.png)
Whether you have a friend or a loved one with COPD or you have COPD yourself, you can likely attest to the fact that this disease can cause significant problems with mobility. The top causes of mobility issues in COPD patients include poor pulmonary function, leg swelling (peripheral edema), and loss of muscle mass (muscle atrophy). Combined with the effects of aging and other chronic conditions like osteoarthritis, COPD patients can experience a lot of difficulties getting around in their day-to-day life.
Aside from supplemental oxygen therapy, a healthy diet, and pulmonary rehabilitation, another thing that can help you get around are mobility aids. A mobility aid is a device that’s used to help older people and people with chronic conditions walk more easily. They’re often designed to improve balance, reduce physical load, and in COPD patients, they can even help to prevent exacerbations and flare-ups. There is a huge variety of mobility aids and you’re not just limited to choosing one or the other.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In the following sections, we’ll help you better understand the mobility options available to you as well as some other helpful information that will help you maintain your mobility as a COPD patient. As always, if you have any questions, please be sure to address them in the comment section or consult your doctor for more specific information pertaining to your disease and treatment plan.
Why Are Mobility Aids Important for COPD Patients?
According to an article published in the National Center for Biotechnology Information, balance deficit is a common issue among COPD patients. COPD is a progressive disease meaning it becomes worse over time. And as symptoms like breathlessness, chronic fatigue, and chest pain progress, so do issues related to balance and mobility. Believe it or not, studies have shown that COPD is one of the chronic illnesses with the highest rate of falls next to osteoarthritis.
Several months ago, we wrote an article discussing a common complication of COPD called peripheral edema. In short, this is a condition where your legs or feet begin to swell due to a buildup of fluid. One of the root causes of this condition is pulmonary hypertension or high blood pressure in the lungs. High blood pressure in the lungs puts more strain on the heart and prevents oxygen-rich blood from circulating to organs like the liver and kidneys. Since these organs are responsible for removing fluids from the body, swelling of the feet or legs are usually a sign of this happening.
While peripheral edema is a complex condition, it’s one of the issues contributing to the high risk of falls in COPD patients. As the disease progresses, COPD patients don’t just have to deal with increased respiratory symptoms, they have to deal with complications that can result from their disease. Someone with peripheral edema may not even realize they have it because it often comes on slowly and doesn’t cause any pain.
-jpg.jpeg)
Another issue contributing to the high rate of falls in COPD patients is muscle atrophy. In other words, as COPD progresses, patients tend to lose muscle mass from a variety of issues like a changed diet and reduced physical activity. Similar to peripheral edema, a patient may not realize that they are losing muscle mass until they experience a fall. This is why pulmonary rehabilitation is such an important part of any COPD treatment plan.
One final problem that can contribute to the fall rate in COPD is an exacerbation. An exacerbation is an event where respiratory symptoms suddenly worsen. According to COPD.com, the most common cause of exacerbation is a bacterial infection, but air pollution is another common cause. COPD exacerbations can lead to problems walking, balance issues, chest pain, headaches, and confusion, all of which can increase your risk of falls.

While mobility aids are not a replacement for your treatment plan, they play a crucial role in preventing falls, especially in people with late-stage COPD where the disease is the least predictable. Mobility aids don’t need to be prescribed by your doctor so it’s up to you and your loved ones to determine whether you need one or not. Continue reading to learn about some of the mobility options available to COPD patients.
Canes
Walking canes are the oldest type of mobility aid and they’re also one of the simplest. Most walking canes are made of wood or a light metal material meaning they’re easy to carry despite your level of physical impairment. Canes are also widely accessible, and you can buy them just about anywhere, or you could even make your own if you have time. Walking canes are great for taking weight off your joints and providing you with a little extra stability as you walk.

The key to improving your mobility with a cane is to get one that’s the appropriate size. While there is no hard and fast rule as to how you should choose a cane, it should be long enough that you aren’t bending over and straining your back in order to use it and it should be short enough that you can actually lean on it. For most people, this will be somewhere around their hip bone. Luckily, most modern canes are adjustable, so you’ll probably be safe buying one online rather than shopping around for one.

One thing to consider if you want to use a cane is how you will carry your supplemental oxygen device. If you have an oxygen tank and you wheel it behind you using a rolling cart, a walking cane might not be the best option for you because you won’t have any hands free to catch yourself if you fall. A cane is a better option if you carry your oxygen device on your back because it will help you keep a good posture as you walk.
Walkers
Walkers are another mobility option available to COPD patients. There are several different types including traditional walkers, two-wheel walkers, and four-wheel walkers. Traditional walkers tend to be a poor choice for most COPD patients because they need to be picked up as you walk which can be strenuous on your shoulders, arms, and back. Two-wheel walkers provide a little more mobility by allowing you to push the walker rather than lift it. However, for most people, four-wheel walkers, or “rollators” as they’re often called, will be the best option.

Modern rollators are more advanced than other types of walkers because they offer four swivel wheels that afford you more control. They also offer a braking system that’s controlled by two levers on the handlebars on either side of the device. They also provide a padded platform in the middle that you can either sit on or rest your oxygen device, purse, or handbag on as you walk. Some rollators even have a basket in front for added storage.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
It’s a good idea to speak with a mobility aid expert if you want to get a rollator. Since these devices are so popular, there are many different versions and brands available to choose from. What’s more, it’s easier to use one if you’ve been shown how to do so by someone who’s experienced with them. You’ll also need to have one fitted unless you can find one that’s adjustable.
Wheelchairs
When you think of a mobility aid, chances are, wheelchairs are the first thing that comes to mind. They’re commonly used by people who are permanently disabled, but how do they fare when it comes to someone with limited mobility? The answer ultimately depends on your individual circumstances. COPD patients with poor upper body strength may find it difficult to get around in a manual wheelchair, but if you have a caretaker or loved one who can push you around it shouldn’t be a problem.

Another option for you are motorized wheelchairs or “power wheelchairs” as they’re often called. The benefit of investing in a power wheelchair is that you will have the same mobility as a manual wheelchair, but you won’t have to push it with your arms. Power wheelchairs have a joystick that you use to move in any direction. They’re not overly complicated to operate but they can be difficult to transport and you’ll need to keep it charged if you want to stay out of the house for extended periods of time.
Scooters
Mobility scooters are similar to power wheelchairs but they differ in terms of their design. Unlike power wheelchairs which use a joystick, scooters are controlled with handlebars similar to a bike. Scooters can either have three or four wheels depending on what your preferences are. They also have baskets on the front that you can use to store things like your portable oxygen concentrator, a purse, or other personal belongings. Since there are so many options available when it comes to mobility scooters, it’s important to speak with an expert who can align you with the exact product you’re looking for.

Stairlifts
Stairlifts are a mobility aid that many people have never heard of, but they’re incredibly useful. Essentially, a stairlift is a chair that moves up and down a rail that’s installed on a flight of stairs in your home. The chair has a built-in motor that can be controlled with a joystick on the handlebars. This allows you to navigate the stairs in your home without the risk of experiencing a dangerous fall. The one downside to stairlifts is that they can be very expensive and many people can’t justify spending the money to have one installed in their home.

Surprisingly, stairlifts are extremely versatile and can be installed on most staircases regardless of their size or shape. What’s more, if you like to get outside, there are specially designed stairlifts that can be installed on outdoor staircases. They can be installed in several hours so you won’t have to wait days or weeks to start using them.
Will Medicare Pay for a Mobility Aid?
Whenever it comes to medical equipment, questions about health insurance and Medicare are sure to follow. And while it would be nice if Medicare paid for medical expenses like you’d expect them to, it’s never that simple. More often than not, they will cut corners providing you coverage for mobility aids and find any way they can to offer you the bare minimum rather than what you deserve.

In short, Medicare will provide some compensation for manual or power wheelchairs and scooters. Mobility devices like these are covered under Medicare Part B and it is classified as durable medical equipment (DME) the same as oxygen tanks and portable oxygen concentrators. But it’s important to note that not all devices are covered. Medicare has a list of devices that are covered, and some of them require prior authorization. So, it’s best to consult with both the mobility aid supplier and a Medicare representative before you make any decisions.
.jpg)
Another thing to note is that Medicare has a long list of prerequisites that you need to meet in order to qualify for compensation. First and foremost, the doctor that has prescribed you with COPD and the mobility aid supply company needs to be enrolled in Medicare. Additionally, you’ll need a written order from your doctor stating that you have a medical need for a mobility aid. For a full list of requirements, refer to the wheelchair and scooter benefit page of Medicare Part B.
Get a Handicap Parking Permit
Once you have your mobility aid of choice, you may want to consider getting a handicap parking permit. This permit will allow you to park in any handicap spot in the country making it much easier for you to get around. This is especially useful for people who are using electric scooters or power wheelchairs because you won’t have room to unload it in a standard parking spot.

In order to get a handicap parking permit, you’ll need to apply at your local Department of Motor Vehicles (DMV). Every state has different policies but you’ll likely have to provide a doctor’s note which outlines your lung condition and symptoms. You’re more likely to get approved if you can prove that you use an electric scooter or power wheelchair as opposed to a cane or walker so it’s best to put time into finding a mobility aid first.
.jpg)
Last but not least, if you’re given the option between a handicap sticker that goes on your car or a placard that you hang on the mirror, always go with the placard. This is because you can transfer these to any car that you’re in whether it belongs to a family member or friend. Be aware that it is illegal for them to use the placard without you actually being present and most states require you to be recertified for your handicap permit every couple of years.
Conclusion
Making the decision to use a mobility aid is an important step for many COPD patients. People with chronic respiratory conditions are at a higher risk of experiencing falls than the general public, but mobility aids will help to support your balance whether you’re inside or outside the home. Unfortunately, there is no one-size-fits-all solution. Everyone has their own needs and preferences so you should consider all options available to you.
Canes and walkers are a good place to start because they’re affordable and they’re easy to carry. However, you may want to consider a more long-term solution like a mobility scooter or power wheelchair. These devices are generally safe and easy to use, and they will make it easy to carry around your oxygen devices such as your oxygen tank, liquid oxygen tank, or portable oxygen concentrator.
Lastly, you should check with your health insurance to see if your mobility device is covered. This could save you hundreds if not thousands of dollars. You can also file for disability and receive a handicap parking permit which will afford you more convenience and freedom whenever you leave the house. In the meantime, if you’re looking for a lightweight and easy-to-use portable oxygen concentrators such as the Caire FreeStyle Comfort or the Inogen One G5, don’t hesitate to reach out to your respiratory specialists here at LPT Medical.
It is 2021, and no matter who you are, your life was most likely impacted by the global pandemic caused by the novel coronavirus first exposed late in 2019 (COVID-19). This virus is the most dangerous for humans when it infects your respiratory system, so this is obviously frightening for people with COPD and other underlying health conditions and immunodeficiencies.
There is much more that is unknown about the virus than there is any information that is definitive. How fast it spreads, how easily transmittable it is, and so much more will be under scientific scrutiny for months even years to come.
COVID-19 and COPD recommendations
This means that if you have COPD or any respiratory aliment or immunodeficiency it is recommended by medical professionals all over the world, that you especially need to take care to adhere to guidelines and other health related advice.
This means limiting your travel or vacation plans, maintaining social distancing recommendations of at least 6 feet apart, among other requirements.
You might have had plans this year to visit the grandkids, or they were coming to visit you, maybe you were embarking on an adventure, or a relaxing getaway, or maybe you had no plans at all, but are finding the reality of a global pandemic lifestyle unfulfilling.
No matter how serious your COPD is, there are ways you can maintain a positive livelihood without being exposed to COVID-19. Here are the best ways to enjoy this year safely in the midst of a global pandemic if you are immunocompromised or suffer from a respiratory illness such as COPD.

Simplify your life
There is no better time than now to simplify your life. This is often called minimalism. The benefits of simplifying your life are substantial especially at a time of pandemic when our minds are filled with anxieties and uncertainty. Ironically, making things simpler can sometimes be more complicated than you think.
Minimalism and simple living can offer anyone, especially seniors and people living with COPD, many benefits. For example, minimalism can help seniors have a much easier life physically.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
With all of your things organized, you will decrease the annoyance of misplacing something. And with less things, you won’t have to deal with moving things around as much, or moving around and clean as often. Overall, with less to physical material to deal with, comes less stress and anxiety.
By reducing the clutter in your home, yard, and work space, you subsequently make room in your mind for peace and mindfulness, something that might have gotten lost since the global pandemic has shifted reality.
It can be difficult to get rid of older things that have sentimental value to you, so start by cleaning out a shed or garage where the items have less emotional attachments.

You will find a powerful feeling of control and liberation in this stage and will be able to make more decisions about getting rid of things closer to you.
Hold yourself accountable for getting rid of things that do not serve you, for example: donate clothing you don't wear, donate plates and bowls that are taking over your kitchen cabinets, give away books you’ve read and don't want to read again. The act of giving to others through donations or gifts is very fulfilling in itself, so this is a bonus.
In order to avoid going to donation centers, ask a less vulnerable family member or friends if they would help you by picking up boxes of stuff from your home for them to bring to donation centers for you.
Start a garden or doing daily yard work
While at first thought, this sounds exhausting, gardening and 10 minutes of yard work each day can be very exciting and addicting. Being outside and getting physical activity everyday is one of the best treatment options if you have COPD, and starting a garden is one way of doing that.
Gardening is a physical challenge, relieves stress, and improves dexterity, and aspects that will encourage healthier lung functions.

If you do not have a yard or a nearby community garden to plant anything, you can buy a plant and leave it on the stoop of your house. Visit your plant everyday in the sunshine and watch it grow!
Yard work can take up a lot of time and give you a fulfilling mindset at the end of each day. You don't have to do a lot at first, but once you start picking weeds one day, you’ll begin to enjoy cleaning the yard and finding creative ideas for an outdoor sanctuary right in your backyard.
Find a new hobby you can do online
There are a lot of indoor activities that can keep you occupied and busy this summer and beyond. And there are a lot of activities you probably don’t know that you enjoy yet.
One way to try a lot of different hobbies is to join a club, and because of COVID-19 rather that gathering in a large group for a weekly meeting, you can do this online.
Right now there are a lot of resources where you can join a book club online, or spend time virtually connecting to people with similar interests, either through video chat or social media.

If you have a favorite hobby already, you can try to expand on that by dedicating more time to that specific activity, and find a way to get involved with others who enjoy that hobby virtually.
If it brings you joy, prioritize the time you spend doing those things.
If you feel you are struggling alone with COPD, try joining a FaceBook group or a supportive online forums where individuals share their stories and resources about their COPD.
Go hiking or walking
Walking is a safe and effective form of exercise for people living with COPD, and there are a number of reasons walking and hiking relive COPD symptoms.
Walking and hiking can help improve your COPD:
- Low impact activity that will improve your body's ability to use oxygen
- Build endurance
- Strengthen muscles
- Enhance an overall sense of well-being
- Being more self-sufficient
- Tolerate exercise better
There are even more benefits of walking for a person with COPD than whats listed above.

While you should not travel too far away from home, there might be a great walking or hiking trail near you. Try to avoid walking on busy trails by going during the week day rather than the weekends.
Hiking gets you into the outdoors and under the sun, but it is important that you do so safely. Be sure to continue wearing a mask if people are present on the trails. If the parking lot is extremely crowded, come back another day.
If you are curious how to find the best trails near you, be sure to do some research and learn more about how you could go walking and hiking even with COPD or other complicated health issues can enjoy hiking and walking.
Invest in a oxygen concentrator
Even though we are expected to “stay in place” there is no better time to become more mobile while doing so.
Receiving oxygen treatment for conditions such as COPD doesn't have to mean being tethered to a bulky canister of compressed oxygen, and you should not be subject to limited mobility and lack of independence.
You do not have to subject yourself to the unnecessary risks of carrying around an atmosphere of pure oxygen. There are safer and more transportable alternatives available today.
You do not have to carry a heavy tank around, instead portable oxygen concentrator extracts and concentrates pure oxygen and give you therapeutic doses of purified oxygen from the air around you.

Being at home unable to move around easily due to a rolling oxygen cart can be frustrating and upsetting, especially when you have no outlet to go out and do something, go on vacation, or look forward to family members and friends visiting you.
The uncertainty of these times leaves people hesitate to make larger purchases, such as a portable oxygen concentrator. However, when it comes to the air you breathe and the peace of mind you gain by being more physically active with less shortness of breath is priceless.
These long-term investments lead to long-term savings both monetarily and with regard to your livelihood.
You have a plethora of choices to make when it comes to buying an oxygen concentrator. One thing you need to know is there are two ways that concentrators deliver nearly pure oxygen from the air around you and into your lungs:
1. Pulse flow
Pulse flow or pulse dos oxygen concentrator sensors measure your breathing rate and automatically deliver a short bursts of oxygen as needed. This is a more popular choice for those with higher-functioning lungs like people in stages 1, 2, or sometimes 3 of COPD or those seeking an oxygen boost for exercise or at higher altitudes.
2. Continuous flow

Continuous flow oxygen concentrator maintains a steady supply of oxygen to you while it is being produced. This model will generally be heavier with more power and lower battery life. This option is best for you if you have stage 3 or 4 COPD and very limited lung capacity or higher oxygen saturation requirements for your body.
Be sure that you purchase your oxygen concentrator from an authorized dealer that carries devices from well-established manufacturers. By working with an authorized dealer you can be sure that your machine will be serviced and that the warranty is valid.
Medical and healthcare professionals do not advise purchasing portable oxygen concentrators from questionable sources such as amazon or online auction websites because the warranties and support may be fraudulent and the device may not be exactly what is represented online.
Plan ahead
Planning ahead has been recognized as a key to success, so even under the impending uncertainties brought on by COVID-19, you should plan your goals through hard work and strategic thinking.
This can mean:
- Planning to a regular walking routine for the next week
- Planning to call your loved ones once a day for the next month
- Planning a budget to purchase a portable oxygen concentrator within the next year
- Planning a diet for healthier eating habits over the next week
- Planning goals to quit smoking
COPD can cause a lot productivity challenges, due to shortness of breath and common depressive moods and anxiety. Nevertheless it is these times of isolation, where planning is more important than ever.
You can combat depressive moods and especially anxiety, by planning beneficial goals that will help you to attain a higher quality of life. And there is no excuse not to give this a try while you have so much extra time on your hands.
Foster new and old social connections
Social interaction is vital for everyone, and if you have COPD connecting with others is essential.
If you are not used to being all alone and without other people, and are eager to to reach out to find ways to connect with others, it is important to do so safely.
When exposing yourself to other people you should stay the recommended 6 feet apart and everyone should be wearing a mask. But this does not mean that you can’t have fun.
Take a trip with friends and family to the local beach, river bed, or lake, bringing a large towel or blanket to establish physical boundaries and make sure others are staying a safe distance away from you.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Try bringing a king sized bed spread and your spot can be right in the middle of it, creating a perfect distance away while still socializing.
You and your neighbors can have small communal cookouts where families bring their grills to their respective front yard to BBQ and eat together.
If you want to be more creative, have a neighborhood talent show where each house takes turns putting on a show, either playing music, dancing, or magic outside for everyone to watch.
In order to have a successful social-distancing get-together you must do your best to be innovative. And if you have COPD and are rightfully concerned about COVID-19 you should become a leader in your community to help people socialize safely amid the ongoing pandemic.

Enjoy
Taking each of these steps in your own personal way will help you to enjoy your summer to the fullest, despite on-going risks associated with COVID-19.
Simplifying your life will give you the space you need to try new things. And by taking pleasure in the simple things, you will appreciate your new found adoration for gardening, or yard work.
You can also start exploring ways to use the computer to start new hobbies, or join an online club that you've always wanted to try but could never find the time or motivation to get out of the house and do so.

If you find yourself stuck inside unwilling or unable to move around without shortness of breath, this is the best time to purchase a portable oxygen concentrator that will give you the freedom and independence you need to get moving around your house and outside safely.
Once you are ready to explore more with a lightweight oxygen concentrator that you can carry around, you can attempt taking a short hike or going for a walk. If this is within the capabilities of your lungs, be sure you go to less busy hiking trails and try to go on weekdays when trails are less busy.
Remain social by getting "together" with you family and neighbors and try putting on a social gathering where everyone stays in their respective yards for a BBQ or talent show.
Do you best to stay motivated by planning ahead and setting goals for yourself in all aspects of you life. By taking all of these measures in 2021, amidst a global pandemic while also managing a chronic lung disease, will lead you to a more fulfilling and satisfying life.
.png)
Nowadays, life is all about choices. We get to choose where we shop, eat, work, and much more. For the most part, this is a positive thing because it allows us the freedom to create a life that’s suited to our wants and needs. Oxygen patients, for example, can benefit from many decades of improvement in oxygen device technology and they have a wider array of options available to them than ever before including oxygen tanks, liquid oxygen tanks, stationary oxygen concentrators, and portable oxygen concentrators.
Unfortunately, there are downsides to having so many options as well. The more choices that you have, the more research you will need to do to ensure that you’re choosing the right oxygen device for you. Additionally, the more features that are added to oxygen devices, the easier it is to fall victim to scams and false advertising. This is why it’s recommended that you speak with a respiratory specialist after you’ve taken some time to look around for yourself and see what’s out there.

Here at LPT Medical, we understand the need for oxygen patients to choose the oxygen machine that’s right for them. But we also acknowledge that it can be difficult to find exactly what you’re looking for in a market that’s full of jargon and other confusing terminology. If you’d like to speak with someone who will help you understand your options but not pressure you into making an immediate choice, get in touch with our respiratory specialists today.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In the meantime, we’re going to take a look at the benefits of the Inogen One G5, one of our most popular portable oxygen concentrators. If you have any questions, please leave them in the comment section and we’ll get back to you as soon as possible.
It’s Incredibly Easy to Use
If you’ve been a cell phone user for the past couple of decades, you’ve likely begun to notice a trend: they get progressively more complicated as time goes on. And while this might be a good thing for some people, if you’re like most people, you just want to be able to make calls or send a text message without using a bunch of unnecessary features. Many people believe that purchasing an oxygen concentrator will be a similar experience, but this is not the case when it comes to the Inogen One G5.

Inogen has been manufacturing portable oxygen concentrators since the early 2000s meaning they were one of the first companies in the business. And despite adding more features each generation, their POCs have actually gotten easier to use instead of more difficult. In other words, you don’t have to worry about bending over backward to learn how to use the G5. It will likely come naturally and you’ll feel comfortable operating it an hour or two after receiving it in the mail.

One of the reasons the G5 is so simple to operate is because it only has five physical buttons that you need to know how to use. One to turn the device on or off, two for adjusting the flow setting up or down, one to adjust the alarm settings, and one to adjust the volume settings. That’s it! There’s no need to spend hours on the phone with customer support trying to figure out how to operate your new device. The G5 also comes with a very thorough user manual that outlines all the symbols that may appear on the user interface display and what they mean. We recommend folding up your user manual and keeping it with you whenever you leave the house so that you can refer to it if you need to.

Another aspect of the Inogen One G5 that’s easy to use is the battery system. Unlike other portable oxygen concentrators which require you to open the device up in order to replace the batteries, the G5 batteries simply pop off the bottom of the unit and can be replaced in a matter of seconds. This is ideal for people who are on the go and don’t have time to tamper with their POC.
One other aspect of the Inogen G5 that makes it easy to use is the Intelligent Delivery Technology®. This built-in technology isn’t mentioned very often but it’s quite possibly the most important feature of the device. Essentially, what this does is automatically adjust your oxygen flow based on your breathing rate. In other words, you’ll be able to do things like walk, exercise, and even sleep without having to constantly change your oxygen flow setting.
It’s One of the Lightest POCs
One way or another, most people tend to lose muscle function as they get older. It’s a natural part of aging, and COPD patients are especially susceptible because of something called muscle atrophy, or “muscle wasting.” While you can combat this by exercising more often and maintaining a well-balanced diet, you might still need to find a lightweight POC like the Inogen One G5.
Although the Inogen One G5 is not the lightest portable oxygen concentrator on the market, it’s light enough for the vast majority of oxygen patients even people with late-stage COPD. The G5 weighs just 4.7 pounds, making it the third lightest POC ever manufactured behind the AirSep Focus and the Inogen One G4. It’s also lighter than its main competitor, the Caire FreeStyle Comfort.

Whether you struggle with mobility issues or not, the Inogen One G5 makes it easier to get around while still having access to medical-grade oxygen. This is something that simply wasn’t possible in the past with heavy and bulky oxygen tanks. The problem with these devices is that the weight of the unit directly correlates to the amount of oxygen that you have access to. In other words, if you wanted enough oxygen to make it through the day, you’d need to carry or wheel around an extremely cumbersome oxygen tank.
Unfortunately, with the turn of the century, things didn’t improve much. While there were portable oxygen concentrators available in the early 2000s, they were still very heavy and didn’t provide a decent enough battery life to justify getting one. We’re living in a revolutionary time for portable oxygen concentrators because lightweight machines like the G5 and the Caire FreeStyle Comfort are breaking barriers for COPD patients.
It Has the Highest Oxygen Output of any Pulse Dose Unit
One of the nicest things about owning a portable oxygen concentrator is how easy it is to adjust your flow settings. If you’re going out for a walk or to a pulmonary rehabilitation course, you might need to go up a flow setting or two in order to keep your blood oxygen levels stable. However, you can’t do this if you own a portable oxygen concentrator that doesn’t go up to a high flow setting.

The Inogen One G5 uses something called pulse dose technology. Unlike older concentrators which use continuous flow, pulse dose closely monitors your breathing rate and delivers oxygen only when you’re inhaling. Overall, this makes the device much more energy-efficient, affording you the freedom to stay out of the house longer. The Inogen One G5 has 6 pulse flow settings which equates to a maximum oxygen output of 1,260 milliliters per minute (ml/min) of oxygen.
The majority of oxygen patients only need to use a flow setting of 2 or 3, so the Inogen One G5 offers plenty of flexibility to move up if you’re exercising or your respiratory disease progresses. Be sure to maintain open lines of communication with your doctor and let him/her know if you’re feeling breathless and want to increase the amount of medical oxygen you’re receiving.
It Uses Powerful Lithium-Ion Batteries
The only thing making it possible to have portable devices like cellphones, laptops, and even portable oxygen concentrators is the advancement of lithium-ion batteries. These are some of the most powerful and reliable types of batteries out there and the experts at Inogen have crafted one that will afford you a significant amount of freedom with the Inogen One G5 portable oxygen concentrator.

The single battery which comes with the standard G5 package can run for up to 6.5 hours on a flow setting of one. The double battery which is sold separately can run for an astounding 13 hours on a flow setting of one. While this may sound too good to be true, it’s simply a testament to how much time and money Inogen has put into refining their products and ensuring that they offer the best possible value for your money.

There are countless reasons it’s important to have a portable oxygen concentrator with long-lasting batteries. First and foremost, it allows you to have ample oxygen supply whenever you leave the home. Even if you’re leaving the home for a few hours, it’s nice knowing that you have a safety net in case there is an emergency and you are gone longer than expected. If you are going on a flight, most airlines will require that you have at least 1.5 times the duration of the flight in battery life.
It Has a Low Sound Output
One of the things that people are most worried about when looking for a portable oxygen concentrator is that they will be noisy and cause a distraction for themselves and the people around them. And while this is certainly a valid concern, this will not be a problem if you purchase an Imogen One G5 because it only puts out 37 decibels (dBA) of sound on a setting of 2. This is equivalent to a quiet conversation or a slight background humming noise that won’t disrupt your day or anyone else’s.
The benefit of having a quiet portable oxygen concentrator is that you can take it just about anywhere without feeling anxious or worried. Most people report being able to take their Inogen One G5 to church services, libraries, or other quiet places without causing a disruption. Before you do so, however, be sure to read the user manual to figure out how to turn off the audible alarms.
It Can Be Used 24 Hours a Day
Believe it or not, many COPD patients need to be on oxygen 24 hours a day. And if this is you, it means that you need an oxygen concentrator that’s capable of running around the clock without failing. Fortunately, the G5 was designed for just this. The intelligent delivery technology in the G5 will adjust your oxygen supply all night long to make sure you aren’t getting too much or too little oxygen.
.jpg)
The one downside to using the G5 while sleeping is that it is not compatible with CPAP and BiPAP machines used to treat obstructive sleep apnea (OSA). This is a sleep disorder that causes your airways to close up as you sleep causing disruptions and putting you at a higher risk for several serious conditions like heart attack, stroke, and irregular heartbeats. The PAP machines open the airways as you sleep making it easier to breathe. And in certain cases, this disease can overlap with COPD meaning you’ll need to use supplemental oxygen simultaneously.
Backed by a Reputable Brand
One final benefit of the Inogen One G5 is that it’s backed by a reputable brand. Inogen has been in the oxygen industry since the early 2000s and people tend to wait in anticipation of their next product because they know they will be reliable and powerful devices. The Inogen One G5 is their latest generation of portable oxygen concentrator and it’s also their best. While the G5 has a very low failure rate compared to other POCs on the market, you can still rest easy knowing that you have a 3-year manufacturer warranty with the purchase of a new G5.
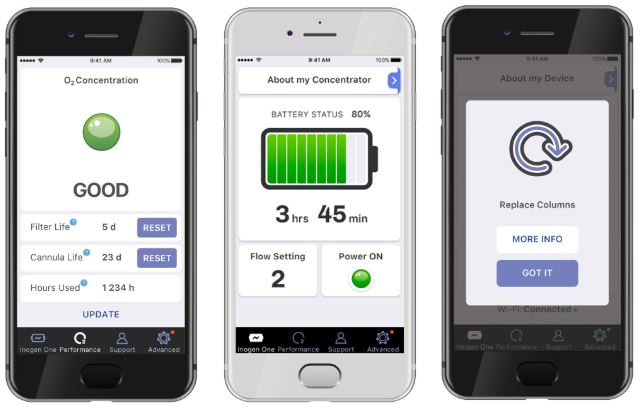
Another way Inogen supports the G5 is with a mobile application called the Inogen Connect. This connects to your device via Bluetooth and enables you to check your battery life, monitor column life status, perform column resets, and access your user manual all without ever touching your POC. This is perfect for people who are on the go often and don’t want to keep checking their device. Simply check the app on your phone and you’ll have all the information you need in one convenient place. Inogen will likely implement similar features into future concentrators because it’s been well-received by oxygen users.
Conclusion
Choosing an oxygen concentrator can seem like an insurmountable challenge at times. Whether you’re in the market for a stationary unit, continuous flow, or pulse dose, you should take some time to understand your options before committing to anything. This post provided you with just a few of the many reasons to invest in an Inogen One G5 over other units on the market. For full details on the specs and benefits of the G5, be sure to visit our product page.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
If you found this post helpful, feel free to bookmark our blog page. We update our site regularly with informational posts that aim to help COPD patients better manage their disease and live long and fulfilling lives. And whether you’re a current customer of ours or you just want more information on medical oxygen devices, please reach out to us either by phone or email.
Getting diagnosed with COPD can seem overwhelming, especially when it catches you by surprise. It's often even more overwhelming to get used to all the new treatments, medications and lifestyle changes required to keep your lungs healthy, especially while you're still trying to come to terms with your diagnosis.
As a chronic disease, COPD requires constant work and careful decision-making to keep the symptoms under control. Because of this, it's no surprise that new COPD patients make a variety of mistakes that can affect their health and well-being.
Between making changes to your diet, exercise routine, medications, and many other activities of daily life, there are a lot of opportunities for error. As you adjust to life with COPD, it's important to avoid making mistakes that could serious consequences for your health, or at least catch and correct them early on.

That's why you should learn and pay attention to the mistakes that other new COPD patients tend to make. It helps you learn more about your disease, what to look out for, and how to keep your body and lungs as healthy as possible.
In this guide, we're going to help you avoid common pitfalls by showing you the mistakes that new COPD patients frequently make. Along with each mistake we've provided solutions so you'll know how to avoid that mistake and do the correct thing instead.
By taking the time to learn from others' mistakes, you'll be much less likely to encounter the same problems yourself. In the next sections, we'll give you all the information you need to avoid falling into the same pitfalls that other patients end up in.
However, it's important to remember that mistakes and struggles are inevitable as you adjust to the many changes that getting diagnosed with COPD brings. But if you educate yourself now, you can easily correct these mistakes and avoid serious problems that could permanently affect your health.
A major part of keeping your lungs healthy and keeping your COPD under control is learning everything you can about your disease. It also means being an active, motivated participant in your treatment and knowing what you shouldn't do just as much as the things you should.
The Mistake: Not Using Your Inhaler Correctly

While inhalers may seem like fairly straightforward devices, a surprisingly large percentage of patients don't use their inhaler correctly. This happens to many patients who never learned the proper technique or forgot the correct steps over time. Other patients get too complacent or careless and skip steps to save time, not realizing each step is important.
Most of the mistakes patients make with their inhalers have to do with preparing the inhaler and using the right breathing technique. This is a serious problem, since these steps are necessary for getting the medication into the lungs where it needs to work.
Unfortunately, many doctors don't do their due diligence in training their patients to use their inhalers correctly. Even though doctors are supposed to check patients' inhaler technique at every appointment, it is often rare for them to take the time to do it properly in practice.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
It doesn't help that many doctors don't even know proper inhaler technique themselves, meaning they can't give their patients adequate instruction. Luckily, the medical community has recently acknowledged the extent of this problem and is making efforts to raise awareness among doctors to correct it.
Here are some of the common mistakes to look out for:
- Not shaking the inhaler before each puff
- Not exhaling fully before using the inhaler
- Not holding the inhaler in the correct position
- Not timing your inhale with the spray from the inhaler
- Not inhaling deeply enough
- Not inhaling slowly enough
- Not holding your breath after inhaling the medication
- Inhaling through your nose instead of your mouth
Making any of these mistakes can result in getting too little medication or none of the medication that you need. This can be very dangerous when you suffer from COPD, because you need your full dose to prevent serious symptoms and exacerbations.
The Solution: Learning Proper Inhaler Technique
Because all inhalers are different, the only way to ensure that you're using your inhaler correctly is to re-read your inhaler's instructions and re-evaluate your technique. That means going over all the steps and guidelines in the information packet that comes with your medication.
This is important whether you're a newly diagnosed COPD patient or you have been treating your disease for some time. No matter how well you think you know it, it never hurts to double check.
You should also take your inhaler with you to every doctor's appointment so you can show your doctor exactly how you usually use it. That way, your doctor can identify any mistakes you make and show you the correct technique.
Every time you use your inhaler, make sure you follow every step and don't rush or cut any corners. Don't forget to shake or prime your inhaler if needed, and always remember to exhale before using it.
Timing your inhale with the spray from your inhaler is extremely important, but also difficult, which is why this step tends to cause patients the most problems. It may take some practice to time correctly, and you may need to use a spacer attached to the mouthpiece to help you do it right.

Studies show that when you inhale too early, then you only get about 35% of the full dose you're supposed to get. If you inhale to late, however, you end up spraying the medication in your mouth and throat instead of inhaling it into your lungs. This makes the medication ineffective and puts your lungs at risk.
To make sure you inhale at the right time and get the full dose, start breathing in slowly just before you press the button to release the medicine. Continue inhaling slowly and deeply as you feel the spray to draw the medication all the way into your lungs.
Remember that inhaling the medication isn't the last step; you still have to hold your breath to keep it in your lungs. Most recommend holding your breath for about ten seconds, then you can slowly and gently exhale.
If you are using an inhaler that contains steroid medications, then you still aren't done quite yet. To prevent the medication from drying out your mouth and throat, you need to rinse your mouth out with water before you're done.
If you ever have any questions or concerns about using your inhaler, don't hesitate to talk to your doctor. You can also ask your pharmacist to demonstrate how to use your inhaler(s) or to answer any other questions you have.
You can also find tips and information online for a variety of different types of inhalers. However, this should never be a replacement for the information you can get from your doctor and prescription information.
The Mistake: Not Knowing When to Take Which Medications

Nearly all COPD patients take two major types of medications: maintenance medications and quick-relief medications (also known as rescue medications). Both medications are delivered via inhaler, which is why patients sometimes get them confused.
This can be dangerous, because you need to use both medications correctly in order to treat your COPD effectively and keep your symptoms under control. Mixing up the two medications or forgetting to take them at the right time could make your symptoms worse or cause you to have a serious COPD exacerbation.
Other medications can be confusing to use, too, especially if you are only supposed to take them on certain occasions. For example, many doctors prescribe oral antibiotics and steroid medications for their patients to use as needed to prevent and treat COPD exacerbations.
The Solution: Following Your COPD Action Plan

Every COPD patient should get a COPD action plan from their doctor shortly after getting diagnosed. If you haven't received one yet, ask your doctor to work one up for you, as studies show that they help patients better manage their COPD at home.
A COPD Action plan acts like a set of guidelines for you to follow based on how bad your symptoms are from day to day. For example, most action plans have three major “zones” that correspond to the severity of your symptoms; the first zone is for when you are feeling fine, the second for mild flare-ups, and the third for more serious symptoms and complications.
Click here to see what a sample COPD action plan looks like.
Every day, you should evaluate your symptoms to determine what “zone” to look at. Then, you simply follow the instructions in that zone for what medications and what doses you should take. Most action plans also include guidelines to let you know when its safe to exert yourself and at what point you should call your doctor when your symptoms flare up.
Because most COPD patients have several different medications to keep track of, it's extremely important to take the time to learn all of the important facts about each of your medications. That includes learning their full names, what they look like, and what you are supposed to use them for.

This ensures that you can match your medications with the instructions in your COPD action plan and use them exactly as your doctor directs you to. It also makes you much less likely to mix your medications up, take them at the wrong time, or forget about them altogether.
You should also bring a complete list of your medications with you anytime you go to the hospital or doctor's office. This will make it easier for the medical professionals who look after you to ensure you get the best treatment possible.
It is also important to bring this list with you whenever you travel, especially if you will be taking your medication with you on a bus, train, or airplane. You may need to present your list of medications to travel personnel, and it will come in handy if you need medical attention while you're away from your regular doctor.
The Mistake: Not Quitting Smoking
One of the most important things you can do for your health when you have COPD is to stop smoking. Unfortunately, too many patients believe it's too late for them to quit and continue to smoke even after their COPD diagnosis.
The thing is, even after you've developed COPD, there are still enormous benefits to quitting. In fact, having COPD makes it even more imperative to quit, since continuing to smoke can cause your disease to rapidly get worse.
COPD is a result of reduced lung function, often due to smoking, but continuing to smoke after COPD has set in will only harm your lungs even more. Smoking causes you to lose lung function at an accelerated rate compared to COPD patients who are able to quit.
Reduced lung function will make it even more difficult to breathe, do physical activities, and can significantly reduce your quality of life. If you quit, however, you may even see an improvement in your COPD symptoms, and you can enjoy the lung function and lifestyle you have for much longer.
While quitting smoking cannot reverse the damage that's already been done to your lungs, it can slow down the damage from getting worse. It can also increase your lifespan and reduce the number of exacerbations, flare-ups, and hospitalizations you experience because of your COPD.
Don't forget that quitting can reduce your chances for a variety of other serious health problems as well. For example, you can significantly reduce your risk for heart disease, lung cancer, and stroke if you successfully quit smoking.
The Solution: Making the Decision to Quit

It's important for every COPD patient to understand that it is never too late to quit smoking. Whether you are 25 or 65, you can improve your health and possibly even your lifespan by making the decision to quit today.
It's not an easy decision to make, and it's even harder to actually follow through. However, every year at least 350,000 smokers in the US are able to quit completely, and there's no reason why you can't be one of them.
Although quitting is hard, there are many things you can do to increase your chances of success. For example, using a quit-smoking medication or joining a quit-smoking program can make your quit attempt more likely to succeed.
When you make the decision to quit, remember that you are not alone and there are many ways to get support. First, you should talk to your doctor to see what kinds of medications and support programs are available to help you.
You may want to try nicotine replacement therapy, which is proven to increase smoking cessation rates. There are many different forms available, too, including nicotine gum, skin patches, tablets, oral sprays, and inhalers.
For more information on how to quit smoking, visit the CDC's website for a variety of helpful links and resources. You can also find helpful quit-smoking tips from the American Lung Association's website or from smokefree.gov.
Don't be discouraged if your first, second, or even tenth attempt to quit smoking ends up failing. It takes most smokers at least six attempts to quit smoking, and sometimes up to twenty, before they are able to quit long-term.
As the CDC puts it, “Quitting smoking is a marathon, not a sprint,” and you have to be in it for the long term if you truly want to live smoke free. Even though it is a long and difficult process, it is more than worth the benefits you will receive through improved health, reduced COPD symptoms, and your overall quality of life.
The Mistake: Not Eating a COPD-Healthy Diet

In order to keep your lungs and the rest of your body strong, you need to feed them the nutrients they need. That means eating a healthy, balanced diet every day to give your body fuel to work as efficiently as possible.
Unfortunately, many new patients find that controlling their weight and eating healthy foods is difficult with COPD. The disease can make it difficult to exercise and prepare healthy meals, both of which are vital for a healthy lifestyle.
COPD can make it difficult to lose weight and difficult to gain weight, which is why some patients struggle with being underweight while others struggle with obesity. Either situation is bad for your health and can make it more difficult to breathe.
If you get too few calories and nutrients, then your lungs won't have enough fuel to keep up with your body's needs. However, eating too much and gaining weight puts extra strain on your muscles and lungs, which can also make your COPD symptoms worse.

Also, because COPD makes your lungs less efficient, it means they have to work harder than healthy lungs in order to get enough oxygen to your body. This means that COPD patients need more calories and more nutrients to fuel the needs of their lungs and breathing muscles.
Another danger that many new COPD are unaware of is eating a diet that's too high in carbohydrates. Carbohydrates actually put extra strain on your lungs when digested, because they release large amounts of CO2 that then has to be processed through your lungs.
The Solution: Eating Whole Foods and Balanced Meals

Staying healthy with COPD requires a variety of lifestyle changes, including changes to your diet and eating habits. While this is never an easy thing to do, it can make a huge difference in your mood, your symptoms, and your overall physical well-being.
It helps to work with your doctor or a licensed dietitian to develop a nutrition plan that works for you. However, it is certainly possible to manage a healthy diet on your own by simply eating a balanced diet.
A healthy diet is one that's full of whole foods, which generally means foods made by starting with raw, unprocessed ingredients. These include whole grains, fresh fruits and vegetables, and lean, unprocessed meats like poultry and fish.
To avoid putting extra strain on your lungs, you should also try to limit the amount of carbohydrates you eat to the minimum healthy amount. That means avoiding processed grains, sugary foods, and processed snacks like crackers and chips.
If you want more information on eating a COPD-healthy diet, take a look at any of the several comprehensive guides we've created to help you out:
The Mistake: Not Getting Enough Exercise
It is common for COPD patients to avoid physical activities because it makes it more difficult to breathe. This causes a vicious cycle of inactivity, where the less exercise you get, the weaker your lungs and breathing muscles become, which in turn makes physical activity even more and more difficult to bear.
It doesn't help that COPD can cause fatigue, coughing, depression, and other symptoms that make it difficult to live an active lifestyle. Some patients give up on exercise altogether, which is devastating to their health.
Living a sedentary lifestyle will only end up making your COPD symptoms worse and can even make the disease progress more rapidly. It can also cause you to gain weight, lose mobility, and raise your risk for heart disease and a variety of other COPD complications.
Studies show that COPD patients who exercise and stay active are less likely to experience exacerbations, hospitalizations, and may even live longer than those who don't. That's why it's so important to work through your symptoms and find ways to stay active in spite of your disease.
The Solution: Stick With an Exercise Plan

Even though it may make you feel short of breath, exercise is healthy for your lungs and your overall well-being. It also helps you maintain a healthy weight and keep your physical mobility as you age.
If you have been diagnosed with COPD, then making the decision to stay active is one of the best things you can do for your health. To help keep you on track, work with your doctor to come up with an exercise plan that is realistic and sufficient for you.
If you find yourself struggling for any reason, never be afraid to talk to your doctor or ask for help and advice. If you're finding exercise too difficult because of your symptoms, ask your doctor about attending a pulmonary rehabilitation class, where you can learn how to better manage all kinds of physical challenges that come with COPD.
By keeping up with your exercise plan, you can keep your body toned, your breathing muscles strong, and live a much better quality of life with COPD.
If you need some help getting started, check out the following guides. They contain a variety of practical tips and tricks you can use today to make exercise easier with COPD.
- Home Exercises for COPD
- How Pulmonary Rehabilitation Can Help You Master Exercise with COPD
- Breathing Techniques and Exercises to Help You Manage Your Breathing
The Mistake: Not Conserving Energy

When you have COPD, you have to adjust to certain physical limitations. You will find that, over time, the disease makes many activities that you are used to doing more difficult by making you feel breathless and run down.
Many patients get frustrated when tasks that used to be easy become a struggle, triggering their COPD symptoms and sapping their energy. This can cause significant anxiety, depression, and cause some patients to give up on hobbies and physical activities they enjoy.
However, these problems can be managed by pacing yourself and learning how to better manage your limited energy reserves. Unfortunately, new patients who are still coming to terms with their limitations often deplete their energy quickly during the day, which causes them to live their lives feeling ever breathless and fatigued.
This can be incredibly disheartening for new COPD patients who haven't got the hang of managing their disease. However, by recognizing your limitations and

Health professionals are some of the most important and trusted members of our society. They’ve gone through many years of schooling and they’ve had to pass rigorous tests that make them qualified to look after our health.
While we can and should hold health professionals in high esteem, it’s important to remember that they aren’t infallible. Just like the rest of us, they are prone to mistakes from time to time.
One mistake health professionals can make is called a “diagnostic error.” This is when a patient receives a delayed diagnosis, wrong diagnosis, or missed diagnosis from a doctor which can lead to a patient using the wrong treatment or no treatment at all.
In this post, we’re going to take a look at how diagnostic errors affect people with lung diseases such as COPD, asthma, and cystic fibrosis (CF). If you have any questions, be sure to leave them in the comment section below and we’ll get back to you as soon as possible.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What is a Diagnostic Error?
According to the National Academy of Medicine, a diagnostic error is the failure to establish a timely and accurate diagnosis of a patient’s health problems or an inability to communicate them effectively. These errors are divided into three groups:
Delayed Diagnosis
This is when a disease is diagnosed much later than it should be. After a delayed diagnosis, patients may have progressed to a point in their disease where it is difficult or impossible to receive certain treatments.
Missed Diagnosis
A missed diagnosis is when a patient has symptoms that are never addressed by a health professional. It’s estimated that 100,000 people in the United States are permanently disabled or die each year due to an illness that was either delayed or missed.
Wrong Diagnosis
A wrong diagnosis or misdiagnosis is when a patient is diagnosed with a condition that they do not have. In a worst-case scenario, a patient is diagnosed with a condition that is less urgent than the condition they actually have. This can lead to the delayed onset of treatment regimes that would improve medical outcomes for the patient.
The Cost of Diagnostic Errors
Diagnostic errors pose a major health risk to people all across the country. According to the Society to Improve Diagnosis in Medicine (SIDM), diagnostic errors are found in 10 to 20 percent of autopsies, meaning that 40,000 to 80,000 people die each year as a result.
![]()
Despite the fact that diagnostic errors affect as many as 12 million Americans every year, there remains a lack of federal funding and research that could help prevent these issues. At this point in time, SIDM is the only organization that is committed to improving the timeliness and accuracy of diagnosis and combating issues associated with diagnostic error.
Another problem with diagnostic error is that it’s very difficult for a patient to take legal action if malpractice is involved. According to Nolo, a legal resource website, medical malpractice cases are some of the most difficult cases a lawyer can take on, especially those involving diagnostic errors.

There are a lot of moving parts in a medical malpractice case and it requires a patient to prove the following:
- A doctor-patient relationship existed
- The doctor did not provide treatment in a timely and skillful manner
- And the doctor’s error resulted in harm to the patient
While this may seem pretty straightforward, there’s a lot of gray area and it requires an attorney to be particularly well-versed in medical jargon and processes. As a result, attorneys often charge a high price for these cases or they will simply turn them down altogether if they believe the case is not worth pursuing. According to the Rosenbaum Firm, even with strong evidence of negligence, patients win an average of 50 percent of medical malpractice cases.
The Role of Diagnostic Error in Lung Disease
Respiratory illness is one of the most common medical conditions in the world. According to the World Health Organization (WHO), chronic obstructive pulmonary disease (COPD) alone accounted for 3 million deaths in 2016, followed closely by lower respiratory infections such as pneumonia.
Not surprisingly, patients suffering from respiratory symptoms can also fall victim to diagnostic error. One of the most common diagnostic errors in terms of lung disease is the overdiagnosis of asthma.and the underdiagnosis of COPD. Since asthma is such a common disease (1 in 13 people have it) it’s not uncommon for health specialists to jump the gun and diagnose it before doing proper testing.
On the other hand, it’s likely that COPD is significantly underdiagnosed because its symptoms are often ignored as a sign of aging. COPD can progress differently depending on the individual, so a patient may experience symptoms for years before finally seeking help. Let’s take a look at some of the top reasons lung disease is often undiagnosed or misdiagnosed.

Similarity of Symptoms
Possibly one of the most common factors affecting the diagnosis of respiratory illness is the similarity of symptoms. For example, the symptoms between asthma and COPD are almost identical making it nearly impossible to diagnose an illness simply based on the symptoms you’re experiencing.
Another problem overlapping symptoms can cause is when comorbidities are present such is the case with cystic fibrosis and bronchiectasis. Cystic fibrosis (CF) is a chronic lung disease that usually begins in early childhood and it’s inherited through genetics. This condition affects the cells that create mucus causing it to become thick and sticky. This leads to coughing, wheezing, and frequent lung infections.
Cystic fibrosis commonly causes a condition called bronchiectasis which occurs later in life. It’s caused by damage and widening of the bronchial tubes which makes it difficult to clear mucus and bacteria from the lungs. If someone has lived with CF their whole life, it may be difficult to recognize the symptoms of bronchiectasis when they appear because they are nearly identical to that of CF.
Errors in Spirometry Testing
Spirometry is a type of lung function test designed to measure how much air you can inhale, exhale, and how quickly you can exhale. While spirometry may seem like a simple test on the surface, it’s actually very difficult to interpret the results correctly. Even a small error in spirometry testing can lead to inaccurate disease diagnosis.

During a spirometry test, patients are asked to exhale for a certain amount of time into a small mouthpiece. This will provide your doctor with two different measurements: forced vital capacity (FVC) and forced expiratory volume (FEV). FVC is the total amount of air you can forcefully exhale and FEV is the amount of air you can exhale in a given period of time.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Once these values are calculated, they are compared to “normal values” based on the patient’s age, gender, height, and weight. If any of this information is entered incorrectly, it could throw off the whole test causing your health specialist to either over exaggerate or under exaggerate the severity of your symptoms.

Aside from issues with interpreting test results, there are also a number of problems that can occur during the test itself. For example, a patient may perform the test incorrectly without the moderator knowing. If the patient does not inhale fully before blowing into the mouthpiece or they have air leaking out the side of their mouth when they exhale, the results could be under interpreted.
Ultimately, there are a lot of different factors involved in getting accurate results from a spirometry test. The test results can easily become skewed if the patient is not aware of how to perform it or the technician conducting the test is careless or inexperienced. When this happens, the results may be misleading or unhelpful when it comes to diagnosing a lung condition such as COPD.
Lack of Appropriate Testing
Another factor that can lead to diagnostic error is a lack of appropriate testing. A medical specialist may not perform the right tests or they may not perform enough tests to get an accurate picture of a patient’s lung condition.
While spirometry is often considered to be the most effective test for diagnosing COPD and asthma, other tests may be more effective when it comes to diagnosing other chronic lung diseases, especially the less common ones.

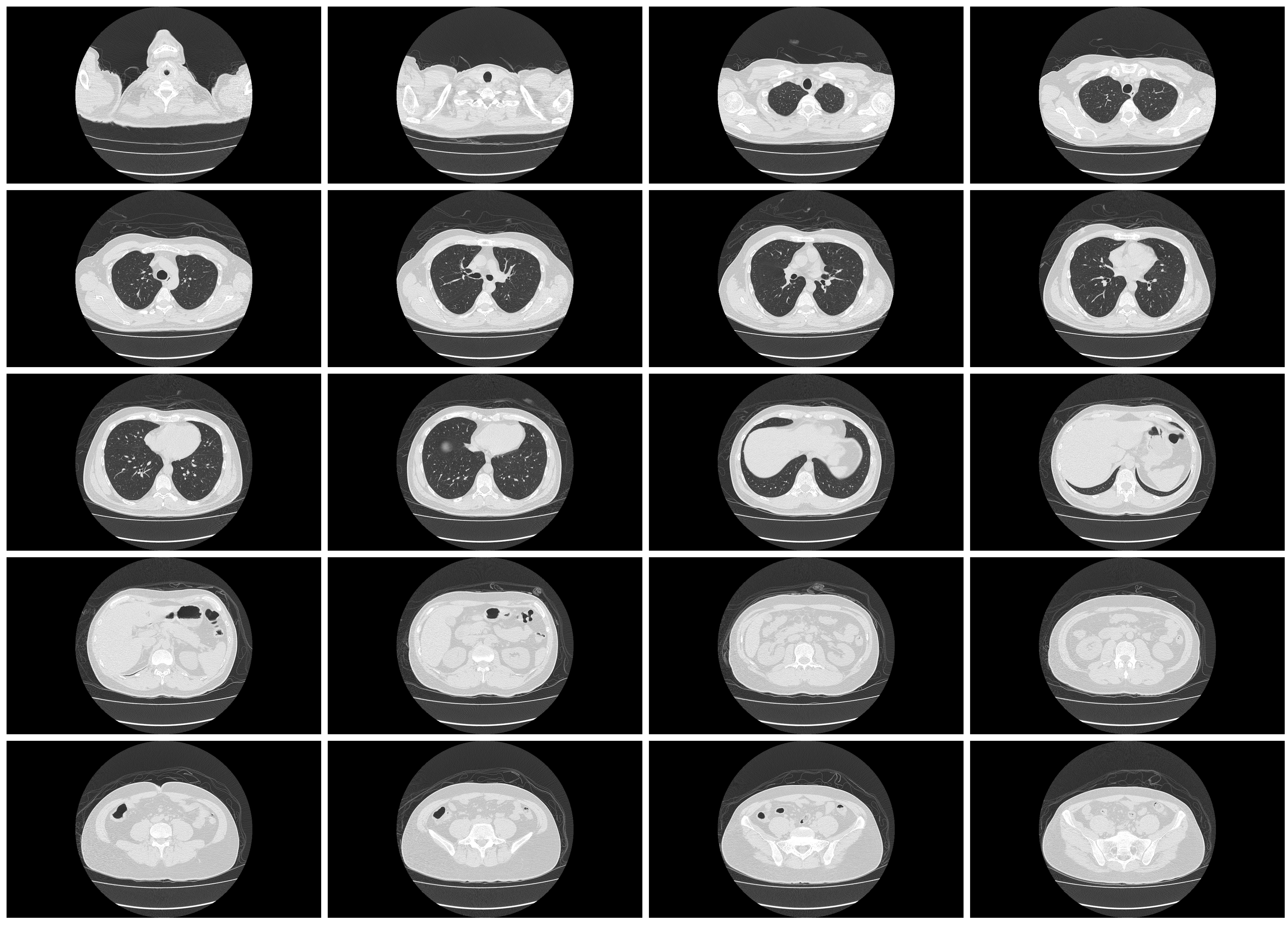
High-resolution computerized tomography (CT) scanning is one test that can be extremely beneficial in diagnosing lung disease. This is similar to an X-ray, but the computer will take multiple pictures from different angles.
Once the images are collected, the computer uses processing to make cross-sectional images of all the tissues in the lungs. Although X-rays can be useful in diagnosing some conditions, CT scans provide medical specialists with a much more detailed view of what’s going on in your lungs.
CT scans help to provide evidence of things like interstitial lung disease, an umbrella term for diseases that cause scarring (fibrosis) in the lungs. It can also be used to provide additional evidence for COPD and other lung diseases in order to provide a more accurate diagnosis.
Last but certainly not least, blood gas analysis can be useful in diagnosing many respiratory illnesses. Your doctor will either recommend that you have your blood drawn so that it can be tested in a lab, or he/she might use a pulse oximeter for a less intrusive option. This is a small device that slips over your finger.
Blood tests will provide your doctor with a lot of important information such as your partial pressure of oxygen (PaO2), partial pressure of carbon dioxide (PaCO2), pH, bicarbonate (HCO3), and oxygen content (O2CT).
Threshold for Defining COPD
Threshold is the value that needs to be crossed in order for COPD to be diagnosed. Currently, the threshold for COPD is an FEV1/FVC ratio of 0.70. While this is considered by many to be the most optimal threshold for COPD, there are other methods out there such as the lower limits of normal (LLN) method.

The LLN method uses an additional step of comparing the FEV1: FVC ratio to demographics such as age, height, race, and gender in order to determine a “normal.” A recent study, however, showed that the fixed threshold of 0.70 was consistently more reliable and accurate than LLN and other methods of diagnosing COPD.
If you’re concerned at all about a diagnosis that you did or didn’t receive, it never hurts to discuss them with your doctor. He/she will likely be very open about the methods used to come to a conclusion, and if you still have doubts, there may be an opportunity to get retested or have your doctor double-check the results.
Miscommunication Between Doctor and Patient
Possibly one of the most common reasons for respiratory illness being misdiagnosed is a miscommunication between a doctor and his/her patient. For example, a patient might wait too long to address their symptoms with their doctor or they might forget certain details about their symptoms.

Genetics is also a major determining factor of whether someone can develop a lung disease so if a patient miscommunicates their family’s history of illness, it may be significantly more difficult for their doctor to discover the root of their problems.
There are many mistakes that can occur on the doctor’s side as well. For example, he/she could keep inaccurate information about your height, age, gender, or weight which could skew the results of any test you take.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
What You Can Do to Ensure Accurate Diagnosis
Be Open and Honest With Your Doctor
The best thing you can do in order to prevent diagnostic errors is to be open and honest with your doctor. Unfortunately, when people start experiencing respiratory problems, their first instinct is to shrug them off as a sign of aging or they wait until their symptoms have progressed to a point where they need to seek help.

Alternatively, you should be contacting your doctor as soon as problems arise. Most conditions such as COPD and asthma can be treated more effectively if they are diagnosed early on. These are both progressive diseases, so there is no way to cure them or reduce the damage effects. All you can do is prevent further damage from occurring.
Don’t be Afraid to Ask Questions
Another thing to remember when you go to the doctor is that there’s no such thing as a silly question when it comes to your health. Chances are if there’s something you’re wondering about, there’s always someone else out there wondering the exact same thing. So, when you go in for a doctor’s appointment, don’t be afraid to ask questions, whether they pertain to your symptoms, treatment plan, or anything else.

Another reason to ask a lot of questions is that it gives your doctor a better understanding of your concerns and more importantly, the way your condition is progressing. The more your doctor knows about your respiratory symptoms, the better he/she will be able to prescribe treatments that work for you.
Schedule Regular Doctor’s Visits
Lastly, you’re going to want to schedule more frequent doctor visits. At the end of the day, the more you communicate with your doctor, the easier it will be for him/her to track your progress. And even if you aren’t experiencing severe symptoms, your doctor may be able to diagnose you sooner, leading to better outcomes. It’s recommended that people 30 years old and younger should visit the doctor once every couple of years. But the older you get, the more frequently you should go.
![]()
Conclusion
Diagnostic error is always a possibility. However, you can significantly improve your odds of receiving a timely and accurate diagnosis by scheduling more frequent doctor visits, not ignoring respiratory symptoms, and not being afraid to ask a lot of questions. As a last resort, you always have the option to file a lawsuit if you believe that negligence or malpractice was involved.
Here at LPT Medical, we aim to provide respiratory patients with transparent and helpful resources for managing their disease. If you’re in the market for a lightweight portable oxygen concentrator like the Inogen One G5 or the Caire FreeStyle Comfort, our respiratory specialists would be glad to help you out by answering any questions you may have. Fill out the contact form at the side of the page to get started.
Chronic obstructive pulmonary disease (COPD) is one of the most common lung diseases in the world. It’s estimated that about 16.4 million people in the United States alone have COPD and millions more are either undiagnosed or at high risk of contracting it. Despite this fact, many people are woefully unaware of what causes this disease and how it should best be managed.
In short, COPD is an umbrella term that denotes two conditions: chronic bronchitis and emphysema. While the symptoms and pathogenesis of these two diseases are slightly different, they are both primarily caused by cigarette smoking. However, in rare instances, someone who has never smoked can contract COPD through something called alpha-1 antitrypsin deficiency (AAT deficiency).
One of the symptoms of COPD that’s particularly vicious is something called an exacerbation. This is similar to an asthma attack in that it causes respiratory symptoms such as breathlessness, chest pain, and sputum production to suddenly become worse, oftentimes requiring you to seek immediate medical attention. In this post, we will help you better understand COPD flare-ups and exacerbations, as well as how to avoid being hospitalized as a result.
If you have any questions or concerns, feel free to leave them in the comment section so we can address them.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What’s the Difference Between a Flare-Up and an Exacerbation?
Generally speaking, the terms “COPD flare-up” and “COPD exacerbation” are used interchangeably. They both refer to respiratory symptoms becoming worse due to environmental causes, infections, or any number of other things. However, when it comes to discussing these symptoms, it’s important to be precise not only about what’s causing them but how severe they are as well.

A mild COPD exacerbation is one that could lead to increased discomfort but is unlikely to cause any serious long-term consequences. These can typically be treated with short-acting bronchodilators (SABD) or “rescue inhalers” which work to quickly open up the airways allowing you to breathe better. Moderate COPD exacerbations should be supplemented with oral corticosteroids which suppress inflammation and antibiotics which can help fight inflammation.

The final type of exacerbation is a severe exacerbation, sometimes called an “acute” exacerbation. This type of exacerbation requires immediate medical attention and can even be life-threatening if it’s not treated appropriately. Ideally, the best way to prepare for this type of exacerbation is to have an action plan and ensure you always have someone on hand to either take you to the hospital or call an ambulance.
Why it’s so Important to Avoid Hospitalization With COPD
According to the American Journal of Respiratory and Critical Care Medicine, COPD is responsible for $72 billion a year in direct healthcare expenditures. The majority of these costs come from hospital visits which range from 4.5 to 8.8 days on average. Around two-thirds of all COPD hospitalizations are due to COPD exacerbations, and the majority of COPD exacerbations are caused by infections — specifically viral infections.

The primary reason it’s important to avoid hospitalization for COPD is because of the risks for your health. According to another study by the aforementioned medical journal, after testing over 2 million patients, the 1-year readmission rate was 64.2% and the 1-year mortality rate was 26.2% both of which were significantly higher than rates among the general COPD population. Readmission and mortality rates are also much higher among patients who were hospitalized with severe exacerbation of COPD.
The second most important reason to avoid hospitalization due to COPD is cost. Frequent or long-term admissions can pose a significant financial burden on people with COPD which can also lead to stress, anxiety, and even depression. In our last post, we highlighted some key ways that you can avoid unnecessary financial costs due to COPD so check it out if you’re interested in learning more.
Have a Plan to Deal With Exacerbations
First and foremost, if you want to avoid hospitalization due to COPD exacerbation, you need to have a plan of action before an emergency occurs. An action plan is a sort of written outline that you will follow in order to accomplish a certain goal. This way, if you notice your COPD symptoms starting to worsen, you can refer to your sheet instead of worrying about making difficult decisions at the moment.

In order to prepare your COPD action plan, you should first consult your doctor. He/she will likely already have a template that you can fill out to make this process a little easier. On this action plan, you will need to create an “action” for every symptom you experience. For example, if the symptom is a gradual decrease in your blood oxygen levels, you might make a note to increase your oxygen flow setting or contact your doctor. If you experience sudden shortness of breath, you might make a note to use your rescue inhaler.
Another important thing to know about your COPD action plan is that it should not be private information. You should make it a priority to go over your plan with friends and family, especially if they spend a lot of time with you. This way, if you are in a situation where you are unable to act out your action plan, they will be able to help. In this post, we discuss how you can prepare for medical emergencies and hospital visits with COPD, so check it out if you want to know more.
![]()
Change Up Your Diet
Diet can be a very difficult topic to discuss in this day and age. Most people have access to more types of food than ever before and there is a near endless list of diets that people swear by. As a result, it can feel like an insurmountable task trying to find something that keeps you happy and healthy. The good news, however, is that many years of research have been dedicated to COPD diets, so you shouldn’t have to do much scrambling to make sense of it all.
![]()
Generally speaking, COPD patients should maintain a diet that’s high in protein, fiber, and fat, but low in carbohydrates. The reason for this is that the metabolism of carbs produces the highest amount of carbon dioxide in the body while the metabolism of fat produces the least. Adequate protein ensures your respiratory muscles stay strong and efficient, and fiber helps to control blood glucose levels and reduce cholesterol in the blood.
Another reason to keep your diet healthy, natural foods rather than processed ones is because weight management is vital to COPD management. Most often, people tend to become underweight after contracting COPD due to a loss of appetite or other factors. Sometimes, people experience a loss of appetite because consuming food is more physically exerting than it was previously, and bloating can contribute to breathing difficulties. COPD patients who are underweight may find that they lack the energy or endurance to make it through the day.
On the other hand, being overweight with COPD can contribute to breathing problems as well. While it is less common for a COPD patient to become overweight than underweight, the problems associated with it can be just as severe. Simply put, having a higher body mass index (BMI) can be obstructive to your breathing by putting more strain on your lungs when you inhale. However, some studies have found mixed results when it comes to being overweight/obese with COPD.
Be Consistent With Your Exercise Routine
Consistency is unbelievably important when it comes to treating COPD and preventing exacerbations. For example, your diet is much more likely to benefit you if you keep up with your goals week in and week out. But if you do well one week then cheat the next, you’re going to put yourself at a much higher risk of COPD complications like exacerbations. This works pretty much the same way when it comes to your exercise routine.

Oftentimes, exercise specialists will talk about getting into a “routine.” In other words, you do the same exercise each day for an allotted period of time. By doing so, it will be much easier to track your progress and catch yourself when you fall back on your plan. This works well for most people who want to commit to an exercise routine, but it’s especially useful for COPD patients who benefit more from consistent moderate exercise rather than high-intensity exercise.
Avoid Getting Sick
Lung infection is both the number one cause of severe COPD exacerbation and the number one cause of hospitalization due to COPD. With that being said, staying healthy and avoiding infection (especially lung infections) is vital. One of the best things you can do right now to avoid getting sick is to quit smoking or avoid second-hand smoke if you live around smokers.
It’s been known for quite some time that smoking reduces the immune response in the body and also makes the smoker more likely to have exaggerated responses to viral infections. During influenza outbreaks and with the current situation we face involving COVID-19, smokers have a much lower survival rate when compared to the general population. Not to mention that smoking and second-hand smoke can trigger COPD exacerbations even if an infection isn’t present.

Another thing you can do to avoid getting sick is to be more conscious of your daily habits. For example, do you wash your hands frequently throughout the day? Do you take care to avoid places that are unclean or unsanitary? Do you stay away from people who exhibit symptoms of the cold or the flu? Do you clean surfaces in your home like door handles, coffee pot handles, or faucet handles? Are you following all the precautions recommended by the World Health Organization (WHO) in order to prevent contracting the novel coronavirus?
Last but certainly not least, you should be getting the doctor-recommended eight hours of sleep each night in order to avoid getting sick. According to WebMD, sleep deprivation suppresses the immune system and puts you at a higher risk of contracting colds, the flu, and other ailments. This is an especially difficult topic for many COPD patients because respiratory symptoms can make it difficult to maintain a healthy sleep schedule. In this post, we take a look at some actionable tips to improve your sleep if you have COPD.
Avoid Environmental Triggers
It can be a scary world out there for anyone who values their lung health. From wildfire smoke to car exhaust and pollen, it’s easy to feel like no place is safe. The Environmental Protection Agency (EPA) even reports that indoor air can be two to five times more polluted than outdoor air. Fortunately, it’s not all grim news for COPD patients who want to avoid exacerbation triggers. Just by following a few simple steps, you’ll be well on your way to avoiding the most common triggers.

Despite summer ending last week, we are still in the midst of wildfire season. As a result, COPD patients need to be aware of when they go outside, especially when it concerns exercising outdoors. Air quality index (AQI) is the measurement we use to determine how safe outdoor air is to breathe. Each day before you go outside, be sure to check AirNow.gov for the AQI in your area. If the AQI is above 100, this is a sign that the air quality is too poor for people with lung diseases like COPD, asthma, or pulmonary fibrosis.
Another thing you should be wary of is seasonal allergies. Contrary to popular belief, allergies are a reality during all times of the year as opposed to only being active during certain seasons. In September and October, allergens like ragweed are typically at their peak. According to WebMD, if you get allergies in the spring, you are about 75% likely to have reactions to ragweed. So, if you’re outside this trying to enjoy the fall colors and cool weather this year, just be aware that allergies are still a reality.

The final airborne COPD exacerbation triggers we’d like to talk about are the ones found in your home. Like we mentioned earlier, indoor air can potentially be more dangerous than outdoor air. This is because the air in your home is extremely concentrated, so if you track things in like dust, allergens, or smoke, it will likely start to build up in one area of your home unless you take the time to clean regularly. While it may not seem that important, taking the time to vacuum, dust, and wipe down surfaces every day can go a long way to preventing COPD exacerbations. What’s more, it will help you get your daily exercise.
Use a Reliable Portable Oxygen Machine
Last but certainly not least, having a reliable portable oxygen device that you can take anywhere will put you in the best position to avoid COPD exacerbations and hospitalization. For the vast majority of COPD patients, supplemental oxygen therapy is a medical necessity. Not only does it stabilize your lung condition, but it also ensures your blood oxygen levels are normal, which in turn saturates every organ in your body with the oxygen it needs to function properly.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
For the foreseeable future, portable oxygen concentrators are your best bet for reliable portable oxygen. Unlike oxygen tanks or liquid oxygen tanks, portable oxygen concentrators are electronic devices. So, instead of having to go out of your way constantly to have your tanks refilled by an oxygen specialist, you simply need to carry batteries with you. Fortunately, these batteries are lightweight and don’t take up very much space in your backpack or handbag.

Currently, the best portable oxygen concentrator on the market is the Caire FreeStyle Comfort. It weighs in at only 5 pounds and it offers 5 different flow settings that you can adjust on the fly as needed. One of the unique features of the FreeStyle Comfort is its ergonomic design which keeps the device comfortably at your side rather than jostling around as some other concentrators do.

Another portable oxygen concentrator we’d like to recommend is the Inogen One G5. While this POC came out last year, it’s still very relevant and a great choice for anyone who needs a reliable 24/7 medical oxygen supply. The Inogen One G5 has one more pulse flow setting than the FreeStyle Comfort and it weighs slightly less at just 4.7 pounds. Inogen is one of the top brands in the medical oxygen industry and they take pride in customer satisfaction.
In rare instances, your doctor may require you to use a continuous flow concentrator. If this is the case, we recommend the Respironics SimplyGo portable oxygen concentrator. This unit is twice as heavy as the Caire FreeStyle Comfort, but since it puts out a continuous flow of oxygen, it can be used with your CPAP or BiPAP machine if you have sleep apnea or another related sleeping disorder. If you’re looking for affordable portable oxygen concentrators, don’t hesitate to visit our online oxygen store.

Conclusion
Unfortunately, exacerbations and flare-ups are a reality for COPD patients. But that doesn’t mean that you can’t take steps to reduce your risk of experiencing hospitalization due to an exacerbation. Above all, following your treatment plan as closely as possible and preventing sickness like the cold or flu will be your best bet if you want to avoid hospital visits.
If you would like to learn more about managing chronic respiratory conditions such as COPD, stay tuned to our blog. We aim to equip our readers with the knowledge they need to combat breathlessness, chest pain, and fatigue in their daily lives, as well as learning how to cope with the mental aspects of chronic disease like anxiety and depression. Feel free to leave a comment below if you have any questions or concerns.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













