Dealing with equipment issues as a chronic obstructive pulmonary disease (COPD) patient is just a part of the process. The equipment can be the most top of the line quality and you still may have malfunctions or trouble getting the equipment to work within your lifestyle.
The truth of the matter is that, once you start to use equipment to help you treat symptoms associated with COPD your lifestyle will be affected. Whether this is in a positive way or a negative way will depend on the equipment you have, and how well you know how to use it.
It is important to learn how to use your equipment correctly as well as know how to troubleshoot issues associated with the equipment.

COPD Equipment
There are therapies you rely on every day to help you breathe. There are a variety of medical devices from inhalers to oxygen concentrators that are designed to treat symptoms associated with COPD either by giving you additional oxygen supply or medication.
Therapies like these allow you to live better with COPD than if you were to live without them, but using the equipment and taking medication everyday does require a bit of a learning curve.

Take the time to learn about all of the common devices prescribed for COPD plus info on how they work in this blog.
In this blog you will learn about portable oxygen concentrators and how to troubleshoot common problems users have with these devices. We will also talk about common problems people have with oxygen tanks, both liquid and compressed oxygen.

Inhalers are a common form of medication for people with COPD, to use these effectively is important so you get the right dosage of medication, we will discuss how to use your inhalers properly.
Beyond inhalers and supplemental oxygen we will also talk about how to use and take advantage of other common COPD equipment!
Supplemental Oxygen
![]()
Supplemental O2: Compressed Oxygen
Even though there are more modern and sleeker forms of oxygen therapy nowadays, when people think of “supplemental oxygen”, the cylindrical metal-tank system typically comes to mind.
The oxygen from this tank is delivered through a thin plastic hose attached to a cannula. These cylindrical tanks come in various sizes, depending on the amount of oxygen you need.
Your doctor will prescribe you the most beneficial amount of oxygen by giving you a flow rate to set your oxygen device.

It is important for your healthcare team to show you how to adjust gauges on the tank to control the oxygen flow rate, it is common for you to need to adjust the “flow rate” depending on your activity status.
You will also need a system to refill the tanks whether you get new tanks delivered weekly from a supply company, or have someone come to refill the tanks.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Streamlining the process of getting your oxygen tanks refilled is challenging because you are dependent and at the will of the oxygen supply companies. Having patiences but also having a full back-up canister is crucial here. Running low on oxygen is a stressful situation you should try to avoid at all costs.
Supplemental O2: Liquid Oxygen
The benefit of a liquid oxygen system is that it doesn't need to be plugged in because it doesn't run off of electricity or batteries, however, it is not the easiest form of supplemental oxygen therapy because it must be refilled, and in doing so it must be handled with caution.
Liquid oxygen is extremely cold— 200 degrees Fahrenheit— it can burn your skin if you’re not careful while handling the equipment for refilling.
Oxygen must be compressed and cooled to a level that it becomes highly concentrated oxygen that you are able to breath in and process in your body easily.

It is likely you will have a stationary storage unit that is a large reservoir of oxygen and a different smaller portable container to bring when you’re moving around.
To streamline this process, you will have to get very good at refilling your portable oxygen canisters, and maintaining sustainable levels of oxygen in the reservoir so you never run low on oxygen. This will require a relationship with an oxygen supply company for deliveries and refills.
Supplemental O2: Oxygen Concentrator

If you are an active person, a traveler, independent, or simply enjoy user-friendly equipment you will need a portable oxygen concentrator as your supplemental oxygen therapy device.
A new generation of lightweight, portable oxygen concentrators, like the Inogen One G5 and the Caire Freestyle Comfort among others, have made it possible to have an active life while using oxygen support like never before.

An oxygen concentrator draws in air from the room around you, purifies it, compresses it, stores it in a tank, then delivers the fresh air via cannula to your waiting lungs. It sounds like a big job for a small compact device! And it is!
Modern technology has allowed for oxygen manufacturers like Inogen to create small lightweight oxygen devices with batteries to last for hours! Meaning you can carry your device with you whenever you go, and simply charge the device as you would a cell phone so you never run low on oxygen.

There are now smaller, more compact portable oxygen concentrators that also have powerful pulse flow settings and long lasting battery life. The rechargeable batteries make it easy to use your device all day and night.
Inhalers

One of the very first things your doctor prescribed to you once you were diagnosed with COPD was some prescription medications to help you manage your symptoms.
There are two types of inhalers that are most common for COPD management, one for daily maintenance meds and another “rescue” inhaler for symptom flare-ups.
Inhaled bronchodilators, for example, work to open airways for easier breathing as needed or long-term, while corticosteroids are used to fight airway inflammation.
How to Use your Inhaler properly
 Every inhaler comes with its own instructions. In general, here’s how to use one:
Every inhaler comes with its own instructions. In general, here’s how to use one:
- Remove the cap from the inhaler.
- With the mouthpiece facing down, shake the inhaler for about five seconds to mix the medicine.
- Then use one of these techniques:
- Open-mouth technique: Hold the mouthpiece 1 1/2 to 2 inches from your mouth.
- Closed-mouth technique: Put the mouthpiece between your lips and close your lips tightly around it.
- With a spacer: Place the MDI inside the spacer and close your lips around the spacer.
- Gently breathe out.
- Press the inhaler and, at the same time, take a deep breath in through your mouth. Keep breathing in for 3 to 5 seconds.
- Hold your breath for 5 to 10 seconds to get the medicine into your airways.
- Relax and breathe out slowly.
- Repeat the process if you need more puffs of the medicine.
Benefits of Inhalers

They are easy to use and can be used with many different types of COPD drugs, including steroids, bronchodilators, and combination medicines. You also get the same dose of medicine each time you use them.
Drawbacks of Inhalers
require you to coordinate between activating the medicine and breathing it in. It’s also necessary that you breathe in slowly and deeply. If you breathe in too quickly, the medicine will hit the back of your throat, and much of it won’t reach your lungs. You may also need to use a spacer to get the medicine into your lungs.
Nebulizers

Nebulizer can be an easier option for people with COPD who find it difficult to take their meds via inhaler.
Nebulizers are machines that convert liquid medicine into a mist. The drug particles are contained in tiny aerosol droplets inside this mist, which you can then inhale through a mouthpiece or mask.
A great advantage of a nebulizer is that it gets the medication deep into your lungs where it's needed most.
For nebulizers to work, you must use it correctly, however patients with COPD using nebulisers at home experienced problems functioning these devices. Talk to your healthcare team and be sure they are effectively supporting you in the use of your nebulisers at home.
Smartphone Apps
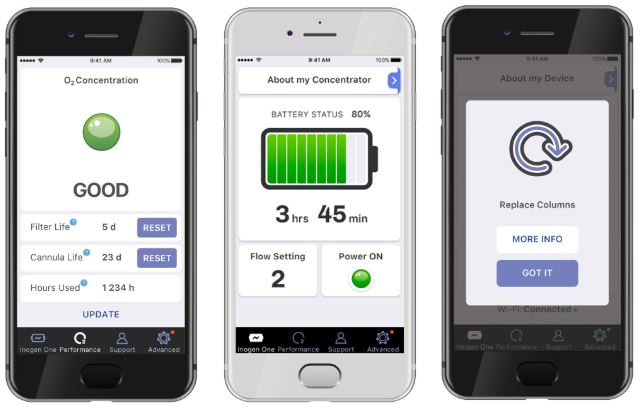
COPD patients can use their smartphones as educational sources and use it to help monitor your COPD symptoms. Your phone is able to alert you when you are experiencing exacerbations that might warrant a call to your pulmonologist.
There are apps you can download that offer a daily questionnaire to rate your symptoms.
You can also check local air quality to avoid airborne irritants via the Environmental Protection Agency’s AirNow app.
CPAP or BiPAP

Often used to treat sleep apnea, continuous positive airway pressure (CPAP) and bi-level positive airway pressure (BiPAP) machines open your airways for better breathing normally while you are sleeping.
Both a CPAP and BiPAP device have a mask that is applied over your face. Then pressure is supplied to open up your airways.
A CPAP machine delivers constant pressure, this pressure can be changed when you aren’t using the device. Most patients require between 6 and 14 cmH20 and the average setting is 10 cmH20, however, the setting you use will depend entirely on your condition and the setting that your doctor prescribes.
![]()
It’s also important to note that every CPAP machine has different capabilities, so you’ll want to make sure it meets your needs before purchasing it.
A BiPAP machine is less common than the CPAP, and it has two different pressure settings: one for inhalation and one for exhalation. The BiPAP machine will automatically detect whether you’re inhaling or exhaling and administer the pressure accordingly. Typically, a higher pressure will be applied when you’re inhaling.
Mucus-Loosening Devices
Mucus build up is a common symptom of COPD. It can affect your breathing by clogging your airways, and it can also induce an uncontrollable cough that lasts the day and night.
A high-frequency chest wall oscillator is an inflatable vest that massages your chest wall to loosen the excess mucus. This will help you cough out the mucus while also using proper coughing and clearing techniques.
Positive expiratory pressure therapy (PEP) is another method to clear mucus. PEP is where you inhale through a mouthpiece, then exhale against a one-way valve that provides resistance. This creates a pressure in your airways to move up mucus.
Overview
We hope that you learned about the equipment that you, as a COPD patient, may need.
A lot of equipment you will need to use everyday, and having the best equipment that you also know how to use is very important for managing this chronic disease.
For instance, a portable oxygen concentrator will be your companion for the rest of your life, therefore it should be reliable and easy to use! Call 1+(800)-946-1201 if you are in the market for a new oxygen device!
Speak with your healthcare team about the other equipment you use, and make sure you are reaping the benefits of the medications and other management tools in your COPD treatment routine!

