
Caregivers are either naturally selfless people or they becomes selfless as their role of a caregiver develops. Caregivers take on a difficult job that often requires sacrifice in order to care for their loved one. This article is for you, the caregivers out there who need some advice about how they can continue to care for their loved one, but also take care of themselves.
It is so important for you to take care of yourself because only when you first help yourself can you effectively help others. Caring for yourself is one of the most important—and one of the most often forgotten—things you can do as a caregiver. When your needs are taken care of, the person you care for will benefit, too.
We hope that the caregiver and the patient can read this article together and find helpful ways to work through their difficulties managing and treating COPD together.
What is COPD
The first thing you must do is to understand what Chronic Obstructive Pulmonary Disease is, and there are three main forms of COPD:
- Chronic bronchitis, which involves a long-term cough with mucus
- Emphysema, which involves damage to the lungs over time
- Some patients have both conditions listed above
All of which make it hard for the COPD patient to breath because their airways become inflamed, damaged, and restricted by excess mucus. This causes a number of other issues throughout their body across all of their systems. With lack of oxygen comes low blood saturation levels, bone decay, added stress on the circulatory system, and a list of other complications.
COPD is treatable, and people can live with this disease for many years despite how severe it gets. There are ways to learn how to manage the disease and even slow down the progression of COPD. It requires a strict treatment plan that the COPD patient and their caregivers can develop with their doctor. Actually executing this treatment is the hard part, and where the caregivers role is essential.
So let's talk about our caregivers.
Being a caregiver
-jpg.jpeg)
There are over 40 million families worldwide in the caregiver role for a spouse, parent, friend, or other loved one, no matter the circumstance this is no easy task but it is an important one. It should not be taken lightly! Both the patients and the caregivers are in a hard position where intense lifestyle changes and everyday norms are flipped upside down.
If the patient has a condition like COPD, the caregiver's role likely evolved over time once their symptoms started progressing and through the diagnosing process, rather than a sudden change like an accident where a patient was healthy one day and hurt the next.
Because COPD is a progressive disease meaning it gets worse over time, both the caregiver and the patient will go through different stages of the disease together changing and altering everyday activities to adjust to a more comfortable lifestyle.
As a COPD caregiver, your main focus will inevitably be your loved one. However, your own health and well-being is important for you and the one you are caring for. This means remembering to take care of your own needs. As we mentioned above, this is not an easy job, and it is easy to feel overwhelmed.

Here are some tips for taking care of yourself as a caregiver:
Some of the most common impacts caregiver experiences are listed below:
- Sleep deprivation
- Poor eating habits
- Failure to exercise
- Failure to stay in bed when ill
- Postponement of or failure to make medical appointments for themselves
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
If you experience any of these lifestyle changes as a caregiver it is important to find tips for managing and adjusting your habits in order to live a more productive and happier life.
Here are some tips you can focus on. These tips were developed to help you get into a sleep scheduled, eat healthier foods, exercise more regularly, taking care of yourself when sick, and to remind you that you should make medical appointments for yourself when necessary.
Tip #1 Reducing stress

Caregivers are under a lot of stress all day long everyday, one of the best easy to avoid feeling stressed is to adjust to a strict sleeping schedule. Studies show the effects of sleep deprivation are related to a person's exposure to severe environmental and operational stress and negatively impacts their cognitive performance. This particular study sourced from Springer Link explains the results of a study that sleep deprivation and environmental stress adversely affects a person’s performance and mood.
You can also work to recognize stress warning signs early. This means realizing your irritability, sleep problems, and forgetfulness early on so it doesn't get worse. You can learn how to recognize your own warning signs, and be capable of making effective changes. Donʼt wait until you are overwhelmed.
You can also begin to identify the sources of your stress. Ask yourself, “What is causing stress for me?”
Sources of stress might include:
- you have too much to do
- family disagreements
- feelings of inadequacy
- the inability to say no
After you can put a source to your stressful feelings identify what you can and cannot change.
Remember, we can only change ourselves and our own behavior, and someone else’s actions are out of our control. When your focus is wrongly adjusted on things you cannot change or control, you will only increase your sense of frustration.
Ask yourself, “What do I have some control over? What can I change?” and even if you can only make a small change, this can make a big difference.
The last thing is to take action. These types of active decisions to reduce stress gives you back a sense of control that you deeply need. Stress reducers can be simple activities:
- Walking
- Other forms of exercise
- Gardening
- Meditation
- Having coffee with a friend
- Identify some other stress reducers that work for you
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Tip #2: Set goals for yourself
You can set a variety of goals all having different timelines, and it's a great way to stay in check with what matters to you.
Some goals you might try to set are:
- Taking a break from caregiving
- Get help with caregiving tasks like bathing and preparing meals
- Engage in activities that will make you feel more healthy
You do not want to get overwhelmed with accomplishing too many goals at once. Instead focus on one of two so that you can work towards those ideas productively.
The next step is to make an action plan, you can do this by asking yourself, “What steps do I need to accomplish to reach my goal?’” Then you can determine which step you will take first, and when.
Here is an example of how to set and make a plan for accomplishing goals:

Tip #3 Finding a solution
Your priority as a caregiver has been to seek solutions for your patients to difficult situations. You also have to do this for yourself!
If there is an issue in your life, for insistence, you are not going to the doctor for your own check ups or you get out of bed while you are sick, you must start taking action to solve this.
Making active choices to change the situation at hand will encourage a positive attitude, also giving you more confidence in your abilities.
Tip #4 Find accurate information

COPD is not always genetic, and it most often caused by smoking or inhaling harmful irritates, therefore, you may have never known anyone with COPD in your life, so understanding this new disease as a caregiver, can come as quite a shock.
A quick google search isn’t always the best way to research aspects about COPD especially because COPD is not a one size fits all diagnosis. This means that whoever you are taking care of with COPD is very different than anyone else with the same diagnosis.
The first thing is creating a strict treatment plan with your doctor, as well as establishing a relationship with your doctor, physical therapist, pulmonary therapist, or other related health care professional. Your doctor will create a specific treatment plan for their COPD and how COPD affects your life. By establishing a relationship you will be able to call and ask questions, seek help, and advice, rather than guessing.
One of the most important parts about a patients COPD treatment regime is long term oxygen therapy. Oxygen therapy is used for COPD who’s oxygen saturation is 92% or below while breathing air. This means the patient has a low enough blood oxygen level, also known as dyspnea, to qualify for a long term oxygen prescription.
The most effective, modern, and cost effective option for long term oxygen therapy, is utilizing a portable oxygen concentrator. These devices are built to last a long time, and they are designed to be portable, and can even be taken on airplanes.
As a caregiver, it is important for you to be able to take time off, and rest.
If your loved one with COPD has their own portable oxygen concentrator, they will be able to take it with them alone to the store, or feel comfortable walking by themselves, because some units like the Caire Freestyle Comfort only weigh 5 pounds! This way if you need to take a break, you can ask for help.
.png)
It gives the person in your life with COPD a sense of independence from you (the caregiver) which is also a very motivating feeling for them!
Finding information about oxygen therapy can be very confusing, the first thing you should know is that not everyone with COPD needs oxygen therapy, only those who have very low blood oxygen levels. You could actually over-saturate your blood with oxygen, which has adverse consequences and can be very dangerous. This is the reason why you will need a written prescription from your doctor in order to buy a portable oxygen concentrator from a licensed distributor.

A reliable place you can speak with a respiratory specialist who knows how to connect any patient with the best portable oxygen concentrator of 2020 is at LPT Medical. You can reach out by phone 1(800)-946-1201 or by email at info@ltpmedical.com.
Tip #5 Effective communication
.jpg)
Being able to communicate as a caregiver is hugely important for yourself, and the one you are caring for. Being able to communicate in ways that are clear, assertive, and constructive, helps you to find the help and support you need.
Communicating is not the easiest thing, but here are some things you can practice to get better at it:
- Try to express your feelings using “I” messages rather than using “you” messages. For example saying “I am angry” rather than “You are making me angry” is much more productive and allows you to speak about your emotions without blaming the other person making them become defensive.
- Accept the emotions of others and respectfully take into consideration their point of view. Avoid intentionally hurting anyone’s feelings by violating their rights, you can do this by recognizing another person’s right to express their feelings.
- Be clear and direct with your words. Speak directly to the person. Do not expect the other person to know how you feel if you haven’t explained your emotions. There are no mind readers. When you are direct about what you need or feel, you are respecting the other person's opinion by directing the conversation in a productive manner. It also allows the other person to speak freely and openly about their emotions and the chances of reaching understanding are greater.
- Be a good listener. Listening is the most important aspect of communication.
Overview
Having COPD is a challenging diagnosis, it requires you to alter your daily lifestyle, break bad habits, and much more. With the help of a caregiver, to comfort and support you, you will be able to stick to a treatment regimen that is healthy and promotes an active lifestyle.
As a COPD patient it is important for you to work with your caregiver in times of hardship, and to frequently do things independently when you can. That means you might need to find innovative ways to do your own chores by carrying your own oxygen device. Even if you need a higher output of oxygen, the Respironics SimplyGO is the lightest pulse and continuous flow concentrator on the market, and give the oxygen user freedom and independence that is healthy for the caregiver and patient's relationship.
We hope all the caregivers and COPD patients can find a rhythm going through their day to day lives living with COPD. We hope these tips are helpful for the caregiver to continue to take care of themselves in order to be the best caregiver for their loved one.
Living with a chronic disease like COPD requires making a variety of changes and lifestyle adjustments. You have to pay extra attention to your overall health in order to keep your lungs and body in the best shape possible.
Of all the healthy habits you can pursue, eating a nutritious, wholesome diet is one of the most important and beneficial. It can also be one of the most challenging to commit to, because it requires you to give up some of the junk food and unhealthy snacks you enjoy.
Eating unhealthy foods isn't just bad for your metabolism or waistline, but can also increase your risk for a variety of conditions including diabetes and heart disease. If you have COPD, eating certain foods can even put strain on your lungs and make it more difficult to breathe.
That's why, in this article, we're going to help you get a jump start on a healthier diet by telling you about eleven foods you should avoid when you have COPD. We'll show you what foods to cut down on, what foods to cut out completely, and what foods you can eat as a healthy alternative to junk in your diet.
So, if you want to improve your diet and learn how to avoid foods that can exacerbate your COPD, this article is for you. You'll learn how your diet can affect your COPD symptoms, how to avoid hidden sources of sugar and salt, and how to start putting together a healthy COPD diet plan that works for you.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
The Foods You Eat Can Affect Your COPD
 |
| Image courtesy of FFCU. |
Many people with COPD and other lung diseases don't realize how much their eating habits can affect their disease and its symptoms. But the truth is that there are certain nutrients, and certain types of foods, that can have a noticeable affect on your lung function, energy levels, and how you feel.
When you have COPD, your lungs have to work extra hard to get enough oxygen to all the parts of your body that need it. Certain foods can actually make your lungs have to work even harder, which can make symptoms like breathlessness and fatigue significantly worse.
COPD symptoms are also affected by a variety of foods that can cause indigestion, bloating, or excess mucus production. Certain foods commonly cause gas, bloating, or heartburn, all of which can cause chest discomfort and make it more difficult to breathe. Increased mucus production can obstruct and narrow airways, which worsens COPD symptoms.
If you have COPD, it's important to understand the dietary factors that can exacerbate existing symptoms and affect your lungs' ability to work efficiently. If you know what foods to avoid, you can reduce your exposure to things that can hurt your lungs and start improving your diet for better overall health.
What You Need to Know About Carbohydrates and COPD
Carbohydrates are one of the most important nutrients to pay attention to if you have a lung disease like COPD. The relationship between carbohydrates and lung function is complicated, but it's vital for every COPD patient to be aware of.
First, you have to understand that there is a direct relationship between the foods we eat and gas exchange in the lungs. Gas exchange is, of course, the lung's main purpose: we exhale carbon dioxide gas and inhale oxygen gas.

Carbon dioxide gas is a waste product that comes from our bodies' metabolic processes, like breaking down food. One of the major purposes of our lungs is to get rid of this carbon dioxide waste by expelling it through our breath when we exhale.
The way our bodies work, carbon dioxide waste is a necessary result of turning food into energy that our muscles and organs can use. Everything we eat gets broken down into both nutrients and waste products, and the carbon dioxide waste always has to get processed by the lungs.
However, researchers have found that some foods create less carbon dioxide waste than others when your body breaks them down. This means that these foods create less work for the lungs, because they produce a smaller load of carbon dioxide for them to process.
 |
| . Image courtesy of herlitz pbs. |
Research also shows that eating foods with a heavier carbon dioxide load can actually make your COPD worse. This happens because the lungs have to work harder and use more energy to get rid of all that extra carbon dioxide.
If you have strong, healthy lungs, having excess carbon dioxide waste to get rid of is not usually a problem. However, if you suffer from COPD or another respiratory condition, it can have detrimental effects.
If you have COPD, excess carbon dioxide waste results in reduced lung function, which can cause a variety of COPD symptoms to get worse. It can make you feel extra breathlessness, chest discomfort, fatigue, and even increase your risk for exacerbations.
So, which foods create the most carbon dioxide, and which foods produce the least? According to researchers, the answer lies in the three main food groups: carbohydrates, fats, and proteins.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Carbohydrates Create the Most Carbon Dioxide Waste

Researcher has found that, of all the major food groups, carbohydrates produce the most carbon dioxide waste by far. Because of this, many doctors recommend that people with COPD avoid diets high in carbs and eat more fat and protein instead.
This aspect of a healthy COPD diet is not negligible, and may be more important than many people understand. A number of researchers have studied the direct effects of carbohydrates on people with COPD, and they've found that their effects on lung function are both significant and measurable.
According to one study, COPD patients who had a single high-carb drink had increased symptoms and reduced lung function afterward. Compared to patients that drank a high-fat drink containing the same number of calories, COPD patients who had the high-carb drink required more oxygen, couldn't walk as far, and had extra difficulty breathing during activity.
This suggests that the carbohydrate and fat content of the food you eat can have a huge effect on your lungs, COPD symptoms, and your ability to exercise. If you want to stay healthy and feel your best, you should always be mindful of the nutrient content of the meals you eat and limit the amount of high-carb foods you eat.
Damaged lungs often have enough difficulty meeting the body's basic respiration needs under even the most ideal circumstances. By avoiding carbohydrates and substituting healthy fats and protein instead, you can significantly reduce the amount of strain you put on your lungs and make it easier to breathe with COPD.
Fats and Proteins Have the Lowest Carbon Dioxide Load
Because of the detrimental effects of carbohydrates on lung function, research supports a COPD diet that's high in fat and protein and low in carbs. These foods create significantly less carbon dioxide waste, and are thus easier on the lungs.
Most doctors recommend that people with COPD eat foods with a lot of healthy fats, such as fish, nuts, and moderate amounts of dairy. This ensures that you get enough calories and nutrients to meet your energy needs while creating the least amount of carbon dioxide for your lungs to process.
You should talk to your doctor to work out a well-balanced high-fat, high-protein diet that you can follow. If you are able to stick to it and minimize the amount of carbohydrates you eat, you will likely find that you can breathe easier, exercise longer, and better manage your COPD.
Foods to Avoid if You Have COPD
Once you've talked to your doctor about what a healthy diet looks like for you, it's all up to you to find and prepare healthy foods that will meet your requirements and help keep your body strong. That's when knowing what foods are healthy and unhealthy and what foods to avoid comes in handy.
We've put together the following list to help you identify unhealthy foods in your diet, replace them with more nutritious alternatives, and make healthier choices at mealtime every day. So to kick start your journey to healthier living, here's eleven foods that you should avoid if you have COPD.
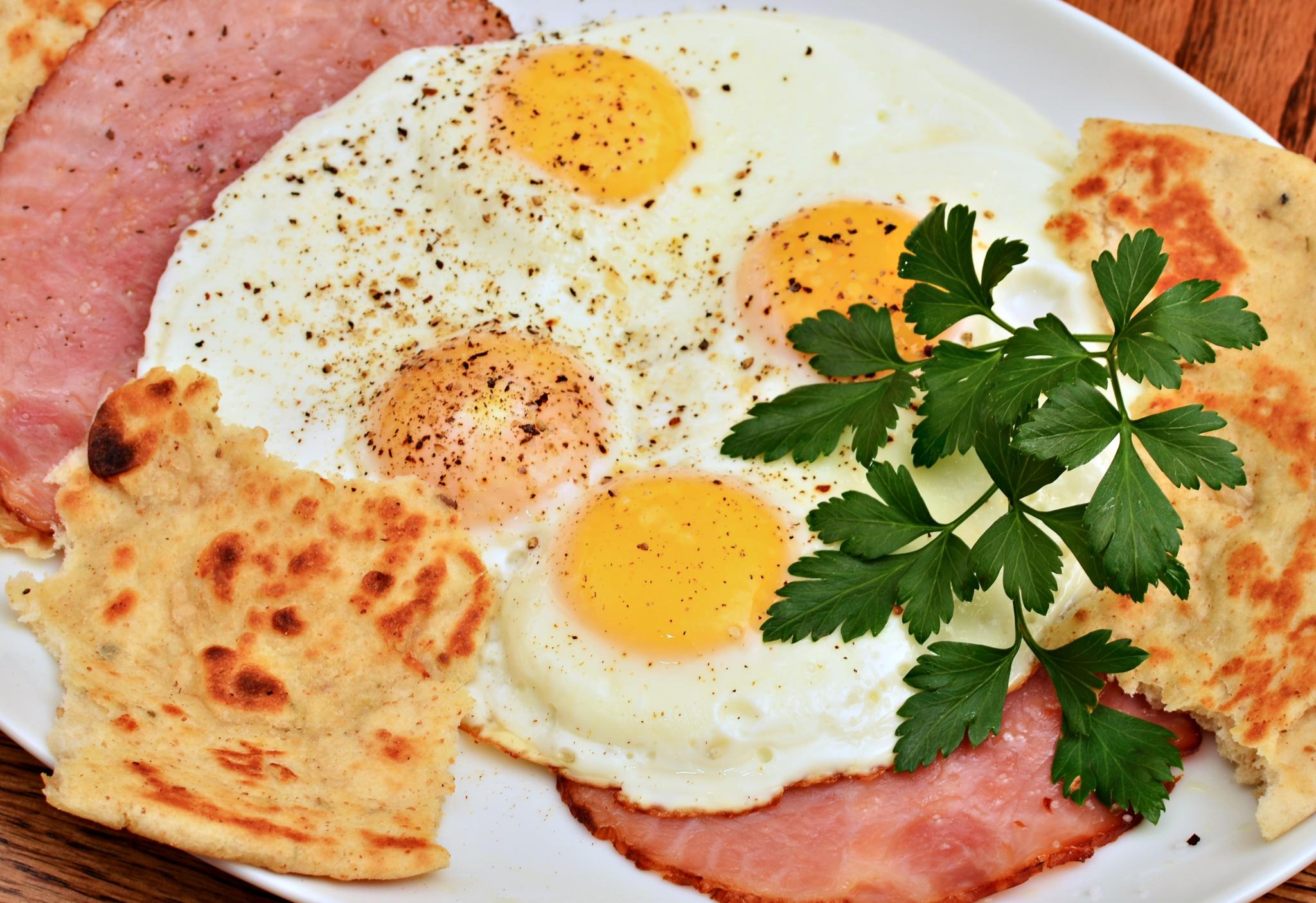
Avoid Processed Meats

Cured and processed meats, such as bacon and ham, are bad for you for a number of reasons. They contain loads of salt, plenty of saturated fat, and can even increase your risk for heart disease, diabetes, and certain types of cancer.
However, processed meats might be particularly dangerous for people who have COPD, according to recent research. Multiple studies have found a link between COPD patients who eat more cured meats and worsened lung function and increased exacerbations and hospitalizations.
Here is a list of cured and processed meats you should avoid:
- Bacon
- Ham
- Corned Beef
- Sausage
- Spam
- Deli Meats
Alternatives to Processed Meats

As an alternative to cured meats, try preparing fresh meats like shredded chicken or baked turkey to use in sandwiches and other dishes. For a quick and easy meat option, use packages of cooked shrimp or canned tuna, instead.
If you're used to packing a quick deli sandwich for lunch every day, you can reduce your processed meat intake by substituting some creative sandwich or salad options on some days, instead. You can experiment with different types of veggie sandwiches and wraps, tuna salad, egg sandwiches, and fruit sandwiches until you find an alternative you like.
Avoid Foods High in Salt

Image By David Dewitt: https://thecozycoffee.com/salt-in-coffee/
Getting too much salt in your diet is bad for your heart and also bad for your COPD. It can also make your body retain extra water, which can make it much more difficult and uncomfortable to breathe.
Even a single high-salt meal can cause bloating and make your COPD symptoms worse. Beware of broths (such as chicken and beef broths), frozen foods, and processed meats, which tend to contain an excessive amount of sodium.
Unfortunately, salt is hidden in a wide variety of everyday foods you wouldn't expect, which is why you should always check nutrition labels. Here are some common sources of excess sodium to avoid:
- Canned foods (including canned beans, vegetables, pastas, and soups)
- Frozen foods (including frozen TV dinners, frozen burritos, and frozen pizzas)
- Salted nuts
- Crackers and potato chips
- Many broths and soups
- Soy sauce and prepackaged marinades
- Instant puddings and baking mixes
- Condiments like mustard and ketchup (in large quantities)
- Pickled vegetables (like olives and pickles)
- Processed cheeses, cheese sauces, and spreads
- Many breads, biscuits, and bread mixes (like pancake mixes, waffle mixes, and Bisquick)
- Canned tomato sauces, salsas, and pasta sauces
- Prepackaged box mixes (e.g. pasta mixes, au gratin potatoes, flavored rice dishes, stuffing mixes, etc.)
Alternatives to High-Salt Foods
Luckily, you can usually find low-sodium versions of many of your favorite foods if you look. You can get low-sodium broths, no-salt-added canned goods, and a variety of salt substitutes at most grocery stores.
Cooking your own meals from scratch at home, however, is the best way to avoid getting too much salt in your diet. When you make your own broths, soups, beans, and raw veggies, you have full control over the ingredients at every step. This makes it much easier to limit the amounts of salt, fat, and other unhealthy ingredients in your meals.
If you often add extra table salt to your food when you eat, try substituting other ingredients and spices, instead. Even though salt is a simple, cheap, and easy flavoring for food, you can make your food much healthier and even more delicious by using salt-free alternatives.
There are hundreds of different spices you can experiment and get creative with, and most are very inexpensive to buy. Try different combinations of flavorings like garlic, onion, paprika, ginger, and other spices, and you'll find that your food doesn't even need the extra salt at all!
Avoid Caffeinated Drinks

Caffeinated, carbonated beverages cause bloating and gas, and are usually overloaded with sugar. They tend to be high in calories, high in salt, and have next to zero nutritional value.
Additionally, caffeine on its own can be problematic for people who suffer from COPD. It increases your heart rate, blood pressure, and breathing rate, all of which puts extra strain on your lungs.
Because of this, caffeine can make it more difficult to breathe and control COPD symptoms like wheezing and fatigue. Doctors recommend that people with the disease limit their caffeine intake as much as possible, especially if it causes their symptoms to get worse.
Alternatives to Caffeinated Drinks

If you're a soda, coffee, or caffeine addict, it can be difficult to quit cold turkey. Caffeine can have very unpleasant withdrawal symptoms, too, including irritability, anxiety, headaches, and fatigue.
It's often easier to cut down or eliminate caffeinated drinks when you do it gradually and replace them with healthier, non-caffeinated alternatives. Try cutting down on your caffeine intake by drinking one less cup per day or per week, that way you have time to adjust and build a healthier habit in the meantime.
Here are some healthy alternatives to caffeinated drinks:
- Fruit- and herb-infused water
- Decaffeinated coffee
- Decaffeinated tea
- Green juices
- Lemon water
- Low-sugar fruit juices (in moderation, ideally with pulp, or diluted with soda water)
Avoid Fried Foods

Despite being a universal favorite, fried foods are some of the most unhealthy foods you can eat. They are chock full empty calories and loaded with large amounts of added oil and fat.
Eating fried foods is bad for COPD because it can give you gas, make you bloated, and make it even more difficult and uncomfortable to breathe. They are also extremely calorie-dense and can make it more difficult to stay at a healthy weight.
You should try to cut fried foods out of your diet as much as possible to stay healthy and reduce your likelihood of experiencing worsened COPD symptoms. Instead, choose healthier baked and grilled options that are lower in fat and easier on your digestive tract.
Substitutes for Fried Foods
The best way to cut fried foods out of your diet is to avoid eating out at fast food restaurants and prepare most of your meals at home. If you do eat out, look for healthier baked or grilled menu items or opt for a light soup or salad instead.
It can be difficult to avoid fried foods like french fries and fried chicken if you're not prepared and don't have other substitutes ready. But you get a little creative, you can always find a healthier and equally delicious way to prepare the same foods that you love to eat fried.
Here are some healthier alternatives to substitute for fried foods in your diet:
Substitute fried meats and veggies for oven-baked, grilled, or steamed versions. This lowers the amount of calories and fat makes them less likely to cause stomach discomfort.
If you're addicted to fries and just can't give them up, try making your own homemade baked french fries from fresh potatoes in your oven at home. You can make them with much less salt and fat than the deep-fried versions at fast food restaurants have, or even use sweet potatoes for extra nutrients.
Avoid Sugary Foods

Sugary foods are difficult to stay away from, but it's worth putting in the effort to cut them out of your diet. Sugars are just empty calories with no real nutritional value, and eating a lot of sugary foods puts you at a greater risk for obesity, diabetes, and heart disease.
It's important to be aware that most processed and prepackaged foods contain a lot of added sugar, even if they aren't foods that you'd think of as being “sweet.” This includes most of the breads, boxed dinners, canned foods, fruit preserves and sauces you can find at the grocery store.
You should also look out for foods labeled as “low-fat” or “gluten-free,” because they are often no more nutritious than the regular version. Stripping the fat or gluten out of a food makes it bland and tasteless, and manufacturers often make up for this by loading their low-fat and gluten-free products with lots of added sugar.
To avoid all of these disguised sources of sugar, always check the nutritional label on the foods you buy. Avoid buying frozen, canned, and processed foods as much as possible and prepare your meals at home, instead.
Sugars are also a major source of refined carbohydrates, which put extra strain on your lungs an make COPD symptoms worse. It's important for people with the disease to limit carbohydrates in their diet, especially refined carbohydrates like sugar, white breads, and pastas.
Here are some common sources of sugar you should avoid:
- Refined carbohydrates (e.g. white breads, pastas, and crackers)
- Store-bought jellies, yogurt, sauces, and dressings
- Store-bought canned pasta sauces
- Breakfast cereals, flavored oatmeal, granola
- Canned soups and beans
- Sodas, fruit juices, sports drinks, coffee drinks, and flavored milk
- Canned fruits and dried fruits
- Many brands of nut butters
- Protein bars and cereal bars
Alternatives to Sugary Foods

Be wary of low-sugar foods that use low-calorie sugar substitutes like xylitol, mannitol, and sorbitol. These sugar alcohols are difficult to digest and cause many people to experience gas, bloating, and diarrhea when eaten in moderate amounts.
The best way to cut sugar out of your diet is to eliminate processed foods and prepare meals from whole ingredients at home. When you do your own cooking, you get to control all the ingredients that go into your food at every step, which makes it easy to cut down the amounts of salt, sugar, and other unhealthy additives.
Here are some common flavoring alternatives that are more nutritious than refined sugar:
- Honey
- Molasses
- Unsweetened applesauce
- Cinnamon
- Lemon or lime
- Fruits (e.g. use cranberries, lemons, blueberries, pureed bananas, etc. as substitutes for sugar in drinks, smoothies, muffins, and other dishes)
- Use milk or cream instead of sugar in your coffee or tea
- Dilute fruit juices with club soda to reduce calories and sugar
Avoid Alcohol (Especially Before Bed)

Alcohol is toxic on a basic level and is not very healthy for anyone to consume. However, if you have COPD, you should be especially careful about when and how much you drink alcoholic beverages.
You should try to limit your alcohol intake as much as possible, but especially at night. If you drink alcohol too close to bedtime, it can disrupt your sleep and even make it more difficult to breathe.
Because alcohol is a sedative, it can make the muscles in your throat to relax too much while you sleep. This narrows your airways and can cause them to collapse together, obstructing your ability to breathe.
Alternatives to Alcohol
If you're used to having a beer or a glass of wine before bed, try having it earlier in the day or replace it with a non-alcoholic alternative. A cup of water, decaffeinated tea, or a glass of warm milk are all soothing options that can help you relax without disrupting your breathing when you sleep.
Another option is to replace alcoholic drinks with non-alcoholic beer or virgin cocktails that mimic the taste. Here are some creative substitutes you can use use instead of liquor to make tasty mocktails at home:
- Vanilla extract instead of bourbon or scotch
- Almond extract instead of amaretto
- Apple juice, apple cider, or white grape juice instead of brandy
- Espresso, coffee syrup, or instant coffee instead of coffee liqueur
- Orange juice, apple juice, or pineapple juice instead of sherry
- Agave juice instead of tequila
- Apricot juice, peach juice, or pear juice instead of cognac
- Orange juice concentrate instead of curacao or triple sec
- Ginger ale or sparkling white grape juice instead of champagne
Foods You Might Need to Limit if You Have COPD
Regular physical activity is a vital part of keeping yourself healthy if you have COPD. Unfortunately, the very nature of the disease makes exercise more difficult, with fatigue and breathing difficulties being some of the major symptoms.
Because of this, doctors have long recommended pulmonary rehabilitation to COPD patients who have trouble staying active or getting enough exercise. Pulmonary rehabilitation classes are designed to help people with breathing disorders learn how to work out and stay healthy while keeping their symptoms under control.
Unfortunately, there are often not enough spaces in pulmonary rehabilitation programs to accommodate every patient who needs to attend. In fact, many patients in rural areas don't even have the option of attending pulmonary rehabilitation without driving many hours from where they live.
Another problem with pulmonary rehabilitation classes is the cost. One study found that the average patient has to pay more than $2,000 just to participate in a single group pulmonary rehabilitation class.
Because of this, many people with COPD and other respiratory diseases who could benefit from pulmonary rehabilitation classes have to do without, either because all the classes in their area are full, there are no nearby programs at all, or because they simply cannot afford the cost. However, researchers have begun identifying alternatives to pulmonary rehabilitation so that more patients with respiratory diseases like COPD can get the treatment they need.
For instance, certain exercise techniques, like Tai Chi and yoga, can be very effective for helping patients with COPD build their exercise tolerance and improve their symptoms. Patients often need help from trained instructors to learn how to exercise well, and attending these types of exercise classes can provide the structure and learning environment that people with COPD need.
While attending an actual pulmonary rehabilitation is still the ideal choice when possible, studies show that techniques like Tai Chi can be just as beneficial for improving your physical health. In this post, we'll introduce you to these techniques and show you how you can use them to improve your fitness, build up your exercise tolerance, and reduce your COPD symptoms.
Tai Chi for COPD

Tai Chi is a lesser-known type of exercise in western countries like the United States, but it has long been recommended to people with COPD for both its mental and physical benefits. It is an exercise style made up of many different “forms,” or poses and movement techniques, that focus on balance, muscle control, and breathing.
The origins of Tai Chi lie in ancient China, where it was originally used as a form of self defense. It is still used today, often as type of gentle, low-impact exercise meant to improve physical fitness and psychological health.
There are many different Tai Chi styles, each of which focuses on a different aspect of the technique. Some forms of Tai Chi emphasize physical strength, some emphasize martial arts, and others put more focus on the meditation and breathing aspects of Tai Chi.
Although Tai Chi is traditionally grounded in the Chinese philosophies of Qi and yin and yang, you don't have to understand or subscribe to these belief systems in order to practice the technique. The exercise techniques alone have been shown to confer a variety of health benefits, especially for people with age-related diseases.
What Makes Tai Chi Special

Tai Chi is considered a wonderful exercise technique for seniors and people with chronic diseases. This is because it uses slow, low-impact movements that are perfect for people with limited strength and physical mobility.
Sometimes described as “meditation in motion,” Tai Chi is known for its integrated mind-body techniques. The different Tai Chi forms are practiced using relaxed, fluid movements that don't stress your muscles and train you to focus on the sensations you feel in your body.
Tai Chi is made up of a variety of different forms, which are individual sets of movements and poses that make up the physical aspect of Tai Chi. Some forms are short and simple, requiring just a few discrete movements at a time, while some are longer and more complex.
Just about anyone can practice Tai Chi, and the techniques can be modified for people with disabilities or people with limited strength and endurance. However, its focus on mindfulness and breathing makes it particularly helpful for people with respiratory diseases like COPD.

Tai Chi not only helps you stretch and tone your muscles, but it teaches you how to manage your thoughts and breathing as you exercise. This makes it a perfect exercise for COPD patients who have trouble exercising without experiencing breathlessness and fatigue learn how to better control their breathing and exercise more effectively.
You can also use the breathing and relaxation techniques you learn from Tai Chi in a variety of circumstances outside of Tai Chi practice. It can help you calm yourself when you feel anxious, steady your breathing when you feel short of breath, and translate the breathing techniques you've learned to other physical activities to reduce your symptoms and increase your endurance.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Studies on Tai Chi and COPD

Health researchers have long been interested in Tai Chi as a form of exercise to improve strength and overall health. More recently, a number of studies have looked at the potential of Tai Chi as a treatment for COPD and come up with encouraging results.
One of the most recent studies, which was published in the journal Chest, found that patients who practiced Tai Chi for twelve weeks showed improvements in muscle strength, respiratory symptoms, and their ability to exercise without feeling breathless. What's more, the patients who did Tai Chi saw just as much improvement, if not more improvement, than patients who attended a standard pulmonary rehabilitation program for the same length of time.
The participants in this particular study used a type of Tai Chi known as the 24-form Yang style, which they practiced for five hours total every week. However, other forms of Tai Chi are also effective, as an academic review of the research on Tai Chi for COPD shows.
A Cochrane review looked at a number of studies on Tai Chi and COPD and found that Tai Chi was just as effective at reducing shortness of breath as standard COPD treatments. And although the evidence for this was not conclusive, the studies also appeared to reveal a slight advantage of Tai Chi over typical treatments, with participants who practiced Tai Chi having slightly better lung function and being able to walk further without feeling too short of breath.

The Cochrane review also found that there were no negative side effects or adverse events from practicing Tai Chi in any of the studies they reviewed. They concluded that “Tai Chi is safe to practice in people with COPD,” although it's still always best to check with your doctor before you starting any new exercise routine.
The American Lung Association also recommends Tai Chi as a form of light exercise and a way to reduce the psychological and emotional stress that many people with COPD suffer. They encourage patients who experience chronic anxiety, fatigue, or frequent COPD symptom flare-ups to try Tai Chi as a way to improve their physical and mental well-being.
Here is a quick run-down of all the major benefits you can get from practicing Tai Chi:
Benefits of Tai Chi
- Teaches you how to regulate your breathing while exercising and doing physical activities
- Puts minimal strain on muscles and joints
- Helps you minimize shortness of breath when you walk and work out
- Can improve your lung function
- Reduces stress and anxiety
- Improves mood and energy
- Improves exercise endurance
- Increases muscle strength and tone
- Increases balance and flexibility
Practicing Tai Chi

If you're interested in trying Tai Chi yourself, the best way to do it is to join a group Tai Chi class. While it is certainly possible to learn and practice it on your own, the help and skill you can gain from having an actual Tai Chi instructor is indispensable.
One of the major benefits of learning Tai Chi in a class is that it gives you the opportunity to get in-person feedback and encouragement. Your instructor can answer your questions, help you learn difficult movements, and correct your form so you learn the proper techniques.
Then, once you've built up your skills to a comfortable level, you will be able to practice Tai Chi effectively on your own. There are even many Tai Chi exercise DVD's and online instructional videos that you can use to and follow along with at home.
As you look around for classes and instructional videos, it helps to know which of the Tai Chi styles you'd like to learn. There are five styles total, but two of them—the Chen style and the Yang style—are the major parent styles from which all the other styles of Tai Chi are derived.
Here's a quick breakdown of the differences between these two main styles to help you as you seek out resources for learning Tai Chi.
The Two Major Tai Chi Styles:
- Chen Style: This is the oldest style of Tai Chi, which is often considered the most difficult. It combines quick, powerful movements along with slow ones and tends to require more strength and skill than other styles.
- Yang Style: This is the most popular form of Tai Chi today and it is practiced as a form of low-impact exercise all across the world. This style uses only slow, flowing movements and is known for its relaxing effects. The 24-form Yang style is a version of this style that uses simpler movements and is more accessible to people with chronic diseases and disabilities.
If you are not familiar with Tai Chi or have limited strength and mobility, you may want to start with the simpler, 24-form yang style. This is the style used in one of the more recent studies on Tai Chi and COPD and is also one of the most common forms practiced in the West.
According to research on Tai Chi and COPD, you should start to see results after about four months of taking classes and practicing at home. Then, if you find that it works well for you, you can continue to use Tai Chi as part of your regular exercise regimen to improve your COPD.
Examples of Tai Chi Forms for COPD

If you think you might be interested in trying Tai Chi, it can help to get a better idea of what it looks like in practice. Here are a few examples of some common Tai Chi movements along with videos to show you how they are done.
Holding Up the Sky
This is one of the most popular Tai Chi forms that is practiced all across the world, and it is a great exercise for beginners. It helps you consciously control your breathing rhythm and put it in sync with your body's movements.
Closing Posture
This form is a great cool-down exercise that can help you relax and steady your breathing. It can also be a great meditative exercise for reducing stress and anxiety.
Windmill Exercise
This Tai Chi form is a slow, relaxing exercise that stretches and tones the muscles in your arms, shoulders, and chest. It can also help you work on your breathing rhythm and open up your chest cavity to give your lungs more room to expand.
Yoga for COPD

Yoga is another form of exercise that studies show can help COPD patients improve their symptoms and their ability to exercise. Similar to Tai Chi, yoga is a thousand-year-old discipline that uses breathing and meditation practices along with low-impact physical activity as an essential part of its practice.
Yoga originally came from India and is made up of two main “pillars”: asana and pranayama. Asanas are the body postures or poses that make up the physical exercise portion of yoga, while pranayama is the deliberate practice of controlling and regulating your breathing.
When most people think of yoga, they think of the asana portion and familiar poses such as “downward facing dog” or the “tree” pose. These poses and the slow, fluid movements you use to transition between them are powerful, yet low-impact exercises that can help you build balance, strength, and muscle control.
However, true yoga practice encompasses much more than the body postures and the flowing movements you use to transition between them. Traditionally, yoga is meant to be a whole-body wellness discipline that promotes mental, emotional, and physical wellbeing.
What Makes Yoga Special?

Yoga is a fantastic exercise for COPD patients because it low-impact, slow-paced, and teaches you how to better control your breathing. Other things that make yoga unique are its mental and meditative practices, which are interwoven with the postures (asanas) and breathing techniques (pranayamas).
The wonderful thing about yoga is that it is accessible to just about anyone, even the elderly and people with chronic illnesses and pain. The different poses, or asanas, are generally simple to perform, and the more advanced positions can be modified for lower strength and skill levels.
The slow, steady movements make most yoga routines easy for people with breathing difficulties to follow without feeling short of breath. However, despite the fact that it is a slow, low-impact exercise, yoga still confers many physical benefits, including better muscle tone, respiration, and cardiovascular health.
image credit: Ryderwear
The different yoga asanas work out a variety of different muscle groups in your arms, legs, shoulders, back, and core, helping you strengthen your body and improve your balance and flexibility. Some studies even show it can help with chronic pain and cardiovascular disease, afflictions that commonly affect people with COPD.
Pranayamas, on the other hand, are meant to help you observe, control, and extend your breaths in time with your movements, and is one of the major features of the exercise that makes it so useful for people with COPD. Being able to regulate and control the rhythm of your breathing is an important skill that can help patients with breathing disorders strengthen their breathing muscles and reduce shortness of breath.
The mental and emotional aspects of yoga are also represented by pranayama, which trains you to calm your mind and body through deep breathing and meditation. Yogic breathing teaches you to focus your mind on your breaths and bodily sensations and get rid of unnecessary thoughts.
Because of this, yogic breathing is a tool that you can use and practice anywhere to reduce anxiety, clear your mind, and steady your breathing. Whenever your mind feels cluttered with negative thoughts and emotions, or you feel anxious or stressed out, you can use the skills you've built through yogic breathing to relax your body and calm your mind.
Studies on Yoga and COPD

Research on yoga as a potential treatment for a variety of diseases has increased in recent years as the practice has become more popular in western societies. As part of this new wave of interest, several studies have been done to evaluate yoga as a potential treatment for COPD, with very positive results.
The meditative and breathing aspects of yoga, in particular, have been shown to help patients with COPD breathe easier and more efficiently while they exercise. One study, published in the Journal of Cardiopulmonary Rehabilitation and Prevention, found that patients were able breathe more slowly and deeply during yoga lessons.
The most promising result, however, was that patients actually showed improvements in their blood oxygen saturation levels during the yoga sessions. This indicates that yogic breathing could not only help patients control and regulate their breaths, but can also improve their overall breathing and respiration efficiency.
Another study found that practicing pranayama (yogic breathing) alone yielded positive results in patients with COPD. Compared to a control group, who only received pranayama education, those who actually practiced pranayama with trained coordinators showed minor improvements in their walking endurance and lung function measures.

Additionally, yoga as an exercise seems to be particularly suited for people with respiratory diseases like COPD who tend to find other exercises tiring and difficult to do without experiencing shortness of breath. Because of this, some researchers even think that yoga could be an effective alternative to pulmonary rehabilitation. Most agree, at the very least, that the practice represents a “tremendous opportunity” for patients with COPD.
One academic review that looked at a variety of different studies on yoga and COPD concluded that, although the evidence was limited, it all points to the encouraging conclusion that yoga training can improve both lung function and exercise capacity in people with COPD. In the future, researchers hope to develop custom yoga programs that are designed specifically to help people with breathing disorders improve their respiration and overall physical health.
Although most of these are still early studies, they show the real-world potential of yoga and yogic breathing as a tool to treat respiratory disorders like COPD. More research is needed to better understand the effects of yoga and whether or not it is an effective replacement for pulmonary rehabilitation, but for now it seems to be a safe and promising option for patients.
Here is a quick run-down of some of the major benefits you can gain from practicing yoga:
Benefits of Yoga
- Improved lung function
- Improved muscle tone
- Improved balance
- Improved core strength
- Improved range of motion
- Reduced anxiety
- Lower blood pressure
- Increased ability to relax and reduce stress
- Improved quality of life
Practicing Yoga
If you have difficulty exercising and experience frequent shortness of breath, practicing yoga can be an effective way to improve your symptoms and exercise endurance. Especially if you are unable to participate a pulmonary rehabilitation program, finding a reputable yoga class could help you achieve many of the same benefits.
By far the best way to practice yoga is by joining a class led by an experienced practitioner. Even better would be to join a yoga program designed specifically for people with breathing disorders or COPD if there are any options in your local area.
Either way, it's best to start with a group class before attempting to do yoga on your own at home. There's no substitute for in-person instruction; it helps you ensure that you're using the correct posture and positions and allows you to master techniques at a level you couldn't reach without feedback from a skilled practitioner.
Pranayama, in particular, is often considered an advanced technique that most people cannot master without proper instruction. However, once you've become confident in your skill, you should be able to reap many of the same benefits of yoga by practicing it at home.
Some people find that taking regular yoga classes is more fun and effective than doing it alone, and continue to take classes even after they've learned the basics. In most places, you can find many different types of yoga classes with different styles and skill levels, so that anyone can find a yoga class they can learn from, whether they're a beginner or advanced.
If you finish taking a yoga class and decide to give it a go on your own, there are thousands of resources you can use to help you practice yoga at home. You can find plenty of instructional DVD's, YouTube videos, and books that can help you hone your technique an
.png)
In this day and age, it’s becoming increasingly more difficult for people to pay their medical bills. Whether it’s a simple visit to the doctor’s office or a major medical procedure, most people have no idea where they’ll be financially after everything is said and done. And there’s certainly no exception when it comes to purchasing oxygen therapy devices like home oxygen concentrators, portable oxygen concentrators, or CPAP and BiPAP machines.
Usually, the first thing people ask when they contact an oxygen concentrator company is, “are portable oxygen concentrators covered by Medicare?” Although you can seek reimbursement for oxygen equipment from Medicare, it’s important to note that they won’t always accept your claims. Unfortunately, as important as oxygen therapy devices are in people’s lives, insurance companies often see them as “luxury items.”
On the other hand, private health insurance company policies vary widely, so you’ll need to get in touch with them to see how it works. However, even when they do cover oxygen therapy devices, you often need to be covered by a specific plan or meet a set of criteria before they will help pay for it.
It’s important to know exactly what your options are when it comes to purchasing an oxygen concentrator or a similar oxygen therapy device so that you can save as much money as possible and don’t end up with the short end of the stick. In the following sections, we’ll outline all you need to know about medicare, private health insurance, and purchasing an oxygen therapy device. Follow the links below to skip to relevant sections of the post.
- Health insurance terms
- Does Medicare cover oxygen equipment?
- Filing a claim for out-of-pocket expenses
- Saving money on oxygen equipment
- Conclusion
Health Insurance Terms You Should Know

Before you get started with purchasing an oxygen therapy device, there are several terms that you need to become acquainted with that will help you out when filing a claim with your health insurance company. Although it’s pretty straightforward for the most part, Medicare and private health insurance companies may use different terms to describe the same concept.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
General Healthcare Terms
Deductible
A deductible is the amount that someone must pay for medical services or products before the insurance company will begin to pay for them. However, depending on your plan, there may be exceptions to this to cover things like preventative care.
Premium
The premium is the amount of money you are paying monthly, quarterly, or yearly in order to maintain your Medicare or private health insurance coverage. Be sure to check with your Medicare provider, private healthcare provider, or employer to learn about any increases in premiums.
Copayments
Copayments are fees that you pay for certain medical supplies or services. These are usually a set cost and can be used to pay for things like doctor’s visits. This should not be confused with coinsurance which is the percentage of a total payment you are required to pay after a deductible is met.
Oxygen Equipment Terms
Durable Medical Equipment (DME)
Durable medical equipment is the term that most companies use to describe long lasting and reusable medical equipment that allows an individual to function on a day-to-day basis. This includes mobility aids like walkers, wheelchairs, and handrails, as well as electrical items including scooters, ventilators and nebulizers, blood and glucose monitors, oxygen concentrators, and CPAP machines. Terms like home medical equipment (HME) and healthcare equipment are often used interchangeably with DME.
DMEPOS
This is an acronym that’s only used by Medicare and stands for Durable Medical Equipment, Prosthetics, Orthotics, and Supplies. Although this is a broader term that incorporates more medical supplies, it’s effectively the same thing if you’re just in the market for an oxygen concentrator.
Home Medical Supplies
Although “home medical supplies” sounds an awful lot like “home medical equipment,” this term usually refers to single use disposable items such as diabetes test strips and other incontinence supplies.
Assistive Technology (AT)
The term “assistive technology” is commonly used by the independent living community but describes essentially the same thing as durable medical equipment. According to the Assistive Technology Act of 1998, assistive technology is:
“any item, piece of equipment, or product system, whether acquired commercially, modified, or customized, that is used to increase, maintain, or improve functional capabilities of individuals with disabilities.”
Does Medicare Cover Oxygen Equipment?
Medicare does cover oxygen equipment as long as certain criteria are met. Since oxygen equipment is considered “durable medical equipment,” it’s covered under Part B of medicare. However, even after all criteria are met, you will still be paying for a portion of the device that you’re purchasing or renting.
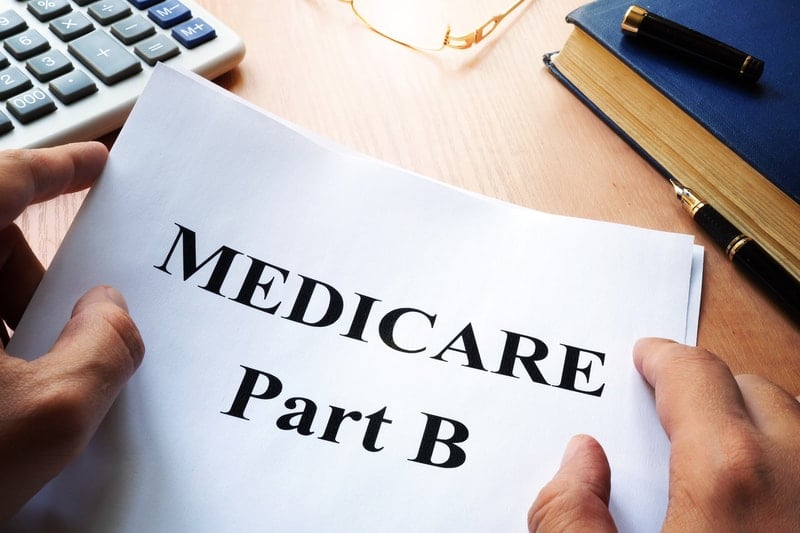
Like with any type of insurance, Medicare will find any excuse they can to deny you coverage, so it’s important to be meticulous in the way that you approach seeking reimbursement for your medical purchases — simply contacting a Medicare provider and asking them to pay you will never work.
Generally, in order to seek reimbursement for oxygen equipment, you will need a medical report that shows you need supplemental oxygen to treat a condition or to maintain healthy blood oxygen levels. Remember that the more documents you have showing your need for supplemental oxygen, the less likely you are to be turned down for financial reimbursement.
Once you reach your deductible, Medicare will pay for 80 percent of the Medicare-approved amount and you will pay the remaining 20 percent out of pocket. The Medicare-approved amount is the sum of money that Medicare agrees to pay a provider for medical items or services.
Medicare will help pay for oxygen equipment and supplies when the following conditions are met:
- Your health will improve with oxygen therapy
- Your arterial blood gas levels are low
- Alternative treatment measures have failed
- Your doctor has confirmed that you have a severe lung disease like COPD, asthma, or pneumonia.
What’s more, your doctor will need to write and sign something called a certificate of medical necessity (CMN) or DME Information Form (DIF). This form helps to document the necessity and coverage criteria for DMEPOS items. Your supplier will need this document before a claim can be submitted for Medicare.
When these criteria are met, Medicare will pay for the following:
- Systems that provide oxygen
- Containers for storing oxygen
-
Oxygen contents and accessories used to deliver oxygen such as tubing and cannulae
Is Every Type of DME Covered Under Part B?
Unfortunately, the catch that many people don’t realize at first is that just because Medicare will help you pay for oxygen supplies doesn’t necessarily mean they will pay you for the one you want. There are a lot of different types of oxygen devices on the market including oxygen tanks, portable liquid oxygen tanks, oxygen concentrators, portable oxygen concentrators, and CPAP and BiPAP machines.
Although every health insurance company is different, most tend to only offer reimbursement for the bare minimum. While oxygen therapy has constantly been evolving over the years, providing patients with more effective portable oxygen devices, Medicare and many private companies will likely only pay for oxygen tanks. However, if certain criteria are met, you may be able to receive an oxygen concentrator on an extended rental basis.
Renting Oxygen Equipment
If your doctor determines that you need a more advanced oxygen therapy device like a portable or home oxygen concentrator and provides adequate documentation, Medicare will enter into a contract with your medicare-approved provider. This contract will allow you to rent an oxygen concentrator for 36 months until the contract needs to be renewed with updated medical information.
It’s very unlikely that Medicare will help you pay for a portable oxygen concentrator but if your condition is severe enough, you may be able to get a home oxygen concentrator. Monthly payments made by Medicare will help pay for things like oxygen machine maintenance, servicing, repairs, as well as accessories like cannulae and oxygen contents.
Steps To Filing a Claim For Out-of-Pocket Expenses
In many cases, your medical equipment provider will file a claim on your behalf as long as they have the necessary documentation and information. However, if for some reason they aren’t able to, you will need to know the steps to filing a claim whether it’s through Medicare or a private health insurance company. You should file your claim within a year of the date that you paid for the medical expenses out of pocket to ensure that you’re reimbursed in full.
Download and Fill Out the Patient Request Form
In order to get started filing your claim for out-of-pocket expenses, you need to fill out the Patient Request for Medical Payment form found here. This form is updated regularly, so it’s important to check back with Medicare.gov for the most up-to-date version. If you’re filing a claim with a private health insurance company, be sure to visit their site for the appropriate form.

With the claim, you’ll also need to provide the itemized bill from your healthcare provider, doctor, or supplier, a letter detailing your reason for submitting the claim, and any other supporting documents.
Submit Your Form
Medicare and most insurance companies will allow you to fax your information or send it by mail, but it’s important that you check on the form to ensure you’re sending it to the correct location. If it’s sent to the wrong location it may delay the process or it may never get into the hands that it needs to in order to be processed.
Track Your Claim
If you’d like updates on your claim, most health insurance companies have a way of tracking it through their website. If not, you can contact member services if you have any questions about your documents or reimbursement. Reimbursement time is usually around 30 days but it can vary.
Healthcare Common Procedure Coding System (HCPCS)
HCPCS is the coding system used by all healthcare companies including Medicare. These codes are used to classify every single task, service, or item that you may receive from a healthcare practitioner or supplier. These are updated regularly so be sure to check online and make sure the correct codes correspond with the ones on your invoice and your claim.
How To Save Money On Oxygen Equipment
If for some reason Medicare or your private health insurance doesn’t help you pay for your new oxygen therapy device, there are many other options available to you. Unfortunately, many insurance companies will exhaust all their available options to prevent your from getting the products or services you need for an affordable price. And nobody should have to feel like they’re putting a strain on their financial well-being, especially with something that concerns your physical health.
Take Advantage of Financing Options
Exploring your financing options is one great way to reduce the financial burden when paying for a home oxygen concentrator, portable oxygen concentrator, or CPAP machine. If you know which oxygen machine you want but aren’t able to pay for it upfront, you can split your payments into smaller and more manageable monthly payments.

Please note, however, that if you choose to finance your oxygen device, you will need to have your credit approved beforehand. If your credit is declined, you can always finance through a family member or friend who has good credit.
Buy from the Right Company
Although it may be tempting to go on Amazon or eBay and purchase the first oxygen concentrator you find, this is never ideal and can put you in a bad situation financially if the device malfunctions and you have no warranty or no one to speak to about getting it fixed.
On the other hand, buying directly from the manufacturer may mean paying higher prices for the oxygen concentrator that you want. Fortunately, distributors like LPT Medical offer such low prices that the manufacturers won’t allow us to advertise our best prices. Speak with a respiratory specialist to learn more about our pricing.
Consider Second Hand Oxygen Concentrators
Buying a used oxygen concentrator can save you a significant amount of money and can be an effective means of getting the exact device that you set out to buy without breaking the bank. Lightly used or second hand oxygen concentrators, especially those from reputable brands like Inogen and Philips Respironics are known to last a long time. The good news is that when newer oxygen concentrator models release, there’s often an influx of used machines in stock that you can choose from.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Conclusion
Medicare and private health insurance companies often make it difficult or impossible to get the funds you need to pay for an oxygen concentrator. Although they’ll typically pay for the bare minimum such as an oxygen tank or portable oxygen tank, this may not be what you want or need.
Portable oxygen concentrators, on the other hand, afford you the mobility and assurance you need to live life to the fullest without anything holding you back. It’s our primary goal to help you achieve this by offering you plenty of options to make paying for a portable oxygen concentrator more affordable, convenient, and reasonable.
Give us a call at 1-800-946-1201 or reach us by email at info@lptmedical.com if you have any questions about Medicare, financing options, or pricing.
We created another holiday blog from LPT Medical, and this one's dedicated to all of the oxygen patients out there! After writing a blog about 2020 holiday gift ideas for people with COPD we decided that we also wanted to create a blog specifically for respiratory patients that utilize supplemental oxygen therapy.
If you are unfamiliar with supplemental oxygen therapy, it is a life saving treatment for people who have hypoxemia, which ultimately means they have very low blood saturation levels. Hypoxemia can be cause for concern because low oxygen levels can cause complications in body tissue and organs. Normally, a PaO2 reading below 80 mm Hg or a pulse ox (SpO2) below 95 percent is considered low, and in these cases, people will normally be prescribed long-term oxygen therapy.
.jpg)
Ultimately, oxygen therapy is prescribed to people who can’t get enough oxygen on their own. Lung conditions are the main causes that prevents the lungs from absorbing oxygen, including:
- Chronic obstructive pulmonary disease (COPD)
- Pneumonia
- Asthma
- Heart failure
- Cystic fibrosis
- Sleep apnea
- Lung disease
- Trauma to the respiratory system
Depending on the severity of the lung condition, oxygen can be administer to slow the progression of chronic illnesses adding years to people's lives, and it also helps everyone who suffers from a lung condition live more active healthier lives.
There are a few ways that oxygen therapy can be administered to the oxygen user. These methods include:
- Oxygen in metal tanks
- Liquid oxygen
- Portable oxygen concentrator
- Home oxygen concentrator

Depending on which method your loved one uses, you can buy little gifts or plan on doing some helpful tasks that make thoughtful holiday gifts.
So, once you determine which type of oxygen device they have, come back to this article, you will find 19 gift ideas for your loved one who uses oxygen.
So let's get into it!
Gift Ideas for Someone on Oxygen

1. Gifting a POC to a loved one with an Oxygen tank
If you are unfamiliar with oxygen therapy products in Denver, CO, portable oxygen concentrators (POC) are the most modern and efficient form of oxygen delivery, over liquid oxygen and oxygen tanks. Portable oxygen concentrators are lightweight, run on a rechargeable battery, and you can take them on airplanes, unlike their counterparts- tanks and liquid oxygen, both are bulky and unsafe to take on a plane.

If your loved one still used an oxygen tank, but would qualify for a portable oxygen concentrator, there are a lot of benefits they could reap by switching from oxygen tanks to a portable oxygen concentrator. First and foremost, if they like to travel, having portable oxygen concentrators is much more reliable for extended periods of time and not having to re-fill the device is much more efficient for extended stays away from home.
There are two kinds of portable oxygen concentrators, one is a pulse flow and the other delivers continuous flow. The most popular pulse flow portable oxygen concentrators on the market are the Inogen One G4 and the Carie Freestyle Comfort. These are in high-demand because of the efficiency and lightweight designs. They are so easy to carry, either with the custom carrying case or in a backpack, but they also offer powerful pulse flow settings, and they can cover most oxygen patients' needs that need pulse dose oxygen flow, and even have some wiggle room should their oxygen prescription increase over time.

With all of this being said, not everyone qualifies for a POC, depending on their oxygen prescription a POC may not be able to fulfill their requirements, in which case they will use oxygen tanks that they have to get refilled bi-weekly.
The other reason people use oxygen tanks rather than POCs is due to the up-front cost associated with a POC. Even though POC are much cheaper in the long-term, because tanks have recurring costs, people shy away from the price tag even though they could be saving thousands of dollars over the course of their life.
Portable oxygen concentrator costs vary depending on the unit in question. There are a lot of products and brands making these oxygen devices, and it can get overwhelming and confusing. So we created a guide that will help narrow down your options and give you the most trusted names in oxygen therapy products.

With all of this in mind, you can discuss with your loved one the potential of upgrading from a tank to a portable oxygen concentrator. This is a wonderful opportunity to give your loved one the gift of freedom and independence, and it is something you can both do together. For more information about the process, purchasing options, warranties call a LPT Medical respiratory specialist at 1-888-416-3855.
Gift Ideas for a Loved One With a Portable Oxygen Concentrator
If you have a loved one with COPD or another lung disease that requires them to be on oxygen 24/7, their oxygen device is with them everyday all day, so the most obvious gift you can get them is something to make their portable oxygen concentrator even better!

A portable oxygen concentrator is a battery powered medical device that does require a doctor’s prescription when you buy from a licensed distributor. These machines are lightweight and dynamic, and can even be taken on airplanes, unlike oxygen tanks and canisters.
Here are some gift ideas that make having a portable oxygen concentrator even easier:
2. An Extra Battery
Oxygen tanks require refills, therefore a delivery company comes and refills empty tanks or replaces empty tanks with filled ones, at least once every two weeks depending on how much oxygen they need.

Every time oxygen is delivered it costs money and time. With a portable oxygen concentrator, all you have to do is charge the batteries!
The batteries can be charged while the user is resting and using the device. However, having an extra battery for a POC has a multitude of benefits. The first being, they can keep an extra battery on them, for extended trips away from home. This way, when their device is running low on battery, they can simply switch the dead battery with a fully charged battery, and they can stay out longer, worry free.
The extra battery is also great to have in the case of emergencies.
3. POC backpack
One of the best aspects of having a portable oxygen concentrator, is the ability to travel and move around so easily! Depending on the device your loved one has, they also likely have a custom carrying case that came with the device when they bought it!
While the custom carrying cases are great for some, backpacks can make caring for their POC along with their belongings even easier. Depending on which POC your loved one has, you can get the matching backpack so the device fits securely into its designated place.
Here are links to some of the Inogen models that are very popular among oxygen users:
Inogen One G3 Rolling Backpack by Portablez




Caire FreeStyle Comfort Backpack


4. GO2 Carry all Inogen One G3 Carrying Bag
The Inogen One G3 is a very popular oxygen device, and because it is an older model, many people still use their One G3, and many people are still buying new ones.

The GO2 Carryall Inogen One G3 bags combine the versatility and lightweight design of the custom carrying case with plenty of additional space for your car keys, wallet, cell phone, and your Inogen G3 accessories. That is not all, the G3 Carryalls are also very fashionable, and it looks more like a purse than a medical carrying case. You can get the carry bag in a black or brown color.
5. External battery charger
While their POC will come with one battery, and AC and DC charging cables, no device comes with an external battery charger. So if your loved one does not have an external charger, this makes a great holiday gift.
Rather than relying on an AC or DC power supply to keep the Inogen One G4 running, with the external chargers, it is easy to swap out a depleted battery for a recharged one at any time. The Inogen One G4 External Battery Charger plugs right into any wall outlet and can charge your single or double batteries quickly and safely.

This will allow you to make sure the battery in your Inogen One G4 is as fresh as possible at all times before you leave your home, and it will also allow you to take an extra battery with you when you're traveling so that you don't run out of power.
The benefits of having a external charger, rather than simply relying on the AC and DC power cords are as follows:
- Charge single and double batteries
- Charges faster than AC and DC power supply
- Indicator to see when your battery is fully charged
6. Larger battery

If your loved one has a POC they will have at least one battery, but with many POCs, there is the option to get the smaller battery or upgrade to a bigger longer-lasting battery. If they only have one small battery, purchasing a compatible larger battery could make a thoughtful holiday gift this year.
Depending on the device they have, you will want to make sure that you get the battery compatible with their device. Most pulse flow devices have the option to upgrade to a larger battery that can last almost twice as long, without having to be switched out or recharged.
You can find links to larger batteries for some of the most popular devices here:
Caire FreeStyle Comfort Large Battery
7. Thrive E- Learning Course

If your loved one did not purchase their oxygen device through LPT Medical, it is possible they weren’t offered this incredible educational course with the purchase of their oxygen device.
The Thrive E-Learning Course is an expert led, Pulmonary education course. Students learn the necessary knowledge and tools to slow chronic disease progression. Respiratory disease should not stop anyone from doing the things they love, this course helps individuals get back to an active and healthy lifestyle.
8. Air Purifier

Someone with COPD needs to breathe clean air as much as possible, this reduces symptoms and even helps to slow down the progression of COPD. So how do you get someone you love clean air in a world filled with wildfires, pollution, dust mites, and some many other irritates?
A high quality air filter is renowned for its ability to remove almost all airborne particles from the air indoors. Having an air filter can relieve allergy symptoms, improve sleep and help improve overall health, for people suffering from COPD an air filter is a wise decision to improve their quality of life not just within their own home, but it will improve their health and wellbeing so they can spend more time outdoors if they chose to.
9. Lung Health Meter
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Keeping track of one’s health is crucial for someone with COPD. Because this disease is chronic and progressive, it is very helpful for doctors and the pulmonary health team to have updated notes on how the disease has progressed since the last time visiting the doctor.
One of the most important tests when measuring respiratory health is the pulmonary function tests, which can be taken with a forced expiratory volume in one second (FEV1). A Lung Health Meter can store up to FEV1 240 readings, so tracking pulmonary health over time is easy.
10. Fingertip Pulse Oximeter

11. Ultra-Breathe Compact Breathing Exerciser
It might not be the first thing that comes to mind when you think about what a respiratory patient needs- but exercise is necessary to maintain good health and slow the progression of COPD. Regular exercise is crucial to maintaining respiratory health, yet finding a balanced exercise that challenges COPD patients without exhausting them can be difficult.
A compact breathing exerciser boosts respiratory performance and it is a great device for those who suffer from shortness of breath by providing breathing resistance that is easily adjustable for varying lung fitness levels.
12. Bike or Home Exercise Bike

As we mentioned before, exercising is crucial for anyone who is looking to improve their muscular strength and endurance, and this includes COPD patients who want to better their respiratory health. That being said, for people with COPD, it can be very challenging to exercise.
An exercise bike gives them the opportunity to work out their cardiovascular system from the comfort of their own homes. An exercise bike does not have to be a demanding work out and it is especially gentle on the joints compared to other workouts.
13. Walking Shoes

.A nice pair of walking shoes is a great gift for a person with COPD because walking is just about the single most important activity a person suffering from chronic lung illnesses can possibly do.
Even if they walk more indoors than outdoors, having a supportive walking shoe with good traction can help them feel motivated and confident to walk safely around their home or neighborhood.
14. COPD Healthy Cookbook and COPD guide books
There’s no known cure for COPD but there are things you can do to live and breathe better and eating healthy is one. Healthy COPD oriented cookbooks can help someone you love, live better with COPD.
When you can't breathe, nothing else matters, what might help is knowing that about 16 Million Americans suffer from COPD as well, and there are a lot of resources, including books, available with tips and tricks on how to manage this disease.
Helpful books about COPD can be about how it affects the patient’s breathing, books about the most up-to-date medication and treatment options, self-help books about how to track symptoms and medications. Books that give the reader breathing techniques to improve oxygen intake or strategies for healthy nutrition and gentle exercise. Or, books about what to eat and what to avoid, with lists of key COPD foods. Lastly, books with stories from others who also have COPD can help pass the time spent in quarantine, and remind them that they are not alone in this.
Free Gifts
15. Your Time

If there is one thing that respiratory patients and people with chronic illness value is time spent with their loved ones. Spending quality time, playing cards, watching a movie, or if you are socially distancing from you family members at this time, simply chatting over FaceTime or Zoom calls can make a big difference and qualifies for one of the best holiday gifts you could offer someone this year.
16. A Favor or Two

Accomplishing the most basic everyday tasks can be increasingly difficult for people who have a chronic lung condition. Work like gardening, cleaning the house, grocery shopping, and cooking take a lot of energy to accomplish and on top of doing the chores, having a hard time breathing on top of that, chores become nearly impossible. Offering to help with one or two of these tasks can make the holidays much more enjoyable, and if you get to spend quality time with that person, it's like two gifts in one.
17. Communication
A phone call, text, or email is a great way to receive love and caring from family members of people with lung conditions. It can truly make a day or even a week to hear from a loved one and know you are being thought of. Communication is so easy (and cheap) … why not make someone’s day with a quick note?
Other Little Gift Ideas

18. Roomba
The Roomba is a great gift for our friends and family that have a hard time vacuuming on their own. Vacuuming and pushing and pulling is too much for oxygen patients, especially if they also have to maneuver their oxygen tank around with them. Vacuuming can also bring up dust and allergy triggers that can induce a COPD exacerbation.
19. Wireless Earbuds
Wireless earbuds are a great gift for oxyg
Staying active is one of the most difficult, yet most important, things you can do to stay healthy with COPD. Regular exercise is not only beneficial for your disease, but it's absolutely necessary for your survival and maintaining a good quality of life.
The good news is that there are plenty of special techniques you can use, and activities you can do, to make exercising with COPD easier and more fun. With the right exercise routine and treatment plan, you can get all the physical activity you need to stay healthy without feeling breathless and fatigued.
Why Exercise is Important When You Have COPD

Regular exercise is necessary for a healthy lifestyle, whether you have a chronic disease or not. But when you have a serious respiratory disease like COPD, regular exercise is a necessity to prevent your disease from getting worse.
Physical activity is just as important for your heart, lungs, and muscles as it is for your psychological and emotional health. It gives you strength, energy, confidence, and is a great mood-lifter, too.
Although you might feel breathless easily when you first start out, regular exercise can actually strengthen your breathing muscles and make it easier to breathe in the long run. Also, getting out your energy through physical activity during the day will help you sleep easier and more comfortably at night.
Staying active will help you feel better, eat better, and increase your overall stamina and endurance. It also helps keep your heart healthy, boosts your immune system, and reduces your risk for heart disease and other complications. But it comes with more than just physical benefits; exercise can improve your mental health, too.
Living with COPD can be stressful and overwhelming, but physical activity can help relieve your worries and stress. Another benefit of staying active that's often underestimated is self-confidence. The satisfaction you gain from seeing yourself make progress and get stronger as you exercise is empowering and invaluable.
How Exercise Benefits Your COPD

It's important to understand that nothing, including exercise, can cure or reverse the severity of your disease. However, it can prevent your COPD symptoms from getting worse, and can slow down the progression of your disease.
Here is a list of some of the most important benefits you can gain from regular exercise when you have COPD:
- Symptom improvement, including reduced breathlessness and fatigue
- Stronger muscles and improved muscle tone
- Improved balance and flexibility
- Better circulation
- Lower blood pressure
- Better sleep and less restlessness
- A healthy weight (and the ability to lose weight, if needed)
- Reduced anxiety and depression
- Stronger bones
- Better self-esteem and self-image
- Increased strength, mobility, and ability to do daily activities
It's hard to overstate the benefits of regular activity when you have COPD. If you have trouble staying motivated, just remember that regular exercise can mean the difference between an early death or a long, fulfilling life with your COPD symptoms under control.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Preventing Progressive Physical Decline
Hopefully, a better understanding of the benefits of exercise is enough to motivate you to get started. However, it's just as important to know the consequences of not exercising and the effects it can have on your COPD.
Here are some of the consequences of not exercising when you have COPD:
- Muscle wasting, weakness, decreased physical strength
- Worsened breathlessness
- Weight gain
- Depression and anxiety
- Loss of independence and increased difficulty with everyday activities
Even if what you have to gain from regular physical activity isn't enough to motivate you, you should understand that you still have a lot to lose if you choose to stay sedentary.
Even if you feel weak and have difficulty breathing right now, it's no excuse to avoid exercise. If it's difficult now, it will only get worse and worse with time if you don't find a way to stay active.
The Basics of Exercising with COPD
Working With Your Doctor
When you have COPD, it's very important that you work with your doctor to put together an exercise routine that works for you. Every person and every case of COPD is unique, and different people might need to focus on different areas of strength.
You should plan to meet with your doctor to discuss physical activity as soon as possible after getting diagnosed with COPD. Make sure to talk to your doctor about all of your symptoms and physical struggles so he can tailor your exercise plan to your needs.
Exercising with COPD often requires special considerations and techniques so as not to make you feel breathless too easily. Make sure you talk to your doctor about how often and how long you should exercise, if there are any activities you should avoid, and if there are medications you can use to make exercising easier.
Exercising at Home
When you have a serious illness that makes it difficult to breathe, it can be hard to make it to the gym on a regular basis. This is especially true if you have decreased mobility or use supplemental oxygen.
That's why many people with COPD opt for exercise routines that they can do at home. It can make it easier to stay motivated, help you stick with a routine, and keeps you close to your medication, supplemental oxygen, and all the comforts of home.
While some people prefer the gym and think that it makes sticking with a routine easier, it's possible to get all the physical activity you need in and around your own home. All you need is an open space to move your body, a chair, and a small set of free weights to do all the exercises you need to stay healthy.
What Kinds of Physical Activities Are Recommended for COPD Patients?
When you have COPD, it's important to start any new exercise routine by taking it slow and setting small, realistic goals. Exercising is safe for your lungs as long as you stay within your doctor's recommendations and limitations, but you should still take care not to overexert yourself or push yourself too hard.
Every person's exercise plan with COPD looks different, and your routine might be more or less intense than other patients' based on your physical condition and the severity of your disease. The important part is to make progress without stretching yourself too far, and to set personal, reasonable goals that you can realistically meet.
That said, there are three things that every healthy exercise plan should include: cardiovascular activity, strength training, and stretching. We'll go through each one by one.
Cardiovascular Exercise

Cardiovascular exercise is a type of activity that includes walking, running, biking, swimming, and much more. It tends to work out large muscle groups and it's all about getting your heart pumping and keeping your body continuously moving.
Regular cardiovascular activity is vital for your heart and lungs and is an effective way to improve your overall tolerance for physical activity. Over time, cardiovascular exercise can lower your blood pressure and heart rate, strengthen up the muscles you use to breathe, and make it so your heart and lungs don't have to work as hard when you're active.
Cardiovascular exercise is also a great way to lose weight and improve your body's overall metabolism. Most doctors recommend getting 20-30 minutes of cardiovascular exercise at least three times a week, but you might need to work up to that amount slowly over time. Also, make sure you talk to your doctor before starting any new exercise routine.
Cardio exercises are usually divided into two groups: high impact (requiring a great deal of exertion) and low impact (requires less exertion). If your COPD is severe or you suffer from chronic pain, you may need to stick with low-impact exercises so you don't push yourself too hard.
Strength Training

Strength training is a kind of anaerobic exercise that includes weight training, abs workouts, lifting, and more. It usually involves standing or sitting in one place and working out one muscle group at a time by flexing and lifting parts of your body.
There are many different benefits of strength training, including increasing your overall strength and endurance and boosting your metabolism. With this kind of exercise, you can gradually build up strength, balance, and endurance and focus your efforts on specific parts of your body that you want to improve.
Strength training exercises are often split up into two more categories: upper and lower body exercises.
Working out the muscles in your upper body is especially important if you have COPD, because it can strengthen the respiratory muscles you use to breathe. Upper-body strength training focuses on the arms, shoulders, neck, chest, abdomen, and back.
Lower-body strength training exercises are also important, because they can improve your mobility by making it easier to stand and walk for extended periods of time. Lower-body exercises include activities that work out your thighs, calves, ankles, and buttocks.
Stretching
Some people do a combination of strength training and cardiovascular training in the same workout, while some people alternate focusing on one or the other on different days of the week. Stretching, however, is something that you should do every day, and especially before every single workout.
Stretching can help you feel better by improving your range of motion, improving your flexibility, and reducing stiffness in your muscles and joints. It's a perfect way to start your day when you get up in the morning or to get your blood flowing when you've been sitting still for awhile.
Stretching is also an important safeguard against getting injured, which is why you should always stretch for 5-10 minutes before beginning any kind of physical activity. You should stretch each part of your body for at least 10 seconds to reduce your chance of muscle strain, soreness, and injury when you exercise.
Warming Up and Cooling Down
Every workout you do should include a brief 5-10 minute warm-up period before your main exercise and a 5-10 minute cool-down session afterward. This helps prevent injury and overexertion, and helps your body slowly adjust to increased activity.
This is especially important to do when you have COPD, so make sure you don't forget these steps.
How to Warm Up
A good warm-up exercise allows you to slowly and gradually increase your heart rate and breathing rate. This reduces strain and pressure on your heart and lets your body get accustomed to the physical activity.
As you do your warm up, start with easy, slow movements and increase your effort and level activity gradually as you go. You should always include at least a few minutes of stretching in your warm-up to loosen up your muscles and joints.
Here are some examples of common, effective warm-up exercises:
- Stretching your legs, arms, waist and neck
- Gently moving your joints, including your ankles, knees, shoulders, and elbows (move them left and right, up and down, and in a circular motion one at a time)
- Walking
- Very light, slow versions of your main workout activities
How to Cool Down
Cool-down sessions are very similar to warm-up sessions, except you want to slowly decrease your level of activity as you go, instead of increasing it. Start by gradually decreasing the intensity of your main workout toward the end, then cool down by walking, stretching, and doing light, low-impact movements.
A good cool-down session will reduce your heart rate and body temperature slowly back to normal and help you feel less sore and fatigued after your workout. Just make sure to decrease your exercise intensity little by little, and don't forget to spend a few minutes stretching your worn-out muscles before you call it a day.
Control Your Breathing
What makes exercising the hardest for people with COPD is the constant threat of breathlessness. If your disease is severe, even short periods of light activity can make it difficult to breathe.
That's why deep breathing techniques are an essential part of exercising when you have COPD. If you can prevent shortness of breath while you exercise, you'll have more energy and endurance to devote to getting in shape.
Make sure to practice breathing exercises and take breaks whenever you feel exhausted or short of breath. If you struggle with breathlessness often, talk to your doctor about pulmonary rehabilitation, supplemental oxygen, or other medications that might help you better control your breathing while you exercise.
It can be overwhelming and difficult to think of what to do when you can't catch your breath, which is why most doctors recommend that you take time to practice breathing exercises every day, even when you don't feel breathless. That way, when the time comes that you are struggling for air, you'll be able to easily remember the steps and bring your breathing back under control.
Pursed Lips Breathing

This breathing technique helps push trapped air out of your lungs and keeps your airways open longer so it's easier to breathe. You should use this breathing technique any time you exert yourself, do any kind of physical activity, or start to feel breathless.
Here's how to practice the pursed lips breathing technique:
- Relax your shoulders and straighten your back
- Take a deep breath in through your nose, making it last about 2-5 seconds.
- Then, purse your lips together, as if you were going to whistle or blow a kiss.
- Breathe out for about twice as long as you inhaled, but through your mouth instead of your nose (about 4-10 seconds).
- Repeat.
Diaphragmatic Breathing
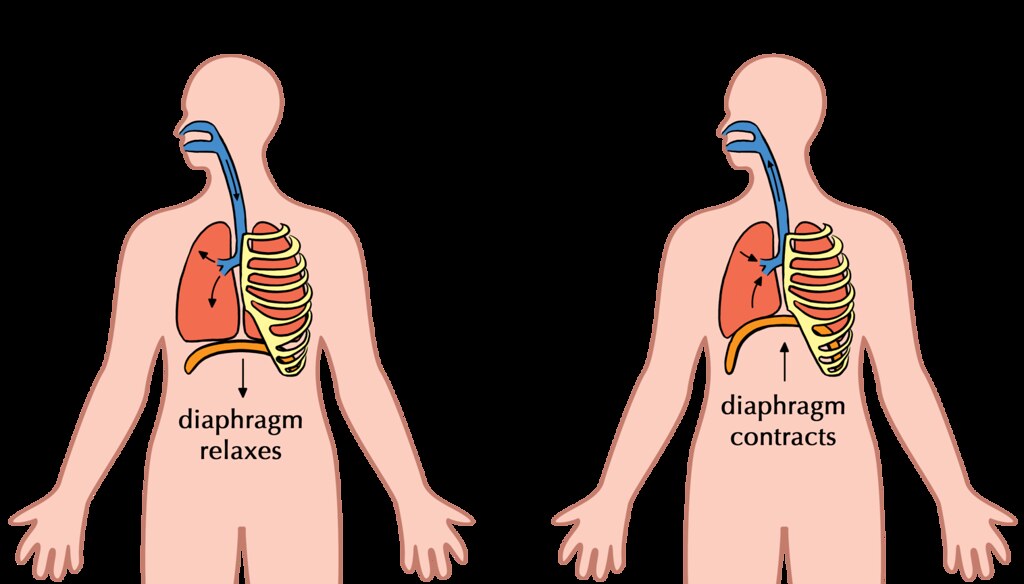
The purpose of diaphragmatic breathing is to help you use your diaphragm, instead of your chest muscles, to breathe. This technique helps you strengthen your diaphragm and use less effort and energy to breathe.
Here's how to practice the diaphragmatic breathing technique:
-
This technique is easiest to practice when you lie down flat on your back, but you can do it while standing or seated as well.
-
Lay one of your hands on your stomach, and the other on your chest.
-
Take a slow, deep breath in through your nose. Pay attention to your hands on your chest and abdomen; you want to feel your stomach rise as you inhale, and your chest to stay still.
-
Exhale slowly through your mouth, again paying attention to how your chest and abdomen move. You should feel your stomach deflate and your chest should stay as still as possible.
- The goal of this exercise is to focus on using your abdomen (diaphragm) to breathe. You should try to keep your chest as relaxed and still as possible, while moving only your stomach when you breathe.
Cardiovascular Exercises You Can Do at Home for COPD
Walking

Walking is a great light, low-impact exercise that's easy to do at home if you have COPD. It's a great way to improve your endurance, and studies show that walking at least four hours per week alone can significantly reduce your risk of heart disease.
The great thing about walking is that you can go at your own pace and it's easy to sit down and take a break whenever you feel tired or breathless. You can get your exercise by walking in your yard or around your neighborhood, or you could go out to a local park or trail for a more scenic stroll.
Here are some tips for walking for exercise when you have COPD:
-
Start small and slow. Don't push yourself too hard at first, but don't give up too easily, either.
-
Add a certain number of feet or steps on to the length of your walk every day (an extra 10 feet a day is a reasonable goal). If you ramp it up gradually, you will steadily get stronger with hardly any extra effort.
-
To control your breathing, exhale through pursed lips for about twice as long as you inhale. It can help to count the number of steps you take while you breathe in, and then take twice as many steps as you breathe out. This is a great way to get a steady rhythm going so you can keep control over your breathing.
- Make sure to turn around soon enough or walk a short enough loop that you can make it back to where you started before you get too fatigued. Don't be afraid to stop and rest any time you feel too tired or breathless, and don't start again until you are breathing normally.
Aerobics

You've probably heard of aerobics classes before; you can usually take them at your local gym or you can follow along with an aerobics training video at home. Even though they had their peak in the 80's, aerobics video routines are still an extremely effective, engaging way to get a good workout.
You can purchase aerobics workout DVDs or get a free aerobics workout by watching any of the many videos available on YouTube and elsewhere online. The best thing about it is that there are so many different kinds and lengths of aerobic workouts. You can tune in to a short ten-minute routine or a 30-minute one, or you can string several short aerobic workouts together with rests in between.
You can do dance aerobics, step aerobics, water aerobics, strength-training aerobics, and more. Aerobic workouts can be extremely satisfying and fun, and you're bound to be able to find a style that fits your interests.
Stair Climbing
Stair climbing is a moderate-intensity activity that you can do at home or any place with a set of stairs. Just make sure you have a handrail to stabilize yourself and stop to take breaks whenever you feel out of breath.
It's important to control your breathing, so practice slow, pursed-lips breathing as you do this exercise.
Tips for Stair Climbing with COPD
- Take a deep breath in before you start ascending the stairs.
- Take two steps up while you exhale slowly through pursed lips.
- Take another breath in and rest a moment before continuing
- Take another two steps up while you exhale again
- Descending the stairs isn't nearly as difficult, and you should be able to take more steps with each breath. Start on the inhale and count how many steps you can take down as you breathe in. Then, try to take twice as many steps down on your exhale as you breathe out slowly.
- Take your time! It's not a race or a contest, and it's okay to take it as slowly as you need to. You'll build up strength with time, but you have to start at your own pace.
Other Aerobic Exercises for COPD
We've listed some of the most common physical activities you can do to get a good aerobic workout with COPD. This is only a small list, however, and the possibilities for aerobic exercise are nearly endless!
Here are a few more ideas for aerobic activities you can do at home with COPD:
- Jogging or Running (high impact)
- Biking (low impact)
- Jump Roping (high impact)
- Playing with pets or children (low impact)
Strength Training Exercises You Can Do at Home

Strength training encompasses a large variety of stationary workouts that flex and strengthen your muscles. Many of these are exercises that don't require any extra equipment, and use simple movements and the weight of gravity to work out your body.
Some home strength training require, or are enhanced, by using free weights. You should start small, with 3 or 5 pound weights, and add more to your collection as you move up to more weight.
Yoga

Yoga is one of the best possible strength training exercises you can do with COPD. Why? Because it's slow-paced, great for your heart, and helps you practice steady, deep breathing while you exercise.
Yoga involves involves slow, steady movements and holding poses that help you build up muscle strength and improve your balance. Practicing controlled, deep breathing is also an integral part of yoga practice, which is particularly helpful if you struggle with breathlessness.
Yoga can help you build the strength you need to do even more kinds of exercise and can help you train yourself to control your breathing whenever you do physical activities. To practice yoga at home you can use yoga DVD's or you can access a huge number of yoga instructional videos online and on YouTube.
Chair Exercises

Many of the techniques we'll show you in the following sections “Upper Body Exercises” and “Lower Body Exercises” can be done as chair exercises. That means you can do them while sitting upright in a chair, and they're a great way to get some extra strength training in without having to leave your seat.
All chair exercises are exercises you can do at home, and they allow you to work out your muscles without having to expend energy to walk or stand. This can help reduce breathlessness and fatigue when you exercise, and is a great solution for people with COPD who have limited energy


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!














