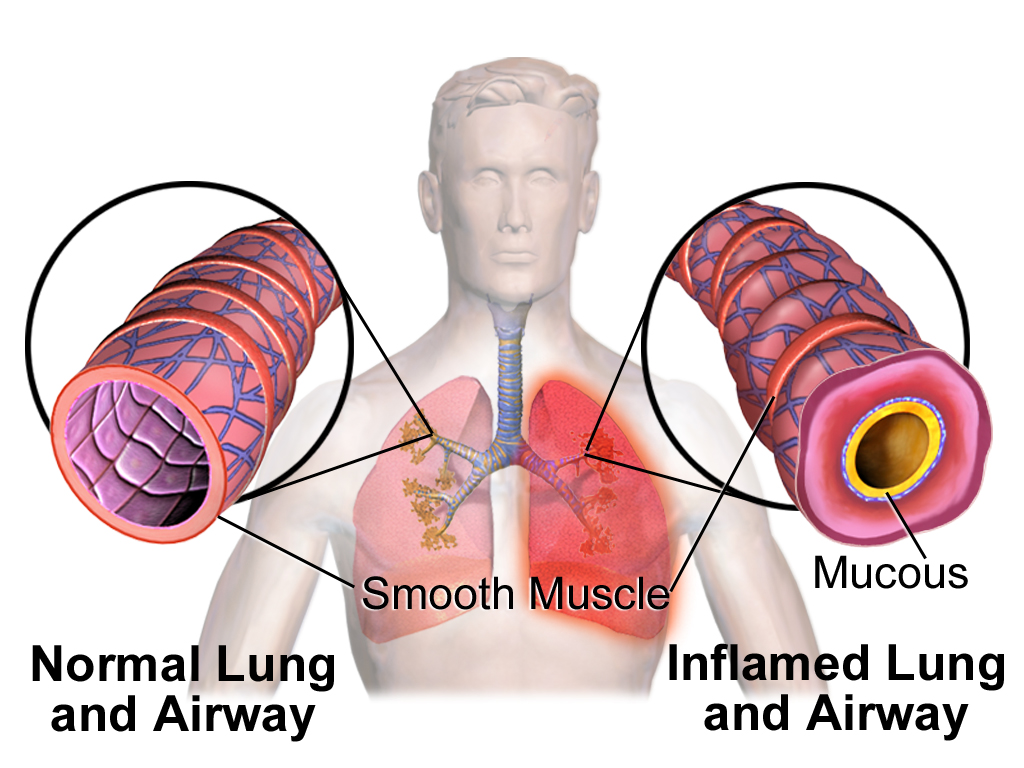
The irritation in your airways causes two problems that prevent enough air from passing through to the lungs:
- The lining of your airways become swollen
- There is too much mucus produced by your lungs
People with chronic bronchitis can have a persistent cough because it is important to regularly clear their swollen airways of this excess mucus, which can sometimes be difficult and require extra attention and treatments, of which, we will discuss in more detail in the What you can do to ease a cough associated with COPD section of this article.
So, coughing caused by COPD is often productive and it is a natural function of your body that plays an important role in your breathing system. Coughing helps to move extra mucus out from your lungs. Coughing is also a reaction that can help remove certain irritants you may inhale into your lungs, like dust, pollution, and other common allergens.
When your cough produces mucus, which is also called sputum or phlegm, that means your body is working correctly to clear the excess mucus up through your swollen airways and into your throat and out of your mouth.
It is normal for the mucus to be clear or white, yellow, or green in color but if the mucus is very mucky, it may be a sign of a respiratory infection. We will go over this in more detail in the When you should see a doctor section
What you can do to ease a cough associated with COPD
To determine whether or not your cough needs to be treated with medication or other remedies, depends on the type of cough you are experiencing and whether or not your cough is actually helping to clear your lungs and airways.
You should consult with your doctor to determine the type of cough you are experiencing and how to deal with it going forward.
As we discussed in the section above, airway clearing coughs serves a meaningful purpose by clearing out mucus from your airways. In this case, it is best for you to continue coughing in order to avoid mucus building up in your lungs.
.png)
That being said, there are certain medications you can take as well as techniques you can learn how to perform in order to couch more effectively.
COPD and coughing medications
If your cough is due to very thick mucus, first you should try to drink more fluids. This can help make your mucus thinner and easier to clear. If this does not work well enough, then there are medicines called “expectorants” that can help make the mucus easier to cough up.
If your coughing becomes painful or difficult to control. In those cases, your doctor might recommend cough suppressants that keeps your body from coughing. These suppressants might also be used for coughs that do not produce mucus, like a dry smoker’s cough.
If you have COPD, coughing can also cause a “bronchospasm” or “spasm.” This happens when your muscles around your airways suddenly tense up causing your airways to become very narrow, This makes it even hard to breathe. To reduce coughing that causes spasms, healthcare providers might prescribe special types of inhaled medications called “bronchodilators” or inhaled steroids.
.png)
If you are not interested in getting on medication for you coughing, there are also three airways clearing techniques you can do to clear your lungs
Airway clearing techniques for COPD
One of the most effective ways to clear your airways is to use the effective, or controlled, cough technique. This cough comes from deep within your lungs and has just enough force to loosen and carry mucus through your airways without causing them to narrow or collapse. By utilizing the controlled coughing practice, you will save energy and therefore, oxygen.
- Controlled coughing: A type of cough that comes from deep in your lungs. It loosens mucus and moves it though your airways
- Postural drainage: You lie down in different positions to help drain mucus from your lungs
- Chest percussion: You lightly tap your chest and back. The tapping loosens the mucus in your lungs
To cough effectively:
- Sit on a chair or on the edge of your bed, with both feet on the floor. Lean slightly forward. Relax
- Fold your arms across your abdomen and breathe in slowly through your nose. (The power of the cough comes from moving air.)
- To exhale: lean forward, pressing your arms against your abdomen. Cough 2-3* times through a slightly open mouth. Coughs should be short and sharp. The first cough loosens the mucus and moves it through the airways. The second and third cough enables you to cough the mucus up and out.
- Breathe in again by "sniffing" slowly and gently through your nose. This gentle breath helps prevent mucus from moving back down your airways
- Rest
- Perform again if needed
Here is a link to postural drainage and chest percussion treatment and how to perform these mucus clearing techniques.

Natural home remedies for helping reduce COPD induced coughing
Eucalyptus oil
Eucalyptus oil contains a natural compound called eucalyptol. Eucalyptol may have the following benefits for people with COPD and may ease uncomfortable coughing symptoms:
- antioxidant and anti-inflammatory properties
- opens up the airways in the lungs
- reduces mucus production
- helps clear mucus from the lungs
- prevents flare-ups in moderate to severe COPD
One way you can use eucalyptus oil is by adding 12 drops of eucalyptus oil to 150 milliliters of boiling water and inhaling up to three times per day.
This will not work for everyone, and if you experience any side effect of the oil, stop using it immediately.
-1.png)
Quit Smoking to reduce dry coughing
Smoking is the leading cause of COPD in the United States and is responsible for around 90 percent of COPD-related deaths.
Tobacco smoke is known to irritate your airways and your lungs. Smoke causes inflammation and obstruction within your airways causing them to narrow, and making it very difficult for air to pass in and out.
If you smoke, the most important step to reduce COPD related symptoms and slowing down the progression of your COPD is to stop smoking. Quitting will put an end to “smoker’s cough,” the dry, hacking cough common among people who smoke.
A deep, productive cough that clears the airways of mucus may replace this dry cough also benefiting you and your breathing.
-png.png)
When you should seek medical attention
Call your doctor within 24 hours if you notice:
- You’re out of breath or coughing more than usual
- Being out of breath affects your daily routine
- You’re coughing up more gunk that normal
- The mucus you are coughing up is dark yellow, dark green, or rust-colored
- You have a fever over 101 F
- You feel dizzy or lightheaded
If you begin to experience any of these symptoms it could mean that you have a respiratory infection or your COPD is getting worse.
Call 911 or go to the emergency room if you’re still out of breath after using the medicines your doctor has prescribed for your COPD.

Other symptoms associated with COPD
One of the other many symptoms of COPD we mentioned very briefly in this article was shortness of breath. When you have COPD your lungs are no longer able to process oxygen like they once did. This is partly due to the irritation in your airways that also causes coughing.
Both chronic bronchitis and emphysema can cause shortness of breath. This symptom is also called “breathlessness” or “dyspnea".
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
If you airways are swollen and filled with mucus, not only does this initiated a coughing reaction, but it also inhibits oxygen from flowing through your lungs and into your blood stream and organs.
Not only is this feeling extremely uncomfortable, it is also life threatening, and if it goes untreated for a long period of time, you will inevitably be taking years off of your life.
Here are positive changes you can make to improve breathing with COPD:
Learn pursed-lip breathing This is a breathing exercise designed for people with COPD: Purse your lips and blow as much air out as you can before taking a deep breath in through your pursed lips again. Then slow down your breath so that you’re using as much of your lungs as you can. This technique slows your breathing rate and helps to keep your airways open which can also help to reduced coughing episodes.
Drink plenty of water because water helps thin out mucus so you can clear it better. Some people with COPD have conditions that could be made worse by extra fluid, however some people with COPD may be very dehydrated.Speak with your doctor to find out how much water you can safely drink.
Get informed and continue learning about COPD and how your lungs function. This can help you better understand and manage your condition. Pulmonary rehabilitation programs often offer this type of education.
Exercising regularly can make a big difference in your breathing capabilities and COPD symptoms. A lot of people with COPD get more and more out of breath as their disease progresses, but it’s not due of their lung function — it's because they’re not conditioning enough. Most doctors recommend walking for people with COPD since it’s moderate in intensity and easily accessible.
Know and avoid your triggers. If you have COPD and allergies, take steps to avoid anything you’re allergic to. This may mean putting dust covers on your pillows and mattress or keeping your pets out of the bedroom. High-efficiency particulate air filters can remove dust and other irritants from the air in your home. You may also consider a humidifier if dry air triggers your symptoms.
Get your rest Many people with COPD have an underlying sleep disorder, like sleep apnea, that makes it difficult to get good sleep. When you sleep better, you’ll feel better and breathe better, so if you are not able to fall asleep, or have trouble staying asleep, speak with your doctor to understand the root of this issue so you can solve it.

Stay on a healthy diet full of nutrient-dense foods is needed with COPD to maintain strength and fight off infections. Eating healthy can help you lose weight and breathe easier. If you’re underweight, ask your doctor about the best foods to eat and if nutritional supplements are right for you.
Take your medication COPD medications can help manage symptoms, including shortness of breath so be sure you’re taking the right medications and get evaluated to make sure your lung function is as good as it can be
If you have severely low oxygen levels this is called hypoxemia, your doctor will likely prescribe you medical-grade oxygen, for home oxygen therapy. Long-term oxygen therapy has many benefits if it is used correctly and It can even help you live longer.

Low oxygen symptoms of hypoxemia vary depending upon how severe your COPD is, and how severely it affects you. If you experience any of the symptoms listed below, contact your doctors as soon as possible. If you experience more than one of the following symptoms at one time, seek medical attention immediately:
- Confusion
- A sense of euphoria
- Restlessness
- Headache
- Shortness of breath
- Rapid breathing
- Dizziness, lightheadedness and/or fainting spells
- Lack of coordination
- Rapid heart rate
- Elevated blood pressure
- Visual disturbances
- A bluish tint to the lips, earlobes, and/or nail beds (cyanosis)
Hypoxemia is the main reason that people with COPD and other lung diseases are prescribed supplemental oxygen. There are a few forms of home oxygen therapy: You can opt for liquid oxygen tanks, gas cylinder tanks, or the most popular, convenient, and cheapest option a portable oxygen concentrator.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
If you are a good candidate for long-term oxygen therapy, this is a blessing in disguise. While it might seem as if you lung function is declining, once you are able to utilize oxygen, your quality of life will improve drastically. When you have adjusted to the oxygen therapy, you will begin to slow the progression of you COPD as well!
Once you find the right POC for you, your bones and muscles will feel stronger and energized, you will have improved exercise tolerance, your mood and stamina will boost, your quality of sleep may improve, and so much more.

If you feel like you have experienced any of the symptoms of hypoxemia, and are curious how to find the best portable oxygen concentrator to fit you oxygen requirements, fill out the blue box to the right, it is our official guide to portable oxygen concentrators.
Cough with a Purpose
Remember, COPD-related lung damage can’t be reversed, but it can be controlled if treated properly.
Now that you understand that your cough can in fact be beneficial for your health and in treating COPD, we hope that you can use the information in this article to cough effectively and efficiently. These coughing techniques, mixed with medication and other home remedies should reduce the dry uncomfortable smokers cough, and help you to cough with a purpose.
Even though this can be a pain, always feel free to excuse yourself during social gatherings, and other outings to clear mucus from your lungs and airways. This will allow you to go longer without coughing and spend more quality time with the ones you love while enjoying the things you like to do.
The more you practice these coughing techniques the more efficient you will become at clearing your airways, and therefore breathing!
If you have any questions please leave a comment on this blog below, and always feel free to share our blog with your friends and family. By explaining how beneficial your cough is for managing your COPD, they will better understand and be willing to help and encourage coughing rather than trying to help you avoid it.

Spring is the season of new beginnings and fresh starts; it's the perfect time to get out your cleaning supplies and do some sprucing around the house. But spring cleaning isn't just a cliché, it makes sense to dedicate time once a year to catch up on chores and give some attention to neglected spaces in your home.
For people with COPD and other respiratory diseases, spring cleaning is an important opportunity to take care of lung irritants and hazards in the home. With spring allergens swelling and summer on the way, it's the perfect time to clear out clutter and make your home the cleanest, healthiest space it can be.
In this post, we're going to help you make the most out of spring cleaning by focusing on tasks that can help your COPD. We'll show you how to get rid of dust, mold, allergens, and how to improve your indoor air quality and ensure it continues to stay clean.
We'll give you tips for organizing your home to keep respiratory irritants at bay and ensuring outdoor allergens and pollutants don't build up in your home. We'll also show you how to protect your lungs from fumes, dust, and other particles while you clean, and how to make difficult cleaning projects easier to manage.
Keeping your home clean is not only good for a sound mind, but for healthy lungs as well. With the tips in this article, you can make sure you do spring cleaning right this year so you can enjoy the benefits of a healthy home the whole year round.
The Basics of Spring Cleaning
Regular cleaning year-round is important, but it's good idea to pause and pay attention to the details every so often. Even if you keep up with the necessities throughout the year, your house will inevitably collect hidden corners of dust and clutter and accumulate little maintenance and deep cleaning tasks that need attention.
If you let these things go for too long, they can become respiratory hazards and make your COPD symptoms worse. Dust, allergens, and toxic particles can sneakily build up in all sorts of places in your house, and spring cleaning is the perfect time to find and eradicate them all.

But before you get started, you should take some time to learn how to protect your lungs and go easy on your body while you clean. In the next sections, we'll discuss what kinds of supplies you'll need, what kinds of chemicals you should use, and how to protect your lungs from dust and fumes.
We'll also give you some general tips for cleaning as efficiently and effectively as possible, so you don't waste time and energy during your spring clean. COPD can make household tasks difficult, but planning ahead and learning new techniques can make cleaning easier and less tiring.
Protect Your Lungs When You Clean
The first thing you should consider is how you are going to protect your lungs from irritating particles and chemical fumes while you clean. After all, cleaning tends to kick up all sorts of respiratory irritants that can irritate your lungs and airways.
When you have COPD, cleaning without taking care to protect your lungs can do more harm than good, causing further lung damage and making your symptoms flare up. To clean safely, you need a two-pronged approach: using safe cleaning products and protecting your mouth and nose while you clean.
Avoiding Chemical Fumes

In general, you should avoid using commercial cleaning products, which are often made with harsh chemicals that can irritate your lungs airways. Instead, look for natural products made with mild ingredients or simply mix your own cleaning solutions at home.
Here are some chemicals that you should look out for and avoid using when you clean:
- Chlorine bleach
- Ammonia
- Detergents
- Aerosol sprays and fresheners
- Pesticides and fungicides
- Varnishes
- Floor wax and polish
- Oven cleaners
- Carpet cleaners
Commercial cleaning products aren't actually necessary for most cleaning tasks, and all you need is a few basic ingredients to make DIY cleaners for your home. Soap, vinegar, and baking soda are surprisingly effective for cleaning, and, when used in moderation, are much gentler on your lungs.
You should also stock some bleach and ammonia for more serious sanitizing, but be careful to never mix bleach and ammonia together. Be very careful to always examine the labels of any chemicals or cleaning products you have and only use them as directed.
Visit our previous post here for some recipes you can use to make your own safe cleaning solutions at home. You can also visit the EPA's website for “Safer Choice” products, which are specially labeled to indicate that they are safer for the environment and your health.
One of the most important things to remember is to never use chemicals in an enclosed space. At the very least, the fumes could irritate your eyes and airways, and at worst, they could even be deadly.
Any time you use a cleaning solution, think first about the space you will use them in and whether or not it needs extra ventilation to be safe. You may need to open some windows, turn on your bathroom vent, or set up a fan to increase air circulation in the room.
Particle Safety
Whenever you dust or do deep cleaning, you are likely to kick up all sorts of particles that have accumulated and laid dormant in dark corners. All of these particles, including dust, mold spores, pet dander, pollen, and smog and smoke particles, can inflame your lungs and cause your COPD symptoms to flare up if you're not careful.
That's why you need extra equipment to protect your mouth and nose from any particles or fumes you encounter when you clean. Even something as simple as covering your face with a scarf can keep you from breathing in large bits of dust, but you may need a special mask to protect your lungs from the smaller particles.

Particle respirators are much more effective than a basic surgical mask or face covering, and can screen out 95 percent of particles as tiny as 0.3 microns in width. This is the best choice if you suffer from allergies or are very sensitive to airborne particles.
To get a proper particle mask, look for an N95 respirator that is certified by the Food and Drug Administration (FDA) or the National Institute of Occupational Health and Safety (NIOSH). You can also see a list of official N95 mask manufacturers at the CDC's website here.
Some people have trouble breathing when using a respirator because of the resistance that the mask creates when you breathe. To reduce this resistance, look for an N95 respirator with an exhalation valve on the front of the mask.
If you have very severe COPD, even a little bit of dust or mold could cause your symptoms to flare up. In this case, you should talk to your doctor about what kinds of cleaning you can manage and enlist someone else to do the hazardous tasks.
Certain chemicals, like bleach, pinesol, and ammonia, can also cause inflammation and COPD flare-ups if you're not careful. Unfortunately, a particle mask alone is not enough to filter these fumes out of the air.
If you have to work with harsh chemicals, you can reduce the chance of exposing yourself to irritating fumes by being extra careful to ventilate the rooms you work in. If they still irritate your airways or you have to clean a more enclosed space, you will need to get a special gas mask or ask someone else to do the work for you.
General Cleaning Safety
Along with protecting your lungs, you should also take care to protect your hands, skin, and eyes from harsh chemicals when you clean. That's why you should always have some gloves and goggles on hand for particularly messy tasks or when you use any hazardous chemicals.

You should also pay special attention to any chemicals you use when you clean, reading the labels and making sure to dilute any concentrated chemicals appropriately. Never use any chemical for an unapproved purpose or mix chemicals together for any reason.
Make sure you wash any sponges or rags you use to clean so they don't accumulate bacteria or mold. Switch to fresh rags often to avoid spreading around bacteria or mold, especially after cleaning very dirty surfaces like toilets and sinks.
Enlist Help When Needed
If you are very sensitive to airborne irritants or have very severe COPD, then you don't want to take any chances when you clean. In some cases, this may mean hiring a cleaning professional or asking friends or family to help you clean your home.
For example, you should ask others to help with any tasks that cause your symptoms to flare up or require you to use toxic chemicals. That includes any cleaning projects that kick up a heavy amount of dust or mold, especially if you don't have adequate facial protection.

Make sure you take the time to inform any helpers or professional cleaners about your disease and your sensitivity to chemical fumes and fragrances. Tell them what kinds of products are okay to use and what chemicals are off-limits for your home.
If the work will stir up a lot of dust or requires harsh chemicals, you should be careful to stay out of the way so your lungs don't get inflamed. You might be able to simply go to a different room, or you may need to leave the house entirely until the task is done and your home has a chance to air out.
As your COPD progresses, you may find it too tiring to do major cleaning tasks or find that your lungs are just too sensitive to handle certain things. When this happens, there is no shame in asking for help and letting others take care of the work.
Chemicals and Equipment You Will Need

You don't want to begin your spring cleaning project only to find that you don't have the supplies you need. Before you get started, make sure you have all the basic supplies and cleaning solutions you will have to use.
Not only will this save you time as you clean, but it gives you a chance to replace all of your hazardous commercial cleaning products. Throw out any harsh or scented products and buy the ingredients you need to make your own, lung-healthy cleaning solutions instead.
Here is a general list of cleaning products and appliances you should have for your spring clean:
- Vacuum
- Broom
- Mop
- Sponges
- Dusting tool
- Cleaning rags and towels
- General purpose cleaning solution
- General purpose sanitizing solution
- Gloves
- Goggles
- Particle mask or respirator
- Soap
- Vinegar
- Ammonia
- Baking soda
Work from Top to Bottom

A good general rule of cleaning is to start at the top and work your way down. That way, you can knock dust and other particles down from high places without dirtying something below it that's already clean.
It's important to dust and wipe down all the surfaces in your home before starting on the floors. If you follow the guidelines and steps in this article, you should be able to tackle all the dust and grime in the right order.
Make Cleaning Tasks Easier
If you get breathless easily or have limited mobility, it can make major cleaning tasks difficult. That's why you need to have the right tools and techniques to reduce the strain.
Good Posture

Bending, stooping, and poor posture are all enemies of easy breathing. To reduce the pressure on your lungs and make it easier to catch your breath, make sure you practice proper posture when you clean.
As much as possible, try to keep your back straight, you shoulders back, and your chin parallel to the ground. This will keep your chest open to allow better breathing and prevent your muscles from getting sore.
Take Breaks
It may be unrealistic to try to do a thorough spring cleaning in a single afternoon or weekend. Instead, spread out your tasks over several days so you don't wear yourself out too much at once.
You should also take frequent breaks as you clean, especially when you start to feel tired or short of breath. If you break up tasks up into shorter, manageable chunks, you'll have plenty of time to rest in-between.

Pacing is also important, because trying to do too much at once can deplete all your energy very fast. If you take it slow and spread the work out, you'll be able to do more without feeling fatigued.
Use Proper Cleaning Tools and Aids

As you go about your house and clean, look for ways that you can decrease the amount of strain and energy you have to use. After all, you don't want to waste all your energy on house chores when there are so many other activities in life to enjoy.
For example, you could get a cleaning apron to wear around your waist that has slots for basic supplies like cleaning solutions and rags. Having an apron to store things in not only frees up your hands, but reduces the amount of times you have to walk back and forth across the room to get supplies.

Also, having a tall stool to perch on instead of standing can help you conserve energy and improve your balance. For example, you might pull up a stool to sit on as you wipe down your counters, unload the dishes, or sort and fold laundry.
Short stools are useful to use when you need to clean spaces that are low to the ground. You can use them to make tasks like spot cleaning floors or dusting low shelves much easier to do.
Whenever possible, you should also elect to buy long-handled cleaning tools like dusters, brooms, and mops. That way, you don't have to stoop or strain yourself as often while you clean.
Also take care when storing your cleaning products to ensure that they are within easy reach for next time. Items stored below shoulder height but above knee height are usually the easiest to reach.
Use Breathing Techniques

When you're doing chores around the home and start to feel breathless, pursed-lips breathing is one of your best resources. By helping you pace and control your breaths, pursed lips breathing can help you do more activities for longer without losing your breath.
It also helps to sync your breaths with your actions, timing them together to help you stay in control. To learn more about pursed-lips breathing, see our
Chronic respiratory diseases (CRDs) are diseases within your airways and other parts of your lungs. Some of the most common CRDs are chronic obstructive pulmonary disease (COPD), asthma, pulmonary fibrosis, occupational lung diseases, and pulmonary hypertension. In this particular article we are focusing on COPD, but a lot of the information can be related to other CRDs.
There are a lot of basics your doctor will tell you about COPD once you are diagnosed, but as with anything in life, there are some things that cannot be explained, and instead you learn from experience.
Once you are diagnosis with COPD, there is no straight path you take, there are left turns and right turns obstacles big and small, all of which you will learn to go through. You will learn how to find ways to live with this disease, and we are here to not only help you live with COPD, but live a high quality life with COPD.
You will learn along the way, what COPD triggers are the most harmful to you and how to avoid them, you will learn what foods cause bloating in your body, and how to fit exercise into your daily routine.

While your doctor may suggest healthier habits and give you tips for living a healthier lifestyle, you are the one who has to go home and live with COPD, so you will have to determine how to follow your doctor’s advice in the most effective way possible, and this isn’t always black and white.
We designed this resource guide to help you navigate the reality of living with COPD, if something applies to you take it, if not leave it behind. Everyone is different and COPD affects every individual differently so it is important to listen to your body and mind to get the best possible treatment for your COPD.
COPD is commonly Misdiagnosed

One of the most important things to discuss about COPD, is the diagnosis. First of all, in many cases, people who have COPD are not to be diagnosed until the disease has progressed into a more severe state. More than 16.4 million people have been diagnosed with COPD, but millions more may have the disease without even knowing it.
It is increasingly common to miss the warning signs of COPD early on, as the beginning stages can often be chalked up to “getting older”. Therefore, COPD is often not found until the disease is very advanced, when there is something clearly wrong. This is alarming, and serious action should be taken to prevent it because COPD is a progressive disease, meaning it gets worse over time. If you catch COPD warning signs early, the sooner you can start to treat COPD and slow down the deterioration in your lungs.

Some of the symptoms of COPD are similar to the side effects of “getting older.” If you think you have even mild symptoms of COPD, tell your doctor as soon as possible so they can test you.
Here are some early warning signs to look out for:
- Shortness of breath, especially during physical activities
- Wheezing
- Chest tightness
- A chronic cough that may produce mucus in a clear, white, yellow or greenish color
- Frequent respiratory infections
- Lack of energy
- Unintended weight loss (in later stages)
- Swelling in ankles, feet or legs
You should be considered for diagnosis of COPD if you experience symptoms of a chronic cough, sputum production, dyspnea and a history of exposure to risk factors for the disease.
To diagnose your condition, your doctor will look into you medical and family history before they look at your signs and symptoms. You should also bring up any exposure you've had to lung irritants — especially if you smoke cigarettes or are exposed to cigarette smoke a lot smoke.
Be Careful to Avoid COPD Flare Ups

If you have COPD, you are also likely to experience COPD exacerbations, during which your symptoms become worse than the usual day-to-day symptoms. These episodes can be long-lasting and persist for at least several days, and in some cases you may need to seek medical attention.
There are many triggers of COPD exacerbations, and your trigger may be different than someone else's, but here is a list of some common triggers that you can work to avoid:
- Smoking
- Second-hand smoke
- Air pollutants
- Dust
- Dust mites
- Clean products such as bleach
- Indoor allergens like animal dander
- Outdoor allergens like hay and pollen
- Cold dry outdoor air during winter
- Hot moist steam from showers
If you have COPD it is best for you to avoid these triggers listed above. We wrote a resource guide for people who want to create a COPD safe living space inside their home, you can read it by clicking here.
There is No Cure for Chronic Lung Diseases

CRDs including COPD are not curable, however, various forms of treatment are available. Certain treatments such as supplemental oxygen therapy, can improve shortness of breath and help control symptoms and increase the quality of life for people with the disease.
COPD gets worse over-time, and without the proper treatment, COPD will cause major health issues, and even lead death.
COPD is Commonly Cause by Smoking and Air Pollutants
In addition to tobacco smoke, you can also develop COPD by inhaling other risk factors including air pollution, occupational chemicals and dusts, and frequent respiratory infections during childhood.
COPD is Diagnosed by Your Doctor with a Series of Tests
Common COPD tests are as follows:
Lung (pulmonary) function tests
These tests measure the amount of air you can inhale and exhale, and whether your lungs deliver enough oxygen to your blood.
Chest X-ray. A chest X-ray
X-rays can show emphysema, one of the causes of COPD. An X-ray can also exposure or rule out other lung problems or heart failure.
CT scan. A CT scan of your lungs can help detect emphysema and help determine if you might benefit from surgery for COPD. CT scans can also be used to screen for lung cancer.
Arterial blood gas analysis
This is a blood test which measures how efficient your lungs are transferring gases. So this test specifically looks at the oxygen in your blood and the removal of carbon dioxide.
Laboratory tests
Lab tests will not be used to diagnose COPD, however they can be used to find the cause of your symptoms, and rule out other respiratory conditions.
Spirometry
This is a test designed to diagnose chronic obstructive pulmonary disease (COPD), so it measures how deeply you can breathe and how fast air can move into and out of your lungs. Low results from a spirometry test can be consistent with COPD, but also may not be specific to COPD because it can be caused by other lung diseases and poor performance during testing.
Because COPD develops slowly, it can be hard to diagnose COPD accurately, which is why it is frequently diagnosed later in life, mostly in people 40 years or older.
You Can Treat COPD

While there is no cure from COPD, or other CRDs, you can treat your disease and ease the symptoms. With the correct treatment, medications, and healthy habits you can even slow down the progression of your COPD.
Oxygen therapy is one of the COPD treatments that can extend your life expectancy.
Eating healthy foods that do not cause bloating will help you feel less short of breath.

Exercising or walking regularly strengthens your airways and lung muscles, which helps you manage COPD symptoms more effectively.
Medications, like short-acting bronchodilator help open your airways to make breathing easier in emergency situations, and during a COPD exacerbation. Medications can make the recovery process easier.
If you Need Supplemental Oxygen your Doctor will Prescribe it to You

Supplemental oxygen therapy is a life saving treatment for respiratory patients with low blood oxygen levels. You can be administered oxygen through a liquid oxygen tank, compressed oxygen gas canisters, or a portable oxygen concentrator (POC). All of these methods feed oxygen to the user through an oxygen nasal tub or face mask.
The biggest difference between each of these methods is the tanks and canisters have a finite amount of oxygen that must be refilled, whereas a POC takes ambient air from its surrounding and purifies it into medical-grade oxygen. POCs also runs off of batteries so it will have to be re-charged.

Oxygen therapy will be prescribed to you by your doctor after undergoing tests that will measure your current oxygen intake and transfer of gases in your lungs. If you have Hypoxemia, meaning you have low blood oxygen levels, your doctor will prescribe you a flow rate and give you recommendations for an oxygen device.
You will then want to get in contact with an oxygen device distributing company, possibly in your local area. For example you can google search something like, Denver, Colorado oxygen supplies, and LPT Medical will pop up, same goes for Boca Raton, Florida oxygen equipment. This is one way to find portable oxygen concentrators for sale near you, but you can also order POCs from around the nation and they can be shipped to you.

If you are going to be using an oxygen tank, it is essential there is an oxygen delivery company near your home, because they will have to come and replace empty tanks with filled tanks weekly.
LPT Medical is a family owned and operated business, and while we do a lot of local oxygen sales in Denver and Boca Raton, we also work with customers nationwide. If you are in the market for a portable oxygen concentrator, call us at 1-800-946-1201 so we can help find you an oxygen device that fits your needs.
Too Much Oxygen Can be Dangerous

The reason it is crucial to go through a licensed oxygen distributor like LPT Medical, is because we make sure to look at your doctor’s prescription before we recommend an oxygen device to you.
We would recommend devices like the ARYA portable oxygen concentrator to an oxygen user with a pulse flow rate of 630 - 840 LPM. On the other hand, if you need a continuous flow of oxygen of about 0.5 - 1.0 LPM you would need a device like the Respironics SimplyGo.

If you started to take oxygen more often than your doctor recommended or upped the dosage, you would start to experience something called oxygen toxicity or oxygen poisoning, and this is very dangerous. The first sign of oxygen toxicity, manifests in your Central Nervous System, and you may start to experience things like:
- Visual changes
- Tunnel vision
- Ringing in the ears
- Nausea
- Twitching (especially of the face)
- Behavioral changes (irritability, anxiety, confusion)
- Dizziness
If you continue to use excessive amounts of oxygen, pulmonary toxicity will begin to occur as a result of too much oxygen in your system. After a certain amount of time with too much oxygen saturation tracheobronchitis or inflammation of the upper airways will start to negatively impact your respiratory system.
There will be a decline in your lung function, alveolar damage, and soon acute respiratory distress syndrome will onset. This could all eventually lead to collapse of your alveoli, also known as atelectasis.
The bottomline is that it is very important to follow your oxygen prescription as an oxygen patient. Other folks at risk of oxygen toxicity are deep sea divers. Be sure to ask your pulmonary doctor and respiratory specialist any questions you have, and clearly communicate your confusion.

Your Oxygen Prescription Will Vary Depending on the Severity of you Your Disease
It is possible that you will have to adjust your oxygen levels while you exercise, compared to while you rest. Some people will need to use oxygen 24/7 and others may only need it while they are exerting themselves physically.
All of this will depend on your condition, so you can’t always ask for advice from others who also have COPD or another oxygen user. Their oxygen dosage may be completely different than yours. The best way to get the most out of your oxygen therapy is to understand you and your condition, your oxygen prescription, and how to use your portable oxygen concentrator or oxygen tanks.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!














