
Allergy season is a nuisance for anyone who suffers from allergies, but it can be a serious struggle for people who also suffer from COPD. Common allergens like pollen, dust, and mold can not only cause uncomfortable allergic reactions, but they can also irritate your lungs and airways and make it more difficult to breathe.
At least one in five people in the US suffer from allergies, and that includes many people who also have COPD. Unfortunately, there hasn't been a lot of research on how the two conditions interact, and there are few official treatment guidelines to help COPD patients manage their allergies.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
However, thanks to research from John Hopkins University, we do know that people who suffer from both allergies and COPD are more likely to have worsened symptoms and shortness of breath. They are also more likely to experience exacerbations, which are episodes of increased symptoms that can be serious and even require hospitalization.
Currently, the best known way handle allergies when you have COPD is to treat the symptoms with medication. The best treatment, however, is prevention to keep you from having allergic reactions at all.
If you do your best avoid exposure to pollen, dust, and other allergens, then you can prevent your symptoms from worsening in the first place. That's why, in this guide, we're going to give you a variety of effective tips and techniques to help you keep allergens at bay and prevent them from making your COPD worse.
How Allergies Affect COPD

Seasonal nasal allergies, also known as allergic rhinitis, tend to peak in the summer. However, they can start as early as the spring and last late into the fall, since these warmer months are when plants, mold, fungi, and dust mites thrive.
Some people experience allergies during the winter, too, although it is less common. Most winter allergies come from spending extra time in indoor places with dust and mold.
All of these different factors can trigger respiratory symptoms for the more than 24 million people in the US who suffer from seasonal allergies. But for people who suffer from COPD as well, the pollen, mold spores, and generally poor air quality can actually make their disease worse.
If you suffer from allergies and breathe in allergens like pollen or mold, it triggers the release of histamine that affects your upper and lower respiratory tracts. Histamine causes an inflammatory response, causing irritation, swelling, and increased mucus secretion in the lungs and airways.
Here are some common symptoms associated with seasonal allergies:
- Itchy, watery eyes
- Runny nose
- Nasal and sinus congestion
- Excess mucus production
- Coughing and sneezing
As you can see, many allergy symptoms are respiratory symptoms that have the potential to interact or compound with existing symptoms of COPD like coughing, wheezing and shortness of breath. For example, an allergic reaction can cause excess mucus production and swelling in the airways, which in turn blocks airflow and makes it even more difficult to breathe.
In extreme cases, this can cause a COPD exacerbation, but even minor allergic reactions can be troublesome. When COPD already makes it difficult to breathe and keep your airways clear of mucus, you can't afford to have allergies making the problem even worse.
If you experience allergy symptoms on a regular basis, especially if you notice that they get worse when you spend time outdoors, you might be suffering from seasonal allergies. You should visit your doctor as soon as possible to get an evaluation so you can find an allergy medication to control your symptoms.
Allergies can be uncomfortable for anyone, but if not properly treated they can be serious and debilitating for people who suffer from other respiratory conditions like COPD. It's important for COPD patients to take any increase in respiratory symptoms seriously, because they can quickly lead to serious complications or exacerbations.
Talk to your doctor about tips and techniques for reducing allergens in your home and keeping your symptoms in check when your allergy triggers can't be avoided. Make sure to follow your COPD treatment plan whenever you experience worsened symptoms, and seek medical attention if they get severe or don't go away.
To prevent your symptoms form getting to that point, continue reading this guide for a multitude of tips and tricks to help you avoid and eliminate allergy triggers this season. We've put together a number of ideas and techniques that will help you keep your home hypo-allergenic and allow you to stay happy, healthy, and comfortable throughout allergy season and the rest of the year.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
How to Manage Summer Allergies When You Have COPD
Know Your Triggers
Allergens are everywhere; in the air we breathe, the food we eat, and in our carpets, furniture, and clothes. However, how these allergens effect every individual person is different, and some people are more sensitive to certain types of allergens than others.
If you have COPD and suffer from allergies, it's important to talk to your doctor about your symptoms so you can identify the source. Getting an allergy test or keeping a diary of your symptoms can help you narrow down the possibilities and help you better understand what triggers your allergic reactions.
Once you know what's causing your allergies, you can take steps to avoid coming into contact with whatever causes your symptoms. Read all of the tips in this article to learn techniques for doing just that and to find new ideas and inspiration for keeping your allergies at bay.
Check Allergen Reports
There are many places you can check to get information about allergy conditions in your local area on any given day. You can check your local weather report, pollen.com, or other online sources like The Weather Channel to get daily forecasts for the levels of pollen and other particles in the air.
Some allergy reports give detailed information for specific types of pollen, including pollen from trees, grass, and weeds. This can be helpful if you know which specific plants and types of pollen tend to trigger your allergy symptoms.
You can use this information to schedule outdoor activities and plan your exercise on days when pollen levels are lower. When pollen and other allergens are high, it's best to stay indoors as much as possible to keep it from making your COPD worse.
Take Daily Allergy Medication

No matter how hard you try, you're not going to be able to avoid all of your allergy triggers all the time. Your symptoms are bound to act up at least occasionally, and doctors often recommend taking daily allergy medicine all throughout the allergy season to prevent symptoms before they get worse.
If you suffer from allergies and COPD, it's essential to talk to your doctor and get an allergy medication that works for you. If you don't treat your symptoms daily, they can continue to get worse and cause your COPD to flare up.
Many people have to try a few different allergy medications before they find one that effectively treats their symptoms. Make sure to take your medicine as directed and work with your doctor to find a medicine that's effective for you.
Also, remember than many kinds of allergy medications work best when you take them consistently at the same time every day. They are often less effective if you take them irregularly or skip a dose, which can worsen your symptoms and make your allergies more difficult to control.
Stay Indoors When Pollen and Humidity are High

Sometimes the best way to avoid allergens is to avoid going outside altogether. Of course, you can't avoid going outdoors all the time, but it's a good idea when the allergy forecast looks bad.
Whenever pollen levels are extremely high, you should try to stay indoors as much as possible. Close all your windows, shut all your doors, and turn on your home ventilation system to control allergy levels in your house.
Humid days can also be a problem, since they tend to encourage mold and dust mites to proliferate. Humidity traps smog and lowers air quality, which can be especially irritating to your lungs and airways if you have COPD.
Take Antihistamines
Even if you take allergy medication daily, your allergy symptoms can still act up for many reasons. Being sick, fatigued, or exposed to allergens on high-pollen and high-humidity days can trigger allergic reactions that take a little extra help to keep at bay.
When this happens, taking an antihistamine like benadryl can give your body the extra help it needs to get over the symptoms. However, use them carefully, because antihistamines can sometimes dry up your mucus, make it thicker, and cause you to have even more trouble breathing.
That's why it's important to talk to your doctor before you use any new medication. Whenever your symptoms get worse, you should always follow your COPD action plan first and consult a medical professional before trying any other medicine.
See a Doctor if Your Allergies Get Out of Hand

Sometimes, despite your best efforts to avoid triggers, an allergy attack can hit you out of nowhere. When you have COPD, it's important to seek medical attention right away if your symptoms suddenly worsen and don't get better fast.
Doctors can prescribe you oral or nasal steroids to deal with acute allergy attacks and COPD exacerbations. They can also give you antihistamines, steroid shots, and breathing support if you need them.
Get an Allergy Tracking App for Your Phone
Checking multiple weather and allergy forecasts every day can be bothersome and easy to forget. Luckily, there are a number of great android and iPhone apps you can get that let you track allergy forecasts right on your phone.
Pollen.com has a popular app for both iPhone and android called Allergy Alert that tells you everything you need to know about pollen levels in your area. You can input multiple locations and get accurate 5-day allergy forecasts with detailed information about the types of pollen that are prevalent.
The Allergy Alert app also includes an allergy diary where you can record your daily symptoms and keep track of how your allergies change throughout the season. You can even print out your diary as a chart or calendar to help you and your doctor keep tabs on your symptoms.
Other great allergy apps include WebMD Allergy, Zyrtec AllergyCast, and Allergy Advisor. You can download all of these apps from the Apple or Google app stores.
Allergy-Proof Your Home
Get a Good HVAC Air Filter
All home HVAC ventilation systems include an air filter that has to be cleaned or changed out on a regular basis. Some filters only need to be changed once per season, but others should be swapped out more often, every couple of months or so.
Not all air filters are created equal, and some are much more effective than others at getting out the tiny particles that trigger allergies. Most filters include a MERV rating, which is a standard rating that tells you what kinds of particles a filter can and cannot screen out.
A lower MERV rating is associated with low-quality air filters, while high MERV ratings are given to more effective filters. You should always look for a hypo-allergenic air filter that's fine enough to catch tiny allergens like pollen and mold spores.
Get a Good Air Purifier
While a decent HVAC air filter is important for indoor air quality, you can step it up a notch further by getting a mechanical air purifier. These devices use multiple filters and even UV light to remove allergens from the air much more effectively than an HVAC filter alone.
Air purifiers come in a variety of qualities and sizes, and what kind you get depends on your individual needs. You can get a small, portable device for use in a single room or you can even get a large, whole-house air purifier that hooks up to your home's main ventilation.
Some air purifiers are better than others, and their advertising can be deceptive. Look for air purifiers that are certified by the Asthma and Allergy Foundation of America (AAFA) to ensure that the one you buy can filter common allergens from the air.
HEPA filters are considered to be one of best high-quality air purifiers and is the gold standard for mechanical air filtration. They use multiple filtration steps and can screen out least 99.97% of particles that are 0.3 microns or larger from the air.
Use Smooth Surfaces and Avoid Fabrics

Hardwood floors and tile are much easier to clean than carpet, and they don't collect pollen and other particles like carpet fibers do. Likewise, decorating with fabrics like curtains and rugs provides more places in your home for allergens to build up.
To prevent bothersome allergens and harmful irritants from hanging around your home, make sure to vacuum and dust all surfaces in your house regularly. Don't forget little-used areas like basements and closets, and consider getting rid of rugs, curtains, and other items that attract dust.
It can also help to furnish your house with couches, chairs, and other furniture that won't collect allergens. Wood, leather, and other similar materials are easy to wipe clean, while soft fabrics attract pollen and dust and are difficult to clean thoroughly.
Rinse Off after Being Outside

It's a good idea to take a shower or a quick rinse when you arrive home after being outdoors. Especially if you've been near a lot of grass, trees, or other foliage, you could be carrying a large amount of pollen and mold spores on your person.
But if you take the time to rinse the allergens out of your hair and skin, you'll avoid carrying them around with you throughout the day. It will also prevent you from scattering allergens about your home where they can build up and make your symptoms worse for days.
Change Clothes When You Come Indoors

Pollen and other allergens tend to stick to your clothes and shoes when you spend any extended amount of time outdoors. Especially if you don't have time to shower, you should change into a fresh set of clothes so you don't track allergens all throughout your house.
De-clutter and Deep Clean
Dust mites, mold, pollen, and other allergens can hide in any nook and cranny. That's why it's important to do a thorough, deep cleaning at least a couple times a year, especially if you suffer from allergies.
Your deep clean should include removing any clutter and cleaning behind furniture, cabinets, and other belongings. You don't want to leave any stone unturned, that way you start out with the cleanest, most allergy-free space possible.
You should also extend your deep cleaning to other spaces you spend time in, like your car and garage. Clear out any clutter, vacuum your car seats and mats, and don't forget to wash the outside, too.
Replace the Cabin Air Filter in Your Car
If you have a long commute or take extended trips in your car, having a clean cabin air filter can improve your allergy symptoms. The cabin air filter traps particles from the air that flows through your car's ventilation system, and you should replace it often during the summer when it collects extra pollen and mold.
How often you should do this depends on your car, and your owner's manual will help you figure out the exact time frame. However, as a general rule, the Car Care Council recommends changing out your cabin air filter at least every 12,000 to 15,000 miles you drive.
Dust and Vacuum Regularly

A good air filter or purifier will remove most allergens from the air in your house, but it can't do anything about the dust, pollen, and mold spores that settle on the surfaces in your home. To get rid of all that, you have to dust, vacuum, and sweep regularly.
Don't forget to clean out-of-the-way spaces like high cabinets, closets, corners, rugs and drapes. These are common places where dust and mold tend to collect that people commonly overlook when cleaning.
Check Problem Areas for Mold and Mildew
 |
| Image courtesy of carlpenergy on Flickr. |
There are certain places in houses that tend to have a higher risk of mold build-up. These include basements, bathrooms, attics, crawl spaces, and any areas that might get damp.
You should inspect these areas in your home somewhat regularly to spot mold and mildew growth before it gets out of control. Some mold spots can be cleaned yourself by hand, but you might need to call in a professional for larger problems.
It's also important to identify and repair any leaks in your pipes so they don't cause mold to grow in your walls. If you notice your allergies are acting up in your house, getting it thoroughly inspected for mold and fungus by a professional could help you find and take care of any problems.
Promptly Clean Damp Spots
Water mishaps are not uncommon occurrences in homes. You can never predict when a faucet will burst or a heavy storm will flood your basement.
What you can do, however, is make sure to clean up any spills, floods, or other damp spots as quickly as possible after they happen. If any area remains damp for more than 48 hours, you're almost certain to get mold growth.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Control the Humidity in Your Home

When the humidity in your house climbs higher than sixty percent, the chance for mold growth greatly increases. That's why you should try to keep your home's humidity levels between thirty and fifty percent.
You can do this by using a dehumidifier when the weather is especially humid outside. You can get small, portable dehumidifiers that work for a single room, or you can invest in whole-house units that pull moisture out of all the air in your home.
Running the air conditioner in the summer is another effective way to reduce moisture in the air, as long as the humidity isn't too high. It also helps to vent appliances like dishwashers and dryers outdoors, and to make sure you always open your window or turn on your vent fan when you take a shower.
Wash and Groom Your Pets

If you have pets, they can be a major contributor to your allergies. It's important to wash and groom them regularly to reduce the amount of allergens they bring into your house.
When dogs and cats go outside, all kinds of pollen, dust, and mold spores that are in the grass and in the air stick to their fur. When they come inside, all of those allergens are transferred from their fur onto any carpet, clothes, and furniture they come in contact with.
Giving your pets baths and brushing them regularly helps prevent these allergens from building up in their fur and causing your allergies to act up. It also helps to keep your pets off of your furniture and bedding, so you won't be sitting and sleeping in places where your pets have tracked pollen.
Get a HEPA Vacuum Cleaner
A regular old vacuum can get a lot of the pollen, dust, and other allergens out of your carpet and furniture, but it can only do so much. Sometimes vacuuming can even scatter these particles into the air and actually make your allergies worse.
In order to allergy-proof your home more effectively, you can get a vacuum with a HEPA filter that removes at least 99.97 percent of particles that are 0.3 microns or larger. A regular vacuum can only filter particles that are 50 microns or larger.
Just make sure you get a HEPA filter-compatible vacuum that's large enough to fit the size of your home. Otherwise, you'll end up having to change the filter quite often in order to keep it working properly.
Conclusion
When you have COPD, any problems that affect your respiratory tract and make it difficult to breathe are automatically more serious. Even minor allergies can lead to worsened coughing, wheezing, and breathlessness associated with COPD.
Fortunately, it is totally possible to take control over your allergies and keep yourself healthy during allergy season. It just requires some extra cleaning, extra planning, and arming yourself with the right equipment to keep allergens out of your home.
The relationship between allergies and COPD is still not completely understood, and doctors are still trying to gather more research and information on this topic. But for now, treating symptoms with medication and avoiding the allergens that trigger them are the best way to handle allergies when you have COPD.
If you use the techniques in this guide you'll be able to better protect your lungs and airways from allergy-triggering particles like like pollen, mold, and dust. You'll be able to breathe easier, feel better, and enjoy life even when allergy season is in full swing.
If you suffer from any number of respiratory ailments, you’re likely well aware of the important role oxygen therapy plays in your life. COPD patients, in particular, are able to significantly reduce chronic symptoms like breathlessness and chest pain by using supplemental oxygen on a daily basis. On the other hand, short-term oxygen therapy can assist patients in recovering more quickly after a hospital visit.
But if you’ve kept up with our blogs here at LPT Medical, you know that the way oxygen is administered is often just as important as using supplemental oxygen in the first place. Receiving too little oxygen might cause a flare-up in your symptoms, whereas receiving too much oxygen could lead to oxygen toxicity and other health complications.
One of the first things you should understand about oxygen administration is the difference between a pulse dose oxygen concentrator and a continuous flow oxygen concentrator. While each of these oxygen delivery methods is viable, they each have their pros and cons, and your oxygen therapy experience will vary greatly depending on which one you choose.
Ideally, this post will cover everything you need to know about pulse flow and continuous oxygen concentrators. However, if you still have questions, fill out the form to the right of the page and one of our respiratory specialists will reach out to you.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What is a Continuous Flow Oxygen Concentrator?
As the name suggests, a continuous flow oxygen concentrator administers a constant flow of oxygen to the respiratory patient. A good analogy for continuous flow oxygen is a water fountain. When you use a water fountain, you don’t drink all of the water that is coming out of the spout. The water fountain puts out a consistent amount of water and the amount you drink is a product of the amount and the size of sips that you take. Similarly, with a continuous flow oxygen concentrator, the amount of oxygen that enters your lungs is a product of the amount and size of breaths that you take.

Another medical oxygen device that uses continuous flow oxygen administration are oxygen tanks. Since oxygen tanks used compressed oxygen they don’t need any electrical components to push oxygen out the nasal cannula. All they need is a nozzle that can regulate the amount of oxygen that is coming out of the tank. Liquid oxygen tanks use a similar principle, but instead of the oxygen being compressed inside the tank, it’s compressed as it exits the tank and turns to gas.
They Offer Great Versatility
Possibly the greatest thing about continuous flow oxygen concentrators is how versatile they are. Continuous flow units can be bought as either a portable or a stationary oxygen concentrator (home oxygen concentrator) so you’ll have options based on your wants and needs. Portable oxygen concentrators have batteries so you can use them wherever you want, however, stationary concentrators need to be plugged into a wall to operate.

Another great thing about continuous flow portable oxygen concentrators is that they typically offer a pulse flow setting as well. This can be confusing to many people because when they hear the term “continuous flow portable oxygen concentrator” they assume that it doesn’t offer a pulse flow setting. However, oxygen concentrators like the SeQual Eclipse 5, for example, offer continuous flow settings 0.5-3.0 LPM, but it also offers pulse flow settings 1 through 9. This is much more than what your average pulse flow oxygen concentrator will provide.
They’re CPAP Compatible
COPD commonly coexists with sleeping disorders like obstructive sleep apnea in what’s known as COPD-OSA overlap syndrome. This is partially due to the fact that OSA and COPD are both common conditions, but the higher likelihood of peripheral edema and increased BMI associated with chronic bronchitis also promotes OSA. As such, someone with COPD is more likely to experience sleep disorders.

When a patient with OSA sleeps, their airways collapse making it difficult to breathe properly. If this person also has COPD, they’ll be more likely to experience complications at night due to the restricted airflow. In these situations, it’s advised that the patient uses both a continuous positive airway pressure (CPAP) machine and an oxygen concentrator while sleeping.
Continuous flow is the only type of oxygen administration that is compatible with CPAP and BiPAP machines. Some continuous flow oxygen concentrators can be attached directly to a CPAP machine, but others will require you to buy a “bleed-in adapter.” If you and your doctor determine that this is the best course of action for you, be sure to follow the directions closely in your oxygen concentrator user manual on how to set up and use the device correctly.
They’re FAA Approved
At this point in time, all continuous flow portable oxygen concentrators are approved by the Federal Aviation Administration (FAA) for in-flight use. What this means is that if you ever need to fly across the country or even outside of the United States, you can do so with your portable oxygen concentrator at your side the whole time. While there are no restrictions on oxygen concentrators and flight attendants aren’t allowed to stop you from bringing one on board, you should make sure to contact the airline at least 48 hours ahead of your flight to let them know you’ll have a POC with you. Typically, they’ll ask that you have at least 1.5 times as much battery life as the duration of your trip and they may have an extra charge for a carry on item as well.

They’re Heavy and Bulky
While continuous flow oxygen concentrators have plenty of benefits, we’d be remiss not to discuss the disadvantages as well. Possibly the biggest downside to these machines is that they’re bulky and heavy. Most continuous flow machines weigh between 10 and 20 pounds which tends to be too heavy for most people to sling over their shoulders. Instead, most patients find it more comfortable to use a wheeled cart which either comes with the concentrator or is sold separately.
One people dislike using continuous flow machines is that they’re more cumbersome and difficult to take out of the house. If you ever need to take public transportation, you may find yourself stressing out about your concentrator rather than focusing on what you’re doing. Taking a flight is especially difficult because there’s already limited foot space on a plane, but with a continuous flow POC, you’ll have even less.

They Have Limited Battery Life
Battery life is one of the most important aspects of a portable oxygen concentrator because it determines how long you can be out of the house without having to find a place to recharge. Unfortunately, continuous flow machines don’t offer much in the way of battery life. The average machine will offer between 1 and 10 hours of freedom depending on the flow setting you use and the type of battery you are using.

While this may sound like a lot at first, once you actually get out of the house and start doing things, you’ll be surprised at how fast the time goes. You may find that it’s difficult to take long trips unless you bring extra battery packs. However, even if you do, you’ll have to stop frequently to replace the batteries.
What is a Pulse Dose Oxygen Concentrator?
Pulse dose is the other major type of oxygen delivery along with continuous flow. Whereas continuous flow has been around throughout the whole existence of oxygen therapy, pulse dose is a fairly new technology. Rather than putting out a constant stream of oxygen, a pulse dose machine only puts out oxygen when the patient inhales. Essentially, they’re designed to detect a change of pressure in the user’s nasal cannula when they begin to inhale. It then administers a precisely timed oxygen bolus (dosage).

Pulse dose regulators (oxygen regulators) can be attached to oxygen tanks and they perform the same function as a pulse dose oxygen concentrator would. Normally, oxygen tanks put out continuous flow oxygen, but the regulator will give you precise doses of oxygen that can help you ration the oxygen that’s left in the tank. Certain oxygen conservers can even be used with liquid oxygen tanks.
They’re More Technologically Advanced
One of the first things you’ll notice about pulse dose oxygen concentrators is that they’re significantly more complex than continuous flow oxygen concentrators; not in how difficult they are to use, but in the features that they offer. The Caire FreeStyle Comfort, for example, offers a built-in program called CAIREView. This program enables you to track important information about your oxygen usage including your time of use, oxygen flow setting, and more.

CAIREView is also equipped with something called “telehealth technology.” We talked about this extensively in a previous post, so feel free to check it out if you want to learn more. However, if you don’t want to get into the details, just know that it’s a technology that could be beneficial to a great number of people. Essentially, what it does is send information via a secure network to both the oxygen manufacturer and your doctor allowing them to see up-to-date information about your oxygen usage and the integrity of your portable oxygen concentrator.

While this is one of the first examples of the use of telehealth technology in oxygen concentrators, it’s a good sign for anyone who’s interested in achieving more freedom and independence from their portable oxygen device. With CAIREVIew, you’ll be able to leave your home knowing that you’re always being monitored by a medical professional. If something were to go wrong with your device, the oxygen manufacturer may be able to troubleshoot and fix it without you ever having to ship the device in and wait weeks or months to get it back. It could also save you a significant amount of time and money.
They’re Small and Lightweight
Possibly the greatest benefit to using a pulse dose concentrator over a continuous flow concentrator is how small and lightweight they are. COPD has long been considered a debilitating disease because it’s characterized by chronic lung inflammation, breathlessness, and chest pain. What’s more, in the past, COPD patients had to carry around heavy oxygen tanks which set them back even more.

Pulse flow oxygen concentrators, fortunately, are the lightest oxygen therapy devices ever produced. Due to the way that pulse dose technology works, these concentrators are able to administer oxygen much more efficiently. Unlike continuous flow concentrators, there is no “wasted” oxygen with these units. All oxygen that is put out of the device will be inspired by the oxygen patient. As a result, oxygen manufacturers are able to make them much smaller and lighter to carry.
Another reason pulse dose oxygen concentrators are so efficient is that they have the best batteries offered on the market. These concentrators use lithium-ion batteries which are the same ones that are used in common electronic devices such as cell phones, tablets, and laptops. In the future, you can expect this technology to advance even more quickly due to the high demand for light and efficient portable electronic devices.
They Offer Greater Freedom
Freedom is one of the most fundamental human rights. Without freedom, we would not be able to pursue our dreams, go where we want, and do as we please. Unfortunately, chronic respiratory conditions like COPD and cystic fibrosis can restrict your freedom significantly. Many people with COPD spend their life letting their disease control and define them rather than taking control of their symptoms and taking their life back.
.png)
Instead of forcing you to depend on friends and loved ones like oxygen tanks do, pulse dose oxygen concentrators allow you to experience full freedom and independence. You’ll never have to go out of your way to refill your oxygen tank or rely on other people to help you transport your oxygen therapy machine. Since they’re so simple to use, there are no complicated functions that you’ll need to learn about to get started. Simply turn the power on, adjust your flow setting, and experience full freedom.
They’re FAA Approved
Just like continuous flow portable oxygen concentrators, pulse dose machines are approved by the FAA for in-flight use. In fact, pulse dose machines are favored by most airlines because they offer greater battery life and they take up much less space on the plane. They’re so small that you won’t even need to set them on the floor during take-off and landing, you can simply rest it under your arm where it will be secure.

Another reason pulse flow concentrators are great for flights is because of their long battery life. A typical flight within the country will take around 2 to 5 hours, so having a concentrator like the Inogen One G5 which offers up to 13 hours of battery life on one charge will make this a breeze. Unfortunately, the same can’t be said for continuous flow units. Since the batteries only last a couple of hours, you’re likely going to need to carry one or two extra batteries at the very least. This also means you’ll be spending more time swapping out batteries instead of enjoying your flight.
Conclusion
Currently, both continuous flow concentrators and pulse dose concentrators are viable for long-term oxygen therapy. Both types of oxygen administration afford you the freedom you need to go about your daily life without concern that your oxygen needs are met. However, if you want to get the oxygen machine that’s best for you, you should take some time to consider each option.
Continuous flow portable oxygen concentrators are very versatile. If you suffer from COPD-OSA overlap syndrome, your doctor may advise that you use both a CPAP machine and an oxygen therapy device at night. Continuous flow machines can easily be attached to CPAP and BiPAP machines at night, allowing you to sleep restfully without disruption. Many modern continuous flow concentrators also offer a pulse flow option which will afford you more options.
Pulse dose portable oxygen concentrators are best for people who want the lightest and most efficient machine on the market. The Inogen One G5, for example, weighs only 4.7 pounds which is less than half the weight of the lightest continuous flow units. They’re also significantly smaller meaning you’ll be able to carry them under your arm without bumping into anything or anyone around you. In general, pulse dose machines are the best option for the greatest number of people, but it’s important to speak with your pulmonologist as well as our respiratory specialists before making a decision.
Fill out the form at the side of the page and we’ll get back to you as soon as possible to discuss your portable oxygen concentrator options.

There are many different conditions that can cause lung problems and emphysema, including a variety of heritable diseases. One of these is Alpha-1 antitrypsin deficiency (also known as AAT deficiency or Alpha-1), a rare, incurable genetic disorder that most people have never heard of.
Alpha-1 is the result of a protein deficiency that can cause mild or severe damage to the lungs and liver. Many people with AAT deficiency experience asthma-like symptoms including breathlessness, wheezing, and coughing that can occur in childhood or later in life.
Because Alpha-1 is rare, most doctors don't routinely screen for the condition, and some people with AAT deficiency don't get diagnosed until they develop other liver problems or lung disease. This makes it a difficult disease to catch, especially since, for some people with Alpha-1, symptoms don't show up until late adulthood.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Only about 100,000 people in the United States have been diagnosed with severe AAT deficiency, and there are still many things that doctors and scientists don't understand about the disease. For instance, doctor's don't understand why some people with Alpha-1develop liver disease at a very young age, while many others go their entire lives without experiencing any liver problems.
If you or someone you know has been diagnosed with Alpha-1 antitrypsin deficiency, you probably have a lot of questions and worries. That's why, in this article, we're going to walk you through everything you need to know to better understand the disease, including symptoms, potential complications, and what kind of treatments are available to help people with AAT deficiency.
What is Alpha-1 Antitrypsin Deficiency
Alpha-1 antitrypsin deficiency is a rare, but potentially very serious, genetic disorder that mainly effects the lungs and liver. It occurs when a child gets defective AAT genes from their parents, which prevents their bodies from making enough of an important protein called the alpha-1 antitrypsin protein (AAT protein).
There are several different types of genetic mutations that can cause AAT deficiency, and some lead to more severe symptoms than others. Depending on their individual genes, a person with the disease can have different levels of AAT protein in their bodies, ranging from extremely low to only slightly lowered amounts.
Because of this, some cases of AAT deficiency are mild and don't cause many symptoms. Other cases can be very severe and lead to extensive lung damage, liver damage, and other complications.
People with severe AAT deficiency are prone to liver disease and cirrhosis as well as chronic lung infections, bronchitis, and emphysema. Because of this many people with the disease develop respiratory symptoms like wheezing and difficulty breathing as they get older.
Treatment for Alpha-1 antitrypsin deficiency depends on individual symptoms and the extent of damage to the liver and lungs. Most treatment plans focus on preventing organ damage by keeping the lungs and liver healthy, and avoiding irritants and toxinss that can damage them.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa')}}
How Alpha-1 Antitrypsin Deficiency Affects Your Body
Alpha-1 Antitrypsin Deficiency can take many different forms, and every individual case of the disease is unique. How exactly the disease effects the body depends on the type of genetic mutation that caused it as well as age, lifestyle, and exposure to environmental irritants like dust and smoke.
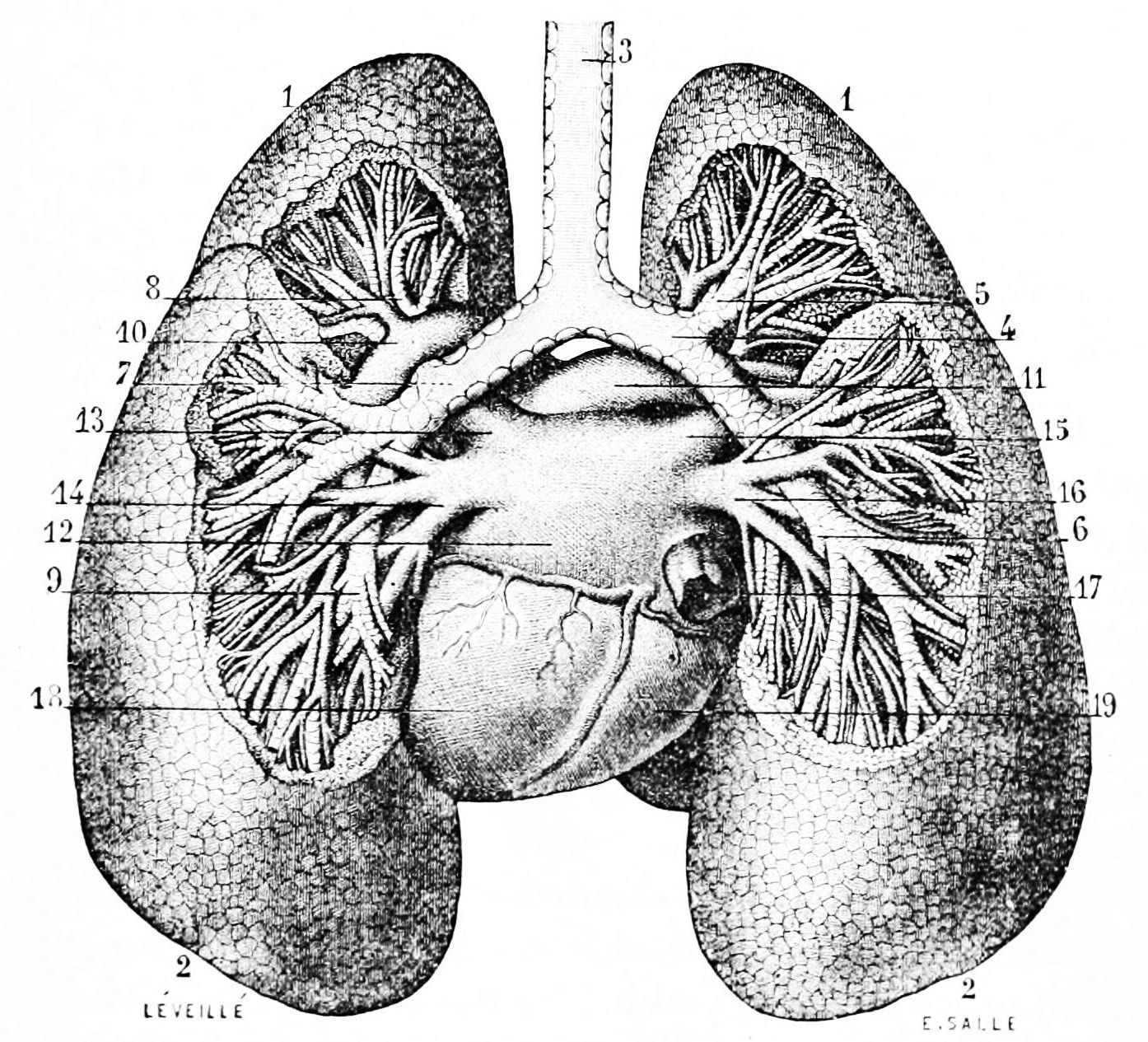
Problems caused by AAT deficiency are all related to the body making a dysfunctional version of the AAT protein. This protein is made primarily in the liver, and in healthy people it moves easily out of the liver and into the bloodstream, where it is carried to the lungs
.

People with Alpha-1 make an abnormal version of the AAT protein that gets stuck in the liver instead of moving into the blood. That means it can't make it into to the lungs to protect them from inflammation and irritation, leaving the lungs vulnerable to damage.
The symptoms of Alpha-1 and how severe they get over time varies widely from person to person. Generally, the less AAT protein a person has in their bloodstream, the more susceptible they are to lung damage and other symptoms.
A large number of people with AAT deficiency eventually experience some level of lung decline, usually between the ages of 20 and 50. Lung damage is accumulative, and how frequently the lungs get inflamed by infections and irritants like dust and smoke has a major effect on the severity of respiratory symptoms and complications.
Although slightly less common, Alpha-1 can also cause liver damage and scarring (cirrhosis). This can occur in both adults and newborn babies with AAT deficiency, although doctors don't understand exactly why it affects some but not others.
The following sections will give you a more detailed understanding of how AAT deficiency causes lung and liver disease in people with Alpha-1.
How AAT Deficiency Affects the Lungs
The AAT protein's purpose is to break down a powerful, caustic enzyme called neutrophil elastase. This enzyme gets into the lungs via white blood cells—immune system cells that circulate in every person's bloodstream ready to fight pathogens and infection when needed.
White blood cells release neutrophil elastase in the lungs whenever the lungs get inflamed by infections or irritants. This enzyme helps white blood cells dissolve bacteria and fight off disease, but it can also break down sensitive lung tissues if it's not tightly controlled.
In healthy people, neutrophil elastase doesn't cause any problems because the AAT protein breaks it down quickly before it can damage the lungs. Unfortunately, people with Alpha-1 antitrypsin deficiency don't have enough AAT protein in their lungs or bloodstream, so the powerful enzyme is left to wreak havoc in their lungs.
Leftover neutrophil elastase damages the tiny air sacs, called alveoli, that allow the lungs to absorb oxygen. Over the span of years, the lung tissue gets so damaged and scarred that it can't get enough oxygen into the bloodstream, causing lung disease and a variety of other complications as it worsens.
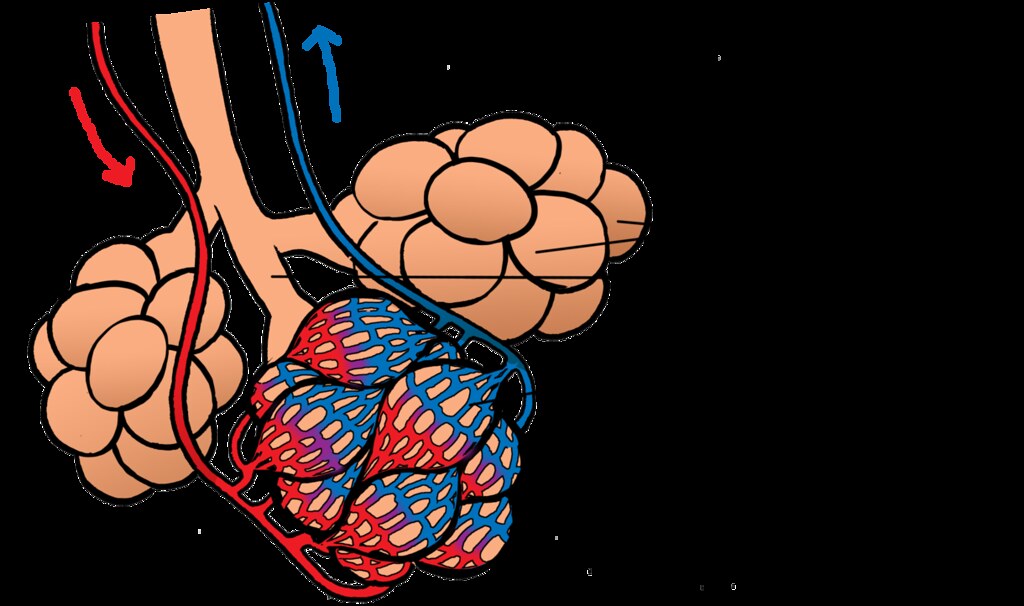
The best way someone with AAT deficiency can prevent this from happening is by taking special precautions to avoid lung infections and irritants like smoke. It is also important to treat any respiratory illnesses that you do get quickly and aggressively. Even minor lung illnesses like the cold or flu can recur again and again, causing chronic inflammation that, over time, can cause permanent damage to the lungs.
Most people with AAT deficiency experience some amount respiratory decline as they get older and their lungs accumulate damage. In people with severe AAT protein deficiency, this can eventually lead to chronic emphysema, shortness of breath, and other respiratory complications.
How AAT Deficiency Affects the Liver

Liver problems are much less common in people with Alpha-1, but when they do occur they can be serious and life-threatening. About five to ten percent of newborn babies with AAT deficiency are born with liver disease, but it's unknown why some babies and adults with Alpha-1 get liver damage while others don't.
Doctors and researchers only have a limited understanding of how AAT deficiency damages the liver and causes cirrhosis (permanent scarring). What they do know is that people with Alpha-1 get large build-ups AAT protein in their livers, which can make them prone to liver disease and dysfunction.
This happens because people with Alpha-1 make an abnormal version of the AAT protein that cannot exit the liver the same way that functional AAT protein does in healthy people. As a result, not enough AAT protein makes it into the bloodstream where it is needed to go to the lungs and protect them from inflammation.
Only about 15 to 20 percent of people with severe AAT deficiency ever experience symptoms of liver disease. For those that do, medications are available to help manage the symptoms and liver transplant surgery may be an option for people who develop life-threatening problems.
Causes of Alpha-1 Antitrypsin Deficiency

Alpha-1 Antitrypsin deficiency is caused by a defect in the gene that tells the body how to make the AAT protein. As a result of this mutated gene, people with the disease make a defective version of the protein that gets stuck in their liver instead of entering the bloodstream like it's supposed to.
This can cause liver problems and makes the lungs prone to inflammation. Over time, lung tissue can become damaged and scarred and lead to emphysema, trouble breathing, and low levels of oxygen in the blood.
In order to get AAT deficiency, you have to inherit two defective AAT protein genes from your parents. There are a couple different types of AAT gene mutations, and some cause a more severe protein deficiency than others.
Alpha-1 is inherited via a pattern known as autosomal codominance, in a way similar to how blood types are passed down through generations. The image below illustrates how this genetic inheritance pattern works.

Here are the three major types of AAT gene mutations:
-
The Z mutation: People with this mutation have extremely low levels of AAT protein in their blood. This is the most common mutation that causes Alpha-1, and it can lead to severe symptoms and disease in people who inherit two copies of the Z gene (ZZ).
-
The S mutation: People with this mutation have moderately low levels of AAT protein in their blood. This is a less common mutation, and usually causes less severe symptoms. People with two copies of the mutation (SS) usually do not have any symptoms at all.
- The M mutation: This is the normal, healthy version of the AAT gene. People with two copies (MM) of this gene type have normal levels of AAT protein in their blood and do not have Alpha-1. People with one normal copy and one mutated copy (MZ or MS) are considered carriers of Alpha-1.
You need to have two of these mutated genes in order to develop an AAT protein deficiency. However, it is possible to get the disease from any combination of the different AAT-deficient mutations.
For example, you could have one gene with the Z mutation and one with the S mutation and only develop a mild form of the disease, or you could have two Z genes (ZZ, the most severe form of the disease) instead. However, since they only have a very mild protein deficiency, people with two S genes (SS) usually don't develop any symptoms or complications at all.
If you only inherit one defective gene, and one normal (M) gene, then that makes you a carrier of Alpha-1. You won't experience any symptoms, but there is a chance you could give AAT deficiency to your children if you have them with someone who is also a carrier of Alpha-1.
Key Facts about Alpha-1 Antitrypsin Deficiency

Alpha-1 deficiency affects about 1 in every 2,500 people in the US. Even more Americans are carriers of the disease—an estimated 19 million people.
If the disease is caught and managed early, many people with Alpha-1 live just as long as people without the disease. With proper treatment and a healthy lifestyle, people with AAT deficiency can live long, active, and healthy lives.
People with the most severe AAT protein deficiencies (such as those with two copies of the Z gene mutation) are the ones that are most likely to develop serious, life-shortening diseases like liver damage and emphysema.
Because Alpha-1 is a relatively rare disease, it's not one that doctors routinely screen their patients for. Many people discover that they have Alpha-1 after they first develop breathing issues or show symptoms of liver decline.
Because the respiratory symptoms associated with AAT deficiency are so similar to other lung conditions, it's common for doctors to confuse the symptoms with asthma or smoking-induced emphysema. Fortunately, all it takes is a simple blood test to determine whether or not you have Alpha-1 deficiency.
Since so many people with Alpha-1 are misdiagnosed with other lung conditions first, medical professionals recommend that anyone diagnosed with a lung or liver disease get tested for AAT deficiency. Detecting the disease as early as possible is key for slowing or preventing further damage.
Unfortunately, researchers estimate that up to three percent of people living with COPD have undiagnosed Alpha-1 deficiency.
Alpha-1 Antitrypsin Deficiency Symptoms

The main symptoms of Alpha-1 include respiratory symptoms like coughing, shortness of breath, and frequent respiratory illnesses. Signs of liver disease, like yellow-tinted skin and eyes, are slightly less common but can be an important early indicator of AAT deficiency.
Every case of Alpha-1 is different, and how the disease affects you depends on how severe your AAT deficiency is and a variety of other factors. Some people with Alpha-1 are born with liver disease, while others develop liver damage later in life, or not at all.
Your individual lifestyle and how careful you are to avoid respiratory toxins and other irritants can play a major role in what symptoms you develop and how severe they become. If you have Alpha-1, you should have frequent visits with your doctor to check for signs of liver and lung damage so you can treat it as early as possible.
If you have AAT deficiency, it is especially important for you to protect your lungs from smoke, infections, and anything else that could cause damage or inflammation. You should also take care to protect your liver to avoid developing symptoms of liver dysfunction.
While some people with Alpha-1 develop organ damage early in life, many others don't notice any symptoms until they are much older. The first symptoms of AAT deficiency can appear as late as fifty or sixty years old.
Common Respiratory Symptoms for Alpha-1
- Shortness of breath and difficulty breathing, especially during physical activity
- Cough, often with phlegm
- Wheezing, especially during exertion
- Frequent respiratory illnesses and infections (e.g. recurring colds)
- Chronic allergies that last all year
Common Liver-Related Symptoms for Alpha-1
- Jaundice (yellowing of the skin and eyes) that can be present at birth or occur later in life
- Frequent itching
- Pale colored stools or blood in stools
- Dark urine
- Fatigue
- Swelling in the abdomen (ascites)
- Swollen, enlarged liver (hepatomegaly) or spleen
Panniculitis is another possible symptom of AAT deficiency. It is a very rare skin condition that causes raised, painful bumps (nodules) or ulcers on the skin.
Complications with Alpha-1 Antitrypsin Deficiency
Liver Disease

Low levels of AAT protein in the blood of people with Alpha-1 occurs because they make a version of the protein that won't leave the liver. As a result, it can't make it into the bloodstream where it's needed and instead builds up in the liver, leaving it prone to inflammation and disease.
Doctors and researchers aren't sure exactly how the buildup of AAT in the liver causes damage in some people with Alpha-1 but not others. However, they do know that, in rare cases, it can cause cirrhosis and serious damage that leads to liver disease over time.
Only a small number of people with Alpha-1 develop liver problems, but all people with AAT deficiency should take precautions to protect their liver from damage. Alcohol, viruses like Hepatitis A and B, and certain medications like acetaminophen can be especially dangerous for people with Alpha-1.
Emphysema
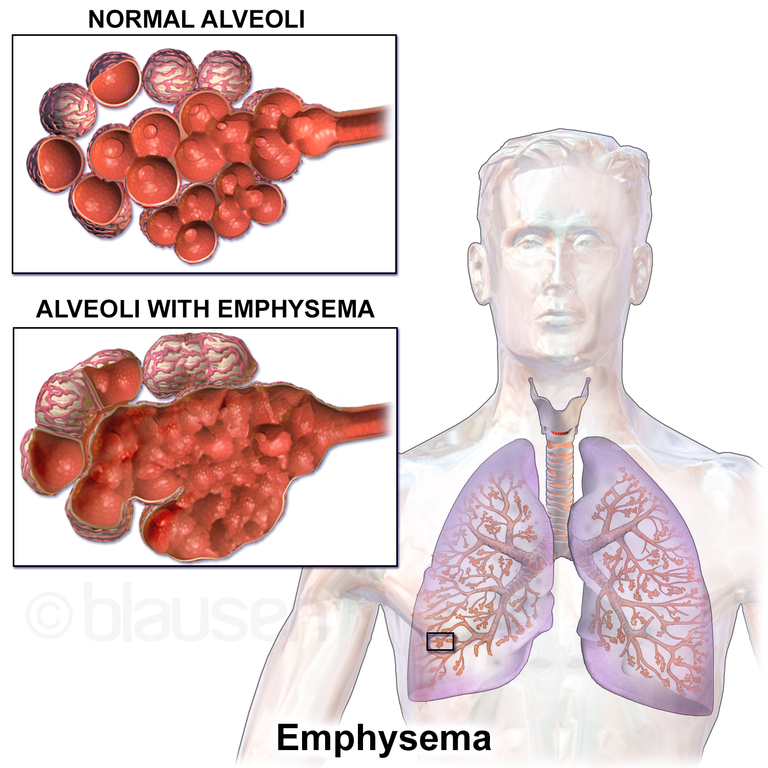
If you have Alpha-1, your lungs are prone to repeated inflammation and infection that can permanently damage delicate lung tissue over time. Because of this, many people with AAT deficiency experience some sort of lung and breathing issues as they get older, and some develop a more serious lung disease called emphysema.
Emphysema is a type of chronic obstructive pulmonary disease (COPD) that occurs when irritants, infections, or inflammation damages the tiny air sacs, or alveoli, in your lungs. This makes it difficult for your lungs to absorb oxygen and causes shortness of breath, wheezing, coughing, and other respiratory symptoms.
Damage to tissues in the lungs and small airways also makes it difficult to move air through the lungs. Unlike healthy, elastic lung tissue, damaged tissues lose their springiness and get stiff. This causes small airways to collapse, blocking air from flowing through and making it difficult to push all the air out of your lungs when you exhale.
Emphysema is an progressive lung disease with no known cure. That means there's no way to stop it from continuing to cause more and more lung damage over time, although medications and lifestyle changes can slow how quickly the disease worsens.
Exposure to toxins and other respiratory conditions can cause emphysema, but when emphysema is caused by AAT deficiency it is often referred to as Alpha-1 COPD. People with Alpha-1 tend to develop emphysema much earlier (by ten years or so) than “healthy” people who acquire it by smoking or exposure to other toxins.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Panniculitis

Panniculits is a rare skin condition that a small percentage of people with AAT deficiency develop. It happens when the layers of skin just under the surface get irritated and cause rash-like raised, red bumps (called nodules) on the skin.
Panniculitis often develops in patches on the thighs and buttocks and any part of the skin that sustains damage. It often only takes minor injury or abrasion to cause nodules to form, which can happen during vigorous physical activity.
The severity of symptoms varies from person to person, ranging from minor irritation to severe pain and discomfort. In the worst cases, panniculitis nodules can turn into more serious skin ulcers, known as necrotizing panniculitis.
Fortunately, panniculitis is extremely rare, even in people with Alpha-1, and can often be treated with medications like corticosteroids, antibiotics, and augmentation therapy (described later in the section on treatments for Alpha-1).
Risk Factors for Alpha-1 Antitrypsin Deficiency

Since Alpha-1 is a genetic disorder, you can only get the disease is if you inherit two of the defective AAT protein genes from your parents. Unfortunately, there's nothing you can do to change your genetics if you get the disease, but a healthy lifestyle and medical treatment can have a major effect on how severe symptoms get over time.
People with Alpha-1 who smoke or are exposed to workplace hazards like dust, pollen, mold, and chemical fumes, are much more likely to develop respiratory problems and emphysema that those who aren't. People who have asthma, a family history of emphysema, or get repeated lung illnesses are also more likely to experience complications with AAT deficiency.
Alpha-1 is most common in white people of European and Middle Eastern descent, where up to 1 in 32 people are carriers of the disease. It is much less common in people with Asian and African ancestry.
Treatment for Alpha-1 Antitrypsin Deficiency

Treatments and medications for Alpha-1 antitrypsin deficiency are mostly aimed at preventing progressive organ damage and managing uncomfortable symptoms. The key focus is prevention, because lung damage and liver cirrhosis caused by AAT deficiency is permanent.
People with Alpha-1 usually need frequent medical checkups, a strict healthy lifestyle, and medication to protect their liver and lung function from declining. There is also a special treatment available, known as augmentation therapy, that can treat the underlying protein deficiency in people who have Alpha-1.
Lifestyle Habits to Treat Alpha-1 Antitrypsin Deficiency
Living a healthy lifestyle is an important part of preventing organ damage in people with AAT deficiency. This includes healthy eating, regular exercise, and avoiding substances that are toxic to liver and lungs.
Healthy Diet & Nutrition
Eating healthy, wholesome foods is an important part of any healthy lifestyle, but it's especially important for people with AAT deficiency. A balanced diet ensures that your liver and lungs have all the nutrients they need to stay healthy and work as efficiently as possible.
A healthy diet and portion control will also help you maintain a healthy BMI and avoid health issues like diabetes and heart disease. If you develop liver damage as a result of AAT deficiency, your doctor might recommend a special diet or supplements to help your liver function better.
Vaccinations

There are several vaccinations that are especially vital for people with Alpha-1 deficiency. These include the hepatitis A and B vaccines, the pneumococcal vaccine, and yearly flu shots.
The pneumococcal vaccine helps prevent pneumonia, a serious lung condition that is even more serious for people prone to lung damage and disease. Yearly flu shots are also important to protect the lungs against the influenza virus.
Getting vaccinated against hepatitis A and B protects the liver from deadly viruses that can cause liver damage and cirrhosis. Since people with Alpha-1are particularly prone to liver damage, this is an important precaution to take against liver disease.
Avoid Lung Irritants and Alcohol

If you have Alpha-1, quitting smoking is by far the most important thing you can do to increase your lifespan and prevent lung damage. Even minor lung irritation from secondhand smoke, dust, or mold can cause serious damage over time.
AAT deficiency also makes your liver prone to getting damaged, which is why doctors recommend that people with Alpha-1 avoid drinking alcohol. Excessive alcohol use can cause cirrhosis even in people who don't have the disease.
Here are some common respiratory irritants you should take care to avoid:
- Smoke, including secondhand smoke, from any source (campfires, wood burning stoves, incense, cigarettes, etc.)
- Chemical fumes
Living healthily and happily with COPD is all about developing healthy lifestyle habits and learning how to keep your symptoms under control. Because it is a chronic disease with no real cure, the only way to manage it is by keeping up with daily medication and carefully following treatment goals.
That's why all COPD patients should have a personalized COPD action plan to help them keep track of their medications and other treatment goals.
A COPD action plan is a comprehensive set of instruction on how to manage and treat your COPD. It's the most important tool you have for keeping your symptoms under control and preserving the health of your lungs and the rest of your body.
A typical action plan includes all the important parts of your COPD treatment, including your medication schedule, what to do when your symptoms act up, and your diet and exercise regimen. It also helps you remember what to do in an emergency and know when to see your doctor for a problem.
In this post, we're going to help you better understand what a COPD action plan is and how you can use it to better manage your disease. We'll show you what a good action plan looks like, how to make one with your doctor, and how to put your treatment plan into action.
Crafting your COPD Action Plan

Putting together your COPD action plan is an individualized process that you and your doctor will go through together. Every patient's action plan is unique and tailored to fit their personal needs.
A good COPD action plan will give you detailed treatment instructions and clear plan for what to do if your symptoms get worse. It should take your medical history, lifestyle, symptoms, and other life factors into account.
As you and your doctor work on your action plan, it's important to have a clear picture of both your current situation and your future goals. Here are some tips to help you and your doctor better understand your condition and get on the same page.
Track Your Symptoms
Helping you manage your COPD symptoms is the most important purpose of a good COPD action plan. But in order for it to be useful and accurate, you and your doctor need to have as much information as possible about all symptoms you experience and how they fluctuate over time.
The best way to get a better understanding of your symptoms is to record them daily with a journal or a symptom checklist. This will help you remember what symptoms you had and when you had them the next time you talk to your doctor, and to track patterns and changes over time.
You should try to make your notes as detailed as you can so that you and your doctor have as much information to work with as possible. Make sure you write down any and all ailments you experience, even ones that seem small or inconsequential.

The more information you have on your condition and symptoms, the more useful your action plan will be. However, it's worth writing down your symptoms even after you have an action plan in place. It will not only make it easier to notice changes in your condition as the disease progresses, but will also help you adjust your action plan as your symptoms change.
Here are some tips for what you should include in your daily symptom diary:
- Write a list of any and all physical and psychological symptoms you experience every day, especially breathing and respiratory problems. (e.g. breathlessness, fatigue, muscle weakness, coughing, anxiety, depression, etc.)
- Record and notable changes or improvements in your symptoms compared to recent days.
- Record any changes in the frequency or severity of your cough, and note any changes in the color and consistency of any mucus you cough up.
- Keep a detailed record of any breathing issues and when they get better or worse throughout the day. Record what kinds of activities cause you to feel short of breath and your general ease of breathing from day to day.
- Keep track of how much sleep you get (in general) and any sleeping difficulties you have, such as insomnia or waking up frequently during the night.
-
Write down the general time and situation in which your symptoms occurred. (e.g. all day long, in the morning, after eating lunch, after exercising, after going to bed, etc.)
- Include any special circumstances surrounding your symptoms. (e.g. you were outside in the heat, your allergies were acting up, you forgot to take your daily medication, etc.)
- Keep track of your overall mood and mental state from day to day. (e.g. you felt tired, you felt motivated, you felt anxious, etc.)
- Record any prescription or over the counter medications you took that day and approximately what time you took them.
- Keep track of any exercise or physical activities you do.
- Record any smoking, tobacco, or other drug use (including alcohol).
As you start your COPD symptom diary, it may help to have a complete list of COPD symptoms on hand to help you know what to look out for. You can also use a COPD symptom checklist, like this one here, to help you remember what's important to keep track of.
Think About Your Goals

In general, it is the goal of every COPD patient to breathe easier and reduce other respiratory symptoms. However, these larger goals are difficult to reach without first breaking them down into smaller goals that are easier to act on.
For example, if you smoke cigarettes, one of your goals could be to reduce the amount of cigarettes you smoke or stop smoking altogether. You could break this goal down into even smaller steps, too, such as going to a smoking cessation counselor or joining a quit smoking program.
You should also think about your lifestyle and any areas that you need to improve. For example, you may need to lose weight, eat more fruits and vegetables, or get more exercise to keep your body strong and prevent COPD complications.
Other goals might relate directly to your symptoms and helping you breathe comfortably throughout the day. Things like always taking your medications as directed, pacing yourself during exercise, and utilizing therapeutic breathing techniques can help you reach those goals.
Once you know what you are striving for, you and your doctor can put together a treatment plan that addresses all of these goals. The following list will give you an idea of some of the major treatment goals that you should consider as you craft your COPD action plan.
General COPD Treatment Goals:
- Quitting smoking
- Improving your ability to breathe
- Getting more exercise to strengthen your body and lungs
- Eating a healthier, COPD-friendly diet
- Reducing coughing, wheezing, and other respiratory symptoms
- Reducing the number of COPD flare-ups and exacerbations you have
- Reducing your risk of COPD complications (e.g. heart attacks and osteoporosis)
- Slowing your disease from progressing further
- Working with your doctor and other medical specialists to track your symptoms and achieve your treatment goals
Consult With Your Doctor

Once you've had time to track your symptoms and brainstorm your treatment goals, it's time to sit down with your doctor to put together a comprehensive COPD action plan. Your doctor may have a standard template, like this one, to fill out, or he might put together a custom document for you to take home.
Make sure you bring your symptom diary and any other information about your medical history that your doctor may need. Your doctor will also use lung function tests, including spirometry, to determine your treatment and medication needs.
It's important for your doctor to include you in his process and thoroughly explain every part of your action plan and how to use it. Take the time to look over your treatment plan carefully and don't be afraid to ask questions or ask for clarification.
While your COPD action plan helps your doctor coordinate your medications and treatment goals, your action plan's primary purpose is to be a resource for you. It is very important that you understand your plan in its entirety and how to use it to manage your disease on a daily basis.
Depending on your condition and situation, you may have a team of doctors and specialists working to help you stay healthy. In this case, you will need to coordinate your action plan with all of your caretakers to ensure your plan is as cohesive and comprehensive as possible.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The Three Zones of Your COPD Action Plan
It's important to understand that your COPD action plan is actually split up into three distinct plans of action. From here on out, we will refer to these three plans as the green zone, yellow zone, and red zone action plans, as this is the typical way to organize them.
These three zones make up the core of your COPD action plan and tell you what to do in different situations. They tell you how manage your COPD when your symptoms are normal (green), worse (yellow), and severe (red), and how to know which zone's action plan to use.
This scheme is very useful for helping you recognize when you experience a flare-up or you need to call your doctor or seek emergency medical attention. It also helps you remember how to stay healthy and what to do when your symptoms get worse.
Think of each zone as representing a specific plan of action depending on how you feel on a particular day. It is composed of two main parts: your symptoms and the actions you should take.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
The first part is a description of the symptoms and the duration of symptoms that correspond to that particular zone. This is meant to help you recognize when your symptoms fit the requirements for that zone's action plan, so you can always tell when to take the actions for that zone.
The second part is a list of actions you should take whenever you experience the symptoms that correspond to that zone. It may include things like what medication to use, how much exercise you should do, breathing techniques, mental health strategies, and other instructions for keeping yourself healthy.
For example, the green zone would include your normal, baseline symptoms and strategies for managing them on a regular basis. It would also include a list of actions to take on a regular day when your symptoms are at a typical level.
The Yellow zone should include a description of what it looks like when your symptoms flare up, and what to do to manage them and keep them from getting even worse. You would refer to the actions and strategies in this zone when you experience a minor flare up or exacerbation.
The red zone gives you instructions on what you should do when your symptoms get more severe. It will help you recognize at what point you should seek medical attention and what to do in an emergency.
The symptoms and actions that go in each zone will depend on your medical history, lung function, and your personal COPD symptoms. Since it is based on your baseline symptoms, which may be more or less severe, your green zone action plan may differ significantly from other patients, and will change as your disease progresses.
Here is an overview of the different action plan zones and when you should use them:
- Green Zone: “I am doing well today.” Use this plan when your symptoms are at a normal, baseline level, and you feel well enough to continue your usual exercise and activities.
- Yellow Zone: “I am not feeling well today or I am experience a COPD flare-up.” Use this plan when your symptoms are worse than normal, you are having difficulty breathing during your usual activities, or you notice a change in your mucus, your sleep quality, your appetite, or the frequency with which you have to use your quick-relief medications.
- Red Zone: “I need urgent medical care.” Use this plan if your symptoms become very severe, to the point that you feel shortness of breath at rest and are unable to do any physical activity. Breathing difficulties that severely interfere with sleep, fever or shaking chills, feeling confused, coughing up blood, or having chest pains are other signs that you need emergency medical care and need to follow your red zone plan.
To see an example of what an actual COPD action plan looks like, you can check out this sample plan from the American Lung Association.
Daily Treatment Goals and Instructions (Green Zone)
Your daily symptom management and treatment goals—the green zone—is one of the most important aspects of your COPD treatment plan. It contains all the medications and actions you should take on a typical-symptom day to stay healthy and keep your symptoms under control.
When your symptoms are at your usual baseline level, you should follow the actions in this plan. If you keep your COPD well-managed and minimize flare-ups, you should be able to use your green zone plan on most days.
It's a good idea to review this part of your plan regularly, even though you use it often, just to jog your memory and review your goals, medications, and treatments. It will help you stay motivated, keep on track, and remind you of any habits or treatment methods you may have gotten lazy about doing.
Your Plan for Managing Flare-ups and Exacerbations (Yellow Zone)
Generally, any noticeable increase in COPD symptoms should direct you to use your yellow zone action plan, including feeling low on energy, experiencing more difficulty breathing, worsened coughing, or changes in your sleep quality and appetite. You should also look for changes in the color and consistency of your mucus and how frequently you have to use your quick relief medications.
When your symptoms flare-up or your breathing problems get worse, your yellow zone plan will tell you exactly what you need to do to keep your symptoms under control. It should include your usual maintenance medication along with instructions on how to use your quick-relief medications effectively.
Your yellow zone action play will likely include other treatments for reducing your symptoms, such as breathing techniques and mucus clearance techniques, which we will discuss more in the following sections. It may also include stricter guidelines for using supplemental oxygen and protecting your lungs from inflammatory environments and irritants.
Your doctor may instruct you to start taking a course of antibiotics or corticosteroid medications when your symptoms get worse as part of your yellow zone action plan. You may also need to call your doctor if your symptoms don't get better within a day or two.
Your Plan For Emergencies (Red Zone)
The purpose of your red zone action plan is to remind you of what to do in an emergency. You should follow this plan when your symptoms become so severe that you have difficulty breathing at rest.
Extreme shortness of breath, severe fatigue that interferes with daily living, or being unable to do light physical activity is a sign that you need to seek immediate medical attention. Other signs include chest pain, coughing up blood, fever, chills, confusion, and symptoms that are so severe that you are unable to sleep at night.
If you experience any of these symptoms, follow your red zone action plan and call 911, or have someone else drive you to the emergency room as quickly as possible. You may also need to take a medication or adjust your oxygen prescription to help you cope until you get to the hospital.
The Components of a Good COPD Action Plan
A good COPD action plan contains everything you need to know about managing your disease on a daily basis and when your symptoms flare up. It should tell you what medications to take every day, what medications to take when your symptoms get worse, and all the actions and habits you need to do on a regular basis to keep your lungs healthy and your symptoms under control.
Many action plans also include information about your diet, exercise, and lifestyle goals related to your COPD. In these next sections, we'll explain all the different components that your COPD action plan may include as part of your green and/or yellow zone plans.
Your Medications

Your COPD action plan should include all of the prescription and over-the-counter medications that you need to treat your COPD. It should tell you what medication to take when your symptoms are at baseline, what medication to use as-needed (and when to use it), as well as the correct dosage and the frequency that you should take it.
Your maintenance medications help you breathe easier on a daily basis and are the cornerstone of daily COPD treatment. However, you have to take them every single day as directed by your doctor in order for them to be as effective as they can be.
On the other hand, not keeping up with your daily maintenance medications can make your symptoms worse and cause your COPD to progress faster. By keeping your symptoms minimized on a daily basis, your maintenance medicine is very important for staving off flare-ups, exacerbations, heart problems, and other serious COPD complications.
Your doctor may also prescribe quick-relief or rescue medications—in addition to your maintenance medicine—to use as part of your yellow zone action plan on days when you experience worsened COPD symptoms. These medications help reduce sudden, uncontrolled symptoms and help you breathe easier when your symptoms flare up.
Your doctor may also give you a course of steroid medication or antibiotics to use when you notice your symptoms getting out of hand. Most of the time, you will be instructed to take them if your symptoms stay worse for more than a day or two or when you notice the signs of an oncoming exacerbation.
Whenever you start a course of antibiotics, it's very important that you continue to take the entire course, even after you start to feel better. As long as you use them correctly and as directed by your doctor, antibiotics and steroid medications can help you avoid serious exacerbations and recover from flare-ups more quickly.
Your COPD action plan should also include information about any vaccines you need, including pneumonia and influenza vaccines. Most adults need another dose of the pneumonia vaccine after the age of 65, and all COPD patients should get their yearly flu shot to stave off exacerbations and infections.
Whatever medications your doctor recommends should be included in your action plan along with enough detail to help you use them reliably and consistently. If you have any questions about your medications or how to use them, talk to your doctor and ask him to clarify the instructions in your plan.
Breathing Exercises

Breathing exercises like pursed lips breathing and diaphragmatic breathing are a vital part of daily COPD management for patients who struggle with shortness of breath. These breathing techniques help you control your breaths and even strengthen the muscles in your chest that you use to breathe.
Practicing breathing techniques every day can help you keep your breathing steady and under control when you exercise and do other active, daily tasks. They can also help you manage minor symptom flare-ups and get through bouts of coughing more easily.
If you deal with breathlessness and coughing often, your doctor may recommend breathing exercises as part of your everyday COPD management plan. They may also be helpful to practice when your symptoms get worse as part of your yellow zone action plan, too.
Managing Airway Congestion
Excess mucus is a common symptom that many COPD patients have to manage. If you don't take care to stay hydrated and clear the mucus out of your lungs, it can make symptoms like coughing and breathlessness worse.
If you let mucus build up in your airways, it narrows the passages that air can flow through and makes it more difficult to breathe. Mucus buildup can also trap bacteria, viruses, and irritating particles that can inflame your airways or cause infections in your lungs.
Because of this, keeping your airways clear of mucus is often an important part of managing COPD. To address this, your treatment plan may include mucus clearance techniques to use when you get excess phlegm.
The goal of mucus clearance techniques is to dislodge stuck mucus from the walls of your airways and cough it up and out of your lungs. Often a two-pronged approach of proper hydration and huff coughing can help you keep congestion under control.
Staying hydrated thins out your mucus, while coughing moves the mucus up through your airways so you can cough it up through your mouth. Your doctor may also recommend a variety of other mucus clearance techniques and aids, such as chest percussion, positional drainage, or using a special high frequency chest wall oscillation vest, as part of your COPD action plan.
Quitting Smoking
If you are a smoker, then quitting should be your number one priority and included as part of your COPD action plan. Quitting smoking will help prevent further damage to your lungs, reduce flare-ups, and preserve the lung function that you still have left.
To help you quit, you may want to include a quit smoking program or therapy as part of your COPD management plan. If you are unable to quit, reducing the number of cigarettes you smoke or seeing a smoking cessation therapist can help put you on the right track to ending your addiction.
If you want help quitting smoking, check out this article, “Where to Get Help When You Decide to Quit Smoking,” from the National Cancer Institute. You can also get more information about smoking cessation and quit smoking resources from the CDC, the American Lung Association, smokefree.gov, and many other places online.
Other Healthy Lifestyle Goals
If you are like most people with COPD, then you probably use an inhaler every day. Inhaled medications like bronchodilators and steroids are some of the most important and effective medications for COPD—that is, as long as you use them correctly.
Unfortunately, studies show that many, if not most, people do not actually use their inhaler correctly. This is a huge problem for all patients who use inhalers, but especially for people with COPD.
Inhaler medications for COPD not only help you feel better, but they help stave off infections, flare-ups, and dangerous exacerbations that can make your disease worse. If you are not using your inhaler correctly, then you don't get the full dose of the medication you need to keep your symptoms under control.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
In this article, we're going to look at why so many people use their inhaler incorrectly and what can be done to solve the problem. We'll show you what proper inhaler technique looks like and how to avoid some of the common mistakes patients make when using their inhalers.
Why is Poor Inhaler Technique So Common?

Inhalers are relatively straightforward and easy to use; after all, it's not uncommon to see very young children use an inhaler for asthma. So you might be wondering, how do you use an inhaler wrong, and is it really that easy to do?
Unfortunately, yes, it is very easy to use an inhaler incorrectly just by rushing, holding it incorrectly, or skipping important steps. Inhalers are not complicated, but they do require a specific technique in order to work effectively.
Too many people either don't know the correct steps or believe that getting a little lazy about their technique isn't a big deal. Even worse, studies show that 85% of doctors do not know how to use an inhaler properly, and are thus unable to teach their patients the proper technique.
This can be very dangerous because, when you use an inhaler incorrectly, the medicine won't be as effective as it should be. Improper inhaler technique can significantly reduce how much medicine you inhale and and cause the treatment to fail.
Studies show that COPD patients who use their inhalers incorrectly have worse symptoms, more hospitalizations, and quicker worsening of their disease. It can also cause you to need to take other medications like antibiotics and oral steroids more frequently because your inhaled medication isn't working as well as it should.
It's important to remember that your inhaler contains a precise amount of medication specially selected by your doctor to be personal to you. It's important that you use you inhaler correctly and as directed to make sure that you get the full dose that you're supposed to take.
Are You Using Your Inhaler Wrong?

There are several different types of common inhalers, and each work slightly differently and require different techniques. That's why it's so important for both doctors and patients to be fully trained in the specific type of inhaler prescribed.
However, studies have identified some common mistakes that people frequently make when using their inhaler. Many of these mistakes have to do with preparing the inhaler and breathing technique during use.
If you suffer from COPD, knowing what proper inhaler technique looks like is absolutely vital for your health. That means following every step for your inhaler carefully and avoiding bad technique.
In these next sections, we're going to look at some of the most frequent mistakes that people make with their inhalers and how to correct them. We'll also show you some great resources you can use to learn proper technique for using your specific brand of inhaler.
However, nothing can substitute for a good demonstration from your doctor or another medical professional trained in proper inhaler use. After reviewing the information in this article, make sure you bring your inhaler to your next doctor's appointment so your doctor can evaluate your technique.
How to Avoid Common Inhaler Mistakes

Prepare Your Inhaler Properly
Most inhalers require you to follow some brief preparation steps before every dose you take. Both pulse-dose and dry powder inhaler require some kind of set up before use.
Load a Dose of Medication

Most pulse-dose inhalers have a lever mechanism that you have to flip up before taking your dose. Many dry powder inhalers have a twist mechanism that you have to turn to load a dose of medication.
Don't forget to do this every time you use your inhaler, otherwise you won't get any medication when you press the button. Some dry powder inhalers also require you to prime it by twisting the mechanism back and forth before loading the first dose. This is a one-time thing that you only have to do right before starting a brand new inhaler.
Shake Your Inhaler (for Pulse-Dose Inhalers)
Most pulse-dose inhalers also need a thorough shaking in order to work properly. This is a step that many patients forget or don't do thoroughly enough.
Make sure you shake your inhaler for the full length of time indicated in its instructions and avoid the temptation to rush. Some inhalers require a full thirty seconds to a minute of vigorous shaking before they are ready to use.
Attach your Spacer

If you need to use a spacer, don't forget to attach it to your inhaler's mouthpiece before you take your dose. Spacers are important because they help you time your inhalation correctly with the spray, and if you don't use it you may not get your full dose of medication.
Check for Grime and Debris

You never know when dust, dirt, or other particles may make it into your inhaler's mouthpiece—that is, not unless you look. That's why you're supposed to check your mouthpiece for grime and foreign particles before every single use.
This is also the reason that you should keep the protective outer cap on your inhaler at all times. If you remember to replace the cap immediately after every single use you'll be less likely to lose or misplace it, and your mouthpiece won't get as dirty over time.
Breathing in dust, dirt, or pollen that settles on your inhaler could irritate your lungs and make your COPD symptoms worse. You should also look out for sticky medication build-up, which can block the spray and make your inhaler less effective.
Most importantly, make sure you understand and follow the directions that come with your inhaler in their entirety without skipping any steps. Don't be afraid to ask your doctor to demonstrate how to prepare your inhaler or go over the instructions as many times as you need.
Hold Your Inhaler Upright
You should take care to hold your inhaler upright when you use it, especially during and after loading a new dose. This is especially important for dry powder inhalers; if the mouthpiece is turned sideways or upside-down any time during or after loading, you could lose some of the medication and get too small a dose.
Be careful to hold your inhaler straight up and down, not at an angle, when you take your dose. You should also make sure to position the inhaler correctly at your lips; leaning in too far can cause the spray of medication to land on your mouth or tongue, instead spraying straight down your throat.
Breathe Out Completely First
When you use your inhaler, you want the medication to make it all the way through your airways and deep into your lungs. This works best when you exhale first to clear your lungs of stale air before inhaling your medication.
Unfortunately, many patients skip this step either because they don't know or because they are in a hurry or forget. Other patients don't take the time to breathe out fully enough, leaving air in their lungs and airways when they take their dose.
However, it's important to make sure that you don't exhale into your inhaler when you breathe out, especially if you use a dry powder inhaler. Instead, turn your head to the side or tilt it up, away from your inhaler, before beginning to exhale.
Aim Your Inhaler Correctly
The primary purpose of an inhaler is to deliver your medication directly to your lungs and airways. This helps the medicine act quickly to reduce inflammation and respiratory symptoms at their source.
However, some people who use inhalers end up aiming the spray in the wrong place when they inhale. This causes the spray to mist your mouth or tongue, and less of the medication actually makes it down your throat.
That's why it's important to take your time and angle the mouthpiece correctly when you use your inhaler. If too much of it ends up in your mouth, you may not breathe in enough medication to receive the full dose you're supposed to take.
Always make sure you hold your inhaler upright and use your spacer if you have one. Do your best to aim the spray right at your throat so you can inhale as much of the spray as possible.
Use Proper Breathing Technique
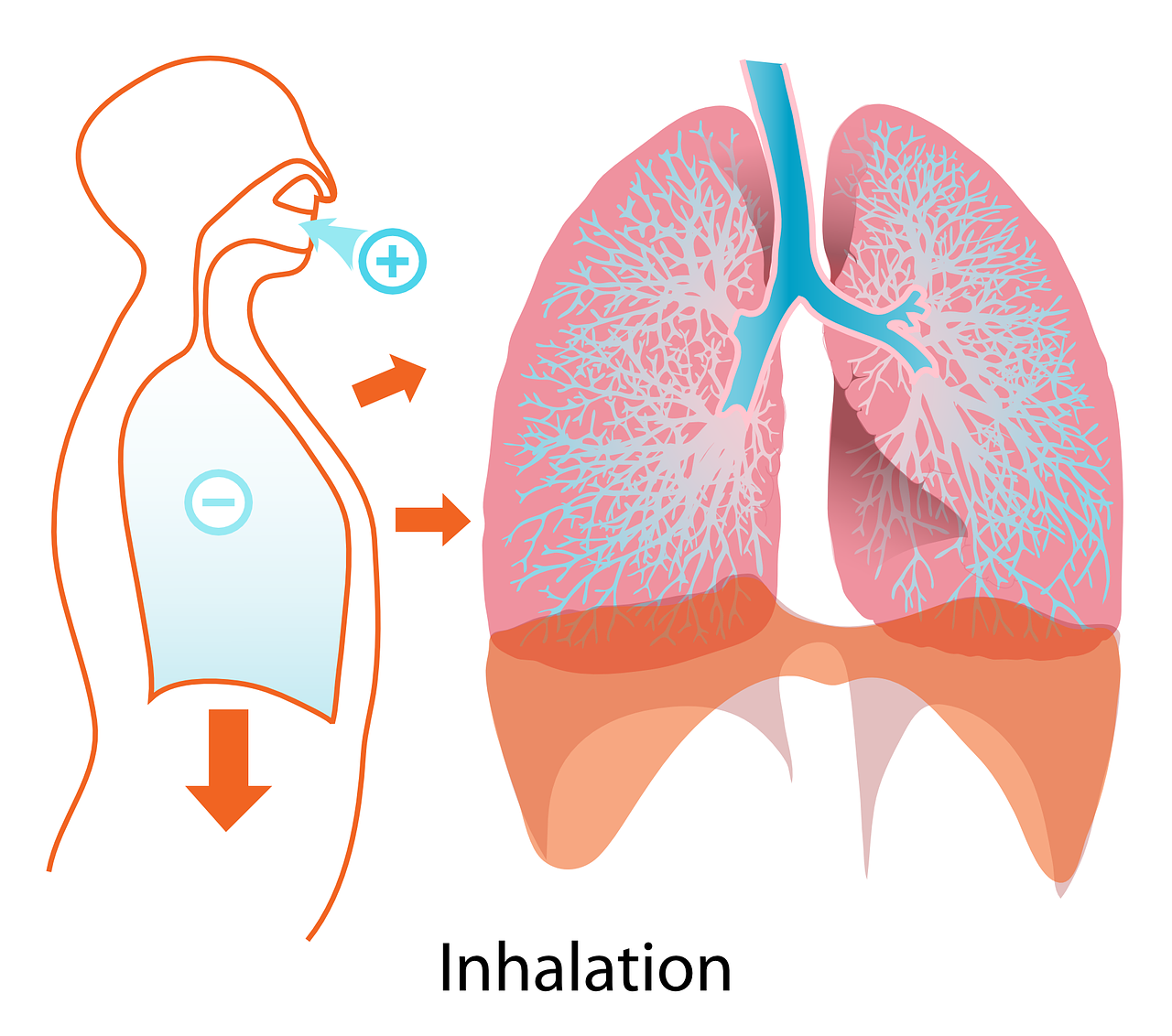 |
| Image courtesy of NIAID. |
Some patients get too little medicine from their inhaler because they don't use proper breathing technique when they take their doses. Some people inhale too quickly, too late, or don't breathe in forcefully enough to take in all the medicine.
When you use your inhaler, you should always take long, slow, deep breaths. If you have trouble with this because of your COPD, take the time to practice some breathing techniques like pursed-lips breathing to help you catch your breath before you take your dose.
To make sure you are inhaling at the correct time, start breathing in slowly just before you you press the button to release the dose. As the dose sprays, begin inhaling more deeply to pull the medicine into your lungs.
If you use a dry powder inhaler, you may have to inhale more forcefully to get the full dose of medication. If you have any trouble timing your inhalation correctly or breathing in deeply enough, talk to your doctor and demonstrate how you use your inhaler so he can help you hone your technique.

Don't Forget to Hold Your Breath

When you breathe in the medication from your inhaler, you should breathe slowly, deeply, and take in as much air as possible. Then, you are supposed to hold your breath to give the medication time to absorb.
This is a step that many patients tend to forget or cut short. You should hold your breath for ten full seconds, or as long as you can if you can't hold your breath for that long.
Holding your breath after using your inhaler is an important part of proper inhaler technique and is important for your medication to work effectively. If you are supposed to take a second dose, you should always wait thirty seconds to a minute (or whatever time is indicated in the instructions) after the first dose before using your inhaler again.
Rinse Out Your Mouth

Even when you use proper inhaler technique, a small amount of the medication inevitably ends up in your mouth instead of your airways. Certain medications, especially corticosteroids, can cause uncomfortable symptoms like mouth dryness and irritation when this happens.
This is important because a dry mouth is more than just uncomfortable; it can actually be bad for your health. When your mouth is dry too often, it creates opportunities for bacteria to grow, and can cause cavities, gingivitis, and even fungal infections in your mouth.
That's why many inhalers, especially steroid inhalers, include instructions to rinse out your mouth right after use. This washes any extra medicine off the surface of your mouth before it has a chance to absorb into the lining.
However, this only works if you wash your mouth out immediately after using your inhaler (and after holding your breath, of course). Even waiting 30 seconds to a minute too long may allow too much of the medication to absorb into your mouth.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
To help you with proper rinsing technique, use your inhaler in front of a sink and make sure you have a small cup of water at the ready. Then, after you use your inhaler, immediately take a large sip of water and swish it around your mouth.
After a few seconds, spit the water back out into the sink. As long as you rinsed your mouth out immediately, this should effectively get most of the medication out of your mouth and help you avoid dryness and irritation.
Never Use an Empty Inhaler
Some patients continue using their inhaler after it's run out of medication because they don't realize that it is empty. This can be very dangerous because you don't get the medication you need to manage your COPD.
Many types of inhalers have dose counters to help you tell when you've run out of doses. Make sure you always pay attention to this counter and start a new inhaler once it reaches zero, even if your inhaler still sprays.
Unfortunately, many metered dose inhalers do not have dose counters to tell you when they are empty. However, you can tell whether or not it is empty by listening for the sound of the medication inside when you shake it. You can also check by spraying the inhaler into the air; if you see a mist, then you know it isn't quite empty yet.
Practice in Front of Your Doctor

Medical experts recommend that doctors have their patients demonstrate using their inhaler in front of them at every doctor's visit. This allows doctors to catch and correct any mistakes and refresh their patients' knowledge of proper inhaler technique.
However, in practice, may doctors and patients get too comfortable and see this part of the examination as unnecessary. Inhaler demonstrations may also get skipped or overlooked when the patient forgets to bring their inhaler to the appointment.
Unfortunately, there is another deeper problem with doctors teaching proper inhaler use: Studies show that the majority of doctors themselves don't know how to follow the steps correctly. That's why it's important to work with a doctor whom you trust and who is thoroughly trained in how to use all the medications he prescribes. It may also be worthwhile to ask your doctor how confident he is about demonstrating proper inhaler technique and how recently he has refreshed his training.
To reduce the chances of error, you and your doctor could go over the detailed instructions that come with your inhaler together as you practice your technique. You can also talk to a licensed pharmacist at the pharmacy when you pick up your prescription; pharmacists are trained in how to use inhalers properly and should be able to show you how use yours right.
Know Your Medications
Managing all the medications you need to take every day is not always easy, especially if you have advanced COPD or suffer from another disease or condition. However, your medications are your lifeline, and it's vital to know each and every one of them and understand how they work.
You need to know your inhalers by more than just their color or brand; you should be able to name each medication and explain what it is for. If you need help, take some time to study the information packet that comes with your prescription or ask your doctor to explain.
You can also talk to your pharmacist if you have any questions about your medications or just need someone to explain them to you in more detail. Never be afraid to ask questions, even if you need to ask the same question more than once; it's easier to understand something when you hear it explained multiple ways.
Medicine and health is a complex topic, and it may take time some and patience to learn all that you need to about your disease and your medications. The more knowledge you have, the better you will be able to manage your disease and take an active role in your own health and treatment.
Here is an overview of some of the most common inhaled medications prescribed for COPD.
Short-acting Bronchodilators: Opens up your airways and makes it easier to breathe, often used in rescue inhalers for quick symptom relief.
- Albuterol
- Levalbuterol
- Ipratropium
- Proventil
Long-acting Bronchodilators: Often used in maintenance inhalers to manage daily,long-term symptoms.
- Aclidinium
- Almeterol
- Arformoterol
- Indacaterol
- Symbicort
- Spiriva
- Atrovent
- Brovana
- Arcapta Neohaler
- Tiotropium
Corticosteroids: Reduce inflammation and are often used to treat COPD exacerbations and daily symptoms.
- Pulmicort
- Fluticasone
- Budesonide
Combination bronchodilator inhalers: Contain a combination of two or more different bronchodilator medications.
- Combivent Respimat
Combination Bronchodilator and Steroid Inhalers: Contains a combined dose of at least one bronchodilator medication and one steroid medication.
- Advair
- Breo Ellipta
Take Your Medication in the Correct Order
![]()
Many patents, especially those with more severe symptoms, have to use more than one inhaler to manage their COPD. When this is the case, the order in which you use your inhalers can be very important and affect how well they work.
For example, many patients have two primary inhalers: a rescue inhaler (usually containing a short-acting bronchodilator) and a maintenance inhaler (often containing a different type of long-acting bronchodilator). Some patients also use steroid medication inhalers or combination inhalers with a mixture of bronchodilators and/or steroids.
Depending on your unique condition
Exercise is absolutely vital for healthy living, especially if you have COPD or another respiratory disease. But when you're hooked up to your oxygen tank or concentrator, it can make working out and doing other physical activities a little bit more tricky.
Fortunately, exercising with oxygen isn't too difficult if you know how to do it right. In fact, the extra oxygen you get should make it easier to exercise by improving your endurance and making it easier to breathe.
In this article, we're going to give you a variety of tips and techniques to help you better manage exercise while you're using supplemental oxygen. That way, you can continue living an active, healthy life without letting your disease or your oxygen therapy get in the way.
How Oxygen Helps You Exercise

Many patients with COPD and other breathing disorders use supplemental oxygen when they exercise, including those who use oxygen 24/7 to manage their disease. If you have mild COPD, your doctor might prescribe you oxygen specifically to use when you work out or do other activities that make you feel short of breath.
When you exercise, your body's oxygen needs go up as your muscles work hard to move your body. This forces your lungs to work harder, too, by taking more frequent breaths.
This is why physical activity can make you feel so short of breath when you have COPD. Because your lungs don't work as efficiently, they have trouble absorbing enough oxygen to keep up with your body's needs.
As a result, your blood oxygen levels can fall, causing you to feel short of breath. It can also trigger other COPD symptoms like coughing, wheezing, and fatigue.
That's where oxygen comes in: it allows your lungs to absorb more oxygen with every breath you take. This keeps your blood oxygen saturation at a healthy level, and it can be particularly helpful during exercise.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
By helping your lungs work more efficiently, supplemental oxygen makes it much easier to exercise and do other activities that put extra strain on your lungs. It can also reduce your respiratory symptoms and make it easier to breathe.
Overall, oxygen therapy allows you to do more physical activity for longer periods of time without feeling as breathless or fatigued. It also helps keep your heart healthy by reducing the strain that is caused when your blood oxygen levels fall too low.
Now that you understand why using your supplemental oxygen is so important, let's take a look at how to use it when you exercise. In the following sections, we'll give you a variety of practical tips and techniques you can use right away to work out more easily on oxygen.
How to Exercise with Oxygen

Getting used to moving around and working out on oxygen isn't exactly easy. Oxygen equipment can be bulky, unwieldy, and difficult to handle, especially during physical activity.
However, the limitations you face because of your oxygen will be different depending on what kind of oxygen supply you use. For example, using a portable oxygen concentrator gives you significantly more mobility than oxygen tanks and full-sized oxygen concentrators.
Luckily, there are many ways to work around the challenges of exercising with all your oxygen equipment in tow. In these next sections, we're going to show you a variety of techniques for working around your equipment and exercising safely and effectively on oxygen.
By learning how to manage your symptoms, your equipment, and find oxygen-friendly exercises, you'll find that you can do all kinds of physical activities while hooked up to your oxygen machine. We'll show you how to make oxygen therapy more comfortable and so you can reap the greatest possible benefits from your oxygen when you work out.
Take heart in the fact that there are many solutions for making oxygen therapy more comfortable and convenient, no matter what kind of physical activity you enjoy. Even though it may take some adjustments, you can make exercise happen, whether you use oxygen just occasionally or 24 hours a day.
Use a Portable Oxygen Concentrator

When you use an oxygen tank or full-sized concentrator, you have to deal with long extension tubes that connect you to the device, which may be several feet away or even in a different room. However, a portable oxygen concentrator is small enough to carry on your person, eliminating the hassle and danger of getting tripped up by long tubes.
Many portable concentrators only weigh a few pounds and are easy to wear on your back or sling over your shoulder. Because you're not tethered to a heavy oxygen machine, this gives you much more freedom and flexibility to move around.
Using a portable oxygen concentrator allows you to go on walks, do aerobic exercises, and all kinds of other activities without hauling or maneuvering around bulky equipment. It also makes it easier to go to the gym when you don't have to wheel a heavy oxygen tank around.

While portable oxygen concentrators can be pricey, they give you much more freedom to live every day to the fullest. Using a portable concentrator can significantly improve your quality of life and make it much easier to stay active while using oxygen.
While you can sometimes rent a portable oxygen concentrator from your oxygen supplier, you will likely need to finance at least some of the cost on your own. Luckily, there are many options for financial assistance and affordable monthly financing with low payments. Depending on your situation, you may even be able to get Medicare or your private insurance provider to cover some of the cost.
Investing in a portable oxygen concentrator if you can is well worth it; they are light, maneuverable, and can make exercising on oxygen much simpler. However, if that is not an option for you, then you can still do many kinds of exercises while using larger oxygen tanks and concentrators.
Double-Check Your Equipment Before Your Workout

When you are exerting yourself during exercise, it's especially important to make sure that your oxygen source is working properly. Otherwise, you risk getting too little oxygen, which makes it much more difficult to exercise.
Because exercise puts extra strain on your lungs, you are at a higher risk of your blood oxygen levels dropping when you work out, which is bad for your heart and lungs. Low blood oxygen makes it more difficult to breathe, makes you feel fatigued, and cause other dangerous symptoms.
To ensure you get enough oxygen, double check your nasal cannula, oxygen mask, and tubing to make sure they are properly attached to your oxygen source. If you are using an oxygen tank, check your pressure gauge to ensure that there is enough oxygen left to last you through your whole workout.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
If you are using a portable oxygen concentrator, then you should always make sure that it is fully charged before you start to work out. It's also a good idea to keep an extra charged battery nearby in case the first one runs out of charge.
You may also want to bring an extra nasal cannula with you just in case you need to switch it out. You can carry all the supplies you need in your portable oxygen concentrator carrying case or in a separate bag or backpack, if needed.
Secure Your Tubing

When you're moving around a lot during exercise, the tubing that connects you to your oxygen machine can be a huge pain to manage. However, it is much easier to keep the tubing out of the way if you fasten it down securely before you work out.
First, you will need to secure the tube that connects your oxygen mask or nasal cannula to the extension tubing. The simplest way to do this is with a clip, which you can use to hook the tube to your shirt or waistband.
You can do this with a large safety pin (being extremely careful not to pierce the tube) or, preferably, with a special tubing clip. Some patients find that clipping their tubing to the back of their shirt is the most effective technique for keeping it out of the way.
You can also thread your tubing underneath your shirt, which can help keep it away from your arms as you exercise. Don't be afraid to keep experimenting with different arrangements until you find a system that works for you.
Next, you will need to secure the long extension tubing that connects your nasal cannula to your oxygen source. Otherwise, you risk tripping over the tube as you move around the room during your workout.
To do this, think about the arrangement of the space you will be exercising in and how much room you need to move around. Try to string your extension tubing off to side or otherwise out of the way of the main space.
To keep your tubing off the ground, string it over a hook positioned several feet off the ground. This will keep the tube away from your feet and reduce your risk for trips and falls.

It's very important to take the time to arrange your equipment and tubing so it won't trip you up as you exercise. Otherwise, you risk damaging your equipment or causing serious injury to yourself if you fall.
If you use a portable oxygen concentrator, then you can avoid this problem altogether by wearing your oxygen source on your body. That way, you can move around freely without any long lengths of tubing to get in the way.
Another thing that can help is to use swivel connectors to connect your nasal cannula to your extension tubing and your extension tubing to your oxygen source. This makes it easier to adjust the position of your tubing and gives you a more flexible range of motion.
Use Cushions to Reduce Irritation
The tubing that contacts your face and loops over your ears can cause irritation over time as it touches your skin and moves around. Exercise can make this skin irritation worse by jostling your oxygen mask, nasal cannula, and tubing around even more.
If you don't use them already, you should consider getting ear cushions to protect your ears from the tubing as you work out. These little pieces of foam absorb the impact of tugging and rubbing and can significantly reduce ear pain caused by oxygen therapy.

You can also get cushions to go right under your nose to prevent chaffing from your nasal cannula. You can also get soft, fabric covers to wrap any other sections of tubing that tend to rub against your skin.
You can find practical solutions to remedy other oxygen therapy side-effects, too, including mouth and nasal dryness, skin irritation, and chronic ear pain. You will be surprised at how much more bearable oxygen therapy becomes once you've implemented some simple measures of comfort.
To learn more about how to make using oxygen more comfortable, check out our previous post here. This guide will introduce you to a variety of special equipment, practical techniques, and DIY fixes that can make you much more comfortable on oxygen.
Clear Your Airways
COPD often causes excess mucus to clog up your lungs and airways, which makes it more difficult to breathe. Nasal secretions can also affect your oxygen therapy by clogging and dirtying your nasal cannula and tubing.
To address both of these problems, you can take some time to clear excess mucus out of your airways before you work out. You can do this with simple techniques like huff coughing or postural drainage, which help move mucus up and out of your respiratory tract.
You can also use tools like a lung flute, which creates vibrations when you blow through it to help dislodge sticky mucus from the walls of your lungs and airways. High-frequency chest wall oscillation works in a similar way, but with a vibrating vest you wear over your chest.
Back and chest percussion is another way to dislodge extra mucus so you can cough it out of your lungs. To do this, you will need a partner to firmly, repeatedly tap on specific places on your back and chest.
While these techniques may not get rid of the mucus completely, they can get rid of a enough of it to make it easier to breathe. By clearing out space in your airways, it allows more air to flow through, and can reduce unwanted coughing when you're trying to work out.
You should also make sure to drink plenty of water every day to keep your mucus thin, which makes it much easier to clear out of your lungs and airways. And, because oxygen therapy can dry out your mouth and throat, staying hydrated can reduce these side-effects and make oxygen more comfortable to use.

You will also need to drink extra water when you exercise, especially if you sweat a lot or work out in warm temperatures. Keeping a water bottle with you when you do physical activities will help you stay hydrated and also combat dryness from your oxygen therapy.
For more tips on how to clear your airways, check out our comprehensive guide on mucus clearance techniques here. The guide covers all the most effective techniques for getting rid of excess mucus in more detail, including more detail on the methods we touched on here.
Find Exercises for Small Spaces

If you are hooked up to a large oxygen tank when you exercise, then you will have some limitations on how much you can move around. Even portable oxygen tanks and concentrators are sometimes too heavy for patients to lug around during fast-paced activities.
That's why it helps to find exercises that you can do while keeping your portable oxygen concentrator or oxygen tank on the ground nearby. These include exercises that allow you to stay stationary or only move within a small area so you can work out without having to move your tank or carry your portable oxygen concentrator around.
Some examples of activities that allow you to stay in one spot include jogging in place, using a stair step machine, or riding a stationary bicycle. Chair exercises are another great idea because you can sit in one spot with your oxygen source nearby and conserve energy while you build muscle tone.
Resistance bands and free weights are also great tools for building muscle while standing in place. If you have a gym membership, you can also use a variety of exercise machines that can help you maintain your balance and learn proper form.
All of these exercises are easier to do on oxygen because they keep you easily within the reach of your oxygen tubing. This allows you to set down your oxygen tank or concentrator nearby and more or less forget about it until it's time to move again.
Slower-paced activities like walking are also easier on oxygen, because they allow you to carry or wheel your oxygen tank or portable concentrator behind you as you go. You can also try yoga or tai chi, which are exercises made up of slow, fluid movements that are less likely to be hindered by your oxygen equipment.

Including these kinds of stationary and slow-paced exercises in your workout will free you from having to worry about re-arranging your tubing or lugging around your oxygen source while you're trying to focus on exercise. You'll find that working out is much more comfortable when your routine isn't constantly interrupted by having to move your equipment around.
Eat a Healthy Diet
Eating a well-balanced diet that's low in carbs is important for your lungs and can make it easier to exercise. As we've discussed on this blog before, eating too many carbohydrates is hard on your lungs, and can actually make it more difficult to breathe.
By eating a healthy diet, you ensure that your lungs have all the vitamins and nutrients they need to work as effectively as they can. By limiting how many carbs you eat, you can help your lungs work more efficiently, which can reduce how breathless you feel when you work out.

Healthy eating habits work in concert with your oxygen therapy to keep your blood oxygen levels up while you exercise. It can also help you stay more active, more healthy, and make a noticeable difference in your COPD symptoms.
Take Breaks When You Need To

Even if you use oxygen properly when you exercise, you might still struggle with breathlessness throughout your workout. If this happens, don't be afraid to slow down or take a break before continuing to exercise.
As long as you stick to a healthy exercise routine, it's okay to take it at your own pace. While you should try to do as much as you can, it's important not to push your body past its limits.
Talk to Your Doctor

As always, you should talk to your doctor before making any major changes to your activity level or workout routine. While most COPD patients are encouraged to stay as active as they can manage, some patients may have special conditions or limitations to consider.
Your doctor can tell you what kinds of activities are safe and if there are any kinds of exercises you should or should not do. Never hesitate to call or schedule an appointment with your doctor any time you have questions or concerns about your exercise routine or the symptoms you experience when you work out.
Other Tips for Exercising with COPD
Many people struggle to exercise because of their COPD symptoms, even when they use supplemental oxygen. Luckily, there are therapies and medications that can help you exercise more effectively while keeping your COPD symptoms under control.
For example, you can ask your doctor to refer you to a pulmonary rehabilitation class, which is a special program designed to help people with breathing disorders like COPD. Pulmonary rehabilitation teaches you how to better manage your symptoms and stay active through exercise classes and hands-on instruction.
Another thing you can do is practice breathing exercises, which can help you improve your breathing technique. By teaching you how to control your breath and push trapped air out of your lungs, breathing exercises can make it easier to breathe and easier to exercise without feeling short of breath.

It's also very important to always take your medication on time every day according to your COPD treatment plan. Some doctors also recommend using your bronchodilator medication before you exercise to make it easier to breathe.
Physical activity is important for your heart, your lungs, and your overall quality of life, which is why it's vital to stay active, even if you have to start small. If you struggle to exercise for any reason, talk to your doctor about what you can do to improve your symptoms and work out within your limitations.
For more tips on how to exercise with COPD, you might want to take a look at our article on Pulmonary Rehabilitation or our guide to Exercising at Home with COPD.
Conclusion
While oxygen can make exercise a little more complicated, there's no reason to let it get in the way of living an active life. If you remember the tips and tricks in this article, you should have no problem working out and staying active while using oxygen.
Whenever you get frustrated or discouraged, remember that your oxygen is your lifeline, and it can allow you to do more as you manage your COPD. Many people are able to live much healthier and active lives with oxygen, and you should think of it as an asset, not a hindrance.
Using oxygen is an adjustment at first, but it gets easier with time. It may take a little practice and patience, but soon you'll find that oxygen makes you even more capable of living the life you desire.
Whatever you do, don't give up on exercise and allow yourself to fall into a sedentary pattern. Take action and take charge of your health instead of letting COPD define and limit what you can do.
Remember that you are not alone in your struggles, and many oxygen patients are managing the same problems that you are every day. Remember that many of them successfully manage these problems and live active, fulfilling lives.
As long as you remain confident in your ability to manage your own health you can handle any challenges that come your way. If you stay motivated, stay active, and follow your COPD treatment plan, you'll be able to manage your COPD and keep your body strong.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!

















